Abstract
Background
Epidemiological studies suggest a low incidence of hot flashes in populations that consume dietary soy. The present study examined the effect of soy nuts on hot flashes and menopausal symptoms.
Methods
Sixty healthy postmenopausal women were randomized in a crossover design to a therapeutic lifestyle changes (TLC) diet alone and a TLC diet of similar energy, fat, and protein content in which one-half cup soy nuts divided into three or four portions spaced throughout the day (containing 25 g soy protein and 101 mg aglycone isoflavones) replaced 25 g of nonsoy protein. During each 8-week diet period, subjects recorded the number of hot flashes and amount of exercise daily. At the end of each 8-week diet period, subjects filled out the menopausal symptom quality of life questionnaire.
Results
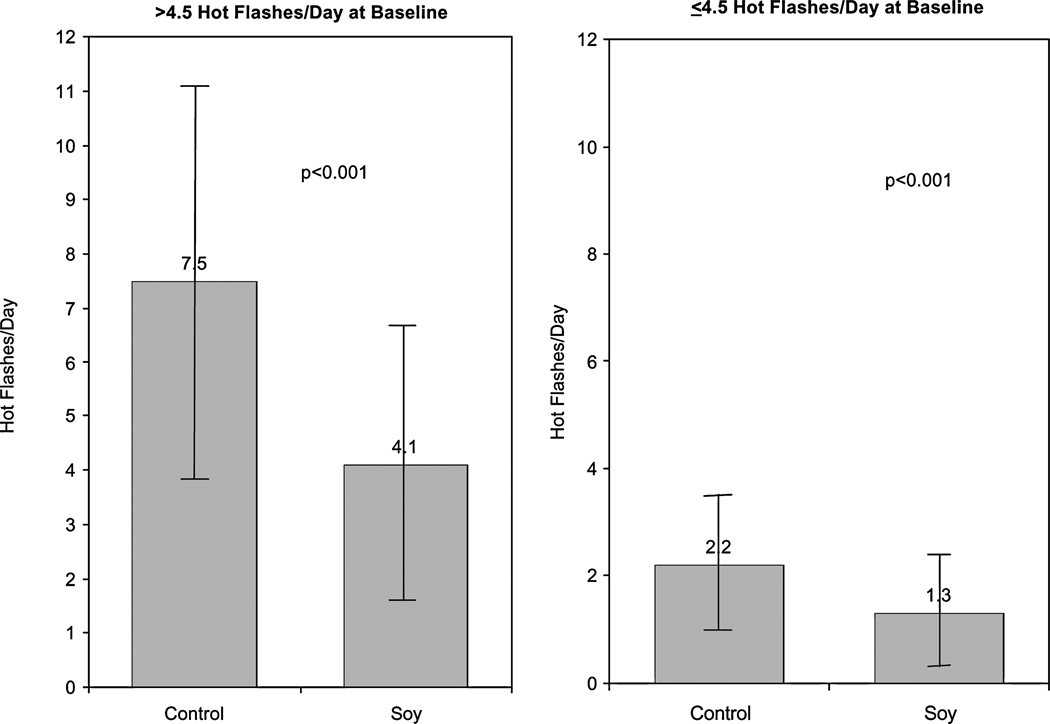
Compared to the TLC diet alone, the TLC diet plus soy nuts was associated with a 45% decrease in hot flashes (7.5 ± 3.6 vs. 4.1 ± 2.6 hot flashes day, respectively, p < 0.001) in women with >4.5 hot flashes/day at baseline and 41% in those with ≤4.5 hot flashes/day (2.2 ± 1.2 vs. 1.3 ± 1.1, respectively, p < 0.001). Soy nut intake was also associated with significant improvement in scores on the menopausal symptom quality of life questionnaire: 19% decrease in vasomotor score (p = 0.004), 12.9% reduction in psychosocial score (p = 0.01), 9.7% decrease in physical score (p = 0.045), and a trend toward improvement in the sexual score, with a 17.7% reduction in symptoms (p = 0.129). The amount of exercise had no effect on hot flash reduction.
Conclusions
Substituting soy nuts for nonsoy protein in a TLC diet and consumed three or four times throughout the day is associated with a decrease in hot flashes and improvement in menopausal symptoms.
INTRODUCTION
Hot flashes can interfere with normal lifestyle and disrupt sleep; therefore, modalities that decrease their frequency and severity are important. Estrogen and combined estrogen plus progestin have been the most successful therapies to reduce hot flashes in postmenopausal women. Until recently, hormone replacement therapy (HRT) was prescribed by many physicians not only for hot flashes but also to prevent coronary heart disease (CHD) in women. This practice was based on the fact that premenopausal women have lower rates of CHD than postmenopausal women at every age,1 a finding suggesting that endogenous estrogen may account for this protection and that HRT may prevent CHD. However, results from recent randomized trial data have not supported a cardioprotective benefit with HRT.2–13 In the Women’s Health Initiative (WHI) Study Group of 16,608 women without cardiovascular disease (CVD), those randomized to estrogen plus progestin (Prempro; Wyeth, Madison, NJ) had an increased risk of 26% for breast cancer (95% CI, 1.00–1.59), 29% for myocardial infarction (MI) (95% CI, 1.02–1.63), 41% for stroke (95% CI, 1.07–1.85), 207% for deep venous thrombosis (DVT) (95% CI, 1.49–2.87), and 213% for pulmonary embolus (95% CI, 1.39–3.25).12 The highest CVD risk was in the 50–59-year-old cohort. The estrogen replacement therapy (ERT) only arm was terminated prematurely because of a 39% increased risk of stroke (95% CI, 1.10–1.77).2 Because of these potential harmful effects, alternatives to ERT and HRT are being sought.
The prevalence of hot flashes is much lower in Asian than in Western countries; 10%–25% of Chinese women and 10%–20% of Indonesian women have hot flashes compared with 58%–93% of western women.14 These findings are thought, at least in part, to be related to consumption of a soy phytoestrogen-rich diet.15,16 The average daily soybean intake is 17–36 g in Japan, Korea, Taiwan, and Indonesia compared with 4 g in the United States.17 Consumption of soy has resulted in variable levels of relief from hot flashes in clinical trials.18 This variation may be related to the amount of soy protein or isoflavones consumed in the study diet. Most studies have used tablets of isoflavone extracted from soy or isolated soy protein in once-daily dosing. Very few studies have used native forms of soy. Exercise is also considered to have some efficacy for alleviating mild hot flashes and is advocated by the North American Menopause Society.19
The current study examined the effect of a native form of soy, soy nuts (which are roasted soybeans), added to the therapeutic lifestyle changes (TLC) diet (currently recommended by the Adult Treatment Panel of the National Cholesterol Education Program to lower risk of CHD)20 on hot flashes and menopausal symptoms in a randomized, crossover trial of 60 postmenopausal women over an 8-week period. Our objectives were to determine if dietary soy decreased hot flashes and improved menopausal symptoms.
MATERIALS AND METHODS
Subjects
Women with absence of menses for at least 12 months or irregular periods and hot flashes were recruited. Exclusion criteria were current cigarette smoking or smoking over the prior year, clinical coronary artery disease (CAD), peripheral artery disease or cerebrovascular disease, known diabetes or fasting glucose ≥ 126 mg/dL, history of breast cancer, fasting triglycerides > 400 mg/dL, systolic BP ≥ 165 or diastolic BP ≥ 100 mm Hg or both, untreated hypothyroidism, systemic or endocrine disease known to affect lipid, mineral, or bone metabolism, or > 21 alcoholic drinks per week. All lipid-lowering drugs, HRT, medications for osteoporosis, and soy products were discontinued for 2 months before entering the study. Subjects took a multivitamin but no additional vitamin or mineral supplements or other soy products during the study. The Institutional Review Board of the Beth Israel Deaconess Medical Center approved the protocol, and all subjects gave informed consent.
Study design and diets
This was a randomized, controlled, crossover trial of the effect of one-half cup soy nuts daily for 8 weeks on systolic and diastolic BP and lipid levels in 60 postmenopausal women. A registered dietitian instructed subjects to eat a TLC diet, which consisted of 30% of energy from total fat (≤ 7% saturated fat, 12% monounsaturated fat, and 11% polyunsaturated fat), 15% of energy from protein, 55% from carbohydrate, < 200 mg cholesterol/day,20 1200 mg calcium, and two fatty fish meals per week. Hypertensive women were counseled to limit sodium intake to < 2 g daily. Those ingesting suboptimal dietary calcium were given calcium carbonate supplementation.
After a 4-week diet run-in, those adherent to the TLC diet (from review of two 3-day food records) were randomized in a crossover design between two diet sequences for 8-week periods: the TLC diet without soy or the TLC diet with prepackaged daily allowances of one-half cup unsalted soy nuts (Genisoy, Fairfield, CA) (containing 25 g soy protein and 101 mg aglycone isoflavones: 61 mg genistein, 30 mg daidzein, 10 mg glycitein) divided into three or four portions spaced throughout the day. After a 4-week washout on the TLC diet alone, subjects crossed over to the other arm for an additional 8 weeks. Subjects were individually advised from which sources to decrease their protein intake to compensate for the 25 g soy protein on the soy arm in order to keep the protein amount similar on both diet arms. At the end of each 8-week period, fasting blood was drawn for lipid levels, and subjects collected a 24-hour urine for isoflavone and creatinine levels.
Urine isoflavone measurements
Isoflavones and metabolites in 24-hour urine samples were analyzed using high performance liquid chromatography (HPLC) with electrochemical detection based on the methods described by the ESA Company (Chelmsford, MA).21,22 The concentrations of isoflavones and metabolites were quantitated using standard curve methods. The detection limits are typically 30–50 femtomoles. Response is linear over at least 3 orders of magnitude (100 fmole–40 pmole) for all analytes studied. Intraassay precision, as percent relative standard deviation (SD), ranged from 1.7% to 10.2%. Urinary isoflavones were expressed as µg/mg creatinine. An equol producer is defined as >1000 nmol/L equol (a metabolite of daidzein) in the urine.23,24
Hot flash and menopausal symptom analysis
Subjects recorded the number of hot flashes daily on monthly calendars. These were averaged over each 8-week diet arm (TLC with soy nuts [soy] and TLC without soy nuts [control]). The baseline number of hot flashes was the average number of hot flashes/day during the control diet arm. Women were divided into low (≤4.5 hot flashes/day) and high (>4.5 hot flashes/day) hot flash groups based on the average number of hot flashes/day during the control diet arm (baseline). At the end of each 8-week period, subjects also completed the Menopause-Specific Quality of Life Questionnaire, which includes vasomotor, psychosocial, physical, and sexual scores.25 Women having no hot flashes were not included in the hot flash analysis, but they were included in the menopausal symptom questionnaire analysis.
Dietary analysis
Nutrient intake was assessed from three sets of 3-day food records (with 1 day being a weekend day) for each diet arm using Nutritionist V, version 3.0 software (N-Squared Computing, Salem Park, OR).
Exercise
At the screening visit, study subjects were counseled to adhere to their current exercise regimen (if active exercisers) or to walk 30 minutes daily if sedentary. During the 4-week run-in and both diet arms, the number of minutes of exercise performed daily was recorded. At randomization (visit 2), women were counseled not to change their exercise throughout the remainder of the study to prevent a confounding effect of weight change or exercise on study results.
Statistical analysis
Results are expressed as mean (SD. Continuous variables were compared with a two-tailed paired t test. To determine if there was a carryover effect from the order of diets for the two-period crossover design, a repeated-measures analysis of variation (ANOVA) with order and treatment as independent variables and outcome as the dependent variable was performed. Pearson’s correlation coefficients were used to assess relationships between continuous variables. A p value < 0.05 was considered significant.
RESULTS
Telephone screens were performed on 197 women. Of 82 subjects enrolled in the study after the run-in period, 22 (25%) dropped out. Reasons for dropouts included flatulence and bloating (3), constipation (1), teeth problems (1), intolerable hot flashes off HRT or soy (4), did not want to be off soy in control arm (1), family death or ill family member (3), work conflict (2), vacation conflict (2), pregnancy (1), entered raloxifene study (1), weight gain (1), started statin drug (1), and lost job and moved (1).
Of the 60 who finished, 39 women had hot flashes. Because initial hot flash frequency may affect the response to soy,18 the women were separated into two groups based on average number of daily hot flashes in the control diet arm, a high hot flash group (>4.5 hot flashes/day) and a low hot flash group (≤4.5 hot flashes/day). Table 1 shows the baseline characteristics by hot flash frequency. Women with > 4.5 hot flashes/day had a significantly lower body mass index (BMI) than women with ≤ 4.5 hot flashes/day; otherwise, there were no significant differences.
Table 1.
Baseline characteristics by hot flash status
| Characteristic | ≤4.5 Hot flashes | >4.5 Hot flashes | p value |
|---|---|---|---|
| Number of subjects | 24 | 15 | |
| Age, years | 51.9 ± 5.5a | 54.6 ± 5.4 | 0.14 |
| BMI (kg/m2) | 27.9 ± 5.5 | 23.9 ± 4.0 | 0.023 |
| Years postmenopause | 3.8 ± 4.2 | 6.1 ± 5.7 | 0.16 |
| Total C (mg/dL) | 227 ± 50 | 222 ± 30 | 0.70 |
| LDL-C (mg/dL) | 140 ± 41 | 136 ± 27 | 0.63 |
| HDL-C (mg/dL) | 58 ± 12 | 57 ± 16 | 0.94 |
| Triglyceride (mg/dL) | 135 ± 78 | 132 ± 104 | 0.91 |
Mean ± SD.
BMI, body mass index (calculated as weight in kilograms divided by the square of height in meters); C, cholesterol; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Urinary isoflavone levels were measured to assess compliance and were significantly higher on the soy arm compared with the control arm for daidzein, genistein, equol, and glycitein (Table 2). Levels of enterolactone, a lignan phytoestrogen found in fruits and vegetables,26 were similar in the control and soy arms, a finding suggesting that fruit and vegetable intake was similar on soy and control arms.
Table 2.
Isoflavone concentrations in control vs. soy diet arms by hot flash status
| ≤4.5 Hot flashes | >4.5 Hot flashes | |||||
|---|---|---|---|---|---|---|
| Control | Soy | p value | Control | Soy | p value | |
| Diadzein (µg/mg Cr)b | 0.14 ± 0.18a | 16.3 ± 9.4 | <0.001 | 0.24 ± 0.26 | 22.8 ± 18.0 | <0.001 |
| Genistein (µg/mg Cr) | 0.13 ± 0.43 | 4.1 ± 3.7 | <0.001 | 0.19 ± 0.33 | 5.8 ± 5.8 | 0.002 |
| Equol (µg/mg Cr) | 0.02 ± 0.12 | 4.6 ± 6.7 | 0.003 | 0.04 ± 0.12 | 7.3 ± 8.0 | 0.007 |
| Glycitein (µg/mg Cr) | 0.23 ± 0.82 | 1.3 ± 0.8 | 0.001 | 0.02 ± 0.03 | 1.7 ± 1.1 | <0.001 |
| Enterolactone (µg/mg Cr) | 2.5 ± 6.0 | 2.0 ± 2.8 | 0.522 | 2.0 ± 2.2 | 3.2 ± 5.3 | 0.47 |
Values are mean ± SD.
Cr, creatinine.
Diet composition (other than the soy nuts) did not significantly differ on the control vs. the soy arm for either hot flash group except for total fat in the low hot flash group (Table 3). Compliance was achieved with < 200 mg cholesterol/day on each diet arm and close to goal (7%) for saturated fat.
Table 3.
Dietary intake in control vs. soy diet arms by hot flash status
| ≤4.5 Hot flashes | >4.5 Hot flashes | |||||
|---|---|---|---|---|---|---|
| Control | Soy | p value | Control | Soy | p value | |
| kcala | 1451 ± 271b | 1406 ± 396 | 0.148 | 1329 ± 266 | 1318 ± 190 | 0.850 |
| Total fat (%) | 25.1 ± 4.8 | 22.0 ± 7.9 | 0.04 | 27.7 ± 8.1 | 25.8 ± 7.8 | 0.887 |
| Saturated fat (%) | 8.2 ± 1.9 | 7.7 ± 2.9 | 0.211 | 9.4 ± 4.2 | 7.3 ± 2.3 | 0.242 |
| Monounsaturated fat (%) | 7.8 ± 2.5 | 7.3 ± 2.2 | 0.107 | 9.0 ± 3.7 | 8.5 ± 3.0 | 0.830 |
| Polyunsaturated fat (%) | 4.7 ± 1.9 | 4.6 ± 1.8 | 0.506 | 5.9 ± 2.6 | 6.0 ± 2.7 | 0.455 |
| Protein (%) | 17.7 ± 2.9 | 17.9 ± 3.7 | 0.550 | 16.8 ± 4.5 | 15.9 ± 3.4 | 0.238 |
| Carbohydrate (%) | 54.2 ± 6.4 | 54.9 ± 9.1 | 0.463 | 51.8 ± 7.4 | 54.4 ± 6.7 | 0.494 |
| Cholesterol (%) | 154 ± 49 | 154 ± 93 | 0.18 | 156 ± 50 | 140 ± 59 | 0.447 |
kcals, kilocalories.
Values are mean ± SD.
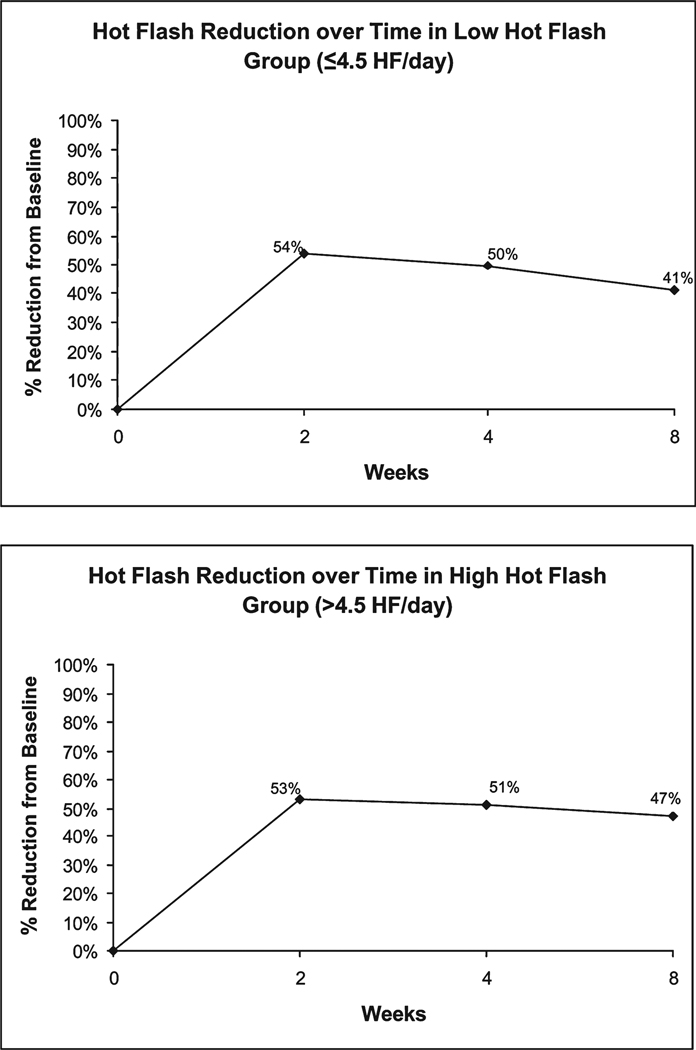
The average number of hot flashes during the first week in the control diet was 22.3 ± 24.9 compared with 23.3 ± 23.5 during the last week of the control diet. Therefore, hot flashes did not decrease in the control group. Compared with the control diet arm, soy nut ingestion was associated with a 45% decrease in hot flashes in women with >4.5 hot flashes/day at baseline (7.5 ± 3.6 vs. 4.1 ± 2.6, respectively, p < 0.001) and a 41% decrease in those with ≤4.5 hot flashes/day (2.2 ± 1.2 vs. 1.3 ± 1.1, respectively, p < 0.001) (Fig. 1). Both equol producers and nonproducers had similar reductions in hot flashes with soy nuts compared with the control diet (44%, p < 0.017 for both groups). The reduction in hot flashes was apparent at 2 weeks of treatment in both groups (53% and 54%, respectively) (Fig. 2). There appeared to be some attenuation in the benefit of soy nuts over time in the low hot flash group. A longer duration study with soy nuts would be necessary to confirm this.
FIG. 1.
Average number of hot flashes/day during each 8-week diet—TLC plus soy (Soy) and TLC without soy (Control)—in women divided into two groups based on the average number of daily hot flashes in the control (baseline) diet arm: > 4.5 hot flashes (left) and ≤ 4.5 hot flashes per day (right). Data are presented as mean with SD bars.
FIG. 2.
Percent reduction from baseline in hot flashes at 2, 4, and 8 weeks of treatment in soy diet arm compared with control arm in women with < 4.5 hot flashes/day (top) and > 4.5 hot flashes/day (bottom).
Compared to the control arm, soy nut ingestion was associated with significant improvement in scores on the menopausal symptom quality of life questionnaire: 19% decrease in vasomotor score (p = 0.004), 12.9% reduction in psychosocial score (p = 0.01), and 9.7% decrease in physical score (p = 0.045) after 8 weeks of ingestion. There was a trend toward improvement in the sexual score, with a 17.7% reduction in symptoms (p = 0.129).
The reduction in hot flashes with soy nuts was compared by quintiles of exercise based on average minutes of exercise per week to test the hypothesis that those who exercised more may have greater reductions in hot flashes. No significant differences in baseline characteristics were observed among the five exercise groups (Table 4). As shown in Table 5, those in the lowest exercise group (0–30 minutes/week) had a similar reduction in hot flashes with soy (56%) compared with those in the highest quintile (>276 minutes/week) (57%). Therefore, amount of exercise did not appear to affect hot flash reductions with soy.
Table 4.
Baseline characteristics stratified by minutes of exercise per week
| 1 0–29 minutes |
2 30–90 minutes |
3 91–179 minutes |
4 180–275 minutes |
5 276+ minutes |
|
|---|---|---|---|---|---|
| Number of subjects | 11 | 6 | 11 | 5 | 6 |
| Age, years | 52.3 ± 6.8a | 54.2 ± 3.1 | 51.9 ± 6.1 | 52.4 ± 5.2 | 55.4 ± 5.1 |
| BMI (kg/m2)b | 27.5 ± 7.6 | 26.0 ± 4.5 | 27.8 ± 4.3 | 22.8 ± 03.9 | 24.9 ± 4.2 |
| Years postmenopause | 4.1 ± 5.1 | 3.7 ± 5.4 | 3.7 ± 3.4 | 8.1 ± 6.0 | 5.7 ± 6.3 |
| Average minutes exercise per week | 6 ± 11 | 61 ± 20 | 123 ± 25 | 235 ± 18 | 349 ± 61 |
Values are mean ± SD.
BMI, body mass index (calculated as weight in kilograms divided by the square of height in meters).
Table 5.
Percent reduction in hot flashes stratified by minutes of exercise per week
| 1 (n = 11) 0–29 minutes |
2 (n = 6) 30–90 minutes |
3 (n = 11) 91–179 minutes |
4 (n = 5) 180–275 minutes |
5 (n = 6) 276+ minutes |
|
|---|---|---|---|---|---|
| Control | 4.1 ± 3.0a | 5.3 ± 7.2 | 3.2 ± 1.9 | 3.6 ± 2.4 | 6.1 ± 2.4 |
| Soy | 1.8 ± 2.1 | 3.2 ± 4.2 | 2.2 ± 1.5 | 2.6 ± 2.1 | 2.6 ± 1.6 |
| % reduction | 56 | 40 | 31 | 28 | 57 |
| p value | 0.012 | 0.147 | 0.001 | 0.058 | 0.034 |
Values are mean ± SD.
DISCUSSION
In this randomized, controlled, crossover trial in postmenopausal women, ingestion of soy nuts containing 25 g soy protein and 101 mg aglycone isoflavones was associated with a decrease in hot flashes and menopausal symptoms in postmenopausal women compared with the TLC diet without soy. Similar reductions were seen in women experiencing both >4.5 hot flashes per day and ≤4.5 hot flashes per day. Therefore, the initial baseline frequency of hot flashes had no effect on efficacy in the current study. This benefit may be of interest to symptomatic postmenopausal women, as estrogen/progestin replacement increased the risk of MI, stroke, breast cancer, and dementia and estrogen alone increased the risk of stroke and dementia in clinical trials.2,3
Prior studies have shown variable reductions in menopausal symptoms with soy preparations.18,27–29 Ten studies have compared soy foods, soy beverage, or soy powder with placebo or control.27 Of eight trials examining hot flash frequency, seven observed no improvement compared with control. Nine trials (two in abstract only) compared soy-derived isoflavones in capsule or tablet form with placebo. Of five published trials examining hot flash frequency, two observed a significant reduction in hot flashes on soy compared with placebo,30,31 whereas three found no difference.32–34
Soy nut ingestion was also associated with a decrease in menopausal symptoms as measured by the Menopause-Specific Quality of Life Questionnaire in the current study. Seven prior trials have reported symptom outcome, with each trial using a different questionnaire.27 None of the trials observed a significant improvement in overall score. Only one trial observed improvement in subscale scores on the soy diet compared with placebo; Washburn et al.35 found that 20 g soy protein with 34 mg isoflavones twice daily improved hot flash severity compared with carbohydrate placebo (p < 0.001).
We may have achieved greater relief from hot flashes and menopausal symptoms relative to other trials, most of which used isoflavone tablets or isolated soy protein products, because we used a native form of soy, which has all active ingredients and a high ratio of isoflavones/protein. Furthermore, the consumption of native soy at three or four times throughout the day in the current study (done to mimic Asian populations who consume soy throughout the day) may have kept isoflavone levels more constant and may be another reason for significant menopausal symptom relief in the current study. It should be noted that because the study was not blinded, the reduction in hot flashes could have been due to a placebo effect. Even if this is the case, a near 50% reduction in hot flashes was beneficial to the women, as reflected by the improvement in scores on the Menopause-Specific Quality of Life Questionnaire.
The current study is the first, to our knowledge, to examine the effect of exercise in combination with soy on hot flash reduction. When this was stratified by minutes of exercise per week, we did not find a greater reduction in hot flashes with soy in women who exercised more, but the sample size within groups was small; therefore, these results should be viewed with caution.
In conclusion, soy nut ingestion was associated with a significant decrease in hot flashes and menopausal symptoms in postmenopausal women. In contrast to most other soy studies, we used a lower amount of native soy protein, 25 g, which is more feasible to incorporate into the diet in populations unaccustomed to consuming soy. Our study was done in the free-living state; therefore, dietary soy may be a practical, safe, and inexpensive modality to reduce menopausal symptoms on a population basis.
ACKNOWLEDGMENT
We are grateful to the study subjects for their time and to Genisoy for donating the soy nuts.
The study was funded by the Harvard Medical School’s Center of Excellence in Women’s Health (National Institutes of Health), contract 00T002244 from the Office in Women’s Health, Department of Health and Human Services, and supported in part by grant RR 01032 to the Beth Israel Deaconess Medical Center General Clinical Research Center from the National Institutes of Health.
REFERENCES
- 1.Colditz GA, Willett WC, Stampfer MJ, Rosner B, Speizer FE, Hennekens CH. Menopause and the risk of coronary heart disease in women. N Engl J Med. 1987;316:1105. doi: 10.1056/NEJM198704303161801. [DOI] [PubMed] [Google Scholar]
- 2.Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: The Women’s Health Initiative randomized controlled trial. JAMA. 2004;291:1701. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 3.Welty FK. Alternative hormone replacement regimens: Is there a need for further clinical trials? Curr Opin Lipidology. 2003;14:585. doi: 10.1097/00041433-200312000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA. 1998;280:605. doi: 10.1001/jama.280.7.605. [DOI] [PubMed] [Google Scholar]
- 5.Grady D, Herrington D, Bittner V, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II) JAMA. 2002;288:49. doi: 10.1001/jama.288.1.49. [DOI] [PubMed] [Google Scholar]
- 6.Simon JA, Hsia J, Cauley JA, et al. Postmenopausal hormone therapy and risk of stroke: The Heart and Estrogen-progestin Replacement Study (HERS) Circulation. 2001;103:638. doi: 10.1161/01.cir.103.5.638. [DOI] [PubMed] [Google Scholar]
- 7.Herrington DM, Reboussin DM, Brosnihan KB, et al. Effects of estrogen replacement on the progression of coronary artery atherosclerosis. N Engl J Med. 2000;343:522. doi: 10.1056/NEJM200008243430801. [DOI] [PubMed] [Google Scholar]
- 8.Viscoli CM, Brass LM, Kernan WN, Sarrel PM, Suissa S, Horwitz RI. A clinical trial of estrogen replacement therapy after ischemic stroke. N Engl J Med. 2001;345:1243. doi: 10.1056/NEJMoa010534. [DOI] [PubMed] [Google Scholar]
- 9.Waters DD, Alderman EL, Hsia J, et al. Effects of hormone replacement therapy and antioxidant vitamin supplements on coronary atherosclerosis in postmenopausal women: A randomized controlled trial. JAMA. 2002;288:2432. doi: 10.1001/jama.288.19.2432. [DOI] [PubMed] [Google Scholar]
- 10.Clarke SC, Kelleher J, Lloyd-Jones H, Slack M, Schofiel PM. A study of hormone replacement therapy in postmenopausal women with ischaemic heart disease: The Papworth HRT atherosclerosis study. BJOG. 2002;109:1056. doi: 10.1111/j.1471-0528.2002.01544.x. [DOI] [PubMed] [Google Scholar]
- 11.Angerer P, Stork S, Kothny W, Schmitt P, von Schacky C. Effect of oral postmenopausal hormone replacement on progression of atherosclerosis: A randomized, controlled trial. Arterioscler Thromb Vasc Biol. 2001;21:262. doi: 10.1161/01.atv.21.2.262. [DOI] [PubMed] [Google Scholar]
- 12.Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 13.Hodis HN, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis: A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2001;135:939. doi: 10.7326/0003-4819-135-11-200112040-00005. [DOI] [PubMed] [Google Scholar]
- 14.Kronenberg F. Hot flashes. In: Lobo RA, editor. Treatment of the postmenopausal woman. Basic and clinical aspects. Philadelphia: Lippincott Williams & Wilkins; 1999. p. 157. [Google Scholar]
- 15.Tham DM, Gardner CD, Haskell WL. Potential health benefits of dietary phytoestrogens: A review of the clinical, epidemiological, and mechanistic evidence. J Clin Endocrinol Metab. 1998;83:2223. doi: 10.1210/jcem.83.7.4752. [DOI] [PubMed] [Google Scholar]
- 16.Beaglehole R. International trends in coronary heart disease mortality, morbidity, and risk factors. Epidemiol Rev. 1990;12:1. doi: 10.1093/oxfordjournals.epirev.a036048. [DOI] [PubMed] [Google Scholar]
- 17.Shu XO, Jin F, Dai Q, et al. Soyfood intake during adolescence and subsequent risk of breast cancer among Chinese women. Cancer Epidemiol Biomarkers Prev. 2001;10:483. [PubMed] [Google Scholar]
- 18.Messina M, Hughes C. Efficacy of soyfoods and soybean isoflavone supplements for alleviating menopausal symptoms is positively related to initial hot flush frequency. J Med Food. 2003;6:1. doi: 10.1089/109662003765184697. [DOI] [PubMed] [Google Scholar]
- 19.North American Menopause Society. Treatment of menopause-associated vasomotor symptoms position statement of The North American Menopause Society. Menopause. 2004;11:11. doi: 10.1097/01.GME.0000108177.85442.71. [DOI] [PubMed] [Google Scholar]
- 20.Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 21.Gamache PH, Acworth IN. Analysis of phytoestrogens and polyphenols in plasma, tissue, and urine using HPLC with coulometric array detection. Proc Soc Exp Biol Med. 1998;217:274. doi: 10.3181/00379727-217-44232. [DOI] [PubMed] [Google Scholar]
- 22.Nurmi T, Adlercreutz H. Sensitive high-performance liquid chromatographic method for profiling phytoestrogens using coulometric electrode array detection: Application to plasma analysis. Anal Biochem. 1999;274:110. doi: 10.1006/abio.1999.4247. [DOI] [PubMed] [Google Scholar]
- 23.Lampe JW, Karr SC, Hutchins AM, Slavin JL. Urinary equol excretion with a soy challenge: Influence of habitual diet. Proc Soc Exp Biol Med. 1998;217:335. doi: 10.3181/00379727-217-44241. [DOI] [PubMed] [Google Scholar]
- 24.Rowland IR, Wiseman H, Sanders TA, Adlercreutz H, Bowey EA. Interindividual variation in metabolism of soy isoflavones and lignans: Influence of habitual diet on equol production by the gut flora. Nutr Cancer. 2000;36:27. doi: 10.1207/S15327914NC3601_5. [DOI] [PubMed] [Google Scholar]
- 25.Hilditch JR, Lewis J, Peter A, et al. A menopause-specific quality of life questionnaire: Development and psychometric properties. Maturitas. 1996;24:161. doi: 10.1016/s0378-5122(96)82006-8. [DOI] [PubMed] [Google Scholar]
- 26.Lampe JW. Isoflavonoid and lignan phytoestrogens as dietary biomarkers. J Nutr. 2003;133:956S. doi: 10.1093/jn/133.3.956S. [DOI] [PubMed] [Google Scholar]
- 27.Krebs EE, Ensrud KE, MacDonald R, Wilt TJ. Phytoestrogens for treatment of menopausal symptoms: A systematic review. Obstet Gynecol. 2004;104:824. doi: 10.1097/01.AOG.0000140688.71638.d3. [DOI] [PubMed] [Google Scholar]
- 28.Haimov-Kochman R, Hochner-Celnikie D. Hot flashes revisited: Pharmacological and herbal options for hot flashes management. What does the evidence tell us? Acta Obstet Gynecol Scand. 2005;84:972. doi: 10.1111/j.0001-6349.2005.00769.x. [DOI] [PubMed] [Google Scholar]
- 29.Geller SE, Studee L. Botanical and dietary supplements for menopausal symptoms: What works, what does not. J Womens Health. 2005;14:634. doi: 10.1089/jwh.2005.14.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faure ED, Chantre P, Mares P. Effects of a standardized soy extract on hot flushes: A multicenter, double-blind, randomized, placebo-controlled study. Menopause. 2002;9:329. doi: 10.1097/00042192-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Han KK, Soares JM, Jr, Haidar MA, de Lima GR, Baracat EC. Benefits of soy isoflavone therapeutic regimen on menopausal symptoms. Obstet Gynecol. 2002;99:389. doi: 10.1016/s0029-7844(01)01744-6. [DOI] [PubMed] [Google Scholar]
- 32.Penotti M, Fabio E, Modena AB, Rinaldi M, Omeodei U, Vigano P. Effect of soy-derived isoflavones on hot flushes, endometrial thickness, and the pulsatility index of the uterine and cerebral arteries. Fertil Steril. 2003;79:1112. doi: 10.1016/s0015-0282(03)00158-4. [DOI] [PubMed] [Google Scholar]
- 33.Quella SK, Loprinzi CL, Barton DL, et al. Evaluation of soy phytoestrogens for the treatment of hot flashes in breast cancer survivors: A North Central Cancer Center Group Trial. J Clin Oncol. 2000;18:1068. doi: 10.1200/JCO.2000.18.5.1068. [DOI] [PubMed] [Google Scholar]
- 34.Upmalis DH, Lobo R, Bradley L, Warren M, Cone FL, Lamia CA. Vasomotor symptom relief by soy isoflavone extract tablets in postmenopausal women: A multicenter, double-blind, randomized, placebo-controlled study. Menopause. 2000;7:213. doi: 10.1097/00042192-200007040-00005. [DOI] [PubMed] [Google Scholar]
- 35.Washburn S, Burke GL, Morgan T, Anthony M. Effect of soy protein supplementation on serum lipoproteins, blood pressure, and menopausal symptoms in perimenopausal women. Menopause. 1999;6:7. [PubMed] [Google Scholar]