Abstract
Chronic diseases are the leading cause of death in the United States. Worksites provide a venue to address risk factors and conditions at work through health promotion aimed at improving individual health behaviors, health protection including occupational safety and health interventions, and efforts to support the interface between work and family. In response to the importance of preventing chronic disease at worksites, the National Institutes of Health and the Centers for Disease Control and Prevention convened a workshop to identify research priorities to advance knowledge and implementation of effective strategies to reduce chronic disease risk. Workshop participants outlined a conceptual framework and corresponding research agenda to address chronic disease prevention through integrating health promotion and health protection in the workplace.
INTRODUCTION
Approximately half of Americans live with a chronic disease and about one-fourth report residual effects from their chronic diseases.1 Chronic diseases, including heart disease, cancer and stroke, are the leading causes of death in the United States (US).2 Disparities in chronic disease exist by race/ethnicity and socioeconomic status, with minorities and lower income groups having a higher prevalence of heart disease, cancer and stroke, and multiple risk factors for these conditions.3–5 Of additional concern, the prevalence of chronic diseases is higher in the US than in other developed countries.6–8 There are more than 81 million people with cardiovascular disease (CVD) in the US, with an estimated cost of $503 billion in 2010.9 In 2005, over 1.3 million people were diagnosed with cancer, with costs in 2007 estimated at $219 billion.10 Almost 24 million Americans have diabetes, at a cost of $174 billion in 2007.11 Approximately 67% of American adults are overweight or obese,12 with a projected cost of $147 billion for 2008.13 In addition, non-fatal chronic conditions, such as musculoskeletal disorders 14 and psychological disorders,15 are major sources of disability.16
Worksites provide a venue to address multiple individual risk factors and risk conditions through worksite health promotion aimed at changes in individual behaviors, worksite health protection including occupational safety and health interventions, and efforts to address unhealthy work-family conflict.17,18 As a venue for delivering chronic disease prevention efforts, worksites provide a ready channel for reaching the large segment of the population that is employed. Worksite conditions also contribute to the development of chronic diseases, for example through hazardous job exposures, high job demands, and inflexible work schedules.
Individual health behaviors contribute significantly to these chronic disease outcomes. In 2000, 435,000 deaths (18.1% of total deaths) were attributed to tobacco use, 365,000 deaths (15.2%) were attributable to a combination of poor diet and lack of physical activity, and 84,000 deaths (3.5%) were related to alcohol misuse.19,20 These four individual health behaviors collectively accounted for approximately 40% of all deaths in the United States in 2000. 21 Worksite health promotion provides an effective way to enhance health-promoting behaviors, to reach a large segment of the population, and to reduce chronic disease risk factors. Comprehensive worksite health promotion has been recommended by the American Heart Association, the American Cancer Society, Healthy People 2010, the National Institute for Occupational Safety and Health, the National Institutes of Health, and the Centers for Disease Control and Prevention (CDC).22–25
In 2006, US healthcare spending was reported to be over 2 trillion dollars26 and employers on average paid more than one-third of this cost.27 A meta-analysis of the literature on costs and savings associated with worksite health promotion programs reported that medical cost reductions of about $3.27 are observed for every dollar invested in these programs.28 This number has been corroborated by recent systematic reviews and economic analysis conducted by the Task Force on Community Preventive Services, which reported an annual savings of $3.20 for every dollar invested.29,30 Other benefits of worksite health promotion include reduced absenteeism28,30 and improved employee attitudes towards work.31
The work environment, encompassing the physical, psychosocial, and organizational environments, directly shapes employee health, safety, and health behaviors.22 In 2008, over 5,000 workers died from occupational injuries,32 and work-related illnesses account for 49,000 deaths annually.33 Over 4.6 million workers experienced non-fatal occupational injuries or illnesses in 2008; about half of these non-fatal injuries and illnesses resulted in time away from work due to recuperation, job transfer or job restriction.34 Employers and insurers spent approximately $85 million in workers’ compensation costs in 2007,35 although this figure is only a portion of the costs borne by employers, workers, and society overall for the costs associated with work-related illness and injury. In 1992, the total economic costs to the nation from occupational illnesses and acute injuries was estimated to total between $15536 and $171 billion, 37 figures that are similar to those for all cancer or all cardiovascular disease in this time period.36,38
Worksite health protection initiatives include efforts to improve occupational safety and health, address organizational factors at work that influence worker health, and support work-life balance. Compliance with safety and health standards were mandated by the passage of the Occupational Safety and Health Act of 1970. OSHA rules, such as those pertaining to cotton dust, inorganic lead, and blood-borne pathogens, have resulted in reduced exposures and illnesses.39 Efforts by government, labor, management and health professionals have also led to reductions in exposure to biomechanical risk factors at work, which contribute to work-related musculoskeletal disorders, the most common category of occupational disease reported to OSHA.14 Labor-management health and safety committees and worker compensation insurers have reported that OSHA’s support of prevention through regulation and training have contributed to the prevention of work-related injuries and illnesses.40 It is also possible for worksite initiatives to redress sources of stress at work including inflexible work schedules, low job control, and excessive job demands, 41,42 which lead to negative health outcomes for employees and their families.
The combination of health behavior change programs with work environment changes may be synergistic and when integrated, may enhance their effectiveness.22,43 Beyond using the worksite as a platform to promote changes in individual health behaviors, such as smoking, dietary intake, physical activity, and weight control, a more integrated approach recognizes that the workplace acts as both an accelerator and preventer of chronic disease and as a key determinant of individual health behaviors, through physical, social, organizational and psychosocial mechanisms. Simply stated, workers may perceive changes in their individual health behaviors as futile in the face of significant occupational exposures that have considerable bearing on their health. Conversely, management and labor efforts to create a healthy work environment may contribute to workers’ motivations to modify their personal health behaviors, and may foster a climate of trust that may support workers’ receptivity to messages from their employer regarding individual health behavior change.44–46 This principle of integrating worksite health protection with worksite health promotion was recently endorsed by the American Heart Association for cardiovascular health promotion.47
In light of the importance of chronic disease prevention at the workplace, the National Heart, Lung, and Blood Institute (NHLBI), the National Institute of Occupational Safety and Health (NIOSH), the Centers for Disease Control and Prevention (CDC), the National Institute for Child Health and Human Development (NICHD), and the National Cancer Institute (NCI), convened a workshop to identify research needed to develop effective programs that reduce chronic disease risk and support worker and family health through effectively promoting healthy and safe individual behaviors, reducing physical, psychosocial and organizational risks at the worksite, and promoting work-life balance. The workshop, held on May 21–22, 2009, was co-chaired by Dr. Barbara Israel, Professor of Health Behavior and Health Education, School of Public Health, University of Michigan, and Dr. Glorian Sorensen, Professor of Society, Human Development and Health, Harvard School of Public Health. The panel, selected by the workshop sponsors to reflect a range of perspectives on chronic disease prevention in the workplace, consisted of specialists in epidemiology, sociology, occupational and preventive medicine, organizational psychology, occupational health psychology, health education and health behavior, environmental and occupational health, economics, exercise physiology, ergonomics, pediatrics and human development. Their interests were varied and included individual behavior and organizational change research, family and community health research, public policy, intervention design and evaluation, translation and outcomes research, participatory action research, and health disparities (see list of participants in Appendix A).
The workshop objective was to develop a comprehensive and coordinated research plan to build the evidence base around effective chronic disease prevention for working adults and their families through worksite interventions. To achieve this objective, the workshop had three main informational sessions: 1) promoting individual behavior change, 2) changing the work environment (physical, psycho-social and organizational), and 3) intervening to influence the work-family-community interface. Each session was guided by eight areas of discussion: 1) research strategy, 2) current state of the science, 3) conceptual models, 4) research design, 5) practices and policies, 6) cost-effectiveness, 7) barriers, and 8) specific populations. This report presents three parallel worksite approaches to preventing chronic disease – through promoting individual behavior change, changing the work environment, and addressing work-family-community interface – and explores opportunities for coordination and integration of these approaches. Further details about these recommendations are presented in Table 1.
TABLE 1.
RECOMMENDATIONS FOR FUTURE RESEARCH
| Assessment of intervention efficacy and characteristics associated with efficacy |
|
| Attending to population, job, and worksite characteristics |
|
| Use of appropriate study designs and methods |
|
| Application of appropriate and expanded measures and metrics |
|
| Studying sustainability and knowledge transfer |
|
| Addressing global concerns |
|
CONCEPTUAL FRAMEWORK
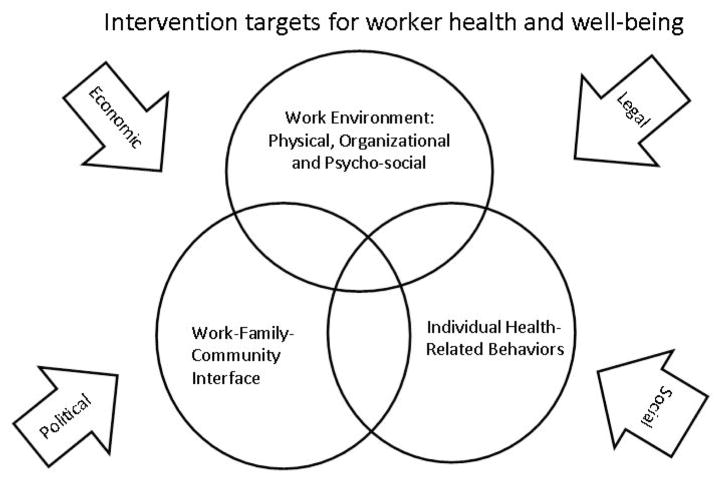
Figure 1 depicts the conceptual framework that guided the workshop discussions. The three circles illustrate the three intervention targets that were the workshop focus: individual health behaviors, the work environment, and impacts on the work, family and community interface. A focus on individual health behaviors, such as smoking, dietary patterns, physical activity, and weight control, may occur singly or as a multiple risk factor approach, and typically utilizes the workplace as a platform for program delivery; changes in the work environment may be implemented to support health behavior changes. Components of the work environment that may influence worker and family health include worksite culture; organizational policies and practices; hazardous chemical, physical and biological exposures; psychological job demands; job control; work schedule and control over work time; work-related rewards; organizational justice; work norms and social support; and union status. Additional attention must be paid to the impact of the interrelated work, family and broader community systems, given the importance of psychological and behavioral spillover and crossover between work and family lives. The conceptual model also acknowledges the roles of economic, legal, political and social factors, which may influence worker health, job insecurity, access to health insurance, and worker and family stress.18 Overlap of the circles shows opportunities for collaboration, integration, and synergy, thereby strengthening the potential for impact on chronic disease prevention at the workplace.
FIGURE 1.
WORKSHOP CONCEPTUAL MODEL.
PROMOTING INDIVIDUAL HEALTH BEHAVIOR CHANGE AT THE WORKPLACE
Workshop participants referred to the Healthy People 2010 Objectives for a definition of “comprehensive” worksite health promotion, which includes several core components: health education programs, a supportive social and physical environment, “integrated” programs (e.g., budget, staffing, resources), screening (including treatment and follow up as needed), and linkage to other assistance programs.25 Worksite health promotion programs also include a needs assessment, individualized health messages, encouragement of self-care, use of incentives, social support, and sufficient duration to enhance implementation and maintenance.48 Through Healthy People 2010, CDC has recommended that at least 75% of worksites offer a comprehensive worksite health promotion program.49 The most recent National Worksite Health Promotion Survey found, however, that only 7% of worksites do so.50 Although larger worksites are less numerous that smaller ones,51 worksites with 750 or more employees were over six times as likely to offer comprehensive worksite programs than those with 50–99 employees.50 Larger worksites also offered more variety in programs such as physical activity, tobacco, fitness and nutrition, and screening services, compared to smaller worksites.50
Barriers to worksite program implementation include low employee participation, lack of employee interest, limited staff resources, cost, misalignment of incentives among different stakeholders, and insufficient management support. 50,52 Workshop participants discussed strategies for increasing employee participation, including peer and management support and incentives, as well as implementing and maintaining a respectful partnership with stakeholders (e.g., employees and their families, labor, management, health professionals, insurance companies, government agencies).
Physical activity provided a useful example of a health behavior that can be effectively influenced through multi-level worksite health promotion. Only about 32% of U.S. adults report engaging in regular leisure-time physical activity, with rates even lower among ethnic minority, low income and other underserved populations;53 rates are also lower when activity is objectively monitored.54 Several studies have demonstrated the potential impact of brief, socially obligatory structured group exercise breaks on paid time.55–58 Future studies may explore the use of physical activity breaks in increasing participation in physical activity and enhancing sustainability, as well as identifying the organizational benefits of exercise for injury prevention.59–63
Participants discussed the challenge of sustaining health promotion programs after implementation, and of the tendency of some programs to degrade from evidence-based models over time. A framework for implementing, sustaining, and evaluating effective programs, such as the RE-AIM model, can be a helpful guide for program planning and evaluation. The RE-AIM framework addresses both employee and organizational interventions by considering the reach and representativeness, as well as efficacy, adoption, implementation and maintenance of comprehensive worksite health promotion programs.64,65
Research gaps and future directions
Workshop participants discussed the need for ongoing research to identify characteristics of successful programs, including through the use of in-depth, mixed methods, and comparative case studies.66 For example, it will be useful to examine the extent to which worksite health promotion efforts may contribute simultaneously or sequentially to multiple health behavior changes, and the extent to which one health behavior change may serve as a “gateway” to other health behavior changes, e.g., increases in physical activity may spark and support changes in dietary patterns. Future research may also test intervention methods for high-risk employees (e.g., overweight or obese employees) via stepped-care approaches or other methods tailored to diverse populations based on race/ethnicity, age, health status, and other key characteristics. Process evaluation methods may be employed to examine program impacts on sub-populations when studies have adequate power for key subgroup analyses. Formative research is needed to understand factors associated with low participation rates among both employees and employers,67 and the role of key social influences on employee participation, such as from family members, management and supervisors, and union representatives. Specifc research is also needed for small businesses.68
Workshop participants stressed the need to identify the level and intensity of intervention exposure needed for optimal efficacy, and to differentiate which intervention components contribute the most to behavior changes. This information is important as well to determine the favorable cost benefit ratios and returns on investment (ROI).69–71 The economic rationale behind health promotion interventions is particularly important because of the need to convince program sponsors to initiate and maintain such programs.72 Future research should consider, for example, the relevance of health promotion programs to employers with fully insured health plans vs. self-insured plans, and the role of behavioral economics in chronic disease prevention.73–75
PROMOTING CHANGES IN THE WORK ENVIRONMENT: PHYSICAL, ORGANIZATIONAL AND PSYCHOSOCIAL CHANGES
The physical, psychosocial, and organizational work environments are important contributors to chronic disease. Cancer is the leading cause of workplace fatalities worldwide, accounting for about one-third of all workplace fatalities.76 The World Health Organization and others have estimated that 8–16% of all cancers are caused by preventable exposures to workplace hazards.76,77 Shift work may also lead to increased cancer risk.78 Workplace risk factors for cardiovascular disease include chemicals such as carbon monoxide, carbon disulfide, solvents, and lead; organizational factors such as work schedules, including long work hours and shift work; and psychosocial stressors, such as high demand-low control work (job strain), high job efforts combined with low job rewards (e.g., income, support, respect and job security), and organizational injustice.15,79 Estimates of the proportion of CVD due to these work-related factors range from 15% 80 to 35%.81 Work schedule factors and psychosocial stressors contribute to obesity, smoking, heavy alcohol use, and lack of exercise;82–84 as well as to musculoskeletal disorders;85 psychological disorders, such as depression, anxiety and “burnout”,15 and work-family stress and conflict.86,87 Workplace risk factors for musculoskeletal disorders include repetition, force, awkward postures, vibration and temperature. Each year, these disorders affect about 1 million workers and cost the nation between $45 billion and $54 billion in compensation expenditures, lost wages, and decreased productivity.14
Risks posed by the work environment do not affect all workers equally. Workshop participants discussed older workers, noting there has been over a 100% increase in the number of workers aged 65 or older between 1997 and 2007, compared to a 59% increase in total employment during that decade.88 Chronic disease is more prevalent in older than younger workers. Research using the work-ability index (WAI),89,90 which captures workers’ assessment of their individual ability to be productive in the job given their current health status, has shown older workers consistently score lower on work-ability compared to younger workers. Although average WAI decreases with age, factors such as improvements in ergonomics, reductions in work stress and work demands, improved supervisor support, flexible work schedules, teamwork, individual lifestyle health promotion (e.g., physical activity), and building workers’ skills and competencies can improve the WAI. 91 Both chronic musculoskeletal disease and low work-ability are highly predictive of disability. 92–94 Participants discussed the utility of the concept of work-ability and other measures to capture an important interplay between health status and efforts to change health and work. Workplace interventions that integrate improved workplace safety and health conditions with personal health promotion or individual interventions may be effective in preserving work-ability, reducing disability and preventing or helping people to manage chronic illnesses as they age.56,95
Risks posed by the work environment also vary by employee socio-economic position, as illustrated by the differential impacts of work stressors, and their relationship to health behaviors and chronic diseases.96 Work stressors associated with chronic disease include work organizational practices and characteristics (e.g., downsizing, restructuring, privatization of public services); production characteristics (e.g., piece-rate incentive pay systems, electronic surveillance, inadequate staffing); task-level psychosocial stressors (e.g., job strain, low job control, long hours, shift work); and other work-related factors (e.g., organizational injustice, job insecurity, safety and health hazards).97,98 Workshop participants noted evidence that socioeconomic position and work stressors interact. For example, blue-collar workers experiencing job strain are more likely than white collar workers with job strain to have heart attacks (among Swedish men),99 and elevated blood pressure (among New York City men).100 The workgroup discussed the growing socioeconomic disparities in cardiovascular disease101 and its risk factors, with risk increasing for lower status (blue collar) workers relative to higher status (white collar) workers.102 Relative to other workers, workers from lower socioeconomic status also face more hazardous physical and psychosocial workplace exposures, and have less access to health promotion programs at work.103 Participants suggested that labor market trends and related changes in working conditions of lower income workers may contribute to chronic disease disparities. These trends include stagnant real income and growing income inequality, the decreasing proportion of the U.S. labor force in unions, increases in precarious or contingent work, deregulation, and privatization of government services.15,97
Research gaps and future directions
Further research is needed to examine the efficacy of interventions promoting changes in the work environment, with attention to modifying factors such as type of job, job status, employment contract, industry and unionization status. This research should examine the range of mechanisms (e.g., toxicity, psychological stress mechanisms, and biomechanical stress) by which hazardous occupational exposures increase the risk of chronic disease. There is also a need for improved understanding of strategies to promote healthy aging at work, and of work environment factors related to competition in the global economy that may explain growing socioeconomic disparities in chronic disease and related risk factors.
Tools for assessing worksite support for workers’ health behaviors (e.g., HeartCheck104) as well as Health Risk Appraisals, need to be expanded to include hazardous occupational exposures. Since worker compensation systems capture only a small fraction of work-related chronic diseases, novel methods, such as access to medical insurance claim databases linked to employment data, are also needed to understand the work-relatedness of chronic disease and its various mechanisms.
Whereas these areas for further research are important, the integration of research methods into practice and operations can provide significant insight into how to implement solutions that work.105 The applicability and acceptability of checklists, measurement tools, and surveys will vary by industry and sector, as well as with the resources the workplace has to redress problems. It is important to consider the applicability of research to practice in examining use of measurement and evaluation tools that may also serve as interventions.
Research is needed on the impact of legislative and regulatory policy changes at state and national levels on exposures in the work environment, worker health behaviors and chronic disease risk. For example, it will be important to track the potential impact of health care reform, changes in federal or state laws on minimum staffing levels among nurses, investments in ventilation systems to control chemical exposures, and state or municipal paid family leave or paid sick leave legislation.106 Research should address the organizational and economic factors that predict how fully workplaces implement these policy changes.107
WORKPLACE INTERVENTIONS AND THE WORK-FAMILY-COMMUNITY INTERFACE
Work also influences health through its interface with workers’ families and their communities. Workshop participants discussed the changing nature of work-family dynamics, the resulting impact of workers’ exposures to stressors at home and on the job, the potential effects not only for workers’ health but also for the health of their families, and the implications for workplace interventions to help reduce work-family stress.
Attention to the work-family interface has increased over the past 30 years with increasing numbers of women working outside of the home, a corresponding increase in dual earner families, delays in childbirth, and an increasing percentage of workers who are caring for both children and aging parents.108 These socio-demographic changes reduce family time, and contribute to work-family stress and broader changes in family members’ roles.109,110 With increases in service sector employment coupled with increases in technology and the global economy, workers are being required to operate in a 24/7 work environment. Many workers occupy low wage, high demand service jobs, requiring them to have second jobs to make ends meet. Work-family conflict, or the stress and interference of engaging in both work and family roles simultaneously, has been linked to mental health problems such as depressive symptoms and psychological distress, lower self-reported health,111–116 more chronic physical symptoms, and higher sickness absence.117,118 Work-family conflict has also been related to higher work stress, family stress, and substance abuse,86,87,119 as well as to decreased healthy eating behaviors.120 Work-family conflict may also result in decreased organizational commitment and job satisfaction, absenteeism, and increased intentions to leave the job.86
While workers’ families and communities clearly may support workers through mechanisms such as positive spillover and social support,121 much research in the area of work and family has identified the detrimental effects of integrating multiple roles on worker and family health.86 These detrimental effects have primarily been examined among white-collar workers with greater access to flexible work schedules and control over work hours. Workshop participants speculated that the impact of work-family conflicts and stress may be more pronounced for lower wage workers due to the lack of workplace support and higher levels of psychosocial stressors such as demanding supervisors, excessive work hours, and unpredictable work schedules.
Formal workplace supports, benefits, and policies that are aimed at reducing such work-family conflict include providing dependent care support via subsidies, resources and referral, alternative work schedules, and increased worker control over when, where and how work is performed. Informal support comes from organizational and management culture. Research has demonstrated that the success of formal supports in impacting worker and family health and well-being is dependent on the level of organizational and managerial informal support for work and family.122 Furthermore, a recent quasi-experimental study of grocery workers and their supervisors found beneficial effects of a supervisory training and a self-monitoring intervention to improve supervisor support for work and family on worker job satisfaction, turnover intentions and self-reported physical health symptoms.123
While there is substantial research indicating that the psychosocial characteristics of the work environment, such as supervisor support, work role demands, and control over work-time, spill over to impact health of workers, there is also evidence that the work environment can impact workers’ family members. This crossover, or the transmission of stress and strain from one individual to another, occurs between workers and their family members.41,42 When considering chronic disease prevention in the workplace, workshop participants recommended a systems perspective to study the effects of workplace prevention programs on the family in addition to the effect on workers, and evaluating the impact of family characteristics on how workers respond to such interventions at work.108 Workplace interventions addressing workers, their family members, and the community are needed to prevent or diminish adverse work-family conflict and crossover effects.
Research gaps and future directions
Much of what is known about workplace supports, benefits, and policies aimed at reducing work-family conflict is based on anecdotal or cross-sectional evidence. The lack of longitudinal research, experimental and quasi-experimental designs, and non-representative samples has limited the ability to draw conclusions about the effectiveness of work-family-specific policies or initiatives.124 Furthermore, participants discussed the impact of formal and informal work-family supports on workers’ ability to integrate work and family. Research on factors that contribute to the adoption, implementation, and utilization of formal work-family policies is needed. Understanding the impact of working conditions such as type of work schedule, high demands, and low control work on working families and their multiple work and family demands would be beneficial. A better understanding of the relationships between community supports and work-family conflicts is needed (e.g., the impact of programs such as Head Start on work-family stress among low-wage families, and the effects of utilization of paid FMLA on workers’ health outcomes). Formal workplace and federal policies that impact workers and their ability to manage work and family should be examined in light of their ultimate impacts on worker and family health.
It is also important to increase understanding of the informal workplace culture, its impact on supporting or hindering worker health and well-being, and ways to intervene to support its positive effects. Factors that contribute to such informal support such as workplace characteristics, individual characteristics, as well as the broader economic, legal, political, and social environments are important to pursue in future research agendas.
Currently, work-family policies and benefits are unequally distributed, with those workplaces with more professional workers being more likely to provide these supports. There is also often unequal access within a workplace, with those in higher-status occupations more likely than other workers to have flexible schedules and eligibility for benefits.125–127 Future research should address whether broadening access to these work-family supports improves the health and well-being of lower-status, lower wage, and older workers and their families, and whether new interventions are needed to address the needs of these workers.
FINDING SYNERGY ACROSS DISCIPLINARY PERSPECTIVES
This workshop explored not only the parallel paths of these three approaches to worker health, but also the potential avenues for synergy, coordination, and integration as a means of strengthening chronic disease prevention efforts at the workplace, increasingly supported by of scientific evidence.22,43–46,128 This approach aims to attend to individual health behaviors and to the work organization and environment, including hazardous exposures, work stressors, and organizational policies and practices, as well as work-family demands.18,129 Research has demonstrated that blue-collar workers are more likely to make health behavior changes, such as quitting smoking, when worksite health promotion programs are coupled with workplace hazard assessments and changes in the work environment.128,130,131 Research is also exploring the links between the physical and psychosocial conditions of work, and a range of musculoskeletal, cardiovascular and mental health outcomes.43,132
National initiatives are now underway to further research in this area. The NIOSH WorkLife Initiative is a broad-based effort aimed at sustaining and improving worker health through worksite programs, policies and practices that promote and protect worker health at the organizational and individual levels.133 NIOSH has identified core “essential elements” of effective workplace programs and policies for improving worker health and wellbeing, as described on the weblink.134 The Work, Family, and Health Network, funded jointly by the Centers for Disease Control and the National Institutes of Health, is another example of a worker health research initiative; the Network is aiming to develop and evaluate the effects of worksite work-family policies and practices that impact health of workers and their families.135
Workshop participants discussed challenges to the development of a shared research agenda aimed at reducing risk of chronic disease among workers and their families. Convening multi-disciplinary teams as a foundation for a trans-disciplinary approach requires surmounting barriers among scientific disciplines, including developing pooled bodies of knowledge based on shared language and jointly developed methods.136,137 These diverse disciplinary perspectives rely on communications through different journals and professional meetings, and on funding mechanisms that cut across NIH Institutes and the CDC. Our diverse backgrounds have contributed to differing perspectives about worker health. For example, the premise that worker health begins with individual behavior change sets in motion a different set of intervention strategies from the legal formulation in the Occupational Safety and Health Act, which starts from the assumption that management bears primary responsibility for worker health and safety on the job. Overcoming the segmentation of these fields ultimately will require an inclusive, comprehensive model of work and health, providing for an understanding of our differences in assumptions, vocabulary, research methods, and intervention approaches. It is possible to expand communication to support inter-disciplinary strategies, for example, through shared journals, shared symposiums, or shared funding opportunities.22,126
WORKSHOP RECOMMENDATIONS FOR FUTURE RESEARCH
Based on the presentations from the three panels, the workshop participants outlined a framework for a research agenda addressing chronic disease prevention that integrates health promotion and heath protection approaches in the workplace, and that takes into consideration the broader work-family-community interface. Workshop participants identified cross-cutting research themes and priorities for future research, with particular attention to research priorities for coordinating and integrating the three parallel targets influencing worker health. After the workshop, participants further developed these themes in a series of conference calls; the writing team consolidated these priorities, which were then vetted by the full group of participants.
As illustrated in Table 1, we identified six broad recommendations for future research:
Assessment of intervention efficacy and characteristics associated with efficacy:48,138–140
As the summary of the three panel discussions illustrates, most worksite research conducted to date has focused independently on one of these three avenues of inquiry. Workshop participants placed a high priority on future research aimed at bridging the divide across the three domains, as illustrated in the conceptual model (Figure 1). It will be important to test the effects of integration across these three intervention targets on worker and family health outcomes, as well as on changes in the work environment. Interventions were defined broadly across multiple levels, including changes in the work environment and policy changes, as well as educational programs for workers and managers. Research is needed to identify opportunities for synergy across the three intervention targets, and to assess contributors to both program adoption and implementation of best practices. For example, interventions may be informed by research that explores the substantial source of stress for workers working and living with musculoskeletal pain, which can inhibit leisure-time exercise, and lead to self-medication (e.g., unhealthy food, drugs, alcohol) for the pain, and contribute to depression.141
It will be important as well to study factors related to both the adoption of integrated interventions leading to both organizational changes and individual changes, and to the participation of organizations, employee representatives and individuals in integrated interventions that change behaviors and sustain behavior changes. Similarly, research needs to examine the impact of formal organizational policies and practices related to health promotion and health protection, management structure, leadership style (e.g., transactional, transformational), and informal management practices in supporting or inhibiting health programs.105,142
Attending to population, job, and worksite characteristics:50,67,98,100,131,143–147
A key theme across the three panel presentations was the persistence of disparities in worker health outcomes, access to worksite programs, and exposures in the work environment. Research is needed to identify ways to redress these disparities and assure broad-based access to interventions across groups of workers, whether defined by occupation, gender, age, socioeconomic position, race/ethnicity or other characteristics. Alternative strategies to provide integrated interventions to blue-collar and other lower status workers, such as through occupational medicine clinics or through collectively bargained programs, need to be explored. Such research must include a broad range of workers and worksites to assure the generalizability of the research findings and to identify factors to improve targeting of interventions to specific groups of workers and worksites.
Use of appropriate study designs and methods:22,143,148–150
Consideration must be given to the selection of research designs appropriate to the nature of the research question and the phase of research, including not only randomized controlled trials but also natural experiments and in-depth, mixed methods, or comparative case studies. These methods must take into account the multi-level nature of this research, requiring multi-level designs that include assessments of management structures, support for workers and their families, and related organizational health outcomes. Workshop participants also recommended the use of participatory approaches that engage a diverse representation of employees in the planning and implementation of these efforts.
Application of appropriate and expanded measures and metrics:30,148,151,152
To permit comparisons across studies, researchers need to employ standardized measures that have demonstrated reliability and validity. There is a need for improved occupational exposure assessments for integrated work environment and health promotion interventions, and to assess the role of unions in worksite chronic disease prevention efforts. From an economic perspective, it will be important to develop standard methods for measuring cost savings and ROI evaluation methods, and creating standards for ROI calculation (e.g., defining the elements that comprise both the cost and benefit sides of the equation).69–71,153,154 Workshop participants also discussed the need to monitor the application of integrated worksite programs, including through an integrated national worksite survey of employers to assess both program adoption and implementation.
Studying sustainability and knowledge transfer:155–158
Also important is the need to identify methods to promote the use of evidence-based interventions and assess their long-term sustainability. Participants stressed the need to minimize the time for transition from research into practice,159 and to assure that evidence-based interventions are effectively adapted and disseminated. Research on the dissemination process may identify methods to engage different types of worksites and organizational leaders, examine the motivational influence of financial and other incentives for worksite participation in chronic disease prevention, investigate the influence of family members on motivation to participate, and assess barriers to effective intervention delivery.
Addressing global concerns:160
Workshop participants additionally noted that worksites exist in a global economy, and that attention needs to be paid to the promoting worker health and healthy work environments beyond the US borders.
Implementation of these recommendations
As noted above, advancing this research agenda requires the creation and nurturing of trans-disciplinary teams and identifying funding sources to support integrated studies. Research networks, centers of excellence, and other collaborative vehicles can promote research across disciplines and with diverse perspectives. Sustained funding of longitudinal research studies is needed to evaluate the effectiveness of interventions that integrate health protection and health promotion strategies. Implementation of these research recommendations will require collaboration across funding bodies. It is imperative that new funding initiatives cut across NIH Institutes and the CDC, in order to foster research on multi-level interventions addressing the three intervention targets discussed here. There is an additional need to develop relationships with journals to promote and support the dissemination of such research, for example through special issues focused on the research priorities described here. This research will also benefit from fostering graduate level training programs that promote comprehensive and integrative approaches to health promotion and health protection, as recommended here.
CONCLUSION
Prevention of chronic disease among workers requires a partnership among federal and state public policy makers, employers, workers, labor union representatives, health professionals and the surrounding community. In the face of an increasing chronic disease burden, rising health care costs and health care reform, it is critically important that part of the solution involves addressing the health of workers. Promising evidence points to the important role that the workplace may play in chronic disease prevention and control. It is important that these prevention efforts also acknowledge the potential impacts of work-related factors on individual health behaviors through physical, social, organizational and psychosocial mechanisms, and potential exposures to hazards on the job that may directly influence work, family and organizational health outcomes. It is critical that rigorous scientific evidence be the cornerstone of the next generation of research on chronic disease prevention in the workplace. Articulation of a research agenda to enhance worker health in the context of healthy workplaces will require the engagement of policy, research and funding organizations. This research will benefit from the contributions of scientists across disciplinary boundaries, including researchers focused on health behaviors and worksite health promotion, occupational safety and health, the work-family-community interface, and the intersections between work and other sectors of workers’ lives. This workshop stimulated a dialogue across these disciplines and identified critical research that may ultimately promote and protect worker health. Systematic implementation of this research vision and effective dissemination of new models of interventions to support worker health outcomes is needed to address chronic disease prevention.
Acknowledgments
This paper is based on findings and recommendations from a national workshop sponsored by the National Heart Lung and Blood Institute, the National Institute of Occupational Safety and Health, the National Institute of Child Health and Human Development, the National Cancer Institute, and the Centers for Disease Control and Prevention, May 21–22, 2009, Bethesda, MD. The authors thank the National Heart, Lung, and Blood Institute, the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention, the National Institute for Child Health and Human Development, and the National Cancer Institute for their support. Dr. Sorensen’s contributions were funded by grants from the National Cancer Institute (5 K05 CA108663-05) and the National Institute for Occupational Safety and Health (5U19 OH008861-04).
APPENDIX A: ROSTER OF WORKSHOP PARTICIPANTS AND THEIR AFFILIATIONS
Audie A. Atienza, Ph.D. (Program Director, National Cancer Institute, NIH, Bethesda, MD)
Ben Amick, Ph.D. (Professor of Behavioral Sciences and Epidemiology, School of Public Health, The University of Texas Health Science Center, Houston, Texas and Scientific Director, Institute for Work & Health, Toronto, Canada)
Cathy L. Backinger, Ph.D, M.P.H. (Chief, Tobacco Control Research Branch, Behavioral Research Program,NCI, Rockville, MD)
Lisa Berkman, Ph.D. (Director, Center for Population and Dev Studies, Thomas D. Cabot Professor of Public Policy and of Epidemiology Harvard School of Public Health, Cambridge, MA)
Rosalind Berkowitz King, Ph.D. (Health Scientist Administrator, National Institute of Child Health and Human Development, Bethesda, MD)
Martin Cherniack, M.D., M.P.H. (Professor of Medicine, University of Connecticut Health Center, Farmington, CT)
Kathy Christensen (Director, Workplace, Work Force & Working Families Program Alfred P. Sloan)
Michael Donovan, Ph.D. (Presidential Management Fellow, NHLBI, Bethesda, MD)
Lawrence Fine, M.D., M.P.H., Dr.P.H. (Chief, Clinical Applications Branch, National Heart, Lung, and Blood Institute, NIH, Bethesda, MD)
Kelly M. Flannery, R.N., M.S. (Ph.D. student, University of Maryland Baltimore, MD)
Ron Z. Goetzel, Ph.D. (Research Professor and Director, Institute for Health and Productivity Studies, Rollins School of Public Health Emory University, Vice President, Consulting and Applied Research, Thomson Reuters, Washington, DC)
Leslie Hammer, Ph.D. (Director, Occupational Health Psychology, Professor of Psychology, Portland State University, Portland, OR)
Christine Hunter, Ph.D., ABPP (LCDR USPHS, Director of Behavioral Research Division of Diabetes, Endocrinology, and Metabolic Diseases, National Institute of Diabetes & Digestive & Kidney Diseases, NIH, Bethesda, MD)
Barbara A. Israel, Dr.P.H., M.P.H. (co-chair) (Professor, Health Behavior & Health Education, University of Michigan, Ann Arbor, MI)
Erin Kelly, Ph.D. (Associate Professor, Department of Sociology, University of Minnesota, Minneapolis, MN)
Supriya Lahiri, Ph.D. (Professor, Department of Economics, University of Massachusetts Lowell Lowell, MA)
Paul Landsbergis, Ph.D., M.P.H. (Associate Professor, Department of Environmental and Occupational Health Sciences, State University of New York-Downstate School of Public Health, Brooklyn, NY)
Laura Linnan, ScD, CHES (Associate Professor, Department of Health Behavior and Health Education, UNC GIllings School of Global Public Health, University of North Carolina, Chapel Hill, NC)
James Merchant, M.D., DrPH (Professor, Department of Occupational and Environmental Health, Iowa City, IA)
Charlotte Pratt, Ph.D., R.D. (Program Director, National Heart, Lung, and Blood Institute, NIH, Bethesda, MD)
Nico Pronk, Ph.D., FACSM (Vice President and Health Science Officer, Senior Research Investigator, HealthPartners Research Foundation, Minneapolis, MN)
Laura Punnett, Sc.D. (Professor, Department of Work Environment, Director, Center to Promote Health in the New England Workplace (CPH-NEW), Senior Associate, Center for Women and Work (CWW) Univ. of Mass. Lowell, MA)
Teresa Schnorr, Ph.D. (Director, Division of Surveillance, Hazard Evaluations, and Field Studies, NIOSH/CDC, Cincinnati, OH)
Mark A. Schuster, M.D., Ph.D. (William Berenberg Professor of Pediatrics, Harvard Medical School, Chief of General Pediatrics & Vice-Chair for Health Policy, Department of Medicine, Children’s Hospital Boston, Boston, MA)
Michael Silverstein, M.D., MPH (Clinical Professor, Environmental & Occupational Health Sciences, Univ. Of Washington School of Public Health, Seattle, WA)
Glorian Sorensen, Ph.D., MPH (co-chair) (Dana-Farber Cancer Institute & Harvard School of Public Health, Professor of Society, Human Development and Health, Department of Society, Human Development, and Health; and Director of the Center for Community-Based Research, Dana Farber Cancer Institute, Boston, Massachusetts)
Thomas M. Vogt, M.D., MPH (Senior Investigator, Kaiser Permanente, Honolulu, HI)
Gregory R. Wagner, M.D. (Harvard School of Public Health Boston, MA and National Institute for Occupational Safety and Health, Washington, DC)
Laura S. Welch, M.D. (Medical Director, CPWR - The Center for Construction Research and Training Silver Spring MD)
Antronette Yancey, M.D., MPH (Professor, Health Services, UCLA School of Public Health, Los Angeles, CA)
Footnotes
Based on findings and recommendations from a national workshop sponsored by the National Heart Lung and Blood Institute, the National Institute of Occupational Safety and Health, the National Institute of Child Health and Human Development, the National Cancer Institute, and the Centers for Disease Control and Prevention, May 21–22, 2009, Bethesda, MD.
Contributor Statement
All authors of this paper contributed substantively to this paper. The named co-authors contributed directly to the writing of this manuscript, including to the conceptualization of the paper, drafting and revising the text of the manuscript, and approval of the final version of the paper. In addition, all workshop participants listed in the roster in the appendix of this paper contributed to the conceptualization of this manuscript and to the content of the paper, through their participation in the workshop, and approved the final content of the manuscript.
Human Participant Protection
Institutional review board approval was not needed for this manuscript.
Contributor Information
Glorian Sorensen, Harvard School of Public Health and the Dana-Farber Cancer Institute.
Paul Landsbergis, State University of New York-Downstate School of Public Health.
Leslie Hammer, Portland State University.
Benjamin Amick, University of Texas Health Science Center and is the Scientific Director of the Institute for Work & Health, Toronto.
Laura Linnan, University of North Carolina Gillings School of Global Public Health.
Antronette Yancey, University of California Los Angeles School of Public Health.
Laura S. Welch, Medical Director at the Center for Construction Research and Training, Silver Spring MD.
Ron Z. Goetzel, Rollins School of Public Health, Emory University and Thomson Reuters, Washington, DC.
Kelly M. Flannery, PhD student at the University of Maryland.
Charlotte Pratt, National Heart, Lung, and Blood Institute, NIH.
References
- 1.Centers for Disease Control & Prevention. [Accessed February 27, 2010];Chronic diseases and health promotion. http://www.cdc.gov.proxy-hs.researchport.umd.edu/chronicdisease/overview/index.htm. Updated 2009.
- 2.Centers for Disease Control & Prevention. [Accessed March 12, 2010];Leading causes of death. http://cdc.gov.proxy-hs.researchport.umd.edu/nchs/fastats/lcod.htm. Updated 2009.
- 3.Office of Minority Health. [Accessed March 12, 2010];Diabetes data/statistics. http://www.omhrc.gov/templates/browse.aspx?lvl=3&lvlid=5. Updated 2009.
- 4.Office of Minority Health. [Accessed March 12, 2010];Heart disease data/statistics. http://www.omhrc.gov/templates/browse.aspx?lvl=3&lvlid=6. Updated 2010.
- 5.Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics 2006 Update: a report from the American Heart Association statistics committee and stroke statistics subcommittee. Circulation. 2006;113(6):85–151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 6.Organization for economic co-operation and development. [Accessed February 25, 2010];Fact book 2009: economic, environmental and social statistics. http://titania.sourceoecd.org/vl=1388841/cl=37/nw=1/rpsv/factbook2009/11/01/04/index.htm.
- 7.Avendano M, Glymour MM, Banks J, Mackenbach JP. Health disadvantage in US adults aged 50 to 74 years: a comparison of the health of rich and poor Americans with that of Europeans. Am J Public Health. 2009;99(3):540–548. doi: 10.2105/AJPH.2008.139469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nolte E, McKee CM. Measuring the health of nations: updating an earlier analysis. Health Aff (Millwood) 2008;27(1):58–71. doi: 10.1377/hlthaff.27.1.58. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control & Prevention. [Accessed March 11, 2010];Chronic disease prevention and health promotion. http://www.cdc.gov.proxy-hs.researchport.umd.edu/chronicdisease/resources/publications/AAG/dhdsp.htm. Updated 2009.
- 10.National Program of Cancer Registries. [Accessed March 11, 2010];National program of cancer registries: facts. http://www.cdc.gov.proxy-hs.researchport.umd.edu/cancer/npcr/about.htm. Updated 2009.
- 11.American Diabetes Association. [Accessed March 11, 2010];Diabetes statistics. http://www.diabetes.org/diabetes-basics/diabetes-statistics/
- 12.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of American Medical Association. 2006;259(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 13.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Affairs (Millwood) 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 14.National Research Council. Musculoskeletal disorders and the workplace. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 15.Schnall P, Dobson M, Rosskam E, editors. Unhealthy work: causes, consequences and cures. Amityville, NY: Baywood Publishing; 2009. [Google Scholar]
- 16.Social Security Administration. Annual statistical report on the social security disability insurance program 2009. Washington, DC: Jul, 2009. SSA Publication No. 13–11826. [Google Scholar]
- 17.Pelletier KR, Herman PM, Metz RD, Nelson CF. Commissioned for the IOM Summit on Integrative Medicine and the Health of the Public. Feb, 2009. Health and medical economics: applications to integrative medicine. [Google Scholar]
- 18.Robert Wood Johnson Foundation. Issue Brief 4: work and health. 2008. pp. 1–18. [Google Scholar]
- 19.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: Actual Causes of Death in the United States, 2000. JAMA. 2005;293(3):293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- 20.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual Causes of Death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 21.Pronk NP, Lowry MK, TE, Austin E, Gallagher J, Katz A. The association between optimal lifestyle adherence and short-term incidence of chronic conditions among employees. In press. [DOI] [PubMed] [Google Scholar]
- 22.Sorensen G, Barbeau E. Steps to a healthier US workforce: integrating occupational health and safety and worksite health promotion: state of the science. The National Institute of Occupational Safety and Health steps to a Healthier US workforce symposium; October 26–28, 2004; Washington, D.C. 2004. [Google Scholar]
- 23.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance. A scientific statement from American heart association council on epidemiology and prevention, interdisciplinary committee for prevention. Circulation. 2008;118(4):428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control & Prevention. MMWR. RR10. Vol. 54. CDC; 2005. Public Health Strategies for Preventing and Controlling Overweight and Obesity in School and Worksite Settings. A Report on Recommendations of the Task Force on Community Preventive Services. [PubMed] [Google Scholar]
- 25.Healthy People 2010. [Accessed July 16, 2009];7: Educational and community-based programs. http://www.healthypeople.gov/document/HTML/Volume1/07Ed.htm#_Toc490550857.
- 26.Poisal JA, Truffer C, Smith S, et al. Health spending projections through 2016: modest changes obscure part D’s impact. Health Affairs (Millwood) 2007;26(2):w242–w253. doi: 10.1377/hlthaff.26.2.w242. [DOI] [PubMed] [Google Scholar]
- 27.Koretz G. Employers tame medical costs: but workers pick up a bigger share. Bus Week. 2002;26:26. [Google Scholar]
- 28.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health Aff (Millwood) 2010;29(2):304–311. doi: 10.1377/hlthaff.2009.0626. [DOI] [PubMed] [Google Scholar]
- 29.Soler RE, Leeks KD, Razi S, et al. A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. Am J Prev Med. 2010;38(2, Supplement 1):S237–S262. doi: 10.1016/j.amepre.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 30.Chapman LS. Meta-evaluation of worksite health promotion economic return studies: 2005 update. Am J Health Promot. 2005;19(6):1–11. doi: 10.4278/0890-1171-19.4.TAHP-1. [DOI] [PubMed] [Google Scholar]
- 31.Holzbach RL, Piserchia PV, McFadden DW, Hatwell TD, Herrman A, Fielding JE. Effect of a comprehensive health promotion program on employee attitudes. J Occup Med. 1990;32(10):973–978. [PubMed] [Google Scholar]
- 32.US Department of Labor, Bureau of Labor Statistics. [Accessed August 12, 2010];National census of fatal occupational injuries in 2008. http://www.bls.gov/news.release/pdf/cfoi.pdf. Updated 2008.
- 33.Steenland K, Burnett C, Lalich N, Ward E, Hurrell J. Dying for work: the magnitude of U.S. mortality from selected causes of death associated with occupation. J Am J Ind Med. 2003;43:461–482. doi: 10.1002/ajim.10216. [DOI] [PubMed] [Google Scholar]
- 34.US Department of Labor, Bureau of Labor Statistics. [Accessed August 12, 2010];Workplace injuries and illnesses in 2008. http://www.bls.gov/news.release/pdf/osh.pdf. Updated 2009.
- 35.Sengupta I, Reno V, Burton JJF. [Accessed August 12, 2010];Workers’ compensation: benefits, coverage, and costs. 2007 http://www.nasi.org/research/2009/report-workers-compensation-benefits-coverage-costs-2007. Updated 2009.
- 36.Leigh JP, Markowitz S, Fahs M, Landrigan P. Costs of occupational injuries and illnesses. Ann Arbor: University of Michigan Press; 2000. [Google Scholar]
- 37.Leigh JP, Markowitz SB, Fahs M, Shin C, Landrigan PJ. Occupational injury and illness in the United States. Estimates of costs, morbidity, and mortality. Arch Intern Med. 1997;157(14):1557–1568. [PubMed] [Google Scholar]
- 38.Department of Labor, Bureau of Labor Statistics. Workplace Injury and Illness Summary. Washington, DC: U.S: 2007. [Google Scholar]
- 39.United States Congress, Office of Technology Assessment. Gauging control technology and regulatory impacts in occupational safety and health an appraisal of OSHA’s analytic approach. Washington, DC: 1995. Publication OTA-ENV-635. [Google Scholar]
- 40.Silverstein M. Getting home safe and sound: occupational safety and health administration at 38. Am J Public Health. 2008;98(3):416–423. doi: 10.2105/AJPH.2007.117382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Almeida DM, Wethington E, Chandler AL. Daily Transmission of Tensions between Marital Dyads and Parent-Child Dyads. Journal of Marriage and the Family. 1999;61(1):49–61. [Google Scholar]
- 42.Hammer LB, Allen E, Grigsby TD. Work family conflict in dual-earner couples: within-individual and crossover effects of work and family. Journal of Vocational Behavior. 1997;50(2):185–203. [Google Scholar]
- 43.Punnett L, Cherniack M, Henning R, Morse T, Faghri P The CPH-NEW Research Team. A conceptual framework for the integration of workplace health promotion and occupational ergonomics programs. Public Health Reports Hyattsville. 2009;124(Suppl 1):16–25. doi: 10.1177/00333549091244S103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sorensen G, Barbeau E, Hunt MK, Emmons K. Reducing social disparities in tobacco use: a social contextual model for reducing tobacco use among blue-collar workers. Am J Public Health. 2004;94(2):230–239. doi: 10.2105/ajph.94.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sorensen G, Himmelstein JS, Hunt MK, et al. A model for worksite cancer prevention: integration of health protection and health promotion in the WellWorks project. Am J Health Promot. 1995;10(1):55–62. doi: 10.4278/0890-1171-10.1.55. [DOI] [PubMed] [Google Scholar]
- 46.Institute of Medicine. [Accessed March 12, 2010];Integrating employee health: a model program for NASA. http://www.iom.edu/Reports/2005/Integrating-Employee-Health-A-Model-Program-for-NASA.aspx. Updated 2005.
- 47.Carnethon M, Whitsel LP, Franklin BA, et al. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120(17):1725–1741. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- 48.Goetzel RZ, Ozminkowski RJ. The health and cost benefits of work site health-promotion programs. Annu Rev Public Health. 2008;29:303–323. doi: 10.1146/annurev.publhealth.29.020907.090930. [DOI] [PubMed] [Google Scholar]
- 49.Healthy People 2010. [Accessed July 16, 2009];7-5: Worksite health promotion programs. http://www.healthypeople.gov/data/midcourse/comments/faobjective.asp?id=7&subid=5.
- 50.Linnan L, Bowling M, Childress J, et al. Results of the 2004 National worksite health promotion survey. Am J Public Health. 2008;98:1503–1509. doi: 10.2105/AJPH.2006.100313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.United States Small Business Administration. [Accessed July 13, 2009];FAQ: advocacy small business statistics and research. http://web.sba.gov/faqs/faqIndexAll.cfm?areaid=24.
- 52.Cherniack M, Lahiri S. Barriers to implementation of workplace health interventions: an economic perspective. Journal of Occupational and Environmental Medicine. doi: 10.1097/JOM.0b013e3181f26e59. In Press. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention. [Accessed July 28, 2009];Early release of selected estimates based on data from the 2008 national health interview survey. http://www.cdc.gov.proxy-hs.researchport.umd.edu/nchs/nhis/released200906.htm#7. Updated 2009.
- 54.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical Activity in the United States Measured by Accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 55.Crawford PB, Gosliner W, Strode P, et al. Walking the talk: fit WIC wellness programs improve self-efficacy in pediatric obesity prevention counseling. Am J Public Health. 2004;94(9):1480–1485. doi: 10.2105/ajph.94.9.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pohjonen T, Ranta R. Effects of worksite physical exercise intervention on physical fitness, perceived health status, and work ability among home care workers: five-year follow-up. Prev Med. 2001;32(6):465–475. doi: 10.1006/pmed.2001.0837. [DOI] [PubMed] [Google Scholar]
- 57.Lara A, Yancey AK, Tapia-Conyer R, et al. Pausa para tu salud: Reduction of weight and waistlines by integrating exercise breaks into workplace organizational routine. Prev Chronic Dis. 2008;5(1):A12. [PMC free article] [PubMed] [Google Scholar]
- 58.Yancey AK. The meta-volition model: organizational leadership is the key ingredient in getting society moving, literally! Prev Med. 2009;49(4):342–351. doi: 10.1016/j.ypmed.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 59.Pronk SJ, Pronk NP, Sisco A, Ingalls DS, Ochoa C. Impact of a daily 10-minute strength and flexibility program in a manufacturing plant. Am J Health Promot. 1995;9(3):175–178. doi: 10.4278/0890-1171-9.3.175. [DOI] [PubMed] [Google Scholar]
- 60.Pronk NP, Kottke TE. Physical activity promotion as a strategic corporate priority to improve worker health and business performance. Prev Med. 2009;49(4):316–321. doi: 10.1016/j.ypmed.2009.06.025. [DOI] [PubMed] [Google Scholar]
- 61.Galinsky T, Swanson N, Sauter S, Dunkin R, Hurrell J, Schleifer L. Supplementary breaks and stretching exercises for data entry operators: a follow-up field study. Am J Ind Med. 2007;50(7):519–527. doi: 10.1002/ajim.20472. [DOI] [PubMed] [Google Scholar]
- 62.Tullar JM, Brewer S, Amick BC, III, et al. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J Occup Rehabil. 2010;20(2):199–219. doi: 10.1007/s10926-010-9231-y. [DOI] [PubMed] [Google Scholar]
- 63.Kennedy CA, Amick BC, III, Dennerlein JT, et al. Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time. J Occup Rehabil. 2010;20(2):127–162. doi: 10.1007/s10926-009-9211-2. [DOI] [PubMed] [Google Scholar]
- 64.Jilcott S, Ammerman A, Sommers J, Glasgow RE. Applying the RE-AIM framework to assess the public health impact of policy change. Ann Behav Med. 2007;34(2):105–114. doi: 10.1007/BF02872666. [DOI] [PubMed] [Google Scholar]
- 65.Institute for Health Research. [Accessed February 27, 2010];RE-AIM. http://www.re-aim.org/index.html.
- 66.Pronk NP, Goetzel RZ. The practical use of evidence. Practice and research connected. Am J Prev Med. 2010;38(2, Supplement 1):S229–S231. doi: 10.1016/j.amepre.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 67.Linnan L, Sorensen G, Colditz G, Klar DN, Emmons KM. Using theory to understand the multiple determinants of low participation in worksite health promotion programs. Health Educ Behav. 2001;28(5):591–607. doi: 10.1177/109019810102800506. [DOI] [PubMed] [Google Scholar]
- 68.Linnan LA, Birken BE. Small businesses, worksite wellness, and public health: a time for action. N C Med J. 2006;67(6):433–437. [PubMed] [Google Scholar]
- 69.Gold MR, Siegal JE, Russell LB, Weinstein MC, editors. Cost-effectiveness in health and medicine. New York: Oxford Univeristy Press; 1996. [Google Scholar]
- 70.Neumann PJ. Using cost-effectiveness analysis to improve health care: opportunities and barriers. New York: Oxford University Press; 2005. [Google Scholar]
- 71.Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 2. New York: Oxford University Press; 2004. [Google Scholar]
- 72.Linnan L. The business case for employee health: what we know and what we must do. In press. [PubMed] [Google Scholar]
- 73.Thaler RH, Sunstein CR. Penguin Books. Nudge: Improving Decision About Health, Wealth And Happiness. New York: 2008. [Google Scholar]
- 74.Akerlof GA, Shiller RJ. Animal Spirits: How Human Psychology Drives The Economy, And Why It Matters For Global Capitalism. Princeton University Press; 2009. [Google Scholar]
- 75.Ariely D. Predictably Irrational: The Hidden Forces That Shape Our Decisions. New York: Harper Collins Publishers; 2008. [Google Scholar]
- 76.Hamalainen P, Takala J, Saarela KL. Global estimates of fatal work-related diseases. Am J Ind Med. 2007;50(1):28–41. doi: 10.1002/ajim.20411. [DOI] [PubMed] [Google Scholar]
- 77.International Agency for Research on Cancer. An updating of IARC monographs. Supplement 7. 1–42. IARC Monographs on the evaluation of carcinogenic risks to humans: overall evaluation of carcinogenicity. [PubMed] [Google Scholar]
- 78.Straif K, Baan R, Grosse Y, et al. Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol. 2007;8(12):1065–1066. doi: 10.1016/S1470-2045(07)70373-X. [DOI] [PubMed] [Google Scholar]
- 79.Schnall P, Belkic K, Landsbergis PA, Baker D. Why the workplace and cardiovascular disease. Occup Med. 2000;15(1):1–6. [PubMed] [Google Scholar]
- 80.Olsen O, Kristensen TS. Impact of work environment on cardiovascular diseases in Denmark. J Epidemiol Community Health. 1991;45(1):4–10. doi: 10.1136/jech.45.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Karasek RA, Theorell T, Schwartz JE, Schnall PL, Pieper CF, Michela JL. Job characteristics in relation to the prevalence of myocardial infarction in the US Health Examination Survey (HES) and the Health and Nutrition Examination Survey (HANES) Am J Public Health. 1988;78(8):910–918. doi: 10.2105/ajph.78.8.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Siegrist J, Rodel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32(6):473–81. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- 83.Kouvonen A, Kivimaki M, Virtanen M, Heponiemi T, Elovainio M, Pentti J, et al. Effort-reward imbalance at work and the co-occurrence of lifestyle risk factors: cross-sectional survey in a sample of 36,127 public sector employees. BMC Public Health. 2006;6:24. doi: 10.1186/1471-2458-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kivimaki M, Leino-Arjas P, Luukkonen R, Riihimaki H, Vahtera J, Kirjonen J. Work stress and risk of cardiovascular mortality: prospective cohort study of industrial employees. BMJ. 2002;325(7369):857. doi: 10.1136/bmj.325.7369.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bongers PM, Kremer AM, Ter Laak J. Are psychosocial factors, risk factors for symptoms and signs of the shoulder, elbow, or hand/wrist?: a review of the epidemiological literature. Am J Ind Med. 2002;41(5):315–342. doi: 10.1002/ajim.10050. [DOI] [PubMed] [Google Scholar]
- 86.Eby LT, Casper WJ, Lockwood A, Bordeaux C, Brinley A. Work and family research in IO/OB: content analysis and review of the literature (1980–2002) J Vocat Behav. 2005;66(1):124–197. [Google Scholar]
- 87.Allen TD, Herst DEL, Bruck CS, Sutton M. Consequences associated with work-to-family conflict: a review and agenda for future research. J Occup Health Psychol. 2000;5(2):278–308. doi: 10.1037//1076-8998.5.2.278. [DOI] [PubMed] [Google Scholar]
- 88.Bureau of Labor Statistics. [Accessed July 13, 2009];Spotlight on statistics: older workers. http://www.bls.gov/spotlight/2008/older_workers/. Updated 2008.
- 89.Ilmarinen JE. Aging workers. Occup Environ Med. 2001;58(8):546–552. doi: 10.1136/oem.58.8.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tuomi K, Huuhtanen P, Nykyri E, Ilmarinen J. Promotion of work ability, the quality of work and retirement. Occup Med (Lond) 2001;51(5):318–324. doi: 10.1093/occmed/51.5.318. [DOI] [PubMed] [Google Scholar]
- 91.Ilmarinen J. Work ability--a comprehensive concept for occupational health research and prevention. Scand J Work Environ Health. 2009;35(1):1–5. doi: 10.5271/sjweh.1304. [DOI] [PubMed] [Google Scholar]
- 92.Alavinia SM, van Duivenbooden C, Burdorf A. Influence of work-related factors and individual characteristics on work ability among Dutch construction workers. Scand J Work Environ Health. 2007;33(5):351–357. doi: 10.5271/sjweh.1151. [DOI] [PubMed] [Google Scholar]
- 93.Kujala V, Tammelin T, Remes J, Vammavaara E, Ek E, Laitinen J. Work ability index of young employees and their sickness absence during the following year. Scand J Work Environ Health. 2006;32(1):75–84. doi: 10.5271/sjweh.979. [DOI] [PubMed] [Google Scholar]
- 94.Liira J, Matikainena E, Leino-Arjasa P, et al. Work ability of middle-aged Finnish construction workers a follow-up study in 1991–1995. Int J Ind Ergon. 2000;25(5):477–481. [Google Scholar]
- 95.Wegman D, McGee J, editors. Health and safety needs of older workers. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 96.Muntaner C, Eaton WW, Miech R, O’Campo P. Socioeconomic position and major mental disorders. Epidemiol Rev. 2004;26:53–62. doi: 10.1093/epirev/mxh001. [DOI] [PubMed] [Google Scholar]
- 97.Landsbergis PA, Schnall PL, Belkic KB, Baker D, Schwartz J, Pickering TG, Quick JC, Tetrick LE. Handbook of Occupational Health Psychology. 2. Vol. 2. Washington DC: American Psychological Association; The workplace and cardiovascular disease. In press. [Google Scholar]
- 98.Karasek RA., Jr Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285–308. [Google Scholar]
- 99.Hallqvist J, Diderichsen F, Theorell T, Reuterwall C, Ahlbom A. Is the effect of job strain on myocardial infarction risk due to interaction between high psychological demands and low decision latitude? Results from Stockholm Heart Epidemiology Program (SHEEP) Soc Sci Med. 1998;46(11):1405–1415. doi: 10.1016/s0277-9536(97)10084-3. [DOI] [PubMed] [Google Scholar]
- 100.Landsbergis PA, Schnall PL, Pickering TG, Warren K, Schwartz JE. Lower socioeconomic status among men in relation to the association between job strain and blood pressure. Scand J Work Environ Health. 2003;29(3):206–215. doi: 10.5271/sjweh.723. [DOI] [PubMed] [Google Scholar]
- 101.Gonzalez MA, Rodriguez Artalejob F, Calero J. Relationship between socioeconomic status and ischemic heart disease in cohort and case-control studies: 1960–1993. Int J Epidemiol. 1998;27(3):350–358. doi: 10.1093/ije/27.3.350. [DOI] [PubMed] [Google Scholar]
- 102.Kanjilal S, Gregg EW, Cheng YJ, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166(21):2348–2355. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- 103.Grosch JW, Alterman T, Petersen MR, Murphy LR. Worksite health promotion programs in the U.S.: factors associated with availability and participation. American journal of health promotion. 1998;13(1):36. doi: 10.4278/0890-1171-13.1.36. [DOI] [PubMed] [Google Scholar]
- 104.Fisher BDGT. Heart check lite: modifications to an established worksite heart health assessment. Am J Health Promot. 2008;22(3):208–212. doi: 10.4278/ajhp.22.3.208. [DOI] [PubMed] [Google Scholar]
- 105.Amick BC, III, Hogg-Johnson SJ. Managing Prevention with Leading and Lagging Indicators in the Workers Compensation System, in Use of Workers’ Compensation Data for Occupational Injury and Illness Prevention Proceedings from September 2009 Workshop. In: Utterback DS, Schnorr TM, editors. DHHS (NIOSH) Document No. 2010–152. Washington DC: 2010. [Google Scholar]
- 106.Schuster MA, Chung PJ, Elliott MN, Garfield CF, Vestal KD, Klein DJ. Awareness and use of California’s Paid Family Leave Insurance among parents of chronically ill children. JAMA. 2008;300(9):1047–1055. doi: 10.1001/jama.300.9.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kelly EL. Failure to update: an institutional perspective on noncompliance with the family and medical leave act. Law & Society Review. 2010;44(1):33–66. [Google Scholar]
- 108.Hammer LB, Zimmerman KL. Handbook of I/O Psychology. In: Zedeck S, editor. Quality of Work Life. 3. Vol. 3. Washington, DC: American Psychological Association; In press. [Google Scholar]
- 109.Greenhaus JH, Beutell NJ. Sources of Conflict between Work and Family Roles. The Academy of Management Review. 1985;10(1):76–88. [Google Scholar]
- 110.Tavares LS, Plotnikoff RC. Not enough time? Individual and environmental implications for workplace physical activity programming among women with and without young children. Health Care Women Int. 2008;29(3):244–281. doi: 10.1080/07399330701880911. [DOI] [PubMed] [Google Scholar]
- 111.Frone MR, Russel M, Cooper ML. Relation of work-family conflict to health outcomes: a four-year longitudinal study of employed parents. Journal of Occupational & Organizational Psychology. 1997;70(4):325–335. [Google Scholar]
- 112.Frone MR. Work-family conflict and employee psychiatric disorders: the national comorbidity survey. J Appl Psychol. 2000;85(6):888–895. doi: 10.1037/0021-9010.85.6.888. [DOI] [PubMed] [Google Scholar]
- 113.Greenhaus JH, Allen TD, Spector PE. Health consequences of work family conflict: the dark side of the work family interface. In: Perrewe PL, Ganster DC, editors. Research in stress and occupational well being. 5. Vol. 5. Emerald; 2006. [Google Scholar]
- 114.Grzywacz JG, Bass BL. Work, family, and mental health: testing different models of work-family fit. Journal of Marriage & Family. 2003;65(1):248–261. [Google Scholar]
- 115.Hammer LB, Cullen JC, Neal MB, Sinclair RR, Shafiro MV. The longitudinal effects of work-family conflict and positive spillover on depressive symptoms among dual-earner couples. J Occup Health Psychol. 2005;10(2):138–154. doi: 10.1037/1076-8998.10.2.138. [DOI] [PubMed] [Google Scholar]
- 116.Melchior M, Berkman LF, Niedhammer I, Zins M, Goldberg M. The mental health effects of multiple work and family demands. A prospective study of psychiatric sickness absence in the French GAZEL study. Soc Psychiatry Psychiatr Epidemiol. 2007;42(7):573–582. doi: 10.1007/s00127-007-0203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Grzywacz JG. Work-family spillover and health during midlife: is managing conflict everything? Am J Health Promot. 2000;14(4):236–243. doi: 10.4278/0890-1171-14.4.236. [DOI] [PubMed] [Google Scholar]
- 118.Vaananen A, Kalimo R, Toppinen-Tanner S, et al. Role clarity, fairness, and organizational climate as predictors of sickness absence: a prospective study in the private sector. Scand J Public Health. 2004;32(6):426–434. doi: 10.1080/14034940410028136. [DOI] [PubMed] [Google Scholar]
- 119.Kossek EE, Ozeki C. Work-family conflict, policies, and the job-life satisfaction relationship: a review and directions for organizational behavior-human resources research. J Appl Psychol. 1998;83(2):139–149. [Google Scholar]
- 120.Allen TD, Armstrong J. Further examination of the link between work-family conflict and physical health: the role of health-related behaviors. American Behavioral Scientist. 2006;49:1204–1221. [Google Scholar]
- 121.Ingersoll-Dayton Berit, Schiller Amy R, Neal MB, Jung-Hwa Ha MB, Hammer LB. Collaboration among siblings providing care for older parents. Journal of Gerontological Social Work. 2003;40(3):51–66. [Google Scholar]
- 122.Allen TD. Family-supportive work environments: the role of organizational perceptions. J Vocat Behav. 2001;58(3):414–435. [Google Scholar]
- 123.Hammer LB, Kossek EE, Anger WK, Bodner T, Zimmerman K. Clarifying work-family intervention processes: the roles of work-family conflict and family supportive supervisor behaviors. Journal of Applied Psychology. doi: 10.1037/a0020927. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kelly EL, Kossek EE, Hammer LB, et al. Getting there from here: research on the effects of work-family initiatives on work-family conflict and business outcomes. In: Walsh JP, Brief A, editors. The Academy of Management Annals. 2. Vol. 2. Routledge; 2008. pp. 305–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Golden L. Flexible work schedules: Which workers get them? The American Behavioral Scientist. 2001;44:1157–1178. [Google Scholar]
- 126.Lambert S, Waxman E. Organizational stratification: distributing opportunities for work-life balance. In: Kossek E, Lambert S, editors. Work and Life Integration: Organizational, Cultural, and Individual Perspectives. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. pp. 103–126. [Google Scholar]
- 127.Swanberg J, Catsouphes M, Drescher-Burke K. A question of justice: disparities in employees’ access to flexible schedule arrangements. Journal of Family Issues. 2005;26:866–895. [Google Scholar]
- 128.Sorensen G, Stoddard A, Hunt MK, et al. The effects of a health promotion-health protection intervention on behavior change: the WellWorks study. Am J Public Health. 1998;88(11):1685–1690. doi: 10.2105/ajph.88.11.1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.National Institute for Occupational Safety and Health. The Changing Organization of Work and the Safety and Health of Working People. 2002–116 2002. [Google Scholar]
- 130.Sorensen G, Stoddard AM, LaMontagne AD, et al. A comprehensive worksite cancer prevention intervention: behavior change results from a randomized controlled trial (United States) Cancer Causes and Control. 2002;13(6):493–502. doi: 10.1023/a:1016385001695. [DOI] [PubMed] [Google Scholar]
- 131.Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multiethnic workers: results of the healthy directions-small business study. Am J Public Health. 2005;95(8):1389–1395. doi: 10.2105/AJPH.2004.038745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Landsbergis PA, Sinclair R, Dobson M, et al. Occupational Health Psychology. In: Anna D, editor. The Occupational Environment: Its Evaluation, Control, and Management. 3. American Industrial Hygiene Association; In press. [Google Scholar]
- 133.National Institute for Occupational Safety and Health. [Accessed February 27, 2010];WorkLife. http://www.cdc.gov.proxy-hs.researchport.umd.edu/niosh/worklife/default.html. Updated 2010.
- 134.National Institute for Occupational Safety and Health. NIOSH WorkLife Initiative. [Accessed March 11, 2010];Essential elements of effective workplace programs and policies for improving worker health and wellbeing. http://www.cdc.gov.proxy-hs.researchport.umd.edu/niosh/worklife/essentials.html. Updated 2009.
- 135.Kaiser Permanente Center for Health Research. [Accessed March 11, 2010];Work, family and health network. http://www.kpchr.org/workfamilyhealthnetwork/public/default.aspx. Updated 2008.
- 136.Holmes JH, Lehman A, Hade E, et al. Challenges for multilevel health disparities research in a transdisciplinary environment. Am J Prev Med. 2008;35(2, Supplement 1):S182–S192. doi: 10.1016/j.amepre.2008.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Stokols D, Misra S, Moser RP, Hall KL, Taylor BK. The ecology of team science: understanding contextual influences on transdisciplinary collaboration. Am J Prev Med. 2008;35(2, Supplement 1):S96–S115. doi: 10.1016/j.amepre.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 138.Kruger J, Yore MM, Bauer DR, Kohl HW. Selected barriers and incentives for worksite health promotion services and policies. Am J Health Promot. 2007;21(5):439–447. doi: 10.4278/0890-1171-21.5.439. [DOI] [PubMed] [Google Scholar]
- 139.Orlandi MA. The diffusion and adoption of worksite health promotion innovations: an analysis of barriers. Prev Med. 1986;15(5):522–536. doi: 10.1016/0091-7435(86)90028-9. [DOI] [PubMed] [Google Scholar]
- 140.Schult TM, McGovern PM, Dowd B, Pronk NP. The future of health promotion/disease prevention programs: the incentives and barriers faced by stakeholders. J Occup Environ Med. 2006;48(6):541–548. doi: 10.1097/01.jom.0000222565.68934.0b. [DOI] [PubMed] [Google Scholar]
- 141.Maceachen E, Kosny A, Ferrier S, Chambers L. The “Toxic Dose” of System Problems: Why Some Injured Workers Don’t Return to Work as Expected. J Occup Rehabil. 2010 Feb 7; doi: 10.1007/s10926-010-9229-5. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 142.Amick BC, III, Habeck RV, Hunt A, et al. Measuring the impact of organizational behaviors on work disability prevention and management. Journal of Occupational Rehabilitation. 2000;10(1):21–38. [Google Scholar]
- 143.Bull SS, Gillette C, Glasgow RE, Estabrooks P. Work site health promotion research: to what extent can we generalize the results and what is needed to translate research to practice? Health Educ Behav. 2003;30(5):537–549. doi: 10.1177/1090198103254340. [DOI] [PubMed] [Google Scholar]
- 144.Kelly EL, Moen P. Rethinking the clockwork of work: why schedule control may pay off at work and at home. Advances in Developing Human Resources. 2007;9(4):487–506. doi: 10.1177/1523422307305489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Thompson SE, Smith BA, Bybee RF. Factors influencing participation in worksite wellness programs among minority and underserved populations. Fam Community Health. 2005;28(3):267–273. doi: 10.1097/00003727-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 146.Sorensen G, Barbeau EM, Stoddard AM, et al. Tools for health: the efficacy of a tailored intervention targeted for construction laborers. Cancer Causes and Control. 2007;18(1):51–59. doi: 10.1007/s10552-006-0076-9. [DOI] [PubMed] [Google Scholar]
- 147.Barbeau EM, Hartman C, Quinn MM, Stoddard AMKN. Methods for recruiting White, Black, and Hispanic working-class women and men to a study of physical and social hazards at work: the united for health study. Int J Health Serv. 2007;37(1):127–144. doi: 10.2190/B0N2-5850-6467-0230. [DOI] [PubMed] [Google Scholar]
- 148.Pronk NP. Designing and evaluating health promotion programs: simple rules for a complex issue. Disease Management & Health Outcomes. 2003;11(3):149–157. [Google Scholar]
- 149.Linnan L, Weiner B, Graham A, Emmons K. Manager beliefs regarding worksite health promotion: findings from the Working Healthy Project 2. Am J Health Promot. 2007;21(6):521–528. doi: 10.4278/0890-1171-21.6.521. [DOI] [PubMed] [Google Scholar]
- 150.Landsbergis PA. The changing organization of work and the safety and health of working people: a commentary. J Occup Environ Med. 2003;45(1):61–72. doi: 10.1097/00043764-200301000-00014. [DOI] [PubMed] [Google Scholar]
- 151.Schulz AJ, Israel BA, Lantz P. Instrument for evaluating dimensions of group dynamics within community-based participatory research partnerships. Eval Program Plann. 2003;26(3):249–262. [Google Scholar]
- 152.Benedict MA, Arterburn D. Worksite-based weight loss programs: a systematic review of recent literature. Am J Health Promot. 2008;22(6):408–416. doi: 10.4278/ajhp.22.6.408. [DOI] [PubMed] [Google Scholar]
- 153.Lahiri S, Gold J, Levenstein C. Estimation of net-costs for prevention of occupational low back pain: three case studies from the US. Am J Ind Med. 2005;48(6):530–541. doi: 10.1002/ajim.20184. [DOI] [PubMed] [Google Scholar]
- 154.Lahiri S, Markkanen P, Levenstein C. The cost effectiveness of occupational health interventions: preventing occupational back pain. American Journal of Industrial Medicine. 2005;48(6):515–529. doi: 10.1002/ajim.20193. [DOI] [PubMed] [Google Scholar]
- 155.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27(1):3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 156.Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93(8):1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kramer DM, Cole DC, Leithwood K. Doing knowledge transfer: engaging management and labor with research on employee health and safety. Bulletin Of Science, Technology Society. 2004;24(4):316–330. [Google Scholar]
- 158.Bowen S, Zwi AB. Pathways to “evidence informed” policy and practice: a framework for action. PLoS Med. 2005;2(7):e166. doi: 10.1371/journal.pmed.0020166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Green LW, Ottoson JM, Garcia C, Hiatt RA. Diffusion theory, and knowledge dissemination, utilization, and integration in public health. Annu Rev Public Health. 2009;30:151–174. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- 160.Engbers L. Monitoring and evaluation of worksite health promotion programs - current state of knowledge and implications for practice. [Accessed July 17, 2009];Background paper prepared for the WHO/WEF joint event on preventing noncommunicable diseases in the workplace. http://www.who.int/dietphysicalactivity/Engbers-monitoringevaluation.pdf. Updated 2008.
- 161.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]