Abstract
Efforts have recently been reported by several research groups on the development of computer-controlled lower limb orthoses to enable legged locomotion in persons with paraplegia. Such systems must employ a control framework that provides essential movements to the paraplegic user (i.e., sitting, standing, and walking), and ideally enable the user to autonomously command these various movements in a safe, reliable, and intuitive manner. This paper describes a control method that enables a paraplegic user to perform sitting, standing, and walking movements, which are commanded based on postural information measured by the device. The proposed user interface and control structure was implemented on a powered lower limb orthosis, and the system was tested on a paraplegic subject with a T10 complete injury. Experimental data is presented that indicates the ability of the proposed control architecture to provide appropriate user-initiated control of sitting, standing, and walking. The authors also provide a link to a video that qualitatively demonstrates the user’s ability to independently control basic movements via the proposed control method.
1 Introduction
One of the most significant impairments resulting from paraplegia is the loss of mobility, particularly given the relatively young age at which such injuries occur [1-3]. In addition to diminished mobility, the inability to stand and walk entails significant physiological impairments, including muscular atrophy, loss of bone mineral content, frequent skin breakdown problems, increased incidence of urinary tract infection, muscle spasticity, impaired lymphatic and vascular circulation, impaired digestive operation, and reduced respiratory and cardiovascular capacities [4].
In an effort to facilitate legged locomotion in individuals with paraplegia, several computer-controlled lower limb orthosis systems have been, and are being, developed and described in the research literature. Some of these include hybrid FES-systems, which combine a computer-controlled orthosis with computer-controlled functional electrical stimulation (FES) of leg muscles, such as the systems described by [5-9]. Recently, a number of powered lower limb orthoses, or exoskeletons, have also been described for purposes of gait assistance for persons with paraplegia, including those described by [10-16]. In addition to these systems, two other exoskeleton systems, developed by commercial entities, are those by Argo Medical Technologies (ReWalk) and Berkeley Bionics (eLEGS). Technical information regarding these two systems have not yet appeared in the engineering literature. In the aforementioned publications describing computer-controlled orthoses (i.e., [5-16]), the authors focus on the capacity of their respective systems to provide legged mobility, but do not focus on specifically on control methods that enable the user to autonomously command various movements. In order to demonstrate mobility, these approaches have either incorporated push-button controls on the stability aid, or have incorporated a system operator, who operates the system (e.g., from a host computer) on behalf of the paraplegic individual. The emerging commercial systems, ReWalk and eLEGS, presumably provide for autonomous user control. To the authors’ knowledge, however, no information has been published in the engineering literature regarding the control methods incorporated by either of these systems. Based on product information available from the respective companies, the ReWalk exoskeleton appears to utilize a tilt-sensor on the torso to gate subsequent steps while walking, and utilizes a wrist-mounted keypad to select between other types of movements. The eLEGS exoskeleton reportedly utilizes instrumentation on the forearm crutches or walker to gate subsequent steps while walking.
To the authors’ knowledge, no publication in the engineering literature has described and demonstrated a method that enables a paraplegic user to intuitively and autonomously control (i.e., without push-button controls or the assistance of a system operator) the basic movements associated with legged mobility (i.e., sitting, standing, and walking). As such, this paper presents a control architecture for a powered lower limb orthosis (or exoskeleton) designed to enable a paraplegic user to autonomously navigate through these movements, without the use of their hands or the aid of an external operator. Specifically, the control architecture enables the user to switch between sitting, standing, and walking, based on the user’s upper body movement. The control architecture was implemented on a powered lower limb orthosis and evaluated on a paraplegic subject with a T10 motor and sensory complete injury (i.e., American Spinal Injury Association, ASIA, A classification). The ability of the user to autonomously control the system was assessed by having the paraplegic user repeatedly perform a timed-up-and-go (TUG) test, which is a standard clinical measure of legged mobility. The paper describes the control architecture and its implementation, and presents experimental results of the TUG tests. The test results support the ability of the proposed control architecture to enable user-autonomous control of the basic movements associated with legged mobility.
2 Powered Orthosis Prototype
Although the proposed control interface is generally applicable to a number of computer-controlled lower limb orthoses (such as those previously described), for purposes of this paper, the architecture was implemented on the powered lower limb orthosis shown in Fig. 1. Specifically, the orthosis shown in Fig. 1 incorporates four motors, which impose sagittal plane torques at each hip and knee joints. As seen in the figure, the orthosis contains five segments, which are: two shank segments, two thigh segments, and one hip segment. Each thigh piece contains two brushless DC motors which are used to drive the hip and knee articulations through a speed-reduction transmission. Each joint can provide up to 12 Nm of continuous torque and 40 Nm for shorter (i.e., 2-sec) durations. As a safety measure, both knee joints include normally locked brakes, in order to preclude knee buckling in the event of a power failure. The system does not contain foot or ankle components, but is designed to be used in conjunction with a standard ankle foot orthosis (AFO) to provide stability for the ankle, and to preclude foot drop during the swing phase of gait. Physical sensing in the orthosis consists of Hall-effect-based angle and angular velocity sensing in each hip and knee joint, and 3-axis accelerometers and single-axis gyroscopes in each thigh segment. A pair of microcontrollers located in the thigh segments, provide low-level control of the orthosis. In the current implementation, the microcontrollers communicate with a host computer via a data tether, which facilitates controller development and data visualization. All power on the orthosis is provided by a lithium polymer battery located in the hip segment (see Fig. 1). A functional schematic of the embedded system on the orthosis is shown in Fig. 2.
Fig. 1.
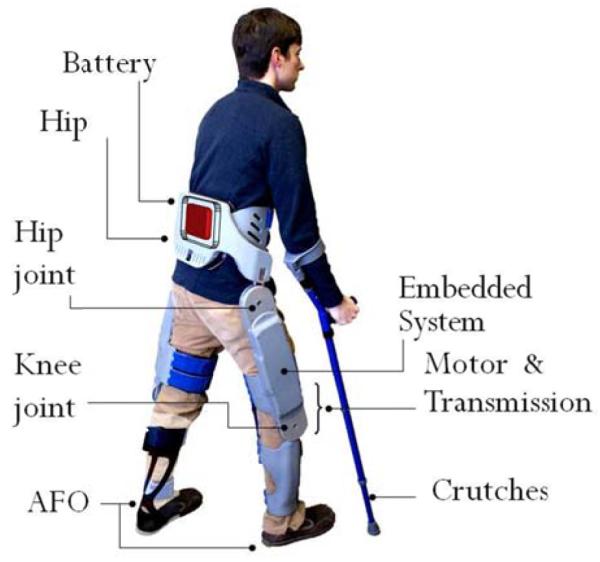
Powered lower limb orthosis.
Fig. 2.
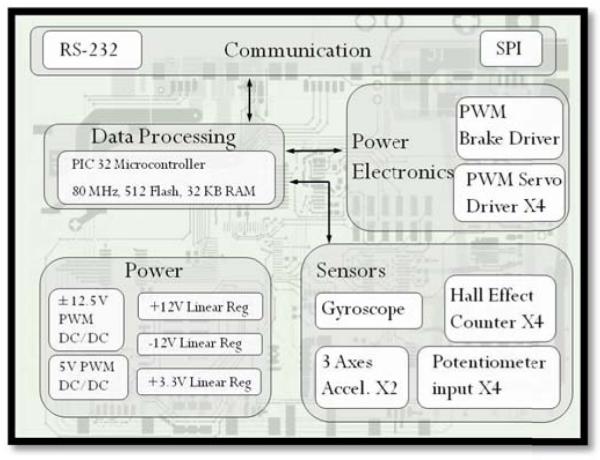
Functional schhematic of embedded system.
3 Powered Orthosis Control Architecture
3.1 Joint-Level Controllers
The general control structure of the orthosis consists of variable-impedance joint-level controllers, the behavior of which is supervised by an event-driven finite-state controller. The joint-level controllers consist of variable-gain proportional-derivate (PD) feedback controllers around each (hip and knee) joint, where at any given time, the control inputs into each controller consists of the joint angle reference, in addition to the proportional and derivative gains of the feedback controller. Note that the latter are constrained to positive values, in order to ensure stability of the feedback controllers. With this control structure, in combination with the open-loop low output impedance of the orthosis joints, the joints can either be controlled in a high-impedance trajectory tracking mode, or in a (relatively) low-impedance mode, by emulating physical spring-damper couples at each joint. The former is used where it may be desirable to enforce a predetermined trajectory (e.g., during the swing phase of gait), while the latter is used when it may be preferable not to enforce a pre-determined joint trajectory, but rather to provide assistive torques that facilitate movement toward a given joint equilibrium point (as in transitioning from sitting to standing), or to impose dissipative behavior at the joint (as in transitioning from standing to sitting).
3.2 Finite-State Control Structure
The joint-level controller receives trajectory commands, as well as PD gains, from a supervisory finite-state machine (FSM), which (for sitting, standing, and walking) consists of 12 states, as shown in Fig. 3. The FSM consists of two types of states: static states and transition states. The static states consist of sitting (S1), standing (S2), right-leg-forward (RLF) double support (S3), and left-leg-forward (LLF) double support (S4). The remaining 8 states, which transition between the four static states, include sit-to-stand (S5), stand-to-sit (S6), stand-to-walk with right half step (S7), stand-to-walk with left half step (S11), walk-to-stand with left half step (S10), walk-to-stand with right half step (S12), right step (S9), and left step (S8).
Fig. 3.
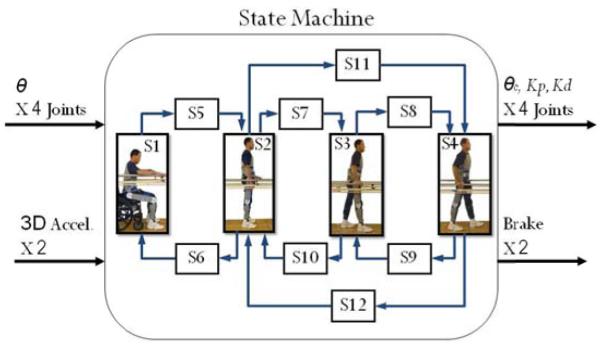
Finite state machine for sitting, standing, and walking.
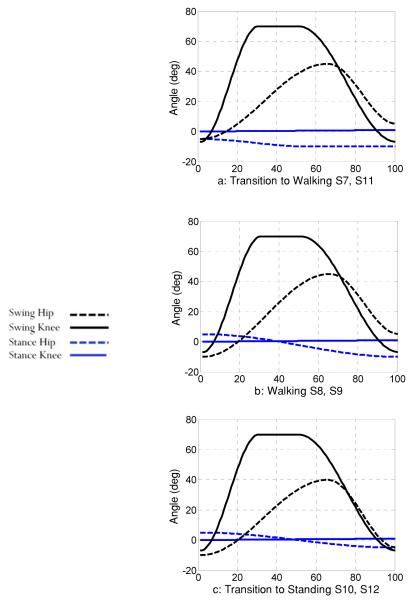
Each state in the FSM is fully defined by the combination of a set of trajectories, and a set of joint feedback gains. In general, the latter are either high or low. The set of trajectories utilized in six of the eight transition states are shown in Fig. 4. For all the trajectories shown in Fig. 4, the joint feedback gains are set high. The final angles of the trajectories shown in Fig. 4 for the various joints define the constant joint angles that correspond to the static states of RLF double support (S3), LLF double support (S4), and standing (S2). Three states remain, which are the static state of sitting and the two transition states of sit-to-stand and stand-to-sit. The static state of sitting (S1) is defined by zero gains, and therefore the joint angles are unimportant. The transition from stand-to-sit (S6) consists of a zero proportional gain and a high derivate gain (i.e., damping without stiffness). Thus, the joint angles are also immaterial for this state, assuming they are constant. Finally, the sit-to-stand (S5) state is defined by standing (S2) joint angles, and utilizes a set of PD gains that ramp up from zero to a value that corresponds to a high impedance state. Table I and Fig. 4 summarize the trajectories and nature of the feedback gains that together define completely the behavior in all states of the FSM shown in Fig. 3
Fig. 4.
Walking trajectories corresponding to finite states as indicated.
Table 1.
Joint controller characteristics within each state
|
| |||
|---|---|---|---|
| CONTROL CHARACTERISTICS IN EACH STATE | |||
| State | Type | Gains | Control Priority |
| S1- Sitting | Static | Low | NA |
| S2- Standing | Static | High | Position |
| S3- Right Forward | Static | High | Position |
| S4- Left Forward | Static | High | Position |
| S5- 1 to 2 | Transition | N.A | Gain |
| S6- 2 to 1 | Transition | N.A | Gain |
| S7- 2 to 3 | Transition | High | Trajectory |
| S8- 3 to 4 | Transition | High | Trajectory |
| S9- 4 to 3 | Transition | High | Trajectory |
| S10- 3 to 2 | Transition | High | Trajectory |
| S11- 2 to 4 | Transition | High | Trajectory |
| S12- 4 to 2 | Transition | High | Trajectory |
3.3 Switching between States
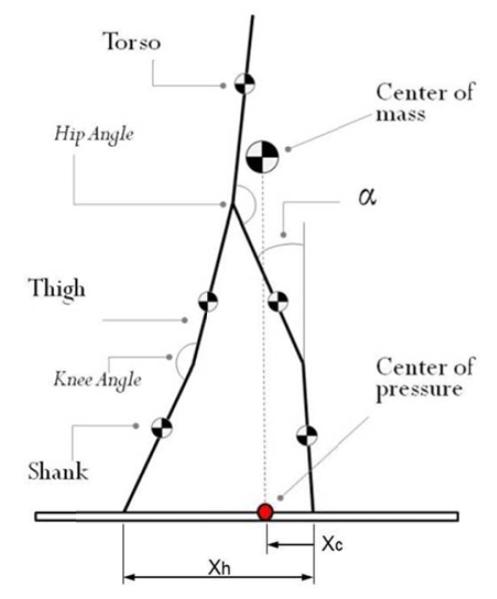
The volitional command of the basic movements in the FSM is based on the location of the (estimated) center of pressure (CoP), defined for the (assumed quasistatic user/orthosis) system as the center of mass projection onto the (assumed horizontal) ground plane. This notion is illustrated in Fig. 5, which indicates the approximate location of the CoP, relative to the forward-most heel. It is assumed that, with the use of the stability aid, the user can affect the posture of his or her upper body, and thus can affect the location of the CoP. By utilizing the accelerometers in the orthosis, which provide a measure of the thigh segment angle (α in Fig. 5) relative to the inertial reference frame (i.e., relative to the gravity vector), in combination with the joint angle sensors (which provide a measure of the configuration of the orthosis and user), the orthosis controller can estimate the location of the CoP (in the sagittal plane). More specifically, in this estimation, the authors assume level ground; that the heels remain on the ground; that the head, arms, and trunk (HAT) can be represented as a single segment with fixed inertial properties; and that out-of-sagittal-plane motion is small. Given these assumptions, along with estimates of the length, mass and location of center of mass of each segment (right and left shank, right and left thigh, and HAT), the controller can estimate the projection of the CoP on the ground. Let the distance from the forward-most heel to the CoP be Xc, where a positive value indicates that the CoP lies anterior to the heel, and a negative number indicates the CoP lies posterior to the heel (see Fig. 5). From a state of double support (S3 or S4), the user commands the next step by moving the CoP forward, until it meets a prescribed threshold, at which point the FSM will enter either the right step or left step states, depending on which foot started forward. From a standing position (S2), the user commands a step by similarly moving the CoP forward until it meets a prescribed threshold, but also leaning to one side in the frontal plane (as indicated by the 3-axis accelerometers in the thigh segments), which indicates that the orthosis should step with the leg opposite the direction of frontal plane lean (i.e., step forward with the presumably unweighted leg). That is, leaning to the right (and moving the CoP forward) will initiate a left step, while leaning to the left (and moving the CoP forward) will initiate a right step. In order to transition from a standing state (S2) to a sitting state, the user shifts the CoP rearward, such that the CoP lies behind the user. Finally, to transition from a sitting to a standing state (S1 to S2), the user leans forward (as illustrated in Fig. 6a), which shifts the CoP forward to a predetermined threshold, which initiates the transition from sitting to standing. Note that the right portion of Fig. 6 shows the case where the user’s CoP is not sufficiently forward to initiate a transition from sitting to standing. Finally the transition from (either case of) double support to standing (i.e., from either S3 or S4, to S2) is based on the timing associated with crossing the CoP threshold. That is, if the CoP does not cross the CoP threshold within a given time following heel strike (i.e., if the controller remains in either state S3 or S4 for a given duration), subsequent crossing of the CoP threshold will transition to standing (S2) rather than to the corresponding double support configuration. That is, a sufficient pause during gait indicates to the system that the user wishes to stand, rather than continue walking forward. A summary of all switching conditions, governing the user interface with the FSM controller, is given in Table 2.
Fig. 5.
Schematic indicating estimated stride length (Xh) and center of pressure (Xc), both estimated based on the configuration of the orthosis.
Fig. 6.
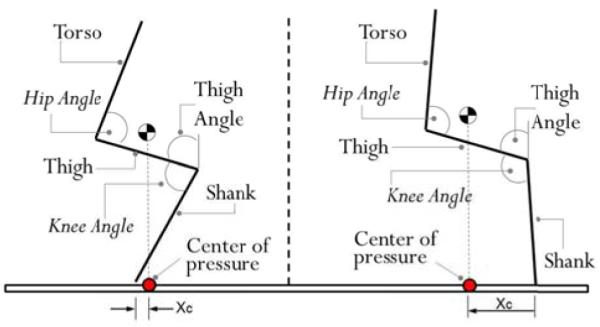
Schematic indicating the use of center of pressure (Xc) estimate for purposes of sit-to-stand and stand-to-sit transitions.
Table 2.
Finite state controller switching conditions
| STATE MACHINE SWITCHING CONDITIONS | |
|---|---|
|
| |
| Transition | Condition |
| S1 to S5 | The user leans forward and pushes up. |
| S5 to S2 | Hip and knee joints meet the Standing (S2) configuration. |
| S2 to S7 | The user leans forward and left. |
| S7 to S3 | Hip and knee joints meet the Right Forward (S3) configuration. |
| S3 to S8 | The user leans forward. |
| S8 to S4 | Hip and knee joints meet the Left Forward (S4) configuration. |
| S4 to S9 | The user leans forward. |
| S9 to S3 | Hip and knee joints meet the Right Forward (S3) configuration. |
| S3 to S10 | The user pauses for a predetermined period prior to leaning forward. |
| S10 to S2 | Hip and knee joints meet the Standing (S2) configuration. |
| S2 to S6 | The user leans backward. |
| S6 to S1 | A predetermined time has lapsed. |
| S2 to S11 | The user leans forward and right. |
| S11 to S4 | Hip and knee joints meet the Left Forward (S4) configuration. |
| S4 to S12 | The user pauses for a predetermined period prior to leaning forward. |
| S12 to S2 | Hip and knee joints meet the Standing (S2) configuration. |
The previous discussion indicates that the user-initiated right and left steps occur when the estimated location of the CoP (relative to the forward heel) exceeds a given threshold. The authors have found that this approach provides enhanced robustness when this threshold is a function of the step length. That is, despite high-gain trajectory control in the joints of the orthosis during swing phase, scuffing of the foot on the ground, as occasionally occurs, in combination with compliance in the orthosis structure, can alter the step length during walking. In the case of a small step length, the forward thigh is nearly vertical, and the user is more easily able to move the CoP forward of the forward heel. In the case of a large step length, the forward thigh is forms a larger angle with the vertical, and moving the CoP forward is more difficult. As such, the CoP threshold during walking was constructed as a linear function, where the CoP threshold (i.e., the amount the CoP must lie ahead of the forward heel) decreases with increasing step size.
4 Experimental Implementation
The proposed control architecture (defined by Fig. 3, Table 1, and Table 2) was implemented on the previously described powered lower limb orthosis, and the ability of the system to enable a user to autonomously perform the basic movements associated with legged mobility (i.e., sitting, standing, and level walking) was assessed in preliminary trials conducted with a paraplegic subject. The subject was a 35-year-old male (1.85 m, 73 kg) with a T10 motor and sensory complete injury (i.e., ASIA A), 9 years post injury. The evaluations were conducted at the Shepherd Center (Atlanta GA, USA), a rehabilitation hospital specializing in spinal cord injury. The testing was approved by both the respective Vanderbilt University and Shepherd Center Institutional Review Boards. All data presented here corresponds to walking conducted using a walker as a stability aid. The subject is shown wearing the orthosis and using the walker in Fig. 7.
Fig. 7.

Photographic sequences showing standing, a left step, and a right step.
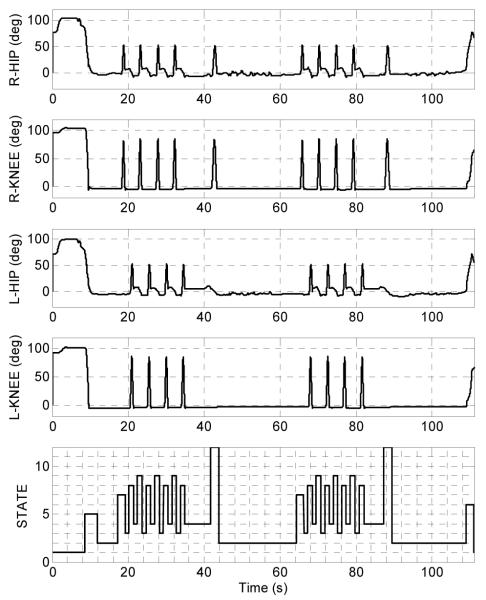
The ability of the powered orthosis and control architecture to provide autonomously commanded sitting, standing, and walking was assessed by having the subject autonomously perform a timed-up-and-go (TUG) test. The TUG test is a standard clinical measure for assessing legged mobility [17]. In this test the subject starts seated in a chair, and given a start command, stands up, walks forward three meters, turns around in place, walks back to the starting point, and sits down in the chair. In order to assess the ability of the subject to autonomously control movements of the orthosis, this test was repeated a number of times, until the subject was comfortable performing the test. Once comfortable with the task, the subject was asked to repeat the TUG test three times. The set of data that corresponds to the third of these three TUG tests is shown in Fig. 8. Specifically, the figure shows the right and left hip and knee joint angles corresponding to this TUG test, along with the corresponding states of the FSM. In the sequence, the user starts in the sitting state (S1), after which the system enters the sitting to standing mode (S5), in which both hips and both knees provide torques to facilitate joint extension. Following S5, the state history depicts a series of consecutive steps, followed by a period of standing (S2), during which the subject turned in place, with the aid of the walker. The first series of steps is then followed by a second series, during which the subject returned to the chair. Once at the chair, the subject again entered standing mode (S2), allowing the subject to turn in place, prior to returning to a seated position in the chair. A video of actual TUG test corresponding to this data can be viewed at: http://research.vuse.vanderbilt.edu/cim/quinteroetal.wmv.
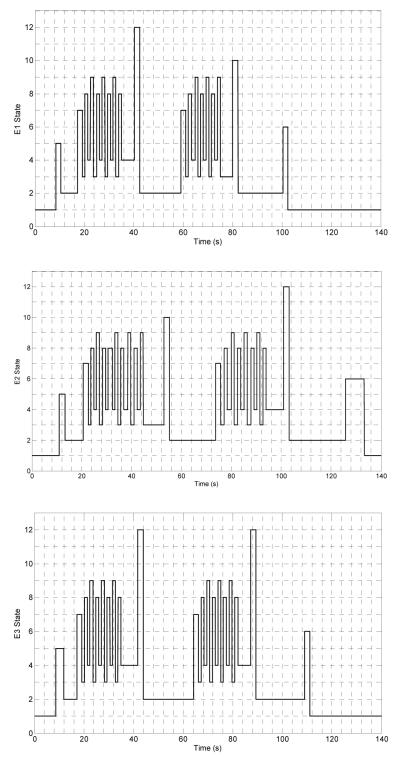
Fig. 8.
Joint angles and controller state during the third TUG test.
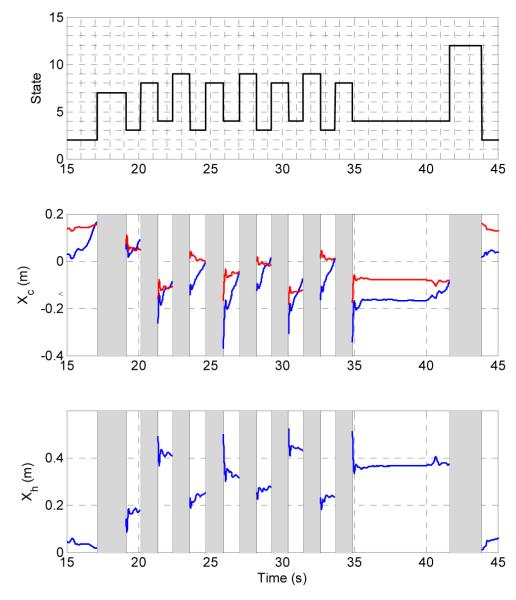
Recall that the threshold for the CoP during walking is function of the step length. Figure 9 shows the system state, the estimated CoP (Xc), and the CoP switching threshold (Xč) for several steps (of slightly varying length). As seen in the figure, the CoP threshold (Xč) varies with step length (Xh). In general, when the CoP (Xc) exceeds the threshold at the end of the swing phase trajectory, the controller will switch immediately to the contralateral swing phase (i.e., switching between S8 and S9). If the CoP does not cross the CoP threshold at the end of swing phase, the controller will remain in the respective double support phase (S3 or S4) until the user shifts the CoP to cross the CoP threshold.
Fig. 9.
Data excerpted from Fig. 8. Top row: finite state corresponding to a sequence of steps. Middle row: center of pressure estimate (Xc, blue) and center of pressure threshold (Xc, red). Bottom row: step length estimate (Xh).
Figure 10 presents the sequences of finite states corresponding to each of the three TUG tests. The subject completed the three tests in 103, 128, and 112 s, respectively. The average time to complete the sequence was 114 s, with a standard deviation of 8.6 s (7.5%). The consistency between trials (i.e., standard deviation of ±7.5%) indicates that the control approach appeared to provide a repeatable means for the subject to control the basic movements associated with legged mobility.
Fig. 10.
Finite states corresponding to each of the three TUG tests.
5 Conclusion
This paper presents a method for the control of a powered orthosis that enables autonomous (user-controlled) basic legged mobility, including sitting, standing, and walking, for persons with paraplegia (i.e., enables the user to autonomously navigate through these movements, without the aid of push-buttons or an external operator). The architecture, summarized by Fig. 3 and Tables 1 and 2, incorporates a finite state structure, in which the joints assume either high or low output impedance, depending on the current finite state. Switching between finite states is largely dependent on an estimate of the location of the CoP relative to the forward heel. The approach was implemented on a powered lower limb orthosis and was assessed by having a subject with a T10 complete injury autonomously perform a series of timed-up-and-go tests. The ability of the subject to perform these tests, and the consistency of the movement between tests, indicate that the control methodology was effective in enabling the user to autonomously perform the basic movements associated with legged mobility (i.e., sitting, standing, and walking).
References
- [1].Spinal Cord Injury Facts and Figures at a Glance. 2011 doi: 10.1179/204577211X13218754005537. https://www.nscisc.uab.edu. [DOI] [PMC free article] [PubMed]
- [2].Brown-Triolo DL, Roach MJ, Nelson K, Triolo RJ. Consumer perspectives on mobility: implications for neuroprosthesis design. Journal of Rehabilitation Research and Development. 2002:659–669. [PubMed] [Google Scholar]
- [3].Hanson RW, Franklin MR. Sexual loss in relation to other functional losses for spinal cord injured males. Archives of Physical Medicine and Rehabilitation. 1976;57:291–293. [PubMed] [Google Scholar]
- [4].Phillips L, Ozer M, Axelson P, Fonseca J. Spinal cord injury: A guide for patient and family. Raven Press; 1987. [Google Scholar]
- [5].Audu ML, To CS, Kobetic R, Triolo RJ. Gait evaluation of a novel hip constraint orthosis with implication for walking in paraplegia. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2010;18(6):610–618. doi: 10.1109/TNSRE.2010.2047594. [DOI] [PubMed] [Google Scholar]
- [6].Kobetic R, To CS, Schnellenberger JR, Audu ML, Bulea TC, Gaudio R, Pinault G, Tashman S, Triolo RJ. Development of hybrid orthosis for standing, walking, and stair climbing after spinal cord injury. Journal of Rehabilitation Research & Development. 2009;43(3):447–462. [PubMed] [Google Scholar]
- [7].To CS, Kobetic R, Schnellenberger JR, Audu ML, Triolo RJ. Design of a variable constraint hip mechanism for a hybrid neuroprosthesis to restore gait after spinal cord injury. IEEE/ASME Transactions on Mechatronics. 2008;13(2):197–205. [Google Scholar]
- [8].Durfee WK, Rivard A. Design and Simulation of a Pneumatic, Stored-energy, Hybrid Orthosis for Gait Restoration. Journal of Biomechanical Engineering. 2005;127(6):1014–1019. doi: 10.1115/1.2050652. [DOI] [PubMed] [Google Scholar]
- [9].Goldfarb M, Korkowski K, Harrold B, Durfee W. Preliminary evaluation of a controlled-brake orthosis for FES-aided gait. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2003;11(3):241–248. doi: 10.1109/TNSRE.2003.816873. [DOI] [PubMed] [Google Scholar]
- [10].Ohta Y, Yano H, Suzuki R, Yoshida M, Kawashima N, Nakazawa K. A two-degree-of-freedom motor-powered gait orthosis for spinal cord injury patients. Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine. 2007;221(6):629–639. doi: 10.1243/09544119JEIM55. [DOI] [PubMed] [Google Scholar]
- [11].Kwa HK, Noorden JH, Missel M, Craig T, Pratt JE, Neuhaus PD. Development of the IHMC mobility assist exoskeleton; Proceedings of the 2009 IEEE international conference on Robotics and Automation; IEEE Press, Kobe, Japan. 2009.pp. 1349–1355. [Google Scholar]
- [12].Neuhaus PD, Noorden JH, Craig TJ, Torres T, Kirschbaum J, Pratt JE. Design and Evaluation of Mina: a Robotic Orthosis for Paraplegics; International Conference on Rehabilitation Robotics; IEEE Press, Zurich, Switzerland. 2011; pp. 870–877. [DOI] [PubMed] [Google Scholar]
- [13].Tsukahara A, Hasegawa Y, Sankai Y. Standing-up motion support for paraplegic patient with Robot Suit HAL; IEEE 11th International Conference on Rehabilitation Robotics; IEEE Press, Kyoto, Japan. 2009.pp. 211–217. [Google Scholar]
- [14].Hasegawa Y, Jang J, Sankai Y. Cooperative walk control of paraplegia patient and assistive system; IEEE/RSJ International Conference on Intelligent Robots and Systems; IEEE Press, St. Lous, USA. 2009.pp. 4481–4486. [Google Scholar]
- [15].Suzuki K, Mito G, Kawamoto H, Hasegawa Y, Sankai Y. Intention-based walking support for paraplegia patients with Robot Suit HAL. Advanced Robotics. 2007;21(12):1441–1469. [Google Scholar]
- [16].Tsukahara A, Kawanishi R, Hasegawa Y, Sankai Y. Sit-to-Stand and Stand-to-Sit Transfer Support for Complete Paraplegic Patients with Robot Suit HAL. Advanced Robotics. 2010;24(11):1615–1638. [Google Scholar]
- [17].Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]