Abstract
Background
Hypertension is a leading cause of cardiovascular disease and death worldwide. Advances in technology have added telemedicine as a tool for managing hypertension. The effectiveness of telemedicine depends upon patients’ ability to adhere to schedules of home monitoring and case management.
Methods
Participants with uncontrolled hypertension in the intervention arm of a randomized trial who had completed 6 months of follow-up were included in this analysis. They were asked to measure their BP a minimum of 6 times per week using a telemonitor that transmitted the readings to their pharmacist case manager.
Results
Hypertensive patients in this study had high adherence to telemonitoring (73% took at least 6 BP readings per week) and phone visits (88% of expected visits were attended). In a multivariate analysis, older age, male gender, and some college education predicted better telemonitoring adherence. White non-hispanic race/ethnicity predicted better adherence to phone visits with pharmacist case managers. Telemonitoring adherence and phone adherence were highly correlated; participants who did not send readings on schedule were more likely to skip at least one phone visit with their pharmacist case manager.
Conclusion
The findings from this analysis indicate that hypertensive patients in this study were able to achieve and maintain high adherence to both the telemonitoring and the phone case management visits.
Background
Hypertension is a chronic condition that affects 1 in 3 US adults, and is a leading cause of cardiovascular disease and death worldwide.1 It is the most common chronic condition for which patients see their physician,2 with 4 or more visits per year on average.3 Home blood pressure (BP) monitoring has long been advocated as a method for improving BP control.4,5 However, home monitoring relies on patient self report of their home BP readings, and confidence in the data may be hampered by inaccurate or selective conveying of BP readings.6,7
Advances in technology have added telemedicine, the exchange of medical information using electronic communications, as a tool for managing chronic diseases and improving the validity of home monitoring.8 Telemedicine has become a viable alternative to traditional face-to-face physician office care, and has become increasingly popular for managing chronic diseases such as heart failure and diabetes.9,10,11 The dual aspects of telemedicine, telemonitoring (transmitting home monitoring readings electronically) and follow-up with phone visits, are also well-suited for the management of hypertension.12 Unfortunately, few evaluations of patient adherence to home BP telemonitoring and phone visit regimens exist.5,13
Telemedicine could be a transformational care management tool that allows comprehensive assessment of many chronic conditions and improves care. However, telemedicine is only a valuable investment if patients are willing to adhere to a schedule of home measurements and phone management with their providers. The purpose of this paper is to provide a comprehensive assessment of patient adherence to BP telemonitoring and case manager phone visits in a cluster randomized clinical trial of BP telemonitoring and pharmacist case management vs. usual physician-led BP care.
Methods
Study Design and Setting
HyperLink is a cluster randomized trial being conducted in 16 primary care clinics in HealthPartners Medical Group, an integrated health care organization based in Minneapolis-St.Paul. Eight clinics were randomized to usual care (UC) and eight clinics to the telemonitoring intervention (TI). Eligibility for the study is determined by at least 2 consecutive elevated BPs (≥140/90) at the most recent primary care visits in the year prior to screening, regardless of whether the patient has been diagnosed with hypertension. Participants must also demonstrate elevated BP (≥140/90 or ≥130/80 if diabetes or kidney disease are diagnosed) in the research clinic to be eligible for the study. Participants are seen in the research clinic every 6 months for the 18-month study duration to assess blood pressure. TI participants receive home blood pressure monitors that store their BP readings and transmit them over the phone to a study clinical case manager. HyperLink clinical case managers are doctoral level pharmacists integrated with the primary care medical team as ‘Medication Therapy Management (MTM)’ pharmacists. MTM pharmacists have collaborative practice agreements with their clinic’s primary care physicians that allow them to see, and prescribe treatment for, primary care patients for select conditions. The pharmacist case managers are able to access participant BP telemonitor readings via a secure website. Participants and their pharmacist case managers meet once in person then intensively by phone every 2 weeks (or monthly, if BP has been controlled at the previous 3 phone visits) for the first 6 months of the study. Randomization assignment was determined by a patient’s primary care clinic, and 4 pharmacist case managers were pre-assigned to the 8 intervention clinics by the medical group. Patients attending the 8 usual care clinics were managed by their primary care provider without telemonitoring. Details of the full study design have been published separately.14
Telemonitoring Intervention
Participants were asked to measure their BP a minimum of 6 times per week, preferably on at least 3 separate days including both morning and evening readings, using a telemonitor that transmitted the readings via a modem and a phone line to their pharmacist case manager. They were encouraged to take 2-3 measurements in succession at one-minute intervals at each measurement session. Alerts were generated by the data collection system to notify pharmacists if readings were very high (>160/100), very low (<90/60), or not being sent at least weekly. Participants were encouraged to adhere to the telemonitoring and phone visit schedule, which was explained at their baseline visit in the research clinic and reinforced at the in-person initial visit with the pharmacist.
Case Management
Schedules of required visits with pharmacist case managers were given to participants at their baseline visit. The schedule requires an in-person intake visit, followed by 6-10 phone visits (6 mandatory visits, 4 optional visits if BP is controlled at the previous 3 visits).
Statistical Methods
This analysis includes 213 of the 228 participants who were randomized to the TI arm (8 clinics) of the trial. We excluded 14 participants who never transmitted any BP readings, and 1 who provided no demographic information. This analysis covers the first 6 months (26 weeks) of the study. The analysis utilized mixed effects linear and logistic regression to adjust for clinics as the unit of randomization. Adherence to telemonitoring (the telemonitoring dependent variable) was defined as a binary variable by week such that a week received a ‘1’ if at least 6 BP readings had been taken that week, and a ‘0’ if less than 6 BP readings had been taken that week. The binary outcomes for each week were summed for each participant and then divided by the 26 weeks enrolled in the study to obtain a continuous proportion of weeks adherent to the intervention for each participant. Adherence to phone visits (the pharmacist case management visit dependent variable) was binary, defined as completing all 6 mandatory visits.
Age, gender, race, income, education, marital status and employment status were collected on a baseline survey instrument as demographic covariates for this analysis. Additionally, prior use of a home BP monitor and number of hypertension drugs taken at enrollment were determined. Bivariate mixed effects models were used to test adherence to telemonitoring and adherence to mandatory phone visits by sex: male/female, race: white non Hispanic/minority, age: <49, 50-64,≥ 65, prior use of home BP monitor: yes/no, on hypertension medication at baseline yes/no, annual income: <$30,000-$49,999, $50,000-$99,999, ≥$100,000; employment: full time, part time, retired, unemployed; marital status: married/live together, divorced/widowed/never married; education: high school graduate or less, some college, 4 year college degree or more. Multivariable mixed effects linear and logistic regression models with all these covariates included in each model were used to predict adherence to telemonitoring (continuous) and adherence to mandatory phone visits (binary). All analyses were conducted using SAS 9.2 (Cary, NC).
Results
Baseline Characteristics
Participants in the intervention arm of the HyperLink study had an average age of 63 years (range 32-91) and were evenly split on gender (45% female), as well as racially representative of the adult population of Minnesota (85% non-Hispanic White, Table 1). The majority were highly educated (52% had a 4-year college degree or higher), had high incomes (68% over $50,000 per year), and were married or living with a partner (72%). Employment status was mixed (38% full-time employment, 13% part-time employment, 40% retired and 9% unemployed). Half of the participants reported using a home BP monitor in the past year (52%) and most were taking BP medications at baseline (78%).
Table 1.
Demographic Characteristics of 213 participants who completed 6 months of Telemonitoring and case management
| Characteristic | N (%) |
|---|---|
| Age | |
| Mean (years) | 63.3 (Range 32-91) |
| <49 | 25 (12%) |
| 50-64 | 100 (47%) |
| >65 | 88(41%) |
| Gender | |
| Male | 118 (55%) |
| Female | 95 (45%) |
| Race | |
| White, non Hispanic | 181 (85%) |
| White, Hispanic | 1 (<1%) |
| African-American | 19(9%) |
| Asian | 3 (1%) |
| Native American | 1 (<1%) |
| Pacific Islander | 0 (0%) |
| More than 1 race | 3 (1%) |
| Other Race | 2(<1%) |
| Refused to answer | 3 (1.4%) |
| Education* | |
| High School diploma or less | 33 (16%) |
| Some College/2yr degree | 67 (32%) |
| 4yr college degree or higher | 108 (52%) |
| Marital Status* | |
| Married/Living Together | 150 (72%) |
| Divorce/Separated/Widowed/Single | 58 (28%) |
| Work Status* | |
| Full Time | 79 (38%) |
| Part Time | 27(13%) |
| Retired | 83 (40%) |
| Unemployed | 19 (9%) |
| Income (household, per year)** | |
| <$30,000 | 31 (18%) |
| $30,000-$49,999 | 25 (14%) |
| $50,000-$99,999 | 66 (37%) |
| <$100,000 | 55 (31%) |
| Used a home BP monitor in the past year | |
| Yes | 110 (52%) |
| No | 103 (48%) |
| Taking Hypertension medications at Baseline | |
| No | 47 (22%) |
| Yes | 166 (78%) |
| Yes: 1 drug | 60 (28%) |
| Yes: 2 drug | 54 (25%) |
| Yes: 3 drug | 34 (16%) |
| Yes: 4 drug | 13 (6%) |
| Yes: 5 drug | 2 (>1%) |
| Yes: 6 drug | 3 (1%) |
Missing data on 5 participants
Missing data on 36 participants
Telemonitoring Adherence
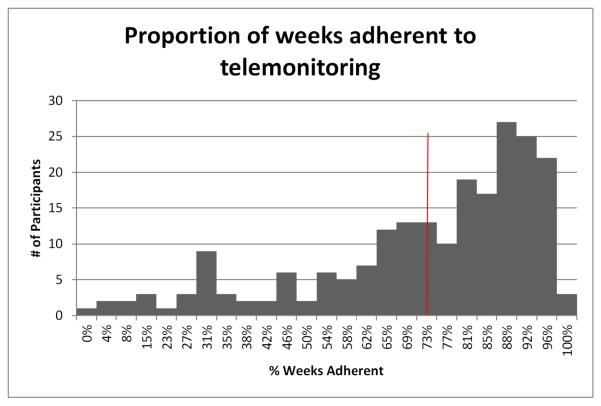
Participants in the HyperLink study were generally very adherent to the protocol of taking at least 6 BP telemonitor readings per week. They took an average of about 31.5 measurements per week, which is likely a reflection of the instruction to measure BP 2-3 times in succession at each measurement session. A steady pattern was reached within 2 weeks and persisted over 6 months. Across the 213 participants, the percentage of weeks with at least 6 readings taken ranged from 0% - 100% (mean 73%, median 81%, 25th percentile: 62%, 75th percentile 88%). The distribution of the proportion of weeks adherent to BP monitoring is presented in Figure 1.
Figure 1.
Patient adherence to the telemonitoring protocol (took at least 6 BP readings per week). Mean (73%) represented by red line.
Adjusting for clustering at the level of the clinic in the bivariate models, mean adherence was higher in older age groups (overall p <.0001), 56.3% in ages <49, 69.8% in ages 49-65 and 79.5% in those aged 65 and older. Race also influenced adherence (overall p=0.03), 74.4% adherence in White non-Hispanics and 60.9% in minorities. A significant difference was also seen by employment status (overall p=0.03), specifically with unemployed participants having lower adherence than participants who either worked full or part time or were retired (77.4% adherent in full-time workers, 72.5% in part-time workers, 76.4% in retirees and 58.9% in unemployed). Finally, adherence differed marginally by income level (overall p=0.09), 65.1% in those earning <$30,000 per year, 68.6% in those earning $30,000-$49,999, 77.0% in those earning $50,000-$99,000 and 71.5% in those earning greater than $100,000. Adherence did not vary significantly by gender (p=0.17), education (overall p=0.34), or marital status (overall p=0.38). Neither previous use of a home BP monitor (p=0.25), nor being treated for hypertension with medications at baseline (p=0.55) were associated with better adherence to telemonitoring. (Table 2).
Table 2.
Univariate and Multivariate model fitted proportion results of telemonitoring adherence by demographic characteristics, adjusted for clinic randomization
| Telemonitoring Intervention Overall=78% |
Univariate |
Multivariate |
||
|---|---|---|---|---|
| Mean % of weeks Adherent |
P-Value | Mean % of weeks Adherent |
P-Value | |
|
| ||||
| Age: | Overall p<0.001 |
Overall p=0.02 |
||
| <49 | 56.3% a | 61.4% a | ||
| 49-64 | 69.8% b | 68.2% a | ||
| ≥65 | 79.5% c | 80.3% b | ||
|
| ||||
| Sex: | ||||
| Male | 74.5% | p=0.17 | 75.9% a | p=0.02 |
| Female | 70.16% | 67.0% b | ||
|
| ||||
| Race: | ||||
| White non-Hispanic | 74.4% a | p=0.03 | 73.4% | p=0.07 |
| Minority | 60.9% b | 63.1% | ||
|
| ||||
| Education: | Overall p=0.34 |
Overall p=0.03 |
||
| HS grad or less | 67.8% | 65.0% a | ||
| Some College/2yr degree | 75.0% | 78.4% b | ||
| 4yr college+ | 72.1% | 69.9% a | ||
|
| ||||
| Marital Status: | p=0.38 | p=0.61 | ||
| Married/Live together | 73.3% | 72.7% | ||
| Divorced/Widowed/Never Married | 70.1% | 70.3% | ||
|
| ||||
| Employment: | Overall p=0.03 |
Overall p=0.83 |
||
| Full-time | 71.4% a | 72.8% | ||
| Part-time | 72.5% a | 73.9% | ||
| Retired | 76.4% a | 71.6% | ||
| Unemployed | 58.9% b | 67.1% | ||
|
| ||||
| Income: | Overall p=0.09 |
Overall p=0.35 |
||
| <$30,000 | 65.1% a | 70.9% | ||
| $30,000-$49,999 | 68.6% ab | 67.0% | ||
| $50,000-$99,999 | 77.0% b | 75.9% | ||
| ≥ $100,000 | 71.5% ab | 70.3% | ||
|
| ||||
| Prior BP monitor Use: | ||||
| Yes | 74.3% | p=0.25 | 71.1% | p=0.61 |
| No | 70.7% | 73.0% | ||
|
| ||||
| Prior BP medication Use: | ||||
| Yes | 73.1% | p=0.55 | 72.1% | p=0.99 |
| No | 70.8% | 72.0% | ||
Different letters (a, b, c) indicate significantly different pairwise comparison p-values. Letters are omitted when pairwise p >.05
In a mixed model multivariable analysis of these factors, age retained its significance (overall p=0.02), with those aged ≥65 having higher rates of adherence (80.3%) than those aged 49-64 (68.2%) and those aged <49 (61.4%). Male gender predicted better adherence, as did education, with those having some college education having better adherence than those with only a high school diploma or a 4 year college degree or higher. (Table 2).
Adherence to Case Management Visits
Adherence to 6 mandatory phone visits per 213 participants with study pharmacists was high, with a mean proportion of 88.4% (1133/1278 visits complete, range 16%-100%, median 100%). Long-term adherence to phone visits over the 6 months, measured as an average adherence across patients, was sustained, averaging 91.5% in months 0-3 and 86.6% in months 3-6. Table 3 presents visit adherence by visit month/type. At the individual level, 139 (65%) participants attended all mandatory phone visits and 74 (35%) missed at least 1 phone visit.
Table 3.
Adherence to Pharmacist Case Management Visits
| Visit | Visit Month |
Actually Completed |
Missed | Adherence Rate |
|---|---|---|---|---|
| Intake | - | 212 | 1 | 99.5% |
| Mandatory | 1 | 203 | 10 | 95.3% |
| Mandatory | 1.5 | 191 | 22 | 89.7% |
| Mandatory | 2 | 201 | 12 | 94.4% |
| Optional | 2.5 | 168 | - | - |
| Mandatory | 3 | 191 | 22 | 89.7% |
| Optional | 3.5 | 141 | - | - |
| Mandatory | 4 | 189 | 24 | 88.7% |
| Optional | 4.5 | 103 | - | - |
| Mandatory | 5 | 183 | 30 | 85.9% |
| Optional | 5.5 | 105 | - | - |
In the bivariate analysis adjusting for randomization clinic, adherence to mandatory phone visits with pharmacist case managers did not differ significantly by age, gender, education, marital status, income, prior use of a home BP monitor, or being on hypertension medications at baseline. Adherence to all mandatory visits differed by race (overall p=0.01), with 69.4% in white non-Hispanics attending all mandatory phone visits and 44.8% in minorities (Table 4). In a multivariate mixed model analysis of all of these factors race remained significantly associated with adherence (overall p=0.01), with 69.9% adherence in white non-Hispanics and 38.9% in minorities. (Table 4). In both the bivariate and multivariate models, there was a suggestion that employment status had an association with visit adherence, with patients who were part-time employed or retired having the highest adherence, although the overall p-values were non-significant.
Table 4.
Univariate and Multivariate model results of pharmacy case management adherence by demographic characteristics, adjusted for clinic randomization
| Phone Visits Overall=70% |
Univariate |
Multivariate |
||
|---|---|---|---|---|
| % Adherent to all 6 visits |
P-Value | % Adherent to all 6 visits |
P-Value | |
|
| ||||
| Age: | ||||
| <49 | 45.2% a | Overall p=0.10 |
68.5% | Overall p=0.93 |
| 49-65 | 65.3% ab | 66.7% | ||
| ≥;65 | 71.1% b | 63.1% | ||
|
| ||||
| Sex: | ||||
| Male | 66.5% | p=0.85 | 70.2% | p=0.17 |
| Female | 65.3% | 59.5% | ||
|
| ||||
| Race: | ||||
| White non-Hispanic | 69.4% a | p=0.01 | 69.6% a | p=0.01 |
| Minority | 44.8% b | 38.9% b | ||
|
| ||||
| Education: | ||||
| HS grad or less | 60.4% | Overall p=0.67 |
61.7% | Overall p=0.49 |
| Some College/2yr degree | 69.2% | 71.7% | ||
| 4yr college+ | 65.0% | 62.7% | ||
|
| ||||
| Marital Status: | ||||
| Married/Live together | 67.1% | p=0.49 | 63.6% | p=0.46 |
| Divorced/Widowed/Never Married | 62.0% | 70.8% | ||
|
| ||||
| Employment: | ||||
| Full-time | 60.5% ab | Overall p=0.12 |
53.9% a | Overall p=0.09 |
| Part-time | 71.1% ab | 76.8% ab | ||
| Retired | 72.7% a | 76.1% b | ||
| Unemployed | 47.9% b | 54.5% ab | ||
|
| ||||
| Income: | ||||
| <$30,000 | 51.6% a | Overall p=0.21 |
52.0% | Overall p=0.44 |
| $30,000-$49,999 | 68.1% ab | 62.8% | ||
| $50,000-$99,999 | 73.9% b | 72.6% | ||
| ≥ $100,000 | 61.9% ab | 66.2% | ||
|
| ||||
| Prior BP monitor Use: | ||||
| Yes | 60.6% | p=0.10 | 58.9% | p=0.08 |
| No | | 71.6% | 72.4% | ||
|
| ||||
| Prior BP medication Use: | ||||
| Yes | 66.6% | p=0.71 | 66.9% | p=0.53 |
| No | 63.6% | 61.2% | ||
Different letters (a, b) indicate significantly different pairwise comparison p-values. Letters are omitted when pairwise p >.05. This model includes all variables listed in the table.
Finally, we tested for a correlation between telemonitoring adherence and phone visit adherence (with both defined as continuous variables), and found that the two were highly correlated (correlation coefficient=0.63, p <0.0001). Participants who did not send telemonitoring readings on schedule were more likely to skip at least one mandatory phone visit with their pharmacist case manager. (Table 5).
Table 5.
Correlation between telemonitoring and phone visit adherence
| Percent of weeks adherent to telemonitoring | Percent of phone visits complete |
|---|---|
| <25% (N=9) | 42% |
| 25-49% (N=25) | 67% |
| 50-74% (N=57) | 92% |
| >75% (N=122) | 95% |
Total number of weeks in the study is 26. Overa l correlation coefficient between the two continuous variables is 0.63, p <.0001.
Discussion
The findings from this analysis indicate that patients in this study with uncontrolled hypertension were able to achieve and maintain high adherence to both the telemonitoring and the phone case management visits over the 6 months of intensive intervention. Older age significantly predicted better telemonitoring adherence in both the bivariate and multivariate analysis, while male gender and education predicted better telemonitoring adherence only in the multivariate analysis. Race significantly predicted phone visit adherence in both models, with the highest adherence in white non-Hispanics and the lowest adherence in minorities. Marital status, income, prior BP monitor use and prior BP medication use were not significant predictors of adherence either to telemonitoring or pharmacist case management phone visits.
These results are mostly consistent with findings from other recent telemonitoring studies in hypertension and heart failure showing that patients are able to make telemonitoring part of their routine and sustain adherence over time.15-17 A recent paper on telemonitoring in a heart failure patient population found adherence to be very low (~55%) although the authors point out that this adherence is probably a best-case scenario for this population.18 Another recent comprehensive review of self-measured blood pressure monitoring found only one study examining how adherence varies by patient characteristics, an observational study of home BP telemonitoring in 377 Korean Americans.19. In this study adherence was greater in older patients, which is consistent with our findings, and lower in patients with depression, which we did not measure.20 Additionally, our finding that older age predicts adherence to telemonitoring is supported by previous studies that have indicated that medication adherence increases with age, perhaps due to older patients having more help with their medication regimes.21 Finally, some authors have pointed out that telemedicine has the potential to interfere with the relationship between health professionals and patients by decreasing face-to-face contact and involving other health professionals in a team-based approach.22 Although we don’t yet have data on that point, the participants in the study maintained high adherence to a very demanding monitoring and phone visit schedule, indicating that it seems prudent to embed telemonitoring programs into primary care, as we have done.
While HyperLink has some features of an efficacy study (participants received more intensive follow-up of missed visits and failure to send readings from the study pharmacists than would be likely in a non-study setting), it also had many features of a pragmatic trial.23 We intentionally used broad inclusion criteria and minimal exclusion criteria, so the participants would likely be more representative of patients with uncontrolled hypertension than those in many previous studies. The intervention was quite flexible and was conducted by pharmacists practicing in the clinics rather than by trained research personnel, and the comparison group received usual care from their primary care providers, all hallmarks of a pragmatic trial.
The participants in this study may be more likely to be adherent to the intervention because they were motivated enough to agree to participate in a clinical trial. In addition, all were seen by primary care physicians for hypertension in the past year, a majority (78%) took hypertension medications at study baseline and over half (52%) already used a home blood pressure monitor. The frequency of BP measurement and telemonitoring were rather aggressive in this trial. Although the frequency seems feasible for the participants in our clinical trial, it may not be practical in routine clinical practice. Also, our findings of high rates of adherence in this population may not be generalizable to patients who are unaware of their hypertension status or are less engaged in their health care. Nevertheless, our results suggest that good fidelity to an intensive telemonitoring protocol can be achieved, and add to the existing knowledge by identifying predictors that influence adherence to telemonitoring interventions.
We expect to be able to report the efficacy of the study intervention for achieving the primary outcome of improved blood pressure control in the near future. Our results will ultimately include a comprehensive cost-analysis, an important strength given the general lack of such data on telemedine interventions.24
Conclusion
The potency of team-based hypertension care in combination with home BP monitoring is garnering increasing attention.11. Comprehensive interventions like those being tested in HyperLink have the potential to improve BP control by conveying reliable blood pressure data to healthcare providers who can then close the feedback loop by making appropriate therapeutic adjustments. The intervention in this study is demanding, but adherence to the protocol and visit schedule was very high, indicating that this sort of intervention would be feasible should it prove effective, although some types of patients may need extra adherence support (younger age, women, those with lower education, and minorities). Future analyses will examine more details of the timing of home BP telemonitoring measurements and whether adherence to telemonitoring and telephone visits is maintained for 6 to 12 months.
Acknowledgments
Financial Disclosure:
This study is supported by a grant from the National Heart, Lung, and Blood Institute (R01HL090965).
References
- 1.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003 May 21;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2007. National Center for Health Statistics. Vital Health Stat. 2011;13(169) [PubMed] [Google Scholar]
- 3.Hyman D, Pavlik V. Characteristics of patients with uncontrollable hypertension in the United States. New England Journal of Medicine. 2001;345:479–486. doi: 10.1056/NEJMoa010273. [DOI] [PubMed] [Google Scholar]
- 4.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. Call to action on use and reimbursement for home blood pressure monitoring: Executive Summary. A joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Clin Hypertens (Greenwich) 2008 Jun;10(6):467–476. doi: 10.1111/j.1751-7176.2008.08418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008 Jun 25;299(24):2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santamore WP, Homko CJ, Kashem A, McConnell TR, Menapace FJ, Bove AA. Accuracy of Blood Pressure Measurements Transmitted Through a Telemedicine System in Underserved Populations. Telemedicine and e-Health. 2008;14(4):333–338. doi: 10.1089/tmj.2007.0063. [DOI] [PubMed] [Google Scholar]
- 7.Johnson KA, Partsch DJ, Rippole LL, McVey DM. Reliability of self-reported blood pressure measurements. Arch Intern Med. 1999 Dec 13-27;159(22):2689–2693. doi: 10.1001/archinte.159.22.2689. [DOI] [PubMed] [Google Scholar]
- 8.Green BB, Ralston JD, Fishman PA, et al. Electronic communications and home blood pressure monitoring (e-BP) study: design, delivery, and evaluation framework. Contemp Clin Trials. 2008 May;29(3):376–395. doi: 10.1016/j.cct.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.AbuDagga A, Resnick HE, Alwan M. Impact of bloof pressure telemonitoring on hypertension outcomes: A literature review. Telemedicine and e-Health. 2010 Sep;16(7):832–838. doi: 10.1089/tmj.2010.0015. [DOI] [PubMed] [Google Scholar]
- 10.Weinberger M, Kirkman MS, Samsa GP, Shortliffe EA, Landsman PB, Cowper PA, Simel DL, Feussner JR. A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: Impact on glycemic control and health-related quality of life. J Gen Intern Med. 1995;10(2):59–66. doi: 10.1007/BF02600227. [DOI] [PubMed] [Google Scholar]
- 11.Carter BL, Bosworth HB, Green BB. The Hypertension Team: The role of the pharmacist, nurse, and teamwork in hypertension therapy. J. Clin. Hypertens. 2012 Jan;14(1):51–65. doi: 10.1111/j.1751-7176.2011.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark RA, Yallp JJ, Piterman L, Croucher J, Tonkin A, Stewart S, Krum H, on behalf of the CHAT Study Team Adherence, adaptation and acceptance of elderly chronic heart failure patients to receiving healthcare via phone-monitoring. Eur J Heart Fail. 2007;9:1104–1111. doi: 10.1016/j.ejheart.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008 Aug;26(8):1505–1526. doi: 10.1097/HJH.0b013e328308da66. [DOI] [PubMed] [Google Scholar]
- 14.Margolis KL, Kerby T, Asche SE, Bergdall AR, Maciosek MV, OConnor PJ, Sperl-Hillen JM. Design and rationale for Home Blood Pressure Telemonitoring and Case Management to Control Hypertension (HyperLink): A cluster randomized trial. Contemp Clin Trials. 2012;33:794–803. doi: 10.1016/j.cct.2012.03.014. doi:10.1016/j.cct.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark RA, Yallop JJ, Piterman L, Croucher J, Tonkin A, Stewart S, Krum H, CHAT Study Team Adherence, adaptation and acceptance of elderly chronic heart failure patients to receiveing healthcare via telemonitoring. Eur J Heart Fail. 2007;9(11):1104–1111. doi: 10.1016/j.ejheart.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Bosworth HB, Olsen MK, McCant F, et al. Hypertension Intervention Nurse Telemedicine Study (HINTS): testing a multifactorial tailored behavioral/educational and a medication management intervention for blood pressure control. Am Heart J. 2007 Jun;153(6):918–924. doi: 10.1016/j.ahj.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Artinian NT, Flack JM, Nordstrom CK, et al. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs Res. 2007 Sep-Oct;56(5):312–322. doi: 10.1097/01.NNR.0000289501.45284.6e. [DOI] [PubMed] [Google Scholar]
- 18.Chaudry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in Patients with Heart Failure. N Engl J Med. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uhlig K, Balk EM, Patel K, Ip S, Kitsios GD, Obadan NO, Haynes SM, Stefan M, Rao M, Kong Win Chang L, Gaylor J, Iovin RC. Self-Measured Blood Pressure Monitoring: Comparative Effectiveness. Agency for Healthcare Research and Quality (US); Rockville, MD: Jan, 2012. [PubMed] [Google Scholar]
- 20.Kim J, Han HR, Song H, et al. JCH. 2010;12(4):253–60. doi: 10.1111/j.1751-7176.2009.00218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wal MHL, Jaarsma T, van Veldhuisen DJ. Non-compliance in patients with heart failure; how can we manage it? Eur J Heart Fail. 2005;7(1):5–17. doi: 10.1016/j.ejheart.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Miller EA. The continuing need to investigate the nature and content of teleconsultation communication using interaction analysis techniques. J Telemed Telecare. 2011;17:55–64. doi: 10.1258/jtt.2010.100203. [DOI] [PubMed] [Google Scholar]
- 23.Thorpe KE, Zwarenstein, Oxman AD, Treweek S, Furberg CD, Altman DG, Tunis S, Bergel E, Harvey I, Magid DJ, Chalkidou K. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. CMAJ. 2009;180(10):E47–E57. doi: 10.1503/cmaj.090523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dávalos ME, French MT, Burdick AE, Simmons SC. Economic Evaluation of Telemedicine: Review of the Literature and Research Guidelines for Benefit-Cost Analysis. Telemedicine and e-Health. 2009;15(10):933–948. doi: 10.1089/tmj.2009.0067. [DOI] [PubMed] [Google Scholar]