Abstract
Objective
To assess relationships between changes in Medicare Advantage (MA) payment rates and Medicare beneficiary hospitalizations and to simulate the effects of scheduled payment cuts on ambulatory care sensitive and elective hospitalization rates.
Data
State Inpatient Database discharge abstracts from Arizona, Florida, and New York merged with administrative Medicare enrollment and MA payment data.
Study Design
Retrospective, fixed effect regression analysis of the relationship between Medicare Advantage payment rates and rates of ambulatory care sensitive and elective hospitalizations amongst Medicare beneficiaries in counties with at least 10,000 Medicare beneficiaries and 3 percent MA penetration from 1999 – 2005.
Principal Findings
MA payment rates were negatively related to rates of ACS admissions. Simulations suggest that payment cuts could be associated with higher rates of ACS admissions. No relationship between MA payments and rates of elective hospitalizations was found.
Conclusions
Reductions in Medicare Advantage payment rates may result in a small increase in ambulatory care sensitive admissions. Trends in ambulatory care sensitive admissions amongst chronically ill Medicare beneficiaries should be tracked following MA payment cuts.
Keywords: Medicare Advantage, payments, hospitalization rates, managed care, quality
The Patient Protection and Affordable Care Act of 2010 (PPACA) is projected to achieve $145 billion in savings through reduced payments to Medicare Advantage plans over the coming decade (Foster, 2010). Medicare Advantage (MA) is a voluntary managed care alternative to Fee-for-Service (FFS) Medicare that provides additional benefits beyond the basic Medicare benefit package to enrollees who join managed care networks. Though managed care plans were initially introduced as a cost-saving mechanism, the Medicare Payment Advisory Commission estimates that payments to MA plans total 114 percent of Fee-for-Service (FFS) spending for otherwise similar beneficiaries (MedPAC, 2009).
However, Medicare Advantage plans are required to use payments exceeding expected costs on additional benefits or reduced cost sharing for enrollees. These benefits may have positive health effects, for example by improving access to care for lower-income seniors who disproportionately enroll (Atherly and Thorpe, 2005). The planned cuts in MA payments have raised concerns about the health implications of benefit reductions for the 23 percent of Medicare beneficiaries currently enrolled in an MA plan (Herszenhorn, 2009).
Limited empirical evidence about the relationship between payments to MA plans and the care provided to Medicare beneficiaries has led to speculation about the value of additional payments to MA plans. President Obama articulates one view, that the additional payments to MA plans are “unwarranted subsidies in Medicare that go to insurance companies—subsidies that do everything to pad their profits but don’t improve the care of seniors” (Wall Street Journal, 2009). Health insurers argue that payment cuts would reduce benefits and increase costs to patients, which could affect utilization and health outcomes. As payment rates become more generous, plans can invest in additional benefits such as disease management or reduced cost sharing for preventive service use; strategies which may reduce hospitalization use. Payment reductions introduced by the 1997 Balanced Budget Act (BBA) were associated with plan withdrawals from many markets and declines in supplemental benefits (Berenson and Dowd, 2009; Gold et al, 2004).
Changes in Medicare Advantage payment rates may also affect the quality of care provided to Fee-for-Service (FFS) participants. Higher plan payments have been shown to increase managed care enrollment (Cawley et al., 2005). Earlier studies have also found significant spillover effects from Medicare managed care influencing treatment patterns of all Medicare beneficiaries (Baker, 1997; Bundorf et al., 2004; Gaskin and Hadley, 1997; Chernew et al., 2008). Chernew et al. (2008) find that higher MA penetration reduces FFS spending and suggest that optimal MMC payment strategy should account for spillovers to FFS with higher payments to MA plans to further encourage enrollment rather than payment cuts. Since spillover effects are more likely under higher levels of managed care penetration, changes in MA payment rates can affect quality of care for all Medicare beneficiaries by altering the nature and magnitude of spillovers as well by changing the composition of program participants.
Improved understanding of the potential consequences of changing Medicare Advantage payment policy is necessary to evaluate the impact of health reform proposals on seniors. If there are adverse health and utilization consequences of payment reductions, policymakers may overstate the potential savings. I used the variation in payments across counties and over time established by federal plan payment policy resulting from a series of Congressional policy changes to study the relationship between payments to MA plans and hospitalization rates amongst Medicare beneficiaries from 1999 to 2005. I examined rates of acute and chronic ambulatory care sensitive (ACS) admissions, which may be influenced by the additional benefits provided by MA plans, and elective hospitalizations, which may become more tightly rationed in response to lower payments. Results from this analysis are used to simulate changes in hospitalization rates which might occur in response to the PPACA payment cuts.
Conceptual Framework
Changes in Medicare Advantage payment rates may affect the type of care provided to Medicare beneficiaries through several channels. Managed care plans may alter benefit packages offered to MA enrollees. In response to the change in benefit availability, MA plans become more or less attractive to enrollees, changing the composition of MA and FFS enrollee groups. Finally, changes in MA market share alter managed care plans’ influence over provider practice patterns.
Benefit Packages
Payment rates may directly affect the types and amount of care provided to MA enrollees. Plans are required to use additional payments to provide enrollees with supplemental benefits, which can include prescription drug coverage, reduced cost sharing, and gym memberships. Thus, payment decreases may increase rates of ambulatory care sensitive admissions by reducing access to pharmaceuticals and outpatient services that help to prevent these types of admissions. Alternatively, plans may try to pass payment cuts on to providers, change or restrict service networks, all of which can create access barriers for patients requiring time-sensitive care or expensive, elective procedures. Other beneficiaries will lose access to supplemental benefits through plan withdrawals; Medicare managed care penetration declined between 1998 and 2001 as plans left the market in response to BBA-induced lower payment rates (Gold, 2003).
Medicare Advantage Enrollment
Reduction in plan payment may lead beneficiaries to move from MA to FFS as less generous benefit packages are provided in exchange for managed care network restrictions. Several studies have shown that both plans and Medicare beneficiaries are more willing to participate in counties with higher per-enrollee payment rates (Cawley et al., 2002; 2005; Chernew et al., 2008). The Centers for Medicare and Medicaid Services Office of the Actuary estimate that MA enrollment will fall by 7.4 million by 2019 in response to PPACA provisions (Foster, 2010). Rate change induced MA disenrollment may increase rates of ambulatory care sensitive admissions as fewer Medicare beneficiaries have access to supplemental benefits.
Spillover Effects
Reductions in MA payment rates will affect care provided to FFS enrollees because managed care spillover effects will decline in markets with shrinking MA penetration. Spillovers can occur, for example, if providers adapt a single practice style with which to treat all patients that is influenced by managed care requirements. A large literature examining managed care in both Medicare and private health insurance finds that managed care and non-managed care markets are linked. Spillovers from managed care have been shown to affect total Fee-for-Service spending (Chernew et al., 2008; Baker, 1997), provider practice patterns (Bundorf et al, 2003; Glied and Zivin, 2002; Zhan et al., 2003; Heidenreich et al, 2002) and market-level health technology (Baker, 2001; Baker et al., 2004). Reduced MA spillovers may increase ambulatory care sensitive admissions since managed care penetration has been linked to greater preventative service use (Zhan et al., 2003; Miller and Luft, 2002). Declines in the spillover influence of managed care practices may also increase rates of elective surgery if managed care plans promote more stringent assessment of need.
Study Data and Methods
Data Sources
I use 7 years of county-level Medicare Advantage payment data and Medicare enrollment data from the Centers for Medicare and Medicaid Services and hospital discharge data from the Healthcare Cost and Utilization Project State Inpatient Databases (SID) for Arizona, Florida, and New York from 1999 – 2005. Nearly one quarter of Medicare Advantage enrollees live in these three states during the study period. Analyses were conducted at the county level, pooling Fee-for-Service and MA enrollees in order to estimate the total effect of changes in MA payment, including direct effects of spending on MA enrollees, compositional changes in MA enrollment, and spillover effects to Fee-for-Service. Since changes in payment rates influence movement in and out of MA plans, regressions of MA-specific hospitalization rates on payments may be biased by selection effects related to both Medicare coverage type and risk of hospitalization.
State Inpatient Databases
The SID contain discharge abstracts for the universe of in-state hospitalizations in the three states. International Classification of Disease, Ninth Revision (ICD-9) codes were used to identify acute and chronic ACS and elective hospitalizations using algorithms developed by the Agency for Healthcare Research and Quality (AHRQ, 2003). These types of admissions have been previously validated as quality indicators and are used by MedPAC to assess quality of care in Fee-for-Service Medicare (UCSF-Stanford, 2001; AHRQ, 2003).
I calculated rates of hospitalization per 1,000 Medicare beneficiaries in each county-year for the three types of hospitalizations. In order to calculate reliable rates of hospitalization, I limited the sample to the 398 county-year observations with at least 10,000 elderly Medicare beneficiaries and at least 3 percent MA market share. ACS and elective hospitalizations were fairly common amongst Medicare beneficiaries (Table 1). Rates of potentially preventable ACS hospitalizations modestly decreased during the study period, from 53.2 per 1,000 beneficiaries in 1999 to 45.2 in 2005, indicating quality improvements overall. Rates of elective procedure use increased between 1999 and 2002 and decreased in subsequent years, averaging 19.0 per 1,000 beneficiaries in both 1999 and 2005.
Table 1.
Rates of Ambulatory Care Sensitive and Elective Hospitalization and Average Beneficiary Characteristics Medicare Beneficiaries in 3 States, 1999 – 2005
| Rates of Hospitalization per 1,000 | County Characteristics | ||
|---|---|---|---|
| All ACS Conditions | 54.0 (10.9) | Medicare Advantage Payment Rate ($2005/month) | 744.8 (127.4) |
| Acute ACS Conditions | 20.8 (4.0) | MA Penetration | 0.19 (0.12) |
| Dehydration | 4.0 (1.1) | Low MA Penetration (< 16%) | 0.3 (0.4) |
| Pneumonia | 11.9 (2.3) | Logged Payment* Low Penetration Interaction Term | 1.7 (2.9) |
| Urinary Tract Infection | 4.9 (1.4) | Black | 0.09 (0.08) |
| Chronic ACS Conditions | 33.2 (7.8) | Hispanic | 0.04 (0.06) |
| Angina | 1.2 (0.7) | Other Race | 0.03 (0.03) |
| Asthma | 1.9 (1.1) | Female | 0.58 (0.02) |
| Chronic Obs Pulmonary Disease | 7.5 (2.2) | Medicaid-Eligible | 0.13 (0.09) |
| Congestive Heart Failure | 17.3 (3.8) | End-Stage Renal Disease | 0.01 (0.00) |
| Diabetes: Amputation | 0.9 (0.3) | Age 75–85 | 0.35 (0.03) |
| Diabetes: L-T Complications | 2.9 (1.2) | Age 85+ | 0.14 (0.03) |
| Diabetes: S-T Complications | 0.4 (0.2) | Observations | 398 |
| Diabetes: Uncontrolled | 0.5 (0.4) | ||
| Elective Procedures | 20.5 (6.2) | ||
| Angioplasty (Non-Heart Attack) | 3.2 (1.2) | ||
| Coronary Artery Bypass Graft | 7.3 (2.9) | ||
| Hip or Knee Replacement | 7.6 (2.9) | ||
| Pacemaker Insertion | 2.4 (1.1) | ||
Standard deviations in parentheses. 398 county-year observations from 74 counties in Arizona, Florida and New York, 1999 – 2005 with at least 10,000 Medicare beneficiaries and 3% MA penetration. Authors’ calculations based on State Inpatient Databases and Medicare denominator file.
Acute ACS admissions rates are driven by admissions that could be avoided through timely antibiotic and vaccination use in the outpatient setting. Chronic ACS admissions reflect complications with beneficiary chronic condition management. Amongst Medicare beneficiaries in the sample, these are primarily congestive heart failure (17.3 per 1,000 beneficiaries) and chronic obstructive pulmonary disease (7.5 per 1,000) (Table 1). While completely eliminating these types of admissions amongst the Medicare population is unlikely, higher risk-adjusted rates typically indicate lower quality of outpatient care or barriers to access. Admissions can arise from inadequate access to prescription drugs or outpatient care. Elective admissions are technologically intensive procedures to replace a non-fractured hip or knee (7.6 per 1,000) or heart surgery for patients not admitted with heart attacks (7.3 per 1,000).
Medicare Administrative Data
Medicare Advantage Payments
Prior to the introduction of the 1997 Balanced Budget Act (BBA), Medicare managed care plans were paid 95 percent of the average county level Medicare spending per beneficiary. The BBA divorced plan payment rates from average county costs as a way to reduce geographic variation in payments and estimated overpayments to plans (Berenson, 2004). As a result of these policy changes, MA plans were paid a legislatively determined payment rate set annually at the county level during the study period. Plans were paid the highest of a minimum 2 percentage point increase over the prior year (in nominal dollars), a guaranteed floor payment (with a separate rate for urban and rural counties) and blend rate based on local and national factors. The Medicare Modernization Act increased payment rates in 2004 and introduced an additional rate category equal to 100 percent of expected Fee-for-Service spending (MedPac, 2004).
I used the unadjusted payment rate (in 2005 dollars), which corresponds to a beneficiary of average risk. While actual payments to plans were adjusted to account for beneficiary demographics, use of the unadjusted rate provides a constant measure of payment generosity across counties that is unaffected by differences in health status across Medicare beneficiaries in different counties.
Beneficiary Characteristics
Medicare administrative data from the 100 percent Beneficiary Annual Summary File including average demographic characteristics related to health care utilization (age, race, sex, state Medicaid buy-in and End-Stage Renal Disease status) for aged beneficiaries age 65 and over enrolled in both managed care and Fee-for-Service were used for risk adjustment. Individual characteristics were aggregated annually at the county level (Table 1). Beneficiaries in study counties were predominantly White; 9 percent were Black and 4 percent were Hispanic. Thirteen percent were Medicaid dual-eligibles.
Analytic Methods
Annual rates of each type of hospitalization per 1,000 Medicare beneficiaries were constructed using Medicare enrollment data and SID hospitalization counts for each county-year cell. I estimated fixed effect regressions of rates of hospitalization on the natural logarithm of MA payment rates and beneficiary characteristics. In order to understand the direct effects of the payment change on MA enrollees, I compared markets with low MA penetration, where spillover effects were unlikely, to high penetration markets. Markets with MA penetration below the median rate of 16 percent were classified as low.i The equation of interest is
| (1) |
County fixed effects controlled for unobservable, time-invariant county characteristics that may influence rates of hospitalization and a series of year indicator variables controlled for time effects across counties. In sensitivity analysis, I included county-specific time trends to control for time-variant market characteristics that may also affect rates of hospitalization amongst Medicare beneficiaries. Observations were weighted by the number of Medicare beneficiaries residing in the county.
Regression coefficients represent the change in hospitalization rates associated with a percentage change in payment rates. During the study period, payment changes were governed by policy change, as will occur under PPACA. To estimate the effect of proposed policy changes on Medicare hospitalizations, I simulated upcoming payment changes by evaluating the payment rate coefficients at reductions of 1, 5, and 10 percent. For an x percent cut in payment rates, the change in hospitalization rates holding other factors constant is ln(1−)*(α) in high penetration counties and ln(1−)*(α+ϕ) in low penetration counties. A 5 percent reduction would be more comparable to a gradual change, while a 10 percent reduction would eliminate a substantial portion of the average difference between Medicare Advantage and Fee-for-Service payments.
In practice, the PPACA-prescribed reductions will lead to different-sized cuts in different counties; two to six year transition begins with a rate freeze for all counties for 2011. Historically, payment changes have also been non-uniform across counties.
I conducted a placebo test to provide additional evidence the estimated relationship between changes in MA payments and changes in rates of hospitalization reflects differences in MA enrollment and benefits by regressing hospitalization rates on MA payment rates and control variables in counties with less than 3 percent MA penetration. In markets without an MA presence, there should be no relationship between MA payment rates and patient outcomes since there are few enrollees to be directly affected and no spillover effects.
Results
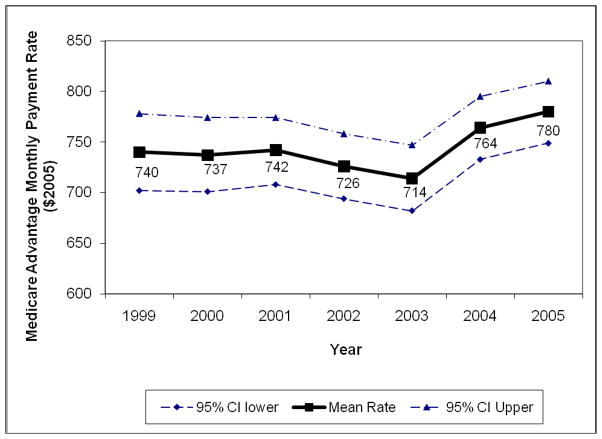
The implementation of the BBA payment rates led to considerable variation in plan payments within and across counties during the study period (Figure 1 and Table 2). Payment changes in nominal terms ranged from cuts of 3 percent to increases of 41 percent (95% CI −3%, 15%) in study counties. Payments to plans remained fairly stable on average from 1999 – 2001, though there was considerable within-county change during this period. Counties receiving only the minimum 2% (nominal) update rate each year saw payments decline by 1.8% in real terms (95% CI −2.1%, −1.6%) or $51 per enrollee per month over the three year period. Floor counties saw major increases in payments; a $57 per month (11%; 95% CI −1.4%, 24%) gain in floor counties between 2000 and 2001 alone. Average MA payments increased sharply in 2004 and 2005 following payment increases legislated in the Medicare Modernization Act; payment increases in 2004 averaged 10 percent (95% CI 2%, 24%).
Figure 1. Average Monthly Medicare Advantage Payment Rates ($2005) in Study Counties, 1999 – 2005.
Source: Author’s calculations based on Medicare Advantage Ratebooks, 1999–2005. 398 county years from 74 counties in Arizona, Florida and New York with at least 10,000 Medicare beneficiaries and 3% Medicare Advantage penetration. All payment rates inflation-adjusted and reported in 2005 dollars.
Table 2.
Average Annual Change in Monthly Medicare Advantage Payment Rates ($2005) By County Payment Rate Category and Proportion of Counties Receiving Each Rate Type
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | |
|---|---|---|---|---|---|---|
| Blend | 7.67 (9.5%) | 19.3 (1.9%) | ||||
| Floor | 57.39 (71.2%) | −0.46 (39.3%) | 26.35 (44.4%) | |||
| Minimum Update | −17.2 (90.5) | −12.04 (28.8%) | −21.61 (60.7%) | −11.03 (100%) | 16.6 (13.0%) | 14.3 (61.3%) |
| 100% FFS | 86.9 (40.7%) | 23.2 (38.7%) |
Average increase in monthly per-enrollee payment rates. Proportion of study counties receiving each rate category in parentheses. 398 county-year observations from 74 counties in Arizona, Florida and New York, 1999 – 2005 with at least 10,000 Medicare beneficiaries and 3% MA penetration.
This variation in payments within counties over time identifies the effect of payment changes on Medicare patient outcomes. While regulations prescribed the annual payment changes for MA plans, spending in FFS Medicare steadily increased at a moderate pace; average FFS spending per capita in the study counties increased between 2 and 5 percent annually.
Medicare Advantage Payments and Medicare Hospitalizations
The multivariate models examined variation in hospitalization rates and Medicare Advantage payments within counties over time. Controlling for beneficiary and county characteristics, I found a negative and statistically significant relationship between MA payment rates and both acute and chronic ACS admissions, but no relationship between payments and elective admissions (Table 3). In high penetration counties, a 1% increase in MA payment rates was associated with 0.057 fewer acute ACS hospitalizations per 1,000 beneficiaries and 0.12 fewer chronic ACS admissions per 1,000 (p < 0.05). The association between logged payment rates and elective surgery was small and statistically insignificant (α = −2.67, se = 4.3)
Table 3.
Medicare Advantage Payments and Rates of Ambulatory Care Sensitive and Elective Hospitalizations Amongst Medicare Beneficiaries, 1999 – 2005
| Acute ACS | Chronic ACS | Elective | |
|---|---|---|---|
| ln(MA Payment Rate) | −5.64** (2.7) | −11.82*** (3.8) | −2.67 (4.3) |
| Low MA Penetration (< 16%) | −17.0 (12.5) | −33.31* (18.0) | 11.0 (15.5) |
| Low Penetration* ln(MA Payment Rate) | 2.6 (1.9) | 5.07* (2.7) | −1.6 (2.4) |
| Black | −19.2 (29.1) | −9.0 (37.1) | −77.98** (36.6) |
| Hispanic | −59.8 (39.0) | −2.9 (50.6) | −147.96* (82.9) |
| Other Race | −53.47*** (17.8) | 10.6 (30.9) | −5.1 (29.8) |
| Female | 233.20*** (76.5) | 167.85* (86.4) | −65.2 (65.5) |
| Medicaid | 58.63** (23.0) | 67.97*** (25.2) | 60.2 (43.4) |
| End-Stage Renal Disease | 224.5 (258.2) | −58.8 (259.5) | 856.44** (357.9) |
| Age 75 – 85 | 34.6 (25.5) | 77.47** (33.2) | 99.19** (43.9) |
| Age 85+ | −6.8 (57.2) | 23.0 (83.8) | −9.3 (56.1) |
| Observations | 398 | 398 | 398 |
| F-Statistic | 13.10 | 25.69 | 32.60 |
| Estimated Changes in Rates of Medicare Ambulatory Care Sensitive and Elective Hospitalizations associated with Potential Medicare Advantage Payment Cuts
| |||
|---|---|---|---|
| Rate Reduction | Acute ACS | Chronic ACS | Elective |
| High MA Penetration Counties | |||
| 1% | 0.06** (0.002, 0.11) | 0.12*** (0.04, 0.19) | 0.03 (−0.06, 0.11) |
| 5% | 0.29** (0.01, 0.57) | 0.61*** (0.22, 0.99) | 0.14 (−0.30, 0.58) |
| 10% | 0.59** (0.02, 1.17) | 1.2*** (0.46, 2.03) | 0.28 (−0.62, 1.19) |
| Low MA Penetration Counties | |||
| 1% | 0.03 (−0.03, 0.09) | 0.07* (−0.01, 0.15) | 0.04 (−0.04, 0.13) |
| 5% | 0.16 (−0.15, 0.46) | 0.35* (−0.06, 0.76) | 0.22 (−0.21, 0.66) |
| 10% | 0.32 (−0.30, 0.9) | 0.71* (−0.13, 1.55) | 0.45 (−0.44, 1.35) |
Robust standard errors (95% confidence intervals) in parentheses.
statistically significant at 10%,
5%,
1%.
398 county-year observations from 74 counties in Arizona, Florida and New York, 1999 – 2005 with at least 10,000 Medicare beneficiaries and 3% MA penetration. Medicare Advantage payments expressed as the natural logarithm of the monthly per-enrollee MA county payment rate ($2005). Low penetration variable indicates counties with MA enrollment below 16%. Models control for county and year fixed effects.
Rates of acute and chronic ACS admissions were also positively related to the proportion of female Medicare beneficiaries and dual-eligible Medicaid enrollees, who often have complex health conditions. Rates of elective hospitalization increased with increases in the proportion of beneficiaries with End-Stage Renal disease and aged 75 – 85. Consistent with the disparities literature, increases in the share of beneficiaries that are Black and Hispanic were related to lower rates of elective procedures.
Since no spillovers to Fee-for-Service are expected in the low penetration market, the combined αln(MAct,) + ϕlowct*ln(MA) term reflects the effect of MA payments on only MA enrollees in low penetration counties. The total effect of the payment rate changes (αln(MAct,) + ϕlowct*ln(MA)) was only statistically significant at 10 percent for chronic ACS admissions (F = 2.84) and insignificant for acute ACS admissions, suggesting that payment changes predominantly affected Medicare beneficiaries in markets where managed care plans had sufficient market share to influence provider behavior.
There is little evidence that changes in MA payments affected use of elective surgery in either high penetration or low penetration markets; coefficients are negative but imprecisely estimated.
In order to gain insight about the mechanisms through which changes in plan payment affected quality of and access to care, Equation (1) is separately estimated for each of the types of hospitalizations listed in Table 1. Results (presented in Appendix Table 1) indicate a negative relationship between MA payment rates and hospitalizations for congestive heart failure (CHF), hypertension, uncontrolled diabetes and urinary tract infections. This relationship could occur through the prescription drug benefits available in many MA plans during the study period, through a managed care emphasis on preventative care facilitating earlier treatment, or improved access to outpatient care through lower cost-sharing in the outpatient setting. Again I found that changes in MA payment rates have less of an impact on beneficiaries in low penetration counties; interaction terms ϕ are positive and statistically significant for rates of dehydration, urinary tract infections, congestive heart failure and uncontrolled diabetes, reducing or negating the overall relationship between payments and hospitalization rates in these counties.
Appendix 1.
Medicare Advantage Payment Changes and Rates of Ambulatory Care Sensitive and Elective Hospitalization Rates amongst Medicare Beneficiaries in 3 States, 1999 – 2005
| ln(MA Payment rate) | Low MA Market Penetration | Low MA * ln(Payment) Interaction | |
|---|---|---|---|
| Acute ACS Conditions | |||
| Dehydration | −1.28 (1.01) | −9.55*** (3.09) | 1.50*** (0.47) |
| Pneumonia | −1.57 (1.98) | 4.86 (9.33) | −0.72 (1.41) |
| Urinary Tract Infection | −2.79** (1.37) | −12.27* (6.55) | 1.85* (0.99) |
| Chronic ACS Conditions | |||
| Angina | −0.22 (0.60) | −0.84 (4.18) | 0.14 (0.64) |
| Asthma | −1.05 (0.74) | −3.47 (3.81) | 0.55 (0.58) |
| Chronic Obs Pulmonary Disease | −0.33 (1.69) | −5.27 (6.65) | 0.8 (1.01) |
| Congestive Heart Failure | −6.91*** (1.84) | −16.94* (9.62) | 2.56* (1.45) |
| Diabetes: Amputation | −0.35 (0.26) | −0.17 (1.04) | 0.03 (0.16) |
| Diabetes: L-T Complications | −0.65 (0.47) | 1.34 (2.17) | −0.21 (0.33) |
| Diabetes: S-T Complications | −0.07 (0.15) | −0.88 (0.75) | 0.14 (0.11) |
| Diabetes: Uncontrolled | −0.42* (0.23) | −2.12*** (0.78) | 0.32*** (0.12) |
| Elective Procedures | |||
| Angioplasty (Non-Heart Attack) | −4.68 (2.94) | 6.7 (9.27) | −1.01 (1.41) |
| Coronary Artery Bypass Graft | 0.99 (0.98) | 4.21 (3.86) | −0.65 (0.59) |
| Hip or Knee Replacement | 1.34 (1.83) | 2.03 (7.65) | −0.26 (1.16) |
| Pacemaker Insertion | −0.32 (0.98) | −1.99 (4.21) | 0.28 (0.64) |
Robust standard errors in parentheses.
statistically significant at 10%,
5%,
1%.
398 county-year observations from 74 counties in Arizona, Florida and New York, 1999 – 2005 with at least 10,000 Medicare beneficiaries and 3% MA penetration.
Medicare Advantage payments expressed as the natural logarithm of the monthly per-enrollee payment rate set at the county level ($2005). Models include average demographic characteristics, county and year fixed effects.
The second panel of Table 3 presents estimated effects of the changes in rates of hospitalization per 1,000 Medicare beneficiaries that would occur if rates to MA plans are reduced by 1, 5, or 10 percent. Reductions in Medicare Advantage payment rates are predicted to be accompanied by a small increase in rates of potentially preventable hospitalizations amongst Medicare beneficiaries in high managed care penetration counties. A 5 percent decrease in payments is associated with a predicted increase in acute ACS admissions of 0.29 per 1,000 beneficiaries, a 1.4 percent increase over the 2005 rate. Chronic ACS admissions are predicted to increase by nearly 2 percent, or 0.61 new admissions per 1,000 Medicare beneficiaries.
A larger, immediate payment cut of 10 percent is associated with predicted increases in rates of acute and chronic ACS admissions of 0.59 and 1.2 per 1,000 respectively. Changes in MA payments recommended in current Congressional proposals would be phased in gradually over 10 year periods. Thus, the 5 percent cuts are likely to more accurately capture the effects of a payment reduction than the full 10 percent estimate. Over a ten year period, plans would have time to adjust benefit design to minimize the effect of payment changes.
While simultaneous changes in enrollment and benefit availability limit my ability to disentangle the mechanisms underlying the increase in hospitalizations expected in response to payment cuts, regressing hospitalization rates on logged MA payments separately for MA and FFS enrollees suggested that the response occurred primarily amongst MA enrollees. Appendix Table 2 presents these results, which are based on data from the 266 county-years with at least 10,000 beneficiaries in both MA and FFS. A 5 percent decrease in MA payments was associated with an increase of 1.4 ACS admissions per 1,000 that is statistically significant at 10 percent. In contrast, the association between FFS admission rates and MA payments is smaller (0.41 per 1,000) and statistically insignificant.
Appendix 2.
Medicare Advantage Payments and Rates of Ambulatory Care Sensitive and Elective Hospitalizations Amongst Medicare Beneficiaries by Medicare Coverage Type, 1999 – 2005
| Acute ACS | Chronic ACS | Elective | |
|---|---|---|---|
| Medicare Advantage Only | |||
| ln(MA Payment Rate) | −6.36 (5.5) | −28.26* (14.1) | 3.02 (6.9) |
| Observations | 266 | 266 | 266 |
| F-Statistic | 112.2 | 183.2 | 543.6 |
| Fee for Service Only | |||
| ln(MA Payment Rate) | 1.65 (4.7) | −6.93 (6.0) | −4.89 (6.4) |
| Observations | 266 | 266 | 266 |
| F-Statistic | 49.7 | 24.6 | 608.2 |
Robust standard errors in parentheses.
statistically significant at 10%,
5%,
1%.
Observations from all county-year-insurance status cells with at least 10,000 Medicare beneficiaries in counties with at least 3% MA penetration. Medicare Advantage payments expressed as the natural logarithm of the monthly per-enrollee payment rate set at the county level ($2005). Models include beneficiary demographics, county and year fixed effects.
Although these coefficients are likely biased by nonrandom selection in and out of managed care, the bias is in the opposite direction of these results. As benefit packages become less generous, sicker MA enrollees are expected to disenroll, which would reduce rates of hospitalization for the average remaining MA enrollee. In contrast, the relationship between payments and hospitalization rates was negative for MA enrollees, indicating that the benefit package effects dominated the selection effect.
Robustness
To provide additional evidence that changes in MA payment rates are linked to changes in rates of hospitalization, I performed a placebo test regressing hospitalization rates on logged MA payment rates in the 453 observations from 79 counties with managed care penetration below 3 percent. As Appendix Table 3 shows, there was no relationship between payment rates and either ACS or elective hospitalization rates; coefficients are smaller in magnitude than those for the MA counties and statistically insignificant.
Appendix 3.
Placebo Test: The Effect of Medicare Advantage Payment Rates on Ambulatory Care Sensitive and Elective Hospitalization Rates in Markets with Low Levels of Medicare Advantage Penetration
| Acute ACS | Chronic ACS | Elective | |
|---|---|---|---|
| ln(MA Payment Rate) | 3.51 (4.4) | −2.9 (6.6) | −4.06 (4.8) |
| Black | −72.9 (71.7) | −34.6 (56.4) | −41.4 (33.6) |
| Hispanic | −1.2 (159.9) | 34.0 (189.4) | −205.3 (165.7) |
| Other Race | 22.3 (144.3) | 162.0 (236.4) | 19.7 (81.3) |
| Female | 114.7 (90.4) | 10.0 (122.0) | −42.8 (82.6) |
| Medicaid | 85.05** (38.8) | −6.5 (44.8) | 12.5 (37.0) |
| End-Stage Renal Disease | 348.3 (337.6) | 557.8 (450.1) | 240.0 (194.1) |
| Age 75 – 85 | 29.0 (43.0) | 42.4 (54.7) | 51.5 (40.5) |
| Age 85+ | 94.23* (53.1) | 133.3 (93.1) | −45.4 (79.6) |
|
| |||
| Observations | 453 | 453 | 453 |
| F-Statistic | 8.55 | 26.5 | 35.4 |
Robust standard errors in parentheses.
statistically significant at 10%,
5%,
1%.
452 county-year observations from 79 counties in Arizona, Florida and New York, 1999 – 2005 with less than 3% MA penetration. Medicare Advantage payments expressed as the natural logarithm of the monthly per-enrollee payment rate set at the county level ($2005).
Results were also robust to the inclusion of county-specific time trends, which control for unobserved market factors that could explain changes in hospitalization rates and in models that exclude observations from 2004. I continued to find a reduction in acute and chronic ACS admissions and no change in elective hospitalizations with changes in MA payments measured in levels rather than logs.
Discussion
Evaluating a series of legislatively determined payment rate changes to Medicare Advantage plans, I found a negative relationship between MA payment rates and rates of ambulatory care sensitive hospitalization rates amongst Medicare beneficiaries. Simulations based on these results suggest that reductions in MA payment rates may result in a small increase in ACS admission rates. Although there is considerable policy debate surrounding additional payments to Medicare Advantage plans relative to Fee-for-Service spending, this study is the first to provide estimates of the potential effects of payment cuts on care provided to Medicare beneficiaries. Largely due to limited data availability, relatively little empirical work has been done in this area.
I did not find evidence that rates of elective procedures were related to MA payment rates, though restricting access to expensive procedures would be one way for plans to limit the cost of care. This finding is consistent with earlier work indicating that managed care plans achieve cost savings by paying lower prices rather than reducing services (Cutler et al., 2000). Rates of elective procedures will also remain stable if sicker patients remain in or disenroll to Fee-for-Service Medicare to avoid HMO restrictions.
I focused on the effect of payment rates on hospitalizations for all beneficiaries rather than just Medicare Advantage enrollees because changes in payment rates will change the composition of the MA enrollee population as well as the benefits they receive. Spending on hospitalizations in Fee-for-Service will be influenced by the resulting change in beneficiary demographics as well as any changes from practice patterns. This analysis is particularly relevant to the PPACA provisions, which are projected to achieve savings by reducing the number of beneficiaries enrolled in MA plans as well as the per-enrollee payments for those who remain. A drawback to this approach is that I cannot separately account for changes in hospitalizations driven by selective enrollment in response to payment cuts and those related to reductions in benefits for MA enrollees.
Comparisons of high and low MA penetration counties offered a potential way to isolate the effect of MA payment changes on MA enrollees, though I generally failed to find a significant effect of payment changes on hospitalization rates in these counties. The limited influence of MA on practice patterns in low-penetration counties is consistent with the spillover and market share literature. Additionally, county level hospitalization rates are weighted averages of the MA and FFS rates, so the modest changes in outcomes for the MA patients are likely dwarfed by the lack of change in FFS hospitalizations; for example a 25 percent reduction in the rate of hospitalizations amongst MA enrollees would not significantly change the average rate of ACS admissions in the average low-penetration county. Separate regressions for MA and FFS enrollees provide descriptive evidence suggesting that the additional hospitalizations occur amongst MA enrollees. This likely reflects plans providing less generous coverage when payment rates are lower (Gold et al., 2004).
Study findings should not be interpreted causally if other unmeasured factors drive both payment rates and hospitalization rates. Several analytic steps were taken to avoid this potential endogeneity. Legislatively determined MA payment rates create a quasi-experimental setting in which to consider the relationship between payments and quality. Use of county fixed effects controlled for persistent county level differences in payment rates, beneficiary acuity, and propensity to use hospital care. Finally, I used standardized payment rates for an average enrollee rather than payments determined by the county’s enrollee characteristics.
Like many other studies, interpretation of this research is limited by a lack of data on utilization by Medicare Advantage enrollees. Consequently, I focused on three states with superior data availability. While large numbers of Medicare beneficiaries, including many MA enrollees reside in these states, results may not generalize to all states, particularly more rural areas.
Since my data ended before the introduction of Part D, MA enrollment was the only way for many seniors to access prescription drug coverage during the study period. Consequently, findings may overstate the relationship between payment rates and ACS hospitalizations if plans now use additional payments to provide benefits that are less effective than drug coverage at preventing hospitalizations. While MA enrollment was dominated by HMOs during the study period, the program currently includes many Private Fee-for-Service and Preferred Provider Organizations. These types of plans typically do less care managing, which would reduce the potential for spillover effects to FFS, again suggesting that results in this paper represent an upper bound estimate of the relationship between MA payment changes and rates of ACS admissions. During the study period, large increases in payment rates were more common than large decreases. The simulation results assume that the response to a payment cut and payment increase are similar in magnitude but move in opposite directions.
It is important to note that quality and access are multidimensional constructs, and the rates of hospitalization included in this study only touch on some of measures. This is unavoidable given current data availability. As PPACA changes are implemented, additional research will be needed to assess the implications of payment cuts for Medicare quality and access. Improved access to MA encounter data can aid these evaluations.
Implications for Health Reform
Recent experience with changes in Medicare Advantage payment rates indicate that implementation of the PPACA provisions to reduce MA payment rates will be associated with an increase in rates of ambulatory care sensitive hospitalizations. It is unknown whether other health reform provisions such as the closing of the donut hole and additional free preventive exams will be sufficient to counteract these effects. One way to mitigate adverse effects of spending cuts is through policy efforts to facilitate access to vaccinations and antibiotics that can help prevent acute ACS hospitalizations. However, ACS admissions amongst MA enrollees related to chronic condition management account for the majority of new hospitalizations projected, highlighting a potential need for alternative care management strategies for Medicare beneficiaries with chronic illnesses.
While the expected increases in acute and chronic ACS admissions associated with a 5 percent rate cut are relatively small in magnitude as proportions of the rate per thousand Medicare beneficiaries, the total number of new hospitalizations will be economically significant when aggregated over 39 million elderly Medicare beneficiaries. Trends in hospitalizations and other quality measures should be monitored as MA payment rates and county benchmarks are reduced to ensure that unintended costs of the policy change do not further strain Medicare sustainability or beneficiary health.
Footnotes
A trichotomous specification (such as that used by Bundorf et al. (2004)) was not possible in this sample because there is insufficient variation amongst counties with very low penetration (under 10 percent) to identify the coefficient in a fixed effect model.
References
- Agency for Healthcare Research and Quality. Tools for Monitoring the Health Care Safety Net. Rockville, MD: Agency for Health care Research and Quality; 2003. [Google Scholar]
- Atherly A, Thorpe KE. Value of Medicare Advantage to Low-Income and Minority Medicare Beneficiaries. Emory University, Rollins School of Public Health; 2005. mimeo. [Google Scholar]
- Baker LC. The effect of HMOs on Fee-for-Service Health Care Expenditures: Evidence from Medicare. Journal of Health Economics. 1997;16(3):453–481. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- Baker L. Managed Care and Technology Adoption in Health Care: Evidence from Magentic Resonance Imaging. Journal of Health Economics. 2001;20(3):395–421. doi: 10.1016/s0167-6296(01)00072-8. [DOI] [PubMed] [Google Scholar]
- Baker L, Brown M. Managed Care, Consolidation among Health Care Providers, and Health Care: Evidence from Mammography. Rand Journal of Economics. 1999;30(2):351–74. [PubMed] [Google Scholar]
- Baker LC, Phillips KA, Haas JS, Liang SY, Sonneborn D. The effect of area HMO market share on cancer screening. Health Services Research. 2004;39(6 pt 1):1751–1772. doi: 10.1111/j.1475-6773.2004.00316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson RA, Dowd BE. Medicare Advantage Plans at a Crossroads—Yet again. Health Affairs. 2009;28(1):w29–w40. doi: 10.1377/hlthaff.28.1.w29. [DOI] [PubMed] [Google Scholar]
- Bundorf MK, Schulman KA, Stafford JA, Gaskin D, Jollis JG, Escarce JJ. Impact of Managed Care on the Treatment, Costs, and Outcomes of Fee-for-Service Medicare Patients with Acute Myocardial Infarction. Health Services Research. 2004;39(1):131–52. doi: 10.1111/j.1475-6773.2004.00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J, Chernew M, McLaughlin C. CMS Payments Necessary to Support HMO Participation in Medicare Managed Care. Forum for Health Economics & Policy. 2002;5(2) http://www.bepress.com/fhep/5/2. [Google Scholar]
- Cawley J, Chernew M, McLaughlin C. HMO Participation in Medicare+Choice. Journal of Economics and Management Strategy. 2005;14(3):543–74. [Google Scholar]
- Chernew M, DiCicca P, Town R. Managed care and medical expenditures of Medicare beneficiaries. Journal of Health Economics. 2008;27(6):1451–61. doi: 10.1016/j.jhealeco.2008.07.014. [DOI] [PubMed] [Google Scholar]
- Cutler DM, McClellan M, Newhouse How Does Managed Care Do It? Rand. Journal of Economics. 2000;31(3):526–48. [PubMed] [Google Scholar]
- Foster RS. [Accessed 28 September 2010];Estimated Financial Effects of the “Patient Protection and Affordable Care Act,” as Amended. 2010 Available at http://www.cms.gov/ActuarialStudies/Downloads/PPACA_2010-04-22.pdf.
- Gaskin DJ, Hadley J. The impact of HMO penetration on the rate of Hospital Cost Inflation, 1985–1993. Inquiry. 1997;4(3):205–216. [PubMed] [Google Scholar]
- Glied S, Zivin JG. How Do Doctors Behave When Some (but Not All) of Their Patients Are in Managed Care. Journal of Health Economics. 2002;21(2):337–53. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- Gold M. Can Managed Care and Competition Control Medicare Costs? Health Affairs. 2003:W3-176–W3-188. doi: 10.1377/hlthaff.w3.176. web exclusive. [DOI] [PubMed] [Google Scholar]
- Gold M, Achman L, Mittler J, Stevens B. Monitoring Medicare + Choice: What have we learned? Findings and operational insights for Medicare Advantage. Washington, DC: Mathematica Policy Research; 2004. [Google Scholar]
- Heidenreich PA, McClellan M, Frances C, Baker LC. The Relationship between Managed Care Market Share and the Treatment of Elderly Fee-for-Service Patients with Myocardial Infarcation. American Journal of Medicine. 2002;112(3):176–82. doi: 10.1016/s0002-9343(01)01098-1. [DOI] [PubMed] [Google Scholar]
- Herszenhorn DM. Medicare Advantage: Suddenly a Battle with Three Fronts. [accessed on 28 September 2009];New York Times Prescriptions Blog. 2009 Sep;2009 Available from: http://prescriptions.blogs.nytimes.com/2009/09/23/medicare-advantage-suddenly-a-battle-with-three-fronts/?scp=1&sq=medicare%20advantage&st=cse. [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Spending Policy. Washington, DC: 2004. [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington, DC: MedPAC; 2009. [Google Scholar]
- Miller RH, Luft HS. HMO plan performance update: An analysis of the literature. Health Affairs. 2002;21(4):63–86. doi: 10.1377/hlthaff.21.4.63. [DOI] [PubMed] [Google Scholar]
- UCSF-Stanford Evidence-based Practice Center. Refinement of the HCUP quality indicators. Rockville, MD: Agency for Health care Research and Quality; 2001. [PubMed] [Google Scholar]
- Wall Street Journal. Anonymous editorial in Wall Street Journal. Vol. 2009. New York, N.Y: 2009. Sep 11, Medicare for Dummies; p. A.18. (Eastern edition) [Google Scholar]
- Zhan C, Miller MR, Wong H, Meyers GS. The effects of HMO penetration on preventable hospitalizations. Health Services Research. 2004;39(2):345–361. doi: 10.1111/j.1475-6773.2004.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]