Abstract
β-alanine, a popular supplement for muscle building, induces itch and tingling after consumption, but the underlying molecular and neural mechanisms are obscure. Here we show that, in mice, β-alanine elicited itch-associated behavior that requires MrgprD, a G protein-coupled receptor expressed by a subpopulation of primary sensory neurons. These neurons exclusively innervate the skin, respond to β-alanine, heat and mechanical noxious stimuli but do not respond to histamine. In humans, intradermally injected β-alanine induced itch but neither wheal nor flare suggesting that the itch was not mediated by histamine. Thus, the primary sensory neurons responsive to β-alanine are likely part of a histamine-independent itch neural circuit and a target for treating clinical itch that is unrelieved by anti-histamines.
Introduction
β-alanine is one of a very few naturally occurring beta amino acids in humans. It is a widely used as a supplement for muscle building because it is a major component of the dipeptide carnosine (beta-alanyl-L-histidine) and can boost the synthesis of intramuscular carnosine, which is an effective buffer to prevent muscle cells from becoming acidic, thereby decreasing fatigue during exercise (Baguet et al., 2010). A common sensory side effect of β-alanine is skin paresthesias including itch and tingling (Décombaz et al., 2012), but the underlying molecular mechanisms remain elusive.
β-alanine is widely distributed not only in muscle but in the nervous system and the skin (Crush, 1970; Tiedje et al., 2010).β-alanine binds and activates MrgprD receptors in humans and rodents (Shinohara et al., 2004). MrgprD, a G protein-coupled receptor (GPCR), is highly expressed in a subset of small-diameter dorsal root ganglion (DRG) neurons implicated in mechano-sensation (Dong et al., 2001; Shinohara et al., 2004; Cavanaugh et al., 2009). Strikingly, MrgprD+ axons exclusively innervate the epidermis of hairy and glabrous skin (Zylka et al., 2005), raising the untested possibility they may be involved in the skin-specific sensation of itch.
GPCRs play essential roles in mediating itch signals by directly detecting pruritic compounds in the skin (Liu et al., 2009; Liu et al., 2011). Therefore, it is interesting to test whether β-alanine-induced itch is mediated by MrgprD. Here we show that a local intradermal injection of β-alanine directly induced itch in humans, confirming that β-alanine induces itch through a peripheral, cutaneous mechanism. We then show that β-alanine given as an oral supplement or injected intradermally elicited itch-associated behavior that was severely reduced in MrgprD−/− mice. Furthermore, β-alanine directly excited DRG neurons via MrgprD. Lastly, by electrophysiologically recording from cutaneous sensory neurons, in vivo, we found that β-alanine activated a subset of MrgprD-expressing C-fiber mechano-sensitive neurons, namely those responsive to heat. Because these neurons did not respond to histamine, they are candidates for mediating the itch and associated sensations elicited by histamine-independent pruritic stimuli including β-alanine, heat and mechanical stimuli.
Materials and Methods
Psychophysical study in humans
Eleven healthy subjects (aged 23–45 years), eight females and three males, were tested with protocols approved by the Yale University Human Investigation Committee.
The volar forearm was intradermally injected with 10 μl of β- or L-alanine (Sigma Aldrich, St. Louis, MO) in amounts of 22.5, 45, 90, or 180 μg dissolved in a vehicle of sterile extracellular fluid (Sikand et al. 2011). The subjects used the generalized labeled magnitude scale to rate the perceived intensity of any itch, pricking/stinging, and burning evoked by the stimulus (Sikand et al., 2011).
Behavioral studies in mice
The behavioral testing and analyses were performed with an experimenter blind to experimental condition using protocols approved by the Animal Care and Use Committee of Johns Hopkins University School of Medicine. The mice (MrgprD knockout) (Zylka et al., 2005; Rau et al., 2009) were 2 to 3 month-old males (20–30 g) that had been backcrossed to C57Bl/6 mice for at least ten generations.
Oral consumption of β-alanine
The previously acclimated mouse, held in the experimenter’s hand, was fed, by pipette, either β-alanine (40 mg/ml) in a vehicle of 5% sucrose in water or the vehicle alone and then placed in a test chamber. Behavior was video recorded for 40 min. From analyses of video recordings, the number of bouts of scratching of the cheek (vs. the back) with the hind paw and the number of wipes of the cheek with the forepaw (Shimada and LaMotte, 2008) were counted as these were the dominant behaviors.
Intradermal injection of β-alanine
In the mouse acclimatized to the test chamber, either β-alanine (50, 20 or 10 mM), histamine dihydrochloride (27 mM) or vehicle (saline) each in 10 μl was injected intradermally into the cheek and behavioral responses video recorded for 15 min. The video recordings were subsequently viewed to extract the number of bouts of scratching and the number of wipes directed toward the site of injection (Shimada and LaMotte, 2008).
Calcium imaging
Dorsal root ganglia from all spinal levels of 3-week-old mice were dissociated cultured 18–20 hours as previously described (Liu et al. 2009). There was no NGF or GDNF in the culture media for calcium imaging experiment whereas GDNF (20 ng/ml) was added to the media for whole-cell recordings. Neurons were loaded with Fura 2-acetomethoxyl ester (Molecular Probes) for 30 min in the dark at room temperature. After washing, cells were imaged at 340 and 380 nm excitation to detect intracellular free calcium. We applied chloroquine (1mM), histamine (100 μM), and β-alanine (1mM) to DRG neurons. To compare the response to histamine or β-alanine between WT and MrgprD-deficient DRG neurons, calcium imaging assays were performed with an experimenter blind to genotype.
Whole-cell current-clamp recordings of cultured DRG neurons
Current clamp recordings were performed as previously described (Liu et al., 2009). Briefly, action potential measurements were performed with an Axon 700B amplifier and the pCLAMP 9.2 software package (Axon Instruments). Electrodes were pulled (Narishige, Model pp-830) from borosilicate glass (WPI, Inc). Neurons were perfused with β-alanine for 10 sec and washed for 3 min. All experiments were performed at room temperature (~25°C).
In-vivo electrophysiological recording
Nine adult male MrgprD-GFP knock-in (expressing GFP in MrgprD expressing neurons) (Zylka et al., 2005) each weighing 23–29 g were used. The use and handling of animals were approved by the Institutional Animal Care and Use Committee of the Yale University School of Medicine.
Primary sensory neurons innervating the skin on the hind limb of the mouse were electrophysiologically recorded in vivo as described (Ma et al., 2010; 2011). Mice were anesthetized with isoflurane inhalation, artificially ventilated and their core maintained at 36–38°C After a laminectomy at the levels of L2–L6, the L3 or L4 DRG was exposed, separated from surrounding tissue, fixed to a plate and superfused with warm, oxygenated, artificial cerebrospinal solution within a pool formed by ring to which the skin was sewn. After removal of the epineurium, the cells on the surface of the ganglion were viewed using an upright microscope at 400X either via reflection microscopy and, to identify the presence of GFP indicative of MrgprD expression (epifluorescence microscopy).
Extracellular recording was performed using a micropipette electrode (Ma et al, 2010; 2011). The sensory submodality of a neuron was classified by its responses to mechanical, thermal and chemical stimulation of its peripheral receptive field, These stimuli included innocuous stroking with a cotton tipped probe, a gentle pinch using the experimenter’s fingers and von Frey filaments with a fixed tip diameter (100 or 200 μm) but delivering different bending forces (for noxious mechanical stimuli), a temperature-controlled chip-resister heating probe, or ice (to deliver noxious thermal stimuli) (Ma et al., 2011). Neurons identified by conduction velocity as having C-fibers were classified as CM if responsive (exhibited multiple action potentials) to noxious mechanical stimuli or CMH if responsive to mechanical and heat noxious stimuli (51 °C, 5 s). Next, 5 μl of vehicle (0.9% NaCl), histamine (1μg/μl in vehicle), or β-alanine (50 mM in vehicle) was injected intradermally into the receptive field using a microsyringe with a 31G needle (sequence of chemical delivery varied). The chemically evoked discharges typically lasted from 2–10 min after which at least 5 min elapsed before the next injection.
Results
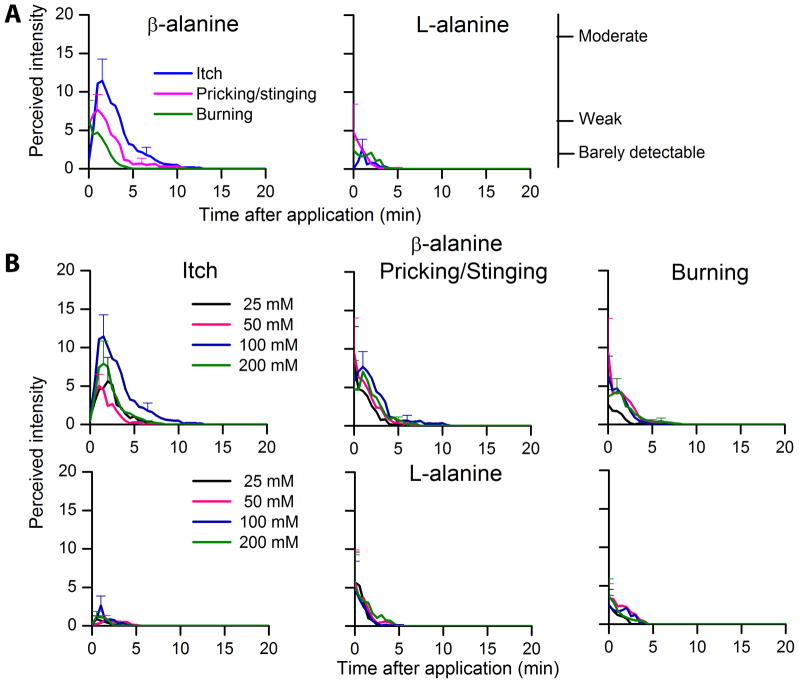
Intradermal injection of β-alanine evokes itch in humans
It is not known whether β-alanine, consumed orally in humans, elicits itch by acting directly (or through a metabolite) on the nerve endings of pruriceptive neurons or at some other site along the pathways mediating itch. Here, in tests in humans, intradermally injected β-alanine (90 μg or 100 mM) elicited itch in all subjects, who also reported lesser sensations of pricking/stinging and burning (Fig. 1A). The sensations peaked within the first few minutes and declined slowly over time. The same dose of L-alanine, the proteinogenic α-amino acid that cannot bind or activate MrgprD (Shinohara et al., 2004), produced a weak, transient itch in only 5 of 11 subject (Fig. 1A). The mean area under the curve (AUC), peak magnitude, and duration of itch were each significantly greater for β-alanine compared to L-alanine (p < 0.05. paired Student’s t-tests). In comparison with β-alanine, L-alanine also evoked significantly lesser sensations of pricking and burning (as measured by peak magnitude, duration and/or AUC (p < 0.05). A significant effect of dose was obtained for AUC (p = 0.012), peak magnitude (p = 0.04), and duration (p = 0.04) of itch only for β-alanine (one-way repeated measures analyses of variance) (Fig. 1B). But the highest magnitude of itch was observed with 90 μg (100 mM). That is, an effect of dose was obtained on all the itch parameters. But there was no effect of dose on any parameters measured for pricking/stinging and burning produced by the 4 tested doses. These studies demonstrate that β-alanine can act directly and peripherally to elicit the sensation of itch. Importantly, no flare or wheal was induced by β-alanine injection in human skin, suggesting that β-alanine -induced itch is mediated by a histamine-independent neural pathway.
Figure 1. Intradermal injection of β-alanine evokes itch in humans.
(A) Time course of the mean perceived intensity of itch and nociceptive sensations evoked by intradermal injection of 90 μg (100 mM) of β-alanine or L-alanine. The mean ratings of itch, pricking/stinging and burning obtained from 11 subjects are plotted for successive intervals of 30 s after injection. Beginning with the peak rating of each sensory quality the SEM is plotted every 5 minutes. The position of three verbal descriptors (right vertical axis) is shown in correspondence with the ratings of mean perceived intensity (left vertical axis). (B) Time course of the mean perceived intensity of itch and nociceptive sensations evoked by different doses of β-alanine and L-alanine in the same subjects.
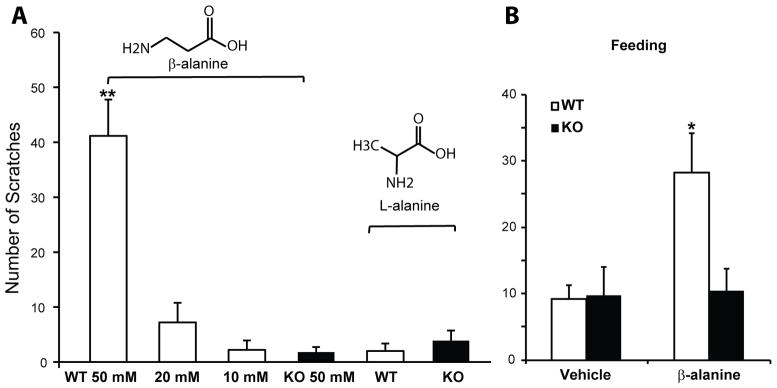
MrgprD mediates β-alanine induced itch
To determine if the β-alanine-induced itch response is mediated by MrgprD, we compared the scratching behavior between wild-type (WT) and MrgprD−/− mice. Cheek injections of a series of concentrations of β-alanine elicited dose-dependent site-directed bouts of scratching in WT mice (Fig. 2A). The mice exhibited few if any pain-associated behaviors denoted by site-directed wiping of the injection site with the forepaw suggesting β-alanine mainly induces itch not pain in mice. However, it cannot be ruled out that non-painful nociceptive sensations, such as the pricking or burning reported by humans in response to β-alanine, might also be present in mice but of insufficient magnitude to elicit site-directed wiping. Almost no scratching was detected in MrgprD−/− mice (WT vs. KO, 41.1 ± 6.5 vs. 1.8 ± 0.9 bouts, n=6 vs. 5, p=0.002) (Fig. 2A). MrgprD−/− mice did not have any scratching deficits in response to cheek injection of histamine (50 μg/10 μl) compared with WT controls (WT vs. KO, 26 ± 3.2 vs. 30.3 ± 11.1 bouts, n=11 vs. 12, p = 0.72), indicating that MrgprD specifically mediates β-alanine-induced itch. As a negative control, L-alanine failed to induce a scratching response (Fig. 2A). These results suggest that β-alanine directly induces itch sensation in an MrgprD-dependent manner.
Figure 2. MrgprD is required for β-alanine -induced scratching in mice.
(A) Cheek injection of β-alanine induced site-directed scratching in WT but not MrgprD−/− mice. β-alanine induced significant scratching in WT during the first 15 min after injection in a dose-dependent manner (WT, 50 mM, n=6; 20 mM, n=5; 10 mM, n=5). By contrast, few scratching bouts were detected in MrgprD−/− mice after β-alanine cheek injection (n=5). L-alanine, the proteinogenic α-amino acid, did not induce a significant itch response (WT, n=6; KO, n=8). (B) Orally administering β-alanine induced itch in wild-type (WT) but not MrgprD−/− (KO) mice. The total number of scratching bouts during the 40 min after β-alanine feeding (40 mg/kg body weight) was significantly higher in WT mice than in MrgprD−/− mice (n=5 per genotype) (*WT vs. KO. All error bars represent standard error of the mean (SEM). * p<0.05, **p<0.01, ***p<0.001; Student’s t-test.
Since oral consumption of β-alanine evokes itch sensation in humans, we asked if feeding mice with β-alanine can induce itch-associated behavior. To establish an animal model for β-alanine-evoked side effects, we fed WT mice sucrose water supplemented with β-alanine (40 mg/kg), a dose equivalent to the lower limit of the dose that people normally take (Harris et al., 2006). The latency of the onset of the scratching (occurring primarily on the cheek and nape around the neck) in mice in each mouse was about 10 min (617 ± 188 sec) which is similar to that reported by humans (about 20 min) when taking β-alanine orally (Harris et al. 2006). MrgprD−/− mice exhibited significantly less scratching than WT controls (28.2± 6.0 vs. 10.4 ± 3.3 bouts, n=5, p=0.032) (Fig. 2B). The level of scratching found in the mutant mice was similar to that of both genotypes after drinking sucrose water (9.75 ± 4.21 bouts). Together, these data demonstrate that oral administration of β-alanine induces itch behavior in mice and that this effect is MrgprD-dependent.
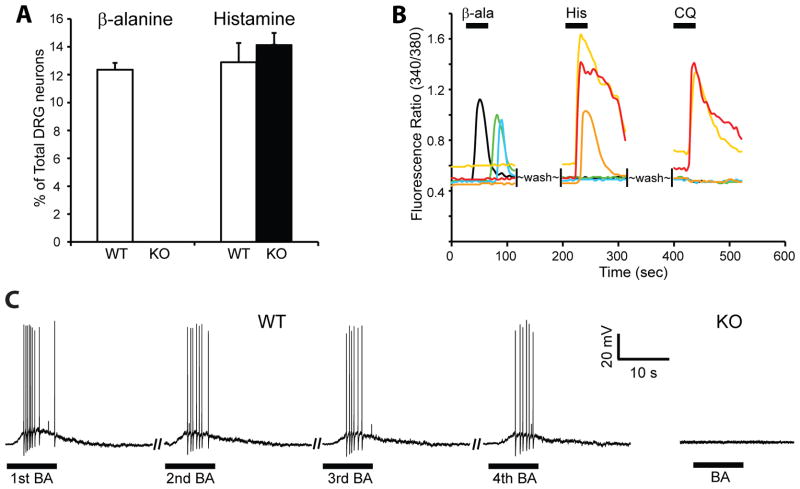
β-alanine directly excites DRG neurons in an MrgprD-dependent manner
We next examined if β-alanine directly activated MrgprD+ DRG neurons and if the lack of β-alanine -induced scratching in MrgprD−/− mice is due to a deficit in the response of mutant DRG neurons to β-alanine. Indeed, 1 mM β-alanine triggered an intracellular calcium increase in approximately 12% of total DRG neurons from WT mice, whereas it failed to activate any DRG neurons from MrgprD−/− mice (Fig. 3A), suggesting that MrgprD is required for the response of DRG neurons to β-alanine. There was no effect of the KO on the responses to histamine (Fig. 3A). To confirm that β-alanine-sensitive neurons express MrgprD, we used MrgprD-GFP knock-in (MrgprDGFP/+ mice that have one copy of WT MrgprD and one copy of MrgprD deleted by GFP knockin) in which MrgprD-expressing neurons are labeled with GFP (Zylka et al., 2005). We found β-alanine only activated GFP+ MrgprD-expressing neurons and not neurons that did not express GFP. In addition, only 43.3% of GFP+ neurons showed intracellular calcium rises in response to β-alanine, suggesting that downstream signaling components are not completely co-expressed with MrgprD. We also examined whether β-alanine induced action potentials in dissociated DRG neurons using whole-cell patch recording. In WT, β-alanine sensitive neurons fired multiple action potentials upon β-alanine treatment and could repeatedly be activated by β-alanine, at intervals after washout of 3 to 5 min, without significant tachyphylaxis (Fig. 3C). In contrast, no MrgprD-deficient neurons (i.e., GFP+ DRG neurons from MrgprDGFP/GFP mice; i.e. two copies of MrgprD deleted by GFP knockin) fired action potentials upon similar treatment (Fig. 3C). These data suggest that β-alanine-induced itch sensation is likely caused by direct activation of MrgprD that leads to firing of DRG neurons.
Figure 3. The response of DRG neurons to β-alanine is MrgprD-dependent.
(A) Approximately 12% of WT DRG neurons responded to β-alanine (1 mM) with increased [Ca2+]i whereas MrgprD−/− DRG neurons did not respond (number of neurons analyzed: WT, n=282; KO, n=212, from 3 mice per genotype). The response to histamine was not impaired in MrgprD−/− neurons. The percentage of MrgprD−/− neurons responding to histamine (100 μM) was similar to that of WT neurons (>300 neurons analyzed, 3–4 mice per genotype). (B) Representative traces of DRG neurons from MrgprDGFP/+ mice in calcium imaging assays. β-alanine only activated GFP+ neurons as monitored by increased [Ca2+]i with calcium imaging. β-alanine -sensitive neurons (black, green, and blue traces; n=91) did not respond to histamine (100 μM) or chloroquine (1 mM), and histamine- and chloroquine-sensitive neurons (yellow, red, and orange traces) did not respond to β-alanine (>200 neurons from 3 mice). (C)β-alanine (1 mM) induced action potentials in DRG neurons. In WT DRG, β-alanine -sensitive neurons (as determined by calcium imaging, n=8) fired action potentials upon repeated β-alanine treatment. In contrast, none of the neurons tested from MrgprD−/− mice showed any response to the drug (n=7). Error bars represent SEM.
β-alanine sensitivity defines a unique subset of histamine-insensitive DRG neurons
To further characterize the population of β-alanine -sensitive neurons, we tested their responsiveness to other itch-inducing molecules in cultured DRG using calcium imaging. All β-alanine -sensitive neurons failed to respond to histamine (Fig. 3B), suggesting that β-alanine sensitivity may define a histamine-independent itch-sensing neuronal population in the DRG. Consistently, the percentages of total WT and MrgprD−/− DRG neurons responding to histamine were similar (Fig. 3A). Furthermore, β-alanine -responding neurons were not sensitive to chloroquine (CQ; Fig. 3B), a drug used to treat and prevent malaria but with serious pruritic side effects (Mnyika and Kihamia, 1991). We previously found that MrgprA3 functions as a major receptor for CQ and mediates CQ-induced itch (Liu et al., 2009). CQ-sensitive DRG neurons also respond to histamine (Liu et al., 2009). In situ hybridization experiments indicated that MrgprA3 and MrgprD are expressed by different populations of DRG neurons (Dong et al., 2001; Zylka et al., 2005), which is consistent with the current finding that β-alanine -sensitive neurons respond to neither CQ nor histamine.
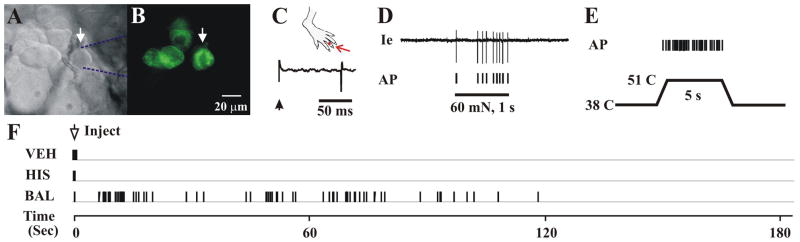
We next studied MrgprD+ neurons in a more physiologically relevant setting with an in vivo electrophysiological recording method (Ma et al., 2010). The advantage of this method is that it allows us to first positively identify neurons of interest (in this case, GFP+ neurons in MrgprDGFP/+ mice; Fig. 4A, B) and then study their peripheral receptive field properties in living animals. A total of 19 GFP+ DRG neurons from MrgprDGFP/+ mice were recorded. All neurons were cutaneous C-nociceptive units (conduction velocity range: 0.50 – 0.75 m/s), including 9 CMH (responding to both mechanical and heat stimuli) and 10 CM (responding only to noxious mechanical stimulation) neurons (Fig. 4C–E). Two of the CMH neurons also responded to cold stimulation (ice, 20 s). All neurons were initially silent (not spontaneously active) before testing. Injection of vehicle never evoked any discharges beyond insertion of the needle. Five of the 9 CMH neurons were tested with β-alanine, another 2 were tested with histamine only, and the remaining 2 CMH neurons were tested with both chemicals. All 10 CM neurons were tested with β-alanine, of which 7 were also tested with histamine. Each chemical was injected intradermally into the receptive field in the hind-paw.β-alanine evoked discharges in all 7 CMH neurons tested but not in any of the 10 CM neurons (Fig. 4F). In contrast, none of the 4 CMH or 7 CM neurons showed any response to histamine (Fig. 4F). Histamine injection was able to activate other CMH neurons that did not express GFP (data not shown). Both in vitro DRG calcium imaging and in vivo DRG recording data demonstrate that MrgprD-expressing neurons were of two types: Those that were activated by β-alanine and by heat and those that were not. Neither type was activated by histamine.
Figure 4. β-alanine -sensitive neurons are C-mechano-heat nociceptive (CMH) neurons and do not respond to histamine.
(A) Bright-field image of a neuronal recording (arrow) with an extracellular electrode (outlined with dashed blue lines). (B) Fluorescent microscopy revealed the expression of GFP (i.e., MrgprD+) in this neuron. (C) Location of the cutaneous receptive field (RF, red dot) of this neuron on the hairy skin of the hind-paw and conduction velocity (0.64 m/s, lower trace) obtained with electrical stimulation (arrow) of the RF. (D) Responses of this neuron to a 60 mN force via a 200 μm diameter probe applied to the RF (1 sec) with original extracellular recording trace and action potentials (AP) indicated below. (E) Response to heat stimulation (38 to 51°C, 5 sec) indicates that this is a CMH nociceptive neuron. (F) Responses of the above CMH neuron to the intradermal injection of vehicle (VEH), histamine (HIS) and β-alanine (BAL).
Discussion
Our findings indicate that skin sensations evoked by β-alanine are mediated by MrgprD expressed in cutaneous sensory neurons. Although another study showed that MrgprD enhanced the excitability of small-diameter DRG neurons (Rau et al., 2009), its function in somatosensation has not been directly demonstrated. In this study, we provide the first evidence that β-alanine can directly trigger action potentials in both in vitro cultures and in vivo DRG neuron recordings. Furthermore, our mouse behavioral and human psychophysical data suggest that a major role of MrgprD in somatosensation is itch. These studies provide a molecular explanation for β-alanine-induced itch and demonstrate that β-alanine -induced itch-mediating neural activity originates in the peripheral- and not central nervous system.
β-alanine sensitivity defines a unique population of itch-mediating neurons and further demonstrates the functional diversity of primary sensory neurons in DRG. MrgprD-expressing neurons comprise a majority of non-peptidergic, small-diameter neurons in the DRG. Dissociated DRG neuron recordings, skin nerve recordings, and neuronal ablation studies suggest MrgprD+ neurons are un-myelinated (C-fiber), mechanosensitive nociceptive neurons (Dussor et al., 2008; Cavanaugh et al., 2009; Rau et al., 2009). Behaviorally, mice lacking MrgprD+ neurons exhibit reduced mechanical but not thermal pain, suggesting MrgprD+ neurons are mainly involved in mechano-sensation in vivo (Cavanaugh et al., 2009). Here we reveal the unexpected heterogeneity and functional diversity of MrgprD+ neurons. Only a subset of MrgprD-expressing neurons is involved in β-alanine evoked itch. Interestingly, this subset has physiological properties distinct from those of β-alanine -insensitive but MrgprD+ neurons. In vivo DRG recordings showed that β-alanine -sensitive neurons account for ~40% of total MrgprD-expressing neurons and respond to heat stimuli. By contrast, the β-alanine -insensitive but MrgprD+ neurons are insensitive to heat. In the future, it would be interesting to investigate the molecular basis of the distinct physiological properties of MrgprD-expressing neurons. Furthermore, β-alanine sensitivity implies a functional diversity of MrgprD-expressing neurons and raises the question of whether a fraction of MrgprD-expressing neurons are dedicated to the transduction of pruritic chemicals and mediate itch whereas others might mediate mechanically evoked pain. Our data are consistent with the presence of two different types of itch mediating neurons, one responsive to β-alanine but not to histamine and another responsive to histamine but not MrgprD+ (Liu et al., 2009). The MrgprD molecular marker coupled with the response to β-alanine provide a means of identifying the same itch-mediating neurons in vitro and in vivo.
Our studies also developed a novel, physiologically relevant method to study itch. Most if not all current animal models of acute itch entail skin injection of itch-inducing compounds. However, most drug-, supplement-, and food-induced itch are triggered by oral consumption. Oral administration of β-alanine provides a valuable way to study itch, especially for investigating itch side effects caused by many orally taken medicines (Reich et al., 2009). Because only healthy volunteers were tested it remains to be determined whether the levels of β-alanine or some other endogenous chemical mediator may be capable of activating MrgprD expressing neurons and contribute to itch under pathological conditions. Taken together, the identification of MrgprD as an itch-mediating receptor should open new avenues for the exploration of pruriceptive neuronal function and circuitry as well as the development of novel anti-pruritic drugs.
Acknowledgments
We thank Drs. David Anderson and Mark Zylka for providing MrgprD-GFP knockin mice. We also thank Kush Patel for helpful comments on the manuscript. The work was supported by grants from the NIH to X.D. (NS054791 and GM087369) and R.H.L. (NS047399 and NS014624).
References
- Baguet A, Koppo K, Pottier A, Derave W. Beta-alanine supplementation reduces acidosis but not oxygen uptake response during high-intensity cycling exercise. Eur J Appl Physiol. 2010;108:495–503. doi: 10.1007/s00421-009-1225-0. [DOI] [PubMed] [Google Scholar]
- Cavanaugh DJ, Lee H, Lo L, Shields SD, Zylka MJ, Basbaum AI, Anderson DJ. Distinct subsets of unmyelinated primary sensory fibers mediate behavioral responses to noxious thermal and mechanical stimuli. Proc Natl Acad Sci U S A. 2009;106:9075–9080. doi: 10.1073/pnas.0901507106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crush KG. Carnosine and related substances in animal tissues. Comp Biochem Physiol. 1970;34:3–30. doi: 10.1016/0010-406x(70)90049-6. [DOI] [PubMed] [Google Scholar]
- Décombaz J, Beaumont M, Vuichoud J, Bouisset F, Stellingwerff T. Effect of slow-release β-alanine tablets on absorption kinetics and paresthesia. Amino Acids. 2012 Jul;43(1):67–76. doi: 10.1007/s00726-011-1169-7. [DOI] [PubMed] [Google Scholar]
- Dong X, Han S, Zylka MJ, Simon MI, Anderson DJ. A diverse family of GPCRs expressed in specific subsets of nociceptive sensory neurons. Cell. 2001;106:619–632. doi: 10.1016/s0092-8674(01)00483-4. [DOI] [PubMed] [Google Scholar]
- Dussor G, Zylka MJ, Anderson DJ, McCleskey EW. Cutaneous sensory neurons expressing the Mrgprd receptor sense extracellular ATP and are putative nociceptors. J Neurophysiol. 2008;99:1581–1589. doi: 10.1152/jn.01396.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris RC, Tallon MJ, Dunnett M, Boobis L, Coakley J, Kim HJ, Fallowfield JL, Hill CA, Sale C, Wise JA. The absorption of orally supplied beta-alanine and its effect on muscle carnosine synthesis in human vastus lateralis. Amino Acids. 2006;30:279–289. doi: 10.1007/s00726-006-0299-9. [DOI] [PubMed] [Google Scholar]
- Liu Q, Tang Z, Surdenikova L, Kim S, Patel KN, Kim A, Ru F, Guan Y, Weng HJ, Geng Y, Undem BJ, Kollarik M, Chen ZF, Anderson DJ, Dong X. Sensory Neuron-Specific GPCR Mrgprs Are Itch Receptors Mediating Chloroquine-Induced Pruritus. Cell. 2009;139(7):1353–65. doi: 10.1016/j.cell.2009.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Weng HJ, Patel KN, Tang Z, Bai H, Steinhoff M, Dong X. The Distinct Roles of Two GPCRs, MrgprC11 and PAR2, in Itch and Hyperalgesia. Sci Signal. 2011;4:ra45. doi: 10.1126/scisignal.2001925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma C, Donnelly DF, LaMotte RH. In vivo visualization and functional characterization of primary somatic neurons. J Neurosci Methods. 2010;191:60–65. doi: 10.1016/j.jneumeth.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma C, Nie H, Gu Q, Sikand P, LaMotte RH. In-vivo responses of cutaneous C-mechanosensitive neurons in mouse to punctate chemical stimuli that elicit itch and nociceptive sensations in humans. J Neurophysiol. 2011;107(1):357–63. doi: 10.1152/jn.00801.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mnyika KS, Kihamia CM. Chloroquine-induced pruritus: its impact on chloroquine utilization in malaria control in Dar es Salaam. J Trop Med Hyg. 1991;94:27–31. [PubMed] [Google Scholar]
- Rau KK, McIlwrath SL, Wang H, Lawson JJ, Jankowski MP, Zylka MJ, Anderson DJ, Koerber HR. Mrgprd enhances excitability in specific populations of cutaneous murine polymodal nociceptors. J Neurosci. 2009;29:8612–8619. doi: 10.1523/JNEUROSCI.1057-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich A, Stander S, Szepietowski JC. Drug-induced pruritus: a review. Acta Derm Venereol. 2009;89:236–244. doi: 10.2340/00015555-0650. [DOI] [PubMed] [Google Scholar]
- Shimada SG, LaMotte RH. Behavioral differentiation between itch and pain in mouse. Pain. 2008;139:681–687. doi: 10.1016/j.pain.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinohara T, Harada M, Ogi K, Maruyama M, Fujii R, Tanaka H, Fukusumi S, Komatsu H, Hosoya M, Noguchi Y, Watanabe T, Moriya T, Itoh Y, Hinuma S. Identification of a G protein-coupled receptor specifically responsive to beta-alanine. J Biol Chem. 2004;279:23559–23564. doi: 10.1074/jbc.M314240200. [DOI] [PubMed] [Google Scholar]
- Sikand P, Shimada SG, Green BG, LaMotte RH. Sensory responses to injection and punctate application of capsaicin and histamine to the skin. Pain. 2011;152:2485–2494. doi: 10.1016/j.pain.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiedje KE, Stevens K, Barnes S, Weaver DF. Beta-alanine as a small molecule neurotransmitter. Neurochem Int. 2010 Oct;57(3):177–88. doi: 10.1016/j.neuint.2010.06.001. [DOI] [PubMed] [Google Scholar]
- Zylka MJ, Rice FL, Anderson DJ. Topographically distinct epidermal nociceptive circuits revealed by axonal tracers targeted to Mrgprd. Neuron. 2005;45:17–25. doi: 10.1016/j.neuron.2004.12.015. [DOI] [PubMed] [Google Scholar]