Abstract
Objectives
To examine the association between policies that govern access to tobacco during adolescence and subsequent adult smoking.
Methods
Adult smoking data from the 1998 through 2006–07 administrations of the U.S. Current Population Survey Tobacco Use Supplement were analyzed using a quasi-experimental approach. Subjects (n = 105,519) were adults, aged 18 to 34 at time of survey. Smoking outcomes included having ever smoked 100 cigarettes, smoking at time of survey, and having smoked 10 or more cigarettes a day conditioned on being an ever-smoker. These were predicted from exposure to state youth access policies at age 17.
Results
Four of the nine policies exhibited significant associations with reduced prevalence of one or more smoking outcomes, primarily among women. Smaller effects for other policies could not be ruled out.
Conclusion
Restrictions on youth access to tobacco may lead to reduction in smoking prevalence later, in adulthood. The effect may be limited to women; we estimate that having all policies in place could be associated with an 14% reduction in lifetime smoking prevalence for women, and an additional 29% reduction in heavy smoking among ever-smokers.
Keywords: tobacco control, policy, adolescence
Introduction
Both opponents of smoking and purveyors of cigarettes have recognized the significance of adolescence as the period during which smoking behaviors are typically developed (1, 2). Accordingly, initiatives to curb youth smoking were among the first federal policy restrictions placed on cigarette sales in the U.S. (3, 4). Adoption of these initiatives was accelerated by passage of the 1992 Synar Amendment to the Federal Alcohol, Drug Abuse, and Mental Health Administration Reorganization Act, which mandated withholding federal block grant money from states that failed to prohibit distribution of tobacco products to persons under age 18, or failed to enforce such prohibitions. Various measures were implemented by individual states to increase retailer compliance with de jure purchase ages, such as restricting physical access to cigarette vending machines and banning the sale of single cigarettes (5, 6).
Adaptation of these policies were partly motivated by community intervention studies suggesting that more uniform compliance with legal purchase age policies would reduce smoking rates among youth (7–11). Some post-implementation studies have suggested that youth access restrictions are effective at reducing smoking among adolescents (12–14), whereas other studies have cast doubt on their effectiveness (6, 15–17). Furthermore, opponents argue that youth access policies could inadvertently glamorize smoking as an adult behavior, thus reinforcing messages historically associated with tobacco advertising (18). Hence, some argue that youth access restrictions divert resources away from well-established and universally targeted tobacco control policies, such as clean indoor air policies, price increases and media campaigns (16, 19).
Youth access measures were not designed to merely delay smoking, but presumably deter progression by delaying onset or reducing intensity of smoking during adolescence. As such, reductions in smoking that persist into adulthood are the proper benchmarks by which these policies should be assessed. In the current study, we examined whether youths who face a restrictive policy environment are less likely to smoke as adults. We analyzed long-term associations between state youth access policies and subsequent adult smoking by taking advantage of state-by-state and year-by-year policy differences as states adopted various measures in response to the Synar Amendment. We expect that policies effective in mitigating youth smoking also influence subsequent adult smoking. It has been shown, for example, that exposure to stricter drinking age laws are associated with lower prevalence of alcohol problems in adulthood, but to our knowledge, parallel studies have not been conducted for tobacco policy (20–22). Hence, we examined whether policy encountered during adolescence is associated with smoking behaviors during adulthood. This hypothesis is consistent with contemporary neurobiological views of adolescence as a critical period for the development of addiction (23–25).
Methods
Overall Approach
Data from the Tobacco Use Supplement (TUS) of the Current Population Survey (CPS) were merged with data on the policy environment that adult participants would have encountered prior to age 18. Past policy exposures were used to predict smoking outcomes at time of survey. State of residence at age 17 and younger would be required to precisely assess exposure; however, the TUS-CPS does not collect historical state of residence data, so we used state of residence at time of survey as a proxy. We describe the reliability of this approximation in detail in the Supplemental Material, wherein we estimate correctly classified policy exposure in 92–96% of cases: We estimate that 86% of the population lived in the same state at time of observation as they lived during adolescence; an additional 6–10% live in states that are concordant with state of emigration with respect to policy. Study procedures were reviewed and approved by the Washington University Human Research Subjects Protection Office.
Subjects
Smoking data from the 1999, 2001–02, 2003, and 2006–07 releases of the TUS-CPS were analyzed. The CPS is a continuing monthly survey—co-sponsored by the U.S. Census Bureau and the U.S. Bureau of Labor Statistics—that collects data on topics related to employment, economic, and demographic characteristics of the U.S. civilian, non-institutionalized population aged 15 and older. The TUS is sponsored by National Cancer Institute (NCI) and the Centers for Disease Control and Prevention (CDC) and is administered along with the CPS during selected months. The TUS-CPS uses a nationally representative sample to provide national and state-level data on smoking and other tobacco use. The survey content, stratified sampling strategy, and detailed methods of the TUS-CPS are described elsewhere (26).
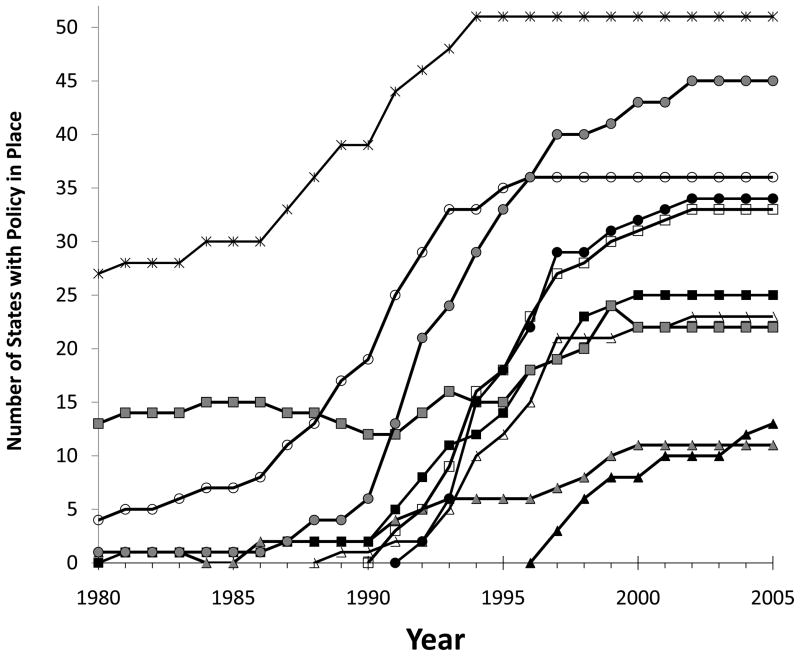
As our interest is in adult smoking, analyses were focused on participants aged 18 and older at time of survey. Because our analytical approach relied on differences across time and state to estimate policy effects, we restricted the analyses to those born during 1973–1986 (N=110,069), as these were the individuals who reached legal purchase age during the period in which youth access policies were changing rapidly (1990 through 2003—see Figure 1). We further restricted the sample to individuals who were living in states where the minimum purchase age for tobacco was 18 or higher (N=105,519 or 95.9% of the sample described above).1 This eliminated heterogeneity with respect to the legal purchase age for tobacco, allowing us to focus on policies that further restrict access to tobacco by youth under age 18.
Figure 1.
Number of states that adopted each of the nine target policies analyzed here, in addition to number of states that adopted a minimum purchase age for tobacco of 18 or older. Policies are: Minimum purchase age of 18 or older (*), signage requirements (○), vending machine restrictions (
 ), inspection requirements (●) statewide enforcement agency mandate (□), graduated penalties (
), inspection requirements (●) statewide enforcement agency mandate (□), graduated penalties (
 ), identification requirements (■), repackaging restrictions (△), free distribution restrictions (
), identification requirements (■), repackaging restrictions (△), free distribution restrictions (
 ), clerk intervention requirements (▲).
), clerk intervention requirements (▲).
Smoking Outcomes
Our first outcome of interest was whether subjects had smoked 100 or more cigarettes in their lifetime (“ever-smoking”), versus those who never smoked, or had smoked fewer than 100 cigarettes. Our second outcome was whether subjects smoked any cigarettes at time of survey. Specifically, subjects were asked whether they “now smoke cigarettes every day, some days, or not at all.” Subjects who reported smoking some days or every day were counted as current smokers and contrasted with those who did not smoke at time of survey. This outcome is not independent from the ever-smoking outcome because CPS-TUS subjects are only asked about current smoking if they reached the 100 cigarette threshold. Nonetheless, it is included because it is the most relevant measure for public health. Finally, among ever-smokers only, we analyzed “current heavy smoking,” defined as smoking 11 or more cigarettes per day at time of survey. For “every day” smokers, cigarettes per day was queried directly; for “some days” smokers, cigarettes per day was determined by multiplying number of days smoked over the past 30 days by number of cigarettes per smoking days and dividing by 30. Heavy smokers were contrasted with light (10 or fewer cigarettes per calendar day) and former smokers. This threshold was based on the “Heaviness of Smoking Index, ” a short test for Nicotine Dependence that counts smoking more than ten cigarettes a day as a symptom of dependence (27).
Independent Variables: Youth Access to Tobacco (YATT) Policies
Smoking outcomes were predicted from nine youth access policy areas that states variously implemented just prior to and after passage of the Synar Amendment. We developed binary scores for each policy that were derived from an ordinal policy coding system proposed by Alciati and colleagues (5) and maintained by the NCI State Cancer Legislative database. Policy data were obtained from the ImpacTeen website, which maintains a database of various tobacco control policies (28). The following contrasts were tested:
Signage Requirements: Provision requiring posting of warning sign about minimum purchase age and penalizing retailers who fail to post such a sign versus no requirement.
Vending Machine Restrictions. Bans or location restrictions on cigarette vending machines versus no bans or restrictions.
Inspection Requirements. Provisions for random inspections of retailers to ensure compliance with youth access laws versus no requirements.
Graduated Penalties. Provisions that establish a series of increasingly steeper penalties to retailers who violate any youth access laws versus non-graduated penalties for some or all youth access laws, or delays of penalties beyond three years.
Identification Requirements. Provisions that require retailers to request identification from individuals appearing to be 21 or younger versus no provision.
Repackaging restrictions. Provisions designed to restrict the sale of single cigarettes, or inexpensive small packages, by requiring that cigarettes be sold in a sealed package that meets federal labeling requirements versus no provision.
Statewide Enforcement Authority. Provision establishing a state-wide enforcement authority for tobacco sales versus no provision, or provision only for a non-statewide authority.
Free Distribution Restrictions. Bans on free samples of tobacco products with minimal exceptions, versus no provision or location restrictions only.
Clerk Intervention Requirements. Provisions mandating that tobacco purchases take place through store clerks versus no policy.
Analytic Plan
Our analytical approach was an extension of a classical “differences-in-differences” method that compares two groups at two different time points, and for which one of the groups underwent an environmental/policy change or treatment while the other serves as a control (29, 30). We used logistic regression to extend the two-by-two analysis to multiple groups at multiple time points. In our case, the groups corresponded to states, and time points to birth years, because these variables determined the policy to which a person was exposed. Hence, these variables were included in all models as fixed-effect, unordered categorical covariates. State effects account for all time-invariant characteristics of each state, and birth year effects account for all state-invariant characteristics of each birth-year, allowing for estimation of the exposure effect (31).
In addition to state and birth year fixed effects, we also included observed individual demographic covariates: Respondent-reported race/ethnicity was coded as non-Hispanic White, non-Hispanic Black, Hispanic and Other; the latter category was chosen to avoid small cell sizes and excessive degrees of freedom. Age was incorporated as a continuous measure. Survey wave was included as a categorical variable. Sex was included as a covariate in primary analyses; sex-stratified analyses were also conducted. In second-stage models, three state policy covariates were included: tobacco excise taxes, an index of clean indoor air laws, and inflation-adjusted state tobacco funding per capita. Excise taxes were obtained from historical data (32) and adjusted for inflation based on the annual Consumer Price Index. Clean indoor air laws were coded using a scoring system developed by Chriqui and colleagues (33); both clean indoor air and state tobacco control spending were obtained from the ImpacTeen website (28).
Parameter estimates and standard errors were calculated using the “surveylogistic” procedure in SAS (Version 9.2, SAS Institute, Cary, NC) using state as the clustering unit (34, 35). This approach accounts for intra-correlation of observations within clusters (states) in estimating standard errors, which is the primary consideration in standard error estimation when applying the differences-in-differences approach (31, 35). Sampling error resulting from lower levels of clustering is expected to be small provided that the sample size from within a state is small relative to the full state population (36, 37). Un-weighted data were used for analyses; this is appropriate providing that policy effects are not substantially heterogeneous with respect to selection probability (38).
Results
Sample Description
Table 1 presents the characteristics of the combined TUS-CPS samples, which, after applying exclusion criteria, comprised 105,519 subjects with complete data. Altogether 34.4% reported ever having smoked 100-cigaretttes, and 24.4% reported current smoking at time of survey. Current heavy smoking, defined as smoking more than 11 cigarettes per day, was endorsed by 44.4% of ever-smokers (37,390 subjects).
Table 1.
Prevalence of ever smoking, current smoking, and current heavy smoking among ever-smokers, by demographic group. Individuals born in the U.S. between 1973 to 1986
| Ever-Smoking (100+ Lifetime Cigarettes) | Current Smoking | Current heavy smoking Among Ever-Smokers (N=35,745) | ||||||
|---|---|---|---|---|---|---|---|---|
| N | % of Column | Prevalence | (SE) | Prevalence | (SE) | Prevalence | (SE) | |
| Sex | ||||||||
| Women | 58,244 | 55.2% | 32.2% | (1.3%) | 22.3% | (1.1%) | 42.1% | (1.4%) |
| Men | 47,275 | 44.8% | 37.2% | (1.0%) | 26.9% | (0.9%) | 46.9% | (1.5%) |
| Race/Ethnicity | ||||||||
| White | 72,267 | 68.5% | 39.9% | (0.7%) | 28.0% | (0.7%) | 47.4% | (1.1%) |
| Black | 15,857 | 15.0% | 20.5% | (1.0%) | 16.7% | (0.9%) | 40.7% | (1.4%) |
| Hispanic | 10,445 | 9.9% | 20.5% | (1.0%) | 14.0% | (1.3%) | 25.1% | (2.4%) |
| Other | 6,950 | 6.6% | 30.1% | (2.3%) | 22.3% | (1.8%) | 37.1% | (2.0%) |
| Birth Year1 | ||||||||
| 1973–1979 | 66,781 | 63.3% | 36.2% | (1.1%) | 24.6% | (0.9%) | 43.7% | (1.5%) |
| 1980–1986 | 38,738 | 36.7% | 31.3% | (1.3%) | 24.0% | (1.1%) | 45.8% | (1.3%) |
| Age2 | ||||||||
| 18–24 | 55,218 | 52.3% | 31.7% | (1.2%) | 25.0% | (1.1%) | 49.0% | (1.3%) |
| 25–29 | 39,521 | 37.5% | 36.4% | (1.1%) | 25.3% | (1.0%) | 43.1% | (1.5%) |
| 30–34 | 10,780 | 10.2% | 34.7% | (1.3%) | 21.6% | (1.0%) | 40.5% | (1.5%) |
| Total | 105,519 | 100.0% | 34.4% | (1.1%) | 24.4% | (1.0%) | 44.4% | (1.4%) |
Category is for descriptive purposes only. Birth year was included in regression analyses as an unordered categorical variable.
Age categories for descriptive purposes only. Age was included in regression analyses as a continuous variable.
Youth Access Policies
Figure 1 plots the number of states that had adopted each of the youth access policies by year, using the coding previously described. The period selected for our analyses, 1990 through 2003, bracket most of the policy change associated with the Synar Amendment (see Figure 1). Individual states strengthened some policies during the 1980s, particularly signage requirements and vending machine restrictions, but most major changes took place during the period on which we focus.
Single-Policy Analyses
We predicted the three smoking outcomes from each of the nine policies. Each policy variable was analyzed separately while adjusting for demographic covariates, state and birth year fixed effects, and survey wave as described. Estimates of policy effects were made for the full sample, for men alone, and for women alone. These results are reported in Table 2. In the full sample, only two of the nine policies were associated with statistically significant (p<.05) reductions in any outcome prevalence. Vending machine restrictions appeared to reduce both current smoking (Odds Ratio [OR]=0.93, 95% Confidence Interval [CI]: 0.87, 0.99) and current heavy smoking among ever-smokers (OR=0.91, 95% CI: 0.84, 0.99). Identification requirements were associated with reductions in prevalence of ever-smoking (OR=0.94, 95% CI: 0.88, 0.997) and current smoking (OR=0.98: 95% CI: 0.87, 0.99).
Table 2.
Adjusted associations between seven youth-access policies, analyzed separately, and ever smoking, current smoking, and current heavy smoking among current smokers.
| Ever-Smoking (100+ Lifetime Cigarettes N =105,519) | Current Smoking (N=105,519) | Current heavy smoking Among Ever-Smokers (N=35,745) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Full Sample | ||||||
| Signage requirements | 1.05 | 0.97 – 1.15 | 1.01 | 0.91 – 1.13 | 0.88 | 0.76 – 1.02 |
| Vending machine restrictions | 0.95 | 0.89 – 1.01 | 0.93 | 0.87 – 0.99 | 0.91 | 0.84 – 0.99 |
| Inspection requirements | 1.01 | 0.96 – 1.06 | 1.00 | 0.94 – 1.06 | 0.98 | 0.90 – 1.08 |
| Graduated penalties | 1.01 | 0.95 – 1.07 | 0.99 | 0.91 – 1.07 | 0.99 | 0.88 – 1.12 |
| Identification requirements | 0.94 | 0.88 – 0.997 | 0.93 | 0.87 – 0.99 | 0.97 | 0.88 – 1.08 |
| Repackaging restrictions | 0.95 | 0.89 – 1.01 | 0.94 | 0.87 – 1.01 | 0.94 | 0.85 – 1.04 |
| Statewide enforcement authority | 0.98 | 0.92 – 1.03 | 0.97 | 0.90 – 1.04 | 0.94 | 0.86 – 1.04 |
| Free distribution restrictions | 0.95 | 0.87 – 1.03 | 1.02 | 0.96 – 1.09 | 1.07 | 0.95 – 1.20 |
| Clerk intervention requirements | 0.99 | 0.93 – 1.07 | 1.00 | 0.86 – 1.15 | 1.01 | 0.82 – 1.24 |
| Women | ||||||
| Signage requirements | 1.07 | 0.95 – 1.20 | 1.00 | 0.87 – 1.15 | 0.92 | 0.73 – 1.15 |
| Vending machine restrictions | 0.91 | 0.84 – 0.98 | 0.89 | 0.82 – 0.96 | 0.86 | 0.77 – 0.97 |
| Inspection requirements | 0.99 | 0.94 – 1.05 | 0.98 | 0.92 – 1.05 | 0.96 | 0.85 – 1.09 |
| Graduated penalties | 1.01 | 0.94 – 1.09 | 1.01 | 0.94 – 1.07 | 0.99 | 0.86 – 1.13 |
| Identification requirements | 0.91 | 0.84 – 0.99 | 0.91 | 0.84 – 0.98 | 0.92 | 0.79 – 1.06 |
| Repackaging restrictions | 0.93 | 0.86 – 1.01 | 0.93 | 0.87 – 0.99 | 0.89 | 0.76 – 1.05 |
| Statewide enforcement authority | 0.97 | 0.91 – 1.04 | 0.97 | 0.89 – 1.05 | 0.87 | 0.77 – 0.98 |
| Free distribution restrictions | 0.88 | 0.77 – 0.996 | 0.96 | 0.87 – 1.06 | 1.09 | 0.91 – 1.30 |
| Clerk intervention requirements | 0.99 | 0.91 – 1.09 | 0.99 | 0.86 – 1.14 | 1.08 | 0.86 – 1.36 |
| Men | ||||||
| Signage requirements | 1.04 | 0.96 – 1.11 | 1.03 | 0.91 – 1.16 | 0.84 | 0.72 – 0.98 |
| Vending machine restrictions | 0.99 | 0.92 – 1.06 | 0.96 | 0.88 – 1.05 | 0.97 | 0.88 – 1.07 |
| Inspection requirements | 1.03 | 0.97 – 1.10 | 1.02 | 0.95 – 1.10 | 1.01 | 0.91 – 1.12 |
| Graduated penalties | 1.00 | 0.93 – 1.08 | 0.97 | 0.86 – 1.10 | 1.01 | 0.87 – 1.17 |
| Identification requirements | 0.96 | 0.89 – 1.03 | 0.95 | 0.88 – 1.03 | 1.04 | 0.93 – 1.16 |
| Repackaging restrictions | 0.96 | 0.88 – 1.05 | 0.95 | 0.84 – 1.06 | 0.99 | 0.89 – 1.12 |
| Statewide enforcement authority | 0.98 | 0.91 – 1.06 | 0.97 | 0.89 – 1.06 | 1.03 | 0.92 – 1.16 |
| Free distribution restrictions | 1.03 | 0.96 – 1.11 | 1.10 | 0.997 – 1.21 | 1.05 | 0.94 – 1.17 |
| Clerk intervention requirements | 1.00 | 0.91 – 1.10 | 1.02 | 0.85 – 1.22 | 0.94 | 0.75 – 1.19 |
Notes: OR= odds ratio; CI = confidence interval. Bold numbers indicate that 95% confidence intervals exclude 1.0
Because some studies have suggested that underage women may have less trouble purchasing cigarettes than young men (11, 32, 39–42) we also conducted sex-stratified analyses. Among women, both vending machine restrictions and ID requirements exhibited stronger associations than in the full sample. In addition, for the women-only analyses, repackaging restrictions were associated with statistically significant reduction in prevalence of current smoking (OR=0.93, 95% CI: 0.87, 0.99); restrictions on free sample distribution were associated with a significant reduction in ever-smoking prevalence (OR=0.88, 95% CI: 0.77, 0.996), and the presence of a statewide enforcement agency was associated with a reduction in prevalence of current heavy smoking among ever-smokers (OR=0.87, 95% CI: 0.77, 0.98). In contrast, for analyses limited to men, only one policy showed significant association with any outcome: signposting requirements were associated with a reduction in current heavy smoking prevalence among ever-smokers (OR=0.84, 95% CI: 0.72, 0.98)
Multi-Policy Models
Some, but not all of the policies analyzed in Table 2 exhibited significant associations with adult smoking, primarily for women. However, interpretation of those results is limited by two factors. First, the policies are correlated with each other. Second, it is impossible to rule out small effects for policies that did not attain nominal statistical significance. Prompted by these limitations, two sets of analyses were conducted to test aggregate policy associations. In the first set, we used the results from single-policy analyses to select those with the strongest evidence of effectiveness, and then tabulated a count of these policies in place for each state and birth year combination. Policies were selected if they exhibited a negative coefficient of association for each outcome in the full-sample analysis and were significantly associated with any outcome in either the full sample or sex-stratified analyses. This resulted in four policies: vending machine restrictions, identification requirements, repackaging restrictions, and presence of a statewide enforcement agency. The predictor variable was the count of these four policies based on state and birth year. The second approach was to use the count of all nine policies, regardless of the results of the single policy analysis. By expressing these variables as counts, these models assume independent, homogenous contribution of each policy to smoking behavior.
Table 3 summarizes the results of the multiple policy analyses. The top half of the Table lists results for the models using the same set of covariates described before, and the bottom half includes models that adjust for potential policy confounders including state tobacco excise tax, clean indoor air policies, and state funding forspending on tobacco control at time of observation. The four-policy count was associated with significant or near-significant reductions in prevalence of ever-smoking, current smoking, and current heavy smoking among ever-smokers in the full-sample, but stratification by sex indicated that the associations were only significant for women. The nine-policy count exhibited similar results, but associations with current heavy smoking among ever-smokers did not meet the statistical significance threshold. After adjustment for additional policy covariates (bottom half of Table 3), both counts were significantly, or near-significantly associated with reductions in all three outcome prevalences for women, but not men. To test whether policy associations diminish with age, interactions between age and policy were incorporated into each model. In no case was the interaction significant (all interaction p > 0.09; see Supplemental Material online Part I).
Table 3.
Adjusted associations between counts of selected four and all nine youth access policies and smoking outcomes.
| Ever-Smoking (100+ Lifetime Cigarettes N =105,519) | Current Smoking (N=105,519) | Current heavy smoking Among Ever-Smokers (N=35,745) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Model | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Model 11 | ||||||
| Full Sample | ||||||
| Selected four policies | 0.974 | 0.956 – 0.993 | 0.968 | 0.950 – 0.987 | 0.968 | 0.937 – 1.000 |
| All nine policies | 0.990 | 0.979 – 1.002 | 0.987 | 0.975 – 1.000 | 0.984 | 0.964 – 1.005 |
| Women | ||||||
| Selected four policies | 0.964 | 0.942 – 0.986 | 0.959 | 0.937 – 0.981 | 0.935 | 0.894 – 0.978 |
| All nine policies | 0.984 | 0.968 – 0.999 | 0.981 | 0.967 – 0.996 | 0.972 | 0.942 – 1.002 |
| Men | ||||||
| Selected four policies | 0.986 | 0.961 – 1.010 | 0.977 | 0.949 – 1.006 | 1.004 | 0.967 – 1.043 |
| All nine policies | 0.998 | 0.985 – 1.010 | 0.994 | 0.978 – 1.010 | 0.998 | 0.973 – 1.022 |
| Model 22 | ||||||
| Full Sample | ||||||
| Selected four policies | 0.975 | 0.957 – 0.993 | 0.968 | 0.950 – 0.987 | 0.967 | 0.936 0.999 |
| All nine policies | 0.990 | 0.979 – 1.002 | 0.987 | 0.974 – 0.999 | 0.983 | 0.962 – 1.004 |
| Women | ||||||
| Selected four policies | 0.964 | 0.942 – 0.987 | 0.959 | 0.937 – 0.981 | 0.935 | 0.893 0.978 |
| All nine policies | 0.984 | 0.968 – 0.999 | 0.980 | 0.966 – 0.995 | 0.970 | 0.940 – 1.001 |
| Men | ||||||
| Selected four policies | 0.986 | 0.962 – 1.010 | 0.977 | 0.950 – 1.006 | 1.004 | 0.966 – 1.043 |
| All nine policies | 0.997 | 0.985 – 1.010 | 0.993 | 0.977 – 1.010 | 0.997 | 0.973 – 1.021 |
Notes:
Adjusted for demographic variables and survey wave (see Methods).
Further adjusted for state excise tax, clean indoor air policy, and tobacco control funding per capita at time of survey.
OR= odds ratio; CI = confidence interval
Selected four policies = the count of vending machine restrictions, identification requirements, packaging restrictions, and presence of a statewide enforcement agency.
All nine policies = the count of all nine policies.
Bold numbers indicate that 95% confidence intervals exclude 1.0
Finally, to test whether states with high baseline smoking prevalence were more or less likely to adopt restrictive youth access policies, we calculated the correlation coefficient between the prevalence of “current smoking” in 1999 and the policy count variable in 2006. The correlation coefficient was small (−0.02) and non-significant (p=0.87).
Discussion
Our findings suggest that restricted access to tobacco during adolescence is associated with reduced smoking prevalence in adulthood, but the associations are observed only among women. No single policy exhibited large associations, but various policies may have had small, additive effects. Significant associations with prevalence of both ever-smoking and current smoking were observed. Additionally, in analyses limited to lifetime smokers, policies were independently associated with lower prevalence of current heavy smoking.
While individual policy associations were small, the aggregate effect of multiple policies could be substantial. For example, the multi-policy models (Table 3) suggested that each of the four most consistently associated policies could decrease odds for ever smoking by 3.6% for women, or that all four combined could lower odds by nearly 14%. Similarly, the cumulative effect of the four policies would be a 29% reduction in odds for current heavy smoking among ever-smokers. Taken together, these findings offer evidence that youth access policies may promote lower rates of smoking initiation among women, while also possibly leading to lighter smoking and/or quitting among those who initiate.
The four policies that exhibited the strongest results when analyzed singularly were vending machine restrictions, identification requirements, repackaging restrictions, and restrictions on free sample distribution. A mandated statewide enforcement agency was associated with reduced current heavy smoking among ever-smokers. Because individual associations were small, we cannot rule out small effects for other policies that were not detected due to power limitations. Accordingly, we predicted smoking from the count of all nine policies. These results were also consistent with the interpretation that youth access policies exhibit small, additive effects on smoking prevalences, but only for women. While we cannot rule out the possibility of small effects for men, the differences in effect sizes between women and men were striking.
Any interpretation of the sex differences in the policy associations is necessarily speculative given our current knowledge. However, given that the Synar policies were intended to intensify the enforcement of nominal purchase ages, a plausible interpretation is that, absent uniform enforcement protocols, girls may have an easier time obtaining age-restricted goods than boys. For example, in a South Australian study, girls under 16 had more success than boys when attempting to illicitly purchase cigarettes (43). In the US, at least five studies—largely conducted prior to the full implementation of Synar amendment policies—exhibited similar findings (11, 39–42). Parallel sex-differences have been reported for field-studies of underage alcohol purchase (44–46). We found no field studies of underage alcohol or tobacco purchase that reported higher success rates for boys. Hence, policies which promote more uniform enforcement of nominal restrictions, such as the Synar policies, may have larger effects on girls’ access to tobacco than on boys’ access.
Interpretation of our results should be tempered by several limitations. Despite using an analytical design that controls for many potential unobserved confounders, alternative explanations for reductions in smoking prevalence among those exposed to more restrictive policies cannot be exhaustively ruled out; potential unmeasured confounders include any factors that changed in the same states and at the same times as state youth access policies. On the other hand, we found no evidence for reverse causation; i.e., there was no correlation between baseline prevalence of smoking at the state level and the number of youth access policies subsequently adopted. Because we examined policy exposure at age 17, and some subjects would have reached smoking milestones prior to this age, the protective effects of policy with ever-smoking prevalence may be underestimated. Nonetheless, the choice of age 17 is appropriate because most young people do not begin smoking regularly prior to 17 (47). Also, because the CPS-TUS provides year, but not exact date of birth, there is some random error introduced into the policy exposure estimation, in addition to that caused by the proxy use of current state of residence for state of residence during adolescence (see Methods and Supplemental Material). Random error would bias our findings toward underestimating the effects of policy exposure. Finally, voluntary retailer practices or local ordinances may place restrictions on youth access to tobacco beyond state policy; these effects would not be detected by our analyses. Limitations notwithstanding, the finding that youth access laws may result in substantial, long-term reductions in smoking prevalence, even if reductions are limited to women, is novel and significant. In addition to replication in other samples, future research on potential meditating mechanisms for youth access policies is warranted. For example, youth access policies may influence social norms and other factors more proximal to youth smoking.
Analyses of long-term effects associated with major policy such as the Synar Amendment help inform evidence-based policy evaluation (48). While a number of studies have described the short-term influence of youth access measures on adolescents (6, 12, 13, 15) the results of this study address an area of unmet need by describing their long-term association with behaviors later in life and providing vital information for evaluating long-term benefits against costs. Policies aimed at affecting the health of adolescents and young adults may have effects that persist into older adulthood (20–22). Our analyses of the long-term outcomes associated with Synar Amendment policies provide evidence that maintaining or even strengthening youth access measures may be a worthwhile endeavor.
Supplementary Material
Footnotes
By 2003 all states had purchase ages of 18 or higher, but a few states did not adopt this criterion until the early 1990s.
Contributors: R.A. Grucza designed and partially conducted the analysis, obtained the funding, completed the statistical analysis, and authored the article. A.D. Plunk conducted supporting analyses and contributed to writing of the article. P.R.. Hipp and M.J. Krauss conducted analyses and contributed to writing of the article. P. Cavazos-Rehg, R.C. Brownson and L.J. Bierut contributed to interpretation of results and writing of the article.
Contributor Information
Richard A. Grucza, Department of Psychiatry, Washington University School of Medicine.
Andrew D Plunk, Department of Psychiatry, Washington University School of Medicine.
Pamela R. Hipp, Department of Psychiatry, Washington University School of Medicine at the time of the study.
Patricia Cavazos-Rehg, Department of Psychiatry, Washington University School of Medicine.
Melissa J. Krauss, Department of Psychiatry, Washington University School of Medicine.
Ross C. Brownson, Prevention Research Center, the Brown School, the Division of Public Health Sciences and the Alvin J. Siteman Cancer Center; Washington University School of Medicine, St. Louis, MO, USA.
Laura J. Bierut, Department of Psychiatry, Washington University School of Medicine.
References
- 1.Kessler DA, Natanblut SL, Wilkenfeld JP, Lorraine CC, Mayl SL, Bernstein IBG, et al. Nicotine addiction: A pediatric disease. The Journal of Pediatrics. 1997;130(4):518–524. doi: 10.1016/s0022-3476(97)70232-4. [DOI] [PubMed] [Google Scholar]
- 2.Brandt AM. The Cigarette Century. New York, NY: Basic Books; 2007. pp. 385–393. [Google Scholar]
- 3.Forster JL, Widome R, Bernat DH. Policy interventions and surveillance as strategies to prevent tobacco use in adolescents and young adults. Am J Prev Med. 2007;33(6 Suppl):S335–9. doi: 10.1016/j.amepre.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 4.DiFranza JR, Dussault GF. The federal initiative to halt the sale of tobacco to children--the Synar Amendment, 1992–2000: lessons learned. Tob Control. 2005;14(2):93–8. doi: 10.1136/tc.2004.009373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alciati MH, Frosh M, Green SB, Brownson RC, Fisher PH, Hobart R, et al. State laws on youth access to tobacco in the United States: measuring their extensiveness with a new rating system. Tob Control. 1998;7(4):345–52. doi: 10.1136/tc.7.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaloupka FJ. Tobacco Control Lessons Learned: The Impact of State and Local Policies. Vol. 2010. Chicago, IL: Robert Wood Johnson Foundation and University of Illinois Chicago; Jan, 2010. Report No.: No. 38. [Google Scholar]
- 7.Rigotti NA, DiFranza JR, Chang Y, Tisdale T, Kemp B, Singer DE. The effect of enforcing tobacco-sales laws on adolescents’ access to tobacco and smoking behavior. N Engl J Med. 1997;337(15):1044–51. doi: 10.1056/NEJM199710093371505. [DOI] [PubMed] [Google Scholar]
- 8.Difranza JR, Carlson RR, Caisse RE. Reducing youth access to tobacco. Tobacco Control. 1992;1(1):58. [Google Scholar]
- 9.Jason LA, Ji PY, Anes MD, Birkhead SH. Active enforcement of cigarette control laws in the prevention of cigarette sales to minors. JAMA. 1991;266(22):3159–61. [PubMed] [Google Scholar]
- 10.Stead LF, Lancaster T. A systematic review of interventions for preventing tobacco sales to minors. Tob Control. 2000;9(2):169–76. doi: 10.1136/tc.9.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forster JL, Murray DM, Wolfson M, Blaine TM, Wagenaar AC, Hennrikus DJ. The effects of community policies to reduce youth access to tobacco. Am J Public Health. 1998;88(8):1193–8. doi: 10.2105/ajph.88.8.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DiFranza JR, Savageau JA, Fletcher KE. Enforcement of underage sales laws as a predictor of daily smoking among adolescents: a national study. BMC Public Health. 2009;9:107. doi: 10.1186/1471-2458-9-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luke DA, Stamatakis KA, Brownson RC. State youth-access tobacco control policies and youth smoking behavior in the United States. Am J Prev Med. 2000;19(3):180–7. doi: 10.1016/s0749-3797(00)00196-3. [DOI] [PubMed] [Google Scholar]
- 14.Lewit EM, Hyland A, Kerrebrock N, Cummings KM. Price, public policy, and smoking in young people. Tob Control. 1997;6 (Suppl 2):S17–24. doi: 10.1136/tc.6.suppl_2.s17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Botello-Harbaum MT, Haynie DL, Iannotti RJ, Wang J, Gase L, Simons-Morton B. Tobacco control policy and adolescent cigarette smoking status in the United States. Nicotine Tob Res. 2009;11(7):875–85. doi: 10.1093/ntr/ntp081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fichtenberg CM, Glantz SA. Youth access interventions do not affect youth smoking. Pediatrics. 2002;109(6):1088–92. doi: 10.1542/peds.109.6.1088. [DOI] [PubMed] [Google Scholar]
- 17.Chaloupka FJ, Wechsler H. Price, tobacco control policies and smoking among young adults. J Health Econ. 1997;16(3):359–73. doi: 10.1016/s0167-6296(96)00530-9. [DOI] [PubMed] [Google Scholar]
- 18.Glantz SA. Preventing tobacco use--the youth access trap. Am J Public Health. 1996;86(2):156–8. doi: 10.2105/ajph.86.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Craig MJ, Boris NW. Youth tobacco access restrictions: Time to shift resources to other interventions? Health Promot Pract. 2007;8(1):22–7. doi: 10.1177/1524839905279882. [DOI] [PubMed] [Google Scholar]
- 20.Norberg KE, Bierut LJ, Grucza RA. Long-Term Effects of Minimum Drinking Age Laws on Past-Year Alcohol and Drug Use Disorders. Alcohol Clin Exp Res. 2009;33(12):2180–2190. doi: 10.1111/j.1530-0277.2009.01056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grucza RA, Hipp PR, Norberg KE, Rundell L, Evanoff A, Cavazos-Rehg P, et al. The legacy of minimum legal drinking age law changes: long-term effects on suicide and homicide deaths among women. Alcohol Clin Exp Res. 2012;36(2):377–84. doi: 10.1111/j.1530-0277.2011.01608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaestner R, Yarnoff B. NBER Working Paper No 15439. Cambridge, MA: National Bureau of Economic Research; 2009. Long term effects of minimum legal drinking age laws on adult alcohol use and driving fatalities. [Google Scholar]
- 23.Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. Am J Psychiatry. 2003;160(6):1041–52. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86(2):189–99. doi: 10.1016/j.pbb.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Slotkin TA. Nicotine and the adolescent brain: insights from an animal model. Neurotoxicol Teratol. 2002;24(3):369–84. doi: 10.1016/s0892-0362(02)00199-x. [DOI] [PubMed] [Google Scholar]
- 26.US Department of Commerce, Census Bureau. National Cancer Institute and Centers for Disease Control and Prevention Co-sponsored Tobacco Use Supplement to the Current Population Survey (1999, 2001–02, 2003, 2006–07) 2008 http://www.census.gov/apsd/techdoc/cps/cps-main.html.
- 27.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–9. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 28.ImpacTeen Project. Tobacco Control Policy and Prevalence Data: 1991–2008 Codebook and Definitions. 2009 http://www.impacteen.org/tobaccodata.htm.
- 29.Ashenfelter O, Card D. Using the Longitudinal Structure of Earnings to Estimate the Effect of Training Programs. The Review of Economics and Statistics. 1985;67(4):648–660. [Google Scholar]
- 30.Snow J. On the Mode of Communication of Cholera. London: Churchill; 1855. [Google Scholar]
- 31.Angrist J, Pischke J-S. Mostly Harmless Econometrics: An Empiricist’s Companion. Princeton University Press; 2008. [Google Scholar]
- 32.Orzechowski W, Walker RC. The Tax Burden on Tobacco: Historical Compilation. Arlington, VA: 2008. [Google Scholar]
- 33.Chriqui JF, Frosh M, Brownson RC, Shelton DM, Sciandra RC, Hobart R, et al. Application of a rating system to state clean indoor air laws (USA) Tob Control. 2002;11(1):26–34. doi: 10.1136/tc.11.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liang KY, Zeger SL. Longitudinal data analysis using generliazed linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 35.Arellano M. Computing Robust Standard Errors for Within-groups Estimators. OxfordBull Econ Statist. 1987;49(4):431–434. [Google Scholar]
- 36.Cochran WG. Sampling Techniques. New York: John Wiley and Sons; 1977. [Google Scholar]
- 37.West BT. Supporting Material for “Applied Survey Data Analysis”. Boca Raton, FL: Chapman Hall / CRC Press; 2010. Accounting for Multi-stage Sample Designs in Complex Sample Variance Estimation (Working Paper) [Google Scholar]
- 38.Groves RM. Survey Errors and Survey Costs. New York: Wiley; 1989. [Google Scholar]
- 39.DiFranza JR, Savageau JA, Aisquith BF. Youth access to tobacco: the effects of age, gender, vending machine locks, and “it’s the law” programs. Am J Public Health. 1996;86(2):221–4. doi: 10.2105/ajph.86.2.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Altman DG, Foster V, Rasenick-Douss L, Tye JB. Reducing the illegal sale of cigarettes to minors. JAMA. 1989;261(1):80–3. [PubMed] [Google Scholar]
- 41.Cismoski J, Sheridan M. Availability of cigarettes to under-age youth in Fond du Lac, Wisconsin. Wis Med J. 1993;92(11):626–30. [PubMed] [Google Scholar]
- 42.Erickson AD, Woodruff SI, Wildey MB, Kenney E. A baseline assessment of cigarette sales to minors in San Diego, California. J Community Health. 1993;18(4):213–24. doi: 10.1007/BF01324432. [DOI] [PubMed] [Google Scholar]
- 43.Wakefield M, Carrangis J, Wilson D, Reynolds C. Illegal cigarette sales to children in South Australia. Tobacco control. 1992;1(2):114–117. [Google Scholar]
- 44.Willner P, Hart K, Binmore J, Cavendish M, Dunphy E. Alcohol sales to underage adolescents: an unobtrusive observational field study and evaluation of a police intervention. Addiction. 2000;95(9):1373–88. doi: 10.1046/j.1360-0443.2000.95913738.x. [DOI] [PubMed] [Google Scholar]
- 45.Gosselt JF, van Hoof JJ, de Jong MD, Prinsen S. Mystery shopping and alcohol sales: Do supermarkets and liquor stores sell alcohol to underage customers? J Adolesc Health. 2007;41(3):302–8. doi: 10.1016/j.jadohealth.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 46.Rossow I, Karlsson T, Raitasalo K. Old enough for a beer? Compliance with minimum legal age for alcohol purchases in monopoly and other off-premise outlets in Finland and Norway. Addiction. 2008;103(9):1468–73. doi: 10.1111/j.1360-0443.2008.02302.x. [DOI] [PubMed] [Google Scholar]
- 47.Dierker L, He J, Kalaydjian A, Swendsen J, Degenhardt L, Glantz M, et al. The Importance of Timing of Transitions for Risk of Regular Smoking and Nicotine Dependence. Annals of Behavioral Medicine. 2008;36(1):87–92. doi: 10.1007/s12160-008-9051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brownson RC, Chriqui JF, Stamatakis KA. Understanding evidence-based public health policy. Am J Public Health. 2009;99(9):1576–83. doi: 10.2105/AJPH.2008.156224. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.