Abstract
Background
Muscle weakness in old age is associated with physical function decline. Progressive resistance strength training (PRT) exercises are designed to increase strength.
Objectives
To assess the effects of PRT on older people and identify adverse events.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialized Register (to March 2007), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2007, Issue 2), MEDLINE (1966 to May 01, 2008), EMBASE (1980 to February 06 2007), CINAHL (1982 to July 01 2007) and two other electronic databases. We also searched reference lists of articles, reviewed conference abstracts and contacted authors.
Selection criteria
Randomised controlled trials reporting physical outcomes of PRT for older people were included.
Data collection and analysis
Two review authors independently selected trials, assessed trial quality and extracted data. Data were pooled where appropriate.
Main results
One hundred and twenty one trials with 6700 participants were included. In most trials, PRT was performed two to three times per week and at a high intensity. PRT resulted in a small but significant improvement in physical ability (33 trials, 2172 participants; SMD 0.14, 95% CI 0.05 to 0.22). Functional limitation measures also showed improvements: e.g. there was a modest improvement in gait speed (24 trials, 1179 participants, MD 0.08 m/s, 95% CI 0.04 to 0.12); and a moderate to large effect for getting out of a chair (11 trials, 384 participants, SMD -0.94, 95% CI -1.49 to -0.38). PRT had a large positive effect on muscle strength (73 trials, 3059 participants, SMD 0.84, 95% CI 0.67 to 1.00). Participants with osteoarthritis reported a reduction in pain following PRT (6 trials, 503 participants, SMD -0.30, 95% CI -0.48 to -0.13). There was no evidence from 10 other trials (587 participants) that PRT had an effect on bodily pain. Adverse events were poorly recorded but adverse events related to musculoskeletal complaints, such as joint pain and muscle soreness, were reported in many of the studies that prospectively defined and monitored these events. Serious adverse events were rare, and no serious events were reported to be directly related to the exercise programme.
Authors' conclusions
This review provides evidence that PRT is an effective intervention for improving physical functioning in older people, including improving strength and the performance of some simple and complex activities. However, some caution is needed with transferring these exercises for use with clinical populations because adverse events are not adequately reported.
Medical Subject Headings (MeSH): Activities of Daily Living, Muscle Weakness [*rehabilitation], Randomized Controlled Trials as Topic, Recovery of Function [physiology], Resistance Training [adverse effects, *methods]
MeSH check words: Aged, Humans
Background
Description of the condition
Muscle strength is the amount of force produced by a muscle. The loss of muscle strength in old age is a prevalent condition. Muscle strength declines with age such that, on average, the strength of people in their 80s is about 40% less than that of people in their 20s (Doherty 1993). Muscle weakness, particularly of the lower limbs, is associated with reduced walking speed (Buchner 1996), increased risk of disability (Guralnik 1995) and falls in older people (Tinetti 1986).
Description of the intervention
Progressive resistance training (PRT) is often used to increase muscle strength. During the exercise, participants exercise their muscles against some type of resistance that is progressively increased as strength improves. Common equipment used for PRT includes exercise machines, free weights, and elastic bands.
How the intervention might work
Contrary to long held beliefs, the muscles of older people (i.e. people aged 60 years and older) continue to be adaptable, even into the extremes of old age (Frontera 1988). Trials have revealed that older people can experience large improvements in their muscle strength, particularly if their muscles are significantly overloaded during training (Brown 1990; Charette 1991; Fiatarone 1994).
Why it is important to do this review
Despite evidence of benefit from PRT in terms of improving muscle strength, there is still uncertainty about how these effects translate into changes in substantive outcomes such a reduction in physical disability (Chandler 1998). Most studies have been under-powered to determine the effects of PRT on these outcomes or have included PRT as part of a complex intervention. In addition, there is uncertainty about the effects of PRT when more pragmatic, home or hospital-based programmes are used, and the safety and effectiveness of this intervention in older adults who have health problems and/or functional limitations. Finally, there is uncertainty about the relative benefits of PRT compared with other exercise programmes, or the effectiveness of varying doses of PRT (i.e. programmes of varying intensity and duration). This update of our review (Latham 2003a) has continued to assess and summarise the evidence for PRT.
Objectives
To determine the effects of progressive resistance strength training (PRT) on physical function in older adults through comparing PRT with no exercise, or another type of care or exercise (e.g. aerobic training). Comparisons of different types (e.g. intensities, frequencies, or speed) of PRT were included also. We considered these effects primarily in terms of measures of physical (dis)ability and adverse effects, and secondary measures of functional impairment (muscle strength & aerobic capacity) and limitation (e.g. gait speed).
Methods
Criteria for considering studies for this review
Types of studies
Any randomised clinical trials meeting the specifications below were included. All non-randomised controlled trials (e.g. controlled before and after studies) were excluded. Also excluded were trials for which details were provided that indicated these used quasi-randomised methods, such as allocation based on date of birth.
Types of participants
Older people, resident in institutions or at home in the community. Trials were included if the mean age of participants was 60 or over, but excluded if participants aged less than 50 were enrolled. The participants could include frail or disabled older people, people with identified diseases or health problems, or fit and healthy people.
Types of interventions
Any trial that had one group of participants who received PRT as a primary intervention was considered for inclusion. PRT was defined as a strength training programme in which the participants exercised their muscles against an external force that was set at specific intensity for each participant, and this resistance was adjusted throughout the training programme. The type of resistance used included elastic bands or tubing (i.e. therabands), cuff weights, free weights, isokinetic machines or other weight machines. This type of training could take place in individual or group exercise programmes, and in a home-based or gymnasium/clinic setting. Studies that utilised only isometric exercises were excluded. Studies that included balance, aerobic or other training as part of the exercise intervention (and not simply part of the warm-up or cool-down) were also excluded.
We found the following comparisons between groups in the trials:
PRT versus no exercise (greatest difference between groups was expected)
Different types of PRT: high intensity versus low intensity, high frequency versus low frequency, or higher speed (power training) versus regular speed (greatest effect expected in the higher intensity groups). Power training refers to the type of PRT that emphasizes speed.
PRT versus regular care (including regular therapy or exercise)
PRT versus another type of exercise (smaller difference between groups expected)
Types of outcome measures
Primary outcomes
This review assessed physical function in older adults at the level of impairment, functional limitation and disability. The primary outcome of this review was physical disability. This was assessed as a continuous variable. The outcomes were categorized based on the Nagi model of health states (Nagi 1991). In this model, disability is considered to be a limitation in performance of socially defined roles and tasks that can relate to self-care, work, family etc. In this review, the primary assessment of physical disability included the evaluation of self-reported measures of activities of daily living (ADL, i.e. the Barthel Index) and the physical domains of health-related quality of life (HRQOL, i.e. the physical function domain of the SF-36). Data from these measures were pooled for the main analysis of physical disability. However, because these two types of measures (ADL and physical domains of HRQOL) evaluate different health concepts, they were also evaluated in separate analyses. The Nagi model also includes firstly, the domain of ‘functional limitations’ which are limitations in performance at the level of the whole person and includes activities such as walking, climbing or reaching, and secondly, ‘impairments’ that are defined as anatomical or physiological abnormalities.
Since the protocol of this review was written, the International Classification of Functioning, Disability and Handicap (ICF) has been released (WHO 2001). Under this system, disability is an umbrella term for impairments, activity limitations and participation restrictions. Using the ICF, the outcome measures evaluated in this review fall under the domains of impairments, limitations in simple activities (similar to ‘functional limitations’ in Nagi's system) and limitations in complex activities (similar to some aspects of disability in Nagi's model).
Secondary outcomes
Measures of impairment (outcome comparisons 2 and 3)
The following secondary outcomes were assessed as continuous variables:
muscle strength (e.g. 1 repetition maximum test, isokinetic and isometric dynamometry)
aerobic capacity (e.g. 6 minute walk test, VO2 max: maximal oxygen uptake during exercise)
Measures of functional limitation (simple physical activities)
The following secondary outcomes were assessed as continuous variables:
balance (e.g. Berg Balance Scale, Functional Reach Test)
gait speed, timed walk
timed ‘up-and-go’ test
chair rise (sit to stand)
stair climbing (added in 2008)
The balance outcome is also reviewed in a separate Cochrane review (Howe 2007).
Other outcomes
The dichotomous secondary outcomes assessed were adverse events, admission to hospital and death. The effect of PRT on falls was also evaluated, although these outcomes are considered in a separate Cochrane review (Gillespie 2003). Pain and vitality measures were evaluated as continuous outcomes, and were used to provide additional information about the potential adverse effects or benefits of PRT.
Outcomes removed after the protocol
In the original protocol for this review, measures of fear of falling and participation in social activities were also included as outcomes. However, when the size and complexity of this review became apparent, the authors decided to limit this review to assessments of physical disability as this was the prespecified primary aim of the review. Therefore, these outcomes are not included in the current review. In addition, the protocol also stated that assessments of disability using the Barthel Index and Functional Independence Measure (FIM) would be dichotomised. However as no trials included the FIM as an outcome and only three trials used the Barthel Index, the decision was made to report these data as continuous outcomes only.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (March 2007), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2002, Issue 2; February 2007), MEDLINE (1966 to May 01, 2008), EMBASE (1980 t February 06, 2007), CINAHL (1982 to July 01, 2007), SPORTDiscus (1948 to February 07, 2007), PEDro - The Physiotherapy Evidence Database (accessed February 07, 2007) and Digital Dissertations (accessed February 01, 2007). No language restrictions were applied.
In MEDLINE (OVID Web) the subject specific search strategy was combined with the first two phases of the Cochrane optimal search strategy (Higgins 2006). This search strategy, along with those for EMBASE (OVID Web), The Cochrane Library (Wiley InterScience), CINAHL (OVID Web), SPORTDiscus (OVID Web) and PEDro, can be found in Appendix 1.
Searching other resources
We contacted authors and searched reference lists of identified studies, and reviews (Anonymous 2001; Buchner 1993; Chandler 1996; Fiatarone 1993; Keysor 2001; King 1998; King 2001; Mazzeo 1998; Singh 2002).
We also handsearched the following conference proceedings:
16th International Association of Gerontology World Congress; 1997; Adelaide (Australia).
17th International Association of Gerontology World Congress; 2001; Vancouver (Canada).
Proceedings of the 13th World Congress of Physical Therapy; 1995; Washington (DC).
Proceedings of the 14th World Congress of Physical Therapy; 1999; Japan.
New Zealand Association of Gerontology Conferences -1996 Dunedin, 1999 Wellington and 2002 Auckland (New Zealand).
The 60th annual scientific meeting of the Gerontological Society of America; 2007, San Francisco, CA.
The American Congress of Rehabilitation Medicine -American Society of Neurorehabilitation Joint Conference; 2006, Boston, MA.
Data collection and analysis
Selection of studies
For this update (Issue 3, 2009), one author (CJL) conducted the searches. Both listed authors (CJL, NL) reviewed the titles, descriptors or abstracts identified from all literature searches to identify potentially relevant trials for full review. A copy of the full text of all trials that appeared to be potentially suitable for the review was obtained. Both authors independently used previously defined inclusion criteria to select the trials. In all cases, the reviewers reached a consensus when they initially disagreed about the inclusion of a trial. Before this update, the same method of identifying and assessing studies was used, although other members of the previous review team assisted (Latham 2003a).
Data extraction and management
Two authors independently extracted the data and recorded information on a standardised paper form. They considered all primary and secondary outcomes. If the data were not reported in a form that enabled quantitative pooling, the authors were contacted for additional information. If the authors could not be contacted or if the information was no longer available, the trial was not included in the pooling for that specific outcome.
Assessment of risk of bias in included studies
The methodological quality of each trial was independently assessed by two authors (NL, CS in the first review; CJL, NL in the update) using a scoring system that was based on the Cochrane Bone, Joint and Muscle Trauma Group's former evaluation tool. The review authors were blinded to the trial authors' institution, journal that the trial was published in and the results of the trial. A third review author (CA) was consulted in the first review if a consensus about the trial quality could not be reached. No third review author was involved in the review update. The criteria for assessing internal and external validity can be found in Table 1.
Assessment of heterogeneity
The chi2 test was used to assess heterogeneity. In future updates, we will also assess heterogeneity by visual inspection of the forest plots and consideration of the I2 statistic.
Data synthesis
Where it was thought appropriate, the results from the studies were combined. Data synthesis was carried out using MetaView in Review Manager version 5.0. For continuous outcomes, mean differences (MD) and 95% confidence intervals (CI) were calculated when similar measurement units were used. To pool outcomes using different units, standardised units (i.e. standardised mean differences, SMD) were created as appropriate. We calculated risk ratios and 95% CI for dichotomous outcomes, where possible. If minimal statistical heterogeneity (P < 0.1) existed, fixed-effect meta-analysis was performed.
For trials that compared two or more different dosages of PRT versus a control group, data from the higher or highest intensity group were used in the analyses of PRT versus control.
Subgroup analysis and investigation of heterogeneity
If substantial statistical heterogeneity existed, the review authors looked for possible explanations. Specifically, we considered differences in age and baseline disability of the study participants, the methodological quality of the trials and the intensity and duration of the interventions. If the statistical heterogeneity could be explained, we considered the possibility of presenting the results as subgroup analyses. If the statistical heterogeneity could not be explained, we considered not combining the studies at all, using a random-effects model with cautious interpretation or using both fixed-effect and random-effects models to assist in explaining the uncertainty around an analysis with heterogeneous studies.
Sensitivity analysis
Sensitivity analyses were conducted to assess the effect of differences in methodological quality. These included allocation concealment, blinding of outcome assessors, statements of intention-to-treat analysis and use of attention control.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
Please see the ‘Characteristics of included studies’.
One hundred and twenty-one trials with 6700 participants at entry were included in this review. Four studies were published only as abstracts and/or theses (Collier 1997; Fiatarone 1997; Moreland 2001; Newnham 1995).
Included studies
There was variation across the trials in the characteristics of the participants, the design of the PRT programmes, the interventions provided for the comparison group and the outcomes assessed. More detailed information is provided in the ‘Characteristics of included studies’; however, a brief summary is provided here.
Language
All reviewed trials were published in English.
Location
Sixty-eight trials were conducted in the USA, 13 in Canada, 9 in Australia or New Zealand, and 31 in various European countries.
Study size
Most of these studies were small, with less than 40 participants in total, but 14 studies had 100 or more participants in total in a PRT group and a control group (Buchner 1997; Chandler 1998; Chin A Paw 2006; de Vos 2005; Ettinger 1997; Jette 1996; Jette 1999; Judge 1994; Latham 2003; Maurer 1999; McCartney 1995; Mikesky 2006; Moreland 2001; Segal 2003).
Participants
Health status
The participants in 59 trials were healthy older adults. In the remaining 62 trials, the participants had a health problem, functional limitation and/or were residing in a hospital or residential care. Thirty-two trials included older people with a specific medical condition, including diabetes (Brandon 2003), prostate cancer (Segal 2003), osteoarthritis (Baker 2001; Ettinger 1997; Foley 2003; Maurer 1999; Mikesky 2006; Schilke 1996; Topp 2002), osteoporosis/osteopenia (Liu-Ambrose 2005), peripheral arterial disease (Hiatt 1994; McGuigan 2001), recent stroke (Moreland 2001; Ouellette 2004), congestive heart failure (Brochu 2002; Pu 2001; Selig 2004; Tyni-Lenne 2001), chronic airflow limitation (Casaburi 2004; Kongsgaard 2004; Simpson 1992), clinical depression (Sims 2006; Singh 1997; Singh 2005), low bonemineral density (Parkhouse 2000), hip replacement due to osteoarthritis (Suetta 2004), hip/lower limb fracture (Mangione 2005; Miller 2006), obesity (Ballor 1996), chronic renal insufficiency (Castaneda 2001; Castaneda 2004) and coronary artery bypass graft surgery three or more months before exercise training (Maiorana 1997). Nineteen other trials recruited participants who did not have a specific health problem, but were considered frail and/or to have a functional limitation (Bean 2004; Boshuizen 2005; Chandler 1998; Fiatarone 1994; Fiatarone 1997; Fielding 2002; Hennessey 2001; Jette 1999; Krebs 2007; Latham 2003; Manini 2005; McMurdo 1995; Mihalko 1996; Miszko 2003; Newnham 1995; Skelton 1996; Sullivan 2005; Topp 2005; Westhoff 2000). In nine trials, the participants resided in a resthome or nursing home (Baum 2003; Bruunsgaard 2004; Chin A Paw 2006; Fiatarone 1994; Hruda 2003; McMurdo 1995; Mihalko 1996; Newnham 1995; Seynnes 2004). In addition, two trials included participants who were in hospital at the time the exercise programme was carried out (Donald 2000; Latham 2001). In the other trials, most or all of the participants lived in the community.
Gender
Most studies included both men and women, although 10 trials included men only (Fatouros 2002; Hagerman 2000; Haykowsky 2000; Hepple 1997; Izquierdo 2004; Katznelson 2006; Kongsgaard 2004; Maiorana 1997; Segal 2003; Sousa 2005) and 22 trials included women only (Bean 2004; Brochu 2002; Charette 1991; Damush 1999; Fahlman 2002; Flynn 1999; Frontera 2003; Haykowsky 2005; Jones 1994; Kallinen 2002; Liu-Ambrose 2005; Macaluso 2003; Madden 2006; Nelson 1994; Nichols 1993; Parkhouse 2000; Pu 2001; Rhodes 2000; Sipila 1996; Skelton 1995; Skelton 1996; Taaffe 1996).
Age
In 49 studies the mean or median age of the participants was between 60 and 69 years old; in 57 studies, the mean/median age was between 70 and 79 years old; and in 20 studies, it was 80 years old or over.
Lifestyle
Fifteen studies specifically recruited participants with a sedentary lifestyle (Ades 1996; Beneka 2005; Charette 1991; Fatouros 2002; Fatouros 2005; Frontera 2003; Kalapotharakos 2005; Katznelson 2006; Malliou 2003; Mihalko 1996; Parkhouse 2000; Pollock 1991; Rhodes 2000; Topp 1996; Tsutsumi 1997).
PRT Programmes
Settings
Most training programmes took place in gym or clinic settings with all sessions fully supervised. Ten studies were entirely home-based (Baker 2001; Chandler 1998; Fiatarone 1997; Jette 1996; Jette 1999; Katznelson 2006; Krebs 2007; Latham 2003; Mangione 2005; McMurdo 1995), while 12 additional studies carried out some of the training at home and some in gym/clinic settings (Boshuizen 2005; Ettinger 1997; Jones 1994; Mikesky 2006; Simoneau 2006; Skelton 1995; Skelton 1996; Topp 1993; Topp 1996; Topp 2002; Topp 2005; Westhoff 2000).
Intensity
The resistance training programmes in most trials (i.e. 83 trials) involved high intensity training. Most of these trials used specialized exercise machines for training. Thirty-six trials used low-intensity to moderate-intensity training, with most using elastic tubing or bands. All of the high-intensity training was carried out at least in part in gym or clinic based settings, with the exception of two published trials (Baker 2001; Latham 2003) and a trial published as an abstract (Fiatarone 1997).
Frequency and duration
The frequency of training was consistent across studies, with the exercise programme carried out two to three times a week in almost all trials. Two exceptions to this were the two trials conducted in hospital which carried out the exercises on a daily basis (Donald 2000; Latham 2001). In contrast, there was large variation in the duration of the exercise programmes and the number of exercises performed in each programme. Although most of the programmes (i.e. 71 trials) were eight to 12 weeks long, the duration ranged from two to 104 weeks. In 54 trials the exercise programme was longer than 12 weeks. The number of exercises performed also varied, from one to more than 14.
Adherence
Data about adherence to the PRT programme are reported in the ‘Characteristics of included studies’. These data are difficult to interpret because different definitions for adherence or compliance were used across the trials. In most trials, adherence referred to the percentage of exercise sessions attended compared with the total number of prescribed sessions and in this case the reported adherence rate is high (i.e. greater than 75%). Many trials only included participants that completed the entire trial (i.e. excluded drop-outs), while some trials reported these data with drop-outs included.
Comparison interventions
Comparisons were conducted between a PRT group and a control group and between a PRT group and a group that received other type of intervention. In addition, comparisons between high intensity or frequency and low intensity or frequency, different sets, and different types of contraction training were also conducted. Multiple comparisons within a trial were possible when the trial included more than two groups that were relevant to the review. Twenty-eight trials had three groups. Among these trials, 14 included an aerobic training group in addition to a PRT group and a control group (Ettinger 1997; Fahlman 2002; Fatouros 2002; Haykowsky 2005; Hiatt 1994; Jubrias 2001; Kallinen 2002; Madden 2006; Malliou 2003; Mangione 2005; Pollock 1991; Sipila 1996; Topp 2005; Wood 2001), and seven included two PRT groups that exercised at different intensities in addition to a control group (de Vos 2005; Fatouros 2005; Hortobagyi 2001; Hunter 2001; Kalapotharakos 2005; Seynnes 2004; Singh 2005). One trial had a PRT group, a functional training group, and a PRT with functional training group (Manini 2005). The other six trials either had a balance training group (Judge 1994), functional training group (Chin A Paw 2006; de Vreede 2007), an endurance training group (Sipila 1996), a mobility training group (McMurdo 1995), or a power training group (Miszko 2003) in addition to a PRT group and a control group. One trial had three groups that exercised at three different frequencies in addition to a control group (Taaffe 1999).
PRT versus controls
One hundred and four trials compared PRT with a control group. The control group might receive no exercise, regular care, or attention control (i.e. the control group receives matching attention as the intervention group).
Comparisons of PRT dosage
High intensity versus low intensity
Ten studies compared PRT programmes at high intensity versus low intensity (Beneka 2005; Fatouros 2005; Harris 2004; Hortobagyi 2001; Seynnes 2004; Singh 2005; Sullivan 2005; Taaffe 1996; Tsutsumi 1997; Vincent 2002).
Different frequencies of PRT
Two trials (DiFrancisco 2007; Taaffe 1999) compared PRT performed at different frequencies (i.e. once, twice, or three times per week).
Different sets
One study compared PRT at different sets, i.e. 3-sets versus 1-set (Galvao 2005). One set of exercise means several continuous repeated movements.
Concentric versus eccentric training
One study (Symons 2005) compared PRT at two types of contraction training: concentric versus eccentric training. During concentric training, speed was added at concentric contraction phase and vise versa for eccentric training.
PRT versus aerobic training
PRT was compared with aerobic (endurance) training in 17 trials (Ballor 1996; Buchner 1997; Earles 2001; Ettinger 1997; Fatouros 2002; Hepple 1997; Hiatt 1994; Izquierdo 2004; Jubrias 2001; Kallinen 2002; Madden 2006; Malliou 2003; Mangione 2005; Pollock 1991; Sipila 1996; Topp 2005; Wood 2001).
PRT versus balance training
One study compared PRT with balance training (Judge 1994). Balance training included training on a computerized balance platform and non-platform training (i.e. balancing on different surfaces, with varying bases of support, with different perturbations). Both exercise programmes were performed in a research center three times per week for three months.
PRT versus functional training
Three studies compared PRT to functional training (Chin A Paw 2006; de Vreede 2007; Manini 2005). Functional training involves game-like activities or exercise movements in various directions. In Chin A Paw 2006, functional training involved game-like or cooperative activities; and in de Vreede 2007, functional training involved moving with a vertical or horizontal component, carrying an object, and changing position between lying, sitting, and standing.
PRT versus flexibility training
One study compared PRT with flexibility training (Barrett 2002).
Power training
Power training refers to the type of PRT that emphasizes speed. Three studies applied this type of training (de Vos 2005; Macaluso 2003; Miszko 2003).
Outcomes
A variety of outcomes were assessed in these studies: the primary outcomes of physical function and secondary outcomes of measures of impairment and functional limitation.
Excluded studies
The excluded studies and their reasons for exclusion are listed in the ‘Characteristics of excluded studies’. The main reasons for exclusion were that the study was not a randomised controlled trial or that the study design caused serious threats to its internal validity (57 trials); the studies used a combination of exercise interventions (i.e. not resistance training alone) (51 trials); the strength training programme did not use a progressive resistance approach (32 trials); and some participants were not elderly (i.e. did not have a mean age of at least 60 years and/or included some participants below 50 years of age) (25 trials).
Studies awaiting assessment
Nine trials were identified on a search update to May 2008, and a further trial was added after a referee's comment.
Risk of bias in included studies
Methodological quality scores of each item for all included studies are given in Table 2. A summary of the findings of key indicators of internal validity are listed below.
Allocation concealment
Eleven studies provided some information about the method of randomisation that suggested that randomisation was probably concealed (i.e. the use of concealed envelopes or the randomisation was generated by an independent person) (Baker 2001; Chin A Paw 2006; Donald 2000; Foley 2003; Jette 1999; Latham 2001; Latham 2003; McMurdo 1995; Moreland 2001; Sims 2006; Sullivan 2005). Nineteen studies used randomisation list/table but allocation concealment was unclear (Barrett 2002; Baum 2003; Buchner 1997; de Vos 2005; de Vreede 2007; DiFrancisco 2007; Ettinger 1997; Krebs 2007; Liu-Ambrose 2005; Maurer 1999; Miller 2006; Schilke 1996; Segal 2003; Singh 1997; Singh 2005; Skelton 1995; Suetta 2004; Vincent 2002; Wieser 2007).
Loss to follow-up
Some trials had high drop-out rates, with several studies reporting more than 20% of their participants were lost to follow-up (Bruunsgaard 2004; Chin A Paw 2006; DeBeliso 2005; Donald 2000; Katznelson 2006; Kongsgaard 2004; Mangione 2005; Mikesky 2006; Topp 1996). In some studies there was clear evidence of bias associated with the deliberate exclusion of patients such as those who failed to adhere to the exercise programme (Izquierdo 2004; Madden 2006; Topp 1996; Vincent 2002) or those who had adverse responses (Hagerman 2000).
Intention-to-treat analysis
Twenty-two studies stated that they used intention-to-treat analysis (Baker 2001; Barrett 2002; Baum 2003; Buchner 1997; Chin A Paw 2006; Ettinger 1997; Fiatarone 1994; Foley 2003; Judge 1994; Katznelson 2006; Latham 2003; Liu-Ambrose 2005; Macaluso 2003; Mikesky 2006; Miller 2006; Moreland 2001; Nelson 1994; Ouellette 2004; Pu 2001; Segal 2003; Sims 2006; Sullivan 2005).
Blinded outcome assessment
Thirty-three studies stated that they used a blinded assessor for all outcome measures (Barrett 2002; Baum 2003; Bean 2004; Boshuizen 2005; Buchner 1997; Casaburi 2004; Castaneda 2004; Chin A Paw 2006; de Vreede 2007; Ettinger 1997; Foley 2003; Haykowsky 2005; Jette 1996; Jette 1999; Jones 1994; Judge 1994; Kalapotharakos 2005; Katznelson 2006; Krebs 2007; Latham 2003; Liu-Ambrose 2005; Mangione 2005; Maurer 1999; McMurdo 1995; Mikesky 2006; Miller 2006; Moreland 2001; Newnham 1995; Segal 2003; Sims 2006; Singh 2005; Sullivan 2005; Westhoff 2000).
Eight additional studies used a blinded outcome assessor for some, but not all outcome assessments (Baker 2001; Castaneda 2001; de Vos 2005; Fiatarone 1994; Ouellette 2004; Pu 2001; Singh 1997; Suetta 2004).
Blinding of participants
Blinding of participants is difficult in studies of exercise interventions. However, the use of attention control groups can help to minimise bias. Thirty-six studies used some type of attention programme for the control group (Baker 2001; Baum 2003; Bean 2004; Brochu 2002; Bruunsgaard 2004; Castaneda 2001; Castaneda 2004; Chin A Paw 2006; Damush 1999; Ettinger 1997; Fiatarone 1994; Fiatarone 1997; Foley 2003; Judge 1994; Kongsgaard 2004; Latham 2003; Liu-Ambrose 2005; Mangione 2005; Maurer 1999; McCartney 1995; McMurdo 1995; Mihalko 1996; Mikesky 2006; Miller 2006;Miszko 2003; Moreland 2001; Newnham 1995; Ouellette 2004; Pu 2001; Seynnes 2004; Simons 2006; Sims 2006; Singh 1997; Suetta 2004; Topp 1993; Topp 1996). In 10 of these studies, the control group received ‘sham’ exercise programmes (Bean 2004; Brochu 2002; Castaneda 2001; Castaneda 2004; Kongsgaard 2004; Liu-Ambrose 2005; Mikesky 2006; Ouellette 2004; Pu 2001; Seynnes 2004).
Duration of follow-up
Five studies continued to follow up the participants after intervention had ended (Buchner 1997; Fiatarone 1994; Moreland 2001; Newnham 1995; Sims 2006). Two of these followed up falls for more than one year (Buchner 1997; Fiatarone 1994).
Effects of interventions
Eleven studies did not report final means and standard deviations for some or all of their outcome measures but instead reported baseline mean scores and mean change in scores from baseline (Baum 2003; Bean 2004; Buchner 1997; Chandler 1998; Fiatarone 1994; Hiatt 1994; Jette 1996; Lamoureux 2003; Madden 2006; Sullivan 2005; Topp 1996). If additional data could not be obtained from the investigators, the final mean score was estimated by adding the change in score to the baseline score, and the standard deviation of the baseline score was used for the final score.
Four studies did not report standard deviations for some or all of their outcome measures but instead reported standardized errors (Ouellette 2004; Seynnes 2004; Suetta 2004; Topp 2002). The standard deviations were estimated based on reported standardized errors and sample sizes.
Eight studies did not report numerical results of outcomes of interest for the purpose of this review and additional data were not provided by the investigators (Castaneda 2004; Fielding 2002; Harris 2004; Haykowsky 2005; Krebs 2007; Miller 2006; Topp 2005; Wieser 2007).
PRT versus control
Measures of physical (dis)ability/HRQOL (complex physical activities)
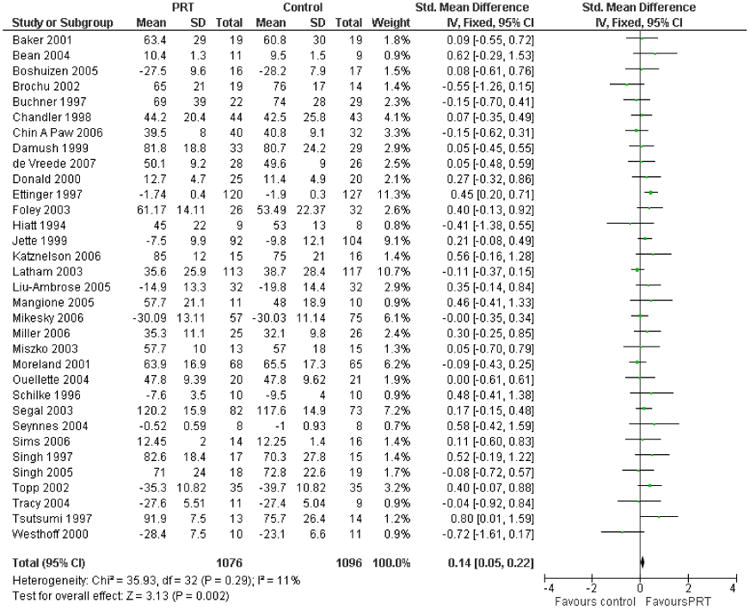
The main function (disability) measures from trials that had appropriate data were pooled using the standardised mean difference (SMD) and a fixed-effect model. Because studies measured function in scales with different directions, a higher score indicates either less disability/better function or more disability/poor function, a transformation was conducted to make all the scales point in the same direction. Mean values from trials in which a higher score indicates more disability/poor function were multiplied by -1. There is a significant effect of PRT in decreasing disability (see Figure 1; Analysis 1.1: 33 trials, 2172 participants; SMD 0.14, 95% CI 0.05 to 0.22). When the physical function domain of SF-36 or SF-12 was pooled from 14 studies (n = 778) using a fixed-effect model, no difference was found (Analysis 1.2: SMD 0.07, 95% CI -0.08 to 0.21). No difference was found from the pooled results of three trials for activity of daily living measures (Analysis 1.3). A number of studies had function measures (i.e. measures of activity, function or HRQOL) that could not be pooled. The available data from these measures are reported in Table 3.
Figure 1. Forest plot of comparison: 1 PRT versus control, outcome: 1.1 Main function measure (higher score = better function).
Measures of impairment
Strength
Many different muscle groups were tested and a number of methods were used to evaluate muscle strength in these trials. To minimise clinical heterogeneity, data were pooled from one muscle group. The leg extensor group of muscles was selected since this group was the most frequently evaluated. The effect size was calculated using standardised mean difference (SMD) to allow the pooling of data that used different units of measurement. Seventy-three studies involving 3059 participants reported the effect of resistance training on a lower-limb extensor muscle group and provided data that allowed pooling. A moderate-to-large beneficial effect was found (Analysis 1.5: SMD 0.84, 95% CI 0.67 to 1.00, random-effects model; fixed-effect model: SMD 0.53, 95% CI 0.46 to 0.61).
Supplementary analyses
Significant statistical heterogeneity was apparent in these data (P < 0.0001). Since a large number of studies assessed this outcome, it was possible to explore this heterogeneity by stratifying the data. Differences in treatment effects due to the quality of the trials were investigated. We also explored subgroups of trials that were based on the design of the treatment programmes and the characteristics of the participants.
To explore the effect of data quality on treatment effects, data were stratified by four design features that are associated with internal validity. These are allocation concealment; blinded assessors; intention-to-treat analysis (ITT); and attention control groups. The fixed-effect model was used throughout in order to obtain the results for the test for subgroup differences. The effect was smaller in the few studies with clear allocation concealment (6 trials, 607 participants) compared with studies with unknown concealment of allocation (67 trials, 2452 participants): Analysis 10.1: test for subgroup differences: Chi2 = 32.69, df = 1 (P < 0.00001). The effect was also smaller in studies that used blinded assessors (19 trials, 1523 participants) compared with studies that did not use blinded assessors (54 trials, 1536 participants): Analysis 10.2: test for subgroup differences: Chi2 = 70.56, df = 1 (P < 0.00001). This was also true for studies that used intention-to-treat analysis (ITT) (12 trials, 1041 participants) versus no ITT (61 trials, 2018 participants): Analysis 10.3: test for subgroup differences: Chi2 = 49.74, df = 1 (P < 0.00001). It is noticable that trials that applied better design features tend to be the larger trials. The effect was smaller when attention control groups were used (attention control: 24 studies, 1408 participants, no attention control: 49 studies, 1651 participants): Analysis 10.4: test for subgroup differences: Chi2 = 25.04, df = 1 (P < 0.00001).
Subgroup analyses were conducted to explore the effect of PRT when the design of the exercise programme and the characteristics of the participants differed. The effect of differences in the exercise programme was explored by examining effect estimates in studies that used different intensity and duration. High intensity strength training was compared with low to moderate intensity training. This analysis suggests that while both training approaches are probably effective in improving strength, higher intensity training (54 trials, 2026 participants) has a larger effect on strength than low to moderate intensity training (19 trials, 1033 participants): Analysis 10.5: test for subgroup differences: Chi2 = 7.24, df = 1 (P = 0.007). Longer duration programmes (i.e. greater than 12 weeks) were also compared with shorter duration programmes (less than 12 weeks). The duration of the trial appeared to have minimal effect on the strength outcome (< 12 weeks: 20 trials, 828 participants; > 12 weeks: 36 trials, 1736 participants): Analysis 10.6: test for subgroup differences: Chi2 = 0.04, df = 1 (P = 0.85).
Treatment effects in older people with and without a chronic disease (or functional limitation) were also assessed. Again, resistance training appeared to be effective in improving strength in both groups of older people, but there was statistical heterogeneity in the effects. Studies that included participants who had specific health problems and/or functional limitations were compared with studies that included only healthy older people. The effect in older adults who were healthy has a larger effect size than older adults with specific health problems (healthy older adults: 46 trials, 1502 participants; older adults with specific health problems: 19 trials, 926 participants): Analysis 10.7: test for subgroup differences: Chi2 = 19.85, df = 1 (P < 0.00001). In addition, PRT in studies that included older adults who had a physical disability or functional limitation appeared to be less effective than in those that included older adults who did not have functional limitations (people with functional limitations: 13 studies, 784 participants; people with no functional limitations: 41 studies, 1349 participants): Analysis 10.8: test for subgroup differences: Chi2 = 29.33, df = 1 (P < 0.00001). However, this result could be confounded by the intensity of the PRT programmes, as almost all programmes that included people with functional limitations were carried out at a low to moderate intensity. There were insufficient data available to compare the results by gender (men only: 5 trials with 107 participants; women only: 15 trials with 486 participants).
Aerobic capacity
The main measure of aerobic capacity was pooled from 29 studies (n = 1138) using a random-effects model. These results suggest that PRT has a significant effect on aerobic capacity (Analysis 1.6: SMD 0.31, 95% CI 0.09 to 0.53). Further analyses were performed for three specific measures of aerobic capacity: VO2 max (ml/kg/min), peak oxygen uptake (L/min) and the six-minute walk test (meters). A consistent significant effect was found for VO2 max (Analysis 1.7: 18 trials, n = 710, MD 1.5 ml/kg/min, 95% CI 0.49 to 2.51). Similarly, a significant positive effect was found for the six-minute walk test (Analysis 1.8: 11 trials, n = 325, MD 52.37 meters, 95% CI 17.38 to 87.37).
Measures of functional limitations (simple physical activities)
Balance/postural control
Results from all balance performance measures were pooled using SMD and a fixed-effect model. Data pooled from 17 studies with 996 participants showed a small but non-significant benefit (higher score indicates better balance) for balance (Analysis 1.9: SMD 0.12 (95% CI 0.00 to 0.25).
Gait speed
Two different measures of walking speed were used: gait speed (measured in meters per second) and timed walk (i.e. time to walk a set distance, measured in seconds). A higher gait speed score indicates faster mobility, while a higher timed walk score indicates slower mobility. Because of this difference, these data were analyzed separately. Data for gait speed were available from 24 studies that included 1179 participants (Analysis 1.11: MD 0.08 m/s, 95% CI 0.04 to 0.12, random-effects). This indicated that PRT has a modest but significant beneficial effect on gait speed. Only eight trials measured the timed walk (seconds) as an outcome measure and no evidence of an effect was found (Analysis 1.12; 204 participants, MD -0.23 seconds, 95% CI -1.07 to 0.62, fixed-effect).
Timed up-and-go
Timed up-and-go (i.e. time to stand from a chair, walk three meters, turn, and return to sitting, measured in seconds) was analysed using a fixed-effect model. Data, available from 12 trials and a total of 691 participants, showed the PRT group took significantly less time to complete this mobility task (Analysis 1.13: MD -0.69 seconds, 95% CI -1.11 to -0.27).
Timed chair rise
Time to stand up from a sitting position data were available in 11 studies (n = 384). Because different numbers of sit-to-stand were counted, SMD and a random-effects model was used to pool these results. These showed a significant, moderate to large effect on this task in favour of the PRT group (Analysis 1.14: SMD -0.94, 95% CI -1.49 to -0.38).
Stair climbing
Time to climb stairs data, which were available from eight trials, also favoured PRT (Analysis 1.15). However, these results were highly heterogenous.
Falls
Thirteen studies collected data about the effect of resistance training on falls or reported the incident of falls, but the outcomes reported did not allow pooling of the data. The available data is reported in Table 4. Three of these studies (Buchner 1997; Fiatarone 1994; Judge 1994) were part of the FICSIT trial, a prospective preplanned meta-analysis to determine the effectiveness of exercise to prevent falls in older people (Province 1995). The data were extracted from the main FICSIT paper, because papers published about the individual exercise programmes did not provide useful data about the effect of resistance training alone on falls. One additional trial investigated the effect of resistance training on falls in older people while they were in hospital (Donald 2000). Another trial also assessed the effect of PRT on frail older people following discharge from hospital (Latham 2003). There is a more comprehensive review of the effect of exercise on falls in a separate Cochrane review (Gillespie 2003).
With the exception of Latham 2003, all of these trials were small (i.e. less than 80 participants in the resistance training and control groups). Only Donald 2000 found a significant reduction in falls, but there were few fall events in this trial.
Adverse events
Adverse events are reported for all trials in the review at the end of the results section.
Vitality
The vitality (VT) domain of the SF-36 health status measure was assessed in 10 studies involving 611 participants. For this measure, a higher score indicates better health (i.e. more vitality): there was no evidence of an effect of PRT from the pooled data (Analysis 1.17: MD 1.33 95% CI -0.89 to 3.55).
Pain
Data of bodily pain (BP) domain of the SF-36 health status measure were provided by 10 studies involving 587 participants. For this measure, a higher score indicates better health (i.e. less pain), there was no evidence that PRT had an effect on bodily pain (Analysis 1.18: MD 0.34, 95% CI -3.44 to 4.12). In contrast, six studies with 503 participants included pain measures where a higher score indicates more pain, and found evidence to support a modest reduction in pain following PRT (Analysis 1.19: SMD -0.30, 95% CI -0.48 to -0.13). These six studies all included participants with osteoarthritis and used pain measures designed specifically for this population, which could have increased their sensitivity to change.
Health service use, hospitalization and death
Five studies provided data about hospitalization rates, length of stay and/or outpatient visits. Donald 2000 reported that people who received PRT in addition to regular in-hospital physiotherapy had a length of stay of 27 days compared with 32 days for the control group. Latham 2003 found that 42/120 people in the PRT group were admitted to hospital over six months compared to 35/123 in the control group. The third trial by Singh 1997 reported that, over a 10 week period, people in the PRT group had mean 2.1 (SD 0.4) visits to a health professional and mean 0.24 (SD 0.2) hospital days compared to controls mean of 2.0 (SD 0.5) visits and mean 0.53 (0.4) hospital days. The fourth study by Singh 2005 reported visits to a health professional over the study (average numbers per person): high intensity group, 2 (2); low intensity group, 2 (1.8); controls, 5 (1.8). The fifth study by Miller 2006 reported participants' discharge destinations but did not specify the group: 52 participants were discharged to a rehabilitation programme, 12 were transferred to a community hospital, 16 were discharged to higher level care, and 20 returned directly to their pre-injury admission accommodation. An additional study, Buchner 1997, provided data about health service use, but only reported data that were pooled to include participants in aerobic training, combined aerobic training and PRT and PRT alone. This study found no change in hospital admissions between those in the exercise and control groups, but an increased number of outpatient visits by those in the control group. Finally, two studies stated that there was no difference in health care visits (Fiatarone 1997) or hospitalization (Pu 2001) but no specific data were provided.
Thirteen studies provided data about participant deaths that allowed pooling (Baum 2003; Boshuizen 2005; Chin A Paw 2006; Donald 2000; Ettinger 1997; Fiatarone 1994; Kallinen 2002; Latham 2003; Mangione 2005; Miller 2006; Moreland 2001; Newnham 1995; Selig 2004). The risk ratio of death in the PRT group was not significantly different from the control group (Analysis 1.20: 20 deaths versus 21 deaths; RR = 0.89, 95% CI 0.52 to 1.54).
Comparisons of PRT dosage
Thirteen trials investigated the effects of different doses of PRT. Note that data from medium intensity were not examined in the following.
High versus low intensity PRT
Physical function, pain and vitality
Of the 10 studies comparing high versus low intensity PRT, only two (Singh 2005; Tsutsumi 1997), evaluated physical function, pain and vitality using the domains of the SF-36. No significant difference was found for physical function (Analysis 2.1) or pain (Analysis 2.4), but vitality scores were statistically significantly higher for high intensity (Analysis 2.5: MD = 6.54, 95% CI 0.69 to 12.39).
Strength
Data from all nine studies (n = 219) were available to examine the effect of high versus low intensity PRT on lower limb strength (Beneka 2005; Fatouros 2005; Harris 2004; Hortobagyi 2001;Seynnes 2004; Sullivan 2005; Taaffe 1996; Tsutsumi 1997; Vincent 2002). The results indicate that high intensity training results in greater lower limb strength, as a moderate effect was seen (Analysis 2.2: SMD = 0.48, 95% CI 0.03 to 0.93; random-effects model).
Aerobic capacity
Three studies compared the effect of high versus low intensity PRT on aerobic capacity (Fatouros 2005; Tsutsumi 1997; Vincent 2002). These studies (n = 101) did not show greater benefit from high intensity compared with low intensity training (Analysis 2.3: MD 1.82 ml/kg/min, 95% CI -0.79 to 4.43; higher score favours high-intensity group).
High intensity versus variable intensity PRT
One trial (Hunter 2001) comparing high intensity PRT with variable intensity PRT showed no statistically significant differences for strength (Analysis 3.1: n = 24, MD = 0.61, 95% CI -0.21 to 1.44) and aerobic capacity (Analysis 3.2).
Frequency
Taaffe 1999 and DiFrancisco 2007 compared PRT at different frequencies, respectively three times a week versus once a week, and twice a week versus once a week. Both studies recruited few participants and applied high intensity intervention. There were no significant differences between the two exercise frequencies in muscle strength (Analysis 4.1: MD = 0.40, 95% CI -0.44 to 1.25; MD = -0.46, 95% CI -1.40 to 0.48).
Sets
Galvao 2005 compared PRT at 3-sets versus 1-set in 28 participants. No significant differences between the two groups were found for muscle strength (Analysis 5.1), six minute walk test (Analysis 5.2), sit-to-stand (Analysis 5.4) and stair climbing (Analysis 5.5). However, participants who exercised at 3-sets walked significantly faster than those who exercised at 1-set (Analysis 5.3: MD = -29.6 seconds, 95% -54.23 to -4.97).
PRT versus aerobic training
Physical function
Five studies evaluated the effect of PRT compared with aerobic training on physical function. Four studies (Buchner 1997; Earles 2001; Hiatt 1994; Mangione 2005) used outcomes in which a higher score indicates less disability (n = 125), and found no significant difference (see Analysis 6.1: SMD -0.21, 95% CI -0.56 to 0.15; lower score favours the aerobic training group). The other study (Ettinger 1997) (n = 237) also found no significant difference between the groups for function (see Analysis 6.2: SMD 0.05, 95% CI -0.21 to 0.30; higher score favours aerobic group).
Strength
Data on lower extremity strength were available from 10 studies (n = 487) (Ballor 1996; Buchner 1997; Earles 2001; Ettinger 1997; Fatouros 2002; Izquierdo 2004; Malliou 2003; Pollock 1991; Sipila 1996; Wood 2001). These data when pooled using a random-effects model showed that PRT had a significant benefit compared with aerobic training on strength (see Analysis 6.3: SMD 0.44, 95% CI 0.08 to 0.80; higher score favours PRT).
Aerobic capacity
Aerobic capacity was evaluated in eight studies involving 423 participants (Ballor 1996; Buchner 1997; Ettinger 1997; Hepple 1997; Hiatt 1994; Kallinen 2002; Madden 2006; Pollock 1991). This was measured using VO2 max in ml/kg/min. Using the random-effects model, aerobic training had a non-significant benefit compared to PRT for this outcome (Analysis 6.4: MD -1.13 ml/kg/min, 95% CI -2.63 to 0.38; higher values favours PRT).
Gait speed
Mangione 2005 reported on gait speed (m/s) and found no significant difference between groups (Analysis 6.6: MD -0.08 m/s, 95% CI -0.30 to 0.14; higher speed favours PRT group)
Pain
Ettinger 1997 found no significant difference between groups in pain (Analysis 6.7: MD 0.12; 95% CI -0.14 to 0.37; lower score favours PRT).
PRT versus balance
One study (Judge 1994) compared PRT with balance retraining (n = 55). This study found that strength improved in the PRT group, but not in the balance training group. Chair rise time and gait speed did not improve in any group, with gait speed actually declining in the balance training group. However, balance improved in the balance training group compared with the PRT group.
PRT versus functional training
Three studies compared PRT with functional training (Chin A Paw 2006; de Vreede 2007; Manini 2005). No significant differences between the two interventions were found for the reported outcomes (see: Analysis 7.1 physical function; Analysis 7.2 strength; Analysis 7.3 timed up and go; Analysis 7.4 vitality; Analysis 7.5 pain).
PRT versus flexibility training
Barrett 2002 (n = 40) compared a group of older adults who undertook PRT with a control group who did mainly stretching for the major muscle groups (flexibility training). No statistically significant differences were found for any of the reported outcomes (see: Analysis 8.1: SF-36 physical function; Analysis 8.2: strength; Analysis 8.3: timed walk; Analysis 8.4: chair stand; Analysis 8.5: vitality; Analysis 8.6: pain).
Power training
Two studies (de Vos 2005; Miszko 2003) (n = 76) compared power training with a control group. de Vos 2005 and another study (Macaluso 2003) also compared different intensities of power training. While the data for muscle strength for de Vos 2005 favoured high intensity power training, data pooling was inappropriate given the substantial and significant heterogeneity (see Analysis 9.1).
Adverse events
Among 121 studies that were reviewed, 53 studies provided no comment at all about adverse events associated with the training programme. Of the remaining 68 studies, 25 reported no adverse events and 43 reported some adverse reaction to the exercise programme. An additional eight studies did not report adverse events as such, but it is possible that an event occurred since these studies reported drop-outs from the exercise group secondary to increasing pain or specific injuries (Chandler 1998; Charette 1991; Fiatarone 1997; Hagerman 2000; Hortobagyi 2001; Jette 1996; Maurer 1999; Topp 1993). Given that there were considerably more drop-outs from the PRT group than from the control group (see methodological quality section above), it is possible that the number of cases of adverse events reported here are an underestimate.
Only nine studies provided an a priori definition of an adverse event in the study methods or objectives (Earles 2001; Ettinger 1997; Judge 1994; Kallinen 2002; Latham 2003; Liu-Ambrose 2005; Moreland 2001; Pollock 1991; Singh 1997). Eight of these nine studies detected adverse events (Earles 2001; Ettinger 1997; Judge 1994; Kallinen 2002; Latham 2003; Liu-Ambrose 2005; Moreland 2001; Pollock 1991). However, there was little consistency in the definition that was used, with some studies only reporting serious events that the investigators thought were possibly related to the exercise programme (i.e. Ettinger 1997) while other studies reported all adverse events that occurred in each group. Most adverse events were musculoskeletal problems. Serious adverse events were rare, and none appeared to be directly related to the exercise programme. One study reported one death of myocardial information in the PRT group (Kallinen 2002). Another two studies reported one death in the PRT group but the reason of death was not reported (Baum 2003; Chin A Paw 2006). Further details about all adverse events reported in these trials can be found in Table 5.
Discussion
Summary of main results
This review identified, graded and synthesized the available literature regarding the effect of a specific exercise intervention, PRT, on a particular population, older people. To increase the generalisability of these data, the trials included participants with a range of health problems, and the dose and delivery of the PRT programmes varied. This made it possible to assess overall effects of the intervention on older people, with a potential for exploring the effects on subgroups (i.e. in different groups of older people or with different doses of PRT). Overall, this review suggests that PRT has a small but significant effect on improving physical function (complex activities), a small to moderate effect on decreasing some impairments and functional limitations, and a large effect on increasing strength. Adverse events were poorly reported in most studies, which limits the ability of this review to assess the risks associated with this intervention. Additionally, there is some preliminary evidence that suggests that PRT might reduce pain in older people with osteoarthritis. The effect of exercise on reducing pain in people with osteoarthritis is reported in another Cochrane review (Brosseau 2003). The sparse data did not allow an adequate assessment of the effect of PRT on fall risk. However, a separate Cochrane review (Gillespie 2003) has reviewed fall prevention.
Overall completeness and applicability of evidence
This review update highlights the fact that exercise training in older adults continues to be a dynamic area of research, with the number of included studies doubling in the five years since the previous review. A quick update extending the MEDLINE search to May 2008 identified nine further studies. However, the majority of the trials continue to be studies with small sample sizes.
This review deliberately used broad inclusion criteria and multiple strategies to try to identify as many studies as possible that used PRT training with older adults. Despite these efforts, given the broad coverage of our review it is inevitable that we have missed some trials. It is particularly challenging to identify unpublished trials in this area because the studies could have been presented at many different types of conferences (stoke, OA, CHD etc). We acknowledge that it was not possible to hand search all of the potential conferences where studies in this area could be presented, and it is therefore possible that we missed some studies that had negative or neutral results and are more difficult to get published. Although we attempted to contact authors when there was any uncertainty about data, it is also likely that data could also have been missed both from the excluded trials (i.e. the outcomes may have been recorded but not reported) and the included trials (i.e. data not reported and/or data not available for pooling).
Quality of the evidence
The 121 studies in this review were generally of poor methodological quality, as most of the studies did not use design features that are known to increase internal validity, such as concealed randomisation; intention-to-treat analysis, blinded outcome assessors, or attention control groups. Only 11 studies used concealed randomisation; 22 studies used intention-to-treat analysis; and 33 studies used blinded outcome assessors for all outcomes. Therefore, caution is required when drawing conclusions from these data. When data were stratified by indicators of study quality for the outcome muscle strength, results from the high quality trials continued to support the positive effect of resistance training on strength. However, these data also indicate that low quality trials, usually small studies, that comprise the majority of the studies in the review probably overestimate the effect of resistance training because of random chance effects from small studies. The long-term outcome of PRT is unclear because the majority of studies stopped following up participants once the intervention had ended.
PRT versus control
PRT shows small positive effect on measures of physical function (disability). PRT also appears to have a positive effect on aerobic capacity and most measures of functional limitations, including gait speed, timed “Up-and-Go” and, the time to stand up from a chair. All of these effects were statistically significant, although the effect sizes tended to be small to moderate, and the clinical significance of these effects is unclear. PRT appears to have a large positive effect on strength and aerobic capacity in older people. However, there was a large amount of statistical heterogeneity associated with the estimate in strength. This variation was reduced, but not eliminated, by investigating differences in outcome in different groups of participants, types of intervention and in trials that used different quality indicators. Please note that results from such exploratory analysis are tentative. In exploratory subgroup analyses, it appeared that training intensity has the greatest effect on strength (i.e. high intensity training has a greater effect on strength than lower intensity training), while the duration of the training appears to have a reduced effect. The magnitude of the effect was influenced by participants' health status or functional status. PRT in healthy participants had a greater effect than in those with a chronic disease or functional limitation. In other words, it appeared that people with a pre-existing health condition or with functional limitations had smaller gains in strength. Additionally, men had larger gains in strength than women; although there were fewer trials in men. These subgroup analyses must be interpreted with caution as the number of participants is reduced which decreases the precision of these estimates. In addition, it is possible that study size is a source of heterogeneity, as several of the largest and highest quality trials included people with function limitations and/or lower intensity training programmes, and study quality appears to reduce the effect estimates. Overall, the effect of PRT on function is positive for older adults; although the effect seems diminished when it transfers from muscle strength to functional limitations and disability.
It was not possible to pool fall data because falls were reported differently in the five studies that measured this outcome. These data might suggest a trend towards PRT reducing falls, since four of the five studies found that participants in the PRT group had fewer falls than those in the control group. However, the effect of PRT alone on falls is still not clear.
Adverse events were poorly monitored and reported in most of these trials. This makes it difficult to assess the risk of injury or other adverse events associated with resistance training. The finding that several studies reported drop-outs from the exercise programme due to pain or injury, yet failed to report any adverse events, suggests that adverse events might have been under-reported in some trials. This hypothesis is further supported by the finding that the studies with a clear definition of adverse events in their study methods were more likely to detect these events than those with no definition. The large number of drop-outs from the PRT group compared to controls also raises the possibility that people are experiencing adverse effects from PRT that are not identified in these trials. However, it is reassuring that participant's pain and vitality were not affected by PRT, and in fact PRT appeared to decrease pain in people with osteoarthritis. Furthermore, there was no evidence of increased risk of hospitalization. A few studies reported decreased use of health care services in the PRT group. Finally, there were a few reports of serious adverse events (i.e. myocardial infarction or death) in the PRT group but there was no evidence that these events were directly associated with the intervention. There was also no evidence of increased risk of death in the PRT group when compared with the control group.
Comparison of PRT dosage
There are currently few randomized data available to guide the dose and prescription of PRT. Trials investigated different aspects of this issue were all small studies and most were of poor quality. When high intensity training was compared with low intensity training, data from 10 trials show that high intensity training has a greater effect on strength than lower intensity training. Among these 10 trials, three show that high intensity training has a greater effect on aerobic capacity. Eight of the 10 trials were healthy older people who participated in highly supervised, gym-based programmes. Therefore, it is not clear if high intensity PRT is more beneficial than low intensity training in less fit or healthy older people and/or in home or hospital based programmes. Limited evidence are available for exercise frequencies and sets.
PRT versus other training
Overall, no significant differences were found between the different types of training. When PRT is compared to aerobic training, PRT tended to produced larger gains in strength than aerobic training. However, these two types of training are not different in aerobic capacity. This finding is to be expected, given that the strength outcome is more specific to PRT. There are fewer data available to determine the comparative effect of these types of training on physical disability, but the available data suggest that the two training programmes have a similar effect on this outcome. There are too few data to draw conclusions about other forms of training such as balance or mobility training compared to PRT.
Authors' Conclusions
Implications for practice
Doing PRT two to three times a week can improve physical function in older adults, including reducing physical disability, some functional limitations (i.e. balance, gait speed, timed walk, timed ‘up-and-go’, chair rise; and climbing stairs) and muscle weakness in older people. Therefore, it would appear to be an appropriate intervention for many older people to improve performance of some simple physical tasks. The training also shows a reduction in pain in people with osteoarthritis. However, some caution is warranted with this intervention as in many studies adverse effects have been poorly monitored. Nonetheless, serious adverse events appear to be rare. When used in clinical practice, clinicians should monitor for adverse effects, particularly when older people who might be at higher risk of injury (i.e. frail or recently ill older people) are undertaking PRT. Additionally, there is no information regarding how long these effects can be maintained because the majority of the studies did not follow up the effect after the training had ended.
Implications for research
We recommend that future trials investigating the effect of PRT in older people should:
minimise bias by using concealed randomisation, blinded outcome assessors, intention-to-treat analysis and attention control groups;
recruit an adequate number of participants so that a precise estimate of the effect of the intervention can be determined (should have a priori power calculations);
include a careful assessment of adverse events in both treatment groups, so that both the benefits and risks of PRT are fully evaluated;
follow up participants after the programmes have completed to examine the long-term effects of PRT.
Future trials should include participants and interventions that are similar to those in health care settings (i.e. frail or recently ill older people), so that, if proven to be effective, resistance training can be incorporated into routine health care services. Well-designed trials are also required to determine the most appropriate dose of PRT to use with different participants and in different settings.
Table 1. Assessment of methodological quality scheme.
| Items | Scores | Notes |
|---|---|---|
| A. Was the assigned treatment adequately concealed prior to allocation? | 2 = method did not allow disclosure of assignment. 1 = small but possible chance of disclosure of assignment or unclear. 0 = quasi-randomised or open list/tables. |
|
| B. Were the outcomes of patients/participants who withdrew described and included in the analysis (intention-to-treat)? | 2 = withdrawals well described and accounted for in analysis. 1 = withdrawals described and analysis not possible. 0 = no mention, inadequate mention, or obvious differences and no adjustment |
|
| C. Were the outcome assessors blind to treatment status? | 2 = effective action taken to blind assessors. 1 = small or moderate chance of un blinding of assessors. 0 = not mentioned, or not possible. |
|
| D. Were the participants blinded to the treatment status? | 2 = effective action taken to blind assessors. 1 = small or moderate chance of un blinding of assessors. 0 = not mentioned, or not possible. |
|
| E. Were the treatment and control group comparable at entry? Specifically, were the groups comparable with respect to age, medical co-morbidities (one or more of history of coronary artery disease, stroke, hypertension, diabetes, chronic lung disease), pre-entry physical dependency (independent vs dependent in self-care ADL) and mental status (clinical evidence of cognitive impairment, yes or no)? | 2 = good comparability of groups, or confounding adjusted for in analysis. 1 = confounding small; mentioned but not adjusted for. 0 = large potential for confounding, or not discussed. |
|
| F. Were care programmes, other than the trial options, identical? | 2 = care programmes clearly identical. 1 = clear but trivial differences. 0 = not mentioned or clear and important differences in care programmes |
|
| G. Were the inclusion and exclusion criteria clearly defined? | 2 = clearly defined. 1 = inadequately defined. 0 = not defined. |
|
| H. Were the interventions clearly defined? | 2 = clearly defined interventions are applied with a standardised protocol. 1 = clearly defined interventions are applied but the application protocol is not standardised. 0 = intervention and/or application protocol are poorly or not defined |
|
| I. Were the outcome measures used clearly defined? | 2 = clearly defined measures and the method of data collection and scoring are clearly described 1 = inadequately defined measures 0 = not defined. |
For our primary outcome, physical disability in terms of self-report measures of physical function, we considered the outcome clearly defined if a validated and standardised scale was used and the method of data collection was clearly described. Our secondary outcome measures included gait speed, muscle strength (e.g. one repetition maximum test, isokinetic and isometric dynamometry), balance (e.g. Berg Balance Scale, Functional Reach Test), aerobic capacity, and chair rise. These secondary outcomes were considered well defined if validated and standardised measures were used, and the method of data collection and scoring of any scales was clearly described |
| J. Was the surveillance active and of clinically appropriate duration (i.e. at least 3 months)? | 2 = active and appropriate duration (three months follow-up or greater). 1 = active but inadequate duration (less than three months follow-up). 0 = not active or surveillance period not defined. |
Table 2. Quality rating of trials.
| Study | Concealed allocation | ITT | Assessor blind | Participants blind | Compable at entry | Identical care | Inclusion/exclusion | Interventions defined | Outcomes defined |
|---|---|---|---|---|---|---|---|---|---|
| Ades 1996 | 1 | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 |
| Baker 2001 | 2 | 2/0 | 2/0 | 2 | 2 | 2 | 2 | 2 | 2 |
| Balagopal 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 1 | 2 |
| Ballor 1996 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Barrett 2002 | 1 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 2 |
| Baum 2003 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Bean 2004 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Beneka 2005 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Bermon 1999 | 1 | 0 | 0 | 0 | 2 | 1 | 0 | 2 | 2 |
| Boshuizen 2005 | 1 | 1 | 2 | 0 | 1 | 2 | 2 | 2 | 2 |
| Brandon 2000 | 0 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Brandon 2003 | 1 | 1 | 0 | 0 | 2 | 0 | 1 | 2 | 2 |
| Brochu 2002 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Bruunsgaard 2004 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 1 |
| Buchner 1997 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Casaburi 2004 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 1 |
| Castaneda 2001 | 1 | 1 | 2/0 | 2 | 2 | 2 | 2 | 2 | 2 |
| Castaneda 2004 | 1 | 0 | 2 | 0 | 2 | 2 | 1 | 2 | 2 |
| Chandler 19981 | 1 | 0 | 1 | 0 | 2 | 2 | 2 | 2 | 2 |
| Charette 1991 | 1 | 0 | 0 | 0 | 1 | 2 | 0 | 2 | 2 |
| Chin A Paw 2006 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Collier 1997 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 1 | 2 |
| Damush 1999 | 1 | 0 | 0 | 1 | 2 | 2 | 1 | 1 | 2 |
| de Vos 20051 | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 |
| de Vreede 2007 | 1 | 1 | 2 | 0 | 2 | 2 | 1 | 2 | 2 |
| DeBeliso 2005 | 1 | 1 | 0 | 0 | 2 | 0 | 1 | 2 | 2 |
| DiFrancisco 2007 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 |
| Donald 2000 | 2 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 2 |
| Earles 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Ettinger 1997 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
| Fahlman 2002 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 |
| Fatouros 2002 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Fatouros 2005 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Fiatarone 1994 | 1 | 2 | 2/0 | 1 | 2 | 2 | 2 | 2 | 2 |
| Fiatarone 1997 | 1 | 0 | 0 | 1 | 0 | 2 | 0 | 2 | 2 |
| Fielding 2002 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Flynn 1999 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Foley 2003 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Frontera 2003 | 1 | 0 | 0 | 0 | 2 | 0 | 1 | 2 | 2 |
| Galvao 2005 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Hagerman 2000 | 1 | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 2 |
| Harris 2004 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Haykowsky 2005 | 1 | 1 | 2 | 0 | 0 | 2 | 1 | 2 | 2 |
| Haykowsky 2000 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 1 | 2 |
| Hennessey 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Hepple 1997 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Hiatt 1994 | 1 | 0 | 0 | 0 | 1 | 2 | 2 | 2 | 2 |
| Hortobagyi 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Hruda 2003 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Hunter 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 1 |
| Izquierdo 2004 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Jette 1996 | 1 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Jette 1999 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Jones 1994 | 1 | 0 | 2 | 0 | 2 | 2 | 1 | 2 | 2 |
| Jubrias 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Judge 1994 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
| Kalapothara 2005 | 1 | 1 | 2 | 0 | 2 | 2 | 1 | 2 | 2 |
| Kallinen 2002 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Katznelson 2006 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Kongsgaard 2004 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Krebs 2007 | 1 | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 2 |
| Lamoureux 2003 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Latham 2001 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Latham 2003 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
| Liu-Ambrose 2005 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Macaluso 2003 | 1 | 2 | 0 | 0 | 0 | 2 | 1 | 2 | 2 |
| Madden 2006 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Maiorana 1997 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 |
| Malliou 2003 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Mangione 2005 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Manini 2005 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Maurer 1999 | 1 | 0 | 2 | 1 | 1 | 2 | 2 | 1 | 2 |
| McCartney 1995 | 1 | 0 | 0 | 1 | 2 | 2 | 2 | 2 | 1 |
| McGuigan 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 1 |
| McMurdo 1995 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 1 | 2 |
| Mihalko 1996 | 1 | 0 | 0 | 1 | 1 | 2 | 0 | 1 | 1 |
| Mikesky 2006 | 1 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 2 |
| Miller 2006 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Miszko 2003 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Moreland 2001 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | 0 | 0 |
| Nelson 1994 | 1 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Newnham 1995 | 1 | 0 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
| Nichols 1993 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 |
| Ouellette 2004 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Parkhouse 2000 | 1 | 0 | 0 | 0 | 1 | 2 | 2 | 1 | 1 |
| Perrig-Chiello 1998 | 1 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
| Pollock 1991 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Pu 2001 | 1 | 2 | 2/0 | 2 | 2 | 2 | 2 | 2 | 2 |
| Rall 1996 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Reeves 2004 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Rhodes 2000 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 1 |
| Schilke 1996 | 1 | 0 | 0 | 0 | 2 | 2 | 0 | 1 | 2 |
| Schlicht 1999 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 |
| Segal 2003 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Selig 2004 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Seynnes 2004 | 1 | 1 | 0 | 2 | 2 | 2 | 2 | 2 | 2 |
| Simons 2006 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Simoneau 2006 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Simpson 1992 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 1 | 1 |
| Sims 2006 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| Singh 1997 | 1 | 0 | 2/0 | 1 | 2 | 2 | 2 | 2 | 2 |
| Singh 2005 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Sipila 1996 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 |
| Skelton 1995 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Skelton 1996 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 1 |
| Sousa 2005 | 1 | 0 | 0 | 0 | 2 | 0 | 1 | 2 | 2 |
| Suetta 2004 | 1 | 1 | 1 | 0 | 2 | 2 | 2 | 2 | 2 |
| Sullivan 2005 | 2 | 2 | 2 | 0/2 | 2 | 2 | 2 | 2 | 2 |
| Symons 2005 | 1 | 1 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Taaffe 1996 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Taaffe 1999 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Thielman 2004 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 |
| Topp 1993 | 1 | 0 | 0 | 1 | 2 | 2 | 1 | 2 | 2 |
| Topp 1996 | 1 | 0 | 0 | 1 | 2 | 2 | 1 | 2 | 2 |
| Topp 2002 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Topp 2005 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Tracy 2004 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Tsutsumi 1997 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Tyni-Lenne 2001 | 1 | 0 | 0 | 0 | 2 | 1 | 2 | 1 | 2 |
| Vincent 2002 | 1 | 0 | 0 | 0 | 2 | 2 | 1 | 2 | 2 |
| Westhoff 2000 | 1 | 0 | 2 | 0 | 2 | 2 | 1 | 2 | 2 |
| Wieser 2007 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
| Wood 2001 | 1 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 |
Note: 2/0 indicates that different standards used to assess different outcomes in the same study
NA = not available, no full report published
Table 3. Functional or quality of life measures that could not be pooled.
| Study | Outcome Measure | Treatment Group | Control Group |
|---|---|---|---|
| Baum 2003 | Physical performance test at 6 month. Mean = baseline score + change score. SD was not reported | 9.2 | 8.1 |
| Buchner 1997 | mean change in number of independent IADL's | mean 0.1 (SD 0.7) | mean 0.2 (SD 0.7) |
| Donald 2000 | Barthel Index (actual data not in paper) | no significant difference | |
| Fiatarone 1994 | ankle activity monitors (counts/day) | mean change 3412 (SD 1700) | mean change -1230 (SD 1670) |
| Fiatarone 1997 | overall self-reported activity level (measure not specified) | significant improvement (p<0.05) in exercise group | NR |
| Fielding 2002 | SF-36-PF | No significant differences between high intensity and low intensity groups | |
| Jette 1996 | SF-36 - PF (actual data not reported) | no significant difference between groups (data not reported) | |
| Kongsgaard 2004 | three ADLs of a questionnaire developed by the Danish Institute of Clinical Epidemiology | Actual data not reported. The author stated that the self-reported ADL level was significantly higher in the Ex group than in the control group | |
| Krebs 2007 | SF-36. 7 people (2 in PRT, 5 in Functional training) reported improvement in the SF-36 items | ||
| Maiorana 1997 | Physical Activity Questionnaire (no reference) self report | mean 209.8 (SD 142.9) kJ/kg | mean 250.1 (SD 225) kJ/kg |
| Maurer 1999 | SF-36 PF (no SD/SE reported) | mean 50.3 | mean 49.2 |
| Maurer 1999 | WOMAC section C (no SD/SE reported) | 464.4 | 606.6 |
| Maurer 1999 | Aims Mobility (no SD/SE reported) | 1.28 | 1.21 |
| McMurdo 1995 | Barthel Index (medians reported) | median change 0 (range -1 to 2) | median change control 0 (range -1 to 1) |
| Mihalko 1996 | adapted version of Lawton and Brody's IADL scale (higher = better, not pooled because study was cluster randomised) | mean 105 (SD 12) | mean 68 (SD 25) |
| Mikesky 2006 | SF-36 physical function at 30 month (the intervention was 1 - year) | n =81, mean = 65.37 (SD = 25.05) | n = 79, mean = 63.88 (SD = 25.48) |
| Nichols 1993 | Blair Seven-day recall Caloric Expenditure (KCalories) | not significantly altered | not significantly altered |
| Schilke 1996 | AIMS mobility score (actual data not reported) | “no significant differences between or within groups” | |
| Singh 1997 | IADL (Lawton Brody Scale) | mean 23.4 (SD 0.4) | mean 23.9 (SD 0.1) |
| Skelton 1996 | Human Activity Profile - (only reported training groups % change and the P-value of the change) | 3.9% change 3.9% change | NR |
| Skelton 1996 | Human Activity Profile - Max Activity Score | 0% change | NR |
| Skelton 1995 | Human Activity Profile | no difference from baseline | no difference from baseline |
| Thielman 2004 | Rivermead Motor Assessment | Significant improvement was found for people in the control group with low-level function | |
| Tyni-Lenne 2001 | Minnesota Living with Heart Failure Questionnaire (lower score = better QOL, medians reported) | median 19 (range 0-61) | median 44 (range 3-103) |
Table 4. Falls.
| Study | Fall Statistic | PRT | Control |
|---|---|---|---|
| Buchner 1997 | 1) Cox regression analysis, time to first fall, 0.53, 95% CI 0.3-0.91 for exercise group (including endurance exercise groups) | ||
| 2) proportion of people who fell in one year | all exercise groups: 42% | 60% | |
| 3) fall rate (falls/year) | all exercise: 0.81 falls/year | 0.49 falls/year | |
| Donald 2000 | 1) number of falls | 7 (n = 32) | 4 (n = 27) |
| 2) number of people who fell | 6 (n = 32) | 2 (n = 27) | |
| * Fiatarone 1994 | 1) average falls/subject | 2.32 | 2.77 |
| 2) covariance adjusted treatment incidence ratio (PRT vs control) | 0.95 (95% CI 0.64, 1.41) | ||
| Fiatarone 1997 | Falls | no difference between groups (no data provided) | |
| * Judge 1994 | 1) Average falls/subject | 0.82 | 1.22 |
| 2) Co-variate adjusted treatment incidence ratio (PRT vs control) | 0.61 (95%CI 0.34,1.09) | ||
| * Buchner 1997 | 1) Average falls/subject | 0.68 | 1.6 |
| 2) Co-variate adjusted treatment incidence ratio (PRT vs control) | 0.91 (95%CI 0.48,1.74) | ||
| Krebs 2007 | 1 in the PRT group sustained an unrelated fall halfway through the 6-week intervention, resulting in injury of her dominate shoulder. Exercise was modified for her | 1 | 0 |
| Latham 2001 | total falls | 164 | 149 |
| Latham 2003 | 1) number of people who fell | 60 | 64 |
| 2) fall-rate, person years | 1.02 | 1.07 | |
| Liu-Ambrose 2005 | the frequency of falls (excluded falls occurred in exercise classes) | 18 (1 subject fell 7 times) | 0 |
| Mangione 2005 | Reported the number of participants fell during post-training examination (n = 1 - group was not reported) | ||
| Miszko 2003 | Report number of people | 5 | 1 |
| Singh 2005 | Numbers per person, no statistical difference between groups | .15 (.37) | 0 |
Note: Data marked with * were obtained from Province 1995
Table 5. Adverse events.
| Study | Any Comment re: AE | AE Occurred (y/n/nr) | Description | Dropout Pathologies | Pain | Medical Care | Deaths |
|---|---|---|---|---|---|---|---|
| Ades 1996 | No | None reported | |||||
| Baker 2001 | Yes | No | NR | Yes, 2 in treatment group (neck arthritis, prior back injury), 2 in control (illness, psoriatic arthritis) | Treatment group decreased in WOMAC, SF-36 BP no change | NR | |
| Balagopal 2001 | No | NR | |||||
| Ballor 1996 | No | NR | |||||
| Barrett 2002 | Yes | Yes | 2 in PRT group, aggravation of OA | 2 in PRT group, aggravation of OA | |||
| Baum 2003 | Yes | Yes | The number of illness was not reported. 13% of repeated measurements after baseline were missing because of death or patient inability to perform the test because of acute illness | 1 in the PRT group | |||
| Bean 2004 | Yes | No | No significant adverse events occurred | ||||
| Beneka 2005 | No | NR | |||||
| Bermon 1999 | No | No | |||||
| Boshuizen 2005 | Yes | Yes | 9 dropout due to illness of participant or partner | 4 reported pain during or after the exercise | 1 in control | ||
| Brandon 2000 | No | NR | NR | ||||
| Brandon 2003 | Yes | 8 members of exercise group had BP raised to over 200 mmHg systolic or 100 mmHg diastolic at some point during the exercises during 24 months; and had to stop exercising that day | Participant's disease (diabetics) got worse; specific number was not reported | ||||
| Brochu 2002 | Yes | Yes | 2 experienced occasional significant exacerbation of arthritic conditions during the training. 1 experienced significant dizziness in a supine position | Yes, 3 due to medical problems that are not related to the training | 2 individuals experienced occasional significant exacerbation of arthritic conditions during the training | NR | NR |
| Bruunsgaard 2004 | No | NR | |||||
| Buchner 1997 | Yes | Yes | 6 Injuries in strength training or in strength/endurance training group (not reported separately, n = 50) | Not described | no significant change in BP of SF-36 | For all exercise groups (i.e. including endurance exercise groups): stable outpatient visits in exercise group/control increased, no difference in hospitalisation rates | |
| Casaburi 2004 | Yes | No | 5 (group?) -non protocol related health problems | NR | |||
| Castaneda 2001 | Yes | No | No | ||||
| Castaneda 2004 | Yes | Yes | The authors did not report the number and group of the dropouts. The statement is “reasons for early termination of the study included loss of greater than 20% of initial body weight, need for dialysis therapy or transplantation, development of a serious condition requiring hospitalization or precluding exercise and signs of malnutrition” | ||||
| Chandler 1998 | No | 9 dropouts due to illness, 1 due to increased hip pain, 1 refused further strength testing (not given by group) | NR | NR | |||
| Charette 1991 | No | 1 discomfort after initial strength testing, 3 intercurrent illness not related to training | NR | NR | |||
| Chin A Paw 2006 | Yes | Yes | None withdrew because of adverse effects | 9 illness in PRT; 9 illness in functional training group; 10 illness in combined training group; 6 illness in control group | 1 in PRT; 4 in functional training; 1 in combined training; 2 in control group | ||
| Collier 1997 | No | No | |||||
| Damush 1999 | No | 6 exercise drop-outs due to illness | |||||
| de Vos 2005 | Yes | Yes | 20 AEs reported in 17 participants. 16 were related to strength testing and 4 were related to power training. 8 were in high intensity group, 7 in medium, 4 in low, and 1 in control. AEs included minor strains, tendonities, and exacerbation of osteoarthritis | 4 (1 in each group) dropout-joint pain 1 inguinal hernia in medium intensity group. 1 medical reason in low intensity group | Joint pain (see dropout pathologies) | ||
| de Vreede 2007 | Yes | Yes | PRT: 1 had muscle strained. 10 reported muscle pain, 5 osteoarthritic joint pain, 3 prosthetic joint pain, and 4 lower back pain | PRT group: 1 hip fracture, 1 pneumonia, & 1 eye operation. Control: 1 wrist fracture | PRT: 10 reported muscle pain, 5 osteoarthritic joint pain, 3 prosthetic joint pain, and 4 lower back pain | ||
| DeBeliso 2005 | Yes | No | no injuries occurred during the training | ||||
| DiFrancisco 2007 | Yes | No | Occasionally complaints of muscle soreness for 2 days after exercise, but it did not affect participants' daily routine or training | ||||
| Donald 2000 | No | not clear | |||||
| Earles 2001 | Yes (a priori outcome) | Yes | 4 reported discomfort, 2 stopped program - 1 due to back pain, 1 due to lumbar disc herniation, possibly due to study intervention | Yes | |||
| Ettinger 1997 | Yes | Yes | PRT: 2 falls, one weight dropped on foot; Aerobic: 2 falls; Control: 1 sudden death (defined AE as death or injury requiring medical care) | NR | less for PRT group vs control | NR | NR |
| Fahlman 2002 | No | NR | |||||
| Fatouros 2002 | No | NR | |||||
| Fatouros 2005 | Yes | Yes | 3 men stopped within the 1st week due to injury | ||||
| Fiatarone 1997 | No | 1 exercise dropout due to increased musculoskeletal pain | NR | no difference in health care visits between groups | NR | ||
| Fiatarone 1994 | Yes | Yes | PRT: 2 reports of joint pain, program was altered No control info No cardiovascular events | 2 exercise drop outs, 1 due to musculoskeletal pain, 1 due to pneumonia | not measured | NR | 0 PRT and 1 control |
| Fielding 2002 | Yes | Yes | see the dropout pathologies | 4 (2 in each group) discontinued secondary to exacerbation of preexist OA. 1 in the high velocity group withdrew secondary to recurrence of chronic plantar fasciicis | |||
| Flynn 1999 | No | NR | NR | NR | NR | ||
| Foley 2003 | Yes | Yes | Gym-based exercise group: 2 had increased pain and 1 had increased blood pressure. 1 -Dr. advised to cease program | Gym-based exercise group: 2 with increased pain, 1 with unrelated surgery, 1 with increased blood pressure, and 1 had joint replacement surgery. Control group: 2 with joint replacement surgery and 1 with illness | 2 reported increased pain the gym-based exercise group. | ||
| Frontera 2003 | No | NR | |||||
| Galvao 2005 | Yes | No | 1 in 1-set group withdrew due to illness, 1 due to injury sustained during part-time work, and 1 due to aggravation of a preexisting hip injury | ||||
| Hagerman 2000 | No | 3 PRT and 1 control withdrew because of minor injuries or previous medical problems exacerbated by testing/training | “no complaints of excess or intolerable muscle soreness or fatigue” | NR | NR | ||
| Harris 2004 | Yes | No | |||||
| Haykowsky 2005 | Yes | Yes | 1 in PRT withdrew because of shoulder discomfort and migraines. 1 in the combination training suffered a lower extremity injury not related to the study | ||||
| Haykowsky 2000 | Yes | No (completed without complications) | NR | ||||
| Hennessey 2001 | No | NR | |||||
| Hepple 1997 | No | No | |||||
| Hiatt 1994 | No | No | |||||
| Hortobagyi 2001 | No (not identified as such) | Yes | Pain and bruising of shoulder from machine - dropped out | Yes | Yes | NR | NR |
| Hruda 2003 | Yes | Yes? | 5 (2 in the PRT group and 3 in the control group) dropped out due to health reasons | ||||
| Hunter 2001 | No | NR | |||||
| Izquierdo 2004 | No | NR | |||||
| Jette 1996 | No (not identified as such) | Yes - 2 dropouts because of the exercises, 1 due to back pain, 1 due to shortness of breath during exercise, | |||||
| Jette 1999 | Yes | No | Reasons not described | NR, but fatigue significantly worse in exercise group | NR | NR | |
| Jones 1994 | Yes | No | NR | ||||
| Jubrias 2001 | Yes | No | NR | ||||
| Judge 1994 | Yes (a priori outcome of study) | Yes | 10/55 people in RT or combined balance and RT developed musculoskeletal complaints, (specific details given), only 1 complaint in balance group, no control report, no serious injuries in any group | NR | NR | ||
| Kalapotharakos 2005 | NR | NR | |||||
| Kallinen 2002 | Yes | Yes | 1 -PRT, died of myocardial infarction at 8 weeks; 1-PRT, unstable angina at 4 weeks; 1 in PRT, began to have occasional angina and dyspnoea at 8 weeks; 1-endurance, brainstem infarction at week 9, 1-endurance, abnormal aortic aneurysm happened after the program | See the description | 1 in PRT, died of myocardial infarction | ||
| Katznelson 2006 | Yes | Yes | 5 were due to events unrelated to study drug, including bruised ribs, need for knee replacement, angina prior to the baseline visit, nausea during the first week of the study, and excessive i e commitments. Another subject in the placebo arm withdrew because of depression | ||||
| Kerr 2001 | No | Yes 3 in FITNESS group, including wrist and back injury | |||||
| Kongsgaard 2004 | No | NR | |||||
| Krebs 2007 | Yes | Yes | 1 in the PRT group sustained an unrelated fall halfway through the 6-week intervention, resulting in injury of her dominate shoulder. Exercise was modified for her | ||||
| Lamoureux 2003 | No | NR | |||||
| Latham 2001 | Yes | No | No | ||||
| Latham 2003 | Yes (a priori outcome) | Yes | 18 musculoskeletal adverse events in PRT group vs 5 in control group | No | 6 in PRT versus 8 in control | ||
| Liu-Ambrose 2005 | Yes | Yes | 10 in PRT group and 2 in stretching control group had minor musculoskeletal complains but resolved or diminished within 3 weeks | Yes, 1 in PRT and 1 in control drop out due to illness | |||
| Macaluso 2003 | Yes | Yes | 1 back pain and 1 spur on the heel | 1 back pain and 1 spur on the heel | 1 back pain | ||
| Madden 2006 | No | NR | |||||
| Maiorana 1997 | Yes (safety an aim of study) | Yes | In ex group: MI (before exercises began), 1 vasovagal episode, 1 musculoskeletal pain. Control: 2 people stop testing because of aggravation of psoriatic arthritis (1) and atrial fibrilation (1) | Yes, as reported | NR | NR ischaemic symptoms/ECG changes during training | |
| Malliou 2003 | No | NR | |||||
| Mangione 2005 | Yes | Yes | several participants reported muscle soreness or fatigue in the PRT group. 1 fell during post-training examination, 4 in the PRT were hospitalized | in the PRT group, 1-illness (progressive neuromuscular disorder), 4 were hospitalized | 1 in aerobic training group was unable to perform exercise at recommended intensity level | 2 (among those who were hospitalized) in the PRT group | |
| Manini 2005 | Yes | Yes | 11 were excluded from the steadiness experiment because of discomfort from knee OA during the testing protocol. 14 dropout for a variety of medical personal reasons | 11 were excluded from the steadiness experiment because of discomfort from knee OA during the testing protocol. 14 others dropped out for a variety of medical and personal reasons | |||
| Maurer 1999 | Yes | No | Yes, 4 dropouts due to increased pain “but neither subjects nor investigators attributed pain to the treatment” | WOMAC pain, 143.8 in PRT vs 167.1 control | NR | NR | |
| McCartney 1995 | Yes | No | 9 exercise drop-outs due to “illness”, 3 controls due to medical problems. Stated “no injuries as a result of training” | ||||
| McGuigan 2001 | No | NR | |||||
| McMurdo 1995 | Yes | No | see hosp admissions | 3 hospital admissions in PRT, 2 in control, 3 in home mobility - reported not related to exercise | 2 in home mobility group, no others - not related to exercise | ||
| Mihalko 1996 | No | NR | |||||
| Mikesky 2006 | Yes | Yes | 1 discontinued in the PRT group because of increased knee pain | 1 discontinued in the PRT group because of increased knee pain | 1 discontinued in the PRT group because of increased knee pain | ||
| Miller 2006 | No | NR | Discharge destination - on discharge from acute care, 52 participants were discharged to a rehabilitation programme, 12 were transferred to a community hospital, 16 were discharged to higher level care and 20 returned directly to their pre-injury admission accommodation | 2 in PRT, 1 in attention control | |||
| Miszko 2003 | Yes | Yes | 6 women fell (5 in PRT, 1 in control) | Some (the number is not specified) due to personal medical reasons or injuries | |||
| Moreland 2001 | Yes (a priori outcome) | Yes | yes to pain or stiffness = 14 in PRT vs 8 in control; other adverse: 8 in PRT vs 3 in control | 5 withdrew due to medical complications in PRT vs 3 in control | |||
| Nelson 1994 | Yes | Yes | 7/20 in PRT group experienced transient musculoskeletal pain; 3 musculoskeletal injuries (2 fractures and 1 sprain) in the control group | No - MI in PRT group occurred while patient was on vacation | |||
| Newnham 1995 | No | No | 3 in each group | ||||
| Nichols 1993 | Yes (safety a priori objective) | Yes | control subject contused sternum during baseline testing, mild to moderate delayed onset muscle soreness | PRT - 1 injury unrelated to program | |||
| Ouellette 2004 | Yes | Yes, 4 events | 1 in the PRT group was withdrawn after coronary artery stent placement unrelated to study participation. 2 subjects did not undergo week-12 strength testing due to recurrence of an inguinal hernia (PRT group) and ECG abnormalities (control group). A fourth subject experienced anginal symptoms consistent with coronary artery disease but returned to the study after medical clearance | Please see the description | |||
| Parkhouse 2000 | No | NR | |||||
| Pollock 1991 | Yes (a-priori outcome, well-defined) | Yes | 11/57 subjects sustained an injury during 1RM testing; 2/23 sustained an injury during training. In aerobic group, no injuries during testing but 9/21 had an injury during training | NR by group | |||
| Pu 2001 | Yes | Yes | 1 control patient developed trochanteric bursitis from 1 RM testing, 4 people had mild musculoskeletal soreness, no cardiac complications, deaths or hospitalisations occurred | No | |||
| Rall 1996 | Yes | No | |||||
| Reeves 2004 | No | NR | |||||
| Rhodes 2000 | No | NR | |||||
| Sartario 2001 | No | NR | |||||
| Schilke 1996 | No | No | decreased in OASI, no difference between groups on AIMS | ||||
| Schlicht 1999 | Yes | No | No | ||||
| Segal 2003 | No | NR | |||||
| Selig 2004 | Yes | Yes | 1 illness (non-cardiac) and 1 died at home in the exercise group | 1 in exercise group | |||
| Seynnes 2004 | Yes | No | No injuries, medical complications, or study-related AE | 3 dropouts because of medical reasons not related to the study | |||
| Simons 2006 | Yes | NR | 2 dropouts for non-study related illnesses | ||||
| Simoneau 2006 | No | NR | |||||
| Simpson 1992 | No | No | |||||
| Sims 2006 | No | No | 1 acquired a health problem that prohibited from driving | ||||
| Singh 1997 | Yes (a priori outcome) | No | No | weeks of pain reported-: mean 5.4 (SD=0.7) in PRT, mean 5.6 (SD 0.7) in control | health prof visits mean 2. 1 (SD 0.4) for PRT; mean 2. 0 (SD 0.5) for control; hospital stays mean 0.24 (SD 0.2) for PRT, mean 0.53 (SD 0.4) for control | ||
| Singh 2005 | Yes | Yes | visits to a health professional, minor illness, pain, injuries requiring training adjustment, hospital days, falls | 2 drop out in low intensity group due to pain. I in the control due to hospitalisation | Muscular pain (number of weeks reported per person): High intensity group-4.1 (2.7); low intensity group-2.9 (2.6); control group-3.6 (2.5) Chest pain (number of weeks reported per person): High intensity group- 0.9 (1.9); low-intensity group-0.5 (0.9);control group-. 5 (0.8) | Visits to a health professional over the study (numbers per person): high intensity group -2 (2); low intensity group -2 (1.8); controls - 5 (1.8) | |
| Sipila 1996 | No | 3 drop-outs due to illness “not related to exercise” | |||||
| Skelton 1995 | Yes | No | 4 exercise and control participants dropped out because of ill-health “not related to exercise” | ||||
| Skelton 1996 | Yes | Yes | patient fainted due to an arythmia during exercise | NR | |||
| Sousa 2005 | No | NR | |||||
| Suetta 2004 | yes | No | 2 became ill (1 in PRT) for reasons unrelated to the study | ||||
| Sullivan 2005 | Yes | Yes | 7 withdrew, developed an exacerbation of an underlying medical problem | 7 withdrew, developed an exacerbation of an underlying medical problem | |||
| Symons 2005 | Yes | Yes | 5 knee discomfort; 1 bruising | 5 knee discomfort; 1 bruising | |||
| Taaffe 1996 | No | 5 drop-outs from exercise groups for medical problems “not related to the exercise program” | |||||
| Taaffe 1999 | No | NR | |||||
| Topp 1993 | No | 1 exercise drop-out due to worsening emphysema, 1 due to a stroke | |||||
| Topp 1996 | No | NR | |||||
| Topp 2002 | No | NR | |||||
| Topp 2005 | No | NR | |||||
| Tracy 2004 | No | NR | |||||
| Tsutsumi 1997 | No | NR | |||||
| Tyni-Lenne 2001 | Yes | Maybe | increased oedema in exercise patient | No | |||
| Vincent 2002 | Yes | Yes | 6 participants stopped exercise for 6 weeks due to hip/knee pain | few (the number is not specified) dropped out for surgery/injury not related to the study protocol | |||
| Westhoff 2000 | Yes (asked about complaints during exercise) | Yes | increased knee pain in person with OA, 1 person had pain from elastic band | 2 drop outs because of medica problems (1 had increased epileptic attacks, 1 was often ill) | |||
| Wieser 2007 | No | NR | |||||
| Wood 2001 | No | NR | stated none of the dropouts left the program as a result of adverse responses to treatment -not information about adverse events overall | No |
Plain Language Summary.
Progressive resistance strength training for improving physical function in older adults
Older people generally lose muscle strength as they age. This reduction in muscle strength and associated weakness means that older people are more likely to have problems carrying out their daily activities and to fall. Progressive resistance training (PRT) is a type of exercise where participants exercise their muscles against some type of resistance that is progressively increased as their strength improves. The exercise is usually conducted two to three times a week at moderate to high intensity by using exercise machines, free weights, or elastic bands. This review sets out to examine if PRT can help to improve physical function and muscle strength in older people.
Evidence from 121 randomised controlled trials (6,700 participants) shows that older people who exercise their muscles against a force or resistance become stronger. They also improve their performance of simple activities such as walking, climbing steps, or standing up from a chair more quickly. The improvement in activities such as getting out of a chair or stair climbing is generally greater than walking speed. Moreover, these strength training exercises also improved older people's physical abilities, including more complex daily activities such as bathing or preparing a meal. PRT also reduced pain in people with osteoarthritis. There was insufficient evidence to comment on the risks of PRT or long term effects.
Acknowledgments
The authors would like to thank the editorial team of the Cochrane Bone, Joint and Muscle Trauma Group, particularly Lindsey Elstub, Lesley Gillespie, Joanne Elliott and Leeann Morton, for their assistance throughout the review process. In particular, thanks to Lesley and Joanne for searching the Cochrane registers and assistance with developing the search strategies. Thank you to Leeann and Lindsey for their advice and guidance about the procedures and content. We would also like to thank the Review Group's editors and the external referees, Prof John Campbell, Dr Keith Hill and Professor David Stott for their helpful comments on earlier drafts of this review.
The reviewers would like to thank Craig Anderson, Derrick Bennett, and Caroline Stretton for their contribution for the first review. The reviewers also would like to thank the National Institute of Disability and Rehabilitation Research (NIDDR) for a post-doctoral fellowship to the first author (H133P001) through Boston University and Switzer research fellowship (H133F060030) and National Institute of Aging (P30 AG031679) to the second author for supporting the review update. In addition, the second author received support for this review through a Pepper Center Trainee award from Boston Pepper Center funded by the National Institute of Aging (1P30Ag031679-01).
Sources of Support
Internal sources
Health and Disability Research Institute, School of Public Health, Boston University, USA.
Department of Occupational Therapy, School of Health and Rehabilitation Sciences, Inidana University at Indianapolis, USA.
External sources
NIDRR Post-doctoral Fellowship, grant # H133P001, USA.
NIDRR Switzer Research Fellowship, grant #H133F060030, USA.
National Institute of Aging, grant # P30 AG031679, USA.
Characteristics of Studies
Characteristics of included studies [ordered by study ID]
Ades 1996.
| Methods | RCT (randomised controlled trial) Method of randomisation: unclear Assessor blinding: no Participant blinding: no Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 24 Sample: healthy, sedentary Age: mean 70.4 years (SD 4) Inclusion criteria: healthy, sedentary older people Exclusion criteria: angina or electrocardiographic ischaemia during exercise test, resting BP >160/90, non-cardiopulmonary limitation of exercise capacity (i.e. claudication, arthritis, cerebrovascular disease) |
|
| Interventions | PRT (progressive resistance strength training) versus control 1. PRT Type of exercises: 4 UL (upper limb), 3LL (lower limb) Equipment: machines (Universal Gym) Intensity: high (50-80% of 1RM) Frequency: Ex3 Reps/ sets: 8/3 Duration: 12 weeks Setting: gym Supervision: not reported Adherence: not reported 2. Control Group: instructed not to alter their home activity habits |
|
| Outcomes | Strength (1 repetition maximum) Peak aerobic capacityComments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Baker 2001.
| Methods | RCT Method of randomisation: generated by statistician, concealed from investigators Assessor blinding: blinded for primary measures, not for secondary (including strength) Participant blinding: yes Loss to follow-up: 2/46 Intention-to-treat analysis: yes for primary, no for secondary measures Post-program follow up: no |
|
| Participants | Location: USA N = 46 Sample: older people with osteoarthritis. Recruited through community advertising Age: mean 68 years (SD 6) in the treatment group Inclusion criteria: age 55 or older, body mass index less than 40 kg/m2, pain on more than half the days of the past month and during activities and radiographic evidence of OA Exclusion criteria: medical condition that precluded safe participation in an exercise program or was more limiting than OA, inflammatory OA, or had participated in any regular exercise program in the last 6 months |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2 functional exercises (squats and step-ups), 5 LL isotonic exercises Equipment: velcro ankle weights (isotonic ex only) Intensity: initially low (3-5 on Borg scale), progressed to 8 (“hard” on Borg scale) Frequency: Ex3 Reps/ sets: 12/2 Program duration: 16 weeks Setting: home-based Supervision: low (12 visits over 16 weeks) Adherence: 84% (SD 27) of sessions 2. Control: given nutrition info, 7 home visits over 16 weeks, kept food logs 3/14 days |
|
| Outcomes | Primary: WOMAC pain and physical function subscales, SF-36 Secondary: Strength (1RM), clinical knee exam, nutrition, physical performance (stair climb, chair stand time) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A – Adequate |
Balagopal 2001.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 20 Sample: healthy older people Age: mean 71 years (SD 1) Inclusion criteria: older people aged 65-79, healthy (based on physical exam and blood tests) Exclusion criteria: subjects who exercised regularly for > or = 2 days per week, women taking hormone replacement |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 4UL, 3LL Equipment: resistance training machines Intensity: 50-80% 1RM Frequency: Ex3 Reps/ sets: 8/3 Duration: 3 months Setting: gym Supervision: full Adherence: not reported 2. Control Group: not reported |
|
| Outcomes | Muscle strength (1RM) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Ballor 1996.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 18 Sample: obese, recently completed dietary program Age: mean 61 years (SE 1) Inclusion criteria: aged 55-70 years, a BMI before weight loss of > 32 kg/m squared, no signs, symptoms or history of heart disease, non-diabetic, non-smoker, resting blood pressure <160/90 mm Hg, no symptoms that would preclude safe participation in an exercise program Exclusion criteria: not reported |
|
| Interventions | PRT versus aerobic 1. PRT Type of Ex: 4UL, 3LL Equipment: machines (Universal Gym) Intensity: 50-80% of 1RM Frequency: Ex3 Reps/ sets: 8/3 Program duration: 12 weeks Setting: gym Supervision: full Adherence: not reported 2. Aerobic Training Group: exercised 3 times per week on a motorised treadmill at approximately 50%of maximum aerobic uptake for 20-60 minutes per session |
|
| Outcomes | Strength (1RM) Aerobic capacity Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Barrett 2002.
| Methods | RCT Method of randomisation: a computer generalized list Assessor blinding: yes Participant blinding: yes Loss to follow-up: 4/44 Intention-to-treat analysis: yes for primary, no for secondary measures Post-program follow up: no |
|
| Participants | Location: Australia N = 40 (20 in each group) Sample: healthy elderly Age: mean 66.6 years Inclusion criteria: not reported Exclusion criteria: if participants general practitioners recommended against participation for health reasons or if for any reason they were unable to participate in a class situation |
|
| Interventions | PRT versus control (flexibility training) 1. PRT Type of Ex: 6UL/6LL Equipment: free weights Intensity: based on perceived exertion scale “hard” to “very hard” Frequency: Ex2 Reps/Sets: 8 reps/1 to 2 sets at the first two sessions; then 8 reps/2 to 3 sets Duration: 10 weeks Setting: recreational clubs (Gyms) Supervision: full by two fitness instructors Adherence: not reported 2. Control group (flexibility training): mainly stretch for the major muscle groups and some light cardiovascular exercise, n = 22, mean age = 69.6 years |
|
| Outcomes | Primary: SF-36 Secondary: muscle strength (force-N/weight-N), sit to stand (seconds) Comments on adverse events: yes |
|
| Notes | Data from PRT and flexibility training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Baum 2003.
| Methods | RCT Method of randomisation: a computer generated algorithm stratified by the location of the facility Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 1/11 in PRT group Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: USA N = 20 (11 in PRT) Sample: frail older adults living in long-term care facility Age: mean 88 years Inclusion criteria: age greater than 65, residence at the facility longer than 3 months, and the ability to ambulate alone, with assistive devises or one caregiver Exclusion criteria: unstable acute illness or chronic illness; an inability to follow a two-step command; and assaultive behavior pattern; or unwilling to discontinue any current physical therapy |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5LL Equipment: soft ankle or wrist weights, therabands, weighted ball Intensity: increased every week Frequency: Ex3 Reps/ sets: increased from 5/1 to 10/2 Duration: 1 year (after 6 months the two groups switched program. the results extracted at the end of the first 6 months) Setting: not reported, (Gym in the facility?) Supervision: full by an exercise physiologist Adherence: (80%-Ex group; 56%-control) 2. Control group: did activities such as painting, drawing, or puzzles with an art therapist or social worker,3 times a week |
|
| Outcomes | Primary: FIM, physical performance test Secondary: TUAG, Berg balance scale Comments on adverse events: yes |
|
| Notes | Means and SDs at 12 months were not reported. Portion results at 6 months could be estimated from baseline score and change score. Because of small sample size, the precision is questionable | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Bean 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 1/10 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 21 (11 in PRT) Sample: community dwelling older females (with physical performance limitations??) Age: mean 77.1 years (SD = 5.7) Inclusion criteria: female sex, age of 70 and older, and a score between four and 10ontheShort Physical Performance Battery Exclusion criteria: unstable acute or chronic medical conditions, a score less than 23 on the MMSE, or a neuromusculoskeletal condition interfering with exercise participation |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2UL/4LL with fast concentric phase Equipment: weighted vest Intensity: increased to the next level (increase 2% of the subject's baseline body mass) after 10 reps/3 sets Frequency: Ex3 Reps/Sets: 8/3 Duration: 12 weeks Setting: research center (Gym?) Supervision: full Adherence: 88 to 90 % 2. Control group: slow velocity and low resistance exercise with body or limb weight, 3 times a week |
|
| Outcomes | Primary: Short Physical Performance Battery (including chair rise) Secondary: Muscle strength Comments on adverse events: yes |
|
| Notes | Post mean = baseline + change score; baseline SD was used | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Beneka 2005.
| Methods | RCT with 4 groups: low intensity, medium intensity and high intensity and control group Method of randomisation: not reported, stratified by gender Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: no Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Greece N = 16 for each group (Control, LI, MI, & HI) Sample: healthy but inactive elderly Age: male-mean 70 years; female-mean 67 years Inclusion criteria: inactive prior to the study, no anaemia, hepatic complications, thyroid disorders, and kidney problems Exclusion criteria: hypertension or taking anti-hypertensive medication, didn't pass diagnostic treadmill test, didn't pass physician's screen |
|
| Interventions | PRT (low intensity, medium intensity, and high intensity) versus control 1. PRT Type of Ex: 3 LL Equipment: Universal machines Intensity: LI-50% of 1 RM; MI-70% of 1 RM; HI-90% of 1 RM Frequency: Ex3 Reps/ sets: LI -12 to 14/3 ; MI-8 to 10 /3; HI-4 to 6 /3 Duration: 16 weeks Setting: not reported (Gym?) Supervision: not reported Adherence: not reported 2. Control group: no training |
|
| Outcomes | Muscle strength Comments on adverse events: no |
|
| Notes | Results from males were extracted Comparisons: low intensity versus high intensity, and high intensity versus control |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Bermon 1999.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 1 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: France N = 32 Sample: healthy older people Age: mean 70 years Inclusion criteria: elderly adults, free of cardiorespiratory and neurological diseases, sedentary to moderately active, passed screening procedure including medical history and physical examination Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 1UL, 2LL Equipment: weight machine (Marcy Vertex II) Intensity: (80% of 1RM) Frequency: Ex3 Reps/ sets: 8/3 Program duration: 8 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: asked to maintain customary activities and dietary patterns |
|
| Outcomes | Strength (1RM) Anthropometry Hormones Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B – Unclear |
Boshuizen 2005.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 18 in total (2 in high-guidance group, 10 in medium-guidance group, and 5 in controls, 1 was not mentioned) Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Netherlands N = 46 (24 in high-guidance group; 22 in control) Sample: experiencing difficulty in chair rising Age: mean = 80 years (SD = 6.7) Inclusion criteria: experiencing difficulty in chair rising Exclusion criteria: with a maximum knee-extensor torque of both legs exceeding 25 kg force; self-reported diseases that would be adversely affected by the exercises |
|
| Interventions | PRT Group (high-guidance) versus control 1. PRT Type of Ex : LLs Equipment: elastic bands Intensity: increased to the next level after 8 reps/3sets Frequency: Ex3 Reps/ sets: 8/3 Duration: 10 weeks Setting: welfare centers (Gym?) Supervision: two supervised sessions/week by two physical therapists and one unsupervised home session/week Adherence: 73% at group sessions and 90% at home sessions 2.Control group: no exercise training |
|
| Outcomes | Primary: disability measure (Groningen Activity Restriction Scale) Secondary: muscle strength, timed walk, TUAG, balance test Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Brandon 2000.
| Methods | RCT BUT some changing of groups allowed before intervention began (husband/wives or people sharing rides changed groups) Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 85 Sample: healthy older adults, participants in community activities Age: mean 72 years Inclusion criteria: “community-dwelling older adults”, no symptoms of cardiovascular disease, consent from physician, Exclusion criteria: depression (according to Beck Inventory), MMSE > 19, contraindications on sub maximal aerobic test |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 3LL Equipment: Nautilaus machines Intensity: moderate-high (50-70% of 1RM) Frequency: Ex3 Reps/ sets: 8-12/3 Duration: 4 months Setting: gym-based Supervision: full Adherence: 95% 2. Control Group: no intervention |
|
| Outcomes | Strength (1RM) Physical Performance Test (PPT)-including chair rise performance Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Brandon 2003.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 13/29 in the PRT group; 8/23 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 52 (29 in PRT) Sample: community dwelling, diabetes Age: mean 65.8 years (SD =7.6) Inclusion criteria: not reported Exclusion criteria: elevated blood glucose, depression, altered cognitive function, cardiovascular diseases, strokes, and hypertension |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5LL Equipment: Nautilus machine Intensity: (50%, 60%, and 70% for set 1, 2, and 3 separately) Frequency: Ex3 during the first 6 months, and Ex2 from month 7 to 24 Reps/Sets: 8-12 /3 Duration: 24 months Setting: not reported, (Gym?) Supervision: full Adherence: > 85% 2. Control group: no training |
|
| Outcomes | Muscle strength (1RM/body weight) TUAG 50-foot walk Walk up and down stairs Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Brochu 2002.
| Methods | RCT Method of randomisation: stratified by physical function scores of SF-36 Assessor blinding: no Participant blinding: no Loss to follow-up: 5/30 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 30 (15 in each group) Sample: disabled women with CHD Age: mean 70.5 years (SD = 4) Inclusion criteria: age > 65 years SF-36 physical function < 85 Had definite CHD Exclusion criteria: hospitalization for an acute coronary syndrome within 6 months, very low threshold angina, exercise-test limiting noncardiac comorbility, uncontrolled BP, sternal nonunion after coronary surgery, recent participation in a cardiac rehabilitation program, inflammatory arthritis, and dementia |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5UL, 3LL Equipment: Universal weights and dumbbells Intensity: high (80% of 1RM) Frequency: Ex3 Reps/Sets: 10/2 Duration: 24 weeks Setting: gym Supervision: not reported Adherence: required to be 75% 2. Control Group: 30 to 40 minutes of stretching, calisthenics, light yoga, and deep-breathing progressiverelaxation exercise |
|
| Outcomes | Primary: CS physical performance test, SF-36 Secondary: strength (1 RM), peak V02, 6-minute walk Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Bruunsgaard 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 18 (39 enrolled) Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Demark N = 21 (10 in PRT) Sample: frail nursing home residents Age: mean 88.6 years-PRT, 90.6 years-control Inclusion criteria: not reported Exclusion criteria: acute illness, hypertension, severe cardiovascular disease, moderate/severe cognitiveimpairment, severe impairment of motor function, and neurological disorder |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2 LL Equipment: training chair (Quadriceps Exercise Table) Intensity: 50% to 80% of 1 RM Frequency: Ex3 Reps/Sets: 8/3 Duration: 12 weeks Setting: nursing home facility (Gym?) Supervision: full by a physiotherapist Adherence: 84% for the PRT group, 97% for the control group 2. Control group: social activities, twice a week by an occupational therapist |
|
| Outcomes | Muscle strength (1 RM) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Buchner 1997.
| Methods | RCT: with four groups: strength training alone, endurance training alone, strength and endurance training and control group Method of randomisation: variation of randomly permuted blocks Assessor blinding: yes Participant blinding: no Loss to follow-up: 4 (from PRT/control) Intention to-treat analysis: yes Post-program follow up: exercisers assessed at 9 months, all participants monitored for falls for median 1.42 years (max 2.35 years) |
|
| Participants | Location: USA N = 105 total (55 in PRT vs control) Sample: older people with muscle weakness, recruited from primary care physicians in a HMO Age: mean 75 years Inclusion criteria: between 68 and 85 years of age; unable to do an eight-step tandem gait without errors; below the 50th percentile in knee extensor strength for the subject's height and weight Exclusion criteria: active cardiovascular, pulmonary, vestibular and bone diseases; positive cardiac stress test; body weight >180% of ideal; major psychiatric illness; active metabolic diseases; chronic anemia; amputation; chronic neurological or muscle disease; inability to walk; dependency in eating, dressing transfer or bathing; inability to speak English or fill out written forms |
|
| Interventions | PRT versus control 1. PRT Type of Ex : 2UL, 9LL, 1Tr Equipment: machines (Cybex) Intensity: high (set 1: 50-60% of 1RM; set 2: 75% of 1RM) Frequency: Ex3 Reps/Sets: 10/2 Program Duration: 24-26 weeks Setting: gym Supervision: not reported Adherence: 95% excluding drop-outs; 81% including drop-outs 2. Control Group: maintained usual activity levels, allowed to join exercise program after 6 months |
|
| Outcomes | Aerobic capacity Strength (isokinetic) Balance Gait SF-36 Sickness Impact Profile Lawton IADL scale Stair climbing Falls Health care use Comments on adverse events: yes |
|
| Notes | Data from PRT and control group were compared Data from PRT and aerobic training group were compared |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B – Unclear |
Casaburi 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 1/12-Tx, 1/12-Control Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N=24 (12 for each group) Sample: people with COPD Age: mean 68.9 years (SD=9.8) Inclusion criteria: age 55 to 80 years, FEV1 of 60% predicted or less, and FEV1 to vital capacity ratio of 60% or less. Screening serum testosterone was 400 ng/dl or less Exclusion criteria: significant cardiovascular or orthopedic impairments, body weight of less than 75% or more than 130% of ideal, symptomatic benign prostatic hypertrophy, prostate cancer history, serum prostate specific antigen of more than 4 ?g/L, or hemoglobin of more than 16 ug/dl |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5 LL with eumetabolic diet Equipment: not reported Intensity: first 4 weeks, 60% of 1RM then increased to 80% of 1 RM Frequency: Ex3 Reps/Sets: first 4 weeks, 12/3 then increased to 8-10 /4 Duration: 10 weeks Setting: not reported Supervision: full by an exercise trainer Adherence: at least 25 of 30 scheduled sessions 2. Control Group: no training |
|
| Outcomes | Muscle strength VO2max Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Castaneda 2001.
| Methods | RCT both groups were also on a low-protein diet (run-in period for 6 weeks to evaluate this); comparison was between low-protein diet alone or low-protein diet plus resistance training Method of randomisation: not reported Assessor blinding: blind for all assessments except strength Participant blinding: yes, sham-exercises Loss to follow-up: no Intention-to-treat analysis: not stated Post-program follow up: no |
|
| Participants | Location: USA N = 26 Sample: patients with moderate chronic renal insufficiency, recruited from nephrology clinics Age: mean 65 years (SD 9) Inclusion criteria: older than 50 years of age; serum creatinine concentrations between 133-422 umol/L (1.5 and 5.0 mg/dL); physician approval to follow a low protein diet; nephrologist confirmed diagnosis of chronic renal insufficiency Exclusion criteria: myocardial infarction within the last 6 months; any unstable chronic condition; dementia; alcoholism; dialysis or previous renal; current resistance training; recent involuntary weight change (+/- 2kg); albumin level less than 30g/L; proteinuria greater than 10g/d; abnormal stress test on screening |
|
| Interventions | PRT versus control 1. PRT plus low-protein diet Type of Ex: 2UL, 3LL Equipment: machines (Keiser) Intensity: 80% of 1RM Frequency: Ex3 Reps/Sets: 8/3 Duration: 12 weeks Setting: gym at research centre Supervision: full Adherence: 91% 2. Control Group: on low-protein diet; performed 5-8 sham exercises (gentle movements while standingsitting and bending) for upper and lower body |
|
| Outcomes | Strength (1RM), Peak oxygen consumption Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Castaneda 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: yes Loss to follow-up: 0 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 26 (14 in PRT) Sample: chronic kidney disease but not on dialysis therapy Age: mean 65 years (SD = 9) Inclusion criteria: older than 50 years old with moderately severe chronic kidney disease and not on dialysis therapy, serum creatinine concentrations from 1.5 to 5.0 mg/dL and to be able to take a low protein diet Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex : 2UL/3 LL Equipment: Keiser Sports Health Equipments Intensity: 80% of 1 RM Frequency: Ex3 Reps/Sets: 8/3 Duration: 12 weeks Setting: research center (Gym?) Supervision: full Adherence: not reported 2.Control group: stretching and flexibility exercise |
|
| Outcomes | Muscle strength (1 RM) Comments on adverse events: yes |
|
| Notes | Reported whole body muscle strength (data were not pooled) | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Chandler 1998.
| Methods | RCT Method of randomisation: block randomised and stratified by 2 levels of functioning Assessor blinding: some measures Participant blinding: no Loss to follow-up: 13 Intention-to-treat analysis: no Post-program follow-up: no |
|
| Participants | Location: USA N = 100 Sample: community-dwelling older people with functional limitations Age: mean 77.6 years Inclusion criteria: community-dwelling; aged 64 or above; unable to descend stairs step over step without holding onto the railing Exclusion criteria: > or = 3 on Reuben's Advanced Activities of Daily Living; terminal illness (i.e. not expected to survive 6 months); severe unstable cardiac disease including MI in the past 6 months; severe fixed or progressive neurologic disease; complete blindness; lower extremity amputation; score below 18 on MM SE and unable to follow a 3-step command |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 8LL Equipment: Theraband Intensity: progressively increased (8 RM to 2 sets of 10RM) Frequency: Ex3 Reps/Sets: 10/2 Duration: 10 weeks Setting: home-based Supervision: not reported Adherence: not reported 2. Control Group: could begin exercise after 10 weeks, one friendly phone call at 5 weeks |
|
| Outcomes | HRQoL (SF-36) Lower limb strength (Cybex) 6-minute walk test Chair rise Functional reach Falls Self-Efficacy (/100) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B- Unclear |
Charette 1991.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding : no Loss to follow-up: 8 Intention-to-treat analysis: no Post-program follow-up: no |
|
| Participants | Location: USA N = 27 Sample: healthy, sedentary women Age: mean 69 years Inclusion criteria: aged 64-86; healthy; female, Palo Alto community Exclusion criteria: pre-existing disability or illness that would preclude participation in a weight training program of moderate intensity |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 7LL Equipment: weight training machines Intensity: 65-75% of 1RM Frequency: Ex3 Reps/Sets: 6/3, increased to 6 sets for leg extension and press after 2 weeks Program Duration: 12 weeks Setting: gym Supervision: full Adherence: 90% completed all sessions 2. Control Group: maintain normal activities, asked not to start an exercise program. Could undertaketraining at the end of the program. Contacted to make appointments/ maintain interest |
|
| Outcomes | Strength (1RM) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Chin A Paw 2006.
| Methods | RCT with 4 groups: PRT, control, functional training, and combined training Method of randomisation: the random allocation sequence was generated by computer by two independent students Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 21/57 in PRT; 22/60 in function-skills; 17/56 in combined training; 23/51 in controls Intention-to-treat analysis: yes. Data analysed: 40 in PRT, 44 in function-skills, 44 in combined training, 31 in controls Post-program follow up: no |
|
| Participants | Location: Netherlands N = 108 (57 in PRT) Sample: elders lived in long-term care facilities Age: mean 81.3 (SD = 4.4) Inclusion criteria: 1) aged 65 or older; 2) living in a nursing home or residential care facility; 3) able to walk 6 m or more (with or without a walking aid); 4) able to comprehend the study procedures; 5) no medical contraindication for study participation; 6) no rapidly progressive or terminal illness; 7) and not moving away from the home within the 6-months intervention period Exclusion criteria: not reported |
|
| Interventions | PRT versus control, versus functional training, and versus combined training 1. PRT Type of Ex: 3UL/2LL Equipment: TechnoGym equipment, dump bells and ankle/wrist weights Intensity: high (60-80% of 1 RM) Frequency: Ex2 Reps/Sets: 8-12/2 Duration: 24 weeks Setting: long-term care facility (Gym?) Supervision: full by a physical therapist and an assistant Adherence: 78 % 2.Control group: mean age =81, educational program (group discussion about topics of interest) 3. Functional training group: N=60, mean age = 82 years, game-like or cooperative activities 4. Combined training group: N=56, mean age = 81 years, one strength training and one functional trainingper week |
|
| Outcomes | Primary: physical activities/ADL disability Secondary: muscle strength, vitality plus scales, balance, gait speed, chair rise Comments on adverse events: yes |
|
| Notes | Comparisons: PRT versus control, PRT versus functional training | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Collier 1997.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 1 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 39 Sample: healthy, community-dwelling Age: range 65-85 years Inclusion criteria: aged 65-85, approval of physician, community residents Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5UL, 2LL Equipment: Universal Hercules Gym Machine Intensity: not specified, but progressed throughout Frequency: Ex3 Reps/Sets: 10/2 Program Duration: 10 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: no active intervention |
|
| Outcomes | Strength (number of reps at % of body weight) Functional Fitness Assessment for adults >60 Agility Assessment (walking between cones) Hand-eye co-ordination (“soda pop” test) Grip strength Physical Self-Efficacy Scale (PSE) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B – Unclear |
Damush 1999.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no, attention control group used Loss to follow-up: 9 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 71 Sample: community-dwelling women, recruited through media-based promotion Age: mean 68 years (SD 5.6) Inclusion criteria: age 55+, living in retirement residential community, clearance from GP Exclusion criteria: GP-identified contraindications to exercise |
|
| Interventions | PRT versus control 1.PRT Type of Ex: 4UL, 3LL Equipment: Theraband Intensity: low to moderate (4/10 on Borg scale) Frequency: Ex3 Reps/Sets: 1 set, as many reps to reach 4/10 on Borg Program Duration: 8 weeks Setting: gym, group-based Supervision: full Adherence: 88% 2. Control Group: attended all of the exercise sessions to allow social contact |
|
| Outcomes | HRQoL (SF-36) Strength (3RM) Grip strength Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B – Unclear |
de Vos 2005.
| Methods | RCT with 4 groups: high intensity, medium intensity, and low intensity, and control Method of randomisation: computerized randomisation program, stratified by gender Assessor blinding: only for tests at baseline Participant blinding: blinded to the research hypothesis Loss to follow-up: 12 (4-high intensity, 3-medium intensity, 3-low intensity, 2-control) Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Australia N = 28-HI; N = 28-MI; N = 28-LI; N = 28-control Sample: independent living older adults Age: mean 69 years Inclusion criteria: > 60 years old, living independently in the community, willingness to be randomized and to commit to the study requirements Exclusion criteria: participation in resistance/power training in the last 6 months, acute or terminal illness, had myocardial infarction in the past 6 months, unstable disease or physical status would interfere with exercise, limb amputation/fraction in the past 3 months, currently symptomatic hernias or hemorrhoids, or cognitive impairment |
|
| Interventions | PRT (high intensity, medium intensity, and low intensity) versus control 1. PRT Type of Ex: rapid concentric and slow eccentric Equipment: Keiser machines Intensity: high (80% of 1RM), medium (50% of 1 RM), low (20% of 1RM) Frequency: Ex2 Reps/Sets: 8/3 Duration: 8-12 weeks (M = 10 weeks) Setting: not reported Supervision: Experienced exercise trainers Adherence: > 90% for each training group 2. Control Group: maintain current level of activities |
|
| Outcomes | Dynamic muscle strength Muscle power Muscle endurance Balance Comments on adverse events: yes |
|
| Notes | Involved power training | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
de Vreede 2007.
| Methods | RCT with 3 groups: PRT, control, and functional task exercise group Method of randomisation: by computer using a random numbers table Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 6/34 in PRT group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Netherlands N = 65 (34 in PRT) Sample: community-dwelling older adults Age: mean 74.8 years (SD = 4) Inclusion Criteria: age over 70 years Exclusion Criteria: recent fractures, unstable cardiovascular or metabolic disease, musculoskeletal condition or chronic illness, severe airflow obstruction, recent depression or emotional distress, loss of mobility for more than one week in the previous months, exercised at a sports club more than 3 times a week |
|
| Interventions | PRT versus control and versus functional task exercise 1. PRT Type of Ex: 5UL, 9LL Equipment: weights, elastic tub Intensity: 7-8 on a 10-point rated perceived exertion scale Frequency: Ex3 Reps/Sets: 10/3 Duration: 12 weeks Setting: a local leisure center Supervision: at least two experienced instructors Adherence: 74% (SD = 34.6%) 2. Control Group: to keep normal activity level 3. Functional task exercise group: N = 33, moving with a vertical component, moving with a horizontal component, carrying an object, and changing position between lying, sitting, and standing. Practice phase for 2 weeks, variation phase for 4 weeks, and daily tasks for 6 weeks |
|
| Outcomes | Primary: SF-36 Secondary: TUAG Comments on adverse events: yes |
|
| Notes | Data of SF-36 were provided by the trial authors Data from PRT and functional training group were compared |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
DeBeliso 2005.
| Methods | RCT Method of randomisation: not reported-stratified by gender and strength Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 8/21 in control; 5/18 in fixed repetition group; 4/21 in periodised group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 18-fixed repetition; N = 21-periodised repetition; N = 21-control Sample: independent and community dwelling older adults Age: fixed repetition, mean 71.4 years (SD = 5.4); periodised, mean = 70.6 years (SD = 4.7) Inclusion Criteria: no previous background in resistance training Exclusion Criteria: not reported |
|
| Interventions | PRT (fixed repetition and periodised repetition) versus control 1. PRT Type of Ex: 5UL/3LL Equipment: Flex machines Intensity: fixed repetition-9 RM; periodised-week 1 to 6, 15 RM; week 7 to 12, 9 RM; week 13 to 18, 6 RM Frequency: Ex2 Reps/Sets: fixed repetition-9/3; periodised-week 1 to 6, 15/2; week 7 to 12, 9/3; week 13 to 18, 6/4 Duration: 18 weeks Setting: training facility (Gym?) Supervision: full by trainers Adherence: fixed repetition group 77%; periodised group 62% 2. Control group: maintain current recreational activities |
|
| Outcomes | Muscle strength (1 RM) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
DiFrancisco 2007.
| Methods | RCT Method of randomisation: a table of random numbers Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 9 for each group Sample: see below Age: mean = 77.3 years (SD = 0.7) Inclusion criteria: convenience sample from Academic Health Care Center Exclusion criteria: participated in a strength-training programme within 6 months, pre-existing orthopaedic complications that would have affected any of the exercise, cardiac and respiratory conditions |
|
| Interventions | PRT (once a week versus twice a week) Type of Ex: 3UL/ 3LL Equipment: Cybex machines Intensity: high (75% of 1RM) Frequency: Ex2 versus Ex1 Reps/Sets: 10-15 /1 for each exercise Duration: 9 weeks Setting: gym Supervision: not reported Adherence: not reported |
|
| Outcomes | Strength (1RM) Comments on adverse events: yes |
|
| Notes | Date from 2 times a week and one time a week were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Donald 2000.
| Methods | RCT, factorial design (comparison of floor surface types not included here) Method of randomisation: randomised envelopes Assessor blinding: no Participant blinding: no Loss to follow-up: 22 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: UK N = 58 Sample: hospitalised older people Age: mean 81 years Inclusion criteria: admitted to elderly care rehabilitation ward from Feb to Sept 1996, consent from patient and carers Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2 LL Equipment: not reported Intensity: high (maximum weight the patient could manage) Frequency: twice daily Reps/Sets: 10/3 Program duration: not reported (length of hospital stay) Setting: hospital Supervision: full Adherence: not reported 2. Control Group: regular in-hospital daily physiotherapy |
|
| Outcomes | Falls (during hospital stay) Barthel Index (ADL measure) Strength (hand-held dynamometer, hand-grip strength) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Earles 2001.
| Methods | RCT, PRT vs moderate aerobic exercise Method of randomisation: randomised, with subjects blocked for gender and residence Assessor blinding: no Participant blinding: no Loss to Follow-up: 3 Intention-to-treat analyses: no Post-program follow up: no |
|
| Participants | Location: USA N = 43 Sample: independent community volunteers Age: mean 77 years (SD 5) in PRT group Inclusion criteria: age greater than 70 years; score of 8 or higher on the Short Physical Performance Battery; ability to travel (by using public or private transportation) to the retirement community where exercise sessions were held; willingness to attend exercise sessions for 12 weeks Exclusion criteria: myocardial infarction in the past 6 months; heart failure (New York Heart Association classification <1); angina with moderate activity; chronic obstructive pulmonary disease or shortness of breath while walking at a normal pace; stroke with residual motor deficits; poorly controlled hypertension (>174mmHg systolic, >100mmHg diastolic); cancer with chemotherapy or radiation in the past year; physical performance limited by arthritis; on any of the following medications: neuroleptics, oral steroids, testosterone or growth hormones |
|
| Interventions | PRT versus aerobic 1. PRT Type of Ex: 2 LL; also did step-ups, chair rises and plantar flexion exercises in standing Equipment: Pneumatic resistance machines Intensity: high for leg press- started at 50% of 1RM, increased by 10% during each week of training; moderate for other exercises Frequency: Ex3 Reps/Sets: 10/3 Duration: 12 weeks Setting: gym at retirement center Supervision: full Adherence: 90% 2. Aerobic training group: moderate intensity exercise 30 minutes daily, 6 days weekly |
|
| Outcomes | Short physical performance battery (SPPB) Balance (semi-tandem stance, single leg stance) Chair rise (5) 8-foot walk Aerobic capacity (6-minute walk) Muscle strength Comments on adverse events: yes |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B- Unclear |
Ettinger 1997.
| Methods | RCT with 3 groups: PRT, aerobic training and health education (attention control) Method of randomisation: stratified, variable block randomisation, computer generated Assessor blinding: yes Participant blinding: attention control group used Loss to follow-up: 75 total (48 from PRT and control group) at 18 months Intention-to-treat analysis: yes Post-program follow up: participants followed after initial supervised sessions (3 months) to home-based sessions (3-18 months) |
|
| Participants | Location: USA N = 439 total (295 in PRT versus control) Sample: community-dwelling people with osteoarthritis resulting in functional limitation Age: mean 68 years (SD 6) in PRT group Inclusion criteria: age 60 years or more, pain on most days in 1 or more knees, difficulty with at least 1 of the following due to knee pain: walking a quarter mile, climbing stairs, getting in and out of a car, lifting and carrying groceries, getting out of bed, getting out of the bathtub or performing shopping, cleaning or self-care activities; radiographic evidence of knee osteoarthritis in the tibial-femoral compartment. Exclusion criteria: person has a medical condition that precluded safe participation in the exercise program or prevented completion of the study (myocardial infarction or stroke in the past 3 months, evidence of ischemia during the exercise treadmill test, congestive heart failure, severe chronic obstructive pulmonary disease, active treatment for cancer, insulin dependent diabetes mellitus, hemoglobin less than 110g/L, creatinine greater than 176.8 umol/L, severe systemic disease or major psychiatric disease), inflammatory arthritis (i.e., rheumatoid or psoriatic), exercised regularly (defined as aerobic activity or resistance training more than 1 time per week for 20 minutes or longer), planned to move from the area or be admitted to a long-term care facility in the next 2 years; unable to walk at least 420 feet in 6 minutes without a cane or assistive device; unable to walk on a treadmill without an assistive device; participating in another research study; resided in a long-term care facility |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 4UL, 4LL, 1Tr Equipment: cuff-weights, dumb bells Intensity: moderate to high (2 sets of 12 reps max) Frequency: Ex3 Reps/Sets: 12/2 Duration: 78 weeks Setting: facility-based group for 3 months, then home- based for 15 months Supervision: high for gym-based, telephone contact and visits during home based phase (diminishing contact over time) Adherence: 70% at 18 months 2. Control Group: health education program (meetings and telephone contact) 3. Aerobic Training Group: walking program for 40 minutes 3 times per week at 50-70% of HR reservegroup facility based for 3 months then home-based for 15 months (same contact as PRT) |
|
| Outcomes | Primary: self-report physical disability (23 item scale developed for use in this trial) Secondary: 6 minute walk test, stair climbing, lifting object, timed task in and out of car, graded sub maximal aerobic treadmill test, strength (isokinetic dynamometer), knee x-rays, knee pain Comments on adverse events: yes |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Fahlman 2002.
| Methods | RCT with 3 groups: PRT, control, and aerobic group Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: N/A Post-program follow-up: no |
|
| Participants | Location: USA N = 30 (15 in each group) Sample: highly active and functioning women Age: mean 73 years (SD = 3) Inclusion criteria: not reported Exclusion criteria: dementia screened by MMSE, did not meet the criteria of the American College of Sports Medicine, the presence of activity-limiting arthritis; being bedridden within 3 months of the study; the presence of central or peripheral nervous system disorders, stroke, acute or chronic infection, major affective disorder, human immunodeficiency virus infection or autoimmune disorders, or metabolic disorders (type I diabetes mellitus); being a smoker or smokeless tobacco user; participating in regular aerobic or resistance training within the previous 3 months; using oral steroids or medications known to have an effect on blood lipids except hormone replacement therapy; having surgery within the previous 3 months; and consuming caffeine in excess of the equivalent of 4 cups of coffee per day |
|
| Interventions | PRT versus control and aerobic 1. PRT Type of Ex: 7 LL Equipment: not reported Intensity: 8RM Frequency: Ex3 Reps/Sets: 8/3 Duration: 10 weeks Setting: not reported Supervision: not reported Adherence: > 95 % 2. Control Group: maintain normal activity level 3. Aerobic training group: stretching and walking exercise at 70% heart rate reserve, duration increasedfrom 20 minutes to 30 minutes through out the program |
|
| Outcomes | Muscle strength (1RM) 1-minet walk (no data available for the PRT group) VO2 max Comments on adverse events: no |
|
| Notes | Comparisions: PRT versus control, and PRT versus aerobic | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Fatouros 2002.
| Methods | RCT with 3 groups: PRT, control, and aerobic group Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: no Post-program follow-up: no |
|
| Participants | Location: Greece N = 8 in each group Sample: inactive elder men Age: mean 71.8 years (SD = 2.5) Inclusion criteria: completely inactive prior to the study, VO2 max below 25 ml/kg/min, no anemia, hepatic complications, thyroid disorders or kidney problems, normal blood pressure Exclusion criteria: respiratory complications or BP > 240/110 mmHg during the exercise test |
|
| Interventions | PRT versus control and versus aerobic (cardiovascular training) 1. PRT Type of Ex: 5 UL/3 LL Equipment: Universal resistance exercise machines Intensity: Week 1-4 (55%-60% of 1 RM); Week 5-8 (60%-70% of 1 RM); week 9-12 (70%-80% of 1 RM); week 13-16 (80% of 1 RM) Frequency: Ex3 Reps/Sets: Week 1-4 (12-14/2); Week 5-8 (10-12/3); week 9-12 (8-10/3); week 13-16 (8/3) Duration: 16 weeks Setting: not reported Supervision: not reported Adherence: required the participants not miss more than 4 training sessions, 2. Control Group: no exercise 3. Cardiovascular training group: walking, jogging on a treadmill, the intensity was increased through out the training |
|
| Outcomes | Muscle strength (1 RM) Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Fatouros 2005.
| Methods | RCT with 3 groups: high intensity PRT, low intensity PRT, and control Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: not reported Intention-to-treat analysis: N/A Post-program follow-up: yes |
|
| Participants | Location: Greece N = 18 (LI); N = 20 (HI); N = 14 (control) Sample: inactive older adults Age: HI-mean 72.4 years (SD = 3.5); LI-mean 70.3 years (SD = 4.4) Inclusion criteria: at least 65 years of age, inactive before the study, free from health problems and potentially damaging orthopedic, neuromuscular, metabolic, and cardiovascular limitations Exclusion criteria: not reported |
|
| Interventions | PRT (high intensity and low intensity) versus control 1. PRT Type of Ex: 5 UL/3LL Equipment: Universal machines Intensity: low- 55% of 1RM; high- 82% of 1RM Frequency: Ex3 Reps/Sets: low intensity: 14-16/2 (after week 8, 3 sets), high intensity: 6-8 /2 (after week 8, 3 sets) Duration: 24 weeks Setting: not reported Supervision: Full Adherence: 98% 2. Control Group: not reported |
|
| Outcomes | Muscle strength VO2max TUAG Step climbing 50-feet walk Comments on adverse comments: yes |
|
| Notes | Data from high intensity and low intensity PRT group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Fiatarone 1994.
| Methods | RCT, factorial design (comparison of nutritional supplements versus placebo not considered here) Method of randomisation: not reported Assessor blinding: for some assessments, not for all Participant blinding: no, but recreational activities offered to control group (? quantity) Loss to follow-up: 6 total (4 in PRT and control groups) Intention-to-treat analysis: yes Post-program follow up: falls monitored median 1.53 years, max 4.11 years |
|
| Participants | Location: USA N = 51 in PRT vs control Sample: residents of a long term care facility for older people Age: mean 87.1 years (SE 0.6) Inclusion criteria: residential status, age over 70 years, ability to walk 6m Exclusion criteria: severe cognitive impairment; rapidly progressive or terminal illness, acute illness or unstable chronic illness; myocardial infarction; fracture of a lower extremity within the six months before the study; insulin dependent diabetes mellitus; on a weight-loss diet or undergoing resistance training at the time of enrolment; tests of muscle strength revealed a musculoskeletal or cardiovascular abnormality |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2LL Equipment: weight training machines Intensity: high (80% of 1RM) Frequency: Ex3 Reps/sets: 8/3 Program duration: 10 weeks Setting: nursing home Supervision: full Adherence: 97% 2. Control Group: engaged in 3 activities of their choice offered by recreational therapy |
|
| Outcomes | Strength (1RM) Gait speed Stair climbing power Anthropometric measurements Physical activity (leg monitors) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Fiatarone 1997.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no, but control group received weekly phone calls Loss to follow-up: 4 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 34 Sample: frail older people Age: mean 82 years Inclusion criteria: community dwelling older people, moderate to severe functional impairment Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 11 total to UL and LL Equipment: arm and leg weights Intensity: high Frequency: Ex3 Reps/Sets: not reported Program Duration: 16 weeks Setting: home-based Supervision: low - 2 weeks of home instruction, then phone calls Adherence: 90% 2. Control Group: weekly phone calls |
|
| Outcomes | Strength Gait velocity Self-reported activity level Attitude towards Ageing on the PGC Morale Scale Bed days Falls Health care visits Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Fielding 2002.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 3/15 in high velocity group, 2/15 in low velocity group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 30 (15 in high velocity, 15 in low velocity) Sample: community dwelling elderly with self reported disability Age: high velocity-mean 73.2 years (SD = 1.2); low velocity-mean 72.1 years (SD = 1.3) Inclusion criteria: at least of 65 years of age, community dwelling, could walk with or without an assistive device, reported 2 or more deficits on the physical function subscale of SF-36 Exclusion criteria: acute or terminal illness, myocardial infarction in the past 6 months, unstable cardiovascular disease or other medical condition, upper extremities or lower extremities fractures in the past 6 months, amputations, cognitive impairments, current participations in regular exercise sessions, and unwilling to be randomised |
|
| Interventions | PRT (high velocity versus low velocity) Type of Ex: 2LL, leg press & knee extension Equipment: machines (Keiser pneumatic resistance training equipment) Intensity: high velocity group-70% of 1 RM, extension as fast as possible during concentric phase, then maintain full extension for 1 second, and eccentric phase of each repetition over 2 seconds; low velocity group- extension concentric phase, maintain full extension, and eccentric phase of each repetition 2, 1, 2 seconds Frequency: Ex3 Reps/Sets: 8/3 Duration: 16 weeks Setting: human physiology lab Supervision: exercise trainers Adherence: 95% for high velocity group, 94% for low velocity group |
|
| Outcomes | Muscle strength Chair rise Stair climbing Comments on adverse events: yes |
|
| Notes | No reported results can be pooled (missing M and SD for each group) | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Flynn 1999.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 29 Sample: healthy older women Age: mean 73 years Inclusion criteria: older community-dwelling women Exclusion criteria: dementia, exclusion criteria of the American College of Sports Medicine, arthritis, bedridden within 3 months of the study, central or peripheral nervous system disorders, stroke, use of antidepressant medications, acute or chronic infection, major affective disorder, human immunodeficiency virus infection or autoimmune disorders, metabolic disorders (type I diabetes mellitus), oral steroid use, cigarette or smokeless tobacco use, regular aerobic or resistance training within previous 3 months, surgery within the previous 3 months, caffeine consumption in excess of four cups of coffee per day, adequate flexibility and mobility (screened with performance tests) |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 8 LLEquipment: not reportedIntensity: high (70-80% of 1RM) Frequency: Ex3 Reps/sets: 8/3 Duration: 10 weeks Setting: gym Supervision: not reported Adherence: not reported 2. Control Group: asked to maintain their normal activity level |
|
| Outcomes | Strength (1RM - ? data collected for controls) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Foley 2003.
| Methods | RCT Method of randomisation: a computer generated randomisation list generated by person external to the study as was managed by an external department Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 3/35 in the gym group, 3/35 in the control group Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: Australia N = 70 (35 in each group) Sample: community living adults with OA of the hip or knee Age: mean 69.8 years (SD = 9.2) Inclusion criteria: read, write, and speak English, could give informed consent, and provide transport to attend the training sessions Exclusion criteria: had received physiotherapy or hydrotherapy in the past 6 weeks, attending community exercise classes; joint replacement surgery within the past 12 months or the next 12 weeks; and cognitive impairment |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 1UE/4 LL Equipment: weighted gaiters Intensity: 10 RM Frequency: Ex3 Reps/Sets: not reported Duration: 6 weeks Setting: gym Supervision: not reported Adherence: 75 % 2. Control Group: telephone calls to record any changes in their condition drug use or injuries |
|
| Outcomes | Primary: SF-12, Adelaide Activities profile, WOMAC Secondary: muscle strength, Arthritis Self-Efficacy Questionnaire Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Frontera 2003.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: N/A Post-program follow up: no |
|
| Participants | Location: USA N = 14 (7 in each group) Sample: community-dwelling healthy women Age: mean 73.7 years (SD = 3.4) Inclusion criteria: not involved in regular exercise Exclusion criteria: had conditions that could interfere with neuromuscular function |
|
| Interventions | PRT versus control 1. PRT Type of Ex: knee extensors/flexors, each leg was trained separately Equipment: Keiser Sports Health Equipment Intensity: (80% of 1 RM) Frequency: Ex3 Reps/Sets: 8/4 Duration: 12 weeks Setting: not reported Supervision: not reported Adherence: 98% 2. Control Group: not reported |
|
| Outcomes | Muscle strength (1RM, isokinetic strength of knee extension) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Items | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Galvao 2005.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 4/16 in 1-set PRT group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Australia N = 16 for each group Sample: community dwelling elderly Age: 1-set PRT group-mean 68.9 years (SD=4.8); 3-set PRT group-mean 69.7 years (SD=4.4) Inclusion criteria: not reported Exclusion criteria: musculoskeletal, cardiovascular, or neurological disorder; PRT in the previous 12 months, inability to undertake upper and lower limb ex. or walk less than 100 meters; unwilling to undertake 20 weeks of training |
|
| Interventions | PRT (3-set versus 1-set) Type of Ex: 4UL/3LL Equipment: Strength Fitness Equipment Intensity: 8 RM Frequency: Ex2 Reps/Sets: 8/3 versus 8/1 Duration: 20 weeks Setting: not reported (Gym?) Supervision: full Adherence: All completed 40 training sessions (make-up sessions were provided) |
|
| Outcomes | Muscle strength (1 RM) Chair rise 6-minute walk Stair climbing 400-m-walk Comments on adverse events: yes |
|
| Notes | 3-set PRT versus 1-set PRT | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Hagerman 2000.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 4 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 22 Sample: untrained but physically active older men Age: mean 63.7 years Inclusion criteria: male, aged 60-75, physically active but not engaged in resistance training Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 3 LL Equipment: machines Intensity: high (85-90% of 1RM) Frequency: Ex2 Reps/Sets: 6-8/3 Program Duration: 16 weeks Setting: gym Supervision: full Adherence: 100% 2. Control Group: not reported |
|
| Outcomes | Strength (1RM) Peak aerobic capacity Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Harris 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 2/19 in LI (2 sets of 15 RM); 1/18 in HI (4 sets of 6 RM) Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N: HI = 18; LI = 19 Sample: independent community dwelling older adults Age: HI- mean =69.4 years (SD = 4.4); LI- mean =71.4 years (SD = 4.6) Inclusion criteria: independent and community dwelling; no previous background in resistance training Exclusion criteria: not reported |
|
| Interventions | PRT (high intensity versus low intensity) Type of Ex : 3LL/5UL Equipment: Flex machines Intensity: HI-6RM; LI-15RM Frequency: Ex2 Reps/Sets:HI-6 /4; LI-15 /2 Duration: 18 weeks Setting: not reported (Gym?) Supervision: full by trainers Adherence: 85.4% |
|
| Outcomes | Muscle strength Comments on adverse events: yes |
|
| Notes | No numerical results for the control group Date from high intensity PRT and low intensity PRT were compared |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Haykowsky 2000.
| Methods | RCT Method of randomisation: matched according to combined leg press and bench press strength scores, then randomly assigned Assessor blinding: no Participant blinding: no Loss to follow-up: 4 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Canada N = 22 Sample: healthy older men Age: mean 68 years (SD 3) Inclusion criteria: aged 61 -76; no clinical evidence of cardiovascular disease or hypertension; normal resting electrocardiograms; normal electrocardiographic response to graded treadmill exercise; not requiring or using cardiovascular medications; no regular participation in endurance or RT; absence of cerebrovascular or orthopaedic disability that would limit RT Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5UL, 3LL Equipment: machines Intensity: 60-80% of 1RM Frequency: Ex3 Reps/Sets: 3/10 Duration: 16 weeks Setting: gym Supervision: not reported Adherence: 97% attended 2. Control Group: continued normal activities |
|
| Outcomes | Strength (1RM) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Haykowsky 2005.
| Methods | RCT with 3 groups: PRT, control, and aerobic group Method of randomisation: not reported Assessor blinding: not reported Participant blinding: yes for echocadiograms Loss to follow-up: no Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Canada N = ? (did not report sample size for each group) Sample: women Age: mean = 70 years (SD = 4) Inclusion criteria: a) no clinical evidence of cardiovascular disease; b) normal resting electrocardiogram (ECG); c) normal ECG response to graded exercise; d) no requirement or use of cardiovascular medications; e) no regular participation in AT and/or ST; and f) absence of any cerebrovascular or orthopedic disability that would limit exercise training. Exclusion criteria: not reported |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 3LL/5UL Equipment: not reported Intensity: 50% of 1RM and increased 2.5% per week until 75% of 1 RM Frequency: Ex3 Reps/Sets: 10/2 Duration: 12 weeks Setting: not reported (Gym?) Supervision: full Adherence: not reported 2. Control group: continue normal daily activities 3. Aerobic training: cycle exercise at 60-80% of heart rate reserve |
|
| Outcomes | Muscle strength Absolute VO2peak Comments on adverse events: yes |
|
| Notes | sample size for each group was not reported. 12 weeks of strength training is as effective as 12 weeks of aerobic training for increasing relative VO2peak, however, strength training is more effective than aerobic training for improving overall muscle strength |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Hennessey 2001.
| Methods | RCT trial with 4 groups: PRT alone, growth hormone treatment alone, PRT and growth hormone treatment and control. Only PRT alone and control are included in this review Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 16 in PRT and control Sample: frail older people Age: mean 71.3 years (SD 4.5) Inclusion criteria: frail which was defined as scoring between 12 and 28 on Reuben's Physical Performance Test; Exclusion criteria: medical conditions (cancer, heart disease, diabetes, recent fracture, carpal tunnel syndrome) that would interfere with administration of growth hormone or the performance of regular exercise 3 times per week; did not expect to spend a year in Rhode Island; their doctor convinced them not to participate for medical reasons or otherwise; unwilling to inject the drug and be randomised to exercise or no exercise |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 11 exercises (UL & LL) Equipment: ankle and wrist weights and exercise equipment Intensity: increased from 20% to 95% of 1 RM-most training was at high intensity Frequency: Ex3 Reps/Sets: 8/3 Duration: 25 weeks Setting: gym (in study facilities or local community centers) Supervision: Full Adherence: not reported 2. Control Group: not reported |
|
| Outcomes | Strength (isokinetic dynamometry) Physical Performance Test (PPT) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Hepple 1997.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to Follow-up: 1 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Canada N = 20 Sample: healthy older men, recruited through newspaper advertisement Age: mean 68.3 years (se 1.1) Inclusion criteria: male, aged 65-74 Exclusion criteria: positive Physical Activity Readiness Questionnaire, abnormal ECG or blood pressure response, musculoskeletal impairment |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 5LL Equipment: cuff weights Intensity: high (6RM) Frequency: Ex3 Reps/Sets: 6/3 Duration: 12 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: usual level of activity 3. Aerobic Training Group: intermittent walking on treadmill until pain subsided, 3 times per week |
|
| Outcomes | Peak VO2 Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Hiatt 1994.
| Methods | RCT with 3 groups: PRT, walking (aerobic training) and control Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 2 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 29 (19 in PRT versus control) Sample: people who have peripheral arterial disease and intermittent claudication Age: mean 67 years Inclusion criteria: intermittent claudication (disabling but stable for 3 months prior to enrolment); peripheral arterial disease Exclusion criteria: leg pain at rest, ischemic ulceration, gangrene, unable to walk on the treadmill at a speed of at least 2mph; exercise capacity limited by symptoms of angina, congestive heart failure, chronic obstructive pulmonary disease, arthritis; diabetes; vascular surgery or angioplasty in the past year |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 5LL Equipment: cuff weights Intensity: high (6RM) Frequency: Ex3 Reps/Sets: 6/3 Duration: 12 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: usual level of activity 3. Aerobic Training Group: intermittent walking on treadmill until pain subsided, 3 times per week |
|
| Outcomes | Strength (Cybex dynamometer) Peak Vo2 Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Hortobagyi 2001.
| Methods | RCT with 3 groups: High-intensity PRT, Low-intensity PRT and Control Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 3 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 30 total (20 in high-intensity PRT versus control) Sample: healthy older people Age: mean 72 years (SD 4.7) Inclusion criteria: older men and women, healthy, had not exercised more than once a week in the previous 3 years, approval of GP Exclusion criteria: more than two risk factors for coronary artery disease; a history of falls, osteoporosis, osteoarthritis, or orthopaedic or neurological conditions (i.e. stroke); took medications that cause dizziness or slow movement; smoked; had a BMI greater than 28 kg/m squared; blood pressure greater than 140/90 mmHg or a heart condition |
|
| Interventions | PRT (high intensity and low intensity) versus control 1. PRT Type of Ex: 1 LL Equipment: machine Intensity: HI - 80% 1RM; LI - 40% 1RM Frequency: Ex3 Reps/Sets: HI: 4-6/5; LI: 8-12/5 Duration: 10 weeks Setting: gym Supervision: not reported Adherence: 98% 2. Control Group: not reported |
|
| Outcomes | Force accuracy and steadiness Maximal strength (Cybex) Comments on adverse events: no (not identified as such) |
|
| Notes | Date from high intensity PRT and low intensity PRT were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Hruda 2003.
| Methods | RCT Method of randomisation: in a lottery format, 2:1 ratio Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 2/20 in PRT group, 3/10 in control group Intention-to-treat analysis: no Program-post follow up: no |
|
| Participants | Location: Canada N = 30 (20 in PRT) Sample: frail older adults (residents of a long-term care facility) Age: mean 84.9 years (SD = 4.8) Inclusion criteria: able to follow directions and walk across the room; no recent history of cardiovascular, cerebrovascular, respiratory, systemic, muscular, or uncontrolled metabolic disease Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex : LLs Equipment: Therabands Intensity: Increasing repetitions, sets, and speed, 20 minutes class progressed to an hour Frequency: Ex3 Reps/Sets: 4-8/1 Duration: 10 weeks Setting: long-term care facility Supervision: not reported Adherence: 71% 2. Control Group: maintain usual daily activities |
|
| Outcomes | TUAG Chair stand 6-meter walk Muscle strength Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Hunter 2001.
| Methods | RCT with people randomised to variable intensity resistance training and high-intensity resistance training NOTE: control group participants were not randomly assigned, and are not included in this review Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 2 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 28 Sample: healthy male and female volunteers over 60 Age: mean 67.4 years in high intensity group Inclusion criteria: normal body mass index, free of metabolic disorders or medications that might affect energy expenditure, non-smokers, stable weight Exclusion criteria: not reported |
|
| Interventions | PRT (high versus variable resistance) versus control 1. PRT Type of Ex: 5 UL, 2LL, 2 Tr Equipment: resistance training machines Intensity: high intensity group: 80% of 1RM; variable resistance group: 50%, 65%, 80% of 1RM across the 3 training days each week Frequency: Ex3 Reps/Sets: 10/2 Duration: 25 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: not randomly assigned, not included in this review |
|
| Outcomes | Strength (1RM and isometric) Perceived exertion and HR during daily tasks Submaximal aerobic capacity Comments on adverse events: no |
|
| Notes | Date from high intensity PRT and variable intensity PRT were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Izquierdo 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: N/A Post-program follow-up: no |
|
| Participants | Location: Spain N = 10 in PRT, N = 11 in endurance training Sample: healthy men Age: mean 64.8 years (SD = 2.6) Inclusion criteria: had not participated in regular resistance/endurance training or competitive sports for the last 5 years Exclusion criteria: cardiovascular, neuromuscular, arthritic, pulmonary, other debilitating diseases |
|
| Interventions | PRT versus endurance training (aerobic) 1. PRT Type of Ex: 4LL/3UL Equipment: resistance machines (Technogym) Intensity: first 8 weeks, 50-70% of 1 RM; last 8 weeks, 70-80% of 1RM Frequency: Ex2 Reps/Sets: first 8 weeks: 10-15/3; last 8 weeks: 5-6/3-5 Duration: 16 weeks + 4 weeks for baseline testing Setting: training facility Supervision: full by researchers Adherence: at least 90% to be considered compliant and remain in the study 2. Endurance training group: mean age =68.2 years, endurance cycling at 60 rpm, the work-rate level wasincreased or decreased accordingly |
|
| Outcomes | Muscle strength (1RM-half squat) Cycling test Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Jette 1996.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: no Loss to follow-up: 9 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 102 Sample: non-disabled community-dwelling older people Age: mean 72 years Inclusion criteria: non-disabled, community dwelling, aged 65 and over; clearance from GP Exclusion criteria: significant coronary artery disease, angina, congestive heart failure, myocardial infarction, cardiac surgery, or significant or new onset rhythm disturbance; neurological disorders with residual deficit; renal failure requiring dialysis; recent cancer with active chemotherapy or radiation treatment; uncontrolled hypertension, diabetes or seizure disorders; recent fracture; legal blindness; major mobility limitations; failed exercise safety evaluation (i.e. resting heart rate greater than 120 bpm, resting systolic/ diastolic great than 165/100 or less than 80/50, or failed treadmill test; English speaking; have access to a VCR or willing and able to use one provided by the study |
|
| Interventions | PRT versus control 1.PRT Type of Ex: 10 exercises to the UL, LL and Tr Equipment: Theraband Intensity: low to moderate Frequency: Ex3 Reps/Sets: 10/1 Duration: 12-15 weeks Setting: home-based Supervision: low Adherence: mean 58%, median 71% 2. Control Group: continued with normal activities, on a waiting list for exercises |
|
| Outcomes | Strength (Cybex isokinetic dynamometer) Psychological well-being (Profile of Mood States battery) SF-36 Comments on adverse events: no (not identified as such) |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Jette 1999.
| Methods | RCT Method of randomisation: randomly permuted blocks by size 4, assigned by a staff member not involved in data collection Assessor blinding: yes Participant blinding: no Loss to follow-up: 15 at 6 months Intention-to-treat analysis: no Post-program follow up: no, but 6 months of exercise |
|
| Participants | Location: USA N = 215 Sample: older adults with disabilities Age: PRT group mean 75.4 years (SD 7.4) Inclusion criteria: aged 60 years or over; limitations in at least one of 9 functional areas Exclusion criteria: medical history that contained current treatment for cancer, kidney disease requiring dialysis, recent fracture, uncontrolled diabetes or seizures, regular use of a wheelchair, current rehabilitation care, current fainting or dizzy spells, sudden loss of coordination or legal blindness or physician identified contraindications to exercise |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 11 exercises to UL, LL and Tr Equipment: Theraband Intensity: low-moderate Frequency: Ex3 Reps/Sets: 10 reps Duration: 6 months Setting: home-based Supervision: low Adherence: 89% 2. Control Group: on a waiting list |
|
| Outcomes | Strength (hand-held dynamometer) Balance (functional reach, unilateral stance, tandem stance) TUAG Profile of Mood States Sickness Impact Profile 68 Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Jones 1994.
| Methods | RCT: (note: data reported by dominant and non-dominant leg. Data for dominant leg used in analyses) Method of randomisation: not stated Assessor blinding: yes Participant blinding: no Loss to follow-up: 4 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 46 Sample: women from a community senior center Age: mean 67.4 years Inclusion criteria: female, from a community senior centre, age>60, independently ambulatory Exclusion criteria: unstable cardiovascular disease, orthopaedic or neurological dysfunction, any other uncontrolled chronic conditions that would interfere with the safety and conduct of the training protocol |
|
| Interventions | PRT versus control 1.PRT Type of Ex: 7 LL Equipment: velcro leg weights Intensity: started low, progressed to moderate Frequency: Ex3 Reps/Sets: 3 of 14 by end of program Duration: 16 weeks Setting: group at local community centre (2 days/week) and home (1 day/week) Supervision: full in group, none at home Adherence: 86-93% 2. Control Group: no intervention - contacted to monitor health and activity level |
|
| Outcomes | Strength and muscular endurance (isokinetic dynamometer) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Jubrias 2001.
| Methods | RCT with 3 groups: PRT, aerobic training and control Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: no Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 40 total (n = 26 in PRT and control) Sample: healthy, active older people Age: 69.2 years (SD = 0.6) Inclusion criteria: healthy (screened with physical exam, exercise testing), physically active, not engaged in PRT or aerobic training before this study Exclusion criteria: not reported |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 1LL, 2 UL Equipment: resistance training machines Intensity: phase 1-60-70% of 1RM; phase 2-70-85% of 1RM Frequency: Ex3 Reps/Sets: phase 1: 10-15/3; phase 2: 4-8/ 3-5 Duration: 24 weeks Setting: gym Supervision: not reported Adherence: 94.2% attendance 2. Control Group: continued normal activities, asked not to begin PRT or aerobic training during thetrial 3. Aerobic Training Group: training began at 60% heart rate reserve for 10-20 minutes, progressed to 80-85% HR reserve for a total of 40 minutes, three times per week |
|
| Outcomes | Muscle size Energy and fibre properties Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Judge 1994.
| Methods | RCT with factorial design: PRT alone, balance training alone, PRT and balance, control Method of randomisation: balance block design (blocks of 4 subjects) Assessor blinding: yes Patient blinding: no, but control group received educational sessions Loss to follow-up: 3 from PRT and control group Intention-to-treat analysis: yes Post-program follow up: yes, monitored for 6 months after intensive program while participants undertook tai chi. Falls monitored for median 0.88 years, max 1.86 years |
|
| Participants | Location: USA N = 110 total (55 in PRT vs control) Sample: ambulatory older people from voter registration list Age: mean 80 years Inclusion criteria: age 75 years or greater, the ability to walk without an assistive device for 8 meters, MMSE >24 Exclusion criteria: symptomatic cardiovascular disease, poorly controlled hypertension (>160/96), history or physical findings of focal neurological deficit, Parkinson disease, peripheral neuropathy of the legs, hip or knee joint replacement, hip fracture, cancer (metastatic or under active treatment), taking neuroleptic, prednisolone > 5mg/day, benzodiazepines, significant hip or knee arthritis that requires a cane for ambulation |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 6 LL Equipment: cuff-weights and exercise machines Intensity: 60-75% for exercises with machines; low to moderate for other Frequency: 3 times per week Reps/Sets: 3 sets to failure with machines; 13/2 with sandbags; 10/2 with body weight Duration: 12 weeks Setting: group exercise Supervision: full Adherence: 82% 2. Control group: 5 education sessions 3. Balance training: 3 times per week, 45 minute sessions, one-on-one with exercise leader includingbalance platform and floor-based exercises (eyes open and closed on different surfaces, with pertubationsand base of support changes) |
|
| Outcomes | Strength (isokinetic dynamometer) Side effects of training (musculoskeletal or neurologic complaints) Gait velocity Chair rise Balance Comments on adverse events: yes (a priority outcome of study) |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Kalapotharakos 2005.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 1 in the high resistance group, 1 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Greece N = 12- HI; N = 12-MI; N = 11-control Sample: healthy, inactive but independent living older adults Age: HI-mean 64.6 years (SD = 5.1); MI-mean 65.7 years (SD = 4.2) Inclusion criteria: non smokers, free of medication, no symptoms of cardiovascular, orthopedic, or neuromuscular disease, and physically inactive before Exclusion criteria: MMSE < 24, depression (GDS > 5) |
|
| Interventions | PRT (high intensity and moderate intensity) versus control 1. PRT Type of Ex: 4UL/2 LL Equipment: Universal gym machines Intensity: high intensity group: 80% of 1 RM; moderate intensity group: 60% of 1 RM Frequency: Ex3 Reps/Sets: 8/3 for high intensity group; 15/3 for moderate intensity group Duration: 12 weeks Setting: not reported Supervision: not reported Adherence: 98.5% 2. Control Group: no exercise |
|
| Outcomes | Muscle strength (1-RM) 6-min walk Chair rise Vertical jump 1-leg standing time, Walking speed Stair climb Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Kallinen 2002.
| Methods | RCT with 3 groups: PRT, control, and aerobic group Method of randomisation: manually perform by drawing lots Assessor blinding: No Participant blinding: not reported Loss to follow-up: 4 in PRT group, 3 in endurance group (aerobic) Intention-to-treat analysis: yes done at the 30th month Post-program follow up: no |
|
| Participants | Location: Finland N = 27 (16 in PRT) Sample: elder women Age: range 76-78 years Inclusion criteria: no severe diseases or functional impairments Exclusion criteria: not reported |
|
| Interventions | PRT versus control and versus aerobic (Note: participants in all groups were given 600mg calcium per day) 1. PRT Type of Ex: 4UL, 4LL Equipment: resistance training machines Intensity: high - completed 8RM Frequency: Ex3 Reps/Sets: 8/3 Program Duration: 2 years Setting: gym Supervision: full Adherence: 74% 2. Control Group: non-exercise group 3. Aerobic Fitness Group: N = 15; 3 sessions per week, performed same exercises as PRT group but withno resistance, plus added stationary cycling for 40 second stations |
|
| Outcomes | PeakVO2 Peak Power Comments on adverse events: yes |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Katznelson 2006.
| Methods | RCT Method of randomisation: by a block design Assessor blinding: yes Participant blinding: yes Loss to follow-up: 4/19- placebo + ex; 1/17- placebo only Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: USA N = 26 (19 in PRT) Sample: men with relative testosterone insufficiency, sedentary and community dwelling Age: mean 72 years (SD = 5.4) Inclusion criteria: a single fasting serum free-testosterone value < 14.5 pg/ml and BMI is between 18-32; sedentary status Exclusion criteria: clinically unstable coronary artery or cerebrovascular disease, osteoarthritis of the lower extremity that could limit ambulation, clinically significant benign prostatic hypertropy (BPH), prostate cancer, an elevated prostate-specific antigen (PSA) value, hematocrit>52%, disorders known to affect body composition including hypokalemia, renal insufficiency, liver dysfunction, diabetes mellitus, hypothyroidism, alcoholism, thromoboembolic disease or coagulopathy, supraphysiologic glucocorticoid medication during the previous 12 months, androgen medications including supplements during the past 5 years, clinically significant psychiatric disease, or known pituitary disease, or radiation of the hypothalamus or pituitary gland |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 11 resistance exercises adapted from the Strong for Life video Equipment: elastic bands Intensity: used the next level of elastic band when the perceived exertion was less than moderate Frequency: 3 to 4 times a week Reps/Sets: 10/1 Duration: 12 weeks Setting: home Supervision: returned for an out-patient visit every two weeks and phone calls Adherence: 90% 2. Control Group: non exercise intervention |
|
| Outcomes | SF-36 Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Kongsgaard 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 3/9 in the ex group; 2/9 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Denmark N = 18 (9 in each group) Sample: home-dwelling elder men with COPD Age: mean 71 years (SD = 1.3) Inclusion criteria: can transport to the hospital Exclusion criteria: fractures of the lower extremities within the last 6 months, neurological disease, cardiovascular diseases, dependence on more than one walking device and cognitive dysfunction |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 3 LL Equipment: Technogym Intensity: 80% of 1 RM Frequency: Ex2 Reps/Sets: 8/4 Duration: 12 weeks Setting: not reported (Gym?) Supervision: full Adherence: extending the training period until a total of 24 training sessions were finished 2. Control Group: daily non-supervised breathing ex |
|
| Outcomes | Primary: simple ADL (interview) Secondary: forced expiratory volume, muscle strength (5 RM), gait speed, timed stair climbing Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Krebs 2007.
| Methods | RCT Method of randomisation: a computer-generated table Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: NA Post-program follow up: no |
|
| Participants | Location: USA N = 15 (6 in PRT) Sample: community dwelling elders with disability Age: mean 70.4 years (SD = 6.5) Inclusion criteria: at least 60 years of age, cognitive intactness, ambulate independently more than 15 feet, had more than one lower-limb impairment, and have more than one functional limitation on SF-36 Exclusion criteria: terminal illness, progressive neurological disease, major loss of vision, and acute pain and non-ambulatory status |
|
| Interventions | PRT versus functional training 1. PRT Type of Ex: resisted proprioceptive neuromuscular facilitation exercise, 9 LL/2UL Equipment: elastic bands Intensity: 10 RM increased to 6 RM Frequency: 3 to 5 times a week Reps/Sets: 4-level of normal progression and 4-level of advanced levels Duration: 6 weeks Setting: home? Supervision: two physical therapists taught the exercises and checked the exercise log at out-patient visits Adherence: PRT group- exercised average 5 days per week; functional training group- exercise average 5. 39 days per week 2. Functional training group: N=6, average age =78.1 years, simulating locomotion activities at 3 differentspeeds, 3-5 days a week |
|
| Outcomes | Primary: SF-36 Secondary: muscle strength, paced gait, chair rise, standing balance Comment on adverse events: yes |
|
| Notes | Numerical results of means and SDs were not reported. Reported/figured % difference | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Lamoureux 2003.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 1/29 in the experimental group, 1/16 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Australia N = 45 (29 in PRT) Sample: community dwelling elderly Age: mean 68.5 years (SD = 1.2) Inclusion criteria: no resistance-training background, no cardiovascular disease, musculoskeletal disorders, neurological dysfunction and uncontrolled chronic conditions Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5 LL Equipment: Pin-loaded weigh machines Intensity: from 60% 1RM in week 1 to 85% 1RM in week 14 Frequency: Ex3 -first 3 months; then Ex2-last 3 months Reps/Sets: 5-8/2-5 Duration: 24 weeks Setting: not reported Supervision: not reported Adherence: 95.5% 2. Control Group: maintain normal activities |
|
| Outcomes | Muscle strength Gait velocity Comments on adverse events: no |
|
| Notes | Final muscle strength outcome was not available Data at week 12 were extracted = baseline + change score. Final SD = baseline SD |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Latham 2001.
| Methods | RCT Method of randomisation: concealed envelopes Assessor blinding: no Participant blinding: no Loss to follow-up: 3 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: New Zealand N = 20 Sample: hospitalised older people Age: mean 81 years (SD 8.6) Inclusion criteria: 65 years or older, patient on hospital ward, expected length of stay of > 1 week Exclusion criteria: unable to perform knee extension against gravity with both legs, recent lower limb fracture, cognitive impairment which limited participation, leg ulcers on lower calf region |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 1 LL Equipment: velcro ankle weights Intensity: 50-80% 1RM Frequency: 5 times a week Reps/Sets: 8/3 Duration: duration of hospital stay (app 2 weeks) Setting: gym in rehabilitation wards of a hospital Supervision: full Adherence: 90% 2. Control Group: regular physiotherapy |
|
| Outcomes | Strength (1RM) Gait speed TUAG Balance (Berg) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Latham 2003.
| Methods | RCT with a factorial design (only information about PRT vs control reported, 3- month outcomes reported) Method of randomisation: central computerised randomisation, blocks of 6 by centre Assessor blinding: yes Participant blinding: no, but attention control Loss to follow-up: 21 Intention-to-treat analysis: yes Post-program follow up: yes, at the 6th month |
|
| Participants | Location: New Zealand and Australia N = 243 Sample: frail older adults recruited from hospital geriatric services Age: mean 79.1 years (SD 6.9) Inclusion criteria: age 65 years or more, receiving hospital care from geriatric services, considered to be frail, not clear indication or contraindication to study treatments Exclusion criteria: responsible physician considered the interventions definitely hazardous or required, patients unlikely to survive 6 months, severe cognitive impairment which could compromise adherence to the exercise programme, not fluent in the English language |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 1 LL Equipment: velcro ankle weights Intensity: aimed for 50-80% for most of the programme Frequency: Ex3 Reps/Sets: 8/3 Duration: 10 weeks Setting: home-based Supervision: limited - fortnightly home visits alternating with phone calls Adherence: 82% (including drop-outs) 2. Control Group: frequency-matched phone calls and home visits |
|
| Outcomes | Primary: falls over 6 months, HRQoL (SF-36) Secondary: balance (Berg), strength (hand-held dynamometer), gait speed, TUAG, Barthel Index, Adelaide Activities Profile, Falls Self-Efficacy Index, adverse events (limitation in ADL for 2+ days and/or attention sought from health care professional) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Liu-Ambrose 2005.
| Methods | RCT Method of randomisation: computer-generalized list Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 2/34 in PRT, 2/34 in stretching Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: Canada N = 68 (34 in each group) Sample: elder women with osteoporosis or osteopenia Age: mean 79.6 years (SD = 2.1) Inclusion criteria: age between 75-85 years with low bone mass and diagnosed with osteoporosis/osteopenia Exclusion criteria: living in care facilities, non-Caucasian, exercise regularly more than 2 times a week, illness or condition that would affect balance, MMSE score lowers than 23 |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 4 UL, 5LL Equipment: machines (Keiser Pressurized Air system) or free weights Intensity: progressed from 50-60 % of 1 RM to 75-85% of 1 RM in 4 weeks Frequency: Ex2 Reps/Sets: 10-15/2 (first 3 weeks); 6-8/2 (after week 3) Duration: 25 weeks Setting: community center Supervision: certified fitness instructors Adherence: 85% for PRT, 79% for stretching (control) 2. Control Group: general stretching, deep breathing and relaxation |
|
| Outcomes | Primary: health related quality of life, general physical function Secondary: muscle strength, gait speed, fall risk assessment Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Macaluso 2003.
| Methods | RCT Method of randomisation: the principal investigator drew numbers from a bowl that had been thoroughly mixed Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 7 Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: UK N = 10-speed group (LI), N= 10-Strength group (HI) Sample: healthy elder women Age: mean = 69 years (SD = 2.7) Inclusion criteria: not reported Exclusion criteria: not “medical stable” for exercise studies |
|
| Interventions | PRT (speed versus strength) Type of Ex: pedal Equipment: mechanically braked cycle ergometer Intensity: speed group (LI)-40% of 2 max resistance to complete 2 revolutions (2RM); strength group (HI)-80% of 2 RM Frequency: Ex3 Reps/Sets: Speed group (LI)-16 pedal revolutions/8 sets; Strength group (HI)-8 pedals revolutions/8sets Duration: 16 weeks Setting: not reported (gym?) Supervision: not reported Adherence: speed group (LI)-93%; strength group (HI)-89% |
|
| Outcomes | Strength measure Max treadmill walking speed Box-stepping test Vertical jump Comments on adverse events: yes |
|
| Notes | Involved power training, no control group | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Madden 2006.
| Methods | RCT with 3 groups: PRT, control, and endurance (aerobic) group Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 5 in the endurance training group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 30 (15 in each group) Sample: healthy elder women Age: mean 69.8 years (SD = 1.5) Inclusion criteria: a normal blood pressure, a normal physical exam, normal resting ECG, normal M-mode and two-dimensional echocardiograms showing no more than mild valvular regurgitation, a normal Bruce protocol treadmill maximal exercise stress test, and a normal hematocrit, fasting blood glucose, total cholesterol, and creatinine. Exclusion criteria: any history of angina, myocardial infarction, stroke, hypertension, chronic pulmonary disease, diabetes, current medication use (prescription or over the counter), current smoking, or exercise-limiting orthopedic impairment |
|
| Interventions | PRT versus control and versus endurance (aerobic) 1. PRT Type of Ex: 10 UL and LL Equipment: not reported (weight?) Intensity: 85% 1RM Frequency: 5 times/week Reps/Sets: 8-12/3 Duration: 24 weeks Setting: not reported (Gym?) Supervision: full-certified trainer Adherence: required participants to attend 90% of all training sessions to remain enrolled in the study 2. Control Group: no training 3. Endurance Ex (aerobic) Group: N=15, mean age=70 years (SD = 2.6), using cycle ergometer, 50-60%Max HR to 80-85% Max HR, 5 times a week |
|
| Outcomes | VO2max Comments on adverse events: no |
|
| Notes | Baseline + relative change score Data from PRT and aerobic training group were compared |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Maiorana 1997.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 5 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Australia N = 31 Sample: men at least 3 months after coronary bypass Age: mean 61.2 years (SD 8.4) in training group Inclusion criteria: male, at least 3 months after coronary artery bypass surgery, low risk for recurrent cardiac events (normal left ventricular function, no residual ischemia, and an exercise capacity exceeding 4 metabolic equivalents during graded exercise testing) Exclusion criteria: not in an exercise rehabilitation programme at time of recruitment, moderate/severe left ventricular function, valve replacement/repair, history of CHF, on beta-blocking medication, significant resting hypertension (systolic BP >160mmHg or diastolic 100 mmHg) angina or significant ST depression during graded exercise testing |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 7UL, 4LL, 1 Tr Equipment: machines, dumb-bells Intensity: 40% of MVC at beginning or program, 60% by end Frequency: Ex3 Reps/Sets: 10-15/3 Duration: 10 weeks Setting: gym Supervision: full Adherence: all subjects completed at least 80% of sessions (excluding drop-outs) 2. Control Group: maintain current physical activity habits |
|
| Outcomes | Strength (1RM) Aerobic capacity (Peak VO2 on treadmill test) Self-efficacy Comments on adverse events: yes (safety an aim of study) |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Malliou 2003.
| Methods | RCT with 3 groups: PRT, functional training, and PRT with functional training group Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: not reported Post-program follow up: no |
|
| Participants | Location: Greece N = 25 (15 in multi-joint resistance training group) Sample: healthy inactive elderly Age: mean 68 years Inclusion criteria: inactive prior to the study, not exhibited anemia, hepatic complications, thyroid disorders or kidney problems, no hypertension, no potential damaging orthopedic and neuromuscular problems. Exclusion criteria: not reported |
|
| Interventions | PRT versus control and versus aerobic 1.PRT Type of Ex: 3 LL- multi-joint resistance training group Equipment: Universal exercise machines Intensity: 90% of 1 RM Frequency: Ex3 Reps/Sets: 12/3 Duration: 10 weeks Setting: not reported (gym?) Supervision: full Adherence: not reported 2. Control group: no training 3. Aerobic ex. group: N = 15, mean age = 69 years, aerobic exercise with light leg weight |
|
| Outcomes | Strength measure Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Mangione 2005.
| Methods | RCT with 3 groups: PRT, control, and aerobic group Method of randomisation: not reported Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 1/11-control group, 1/13-aerobic training group, 6/17-resistance training group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 28 (17 in PRT) Sample: post hip fracture Age: mean 77.9 years (SD = 7.9) Inclusion criteria: successful fixation of a hip fracture, at least 65 years old, living at home, and willing to come to the study site Exclusion criteria: history of unstable angina, uncompensated congestive heart failure, metabolic conditions (i.e., renal dialysis), stroke, Parkinson's disease, life expectancy of less than 6 months, MMSE score is less than 20, and living in a nursing home |
|
| Interventions | PRT versus control and versus aerobic 1.PRT Type of Ex: 4LL Equipment: portable progressive-resistance ex. machine and body weight Intensity: 8 RM Frequency: first 2 months-Ex2, the 3rd month-Ex1 Reps/Sets: 8/3 Duration: 12 weeks Setting: participant's home Supervision: full-6 physical therapists Adherence: 98% 2. Control group: received biweekly mailing of non-ex health topics 3. Aerobic group: N=13, mean age =79.8 years, walking or stepping, LEs/UEs active ROM ex, 65-75%max heart rate |
|
| Outcomes | Primary: SF-36 Secondary: strength measure, 6-minute walking test, walking endurance, gait speed Comments on adverse events: yes |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Manini 2005.
| Methods | RCT with 3 groups: PRT, functional training, and PRT with functional training Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 25 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 9-PRT Sample: functional limited older adults (low isometric knee extension strength) Age: mean 72 years (SD =10) Inclusion criteria: bilateral isometric knee extension strength test < 3Nm/Kg; pass physician's clearance Exclusion criteria: had cardiac or pulmonary difficulty |
|
| Interventions | PRT versus functional training and versus PRT with functional training 1.PRT Type of Ex: 3 LL Equipment: Life-Fitness Inc. Intensity: 10 RM Frequency: Ex2 Reps/Sets: 8/2 Duration: 10 weeks (8-10 weeks of control period before intervention) Setting: not reported (Gym?) Supervision: not reported Adherence: not reported 2. Functional training group: N=7, rising from a chair, rising from kneeling, stair ascending/descending 3. PRT and functional training group: N = 8, 1/week PRT training and 1/week of functional training |
|
| Outcomes | Muscle strength Max. knee isometrics Comments on adverse events: yes |
|
| Notes | Data from PRT and functional training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Maurer 1999.
| Methods | RCT Method of randomisation: random number generator, stratified by disease severity Assessor blinding: yes Participant blinding: no, but attention control group Loss to Follow-up: 15 Intention-to-treat analysis: no Post-program follow up: yes - at 12 weeks (after 8 weeks of training) |
|
| Participants | Location: USA N = 113 Sample: people with diagnosed OA of the knee Age: mean 66.3 years (SD 8.8) in treatment group Inclusion criteria: met current American College of Rheumatology criteria for OA, between 50-80 years, receiving no drugs for their arthritis other than stable doses of analgesics or NSAIDs, had mild to moderate knee pain for at least the previous 3 months, scored 1-3 on the Kellgren radiographic scale Exclusion criteria: concurrently receiving physical therapy, actively involved in any other pharmaceutical or exercise study or had undergone isokinetic strength training within the previous 3 years, had significant cardiovascular disease, more than mild knee swelling, large popliteal cysts, knee instability, major hip or knee surgery on the side to be treated, systemic disease other than OA that might affect muscle function, severe osteopenia, history of fracture in the area of the joint to be treated, paresis of the lower extremity |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 1 LL Equipment: isokinetic dynamometer Intensity: appears high Frequency: Ex3 Reps/Sets: 3 reps at 3 speeds (total 9 reps) in 3 sets Program Duration: 8 weeks Setting: gym Supervision: not reported Adherence: not reported 2. Control Group: four classes on OA education and self-management |
|
| Outcomes | Primary: WOMAC, SF-36 Secondary: strength (isokinetic dynamometer), AIMS index Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
McCartney 1995.
| Methods | RCT. All results broken down into four groups by sex and age (60-70 or 70-80, only results for women aged 70-80 - the largest group - used for pooled comparisons in review) Method of randomisation: not reported Assessor blinding: no Participant blinding: no, but attention/exercise control group Loss to follow-up: 23 Intention-to-treat analysis: no Post-program follow up: no, but exercise program had 2 year duration |
|
| Participants | Location: Canada N = 142 Sample: healthy volunteers Age: mean 64 years (SD 2.4) for exercise group Inclusion criteria: approval of family physician, successful completion of cycle ergometer test, aged 60-80 years, no prior resistance training experience Exclusion criteria: evidence of coronary artery disease, chronic obstructive or restrictive lung disease, osteoporosis, major orthopaedic disability, smoking, body weight greater than 130% of ideal |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 3UL, 3LL, 1Tr Equipment: weight-lifting machines Intensity: 50-80% 1RM Frequency: Ex2 Reps/Sets: 10-12/3 Program Duration: 42 weeks Setting: gym Supervision: not reported Adherence: 88% (at 1 year) 2. Control Group: 2 times per week low-intensity walking |
|
| Outcomes | Strength (1RM) Maximum cycle ergometry Treadmill testing Stair climbing ergometric muscle cross-sectional area Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
McGuigan 2001.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 4 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Australia N = 20 Sample: people with peripheral arterial disease Age: mean 66 years (SD 6) exercise group Inclusion criteria: PAD diagnosed by a vascular surgeon Exclusion criteria: leg pain at rest, ischemic ulceration or gangrene, inability to walk at lest 2km/h on a treadmill, limited exercise capacity by factors other than claudication, vascular surgery or angioplasty in previous year, smoking of cigarettes |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 8 exercise that included UL, LL, Tr, combination varied in each session (1-3) per week Equipment: machines Intensity: used linear periodization, intensity varied with reps Frequency: Ex3 Reps/Sets: 8-15/2 Program Duration: 24 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: no intervention |
|
| Outcomes | Strength (10 RM) 6 minute walk test Treadmill walk time Hemodynamic measures Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
McMurdo 1995.
| Methods | RCT with three groups, PRT, mobility exercise programme and attention control Method of randomisation: sealed envelopes in sequence, computer generated random number tables generated the sequence Assessor blinding: yes Participant blinding: no, but attention control used Loss to follow-up: 7 from PRT and control group Intention-to-treat analysis: no Post-program follow up: no, but program 6 months long |
|
| Participants | Location: UK N = 86 total (55 in PRT vs control) Sample: residents of sheltered housing complexes Age: mean 82 years Inclusion criteria: age 75 years and over, limited mobility requiring the use of a walking aid, dependence in functional activities of daily living requiring the assistance of home help at least once per week Exclusion criteria: major neurological disease, unstable cardiovascular disease, severe cognitive impairment |
|
| Interventions | PRT versus control and versus mobility 1. PRT Type of Ex: 24 (UL, LL, trunk) Equipment: theraband, progressive thickness Intensity: low-moderate Frequency: daily Reps/Sets: 5-10/1 Program Duration: 26 weeks Setting: home Supervision: low - visited at home every 3-4 weeks Adherence: not reported 2. Control Group: health education visits every 3-4 weeks 3. Mobility Group: same 24 exercises, but with no resistance |
|
| Outcomes | TUAG Sit to stand test (time to complete 10 full stands) Grip strength Functional reach ADL (Barthel Index) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Mihalko 1996.
| Methods | RCT cluster randomised by residence Method of randomisation: not reported Assessor blinding: no Participant blinding: no, but attention control group Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 58 Sample: sedentary residents of senior citizen or residential nursing homes Age: mean 82.7 years (SD 7.7) Inclusion criteria: residents of senior citizen and residential nursing home facilities, sedentary, clearance form personal physician Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5 UL Equipment: dumb bells Intensity: high - worked until failure Frequency: Ex3 Reps/Sets: 10-12 reps Program Duration: 8 weeks Setting: gym Supervision: not reported Adherence: not reported 2. Control Group: fluid movement program |
|
| Outcomes | ADL performance (modified version of Lawton and Brody's IADL scale) Strength (1RM) Satisfaction with Life Scale Positive and negative affect Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Mikesky 2006.
| Methods | RCT Method of randomisation: not reported-stratified Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 36% in PRT, 24% in Control (range of motion) Intention-to-treat analysis: yes, done at the 30th month Post-program follow up: no |
|
| Participants | Location: USA N = 221 (113 in PRT) Sample: knee OA Age: mean = 69.4 years (SD = 8) Inclusion criteria: not clearly described Exclusion criteria: cannot walk without assistance, amputation of either lower extremity, knee or hip replacement, history of stroke, myocardial infarction, CHF, uncontrolled hypertension, fibromyalgia… |
|
| Interventions | PRT versus flexibility (control) 1.PRT Type of Ex: 2UL/2LL Equipment: CYBEX machines at gym; Elastic bands at home, Intensity: 8-10 RM Frequency: Ex3; first 3 months (2/week in the gym, 1/week at home), month 4-6 (1/week in the gym, 2/week at home), month 7-9 (2/month in the gym, 3/week at home); month 10-12 (1/month in the gym, 3/week at home) Reps/Sets: from 8-10/ 3 to 12/2 Duration: 1 year Setting: gym and home Supervision: full-1 fitness trainer in the gym Adherence: attending gym (PRT-59%, control/ROM-64%); home ex (PRT-56%, control/ROM-62%) 2. Flexibility exercise group: N=108, mean age = 68.6 years (SD = 7.5), flexibility ex, 3 times/week |
|
| Outcomes | Primary: SF-36 (at the 30 month), WOMAC Secondary: Strength measure (1RM) Comments on adverse events: yes |
|
| Notes | SF-36 was not pooled because it was not measured right after the training | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Miller 2006.
| Methods | RCT Method of randomisation: computer generated sequence, stratified and block randomization Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 3 withdrawn (1 in control), 4 death (2 in PRT) Intention-to-teat analysis: yes Post-program follow up: no |
|
| Participants | Location: Australia N = 51 (25 in PRT) Sample: fall-related lower limb fracture Age: mean 84.8 years Inclusion criteria: at least 70 years old, fall-related lower limb fracture Exclusion criteria: (1) did not reside within southern Adelaide, (2) were unable to comprehend instructions relating to positioning of the upper arm for eligibility assessment, (3) were unable to fully weight bear on the side of the injury for more than seven days post admission, (4) were not independently mobile prefracture, (5) were medically unstable more than 7 days post admission, (6) were suffering from cancer, chronic renal failure, unstable angina or unstable diabetes or (7) were not classified as malnourished |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5 LL Equipment: elastic band Intensity: was appropriate to baseline strength, pain level and range of motion Frequency: Ex3 Reps/Sets: increased to 8/2 if exercise could be completed in good form Duration: 12 weeks Setting: a teaching hospital Supervision: full-pysiotherapist Adherence: > 86% 2. Control group: attention control, week 1-6: tri-weekly home visits, week 7-12: weekly home visit;discussion of general information during the visit |
|
| Outcomes | Primary: SF-12 Secondary: strength measure, gait speed Comments on adverse events: no |
|
| Notes | Reported Median & 95%CI. Data from participants who took nutrition supplementation were not extracted | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Miszko 2003.
| Methods | RCT with 3 groups: PRE, control, and power exercise Method of randomisation: stratified by sex Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 4/17 in PRT, 7/18 in power Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 28 (13 in PRT) Sample: older adults with below average leg extensor power Age: mean 72.8 years (SD = 5.4) Inclusion criteria: below-average leg extensor power Exclusion criteria: poorly controlled or unstable cardiovascular disease or diabetes, recent unhealed bone fracture (within the past 12 months), severe hypertension while resting quietly in the supine position, leg or arm amputation, excessive alcohol intake (more than three drinks per day), a classic anterior compression fracture, neuromuscular disorders, being nonambulatory, or having recent (within 6 months) involvement in a strength-training or running or jogging program |
|
| Interventions | PRT versus control and versus power exercise 1.PRT Type of Ex: 4UL/4LL & squats Equipment: Keiser Inc. Intensity: 50% -> 70% of 1RM by week 8, 80% of 1RM the last 8 weeks Frequency: Ex3 Reps/Sets: 6-8/3 Duration: 16 weeks Setting: not reported (Gym?) Supervision: not reported Adherence: not reported 2. Control Group: maintain usual activity and attend 3 educational presentations over the study period 3. Power Ex Group: N=11, mean age = 72.3 years (SD = 6.7), the same exercise as the PRT group butdid jump squats instead of squats, 6-8 repetition at 40% of 1RM, move as fast as possible |
|
| Outcomes | Primary: Continuous Scale Physical Functional Performance Secondary: strength measure (1 RM) Comments on adverse events: yes |
|
| Notes | Involved power training | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Moreland 2001.
| Methods | RCT Method of randomisation: concealed, phoned central office Assessor blinding: yes Participant blinding: not reported Loss to follow-up: 10 Intention-to-treat analysis: yes Post-program follow up: yes, at the 6th month |
|
| Participants | Location: Canada N = 133 (68 in PRT) Sample: people post-stroke Age: mean 69 years Inclusion criteria: not reported Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1.PRT Type of Ex: UL, LL Equipment: not reported Intensity: not reported Frequency: not reported Reps/Sets: not reported Program Duration: until hospital discharge Setting: hospital Supervision: full Adherence: not reported 2. Control Group: regular therapy |
|
| Outcomes | Primary: Chedoke-McMaster Stroke Assessment Secondary: 2-minute walk test Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Nelson 1994.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 1 Intention-to-treat analysis: yes Post-program follow up: no, but program had 1-year duration |
|
| Participants | Location: USA N=40 Sample: healthy females post-menopause Age:mean 61.1 years (SD 3.7) Inclusion criteria: at least 5 years post-menopausal but not older than 70, do not engage in any regular physical training, weigh less than 130% of ideal body weight, currently non-smoking, do not have more than one crush fracture of the spine, no history of other osteoporotic fractures, have not taken estrogen or other medications known to affect bone for 12 months, passed physical screening (including ECG during strength training session) Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1.PRT Type of Ex: 2 LL, 1 UL, 2Tr Equipment: pneumatic resistance machines (Keiser) Intensity: 80% of 1RM Frequency: Ex2 Reps/Sets: 8/ 3 Program Duration: 52 weeks Adherence: 87.5% Setting: gym Supervision: full 2. Control Group: asked to maintain normal level of activity, could receive the exercise program at the end of the trial |
|
| Outcomes | Strength (1RM) Balance (backward walking) Physical activity (Harvard Alumini Questionnaire, kJ/week) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Newnham 1995.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: no, but attention control Loss to follow-up: 6 Intention-to-treat analysis: no Post-program follow up: yes, at the 24 week |
|
| Participants | Location: Canada N = 30 Sample: residents of long-term care facility Age: mean 81.7 years (SD 5.6) Inclusion criteria: age 70+, independent in ambulation (with or without walking aid) over 40m at <0.9m/s, 20+ on TUAG; at least 90 degrees of available ROM at knee, can follow a 3-step command Exclusion criteria: have Parkinsons Disease or CVA; participation in strength training in the past year; unstable medical conditions |
|
| Interventions | PRT versus control 1. PRT Type of Ex: UL, LL Equipment: pullies Intensity: 80% of 1RM Frequency: Ex3 Reps/Sets: 10/3 Program Duration: 12 weeks Setting: gym in nursing home Supervision: full Adherence: 86% 2. Control Group: attention control |
|
| Outcomes | Strength (1RM) Gait velocity TUAG Balance (Berg) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Nichols 1993.
| Methods | RCT Method of randomisation: stratified into rank-ordered pairs and randomised Assessor blinding: no Participant blinding: no Loss to follow-up: 6 Intention-to-treat analysis: no Post-program follow up: no, but 6 month duration of program |
|
| Participants | Location: USA N = 36 Sample: active healthy women Age: mean 67.8 years (SE 1.6) Inclusion criteria: greater than 60 years, active for at least 6 months prior to the trial with exercise at least 3 times per week, physician's consent Exclusion criteria: previous weight training, history of cardiovascular disease, taking thyroid or cardiac medications, nonestrogen repleted |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 4UL, 2LL, 1Tr Equipment: variable resistance machines (Polaris) Intensity: 80% 1RM Frequency: Ex3 Reps/Sets: 8-10/3 Program Duration: 24 weeks Setting: gym Adherence: 87% of sessions Supervision: full 2. Control Group: maintain current routine |
|
| Outcomes | Strength (1RM) Activity performance Blair Seven Day Recall Comments on adverse events: yes (safety a priority objective) |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Ouellette 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to Follow-up: 0 Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: USA N = 42 (21 in each group) Sample: single mild to moderate stroke Age: mean 65.8 years (SD = 2.5) Inclusion criteria: subjects aged at least 50 years, 6 months to 6 years following a single unilateral mild to moderate stroke with residual lower extremity hemiparesis, community dwelling, independent ambulation with or without an assistive device, report of 2 or more limitations on the physical function subscale (PF 10) of the Medical Outcomes Survey Short-Form, ability to travel to the exercise laboratory, and willingness to be randomized. Stroke was diagnosed by history and clinical examination, and confirmed via medical records review. Exclusion criteria: myocardial infarction within the past 6 months, symptomatic coronary artery disease or congestive heart failure, uncontrolled hypertension, fracture within the past 6 months, acute or terminal illness, score less than 20 on the MMSE, inability to follow a 3-step command, current participation in regular strength training or supervised physical therapy, or pain during exercise |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 4 LLs Equipment: Pneumatic resistance training equipment (Keiser Sports Health Equipment) and modified stack-pulley system (Therapy Systems) Intensity: 70% of 1RM Frequency: Ex3 Reps/Sets: 8-10/3 Duration: 12 weeks Setting: gym Supervision: full Adherence: 85.4%-PRT; 79.9%-controls 2. Control group: bilateral range of motion ex and upper body flexibility exercise |
|
| Outcomes | Primary: Late-Life Function and Disability Instrument, sickness impact profile Secondary: strength measure (1 RM), 6-minutes walk, gait speed, stair climb, chair rise Comments on adverse events: yes |
|
| Notes | SD is obtained from SE for LLFD 1 | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Parkhouse 2000.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to Follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Canada N = 22 Sample: sedentary older women with low bone mineral density Age: mean 68.1 years Inclusion criteria: community-dwelling, sedentary, post-menopausal women, aged 60-80 years, low bone mineral density Exclusion criteria: medical or orthopaedic problems that would interfere with their ability to participate in physical activity, on hormone replacement |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 9 LL Equipment: not reported Intensity: 75-80% of 1RM Frequency: Ex3 Reps/Sets: 8-10/3 Program Duration: 8 months Setting: gym Supervision: not reported Adherence: not reported 2. Control Group: not reported |
|
| Outcomes | Strength (1RM) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Pollock 1991.
| Methods | RCT with 3 groups: PRT, control, and aerobic training group Method of randomisation: rank ordered then randomly stratified into 3 groups, with the restriction that more would be assigned to training groups Assessor blinding: no Participant blinding: no Loss to Follow-up: 8 total (4 in PRT and control) Intention-to-treat analysis: no Post-program follow up: no, but 6 month exercise program |
|
| Participants | Location: USA N = 57 in total (36 in PRT and control) Sample: sedentary men and women Age: mean 72 years Inclusion criteria: free from overt evidence of coronary heart disease or any other conditions that would limit their participation in vigorous exercise; aged 70-79, sedentary for one year Exclusion criteria: blood pressure > 160/100; ECG changes or cardiac symptoms during exercise testing |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 5UL, 2LL, 3 Tr Equipment: variable resistance machines (Nautilus) Intensity: initially light to moderate, by week 14 encouraged to train to fatigue Frequency: Ex3 Reps/Sets: 8-12/ 1 Program Duration: 26 weeks Setting: gym Supervision: not reported Adherence: 97.8% sessions attended (excluding drop-outs), 87% stayed with program 2. Control Group: not reported 3. Aerobic Training Group: 3 sessions per week of walk/jog program for 26 weeks, aimed for duration of35-45min minutes at 75-85% VO2 max by week 26 |
|
| Outcomes | Strength VO2 max Adverse events Reaction time Comments on adverse events: yes (a priority outcome, well- defined) |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Pu 2001.
| Methods | RCT Method of randomisation: matched by age then randomised Assessor blinding: no Participant blinding: no Loss to follow-up: 2 Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: USA N = 16 Sample: older women with CHF Age: mean 77 years (SE 6) Inclusion criteria: community-dwelling women; 65 years or older; mild to moderate systolic heart failure New York Heart Association (NYHA) class I to III; resting ejection fraction less than or equal to 45%, Exclusion criteria: NYHA class IV heart failure; myocardial infarction within 6 months of randomisation, hospitalization for CHF within 2 months, change of CHF therapy within 1 MO; unstable angina pectoris, fixed ventricular rate pacemaker, abdominal aortic aneurysm >4cm, major limb amputation, symptomatic abdominal or inguinal hernias, MMSE <23, signification abnormalities on treadmill or strength testing, any unstable medical conditions |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2UL, 2LL Equipment: pneumatic resistance equipment (Keiser) Intensity: 80% of 1RM Frequency: Ex3 Reps/Sets: 8/3 Program Duration: 10 weeks Setting: Gym Adherence: 98% Supervision: Full 2. Control Group: sham exercise group 2 time per week of supervised, low-intensity stretches for 10 weeks |
|
| Outcomes | Exercise capacity (6-minute walk) Maximal oxygen consumption Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Rall 1996.
| Methods | RCT: (groups of healthy young people and middle-aged people with RA not included in this review) Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 0 Intention-to-treat analysis: no drop-outs, not stated Post-program follow up: no |
|
| Participants | Location: USA N = 14 Sample: healthy elderly Age: mean 70.3 years (SD 5) Inclusion criteria: healthy older people (ages 65-80) Exclusion criteria: obese (BMI>30), diabetes, cancer, renal disease, liver disease, cardiac artery disease, endocrine disorder, autoimmune disease |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 1UL, 2LL, 2 Tr Equipment: pneumatic resistance machines (Keiser) Intensity: 80% of 1 RM Frequency: Ex2 Reps/Sets: 8/ 3 Program Duration: 12 weeks Setting: gym Supervision: full Adherence: 92% 2. Control Group: 15 minutes of water exercises |
|
| Outcomes | Strength (1RM) Aerobic capacity - VO2 max Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Reeves 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: not reported Post-program follow up: no |
|
| Participants | Location: UK N = 18 (9 in each group) Sample: physically active volunteers Age: mean 74.3 years (SD = 3.5) Inclusion criteria: no neurological or musculoskeletal disorder that might prevent participation Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2UL/2LL Equipment: Technogym machines Intensity: 80% of 5 RM Frequency: Ex3 Reps/Sets: 10/2 Duration: 14 weeks Setting: not reported Supervision: full Adherence: 93% 2. Control Group: to keep normal activity level |
|
| Outcomes | Muscle strength Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Rhodes 2000.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 6 Intention-to-treat analysis: no Post-program follow up: no, but exercise program 1 year duration |
|
| Participants | Location: Canada N = 44 Sample: healthy, community-dwelling sedentary women Age: mean 68.8 years Inclusion criteria: aged 65-75, not actively engaged in an organised activity program, had independent community dwelling status, passed medical screening by doctor Exclusion criteria: recent hospital stay, blind, severe hearing impairment, uncontrolled hypertension and diabetes, symptomatic cardiorespiratory disease, severe renal or hepatic disease, uncontrolled epilepsy, progressive neurological disease, chronic disabling arthritis, MMSE<25/30, anaemia, marked obesity with the inability to exercise, regular exercise at the time of screening more than 3 times 30 minutes per week, current use of Beta-blockers, oral anti-coagulants or central nervous system stimulants |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 3UL, 3LL Equipment: weight-lifting equipment (Universal Gym) Intensity: 75% 1RM Frequency: Ex3 Reps/Sets: 8/3 Program duration: 1 year Setting: first 3 months in supervised gym, last 9 months at a recreation facility close to participants' home Supervision: supervised for first 3 months, last 9 months had occasional visits from study staff Adherence: 86% (attendance) 2. Control Group: asked to maintain normal lifestyle, could participate in exercises at the end of the trial |
|
| Outcomes | Muscle strength (1RM, hand grip) Flexibility (trunk flexion test) Comments on adverse events: no | |
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Schilke 1996.
| Methods | RCT Method of randomisation: table of random numbers used Assessor blinding: no Participant blinding: no Loss to follow-up: no Intention-to-treat analysis: No dropouts, not stated ITT Post-program follow up: no |
|
| Participants | Location: USA N = 20 Sample: man and women with knee OA Age: mean 64.5 years in PRT group Inclusion criteria: from rheumatology clinic, no condition to preclude increased activity/strength training, not currently involved in a scheduled program of regular of exercise and had not participated in a strength-training program in the last 6 months Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1.PRT Type of Ex: 1LL Equipment: isokinetic dynamometer (Cybex II) Intensity: high - maximal contractions Frequency: Ex3 Reps/Sets: 5/ 6 by session 6 (the end of week 2) Program duration: 8 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: usual activities |
|
| Outcomes | Strength (isokinetic dynamometer) Timed walk Range of motion Health status (Arthritis Impact Measurement Scales; higher score = poor health status) Osteoarthritis Screening Index (OASI; modified from RheumatoidArthritis Disease Activity Index; higher score = worse health) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Schlicht 1999.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 2 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N=24 Sample: moderately active, community-dwelling men and women Age: mean 72 years (SD 6.3) Inclusion criteria: 60 years and older, community-dwelling, physician consent to participate Exclusion criteria: dependent living status, current involvement in a strength training program, physiological disorders that precluded strenuous exercise or affected vestibular function |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 6LL Equipment: resistance training machines (Universal, Cybex and Paramount equipment) Intensity: 75% of 1RM Frequency: Ex3 Reps/Sets: 10/2 Program Duration: 8 weeks Setting: gym Supervision: not reported Adherence: 99% (excluding drop outs) 2. Control Group: not reported |
|
| Outcomes | Muscle strength (1 RM) Maximum walking speed 5-rep sit-to-stand Balance (1-leg stance with eyes shut) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Segal 2003.
| Methods | RCT Method of randomisation: using a table of random numbers, which was stratified by study centers and intent of treatment (curative or palliative) Assessor blinding: yes Participant blinding: no Loss to follow-up: 8/82 in the PRT group; 12/73 in the control group Intention-to-treat analysis: yes Post-program follow up: no |
|
| Participants | Location: Canada N = 155 (82 in PRT) Sample: men with prostate cancer Age: mean 68.2 years (SD = 7.9) Inclusion criteria: had prostate cancer, would received androgen deprivation therapy for at least 3 months after recruitment, and the treating oncologist provided consent Exclusion criteria: severe cardiac disease, uncontrolled hypertension, pain, unstable bone lesions, and residence more than 1 hr from the study center |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 6UL/3LL Equipment: not reported Intensity: 60-70% of 1 RM, increased 5 lb after 12 successful repetitions Frequency: Ex3 Reps/Sets: 8-12/2 Duration: 12 weeks Setting: fitness center Supervision: full Adherence: 79% 2. Control Group: on a waiting list, offered the identical exercise advice and guideline as the exercisegroup after the study period |
|
| Outcomes | Primary: Health-related quality of life Secondary: Muscle fatigue (Number of repetition) Comments of adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Selig 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 3/19 in the PRT group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Australia N = 33 (14 in PRT) Sample: with chronic heart failure Age: mean 65 years (SD = 13) Inclusion criteria: left ventricular systolic failure except aortic stenosis, left ventricular ejection fraction below 40%, and stable pharmacologic therapy Exclusion criteria: New York Heart Association Class I or IV, mayocardiact infarction in the previous 6 months, cardiac arrest, symptomatic, sustained ventricular tachycardia, current angina, conditions that constraindicate exercise, did not pass baseline assessment |
|
| Interventions | PRT versus control 1. PRT Type of Ex : 5 UL/4 LL Equipment: multistation hydraulic resistance training system Intensity: by increasing resistance or the number of sets Frequency: Ex3 Reps/Sets: not reported Duration: 12 weeks Setting: hospital rehabilitation gym Supervision: not reported Adherence: not reported 2. Control Group: usual care |
|
| Outcomes | Muscle strength VO2 max Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Seynnes 2004.
| Methods | RCT with 3 groups: high intensity, low intensity, and control Method of randomisation: not reported Assessor blinding: no Participant blinding: yes Loss to follow-up: 5/27 drop out Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: France N = 8-HI; N = 6-LI; N = 8-control Sample: institutionalized elders Age: HI-mean 83.3 years (SD = 2.8); LI-mean 80.7 years (SD = 2.3) Inclusion criteria: at least 70 years of age, ambulatory, and understand simple instructions Exclusion criteria: (a) cognitive impairment precluding understanding of the written informed consent; (b) practice of regular exercise outside of the research activities; (c) unstable cardiovascular disease, hypertension, diabetes, or any other unstable medical condition; (d) amputations; (e) hernias; (f) symptomatic known unrepaired aortic aneurysm; (g) recent (within 6 months) hospitalization for myocardial infarction, stroke, fracture, eye surgery, or laser treatment; (h) skin disease precluding placement of ankle weights; (i) musculoskeletal deformity; (j) neuromuscular disease; and (k) symptomatic rheumatoid or osteoarthritis precluding planned exercises |
|
| Interventions | PRT (high intensity and low intensity) versus control 1. PRT Type of Ex: 1LL Equipment: ankle cuff Intensity: HI-80% of 1RM; LI-40% of 1RM Frequency: Ex3 Reps/Sets: 8/3 Duration: 10 weeks Setting: not reported-gym? Supervision: full Adherence: 99% 2. Control Group: wearing empty ankle cuff and did the same exercise as the Ex group but without weights |
|
| Outcomes | Primary: self-reported disability Secondary: muscle strength (1RM), muscle endurance, 6-minute walking, chair rising, stair climbing Comments on adverse events: yes |
|
| Notes | SD was calculated from SEM Date from high intensity PRT and low intensity PRT were compared |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Simoneau 2006.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: not reported Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: France N = 20 (11 in PRT) Sample: healthy and community dwelling people Age: mean 78.1 years (SD = 3.1) Inclusion criteria: no muscular, neurological, cardiovascular, metabolic, and inflammatory disease' moderately active individuals Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex : 1 LL-ankle joint Equipment: elastic bands-home Intensity: increased progressively from 50% - 55% of 3RM to 70% of 3 RM Frequency: Ex3 (2 supervised and 1 at home) Reps/Sets: 8/3 Duration: 24 weeks Setting: gym and home Supervision: 2 sessions were supervised Adherence: not reported 2. Control Group: maintain usual activities |
|
| Outcomes | Muscle strength (Torques) Comments on adverse events: no |
|
| Notes | Training at ankle joints | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Simons 2006.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 2/21 in the PRT group; 1/21 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 42 (21 in each group) Sample: older adults from independent living facility Age: mean 84.6 years (SD = 4.5) Inclusion criteria: had clearance by the primary physician, lack of regular exercise more than 1 year, and at least 65 years of age Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 3UL/3LL Equipment: Keiser machines Intensity: 75% of 1 RM, increased the load of 5% Frequency: Ex2 Reps/Sets: 10/1 Duration: 16 weeks Setting: fitness center Supervision: full, by trained instructors Adherence: not reported 2. Control Group: controls and Ex group all had 6 one-hour health lectures at 3-week intervals |
|
| Outcomes | Muscle strength (1RM) Flexibility Balance and agibility Eye-hand coordination Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Simpson 1992.
| Methods | RCT Method of randomisation: stratified (don't know how) and randomly assigned Participant blinding: no Assessor blinding: no Loss to follow-up: 6 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Canada N = 34 Sample: people with chronic airflow obstruction Age: mean 73 years (SD 4.8) in PRT group Inclusion criteria: aged 58-80, attending a respiratory outpatient clinic, in a clinically stable state, no recent infective exacerbation, drug management was considered to be optimal, FE to VC ratio of less than 0.7, body weight within 30% of ideal weight, absence of disorders likely to affect exercise, capacity to take part in the training program, Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 1UL, 2LL Equipment: weight-lifting machines Intensity: 50-85% of 1RM Frequency: Ex3 Reps/Sets: 10/3 Program Duration: 8 weeks Setting: gym Supervision: not reported Adherence: 90% 2. Control Group: only attended testing sessions |
|
| Outcomes | Strength (1RM) Spirometry Aerobic capacity (VO2 max) 6-minute walk test Likert scale rating of discomfort during four daily activities (1= extreme disability, 7=none) assessed for fatigue, dyspnoea, emotion and mastery Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Sims 2006.
| Methods | RCT Method of randomisation: by an independent person with a previously block randomised list Assessor blinding: yes Participant blinding: no Loss to follow-up: 6 Intention-to-treat analysis: yes Post-program follow up: yes, at the 6th month |
|
| Participants | Location: Australia N = 32 (14 in PRT) Sample: older adults with depression symptoms Age: mean 74.28 years(SD = 5.87) Inclusion criteria: at least 65 years old; GDS score > 11 Exclusion criteria: unsuitable to exercise according to the score of the Physical Activity Readiness Questionnaire. Alcohol or drug related depression; depression with psychotic features; schizophrenia; bipolar disorder; other psychiatric diagnoses; suicidal ideation; dementia; terminally ill; uncontrolled hypertension, unstable insulin dependent diabetes, and unstable angina. They excluded those currently receiving antidepressants in order to determine the independent impact of PRT |
|
| Interventions | PRT versus control 1. PRT Type of Ex: major UL and LL muscles Equipment: weights Intensity: 80% of 1RM & Borg's perceived exertion scale Frequency: Ex3 Reps/Sets: 8-10/3 Duration: 10 weeks Setting: gym Supervision: full Adherence: 5 attended 2-15 sessions, 7 attended 18-30 sessions 58% meet the adherence criterion of 60% of sessions completed 2. Control group: received ex information (Ex group received it too) |
|
| Outcomes | Human Activity Profile WHO-QOL PASE-functional health status PGMS-well being Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Singh 1997.
| Methods | RCT Method of randomisation: computer-generated list in blocks of five Assessor blinding: all outcomes except strength Participant blinding: no, but attention control group Loss to follow-up: 0 Intention-to-treat analysis: no drop-outs but not stated Post-program follow up: no |
|
| Participants | Location: USA N = 32 Sample: community-dwelling depressed older people Age: mean 70 years (SD 1.5) in PRT group Inclusion criteria: age 60 and over, fulfil DSM-IV diagnostic criteria for either unipolar major or minor depression or dysthymia. Exclusion criteria: dementia, MM SE<23, unstable diseases, bipolar disorder, active psychosis, suicidal plans, currently seeing a psychiatrist, on antidepressant drugs within the last 3 months, participating in any progressive resistance training or in aerobic exercise more than twice a week in the previous month |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2UL, 3LL Equipment: exercise machines (Keiser) Intensity: 80% of 1RM Frequency: Ex3 Reps/Sets: 8/3 Program Duration: 10 weeks Setting: gym Supervision: full Adherence: median 93% 2. Control Group: health education program, 2 times per week for 1 hour |
|
| Outcomes | Sickness Impact Profile Katz ADL scale Lawton Brody IADL scale SF-36 Strength (1RM) Adverse events (chest pain, musculoskeletal pain, medication change, intercurrent illness, hospitalisation, visits to a health professional, worsening of suicidality Comments on adverse events: yes (a priority outcome) |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Singh 2005.
| Methods | RCT with 3 groups: high intensity, low intensity, and control Method of randomisation: by a computer generated random number program in blocks of 15 Assessor blinding: yes Participant blinding: yes Loss to follow-up: 2/20 in the high intensity group; 3/20 in the low intensity group; 1/20 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Australia N = 20 in each group Sample: major or minor depression Age: HI-mean 69 years (SD=5); LI- mean 70 years (SD = 7) Inclusion criteria: aged 60 years; major depression, minor depression, or dysthymia; and had a GDS score at least 14. Exclusion criteria: if demented clinically according to DSM-IV criteria or if their MMSE score was less than 23, if they were suffering from unstable medical disease which would preclude resistance training, had bipolar disorder or active psychosis, or were determined by the study physician to be actively suicidal. They were also excluded if they were currently seeing a psychiatrist, prescribed antidepressant drugs within the last 3 months, or were currently participating in any exercise training more than twice a week |
|
| Interventions | PRT (high intensity versus low intensity) versus control 1. PRT Type of Ex: 3UL/3LL Equipment: Keiser Sports Health Equipment intensity: high intensity group- 80% of 1RM; low intensity group- 20% of 1 RM Frequency: Ex3 Reps/Sets: 8/3 Duration: 8 weeks Setting: outpatient gym in a hospital Supervision: full Adherence: high intensity group: 95-100%; low intensity group: 99-100% 2. Control Group: usual care |
|
| Outcomes | Primary: SF-36 Secondary: muscle strength (1RM) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Sipila 1996.
| Methods | RCT with 3 groups: PRT, control and aerobic training group Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 4 in PRT/controls (8 total) Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Finland N = 42 total (27 in PRT and control) Sample: healthy older women Age: 76-78 years Inclusion criteria: born between 1915-17 (aged 76-78), no severe diseases or functional impairments, no indications against intensive physical exercise (medical exam and exercise test screening) Exclusion criteria: not reported |
|
| Interventions | PRT versus control and versus endurance (aerobic) 1. PRT Type of Ex: 4LL Equipment: variable resistance machines (HUR equipment) Intensity: 60-75% of 1RM Frequency: Ex3 Reps/Sets: 8-10/3-4 Program duration: 18 weeks Setting: gym Supervision: full Adherence: 71-86% (varied depending upon muscle group/exercise type) 2. Control Group: instructed to continue daily routines and not change their physical activity levels 3. Endurance exercise group: 18 weeks of track walking (2 times per week) and step aerobics (once perweek) at 50%-80% of initial maximum heart rate reserve |
|
| Outcomes | Strength Walking speed Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Skelton 1995.
| Methods | RCT Method of randomisation: a random numbers table Assessor blinding: no Participant blinding: no Loss to follow-up: 7 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: UK N = 47 Sample:healthy, independent women Age: median 79.5 years (range 76-93) in PRT group Inclusion criteria: healthy; medically stable; no recent history of cardiovascular, cerebrovascular, respiratory, systemic or muscular disease; any impairment that interfered with mobility, live independently, require not help with ADLs Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 3UL, 6LL Equipment: rice bags and elastic tubing Intensity: resistance increased as soon as participant could complete 3 sets of 8 reps Frequency: Ex3 Reps/Sets: 4-8/ 3 Program duration: 12 weeks Setting: group exercise class 1 day per week, home 2 days Supervision: not reported Adherence: no one attended fewer than 6 classes or 11 home sessions 2. Control Group: asked not to change their activities |
|
| Outcomes | Human Activity Profile Anthropometry Strength (isometric strength and handgrip): such as extensor power Functional reach Chair rise Timed walk Stair walking Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Skelton 1996.
| Methods | RCT Method of randomisation: matched by age then randomised Assessor blinding: no Participant blinding: no Loss to follow-up: 2 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: UK N = 20 Sample: women with functional limitations Age: median 81 years Inclusion criteria: age:75+, from GP practice, have minor or major functional/mobility laminations Exclusion criteria: any disease / condition adversely affected by exercise |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2UL, 6LL Equipment: theraband, cuff-weights Intensity: resistance increased as soon as participant could complete 3 sets of 8 reps Frequency: Ex3 Reps/Sets: 4-8/3 Program Duration: 8 weeks Setting: 1 class per week, 2 home sessions per week Supervision: class supervised, home exercises unsupervised Adherence: no subject performed fewer than 30 complete sessions 2. Control Group: asked not to change activities |
|
| Outcomes | Human Activity Profile Strength (isometric strength and handgrip) 1 -legged balance Chair rise Timed walk Timed up-and-go Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Sousa 2005.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: NA Post-program follow up: no |
|
| Participants | Location: Portugal N = 20 (10 in each group) Sample: healthy men Age: mean 73 years (SD = 6) Inclusion criteria: family physician's approval Exclusion criteria: taking medications that could affect balance, smokers, history of falls, and orthopedic, neurological, cardiac, or pulmonary problems |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 4UL/3LL Equipment: Image Sport Machines Intensity: increased progressively from 50% to 80% of 1RM over the program Frequency: Ex3 Reps/Sets: first 8 weeks: 8-12/2-3; then 6-10/2-3 Duration: 14 weeks Setting: not reported-gym? Supervision: not reported Adherence: 95% 2. Control Group: not reported |
|
| Outcomes | Primary: self-reported disability Secondary: Muscle strength (1 RM), TUAG, functional reach test Comment on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Suetta 2004.
| Methods | RCT Method of randomisation: by a computer program Assessor blinding: On measuring muscle cross-sectional area Participant blinding: not reported Loss to follow-up: 2/13-PRT group, 3/12-Control Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Denmark N = 25 (13 in PRT) Sample: unilateral hip replacement due to OA Age: Mean 71 years Inclusion criteria: age at least of 60 years, and unilateral primary hip replacement due to OA Exclusion criteria: cardiopulmonary, neurological, or cognitive problems |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 2 LL and standard care Equipment: sandbags strapped to the ankle of the operated leg during hospitalization, after day 7, Technogym International machines Intensity: week 0-6, 20 to 12 RM; the last 6 weeks, 8 RM Frequency: daily during hospitalization, Ex3 after day 7 Reps/Sets: week 0-6, 10/ 3-5; the last 6 weeks, 8/3-5 Duration: 12 weeks Setting: not reported Supervision: physical therapist Adherence: not reported 2. Control Group: home-based standard care |
|
| Outcomes | Muscle strength Gait speed Stair climbing Sit-to-stand Comments on adverse events: yes |
|
| Notes | SD was calculated from SE | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Sullivan 2005.
| Methods | RCT Method of randomisation: done by a biostatistician Assessor blinding: yes Participant blinding: yes for the testosterone Loss to follow-up: 2/17 in low resistance group with placebo, 4/17 in high resistance group with placebo Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 17-HI; N = 17-LI Sample: recent functional decline Age: mean 78.2 years (SD = 6.4) Inclusion criteria: recent functional decline, at least 65 years old, serum total testosterone less than 480 ngd/L, and can give informed consent Exclusion criteria: near terminal medical disorder, unresolved malignancy, prostate specific antigen > 10 ngm/L, possibility of prostate cancer, history of prostate cancer, disabling arthritis, neurological diseases or unstable cardiovascular disease |
|
| Interventions | PRT (High intensity versus low intensity) Type of Ex: 2 LL Equipment: Keiser Sport Health Equipment Intensity: low intensity: 20% 1RM; high intensity: 80% of 1 RM Frequency: Ex3 Reps/Sets: 8/3 Duration: 12 weeks Setting: not reported Supervision: not reported Adherence: 99% |
|
| Outcomes | Muscle strength Sit-to-stand Gait speed Stair climb Comments on adverse events: yes |
|
| Notes | Reported absolute change. High-intensity leg exercise led to greater leg strength, No significance in aggregate physical performance score change between any intervention groups. Final score = baseline + change score. Final SD = baseline SD Date from high intensity PRT and low intensity PRT were compared |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Yes | A - Adequate |
Symons 2005.
| Methods | RCT Method of randomisation: random selection with continuing replacement method Assessor blinding: no Participant blinding: not reported Loss to follow-up: 5/14 in isokinetic eccentric group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Canada N = 10-isokinetic concentric; N = 14-isokinetic eccentric Sample: healthy adults Age: mean 72 years Inclusion criteria: free of any debilitating cardiovascular, lower limb musculoskeletal or neuromuscular limitations; had not participated in resistance training for a period of at least 6 months Exclusion criteria: not reported |
|
| Interventions | PRT (isokinet concentric versus excentric) Type of Ex: voluntary contractions of the knee extensors using the specific contraction type of the training group Equipment: Biodex dynamometer Intensity: 10 RM Frequency: Ex3 Reps/Sets: 10/3 Duration: 12 weeks Setting: not reported (Gym?) Supervision: not reported Adherence: 90% |
|
| Outcomes | Muscle strength Stair climb Gait speed Comments on adverse events: yes |
|
| Notes | Eccentric versus concentric | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Taaffe 1996.
| Methods | RCT with 3 groups: high intensity training, low intensity and control (high-intensity only used for main comparisons) Method of randomisation: not reported Participant blinding: no Assessor blinding: no Loss to follow-up: 11 total (5 from HI PRT and control) Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 36 total (23 in control and main PRT group) Sample: healthy older women Age: mean 67 years (SE 0.2) in HI-PRT group Inclusion criteria: female, did not participate in a strength-training program; not taking HRT or on HRT for more than one year Exclusion criteria: evidence of acute or uncontrolled chronic illness or condition that would prevent participation in a resistance training program; presence of vertebral compression fracture; evidence of any disorder that would affect bone metabolism |
|
| Interventions | PRT (high intensity and low intensity) versus control 1. PRT Type of Ex: 3LL Equipment: weight machines (Universal Gym, and Marcy equipment) Intensity: HI-80% of 1RM; LI-40% of 1RM Frequency: Ex3 Reps/Sets: HI= first set at 40% 1RM for 14 reps, last 2 had 7 reps; LI=14/3 Program Duration: 52 weeks Setting: gym Supervision: full Adherence: 79% 2. Control Group: maintain customary dietary and activity patterns |
|
| Outcomes | Strength (1RM), Habitual activity (4 day activity records) Comments on adverse events: no |
|
| Notes | Date from high intensity PRT and low intensity PRT were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Taaffe 1999.
| Methods | RCT with 4 groups, PRT once per week, twice per week, 3 times per week and control (main analyses with 3 times per week and control) Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 7 total (2 in control and Ex3) Intention-to-treat analysis: no Post-program follow up: no, but 24 weeks duration |
|
| Participants | Location: USA N = 46 total (25 in Ex3 and control) Sample: community-dwelling, healthy men and women Age: mean 71.0 years (SD 4.1) in Ex3 group Inclusion criteria: aged 65-79 years, apparently healthy, BMI<30, no musculoskeletal disorder that could inhibit them from exercising, no weight training in previous 12 months, passed medical screening (including maximum exercise stress test) |
|
| Interventions | PRT (at different frequencies) versus control 1. PRT Type of Ex: 6UL, 6LL Equipment: Universal Gym, Marcy and Nautilus equipment Intensity: 80% 1RM Frequency: Ex1, Ex2, Ex3 Reps/Sets: 8/3 Program Duration: 24 weeks Setting: gym Supervision: full Adherence: 97-99% 2. Control Group: maintain customary dietary and activity patterns |
|
| Outcomes | Strength (1RM) Timed backward tandem walk Chair rise Comments on adverse events: no |
|
| Notes | Data from 3 times per week and one time per week group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Topp 1993.
| Methods | RCT (note: results extrapolated from graph) Method of randomisation: not reported Assessor blinding: no Participant blinding: no but attention control group Loss to follow-up: 7 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 63 Sample: community-dwelling men and women Age: mean 69.2 years (SE 0.8) in the PRT group Inclusion criteria: community-dwelling, 65+, Exclusion criteria: cardiopulmonary/ cardiovascular disease, intolerance to exercise, functional disabilities that would contraindicate strength training, unable to commit to a 12-week program, currently involved in strength training more than 1 hour per week |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 6UL, 6LL Equipment: surgical tubing Intensity: low-moderate - increased tubing thickness when they could perform 12 reps of an exercise Frequency: Ex3 Reps/Sets: upper body 10/ 2; lower body 10/3 Program Duration: 12 weeks Setting: exercise class for at least one session per week, home for other session(s) Supervision: full in exercise class, low at home Adherence: 90% 2. Control Group: attended two 3-hour driver education classes, continue usual activities, could have 4weeks of exercise at the end of the trial |
|
| Outcomes | Gait speed Balance (modified Romberg protocol) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Topp 1996.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no, but attention control group Loss to follow-up: 19 Intention-to-treat analysis: no - excluded people who completed <70% of prescribed sessions Post-program follow up: no |
|
| Participants | Location: USA N = 61 Sample: community-dwelling, sedentary Age: mean 70.8 years (SE 1.03) in exercise group Inclusion criteria: community dwelling older adults Exclusion criteria: any contraindications to participating in regular exercise including a history of coronary artery disease, more than one major coronary risk factor or major symptoms or signs of cardiopulmonary or metabolic disease evident during a medically supervised history and physical; already participating in a program of regular resistance training, unable to make a 14-week commitment to the project |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 11 exercises (UL, LL, Tr) Equipment: theraband Intensity: low-moderate - used theraband of a thickness sufficient to produce moderate fatigue during the final 2 reps of an exercise Frequency: Ex3 Reps/Sets: by end of study, 2/10 for UL, 3/10 for LL Program duration: 14 weeks Setting: exercise class at least once per week, home for other session(s) Supervision: full for exercise class, none for home Adherence: 93% (excluding drop-outs) 2. Control Group: two 3-hour supervised driver-education classes |
|
| Outcomes | Strength Postural control (measured using a force plate) Gait speed Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Topp 2002.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 Intention-to-treat analysis: N/A Post-program follow up: no |
|
| Participants | Location: USA N = 35 Sample: adults with knee OA Age: mean = 65.57 years (SD = 1.82) estimated Inclusion criteria: knee pain due to OA (based on WOMAC); physician validated the knee pain and the diagnosis of OA Exclusion criteria: had any contraindications for exercise, including a history of uncontrolled angina, cardiomyopathy severe enough to compromise cardiac functioning, electrolyte or metabolic disturbances, disabilities that prohibited resistance training of the lower extremities, or if they were currently taking nitrates, digitalis, or phenothiazine. Individuals were also excluded if they were currently participating in an organized exercise program or exercised more than 1 hour per week |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 6 LL for 30 minutes Equipment: Thera-Band elastic bands Intensity: self exertion of mild fatigue after 8RM Frequency: Ex3 (2 at home 1 at gym) Reps/Sets: increasing reps and sets every week and then reached 12 reps/3sets at week 9 to 16 Duration: 16 weeks Setting: home and gym Supervision: provided in the gym Adherence: each participant had exercise log, but results were not reported 2. Control Group: no intervention |
|
| Outcomes | WOMAC Knee pain Stair climbing Down and up off the floor Comments on adverse events: no |
|
| Notes | Calculated SDs from reported SEMs | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Topp 2005.
| Methods | RCT with 3 groups: PRT, control, and aerobic groups Method of randomisation: two-coin-flip methodology Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: yes, but the number was not reported Intention-to-treat analysis: not reported Post-program follow up: no |
|
| Participants | Location: USA N = 66 (31 in each group) Sample: older adults with limited functional ability, community dwelling Age: mean 74.1 years (SD = 6.2) Inclusion criteria: score lower then 24 in physical function domain of SF-36 Exclusion criteria: could not climb 26 stairs in 126 seconds; had contraindications to exercise |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 12 exercises Equipment: Thera-Band elastic bands Intensity: self exertion of mild fatigue after 8RM Frequency: Ex3 (2 at home 1 at gym) Reps/Sets: started with 10/1-2, mild fatigue; then increased to 10/3 moderate fatigue at week 8 to week 16 Duration: 16 weeks Setting: home and gym Supervision: provided in the gym Adherence: each participant had exercise log, but results were not reported Participants in the final analysis had 70% compliance rate. 2. Control Group: no intervention, maintain usual activities 3. Aerobic walking group: N=33, 3 times/week; between 50% METs to 75% METs; endurance increasedfrom 10 minutes to 35 minutes |
|
| Outcomes | Arm curls (repetitions) Chair rise (repetitions) Stair ascend/descend Down and up off the floor Comments on adverse events: no |
|
| Notes | Numerical results of SDs were not reported. Data were not pooled | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Tracy 2004.
| Methods | RCT Method of randomisation: not reported Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 (?) Intention-to-treat analysis: N/A Post-program follow up: no |
|
| Participants | Location: USA N = 20 (11 in PRT) Sample: healthy older adults Age: mean 73.1 years (SD = 4.9) Inclusion criteria: no neurological disease, free of medications known to affect the outcome measures; less than 3 hours a week of low to moderate intensity endurance exercise Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex : knee extension, each leg trained separately Equipment: weight-stack machine (Icarian) Intensity: 80% of 1RM Frequency: Ex3 Reps/Sets: 10/3 Duration: 16 weeks Setting: lab Supervision: full Adherence: not reported 2. Control Group: no training involved |
|
| Outcomes | Primary: physical function tests (including gait speed, chair rise, stair ascent/descent) Secondary: muscle strength (1RM) Comments on adverse events: no |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Tsutsumi 1997.
| Methods | RCT with 3 groups: High-intensity PRT, low-intensity PRT, and control Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 1 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 42 total (28 in HI and control) Sample: sedentary, healthy Age: mean 68.9 years (SD 5.7 years) Inclusion criteria: aged 60+, medically healthy, sedentary (no involvement in regular exercise for the previous 6 months) Exclusion criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 7UL/2LL, 2Tr Equipment: dynamic variable resistance weight machines Intensity: HI-75-85% 1RM; LI-55-65% 1RM Frequency: Ex3 Reps/Sets: HI 8-12/2; LI 12-16/2 Program duration: 12 weeks Setting: gym Supervision: full Adherence: not reported 2. Control Group: not reported |
|
| Outcomes | Strength (1RM) Aerobic capacity (VO2 max; bicycle ergometer testing) SF-36 Physical self-efficacy Comments on adverse events: no |
|
| Notes | Date from high intensity PRT and low intensity PRT were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Tyni-Lenne 2001.
| Methods | RCT Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 0 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Sweden N = 24 Sample: people with moderate to severe CHF Age: mean 63 years (SD 9) in PRT group Inclusion criteria: diagnosed with CHF; medically stable CHF in New York Heart Association Class II or III Exclusion criteria: angina pectoris, valvular heart disease determined by Doppler, co-morbidity such as intermittent claudication, diabetes mellitus, chronic obstructive pulmonary disease or any other disorder limiting physical performance other than heart failure |
|
| Interventions | PRT versus control 1. PRT Type of Ex: many UL and LL exercises Equipment: theraband Intensity: low-moderate, used Borg rating scale and increased resistance when people rated peripheral resistance <13 Frequency: Ex3 Reps/Sets: 25/2 Program Duration: 8 weeks Setting: group activity Supervision: full Adherence: 95% 2. Control Group: not reported |
|
| Outcomes | Aerobic capacity (Peak VO2 and 6 minute walk test) Quality of life (Minnesota Living with Heart Failure Index) Comments on adverse events: yes |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Vincent 2002.
| Methods | RCT with 3 groups: High-intensity PRT, low-intensity PRT and control Method of randomisation: stratified by strength, randomised using a random numbers table Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 22 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 38 (in HI group and control); N=36-LL Sample: healthy men and women Age: mean 67 years (SD 7) Inclusion criteria: free from cardiovascular or orthopedic problems that would limit exercise (assessment included physical exam), had not participated in resistance exercise for at least one year Excludion Criteria: not reported |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 5UL/ 6LL Equipment: resistance machines (MedX) Intensity: high intensity: (80% of 1RM); low Intensity: (50% of 1RM) Frequency: Ex3 Reps/Sets: high Intensity: 8/1; low Intensity: 13/1 Program Duration: 6 months Setting: gym Supervision: full Adherence: excluded those who completed less than 85% of sessions 2. Control Group: instructed not to make any changes in their lifestyle during the study |
|
| Outcomes | Strength (1RM) Peak VO2 (update) Stair climb (update) Comments on adverse events: yes |
|
| Notes | Added results from more recent publications Date from high intensity PRT and low intensity PRT were compared |
|
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B- Unclear |
Westhoff 2000.
| Methods | RCT Method of randomisation: not reported Assessor blinding: yes Participant blinding: no Loss to follow-up: 5 Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: The Netherlands N = 26 Sample: low knee-extensor muscle strength Age: mean 75.9 years (SD 6.8) in the exercise group Inclusion criteria: local residents 65 years and over Exclusion criteria: maximum knee extensor torque for both legs >87.5 Nm, self-reported disease or condition such as uncontrolled heart failure or a neurological disease that would be adversely affected by the exercises in the program |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 5UL, 3LL Equipment: resistance training machines Intensity: 75% of 5RM at first, progressed to 8-12RM Frequency: Ex3 Reps/Sets 8-12/1-2 Program Duration: 12 weeks Setting: gym Supervision: not reported Adherence: excluded those who did not have 80% or more attendance 2. Control Group: asked not to make significant changes in their physical activity and nutrition habitsover a 12-week period 3. Aerobic Training: trained on treadmills and cycle ergometers 3 times per week at 60-70% estimatedHR reserve, for 21- 45 minutes per session |
|
| Outcomes | Strength (maximum torque measured by the Quadriso-tester) Gronigen Activity Restriction Scale, an ADL/IADL Index with scores from 18 (no limitations) to 72 (fully dependent) Timed walking test Timed up-and-go Balance (FICSIT balance test, graded from 1-6) Comments on adverse events: yes (asked about complaints during exercise) |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Wieser 2007.
| Methods | RCT Method of randomisation: used www.randomization.com Assessor blinding: not reported Participant blinding: not reported Loss to follow-up: 0 in PRT group, 4/14 in the control group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: Austria N = 28 (14 in each group) Sample: healthy older adults Age: mean 76.2 years (SD = 3.2) Inclusion criteria: older than 70 years, healthy cardio-pulmonary system, untrained Exclusion criteria: participated in a resistance training program; or cardiac arrhythmia, recent myocardial infarct, stroke, cancer, or an ill-treated hypertonia |
|
| Interventions | PRT versus control 1. PRT Type of Ex: 4UL/1LL Equipment: machines Intensity: increase weight after 1 0th repetitions Frequency: Ex2 Reps/sets week 1-4: 8/1 week 5-8: 8/3; week 9-12: 8/4 Duration: 12 weeks Setting: not reported Supervision: not reported Adherence: not reported, provided make-up sessions 2. Control Group: not reported |
|
| Outcomes | VO2max Muscle strength Comments on adverse events: no |
|
| Notes | Numerical results of muscle strength were not reported | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
Wood 2001.
| Methods | RCT with 4 groups: PRT alone, aerobic training alone, combined PRT and aerobic training and control Method of randomisation: not reported Assessor blinding: no Participant blinding: no Loss to follow-up: 9 in four groups - drop outs not reported by group Intention-to-treat analysis: no Post-program follow up: no |
|
| Participants | Location: USA N = 45 total (16 in PRT and control) Sample: healthy older people Age: mean 69.8 years (SD 6) in PRT Inclusion criteria: aged 60-84, no diseases or conditions that would put them at high risk for adverse responses to exercise Inclusion criteria: history of surviving sudden cardiac death, recent myocardial infarction, unstable angina, poorly controlled hypertension, poorly controlled diabetes mellitus, frequent or complex ventricular ec-topy, significant cognitive dysfunction that might interfere with one's ability to adhere to exercise protocols, in the inflammatory stage of arthritis, receiving medical treatment for osteoporosis |
|
| Interventions | PRT versus control and versus aerobic 1. PRT Type of Ex: 5UL, 3LL Equipment: resistance training machines Intensity: 75% of 5RM at first, progressed to 8-12RM Frequency: Ex3 Reps/Sets 8-12 from progressed from 1 set to 2 sets Program Duration: 12 weeks Setting: gym Supervision: not reported Adherence: excluded those who did not have 80% or more attendance 2. Control Group: asked not to make significant changes in their physical activity and nutrition habitsover a 12-week period 3. Aerobic Training: trained on treadmills and cycle ergometers 3 times per week at 60-70% estimatedHR reserve, for 21- 45 minutes per session |
|
| Outcomes | Strength (5RM) Submaximal aerobic capacity Co-ordination Comments on adverse events: no |
|
| Notes | Data from PRT and aerobic training group were compared | |
| Risk of bias | ||
| Item | Authors' judgement | Description |
| Allocation concealment? | Unclear | B - Unclear |
ADL: activities of daily living
Age: overall age of all groups. If this is not available age for progressive resistance training group alone is reported
CHF: congestive heart failure
CHD:coronary heart disease
COPD: chronic obstructive pulmonary disease
Ex: exercise
Ex1: exercise once per week
Ex2: exercise twice per week
Ex3: exercise three times per week
HI: high intensity
MI: Medium intensity
LI: low intensity
LL: lower limb
METs: maximum metabolic equivalents
MMSE: the Mini-Mental State Examination
N: number of participants allocated to strength training group and control group; or number of participants allocated to additional intervention group
NA: not applicable
OA: osteoarthritis
PAD: peripheral arterial disease RCT: Randomised controlled trial
PRT: progressive resistance strength training Reps: repetitions
RM: repetition maximum
SF-36: Medical Outcome Studies 36 Item Short Form questionnaire
Tr: trunk
TUAG: timed “up-and-go” test
UL: upper limb
WOMAC: Western Ontario/McMaster Universities Arthritis Index
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adami 1999 | Not a RCT |
| Adams 2001 | Participants too young (mean age <60) |
| Agre 1988 | Not a RCT |
| Alexander 2003 | Combined program - not PRT alone |
| Aniansson 1981 | Not a RCT |
| Annesi 2004 | Combined intervention program - not PRT alone |
| Ardman 1998 | Not a RCT |
| Ballard 2004 | Combined program - not PRT alone |
| Barbosa 2002 | Not a RCT |
| Baum 2003b | Does not meet criteria for PRT |
| Bean 2002 | Does not meet criteria for PRT |
| Bellew 2003 | Not a RCT |
| Beniamini 1997 | Participants too young (mean age <60) |
| Beniamini 1999 | Participants too young (mean age <60) |
| Berg 1998 | Not a RCT |
| Bernard 1999 | Combined program - not PRT alone |
| Bilodeau 2000 | Participants too young (mean age <60) |
| Binda 2003 | Does not meet for criteria for PRT |
| Binder 2002 | Combined program - not PRT alone |
| Boardley 2007 | No relevant outcomes to the review |
| Braith 2005 | No relevant outcomes to the review |
| Brandon 2003b | Does not meet the criteria for PRT - not progressive |
| Brandon 2004 | Combined program - not PRT alone |
| Brill 1998 | Not a RCT |
| Brose 2003 | Combined program - not PRT alone |
| Brown 1990 | Not a RCT |
| Brown 1991 | Combined program - not PRT alone |
| Brown 2000 | Combined program - not PRT alone |
| Bunout 2001 | Combined program - not PRT alone |
| Campbell 2002 | No relevant outcomes to the review |
| Campbell 2004 | No relevant outcomes to the review |
| Cancela 2003 | Article cannot be located. |
| Candow 2004 | Combined program (with supplement) - not PRT alone |
| Capodaglio 2002 | Not a RCT |
| Carter 2002 | Does not meet the criteria for PRT |
| Carter 2005 | Included participants younger than 60 |
| Carvalho 2002 | No relevant outcomes to the review |
| Cauza 2005 | No relevant outcomes to the review |
| Cauza 2005b | Included young participants (younger than 60 years old) |
| Chaloupka 2000 | Participants too young (mean age <60) |
| Chetlin 2004 | Included young participants (younger than 60 years old) |
| Chiba 2006 | Not a RCT |
| Chien 2005 | Does not meet the criteria for PRT |
| Connelly 1995 | Not a RCT |
| Connelly 2000 | Not a RCT |
| Cramp 2006 | Not a RCT |
| Cress 1991 | Not a RCT |
| Cress 1999 | Combined program - not PRT alone |
| Daepp 2006 | Does not meet the criteria for PRT |
| Daly 2005 | Combined program - not PRT alone |
| de Bruin 2007 | No relevant comparisons to the review |
| de Vito 1999 | Combined program - not PRT alone |
| DeBolt 2004 | Included young participants (younger than 60 years old) |
| Delagardelle 2002 | Combined program - not PRT alone |
| Delecluse 2004 | Combined program - not PRT alone |
| DeVito 2003 | Combined program - not PRT alone |
| Dibble 2006 | Not a RCT |
| Dibble 2006b | Not a RCT |
| Dunstan 2002 | Not PRT alone – with eating plan |
| Dunstan 2005 | Not PRT alone – with eating plan |
| Dupler 1993 | Not a RCT |
| Fernandez Ramirez 99 | Combined program - not PRT alone |
| Ferrara 2006 | Not a RCT |
| Ferri 2003 | Not a RCT |
| Fiatarone 1990 | Not a RCT |
| Fisher 1991 | Not a RCT |
| Forte 2003 | Not a RCT |
| Frontera 1988 Frontera 1990 | Not a RCT Not a RCT |
| Frontera 1990 | Not a RCT |
| Galvao 2006 | Not a RCT |
| Grimby 1992 | Not a RCT |
| Gur 2002 | Included young participants (younger than 60 years old) |
| Hageman 2002 | Not a RCT |
| Hakkinen 1999 | Participants too young (mean age <60) |
| Hameed 2004 | Combined program (with hormone intervention) |
| Hartard 1996 | Not a RCT |
| Haub 2002 | Combined program (protein) - not PRT alone |
| Heiwe 2005 | No relevant outcomes to the review |
| Henwood 2006 | Does not meet the criteria for PRT - not progressive |
| Hess 2005 | Not a RCT |
| Hess 2006 | Not a RCT |
| Hirsch 2003 | Combined program - not PRT alone |
| Host 2007 | Combined program - not PRT alone |
| Huggett 2004 | No relevant outcomes to the review |
| Hughes 2004 | Combined program - not PRT alone |
| Humphries 2000 | Participants too young (mean age <60) |
| Hung 2004 | Does not meet the criteria for PRT |
| Hunter 1995 | Not a RCT |
| Hunter 2002 | Not a RCT |
| Ibanez 2005 | Not a RCT |
| Ivey 2000 | Not a RCT |
| Johansen 2006 | Included young participants (younger than 60 years old) |
| Jones 1987 | Participants too young (mean age <60) |
| Judge 2005 | No relevant outcomes to the review |
| Katula 2006 | Not a RCT |
| Kerr 2001 | No relevant outcomes to the review |
| Kolbe-Alexander 2006 | Not a RCT |
| Komatireddy 1997 | Participants too young (mean age <60) |
| La Forge 2002 | No relevant outcomes to the review |
| Labarque 2002 | Training did not meet criteria for PRT |
| Lambert 2002 | No relevant outcomes to the review |
| Lambert 2003 | Combined program (with hormone) - not PRT alone |
| Lamotte 2005 | No relevant outcomes to the review |
| Levinger 2005 | Included young participants (younger than 60 years old) |
| Lexell 1992 | Not a RCT |
| Lexell 1995 | Not a RCT (not clearly stated that patients were randomised) |
| Littbrand 2006 | Combined program - not PRT alone |
| Liu 2004 | Training did not meet criteria for PRT - not progressive |
| Liu-Ambrose 2004 | No relevant outcomes to the review |
| Loeppky 2005 | Does not meet the criteria for PRT |
| Lohman 1995 | Participants too young (mean age <60) |
| Maddalozzo 2000 | Participants too young (mean age <60) |
| Magnusson 1996 | Participants too young (mean age <60) |
| Marcora 2005 | Not a RCT |
| Martin Ginis 2006 | No relevant comparisons to the review |
| McCool 1991 | Not a RCT |
| McMurdo 1994 | Training did not meet criteria for PRT |
| Mobily 2004 | Not a RCT |
| Morey 1989 | Combined program - not PRT alone |
| Morey 1991 | Combined program - not PRT alone |
| Morse 2005 | Combined program - not PRT alone |
| Narici 1989 | Participants too young (mean age <60) |
| Nelson 1997 | Combined program - not PRT alone |
| Ochala 2005 | Training did not meet criteria for PRT |
| Ohira 2006 | Training did not meet criteria for PRT - not progressive/included young participants |
| Oka 2000 | Combined program - not PRT alone |
| Okawa 2004 | Included younger participants (middle age) |
| Okumiya 1996 | Combined program - not PRT alone |
| Panton 2004 | Combined program - not PRT alone |
| Parsons 1992 | Not a RCT |
| Perhonen 1992 | Training did not meet criteria for PRT |
| Perkins 1961 | Training did not meet criteria for PRT |
| Perrig-Chiello 1998 | No relevant outcomes to the review |
| Petrella 2000 | Training did not meet criteria for PRT |
| Phillips 2004 | Not a RCT |
| Pyka 1994 | Serious threats to internal validity - participants allowed to move from exercise to control group-Not a RCT |
| Rabelo 2004 | Training did not meet criteria for PRT - not progressive |
| Ramsbottom 2004 | Combined program - not PRT alone |
| Reeves 2004b | Does not meet the criteria for PRT |
| Reeves 2005 | Not a RCT |
| Reeves 2006 | Does not meet the criteria for PRT |
| Richards 1996 | Not a RCT |
| Roman 1993 | Not a RCT |
| Rooks 1997 | Training did not meet criteria for PRT |
| Salli 2006 | Training did not meet criteria for PRT - not progressive |
| Sallinen 2006 | Combined program (with diet) - not PRT alone |
| Sanders 1998 | Not a RCT |
| Sartorio 2001 | No relevant outcomes to the review |
| Sauvage 1992 | Combined program - not PRT alone |
| Sayers 2003 | Not a RCT |
| Schott 2006 | Combined program (with supplement) - not PRT alone |
| Sharp 1997 | Not a RCT |
| Shaw 1998 | Not a RCT |
| Sherrington 1997 | Training did not meet criteria for PRT |
| Signorile 2005 | Does not meet the criteria for PRT - not progressive |
| Sinaki 1996 | Participants too young (mean age <60) |
| Sipila 1994 | Not a RCT |
| Spruit 2002 | Combined program - not PRT alone |
| Sullivan 2001 | Not a RCT |
| Taaffe 1997 | Not a RCT |
| Teixeira 2002 | Does not meet the criteria for PRT |
| Teixeira 2003 | Included young participants (younger than 60 years old) |
| Teixeira-Salm. 2005 | Combined program - not PRT alone |
| Thielman 2004 | No relevant outcomes to the review |
| Thomas 2004 | Combined program - not PRT alone |
| Thomas 2005 | Training did not meet criteria for PRT - The resistance was not progressively increased |
| Thompson 1988 | Combined program - not PRT alone |
| Timonen 2002 | Combined program - not PRT alone |
| Timonen 2006 | Combined program - not PRT alone |
| Timonen 2006b | Combined program - not PRT alone |
| Treuth 1994 | Not a RCT |
| Trudelle-Jack. 2004 | Combined program - not PRT alone |
| Tsuji 2000 | Combined program - not PRT alone |
| Vad 2002 | Combined program - not PRT alone |
| Vale 2003 | Article cannot be identified |
| Valkeinen 2005 | Participants too young (mean age of the control group < 60) |
| Van den Ende 2000 | Combined program - not PRT alone |
| Vanbiervliet 2003 | Included young participants (younger than 60 years old) |
| Veloso 2003 | Does not meet the criteria for PRT |
| Verfaillie 1997 | Combined program - not PRT alone |
| Villareal 2003 | Combined program (with hormone)-not PRT alone |
| Villareal 2006b | Combined program - not PRT alone |
| Vincent 2002b | No relevant outcomes to the review |
| Vincent 2003 | No relevant outcomes to the review |
| Vincent 2006 | Included young participants (younger than 60 years old) |
| Woo 2007 | Training did not meet criteria for PRT. The resistance was not progressively increased |
| Yang 2006 | Does not meet the criteria for PRT |
| Zion 2003 | Not a RCT |
RCT = randomised controlled trial; PRT = progressive resistance strength training
Data and Analyses
Comparison 1. PRT versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main function measure (higher score = better function) | 33 | 2172 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [0.05, 0.22] |
| 2 Physical function domain of SF-36/SF-12 (Higher score = better function) | 14 | 778 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [-0.08, 0.21] |
| 3 Activities of daily living measure (higher score = better function) | 3 | 330 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.04 [-0.18, 0.26] |
| 4 Activity level measure (kJ/week) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Main lower limb (LL) strength measure | 73 | 3059 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.67, 1.00] |
| 6 Main measure of aerobic function | 29 | 1138 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [0.09, 0.53] |
| 7 VO2 or peak oxygen uptake | 19 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 VO2max-ml/kg.min | 18 | 710 | Mean Difference (IV, Random, 95% CI) | 1.50 [0.49, 2.51] |
| 7.2 Peak oxygen uptake-L/min | 2 | 47 | Mean Difference (IV, Random, 95% CI) | 0.10 [-0.04, 0.24] |
| 8 Six-minute walk test (meters) | 11 | 325 | Mean Difference (IV, Random, 95% CI) | 52.37 [17.38, 87.37] |
| 9 Balance measures (higher = better balance) | 17 | 996 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [-0.00, 0.25] |
| 10 Balance measures (Low = better balance) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 PRT (high intensity) versus control | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 10.2 PRT (low intensity) versus control | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 11 Gait speed (m/s) | 24 | 1179 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.04, 0.12] |
| 12 Timed walk (seconds) | 8 | 204 | Mean Difference (IV, Fixed, 95% CI) | -0.23 [-1.07, 0.62] |
| 13 Timed “Up-and-Go” (seconds) | 12 | 691 | Mean Difference (IV, Fixed, 95% CI) | -0.69 [-1.11, -0.27] |
| 14 Time to stand from a chair | 11 | 384 | Std. Mean Difference (IV, Random, 95% CI) | -0.94 [-1.49, -0.38] |
| 15 Stair climbing (seconds) | 8 | 268 | Mean Difference (IV, Random, 95% CI) | -1.44 [-2.51, -0.37] |
| 16 Chair stand within time limit (number of times) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17 Vitality (SF-36/Vitality plus scale, higher = more vitality) | 10 | 611 | Mean Difference (IV, Fixed, 95% CI) | 1.33 [-0.89, 3.55] |
| 18 Pain (higher = less pain, Bodily pain on SF-36) | 10 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [-3.44, 4.12] |
| 19 Pain (lower score = less pain) | 6 | 503 | Std. Mean Difference (IV, Fixed, 95% CI) | -0.30 [-0.48, -0.13] |
| 20 Death | 13 | 1125 | Risk Ratio (M-H, Fixed, 95% CI) | 0.89 [0.52, 1.54] |
Comparison 2. High versus low intensity PRT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main function measure (higher score = better function) | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | -0.17 [-0.67, 0.33] |
| 2 Main lower limb (LL) strength measure | 9 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [0.03, 0.93] |
| 3 VO2 Max (ml/kg/min) | 3 | 101 | Mean Difference (IV, Random, 95% CI) | 1.82 [-0.79, 4.43] |
| 4 Pain (higher score = less pain) | 2 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | -0.05 [-0.55, 0.45] |
| 5 Vitality (SF-36, higher score = more vitality) | 2 | 62 | Mean Difference (IV, Fixed, 95% CI) | 6.54 [0.69, 12.39] |
Comparison 3. High versus variable intensity PRT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main lower limb (LL) strength measure | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 VO2 Max (ml/kg/min) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 4. PRT frequency.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main LL strength measure | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Three times versus once per week | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 1.2 Twice versus once per week | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
Comparison 5. PRT: 3-sets versus 1-sets.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main lower limb (LL) strength measure | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Six-minute walk test (meters) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Timed walk (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Time to stand from a chair (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Stair climbing (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 6. PRT versus aerobic training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main function measure (higher score = better function) | 4 | 125 | Std. Mean Difference (IV, Fixed, 95% CI) | -0.21 [-0.56, 0.15] |
| 2 Main function measure (lower score = better function) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Main lower limb strength measure | 10 | 487 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.08, 0.80] |
| 4 VO2 max (ml/kg.min) | 8 | 423 | Mean Difference (IV, Random, 95% CI) | -1.13 [-2.63, 0.38] |
| 5 Six minute walk test (meters) | 2 | 63 | Mean Difference (IV, Fixed, 95% CI) | -4.28 [-48.24, 39. 67] |
| 6 Gait speed (m/s) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Pain (lower score = less pain) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 7. PRT versus functional exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main function measure (higher score = better function) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Main lower limb strength measure | 3 | 158 | Mean Difference (IV, Fixed, 95% CI) | -6.51 [-21.05, 8.04] |
| 3 Timed “Up-and-Go” (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Vitality (SF-36/Vitality plus scale, higher = more vitality) | 2 | 147 | Mean Difference (IV, Fixed, 95% CI) | -0.07 [-2.68, 2.54] |
| 5 Pain (higher = less pain, Bodily pain on SF-36) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 8. PRT versus flexibility training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SF36 (higher score = better function) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Main lower limb (LL) strength measure | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Timed walk (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Time to stand from a chair (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Vitality (SF-36/Vitality plus scale, higher = more vitality) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Pain (higher = less pain, Bodily pain on SF- 36) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 9. Power training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Main lower limb strength measure | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 High intensity (power treatment) versus control (control) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 1.2 High intensity (treatment) versus low intensity (control) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
Comparison 10. PRT versus control supplementary analyses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Strength (grouped by allocation concealment) | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Allocation concealed | 6 | 607 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [-0.04, 0.28] |
| 1.2 Concealment unknown | 67 | 2452 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.56, 0.73] |
| 2 Strength (grouped by assessor blinding) | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Blinded assessors | 19 | 1523 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.23 [0.13, 0.34] |
| 2.2 Assessors were not blinded | 54 | 1536 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.88 [0.77, 0.99] |
| 3 Strength (grouped by intention-to-treat) | 73 | 3059 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.46, 0.61] |
| 3.1 Intention-to-treat was used | 12 | 1041 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.18 [0.06, 0.30] |
| 3.2 Intention-to-treat was not used | 61 | 2018 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.74 [0.64, 0.83] |
| 4 Strength (grouped by attention control) | 73 | 3059 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.46, 0.61] |
| 4.1 Attention control | 24 | 1408 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.34 [0.23, 0.44] |
| 4.2 No attention control | 49 | 1651 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.61, 0.82] |
| 5 Strength (grouped by exercise intensity) | 72 | 3052 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.45, 0.60] |
| 5.1 High intensity | 54 | 2026 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.51, 0.70] |
| 5.2 Low-to-moderate intensity | 19 | 1026 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [0.26, 0.51] |
| 6 Strength (grouped by exercise duration) | 56 | 2564 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.45, 0.61] |
| 6.1 Less than 12 weeks | 20 | 828 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.37, 0.66] |
| 6.2 Longer than 12 weeks | 36 | 1736 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.43, 0.63] |
| 7 Strength (grouped by health status) | 65 | 2428 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.52, 0.69] |
| 7.1 Healthy participants | 46 | 1502 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.77 [0.66, 0.88] |
| 7.2 Older adults with a specific health problem | 19 | 926 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.24, 0.51] |
| 8 Strength (grouped by functional limitations) | 54 | 2133 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.51, 0.70] |
| 8.1 No functional limitations | 41 | 1349 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.81 [0.69, 0.93] |
| 8.2 With functional limitations | 13 | 784 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.30 [0.16, 0.44] |
Analysis 1.1. Comparison 1 PRT versus control, Outcome 1 Main function measure (higher score = better function).
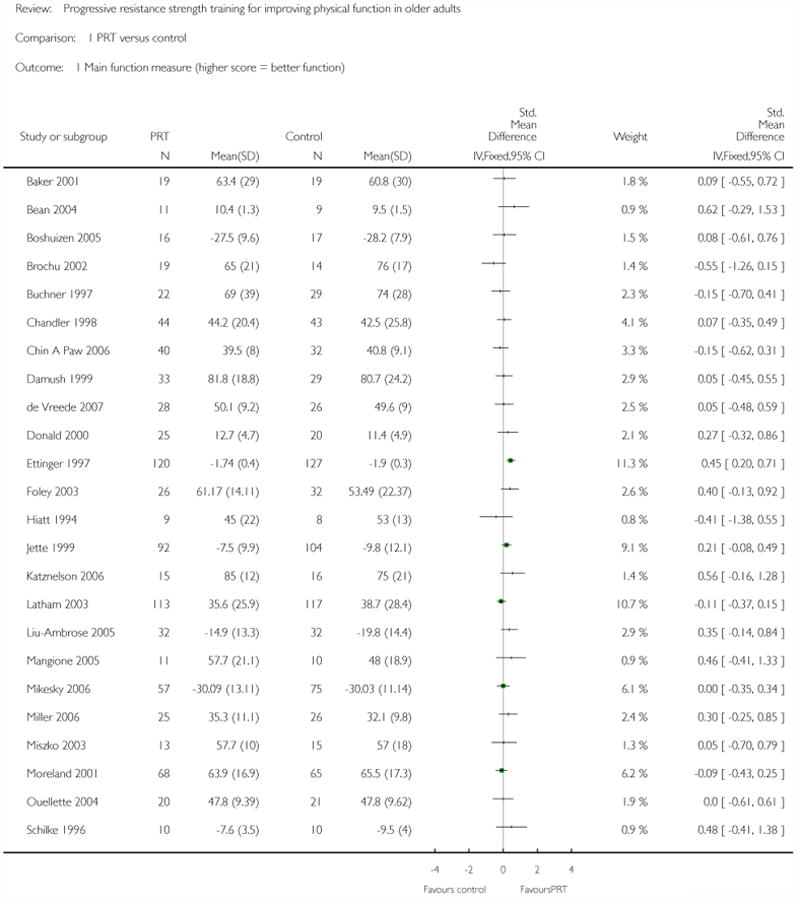
|
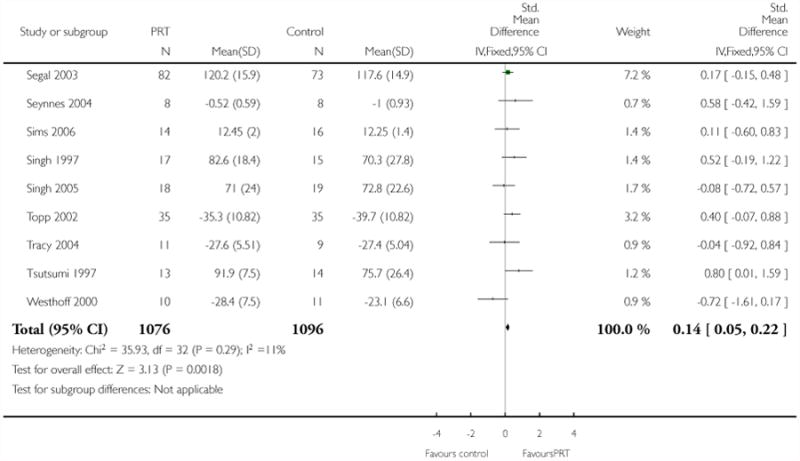
|
Analysis 1.2. Comparison 1 PRT versus control, Outcome 2 Physical function domain of SF-36/SF-12 (Higher score = better function).
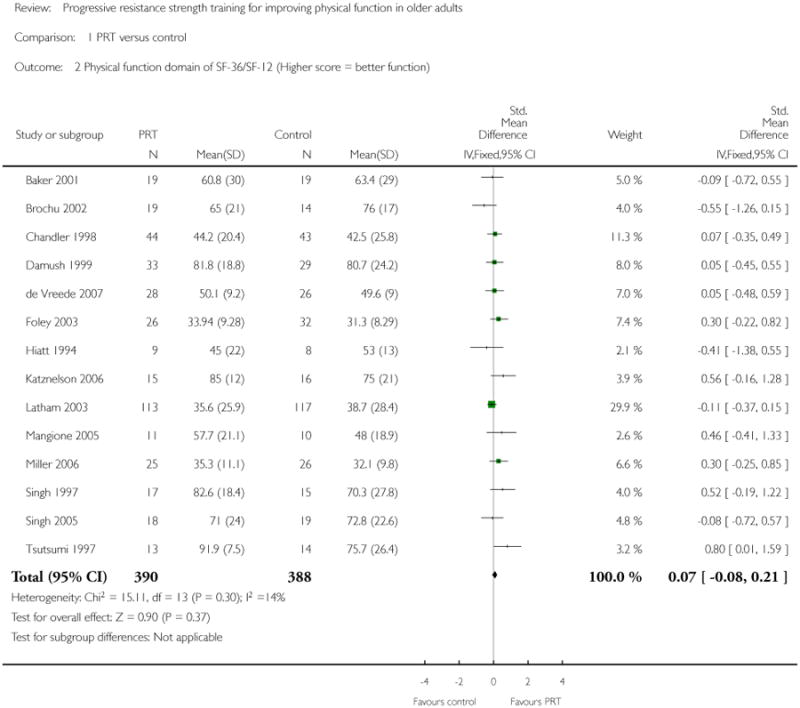
|
Analysis 1.3. Comparison 1 PRT versus control, Outcome 3 Activities of daily living measure (higher score = better function).
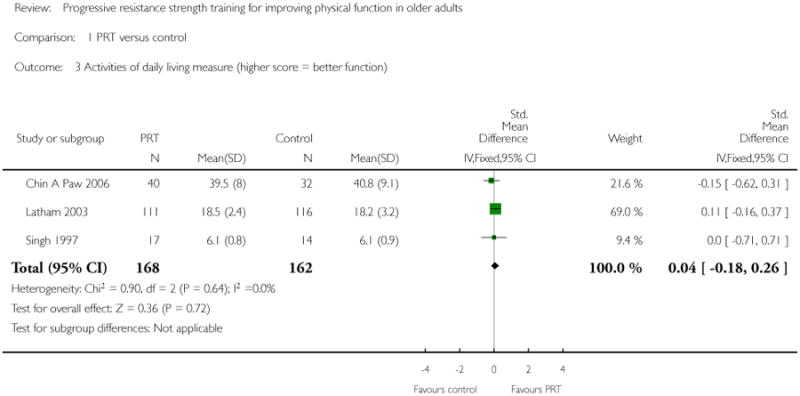
|
Analysis 1.4. Comparison 1 PRT versus control, Outcome 4 Activity level measure (kJ/week).
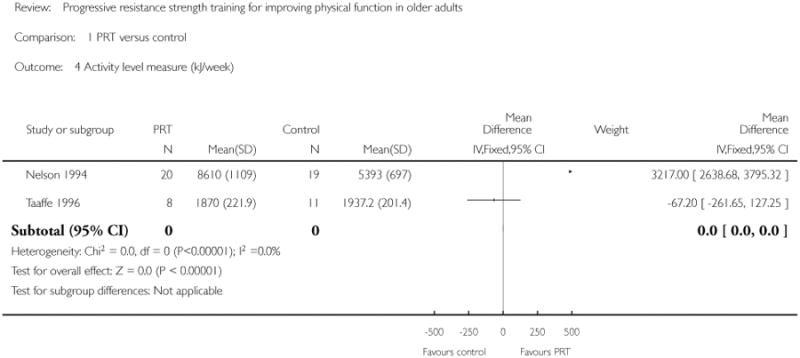
|
Analysis 1.5. Comparison 1 PRT versus control, Outcome 5 Main lower limb (LL) strength measure.
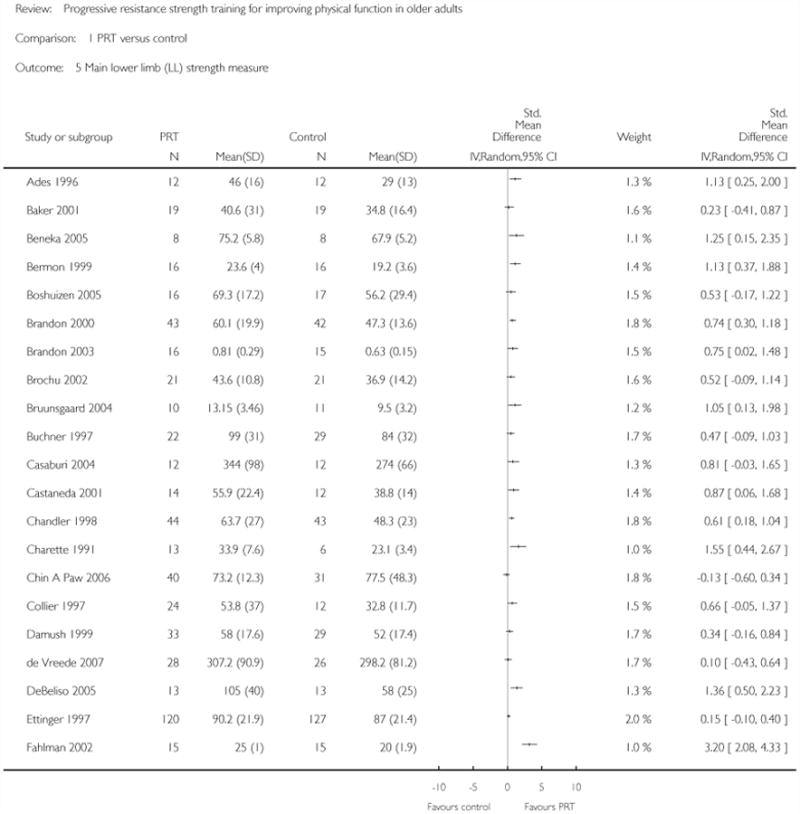
|
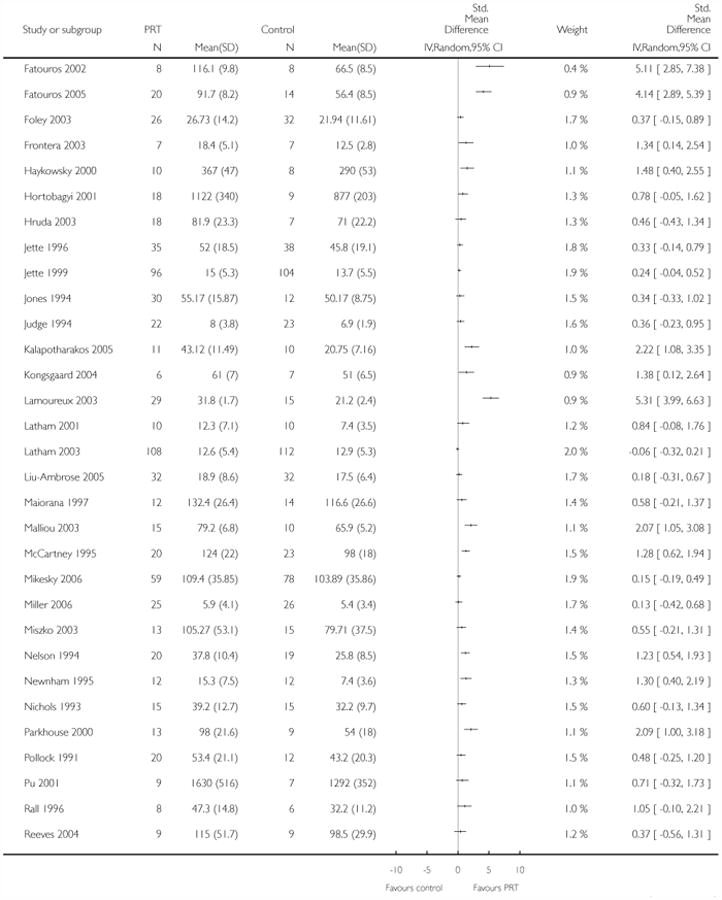
|

|
Analysis 1.6. Comparison 1 PRT versus control, Outcome 6 Main measure of aerobic function.
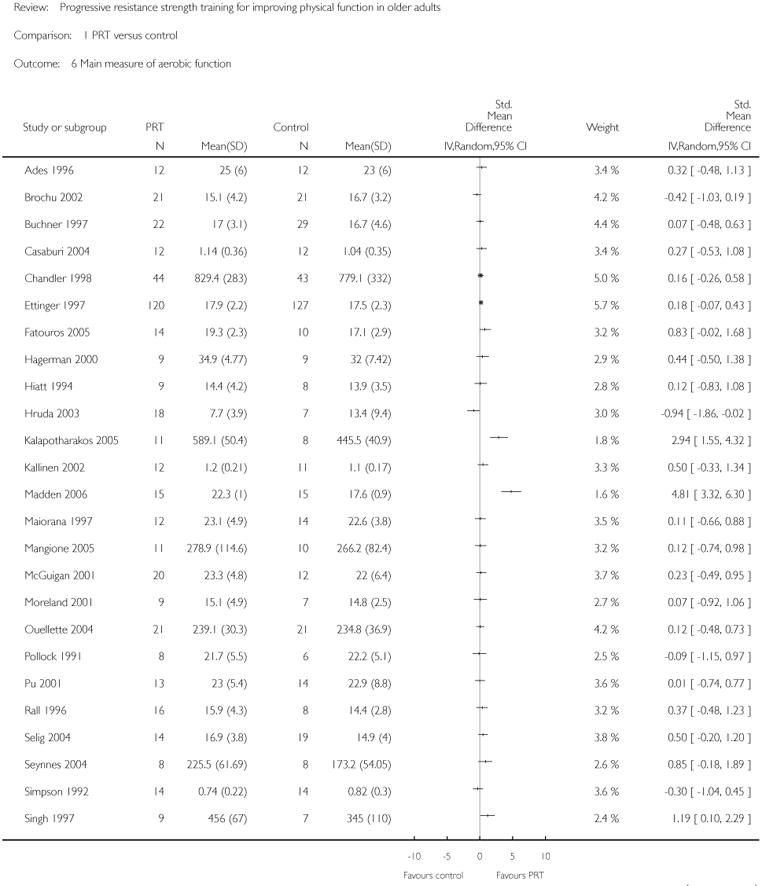
|
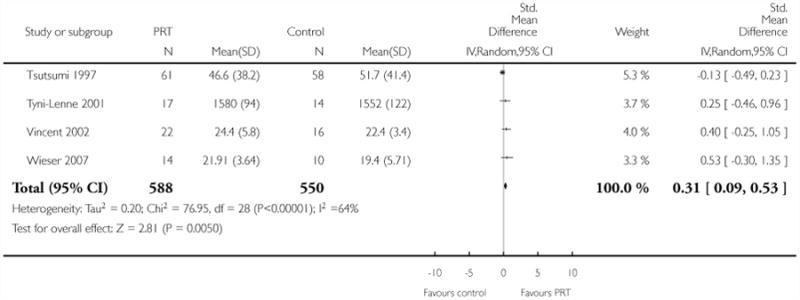
|
Analysis 1.7. Comparison 1 PRT versus control, Outcome 7 VO2 or peak oxygen uptake.
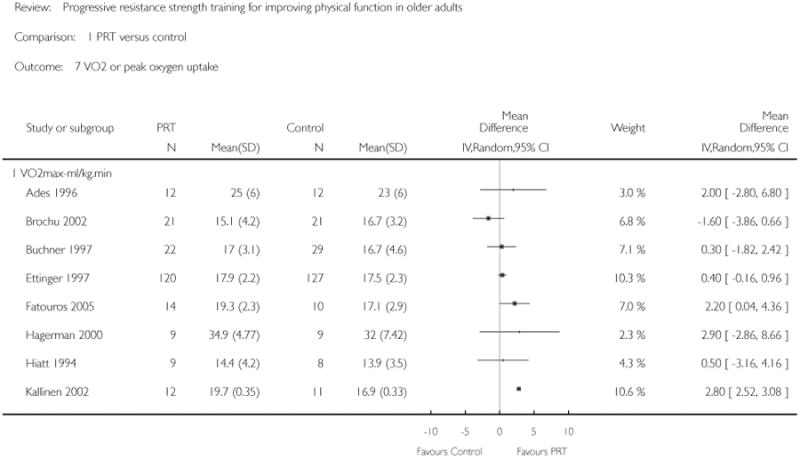
|
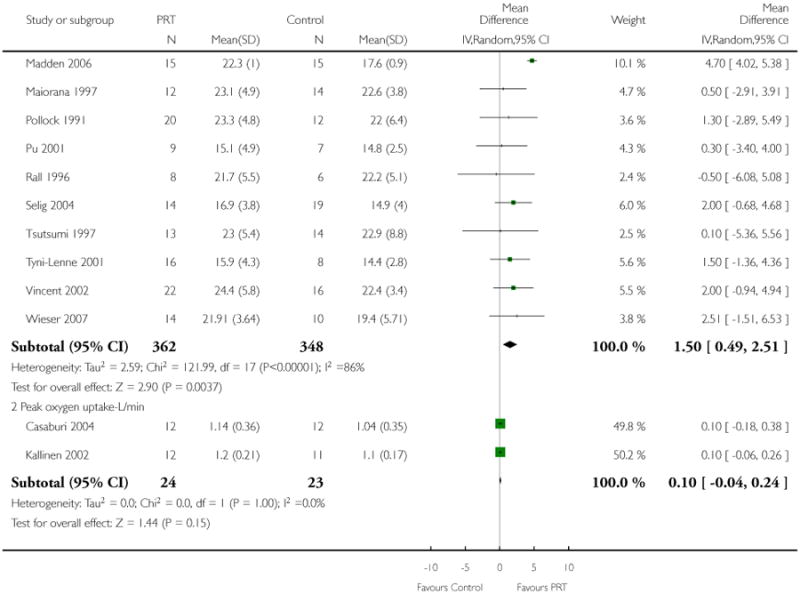
|
Analysis 1.8. Comparison 1 PRT versus control, Outcome 8 Six-minute walk test (meters).
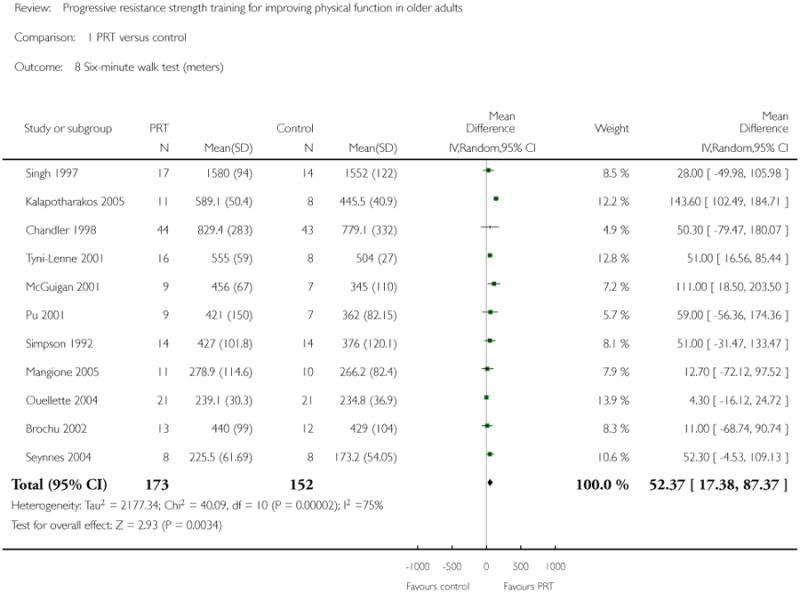
|
Analysis 1.9. Comparison 1 PRT versus control, Outcome 9 Balance measures (higher = better balance).
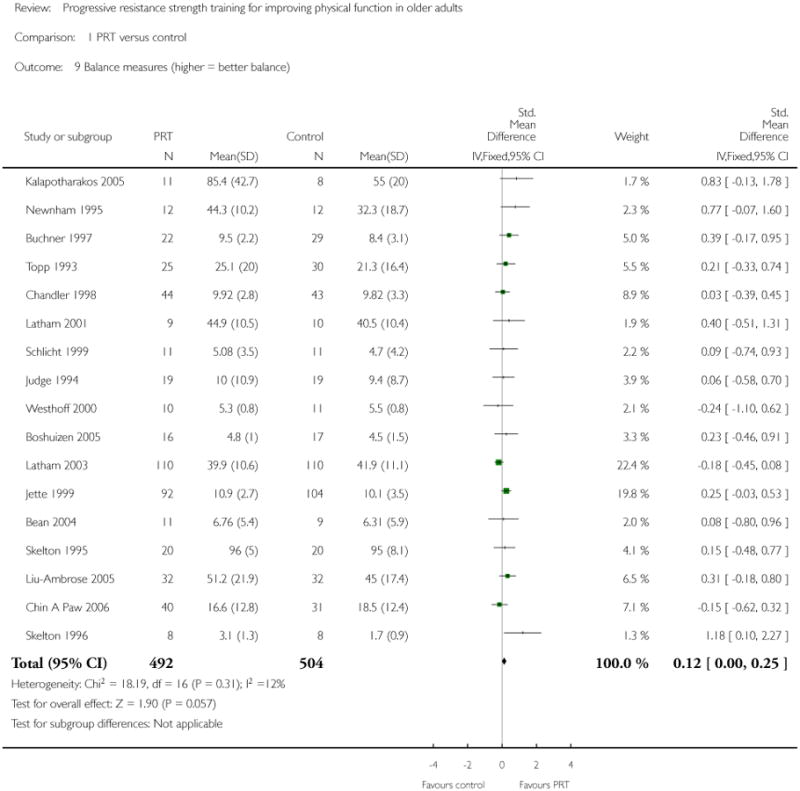
|
Analysis 1.10. Comparison 1 PRT versus control, Outcome 10 Balance measures (Low = better balance).
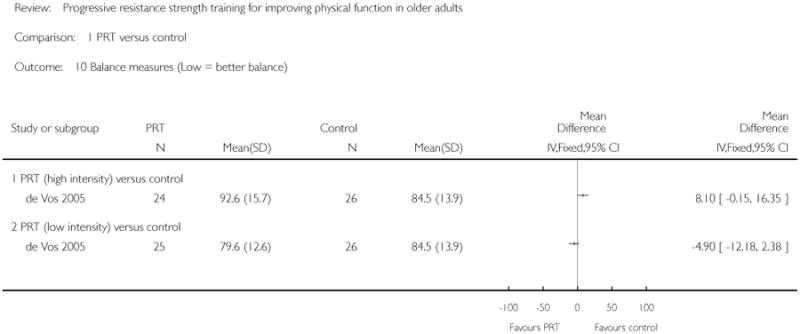
|
Analysis 1.11. Comparison 1 PRT versus control, Outcome 11 Gait speed (m/s).
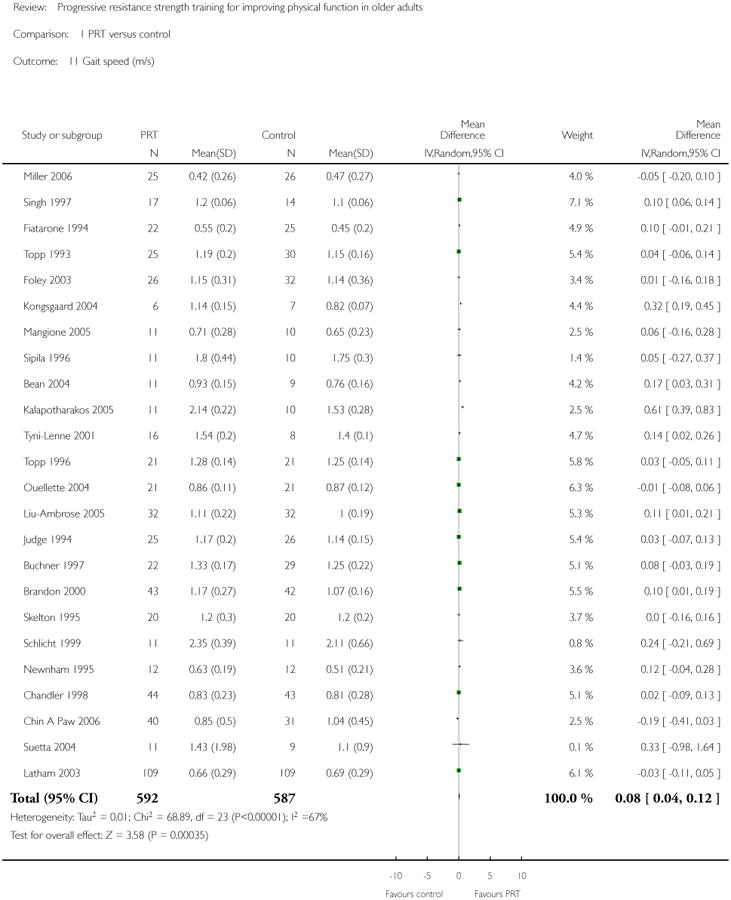
|
Analysis 1.12. Comparison 1 PRT versus control, Outcome 12 Timed walk (seconds).
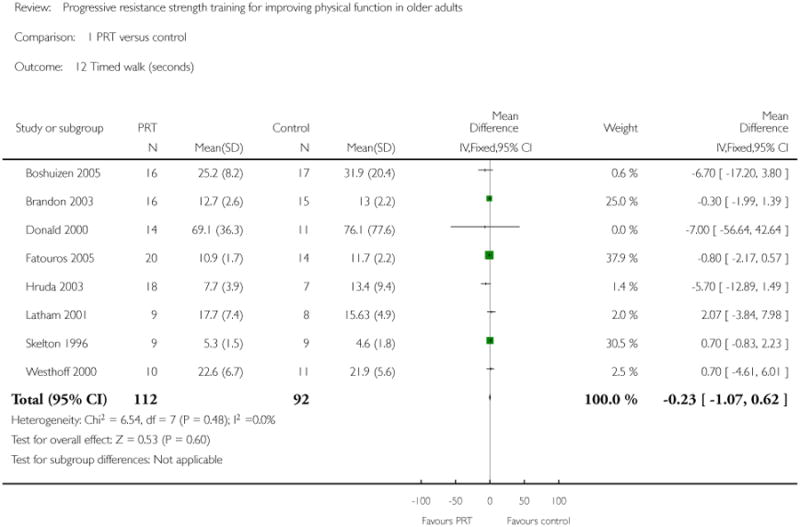
|
Analysis 1.13. Comparison 1 PRT versus control, Outcome 13 Timed “Up-and-Go” (seconds).
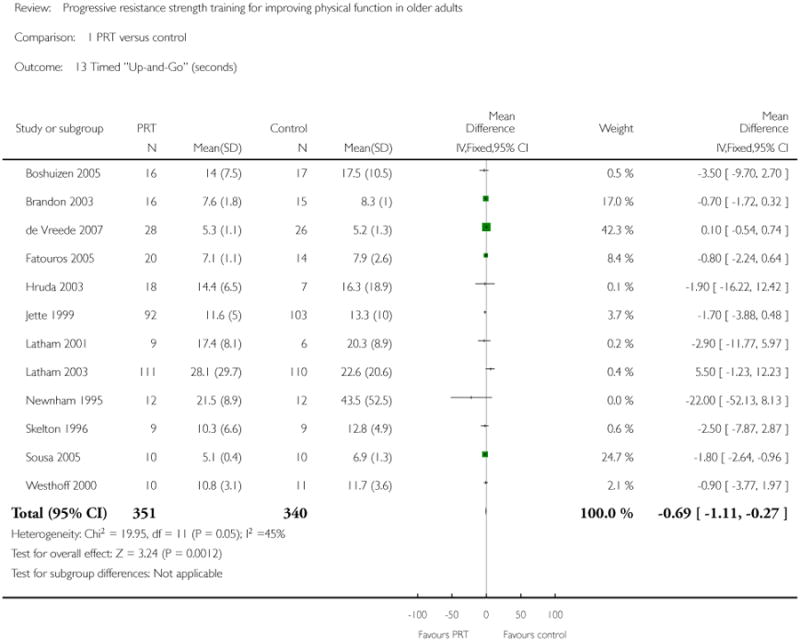
|
Analysis 1.14. Comparison 1 PRT versus control, Outcome 14 Time to stand from a chair.
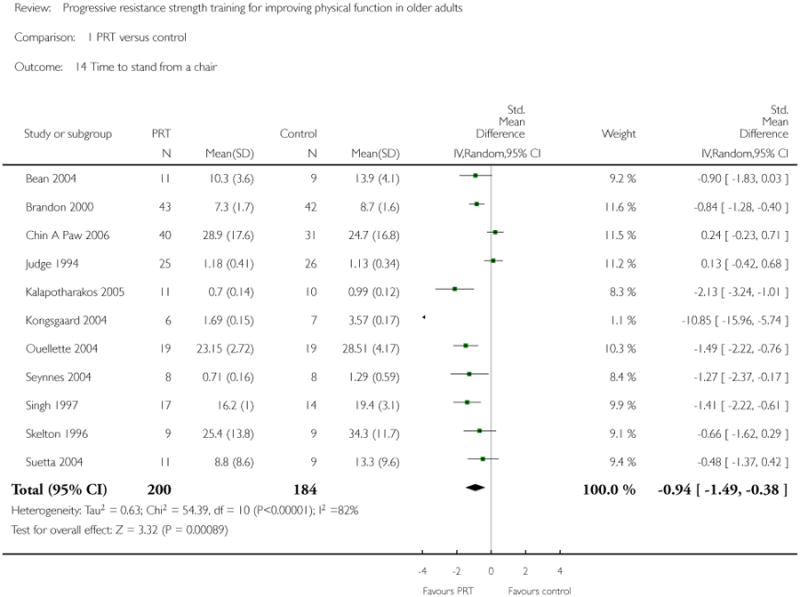
|
Analysis 1.15. Comparison 1 PRT versus control, Outcome 15 Stair climbing (seconds).
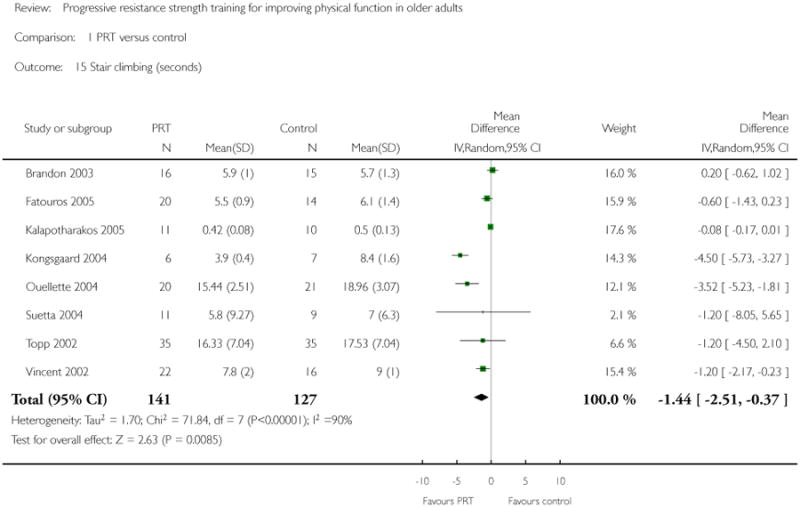
|
Analysis 1.16. Comparison 1 PRT versus control, Outcome 16 Chair stand within time limit (number of times).
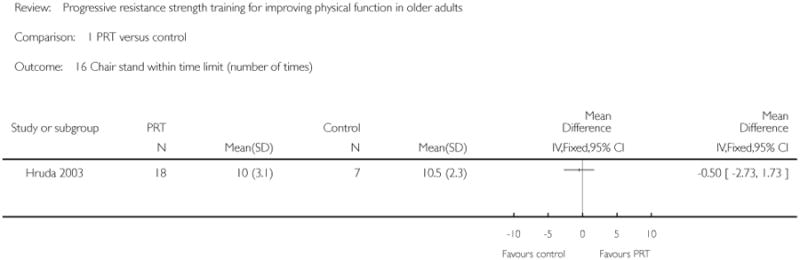
|
Analysis 1.17. Comparison 1 PRT versus control, Outcome 17 Vitality (SF-36/Vitality plus scale, higher = more vitality).
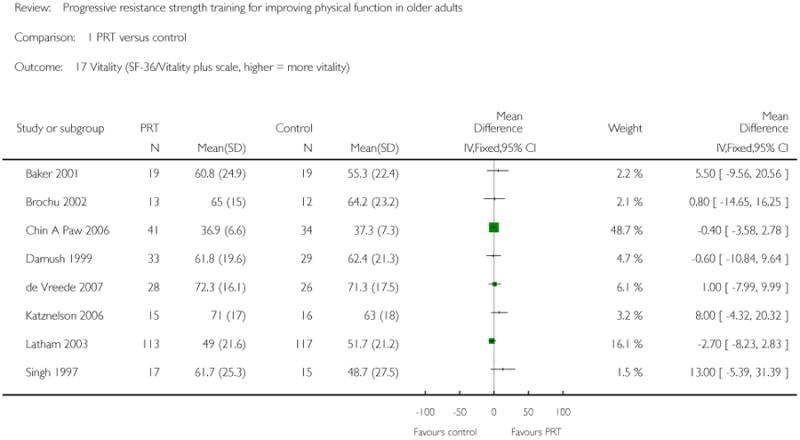
|
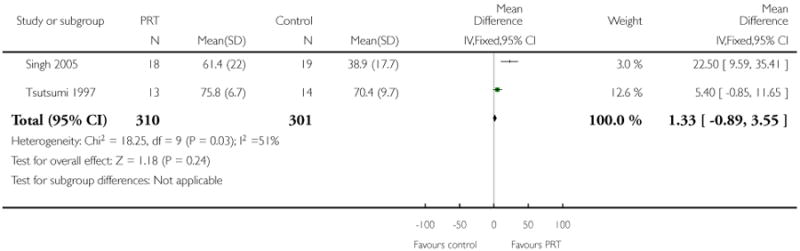
|
Analysis 1.18. Comparison 1 PRT versus control, Outcome 18 Pain (higher = less pain, Bodily pain on SF-36).
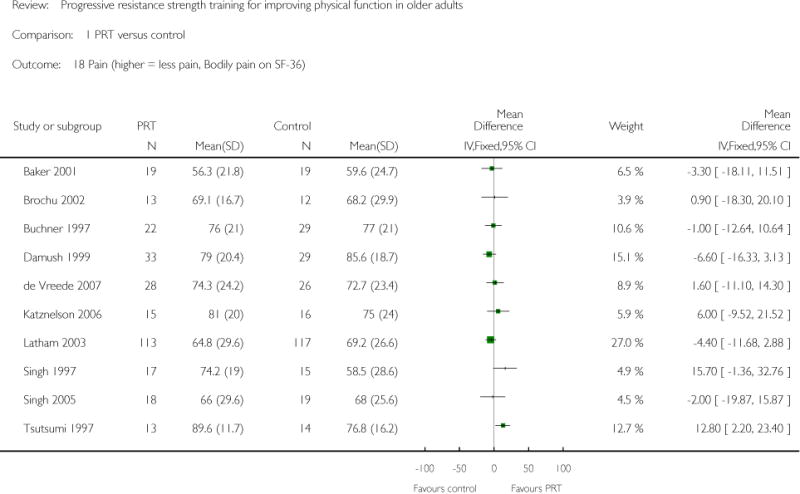
|
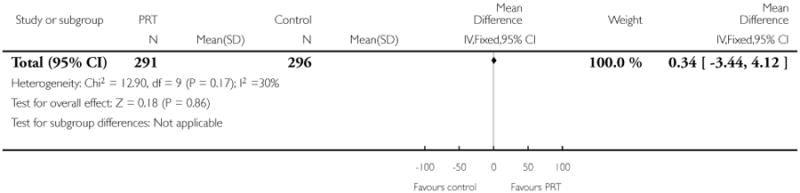
|
Analysis 1.19. Comparison 1 PRT versus control, Outcome 19 Pain (lower score = less pain).
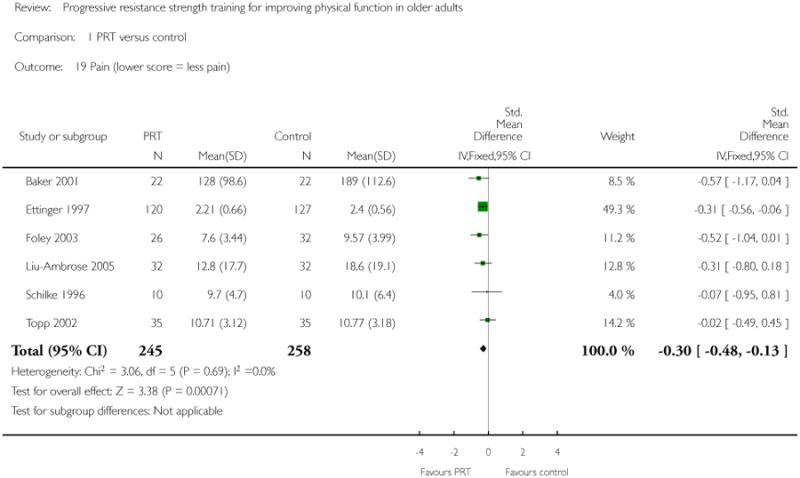
|
Analysis 1.20. Comparison 1 PRT versus control, Outcome 20 Death.
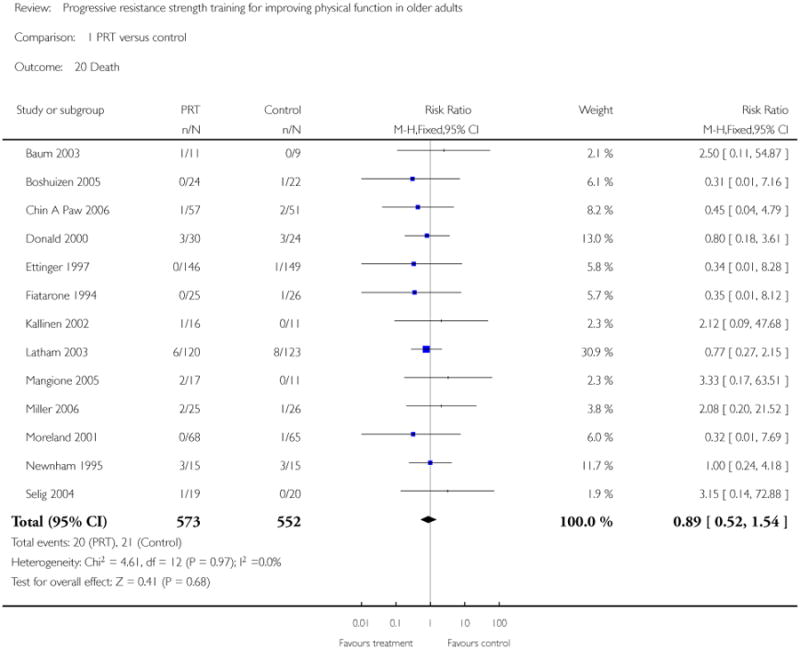
|
Analysis 2.1. Comparison 2 High versus low intensity PRT, Outcome 1 Main function measure (higher score = better function).
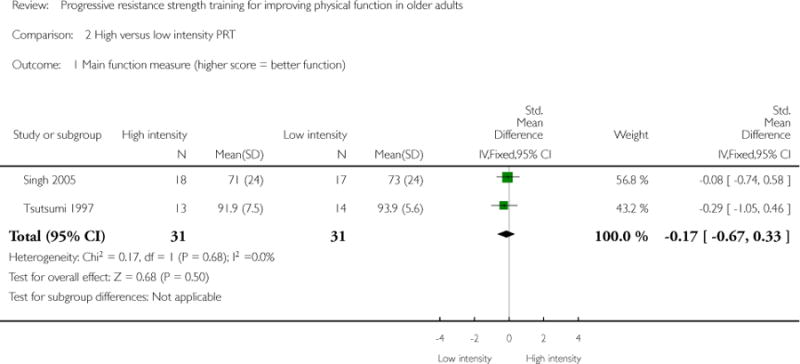
|
Analysis 2.2. Comparison 2 High versus low intensity PRT, Outcome 2 Main lower limb (LL) strength measure.
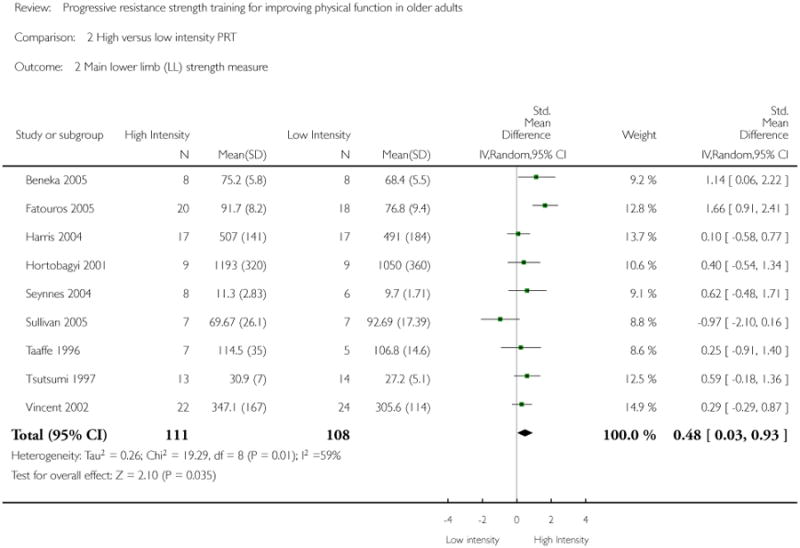
|
Analysis 2.3. Comparison 2 High versus low intensity PRT, Outcome 3 VO2 Max (ml/kg/min).
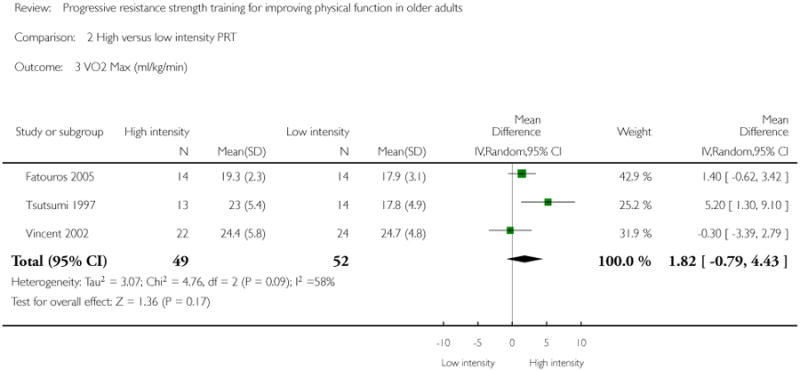
|
Analysis 2.4. Comparison 2 High versus low intensity PRT, Outcome 4 Pain (higher score = less pain).
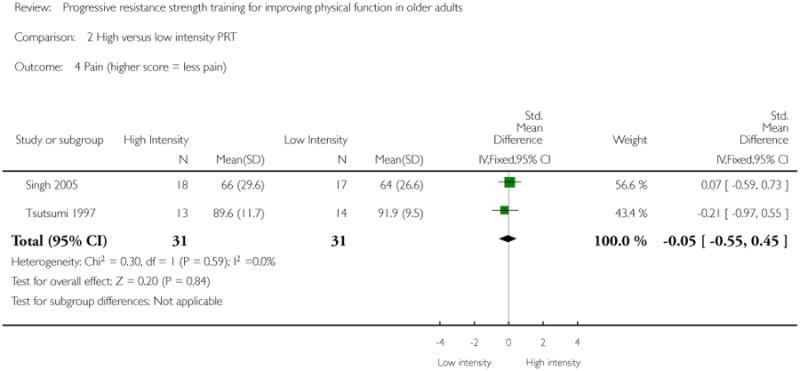
|
Analysis 2.5. Comparison 2 High versus low intensity PRT, Outcome 5 Vitality (SF-36, higher score = more vitality).
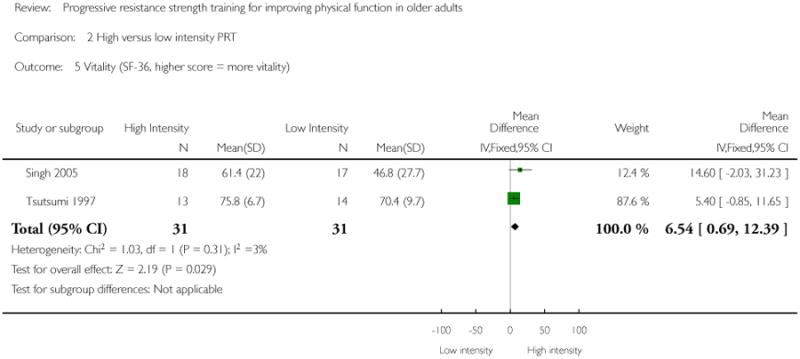
|
Analysis 3.1. Comparison 3 High versus variable intensity PRT, Outcome 1 Main lower limb (LL) strength measure.
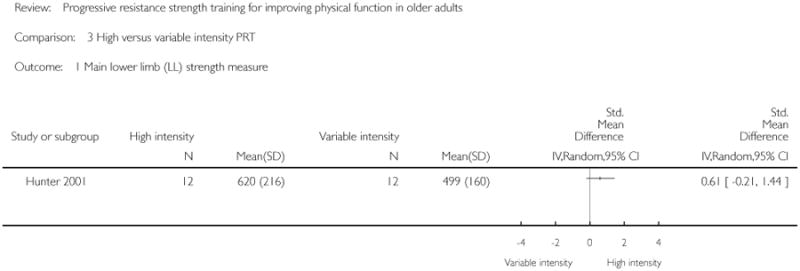
|
Analysis 3.2. Comparison 3 High versus variable intensity PRT, Outcome 2 VO2 Max (ml/kg/min).
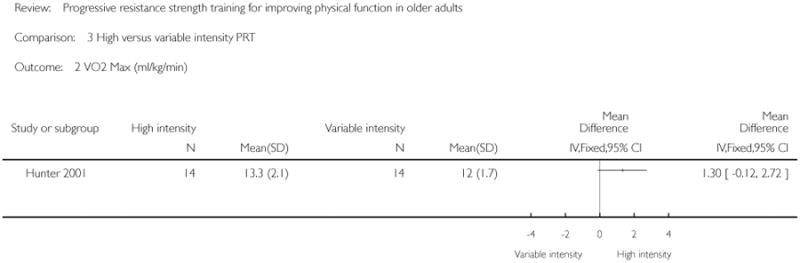
|
Analysis 4.1. Comparison 4 PRT frequency, Outcome 1 Main LL strength measure.
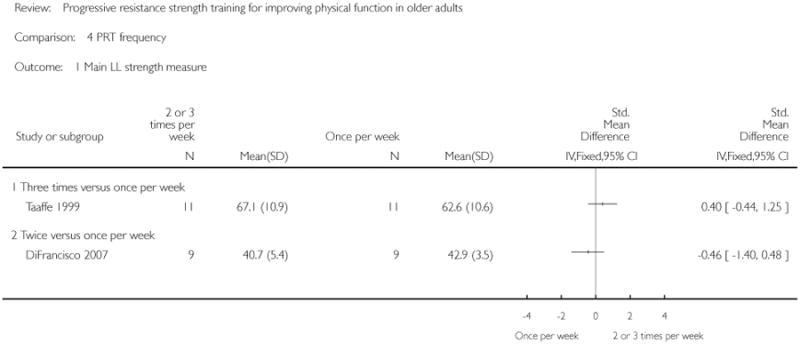
|
Analysis 5.1. Comparison 5 PRT: 3-sets versus 1-sets, Outcome 1 Main lower limb (LL) strength measure.
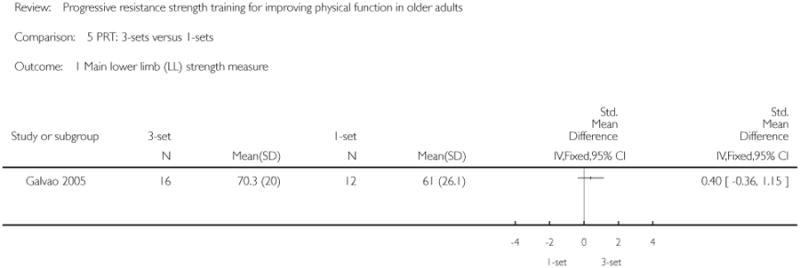
|
Analysis 5.2. Comparison 5 PRT: 3-sets versus 1-sets, Outcome 2 Six-minute walk test (meters).
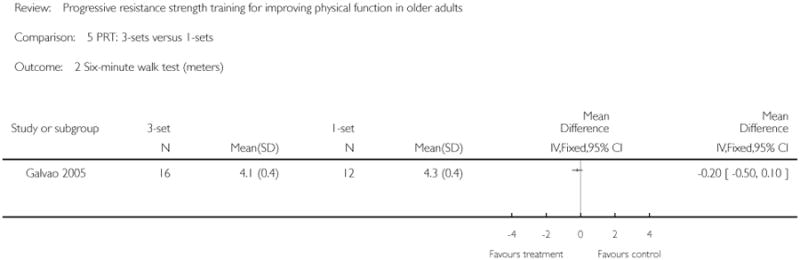
|
Analysis 5.3. Comparison 5 PRT: 3-sets versus 1-sets, Outcome 3 Timed walk (seconds).
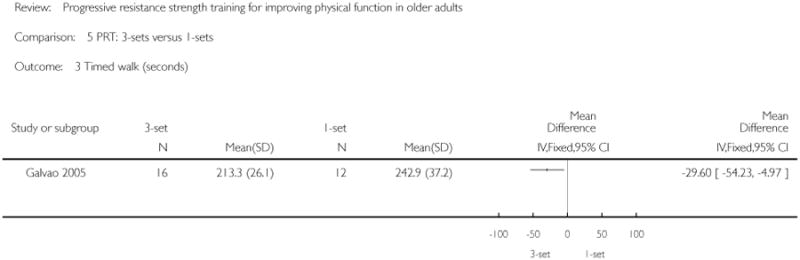
|
Analysis 5.4. Comparison 5 PRT: 3-sets versus 1-sets, Outcome 4 Time to stand from a chair (seconds).
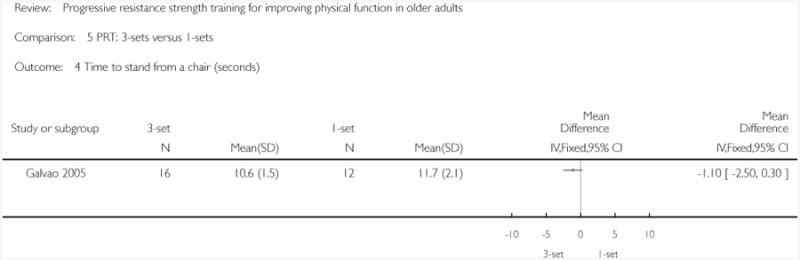
|
Analysis 5.5. Comparison 5 PRT: 3-sets versus 1-sets, Outcome 5 Stair climbing (seconds).
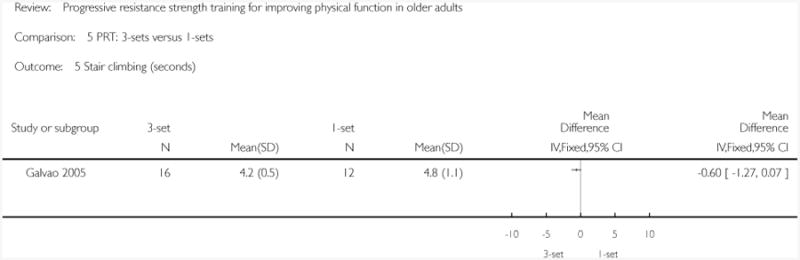
|
Analysis 6.1. Comparison 6 PRT versus aerobic training, Outcome 1 Main function measure (higher score = better function).
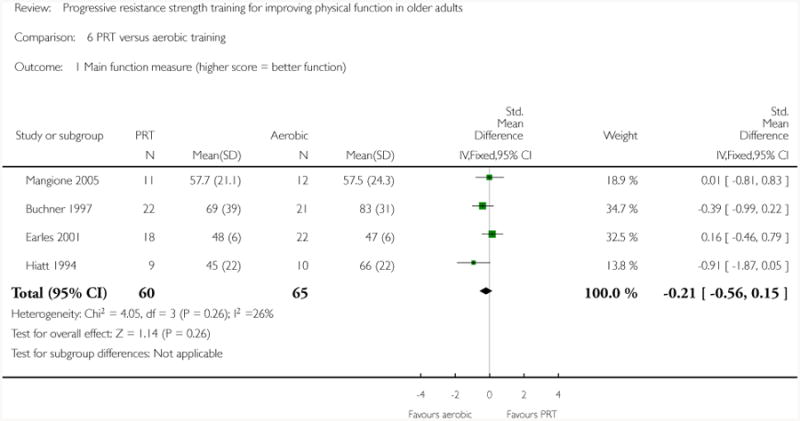
|
Analysis 6.2. Comparison 6 PRT versus aerobic training, Outcome 2 Main function measure (lower score = better function).
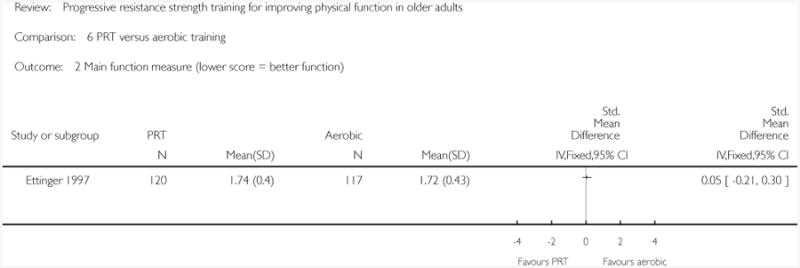
|
Analysis 6.3. Comparison 6 PRT versus aerobic training, Outcome 3 Main lower limb strength measure.
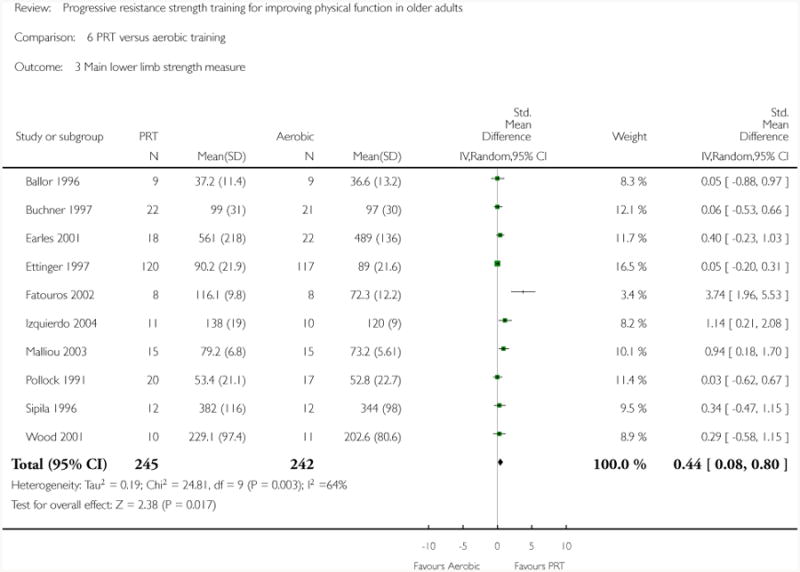
|
Analysis 6.4. Comparison 6 PRT versus aerobic training, Outcome 4 VO2 max (ml/kg.min).
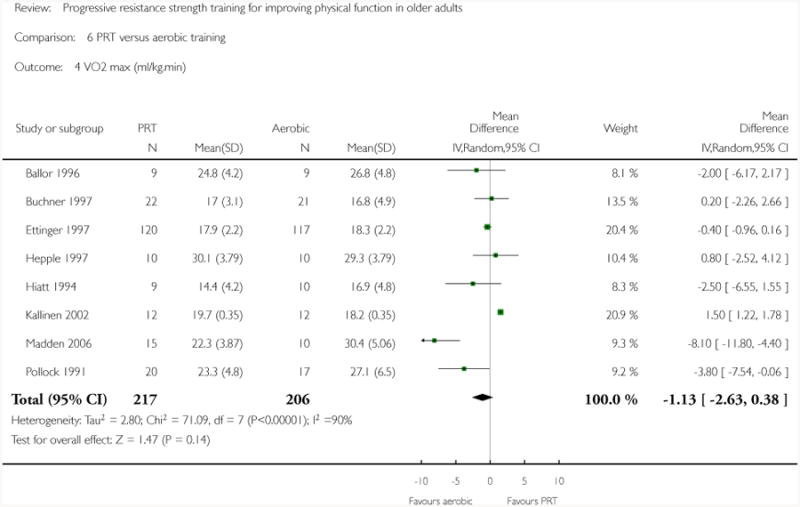
|
Analysis 6.5. Comparison 6 PRT versus aerobic training, Outcome 5 Six minute walk test (meters).
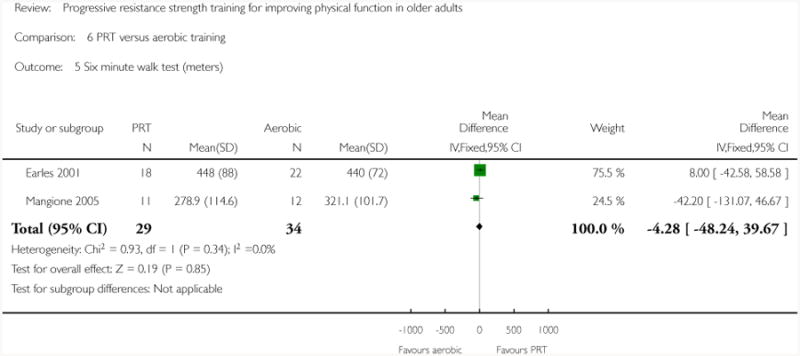
|
Analysis 6.6. Comparison 6 PRT versus aerobic training, Outcome 6 Gait speed (m/s).
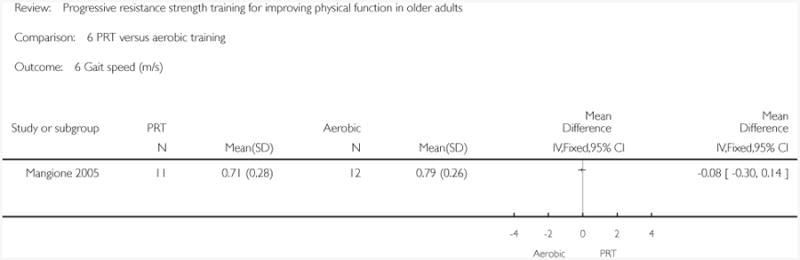
|
Analysis 6.7. Comparison 6 PRT versus aerobic training, Outcome 7 Pain (lower score = less pain).

|
Analysis 7.1. Comparison 7 PRT versus functional exercise, Outcome 1 Main function measure (higher score = better function).
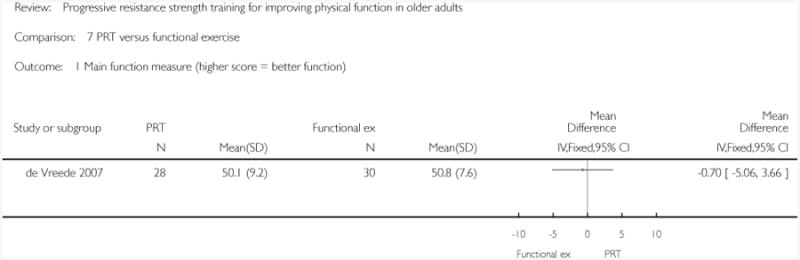
|
Analysis 7.2. Comparison 7 PRT versus functional exercise, Outcome 2 Main lower limb strength measure.
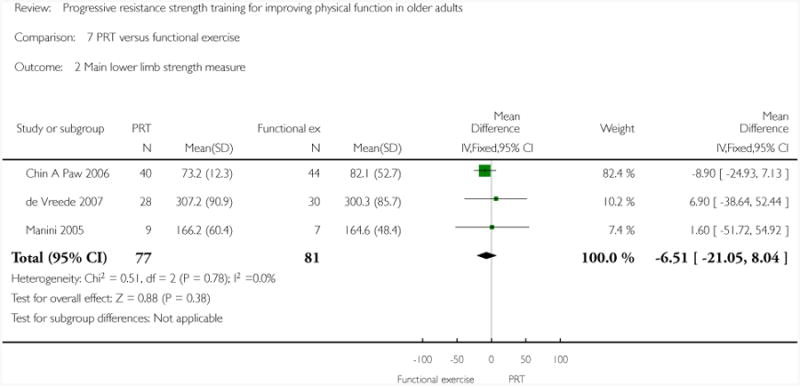
|
Analysis 7.3. Comparison 7 PRT versus functional exercise, Outcome 3 Timed “Up-and-Go” (seconds).
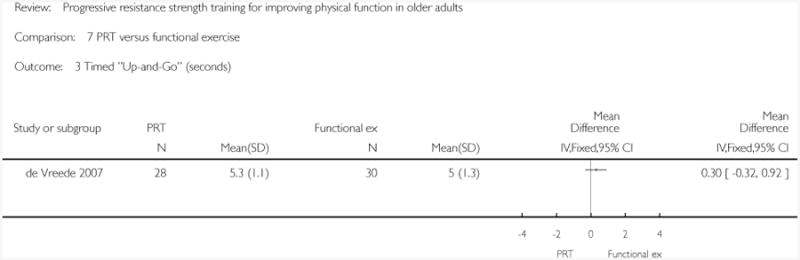
|
Analysis 7.4. Comparison 7 PRT versus functional exercise, Outcome 4 Vitality (SF-36/Vitality plus scale, higher = more vitality).
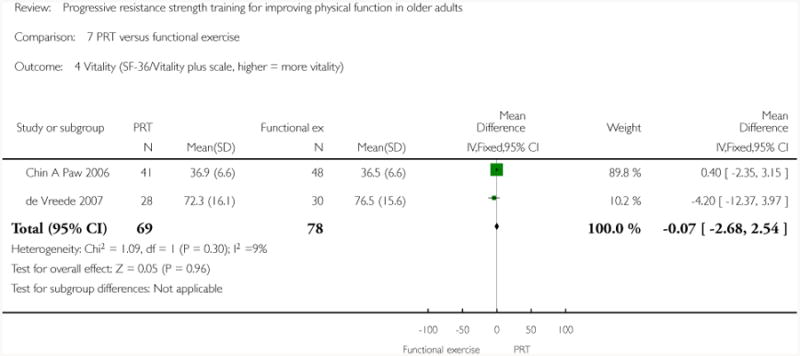
|
Analysis 7.5. Comparison 7 PRT versus functional exercise, Outcome 5 Pain (higher = less pain, Bodily pain on SF-36).
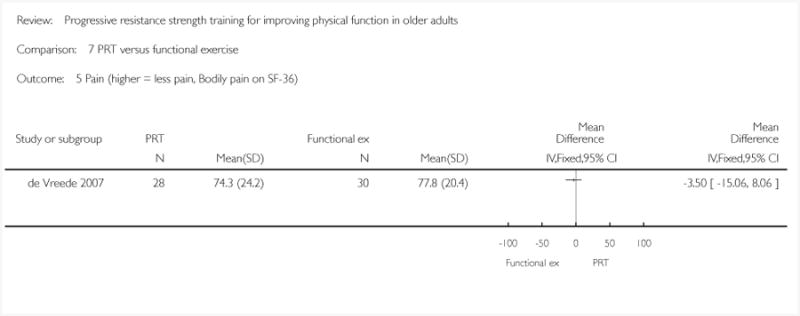
|
Analysis 8.1. Comparison 8 PRT versus flexibility training, Outcome 1 SF36 (higher score = better function).
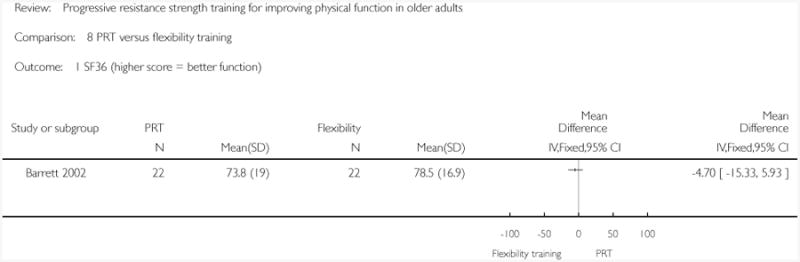
|
Analysis 8.2. Comparison 8 PRT versus flexibility training, Outcome 2 Main lower limb (LL) strength measure.
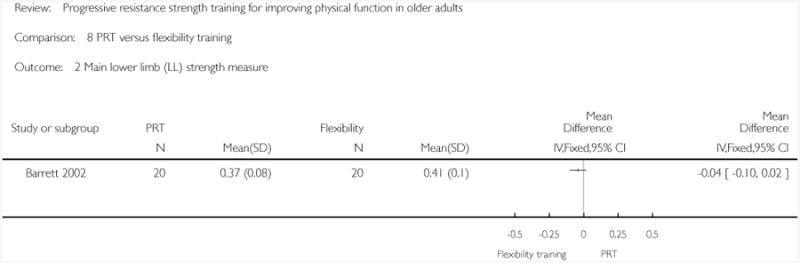
|
Analysis 8.3. Comparison 8 PRT versus flexibility training, Outcome 3 Timed walk (seconds).
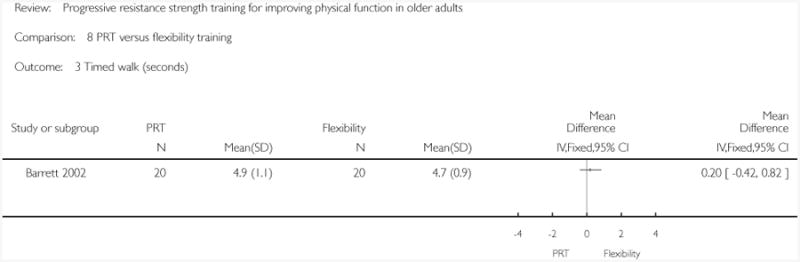
|
Analysis 8.4. Comparison 8 PRT versus flexibility training, Outcome 4 Time to stand from a chair (seconds).
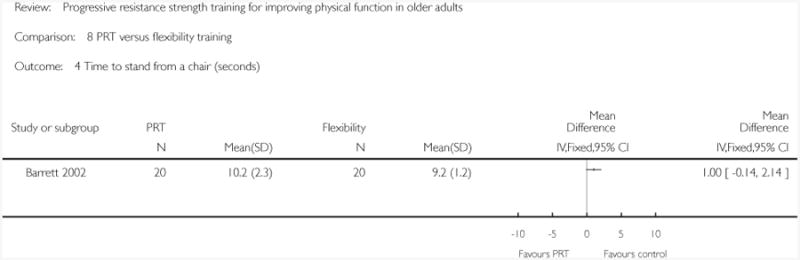
|
Analysis 8.5. Comparison 8 PRT versus flexibility training, Outcome 5 Vitality (SF-36/Vitality plus scale, higher = more vitality).
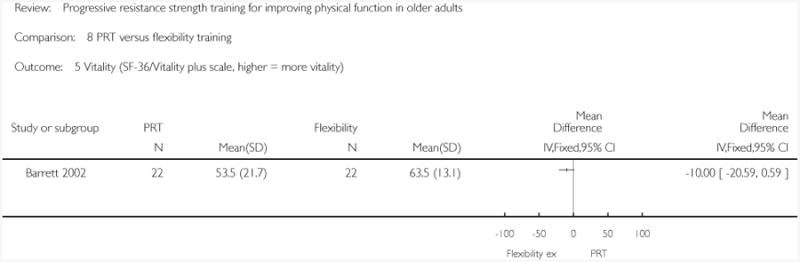
|
Analysis 8.6. Comparison 8 PRT versus flexibility training, Outcome 6 Pain (higher = less pain, Bodily pain on SF- 36).
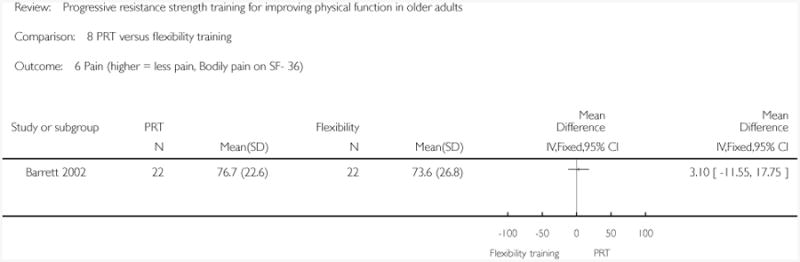
|
Analysis 9.1. Comparison 9 Power training, Outcome 1 Main lower limb strength measure.
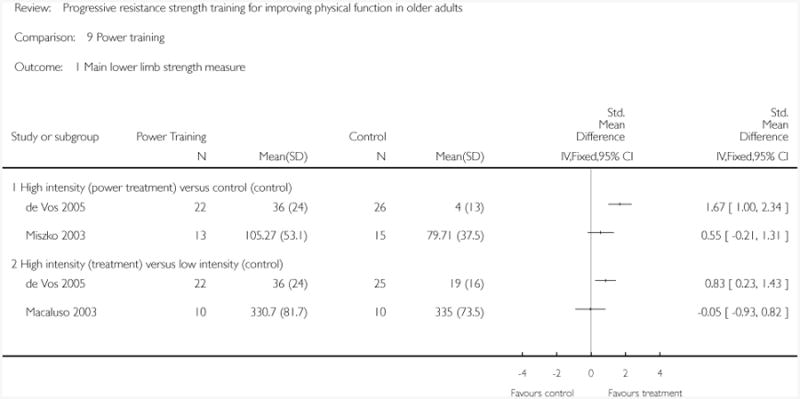
|
Analysis 10.1. Comparison 10 PRT versus control supplementary analyses, Outcome 1 Strength (grouped by allocation concealment).
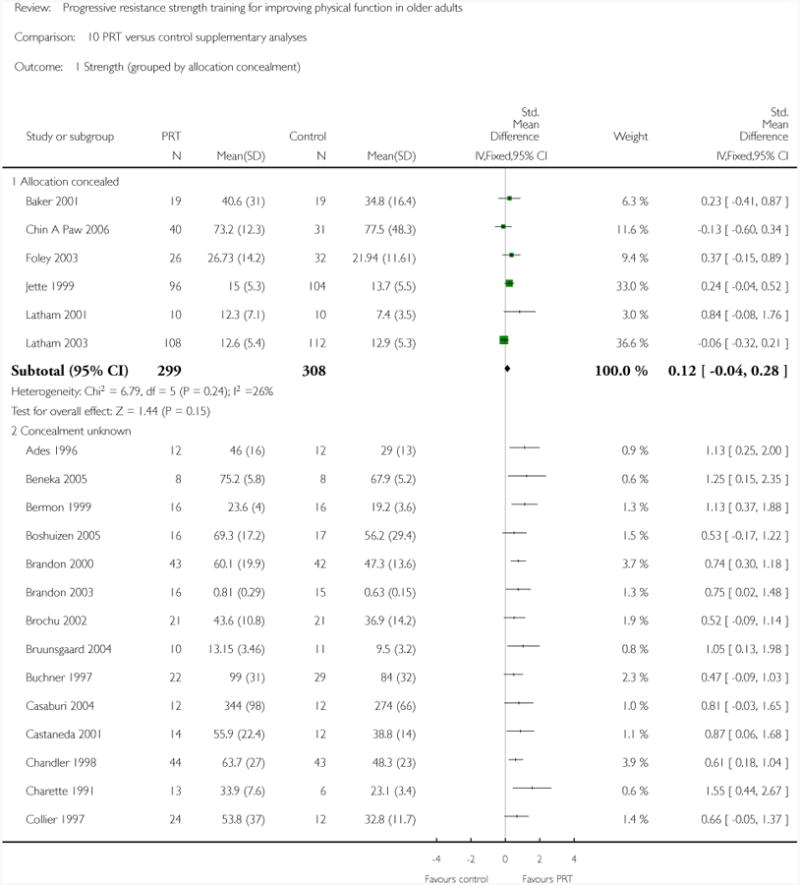
|
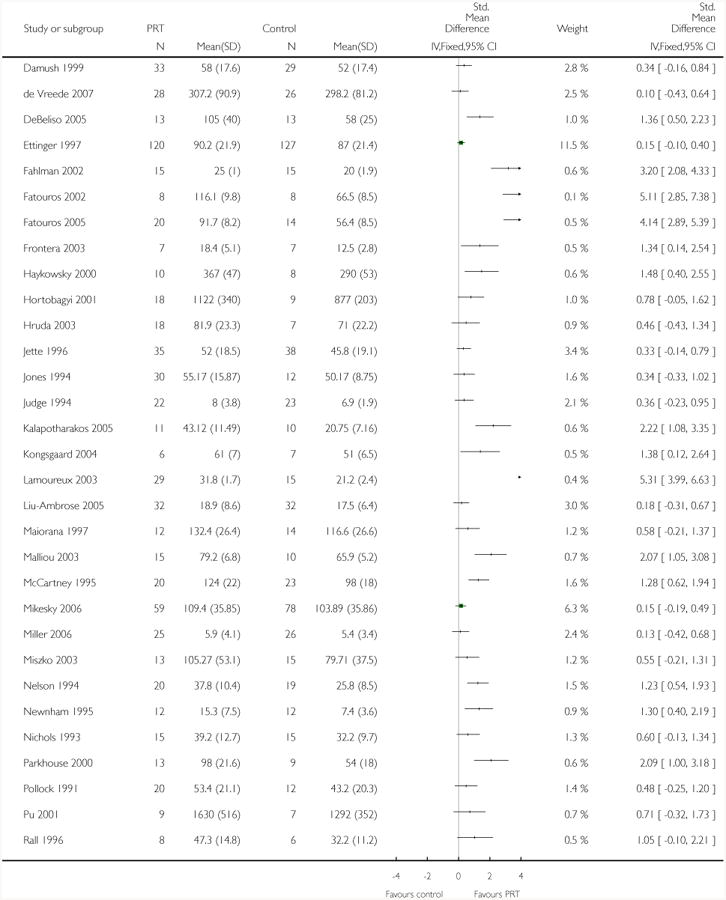
|
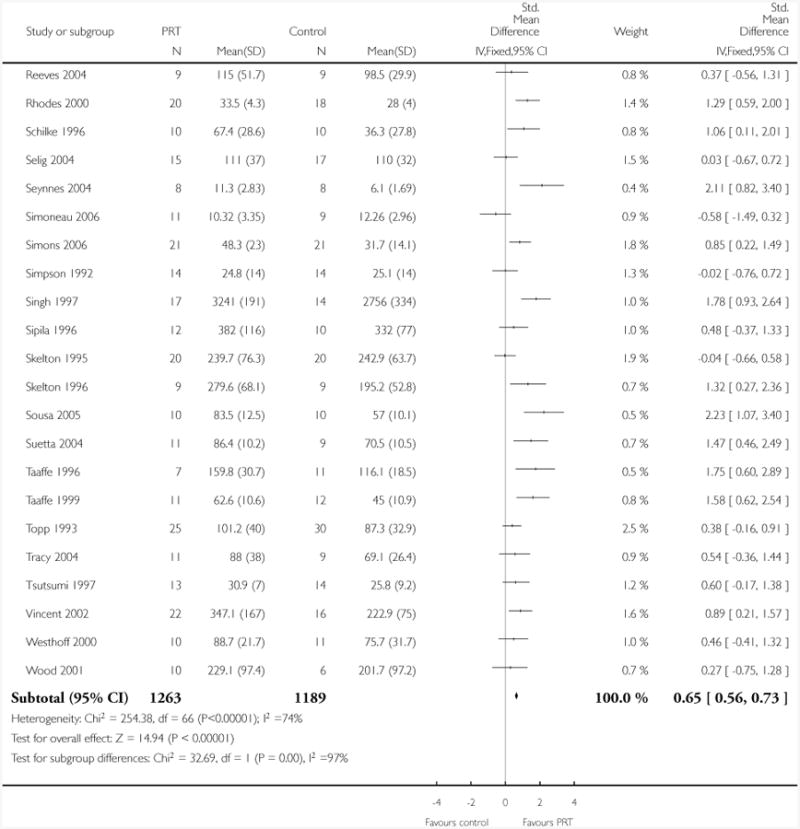
|
Analysis 10.2. Comparison 10 PRT versus control supplementary analyses, Outcome 2 Strength (grouped by assessor blinding).
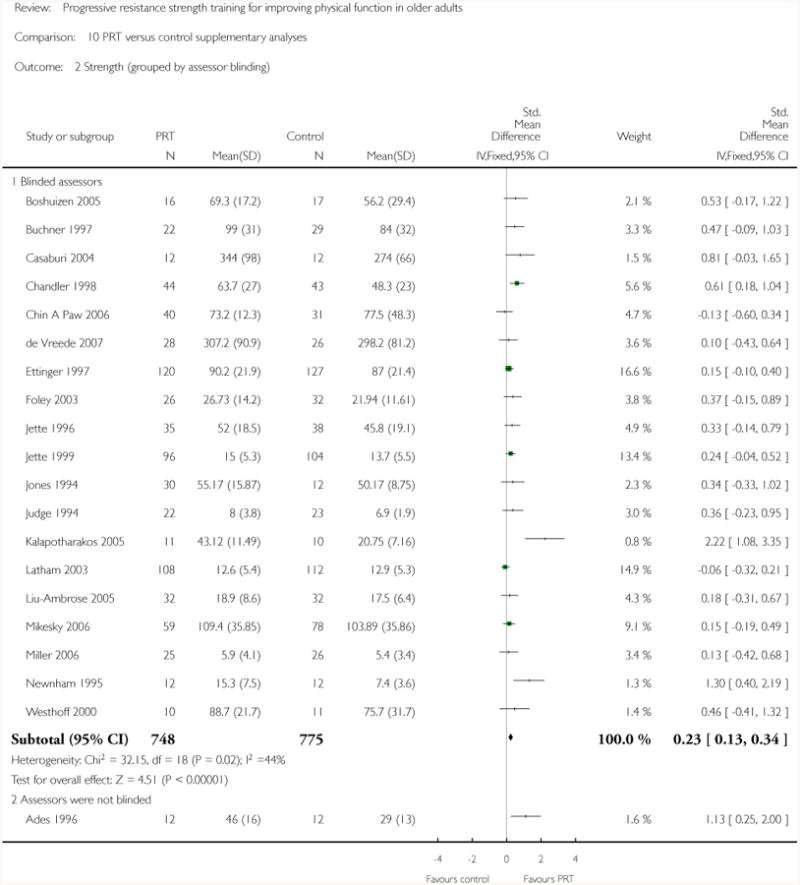
|
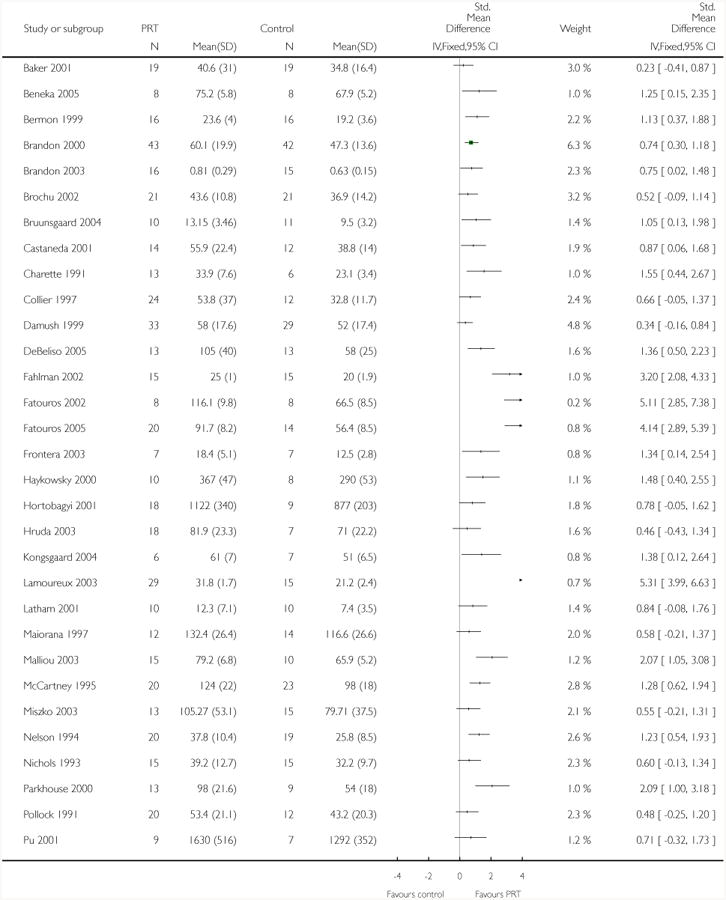
|
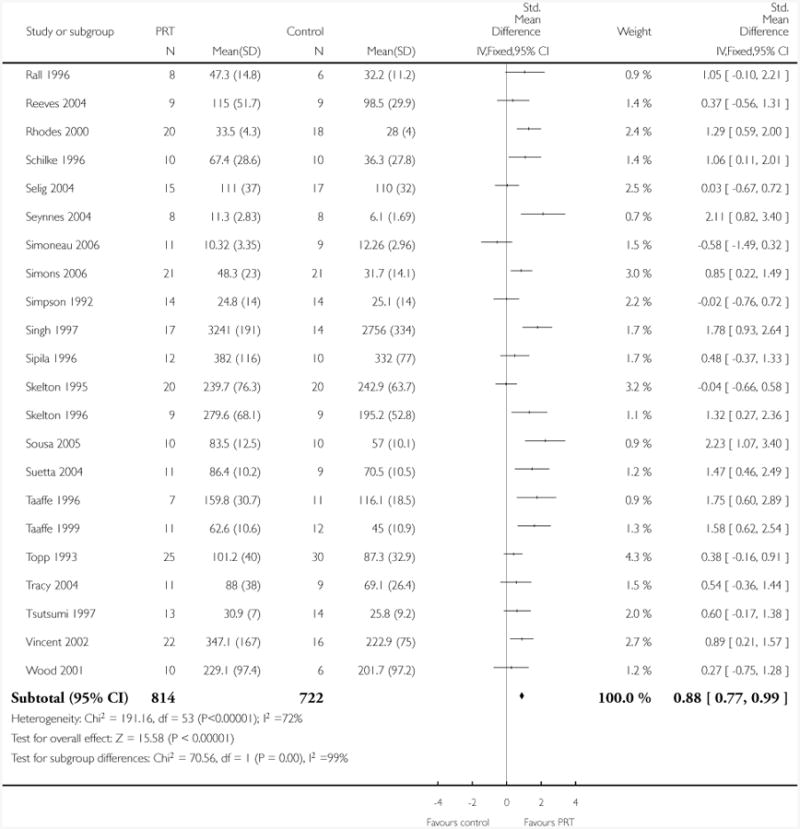
|
Analysis 10.3. Comparison 10 PRT versus control supplementary analyses, Outcome 3 Strength (grouped by intention-to-treat).
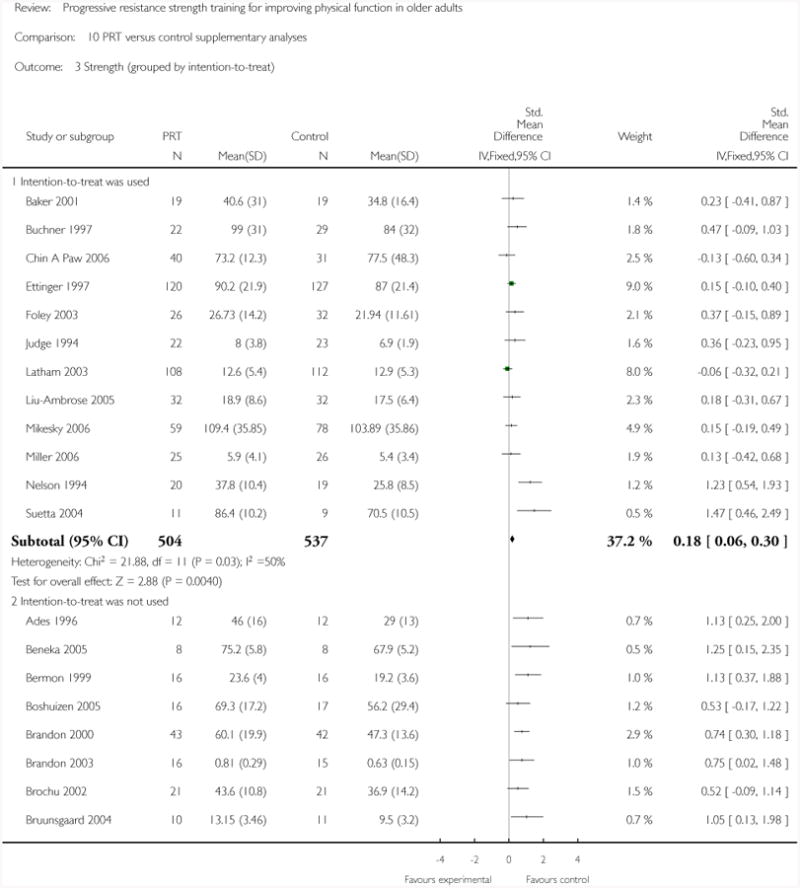
|
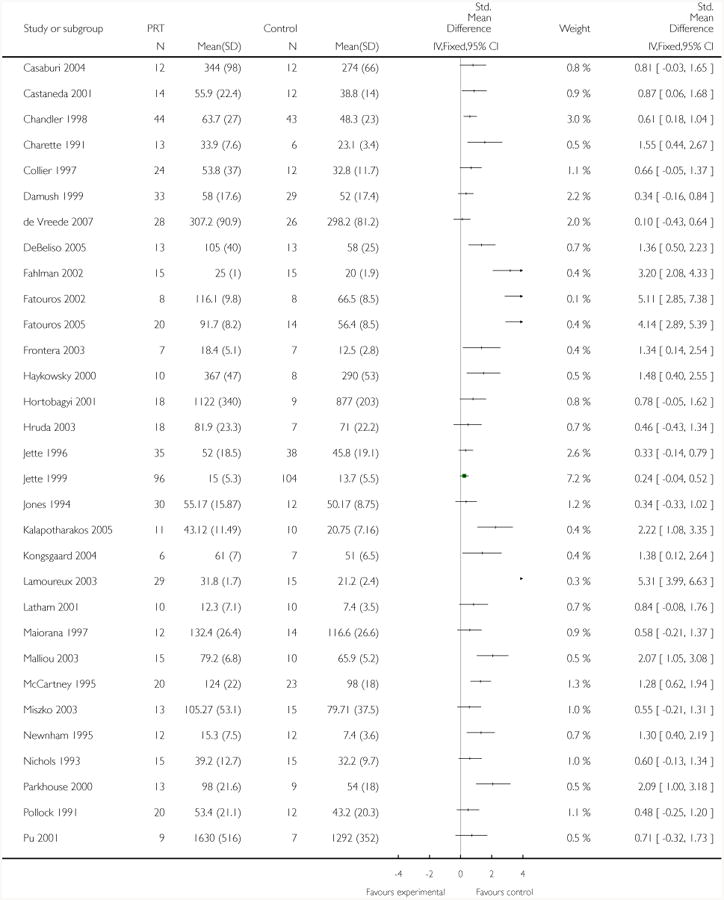
|
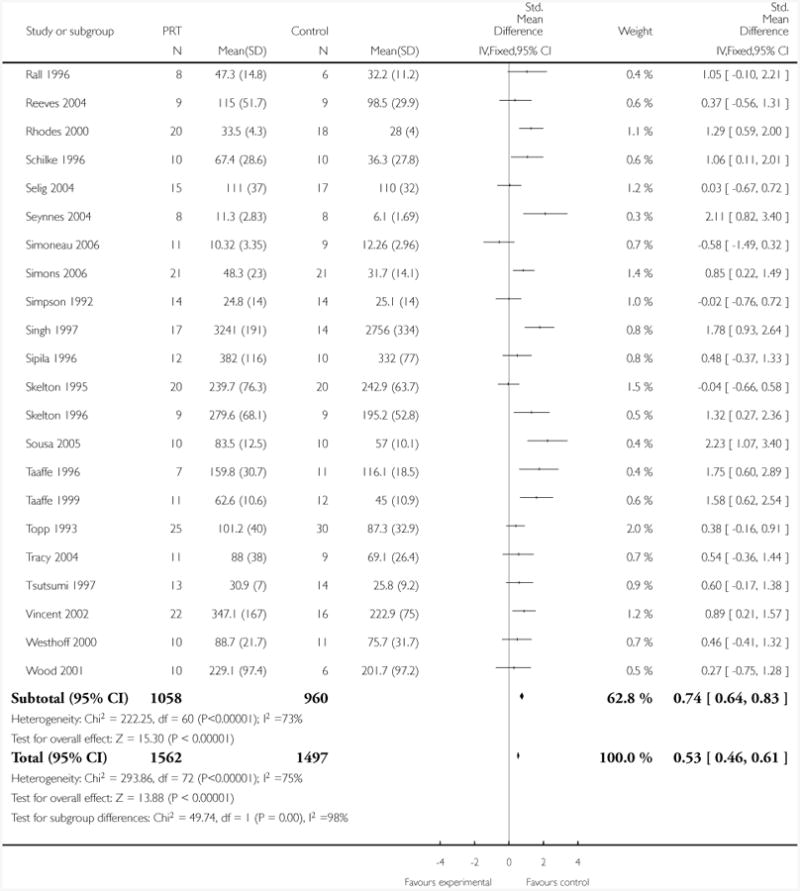
|
Analysis 10.4. Comparison 10 PRT versus control supplementary analyses, Outcome 4 Strength (grouped by attention control).
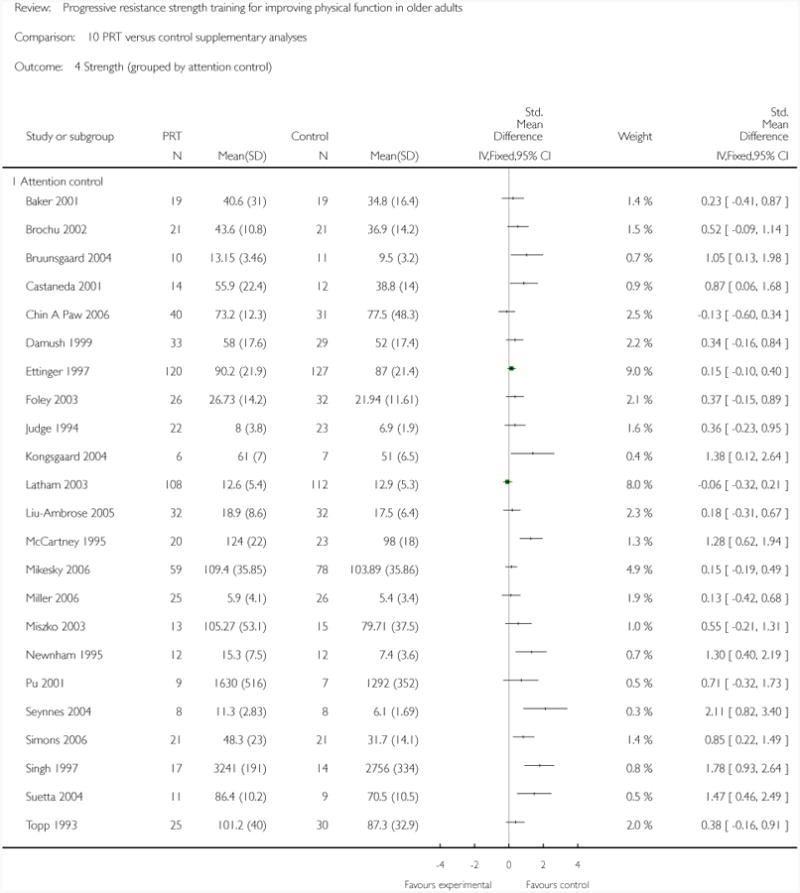
|
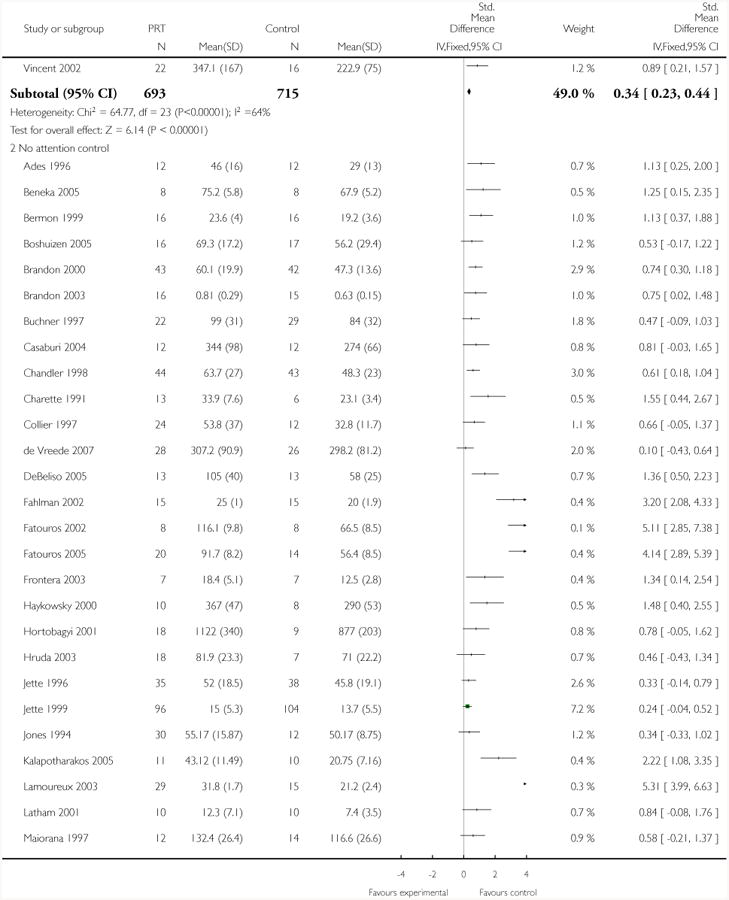
|
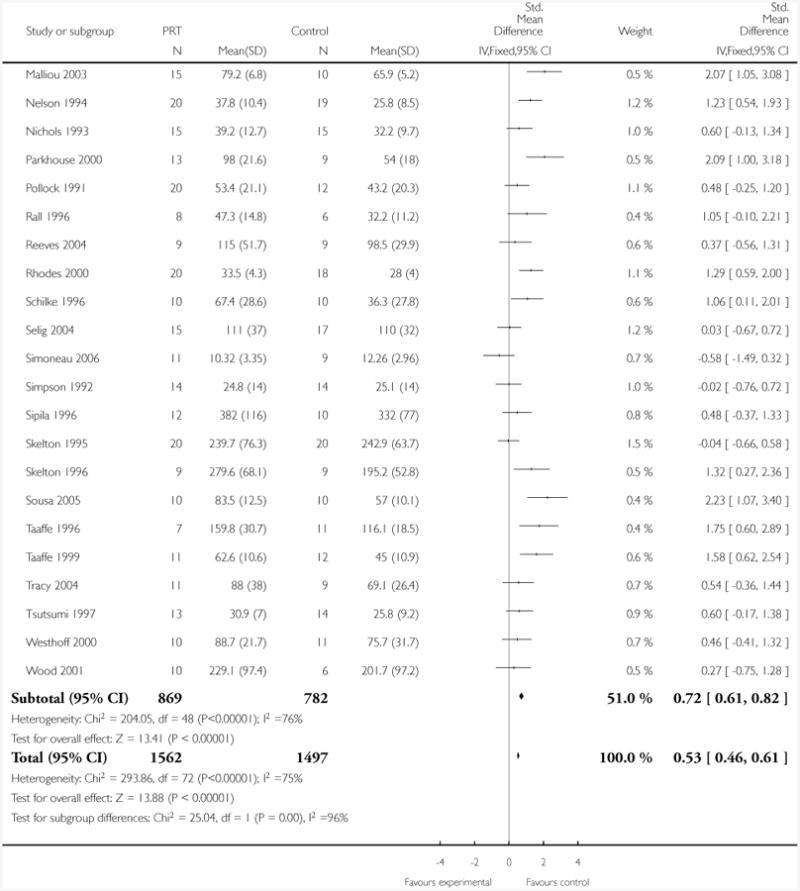
|
Analysis 10.5. Comparison 10 PRT versus control supplementary analyses, Outcome 5 Strength (grouped by exercise intensity).
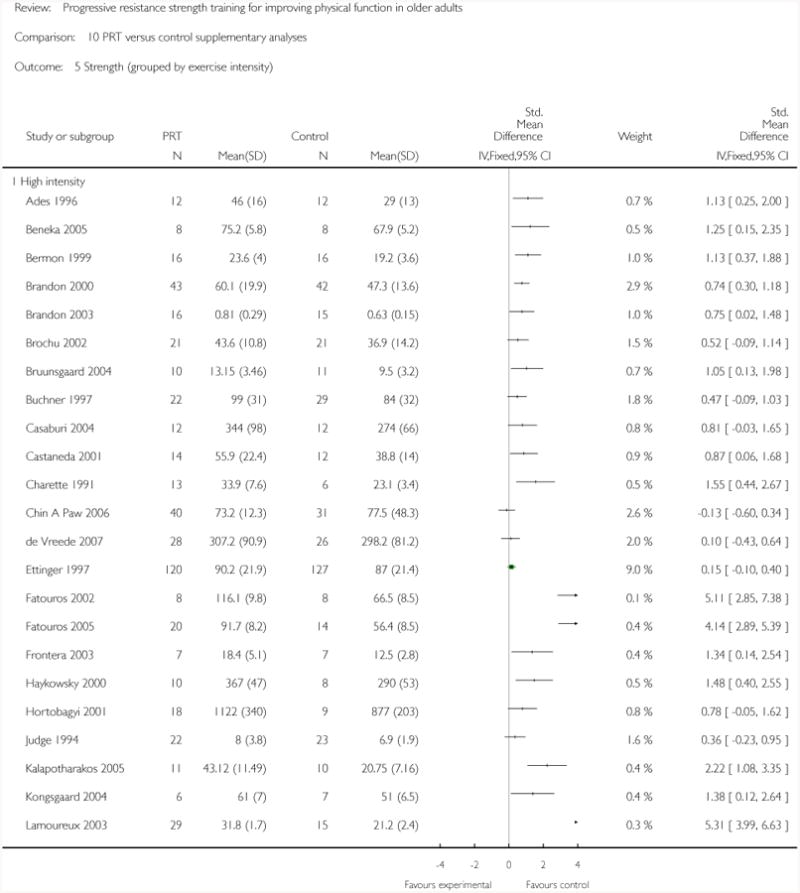
|
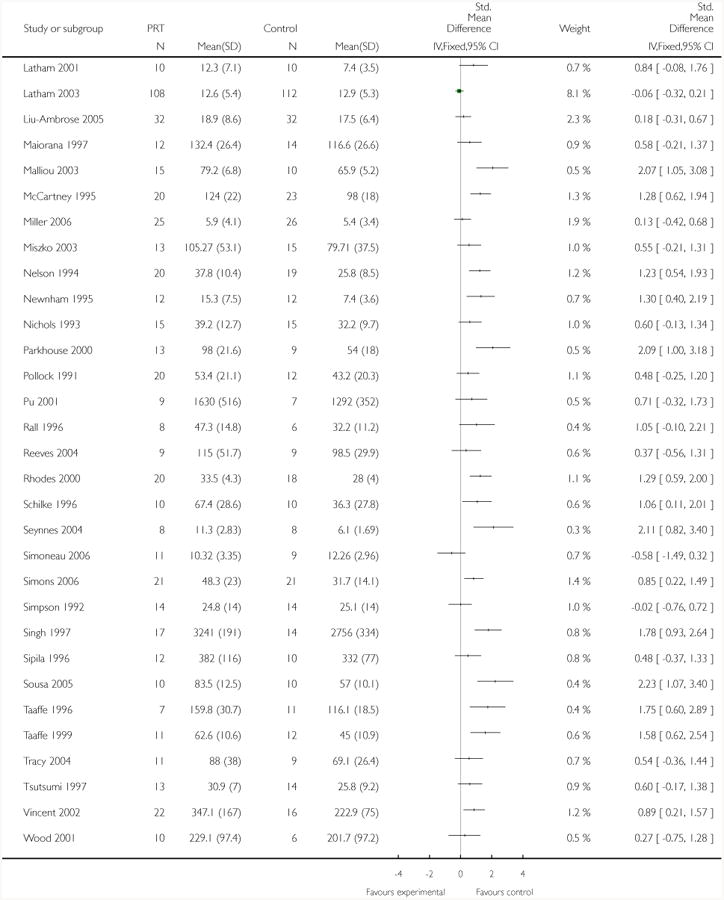
|
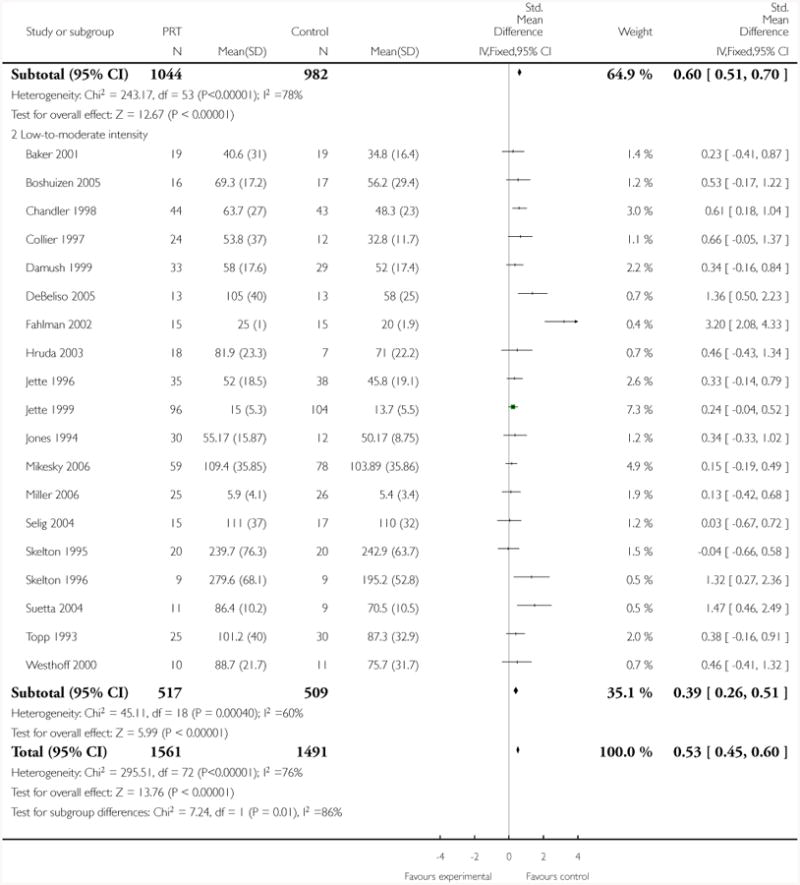
|
Analysis 10.6. Comparison 10 PRT versus control supplementary analyses, Outcome 6 Strength (grouped by exercise duration).
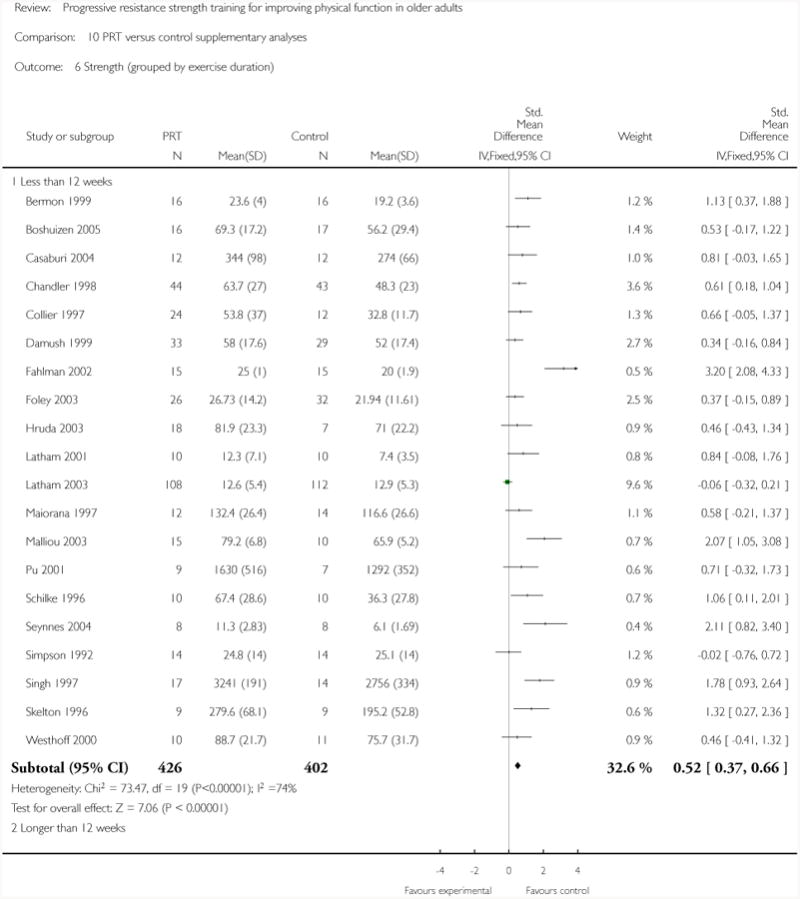
|
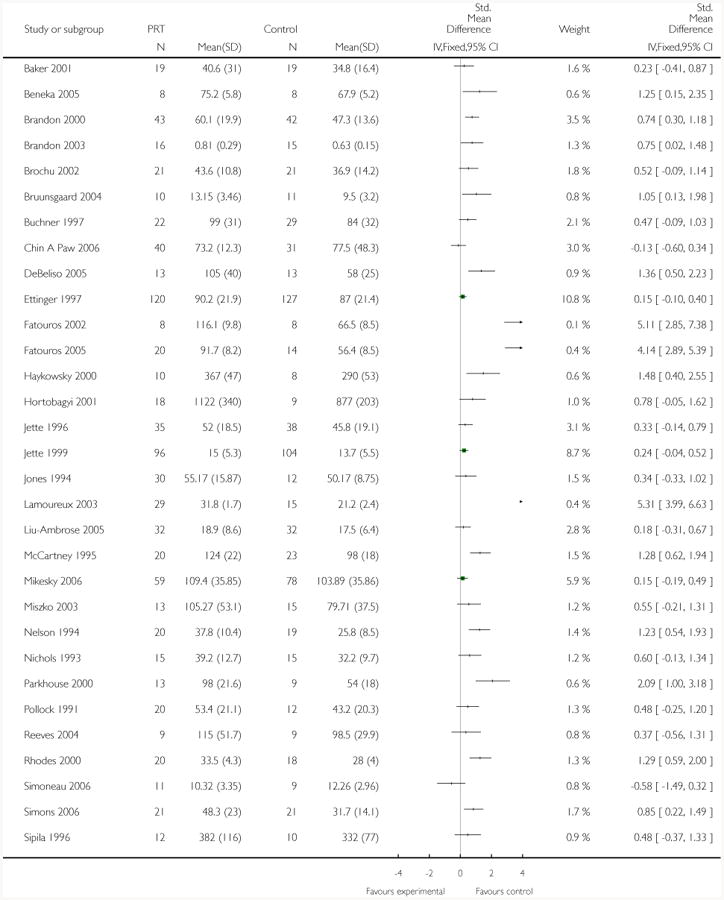
|
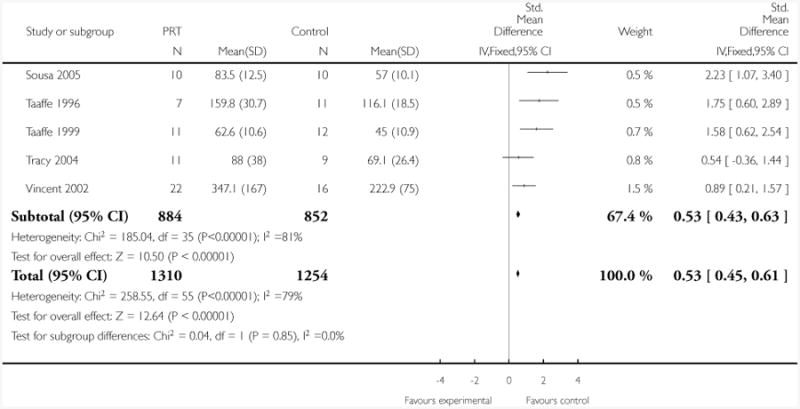
|
Analysis 10.7. Comparison 10 PRT versus control supplementary analyses, Outcome 7 Strength (grouped by health status).
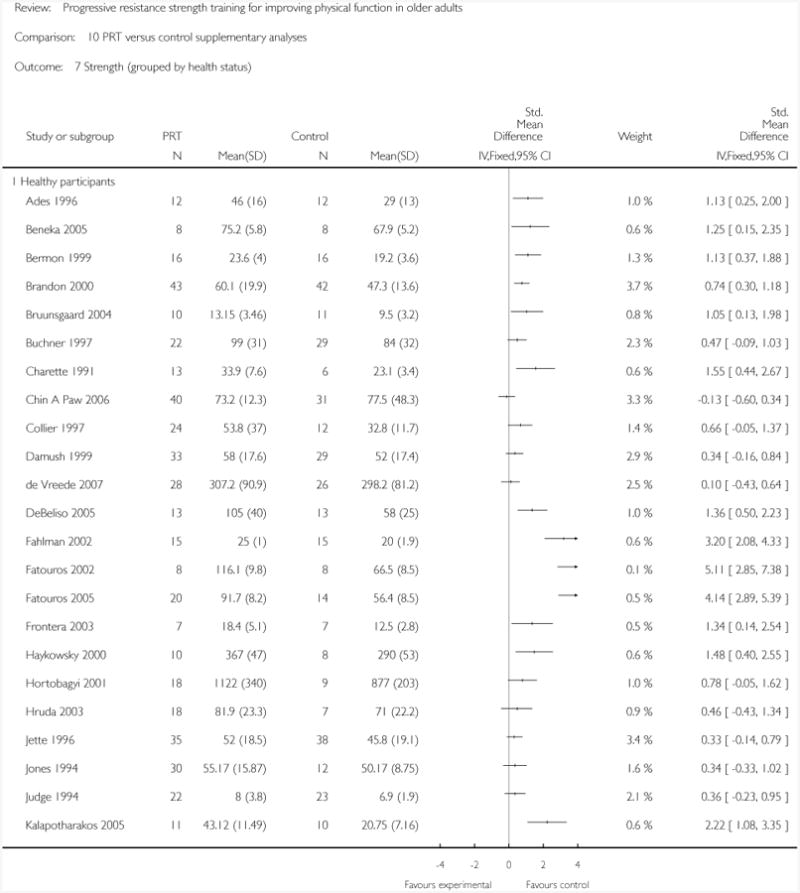
|
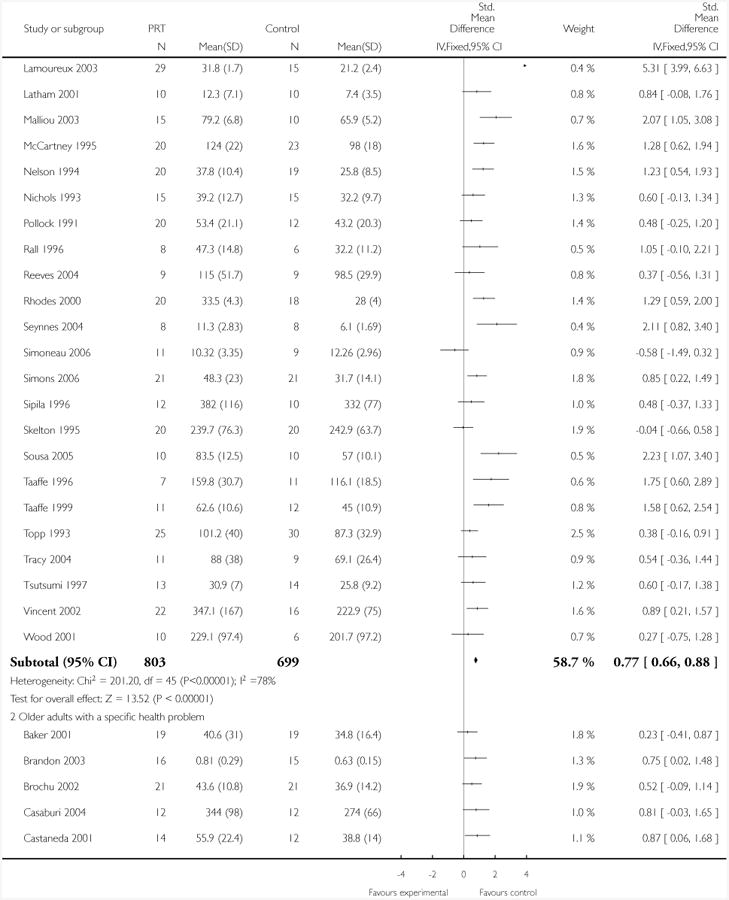
|
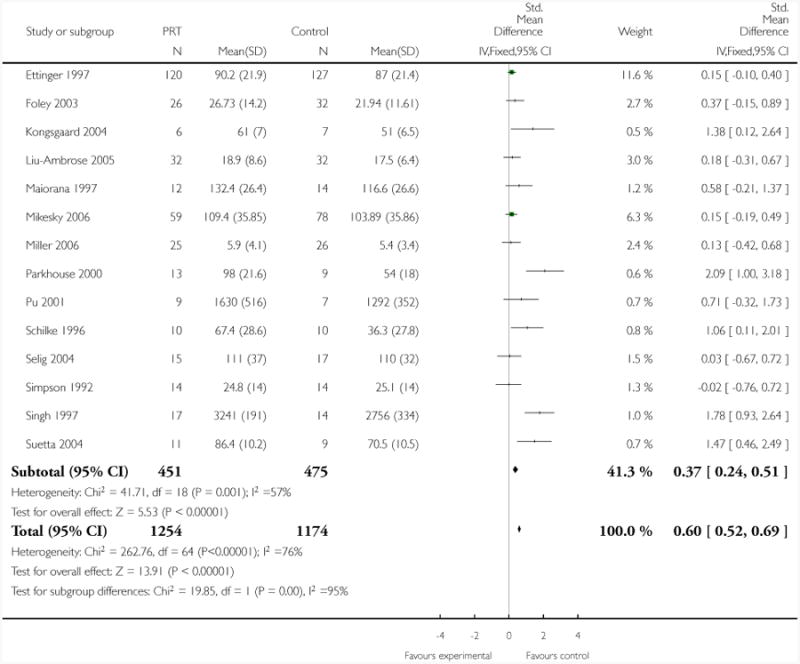
|
Analysis 10.8. Comparison 10 PRT versus control supplementary analyses, Outcome 8 Strength (grouped by functional limitations).
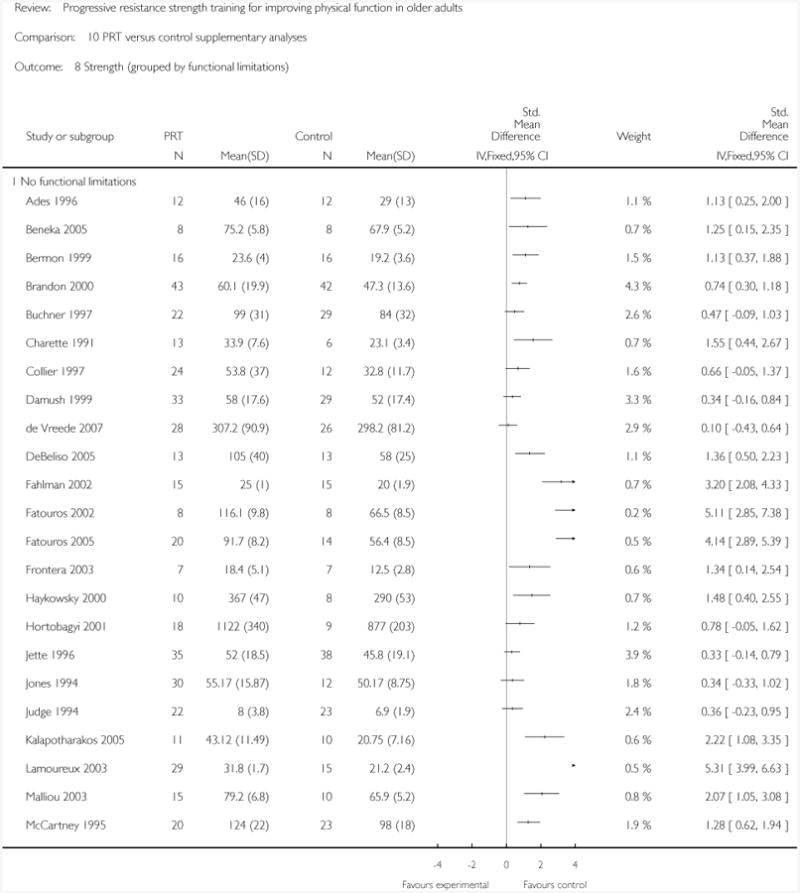
|
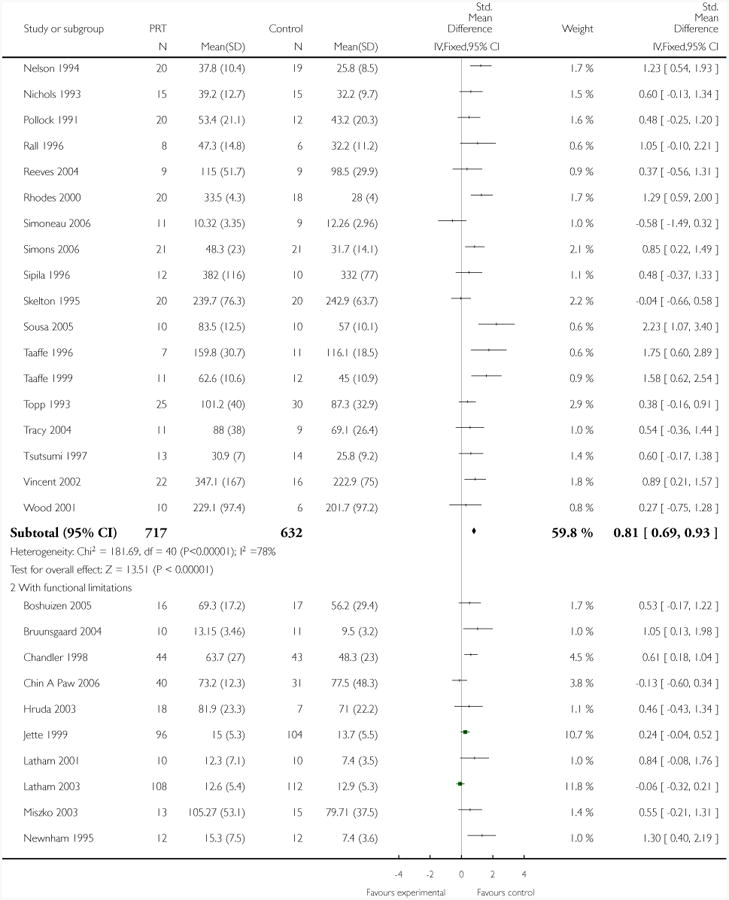
|
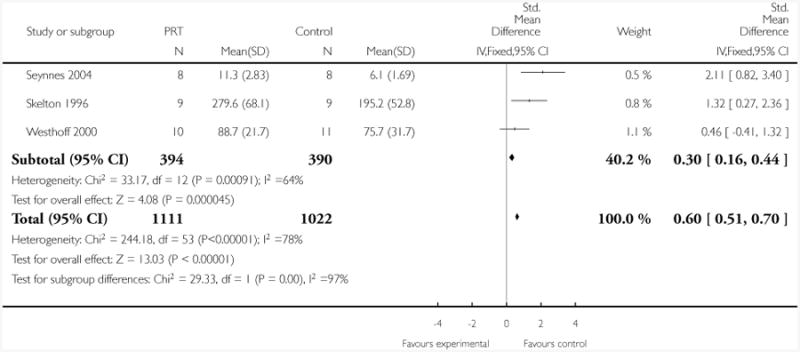
|
Appendix 1. Search strategies
Medline (OVID WEB)
((strength$ or resist$ or weight$) adj3 training).tw.
progressive resist$.tw.
or/1-2
Exercise/
Exercise Therapy/
exercise$.tw.
or/4-6
(Resist$ training or strength$).tw.
and/7-8
or/3,9
limit 10 to (“all aged (65 and over)” or “aged (80 and over)”)
(elderly or senior$).tw.
and/10,12
or/11,13
randomized controlled trial.pt.
controlled clinical trial.pt.
Randomized Controlled Trials/
Random Allocation/
Double Blind Method/
Single Blind Method/
or/15-20
Animals/not Humans/
21 not 22
clinical trial.pt.
exp Clinical Trials as topic/
(clinic$ adj25 trial$).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw.
Placebos/
placebo$.tw.
random$.tw.
Research Design/
or/24-31
32 not 22
33 not 23
or/23,34
and/14,35
Embase (OVID WEB)
((strength$ or resist$ or weight$) adj3 training).tw.
progressive resist$.tw.
or/1-2
Exercise/
Kinesiotherapy/or Therapy Resistance/
exercise$.tw.
or/4-6
(resist$ or strength$).tw.
and/7-8
or/3,9
limit 10 to aged <65+ years>
(elderly or senior$).tw.
and/10,12
or/11,13
Clinical trial/
Randomized controlled trial/
Randomization/
Single blind procedure/
Double blind procedure/
Crossover procedure/
Placebo/
Randomi?ed controlled trial$.tw.
Rct.tw.
Random allocation.tw.
Randomly allocated.tw.
Allocated randomly.tw.
(allocated adj2 random).tw.
Single blind$.tw.
Double blind$.tw.
((treble or triple) adj blind$).tw.
Placebo$.tw.
Prospective study/
or/15-32
Case study/
Case report.tw.
Abstract report/or letter/
or/34-36
33 not 37
limit 38 to human
and/14,39
The Cochrane Library (Wiley)
#1 ((strength* or resist* or weight*) NEAR/3 training):ti,ab,kw
#2 (progressive resist*):ti,ab,kw
#3 #1 OR #2
#4 MeSH descriptor Exercise, this term only
#5 MeSH descriptor Exercise Therapy, this term only
#6 (exercise*):ti,ab,kw
#7 (#4 OR #5 OR #6)
#8 (resist* or strength*):ti,ab,kw
#9 (#7 AND #8)
# 10(#3 OR #9)
#11 (elderly or senior*):ti,ab,kw
#12 (#10 AND #11)
Cinahl (OVID WEB)
((strength$ or resist$ or weight$) adj3 training).tw.
progressive resist$.tw.
or/1-2
Exercise/
Therapeutic Exercise/
“Exercise therapy: ambulation (iowa nic)”/or “Exercise therapy: balance (iowa nic)”/or “Exercise therapy: joint mobility (iowa nic)”/or “Exercise therapy: muscle control (iowa nic)”/or “Teaching: prescribed activity/exercise (iowa nic)”/
exercise$.tw.
or/4-7
(resist$ or strength$).tw.
and/8-9
or/3,10
limit 11 to (aged <65 to 79 years> or “aged <80 and over>”)
(elderly or senior$).tw.
and/11,13
or/12,14
exp Clinical Trials/
exp Evaluation Research/
exp Comparative Studies/
exp Crossover Design/
clinical trial.pt.
or/16-20
((clinical or controlled or comparative or placebo or prospective or randomi#ed) adj3 (trial or study)).tw.
(random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw.
(cross?over$ or (cross adj1 over$)).tw.
((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw.
or/22-26
or/21,27
and/15,28
SPORTDiscus (OVID WEB)
((strength$ or resist$ or weight$) adj3 training).tw.
progressive resist$.tw.
or/1-2
Exercise/
Exercise therapy/
exercise$.tw.
or/4-6
(resist$ or strength$).tw.
and/7-8
or/3,9
(elderly or senior$).tw.
and/10-11
exp Clinical trial/
exp Randomized controlled trial/
Placebo/
((clinical or controlled or comparative or placebo or prospective or randomi#ed) adj3 (trial or study)).tw.
(random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw.
(cross?over$ or (cross adj1 over$)).tw.
((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw.
or/13-20
and/12,21
Footnotes
Indicates the major publication for the study
Contributions of Authors: For the first version of the review (completed 2002), Dr Nancy Latham, Dr Craig Anderson, Dr Derrick Bennett and Dr Caroline Stretton contributed to the development of the protocol, the analysis and interpretation of the data and the write-up of the review. Dr Nancy Latham took the lead in conducting the analyses and writing the protocol and review. In addition, Dr Latham and Dr Stretton conducted the searches, identified the trials, conducted the quality assessments and extracted the data. Dr Bennett provided methodological and statistical guidance for the review. Dr Anderson served as the adjudicator when a consensus about data issues could not be reached between the two reviewers, and provided guidance about the methods and interpretation of the review.
The review was substantially updated in 2009 by Dr Chiung-ju Liu and Dr Nancy Latham. Dr Liu took the lead in conducting the update, which included undertaking the searches, screening search results, organizing retrieval of papers, screening retrieved papers against inclusion criteria, appraising quality of papers, extracting data, contacting authors for additional information, entering data into RevMan, doing the analyses and writing up. The project was completed when Dr Liu was a post-doctoral research fellow at the Health and Disability Research Institute at Boston University. Dr Latham assisted in identifying the trials, conducting the quality assessments, extracting the data, interpreting the results and writing the review.
Both Dr Chiung-ju Liu and Dr Nancy Latham are guarantors for the review.
Declarations of Interest: Dr. Latham is an author for two trials. The trials were rated independently by other reviewers in the first review.
Notes: Substantial updates of reviews such as this one often take a considerable time to prepare and then take through the editorial process. They can therefore seem ‘out of date’ before publication, particularly in research active areas. However, although an updated search made in May 2008 revealed nine more potentially eligible trials (which await assessment, pending the next update), it is unlikely that the review's main findings will be substantively changed by these. [Comment by Helen Handoll, Co-ordinating Editor, May 2009]
References to studies included in this review
- Ades PA, Ballor DL, Ashikaga T, Utton JL, Nair KS. Weight training improves walking endurance in healthy elderly persons. Annals of Internal Medicine. 1996;124(6):568–72. doi: 10.7326/0003-4819-124-6-199603150-00005. MEDLINE: 96175655. [DOI] [PubMed] [Google Scholar]
- Baker KR, Nelson ME, Felson DT, Layne JE, Sarno R, Roubenoff R. The efficacy of home based progressive strength training in older adults with knee osteoarthritis: A randomized controlled trial. Journal of Rheumatology. 2001;28:1655–65. [PubMed] [Google Scholar]
- Balagopal P, Schimke JC, Ades P, Adey D, Nair KS. Age effect on transcript levels and synthesis rate of muscle MHC and response to resistance exercise. American Journal of Physiology Endocrinology and Metabolism. 2001;280(2):E203–8. doi: 10.1152/ajpendo.2001.280.2.E203. [DOI] [PubMed] [Google Scholar]
- Ballor DL, Harvey-Berino JR, Ades PA, Cryan J, Calles-Escandon J. Contrasting effects of resistance and aerobic training on body composition and metabolism after diet-induced weight loss. Metabolism: Clinical & Experimental. 1996;45(2):179–83. doi: 10.1016/s0026-0495(96)90050-5. [DOI] [PubMed] [Google Scholar]
- Barrett CJ, Smerdely P. A comparison of community-based resistance exercise and flexibility exercise for seniors. Australian Journal of Physiotherapy. 2002;48(3):215–9. doi: 10.1016/s0004-9514(14)60226-9. [DOI] [PubMed] [Google Scholar]
- Baum EE, Jarjoura D, Polen AE, Faur D, Rutechi G. Effectiveness of a group exercise program in a long-term care facility: a randomized pilot trial. Journal of the American Medical Directors Association. 2003;4(2):74–80. doi: 10.1097/01.JAM.0000053513.24044.6C. [DOI] [PubMed] [Google Scholar]
- Bean JF, Herman S, Kiely DK, Frey IC, Leveille SG, Fielding RA, et al. Increased Velocity Exercise Specific to Task (InVEST) training: a pilot study exploring effects on leg power, balance, and mobility in community-dwelling older women. Journal of the American Geriatrics Society. 2004;52(5):799–804. doi: 10.1111/j.1532-5415.2004.52222.x. [DOI] [PubMed] [Google Scholar]
- Beneka A, Malliou P, Fatouros I, Jamurtas A, Gioftsidou A, Godolias G, et al. Resistance training effects on muscular strength of elderly are related to intensity and gender. Journal of Science & Medicine in Sport. 2005;8(3):274–83. doi: 10.1016/s1440-2440(05)80038-6. [DOI] [PubMed] [Google Scholar]
- Bermon S, Philip P, Ferrari P, Candito M, Dolisi C. Effects of a short-term strength training programme on lymphocyte subsets at rest in elderly humans. European Journal of Applied Physiology and Occupational Physiology. 1999;79(4):336–40. doi: 10.1007/s004210050517. [DOI] [PubMed] [Google Scholar]
- Boshuizen HC, Stemmerik L, Westhoff MH, Hopman-Rock M. The effects of physical therapists' guidance on improvement in a strength-training program for the frail elderly. Journal of Aging & Physical Activity. 2005;13(1):5–22. doi: 10.1123/japa.13.1.5. [DOI] [PubMed] [Google Scholar]
- Brandon LJ, Boyetter LW, Gaasch DA, Lloyd DG. Effects of lower extremity strength training on functional mobility in older adults. Journal of Aging & Physical Activity. 2000;8(3):214–27. [Google Scholar]
- Brandon LJ, Gaasch DA, Boyette LW, Lloyd AM. Effects of long-term resistive training on mobility and strength in older adults with diabetes. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(8):740–5. doi: 10.1093/gerona/58.8.m740. [DOI] [PubMed] [Google Scholar]
- Ades PA, Savage PD, Brochu M, Tischler MD, Lee NM, Poehlman ET. Resistance training increases total daily energy expenditure in disabled older women with coronary heart disease. Journal of Applied Physiology. 2005;98(4):1280–5. doi: 10.1152/japplphysiol.00360.2004. [DOI] [PubMed] [Google Scholar]
- Ades PA, Savage PD, Cress ME, Brochu M, Lee NM, Poehlman ET. Resistance training on physical performance in disabled older female cardiac patients. Medicine & Science in Sports & Exercise. 2003;35(8):1265–70. doi: 10.1249/01.MSS.0000079044.21828.0E. [DOI] [PubMed] [Google Scholar]
- *.Brochu M, Savage P, Lee M, Dee J, Cress ME, Poehlman ET, et al. Effects of resistance training on physical function in older disabled women with coronary heart disease. Journal of Applied Physiology. 2002;92(2):672–8. doi: 10.1152/japplphysiol.00804.2001. [DOI] [PubMed] [Google Scholar]
- Bruunsgaard H, Bjerregaard E, Schroll M, Pedersen BK. Muscle strength after resistance training is inversely correlated with baseline levels of soluble tumor necrosis factor receptors in the oldest old. Journal of the American Geriatrics Society. 2004;52(2):237–41. doi: 10.1111/j.1532-5415.2004.52061.x. [DOI] [PubMed] [Google Scholar]
- *.Buchner DM, Cress ME, de Lateur BJ. The effect of strength and endurance training on gait, balance, fall risk and health services use in community-living older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 1997;52(4):M218–24. doi: 10.1093/gerona/52a.4.m218. [DOI] [PubMed] [Google Scholar]
- Buchner DM, Cress ME, de Lateur BJ, Wagner EH. Variability in the effect of strength training on skeletal muscle in older adults. Facts and Research in Gerontology. 1993;7:143–53. [Google Scholar]
- Coleman EA, Buchner DM, Cress ME, Chan BKS, de Lateur BJ. The relationship of joint symptoms with exercise performance in older adults. Journal of the American Geriatrics Society. 1996;44(1):14–21. doi: 10.1111/j.1532-5415.1996.tb05632.x. [DOI] [PubMed] [Google Scholar]
- Casaburi R, Bhasin S, Cosentino L, Porszasz J, Somfay A, Lewis MI, et al. Effects of testosterone and resistance training in men with chronic obstructive pulmonary disease. American Journal of Respiratory & Critical Care Medicine. 2004;170(8):870–8. doi: 10.1164/rccm.200305-617OC. [DOI] [PubMed] [Google Scholar]
- Castaneda C, Gordon PL, Uhlin KL, Levery AS, Kehayias JJ, Dwyer JT, et al. Resistance training to counteract the catabolism of a low-protein diet in patients with chronic renal insufficiency. Annals of Internal Medicine. 2001;135(11):965–76. doi: 10.7326/0003-4819-135-11-200112040-00008. [DOI] [PubMed] [Google Scholar]
- Castaneda C, Gordon PL, Parker RC, Uhlin KL, Roubenoff R, Levey AS. Resistance training to reduce the malnutrition-inflammation complex syndrome of chronic kidney disease. American Journal of Kidney Diseases. 2004;43(4):607–16. doi: 10.1053/j.ajkd.2003.12.025. [DOI] [PubMed] [Google Scholar]
- Chandler JM, Duncan PW, Kochersberger G, Studenski S. Is lower extremity strength gain associated with improvement in physical performance and disability in frail, community-dwelling elders? Archives of Physical Medicine and Rehabilitation. 1998;79(1):24–30. doi: 10.1016/s0003-9993(98)90202-7. [DOI] [PubMed] [Google Scholar]
- Charette S, McEvoy L, Pyka G. Muscle hypertrophy response to resistance training in older women. Journal of Applied Physiology. 1991;70(5):1912–6. doi: 10.1152/jappl.1991.70.5.1912. [DOI] [PubMed] [Google Scholar]
- Chin A Paw MJM, Van Poppel MNM, Twisk JWR, Van Mechelen W. Effects of resistance and all-round, functional training on quality of life, vitality and depression of older adults living in long-term care facilities: A ‘randomized’ controlled trial. BMC Geriatrics. 2004;4:1–9. doi: 10.1186/1471-2318-4-5. ISRCTN87177281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Chin A Paw MJM, Van Poppel MNM, Twisk JWR, Van Mechelen W. Once a week not enough, twice a week not feasible? A randomised controlled exercise trial in long-term care facilities. Patient Education & Counseling. 2006;63(1-2):205–14. doi: 10.1016/j.pec.2005.10.008. ISRCTN87177281. [DOI] [PubMed] [Google Scholar]
- Chin A Paw MJM, Van Poppel MNM, Van Mechelen W. Effects of resistance and functional-skills training on habitual activity and constipation among older adults living in long-term care facilities: A randomized controlled trial. BMC Geriatrics. 2006;6:9. doi: 10.1186/1471-2318-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier CD. Isotonic resistance training related functional fitness, physical self-efficacy and depression in adults ages 65-85 (thesis) Stillwater (OK): Oklahoma State University; 1997. [Google Scholar]
- Damush TM, Damush JG., Jr The effects of strength training on strength and health-related quality of life in older adult women. Gerontologist. 1999;39(6):705–10. doi: 10.1093/geront/39.6.705. [DOI] [PubMed] [Google Scholar]
- *.de Vos NJ, Singh NA, Ross DA, Stavrinos TM, Orr R, Fiatarone-Singh MA. Optimal load for increasing muscle power during explosive resistance training in older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2005;60(5):638–47. doi: 10.1093/gerona/60.5.638. [DOI] [PubMed] [Google Scholar]
- Orr R, de Vos NJ, Singh NA, Ross DA, Stavrinos TM, Fiatarone-Singh MA. Power training improves balance in healthy older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2006;61(1):78–85. doi: 10.1093/gerona/61.1.78. [DOI] [PubMed] [Google Scholar]
- de Vreede PL, Samson MM, Van Meeteren NL, Van der Bom JG, Duursma SA, Verhaar HJ. Functional tasks exercise versus resistance exercise to improve daily function in older women: a feasibility study. Archives of Physical Medicine & Rehabilitation. 2004;85(12):1952–61. doi: 10.1016/j.apmr.2004.05.006. [DOI] [PubMed] [Google Scholar]
- de Vreede PL, Samson MM, Van Meeteren NLU, Duursma SA, Verhaar HJJ. Functional-task exercise versus resistance strength exercise to improve daily function in older women: A randomized, controlled trial. Journal of the American Geriatrics Society. 2005;53(1):2–10. doi: 10.1111/j.1532-5415.2005.53003.x. [DOI] [PubMed] [Google Scholar]
- *.de Vreede PL, Van Meeteren NL, Samson MM, Wittink HM, Duursma SA, Verhaar HJ. The effect of functional tasks exercise and resistance exercise on health-related quality of life and physical activity: A randomized controlled trial. Gerontology. 2007;53(1):12–20. doi: 10.1159/000095387. [DOI] [PubMed] [Google Scholar]
- DeBeliso M, Harris C, Spitzer-Gibson T, Adams KJ. A comparison of periodised and fixed repetition training protocol on strength in older adults. Journal of Science & Medicine in Sport. 2005;8(2):190–9. doi: 10.1016/s1440-2440(05)80010-6. [DOI] [PubMed] [Google Scholar]
- DiFrancisco-Donoghue J, Werner W, Douris P. Comparison of once-weekly and twice-weekly strength training in older adults. British Journal of Sports Medicine. 2007;41(1):19–22. doi: 10.1136/bjsm.2006.029330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donald IP, Pitt K, Armstrong E, Shuttleworth H. Preventing falls on an elderly care rehabilitation ward. Clinical Rehabilitation. 2000;14(2):178–85. doi: 10.1191/026921500677888641. [DOI] [PubMed] [Google Scholar]
- Earles DR, Judge JO, Gunnarsson OT. Velocity training induces power-specific adaptations in highly functioning older adults. Archives of Physical Medicine and Rehabilitation. 2001;82(7):872–8. doi: 10.1053/apmr.2001.23838. [DOI] [PubMed] [Google Scholar]
- *.Ettinger WH, Jr, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST) JAMA. 1997;277(1):25–31. [PubMed] [Google Scholar]
- Mangani I, Cesari M, Kritchevsky SB, Maraldi C, Carter CS, Atkinson HH, et al. Physical exercise and comorbidity. Results from the Fitness and Arthritis in Seniors Trial (FAST) Aging-Clinical & Experimental Research. 2006;18(5):374–80. doi: 10.1007/BF03324833. [DOI] [PubMed] [Google Scholar]
- Messier SP, Royer TD, Craven TE, O'Toole ML, Burns R, Ettinger WH., Jr Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the Fitness, Arthritis and Seniors Trial (FAST) Journal of the American Geriatrics Society. 2000;48(2):131–8. doi: 10.1111/j.1532-5415.2000.tb03903.x. [DOI] [PubMed] [Google Scholar]
- Penninx B, Rejeski WJ, Pandya J, Miller ME, Di Bari M, Applegate WB, et al. Exercise and depressive symptoms: A comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2002;57(2):124–32. doi: 10.1093/geronb/57.2.p124. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Ettinger WH, Jr, Martin K, Morgan T. Treating disability in knee osteoarthritis with exercise therapy: a central role for self-efficacy and pain. Arthritis Care & Research. 1998;11(2):94–101. doi: 10.1002/art.1790110205. [DOI] [PubMed] [Google Scholar]
- Sevick MA, Bradham DD, Muender M, Chen GJ, Enarson C, Dailey M, et al. Cost-effectiveness of aerobic and resistance exercise in seniors with knee osteoarthritis. Medicine & Science in Sports & Exercise. 2000;32(9):1534–40. doi: 10.1097/00005768-200009000-00002. [DOI] [PubMed] [Google Scholar]
- Fahlman MM, Boardley D, Lambert CP, Flynn MG. Effects of endurance training and resistance training on plasma lipoprotein profiles in elderly women. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2002;57(2):B54–60. doi: 10.1093/gerona/57.2.b54. [DOI] [PubMed] [Google Scholar]
- Fatouros I, Taxildaris K, Tokmakidis S, Kalapotharakos VI, Aggelousis N, Athanasopoulos S, et al. The effects of strength training, cardiovascular training and their combination on flexibility of inactive older adults. International Journal of Sports Medicine. 2002;23(2):112–9. doi: 10.1055/s-2002-20130. [DOI] [PubMed] [Google Scholar]
- Fatouros IG, Kambas A, Katrabasas I, Leontsini D, Chatzinikolaou A, Jamurtas AZ, et al. Resistance training and detraining effects on flexibility performance in the elderly are intensity-dependent. Journal of Strength & Conditioning Research. 2006;20(3):634–42. doi: 10.1519/R-17615.1. [DOI] [PubMed] [Google Scholar]
- *.Fatouros IG, Kambas A, Katrabasas I, Nikolaidis K, Chatzinikolaou A, Leontsini D, et al. Strength training and detraining effects on muscular strength, anaerobic power, and mobility of inactive older men are intensity dependent. British Journal of Sports Medicine. 2005;39(10):776–80. doi: 10.1136/bjsm.2005.019117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatouros IG, Tournis S, Leontsini D, Jamurtas AZ, Sxina M, Thomakos P, et al. Leptin and adiponectin responses in overweight inactive elderly following resistance training and detraining are intensity related. Journal of Clinical Endocrinology & Metabolism. 2005;90(11):5970–7. doi: 10.1210/jc.2005-0261. [DOI] [PubMed] [Google Scholar]
- *.Fiatarone MA, O'Neill EF, Ryan ND, Clements KM, Solares GR, Nelson ME, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. New England Journal of Medicine. 1994;330(25):1769–75. doi: 10.1056/NEJM199406233302501. [DOI] [PubMed] [Google Scholar]
- Singh MA, Ding W, Manfredi TJ, Solares GS, O'Neill EF, Clements KM. Insulin-like growth factor I in skeletal muscle after weight-lifting exercise in frail elders. American Journal of Physiology Endocrinology and Metabolism. 1999;277(40):E135–43. doi: 10.1152/ajpendo.1999.277.1.E135. [DOI] [PubMed] [Google Scholar]
- Fiatarone MA, O'Neill EF, Doyle RN, Clements K. Efficacy of home-based resistance training in frail elders; Abstracts of the 16th Congress of the International Association of Gerontology; Bedford Park, South Australia. 1997 World Congress of Gerontology Inc; 1997. Abstract 985. [Google Scholar]
- *.Fielding RA, LeBrasseur NK, Cuoco A, Bean J, Mizer K, Fiatarone Singh MA. High-velocity resistance training increases skeletal muscle peak power in older women. Journal of the American Geriatrics Society. 2002;50(4):655–62. doi: 10.1046/j.1532-5415.2002.50159.x. see comment. [DOI] [PubMed] [Google Scholar]
- Sayers SP, Bean J, Cuoco A, LeBrasseur NK, Jette A, Fielding RA. Changes in function and disability after resistance training: does velocity matter? A pilot study. American Journal of Physical Medicine & Rehabilitation. 2003;82(8):605–13. doi: 10.1097/01.PHM.0000078225.71442.B6. [DOI] [PubMed] [Google Scholar]
- Flynn MG, Fahlman M, Braun WA, Lambert CP, Bouillon LE, Brolinson PG, et al. Effects of resistance training on selected indexes of immune function in elderly women. Journal of Applied Physiology. 1999;86(6):1905–13. doi: 10.1152/jappl.1999.86.6.1905. [DOI] [PubMed] [Google Scholar]
- Foley A, Halbert J, Hewitt T, Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis - A randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Annals of the Rheumatic Diseases. 2003;62(12):1162–7. doi: 10.1136/ard.2002.005272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera WR, Hughes VA, Krivickas LS, Kim SK, Foldvari M, Roubenoff R. Strength training in older women: early and late changes in whole muscle and single cells. Muscle & Nerve. 2003;28(5):601–8. doi: 10.1002/mus.10480. [DOI] [PubMed] [Google Scholar]
- Galvao DA, Taaffe DR. Resistance exercise dosage in older adults: Single- versus multiset effects on physical performance and body composition. Journal of the American Geriatrics Society. 2005;53(12):2090–7. doi: 10.1111/j.1532-5415.2005.00494.x. [DOI] [PubMed] [Google Scholar]
- Hagerman FC, Walsh SJ, Staron RS, Hikida RS, Gilders RM, Murray TF, et al. Effects of high-intensity resistance strength training on untrained older men 1. Strength, cardiovascular and metabolic responses. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2000;55A(7):B336–46. doi: 10.1093/gerona/55.7.b336. [DOI] [PubMed] [Google Scholar]
- Harris C, DeBeliso MA, Spitzer-Gibson TA, Adams KJ. The effect of resistance-training intensity on strength-gain response in the older adult. Journal of Strength & Conditioning Research. 2004;18(4):833–8. doi: 10.1519/14758.1. [DOI] [PubMed] [Google Scholar]
- Haykowsky M, Humen D, Teo K, Quinney A, Souster M, Bell G, et al. Effects of 16 weeks of resistance training on left ventricular morphology and systolic function in healthy men >60 years of age. American Journal of Cardiology. 2000;85(8):1002–6. doi: 10.1016/s0002-9149(99)00918-2. [DOI] [PubMed] [Google Scholar]
- Haykowsky M, McGavock J, Vonder Muhll I, Koller M, Mandic S, Welsh R, et al. Effect of exercise training on peak aerobic power, left ventricular morphology, and muscle strength in healthy older women. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2005;60(3):307–11. doi: 10.1093/gerona/60.3.307. [DOI] [PubMed] [Google Scholar]
- Hennessey JV, Chromiak JA, DellaVentura S, Reinert SE, Puhl J, Kiel DP, et al. Growth hormone administration and exercise effects on muscle fibre type and diameter in moderately frail older people. Journal of the American Geriatrics Society. 2001;49(7):852–8. doi: 10.1046/j.1532-5415.2001.49173.x. [DOI] [PubMed] [Google Scholar]
- Hepple RT, Mackinnon SL, Goodman MJ, Thomas SG, Plyley MJ. Resistance and aerobic training in older men: effects on VO2 peak and the capillary supply to skeletal muscle. Journal of Applied Physiology. 1997;82(4):1305–10. doi: 10.1152/jappl.1997.82.4.1305. [DOI] [PubMed] [Google Scholar]
- *.Hiatt WR, Wolfel EE, Meier RH, Regensteiner JG. Superiority of treadmill walking exercise versus strength training for patients with peripheral arterial disease. Circulation. 1994;90(4):1866–74. doi: 10.1161/01.cir.90.4.1866. [DOI] [PubMed] [Google Scholar]
- Regensteiner JG, Steiner JF, Hiatt WR. Exercise training improves functional status in patients with peripheral arterial disease. Journal of Vascular Surgery. 1996;23(1):104–15. doi: 10.1016/s0741-5214(05)80040-0. [DOI] [PubMed] [Google Scholar]
- Hortobagyi T, Tunnel D, Moody J, Beam S, DeVita P. Low- or high-intensity strength training partially restores impaired quadriceps force accuracy and steadiness in aged adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2001;56(1):B38–47. doi: 10.1093/gerona/56.1.b38. [DOI] [PubMed] [Google Scholar]
- Hruda KV, Hicks AL, McCartney N. Training for muscle power in older adults: effects on functional abilities. Canadian Journal of Applied Physiology. 2003;28(2):178–89. doi: 10.1139/h03-014. [DOI] [PubMed] [Google Scholar]
- Hunter GR, Wetzstein CA, McLafferty CL, Jr, Zuckerman PA, Landers KA, Bamman MM. High-resistance versus variable-resistance training in older adults. Medicine & Science in Sports & Exercise. 2001;33(10):1759–64. doi: 10.1097/00005768-200110000-00022. [DOI] [PubMed] [Google Scholar]
- Izquierdo M, Ibanez J, Hakkinen K, Kraemer WJ, Larrion JL, Gorostiaga EM. Once weekly combined resistance and cardiovascular training in healthy older men. Medicine & Science in Sports & Exercise. 2004;36(3):435–43. doi: 10.1249/01.mss.0000117897.55226.9a. [DOI] [PubMed] [Google Scholar]
- Jette AM, Harris BA, Sleeper L, Lachman ME, Heislein D, Giorgetti M, et al. A home-based exercise program for nondisabled older adults. Journal of the American Geriatrics Society. 1996;44(6):644–9. doi: 10.1111/j.1532-5415.1996.tb01825.x. [DOI] [PubMed] [Google Scholar]
- Dancewicz TM, Krebs DE, McGibbon CA. Lower-limb extensor power and lifting characteristics in disabled elders. Journal of Rehabilitation Research and Development. 2003;40(4):337–47. doi: 10.1682/jrrd.2003.07.0337. [DOI] [PubMed] [Google Scholar]
- *.Jette AM, Lachman M, Giorgetti MM, Assman SF, Harris BA, Levenson C, et al. Exercise - it's never too late: The strong-for-life program. American Journal of Public Health. 1999;89(1):66–72. doi: 10.2105/ajph.89.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs DE, Jette AM, Assmann SF. Moderate exercise improves gait stability in disabled elders. Archives of Physical Medicine & Rehabilitation. 1998;79(12):1489–95. doi: 10.1016/s0003-9993(98)90408-7. [DOI] [PubMed] [Google Scholar]
- Jones CJ, Rikli RE, Benedict J, Williamson P. Effects of a resistance training program on leg strength and muscular endurance in older women. Scandinavian Journal of Medicine and Science in Sports. 1995;5(6):329–41. [Google Scholar]
- Jubrias SA, Esselman PC, Price LB, Cress ME, Conley KE. Large energetic adaptations of elderly muscle to resistance and endurance training. Journal of Applied Physiology. 2001;90(5):1663–70. doi: 10.1152/jappl.2001.90.5.1663. [DOI] [PubMed] [Google Scholar]
- *.Judge JO, Whipple RH, Wolfson LI. Effects of resistance and balance exercises on isokinetic strength in older persons. Journal of the American Geriatrics Society. 1994;42(9):937–46. doi: 10.1111/j.1532-5415.1994.tb06584.x. [DOI] [PubMed] [Google Scholar]
- Wolfson L, Whipple R, Derby C, Judge J, King M, Amerman P, et al. Balance and strength training in older adults: intervention gains and tai chi maintenance. Journal of the American Geriatrics Society. 1996;44(5):498–506. doi: 10.1111/j.1532-5415.1996.tb01433.x. [DOI] [PubMed] [Google Scholar]
- *.Kalapotharakos VI, Michalopoulos M, Tokmakidis SP, Godolias G, Gourgoulis V. Effects of a heavy and a moderate resistance training on functional performance in older adults. Journal of Strength & Conditioning Research. 2005;19(3):652–7. doi: 10.1519/15284.1. [DOI] [PubMed] [Google Scholar]
- Kalapotharakos VI, Michalopoulou M, Godolias G, Tokmakidis SP, Malliou PV, Gourgoulis V. The effects of high- and moderate-resistance training on muscle function in the elderly. Journal of Aging & Physical Activity. 2004;12(2):131–43. doi: 10.1123/japa.12.2.131. [DOI] [PubMed] [Google Scholar]
- Kalapotharakos VI, Michalopoulou M, Tokmakidis S, Godolias G, Strimpakos N, Karteroliotis K. Effects of a resistance exercise programme on the performance of inactive older adults. International Journal of Therapy and Rehabilitation. 2004;11(7):318–23. [Google Scholar]
- Kalapotharakos VI, Tokmakidis SP, Smilios I, Michalopoulos M, Gliatis J, Godolias G. Resistance training in older women: effect on vertical jump and functional performance. Journal of Sports Medicine & Physical Fitness. 2005;45(4):570–5. [PubMed] [Google Scholar]
- Kallinen M, Sipila S, Alen M, Suominen H. Improving cardiovascular fitness by strength or endurance training in women aged 76-78 years. A population-based, randomized controlled trial. Age and Ageing. 2002;31(4):247–54. doi: 10.1093/ageing/31.4.247. [DOI] [PubMed] [Google Scholar]
- Katznelson L, Robinson MW, Coyle CL, Lee H, Farrell CE. Effects of modest testosterone supplementation and exercise for 12 weeks on body composition and quality of life in elderly men. European Journal of Endocrinology. 2006;155(6):867–75. doi: 10.1530/eje.1.02291. [DOI] [PubMed] [Google Scholar]
- Kongsgaard M, Backer V, Jorgensen K, Kjaer M, Beyer N. Heavy resistance training increases muscle size, strength and physical function in elderly male COPD-patients - a pilot study. Respiratory Medicine. 2004;98(10):1000–7. doi: 10.1016/j.rmed.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Krebs DE, Scarborough DM, McGibbon CA. Functional vs. strength training in disabled elderly outpatients. American Journal of Physical Medicine & Rehabilitation. 2007;86(2):93–103. doi: 10.1097/PHM.0b013e31802ede64. [DOI] [PubMed] [Google Scholar]
- *.Lamoureux E, Sparrow WA, Murphy A, Newton RU. The effects of improved strength on obstacle negotiation in community-living older adults. Gait & Posture. 2003;17(3):273–83. doi: 10.1016/s0966-6362(02)00101-7. [DOI] [PubMed] [Google Scholar]
- Lamoureux EL, Murphy A, Sparrow A, Newton RU. The effects of progressive resistance training on obstructed-gait tasks in community-living older adults. Journal of Aging and Physical Activity. 2003;11(1):98–110. [Google Scholar]
- Latham NK, Stretton CS, Ronald M. Progressive resistance strength training in hospitalised older people: a preliminary investigation. New Zealand Journal of Physiotherapy. 2001;29(2):41–8. [Google Scholar]
- *.Latham NK, Anderson CS, Lee A, Bennett D, Moseley AM, Cameron ID. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS) Journal of the American Geriatrics Society. 2003;51(3):291–9. doi: 10.1046/j.1532-5415.2003.51101.x. [DOI] [PubMed] [Google Scholar]
- Liu-Ambrose T, Khan KM, Eng JJ, Janssen PA, Lord SR, McKay HA. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: a 6-month randomized, controlled trial. Journal of the American Geriatrics Society. 2004;52(5):657–65. doi: 10.1111/j.1532-5415.2004.52200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu-Ambrose T, Khan KM, Eng JJ, Lord SR, McKay HA. Balance confidence improves with resistance or agility training: Increase is not correlated with objective changes in fall risk and physical abilities. Gerontology. 2004;50(6):373–82. doi: 10.1159/000080175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Liu-Ambrose TYL, Khan KM, Eng JJ, Lord SR, Lentle B, McKay HA. Both resistance and agility training reduce back pain and improve health-related quality of life in older women with low bone mass. Osteoporosis International. 2005;16(11):1321–9. doi: 10.1007/s00198-005-1842-3. [DOI] [PubMed] [Google Scholar]
- Liu-Ambrose TYL. Studies of fall risk and bone morphology in older women with low bone mass. British Columbia (Canada): The University of British Columbia; 2004. dissertation. [Google Scholar]
- Macaluso A, Young A, Gibb KS, Rowe DA, De Vito G. Cycling as a novel approach to resistance training increases muscle strength, power, and selected functional abilities in healthy older women. Journal of Applied Physiology. 2003;95(6):2544–53. doi: 10.1152/japplphysiol.00416.2003. [DOI] [PubMed] [Google Scholar]
- Madden KM, Levy WC, Stratton JK. Exercise training and heart rate variability in older adult female subjects. Clinical & Investigative Medicine - Medecine Clinique et Experimentale. 2006;29(1):20–8. [PubMed] [Google Scholar]
- Maiorana AJ, Briffa TG, Goodman C, Hung J. A controlled trial of circuit weight training on aerobic capacity and myocardial oxygen demand in men after coronary artery bypass surgery. Journal of Cardiopulmonary Rehabilitation. 1997;17(4):239–47. doi: 10.1097/00008483-199707000-00004. [DOI] [PubMed] [Google Scholar]
- Malliou P, Fatouros I, Beneka A, Gioftsidou A, Zissi V, Godolias G, et al. Different training programs for improving muscular performance in healthy inactive elderly. Isokinetics and Exercise Science. 2003;11(4):189–95. [Google Scholar]
- Mangione KK, Craik RL, Tomlinson SS, Palombaro KM. Can elderly patients who have had a hip fracture perform moderate- to high-intensity exercise at home? Physical Therapy. 2005;85(8):727–39. [PubMed] [Google Scholar]
- Manini TM, Clark BC, Tracy BL, Burke J, Ploutz-Snyder L. Resistance and functional training reduces knee extensor position fluctuations in functionally limited older adults. European Journal of Applied Physiology. 2005;95(5-6):436–46. doi: 10.1007/s00421-005-0048-x. [DOI] [PubMed] [Google Scholar]
- Maurer BT, Stern AG, Kinossian B, Cook KD, Schumacher HR. Osteoarthritis of the knee: isokinetic quadriceps exercise versus an educational intervention. Archives of Physical Medicine and Rehabilitation. 1999;80(10):1293–9. doi: 10.1016/s0003-9993(99)90032-1. [DOI] [PubMed] [Google Scholar]
- McCartney N, Hicks A, Martin J, Webber C. A longitudinal trial of weight training in the elderly: continued improvements in year 2. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 1996;51(6):B425–33. doi: 10.1093/gerona/51a.6.b425. [DOI] [PubMed] [Google Scholar]
- *.McCartney N, Hicks AL, Martin J, Webber CE. Long-term resistance training in elderly: Effects on dynamic strength, exercise capacity, muscle and bone. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 1995;50(2):B97–104. doi: 10.1093/gerona/50a.2.b97. [DOI] [PubMed] [Google Scholar]
- McGuigan MR, Bronks R, Newton RU, Sharman MJ, Graham JC, Cody DV, et al. Resistance training in patients with peripheral arterial disease: effects on myosin isoforms, fiber type distribution and capillary supply to skeletal muscle. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2001;56(7):B302–10. doi: 10.1093/gerona/56.7.b302. [DOI] [PubMed] [Google Scholar]
- McMurdo ME, Johnstone R. A randomized controlled trial of a home exercise programme for elderly people with poor mobility. Age and Ageing. 1995;24(5):425–8. doi: 10.1093/ageing/24.5.425. [DOI] [PubMed] [Google Scholar]
- Mihalko SL, McAuley E. Strength training effects on subjective well-being and physical function in the elderly. Journal of Aging and Physical Activity. 1996;4(1):56–68. [Google Scholar]
- Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis and Rheumatism - Arthritis Care and Research. 2006;55(5):690–9. doi: 10.1002/art.22245. [DOI] [PubMed] [Google Scholar]
- Miller MD, Crotty M, Whitehead C, Bannerman E, Daniels LA. Nutritional supplementation and resistance training in nutritionally at risk older adults following lower limb fracture: a randomized controlled trial. Clinical Rehabilitation. 2006;20(4):311–23. doi: 10.1191/0269215506cr942oa. [DOI] [PubMed] [Google Scholar]
- Miszko TA, Cress ME, Slade JM, Covey CJ, Agrawal SK, Doerr CE. Effect of strength and power training on physical function in community-dwelling older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(2):171–5. doi: 10.1093/gerona/58.2.m171. [DOI] [PubMed] [Google Scholar]
- *.Moreland J. Personal Communication. 2001 [Google Scholar]
- Moreland JD, Goldsmith CH, Huijbregts MP, Anderson RE, Prentice DM, Brunton KB, et al. Progressive resistance strengthening exercises after stroke: a single-blind randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2003;84(10):1433–40. doi: 10.1016/s0003-9993(03)00360-5. [DOI] [PubMed] [Google Scholar]
- Morganti CM, Nelson ME, Fiatarone MA, Dallal GE, Economos CD, Crawford BM, et al. Strength improvements with 1 yr of progressive resistance training in older women. Medicine & Science in Sports & Exercise. 1995;27(6):906–12. [PubMed] [Google Scholar]
- *.Nelson ME, Fiatarone MA, Morganti CM, Trice I, Greenberg RA, Evans WJ. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. JAMA. 1994;272(24):1909–14. doi: 10.1001/jama.1994.03520240037038. [DOI] [PubMed] [Google Scholar]
- Newnham J. The effects of a strengthening program on muscle function and mobility skills in an elderly instituionalised population [thesis] Montreal (Quebec): McGill University; 1995. [Google Scholar]
- Nichols JF, Omizo DK, Peterson KK, Nelson KP. Efficacy of heavy-resistance training for active women over sixty: Muscular strength, body composition and program adherence. Journal of the American Geriatrics Society. 1993;41(3):205–10. doi: 10.1111/j.1532-5415.1993.tb06692.x. [DOI] [PubMed] [Google Scholar]
- Ouellette MM, LeBrasseur NK, Bean JF, Phillips E, Stein J, Frontera WR, et al. High-intensity resistance training improves muscle strength, self-reported function, and disability in long-term stroke survivors. Stroke. 2004;35(6):1404–9. doi: 10.1161/01.STR.0000127785.73065.34. [DOI] [PubMed] [Google Scholar]
- Parkhouse WS, Coupland DC, Li C, Vanderhoek KJ. IGF-1 bioavailabililty is increased by resistance training in older women with low bone mineral density. Mechanisms of Ageing and Development. 2000;113(2):75–83. doi: 10.1016/s0047-6374(99)00103-7. [DOI] [PubMed] [Google Scholar]
- Hagberg JM, Graves JE, Limacher M, Woods DR, Leggett SH, Cononie C, et al. Cardiovascular responses of 70- to 79-year-old mean and women to exercise training. Journal of Applied Physiology. 1989;66(6):2589–94. doi: 10.1152/jappl.1989.66.6.2589. [DOI] [PubMed] [Google Scholar]
- Panton LB, Graves JE, Pollock ML, Hagberg JM, Chen W. Effect of aerobic and resistance training on fractionated reaction time and speed of movement. Journal of Gerontology. 1990;45(1):M26–31. doi: 10.1093/geronj/45.1.m26. [DOI] [PubMed] [Google Scholar]
- *.Pollock ML, Carroll JF, Graves JE, Leggett SH, Braith RW, Limacher M, et al. Injuries and adherence to walk/jog and resistance training programs in the elderly. Medicine & Science in Sports & Exercise. 1991;23(10):1194–200. [PubMed] [Google Scholar]
- Pu CT, Johnson MT, Forman DE, Hausdorff JM, Roubenoff R, Foldvari M, et al. Randomized trial of progressive resistance training to counteract the myopathy of chronic heart failure. Journal of Applied Physiology. 2001;90(6):2341–50. doi: 10.1152/jappl.2001.90.6.2341. [DOI] [PubMed] [Google Scholar]
- Rall LC, Meydani SN, Kehayias JJ, Dawson Hughes B, Roubenoff R. The effect of progressive resistance training in rheumatoid arthritis. Increased strength without changes in energy balance or body composition. Arthritis and Rheumatism. 1996;39(3):415–26. doi: 10.1002/art.1780390309. [DOI] [PubMed] [Google Scholar]
- Rall LC, Rosen CJ, Dolnikowski G, Hartman WJ, Lundgren N, Abad LW, et al. Protein metabolism in rheumatoid arthritis and aging. Effects of muscle strength training and tumor necrosis factor alpha. Arthritis and Rheumatism. 1996;39(7):1115–24. doi: 10.1002/art.1780390707. [DOI] [PubMed] [Google Scholar]
- *.Rall LC, Roubenoff R, Cannon JG, Abad LW, Dinarello CA, Meydani SN. Effects of progressive resistance training on immune response in aging and chronic inflammation. Medicine & Science in Sports & Exercise. 1996;28(11):1356–65. doi: 10.1097/00005768-199611000-00003. [DOI] [PubMed] [Google Scholar]
- *.Reeves ND, Narici MV, Maganaris CN. In vivo human muscle structure and function: adaptations to resistance training in old age. Experimental Physiology. 2004;89(6):675–89. doi: 10.1113/expphysiol.2004.027797. [DOI] [PubMed] [Google Scholar]
- Reeves ND, Narici MV, Maganaris CN. Strength training alters the viscoelastic properties of tendons in elderly humans. Muscle & Nerve. 2003;28(1):74–81. doi: 10.1002/mus.10392. [DOI] [PubMed] [Google Scholar]
- Rhodes EC, Martin AD, Taunton JE, Donnely M, Warren J, Elliot J. Effects of one year of resistance training on the relation between muscular strength and bone density in elderly women. British Journal of Sports Medicine. 2000;34(1):18–22. doi: 10.1136/bjsm.34.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilke JM, Johnson GO, Housh TJ, O'Dell JR. Effects of muscle-strength training on the functional status of patients with osteoarthritis of the knee joint. Nursing Research. 1996;45(2):68–72. doi: 10.1097/00006199-199603000-00002. [DOI] [PubMed] [Google Scholar]
- *.Schlicht J. Effect of intense strength training on walking speed, standing balance and sit-to-stand performance in older adults [thesis] Storrs (CT): Univ. of Connecticut; 1999. [DOI] [PubMed] [Google Scholar]
- Schlicht J, Camaione DN, Owen SV. Effect of intense strength training on standing balance, walking speed and sit-to-stand performance in older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2001;56(5):M281–6. doi: 10.1093/gerona/56.5.m281. [DOI] [PubMed] [Google Scholar]
- Segal RJ, Reid RD, Courneya KS, Malone SC, Parliament MB, Scott CG, et al. Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. Journal of Clinical Oncology. 2003;21(9):1653–9. doi: 10.1200/JCO.2003.09.534. [DOI] [PubMed] [Google Scholar]
- Selig SE, Carey MF, Menzies DG, Patterson J, Geerling RH, Williams AD, et al. Moderate-intensity resistance exercise training in patients with chronic heart failure improves strength, endurance, heart rate variability, and forearm blood flow. Journal of Cardiac Failure. 2004;10(1):21–30. doi: 10.1016/s1071-9164(03)00583-9. [DOI] [PubMed] [Google Scholar]
- Seynnes O, Fiatarone Singh MA, Hue O, Pras P, Legros P, Bernard PL. Physiological and functional responses to low-moderate versus high-intensity progressive resistance training in frail elders. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2004;59(5):503–9. doi: 10.1093/gerona/59.5.m503. [DOI] [PubMed] [Google Scholar]
- Simoneau E, Martin A, Porter MM, Van Hoecke J. Strength training in old age: adaptation of antagonist muscles at the ankle joint. Muscle & Nerve. 2006;33(4):546–55. doi: 10.1002/mus.20492. [DOI] [PubMed] [Google Scholar]
- Simons R, Andel R. The effects of resistance training and walking on functional fitness in advanced old age. Journal of Aging & Health. 2006;18(1):91–105. doi: 10.1177/0898264305281102. [DOI] [PubMed] [Google Scholar]
- Simpson K, Killian K, McCartney N, Lloyd DG, Jones NL. Randomised controlled trial of weightlifting exercise in patients with chronic airflow limitation. Thorax. 1992;47(2):70–5. doi: 10.1136/thx.47.2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims J, Hill K, Davidson S, Gunn J, Huang N. Exploring the feasibility of a community-based strength training program for older people with depressive symptoms and its impact on depressive symptoms. BMC Geriatrics. 2006;6:18. doi: 10.1186/1471-2318-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Singh NA, Clements KM, Fiatarone MA. A randomised trial of progressive resistance training in depressed elders. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 1997;52(1):M27–35. doi: 10.1093/gerona/52a.1.m27. [DOI] [PubMed] [Google Scholar]
- Singh NA, Clements KM, Fiatarone Singh MA. The efficacy of exercise as a long-term antidepressant in elderly subjects: a randomized controlled trial. Journals of Gerontology Series A-Biological Sciences and Medical Sciences. 2001;56(8):497–504. doi: 10.1093/gerona/56.8.m497. [DOI] [PubMed] [Google Scholar]
- Singh NA, Stavrinos TM, Scarbek Y, Galambos G, Liber C, Fiatarone Singh MA. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2005;60(6):768–76. doi: 10.1093/gerona/60.6.768. [DOI] [PubMed] [Google Scholar]
- Siplia S, Multanen J, Kallinen M, Era P, Suominen H. Effects of strength and endurance training on isometric muscle strength and walking speed in elderly women. Acta Physiologica Scandinavica. 1996;156(4):457–64. doi: 10.1046/j.1365-201X.1996.461177000.x. [DOI] [PubMed] [Google Scholar]
- Skelton DA, Young A, Greig CA, Malbut KE. Effects of resistance training on strength, power, and functional abilities of women aged 75 and older. Journal of the American Geriatrics Society. 1995;43(10):1081–7. doi: 10.1111/j.1532-5415.1995.tb07004.x. [DOI] [PubMed] [Google Scholar]
- Skelton DA, McLaughlin AW. Training functional ability in old age. Physiotherapy. 1996;82(3):159–67. [Google Scholar]
- Sousa N, Sampaio J. Effects of progressive strength training on the performance of the Functional Reach Test and the Timed Get-Up-and-Go Test in an elderly population from the rural north of Portugal. American Journal of Human Biology. 2005;17(6):746–51. doi: 10.1002/ajhb.20446. [DOI] [PubMed] [Google Scholar]
- Suetta C, Aagaard P, Rosted A, Jakobsen AK, Duus B, Kjaer M, et al. Training-induced changes in muscle CSA, muscle strength, EMG, and rate of force development in elderly subjects after long-term unilateral disuse. Journal of Applied Physiology. 2004;97(5):1954–61. doi: 10.1152/japplphysiol.01307.2003. [DOI] [PubMed] [Google Scholar]
- Suetta C, Magnusson SP, Rosted A, Aagaard P, Jakobsen AK, Larsen LH, et al. Resistance training in the early postoperative phase reduces hospitalization and leads to muscle hypertrophy in elderly hip surgery patients - A controlled, randomized study. Journal of the American Geriatrics Society. 2004;52(12):2016–22. doi: 10.1111/j.1532-5415.2004.52557.x. [DOI] [PubMed] [Google Scholar]
- *.Sullivan DH, Roberson PK, Johnson LE, Bishara O, Evans WJ, Smith ES, et al. Effects of muscle strength training and testosterone in frail elderly males. Medicine & Science in Sports & Exercise. 2005;37(10):1664–72. doi: 10.1249/01.mss.0000181840.54860.8b. [DOI] [PubMed] [Google Scholar]
- Sullivan DH, Roberson PK, Smith ES, Price JA, Bopp MM. Effects of muscle strength training and megestrol acetate on strength, muscle mass, and function in frail older people. Journal of the American Geriatrics Society. 2007;55(1):20–8. doi: 10.1111/j.1532-5415.2006.01010.x. [DOI] [PubMed] [Google Scholar]
- Symons TB, Vandervoort AA, Rice CL, Overend TJ, Marsh GD. Effects of maximal isometric and isokinetic resistance training on strength and functional mobility in older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2005;60(6):777–81. doi: 10.1093/gerona/60.6.777. [DOI] [PubMed] [Google Scholar]
- Pruitt LA, Taaffe DR, Marcus R. Effects of a one-year high-intensity versus low-intensity resistance training program on bone mineral density in older women. Journal of Bone & Mineral Research. 1995;10(11):1788–95. doi: 10.1002/jbmr.5650101123. [DOI] [PubMed] [Google Scholar]
- *.Taaffe DR, Pruitt L, Pyka G, Guido D, Marcus R. Comparative effects of high- and low- intensity resistance training on thigh muscle strength, fiber area, and tissue composition in elderly women. Clinical Physiology. 1996;16(4):381–92. doi: 10.1111/j.1475-097x.1996.tb00727.x. [DOI] [PubMed] [Google Scholar]
- Taaffe DR, Pruitt L, Reim J, Butterfield G, Marcus R. Effect of sustained resistance training on basal metabolic rate in older women. Journal of the American Geriatrics Society. 1995;43(5):465–71. doi: 10.1111/j.1532-5415.1995.tb06090.x. [DOI] [PubMed] [Google Scholar]
- Taaffe DR, Duret C, Wheeler S, Marcus R. Once-weekly resistance exercise improves strength and neuromuscular performance in older adults. Journal of the American Geriatrics Society. 1999;47(10):1208–14. doi: 10.1111/j.1532-5415.1999.tb05201.x. [DOI] [PubMed] [Google Scholar]
- Mikesky AE, Topp R, Wigglesworth JK, Harsha DM, Edwards JE. Efficacy of a home-based training program for older adults using elastic tubing. European Journal of Applied Physiology and Occupational Physiology. 1994;69(4):316–20. doi: 10.1007/BF00392037. [DOI] [PubMed] [Google Scholar]
- *.Topp R, Mikesky A, Wigglesworth J, Holt W, Edwards JE. The effect of a 12-week dynamic resistance strength training on gait velocity and balance in older adults. Gerontologist. 1993;33(4):501–6. doi: 10.1093/geront/33.4.501. [DOI] [PubMed] [Google Scholar]
- Topp R, Mikesky A, Dayhoff NE, Holt W. Effect of resistance training on strength, postural control and gait velocity in older adults. Clinical Nursing Research. 1996;5(4):407–21. doi: 10.1177/105477389600500404. [DOI] [PubMed] [Google Scholar]
- Topp R, Woolley S, Hornyak J, 3rd, Khuder S, Kahaleh B. The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Archives of Physical Medicine & Rehabilitation. 2002;83(9):1187–95. doi: 10.1053/apmr.2002.33988. [DOI] [PubMed] [Google Scholar]
- Topp R, Boardley D, Morgan AL, Fahlman M, McNevin N. Exercise and functional tasks among adults who are functionally limited. Western Journal of Nursing Research. 2005;27(3):252–70. doi: 10.1177/0193945904271447. [DOI] [PubMed] [Google Scholar]
- Tracy BL, Byrnes WC, Enoka RM. Strength training reduces force fluctuations during anisometric contractions of the quadriceps femoris muscles in old adults. Journal of Applied Physiology. 2004;96(4):1530–40. doi: 10.1152/japplphysiol.00861.2003. [DOI] [PubMed] [Google Scholar]
- *.Tsutsumi T. The effects of strength training on mood, self-efficacy, cardiovascular reactivity and quality of life in older adults [thesis] Boston (MA): Boston University; 1997. [Google Scholar]
- Tsutsumi T, Don BM, Zaichkowsky LD, Delizonna LL. Physical fitness and psychological benefits of strength training in community dwelling older adults. Applied Human Science. 1997;16(6):257–66. doi: 10.2114/jpa.16.257. [DOI] [PubMed] [Google Scholar]
- Tsutsumi T, Don BM, Zaichkowsky LD, Takenaka K, Oka K, Ohno T. Comparison of high and moderate intensity of strength training on mood and anxiety in older adults. Perceptual and Motor Skills. 1998;87(3 Pt 1):1003–11. doi: 10.2466/pms.1998.87.3.1003. [DOI] [PubMed] [Google Scholar]
- Tyni-Lenne R, Dencker K, Gordon A, Jansson E, Sylven C. Comprehensive local muscle training increases aerobic working capacity and quality of life and decreases neurohormonal activation in patients with chronic heart failure. European Journal of Heart Failure. 2001;3(1):47–52. doi: 10.1016/s1388-9842(00)00087-8. [DOI] [PubMed] [Google Scholar]
- *.Vincent KR, Braith BW. Resistance exercise and bone turnover in elderly men and women. Medicine & Science in Sports & Exercise. 2002;34(1):17–23. doi: 10.1097/00005768-200201000-00004. [DOI] [PubMed] [Google Scholar]
- Vincent KR, Braith RW, Bottiglieri T, Vincent HK, Lowenthal DT. Homocysteine and lipoprotein levels following resistance training in older adults. Preventive Cardiology. 2003;6(4):197–203. doi: 10.1111/j.1520-037x.2003.01723.x. [DOI] [PubMed] [Google Scholar]
- Vincent KR, Braith RW, Feldman RA, Kallas HE, Lowenthal DT. Improved cardiorespiratory endurance following 6 months of resistance exercise in elderly men and women. Archives of Internal Medicine. 2002;162(6):673–8. doi: 10.1001/archinte.162.6.673. [DOI] [PubMed] [Google Scholar]
- Vincent KR, Braith RW, Feldman RA, Magyari PM, Cutler RB, Persin SA, et al. Resistance exercise and physical performance in adults aged 60 to 83. Journal of the American Geriatrics Society. 2002;50(6):1100–7. doi: 10.1046/j.1532-5415.2002.50267.x. [DOI] [PubMed] [Google Scholar]
- Westhoff MH, Stemmerik L, Boshuizen HC. Effects of a low-intensity strength-training program on knee-extensor strength and functional ability of frail older people. Journal of Aging and Physical Activity. 2000;8(4):325–42. [Google Scholar]
- Wieser M, Haber P. The effects of systematic resistance training in the elderly. International Journal of Sports Medicine. 2007;28(1):59–65. doi: 10.1055/s-2006-924057. [DOI] [PubMed] [Google Scholar]
- Wood RH, Reyes R, Welsch MA, Favaloro-Sabatier J, Sabatier M, Lee CM, et al. Concurrent cardiovascular and resistance training in healthy older adults. Medicine & Science in Sports & Exercise. 2001;33(10):1751–8. doi: 10.1097/00005768-200110000-00021. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Adami S, Gattie D, Braga V, Bianchini D, Rossini M. Site-specific effects of strength training on bone structure and geometry of ultradistal radius in postmenopausal women. Journal of Bone and Mineral Research. 1999;14(1):120–4. doi: 10.1359/jbmr.1999.14.1.120. [DOI] [PubMed] [Google Scholar]
- Adams KJ, Swank AM, Berning JM, Sevene-Adams PG, Barnard KL, et al. Progressive strength training in sedentary older African American women. Medicine & Science in Sports & Exercise. 2001;33(9):1567–76. doi: 10.1097/00005768-200109000-00021. [DOI] [PubMed] [Google Scholar]
- *.Agre JC, Pierce LE, Raab DM, McAdams M, Smith EL. Light resistance and stretching exercise in elderly women: effect upon strength. Archives of Physical Medicine and Rehabilitation. 1988;69(4):273–6. [PubMed] [Google Scholar]
- Raab DM, Agre JC, McAdam M, Smith EL. Light resistance and stretching exercise in elderly women: effect upon flexibility. Archives of Physical Medicine and Rehabilitation. 1988;69(4):268–72. [PubMed] [Google Scholar]
- Alexander JL. Effect of strength training on functional fitness in older chronic obstructive pulmonary disease patients. Arizona State University; 2003. dissertation. [Google Scholar]
- Aniansson A, Gustafsson E. Physical training in elderly men with special reference to quadriceps muscle strength and morphology. Clinical Physiology. 1981;1(1):87–98. [Google Scholar]
- Annesi JJ, Gann S, Westcott WW, Annesi JJ, Gann S, Westcott WW. Preliminary evaluation of a 10-wk. resistance and cardiovascular exercise protocol on physiological and psychological measures for a sample of older women. Perceptual & Motor Skills. 2004;98(1):163–70. doi: 10.2466/pms.98.1.163-170. [DOI] [PubMed] [Google Scholar]
- Ardman O. The effects of strength training on strength, mobility and balance in two groups of institutionalized elderly subjects. Montreal (Quebec): McGill University; 1998. dissertation. [Google Scholar]
- Ballard JE, McFarland C, Wallace LS, Holiday DB, Roberson G. The effect of 15 weeks of exercise on balance, leg strength, and reduction in falls in 40 women aged 65 to 89 years. Journal of the American Medical Womens Association. 2004;59(4):255–61. [PubMed] [Google Scholar]
- Barbosa AR, Santarem JM, Filho WJ, Marucci MFN. Effects of resistance training on the sit-and-reach test in elderly women. Journal of Strength & Conditioning Research. 2002;16(1):14–8. [PubMed] [Google Scholar]
- Baum K, Ruether T, Essfeld D. Reduction of blood pressure response during strength training through intermittent muscle relaxations. International Journal of Sports Medicine. 2003;24(6):441–5. doi: 10.1055/s-2003-41172. [DOI] [PubMed] [Google Scholar]
- Bean J, Herman S, Kiely DK, Callahan D, Mizer K, Frontera WR, et al. Weighted stair climbing in mobility-limited older people: a pilot study. Journal of the American Geriatrics Society. 2002;50(4):663–70. doi: 10.1046/j.1532-5415.2002.50160.x. [DOI] [PubMed] [Google Scholar]
- Bellew JW, Yates JW, Gater DR. The initial effects of low-volume strength training on balance in untrained older men and women. Journal of Strength & Conditioning Research. 2003;17(1):121–8. doi: 10.1519/1533-4287(2003)017<0121:tieolv>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Beniamini Y, Rubenstein JJ, Zaichkowsky LD, Leonard D, Crim MC. Effects of high-intensity strength training on quality-of-life parameters in cardiac rehabilitation patients. American Journal of Cardiology. 1997;80(7):841–6. doi: 10.1016/s0002-9149(97)00533-x. [DOI] [PubMed] [Google Scholar]
- Beniamini Y, Rubenstein JJ, Faigehbaum AD, Lichenstein AH, Crim MC. High-intensity strength training of patients enrolled in an outpatient cardiac rehabilitation program. Journal of Cardiopulmonary Rehabilitation. 1999;19(1):8–17. doi: 10.1097/00008483-199901000-00001. [DOI] [PubMed] [Google Scholar]
- Berg WP, Lapp BA. The effect of a “practical” resistance training intervention on mobility in independent, community-dwelling older adults. Journal of Aging and Physical Activity. 1998;6(1):18–35. [Google Scholar]
- Bernard S, Whittom F, Leblanc P, Jobin J, Belleau R, Berube C, et al. Aerobic and strength training in patients with chronic obstructive pulmonary disease. American Journal of Respiratory Care and Critical Care Medicine. 1999;159(3):896–901. doi: 10.1164/ajrccm.159.3.9807034. [DOI] [PubMed] [Google Scholar]
- Bilodeau M, Keen DA, Sweeney PJ, Shields RW, Enoka RM. Strength training can improve steadiness in persons with essential tremor. Muscle and Nerve. 2000;23:771–8. doi: 10.1002/(sici)1097-4598(200005)23:5<771::aid-mus15>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Binda SM, Culham EG, Brouwer B, Binda SM, Culham EG, Brouwer B. Balance, muscle strength, and fear of falling in older adults. Experimental Aging Research. 2003;29(2):205–19. doi: 10.1080/03610730303711. [DOI] [PubMed] [Google Scholar]
- Binder EF, Schechtman KB, Ehsani AA, Steger-May K, Brown M, Sinacore DR, et al. Effects of exercise training on frailty in community-dwelling older adults: results of a randomized, controlled trial. Journal of the American Geriatrics Society. 2002;50(12):1921–8. doi: 10.1046/j.1532-5415.2002.50601.x. [DOI] [PubMed] [Google Scholar]
- Binder EF, Yarasheski KE, Steger-May K, Sinacore DR, Brown M, Schechtman KB, et al. Effects of progressive resistance training on body composition in frail older adults: Results of a randomized, controlled trial. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2005;60(11):1425–31. doi: 10.1093/gerona/60.11.1425. [DOI] [PubMed] [Google Scholar]
- Boardley D, Fahlman M, Topp R, Morgan AL, McNevin N. The impact of exercise training on blood lipids in older adults. American Journal of Geriatric Cardiology. 2007;16(1):30–5. doi: 10.1111/j.1076-7460.2007.05353.x. [DOI] [PubMed] [Google Scholar]
- Braith RW, Magyari PM, Pierce GL, Edwards DG, Hill JA, White LJ, et al. Effect of resistance exercise on skeletal muscle myopathy in heart transplant recipients. American Journal of Cardiology. 2005;95(10):1192–8. doi: 10.1016/j.amjcard.2005.01.048. [DOI] [PubMed] [Google Scholar]
- Brandon LJ, Gaasch DA, Boyette LW, Lloyd AM. Effects of long-term resistive training on mobility and strength in older adults with diabetes. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(8):740–5. doi: 10.1093/gerona/58.8.m740. [DOI] [PubMed] [Google Scholar]
- Brandon LJ, Boyette LW, Lloyd A, Gaasch DA. Resistive training and long-term function in older adults. Journal of Aging and Physical Activity. 2004;12(1):10–28. doi: 10.1123/japa.12.1.10. [DOI] [PubMed] [Google Scholar]
- *.Brill PA, Matthews M, Mason J, Davis D, Mustafa T, Macera C. Improving functional performance through a group-based free weight strength training program in residents of two assisted living communities. Physical & Occupational Therapy in Geriatrics. 1998;15(3):57–69. [Google Scholar]
- Brill PA, Probst JC, Greenhouse DL, Schell B, Macera CA. Clinical feasibility of a free-weight strength-training program for older adults. Journal of the American Board of Family Practice. 1998;11(6):445–51. doi: 10.3122/jabfm.11.6.445. [DOI] [PubMed] [Google Scholar]
- Brose A, Parise G, Tarnopolsky MA. Creatine supplementation enhances isometric strength and body composition improvements following strength exercise training in older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(1):11–9. doi: 10.1093/gerona/58.1.b11. [DOI] [PubMed] [Google Scholar]
- Brown AB, McCartney N, Sale DG. Positive adaptations to weight-lifting in the elderly. Journal of Applied Physiology. 1990;69(5):1725–33. doi: 10.1152/jappl.1990.69.5.1725. [DOI] [PubMed] [Google Scholar]
- Brown M, Holloszy JO. Effects of a low intensity exercise program on selected physical performance characteristics of 60- to 70- year olds. Aging (Milan, Italy) 1991;3(2):129–39. doi: 10.1007/BF03323989. [DOI] [PubMed] [Google Scholar]
- Brown M, Sinacore DR, Ehsani AA, Binder EF, Holloszy JO, Kohrt WM. Low-intensity exercise as a modifier of physical frailty in older adults. Archives of Physical Medicine and Rehabilitation. 2000;81(7):960–5. doi: 10.1053/apmr.2000.4425. [DOI] [PubMed] [Google Scholar]
- Bunout B, Barrera G, de la Maza P, Avendano M, Gattas V, Petermann M, et al. Effects of nutritional supplementation and resistance training on muscle strength in free living elders. Results of one year follow. Journal of Nutrition, Health & Aging. 2004;8(2):68–75. [PubMed] [Google Scholar]
- Bunout D, Barrera G, Avendano M, de la Maza P, Gattas V, Leiva L, et al. Results of a community-based weight-bearing resistance training programme for healthy Chilean elderly subjects. Age and Ageing. 2005;34(1):80–3. doi: 10.1093/ageing/afi005. [DOI] [PubMed] [Google Scholar]
- Bunout D, Barrera G, de la Maza P, Avendano M, Gattas V, Petermann M, et al. The impact of nutritional supplementation and resistance training on the health and function of free-living Chilean elders: results of 18 months of follow-up. Journal of Nutrition. 2001;131(9):2441S–6S. doi: 10.1093/jn/131.9.2441S. [DOI] [PubMed] [Google Scholar]
- Bunout D, Barrera G, Leiva L, Gattas V, de la Maza MP, Avendano M, et al. Effects of vitamin D supplementation and exercise training on physical performance in Chilean vitamin D deficient elderly subjects. Experimental Gerontology. 2006;41(8):746–52. doi: 10.1016/j.exger.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Campbell WW, Joseph LJO, Anderson RA, Davey SL, Hinton J, Evans WJ. Effects of resistive training and chromium picolinate on body composition and skeletal muscle size in older women. International Journal of Sport Nutrition and Exercise Metabolism. 2002;12(2):125–35. doi: 10.1123/ijsnem.12.2.125. MEDLINE: Wrong outcomes and involved medication, not RCT. [DOI] [PubMed] [Google Scholar]
- Campbell WW, Joseph LJO, Ostlund RE, Jr, Anderson RA, Farrell PA, Evans WJ. Resistive training and chromium picolinate: Effects on inositols and liver and kidney functions in older adults. International Journal of Sport Nutrition & Exercise Metabolism. 2004;14(4):430–42. doi: 10.1123/ijsnem.14.4.430. [DOI] [PubMed] [Google Scholar]
- Cancela Carral JM, Romo Perez V, Camina Fernandez F. Effect of strength program on a 65 years old elderly woman [Spanish] Gerokomos. 2003;14(2):80–9. [Google Scholar]
- Candow DG, Chilibeck PD, Chad KE, Chrusch MJ, Shawn Davison K, Burke DG. Effect of ceasing creatine supplementation while maintaining resistance training in older men. Journal of Aging & Physical Activity. 2004;12(3):219–31. doi: 10.1123/japa.12.3.219. [DOI] [PubMed] [Google Scholar]
- Capodaglio P, Facioli M, Burroni E, Giordano A, Ferri A, Scaglioni G. Effectiveness of a home-based strengthening program for elderly males in Italy. A preliminary study. Aging-Clinical & Experimental Research. 2002;14(1):28–34. doi: 10.1007/BF03324414. [DOI] [PubMed] [Google Scholar]
- Carter ND, Khan KM, McKay HA, Petit MA, Waterman C, Heinonen A, et al. Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: randomized controlled trial. CMAJ. 2002;167(9):997–1004. [PMC free article] [PubMed] [Google Scholar]
- Carter JM, Bemben DA, Knehans AW, Bemben MG, Witten MS. Does nutritional supplementation influence adaptability of muscle to resistance training in men aged 48 to 72 years. Journal of Geriatric Physical Therapy. 2005;28(2):40–7. doi: 10.1519/00139143-200508000-00002. [DOI] [PubMed] [Google Scholar]
- Carvalho J, Oliveira J, Magalhaes J, Ascensao A, Cabri J, Soares JMC. The influence of initial strength levels on isokinetic torque after training in elderly adults; European College of Sport Science, Proceedings of the 7th annual congress of the European College of Sport Science; 2002 July 24-28; Athens Greece. Pashalidis Medical Publisher; p. 513. [Google Scholar]
- Cauza E, Hanusch-Enserer U, Strasser B, Kostner K, Dunky A, Haber P. Strength and endurance training lead to different post exercise glucose profiles in diabetic participants using a continuous subcutaneous glucose monitoring system. European Journal of Clinical Investigation. 2005;35(12):745–51. doi: 10.1111/j.1365-2362.2005.01573.x. [DOI] [PubMed] [Google Scholar]
- Cauza E, Hanusch-Enserer U, Strasser B, Ludvik B, Metz-Schimmerl S, Pacini G, et al. The relative benefits of endurance and strength training on the metabolic factors and muscle function of people with type 2 diabetes mellitus. Archives of Physical Medicine and Rehabilitation. 2005;86(8):1527–33. doi: 10.1016/j.apmr.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Chaloupka V, Elbl L, Nehyba S. Strength training in patients after myocardial infarct. Vnitrni Lekarstvi. 2000;46(12):829–34. Silovy trenink u nemocnych po infarktu myokardu. [PubMed] [Google Scholar]
- Chetlin RD, Gutmann L, Tarnopolsky M, Ullrich IH, Yeater RA. Resistance training effectiveness in patients with Charcot-Marie-Tooth disease: recommendations for exercise prescription. Archives of Physical Medicine & Rehabilitation. 2004;85(8):1217–23. doi: 10.1016/j.apmr.2003.12.025. [DOI] [PubMed] [Google Scholar]
- Chiba A. Positive effects of resistance training on QOL in the frail elderly. Japanese Journal of Public Health. 2006;53(11):851–8. [PubMed] [Google Scholar]
- Chien MY, Yang RS, Tsauo JY. Home-based trunk-strengthening exercise for osteoporotic and osteopenic postmenopausal women without fracture - A pilot study. Clinical Rehabilitation. 2005;19(1):28–36. doi: 10.1191/0269215505cr844oa. [DOI] [PubMed] [Google Scholar]
- Connelly DM, Vandervoort AA. Effects of detraining on knee extensor strength and functional mobility in a group of elderly women. Journal of Orthopaedic & Sports Physical Therapy. 1997;26(6):340–6. doi: 10.2519/jospt.1997.26.6.340. [DOI] [PubMed] [Google Scholar]
- *.Connelly DM, Vandervoort AA. Improvement in knee extensor strength of institutionalized elderly women after exercise with ankle weights. Physiotherapy Canada. 1995;41(1):15–23. [Google Scholar]
- Connelly DM, Vandervoort AA. Effects of isokinetic strength training on concentric and eccentric torque development in the ankle dorsiflexors of older adults. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2000;55:B465–72. doi: 10.1093/gerona/55.10.b465. [DOI] [PubMed] [Google Scholar]
- Cramp MC, Greenwood RJ, Gill M, Rothwell JC, Scott OM. Low intensity strength training for ambulatory stroke patients. Disability & Rehabilitation. 2006;28(13-14):883–9. doi: 10.1080/09638280500535157. [DOI] [PubMed] [Google Scholar]
- Cress ME, Thomas DP, Johnson J, Kasch FW, Cassens RG, Smith EL, et al. Effect of training on VO2 max, thigh strength and muscle morphology in septuagenarian women. Medicine and Science in Sports and Exercise. 1991;23:752–8. [PubMed] [Google Scholar]
- Cress ME, Buchner DM, Questad KA, Esselman PC, de Lateur BJ, Schwartz RS. Exercise: effects on physical functional performance in older adults. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 1999;54(5):M242–8. doi: 10.1093/gerona/54.5.m242. [DOI] [PubMed] [Google Scholar]
- Daepp C, Vogt M, Klossner S, Popp A, Lippuner K, Hoppeler H. Slimmer and stronger - the effect of eccentric exercise in the elderly. Schweizerische Zeitschrift Fuer Sportmedizin Und Sporttraumatologie/Revue Suisse De Medecine Et De Traumatologie Du Sport/Rivista Svizzera Di Medicina e Traumatologia Dello Sport. 2006;54(2):71. 1422–0644. [Google Scholar]
- Daly RM, Dunstan DW, Owen N, Jolley D, Shaw JE, Zimmet PZ. Does high-intensity resistance training maintain bone mass during moderate weight loss in older overweight adults with type 2 diabetes? Osteoporosis International. 2005;16(12):1703–12. doi: 10.1007/s00198-005-1906-4. [DOI] [PubMed] [Google Scholar]
- de Bruin ED, Menzi C, Waelle R, Murer K. Strength training and balance performance compared to combined strength and agility training in elderly over 80 years: a three months RCT. Isokinetics and Exercise Science. 2004;12(1):33–4. [Google Scholar]
- *.de Bruin ED, Murer K. Effect of additional functional exercises on balance in elderly people. Clinical Rehabilitation. 2007;21(2):112–21. doi: 10.1177/0269215506070144. [DOI] [PubMed] [Google Scholar]
- de Vito G, Bernardi M, Forte R, Pulejo C, Figura F. Effects of a low-intensity programme on VO2 max and maximal instantaneous peak power in elderly women. European Journal of Applied Physiology and Occupational Physiology. 1999;80(3):227–32. doi: 10.1007/s004210050586. [DOI] [PubMed] [Google Scholar]
- DeBolt LS, McCubbin JA, DeBolt LS, McCubbin JA. The effects of home-based resistance exercise on balance, power, and mobility in adults with multiple sclerosis. Archives of Physical Medicine & Rehabilitation. 2004;85(2):290–7. doi: 10.1016/j.apmr.2003.06.003. [DOI] [PubMed] [Google Scholar]
- Delagardelle C, Feiereisen P, Autier P, Shita R, Krecke R, Beissel J. Strength/endurance training versus endurance training in congestive heart failure. Medicine & Science in Sports & Exercise. 2002;34(12):1868–72. doi: 10.1097/00005768-200212000-00002. [DOI] [PubMed] [Google Scholar]
- Delecluse C, Colman V, Roelants M, Verschueren S, Derave W, Ceux T, et al. Exercise programs for older men: mode and intensity to induce the highest possible health-related benefits. Preventive Medicine. 2004;39(4):823–33. doi: 10.1016/j.ypmed.2004.03.023. [DOI] [PubMed] [Google Scholar]
- De Vito CA, Morgan RO, Duque M, Abdel-Moty E, Virnig BA. Physical performance effects of low-intensity exercise among clinically defined high-risk elders. Gerontology. 2003;49(3):146–54. doi: 10.1159/000069168. [DOI] [PubMed] [Google Scholar]
- Dibble LE, Hale T, Marcus RL, Gerber JP, Lastayo PC. The safety and feasibility of high-force eccentric resistance exercise in persons with Parkinson's disease. Archives of Physical Medicine & Rehabilitation. 2006;87(9):1280–2. doi: 10.1016/j.apmr.2006.05.016. [DOI] [PubMed] [Google Scholar]
- Dibble LE, Hale TF, Marcus RL, Droge J, Gerber JP, LaStayo PC. High-intensity resistance training amplifies muscle hypertrophy and functional gains in persons with Parkinson's disease. Movement Disorders. 2006;21(9):1444–52. doi: 10.1002/mds.20997. [DOI] [PubMed] [Google Scholar]
- Dunstan DW, Daly RM, Owen N, Jolley D, De Courten M, Shaw J, et al. High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Diabetes Care. 2002;25(10):1729–36. doi: 10.2337/diacare.25.10.1729. [DOI] [PubMed] [Google Scholar]
- Dunstan DW, Daly RM, Owen N, Jolley D, Vulikh E, Shaw J, et al. Home-based resistance training is not sufficient to maintain improved glycemic control following supervised training in older individuals with type 2 diabetes. Diabetes Care. 2005;28(1):3–9. doi: 10.2337/diacare.28.1.3. [DOI] [PubMed] [Google Scholar]
- Dupler TL, Cortes C. Effects of a whole-body resistive training regimen in the elderly. Gerontology. 1993;39(6):314–9. doi: 10.1159/000213548. [DOI] [PubMed] [Google Scholar]
- Fernandez Ramirez AI, Fernandez Ramirez AS. Effect of an exercise program on physical fitness of institutionalized elderly men. Archivos de Medicina del Deporte. 1999;16(72):325–32. [Google Scholar]
- Ferrara CM, Goldberg AP, Ortmeyer HK, Ryan AS. Effects of aerobic and resistive exercise training on glucose disposal and skeletal muscle metabolism in older men. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2006;61(5):480–7. doi: 10.1093/gerona/61.5.480. [DOI] [PubMed] [Google Scholar]
- Ferri A, Scaglioni G, Pousson M, Capodaglio P, Van Hoecke J, Narici MV. Strength and power changes of the human plantar flexors and knee extensors in response to resistance training in old age. Acta Physiologica Scandinavica. 2003;177(1):69–78. doi: 10.1046/j.1365-201X.2003.01050.x. [DOI] [PubMed] [Google Scholar]
- Fiatarone MA, Marks ED, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA. 1990;263(22):3029–34. [PubMed] [Google Scholar]
- Fisher NM, Pendergast DR, Calkins E. Muscle rehabilitation in impaired elderly nursing home residents. Archives of Physical Medicine and Rehabilitation. 1991;72:181–5. [PubMed] [Google Scholar]
- *.Fisher NM, Pendergast DR, Gresham GE, Calkins E. Muscle rehabilitation: its effect on muscular and functional performance of patients with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation. 1991;72(6):367–74. [PubMed] [Google Scholar]
- Forte R, De Vito G, Figura F. Effects of dynamic resistance training on heart rate variability in healthy older women. European Journal of Applied Physiology. 2003;89(1):85–9. doi: 10.1007/s00421-002-0775-1. [DOI] [PubMed] [Google Scholar]
- Frontera WR, Meredith C, O'Reilly KP, Knuttgen HG, Evans W. Strength conditioning in older men: skeletal muscle hypertrophy and improved function. Journal of Applied Physiology. 1988;64(3):1038–44. doi: 10.1152/jappl.1988.64.3.1038. [DOI] [PubMed] [Google Scholar]
- Frontera WR, Meredith CN, O'Reilly KP, Evans WJ. Strength training and determinants of VO2 Max in older men. Journal of Applied Physiology. 1990;68(1):329–33. doi: 10.1152/jappl.1990.68.1.329. [DOI] [PubMed] [Google Scholar]
- Galvao DA, Nosaka K, Taaffe DR, Spry N, Kristjanson LJ, McGuigan MR, et al. Resistance training and reduction of treatment side effects in prostate cancer patients. Medicine & Science in Sports & Exercise. 2006;38(12):2045–52. doi: 10.1249/01.mss.0000233803.48691.8b. [DOI] [PubMed] [Google Scholar]
- Grimby G, Aniansson A, Hedberg M, Henning GB, Grangard U, Kvist H. Training can improve muscle strength and endurance in 78- to 84-year-old men. Journal of Applied Physiology. 1992;73(6):2517–23. doi: 10.1152/jappl.1992.73.6.2517. [DOI] [PubMed] [Google Scholar]
- Gur H, Cakin N, Akova B, Okay E, Kucukoglu S. Concentric versus combined concentric-eccentric isokinetic training: effects on functional capacity and symptoms in patients with osteoarthritis of the knee. Archives of Physical Medicine and Rehabilitation. 2002;83(3):308–16. doi: 10.1053/apmr.2002.30620. [DOI] [PubMed] [Google Scholar]
- Hageman PA, Thomas VS. Gait performance in dementia: the effects of a 6-week resistance training program in an adult day-care setting. International Journal of Geriatric Psychiatry. 2002;17(4):329–34. doi: 10.1002/gps.597. [DOI] [PubMed] [Google Scholar]
- Hakkinen A, Sokka T, Kotaniemi A, Kautiainen H, Jappinen I, Laitinen L, et al. Dynamic strength training in patients with early rheumatoid arthritis increases muscle strength but not bone mineral density. Journal of Rheumatology. 1999;26(6):1257–63. [PubMed] [Google Scholar]
- Hameed M, Lange KHW, Andersen JL, Schjerling P, Kjaer M, Harridge SDR, et al. The effect of recombinant human growth hormone and resistance training on IGF-I mRNA expression in the muscles of elderly men. Journal of Physiology. 2004;555(1):231–40. doi: 10.1113/jphysiol.2003.051722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartard M, Haber P, Ilieva D, Preisinger E, Seidl G, Huber J. Systematic strength training as a model of therapeutic intervention. A controlled trial in postmenopausal women with osteopenia. American Journal of Physical Medicine & Rehabilitation. 1996;75(1):21–8. doi: 10.1097/00002060-199601000-00006. [DOI] [PubMed] [Google Scholar]
- Haub MD, Wells AM, Tarnopolsky MA, Campbell WW. Effect of protein source on resistive-training-induced changes in body composition and muscle size in older men. American Journal of Clinical Nutrition. 2002;76(3):511–7. doi: 10.1093/ajcn/76.3.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiwe S, Clyne N, Tollback A, Borg K. Effects of regular resistance training on muscle histopathology and morphometry in elderly patients with chronic kidney disease. American Journal of Physical Medicine & Rehabilitation. 2005;84(11):865–74. doi: 10.1097/01.phm.0000184244.86297.6b. [DOI] [PubMed] [Google Scholar]
- Henwood TR, Taaffe DR. Short-term resistance training and the older adult: The effect of varied programmes for the enhancement of muscle strength and functional performance. Clinical Physiology & Functional Imaging. 2006;26(5):305–13. doi: 10.1111/j.1475-097X.2006.00695.x. [DOI] [PubMed] [Google Scholar]
- Hess JA, Woollacott M. Effect of high-intensity strength-training on functional measures of balance ability in balance-impaired older adults. Journal of Manipulative & Physiological Therapeutics. 2005;28(8):582–90. doi: 10.1016/j.jmpt.2005.08.013. [DOI] [PubMed] [Google Scholar]
- Hess JA, Woollacott M, Shivitz N. Ankle force and rate of force production increase following high intensity strength training in frail older adults. Aging-Clinical & Experimental Research. 2006;18(2):107–115. doi: 10.1007/BF03327425. [DOI] [PubMed] [Google Scholar]
- Hirsch MA, Toole T, Maitland CG, Rider RA. The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson's disease. Archives of Physical Medicine and Rehabilitation. 2003;84(8):1109–17. doi: 10.1016/s0003-9993(03)00046-7. [DOI] [PubMed] [Google Scholar]
- Host HH, Sinacore DR, Bohnert KL, Steger-May K, Brown M, Binder EF. Training-induced strength and functional adaptations after hip fracture. Physical Therapy. 2007;87:292–303. doi: 10.2522/ptj.20050396. [DOI] [PubMed] [Google Scholar]
- Huggett DL, Elliott ID, Overend TJ, Vandervoort AA. Comparison of heart-rate and blood-pressure increases during isokinetic eccentric versus isometric exercise in older adults. Journal of Aging & Physical Activity. 2004;12(2):157–69. doi: 10.1123/japa.12.2.157. [DOI] [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell R, Pollak N, Huber G, Sharma L. Impact of the fit and strong intervention on older adults with osteoarthritis. Gerontologist. 2004;44(2):217–28. doi: 10.1093/geront/44.2.217. [DOI] [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell RT, Huber G, Pollak N, Sharma L, et al. Long-term impact of fit and strong! On older adults with osteoarthritis. Gerontologist. 2006;46(6):801–14. doi: 10.1093/geront/46.6.801. [DOI] [PubMed] [Google Scholar]
- Humphries B, Newton RU, Bronks R, Marshall S, McBride J, Triplett-McBride T, et al. Effect of exercise intensity on bone density, strength, and calcium turnover in older women. Medicine & Science in Sports & Exercise. 2000;32(6):1043–50. doi: 10.1097/00005768-200006000-00002. [DOI] [PubMed] [Google Scholar]
- Hung C, Daub B, Black B, Welsh R, Quinney A, Haykowsky M. Exercise training improves overall physical fitness and quality of life in older women with coronary artery disease. Chest. 2004;126(4):1026–31. doi: 10.1378/chest.126.4.1026. see comment. [DOI] [PubMed] [Google Scholar]
- Hunter GR, Treuth MS, Weinsier RL, Kekes-Szabo T, Kell SH, Roth DL, et al. The effects of strength conditioning on older women's ability to perform daily tasks. Journal of the American Geriatrics Society. 1995;43(7):756–60. doi: 10.1111/j.1532-5415.1995.tb07045.x. [DOI] [PubMed] [Google Scholar]
- Hunter GR, Bryan DR, Wetzstein CJ, Zuckerman PA, Bamman MM. Resistance training and intra-abdominal adipose tissue in older men and women. Medicine & Science in Sports & Exercise. 2002;34(6):1023–8. doi: 10.1097/00005768-200206000-00019. [DOI] [PubMed] [Google Scholar]
- Ibanez J, Izquierdo M, Arguelles I, Forga L, Larrion JL, Garcia-Unciti M, et al. Twice-weekly progressive resistance training decreases abdominal fat and improves insulin sensitivity in older men with type 2 diabetes. Diabetes Care. 2005;28(3):662–7. doi: 10.2337/diacare.28.3.662. [DOI] [PubMed] [Google Scholar]
- Ivey FM, Tracy BL, Lemmer JT, NessAiver M, Metter EJ, Fozard JL, et al. Effects of strength training and detraining on muscle quality: age and gender comparisons. Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2000;55(3):B152–7. doi: 10.1093/gerona/55.3.b152. [DOI] [PubMed] [Google Scholar]
- Johansen KL, Painter PL, Sakkas GK, Gordon P, Doyle J, Shubert T. Effects of resistance exercise training and nandrolone decanoate on body composition and muscle function among patients who receive hemodialysis: A randomized, controlled trial. Journal of the American Society of Nephrology. 2006;17(8):2307–14. doi: 10.1681/ASN.2006010034. [DOI] [PubMed] [Google Scholar]
- Jones D, Rutherford O. Human muscle strength training: The effects of three different regimes and the nature of the resultant changes. Journal of Physiology. 1987;391:1–11. doi: 10.1113/jphysiol.1987.sp016721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judge JO, Kleppinger A, Kenny A, Smith JA, Biskup B, Marcella G. Home-based resistance training improves femoral bone mineral density in women on hormone therapy. Osteoporosis International. 2005;16(9):1096–108. doi: 10.1007/s00198-004-1816-x. [DOI] [PubMed] [Google Scholar]
- Katula JA, Sipe M, Rejeski WJ, Focht BC. Strength training in older adults: an empowering intervention. Medicine and Science in Sports and Exercise. 2006;38(1):106–11. doi: 10.1249/01.mss.0000183373.95206.2f. [DOI] [PubMed] [Google Scholar]
- Kerr D, Ackland T, Maslen B, Morton A, Prince R. Resistance training over 2 years increases bone mass in calcium-replete postmenopausal women. Journal of Bone & Mineral Research. 2001;16(1):175–81. doi: 10.1359/jbmr.2001.16.1.175. [DOI] [PubMed] [Google Scholar]
- Kolbe-Alexander TL, Charlton KE, Lambert EV. Effectiveness of a community based low intensity exercise program for older adults. Journal of Nutrition, Health & Aging. 2006;10(1):21–9. [PubMed] [Google Scholar]
- Komatireddy GR, Leitch RW, Cella K, Browning G, Minor M. Efficacy of low load resistive muscle training in patients with rheumatoid arthritis functional class II and III. Journal of Rheumatology. 1997;24(8):1531–9. [PubMed] [Google Scholar]
- La Forge R. Effect of high-intensity resistance exercise on elderly bones. IDEA Health & Fitness Source. 2002;20(5):17. 1096–8156. [Google Scholar]
- Labarque V, 'T Eijnde BO, Van Leemputte M. Resistance training alters torque-velocity relation of elbow flexors in elderly men. Medicine & Science in Sports & Exercise. 2002;34(5):851–56. doi: 10.1097/00005768-200205000-00019. L ' entrainement de force altere la relation torsion–velocite des muscles flechisseurs du coude chez les hommes ages. 0195–9131. [DOI] [PubMed] [Google Scholar]
- Lambert CP, Sullivan DH, Freeling SA, Lindquist DM, Evans WJ. Effects of testosterone replacement and/or resistance exercise on the composition of megestrol acetate stimulated weight gain in elderly men: A randomized controlled trial. Journal of Clinical Endocrinology & Metabolism. 2002;87(5):2100–6. doi: 10.1210/jcem.87.5.8505. [DOI] [PubMed] [Google Scholar]
- Lambert CP, Sullivan DH, Evans WJ. Megestrol acetate-induced weight gain does not negatively affect blood lipids in elderly men: Effects of resistance training and testosterone replacement. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(7):644–647. doi: 10.1093/gerona/58.7.m644. [DOI] [PubMed] [Google Scholar]
- Lamotte M, Niset G, Van de Borne P. The effect of different intensity modalities of resistance training on beat-to-beat blood pressure in cardiac patients. European Journal of Cardiovascular Prevention & Rehabilitation. 2005;12(1):12–7. [PubMed] [Google Scholar]
- Levinger I, Bronks R, Cody DV, Linton I, Davie A. Resistance training for chronic heart failure patients on beta blocker medications. International Journal of Cardiology. 2005;102(3):493–9. doi: 10.1016/j.ijcard.2004.05.061. [DOI] [PubMed] [Google Scholar]
- Lexell J, Robertsson E, Stenstrom E. Effects of strength training in elderly women. Journal of the American Geriatrics Society. 1992;40(2):190–1. doi: 10.1111/j.1532-5415.1992.tb01946.x. letter. [DOI] [PubMed] [Google Scholar]
- Lexell J, Downham DY, Larsson Y, Bruhn E, Morsing B. Heavy-resistance training in older Scandinavian men and women: short- and long-term effects on arm and leg muscles. Scandinavian Journal of Medicine & Science in Sports. 1995;5(6):329–41. doi: 10.1111/j.1600-0838.1995.tb00055.x. [DOI] [PubMed] [Google Scholar]
- Littbrand H, Rosendahl E, Lindelof N, Lundin-Olsson L, Gustafson Y, Nyberg L. A high-intensity functional weight-bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: evaluation of the applicability with focus on cognitive function. Physical Therapy. 2006;86(4):489–98. [PubMed] [Google Scholar]
- Liu SW, Liu HB, Tang D. Strengthened training of knee joint isolated movement for ambulation ability in patients with stroke. Zhongguo Linchuang Kangfu. 2004;8(25):5214–5. Chinese. [Google Scholar]
- Liu-Ambrose TYL, Khan KM, Eng JJ, Heinonen A, McKay HA. Both resistance and agility training increase cortical bone density in 75- to 85-year-old women with low bone mass: A 6-month randomized controlled trial. Journal of Clinical Densitometry. 2004;7(4):390–8. doi: 10.1385/jcd:7:4:390. [DOI] [PubMed] [Google Scholar]
- Loeppky JA, Gurney B, Kobayashi Y, Icenogle MV. Effects of ischemic training on leg exercise endurance. Journal of Rehabilitation Research and Development. 2005;42(4):511–21. doi: 10.1682/jrrd.2004.06.0069. [DOI] [PubMed] [Google Scholar]
- Lohman T, Going S, Pamenter R, Hall M, Boyden T, Houtkooper L, et al. Effects of resistance training on regional and total bone mineral density in premenopausal women: a randomized prospective study. Journal of Bone & Mineral Research. 1995;10(7):1015–24. doi: 10.1002/jbmr.5650100705. [DOI] [PubMed] [Google Scholar]
- Maddalozzo GF, Snow CM. High intensity resistance training: effects on bone in older men and women. Calcified Tissue International. 2000;66(6):394–404. doi: 10.1007/s002230010081. [DOI] [PubMed] [Google Scholar]
- Magnusson G, Gordon A, Kaijser L, Sylven C, Isberg B, Karpakka J, et al. High intensity knee extensor training in patients with chronic heart failure. European Heart Journal. 1996;17(7):1048–55. doi: 10.1093/oxfordjournals.eurheartj.a015001. [DOI] [PubMed] [Google Scholar]
- Marcora SM, Lemmey AB, Maddison PJ. Can progressive resistance training reverse cachexia in patients with rheumatoid arthritis? Results of a pilot study. Journal of Rheumatology. 2005;32(6):1031–9. [PubMed] [Google Scholar]
- Martin Ginis KA, Latimer AE, Brawley LR, Jung ME, Hicks AL. Weight training to activities of daily living: Helping older adults make a connection. Medicine & Science in Sports & Exercise. 2006;38(1):116–21. doi: 10.1249/01.mss.0000183200.64996.ef. [DOI] [PubMed] [Google Scholar]
- McCool J, Schneider J. Home-based leg strengthening for older adults initiated through private practice. Preventative Medicine. 1991;28:105–10. doi: 10.1006/pmed.1998.0406. [DOI] [PubMed] [Google Scholar]
- McMurdo M, Rennie L. Improvements in quadriceps strength with regular seated exercise in the institutionalised elderly. Archives of Physical Medicine and Rehabilitation. 1994;75:600–3. [PubMed] [Google Scholar]
- Mobily KE, Mobily PR, Raimondi RM, Walter KL, Rubenstein LM. Strength training and falls among older adults: a community-based TR intervention. Annual in Therapeutic Recreation. 2004;13:1–11. 109–18. [Google Scholar]
- Morey MC, Cowper PA, Feussner JR, DiPasquale RC, Crowley GM, Kitzman DW, et al. Evaluation of a supervised exercise program in a geriatric population. Journal of the American Geriatrics Society. 1989;37:348–54. doi: 10.1111/j.1532-5415.1989.tb05503.x. [DOI] [PubMed] [Google Scholar]
- Morey MC, Cowper PA, Feussner JR, DiPasquale RC, Crowley GM, Sullivan RJ., Jr Two-year trends in physical performance following supervised exercise among community-dwelling older veterans. Journal of the American Geriatrics Society. 1991;39(6):549–54. doi: 10.1111/j.1532-5415.1991.tb03591.x. [DOI] [PubMed] [Google Scholar]
- Morse CI, Thom JM, Mian OS, Muirhead A, Birch KM, Narici MV. Muscle strength, volume and activation following 12-month resistance training in 70-year-old males. European Journal of Applied Physiology. 2005;95(2-3):197–204. doi: 10.1007/s00421-005-1342-3. [DOI] [PubMed] [Google Scholar]
- Narici MV, Roi GS, Landoni L, Minetti AE, Cerretelli P. Changes in force, cross-sectional area and neural activation during strength training and detraining of the human quadriceps. European Journal of Applied Physiology and Occupational Physiology. 1989;59(4):310–9. doi: 10.1007/BF02388334. [DOI] [PubMed] [Google Scholar]
- Hausdorff JM, Nelson ME, Kaliton D, Layne JE, Bernstein MJ, Nuernberger A, et al. Etiology and modification of gait instability in older adults: A randomized controlled trial of exercise. Journal of Applied Physiology. 2001;90:2117–29. doi: 10.1152/jappl.2001.90.6.2117. [DOI] [PubMed] [Google Scholar]
- *.Nelson ME, Layne JE, Nuernberger A, Allen MJ, Judge J, Kailiton D, et al. Home-based exercise training in the frail elderly: Effects on physical performance. Medicine and Science in Sports and Exercise. 1997;29(Suppl 5):S110. [Google Scholar]
- Ochala J, Lambertz D, Van Hoecke J, Pousson M, Ochala J, Lambertz D, et al. Effect of strength training on musculotendinous stiffness in elderly individuals. European Journal of Applied Physiology. 2005;94(1-2):126–33. doi: 10.1007/s00421-004-1299-7. [DOI] [PubMed] [Google Scholar]
- Ohira T, Schmitz KH, Ahmed RL, Yee D. Effects of weight training on quality of life in recent breast cancer survivors: the Weight Training for Breast Cancer Survivors (WTBS) study. Cancer. 2006;106(9):2076–83. doi: 10.1002/cncr.21829. [DOI] [PubMed] [Google Scholar]
- Oka RK, De Marco T, Haskell WL, Botvinick E, Dae MW, Bolen K, et al. Impact of a home-based walking and resistance training program on quality of life in patients with heart failure. American Journal of Cardiology. 2000;85(3):365–9. doi: 10.1016/s0002-9149(99)00748-1. [DOI] [PubMed] [Google Scholar]
- Okawa T, Sato T, Koike T. Effect of exercises on bone mineral density and physical strength in elderly women. Nippon Rinsho - Japanese Journal of Clinical Medicine. 2004;62(Suppl 2):510–4. [PubMed] [Google Scholar]
- Okumiya K, Matsubayashi K, Wada T, Kimura S, Doi Y, Ozawa T. Effects of exercise on neurobehavioral function in community-dwelling older people more than 75 years of age. Journal of the American Geriatrics Society. 1996;44(5):569–72. doi: 10.1111/j.1532-5415.1996.tb01444.x. [DOI] [PubMed] [Google Scholar]
- Panton LB, Golden J, Broeder CE, Browder KD, Cestaro-Seifer DJ, Seifer FD. The effects of resistance training on functional outcomes in patients with chronic obstructive pulmonary disease. European Journal of Applied Physiology. 2004;91(4):443–9. doi: 10.1007/s00421-003-1008-y. [DOI] [PubMed] [Google Scholar]
- Parsons D, Foster V, Harman F, Dickinson A, Olivia P, Westerlind K. Balance and strength changes in elderly subjects after heavy resistance strength training. Medicine and Science in Sports and Exercise. 1992;24(Suppl 5):S21. abstract. [Google Scholar]
- Perhonen M, Komi P, Hakkinen K, Von Bonsdorff H, Partio E. Strength training and neuromuscular function in elderly people with total knee endoprosthesis. Scandinavian Journal of Medicine & Science in Sports. 1992;2:234–43. [Google Scholar]
- Perkins L, Kaiser H. Results of short-term isotonic and isometric exercise programs in persons over sixty. Physical Therapy Review. 1961;41:633–5. doi: 10.1093/ptj/41.9.633. [DOI] [PubMed] [Google Scholar]
- Perrig-Chiello P, Perrig WJ, Ehrsam R, Staehelin HB, Krings F. The effects of resistance training on well-being and memory in elderly volunteers. Age and Ageing. 1998;27(4):469–76. doi: 10.1093/ageing/27.4.469. [DOI] [PubMed] [Google Scholar]
- Petrella R, Bartha C. Home based exercise therapy for older patients with knee osteoarthritis: a randomized clinical trial. Journal of Rheumatology. 2000;27(9):2215–21. [PubMed] [Google Scholar]
- Phillips WT, Ziuraitis JR. Energy cost of single-set resistance training in older adults. Journal of Strength and Conditioning Research. 2004;18(3):606–9. doi: 10.1519/1533-4287(2004)18<606:ECOSRT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Pyka G, Lindenberger E, Charette S, Marcux R. Muscle strength and fiber adaptations to a year-long resistance training program. Journal of Gerontology. 1994;49(1):M22–7. doi: 10.1093/geronj/49.1.m22. [DOI] [PubMed] [Google Scholar]
- Rabelo HT, Oliveira RJ, Bottaro M. Effects of resistance training on activities of daily living in older women. Biology of Sport. 2004;21(4):325–36. 0860–021X. [Google Scholar]
- Ramsbottom R, Ambler A, Potter J, Jordan B, Nevill A, Williams C. The effect of 6 months training on leg power, balance, and functional mobility of independently living adults over 70 years old. Journal of Aging & Physical Activity. 2004;12(4):497–510. doi: 10.1123/japa.12.4.497. [DOI] [PubMed] [Google Scholar]
- Reeves ND, Narici MV, Maganaris CN. Effect of resistance training on skeletal muscle-specific force in elderly humans. Scandinavian Journal of Medicine & Science in Sports. 2004;14(2):134–5. doi: 10.1152/japplphysiol.00688.2003. Abstract. 0905–7188. [DOI] [PubMed] [Google Scholar]
- Reeves ND, Maganaris CN, Narici MV. Plasticity of dynamic muscle performance with strength training in elderly humans. Muscle & Nerve. 2005;31(3):355–64. doi: 10.1002/mus.20275. [DOI] [PubMed] [Google Scholar]
- Reeves ND, Narici MV, Maganaris CN. Musculoskeletal adaptations to resistance training in old age. Manual Therapy. 2006;11(3):192–6. doi: 10.1016/j.math.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Richards D. Efficacy of upper extremity strength training on upper extremity functional performance among elderly long-term care residents [thesis] Pittsburgh (PA): Univ. of Pittsburgh; 1996. [Google Scholar]
- Roman WJ, Fleckenstein J, Stray-Gundersen J, Alway SE, Peshock R, Gonyea WJ. Adaptations in the elbow flexors of elderly males after heavy-resistance training. Journal of Applied Physiology. 1993;74(2):750–4. doi: 10.1152/jappl.1993.74.2.750. [DOI] [PubMed] [Google Scholar]
- Rooks D, Kiel D, Parsons C, Hayes W. Self-paced resistance training and walking exercise in community-dwelling older adults: effects on neuromotor performance. Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 1997;52(3):M161–8. doi: 10.1093/gerona/52a.3.m161. [DOI] [PubMed] [Google Scholar]
- Salli A, Ugurlu H, Emlik D. Comparison of the effectiveness of concentric, combined concentric-eccentric and isometric exercises on symptoms and functional capacity in patients with knee osteoarthritis. Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi. 2006;52(2):61–7. Diz Osteoartritinde Konsantrik, Kombine Konsantrik–Eksantrik ve Izometrik Egzersizlerin Semptomlar ve Fonksiyonel Kapasite Uzerine Etkinliginin Karsilastirilmasi. [Google Scholar]
- Sallinen J, Pakarinen A, Fogelholm M, Sillanpaa E, Alen M, Volek JS, et al. Serum basal hormone concentrations and muscle mass in aging women: effects of strength training and diet. International Journal of Sport Nutrition & Exercise Metabolism. 2006;16(3):316–31. doi: 10.1123/ijsnem.16.3.316. [DOI] [PubMed] [Google Scholar]
- Sanders S. The effects of two modes of strength training on elderly men [thesis] Minneapolis (MN): Walden University; 1998. [Google Scholar]
- Sartorio A, Lafortuna C, Capodaglio P, Vangeli V, Narici MV, Faglia G. Effects of a 16-week progressive high-intensity strength training (HIST) on indexes of bone turnover in men over 65 years: A randomized controlled study. Journal of Endocrinological Investigation. 2001;24(11):882–6. doi: 10.1007/BF03343946. [DOI] [PubMed] [Google Scholar]
- Sauvage LJ, Myklebust B, Crow-Pan J, Novak S, Millington P, Hoffman MD, et al. A clinical trial of strengthening and aerobic exercise to improve gait and balance in elderly male nursing home residents. American Journal of Physical Medicine and Rehabilitation. 1992;71:333–42. doi: 10.1097/00002060-199212000-00005. [DOI] [PubMed] [Google Scholar]
- Sayers SP, Bean J, Cuoco A, LeBrasseur NK, Jette A, Fielding RA. Changes in function and disability after resistance training: does velocity matter? A pilot study. American Journal of Physical Medicine & Rehabilitation. 2003;82(8):605–13. doi: 10.1097/01.PHM.0000078225.71442.B6. [DOI] [PubMed] [Google Scholar]
- Schott N, Konietzny S, Raschka C. Red ginseng enhances the effectiveness of strength training in elderly: A randomized placebo-controlled double-blind trial. Schweizerische Zeitschrift fur Ganzheitsmedizin. 2006;18(7-8):376–83. Einfluss von Rotem Ginseng auf ein Krafttraining bei alteren Erwachsenen: Eine randomisierte placebokontrollierte Doppelblindstudie. [Google Scholar]
- Sharp S, Brouwer B. Isokinetic strength training of the hemiparetic knee: effects on function and spasticity. Archives of Physical Medicine and Rehabilitation. 1997;78:1231–6. doi: 10.1016/s0003-9993(97)90337-3. [DOI] [PubMed] [Google Scholar]
- Shaw JM, Snow CM. Weighted vest exercise improves indices of fall risk in older women. Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 1998;53(1):M53–8. doi: 10.1093/gerona/53a.1.m53. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Lord SR. Home exercise to improve strength and walking velocity after hip fracture: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 1997;78:208–12. doi: 10.1016/s0003-9993(97)90265-3. [DOI] [PubMed] [Google Scholar]
- Signorile JF, Carmel MP, Lai S, Roos BA. Early plateaus of power and torque gains during high- and low-speed resistance training of older women. Journal of Applied Physiology. 2005;98(4):1213–20. doi: 10.1152/japplphysiol.00742.2004. [DOI] [PubMed] [Google Scholar]
- Sinaki M, Wahner H, Bergstralh E, Hodgson SF, Offord KP, Squires RW, et al. Three-year controlled, randomized trial of the effect of dose-specified loading and strengthening exercises on bone mineral density of spine and femur in nonalthletic, physically active women. Bone. 1996;19(3):233–44. doi: 10.1016/8756-3282(96)00174-3. [DOI] [PubMed] [Google Scholar]
- Sipila S, Suominen H. Knee extension strength and walking speed in relation to quadriceps muscle composition and training in elderly women. Clinical Physiology. 1994;14(4):433–42. doi: 10.1111/j.1475-097x.1994.tb00402.x. [DOI] [PubMed] [Google Scholar]
- Spruit MA, Gosselink R, Troosters T, De Paepe K, Decramer M. Resistance versus endurance training in patients with COPD and peripheral muscle weakness. European Respiratory Journal. 2002;19(6):1072–8. doi: 10.1183/09031936.02.00287102. [DOI] [PubMed] [Google Scholar]
- Sullivan DH, Wall PT, Bariola JR, Bopp MM, Frost YM. Progressive resistance muscle strength training of hospitalized frail elderly. American Journal of Physical Medicine & Rehabilitation. 2001;80:503–9. doi: 10.1097/00002060-200107000-00007. [DOI] [PubMed] [Google Scholar]
- Taaffe DR, Marcus R. Dynamic muscle strength alterations to detraining and retraining in elderly men. Clinical Physiology. 1997;17(3):311–24. doi: 10.1111/j.1365-2281.1997.tb00010.x. [DOI] [PubMed] [Google Scholar]
- Teixeira R, Guerra S, Esculcas C, Ribeiro JC, Carvalho J, Mota J. Influence of age on physical fitness improvements after training on elderly women. Koskolou. 2002;514 Abstract. [Google Scholar]
- Teixeira PJ, Going SB, Houtkooper LB, Metcalfe LL, Blew RM, Flint-Wagner HG, et al. Resistance training in postmenopausal women with and without hormone therapy. Medicine and Science in Sports and Exercise. 2003;35(4):555–62. doi: 10.1249/01.MSS.0000058437.17262.11. [DOI] [PubMed] [Google Scholar]
- Teixeira-Salmela LF, Santiago L, Lima RC, Lana DM, Camargos FF, Cassiano JG. Functional performance and quality of life related to training and detraining of community-dwelling elderly. Disability & Rehabilitation. 2005;27(17):1007–12. doi: 10.1080/09638280500030688. [DOI] [PubMed] [Google Scholar]
- Thielman GT, Dean CM, Gentile AM. Rehabilitation of reaching after stroke: Task-related training versus progressive resistive exercise. Archives of Physical Medicine & Rehabilitation. 2004;85(10):1613–8. doi: 10.1016/j.apmr.2004.01.028. [DOI] [PubMed] [Google Scholar]
- Thomas KJ, Tomsic JB, Martin MS. Does participation in light to moderate strength and endurance exercise result in measurable physical benefits for older adults? Journal of Geriatric Physical Therapy. 2004;27(2):53–8. [Google Scholar]
- Thomas GN, Hong AW, Tomlinson B, Lau E, Lam CW, Sanderson JE, et al. Effects of Tai Chi and resistance training on cardiovascular risk factors in elderly Chinese subjects: a 12-month longitudinal, randomized, controlled intervention study. Clinical Endocrinology. 2005;63(6):663–9. doi: 10.1111/j.1365-2265.2005.02398.x. [DOI] [PubMed] [Google Scholar]
- Thompson RF, Crist DM, Marsh M, Rosenthal M. Effects of physical exercise for elderly patients with physical impairments. Journal of the American Geriatrics Society. 1988;36(2):130–5. doi: 10.1111/j.1532-5415.1988.tb01782.x. [DOI] [PubMed] [Google Scholar]
- Timonen L, Rantanen T, Ryynanen OP, Taimela S, Timonen TE, Sulkava R. A randomized controlled trial of rehabilitation after hospitalization in frail older women: effects on strength, balance and mobility. Scandinavian Journal of Medicine & Science in Sports. 2002;12(3):186–92. doi: 10.1034/j.1600-0838.2002.120310.x. [DOI] [PubMed] [Google Scholar]
- Timonen L, Rantanen T, Makinen E, Timonen TE, Tormakangas T, Sulkava R. Effects of group-based exercise program on functional abilities in frail older women after hospital discharge. Aging-Clinical & Experimental Research. 2006;18(1):50–6. doi: 10.1007/BF03324640. [DOI] [PubMed] [Google Scholar]
- Timonen L, Rantanen T, Timonen TE, Sulkava R. Effects of a group-based exercise program on the mood state of frail older women after discharge from hospital. International Journal of Geriatric Psychiatry. 2006;17(12):1106–11. doi: 10.1002/gps.757. [DOI] [PubMed] [Google Scholar]
- Treuth MS, Ryan AS, Pratley RE, Rubin MA, Miller JP, Nicklas BJ, et al. Effects of strength training on total and regional body composition in older men. Journal of Applied Physiology. 1994;77(2):614–20. doi: 10.1152/jappl.1994.77.2.614. [DOI] [PubMed] [Google Scholar]
- Trudelle-Jackson E, Smith SS. Effects of a late-phase exercise program after total hip arthroplasty: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2004;85(7):1056–62. doi: 10.1016/j.apmr.2003.11.022. [DOI] [PubMed] [Google Scholar]
- Tsuji I, Tamagawa A, Nagatomi R, Irie N, Ohkubo T, Saito M, et al. Randomised controlled trial of exercise training for older people: study design and primary outcome. Journal of Epidemiology. 2000;10(1):55–64. doi: 10.2188/jea.10.55. [DOI] [PubMed] [Google Scholar]
- Vad E, Worm C, Lauritsen JM, Poulsen PB, Puggaard L, Stovring H, et al. Physical training as treatment of reduced functional ability in frail 75+ year-olds living at home. A randomized intervention study in general practice with technological assessment elements. Ugeskrift for Laeger. 2002;164(44):5140–4. Fysisk traening som behandling af nedsat funktionsevne hos svage, hjemmeboende 75+ –arige. Et randomiseret interventionsstudie i almen praksis omfattende elementer til en teknologivurdering. [PubMed] [Google Scholar]
- Vale RGS, Damasceno V, Cordeiro LS, Baptista MR, Pernambuco CS, Motta T, et al. Effects of supine resistance strength training in independent elderly women. Fitness & Performance Journal. 2003;2(4):255. Efeitos de um treinamento resistido de forca no supino reto em idosas independentes [Abstract] 1519–9088. [Google Scholar]
- Valkeinen H, Hakkinen K, Pakarinen A, Hannonen P, Hakkinen A, Airaksinen O, et al. Muscle hypertrophy, strength development, and serum hormones during strength training in elderly women with fibromyalgia. Scandinavian Journal of Rheumatology. 2005;34(4):309–14. doi: 10.1080/03009740510018697. [DOI] [PubMed] [Google Scholar]
- Van den Ende CH, Breedveld FC, le Cessie S, Dijkmans BA, de Mug AW, Hazes JM. Effect of intensive exercise on patients with active rheumatoid arthritis: a randomised clinical trial. Annals of the Rheumatic Diseases. 2000;59(8):615–21. doi: 10.1136/ard.59.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanbiervliet W, Pelissier J, Ledermann B, Kotzki N, Benaim C, Herisson C, et al. Strength training with elastic bands: measure of its effects in cardiac rehabilitation after coronary diseases. Annales de Readaptation et de Medecine Physique. 2003;46(8):545–52. doi: 10.1016/j.annrmp.2003.03.001. Le renforcement musculaire par bandes elastiques: evaluation de ses effets dans le reentrainement a l'effort du coronarien. [DOI] [PubMed] [Google Scholar]
- Veloso U, Monteiro W, Farinatti P. Do continuous and intermittent exercises sets induce similar cardiovascular responses in the elderly women? Revista Brasileira de Medicina do Esporte. 2003;9(2):85–90. 1517–8692. [Google Scholar]
- Verfaillie D, Nichols J, Turkel E, Hovell M. Effects of resistance, balance and gait training on reduction of risk factors leading to falls in elders. Journal of Aging and Physical Activity. 1997;5:213–28. [Google Scholar]
- Villareal DT, Binder EF, Yarasheski KE, Williams DB, Brown M, Sinacore DR, et al. Effects of exercise training added to ongoing hormone replacement therapy on bone mineral density in frail elderly women. Journal of the American Geriatrics Society. 2003;51(7):985–90. doi: 10.1046/j.1365-2389.2003.51312.x. [DOI] [PubMed] [Google Scholar]
- Villareal DT, Holloszy JO. DHEA enhances effects of weight training on muscle mass and strength in elderly women and men. American Journal of Physiology -Endocrinology & Metabolism. 2006;291(5):E1003–8. doi: 10.1152/ajpendo.00100.2006. [DOI] [PubMed] [Google Scholar]
- Vincent KR, Vincent HK, Braith RW, Lennon SL, Lowenthal DT. Resistance exercise training attenuates exercise-induced lipid peroxidation in the elderly. European Journal of Applied Physiology. 2002;87(4/5):416–23. doi: 10.1007/s00421-002-0640-2. 1439–6327. [DOI] [PubMed] [Google Scholar]
- Vincent KR, Vincent HK, Braith RW, Bhatnagar V, Lowenthal DT. Strength training and hemodynamic responses to exercise. American Journal of Geriatric Cardiology. 2003;12(2):97–106. doi: 10.1111/j.1076-7460.2003.01588.x. [DOI] [PubMed] [Google Scholar]
- Vincent KR, Braith RW, Vincent HK. Influence of resistance exercise on lumbar strength in older, overweight adults. Archives of Physical Medicine and Rehabilitation. 2006;87(3):383–9. doi: 10.1016/j.apmr.2005.11.030. 0003–9993. [DOI] [PubMed] [Google Scholar]
- Woo J, Hong A, Lau E, Lynn H. A randomised controlled trials of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age and Ageing. 2007;36:262–8. doi: 10.1093/ageing/afm005. [DOI] [PubMed] [Google Scholar]
- Yang Y, Wang R, Lin K, Chu M, Chan R. Task-oriented progressive resistance strength training improves muscle strength and functional performance in individuals with stroke. Clinical Rehabilitation. 2006;20(10):860–70. doi: 10.1177/0269215506070701. [DOI] [PubMed] [Google Scholar]
- Zion AS, De Meersman R, Diamond BE, Bloomfield DM, Zion AS, De Meersman R, et al. A home-based resistance-training program using elastic bands for elderly patients with orthostatic hypotension. Clinical Autonomic Research. 2003;13(4):286–92. doi: 10.1007/s10286-003-0117-3. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
- Bennell KL, Hunt MA, Wrigley TV, Hunter DJ. The effects of hip muscle strengthening on knee load, pain, and function in people with knee osteoarthritis: a protocol for a randomised, single-blind controlled trial. BMC Musculoskeletal Disorders. 2007;8:121. doi: 10.1186/1471-2474-8-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheema B, Abas H, Smith B, O'Sullivan A, Chan M, Patwardhan A, et al. Progressive exercise for anabolism in kidney disease (PEAK): a randomized, controlled trial of resistance training during hemodialysis. Journal of the American Society of Nephrology. 2007;18(5):1594–601. doi: 10.1681/ASN.2006121329. [DOI] [PubMed] [Google Scholar]
- Fahlman M, Morgan A, McNevin N, Topp R, Boardley D. Combination training and resistance training as effective interventions to improve functioning in elders. Journal of Aging & Physical Activity. 2007;15(2):195–205. doi: 10.1123/japa.15.2.195. [DOI] [PubMed] [Google Scholar]
- *.Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2008;63(1):83–91. doi: 10.1093/gerona/63.1.83. [DOI] [PubMed] [Google Scholar]
- Karinkanta S, Heinonen A, Sievanen H, Uusi-Rasi K, Pasanen M, Ojala K, et al. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: randomized, controlled trial. Osteoporosis International. 2007;18(4):453–62. doi: 10.1007/s00198-006-0256-1. MEDLINE: Yes. [DOI] [PubMed] [Google Scholar]
- Lin DH, Lin YF, Chai HM, Han YC, Jan MH. Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clinical Rheumatology. 2007;26(4):520–8. doi: 10.1007/s10067-006-0324-0. erratum appears in Clin Rheumatol. 2007 Apr;26(4):617 Note: Chai, Hei-Min [corrected to Chai, Huei-Ming] MEDLINE: yes. [DOI] [PubMed] [Google Scholar]
- Mitchell SL, Stott DJ, Martin BJ, Grant SJ. Randomized controlled trial of quadriceps training after proximal femoral fracture. Clinical Rehabilitation. 2001;15(3):282–290. doi: 10.1191/026921501676849095. [DOI] [PubMed] [Google Scholar]
- O'Shea SD, Taylor NF, Paratz JD. A predominantly home-based progressive resistance exercise program increases knee extensor strength in the short-term in people with chronic obstructive pulmonary disease: a randomised controlled trial. Australian Journal of Physiotherapy. 2007;53(4):229–37. doi: 10.1016/s0004-9514(07)70003-x. [DOI] [PubMed] [Google Scholar]
- Raso V, Benard G, Da Silva Duarte AJ, Natale VM. Effect of resistance training on immunological parameters of healthy elderly women. Medicine & Science in Sports & Exercise. 2007;39(12):2152–9. doi: 10.1249/mss.0b013e318156e9fa. [DOI] [PubMed] [Google Scholar]
- Williams AD, Carey MF, Selig S, Hayes A, Krum H, Patterson J, et al. Circuit resistance training in chronic heart failure improves skeletal muscle mitochondrial ATP production rate - a randomized controlled trial. Journal of Cardiac Failure. 2007;13(2):79–85. doi: 10.1016/j.cardfail.2006.10.017. [DOI] [PubMed] [Google Scholar]
Additional references
- Anonymous. Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Journal of the American Geriatrics Society. 2001;49(5):664–72. [PubMed] [Google Scholar]
- Brosseau L, MacLeay L, Welch V, Tugwell P, Wells G. Intensity of exercise for the treatment of osteoarthritis. Cochrane Database of Systematic Reviews. 2003;(2) doi: 10.1002/14651858CD004259. [DOI] [PubMed] [Google Scholar]
- Buchner DM. Understanding variability in studies of strength training in older adults: a meta-analytic perspective. Topics in Geriatric Rehabilitation. 1993;8(3):1–21. [Google Scholar]
- Buchner D, Larson E, Wagner E, Koepsell T, De Lateur B. Evidence for a non-linear relationship between leg strength and gait speed. Age and Ageing. 1996;25:386–91. doi: 10.1093/ageing/25.5.386. [DOI] [PubMed] [Google Scholar]
- Chandler JM, Hadley EC. Exercise to improve physiologic and functional performance in old age. Clinics in Geriatric Medicine. 1996;12(4):761–84. [PubMed] [Google Scholar]
- Doherty TJ, Vandervoort AA, Brown WF. Effects of ageing on the motor unit: A brief review. Canadian Journal of Applied Physiology. 1993;18(4):331–58. doi: 10.1139/h93-029. [DOI] [PubMed] [Google Scholar]
- Fiatarone M, Evans W. The etiology and reversibility of muscle dysfunction in the aged. Journals of Gerontology. 1993;48(special):77–83. doi: 10.1093/geronj/48.special_issue.77. [DOI] [PubMed] [Google Scholar]
- Frontera W, Meredith CN, O'Reilly K, Knuttgen H, Evans W. Strength conditioning in older men: skeletal muscle hypertrophy and improved function. Journal of Applied Physiology. 1988;64(3):1038–44. doi: 10.1152/jappl.1988.64.3.1038. [DOI] [PubMed] [Google Scholar]
- Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858CD000340.pub2. [DOI] [Google Scholar]
- Guralnik J, Ferrucci L, Simonsick E, Salive M, Wallace R. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. The New England Journal of Medicine. 1995;332:556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S. Highly sensitive search strategies for identifying reports of randomized controlled trials in MEDLINE. [accessed 01 May 2007];Cochrane Handbook for Systematic Reviews of Interventions 4 2 6. updated September 2006; Appendix 5b. www.cochrane.org/resources/handbook/hbook.htm.
- Howe TE, Rochester L, Jackson A, Banks PMH, Blair VA. Exercise for improving balance in older people. Cochrane Database of Systematic Reviews. 2007;(4) doi: 10.1002/14651858.CD004963.pub2. [DOI] [PubMed] [Google Scholar]
- Keysor JJ, Jette AM. Have we oversold the benefit of late-life exercise? Journals of Gerontology: Medical Sciences. 2001;56A(7):M412–M23. doi: 10.1093/gerona/56.7.m412. [DOI] [PubMed] [Google Scholar]
- King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults: a critical review and recommendations. American Journal of Preventative Medicine. 1998;15(4):316–33. doi: 10.1016/s0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- King AC. Interventions to promote physical activity by older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2001;56(Spec No 2):36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- Mazzeo RS, Cavanagh P, Evans WJ, Fiatarone M, Hagberg J, McAuley E, et al. American College of Sports Medicine position stand: exercise and physical activity for older adults. Medicine and Science in Sports and Exercise. 1998;30(6):992–1008. [PubMed] [Google Scholar]
- Nagi SZ. Disability concepts revisited: Implications for prevention. In: Pope AM, Tarlov AR, editors. Disability in America: Toward a national agenda for prevention. Washington, D.C: National Academy Press; 1991. pp. 309–327. [Google Scholar]
- Province MA, Hadley EC, Hornbrook MC, Lipsitz LA, Philip-Miller J, Mulrow CD, et al. The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT trials. Journal of the American Geriatrics Society. 1995;273(17):1341–7. [PubMed] [Google Scholar]
- Singh MA. Exercise comes of age: rationale and recommendations for a geriatric exercise prescription. Journals of Gerontology: Medical Sciences. 2002;57(5):M262–82. doi: 10.1093/gerona/57.5.m262. [DOI] [PubMed] [Google Scholar]
- Tinetti M, Williams T, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. The American Journal of Medicine. 1986;80:429–34. doi: 10.1016/0002-9343(86)90717-5. [DOI] [PubMed] [Google Scholar]
- World Health Organization. ICIDH-2: International classification of functioning, disability and health (final draft) Geneva: World Health Organization; 2001. [Google Scholar]
References to other published versions of this review
- Latham NK, Anderson CS, Bennett DA, Stretton C. Progressive resistance strength training for physical disability in older people. Cochrane Database of Systematic Reviews. 2003a;(2) doi: 10.1002/1465.1858.CD002759. [DOI] [PubMed] [Google Scholar]
- Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2004;59(1):48–61. doi: 10.1093/gerona/59.1.m48. [DOI] [PubMed] [Google Scholar]


