Abstract
The dominant paradigm of changing multiple health behaviors (MHBs) is based on treating, assessing, and studying each behavior separately. This study focused on individuals with co-occurring baseline health-risk behavior pairs and described whether they changed over time on both or only one of the behaviors within each pair. Data from five randomized trials of computer-tailored interventions (CTIs) that simultaneously treated MHBs were analyzed. The differences between treatment and control proportions that achieved paired action and singular action at 24 months follow-up, and the proportional contribution of paired action to overall change on each behavior, were assessed across 12 behavior pairs (including energy balance, addictive, and appearance-related behaviors). CTIs consistently produced more paired action across behavior pairs. Paired action contributed substantially more to the treatment-related outcomes than singular action. Studying concurrent changes on MHBs as demonstrated allows the effect of simultaneously treating MHBs to be assessed.
Keywords: Multiple behavior change, Multiple behavior interventions, Paired action, Singular action, Behavior pairs, Stages of change, TTM-tailored CTIs
INTRODUCTION
One of the greatest challenges facing the field of health behavior change is how to most effectively treat multiple health behavioral risks in order to prevent chronic diseases. Most of the US population has been reported to have co-occurring multiple behavioral risks [1, 2] resulting in disproportionately higher rates of morbidity, disability, and premature mortality [3–6]. The presence of multiple risk behaviors has been shown to have a negative synergistic influence on health. For example, physical inactivity combined with a poor diet greatly increases the likelihood of cardiovascular disease, type 2 diabetes, and cancer [7, 8]. The risk of head and neck cancers is multiplied with tobacco and alcohol use, to an extent that is greater than the sum of the two risks individually [9, 10].
Beyond the health repercussions, excess behavioral risks also have serious cost implications. Modifiable health risks, such as tobacco use, stress, and overweight status, are associated with both short-term increases in the likelihood of incurring health expenditures and the magnitude of those expenditures [11]. For example, in large worksite samples, employees’ excess risk factors have predicted incremental increases in pharmaceutical, disability, and overall medical costs [11–15]. Longitudinal data have also shown that effectively treating two behaviors in an individual reduces medical costs by approximately $2,000 per year [14]. Consequently, targeting change in multiple health-risk behaviors offers the potential for greater health benefits, enhanced disease prevention, and reduced health care costs. Of particular significance is that multiple health-risk behaviors are initiated and established during adolescence, including declines in physical activity and healthy diet practices and increases in stress, smoking, and alcohol use [16, 17].
There is growing programmatic research demonstrating that multiple health-risk behaviors can be changed simultaneously within high-risk populations. A previous attempt to review multiple health behavior change (MHBC) interventions in primary care found that there was insufficient literature available to review and large gaps in the field’s knowledge base [18]. In response to such knowledge gaps, the recent National Institutes of Health (NIH) science of behavior change meeting summary report identified simultaneously changing multiple behaviors as a top NIH priority [19]. There has been an increase in recent years in MHBC research as a result of the funding initiatives of NIH and several of its institutes [20]. For example, research applying computer-tailored interventions (CTIs) based on the transtheoretical model (TTM) simultaneously treated multiple health-risk behaviors and demonstrated significant impacts on multiple health behaviors with adults and adolescents [21–25]. Empirically based tailoring is especially relevant in population-based interventions when not everyone is prepared to change their risk behavior(s). Fully TTM-tailored CTIs assess each TTM construct (stage of change, pros, self-efficacy, and processes of change) and provide feedback based on an individual’s scores on each construct. Moderate tailoring only includes assessments and feedback on stage, decisional balance, and efficacy, while minimal tailoring may only include feedback based on stage of change [23, 24, 26, 27].
There are increasing efforts in the field to simultaneously treat a set of multiple behavioral risks. In most of these projects, however, each behavior in the set is still treated separately, analyzed separately, and studied separately [28]. In previous research, for example, we treated each behavior with a separate module, analyzed changes in each behavior separately, and reported significant effects on each separate behavior [21–23, 29]. An earlier attempt to examine behavior change in the context of co-occurring risks analyzed data from some of these same studies but assessed whether a single behavior outcome (smoking cessation) was consistent across smokers who were simultaneously treated for either zero, one, or two identified co-occurring risks [30]. More recently, when we studied the predictors of successful changes in a set of multiple health-risk behaviors, we analyzed the consistency of four effects (i.e., treatment, stage, severity, and effort) on each behavior separately rather than on any combination of behaviors [31]. The science and practice of behavior change are still fundamentally based on a separate behavior paradigm rather than a multiple behavior paradigm.
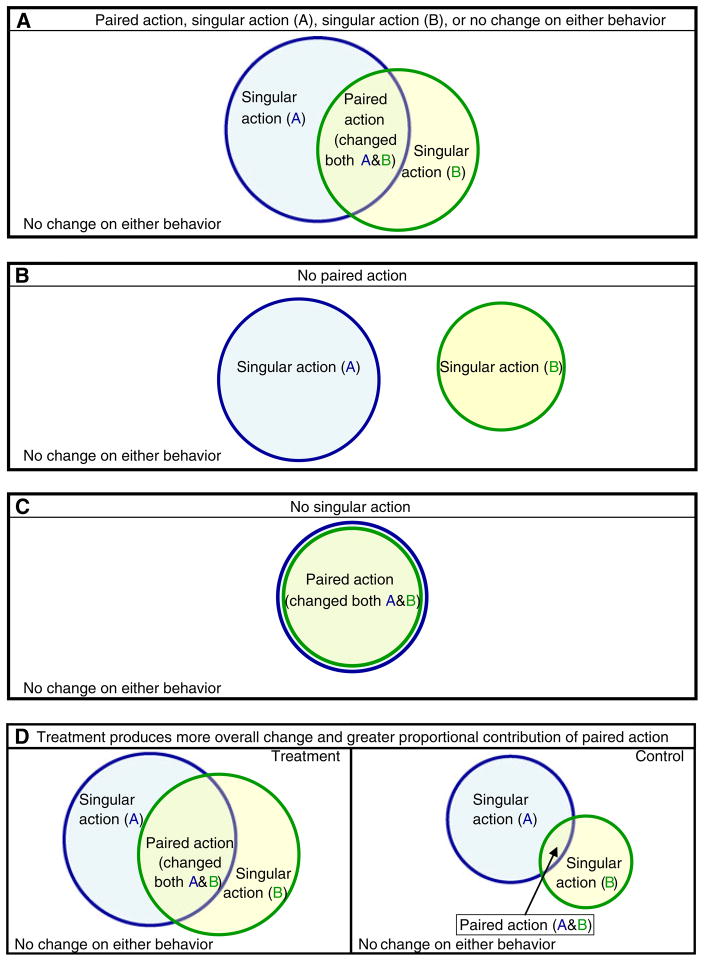
One way to start conceptualizing multiple behavior changes is by studying individuals with co-occurring behavioral risks and whether they change one or more of those behaviors over time. To help the field begin the shift toward a multiple behavior paradigm, this study focuses on those individuals with pairs of co-occurring health-risk behaviors at baseline and will describe the longitudinal behavior changes observed within each assessed behavior pair. Figure 1 provides a representation of the four possible outcome patterns, given co-occurrence of a pair of baseline behavioral risks: paired action (the outcome when individuals change both behaviors during the same time period), singular action (i.e., the outcome when individuals change on only one behavior in the pair, either behavior A or B), and no change in either behavior. In this illustration, the size of the individual circles shows the total amount of change for each behavior. The degree of overlap of the two circles indicates the amount of paired action (Fig. 1a) and could, in principle, range from no overlap (i.e., individuals change only one behavior; Fig. 1b) to complete overlap (all individuals who change do so only on both behaviors; Fig. 1c). This study assessed and compared the consistency and magnitude of the differences between treatment and control groups on both paired and singular action rates for a number of health behavior pairs. This study also explored the differential contribution of paired action to the total amount of change on each behavior in treatment versus control groups for the same health behavior pairs.
Fig 1.
Visual representation of possible outcomes given a pair of behavioral risks at baseline
The current study builds on two earlier studies on coaction, defined as the extent to which change on one behavior (e.g., diet) was associated with increased odds of change on a second behavior (e.g., physical activity) at the same follow-up time point [32]. The first study examined coaction in adults with pairs of co-occurring baseline health risks, including an addictive behavior (smoking), energy balance behavior (diet), and sun protection behavior that is often appearance related. Despite the differences among these behaviors, significant coaction was revealed in the treatment group, whereas there was minimal or no coaction in the control group. The combined 24-month coaction odds ratios (ORs) were 1.77 (95 % confidence interval 1.39, 2.25) for the treatment group and 1.09 (0.81, 1.46) for the control group [32]. The second study assessed coaction in energy balance behaviors in three separate samples: high school students, middle school students, and adults. Again, most of the coaction ORs for the control groups were around 1.0, indicating minimal or no coaction. In contrast, the ORs for the treatment groups were in the 2.5 range, indicating substantial coaction (S. S. J., unpublished data, 2012).
Although coaction is a promising phenomenon that also requires co-occurrence of at least two baseline risks, its focus is on the extent to which change on one behavior is associated with change on a second behavior at the same follow-up time point. Coaction ORs do not show the actual proportions of participants who changed both behaviors or only one of their co-occurring baseline risk behaviors, nor do they allow direct comparisons of specific behavior change rates to be made between groups. Working with primary data from the same set of studies, this study assessed paired and singular action rates for treatment and control groups across 12 pairs of health behaviors and described the magnitude of the difference between treatment and control groups on paired action and singular action. First, it compared the proportions within treatment and control groups who changed both behaviors in a pair for which they were at risk at baseline (e.g., physical activity and diet). Next, this study compared the proportions that changed just one of the pair of behaviors but not both (i.e., singular action), separately in treatment and control groups. The two previous studies on coaction compared the associations (ORs) between change on one behavior and taking action on a second behavior for treatment versus control groups. The present study on paired action and singular action provides an alternative and, perhaps, more intuitive way of describing the phenomena of multiple behavior change in the same sample of individuals with co-occurring baseline risk pairs. This study also presents effect sizes for the magnitude of the differences between treatment and control groups on the rates of paired and singular action. Finally, this study examined the differences between treatment and control groups on the contribution to overall change on each behavior in a pair from individuals who achieved paired action.
Given that the five randomized trials analyzed in this study differed on important variables such as treatment intensity (e.g., full, moderate, and minimal tailoring), populations (adults and adolescents), and behaviors (e.g., energy balance and addictive), we will explore possible relationships between some of these types of variables to paired and singular action. Previous meta-analyses support the effectiveness of tailoring in health interventions based on several different models of behavior change [33, 34]. In terms of population characteristics, neither age nor gender has been found to be significant moderators for single behavior outcomes [33, 34]. Of the three factors mentioned, types of behaviors have made the biggest differences in single behavior outcomes ranging from about 25 % for smoking [35] to about 45 % for energy balance behaviors [23] to 65 % for affective behaviors [29, 36]. Extrapolating from these single behavior results, we would expect to see greater differences in paired and singular action rates depending on the types of behaviors included in the pairs, rather than across population types.
Based on previous research on coaction and the overall outcomes of these multiple health behavior studies, we predicted that intervention would produce consistently higher rates of paired action on an absolute basis when comparing treatment to control groups and that these effects would be statistically significant. Based on the overall outcomes of these interventions, we expected that the treatment groups would also show consistently more singular action than the control groups, with significant intervention effects. We had no empirical basis to predict whether the treatment effect sizes would be greater for paired action (i.e., simultaneous changes on two behaviors) or for singular action taken on only one of the behaviors in a pair. By extension, we expected that the effect of simultaneously treating pairs of health-risk behaviors would be reflected by greater proportional contributions from paired action to the overall amount of change on each treated behavior when comparing treatment to controls.
METHODS
Participants and procedure
Data from five randomized trials were available for analysis. Study 1 included 4,158 students from 20 middle schools in a northeastern state [mean age= 11.40 years (SD=0.69); 47.8 % female, 65.0 % White, 3.8 % Black, 15.6 % Hispanic, and 25.9 % other]. A computerized, TTM-tailored multiple energy balance behavior intervention program was offered to a randomized comparison group of students in ten schools participating in a larger study [25, 37]. Details of the intervention have been reported previously [24]. The targeted behaviors were physical activity (PA; 60 min daily), fruit and vegetable (FV) consumption (five servings daily), and reducing TV time to less than 2 h per day (TV). Students in the treatment arm received a combination of fully TTM-tailored interventions for physical activity and alternating moderately tailored and stage-matched interventions for fruit and vegetable intake and TV time [24]. This study did not have a true control group. Students in the ten comparison group schools received the same number of TTM CTI sessions for substance use prevention instead of energy balance behaviors. Students completed annual health risk assessments, including stage of change for each behavior, and participated in one intervention session during year 1, three sessions during year 2, and one session in year 3. There were 2,416 students at baseline who were at risk for two or more targeted behaviors (PA, FV, and TV). Analyses reported here include complete case data from the first 2 years of the study.
In study 2, a national sample of 1,277 overweight and moderately obese adults (mean age=45.37; mean BMI=30.75; 47.6 % female, 79.1 % White, 6.5 % Black, 7.0 % Hispanic, and 7.2 % other) was randomized to receive either usual care or fully tailored TTM feedback reports for up to three risk behaviors based on the national guidelines at the time: healthy eating (reducing caloric intake by 500 calories per day and total fat intake to less than 30 % of calories), regular exercise (30 min of moderate exercise on at least five days a week), and managing emotions without eating. Intervention group participants received four fully tailored reports that provided feedback on stage of change, decisional balance, self-efficacy, and up to six stage-matched processes, and a stage-matched manual addressing energy balance behaviors and fruit and vegetable consumption. Participants did not receive tailored feedback on FV. Additional details about the participants, intervention, and design have been reported elsewhere [23]. Control participants completed assessments at baseline and 6 months. Follow-up assessments were conducted with all participants at 12 and 24 months. A total of 1,200 participants were at risk for two or more of the behaviors (exercise, healthy eating, emotional eating, and FV) at baseline.
Sample 3 pooled treatment and control participants from three separate randomized controlled trials in our National Cancer Institute Center grant which used common interventions, procedures, measures, and assessment schedules, in trials that recruited parents, primary care patients, and employees who were at risk for at least one targeted behavior (smoking, diet, and sun protection) [21, 22, 38, 39]. The demographics and stage distributions for the combined treatment and control groups (N= 9,461) were comparable [32], so it was reasonable to pool the data from all three trials. The majority were married, non-Hispanic Caucasian females with a mean age of 44 years. The total group of participants was least prepared to change smoking (21.8 % in preparation), then diet (33.0 % in preparation), and most prepared to change sun protection (43.9 % in preparation). Assessments were conducted at baseline, 12 and 24 months. Participants randomized to the intervention group received fully tailored TTM CTIs mailed to their homes for all targeted behaviors that they were at risk for (e.g., only smokers got feedback on smoking) at baseline, 6 and 12 months. In addition to the CTIs, participants in the treatment group also received a stage-matched multiple behavior change manual at baseline that presented principles for progressing from one stage to the next and how to apply these change principles across multiple behaviors. A total of 5,517 participants at baseline had at least two of the three risk behaviors (smoking, diet, and sun protection). All primary studies were approved by the Institutional Review Boards at the University of Rhode Island (studies 1 and 3) and Pro-Change Behavior Systems, Inc. (study 2), respectively.
Measures
The main measure for behavior change was the percentage in each group who progressed from pre-action (i.e., precontemplation, contemplation, or preparation) stages at baseline to action or maintenance stages at follow-up. This approach provides a common metric for progressing from not being at public health criteria for the behavioral risk (e.g., smoking at baseline) to being at criteria at follow-up [e.g., point prevalence (action) or prolonged abstinence (maintenance) at follow-up].
Analysis
Paired action and singular action for each of the two behaviors were assessed at 24 months follow-up on complete cases who were at risk at baseline for each pair of behaviors being assessed. Twelve behavior dyads were assessed at 24 months, resulting in 12 comparisons for paired action and 24 comparisons for singular action. The contribution of paired action to change on each of the two behaviors was assessed at 24 months for the same behavior dyads, resulting in 24 comparisons.
Paired action proportions were compared between treatment and control groups for each behavior dyad. Singular action proportions were also compared between treatment and control groups for each behavior dyad. For each behavior in a pair, the proportional contribution from paired action to overall change on each behavior was determined and compared between treatment and control groups for each behavior dyad.
Effect sizes (ESs) for the difference in magnitude between treatment and control group proportions were computed separately for paired action, singular action, and contribution of paired action to overall change on each behavior, for each behavior dyad assessed (Cohen’s h for proportions, comparable to Cohen’s d for interpretation [40–42]). Individual ESs (h) for behavior pairs were combined using standard meta-analytic techniques [43, 44] to obtain aggregate ESs for the differences between treatment and control groups on paired action, singular action, and proportional contribution from paired action to overall change on each behavior at 24 months.
The 24-month completion rates among participants with two or more baseline risks were 65.9 % (N=1,591) for study 1, 50.7 % (N=608) for study 2, and 65.5 % (N=3,611) for study 3, respectively. The baseline characteristics of dropouts and completers were similar, confirming assumptions of the missing at random model. Sensitivity analyses were performed in which individual ESs for each behavior pair were computed for all participants who were at risk at baseline for two or more behaviors, based on imputing the last observation carried forward (i.e., 12 months when available or baseline), then compared to the ESs found in complete case analyses.
RESULTS
Table 1 shows that across all 12 behavior dyads at 24 months, the treatment groups produced more paired action than the control or comparison groups, with significant differences for 9 of the 12 comparisons (75 %). Using meta-analytic procedures, the ESs (h) comparing treatment to control/comparison group outcomes for paired action at 24 months were combined across all 12 behavior pairs. The combined ES was significant for paired action at 24 months, h̄ = 0.28(95% CI 0.24, 0.32).
Table 1.
Behavior dyads–paired action proportions within treatment and control groups at 24 months
| Treatment
|
Control
|
|||||
|---|---|---|---|---|---|---|
| Proportion | 95% CI | Proportion | 95% CI | |||
| Study 1: adolescents | ||||||
|
| ||||||
| Exercise and TV time | n=377 | n=329 | ||||
|
| ||||||
| Proportion that changed on both exercise and TV time | 0.236* | 0.193, 0.279 | 0.073* | 0.045, 0.101 | ||
|
| ||||||
| Exercise and fruit and vegetable consumption | n=506 | n=453 | ||||
|
| ||||||
| Proportion that changed on both exercise and FV | 0.146* | 0.115, 0.177 | 0.044* | 0.025, 0.063 | ||
|
| ||||||
| TV time and FV | n=526 | n=464 | ||||
|
| ||||||
| Proportion that changed on both TV time and FV | 0.120* | 0.092, 0.148 | 0.026* | 0.011, 0.040 | ||
|
| ||||||
| Study 2: adults | ||||||
|
| ||||||
| Exercise and healthy eating | n=167 | n=190 | ||||
|
| ||||||
| Proportion that changed on both exercise and healthy eating | 0.305* | 0.236, 0.375 | 0.142* | 0.092, 0.192 | ||
|
| ||||||
| Exercise and emotional eating | n=57 | n=76 | ||||
|
| ||||||
| Proportion that changed on both exercise and emotional eating | 0.263* | 0.149, 0.377 | 0.105* | 0.036, 0.174 | ||
|
| ||||||
| Healthy eating and emotional eating | n=94 | n=106 | ||||
|
| ||||||
| Proportion that changed on both healthy eating and emotional eating | 0.330* | 0.235, 0.425 | 0.104* | 0.046, 0.162 | ||
|
| ||||||
| Exercise and FV | n=142 | n=155 | ||||
|
| ||||||
| Proportion that changed on both exercise and FV | 0.211 | 0.144, 0.278 | 0.148 | 0.092, 0.204 | ||
|
| ||||||
| Healthy eating and FV | n=205 | n=243 | ||||
|
| ||||||
| Proportion that changed on both healthy eating and FV | 0.229* | 0.172, 0.287 | 0.128* | 0.086, 0.170 | ||
|
| ||||||
| Emotional eating and FV | n=71 | n=71 | ||||
|
| ||||||
| Proportion that changed on both emotional eating and FV | 0.239 | 0.140, 0.339 | 0.127 | 0.049, 0.204 | ||
|
| ||||||
| Study 3: adults | ||||||
|
| ||||||
| Smoking and diet | n=360 | n=539 | ||||
|
| ||||||
| Proportion that changed on both smoking and diet | 0.047 | 0.025, 0.069 | 0.024 | 0.011, 0.037 | ||
|
| ||||||
| Smoking and sun protection | n=388 | n=520 | ||||
|
| ||||||
| Proportion that changed on both smoking and sun protection | 0.044* | 0.023, 0.064 | 0.017* | 0.006, 0.029 | ||
|
| ||||||
| Diet and sun protection | n=1,310 | n=1,764 | ||||
|
| ||||||
| Proportion that changed on both diet and sun protection | 0.073* | 0.059, 0.087 | 0.023* | 0.016, 0.030 | ||
FV fruit and vegetable consumption
p <0.05; treatment and control proportions were significantly different
Table 2 shows that the treatment groups also produced more singular action than the control groups. On an absolute basis, 16 of the 24 comparisons (66.7 %) favored treatment groups. Singular action proportions were significantly higher in the treatment group in 4 of the 24 comparisons (16.7 %). The ESs (h) comparing singular action proportions in treatment to control groups at 24 months were combined across all 12 behavior pairs. The combined ES for singular action at 24 months was also significant, h̄ = 0.08(0.05, 0.11), although much smaller compared to the paired action ES.
Table 2.
Behavior dyads–singular action proportions within treatment and control groups at 24 months
| Treatment
|
Control
|
|||||
|---|---|---|---|---|---|---|
| Proportion | 95% CI | Proportion | 95% CI | |||
| Study 1: adolescents | ||||||
|
| ||||||
| Exercise and TV time | n=377 | n=329 | ||||
|
| ||||||
| Proportion that changed on exercise only | 0.239 | 0.196, 0.282 | 0.277 | 0.229, 0.325 | ||
|
| ||||||
| Proportion that changed on TV time only | 0.186 | 0.147, 0.225 | 0.146 | 0.108, 0.184 | ||
|
| ||||||
| Exercise and fruit and vegetable consumption | n=506 | n=453 | ||||
|
| ||||||
| Proportion that changed on exercise only | 0.316 | 0.275, 0.357 | 0.318 | 0.275, 0.361 | ||
|
| ||||||
| Proportion that changed on FV only | 0.089* | 0.064, 0.114 | 0.051* | 0.031, 0.071 | ||
|
| ||||||
| TV time and FV | n=526 | n=464 | ||||
|
| ||||||
| Proportion that changed on TV time only | 0.344* | 0.303, 0.385 | 0.241* | 0.202, 0.280 | ||
|
| ||||||
| Proportion that changed on FV only | 0.133* | 0.104, 0.160 | 0.086* | 0.060, 0.112 | ||
|
| ||||||
| Study 2: adults | ||||||
|
| ||||||
| Exercise and healthy eating | n=167 | n=190 | ||||
|
| ||||||
| Proportion that changed on exercise only | 0.132 | 0.081, 0.183 | 0.184 | 0.129, 0.239 | ||
|
| ||||||
| Proportion that changed on healthy eating only | 0.210 | 0.148, 0.272 | 0.153 | 0.102, 0.204 | ||
|
| ||||||
| Exercise and emotional eating | n=57 | n=76 | ||||
|
| ||||||
| Proportion that changed on exercise only | 0.228 | 0.119, 0.337 | 0.197 | 0.108, 0.286 | ||
|
| ||||||
| Proportion that changed on emotional eating only | 0.158 | 0.063, 0.253 | 0.118 | 0.045, 0.191 | ||
|
| ||||||
| Healthy eating and emotional eating | n=94 | n=106 | ||||
|
| ||||||
| Proportion that changed on healthy eating only | 0.266 | 0.177, 0.355 | 0.255 | 0.172, 0.338 | ||
|
| ||||||
| Proportion that changed on emotional eating only | 0.117 | 0.052, 0.182 | 0.142 | 0.076, 0.208 | ||
|
| ||||||
| Exercise and FV | n=142 | n=155 | ||||
|
| ||||||
| Proportion that changed on exercise only | 0.190 | 0.125, 0.255 | 0.239 | 0.172, 0.306 | ||
|
| ||||||
| Proportion that changed on FV only | 0.176 | 0.113, 0.239 | 0.142 | 0.087, 0.197 | ||
|
| ||||||
| Healthy eating and FV | n=205 | n=243 | ||||
|
| ||||||
| Proportion that changed on healthy eating only | 0.244 | 0.185, 0.303 | 0.181 | 0.133, 0.229 | ||
|
| ||||||
| Proportion that changed on FV only | 0.141 | 0.093, 0.189 | 0.140 | 0.096, 0.184 | ||
|
| ||||||
| Emotional eating and FV | n=71 | n=71 | ||||
|
| ||||||
| Proportion that changed on emotional eating only | 0.211 | 0.116, 0.306 | 0.127 | 0.050, 0.204 | ||
|
| ||||||
| Proportion that changed on FV only | 0.225 | 0.128, 0.322 | 0.296 | 0.190, 0.402 | ||
|
| ||||||
| Study 3: adults | ||||||
|
| ||||||
| Smoking and diet | n=360 | n=539 | ||||
|
| ||||||
| Proportion that changed on smoking only | 0.178 | 0.138, 0.218 | 0.154 | 0.124, 0.184 | ||
|
| ||||||
| Proportion that changed on diet only | 0.133 | 0.098, 0.168 | 0.117 | 0.090, 0.144 | ||
|
| ||||||
| Smoking and sun protection | n=388 | n=520 | ||||
|
| ||||||
| Proportion that changed on smoking only | 0.191 | 0.152, 0.230 | 0.154 | 0.123, 0.185 | ||
|
| ||||||
| Proportion that changed on sun protection only | 0.142 | 0.107, 0.177 | 0.102 | 0.076, 0.128 | ||
|
| ||||||
| Diet and sun protection | n=1,310 | n=1,764 | ||||
|
| ||||||
| Proportion that changed on diet only | 0.138 | 0.119, 0.157 | 0.136 | 0.120, 0.152 | ||
|
| ||||||
| Proportion that changed on sun protection only | 0.155* | 0.135, 0.175 | 0.103* | 0.089, 0.117 | ||
FV fruit and vegetable consumption
p < 0.05; treatment and control proportions were significantly different
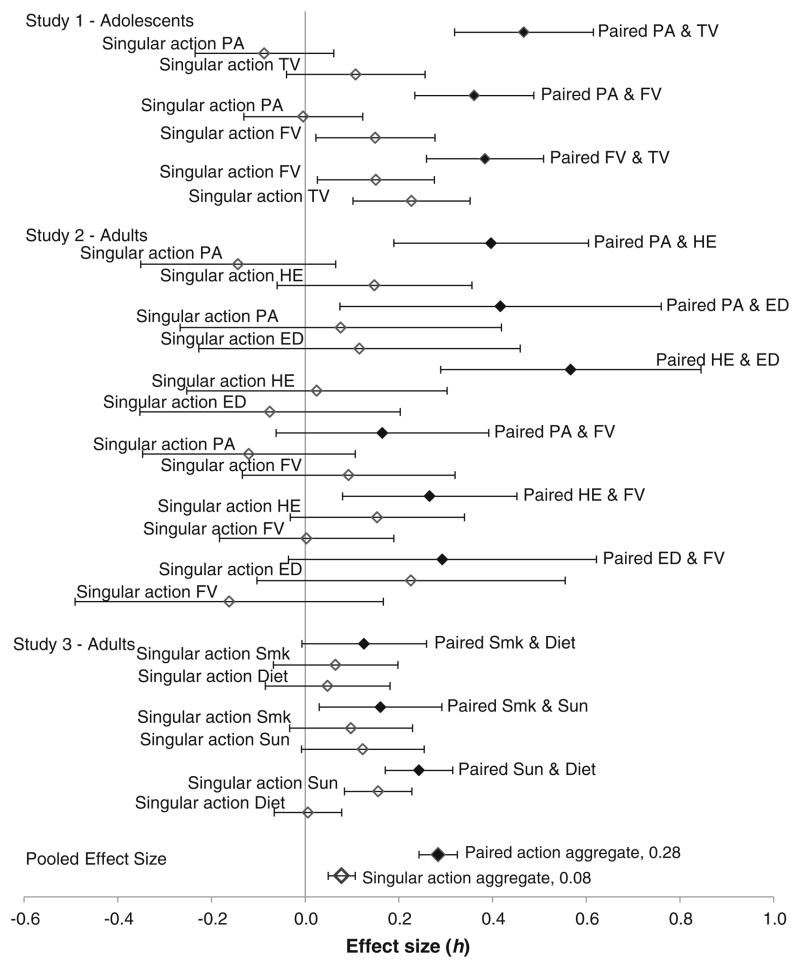
Figure 2 shows that in adolescents, the treatment ESs for paired action were consistently higher than the treatment ESs for singular action for each pair of behaviors. Figure 2 also shows that for both energy balance and cancer prevention behaviors in adults, the treatment ESs for paired action were also consistently higher than the treatment ESs for singular action in all nine assessed behavior pairs. It is worth noting that the results at 12 months follow-up for these same studies were quite similar, with significant albeit slightly smaller effects consistently in favor of the treatment group for paired action, h̄ = 0.21(0.18, 0.25), and singular action, h̄ = 0.06(0.04, 0.09).
Fig 2.
Treatment effect sizes (h) for paired action and singular action at 24 months. Paired paired action, PA exercise, FV fruit and vegetable consumption, HE healthy eating, ED managing emotional distress without eating, Smk smoking, Sun sun protection
Comparing across studies, two of the energy balance pairs in adults (i.e., healthy eating and physical activity, and healthy eating and emotional eating) had the highest rates for paired action (30.5 and 33.0 %, respectively). The two smallest effect sizes for paired action at 24 months were observed with behavior pairs in adults that included smoking (study 3; smoking and sun protection, h=0.16; and smoking and diet, h= 0.13). Further exploration suggested that with weight management in adults (study 2), the three behavior pairs that received full TTM tailoring had substantial effect sizes for paired action at 24 months, h̄ = 0.45(0.30, 0.60). In comparison, the three pairs that included fruit and vegetable consumption that received no TTM tailoring (FV and exercise, healthy eating, or emotional eating) had smaller effect sizes, h̄ = 0.24(0.10, 0.37) for paired action at 24 months.
The proportional contribution of paired action to overall change on each behavior was consistently greater in the treatment than control groups across all 12 behavior pairs at 24 months. The aggregate contribution of paired action to total amount of change on each behavior was approximately 39.5 % in treatment compared to 22.4 % in the control or comparison groups. The combined ES across 12 behavior dyads was substantial and significant at 24 months, h̄ = 0.37(0.34, 0.40).
These results based on complete case analyses were found to be robust in sensitivity analyses that also included all participants at baseline as randomized to study conditions in the original trials. The patterns of individual ESs for the difference between treatment and control groups on paired action, singular action, and contribution of paired action to overall change on each behavior were highly consistent in direction, magnitude, and significance.
DISCUSSION
TTM interventions consistently produced higher rates of paired action on an absolute basis than did the assessment-only control or comparison groups. There were no exceptions to this prediction with 12 out of 12 comparisons favoring treatment conditions. Paired action rates were significantly higher in the treatment than in control or comparison groups in 9 out of 12 comparisons. These comparisons were consistent despite the fact that the studies analyzed involved different types of populations (e.g., adolescents and adults), behaviors (e.g., energy balance, addictive, and appearance related), and treatment intensities (e.g., full, moderate, and minimal tailoring). These uniform results suggest that treatment-enhanced paired action is a robust phenomenon. The magnitude of the pooled ES for paired action (h̄ = 0.28) indicates a substantial effect of simultaneously treating multiple behaviors in individuals with pairs of co-occurring health-risk behaviors.
For singular action, the pooled ES at 24 months (h̄ = 0.08) indicates a significant but very small treatment effect in addition to the effects on paired action. Taken together, these results suggest that when treating individuals for co-occurring pairs of behavioral risks, those who change both behaviors in a pair (paired action) often contribute substantially more (h̄ = 0.37) to the combined population-level treatment effects than those who change on just one of the behaviors in the pair (singular action). These results suggest that TTM-tailored multiple behavior treatments produce some synergy with behavior pairs. In this context then, the significant but low rates of singular action for the treatment groups simply mean that most of the treatment-related outcome is reflected in the paired action results.
A closer exploration of paired action in different types of behaviors suggests that more paired action was produced with two energy balance behaviors that could be expected to be more closely related (e.g., healthy eating and emotional eating, 33.0 %; and physical activity and healthy eating, 30.5 %) than with pairs of cancer risk behaviors that might not be expected to be related (e.g., smoking and diet, 4.7 %; and smoking and sun protection, 4.4 %). These results suggest that simultaneously treating certain types of behavior pairs (e.g., energy balance) may produce greater synergy compared to pairs that include a difficult behavior like smoking. Results from study 2 showing that paired action rates were higher in pairs of energy balance behaviors that received full TTM tailoring for both behaviors, compared to pairs where one behavior received full tailoring and the other (FV) received non-tailored recommendations from a multiple behavior manual, may suggest that within the same population, more intensive treatment as measured by the degree of tailoring delivered may produce greater paired action with energy balance behaviors.
Taken together, what tentative conclusions can be drawn? First, treatment-enhanced paired action looks to be a robust phenomenon in participants with co-occurring behavioral risk pairs, which is reflected by absolute rate differences between treatment and control groups and significant treatment effects on paired action. Treatment further increases singular action (i.e., taking effective action on just one behavior in a pair) in those who did not achieve paired action. Finally, treatment-enhanced paired action contributes substantially to the overall population-level treatment effects in individuals with co-occurring behavioral risks. This would be represented on a Venn diagram by circles with larger areas in the treatment group and a greater degree of overlap between the circles, as shown in Fig. 1d. These observations could not have been derived from research based on the separate behavior paradigm. Comparing paired action rates and the proportional contributions from paired action to the overall amount of change on each treated behavior between treatment and control groups allows direct examination of the effect of simultaneously treating pairs of health-risk behaviors. In this study, we used behavior pairs to demonstrate that studying individuals with co-occurring behavioral risks and whether they change one or more of those behaviors provides richer information about concurrent changes on multiple health behaviors. In principle, this approach could also be extended to studying individuals with more than two co-occurring behavioral risks and the combinations of outcomes on those behaviors. This is an advantage over coaction analyses, which is limited to studying outcomes for pairs of behaviors.
These results from examining pairs of behaviors may be one important step towards a new paradigm for multiple health behavior change research that could complement the separate behavior paradigm that currently dominates this field. In all of our research to date on single and multiple behavior change, the control groups have not been static over time but rather showed modest improvements in behaviors that were greater than the changes that would be expected from secular trends alone. Almost always, treatment conditions showed significantly greater percentages in action or maintenance by final follow-up because the TTM-tailored interventions were able to accelerate the process of behavior change. In spite of our initial hypotheses that some coaction would occur naturally in the control groups due to increased self-efficacy or motivation from successful action taken on one behavior, we found that coaction essentially occurred only in the treatment groups. We believe that with a new paradigm for studying outcomes combined across multiple risk behaviors, beginning with pairs as we have demonstrated here, we are more likely to find evidence for treatment-enhanced synergy where changes on one or more behaviors are closely linked to changes on other behaviors.
These treatment effects on paired and singular action related to types of behaviors, populations, and treatment are suggestive but speculative, given the limited number of comparisons available in this study. This was especially apparent for both the treatment type (one level; TTM CTIs only) and treatment intensity (tailoring) factors. Hopefully, as more studies accumulate with different levels of tailoring, future analyses can shed more light on this potentially important variable. Given the potential importance of such effects for the science and practice of multiple behavior change, future research needs to include many additional types of behaviors, populations, and treatments that may moderate the effects on paired action. Our use of complete case analyses of paired and singular action is offset by the absence of meaningful differences between participants with two or more behavioral risks at baseline who were retained in the study and those who were not retained over time, and especially by the sensitivity analyses that found comparable results.
This study represents preliminary findings in a program of research that can better determine which patterns of multiple behavior change outcomes are most consistent, robust, and synergistic, and which vary the most across different factors related to the complexities of multiple behavior change. Such research can contribute towards a new paradigm based on combined behaviors that can complement the current paradigm based on treating, assessing, and studying each behavior separately.
Implications.
Research
More multiple behavior change studies are needed across a wider range of behaviors, populations, treatments, and time frames. Concurrent change in multiple behaviors should be assessed in the context of co-occurring risks to determine the consistency, robustness, and synergy in patterns of multiple behavior change outcomes.
Practice
Practitioners should consider co-occurring behavioral risks and select evidence-based treatments that simultaneously target those behaviors, in order to maximize synergy in multiple behavior change.
Policy
Policies and interventions that demonstrate effectiveness in enhancing multiple behavior change should be endorsed.
Acknowledgments
Funding for this research, including the primary studies, was provided by the National Cancer Institute (grant no. P01CA050087), the National Heart, Lung, and Blood Institute (grant no. R44HL070549), the National Institute on Drug Abuse (grants nos. R01DA020112 and R01DA023191), and the National Institute of Aging (grant no. R01AG024490). The authors wish to thank Jayson Spas for his helpful suggestions on an earlier draft of this manuscript.
References
- 1.Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Prev Med. 2003;36 (5):615–623. doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- 2.Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors: 2001 national health interview survey. Am J Prev Med. 2004;27(2S):18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 4.Khaw K, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 2008;5(1):e12. doi: 10.1371/journal.pmed.0050012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kvaavik E, Batty G, Ursin G, Huxley R, Gale CR. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom health and lifestyle survey. Arch Intern Med. 2010;170(8):711–718. doi: 10.1001/archinternmed.2010.76. [DOI] [PubMed] [Google Scholar]
- 6.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. Br Med J. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Djoussé L, Driver JA, Gaziano J. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302 (4):394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irwin ML, Mayne ST. Impact of nutrition and exercise on cancer survival. Cancer J. 2008;14(6):435–441. doi: 10.1097/PPO.0b013e31818daeee. [DOI] [PubMed] [Google Scholar]
- 9.Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48:3282–3287. [PubMed] [Google Scholar]
- 10.Xu W, Zhang X, Gao Y, et al. Joint effect of cigarette smoking and alcohol consumption on mortality. Prev Med. 2007;45(4):313–319. doi: 10.1016/j.ypmed.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goetzel RZ, Anderson DR, Whitmer R, et al. The relationship between modifiable health risks and health care expenditures: an analysis of the multi-employer HERO health risk and cost database. J Occup Environ Med. 1998;40(10):843–854. doi: 10.1097/00043764-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Burton WN, Chen CC, Daniel J, Schultz AB, Edington DW. Measuring the relationship between employees’ health risk factors and corporate pharmaceutical expenditures. J Occup Environ Med. 2003;45(8):793–802. doi: 10.1097/01.jom.0000079090.95532.db. [DOI] [PubMed] [Google Scholar]
- 13.Wright DW, Beard MJ, Edington DW. Association of health risks with the cost of time away from work. J Occup Environ Med. 2002;44(12):1126–1134. doi: 10.1097/00043764-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Edington DW. Emerging research: a view from one research center. Am J Health Promot. 2001;15(5):341–349. doi: 10.4278/0890-1171-15.5.341. [DOI] [PubMed] [Google Scholar]
- 15.Wright D, Adams L, Beard MJ, et al. Comparing excess costs across multiple corporate populations. J Occup Environ Med. 2004;46(9):937–945. doi: 10.1097/01.jom.0000137949.40596.ff. [DOI] [PubMed] [Google Scholar]
- 16.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance — United States, 2005. J Sch Health. 2006;76:353–372. doi: 10.1111/j.1746-1561.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- 17.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(SS05):1–142. [PubMed] [Google Scholar]
- 18.Goldstein MG, Whitlock EP, DePue J. Multiple behavioral risk factor interventions in primary care: summary of research evidence. Am J Prev Med. 2004;27(2S):61–79. doi: 10.1016/j.amepre.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 19.National Institutes of Health. [Accessed November 17, 2011];NIH science of behavior change—meeting summary report. 2009 http://commonfund.nih.gov/pdf/SOBC_Meeting_Summary_2009.pdf.
- 20.Prochaska JJ, Prochaska JO. A review of multiple health behavior change interventions for primary prevention. Am J Lifestyle Med. 2011;5(3):208–221. doi: 10.1177/1559827610391883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prochaska JO, Velicer WF, Rossi JS, et al. Multiple risk expert systems interventions: impact of simultaneous stage-matched expert system interventions for smoking, high-fat diet, and sun exposure in a population of parents. Health Psychol. 2004;23 (5):503–516. doi: 10.1037/0278-6133.23.5.503. [DOI] [PubMed] [Google Scholar]
- 22.Prochaska JO, Velicer WF, Redding C, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Prev Med. 2005;41(2):406–416. doi: 10.1016/j.ypmed.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 23.Johnson SS, Paiva AL, Cummins CO, et al. Transtheoretical model-based multiple behavior intervention for weight management: effectiveness on a population basis. Prev Med. 2008;46(3):238–246. doi: 10.1016/j.ypmed.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mauriello LM, Ciavatta MMH, Paiva AL, et al. Results of a multi-media multiple behavior obesity prevention program for adolescents. Prev Med. 2010;51(6):451–456. doi: 10.1016/j.ypmed.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Velicer WF, Redding CA, Paiva AL, et al. Multiple behavior interventions to prevent substance abuse and increase energy balance behaviors in middle school students. Transl Behav Med. doi: 10.1007/s13142-013-0197-0. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Velicer WF, Prochaska JO, Bellis JM, DiClemente CC, Rossi JS, Fava JL, Steiger JH. An expert system intervention for smoking cessation. Addict Behav. 1993;13:269–290. doi: 10.1016/0306-4603(93)90029-9. [DOI] [PubMed] [Google Scholar]
- 27.Redding CA, Prochaska JO, Pallonen UE, et al. Transtheoretical individualized multimedia expert systems targeting adolescents’ health behaviors. Cog Behav Prac. 1999;6:144–153. [Google Scholar]
- 28.Prochaska JJ, Velicer WF, Nigg CR, Prochaska JO. Methods of quantifying change in multiple risk factor interventions. Prev Med. 2008;46:260–265. doi: 10.1016/j.ypmed.2007.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prochaska JO, Butterworth S, Redding CA, et al. Initial efficacy of MI, TTM tailoring and HRI’s with multiple behaviors for employee health promotion. Prev Med. 2008;46(3):226–231. doi: 10.1016/j.ypmed.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prochaska JJ, Velicer WF, Prochaska JO, Delucchi K, Hall SM. Comparing intervention outcomes in smokers treated for single versus multiple behavioral risks. Health Psychol. 2006;25:380–388. doi: 10.1037/0278-6133.25.3.380. [DOI] [PubMed] [Google Scholar]
- 31.Blissmer B, Prochaska JO, Velicer WF, et al. Common factors predicting long-term changes in multiple health behaviors. J Health Psychol. 2010;15(2):205–214. doi: 10.1177/1359105309345555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paiva AL, Prochaska JO, Yin H-Q, et al. Treated individuals who progress to action or maintenance for one behavior are more likely to make similar progress on another behavior: coaction results of a pooled data analysis of three trials. Prev Med. 2012;54(5):331–334. doi: 10.1016/j.ypmed.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noar S, Benac C, Harris M. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 34.Krebs P, Prochaska J, Rossi J. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51(3–4):214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Velicer WF, Redding CA, Sun X, Prochaska JO. Demographic variables, smoking variables, and outcome across five studies. Health Psychol. 2007;26(3):278–287. doi: 10.1037/0278-6133.26.3.278. [DOI] [PubMed] [Google Scholar]
- 36.Evers KE, Prochaska JO, Johnson JL, Mauriello LM, Padula JA, Prochaska JM. A randomized clinical trial of a population- and transtheoretical model-based stress-management intervention. Health Psychol. 2006;25(4):521–529. doi: 10.1037/0278-6133.25.4.521. [DOI] [PubMed] [Google Scholar]
- 37.Velicer WF, Redding CA, Paiva AL, et al. Project BEST: tailored interventions for multiple risk factor prevention for adolescents. Ann Behav Med. 2011;41:s139. [Google Scholar]
- 38.Linnan LA, Emmons KM, Klar N, Fava JL, Laforge RG, Abrams DB. Challenges to improving the impact of worksite cancer prevention programs: comparing reach, enrollment, and attrition using active versus passive recruitment strategies. Ann Behav Med. 2002;24(2):157–166. doi: 10.1207/S15324796ABM2402_13. [DOI] [PubMed] [Google Scholar]
- 39.Velicer WF, Prochaska JO, Redding CA, et al. Efficacy of expert system interventions for employees to decrease smoking, dietary fat, and sun exposure. Int J Behav Med. 2004;11(S1):277. [Google Scholar]
- 40.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: L. Erlbaum Associates; 1988. [Google Scholar]
- 41.Rossi JS. Tables of effect size for z score tests of differences between proportions and between correlation coefficients. Educ Psychol Meas. 1985;45(4):737–743. [Google Scholar]
- 42.Rossi JS. Statistical power analysis. In: Weiner IB, Schinka JA, Velicer WF, editors. Handbook of psychology. Volume 2: research methods in psychology. 2. Hoboken: John Wiley; 2013. [Google Scholar]
- 43.Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks: Sage Publications; 2001. [Google Scholar]
- 44.Cooper HM, Hedges LV, Valentine JC. The handbook of research synthesis and meta-analysis. New York: Russell Sage Foundation; 2009. [Google Scholar]