Abstract
Objective
The inner mucus layer in mouse colon normally separates bacteria from the epithelium. Do humans have a similar inner mucus layer and are defects in this mucus layer a common denominator for spontaneous colitis in mice models and ulcerative colitis?
Methods and Results
The colon mucus layer of mice deficient in the Muc2 mucin, Core 1 O-glycans, Tlr5, IL10 and Slc9a3 (Nhe3) together with dextran sulfate (DSS) treated mice was immunostained for Muc2 and the bacterial localization in the mucus was analyzed. All murine colitis models revealed bacteria in contact with the epithelium. Additional analysis of the less inflamed IL10−/− mice revealed a thicker mucus layer than WT, but the properties were different as the inner mucus layer could be penetrated both by bacteria in vivo and by fluorescent beads the size of bacteria ex vivo. Clear separation between bacteria or fluorescent beads and the epithelium mediated by the inner mucus layer was also evident in normal human sigmoid colon biopsies. In contrast, mucus on colon biopsies of ulcerative colitis (UC) patients with acute inflammation had a highly penetrable mucus. Most UC patients in remission had similar to controls an impenetrable mucus layer.
Conclusions
Normal human sigmoid colon has an inner mucus layer impenetrable to bacteria. The colon mucus in animal models that spontaneously develop colitis and in UC patients with active disease allows bacteria to penetrate and reach the epithelium. Thus colon mucus properties can be modulated and suggest a novel model of UC pathophysiology.
Keywords: Mucin, MUC2, Inflammation, Mucous, Barrier, IL10, Tlr5, Slc9a3, Nhe3, Core 1 glycan, Dextran Sulfate, DSS
INTRODUCTION
Inflammatory bowel disease (IBD), on the rise in the Western world, is divided into Crohn’s disease (CD) and Ulcerative Colitis (UC). Both these diseases are dependent on the presence of intestinal microbiota although specific bacteria have not been linked to disease (1;2). Classical CD has been genetically and functionally linked to proteins, like NOD2 and ATG16L1 (3). UC is less well understood than CD, restricted to the colon and rectum and characterized by a superficial mucosal inflammation (4). The disease is likely to occur in genetically predisposed individuals in combination with environmental and microbial exposure (5). A morphological characteristic used to assess disease activity is the typical goblet cell depletion reflecting emptied goblet cells, something that may suggest a role of the mucus system in UC.
The gut epithelium can manage the enteric bacterial flora in a way that allows a symbiotic relation between host and microbes. The functions, and thus the needs for the epithelium, are different along the intestine and protection of these surfaces are accordingly handled in different ways (6). The small intestinal epithelium mediates nutritional uptake, and the mucus covering these surfaces allows this transport. The bacterial load of the intestine however increases dramatically in the distal direction with a massive colonization in colon. These numerous bacteria are normally handled without causing inflammation, but sometimes the immune system is strongly activated and severe inflammation is observed. How this balance is controlled is still not fully understood, but the recently discovered inner mucus layer in colon, impervious to bacteria, that physically separates bacteria from the epithelium has provided a novel insight into this function (7). It has been suggested that there is a separation between bacteria and epithelium also in humans, (2;8;9) but it is still not clear if humans have a similar protective mucus layer built by the MUC2 mucin although a stratified mucus has been suggested (10).
Colonic mucus is produced by the goblet cell, a cell-type devoted to this task. The main mucus component in the intestine is the MUC2 mucin, a large and heavily O-glycosylated gel-forming mucin that forms enormous polymeric nets by C-terminal dimerization and N-terminal trimerization (11;12). Upon secretion from the goblet cells, the mucus expands rapidly and builds a stratified dense layer that is attached to the epithelium (13). This mucus contains additional proteins of which the FCGBP protein is important as it can stabilize the mucus by additional crosslinks (14). At a distance, far from the epithelial surface, the inner mucus is transformed into a soluble and less organized outer mucus layer that by proteolytic expansion generates a preferred habitat for the commensal microbes (11). Development of spontaneous colitis in Muc2-deficient mice confirms the protective properties of the inner colonic mucus layer (7;15). In these mice, bacteria are found in direct contact with the epithelial cells, far down in the colonic crypts and inside enterocytes, locations never observed in wild-type (WT) animals. These observations and earlier studies on humans with ulcerative colitis showing bacteria in contact with the epithelium (16;17) may suggest that defects in the inner mucus layer that allow bacteria to reach the epithelium in larger quantities can activate the immune system. This made us address, both in mouse models and in human UC, if there are defects of the inner colon mucus layer that can be linked to colitis. We now show that colitic mouse models and patients with UC have dysfunctional colonic mucus that is penetrable to bacteria.
MATERIALS AND METHODS
Animals
Experiments were performed using wild type C57/Bl6, IL10−/−, Slc9a3−/−, C1galt−/− and Tlr5−/− mice all on a C57/Bl6 background (male 8–12 weeks) according to local ethics committee guidelines. All experiments included controls from the same animal facility as the knock-out strains. DSS experiments were performed as described (18;19).
Human subjects and biopsies
Subjects were recruited among patients referred for colonoscopy at Sahlgrens’ University Hospital, Gothenburg, Sweden. Biopsies from the sigmoid colon were assessed from 28 patients with UC. Disease activity was determined by the endoscopic Mayo Score (20). Clinical information regarding the UC patients is presented in Table 1. Biopsies were also obtained from 12 patients with macro- and microscopically normal mucosa (control group). Clinical information on these patients is presented in Table S1. Written and informed consent was obtained from all study subjects and approval for this study was granted by the Human Research Ethical Committee, University of Gothenburg. Biopsies were collected one at the time using single-use large capacity forceps (Olympus) and instantly put into ice-cold oxygenated Krebs solution or fixed in Carnoy’s fixative (7).
Table 1.
Clinical information on the analyzed UC patients.
| No | Gendera | Age | Mayo Score (endoscopic 0–3) | Histological assessmentb | Medication | Relapses/Year(Disease onset)c | PSCd |
|---|---|---|---|---|---|---|---|
| 1 | M | 47 | 0 | A, L | 5-ASA | <1 | x |
| 2 | M | 24 | 0 | NAD | 5-ASA + Azathioprine | <1 | x |
| 3 | M | 26 | 0 | A, L, E | 5-ASA + Azathioprine | <1 | |
| 4 | M | 57 | 0 | NAD | 5-ASA | <1 | |
| 5 | M | 29 | 0 | A | 5-ASA | <1 | |
| 6 | M | 53 | 0 | A | 5-ASAe | <1 | |
| 7 | F | 58 | 0 | NAD | 5-ASA | <1 | |
| 8 | M | 32 | 0 | NAD | 5-ASA + Azathioprine | ≥1 | |
| 9f | M | 24 | 0 | A | 5-ASA + Azathioprine | <1 | x |
| 10 | M | 27 | 0 | A | 5-ASA | (Onset 2011) | |
| 11 | F | 22 | 0 | L, C | 5-ASA + Steroids | (Onset 2011) | |
| 12 | M | 74 | 0 | A | 5-ASA | <1 | |
| 13 | F | 55 | 0 | A | 5-ASA | <1 | |
| 14 | M | 34 | 0 | NAD | None | <1 | |
| 15 | M | 27 | 0 | NAD | 5-ASA | ≥1 | |
| 16 | M | 72 | 0 | NAD | 5-ASA | <1 | |
| 17 | M | 38 | 0 | NAD | 5-ASA | (Onset 2011) | |
| 18 | F | 65 | 1 | A, L, E, P, N, C, CA | 5-ASA | <1 | |
| 19 | F | 37 | 1 | L, E, C, CA | 5-ASA | <1 | |
| 20 | M | 52 | 2 | L, E, P, CA, U | 5-ASA | (Onset 2008) | |
| 21 | M | 28 | 2 | A, L, E, C, CA | 5-ASA | (Onset 2009) | |
| 22 | F | 31 | 2 | A, L, E, C | 5-ASA | ≥1 | |
| 23 | M | 36 | 3 | A, L, N, D | 5-ASA + Azathioprine | ≥1 | |
| 24 | M | 62 | 1 | A, L, C | 5-ASA + Steroids | ≥1 | |
| 25 | M | 26 | 2 | A, L, E, P, C, CA | 5-ASA + Azathioprine | ≥1 | |
| 26 | M | 45 | 2 | A, L, C | 5-ASA + Azathioprine | ≥1 | |
| 27 | M | 18 | 2 | A, L, E, P, C, CA, D, U | 5-ASA + Azathioprine | ≥1 | |
| 28 | F | 21 | 1 | A, L, E, P | 5-ASA + TNFα inhibitors | ≥1 |
M: male, F: female
A: Alterations in crypt architecture, L: Lymphocytes, E: Eosinophiles, P: Plasma cells, N: Neutrophiles, C: Cryptitis, CA: Crypt abscesses, U: Ulceration, D: Denuded epithelium, NAD: Nothing abnormal detected, 5-ASA: 5-aminosalicylic acid
For patients with recent onset of disease the number of relapses cannot be given. Instead year of debut is stated in parenthesis.
PSC: Primary sclerosing cholangitis
Medication with TNF-α inhibitor for rheumatoid arthritis
This patient had inflammation in more proximal part
FISH and immunostaining
Paraffin embedded Carnoy fixed sections were dewaxed and stained with H&E, Alcian blue/PAS or hybridized with 10 ng/μl of a general bacterial 16S rRNA probe (EUB 338) and immunostained for Muc2 using the MUC2C3 antisera or DNA by DAPI (7). Images were obtained with an Axio Examiner Z1 LSM 700 confocal microscope and the ZEN 2010 software (Zeiss).
Mucus penetration score, histology score and goblet cell measurements
Mucus penetration by bacteria was blindly evaluated on DNA stained sections (n=5 for IL10−/− and WT) by two independent observers. The scores (0–4) were based on observations from a whole intestinal cross section per sample and increased scores correspond to increased contact between bacteria and epithelium. Histological scoring of inflammation was performed on H&E and Alcian blue/PAS sections (n=3 per genotype) in a blinded fashion by two independent observers evaluating one whole tissue section per sample. The sum of scores for inflammatory cell infiltration (score, 0–4), goblet cell depletion or decreased mucus accumulation (score, 0–4), mucosa thickening (score, 0–4), destruction of architecture (score, 0 or 3–4) and loss of crypts (score, 0 or 3–4) was calculated (maximum 20). All data are presented as mean±SEM.
Number of goblet cells was counted as described in the supplement. Data is presented as area±SEM with 34 human samples (10 controls, 14 UC patients in remission, 10 UC patients with active disease) and 10 mouse samples (5 WT, 5 IL10−/−). Mucus filled theca area of goblet cells were measured on pictures of anti-MUC2C3 stained sections as described in the supplement. Data is presented as area±SEM with 34 human samples (10 controls, 14 UC patients in remission, 10 UC patients with active disease) and 10 mouse samples (5 WT, 5 IL10−/−).
Preparation of mouse tissue for in vivo and ex vivo experiments
For the in vivo experiments mice were anesthetized by isoflurane (Isoba vet, Schering Plough) with continuous administration. The abdomen was opened and a cup was placed on the opened intestinal segment and filled with warm saline. For the ex vivo experiments mice were anaesthetized with isoflurane and euthanized by cervical dislocation. The distal colon was dissected, flushed and the longitudinal muscle layer removed. The tissue explant was mounted in a horizontal perfusion chamber.
Mucus thickness
The thickness of the colonic mucus was measured as described previously (19). Briefly, the upper surface of the colonic mucus was visualized by addition of charcoal particles. The mucus thickness was determined by measuring the distance between the epithelial surface and the mucus surface by a micropipette viewed through a stereomicroscope (Leica MZ12).
Mucus penetrability
Mucus penetrability was measured as described previously (19). Briefly, colonic explants were mounted in the perfusion chamber and incubated for 20 min followed by addition of a suspension of 2 μm green beads and 0.5 μm red beads to the apical surface (Fluospheres, Invitrogen). The beads were left to sediment through the mucus for 40 min after which the position of the beads in relation to the epithelium was analyzed by taking confocal images in XY stacks with an LSM 700 Axio Examiner Z.1 confocal imaging system and ZEN 2009 software (Zeiss, Germany) Results were analyzed using the Volocity 5.5.1 software (Perkin-Elmer). The mucus penetrability was analyzed to reveal beads close to the epithelium and the mucus thickness containing beads. A detailed methods description is available in the supplement.
Statistical analysis
Mouse data was analyzed using a two-tailed Mann-Whitney U test. For the human data the Kruskal-Wallis test with Dunns’ correction for multiple comparisons was used. A p-value <0.05 was regarded as statistically significant.
Detailed materials and methods are found in the supplement.
RESULTS
The inner mucus layer is defective in animal models that spontaneously develop colitis
The inner mucus layer of the distal colon is built by sheets of the Muc2 mucin organized in stacked layers in a stratified way that does not allow bacteria to penetrate. This physically separates bacteria from the epithelium (figure 1, WT). Animals deficient in the Muc2 gene are devoid of secreted mucus layers, resulting in constant contact between bacteria and the epithelium (figure 1, Muc2−/−) (7). The presence of bacteria in contact with the epithelium was estimated (figure 2A and S1A), and the level of inflammation was estimated on H&E and Alcian blue/PAS stained tissue sections evaluating immune cell infiltration, crypt architecture, and goblet cell filling (‘depletion’) (figure 2B, C and S1B). As observed previously, the Muc2−/− animals showed severe inflammation marked by infiltration of leukocytes and increased cell proliferation as evidenced by crypt elongation (figure 2C, Muc2−/−) (15). A more subtle way to modify the Muc2 mucin is to alter its glycosylation by shortening the O-glycans. Blocking the core 1 extensions by a deletion of the C1galt1 glycosyltransferase results in reduced mucin glycosylation which causes spontaneous colitis (21). These animals show a defective inner mucus layer that allows bacteria to penetrate and come in contact with the epithelium (figure 1 and S1A, C1galt−/−).
Figure 1.
Bacteria localization in the inner mucus layer of colon in different mouse colitis models. (A) Fixed colon sections with preserved mucus was immunostained for Muc2 (green) and bacteria as detected by FISH with general bacterial 16S probes (red) and DNA stained using DAPI (blue). WT was compared to the spontaneous colitis models with different disrupted genes (Muc2−/−, C1galT1−/−, Slc9a3−/−, Tlr5−/− and IL10−/−). Mice were treated with 3% Dextran sulfate (DSS) for 12h or 5 days. Doubled headed arrows show the inner mucus layer not always free of bacteria. Arrows point to bacteria close to the epithelial cells. Scale bars are 20 μm.
Figure 2.
Bacteria penetration and inflammation in different colitis models. (A) Bacteria penetration of the inner mucus was scored for IL10−/− and WT (n=5) with Muc2−/− that have high numbers of bacteria in contact with the epithelium as comparison (n=3). Data is presented as mean±SEM. NI means non-inflamed, I means inflamed. Penetration scores for all the genotypes are presented in Figure S1. (B) Inflammation was monitored as histology scores for IL10−/− and WT (n=5) with Muc2−/− as a severely inflamed comparison (n=3). Data is presented as mean±SEM. Histology scores for all the genotypes are presented in Figure S1. (C) H&E stained tissue sections corresponding to samples in figure 1. Scale bars in all panels are 100 μm.
Sodium-hydrogen exchanger Slc9a3 (Nhe3) deleted mice have been shown to develop spontaneous colitis (22;23). When colon tissue sections from these mice were analyzed an essentially normal mucus was observed with regards to thickness and stratified appearance, but it was penetrated by bacteria (figure 1 and S1A, Slc9a3−/−). As previously described, the tissue sections also showed signs of inflammation with infiltration of immune cells (figure 2C and S1B, Slc9a3−/−). The reason for this mucus phenotype is not understood, but an optimal local ion milieu is believed to be necessary for normal mucus expansion and organization.
The most widely used colitis model is the Dextran Sodium Sulfate (DSS) model where rodents are given 2–5% DSS in the drinking water (24). Inflammation typically appears after 3–5 days. When distal colon tissue sections were examined after 12 h exposure, the inner mucus layer looked relatively normal in thickness and with a stratified pattern. However, bacteria had penetrated the mucus and were found close to the non-inflamed epithelium (figure 1 and S1A, DSS) (18). After 5 days of DSS, the inner mucus layer was lost and the tissue severely inflamed.
Bacteria recognition is part of the innate response and a subgroup of Tlr5-deficient mice spontaneously develop colitis (25). When such animals were studied, an inner mucus layer was observed, but it was penetrated by bacteria and massive infiltration of immune cells was observed (figure 1 and 2C, Tlr5−/− Infl.). The non-inflamed Tlr5 deficient mice revealed a more intact and bacteria free inner mucus (figure 1, Tlr5−/− Non-Infl.).
One of the earliest knock-out animals generated was the one lacking IL10, leading to inflammation that is dependent on the presence of bacteria (26;27). When these animals were analyzed they had a very mild inflammation and a normal thickness and stratified pattern of the inner mucus layer. Interestingly, their inner mucus was also penetrated by bacteria (figure 1 and 2A, IL10−/−). In general terms, more severe inflammation often correlated with a high number of bacteria in contact with the epithelium. The major exception to the rule was the animals exposed to DSS for only 12 h where the bacteria had penetrated the inner mucus layer before development of colitis. This indicates that bacterial contact with the epithelium precedes inflammation and that bacterial contact could trigger subsequent inflammation. The IL10−/− mice showed a low histology score and at the same time also a small mucus penetration score suggesting a relation between bacterial penetration and inflammation. Thus all tested mouse models that developed colitis showed bacteria in direct contact with the epithelium in the distal colon.
The secreted mucus layers are not thinner in IL10 deficient mice with colitis
Because the IL10−/− mice have become a prototype of experimental colitis and do not have a primary defect in any mucus component, we analyzed this model in more detail. As bacteria penetrating the inner mucus layer appears to be a hallmark of murine colitis, one could speculate that this is due to a thinner mucus layer. To address this, the mucus thickness in the distal colon was measured both in vivo and ex vivo in young IL10−/− mice with low grade inflammation as well as in WT mice (figure 3B, C). In vivo the total (inner and outer) mucus layer thickness was measured directly followed by aspiration of the loose outer mucus and measurements of the inner firmly adherent mucus thickness. The total thickness did not differ between IL10−/− and the WT mice, but the adherent mucus was significantly thicker in the IL10−/− mice (figure 3A). Distal colon tissue was also mounted in a horizontal perfusion chamber and the mucus growth was followed ex vivo for 1h (19). The mucus thickness and growth during this time did not differ between IL10−/− and WT mice (figure 3B). Thus, a thinner mucus layer cannot explain why bacteria are found close to the epithelium in the IL10−/− mice.
Figure 3.

Mucus thickness in WT and IL10−/− mice. (A) In vivo measurements of the initial mucus thickness in WT (n=7) and IL10−/− (n=5) mice. The total mucus thickness (Total) was measured followed by aspiration of the mucus and measurement of the remaining mucus thickness (Adherent). (B) Ex vivo measurements of the growth in total mucus thickness over time in WT (n=5) and IL10−/− (n=6) mice. (C) Area of the goblet cell theca in Anti-MUC2C3 stained colon section of WT (n=3) and IL10−/− (n=3) mice. Data is presented as mean ± SEM and the two-tailed Mann-Whitney U test was used to compare the mucus thickness in WT and IL10−/− mice.
The mucus stored in the goblet cells is the material that can build up and renew the secreted mucus layer. The number of goblet cells in the upper 100μm of the crypt were counted in IL10−/− and WT colon sections. The amount of goblet cells did not differ between these groups (figure 3C). The amount of stored mucus was assessed by measuring the area of the mucus filled theca in goblet cells of the upper part of the crypt. There was no significant difference in the size of the mucus filled theca of the goblet cells between WT and IL10−/− mice (figure 3C). The stored mucus available for secretion is thus not altered in the IL10−/− mice.
The mucus quality is defective in IL10 deficient mice
As the inner mucus was not found to be thinner in the IL10−/− mice, we instead analyzed the mucus penetrability to beads the size of bacteria. Colonic explants were mounted in the horizontal perfusion chamber and allowed to secrete mucus for 20 min, followed by the addition of fluorescent beads (0.5 and 2 μm) on top of the formed mucus. The beads were allowed to sediment for 40 min and the position of the beads in relation to the epithelium was determined by confocal microscopy. Mucus on WT explants mucus did not allow the beads to penetrate and separated both the 0.5 and 2 μm beads from the epithelium (figure 4A). On the other hand, mucus produced by the IL10−/− mice was unable to create such separation (figure 4A). To quantify the mucus penetrability we estimated the proportion of bead intensity found in close proximity to the epithelium (figure 4B). In the IL10−/− mice almost 50% of the bead intensity was found close to the epithelium compared to 1% in the WT mice. The IL10−/− mucus was completely penetrable, while the controls had about 200 μm thick non-penetrable inner mucus (figure 4C). Thus, the inner mucus quality is compromised in IL10−/− mice. The thickness is based on the mucus containing beads and as the mucus in IL10−/− colon is very penetrable this results in a value smaller than in figure 3B where the mucus thickness is based on charcoal binding to the mucus surface.
Figure 4.
Mucus penetrability in WT (n=5) and IL10−/− (n=5) mice. (A) Representative Z-stack projections with the respective normalized intensity plots. Scale bars 100 μm. (B) Percent of the total bead intensity in close proximity to the epithelial surface (40 μm). Differences between the groups were analyzed using a two-tailed Mann-Whitney U test. (C) Relation between penetrable and impenetrable mucus. The black part of the bar represents impenetrable mucus and the green part mucus containing the 2 μm beads.
Normal human sigmoid colon has their bacteria well separated from the epithelium
As we previously have described that mouse colon has a two layered mucus system where the inner layer is devoid of bacteria, we first asked if humans had the same organization. Patients referred for colonoscopy were included after informed consent. Clinical information on the control patients is compiled in table S1. Penetrability measurements of the secreted mucus from sigmoid biopsies were performed as for mouse colon and representative z-stack projections and corresponding normalized intensity plots for the different groups were collected (figure 5). Control patients showed an impenetrable mucus layer, on the average 400 μm thick, separating beads from the epithelium (figure 5A and D). To confirm that the human colonic mucus forms an inner mucus layer similar to that observed in mouse colon (7), we analyzed control sigmoid samples not pretreated with laxative (figure 6Ca and Da for H&E). Biopsies were fixed to preserve the mucus, immunostained for MUC2 and counterstained for DNA to visualize cell nuclei and bacteria (FISH probes do not detect all bacteria associated with the biopsies). Similar to the mice, a stratified mucus layer was observed with bacteria only present at the luminal surface of the mucus.
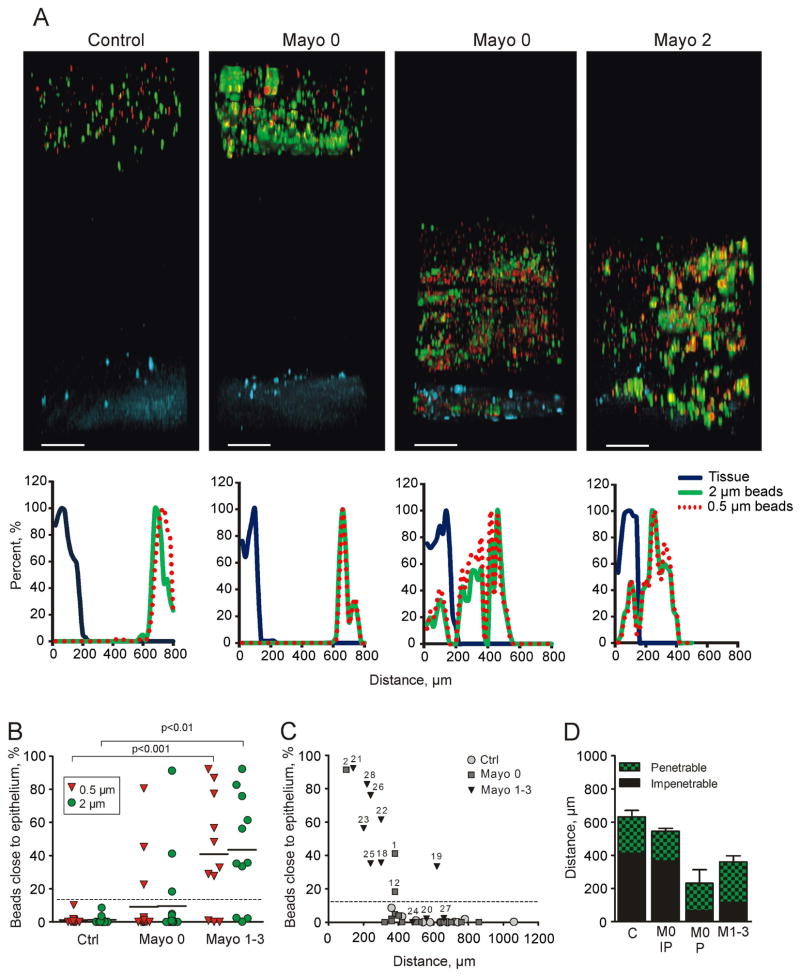
Figure 5.
Mucus penetrability in human colonic biopsies from controls (n=12) and UC patients (Mayo 0 n=17, Mayo 1–3 n=11). (A) Representative Z-stack projections with the respective normalized intensity plots. Scale bars 100 μm. (B) Percent of total bead intensity in close proximity to the epithelial surface (<120 μm). Differences between groups were analyzed using the Kruskal-Wallis test with Dunns’ correction for multiple comparisons (primary analysis p=0.0009 for the 2 μm beads and p=0.0004 for the 0.5 μm beads). (C) Percent beads in in relation to total mucus thickness of individual patients. Numbers refer to Table 1. (D) Relation between penetrable and impenetrable mucus of the 2 μm green beads. M0 IP refers to patients with Mayo endoscopic score 0 and impenetrable mucus. M0 P refers to Mayo score 0 and penetrable mucus (patients #1, 2, and 12). M1–3 to Mayo score 1–3.
Figure 6.

Mucus filled goblet cells and bacteria of fixed human sigmoid biopsies. Human colon biopsies were Carnoy fixed to preserve the mucus and immunostained for MUC2 in combination with DAPI for DNA in nuclei and bacteria. (A) The goblet cell theca area was measured in fixed and MU2 stained sections from UC patients and controls. Data is presented as mean ± SEM and the two-tailed Mann-Whitney U test was used to compare the UC patients with active disease to the control group. (B) Sections from human sigmoid biopsies stained for MUC2 (green) and DAPI (blue). (a) A biopsy collected and directly fixed from sigmoid colon of a control patient without preceding laxative treatment. (b) A biopsy from a control patient included in the penetrability study that was pretreated with laxatives before colonoscopy. (c) Biopsy from UC patient pretreated with laxative and with endoscopic Mayo score of 2 at colonoscopy. Pictures to the right only show the DAPI staining. Bacteria (arrows) are found on the outer surface of the mucus in control patients (a and b). Bacteria are found inside the inner mucus and close to the epithelium in the active UC patient (c). Some detached cells can be observed (arrowheads). (C) H&E stained tissue each corresponding to (B a–c). Scale bars are 10 μm (B) and 100 μm (C).
UC patients with active disease and a subgroup of UC patients in remission have penetrable mucus
Considering that increased bead penetrability correlated with bacteria close to the epithelium in mouse colitis models, we asked whether this also translated to human UC patients. Patients with UC were divided into two groups; UC patients in remission (Mayo endoscopic score 0) and UC patients with active disease (Mayo endoscopic score 1–3). Clinical information on the UC patients is compiled in table 1. The patients with an active disease display many more inflammatory associated histological changes compared to the patients in remission. Penetrability measurements of the secreted mucus from sigmoid biopsies were performed and representative Z-stack projections and corresponding normalized intensity plots for the different groups were collected (figure 5). UC patients in remission (Mayo 0) also had a mucus thickness similar the control patients except for three patients (figure 5D). In contrast, most patients with active UC had a thinner mucus layer that was penetrable by beads. Mucus penetrability, quantified as amount of beads close to the epithelium (20 μm into the tissue and 120 μm into the lumen), showed around 40% penetrability in the active patients, 10% penetrability in the remission patients and close to zero in the controls (figure 5B). The individual values for penetrability versus mucus thickness (defined as bead-containing material) show heterogeneity especially in the remission patients (Mayo 0) (figure 5C). Interestingly, three of the remission patients (#1, 2, and 12) produced mucus that was penetrable to the beads. When these penetrable (P) patients were plotted separately from the remission group, the impenetrable (IP) looked like the control patients and the P group as the active (Mayo 1–3) (figure 4D). Thus, mucus secreted from human sigmoid colon was normally dense and thick, whereas the mucus was thinner and penetrable in UC patients with active inflammation and in a sub-group of UC patients in remission. The mucus quality did not correlate with azathioprine treatment. The number of goblet cells in the upper 150 μm crypt was determined and no differences were observed in any of the groups indicating that there are not fewer goblet cells in either remission or actively inflamed UC patients (figure 6A). The mucus stored in the goblet cells of the upper crypts measured as theca area did not differ between controls and UC patients in remission (figure 6B). The patients in remission identified to have penetrable mucus (figure 5B, C) had goblet cell theca area of similar size arguing for normal stored mucus amounts (figure 6B). The actively inflamed patients were however observed to have less filled goblet cells seen as smaller theca areas which would correspond to the thinner mucus layer observed (figure 6B).
We finally asked if the difference in mucus quality of the inflamed UC patients that allowed beads to sediment down to the epithelium reflected bacteria penetrating the inner mucus. Biopsies taken from the same individuals as used for penetrability measurements were fixed to preserve the mucus, immunostained for MUC2 and counterstained for DNA to visualize cell nuclei and bacteria. These patients were all pretreated with oral laxative to clear the intestine for routine colonoscopy. This treatment affects the mucus and its turnover and the fixed material shows a more voluminous and unstructured mucus also in control patients (figure 6Cb, Db). The amount of mucus that remained attached to the epithelial surface varied between the biopsies which excluded evaluation of all patients. In comparison to the laxative treated control patients, the inflamed patients had less attached mucus and bacteria penetrated this mucus and reached the epithelium (figures 6C and 6B).
DISCUSSION
The inner mucus layer forms a barrier that separates bacteria from the epithelium in the normal healthy colon of mice as demonstrated previously (7). This was shown by Carnoy fixation on intact tissue without previous washing of the luminal content. We have now studied a number of different colitis models and confirmed mucus defects in all of them. It is well established that intestinal bacteria are necessary for all these models and that the composition of the microbiota influences the severity and outcome of the inflammation. The Muc2-null mice totally lack mucus and spontaneously develop severe inflammation (7;15) while the other models all have a more or less intact inner mucus layer that is however penetrated by bacteria. The glycan deficient Core 1-deficient mice have a less glycosylated Muc2 mucin that probably is easier to degrade by the bacteria (21). DSS induce inflammation initiated by a direct toxic effect on the mucus (18;28). Tlr5−/− mice have a thinner and defective inner mucus layer (29). Nhe3-deficient and IL10−/− mice display a morphologically stratified inner mucus layer that is still penetrable to bacteria (22;23). These data argue for an impaired mucus layer that allows bacteria to penetrate as a potential mechanism involved in the development of colon inflammation.
Assuming that the inner mucus layer in colon is vitally important for colon barrier function, a thinner mucus layer could be associated with inflammation. However, the mucus thickness alone was not a useful indicator of mucus barrier function since for example the IL10-deficient mice had a thicker inner attached mucus layer. Instead, these animals had an increased mucus secretion, maybe as an attempt to try to overcome the mucus barrier defect. We can now show that also human sigmoid colon of healthy individuals has an inner stratified MUC2 containing mucus layer that separates the bacteria from the epithelium. Bacterial contact with the epithelium has previously been observed in inflamed intestinal samples, but it was only analyzed on fixed biopsies (16;17). The mucus is then often lost or collapsed, problems that can hamper the evaluation. We have now studied the protective quality of the mucus by assessing its ability to restrict small spherical particles to sediment down to the epithelial surface to illustrate its property to exclude bacteria close to the epithelium. This is performed on live explant at physiological conditions to gain information about its normal in vivo function. The distance between beads and cells were about 200 μm in the mouse, something that should be compared to the about 50 μm thick inner mucus layer as measured after aspiration of the outer loose mucus layer (7). That the beads did not pass all the way down to 50 μm suggest that the outer mucus layer is not homogenous and that it is denser close to the border between inner and outer mucus layer. This is in line with the prediction of proteolytic activities being responsible for the conversion from inner dense to the outer loose mucus layer (7). The mucus separating the beads was about 400 μm in the humans and thus the inner mucus layer can be predicted to be about twice as thick in humans compared to mice.
The IL10−/− model is one of the oldest colitis models studied where the inflammation is explained by the loss of the anti-inflammatory effects of IL10 (30). The pro-inflammatory initiating effect is mediated by colonic mononuclear phagocytes of the innate defense (31). The IL10−/− mice maintained in our animal house display only minor histological inflammatory signs, but still have a penetrable mucus layer both to beads and bacteria. This argues for a link between mucus properties and the immune system and produced cytokines. The mechanism behind the IL10 effect on the mucus producing goblet cells is not understood, but the number of goblet cells and size of the theca with the mucus granulae in the goblet cells are not different compared to WT mice. This implies changes not relating to mucus amounts and may suggest other mechanisms. The mucus organization and expansion at secretion is dependent on the external milieu and alterations could have devastating effects (13;32). The mucus organization is also a result of additional crosslinking and processing where defects also could contribute to the identified penetrable mucus.
UC is not caused by pathogenic bacteria, but is rather the result of abnormal reactions to the normal microbiota possibly associated with dysbiosis (3;4;33;34). Antibiotic treatments and fecal deviation can sometimes be beneficial for colitis patients (35;36), although the best arguments for the importance of lowering the load of commensal bacteria in contact with the epithelium are based on mouse studies. The surface epithelial cell layer probably can withstand and handle some bacteria, but will likely have difficulties in withstanding a massive direct bacterial contact for a longer period. A higher bacterial contact will cause bacterial leakage into the tissue, something that could trigger the subepithelial adaptive immune system.
Most of the UC patients in remission (Mayo score 0) had, like the control patients, a thick inner mucus layer that was not penetrated by fluorescent beads. However, three of these patients had mucus that was more or less totally penetrable to the beads, but did not have smaller goblet cell theca area in analogy with the IL10−/− mice. Two of them had primary sclerosing cholangitis (PSC). As all the spontaneous mouse colitis models had mucus penetrable to bacteria, it is expected that some UC patients might also have mucus defects making their mucus less protective. The reason for the observed mucus alterations in active colitis patients may reflect higher mucus secretion as shown by the same number of but less filled goblet cells, observed as smaller theca area, or more empty goblet cells, described after PAS staining as goblet cell depletion. This characteristic is mainly attributed to more severely inflamed tissue and not observed in inactive disease or the less inflamed IL10−/− animals. As the generation of the enormously large MUC2 polymeric network is time consuming and difficult, a high demand and fast turnover, as in inflammation, are likely to generate a mucus of poorer quality (37). This was recently illustrated by studies of colon ischemia where reperfusion emptied the crypt goblet cells with a concomitant clearance of bacteria (38). After this, the goblet cells were not refilled for many hours and another challenge should be less efficiently handled. An inner mucus gel that is less dense with the MUC2 mucin is likely to be more penetrable, but other more sophisticated mechanisms are likely to be involved. The genetic and environmental factors causing and maintaining UC are likely numerous. Our observations suggest that the inner mucus and its barrier function are an important factor in limiting bacterial contact with the epithelium and that defects in this system might trigger inflammation. The colon mucus properties are also shown to be dynamic and probably modulated by both bacteria and host factors using only partly known mechanisms. Understanding these mechanisms might provide novel approaches for prolonging remission periods for the UC patients.
Supplementary Material
Significance of this study.
What is already known about this subject?
In mouse colon bacteria are separated from the epithelial cells by the inner mucus layer formed by the MUC2 mucin.
Muc2 deficient mice do not have any secreted mucus and have bacteria in direct contact with the epithelium. These mice develop colitis and later on colon cancer.
What are the new findings?\
Humans have an inner mucus layer that normally separates bacteria from coming in contact with the epithelial cells.
Penetration of the inner mucus layer by beads the size of bacteria correlate with bacterial penetration.
Mouse models of colitis have bacteria and beads penetrating the inner mucus layer.
Humans with active ulcerative colitis have an inner mucus layer that is penetrable.
Some ulcerative colitis patients in remission do also have an inner mucus layer that is penetrable.
How might it impact on clinical practice in the foreseeable future?
This observation will give a new understanding of ulcerative colitis and open new lines of research.
An understanding on how the penetrability properties of the inner mucus are regulated will provide novel therapeutic opportunities. An improved mucus protection could be instrumental for UC remission maintenance.
Acknowledgments
Funding This work was supported by the Swedish Research Council (no. 7461, 21027), The Swedish Cancer Foundation, The Knut and Alice Wallenberg Foundation, IngaBritt and Arne Lundberg Foundation, Sahlgren’s University Hospital (LUA-ALF), Wilhelm and Martina Lundgren’s Foundation, Torsten och Ragnar Söderbergs Stiftelser, The Sahlgrenska Academy, National Institutes of Health (U01AI095473, R01DK073638, the content is solely the responsibility of the authors and does not necessarily the National Institutes of Health), The Swedish Foundation for Strategic Research - The Mucus-Bacteria-Colitis Center (MBC) of the Innate Immunity Program and Assar Gabrielsson foundation.
Drs. Herbert Helander och Mats Wolving are acknowledged for pathological examinations.
Abbreviations
- UC
ulcerative colitis
- CD
Crohn’s disease
- DSS
Dextran Sodium Sulfate
- WT
wild type
- FISH
fluorescent in situ hybrization
- PSC
primary sclerosing cholangitis
- PAS
periodate acid Schiff
Footnotes
Competing interest None.
Ethics approval All animal studies were approved by the animal ethics committee of the respective universities: Gothenburg, Emroy, Arizona and Oklahoma. The human studies were approved by the Human Research Ethical Committee, University of Gothenburg.
Contributions M.E.V.J. and G.C.H. conceived the original idea. M.E.V.J., J.K.G., J.H.L., H.S., K.S.J. and G.C.H. designed the study, analyzed the data and wrote the manuscript. M.E.V.J., J.K.G. and J.H.L. conducted the experiments, and analyzed the data. L.X., H.X., F.K.G., F.A.C., and A.T.G. provided genetically modified mouse tissues. K.S.J., and H.S. analyzed the patients.
References
- 1.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–34. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 2.Sartor RB. Therapeutic manipulation of the enteric microflora in inflammatory bowel diseases: Antibiotics, probiotics, and prebiotics. Gastroenterology. 2004;126:1620–33. doi: 10.1053/j.gastro.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 3.Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474:307–17. doi: 10.1038/nature10209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danese S, Fiocchi C. Ulcerative Colitis. New Engl J Med. 2011;365:1713–25. doi: 10.1056/NEJMra1102942. [DOI] [PubMed] [Google Scholar]
- 5.Schirbel A, Fiocchi C. Inflammatory bowel disease: Established and evolving considerations on its etiopathogenesis and therapy. J Dig Dis. 2010;11:266–76. doi: 10.1111/j.1751-2980.2010.00449.x. [DOI] [PubMed] [Google Scholar]
- 6.Johansson MEV, Hansson GC. Keeping Bacteria at a Distance. Science. 2011;334:182–3. doi: 10.1126/science.1213909. [DOI] [PubMed] [Google Scholar]
- 7.Johansson MEV, Phillipson M, Petersson J, et al. The inner of the two Muc2 mucin dependent mucus layers in colon is devoid of bacteria. Proc Natl Acad Sci USA. 2008;105:15064–9. doi: 10.1073/pnas.0803124105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Waaij LA, Harmsen HJM, Madjipour M, et al. Bacterial population analysis of human colon and terminal ileum biopsies with 16S rRNA-based fluorescent probes: Commensal bacteria live in suspension and have no direct contact with epithelial cells. Inflamm Bowel Dis. 2005;11:865–71. doi: 10.1097/01.mib.0000179212.80778.d3. [DOI] [PubMed] [Google Scholar]
- 9.Swidsinski A, Loening-Baucke V, Lochs H, et al. Spatial organization of bacterial flora in normal and inflamed intestine: A fluorescence in situ hybridization study in mice. World J Gastroenterol. 2005;11:1131–40. doi: 10.3748/wjg.v11.i8.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsuo K, Ota H, Akamatsu T, et al. Histochemistry of the surface mucous gel layer of the human colon. Gut. 1997;40:782–9. doi: 10.1136/gut.40.6.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johansson MEV, Holmen Larsson JM, Hansson GC. The two mucus layers of colon are organized by the MUC2 mucin, whereas the outer layer is a legislator of host-microbial interactions. Proc Natl Acad Sci USA. 2011;108:4659–65. doi: 10.1073/pnas.1006451107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Godl K, Johansson MEV, Karlsson H, et al. The N-termini of the MUC2 mucin form trimers that are held together within a trypsin-resistant core fragment. J Biol Chem. 2002;277:47248–56. doi: 10.1074/jbc.M208483200. [DOI] [PubMed] [Google Scholar]
- 13.Ambort D, Johansson MEV, Gustafsson JK, et al. Calcium and pH-dependent Packing and Release of the Gel-forming MUC2 Mucin. Proc Natl Acad Sci U S A. 2012;109:5645–50. doi: 10.1073/pnas.1120269109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johansson MEV, Thomsson KA, Hansson GC. Proteomic Analyses of the Two Mucus Layers of the Colon Barrier Reveal That Their Main Component, the Muc2 Mucin, Is Strongly Bound to the Fcgbp Protein. J Proteome Res. 2009;8:3549–57. doi: 10.1021/pr9002504. [DOI] [PubMed] [Google Scholar]
- 15.Van der SM, de Koning BA, De Bruijn AC, et al. Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterology. 2006;131:117–29. doi: 10.1053/j.gastro.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 16.Swidsinski A, Loening-Baucke V, Theissig F, et al. Comparative study of the intestinal mucus barrier in normal and inflamed colon. Gut. 2007;56:343–50. doi: 10.1136/gut.2006.098160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schultsz C, van den Berg FM, en Kate FW, Tytgat GNJ, Dankert J. The intestinal mucus layer from patients with inflammatory bowel disease harbors high numbers of bacteria compared with controls. Gastroenterology. 1999;117:1089–97. doi: 10.1016/s0016-5085(99)70393-8. [DOI] [PubMed] [Google Scholar]
- 18.Johansson MEV, Gustafsson JK, Sjoberg KE, et al. Bacteria penetrate the inner mucus layer before inflammation in the Dextran sulfate colitis model. PLoS ONE. 2010;5:e12238. doi: 10.1371/journal.pone.0012238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gustafsson JK, Ermund A, Johansson MEV, et al. An ex vivo method for studying mucus formation, properties and thickness in human colonic biopsies and mouse small and large intestinal explants. Amer J Physiol Gastrointest Liver Physiol. 2011;302:G430–G438. doi: 10.1152/ajpgi.00405.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewis JD, Chuai S, Nessel L, et al. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14:1660–6. doi: 10.1002/ibd.20520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fu J, Wei B, Wen T, et al. Loss of intestinal core 1-derived O-glycans causes spontaneous colitis. J Clin Invest. 2011;121:1657–66. doi: 10.1172/JCI45538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schultheis PJ, Clarke LL, Meneton P, et al. Renal and intestinal absorptive defects in mice lacking the NHE3 Na+/H+ exchanger. Nat Genet. 1998;19:282–5. doi: 10.1038/969. [DOI] [PubMed] [Google Scholar]
- 23.Laubitz D, Larmonier CB, Bai A, et al. Colonic gene expression profile in NHE3-deficient mice: evidence for spontaneous distal colitis. Am J Physiol Gastrointest Liver Physiol. 2008;295:G63–G77. doi: 10.1152/ajpgi.90207.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Isao O, Shigeru H, Masahiro Y, et al. A novel method in the induction of reliable experimental acute and chronic ulcerative colitis in mice. Gastroenterology. 1990;98:694–702. doi: 10.1016/0016-5085(90)90290-h. [DOI] [PubMed] [Google Scholar]
- 25.Vijay-Kumar M, Sanders CJ, Taylor RT, et al. Deletion of TLR5 results in spontaneous colitis in mice. J Clin Invest. 2007;117:3909–21. doi: 10.1172/JCI33084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuhn R, Lohler J, Rennick D, et al. Interleukin-10-deficient mice develop chronic enterocolitis. Cell. 1993;75:263–74. doi: 10.1016/0092-8674(93)80068-p. [DOI] [PubMed] [Google Scholar]
- 27.Sellon RK, Tonkonogy S, Schultz M, et al. Resident enteric bacteria are necessary for development of spontaneous colitis and immune system activation in interleukin-10-deficient mice. Infect Immun. 1998;66:5224–31. doi: 10.1128/iai.66.11.5224-5231.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yan Y, Kolachala V, Dalmasso G, et al. Temporal and Spatial Analysis of Clinical and Molecular Parameters in Dextran Sodium Sulfate Induced Colitis. PLoS ONE. 2009;4:e6073. doi: 10.1371/journal.pone.0006073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carvalho FA, Koren O, Goodrich, et al. Transient Inability to Manage Proteobacteria Promotes Chronic Gut Inflammation in TLR5-Deficient Mice. Cell Host & Microbe. 2012;12:139–52. doi: 10.1016/j.chom.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Izcue A, Coombes JL, Powrie F. Regulatory Lymphocytes and Intestinal Inflammation. Annu Rev Immunol. 2009;27:313–38. doi: 10.1146/annurev.immunol.021908.132657. [DOI] [PubMed] [Google Scholar]
- 31.Hoshi N, Schenten D, Nish SA, et al. MyD88 signalling in colonic mononuclear phagocytes drives colitis in IL-10-deficient mice. Nat Commun. 2012;3:1120. doi: 10.1038/ncomms2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gustafsson JK, Ermund A, Ambort D, et al. Bicarbonate and functional CFTR channel is required for proper mucin secretion and link Cystic Fibrosis with its mucus phenotype. J Exp Med. 2012;209:1263–72. doi: 10.1084/jem.20120562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mannon PJ, Hornung RL, Yang Z, et al. Suppression of inflammation in ulcerative colitis by interferon-beta-1a is accompanied by inhibition of IL-13 production. Gut. 2011;60:449–55. doi: 10.1136/gut.2010.226860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology. 1998;115:182–205. doi: 10.1016/s0016-5085(98)70381-6. [DOI] [PubMed] [Google Scholar]
- 35.Gilat T, Leichtman G, Delpre G, et al. A comparison of metronidazole and sulfasalazine in the maintenance of remission in patients with ulcerative colitis. J Clin Gastroenterol. 1989;11:392–5. doi: 10.1097/00004836-198908000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Gionchetti P, Rizzello F, Ferrieri A, et al. Rifaximin in patients with moderate or severe ulcerative colitis refractory to steroid-treatment: a double-blind, placebo-controlled trial. Dig Dis Sci. 1999;44:1220–1. doi: 10.1023/a:1026648812439. [DOI] [PubMed] [Google Scholar]
- 37.Johansson MEV, Ambort D, Pelaseyed T, et al. Composition and functional role of the mucus layers in the intestine. Cell Mol Life Sci. 2011;68:3535–641. doi: 10.1007/s00018-011-0822-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grootjans J, Hundscheild IH, Lenaerts K, et al. Ischemia-induced mucus barrier loss and bacterial penetration are rapidly counteracted by increased goblet cell secretory activity in human and rat colon. Gut. 2012 doi: 10.1136/gutjnl-2011-301956. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.