Abstract
Objectives
We examined the impact of expanding health insurance coverage on socioeconomic disparities in total and cardiovascular disease mortality from 1998 to 2007 in Colombia.
Methods
We used Poisson regression to analyze data from mortality registries (633 905 deaths) linked to population census data. We used the relative index of inequality to compare disparities in mortality by education between periods of moderate increase (1998–2002) and accelerated increase (2003–2007) in health insurance coverage.
Results
Disparities in mortality by education widened over time. Among men, the relative index of inequality increased from2.59 (95% confidence interval [CI] = 2.52, 2.67) in 1998–2002 to 3.07 (95% CI = 2.99, 3.15) in 2003–2007, and among women, from 2.86 (95% CI = 2.77, 2.95) to 3.12 (95% CI = 3.03, 3.21), respectively. Disparities increased yearly by 11% in men and 4% in women in 1998–2002, whereas they increased by 1% in men per year and remained stable among women in 2003–2007.
Conclusions
Mortality disparities widened significantly less during the period of increased health insurance coverage than the period of no coverage change. Although expanding coverage did not eliminate disparities, it may contribute to curbing future widening of disparities.
Recent health care reform in the United States has sparked debate on the potential impact of expanding health insurance coverage on access to care and disparities in health care.1 People with lower socioeconomic status are at increased risk of many conditions and are therefore more likely to benefit from an expansion in health insurance coverage.1 Previous observational studies in the United States have suggested that a lack of health insurance was associated with an increased risk of subsequent mortality in all socioeconomic groups.2 However, little is known about the impact of health insurance coverage on socioeconomic disparities in mortality following a major expansion in insurance coverage. In1993, the Colombian government implemented a major health care reform that introduced mandatory health insurance.3 As a result, coverage increased from 47% in 19944 to 98% in 2010.5 Although the social and economic context of Colombia differs substantially from that in the United States, lessons from the Colombian reform can shed light on the potential impact of increased health insurance coverage on health disparities in the United States and middle-income countries currently expanding insurance coverage.
A desirable outcome of coverage expansion is that it will have a larger impact on the health of the poor and will contribute to a reduction in health disparities.3,6 The reform in Colombia established a scheme of subsidies targeted to the poor, assigning citizens to 2 schemes on the basis of income: (1) the contributory scheme, which covers workers and their families with an income above the cut-off and is financed through payroll and employer’s contributions, and (2) the subsidized scheme, which covers the poor as identified through a proxy means test.6
In the poorest income quartile, health insurance coverage increased from 6% in 1993 to more than 70% in 2007,6 an increase attributable to the subsidized scheme.5 Increased coverage among the poor is expected to improve health outcomes by ensuring timely care and bringing them into closer contact with the health care system.7 However, the reform also increased the complexity of the system potentially leading to delays in some types of care8 and reducing spending in prevention and public health.9 Previous dynamic simulations for the United States have suggested that expanding health insurance coverage is cost-effective, but failing to also expand the primary care capacity for the disadvantaged could lead to increasing health disparities.10 There have been no empirical studies examining these issues in the context of a major health care reform.
Most previous studies have focused on the impact of health care reform on utilization and access to health care services, with only some studies examining the impact on population health.7,11–13 A recent review of available evidence concluded that expanding health insurance coverage generally improves access to care and population health particularly for lower income groups, but health gains may be dependent on the institutional framework and governance arrangements.14 On the other hand, the World Health Organization Commission on Social Determinants of Health concluded that, although inequity in health care is critical, the largest burden of illness arises in large part because of the conditions in which people are born, grow, live, work, and age.15
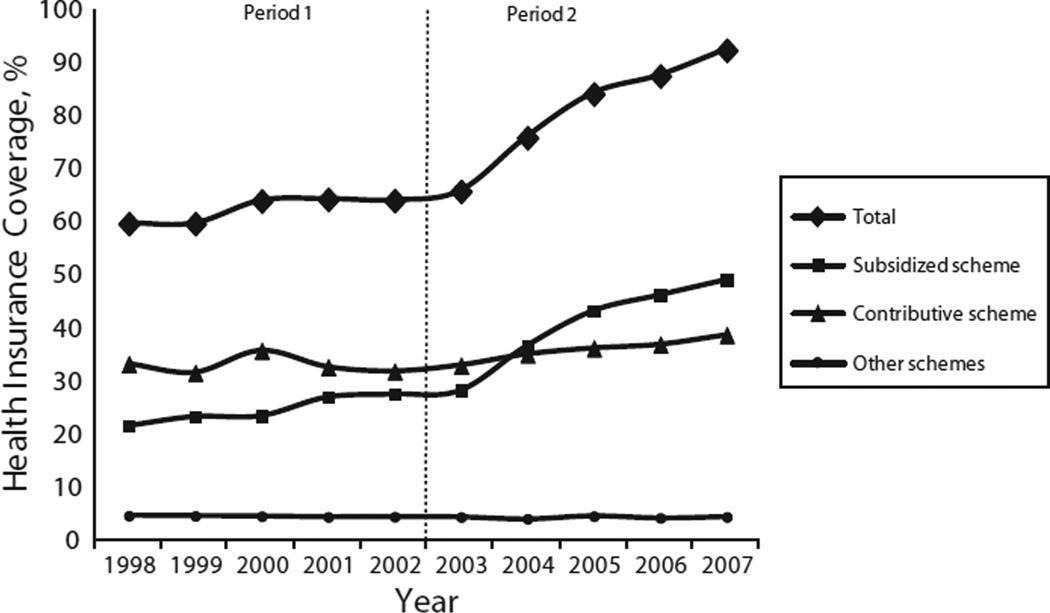
We examined whether expanding health insurance coverage is associated with trends in socioeconomic disparities in mortality in the aftermath of the health care reform in Colombia. Findings from this study are of potential interest to the United States and middle-income countries that have recently implemented reforms to achieve universal access. We hypothesized that expanding health insurance coverage will contribute to curbing unfavorable trends in mortality disparities. To assess the impact of this expansion, we examined trends in mortality disparities by educational level separately for 2 divergent periods. In 2002, a process of decentralization led to a sharp increase in resource allocation to the subsided scheme in regional areas.16 As a result, whereas in the period 1998–2002 there was a moderate increase in total health insurance coverage (coverage went from 59.8% in 1998 to 64.1% in 2002), thereafter total coverage increased rapidly from 65.9% (2003) to 92.5% (2007; Figure 1). This corresponds to a statistically significant increase of 5.1% per year (P < .001) in the period 2003–2007. As illustrated in Figure 1, this increase was driven by a particularly steep increase in affiliates to the subsidized scheme in 2003–2007 (15.1% per year; P < .001), as opposed to a much smaller increase in the period 1998–2002 (6.4% per year; P < .001), suggesting that it may have particularly reached the lower socioeconomic groups. The discrepancy in health insurance coverage trends between these 2 periods thus provides a natural experiment to examine the impact of health insurance coverage on socioeconomic disparities in mortality.
FIGURE 1.
Percentage of population with health insurance coverage: Colombia, 1998–2007.
Note. Other schemes include primarily members of the military and teacher and oil workers syndicate members.
Source. Annual reports of the Ministry of Health and Social Protection.5,17–19
Our specific aim was to evaluate to what extent increased health insurance coverage has contributed to diminishing socioeconomic inequalities in mortality in Colombia. If socioeconomic differences in mortality were responsive to increased health insurance coverage, we would expect a more favorable trend in socioeconomic differences in mortality during the second than the first period. If increased insurance coverage had no impact on socioeconomic disparities in mortality, we would expect similar trends in socioeconomic disparities in mortality between the 2 periods.
METHODS
Data on deaths came from the national statistics agency, which collects and harmonizes data on all deaths from all regions based on international guidelines. Causes of death were coded according to the International Classification of Diseases (ICD-10).20 We focused on total mortality and mortality from cardiovascular diseases (CVDs), which is the major cause of death in Colombia and partly reflects changes in lifestyle associated with the epidemiological transition.21 We defined CVD as codes I00 to I99 (Chapter IX, ICD-10).
For all deceased individuals (633 905 deaths), data were recorded on gender, age of death, and educational level. Data on age and gender were available for more than 99% of all deaths, and data on educational level was missing for approximately a third of deceased cases. We used multiple imputation methods as developed by Raghunathan et al.22 and implemented in SAS version 9.2 through the IMPUTE procedure (SAS Institute, Cary, NC) to impute educational level for these individuals. This was done to avoid bias because of the potentially higher rates of missing education for lower-educated individuals, and to minimize the potential for numerator–denominator bias.23,24 In short, this procedure fits a sequence of regression models and draws values from the corresponding predictive distributions. We applied the sequential regression procedure based on a model that included gender, region, age, andmarital status as covariates. Full details on the procedure are available elsewhere.22
We restricted the sample to ages 25 to 64 years because our interest was on avoidable mortality at adult age. In addition, data on educational level from death registries has been shown to be unreliable at ages 65 years and older, potentially leading to biased estimates of differences in mortality by education.23
We obtained data on midyear population counts with the following procedure: First, we extracted data on the proportion of individuals in each educational level from the International Institute of Applied System Analysis and the Vienna Institute of Demography of the Austrian Academy of Sciences (IIASA/VID) database.25 This database contains information on the distribution of education for every 5-year age group, gender, and year combinations every 5 years for the period 1970 through 2010, obtained from census, national surveys, and demographic projections for 120 countries. Second, we obtained data on yearly population counts for the entire population in Colombia from census and statistical projections from the national statistical office. Third, we estimated the yearly population in each educational group by multiplying the proportion of individuals in each educational category obtained from the IIASA/ VID database by population counts from national census and statistical projections. The IIASA/VID database contained distributions of education every 5 years only. Therefore, we performed demographic projections to obtain population counts for years between every lustrum by using the demographic Software Population Analysis Spreadsheets (PAS).26
We then combined data on population counts with data on deaths to obtain a complete database of mortality by educational level. We reclassified national educational levels into 3 categories based on highest educational attainment. These levels corresponded approximately to the following US education system categories (in reference to the highest level attained): (1) primary (elementary or primary school), (2) secondary (high-school diploma), and (3) tertiary education (postsecondary education after high school including college and university).
We first calculated age-standardized mortality rates by educational level, gender, and year by using the World Health population of 199727 as reference. Subsequently, we implemented separate Poisson regression models with number of deaths as dependent variable and the natural log of person-years as offset variable, incorporating age and educational level as independent variables. We used Poisson regression because data were aggregated as counts of deaths per population, and because death counts followed a Poisson probability distribution.
First, to assess mortality trends by educational level, we estimated the annual percent change (APC) in mortality based on a Poisson model that incorporated an interaction between educational level and year. The APC is the average rate of change in the mortality rate per year in a given time frame (how quickly mortality has increased or decreased each year over a period of years).28 It is presented as a percentage, such as a 1% per year increase. A negative APC describes a decreasing mortality trend, whereas a positive APC describes an increasing mortality trend.
At a second stage, we estimated 2 complementary measures of disparities separately for the periods 1998–2002 and 2003–2007. We started by estimating the rate ratio (RR) of mortality by educational level, which compared the mortality of all educational groups to the mortality in the tertiary education group. Changes in the RR over time result from changes in both risks and the distribution of educational level.29 Therefore, to assess changes in disparities with control for changes in the educational distribution, we estimated the relative index of inequality (RII), a widely used measure to examine trends in health disparities.30 The RII is a regression-based measure that takes into account the size of each educational group by regressing mortality on the midpoint of the cumulative distribution of education.29 The RII can be interpreted as the ratio of the mortality rate of those at the bottom of the distribution of education compared with the rate of those at the top of the distribution of education.29 An increase in the RII indicates an increase in disparities in mortality across educational level. Further details on the RII are available elsewhere.29
To estimate whether changes in disparities by educational level differed between the period of moderate increase (1998–2002) and the period of rapid increase in health insurance coverage (2003–2007), we incorporated interaction terms between educational level and year within each period. A significant positive interaction indicated a significant increase in disparities in mortality by education. To assess whether yearly changes in disparities between the 2 periods were statistically significant, we implemented a single model that incorporated a 3-way interaction among period, year, and educational level. A significant interaction was interpreted as indication of an effect of health insurance coverage on disparities in mortality by educational level.
We carried out all regression analyses in each of the 5 multiple databases generated by the multiple imputation process. Because results were nearly identical for all imputations, we used standard techniques as implemented in the PROC MIANALYZE procedure in SAS to combine estimates from all databases and adjust standard errors to account for uncertainty in the imputation.31 This procedure reads the parameter estimates and associated covariance matrix for each imputed data set, and then derives valid multivariate inferences for these parameters. This allows for valid statistical inference that appropriately reflects uncertainty attributable to missing values.31
RESULTS
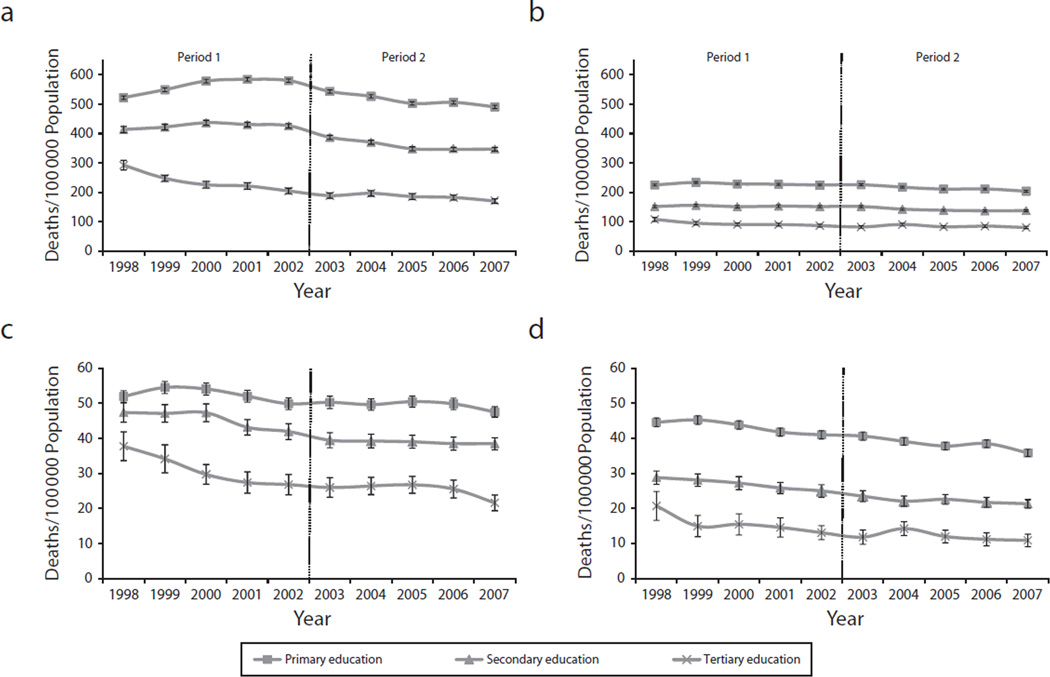
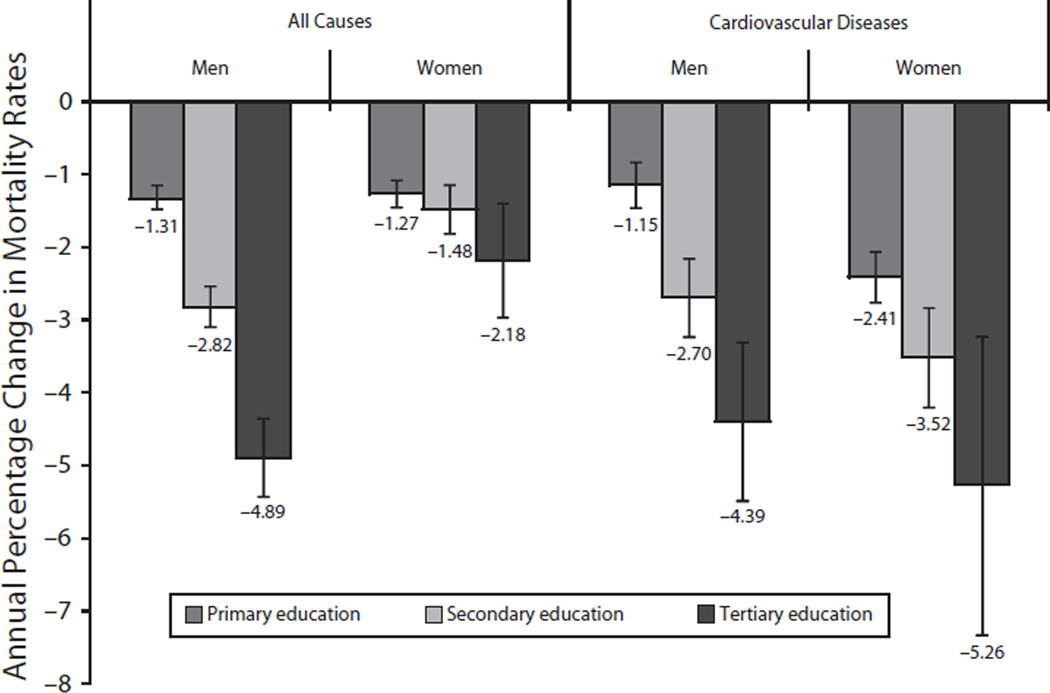
Table 1 summarizes data on deaths and midyear population (person-years). There was a total of 633 933 deaths over the period 1998–2007. Imputation of education was not possible in 6.4% of deceased cases, leaving a total of 593 173 deaths for analysis. Total mortality rates were 537.8 deaths per 100 000 population among men and 281.6 among women, and CVD rates were 115.5 and 78.0, respectively. From 1998 to 2007, men and women with only primary education or less schooling had higher mortality rates than their higher-educated counterparts (Figure 2). In all educational groups, mortality from both total and CVD declined over the study period. However, Figure 3 shows that men and women with tertiary education experienced a faster decline in mortality than their less-educated counterparts. The average APC in mortality according to educational level was –4.89% (95% CI = –5.35, –4.36) in men and –2.18 (95% CI = –2.96, –1.39) in women with tertiary education, compared with –1.31% (95% CI = –1.48, –1.15) in men and –1.27% (95% CI = –1.45, –1.08) in women with only primary education. We observed similar disparities for CVD mortality.
TABLE 1.
Descriptive Statistics Before and After Expanded Health Care Insurance: Colombia, 1998–2007
| Period 1: 1998–2002 |
Period 2: 2003–2007 |
|||||||
|---|---|---|---|---|---|---|---|---|
| Person-Years | % | CVD deaths |
All Deaths | Person-Years | % | CVD deaths |
All Deaths | |
| Age groups, y | ||||||||
| 25–29 | 15 681 229 | 18.3 | 1286 | 41 610 | 16 790 652 | 17.7 | 1254 | 35 447 |
| 30–34 | 15 295 439 | 17.9 | 1889 | 37 838 | 15 170 633 | 16.0 | 1676 | 31 311 |
| 35–39 | 14 113 107 | 16.5 | 3046 | 36 466 | 14 845 056 | 15.7 | 2736 | 31 442 |
| 40–44 | 11 924 028 | 14.0 | 5194 | 35 185 | 13 808 189 | 14.6 | 4712 | 32 899 |
| 45–49 | 9 636 969 | 11.3 | 7671 | 35 342 | 11 662 310 | 12.3 | 7876 | 36 109 |
| 50–54 | 7 672 753 | 9.0 | 10 436 | 37 543 | 9 383 845 | 9.9 | 11 112 | 41 478 |
| 55–59 | 6 053 379 | 7.1 | 13 451 | 41 850 | 7 399 564 | 7.8 | 14 522 | 46 499 |
| 60–64 | 5 090 243 | 6.0 | 20 063 | 56 203 | 5 732 546 | 6.0 | 19 445 | 56 684 |
| Gender | ||||||||
| Men | 41 329 276 | 48.4 | 5868 | 218 802 | 45 764 081 | 48.3 | 37 156 | 206 225 |
| Women | 44 137 871 | 51.6 | 27 168 | 103 149 | 49 028 714 | 51.7 | 26 177 | 105 578 |
| Missing | … | … | 86 | … | … | 66 | ||
| Educational attainmenta | ||||||||
| Primary | 42 062 366 | 49.2 | 44 541 | 197 754 | 41 221 063 | 43.5 | 42 584 | 184 632 |
| Secondary | 32 349 705 | 37.9 | 13 393 | 84 445 | 38 739 709 | 40.9 | 15 350 | 91 178 |
| Tertiary | 11 055 076 | 12.9 | 3014 | 16 493 | 14 832 022 | 15.6 | 3718 | 18 671 |
| Missing | … | 2088 | 23 345 | … | 1681 | 17 388 | ||
| Total | 85 467 147 | 63 036 | 322 037 | 94 792 795 | 63 333 | 311 869 | ||
Note. CVD = cardiovascular disease.
Educational attainment values registered after final imputation: primary = elementary or primary school; secondary = high-school diploma; tertiary = postsecondary education after high school including college and university.
FIGURE 2.
Age-standardized rates of mortality at ages 25–64 years according to educational level from (a) all-causes among men, (b) all-causes among women, (c) CVD among men, and (d) CVD among women: Colombia, 1998–2007.
Note. CVD = cardiovascular disease; Primary = elementary or primary school; secondary = high-school diploma; tertiary = postsecondary education after high school including college and university.
FIGURE 3.
Annual percentage change in mortality rates at ages 30–64 years according to educational level: Colombia, 1998–2007.
Note. Primary = elementary or primary school; secondary = high-school diploma; tertiary = postsecondary education after high school including college and university. Annual percent change comes from separate Poisson regression models for men and women that control for age, year, and education.
Table 2 summarizes the RR (model 1) and RII (model 2) separately for the periods 1998–2002 and 2003–2007. Both measures suggest that disparities by education in total and CVD mortalitywidened over the study period in bothmen and women. For total mortality, the RII increased from 2.59 (95% CI = 2.52, 2.67) in 1998– 2002 to 3.07 (95% CI = 2.99, 3.15) in 2003– 2007 in men, and from 2.86 (95% CI = 2.77, 2.95) in 1998–2002 to 3.12 (95% CI = 3.03, 3.21) in 2003–2007 in women. There was a particularly steep increase in disparities in CVD mortality in women, which increased from 3.33 (95% CI = 3.10, 3.59) in 1998–2002 to 4.20 (95% CI = 3.94, 4.47) in 2003–2007.
TABLE 2.
Relative Disparities in Mortality by Educational Level as Measured by the Rate Ratio and the Relative Index of Inequality for Men and Women Aged 25–64 Years: Colombia, 1998–2002 and 2003–2007
| Men |
Women |
|||
|---|---|---|---|---|
| 1998–2002, RR (95% CI) |
2003–2007, RR (95% CI) |
1998–2002, RR (95% CI) |
2003–2007, RR (95% CI) |
|
| All-cause mortality | ||||
| Model 1a | ||||
| Tertiary education (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Secondary education | 1.80 (1.76, 1.84) | 1.96 (1.91, 2.00) | 1.63 (1.56, 1.70) | 1.69 (1.64, 1.74) |
| Primary education | 2.41 (2.36, 2.47) | 2.76 (2.68, 2.83) | 2.43 (2.34, 2.52) | 2.56 (2.49, 2.63) |
| Year | 0.92 (0.91, 0.94) | 0.97 (0.96, 0.99) | 0.95 (0.93, 0.98) | 0.99 (0.97, 1.01) |
| Secondary × year | 1.09 (1.07, 1.11) | 1.00 (0.98, 1.02) | 1.04 (1.02, 1.07) | 0.99 (0.97, 1.01) |
| Primary × year | 1.11 (1.09, 1.13) | 1.00 (0.99, 1.02) | 1.04 (1.02, 1.07) | 0.99 (0.97, 1.01) |
| Model 2 | ||||
| Relative index of inequality | 2.59 (2.52, 2.67) | 3.07 (2.99, 3.15) | 2.86 (2.77, 2.95) | 3.12 (3.03, 3.21) |
| Year | 0.95 (0.94, 0.96) | 0.96 (0.95, 0.97) | 0.96 (0.95, 0.98) | 0.97 (0.96, 0.99) |
| Relative index of inequality × year | 1.11 (1.09, 1.13) | 1.01 (1.00, 1.03) | 1.04 (1.02, 1.06) | 1.00 (0.98, 1.02) |
| Cardiovascular disease mortality | ||||
| Model 1a | ||||
| Tertiary education (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Secondary education | 1.47 (1.40, 1.54) | 1.55 (1.47, 1.62) | 1.73 (1.56, 1.90) | 1.85 (1.69, 2.03) |
| Primary education | 1.70 (1.63, 1.78) | 1.97 (1.88, 2.05) | 2.76 (2.50, 3.05) | 3.20 (2.96, 3.46) |
| Year | 0.91 (0.88, 0.96) | 0.96 (0.92, 1.00) | 0.91 (0.86, 0.97) | 0.96 (0.91, 1.01) |
| Secondary × year | 1.06 (1.01, 1.11) | 1.03 (0.99, 1.08) | 1.06 (0.99, 1.12) | 1.02 (0.97, 1.08) |
| Primary × year | 1.08 (1.03, 1.13) | 1.03 (0.99, 1.08) | 1.07 (1.01, 1.14) | 1.02 (0.96, 1.07) |
| Model 2 | ||||
| Relative index of inequality | 1.75 (1.66, 1.84) | 2.18 (2.07, 2.29) | 3.33 (3.10, 3.59) | 4.20 (3.94, 4.47) |
| Year | 0.92 (0.90, 0.95) | 0.97 (0.95, 1.00) | 0.92 (0.89, 0.95) | 0.96 (0.93, 0.99) |
| Relative index of inequality × year | 1.09 (1.04, 1.14) | 1.02 (0.98, 1.06) | 1.07 (1.02, 1.12) | 1.01 (0.96, 1.05) |
Note. CI = confidence interval; RR = rate ratio. Table presents estimates that combine results from 5 databases generated by multiple imputation, appropriately reflecting uncertainty attributable to missing values. Model 1 shows RRs from a model that includes as independent variables educational level, age in 5-year age categories, a linear year trend, and an interaction between educational level and the linear year trend. Model 2 estimates the relative index of inequality based on a regression of mortality on the midpoint of the cumulative distribution of education, age in 5-year age categories, a linear year trend, and an interaction between the midpoint of the cumulative distribution of education and the linear year trend. It can be interpreted as the ratio of the mortality rate of those at the bottom of the distribution of education compared with the rate of those at the top of the distribution of education. An increase in the relative index of inequality indicates an increase in disparities in mortality by educational level.29
Primary = elementary or primary school; secondary = high-school diploma; tertiary = postsecondary education after high school including college and university.
As shown in Table 2, disparities in mortality widened significantly less in the period of accelerated increase in health insurance coverage (2003–2007) than in the period of moderate increase in coverage (1998–2002). The RII for total mortality increased by 11% (RR = 1.11; 95% CI = 1.09, 1.13) in men and 4% in women (RR = 1.04; 95% CI = 1.02, 1.06) per year in the period 1998–2002, whereas it increased by only 1% (RR = 1.01; 95% CI = 1.00, 1.03) in men and remained stable among women (RR = 1.00; 95%CI = 0.98, 1.02) in the period 2003–2007. Similarly, the RII for CVD mortality increased by 9% in men and 7% in women in 1998–2002, whereas there was no significant change in disparities in the period 2003–2007. The interaction between the RII and year was always significant for the period 1998–2002, whereas in the second period, it was only significant for total mortality in men.
DISCUSSION
Our analyses suggest that there are large disparities in mortality by educational level in Colombia, which widened significantly during the post–health care reform period owing to larger decreases in mortality among higher-educated persons. However, socioeconomic disparities in mortality widened significantly less during a period of rapid expansion in insurance coverage, compared with a period of moderate increase in coverage. Findings suggest that expanding insurance coverage may not eliminate disparities in the short term, but over the long run, it may partly contribute to curbing widening disparities in mortality.
Interpretation of Results
There is controversy on the impact of insurance coverage on health outcomes and health disparities in Colombia,3,6–9,13 the United States,1,2,10,32 and elsewhere.33–36 Although some studies have suggested that the subsidized scheme led to improvements in maternal and children’s health,6 little is known about impact on adult outcomes and mortality. The slowdown in the rate of increase in disparities in adult mortality observed in our study during the period of rapid increase in coverage may have been the result of increased access to care.7 Those insured in the subsidized scheme were approximately 40% more likely to have used outpatient visits in the past year than were the uninsured, half as likely to have experienced barriers to access when needing care,6 and less likely to have experienced catastrophic spending.6 In addition, studies from other countries have suggested that increased coverage may contribute toward reducing disparities in health care utilization. A study in Taiwan, which in 1995 implemented a similar insurance-based reform, found that increased coverage significantly increased physician visits in all income groups,33 but middle and lower household income groups benefited more than their higher-income counterparts.33
Despite almost universal coverage, lowincome groups still face more barriers in access to care than their higher-income counterparts. 13 Following a large health care reform that increased coverage in Thailand, large disparities in health care utilization remained.34 Several studies have shown that even European countries with universal health care coverage have large disparities in mortality that have persisted and increased during the past decades.35–37 A possible explanation of our results is the persistence of disparities in behavioral determinants of mortality uninfluenced by access to care. In 2003, the prevalence of smoking among lower-educated Colombians was 41%, compared with 26% in those with college education.38 Similarly, a recent study estimated that 26% of lower-educated Colombians aged 25 to 50 years have at least a risk factor for CVD, as opposed to only 5.9% in those with a university degree.39
Despite potential beneficial effects, several studies support the hypothesis that health insurance is only 1 among many determinants of disparities in health and mortality.2,32 Disparities in behavioral risk factors, psychosocial wellbeing, parental socioeconomic status, and childhood living circumstance may all contribute to disparities in mortality.40 In addition, health care reform may not have been sufficient to curb autonomous trends in chronic disease risk factors resulting from secular lifestyle changes toward more sedentary lifestyles and higher obesity.21 Socioeconomic disparities in distal determinants of mortality such as poverty, living conditions, and working conditions may also have contributed to disparities. The gap in earnings among higher- and lower-educated workers has grown during the past decades.41 It is estimated that 59% of lower-educated households live in poverty, as opposed to only 4.1% among their higher-educated counterparts. 42 Among households in the highest income quintile, 96% have access to water services as opposed to 75% in the lowest income quintile. Similarly, 90% of households in the highest income quintile have access to drainage services, in contrast to 54% in the lowest income quintile.43 The persistence of disparities in these social and behavioral determinants of mortality may explain why disparities persist even after universal access to care has been achieved.
Limitations of the Study
Despite several strengths, some limitations should be considered in our study. Data on mortality came from mortality registries, whereas data on the population distribution by education came from census and demographic projections. This may have led to the so-called numerator– denominator bias, which generally results in an overestimation of disparities.23,24 Another limitation is that, for some years, data on population size came from demographic projections combined with distributions of education from surveys. To assess the impact of this potential bias, we experimented with different education distributions from multiple data sources.25,44,45 Overall, although distributions and absolute rates sometimes differed, the overall trends observed in our study were robust to different assumptions on the distribution of education.
Education was missing for 38.4% of death records in the first period and 29.9% of records in the second period. This may have led to underestimation of disparities, as missing values are likely to be more common in less-educated and higher-mortality areas. However, we imputed values for individuals with missing education based on a rich set of variables available for most deceased individuals that strongly predicted education, minimizing the potential impact of this source of bias. Overall, because of relatively small changes in the proportion of missing over time, these trends may generally lead to underestimation of disparities, but they are unlikely to account for differences in trends in disparities over the 2 periods assessed.
Our study was based on a comparison of trends in socioeconomic disparities in mortality between 2 periods.We assumed a common trend in factors other than coverage between the first and second periods. In preliminary analyses, we found that our results were robust to adjustment for several national-level variables such as gross domestic product growth and employment rates, which showed similar trends in both periods. However, we cannot discard the possibility that other timevarying covariates contributed to trends in mortality. Most importantly, increased coverage may have occurred parallel to other changes in the health care system.4,6 Our results may therefore reflect not only the impact of increased coverage but also the impact of other aspects of the health care reform.
Conclusions
Socioeconomic disparities in mortality widened throughout the period 1998–2007, but they increased significantly less during a period of increased insurance coverage than during a period of moderate increase in coverage. The reform may take several decades to have a meaningful impact on the mortality of disadvantaged populations. Therefore, future studies should closely monitor changes in disparities in mortality in the coming years. Our findings underscore the importance of understanding the impact of determinants other than health care in explaining disparities in mortality, including lifestyle, as well as the living and working conditions of the poor. Given trends in these determinants, increasing insurance coverage may not be sufficient to eliminate disparities, but our findings suggest that it may contribute to curb increasing trends in disparities in mortality.
Acknowledgments
M. Avendano was supported by a Starting Researcher Grant from the European Research Council (grant 263684), a fellowship from Erasmus University Rotterdam, and a grant from the National Institute of Ageing (R01AG037398-01, R01AG037398-02). I. Arroyave was supported by the European Union Erasmus Mundus Partnerships Programme Erasmus-Columbus and by the Programme Enlazamundos (Municipality of Medellin and Centre for Science and Technology of Antioquia).
Footnotes
Contributors
I. Arroyave was the leading author and developed the article idea, constructed and analyzed the data set, and wrote drafts of article. D. Cardona contributed to the quantitative analysis and commented on all drafts of the article. A. Burdorf contributed to interpretation of results and commented on all drafts. M. Avendano analyzed data, wrote sections of the article, and contributed to the coordination of all steps of the analysis and article preparation.
Human Participant Protection
This article is based on secondary analysis of data on deaths and population counts in aggregate form made publically available by the National Statistics Office in Colombia. Ethical approval for this study was not required.
Contributor Information
Ivan Arroyave, Erasmus University Medical Center, Rotterdam, The Netherlands; the Public Health Observatory, Faculty of Medicine, Universidad CES, Medellin, Colombia; and the Epidemiology Research Group, National School of Public Health, Universidad de Antioquia, Medellin..
Doris Cardona, Group of Demographic and Statistics Research, Faculty of Medicine, Universidad CES..
Alex Burdorf, Occupational Health and Social Determinants of Health sections, Public Health Department, Erasmus Medical Center..
Mauricio Avendano, London School of Economics and Political Science, Department of Social Policy, the Department of Public Health of the Erasmus University Medical Center, and the Department of Society, Human Development and Health, Harvard School of Public Health, Boston, MA..
References
- 1.Qin X, Liu GG. Does the US health care safety net discourage private insurance coverage? Eur J Health Econ. 2012 doi: 10.1007/s10198-012-0389-4. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 2.Franks P, Clancy CM, Gold MR. Health insurance and mortality: evidence from a national cohort. JAMA. 1993;270(6):737–741. [PubMed] [Google Scholar]
- 3.Calderón CAA, Botero JC, Bolaños JO, Martínez RR. The Colombian healthcare system: 20 years of achievements and problems [in Spanish] Cien Saude Colet. 2011;16(6):2817–2828. doi: 10.1590/s1413-81232011000600020. [DOI] [PubMed] [Google Scholar]
- 4.Restrepo Zea JH. Health insurance in Colombia: universal coverage? [in Spanish] Revista Gerencia y Políticas de Salud. 2002;(2):25–40. [Google Scholar]
- 5.Republica de Colombia. Activity Report 2009–2010-Report of Quadrennium 2006–2010 to the Honourable Congress of the Republic [in Spanish] 1st ed. Bogotá, Colombia: Ministerio de la Protección Social; 2010. [Google Scholar]
- 6.Giedion U, Uribe MV. Colombia’s universal health insurance system. Health Aff (Millwood) 2009;28(3):853–863. doi: 10.1377/hlthaff.28.3.853. [DOI] [PubMed] [Google Scholar]
- 7.Ruiz F, Amaya L, Venegas S. Progressive segmented health insurance: Colombian health reform and access to health services. Health Econ. 2007;16(1):3–18. doi: 10.1002/hec.1147. [DOI] [PubMed] [Google Scholar]
- 8.Abadia CE, Oviedo DG. Bureaucratic itineraries in Colombia. A theoretical and methodological tool to assess managed-care health care systems. Soc Sci Med. 2009;68(6):1153–1160. doi: 10.1016/j.socscimed.2008.12.049. [DOI] [PubMed] [Google Scholar]
- 9.De Groote T, De Paepe P, Unger J-P. Colombia: in vivo test of health sector privatization in the developing world. Int J Health Serv. 2005;35(1):125–141. doi: 10.2190/LH52-5FCB-4XDE-76CW. [DOI] [PubMed] [Google Scholar]
- 10.Milstein B, Homer J, Hirsch G. Analyzing national health reform strategies with a dynamic simulation model. Am J Public Health. 2010;100(5):811–819. doi: 10.2105/AJPH.2009.174490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knaul FM, González-Pier E, Gómez-Dantés O, et al. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet. 2012;380(9849):1259–1279. doi: 10.1016/S0140-6736(12)61068-X. [DOI] [PubMed] [Google Scholar]
- 12.Patcharanarumol W, Tangcharoensathien V, Limwattananon S, et al. Why and how did Thailand achieve good health at low cost? In: Balabanova D, McKee M, Mills A, editors. Good Health at Low Cost 25 Years On. What Makes a Successful Health System? London, England: London School of Hygiene & Tropical Medicine; 2011. pp. 193–223. [Google Scholar]
- 13.Alvarez LS, Salmon JW, Swartzman D. The Colombian health insurance system and its effect on access to health care. Int J Health Serv. 2011;41(2):355–370. doi: 10.2190/HS.41.2.i. [DOI] [PubMed] [Google Scholar]
- 14.Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet. 2012;380(9845):917–923. doi: 10.1016/S0140-6736(12)61039-3. [DOI] [PubMed] [Google Scholar]
- 15.Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 16.Lozano I, Ramos J, Rincón H. Fiscal and Sectorial Effects of the Subnational Transfers Bill in Colombia [in Spanish] Bogotá, Colombia: Bancode laRepublica deColombia; 2007. [Google Scholar]
- 17.Republica de Colombia. Activity Report 1999–2000 to the Honourable Congress of the Republic [in Spanish] Bogotá, Colombia: Ministerio de la Salud; 2000. [Google Scholar]
- 18.Republica de Colombia. Activity Report 2000–2001 to the Honourable Congress of the Republic [in Spanish] 1st ed. Bogotá, Colombia: Ministerio de Salud; 2001. [Google Scholar]
- 19.Republica de Colombia. Report of Quadrennium 2002–2006 to the Honourable Congress of the Republic [in Spanish] 1st ed. Bogotá, Colombia: Ministerio de la Protección Social; 2006. [Google Scholar]
- 20.International Classification of Diseases-10. Geneva, Switzerland: World Health Organization; 2010. [Accessed February 1, 2012]. Available at: http://apps.who.int/classifications/icd10/browse/2010/en. [Google Scholar]
- 21.Stuckler D. Population causes and consequences of leading chronic diseases: a comparative analysis of prevailing explanations. Milbank Q. 2008;86(2):273–326. doi: 10.1111/j.1468-0009.2008.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raghunathan T, Lepkowski J, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27(1):85–95. [Google Scholar]
- 23.Kunst AEGF, Borgan JK, Costa G, et al. Socioeconomic inequalities in mortality. Methodological problems illustrated with three examples from Europe. Rev Epidemiol Sante Publique. 1998;46(6):467–479. [PubMed] [Google Scholar]
- 24.Kunst AE, Bos V, Andersen O, et al. Monitoring of trends in socioeconomic inequalities in mortality: experiences from a European project. Demogr Res. 2004;S2(9):229–254. [Google Scholar]
- 25.Vienna, Austria: International Institute of Applied System Analysis; Vienna Institute of Demography of the Austrian Academy of Sciences; 2010. Reconstruction of populations by age, sex and level of educational attainment for 120 countries for 1970–2000 using demographic back-projection methods: IVEP-1.0 [IIASA/VID education database] [Google Scholar]
- 26.Population Analysis System (PASEX spreadsheets) 2.04g ed. Washington, DC: US Census Bureau; 2011. [Google Scholar]
- 27.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Sstandard. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 28.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–3682. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44(6):757–771. doi: 10.1016/s0277-9536(96)00073-1. [DOI] [PubMed] [Google Scholar]
- 30.Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman ME. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area-socioeconomic position and race-ethnicity, 1992–2004. Am J Epidemiol. 2008;167(8):889–899. doi: 10.1093/aje/kwn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.User’sGuide SAS/STAT 9.2. Version 8. Cary, NC: SAS Institute Inc; 2008. TheMIANALYZE procedure; pp. 201–233. [Google Scholar]
- 32.Katz SJ, Hofer TP. Socioeconomic disparities in preventive care persist despite universal coverage. Breast and cervical cancer screening in Ontario and the United States. JAMA. 1994;272(7):530–534. [PubMed] [Google Scholar]
- 33.Cheng SH, Chiang TL. The effect of universal health insurance on health care utilization in Taiwan. JAMA. 1997;278(2):89–93. doi: 10.1001/jama.278.2.89. [DOI] [PubMed] [Google Scholar]
- 34.Suraratdecha C, Saithanu S, Tangcharoensathien V. Is universal coverage a solution for disparities in health care?: findings from three low-income provinces of Thailand. Health Policy. 2005;73(3):272–284. doi: 10.1016/j.healthpol.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 35.Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358(23):2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 36.Stirbu I, Kunst AE, Bopp M, et al. Educational inequalities in avoidable mortality in Europe. J Epidemiol Community Health. 2010;64(10):913–920. doi: 10.1136/jech.2008.081737. [DOI] [PubMed] [Google Scholar]
- 37.Avendano M, Kunst AE, Huisman M, et al. Socioeconomic status and ischaemic heart disease mortality in 10 western European populations during the 1990s. Heart. 2006;92(4):461–467. doi: 10.1136/hrt.2005.065532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Storr CL, Cheng H, Posada-Villa J, Aguilar-Gaxiola S, Anthony JC. Adult smokers in Colombia: who isn’t giving it up? Addict Behav. 2008;33(3):412–421. doi: 10.1016/j.addbeh.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patiño-Villada FA, Arango-Vélez EF, Quintero-Velásquez MA, Arenas-Sosa MM. Cardiovascular risk factors in an urban Colombia population [in Spanish] Rev Salud Publica (Bogota) 2011;13:433–445. [PubMed] [Google Scholar]
- 40.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712–722. doi: 10.1038/nrcardio.2009.163. [DOI] [PubMed] [Google Scholar]
- 41.Arango LE, Posada CE, Uribe JD. Changes in the Structure of Urban Wages in Colombia (1984–2000) [in Spanish] Bogotá, Colombia: Banco de la República; 2004. [Google Scholar]
- 42.Núñez J, Ramírez JC, Cuesta L. Determinants of Poverty in Colombia, 1996–2004 [in Spanish] Bogotá, Colombia: Universidad de Los Andes; 2005. [Google Scholar]
- 43.Acting on the Future: Breaking the Intergenerational Transmission of Inequality. San José, Costa Rica: United Nations Development Programme; 2010. [Google Scholar]
- 44.World Development Indicators. Washington, DC: World Bank; 2011. [Google Scholar]
- 45.Barro RJ, Lee J-W. A New Data Set of Educational Attainment in the World, 1950–2010. Cambridge, MA: National Bureau of Economic Research; 2010. [Google Scholar]