Abstract
Background
A challenge for the widespread dissemination of Internet-based programs designed to produce weight maintenance/loss in defined (high school) populations is to adapt them to local needs and interests, whereas demonstrating effectiveness and salience for both universal and targeted populations.
Objective
The objective of this study is to examine the feasibility of providing an inexpensive, Internet-based universal (healthy weight regulation) and targeted (weight maintenance/loss) health program to all ninth-grade students in a high school serving a lower socioecnomic status, diverse population.
Design
A total of 118 normal-weight and 64 overweight/obese students in the same ninth-grade class completed a baseline screen and were allocated to a healthy weight regulation program or a weight-loss maintenance program. Both groups simultaneously received a 10-week Internet-based intervention. Program implementation required minimal teacher time. Measurement included self-reported fruit, vegetable and high-fat/-calorie food consumption, self-reported change in body mass index (BMI), weight and shape concerns, as well as program engagement.
Results
The program was successfully implemented in nine classes, with minimal help from the investigators. There was a significant increase in self-reported consumption of fruits and vegetables (P=0.001). There was a significant reduction in self-reported BMI in the overweight/obese group (P=0.001). Students found the program helpful and engaging. There was a significant reduction in weight and shape concerns in the high-risk female students, consistent with a reduced risk for the development of an eating disorder. Providing a universal and targeted online healthy weight regulation program to ninth-grade students is feasible and inexpensive. The results suggest the program can serve as ‘core’ for future studies using adaptive, continuous quality-improvement designs.
Introduction
The prevention of obesity should start early, but programs still need to address the high percentage of older students who are overweight or obese when they enter high school. In 2009, about 29% of high-school students were overweight or obese (http://www.cdc.gov/healthyyouth/yrbs/pdf/us_obesity_trend_yrbs.pdf). During high school, students develop a number of life-long habits related to exercise and nutrition, and unfortunately, data suggest that few students are offered physical activity programs, particularly after ninth grade. Late adolescence is a time when students are more independent and begin to have more agency over lifestyle choices.
The Internet is an ideal medium to reach the adolescent population. Recent studies have demonstrated that computer-based approaches are feasible and can lead to self-reporting of behavior changes and weight loss in children and adolescents.1, 2 However, few studies have shown that Internet-based interventions can reduce/maintain weight in older overweight adolescents, and no studies have examined the use of such programs in high schools in spite of the huge need to provide weight management skills to this population.
In addition, a number of other issues need to be addressed for widespread dissemination of Internet-based programs.3 Glasgow et al.4 have recently noted the limitations of the traditional efficacy to effectiveness model as applied to public health problems and argue that a model likely to have greater reach would use a set of programs adapted to defined populations. In an ideal world, a program reaching a defined population would be effective, but would also evolve to incorporate new interventions and activities of potential benefit. Connecting effective individual-focused intervention-based programs with social, community, school, family and environment activities is even more important for school-based health promotion activities. In the research model, we propose that a core program be developed first using traditional evidence-based pilot studies and a comprehensive needs assessment. Such a program would be tailored to individual student-learning styles, interests and needs. The software would permit rapid changes based on individual and group outcomes and the incorporation of new activities such as games. Once efficacy has been established, the program would be offered to a variety of schools and further adapted on an individual and school level. These studies would use the classroom as the unit of analysis. The adaptations would address potentially important demographic, learning and other issues, and this set of programs would presumably increase the appeal of the program. Once a set of adapted core programs have been developed, a next step might be to examine how outcomes can be enhanced by incorporating environmental and other activities at the school level.
Although program revision and adaptation is a relatively straightforward process, demonstrating that the adapted programs are effective is more problematic. Traditional, large controlled effectiveness studies require ‘fixed’ interventions, and usually study only one intervention. It has not been possible to use this traditional efficacy-effectiveness model in which a set of related interventions needs to be studied. Fortunately, new trial designs allow for the examination of the efficacy of programs adapted to targeted populations. For instance, factorial designs and adaptive designs with continuous quality improvement have been proposed as a way to examine a number of variations of programs simultaneously.5, 6, 7 However, such designs require large numbers of subjects, followed up with standardized assessments and replicable, easily implemented interventions. For instance, as many as 10 schools, 50 classes and 20 000 students may be necessary to examine the efficacy of 6 or 7 variations of a program.
The purpose of this study was to determine the feasibility of providing a universal and targeted healthy weight regulation program to all ninth-grade students in the same high school. Feasibility was determined on the basis that the schools could provide the program to all students with minimal effort and cost, that short-term results would suggest that the program was beneficial, and that students would find the program engaging. We also wanted to identify potential barriers to wide-scale dissemination that need to be resolved.
Methods
Letters were sent to 12 high schools in the San Francisco Bay Area Peninsula, offering the use of the StayingFit program (described below), of which 5 expressed interest. One high school was selected to participate based on the diversity of the student body (49% Hispanic, 37% White, 7% Asian, 6% African American, 2% other) and proximity to the investigators.
Measures
Body mass index (BMI) data, obtained by the schools using digital scales and wall measures of height, were used to determine which program track (universal healthy weight regulation or overweight/maintenance) was recommended to students. Nutrition and self-reported physical activity were assessed using selected items from the Center for Disease Control Youth Risk Behavior Survey,8 and weight and shape concerns were assessed using the Weight and Shape Concerns Scale.9 Process measures included post-session assessment of knowledge, intention, efficacy and engagement (helpful, interesting, fun). Students also reported food consumption, activity and meal-size information on weekly logs.
Intervention
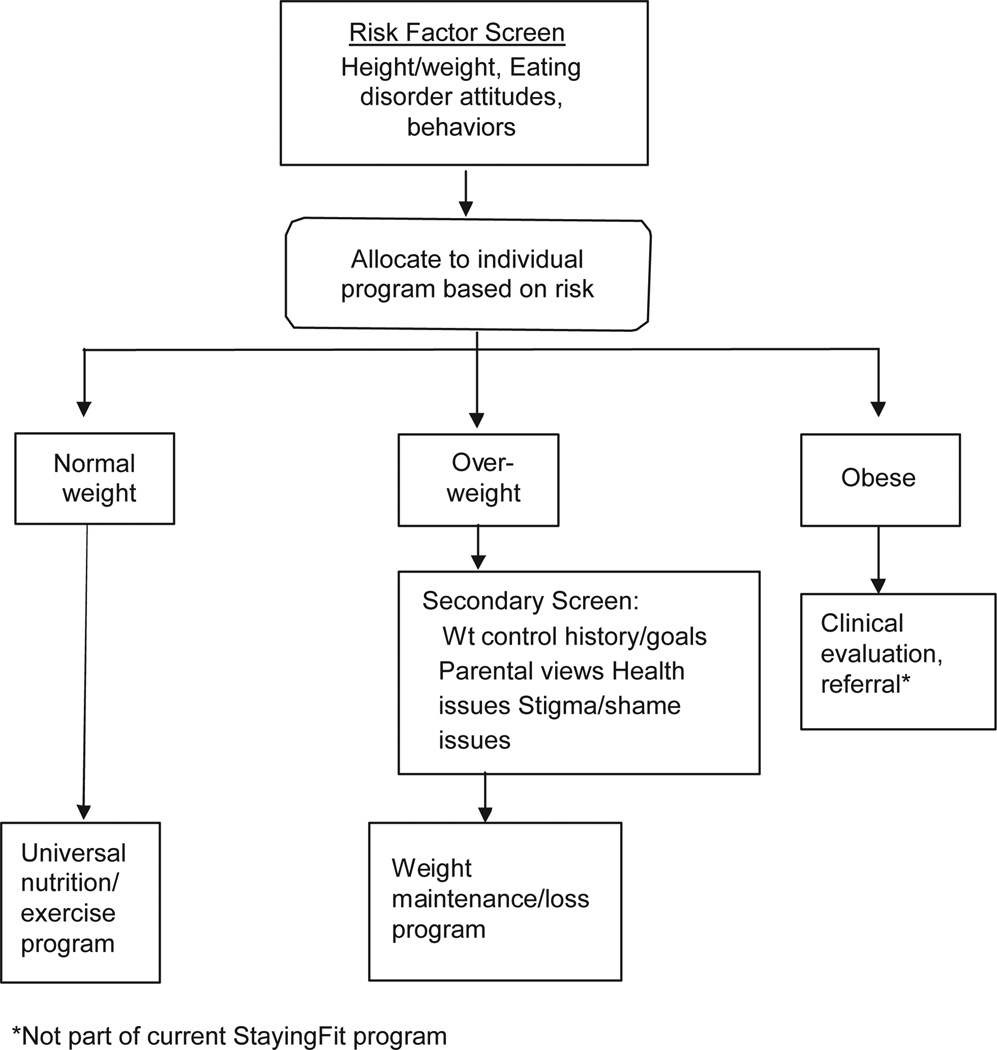
StayingFit is a 10-week, two-track program emphasizing healthy habits and positive body image. Students above the 85th percentile BMI for their age and sex are given StayingFit weight maintenance. Students below the 85th percentile BMI for their age and sex are given StayingFit general (see Figure 1). The interventions are based on a number of previous efficacy studies.10, 11, 12, 13, 14, 15, 16 The weight maintenance intervention incorporates cognitive behavioral principles,17 adolescent weight-loss interventions,18 and hunger and satiety awareness skills. The intervention combines psychoeducation and behavioral interventions, such as self-monitoring, goal setting, stimulus control and appetite awareness, and introduces emotion regulation skills. The program introduces a new topic related to healthy eating, physical activity, binge eating and weight loss/maintenance each week, with content from previous weeks remaining accessible at any time. The general track focuses on developing healthy eating and activity habits, and includes information about maintaining a positive body image. The program also included an asynchronous discussion group moderated by a research assistant. Early versions of the program underwent extensive pilot testing. The content of the program was designed to cover the State of California ninth-grade nutrition standards and to support students passing the Fitnessgram.19 Text was written at a sixth- to ninth-grade level.
Figure 1.
Universal, targeted and indicate eating disorders/weight management program for high school students.
HealthmunkLLC authored the software
All program content was put on masters to allow for rapid, inexpensive program revision.
Results
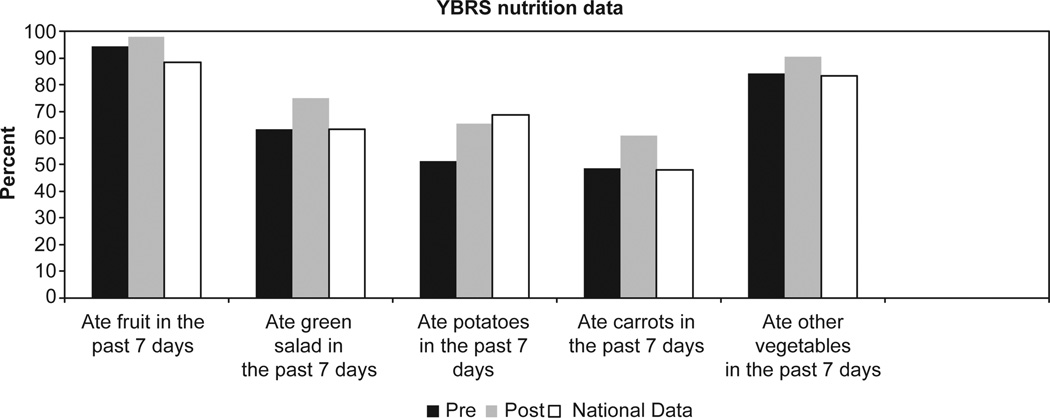
In all, 53% (191/360) of students provided parental consent. Of these, 118 were allocated to the healthy weight regulation program and 64 to the weight maintenance program (9 were lost to follow-up), in 9 classes. From pre- to post-assessment, by self-reporting, BMI increased slightly in the general group, from 20.3 (s.d.=2.2) to 20.7 (s.d.=2.4), and decreased slightly in the weight maintenance group, from 27.5 (s.d.=5.2) to 26.6 (s.d.=5.7; t=2.98, P=0.005). There was an increase in the number of students who reported eating fruit, green salad, carrots and other vegetables (see Figure 2). The mean ratings of the sessions were 3.5/5 for interesting, 3.4/5 for helpful and 3.1/5 for fun. There was a significant reduction in weight and shape concerns for young women at risk for overweight, from 53.8 (s.d.=20.5) to 43.2 (s.d.=17.2; t=3.2, P=0.001), and for women at any weight with high weight and shape concerns, from 62.2 (s.d.=12.5) to 50.2 (s.d.=15.8; t=3.7, P=0.001.)
Figure 2.
Pre-post changes in Youth Risk Behavior Survey nutrition data compared with national norms.
Discussion
The results suggest the StayingFit program is feasible to deliver to high schools interested in a universal and targeted healthy weight regulation program for ninth-grade students. The program can serve as the framework for adaptive continuous quality-improvement trials. After the first session, the investigators were available for help with computer problems, but the program was run entirely by the teachers with no training. Most importantly, the school wanted to run the program again the following year.
Results also suggest the intervention may have improved healthy food choices in the general group, whereas leading to weight loss in the weight maintenance group. Equally important is the fact that the study suggests a weight maintenance intervention combined with psychoeducation related to body image does not increase eating disorder risk as reflected in a significant reduction in weight and shape concerns. However, these data are based on self-report, and this was not designed as an efficacy trial.
The largest cost to the investigators was to provide monitoring of the asynchronous discussion group. Content analysis suggested that this feature did not contribute to outcome and that it could be dropped, thus reducing the cost and increasing the feasibility of dissemination. Teachers are required to provide core nutrition and physical activity information so that the time students spent on the program would have been spent in face-to-face teaching. We have no evidence that the program is more effective at increasing knowledge and other variables; however, by having the teachers monitor the students’ work on the computers, they are free to address individual questions. Furthermore, it is very difficult to provide universal and targeted programs simultaneously with face-to-face instruction.
Assuming that StayingFit has been shown to be feasible and has a reasonable effect size in the pilot, the next step in traditional research would be to examine the efficacy of StayingFit in randomized populations. However, as the core weight maintenance program has already been shown to be efficacious in two randomized trials in this age group,10, 12 and this study has shown the feasibility of inexpensive implementation, then a strategy more likely to provide a program of potential use and benefit to schools would be to incorporate the core program in an adaptive continuous quality-improvement design.7 Such a model would provide both real-world effectiveness and permit adaptation to local school environments. In this model, program effectiveness would be defined as weight maintenance for the normal-weight group and weight loss for the overweight/obese group. In addition, process data, such as adherence to logs, and moderating variables, such as demographics, would be examined to determine how the program might be improved/adapted to local school environments. For instance, some schools might require a shorter version or a version tailored to a specific community. As another example, the program might benefit from incorporating features of mobile technology (applications, global positioning system), games and virtual reality. In addition, the program might be expanded to deal with issues of affect. Any changes presumably affecting outcome would be examined in adaptive designs.
Once the core program reaches predetermined goals (weight maintenance/loss, accepted levels of adherence and engagement), the next step will be to determine how the online program can be combined with social networking, and environmental, family and community activities to achieve even more robust changes.
Acknowledgements
CBT received grant sponsorship from the NIMIA (I RO1MH081124-01A2) and the NHMRC (003813); JW received grant sponsorship from the National Health and Medical Research Council of Australia Project Grant ID 1003813. We thank Healthmunk LLC for providing the software program, and the staff, faculty and students of Woodside High School for their help with this study. Publication of this supplement was partially supported by Nutrilite Health Institute with an unrestricted educational contribution to Stanford Prevention Research Center.
Footnotes
Conflict of interest
DEW received consulting fees from Jenny Craig/Nestle and United Health Group and grant support from Shire. The remaining authors declare no conflict of interest.
References
- An JY, Hayman LL, Park YS, Dusaj TK, Ayres CG. Web-based weight management programs for children and adolescents: a systematic review of randomized controlled trial studies. ANS Adv Nurs Sci. 2009;32:222–240. doi: 10.1097/ANS.0b013e3181b0d6ef. [DOI] [PubMed] [Google Scholar]
- Tate DF. Handbook of Childhood and Adolescent Obesity Issues in Clinical Child Psychology. Vol. VI. New York City: SpringerLink; 2009. Application of innovative technologies in the prevention and treatment of overweight in children and adolescents; pp. 387–404. [Google Scholar]
- Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, Gonder-Frederick LA. A behavior change model for Internet interventions. Ann Behav Med. 2009;38:18–27. doi: 10.1007/s12160-009-9133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research in practice: Rethinking the efficacy-to-effectiveness transition. Am J Pub Health. 2003;9:1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Murphy SA, Bierman KL. A conceptual framework for adaptive preventive interventions. Prev Sci. 2004;5:185–196. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair V, Strecher V, Fagerlin A, Ubel P, Resnicow K, Murphy S, et al. Screening experiments and the use of fractional factorial designs in behavioral intervention research. Am J Public Health. 2008;98:1354–1359. doi: 10.2105/AJPH.2007.127563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CH, Ten Have TR, Jo B, Dagne G, Wyman PA, Muthén B, et al. Adaptive designs for randomized trials in public health. Annu Rev Public Health. 2009;30:1–2. doi: 10.1146/annurev.publhealth.031308.100223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Collins JL, Kann L, Warren CW, Williams BI. Reliability of the Youth Risk Behavior Survey Questionnaire. Am J Epidemiol. 1995;141:575–580. doi: 10.1093/oxfordjournals.aje.a117473. [DOI] [PubMed] [Google Scholar]
- Jacobi C, Abascal L, Taylor CB. Screening for eating disorders and high-risk behavior: Caution. Int J Eat Disord. 2004;36:280–295. doi: 10.1002/eat.20048. [DOI] [PubMed] [Google Scholar]
- Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE. Reduction of overweight and eating disorder symptoms via the Internet in adolescents: A randomized controlled trial. J Adol Health. 2008;43:172–179. doi: 10.1016/j.jadohealth.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Morris L, Beckers C, Bronisch-Holtze J, Winter J, Winzelberg AJ, et al. Maintenance of internet-based prevention: a randomized controlled trial. Int J Eat Disord. 2007;40:114–119. doi: 10.1002/eat.20344. [DOI] [PubMed] [Google Scholar]
- Jones M, Luce KH, Osborne MI, Taylor K, Cunning D, Doyle AC, et al. Randomized, controlled trial of an internet-facilitated intervention for reducing binge eating and overweight in adolescents. Pediatrics. 2008;121:453–462. doi: 10.1542/peds.2007-1173. [DOI] [PubMed] [Google Scholar]
- Luce KH, Osborne MI, Winzelberg AJ, Das S, Abascal LB, Celio AA, et al. Application of an algorithm-driven protocol to simultaneously provide universal and targeted prevention programs. Int J Eat Disord. 2005;37:220–226. doi: 10.1002/eat.20089. [DOI] [PubMed] [Google Scholar]
- Beinter A, Jacobi C, Taylor CB. Effects of an Internet-based prevention program for eating disorders in the U.S. and Germany—a meta-analytic review. Eur Rev Eat Dis. 2012;20:1–8. doi: 10.1002/erv.1130. [DOI] [PubMed] [Google Scholar]
- Abascal L, Bruning Brown J, Winzelberg AJ, Dev P, Taylor CB. Combining universal and targeted prevention for school-based eating disorder programs. Int J Eat Disord. 2004;35:1–9. doi: 10.1002/eat.10234. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, et al. Prevention of eating disorders in at-risk college-age women. Arch Gen Psychiatry. 2006;63:881–888. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG. Overcoming Binge Eating. New York, NY: Guilford Press; 1995. [Google Scholar]
- Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Weight control for overweight adolescents initiated in primary care. Obes Res. 2002;10:22–32. doi: 10.1038/oby.2002.4. [DOI] [PubMed] [Google Scholar]
- Plowman SA, Sterling CL, Corbin CB, Meredith MD, Welk GJ, Morrow JR. The history of FITNESSGRAM®. J Phys Act Health. 2006;3:S5–S20. [Google Scholar]