Abstract
Increased susceptibility to tuberculosis following HIV-1 seroconversion contributes significantly to the tuberculosis epidemic in sub-saharan Africa. Lung specific mechanisms underlying the interaction between HIV-1 and Mycobacterium (M.) tuberculosis infection are incompletely understood. This study addressed the effect of HIV-1 and latent M. tuberculosis infection on viral-entry receptors and ligands in bronchoalveolar lavage (BAL). Median fluorescence intensity (MFI) of entry receptor expression was measured by multiparameter flow cytometry and chemokine expression by multiplex bead array.
Irrespective of HIV-1 status, BAL T-cells expressed higher MFI for the beta-chemokine receptor (CCR)5 than peripheral blood T-cells (p<0.001), in particular the CD8+ T-cells of HIV-1 infected persons showed elevated CCR5 expression (p=0.026). The concentration of BAL CCR5 ligands, regulated upon activation normal T-cell expressed and secreted (RANTES; p<0.001) and macrophage inflammatory protein (MIP)-1β (p=0.004) were elevated in the BAL of HIV-1 infected persons compared to controls. CCR5 expression and RANTES concentration correlated strongly with HIV-1 viral load in BAL. By contrast these alterations were not associated with M. tuberculosis sensitization in vivo nor did M. tuberculosis infection of BAL cells ex vivo change RANTES expression.
These data suggest ongoing HIV-1 replication predominantly drives local pulmonary CCR5+ T-cell activation in HIV/latent M. tuberculosis co-infection.
Keywords: BAL, CCR5, RANTES, TB, viral load
Introduction
Tuberculosis and AIDS are amongst the leading causes of deaths worldwide. In the majority of cases in immunocompetent persons, M. tuberculosis is successfully controlled by local immune responses leading to isolation of infected alveolar macrophages and the formation of granulomas. In HIV-1 infection, the rate of active tuberculosis following primary infection and the rate of reactivation of tuberculosis in individuals with latent M. tuberculosis infection is greatly increased although the underlying mechanisms are not well understood [1].
T-cell mediated immunity is critical for immune control of tuberculosis. HIV-1 replicates in activated CD4+ T-cells, monocytes or dendritic cells and leads to immunodeficiency characterized by progressive CD4+ T cell depletion. Moreover, despite relatively normal numbers of circulating CD4+ T-cells HIV-1 infected persons are already at increased risk of tuberculosis in the first year following seroconversion [2]. HIV-1 infection impairs not only the quantity but also the quality of M. tuberculosis specific immune responses [3]. In addition mortality remains higher after successful anti-tuberculosis treatment of HIV-1 infected persons [4], even though CD4+ T-cell numbers partially reconstitute after initiation of antiretroviral therapy (ART) [5].
T-cell activation is an important mechanism of HIV-1 pathogenesis [6] and persistent cell expression of activation markers predicts the progression into AIDS [7]. So far only a few studies have investigated the activation markers CD38, CD69 and Ki67 on BAL cells at the site of active tuberculosis disease [6, 8, 9]. Chronic antigen exposure in latent M. tuberculosis infection may lead to a persistent localized immune-activation that facilitates HIV-1 entry into CD4+ T-cells in lungs. The alpha (CXCR)4 and beta chemokine receptors (CCR)5 are the most important coreceptors for HIV-1 entry and infection of CD4+ T-cells [10, 11]. CCR5 expression on CD8+ T-cells mediates the migration of antigen-specific effector and differentiated memory CD8+ T-cells to the site of inflammation and it has been suggested that these CD8+ T-cells are important in eradication of virus-infected CD4+ T-cells. The β-chemokines MIP1α, MIP1β and RANTES attract CCR5+ T-cells to the region [12].
To evaluate the hypothesis that HIV-1 infection or M. tuberculosis exposure influence CCR5 and CXCR4 receptor and agonist expression, receptor expression and chemokine profiles from the peripheral blood and BAL mononuclear cells were compared between in HIV-1 infected and uninfected persons with and without evidence of M. tuberculosis sensitization.
Results
Participants
Blood and BAL cells from age and sex matched groups of 15 HIV-1 infected and 21 HIV-1 uninfected persons from an area of high tuberculosis incidence and high HIV-1 prevalence were investigated [3] (Table 1). Ten HIV-1-infected and 11 HIV-1 uninfected participants were diagnosed with latent M. tuberculosis infection by a positive ESAT-6 and/ or CFP-10 specific IFN-γ immune response in an ELISpot assay performed with PBMC in the absence of active tuberculosis disease. HIV-1 infected persons had a median CD4 count of 226 cells/µL. Frequencies of CD4+ CD3+ T-cells were significantly lower in blood (median 10.0 vs. 42.4%; p<0.001) and BAL lymphocytes (median 7.7 vs. 37.7%; p<0.001) when compared to HIV-1 uninfected persons (Table 1).
Table 1.
Characteristics of persons enrolled to the study
| HIV-1 infected | HIV-1 uninfected | p-value | |
|---|---|---|---|
| N | 15 | 21 | |
| Sex: female/male, n | 11/4 | 13/8 | 0.564 |
| Age, mean years (range) | 34.3 (24–51) | 32.7 (21–55) | 0.531 |
| CD4, median CD4 cells/µL (range) | 226 (61–595) | 786 (461–1,225) | <0.001 a |
| Blood CD4+, median CD4+ as % of CD3+ T-cells (range) | 10.0 (3.45–28.9) | 42.4 (9.46–67.8) | <0.001 a |
| BAL CD4+, median CD4+ as % of CD3+ T-cells (range) | 7.7 (1.33–31.30) | 37.7 (12.5–78.7) | <0.001 a |
| Blood Viral load, median RNA copies/mL, (range) | 22,000 (590–660,000) | ||
| BAL Viral load, median RNA copies/mL, (range) | 1,964 (855–709,088) | ||
| Response to ESAT-6/CFP-10, blood: positive/negative | 10/5 | 11/10 | 0.190 b |
Differences between the HIV-1 infected and HIV-1 uninfected groups were compared using the Mann Whitney U test.
Difference of ESAT-6/CFP-10 induced IFNγ-response in PBMC between HIV-1 infected and HIV-1 uninfected groups was compared using Fisher’s exact test of probability.
HIV-1 viral load
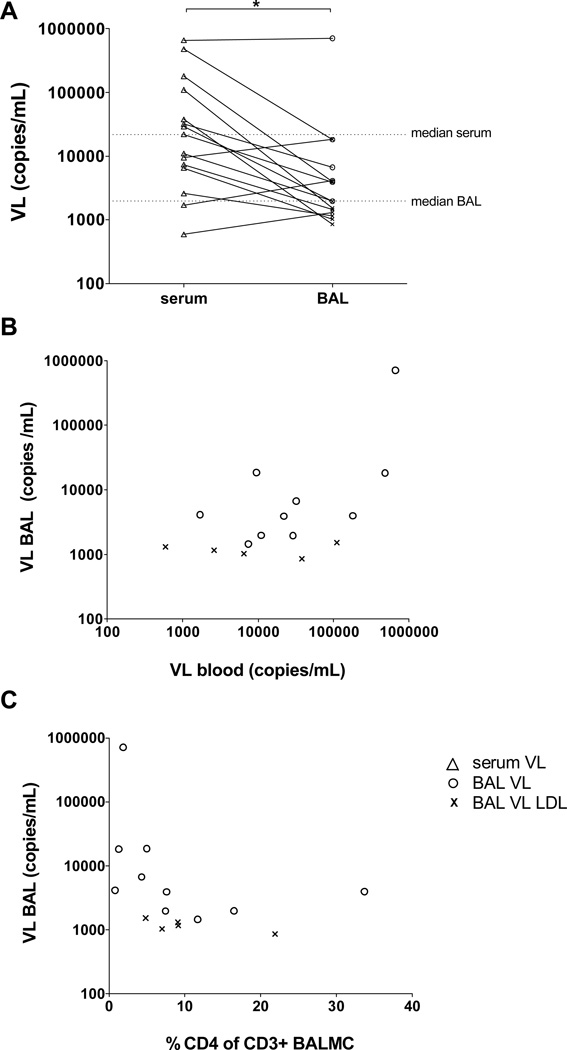
Stratification of BAL urea level by HIV-1 status revealed no difference between HIV-1 uninfected and HIV-1 infected people (p=0.64, data not shown). To compare the tissue load of HIV-1 in the lungs with the levels in blood, the viral load was determined in serum and BAL (Figure 1A). In five out of 15 HIV-1 infected persons the viral load in BAL was below the detection limit (individuals marked in the graphs). The median viral load in serum was 22,000 RNA copies/mL (range 590 – 660,000 copies/mL). A significantly lower median of 1,964 RNA copies/mL (range 855 – 709,088 copies/mL) was found in BAL (p=0.030). Nevertheless, in three cases the viral load in the BAL was higher than the viral load in serum. There was a positive correlation between the viral load in serum and in lungs (rho=0.787, p<0.001, Figure 1B). Figure 1C demonstrates an inverse correlation (rho= −0.586, p=0.022) between viral load and the proportion of CD4+ in BAL.
Figure 1.
Viral load (VL) in bronchoalveolar lavage (BAL). (A) Paired VL in serum (n=15, open triangles) and BAL fluid (n=15) was measured by nucleic acid amplification tests of gag for the quantitation of human HIV-1 RNA. The detection limit was 20 copies/800µL pure BAL fluid. BAL VL above the detection limit are depicted with open circles (n=10). BAL VL values lower the detection limit (LDL) were set to a value of 19 copies/mL and normalized according to the Urea method (n=5, symbol x). Each sign is representative of one sample, horizontal lines represent median VL of serum and BAL. (A) The difference between VL in serum and BAL was p=0.030, using the Wilcoxon signed rank test. (B) Correlation between VL in serum and BAL was assessed by Pearson (rho=0.787, p<0.001) and (C) correlation between VL BAL and the relative frequency of CD4+ CD3+ BAL T-cells was assessed by Spearman (rho= −0.586, p=0.022).
HIV-1 receptor expression on bronchoalveolar T-cells
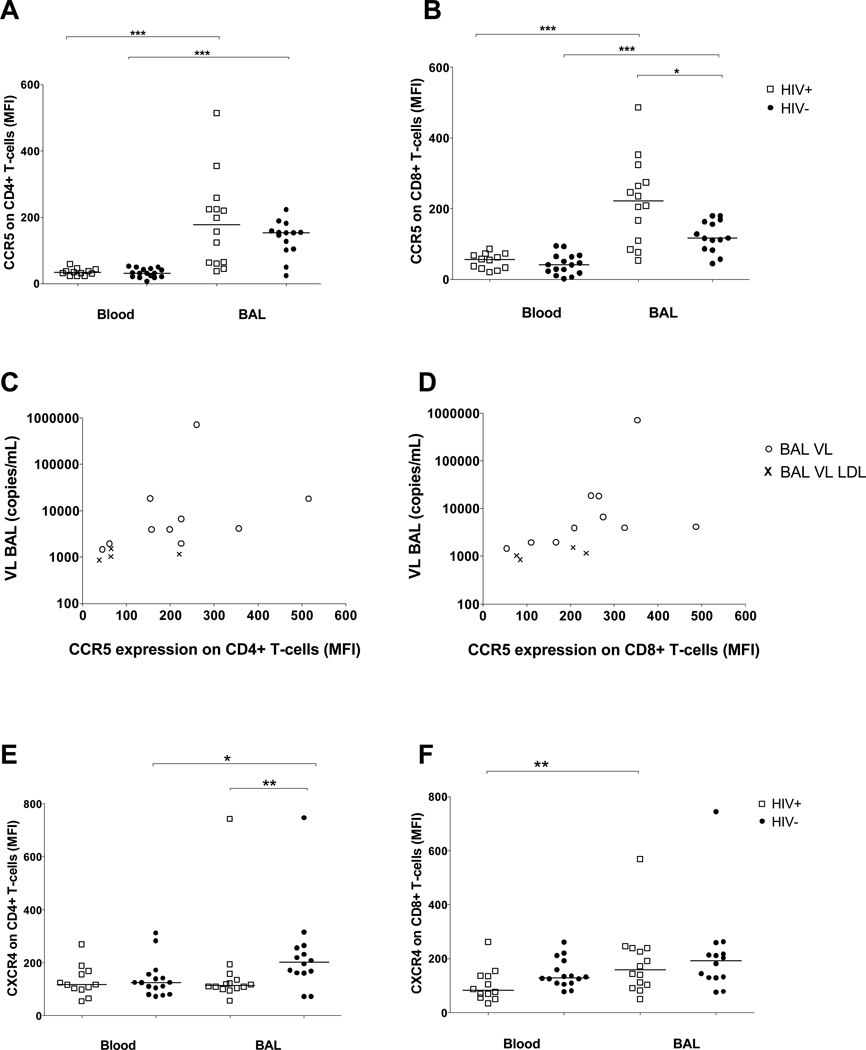
Several mechanisms of increased HIV-1 replication have been described at the site of M. tuberculosis infection [13]. In the previous study with the same participants investigation of the T-cell memory phenotype revealed no differences between HIV-1 infected and uninfected persons, but predominantly CD4+ effector T-cells in BAL when compared to blood [3]. As these activated effector T-cells in the lungs may facilitate HIV-1 entry, BALMC were characterised for their expression of the HIV-1 entry receptors CCR5 and CXCR4. Comparing the compartments, CD4+ (Figure 2A) and CD8+ BALMC (Figure 2B) invariably had significantly higher expression of the CCR5 receptor than PBMC (p<0.001), measured by median fluorescence intensity (MFI). No differences in CCR5 expression by CD4+ blood T-cells were found between HIV-1 infected and HIV-1 uninfected persons, whereas CCR5 expression by CD4+ T-cells in BAL was slightly higher in HIV-1 infected persons than in HIV-1 uninfected participants (178 vs. 153) although the difference was not significant (p= 0.37, Figure 2A). Similarly, CCR5 expression by peripheral CD8+ T-cells did not differ between HIV-1 infected and HIV-1 uninfected persons. By contrast, CCR5+ expression by CD8+ T-cells in BAL was moderately higher in HIV-1-infected persons (222.5 vs. 116.5, p=0.026, Figure 2B). Levels of CCR5 on CD4+ and CD8+ BAL T-cells were directly correlated with viral load in BAL (rho=0.706, p=0.005, Figure 2C and rho=0.793, p<0.001, Figure 2D respectively). By contrast, stratifying CCR5 expression on CD4+ and CD8+ BALMCs by M. tuberculosis infection status did not reveal any difference (data not shown). The pattern of CXCR4 expression on T-cells differed from CCR5 expression. Levels of CXCR4 expression on CD4+ T-cells trended to be higher on BALMC than on PBMC in HIV-1 uninfected subjects (201.5 vs. 124.5, p=0.049), whereas no difference in CXCR4 expression was observed between BAL or blood CD4+ T-cells of HIV-1 infected persons. CXCR4 expression on CD4+ BALMC was significantly higher in the HIV-1 uninfected control group when compared to HIV-1 infected persons (201.5 vs. 114.5, p=0.009, Figure 2E). No correlation was found between CXCR4 expression by CD4+ BALMC and viral load in BAL in HIV-1 infected persons (data not shown). CXCR4+ expression on CD8+ PBMC did not differ by HIV-1 status. BALMC CD8+ T-cells expressed higher levels of CXCR4+ than PBMC in HIV-1 infected persons (159.5 vs. 83.9 respectively, p=0.003, Figure 2F), whereas the slightly higher CXCR4 expression on CD8+ BAL T-cells compared with PBMC in the HIV-1 uninfected group was not significant (193 vs. 129.5 , p=0.059).
Figure 2.
CCR5 and CXCR4 expression on CD4+ or CD8+ T-cells in blood and bronchoalveolar lavage (BAL). Median fluorescence intensity (MFI) of CCR5 (A,B) and CXCR4 (E,F) receptor expression was measured by flow cytometry on CD4+ (A,E) and CD8+ (B,F) cells from blood and BAL of HIV-1 infected (n=12 in blood, n=14 in BAL, open squares) and HIV-1 uninfected persons (n=16 in blood, n=14 in BAL, solid circles), each sign represents one individual, bars represent medians. Differences between CCR5 expression on CD4+ and CD8+ T-cells from paired blood and BAL samples were calculated by Wilcoxon signed rank test (all p<0.001). The CCR5 expression on CD8+ BAL T-cells was significantly higher in HIV-1 infected compared to HIV-1 uninfected persons (p=0.026, by Mann Whitney U test). Correlation between viral load (VL) in BAL and MFI of CCR5+ on CD4+ (rho=0.706, p=0.005, C) or CD8+ (rho=0.793, p<0.001, D) BAL T-cells of HIV-1 infected participants was assessed by Spearman. Open circles, BAL VL; symbol x, BAL VL lower detection limit (LDL) were set to a value of 19 copies/mL and normalized according to the Urea method. (E) The difference of CXCR4 expression on CD4+ paired blood and BAL T-cells was p=0.049 (Wilcoxon signed rank test). MFI of CXCR4+ CD4+ BALMC was significantly higher in the HIV-1 uninfected control group when compared to HIV-1 infected persons (p=0.009, Mann Whitney U test). BALMC CD8+ T-cells expressed higher levels of CXCR4+ than PBMC in HIV-1 infected persons (p=0.003), differences between the HIV-1 status were assessed by Mann Whitney U test.
Level of CCR5 ligands
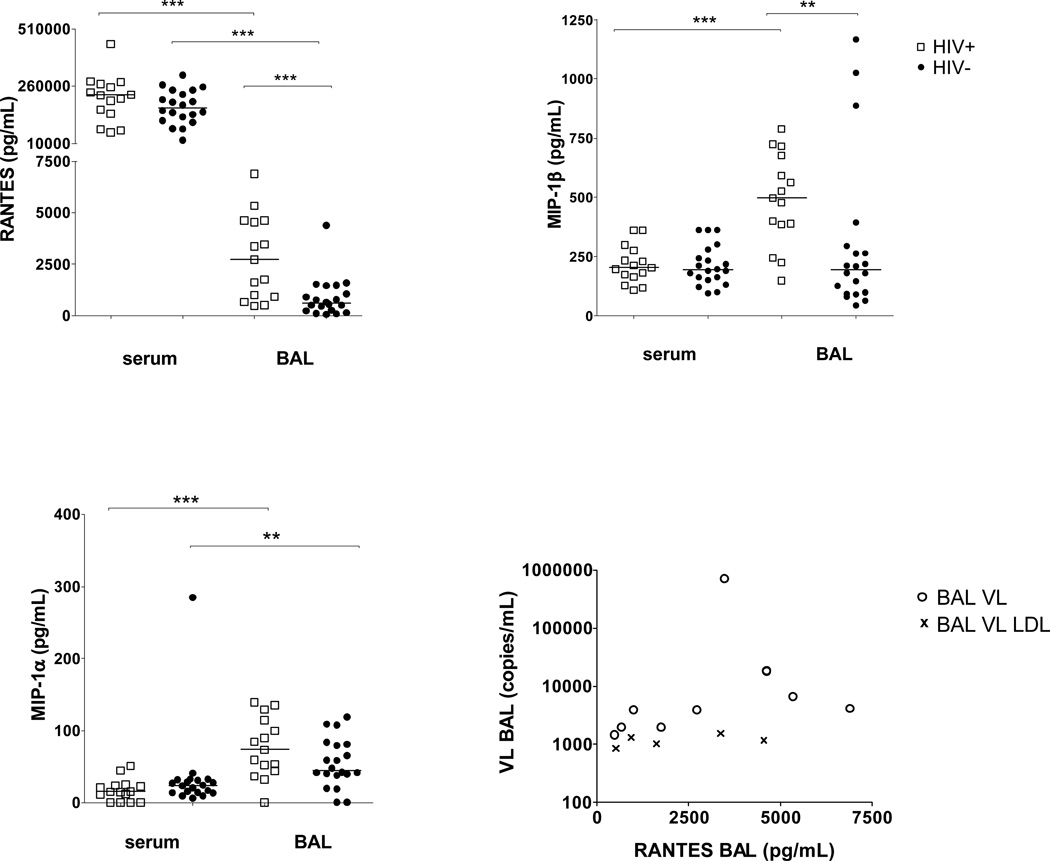
Blockade of the CCR5 receptor by drugs, such as Maraviroc, can prevent the entry of CCR5-tropic HIV-1 into target cells [14,15]. As differences were observed in the expression of CCR5 in BAL compared to blood, CCR5 ligand levels were ascertained in the two compartments by measuring the transcript levels of the three CCR5 agonists RANTES, MIP-1β and MIP-1α in BALMC. A lower threshold cycle (ΔCT) represents a higher abundance (Figure 3). RANTES abundance was significantly higher in HIV-1 infected than in uninfected participants (median ΔCT 2.68 vs. 7.27, p=0.003). The mean abundance of MIP-1β was slightly but not significantly higher in HIV-1 infected (median ΔCT 5.70), when compared to HIV-1 uninfected persons (median ΔCT 7.02, p=0.225), whereas MIP-1α transcript abundance in BAL was comparable in HIV-1 infected and uninfected persons.
Figure 3.
Constitutive transcript abundance of CCR5 ligands in bronchoalveolar lavage cells. Constitutive transcript abundance was assessed in freshly isolated BALMC of HIV-1 infected persons (n=12, open squares) and HIV-1 uninfected persons (n=10, solid circles). ΔCT = (CT gene of interest) – (CT β-Actin). A lower ΔCT indicates higher transcript abundance. Each sign represents one sample, bars represent medians. Differences between constitutive RANTES transcript abundance of HIV-1 infected and HIV-1 uninfected persons was p=0.003 (Mann Whitney U test).
Having observed differences in transcript abundance, the protein levels of RANTES, MIP-1β and MIP-1α were investigated by multiplex bead array in blood and BAL. RANTES was found at high concentrations in serum, but at significantly lower concentrations in the BAL (p<0.001). The level of this chemokine in serum was independent of HIV-1 status, whereas significantly higher RANTES levels were recorded in the BAL of HIV-1 infected versus HIV-1 uninfected persons (2,725 pg/mL vs. 594.6 pg/mL, p<0.001, Figure 4A). The RANTES levels in BAL also correlated with viral load in the same compartment (rho=0.635, p=0.011, Figure 4D), whereas elevated RANTES levels were not associated with M. tuberculosis sensitization status (data not shown).
Figure 4.
Chemokine concentration of RANTES, MIP-1β and MIP-1α in serum and bronchoalveolar lavage (BAL) of HIV-1 infected (n=15, open squares) or HIV-1 uninfected (=20, solid circles) persons. Chemokine concentration was measured by multiplex bead array, each sign represents one sample, bars represent medians. (A) Differences of RANTES concentration between paired serum and BAL samples of HIV-1 infected (p<0.001) and HIV-1 uninfected persons were assessed by Wilcoxon signed rank test. The RANTES level in BAL in HIV-1 infected in comparison with HIV-1 uninfected (p<0.001) was calculated by Mann Whitney U test. (B) Difference of MIP-1β concentration between paired serum and BAL samples of HIV-1 infected participants (p<0.001) was assesses by Wilcoxon signed rank test. MIP-1β level in BAL was higher in HIV-1 infected versus HIV-1 uninfected persons (p=0.004, Mann Whitney U test). (C) Wilcoxon signed rank test was used to compare MIP-1α level in paired blood and BAL samples (p<0.001 in HIV-1 infected, p=0.01 in HIV-1 uninfected persons). (D) Correlation between RANTES concentration in BAL and viral load (VL) in BAL were assessed by Spearman (rho=0.635, p=0.011). Open circles, BAL VL; symbol x, BAL VL lower detection limit (LDL) were set to a value of 19 copies/mL and normalized according to the Urea method.
MIP-1β levels in blood were comparable in HIV-1 uninfected and HIV-1 infected persons. In contrast, MIP-1β was elevated in the BAL of HIV-1 infected compared to HIV-1 uninfected persons (497.2 pg/mL vs. 194.3 pg/mL, p=0.004). Furthermore, MIP-1β levels in the BAL of HIV-1 infected participants were significantly higher when compared to the blood compartment (497.2 pg/mL vs. 202.8 pg/mL, p<0.001, Figure 4B).
Only low concentrations of MIP-1α were detected in both blood and serum. The serum levels of MIP-1α in HIV-1 infected participants did not differ from uninfected persons. The MIP-1α level in the BAL tended to be slightly higher in HIV-1 infected versus uninfected persons (73.7 pg/mL vs. 44.7 pg/mL, p= 0.113). Comparing both blood and BAL compartments, significantly higher levels of MIP-1α were found in the BAL compared to serum in HIV-1 infected (73.7 pg/mL vs. 15.2 pg/mL respectively, p<0.001) and HIV-1 uninfected participants (44.7 pg/mL vs. 23.5 pg/mL, p=0.01, Figure 4C).
No difference in the concentration of CXCR4 ligand SDF-1α in serum was observed between HIV-1 infected and HIV-1 uninfected persons. Levels of SDF-1α in BAL samples were all below the detection limit of 18.9 pg/mL (data not shown).
Effect of M. tuberculosis infection on CCR5 ligand expression
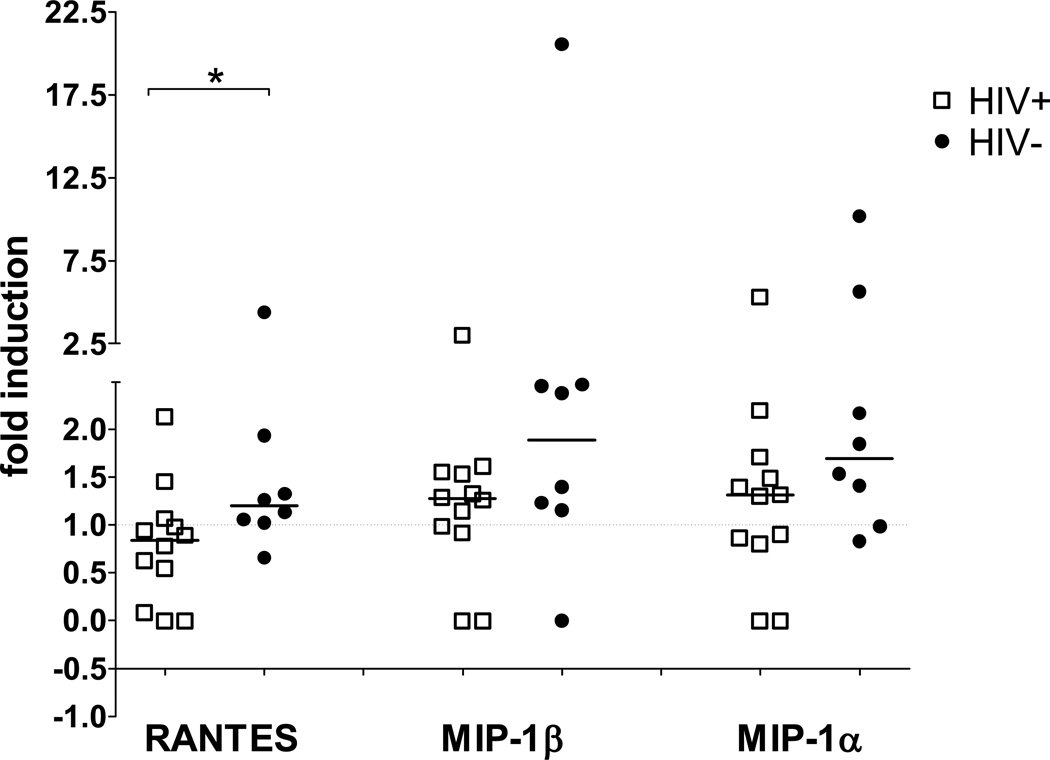
To investigate if differences in CCR5 ligand expression were due to HIV-1 infection or M. tuberculosis, BALMC were cultured in the presence or absence of M. tuberculosis H37Rv for 24 hours and transcript abundance measured by RT-PCR. Incubation with H37Rv decreased RANTES expression in BALMC from HIV-1 infected persons (median 0.84-fold induction), BALMC of HIV-1 uninfected persons showed a slight increase in RANTES expression (median 1.20-fold, p= 0.034, the difference is within experimental error). H37Rv induced little increase in MIP-1β (medians 1.28-fold in HIV-1 infected in comparison to 1.89-fold in HIV-1 uninfected). Similarly, median fold increases of 1.31 and 1.69 were observed in MIP-1α transcripts in HIV-1 infected and uninfected persons, respectively. Therefore the influence of M. tuberculosis on the gene expression level of CCR5 agonists was not great, with RANTES gene expression even diminished in HIV-1 infected persons (Figure 5).
Figure 5.
Fold induction of CCR5 ligands in bronchoalveolar lavage cells after 24h M. tuberculosis stimulation. 5×105 BALMC of HIV-1 infected (n=12, open squares) and HIV-1 uninfected participants (n=8, solid circles) were cultured for 24 hours in the presence or absence of M. tuberculosis H37Rv at MOI 1:1. Fold induction was calculated as (ΔCT in the presence of H37Rv) – (ΔCT in the absence of H37Rv), values normalised by power 2x transformation. Each sign is representative of one sample, bars represent medians. Differences between RANTES constitutive transcript abundance of HIV-1 infected and HIV-1 uninfected persons (p=0.034) were assessed by Mann Whitney test.
Discussion
The immunological mechanisms underlying the increased risk of tuberculosis in persons with HIV-1 co-infection, and those that exacerbate the course of both diseases, are unclear. The aim of this study was to investigate the influence of HIV-1 infection on immune activation of resident bronchopulmonary lymphocytes and a possible permissive environment for HIV-1 entry and replication. Therefore, chemokine receptors and chemokine profiles of the two compartments lavage and blood of HIV-1 infected and HIV-1 uninfected persons from an area of high tuberculosis exposure were compared. The key findings of this study are: (1) viral load correlates inversely with the number of CD4+ T-cells in BAL, (2) CD8+ BAL T-cells of HIV-1 infected persons express higher levels of CCR5 compared to HIV-1 uninfected persons, and (3) the observed elevation of MIP-1β and RANTES levels in BAL of HIV-1 infected persons was not further upregulated by ex vivo M. tuberculosis infection.
In this study HIV-1 viral load in BAL correlated directly with viral load in serum and inversely with CD4 cell count in BAL. These data support previous observations of HIV-1 replication in lungs [16,17]. Previous studies have demonstrated that HIV-1 replicates in alveolar macrophages [18,19], others showed that CCR5+ CD4+ BAL T-cells support replication [5, 20]. These results show in some people an elevation of HIV-1 RNA concentration in BAL fluid compared to serum, which supports compartmentalized local viral replication in human lungs. Furthermore, lung segments affected by tuberculosis disease have significantly higher HIV-1 viral load than uninvolved paired lung segment [21]. This may be partially explained by the finding that activated T cells display greater permissiveness to infection and viral replication, compared with quiescent cells [22]. To this end, HIV-1 replication was recently associated with M. tuberculosis-specific CD4+ T-cells, compared with CMV-specific CD4+ T-cells [23].
This study compared expression of the HIV-1 entry receptors on BAL and blood T-cells of HIV-1 infected and HIV-1 uninfected persons living in an area of high tuberculosis incidence. There was a wide range of CXCR4 expression levels on T-cells, with significantly decreased levels of CXCR4+ on CD4+ BAL T-cells of HIV-1 infected compared to HIV-1 uninfected persons. However, CXCR4 expression by CD4+ BALMC was not associated with HIV-1 viral load in the same compartment, confirming previous findings [24].
Higher levels of CCR5 expression were observed on CD4+ BAL T-cells by comparison with peripheral blood cells. This may be due to the fact that CCR5 is mainly expressed on effector memory (CD45RA- and CD27-) T-cell [25], the predominant T cell subset in BAL [3]. As CCR5 expression increases permissiveness to HIV-1 infection [11], the elevated expression of CCR5 on CD4+ BAL T-cells might increase BALMC susceptibility to HIV-1 infection. Our finding that HIV-1 viral load correlated with CCR5 expression on CD4+ BAL T-cells supports this hypothesis. Therefore these data add to previous descriptions of BALMC expression of CCR5 [5, 9, 20, 26] at the site of M. tuberculosis infection.
Findings from this study suggest that HIV-1 infection induces the elevation of CCR5+ expression on CD8+ BAL T-cells. Although increased expression of CCR5 on CD8+ T-cells is not directly related to HIV-1 susceptibility, CD8+ T-cells play a critical role in the control of viral infection. During HIV-1 infection cytotoxic T-lympocytes eliminate HIV-1 infected cells and secrete β-chemokines [27], which recruit monocytes and T-cells to inflammatory sites. Because our results showed an increased presence of CD8+ T-cells at the site of infection, we expected to find an elevation of the β-chemokines RANTES, MIP-1β and MIP-1α in BAL. This hypothesis was confirmed as higher levels of RANTES and MIP-1β were found in the BAL of HIV-1 infected in comparison to HIV-1 uninfected persons. It should be noted that soluble chemokines can be used to determine relative changes of these peptides during an inflammatory process but may more represent evidence of inflammation than a biological relevant form of these mediators. Since minimal concentrations of RANTES required for activation of CCR5 on T-cells are between 1 and 10 nM [28], about three-fold lower levels found in BAL derived from HIV-infected patient (2700 pg/mL; ~0.35 nM) are unlikely able to modulate the receptor status, but indicate to a higher status of cell activation in the lungs of HIV-1 infected persons.
RANTES levels directly correlated with viral load in BAL. On restimulation of BAL cells with M. tuberculosis no upregulation of the RANTES gene expression was observed. This suggests that CCR5 agonist levels in BALMC are influenced rather by HIV-1 status than by M. tuberculosis infection. Regulation of β-chemokine expression in BAL cells may differ from peripheral blood cells, as the latter showed higher β-chemokine levels in active tuberculosis, compared with healthy controls [29] and peripheral levels remained elevated in HIV-1 and M. tuberculosis coinfected persons despite anti-tuberculosis treatment [30].
HIV-1 viral replication in the lungs may drive the production of MIP-1β and RANTES. We speculate that this, at least in part, reflects compartmentalised cytolytic activity of HIV-1 specific CD8+ T-cells [31, 32]. Circulating T-cells that have been activated by β-chemokines and migrate to the site of infection, may thus be preferentially infected by HIV-1 [33]. By contrast, locally primed antigen specific T-cells are less permissive to HIV-1 infection, as CCR5 agonists compete with HIV-1 for binding sites of the CCR5 receptor resulting in an inhibitory effect for HIV-1 entry [14, 30, 33].
Our study had several limitations. Due to restricted numbers of BAL cells we were unable to better characterize the CCR5+ T-cell populations in respect of memory or effector phenotyping and to investigate the HIV-1 specific immune response. Such investigations would have allowed us to address whether, as shown for peripheral blood cells, antigen-specific CD4+ BAL T-cells that express high levels of CCR5 are preferentially eliminated [34] or if ongoing viral replication would be a similar predictor of HIV-1 specific CD8+ T-cell loss in BAL [35]. Secondly, it might be possible that HIV-1 infection preferentially depletes M. tuberculosis specific CCR5+ CD4+ T-cells [9, 23, 36]. Although we have not addressed this question specifically, data from the same participants show that M. tuberculosis specific T-cell responses in lungs of HIV-1 infected persons are markedly impaired [3]. It will be important to also study these effects of HIV infection in patients with active pulmonary tuberculosis.
Conclusion
Elevated levels of CCR5, the coreceptor for HIV-1, on CD4+ BAL T-cells in comparison to peripheral blood cells suggest a local permissive environment for HIV-1 infection in human lungs. HIV-1 infected persons also exhibited higher expression of CCR5 by CD8+ BAL T-cells, suggesting that CCR5 may play an important role in the recruitment of HIV-1 specific CD8+ effector T-cells into inflamed tissue where these CD8+ T-cells may mediate killing of HIV-infected cells. These results provide further evidence that ongoing HIV-1 replication is an important factor in the elevation of MIP-1β and RANTES levels in BAL from persons with HIV/ latent M. tuberculosis co-infection.
Methods
Participants
The study was approved by the Research Ethics Committees of the Universities of Cape Town, South Africa (REC 381/2006), and Lübeck, Germany (05–096) and all participants provided written informed consent. These investigations were performed as part of a larger study. Cells from the same patient samples were used for different experiments, these results focussing on the influence of HIV-1 on M. tuberculosis specific- T-cell immune responses have been previously published [3].
Briefly, participants were recruited at the Khayelitsha Site B Clinic in Cape Town, South Africa. In compliance with South African national guidelines HIV-1 care including ART was offered to all HIV-1 infected persons. A symptom screen and physical examination were performed, persons with active or a past history of tuberculosis, or isoniazid preventive therapy were excluded. Smoking, pregnancy, chronic cardiovascular or metabolic illnesses, immunosuppressive medication, and age less than 21 years also constituted exclusions. All participants had negative cultures for M. tuberculosis in BAL and had no radiological evidence of lung disease.
BAL and blood collection and processing
Bronchoscopy and blood collection were performed before patients were initiated on ART. Standard flexible diagnostic bronchoscopy including a BAL of the middle lobe with 300mL sterile saline and isolation of the bronchoalveolar mononuclear cells (BALMC) were conducted as described previously [3, 37]. BAL fluid was harvested and aliquots were frozen immediately at −80°C. Peripheral blood mononuclear cells (PBMC) were prepared as described previously [3, 37]. Serum samples were centrifugated at 3000rpm for 15 minutes at 20°C, aliquoted and frozen at −80°C.
Latent M. tuberculosis infection
Sensitization by M. tuberculosis was defined by the immune responses to the M. tuberculosis-specific antigens early-secreted antigenic target (ESAT)-6 and culture filtrate protein (CFP)-10 measured in PBMC by Interferon (IFN)-γ ELISpot assay, MABTECH, Nacka, Sweden) as reported previously [3].
HIV-1 viral load
Plasma HIV-1 viral load was detected by Nuclisens (BioMerieux, Randburg, South Africa). Viral load in BAL fluid was measured by Cobas TaqMan HIV-1 test (Roche Diagnostics GmbH, Grenzach-Wyhlen, Germany). Both assays are accredited in vitro nucleic acid amplification tests of gag for the quantitation of human HIV-1 RNA and both determine the results in copies/ml. The limit of agreement between the two assays is reported to be 0.126 copies/mL [38]. The detection limit was 20 copies/800µL pure BAL fluid. For analysis, values below the detection limit were assigned 19 copies/800µL BAL fluid. These values are specifically marked in the figures. To allow direct comparison between viral load in serum and BAL fluid, the dilution factor of the BAL procedure was assesed by the urea method [39]. Urea was measured by BUN Flex reagent cartridge (DF21, Siemens Healthcare Diagnostics GmbH, Eschborn, Germany). All data refer to copies/mL alveolar lining fluid, for easier reading the term copies/mL BAL will be used throughout the text.
Flow Cytometry
For phenotypic analysis freshly isolated PBMC and BALMC were stained with the surface marker antibodies (BD Biosciences, Johannesburg, South Africa) anti-CD3 Pacific Blue (UCTH1), anti-CD4 Alexa Fluor 700 (RPA-T4), anti-CD8 PerCP-Cy5.5 (SK1), anti-CD184 APC (12G5/CXCR4) and anti-CD195 PE (2D7/CCR5). Staining and acquisition was performed as previously described [3]. The flow cytometric gating strategy is illustrated in the Supporting Information Figure 1. PMT voltage settings were not changed in between group comparison. Data analysis was performed with FlowJo software version 9.2 (TreeStar, Ashland, TX, USA).
mRNA analysis
To estimate constitutive transcript abundance RNA samples were extracted immediately after BALMC isolation. To compare the differences in transcript abundance threshold cycle (CT) values for β-Actin were subtracted from the CT values of the gene of interest. To analyse M. tuberculosis induced changes in transcript levels, 5×105 BALMC were cultured for 24 hours in a 24-well plate with 1mL RPMI and 10% heat-inactivated fetal calf serum (Gibco, Mowbray, South Africa) in the presence or absence of M. tuberculosis H37Rv at MOI 1:1. RNA isolation and quantitative RT-PCR were performed as previously described [40]. The fold induction of genes was calculated by the ΔΔCT method (ΔCT in the presence of H37Rv minus ΔCT in the absence of H37Rv in culture) and values normalised by power 2x transformation. RANTES, MIP-1α and MIP-1β primers and probes were obtained from Applied Biosystems (Foster City, CA, USA).
Multiplex bead array
MIP-1α, MIP-1β, RANTES and SDF-1α levels in serum and BAL fluid were assayed in batches by multiplex bead array (Bio-Rad Laboratories, Munich, Germany). Serum testing was performed according to the manufacturer´s instructions [User Bulletin #10014905 Rev C, download from http://bio-rad.com/bioplex]. 500µl BAL fluid was incubated with multiplex beads, 1% bovine serum albumin (Sigma-Aldrich, Steinheim, Germany) and protease inhibitor (Roche, Mannheim, Germany) on a roller device at 4°C overnight. BAL fluid volume was subsequently reduced on the 96-well Biorad plate with vacuum manifold. Samples were read on the Biorad Luminex reader using Bioplex manager 4.1 software. Chemokine levels in BAL fluid were normalized by the urea method as pg/mL alveolar lining fluid, which for easier reading is reported as pg/mL BAL throughout the manuscipt.
Data analysis
Due to relatively small cell numbers in individual samples, not all analyses could be performed on all subjects. Statistical tests between groups were performed by the Mann Whitney U test, for paired data with the Wilcoxon Signed Rank test and for 2×2 tables Fisher’s exact test of probability. Nonparametric correlation was assessed by Spearman co-efficient, association between normally distributed data was tested by Pearson´s correlation test. Comparison in figures are indicated as * p<0.05; ** p<0.005, and *** p<0.0005.
Supplementary Material
Acknowledgements
We are grateful to the study participants and thank the staff at Ubuntu Clinic for assistance in recruitment. We thank Prof. Mark Nicol for providing the M. tuberculosis strain, H37Rv.
BK was funded by the German Research Foundation (DFG SCHE1556) and German National Respiratory Society (DGP). TJS, WH and RJW are funded by the Wellcome Trust (088316, 080929, 084323). TJS and WH have additional support from the Aeras Global TB Vaccine Foundation, Gates Foundation and the NIH (RO1-AI-087915 and NO1-AI-70022). KS and CL were supported by the HW & J Hector Foundation, Weinheim, Germany. RJW also has additional support from the MRC (U.1175.02.002.00014.01) and European Union (Sante/2006/105-061).
List of abbreviations
- ART
antiretroviral therapy
- BAL
bronchoalveolar lavage
- BALMC
bronchoalveolar lavage mononuclear cells
- CCR5
beta chemokine receptor 5
- CFP-10
culture filtrate protein 10
- CXCR4
alpha chemokine receptor 4
- ESAT-6
early-secreted antigenic target 6
- M. tuberculosis
Mycobacterium tuberculosis
- SDF-1
stromal cell-derived factor 1
Footnotes
Conflict of interest
The authors state that they have no conflict of interest.
References
- 1.Getahun H, Gunneberg C, Granich R, Nunn P. HIV infection-associated tuberculosis: the epidemiology and the response. Clin Infect Dis. 2010;50(Suppl 3):201–207. doi: 10.1086/651492. [DOI] [PubMed] [Google Scholar]
- 2.Sonnenberg P, Glynn JR, Fielding K, Murray J, Godfrey-Faussett P, Shearer S. How soon after infection with HIV does the risk of tuberculosis start to increase? A retrospective cohort study in South African gold miners. J Infect Dis. 2005;191:150–158. doi: 10.1086/426827. [DOI] [PubMed] [Google Scholar]
- 3.Kalsdorf B, Scriba TJ, Wood K, Day CL, Dheda K, Dawson R, Hanekom WA, et al. HIV-1 infection impairs the bronchoalveolar T-cell response to mycobacteria. Am J Respir Crit Care Med. 2009;180:1262–1270. doi: 10.1164/rccm.200907-1011OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manas E, Pulido F, Pena JM, Rubio R, Gonzalez-Garcia J, Costa R, Perez-Rodriguez E, et al. Impact of tuberculosis on the course of HIV-infected patients with a high initial CD4 lymphocyte count. Int J Tuberc Lung Dis. 2004;8:451–457. [PubMed] [Google Scholar]
- 5.Knox KS, Vinton C, Hage CA, Kohli LM, Twigg HL, III, Klatt NR, Zwickl B, et al. Reconstitution of CD4 T cells in bronchoalveolar lavage fluid after initiation of highly active antiretroviral therapy. J Virol. 2010;84:9010–9018. doi: 10.1128/JVI.01138-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barry SM, Johnson MA, Janossy G. Increased proportions of activated and proliferating memory CD8+ T lymphocytes in both blood and lung are associated with blood HIV viral load. J Acquir Immune Defic Syndr. 2003;34:351–357. doi: 10.1097/00126334-200312010-00001. [DOI] [PubMed] [Google Scholar]
- 7.Hazenberg MD, Otto SA, van Benthem BH, Roos MT, Coutinho RA, Lange JM, Hamann D, et al. Persistent immune activation in HIV-1 infection is associated with progression to AIDS. AIDS. 2003;17:1881–1888. doi: 10.1097/00002030-200309050-00006. [DOI] [PubMed] [Google Scholar]
- 8.Raju B, Tung CF, Cheng D, Yousefzadeh N, Condos R, Rom WN, Tse DB. In situ activation of helper T cells in the lung. Infect Immun. 2001;69:4790–4798. doi: 10.1128/IAI.69.8.4790-4798.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santucci MB, Bocchino M, Garg SK, Marruchella A, Colizzi V, Saltini C, Fraziano M. Expansion of CCR5+ CD4+ T-lymphocytes in the course of active pulmonary tuberculosis. Eur Respir J. 2004;24:638–643. doi: 10.1183/09031936.04.000105403. [DOI] [PubMed] [Google Scholar]
- 10.Morris L, Cilliers T, Bredell H, Phoswa M, Martin DJ. CCR5 is the major coreceptor used by HIV-1 subtype C isolates from patients with active tuberculosis. AIDS Res Hum Retroviruses. 2001;17:697–701. doi: 10.1089/088922201750236979. [DOI] [PubMed] [Google Scholar]
- 11.Gorry PR, Ancuta P. Coreceptors and HIV-1 Pathogenesis. Curr HIV/AIDS Rep. 2011;8:45–53. doi: 10.1007/s11904-010-0069-x. [DOI] [PubMed] [Google Scholar]
- 12.Fukada K, Sobao Y, Tomiyama H, Oka S, Takiguchi M. Functional expression of the chemokine receptor CCR5 on virus epitope-specific memory and effector CD8+ T cells. J Immunol. 2002;168:2225–2232. doi: 10.4049/jimmunol.168.5.2225. [DOI] [PubMed] [Google Scholar]
- 13.Toossi Z. Virological and immunological impact of tuberculosis on human immunodeficiency virus type 1 disease. J Infect Dis. 2003;188:1146–1155. doi: 10.1086/378676. [DOI] [PubMed] [Google Scholar]
- 14.Cocchi F, DeVico AL, Garzino-Demo A, Arya SK, Gallo RC, Lusso P. Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 15.Vandekerckhove L, Verhofstede C, Vogelaers D. Maraviroc: integration of a new antiretroviral drug class into clinical practice. J Antimicrob Chemother. 2008;61:1187–1190. doi: 10.1093/jac/dkn130. [DOI] [PubMed] [Google Scholar]
- 16.Koziel H, Kim S, Reardon C, Li X, Garland R, Pinkston P, Kornfeld H. Enhanced in vivo human immunodeficiency virus-1 replication in the lungs of human immunodeficiency virus-infected persons with Pneumocystis carinii pneumonia. Am J Respir Crit Care Med. 1999;160:2048–2055. doi: 10.1164/ajrccm.160.6.9902099. [DOI] [PubMed] [Google Scholar]
- 17.Wood KL, Chaiyarit P, Day RB, Wang Y, Schnizlein-Bick CT, Gregory RL, Twigg HL., III Measurements of HIV viral loads from different levels of the respiratory tract. Chest. 2003;124:536–542. doi: 10.1378/chest.124.2.536. [DOI] [PubMed] [Google Scholar]
- 18.Toossi Z, Nicolacakis K, Xia L, Ferrari NA, Rich EA. Activation of latent HIV-1 by Mycobacterium tuberculosis and its purified protein derivative in alveolar macrophages from HIV-infected individuals in vitro. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;15:325–331. doi: 10.1097/00042560-199708150-00001. [DOI] [PubMed] [Google Scholar]
- 19.Kaner RJ, Santiago F, Rahaghi F, Michaels E, Moore JP, Crystal RG. Adenovirus vectors block human immunodeficiency virus-1 replication in human alveolar macrophages by inhibition of the long terminal repeat. Am J Respir Cell Mol Biol. 2010;43:234–242. doi: 10.1165/rcmb.2008-0063OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brenchley JM, Knox KS, Asher AI, Price DA, Kohli LM, Gostick E, Hill BJ, et al. High frequencies of polyfunctional HIV-specific T cells are associated with preservation of mucosal CD4 T cells in bronchoalveolar lavage. Mucosal Immunol. 2008;1:49–58. doi: 10.1038/mi.2007.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakata K, Rom WN, Honda Y, Condos R, Kanegasaki S, Cao Y, Weiden M. Mycobacterium tuberculosis enhances human immunodeficiency virus-1 replication in the lung. Am J Respir Crit Care Med. 1997;155:996–1003. doi: 10.1164/ajrccm.155.3.9117038. [DOI] [PubMed] [Google Scholar]
- 22.Owen RE, Heitman JW, Hirschkorn DF, Lanteri MC, Biswas HH, Martin JN, Krone MR, et al. HIV+ elite controllers have low HIV-specific T-cell activation yet maintain strong, polyfunctional T-cell responses. AIDS. 2010;24:1095–1105. doi: 10.1097/QAD.0b013e3283377a1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geldmacher C, Ngwenyama N, Schuetz A, Petrovas C, Reither K, Heeregrave EJ, Casazza JP, et al. Preferential infection and depletion of Mycobacterium tuberculosis-specific CD4 T cells after HIV-1 infection. J Exp Med. 2010;207:2869–2881. doi: 10.1084/jem.20100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoshino Y, Tse DB, Rochford G, Prabhakar S, Hoshino S, Chitkara N, Kuwabara K, et al. Mycobacterium tuberculosis-induced CXCR4 and chemokine expression leads to preferential X4 HIV-1 replication in human macrophages. J Immunol. 2004;172:6251–6258. doi: 10.4049/jimmunol.172.10.6251. [DOI] [PubMed] [Google Scholar]
- 25.Groot F, van Capel TM, Schuitemaker J, Berkhout B, de Jong EC. Differential susceptibility of naive, central memory and effector memory T cells to dendritic cell-mediated HIV-1 transmission. Retrovirology. 2006;3:52–61. doi: 10.1186/1742-4690-3-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fraziano M, Cappelli G, Santucci M, Mariani F, Amicosante M, Casarini M, Giosue S, et al. Expression of CCR5 is increased in human monocyte-derived macrophages and alveolar macrophages in the course of in vivo and in vitro Mycobacterium tuberculosis infection. AIDS Res Hum Retroviruses. 1999;15:869–874. doi: 10.1089/088922299310575. [DOI] [PubMed] [Google Scholar]
- 27.Gulzar N, Copeland KF. CD8+ T-cells: function and response to HIV infection. Curr HIV Res. 2004;2:23–37. doi: 10.2174/1570162043485077. [DOI] [PubMed] [Google Scholar]
- 28.Taub DD, Turcovski-Corrales SM, Key ML, Longo DL, Murphy WJ. Chemokines and T Lymphocyte Activation: β Chemokines Costimulate Human T Lymphocyte Activation In Vitro. J Immunol. 1996;156:2095–2103. [PubMed] [Google Scholar]
- 29.Mayanja-Kizza H, Wajja A, Wu M, Peters P, Nalugwa G, Mubiru F, Aung H, et al. Activation of beta-chemokines and CCR5 in persons infected with human immunodeficiency virus type 1 and tuberculosis. J Infect Dis. 2001;183:1801–1804. doi: 10.1086/320724. [DOI] [PubMed] [Google Scholar]
- 30.Wolday D, Tegbaru B, Kassu A, Messele T, Coutinho R, van Baarle D, Miedema F. Expression of chemokine receptors CCR5 and CXCR4 on CD4+ T cells and plasma chemokine levels during treatment of active tuberculosis in HIV-1-coinfected patients. J Acquir Immune Defic Syndr. 2005;39:265–271. doi: 10.1097/01.qai.0000163027.47147.2e. [DOI] [PubMed] [Google Scholar]
- 31.Wagner L, Yang OO, Garcia-Zepeda EA, Ge Y, Kalams SA, Walker BD, Pasternack MS, et al. β-Chemokines are release from HIV-1-specific cytolytic T-cell granules complexed to proteoglycans. Nature. 1998;391:908–911. doi: 10.1038/36129. [DOI] [PubMed] [Google Scholar]
- 32.Stegelmann F, Bastian M, Swoboda K, Bhat R, Kiessler V, Krensky AM, Roellinghoff M, et al. Coordinate Expression of CC Chemokine Ligand 5, Granulysin, and Perforin in CD8 + T Cells Provides a Host Defense Mechanism against. M. tuberculosis. J Immunol. 2005;175:7474–7483. doi: 10.4049/jimmunol.175.11.7474. [DOI] [PubMed] [Google Scholar]
- 33.Kelly MD, Naif HM, Adams SL, Cunningham AL, Lloyd AR. Dichotomous effects of beta-chemokines on HIV replication in monocytes and monocyte-derived macrophages. J Immunol. 1998;160:3091–3095. [PubMed] [Google Scholar]
- 34.Veazey RS, Marx PA, Lackner AA. Vaginal CD4+ T cells express high levels of CCR5 and are rapidly depleted in simian immunodeficiency virus infection. J Infect Dis. 2003;187:769–776. doi: 10.1086/368386. [DOI] [PubMed] [Google Scholar]
- 35.Geldmacher C, Gray C, Nason M, Currier JR, Haule A, Njovu L, Geis S, et al. A high viral burden predicts the loss of CD8 T-cell responses specific for subdominant gag epitopes during chronic human immunodeficiency virus infection. J Virol. 2007;81:13809–13815. doi: 10.1128/JVI.01566-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jambo KC, Sepako E, Fullerton DG, Mzinza D, Glennie S, Wright AK, Heyderman RS, Gordon SB. Bronchoalveolar CD4+ T cell responses to respiratory antigens are impaired in HIV-infected adults. Thorax. 2011;66(5):375–382. doi: 10.1136/thx.2010.153825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jafari C, Ernst M, Strassburg A, Greinert U, Kalsdorf B, Kirsten D, Lange C. Local immunodiagnosis of pulmonary tuberculosis by enzyme-linked immunospot. Eur Respir J. 2008;31:261–265. doi: 10.1183/09031936.00096707. [DOI] [PubMed] [Google Scholar]
- 38.Scott LE, Noble LD, Moloi J, Erasmus L, Venter WDF, Stevens W. Evaluation of the Abbott m2000 RealTime Human Immunodeficiency Virus Type 1 (HIV-1) Assay for HIV Load Monitoring in South Africa Compared to the Roche Cobas AmpliPrep-Cobas Amplicor, Roche Cobas AmpliPrep-Cobas TaqMan HIV-1, and BioMerieux NucliSENS EasyQ HIV-1 Assays. J Clin. Microbiol. 2009;47:2209–2217. doi: 10.1128/JCM.01761-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rennard SI, Basset G, Lecossier D, O'Donnell KM, Pinkston P, Martin PG, Crystal RG. Estimation of volume of epithelial lining fluid recovered by lavage using urea as marker of dilution. J Appl Physiol. 1986;60:532–538. doi: 10.1152/jappl.1986.60.2.532. [DOI] [PubMed] [Google Scholar]
- 40.Tadokera R, Meintjes G, Skolimowska KH, Wilkinson KA, Matthews K, Seldon R, Chegou NN, et al. Hypercytokinaemia accompanies HIV-tuberculosis immune reconstitution inflammatory syndrome. Eur Respir J. 2011;37:1248–1259. doi: 10.1183/09031936.00091010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.