Abstract
Objective
To describe the establishment and integration of a free-care acupuncture clinic within an urban hospital with an underserved minority adolescent population and to study patient utilization.
Background
Surveys often show low use of acupuncture among underserved non-Asian minority populations. We hypothesized that it would be possible to integrate an acupuncture clinic into a biomedical setting. We also hypothesized that the removal of economic and logistical barriers would increase usage of an acupuncture service among minority adolescent and pediatric populations, who may otherwise have had little cultural exposure to the modality.
Methods
A review of the process involved in establishing a free acupuncture clinic, and an analysis of visit data.
Results
A free faculty-supervised student acupuncture clinic was successfully integrated into an urban hospital-based adolescent clinic serving predominantly low-income minorities. During 2004–2006, the acupuncture clinic had 544 visits for a wide range of conditions. Visits increased 65% from the first to the third year of operation.
Conclusions
An acupuncture service can be successfully integrated into care provided by an urban hospital that serves low-income minority and immigrant patients. Strategic removal of barriers to access can result in patients previously unfamiliar with acupuncture choosing to access the modality.
Introduction
Use of specific modalities grouped under the heading of “complementary and alternative medicine” (CAM) has become increasingly widespread in the United States, and better understood over the past 3 decades. Surveys of CAM use include such therapies as herbal medicine, massage, megavitamins, self-help groups, folk remedies, energy healing, and homeopathy,1 with increasing attention being given to different subpopulations in the United States. One of the modalities regularly included is acupuncture. Interest in acupuncture has increased over time, resulting in training programs, licensing, and credentialing procedures. Growing professionalization of acupuncturists has led to some of them working within mainstream medical settings.2
Acupuncture is one of the CAM therapies most positively viewed by physicians. Twenty-five (25) surveys conducted between 1982 and 1995 showed that acupuncture had the highest rate of physician referral (43%), leading among the top five preferred CAM therapies (chiropractic, homeopathy, herbal medicine, and massage).3 One (1) recent survey showed that 41% of primary care physician respondents would consider participating in acupuncture research.4 In a 2002 national survey of CAM use in adults, 4.1% of the 31,044 respondents reported using acupuncture at least once in their lifetime, and 1.1% (representing 2.13 million Americans) reported use of acupuncture within the previous year. Recent use was associated with female gender, higher education, more frequent visits to regular physicians, self-reported poor health, specific illness such as back or neck pain, and living in areas where there was greater access to CAM providers. Insurance reimbursement for visits was also a factor.5,6
A small but growing number of studies have focused on minority patient use of CAM in general, and of acupuncture in particular.7–14 Moreover, data suggest that primarily “Asian” patients use acupuncture, whereas African American and Latino/Latina patients reportedly prefer other CAM modalities. One study of CAM use by minority women, for example, showed that of 1026 Chinese American women, 7.8% used acupuncture as compared with 2.5% of non-Hispanic white women (n = 747), 1.9% of Mexican Americans (n = 1057), and 0.9% of African American women (n = 1081). Multivariate models of CAM use indicate that ethnicity is independently associated with CAM modalities use, the use of CAM practitioners, and the health problems for which CAM is used.15
Even studies that do report on different minority groups generally do not focus on urban underserved patient populations. It is therefore not clear to what extent low acupuncture use by these populations represents a lack of familiarity, and/or the impact of actual barriers to access. According to an Institute of Medicine Report, minorities are less likely than whites to receive needed medical services.16 Disparities exist in specific disease areas and across a range of procedures. Moreover, to the extent that modalities such as acupuncture are not covered by insurance, but must be paid for out of pocket, cost can become a significant barrier.
There are even fewer data in relation to CAM use in pediatric populations, among whom the overall use of CAM has generally been studied in relation to specific illnesses17–23 and specific clinics.24 Predictors of CAM use by children include parental use, sociodemographics, the ability to pay out of pocket, and severity of illness.25 Insurance coverage can also be a factor.26 Such studies do not generally focus on the use of specific modalities such as acupuncture, although one study of patients referred by a pediatric pain service suggested that acupuncture is a reasonable addition to standard biomedical care, that it is tolerated by adolescents, and useful in helping to reduce pain and relieve anxiety.27 As in the case of adult underserved minority patients, the use of acupuncture by underserved pediatric populations has not been well studied.
For minority pediatric patients, barriers to accessing even conventional health care exist, and involve multiple risk factors such as race/ethnicity, poverty, parent education, insurance, and language.28 Parents have identified barriers such as not having the necessary skills and prerequisites for gaining access to the system, being alienated by front office experiences, and negative interactions with physicians.29
Against this backdrop, access to CAM therapies such as acupuncture for children may be further limited not only by financial barriers, but also by parents’ lack of familiarity with acupuncture, lack of physician knowledge about appropriate use, and the absence of acupuncturists in hospital or clinic settings. To the best of our knowledge, the availability of acupuncture for pediatric populations, with some notable exceptions, is limited to private clinics, and is rarely if ever provided in urban hospitals and neighborhood health clinics—sites where underserved minority patients are more likely to seek care. We hypothesized that it would be possible to integrate acupuncture fully into clinical services provided by an urban hospital serving these minority and underserved adolescents and pediatric patients. In light of growing efforts to integrate CAM services into mainstream medical settings,30–32 we also hypothesized that, if acupuncture were made available and affordable to underserved minority patients from different age groups, it would be increasingly accepted and utilized as a CAM modality.
Methods
To document the process of establishing this clinic, we collected and archived all related correspondence, memos, and meeting notes. In relation to the credentialing mechanism, we collected credentialing tools from other hospitals, and crafted a credentialing form relevant to acupuncture at Boston Medical Center (BMC). We posted information about the clinic supervisor, including experience and background, and about acupuncture, including information on appropriate referrals, to the hospital’s internal Web site. We also saved copies of all in-service presentations and educational materials for clinicians and patients. These materials were organized chronologically, and used as source materials with which to describe the process.
Patient visits in the Adolescent Center were kept in a weekly log. The supervisor tabulated results of patient visits for each week, month, and year. The following information was noted: (1) New or follow-up patient visit, (2) No shows/Cancellations, (3) Gender, (4) Walk-ins, and (5) Intern treating each patient. No chart review was used for any of this information. All the logs were recorded by the Supervisor and kept locked in the clinic when not in use. All clinic visits were tracked, and since patients were coming in through the Adolescent Center, and referred by pediatricians, most were in an age range of 8–27.
Results
Brokering agreements
A faculty member in the Department of Pediatrics at Boston University School of Medicine (L.B.) and a local non-physician acupuncturist experienced in working in hospital settings with pediatric patients (E.S.H.) facilitated a new relationship between Boston Medical Center (BMC) and the New England School of Acupuncture (NESA). Discussions were initiated with the Chief of Pediatrics at BMC and NESA’s President, and Academic and Clinical Deans. An agreement was reached whereby BMC would donate available clinic space during evening hours, as well as the use of support staff, in the ambulatory Adolescent Center (AC). NESA would place advanced students as Acupuncture Interns for semester-long rotations. A licensed acupuncturist from the NESA faculty would supervise the students, and NESA would compensate the acupuncture supervisor.
Adolescent patients already served by the AC would be able to access this new modality in a familiar and convenient setting, referred by their own pediatricians and nurses. Costs to the hospital would be minimal, as the new free-care acupuncture clinic would be located in an existing space during hours (5:30–8:30 PM) when most pediatricians were not in their clinical sessions. Although NESA has a history of creating externships in a variety of settings, this was the first to be located in a pediatric ambulatory clinic, with the benefit of working alongside hospital personnel.
Credentialing and integration
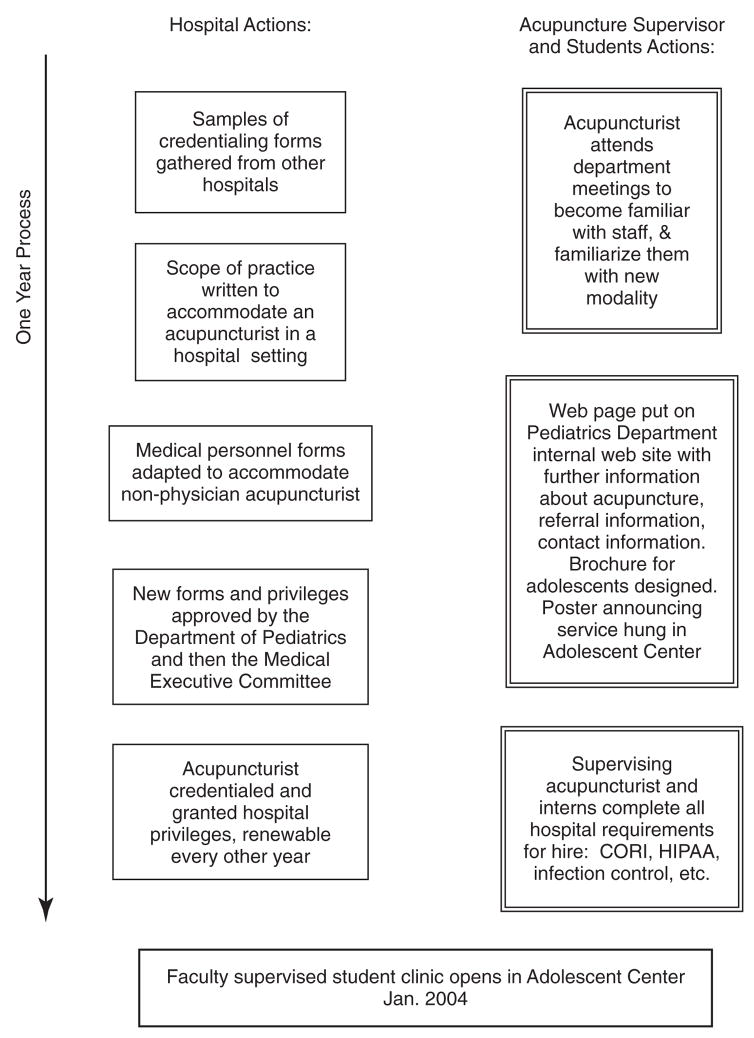
Figure 1 provides an overview of the steps taken to establish the clinic. For a licensed nonphysician acupuncturist to supervise the acupuncture interns in this setting, there was a need to design a new credentialing mechanism that was sufficiently standardized without being unduly burdensome.33 We collected samples of credentialing forms from other local hospitals with acupuncture services, and used them as models from which to create a credentialing instrument for BMC. It was reviewed and approved first by the Department of Pediatrics, and then by the hospital’s Medical Executive Committee. E.S.H. was then credentialed and granted hospital privileges as the acupuncture supervisor for the AC. While negotiations and credentialing processes were under way, she attended a series of all-staff meetings in the AC to familiarize staff with the uses, indications, and contraindications for acupuncture, and with appropriate procedures for making adolescent referrals. A web page about the acupuncture service was added to the Pediatrics internal hospital web site. It introduced E.H.S. and provided information for providers about acupuncture, along with contact information. This entire process took approximately 1 year. The acupuncture supervisor, as well as the acupuncture interns, adhered to usual hospital requirements such as Criminal Offender Record Information (CORI) checks, tuberculosis screening, Health Insurance Portability and Accountability Act, and infection control training.
FIG. 1.
Overview of steps taken to establish a free-care acupuncture clinic. CORI Criminal Offender Record Information; HIPAA, Health Insurance Portability and Accountability Act.
The adolescent center free-care clinic opens
The acupuncture clinic opened in January 2004 in the AC, with a once-a-week, 3-hour, evening free-care acupuncture service (see Appendices 1 and 2: the BMC Acupuncture Practice Policy and Acupuncture Privileges Form.) The new service was integrated into the regular clinic routine as seam-lessly as possible, making it similar to other specialty clinics operating out of the space, such as the pediatric human immunodeficiency virus positive and pediatric obstetrics/gynecology clinics. Our larger goal was to work toward a fully integrated service.
We began this integration in three key ways: (1) handling of patient appointments by the same staff that managed regular pediatric appointments; (2) adapting the hospital’s electronic medical record system so that physicians and nurses could enter a referral for acupuncture, acupuncturists could enter patient notes, and the referring physician and other providers could review these notes; and (3) training the acupuncture preceptor and interns in the use of the electronic medical record system.
While first building a patient base, E.H.S. and the interns provided acupuncture treatments for interested physicians, nurses, and other staff, positing that familiarity with the modality would increase patient referrals. The medical, nursing, and support staff at the AC not only availed themselves of acupuncture treatments; they also shared their conference room with the acupuncture team, which facilitated a collegial teaching and learning environment. It allowed staff to ask the team questions about acupuncture, and the acupuncture interns to ask questions about various disease states. Referrals came from pediatricians, nurses, and other medical staff in the AC. Pediatrics residents and medical students doing their Pediatrics clerkship were encouraged to shadow the team when possible. Some subsequently referred patients and followed up on the results.
Acupuncture also needed to be introduced to patients and their parents. The preceptor and students provided direct patient education through discussions and literature during consultations, as requested by the pediatricians. A hospital-approved poster was placed in the waiting area and restroom in the AC. An age-appropriate and visually appealing brochure was left in informational pockets in each treatment room. Patients made appointments and checked in through the regular front desk staff. They were seen in the regular treatment rooms. As the acupuncture interns were placed at this clinic to enhance their training, each of them usually saw about one patient per hour (sometimes less, depending on patient attendance) for intake and treatment.
Following NESA protocols, all new patients were given a health history form to fill out, and were instructed to leave any areas blank if they did not know how to fill them in. On the first visit, the intern reviewed a consent form for acupuncture treatment with the patient and asked them to sign it. Patients under 18 years were asked to have their parents sign. Patients were asked to agree to come for a total of at least four treatments in order to determine whether acupuncture would benefit them. NESA interns were able to access full medical records in the electronic medical record system for all in-coming patients, in order to check previous history and current medications. All acupuncture treatments, including Traditional Chinese Medical diagnosis and treatment-point selections, were also entered into the electronic record.
Providers referred outpatients most commonly for headaches (including migraines), injuries related to motor vehicle accidents, back pain, tobacco smoking, substance use, asthma, joint pain, sickle cell disease, and stress. In 2004 the interns provided a total of 147 acupuncture treatments to 40 different patients. In addition, 9 staff were also treated. Patients’ ages ranged from 11 to 27 years old. Older patients were often “referred” by their children, friends or other relatives. We asked that the adolescents return for at least 4 visits, but many of them found the acupuncture helpful enough to return for many more.
Data were kept for female versus male visits. In 2004, male visits to the Adolescent Acupuncture Clinic were 12.3% of the total visits (n = 18). In 2005, male visits comprised 2.3% of the total visits (n = 4), and in 2006, male visits comprised 20% of the total visits (n = 45).
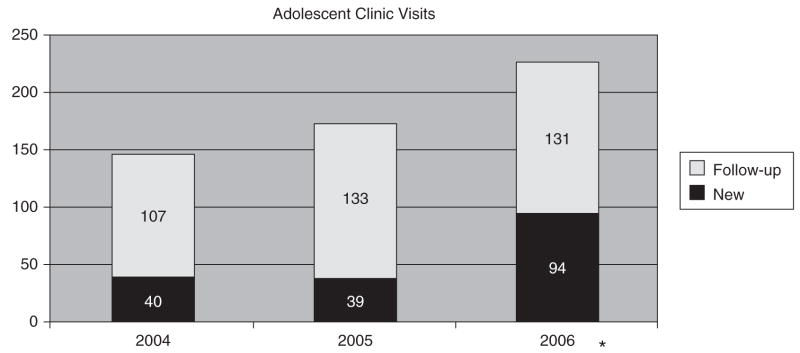
During 2005, efforts to publicize the AC clinic at BMC continued, with a resulting increase in the number of patients receiving acupuncture. The total number of visits saw an increase of 15% in 2005. There was a decrease in male attendance during 2005 that is unexplained. In 2006, the AC clinic expanded to include adult patients from the Family Medicine Department. These patients also received acupuncture at no cost. Figure 2 and Table 1 show the volume of patient visits over 3 years.
FIG. 2.
Externship clinic visits 2004–2006. *Clinic attendance in 2006 included adults from family medicine.
Table 1.
Total numbers of Patient Visit to the Free-Care Adolescent Acupuncture Clinic
| 2004 | 2005 | 2006 | Totals | |
|---|---|---|---|---|
| Total treatments delivered | 147 | 173 | 225 | 545 |
| Number of new patients | 40 | 39 | 94 | 173 |
| Number of follow-up visits | 107 | 133 | 131 | 372 |
| Total males | 18 | 4 | 45 | 67 |
| Total females | 126 | 169 | 180 | 475 |
| Number of walk-ins | 11 | 21 | 20 | 52 |
| Total cancels/no shows | 56 | 78 | 90 | 224 |
| Number of new patient no shows | 24 | 26 | 47 | 97 |
Discussion
We had hypothesized that it would be possible to integrate an acupuncture service successfully into the care provided by a large urban hospital that serves primarily underserved minority and immigrant patient communities, many of whom are among the city’s most economically marginalized and/or working poor. Data were not kept on patients’ ethnicities, but, because the patients were drawn from the patient population of the existing adolescent clinic, patients from the Dominican Republic, Haiti, Cape Verde, Nigeria, Peru, as well as African Americans and European Americans were all represented in the acupuncture clinic’s population.
BMC is a large urban hospital that draws its population mainly from the surrounding neighborhoods. The population of Boston in 2005 was 520,702.15 Demographically, the population is 45% white, 25% black, 15% latino, 9% Asian, and 6% other. The poverty rate for individuals is 22.3%—well above the 13.3% observed nationally. The poverty rate for families is also high (17.8% compared to 10.2% nationally).34 Providing a free service is within the hospital’s mission of “exceptional care without exception” and is particularly necessary for acupuncture services, since Massachusetts health insurance companies do not reimburse licensed acupuncturists. Economic barriers and lack of insurance reimbursement have restricted access to acupuncture to only those who can pay out of pocket, or to patients with access to services that are subsidized or free. For patients who already face multiple barriers to accessing care, and who have little to no familiarity with acupuncture, there may be little opportunity to try the modality.
Our experience indicates, however, that when barriers to access are reduced, both pediatric and adult patients from underserved minority patient groups will utilize acupuncture and, in some cases, will make it an ongoing part of their care. Utilization of acupuncture was not limited to specific disease states, but instead spanned multiple disorders, indicating that a wide age range of patients were willing to seek acupuncture for diverse health problems, such as pain, stress, headaches, and fatigue. Our experience suggests that when such clinics are implemented, patients will indeed come.
Six factors contributed to this clinic’s feasibility (Appendix 3). First was the presence of an urban hospital with an acupuncture school in close proximity. Second, the cultures of both BMC and NESA encourage leadership and innovation. Both institutions were willing to embark on a small but serious experiment involving integration of a CAM modality into a conventional biomedical clinic. Third, faculty from both institutions were willing to take responsibility for the necessary institutional steps (e.g., developing the credentialing mechanism, and brokering the relationship between the two institutions). Fourth, the acupuncture supervisor and interns were willing to invest time in providing extensive in-service training and treatment experience for hospital staff, thus ensuring that staff understood the modality and could make knowledgeable referrals. Fifth, BMC’s inner city location made it easier for underserved patient communities to access the free-care acupuncture clinic and to gain exposure to the modality. Patient utilization correlated strongly with the amount of education and exposure that the medical staff received in relation to the availability of acupuncture, and its potential risks and benefits. Finally, the externship model allowed costs for care to remain low, making the collaboration financially feasible. The externship model has the potential for sustainability, because it is not dependent on outside funding or on reimbursement for services.
Many questions still remain as to why these patients chose to come for acupuncture originally and why they returned. Future work will survey clinic users to understand more clearly reasons for choosing acupuncture, patient satisfaction, and perceived efficacy of these interventions.
Acknowledgments
The authors wish to acknowledge the staff of the BMC Adolescent Center, Kathy Seltzer, Academic Dean New England School of Acupuncture, and Mary McLellan, Children’s Hospital Boston, for help with charts. Dr. Barnes was supported by a grant from the Ford Foundation. Dr. Saper was supported by a Career Development Award (K07 AT002915-03) from the National Center for Complementary and Alternative Medicine, National Institutes of Health.
Appendix 1. Boston Medical Center Department of Family Medicine Delineation of Privileges
ACUPUNCTURE PRACTICE POLICY
APPROVAL
Acupuncture may be performed only by an acupuncturist or a fully licensed physician duly licensed by the Common-wealth of Massachusetts. No member of the BMC Department of Family Medicine may practice acupuncture at Boston Medical Center, its outpatient facilities, and affiliated clinics until his/her credentials and qualifications have been approved by the Chairman of the Department of Medical Executive Committee as described below.
-
Criteria
-
For licensed acupuncturists, the individual must:
provide a copy of a valid and current Massachusetts license to practice acupuncture;
provide a copy of the most recent completed Massachusetts application form for acupuncture licensure;
provide three (3) letters of recommendation from colleagues or teachers knowledgeable in the individual’s competency and professionalism as an acupuncturist.
provide proof of malpractice insurance
satisfactorily complete health screening procedures as required by Occupational Health Services.
-
For physicians, the individual must:
be a member of the BMC medical staff with current privileges and licensure;
have successfully completed at least two hundred (200) hours of graduate training in medical acupuncture of AMA category I certified programs or equivalents thereof, as determined by the American Academy of Medical Acupuncture;
provide three (3) letters of recommendation specifically addressing the individual’s abilities and experience in acupuncture.
provide satisfactory evidence of at least thirty (30) accredited hours, over a three (3) year period, of continuing education in medical acupuncture.
Renewal of medical staff privileges shall include a review of the individual’s clinical experience and/or quality assurance data with regard to the practice of acupuncture.
-
Appendix 2. Acupuncture Privileges Form
| Print Name | |
| (Check those requested) | |
| —— | Outpatient consultations |
| —— | Inpatient consultations |
| —— | Pediatric acupuncture (0–17 years old) |
| —— | Adult acupuncture (≥18 years old) |
| —— | Pregnancy, labor and delivery |
| —— | Access to and documentation in medical record |
| —— | Performance of traditional Chinese physical diagnosis and assessment |
| —— | Placement of acupuncture needles |
| —— | Stimulation of acupuncture needles manually, electrically, or thermally |
| —— | Ear acupuncture |
| —— | Noninvasive modalities including traditional Asian therapeutic massage and cupping |
| Signature of Applicant | Date |
| Signature of Department Chair | Date |
Appendix 3. Six Factors Leading to Integration of Free-Care Acupuncture Clinic in an Urban Hospital
Hospital and acupuncture school in close proximity.
Cultures in both institutions encourage leadership and innovation.
Willingness of both institutions to make internal changes; create new credentialing/new privileging, create new externship site.
Willingness of supervisor, interns, and hospital staff to be educated in each other’s modalities, recording-keeping methods, etc. Willingness on both sides to seek each other’s expertise. Willingness of hospital staff to try acupuncture for themselves.
BMC’s inner city location made it possible for patients to utilize the clinic easily.
Externship model keeps costs low.
References
- 1.Upchurch DM, Chyu L, Greendale GA, et al. Complementary and alternative medicine use among American women: Findings from the National Health Interview Survey, 2002. Journal of Women’s Health. 2007;16:102–113. doi: 10.1089/jwh.2006.M074. [DOI] [PubMed] [Google Scholar]
- 2.Barnes LL. The acupuncture wars: The professionalizing of acupuncture in the United States. A view from Massachusetts. Med Anthro. 2003;22:261–301. doi: 10.1080/01459740306772. [DOI] [PubMed] [Google Scholar]
- 3.Astin J, Marie A, Pelletier KR, et al. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med. 1998;158:2303–2310. doi: 10.1001/archinte.158.21.2303. [DOI] [PubMed] [Google Scholar]
- 4.van Haselen RA, Reiber U, Nickel I, et al. Providing complementary and alternative medicine in primary care: The primary care workers’ perspective. Complement Ther Med. 2004;12:6–16. doi: 10.1016/S0965-2299(03)00140-7. [DOI] [PubMed] [Google Scholar]
- 5.Burke A, Upchurch DM, Dye C, Chyu L. Acupuncture use in the United States: Findings from the National Health Interview Survey. J Altern Complement Med. 2006;12:639–648. doi: 10.1089/acm.2006.12.639. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg DM, Davis RB, Ettner SL, et al. Insurance coverage, medical conditions, and visits to alternative medicine providers: Results of a national survey. Arch Intern Med. 2002;162:281–287. doi: 10.1001/archinte.162.3.281. [DOI] [PubMed] [Google Scholar]
- 7.Mackenzie ER, Taylor L, Bloom BS, et al. Ethnic minority use of complementary and alternative medicine (CAM): A national probability survey of CAM users. Altern Ther Health Med. 2003;9:50–56. [PubMed] [Google Scholar]
- 8.Najm W, Reinsch S, Hoehler F, Tobis J. Use of complementary and alternative medicine among the ethnic elderly. Altern Ther Health Med. 2003;9:50–57. [PubMed] [Google Scholar]
- 9.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;27:1–19. [PubMed] [Google Scholar]
- 10.Graham RE, Ahn AC, Davis RB, et al. Use of complementary and alternative medical therapies among racial and ethnic minority adults: Results from the 2002 National Health Interview Survey. J Natl Med Assoc. 2005;97:535–545. [PMC free article] [PubMed] [Google Scholar]
- 11.Ortiz Bi, Shields KM, Clauson KA, Clay PG. Complementary and alternative medicine use among Hispanics in the United States. Ann Pharmacother. 2007;41:994–1104. doi: 10.1345/aph.1H600. [DOI] [PubMed] [Google Scholar]
- 12.Brown CM, Barner JC, Richards KM, Bohman TM. Patterns of complementary and alternative medicine use in African Americans. J Altern Complement Med. 2007;13:751–758. doi: 10.1089/acm.2006.6392. [DOI] [PubMed] [Google Scholar]
- 13.Xu KT, Farrell TW. The complementarity and substitution between unconventional and mainstream medicine among racial and ethnic groups in the United States. HSR Health Serv Res. 2007;42:811–826. doi: 10.1111/j.1475-6773.2006.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moyad MA, Lusk W, Schwartz LR. Alternative medicine utilization by African Americans and improving life expectancy: Is there a correlation? Urol Nurs. 2007;27:449–451. [PubMed] [Google Scholar]
- 15.Kronenberg F, Cushman LF, Wade CM, et al. Race/ethnicity and women’s use of complementary and alternative medicine in the United States: Results of a national survey. Am J Pub Health. 2006;96:1236–1242. doi: 10.2105/AJPH.2004.047688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smedley BD, Stith AY, Nelson AR, editors. [Accessed March 2, 2007];Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care 2006. Online document at: http://nap.edu/catalog/10260.html. [PubMed]
- 17.Dune LS, Shiao SYPK. Metaanalysis of acustimulation effects on postoperative nausea and vomiting in children. Explore. 2006;2:314–320. doi: 10.1016/j.explore.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Gottschling S, Langler A, Tautz C, Graf N. Complementary and alternative medicine in pediatric oncology. Klin Padiatr. 2006;218:157–164. doi: 10.1055/s-2006-933400. [DOI] [PubMed] [Google Scholar]
- 19.Ladas EJ, Post-White J, Hawks R, Taromina K. Evidence for symptom management in the child with cancer. J Pediatr Hematol Oncol. 2006;28:601–615. doi: 10.1097/01.mph.0000212989.26317.52. [DOI] [PubMed] [Google Scholar]
- 20.Reindl TK, Geilen W, Hartmann R, et al. Acupuncture against chemotherapy-induced nausea and vomiting in pediatric oncology: Interim results of a multicenter crossover study. Support Care Cancer. 2006;14:172–176. doi: 10.1007/s00520-005-0846-z. [DOI] [PubMed] [Google Scholar]
- 21.Miller V, Michels H. Complementary and alternative medicine in pediatric rheumatology. Aktuelle Rheumatol. 2005;30:195–198. [Google Scholar]
- 22.Streitberger K, Ezzo J, Schneider A. Acupuncture for nausea and vomiting: An update of clinical and experimental studies. Autonom Neurosci. 2006;129(sp iss SI OCT 30 1–2):107–117. doi: 10.1016/j.autneu.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 23.Li YC, Ly H, Golianu B. Acupuncture pain management for patients with cystic fibrosis: A pilot study. Am J Chi Med. 2005;33:151–156. doi: 10.1142/S0192415X05002758. [DOI] [PubMed] [Google Scholar]
- 24.Hughes SC, Wingard DL. Children’s visits to providers of complementary and alternative medicine in San Diego. Ambul Pediatr. 2006;6:293–296. doi: 10.1016/j.ambp.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Yussman SM, Ryan SA, Auinger P, Weitzman M. Visits to complementary and alternative medicine providers by children and adolescents in the United States. Ambul Pediatr. 2004;4:429–435. doi: 10.1367/A03-091R1.1. [DOI] [PubMed] [Google Scholar]
- 26.Bellas A, Lafferty WE, Lind B, Tyree PT. Frequency, predictors, and expenditures for pediatric insurance claims for complementary and alternative medical professionals in Washington state. Arch Pediatr Adolesc Med. 2005;159:367–372. doi: 10.1001/archpedi.159.4.367. [DOI] [PubMed] [Google Scholar]
- 27.Kemper KJ, Sarah R, Silver-Highfield E, et al. On pins and needles: Children’s experience with acupuncture. J Ambul Pediatr Assoc. 2000;105:941–947. [PubMed] [Google Scholar]
- 28.Stevens GD, Halfon N, Seld M, Mistry R. Disparities in primary care for vulnerable children: The influence of multiple risk factors. Health Serv Res. 2006;41:507–531. doi: 10.1111/j.1475-6773.2005.00498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sobo EJ, Seid M, Reyes Gelhard L. Parent-identified barriers to pediatric health care: A process-oriented model. Health Serv Res. 2006;41:148–172. doi: 10.1111/j.1475-6773.2005.00455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santa Ana CF. The adoption of complementary and alternative medicine by hospitals: A framework for decision-making. J Healthc Manag. 2001;46:250–260. [PubMed] [Google Scholar]
- 31.Giordano J, Boatwright D, Stapleton S, Huff L. Blending the boundaries: Steps toward an integration of complementary and alternative medicine into mainstream practice. J Altern Complement Med. 2002;8:897–906. doi: 10.1089/10755530260511892. [DOI] [PubMed] [Google Scholar]
- 32.Highfield ES, Kaptchuk TJ, Kemper KJ, et al. Availability of acupuncture in the hospitals of a major academic medical center. Complement Ther Med. 2003;11:177–183. doi: 10.1016/s0965-2299(03)00069-4. [DOI] [PubMed] [Google Scholar]
- 33.Eisenberg DM, Cohen MH, Hrbek A, et al. Credentialing complementary and alternative medical providers. Ann Intern Med. 2002;137:965–973. doi: 10.7326/0003-4819-137-12-200212170-00010. [DOI] [PubMed] [Google Scholar]
- 34.US Census. [Accessed August 2, 2007];American Community Survey, Boston Massachusetts. 2005 Online document at: http://factfinder.cen-sus.gov.