Abstract
Background and purpose
Changes of the major forebrain commissures in lissencephaly have not been systematically studied. This study investigated the developmental differences of the commissures in patients with varying types of lissencephaly to determine whether specific commissural features may help in distinguishing among lissencephaly phenotypes.
Materials and methods
MRI of 124 patients were retrospectively reviewed. Patients were classified as classic(cLIS), variant(vLIS) and Cobblestone lissencephaly(CBSC) according to cortical phenotype; few patients had genetic diagnoses. Abnormalities of the corpus callosum, anterior (AC), and hippocampal commissures (HC) were recorded, and the overall shape was regarded as hypogenetic, hypoplastic, dysmorphic, angled splenium and convex corpus compared with ge matched controls. Correlations between commissural characteristics and cortical patterns were analyzed using Monte Carlo simulation of chi-square, ‘extention to mxn table’, and Fisher’s exact tests as appropriate (p<0.05).
Results
Patients were classified as cLIS (57.4%), vLIS (38.4%) or CBSC (4.2%). The most common callosal developmental anomaly was hypogenesis with absent rostrum, small inferior genu and small splenium. An angled (90°) splenium was found to be significantly associated with cLIS; and excessively convex corpus callosum with VLDLR mutations. ACC with enlarged anterior commissure was found in all ARX mutations.
Conclusion
Specific patterns of the commissure anomalies were associated with certain types of lissencephaly. Callosal anomalies were more common than those of AC or HC. Developmental differences of commissures may be useful as an imaging criterion in differentiating the groups of lissencephalies and may give insight into the processes causing these malformations.
INTRODUCTION
Cerebral corticogenesis includes three major steps: 1) cell proliferation, 2) cell migration and differentiation and, 3) cortical organization with formation of mature cortex (1). Lissencephalies result from impaired migration of neurons from germinal matrices to the developing cerebral cortex (1–4). Disruption of normal neuronal migration can result from many different genetic and environmental disturbances; the result is usually a major brain malformation, including many types of heterotopia, lissencephaly, and cobblestone malformations (also called dystroglycanopathies because they result from abnormal glycosylation of alpha-dystroglycan) (4–9).
Lissencephalies were previously divided into 2 distinct groups: type I (classic) and type II (cobblestone). Recently, this classification has been expanded and the groups separated on the basis of pathologic, imaging, and genetic features (4,8,10). A recently proposed classification includes: LIS1 and DCX, mutations causing classic lissencephalies; ARX, RELN, and VLDLR mutations and 2-layered cortex causing vLIS; and FCMD, FKRP, LARGE, POMT1, POMT2, and POMGnT1 mutations causing CBSC (10). Almost all patients have neonatal hypotonia, epilepsy, and little developmental progress. The diagnosis is difficult when based only on clinical and laboratory findings, which are time-consuming and expensive. Fortunately, typical imaging features have been described in association with many mutations causing lissencephalies. This imaging phenotypic characterization may help in differentiating among these malformations (11–35).
Various anomalies of the major forebrain commissures, namely the CC, the AC and the HC, are commonly observed in human lissencephalies. The aim of our study was to investigate and categorize the developmental differences of the forebrain commissures in a large group of patients encompassing all lissencephaly types (classical, variant and cobblestone) to determine if specific features of size and shape may help to distinguish among the lissencephaly phenotypes.
MATERIALS AND METHODS
MRI scans or portions of MRI scans of 124 patients were retrospectively reviewed. The scans were acquired from the private teaching collection of the senior author, acquired over 23 years, from the teaching file of the Radiology Department at our institution (searching using lissencephaly, agyria, pachygyria, band heterotopia, cobblestone malformation, and congenital muscular dystrophy as key words), and from MRIs reviewed for a grant studying the genetics of epilepsy. The MRIs were included only if they had good quality images through the cerebrum (to assess the type and severity of the cortical malformation) and through the cerebral commissures as determined by a consensus of the authors. All studies included T1-weighted and T2-weighted images with scans performed in at least two planes (sagittal and axial). All cases included were confirmed unanimously by the authors to show agyria, pachygyria, or cobblestone cortex in some part of the cerebrum. As the cases were largely from radiological referrals, clinical information was usually rather sparse (typically including only a short report describing developmental delay, seizures, and family history) or, in some cases, completely absent. Sixteen cases without midsagittal images, and six with only CT images were excluded. Eight patients with Walker-Warburg disease who had severe hydrocephalus limiting assessment of some commissural structures were also excluded. The available data of the remaining 94 patients showed a mean age of 5.5 ± 7.5 years (range: 1 day to 32 years;, median: 2 years) at the time of imaging. The group included 33 females, 44 males, and 17 with unavailable gender information.
MRIs of 50 gender- and age-matched patients who were scanned for headaches, suspected macrocephaly, or epilepsy and interpreted as normal by a board-certified neuroradiologist were reviewed as controls. The lack of abnormality was confirmed unanimously by all authors in all cases. These control MRIs established the normal appearance of the forebrain commissures for comparison with our patients. All control MRIs had sagittal T1-weighted images, axial T1-weighted images, and axial and coronal T2-weighted images with slice thickness of 3–5 mm.
The authors reviewed the cases jointly with special attention to the cortical involvement. The patients were then classified to a presumed genotype based upon the imaging phenotype. Information about genotype was available only for a small percentage of our patients, because most were studied before the genetic tests for lissencephalies (LIS1, DCX, TUBA1A, ARX, VLDLR, RELN) or cobblestone malformations (FCMD, FKRP, POMT1, POMT2, LARGE, POMGnT1) were available. These many patients were classified as presumed (p) genotypes, (p)LIS1, (p)DCX, (p)ARX, (p)RELN, (p)VLDLR, if the imaging findings were highly suggestive of a specific gene mutation as detailed in a previous paper (10). Cobblestone malformations were not subclassified, since it has been well established that mutations of many glycosyltransferase enzyme genes can cause any of the clinical phenotypes; the clinicoradiologic phenotype is more dependent on the severity of the mutation (and presumably other, still unknown causes) than on the gene that is mutated (9, 34–36). All cases with ARX had a genetically proven diagnosis. All mutations (proven and presumed) were further grouped together into the three main groups such as cLIS, vLIS and CBSC for comparisons of imaging features.
We assessed the forebrain commissures, white matter volume, and myelination for each patient and compared these features with respect to main groups. We compared the shapes of the CC in the midsagittal plane with those in the control group. The shape and size of each commissure was determined by visually comparing each subject with age-matched controls. As there is significant variation in the size of the callosal components and of the commissures with age, as well as some variation among controls of the same age, only those commissures and callosal components judged unanimously by the three authors as significantly different from controls were graded as abnormal. The CC was categorized as follows.
-
Developmental appearance
Agenesis (absence of the entire CC), hypogenesis (absence of the rostrum associated with small or absent splenium, small or absent inferior genu), hypoplasia (all parts formed, but decreased thickness, presumably due to reduced number of crossing axons, of any part of the CC), dysmorphic (abnormal shape of any part of the CC, presumably due to abnormal development).
-
Size of parts (rostrum, genu, body, splenium) and overall shape of the CC
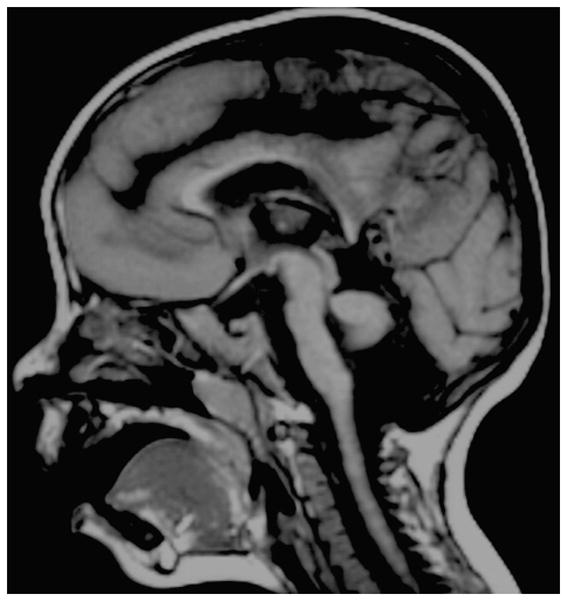
Changes in size and shape of at least one part or another of the CC led us to observe mainly two recurrent overall callosal shapes in a large number of patients. Some had an absent rostrum, small inferior genu, and small splenium with a convex upward shape and a sharp angle at the level of the midcallosal body (Fig. 4). Other patients had absence of the rostrum, small inferior genu, abnormally thin flat callosal body, and a sharp angle (about 90 degrees) between the body and a vertical splenium (Fig. 5). These specific features were reminiscent of a hypogenetic dysmorphic CC.
Figure 4.

Figure 5.
The HC and AC were assessed on midsagittal T1 and coronal T1 or T2 weighted images. Coronal images were particularly helpful for assessment of the HC as it connects the fornices and is usually largest immediately anterior and inferior to the callosal splenium. The size of the commissures was graded by visual assessment as small, normal or enlarged compared with the control group.
The degree of myelination was reviewed and compared with the standards for the patient’s age (36). For patients less than one year old, myelination more than 2 months below standards for age was considered as delayed. For infants between one- and two years old, myelination more than 3 months below standards was considered as delayed. For children beyond their second birthday, only grossly reduced cerebral myelination was recorded as delayed. When a patient’s age could not be determined or the images were insufficient for reviewing the myelination, it was recorded as non-assessed (NA). White matter volume was visually assessed by the authors and considered as normal or reduced. The proximity of cortical sulci to the lateral margins of the cerebral ventricles and the relative ratio of white matter to ventricular size after comparison with normal controls were the criteria used for this assessment. Consensus was achieved among the authors for all cases; patients with questionable findings but close to normal status were considered to be normal.
Statistical comparisons of overall callosal shapes between classical and variant groups were carried out by the ‘extension to mxn table, Monte Carlo simulation of chi-square and Fisher’s exact tests as appropriate. ACC, hypogenesis, hypoplasia, angled splenium, convex corpus and normal shape underwent statistical comparisons. A p value less than 0.05 was considered as significant. All statistical analyses were performed with the Statistical Package for Social Sciences (SPSS, version 15.0, Chicago, IL, USA).
RESULTS
Among our 94 patients, 23 (24.46%) patients had a confirmed genetic diagnosis. 57.4% were classified as cLIS (LIS1=3.7%, (p)LIS1=53.7%, DCX= 11.1%, (p)DCX= 29.6%, and 1 patient with no mutation), 38.4% as vLIS (ND= 58.3%, RELN= 2.8%, (p)RELN= 5.5%, ARX=11.1%, VLDLR= 5.5%, (p)VLDLR= 16.6%), and 4.2% had cobblestone complex (CMD-ND= 50% and MEBD= 50%).
Most of the cases had developmental abnormalities of the forebrain commissures. The CC was more commonly affected than the AC and HC. The CC was most often hypogenetic and dysmorphic. This appearance of CC clearly differed from that seen in the control group. Combining the proven and presumed same mutation groups, we applied statistics to evaluate group differences based on the forebrain developmental abnormalities.
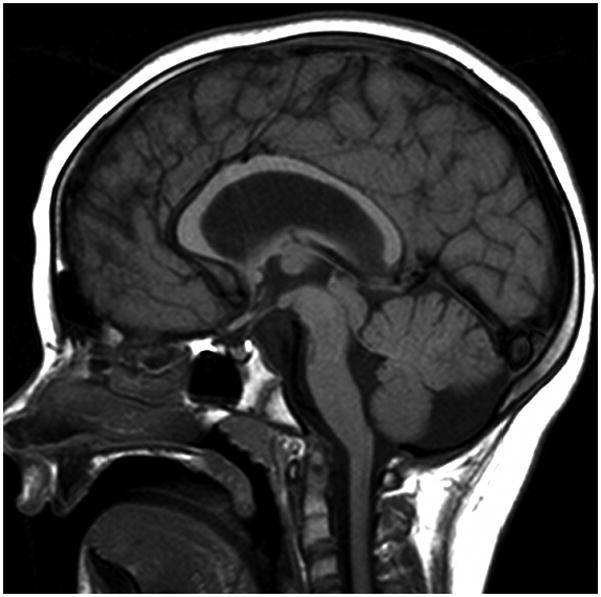
In cLIS, most of the LIS1 patients (70.9%) had callosal hypogenesis (Fig. 1) with a thin flat body and vertical splenium shape in about half cases (48.4%) (Fig. 5), which made a significant difference between LIS1 and other groups (p=0.011). The AC and HC were normal in most of the cases. In DCX patients, we found hypogenetic CC (68.1%) with no specific dysmorphic shape. The AC and HC were mostly normal.
Figure 1.
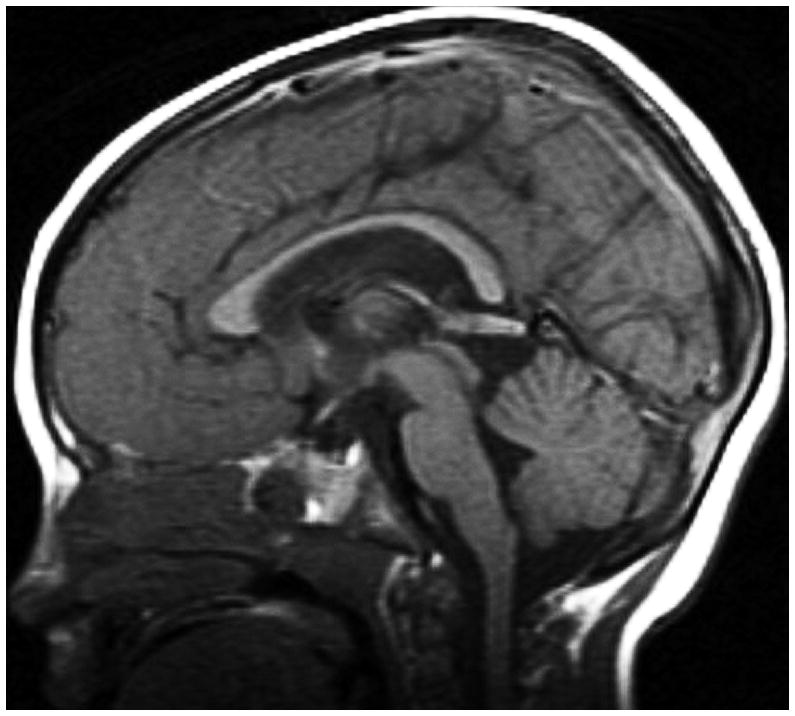
In vLIS group, all ARX patients had ACC with enlarged AC (Fig. 6). The patients with RELN mutation phenotype had a hypoplastic CC in all cases with absent (33%) or small (66%) inferior genu. The AC was absent in 66% while the HC was normal in all. The VLDLR phenotype was significantly associated with a hypogenetic convex upward CC body which differed from other groups (p=0.011). The AC was predominantly small (62.5%) and the HC was mostly non assessed (75%). The shape of the CC showed a significant difference between the cLIS and vLIS groups (p=0.017). The CBSC patients typically had absent rostrum (75%), a thin or normal genu (75%), a thin or normal body (75%), and a thin splenium (50%). Because many of these patients had hydrocephalus or shunted hydrocephalus, the CC was often distorted and had variable general appearances. Patients without severe hydrocephalus often had a smoothly arched callosal body (Fig. 4). The AC and HC were normal in half of the cases.
Figure 6.
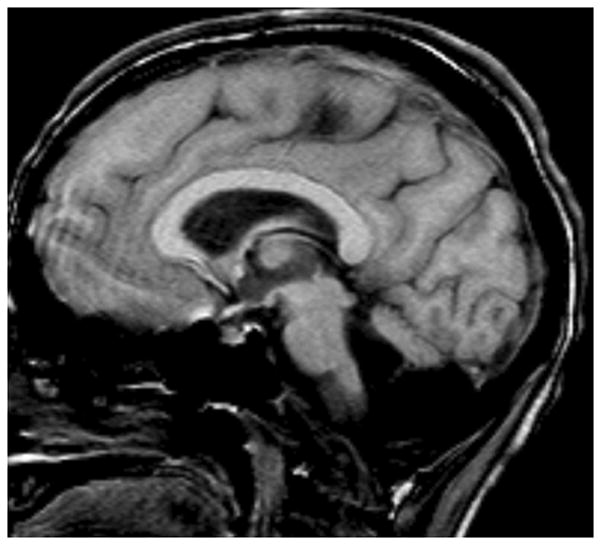
Myelination was normal in 43.6% of all lissencephaly cases. Sixty-four percent of cLIS and 18.9% of vLIS patients showed normal myelination. Delayed myelination was found in half of the vLIS cases. The white matter volume was regarded as normal in only 6.4% of cases who had a normal CC (Fig. 7). The remaining patients (93.6%) had differing severities of reduced white matter volume. All cases in vLIS group showed reduced white matter volume.
Figure 7.
Considering the components of the CC, the rostrum was absent in 70.3% of cLIS and in 75% of vLIS cases. The genu was absent in only 7.4% of cLIS but in 30.6% of vLIS. A small inferior part of the genu was found in 59.3% of cLIS and in 38.9% in of vLIS patients. A thin flat body was seen more commonly in cLIS; it was frequently convex upward in vLIS patients (as stated above). The splenium was normal in only 18% of all patients. When it was not associated with a particular overall shape of the CC as previously defined, it appeared small in all other cases when seen. Statistical results are summarized in Table 1.
Table 1.
Significant differences between the major types of lissencephaly for each structure and specific features.
| Structure | Groups compared and associated features | p value |
|---|---|---|
| Splenium | cLIS – vertical or thin vLIS – absent or thin, and small |
p< 0.001 |
| Brain involvement | cLIS – pachygyria (P>A, central, A>P) vLIS – pachygyria entire brain |
p< 0.001 |
| Myelination | cLIS - normal vLIS – delayed |
p< 0.001 |
| CC genu | cLIS – small inferior or N vLIS – absent or small inferior CBSC – normal genu |
p= 0.002 |
| HC | cLIS – normal | p= 0.003 |
| AC | cLIS – normal or small vLIS – absent |
p= 0.047 |
| CC body | cLIS – normal or flat thin vLIS – convex upward |
p= 0.011 |
DISCUSSION
This detailed review of a large number of MRI scans of patients with various types of lissencephaly showed developmental abnormalities of the major forebrain commissures almost in all patients ; the CC was the commissure most commonly involved. This result is not surprising, as the CC is composed of axons from cerebral cortical neurons which are abnormal in location and possibly in function in lissencephalies (37). Neurites from these abnormal neurons might be expected to experience errors in pathfinding through the many signals that normally guide them across the midline in the developing brain (38–39). Although many variations were seen, the most common anomaly consisted of absent rostrum, small inferior genu, and small or abnormally shaped splenium: this configuration has been defined as hypogenetic (36,40). In addition, malformations secondary to specific mutations and presumed mutations seemed to have a characteristic overall shape of the CC.
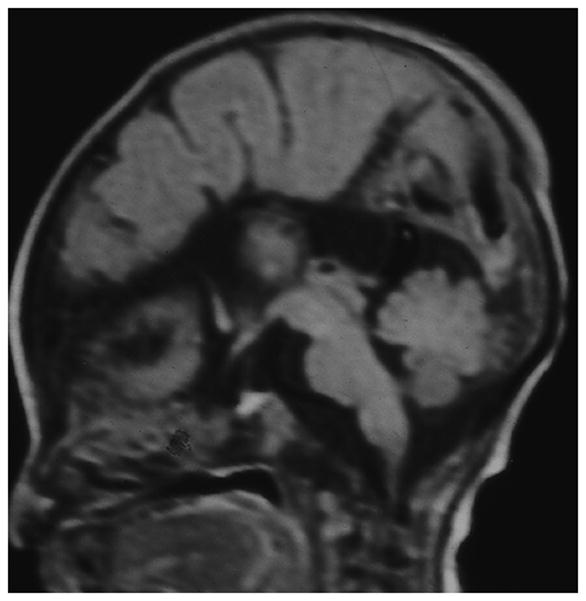
The LIS1 patients had predominantly callosal hypogenesis with thin flat body and vertical splenium shape (Fig. 5) while the DCX phenotype was significantly associated with hypogenetic CC without any specific overall CC shape. ARX mutation with the XLAG phenotype is known to have callosal agenesis in nearly all cases (by definition). Therefore, finding ACC in our ARX patients was expected. ACC was also found in other vLIS cases and could potentially be used to differentiate cLIS from vLIS. The RELN patients mainly had a hypoplastic CC (Fig. 2), while the CC in VLDLR patients was generally hypogenetic with a convex upward body shape (Fig. 4). The CBSC patients were included even though they have distinctive characteristic MRI features of the cerebral cortex and posterior fossa structures, because we aimed to explore the forebrain commissures within the full range of lissencephalies. We thus propose to include our findings in the differential criteria of various lissencephaly MRI phenotypes.
Figure 2.
The AC and the HC were assessed along with the CC since all are composed of axons from cortical neurons crossing through the cerebral midline (40). Thus, some developmental disturbances affecting the midline crossing callosal axons might be expected to involve the other commissures as well. Absence of the AC was common in patients with vLIS, and its enlargement was consistently detected in ARX (along with ACC). The significance of such enlargement is unclear. Regarding the HC, it was enlarged in some vLIS patients, but this appearance was not helpful in differentiating among the lissencephalies groups.
The developmental differences of forebrain commissures in various types of lissencephalic cortical malformations are likely related to the causes of these malformations, which means the effects of gene mutations on neurogenesis, neuronal migration, and neurite development. Axons from abnormal neurons or from neurons in abnormal locations are less likely to navigate normally across the midline via the cerebral commissures. As the physiological basis of neuronal and neurite development and migration is complex and incompletely understood to date, it is not helpful to speculate on the physiologic and molecular biologic differences that have resulted in the commissural anomalies described in this study. Nonetheless, a few general concepts seemed to emerge. Patients with the LIS1 pattern of cortical involvement (pachygyria gradient more severe posteriorly, involving parietal and occipital lobes) had a more vertical splenium (Figs. 1, 5), while those with the DCX pattern (more severe anteriorly involving posterior frontal lobes) more often had normal or slightly thin splenium. Patients with the vLIS patterns of lissencephalic cortical malformations, which, other than VLDLR, have less organized cortical histology than the cLIS patterns (8), had the most severe commissural anomalies with frequent ACC or CC hypoplasia. Although VLDLR patients sometimes had nearly normal CCs, they more commonly had a relatively sharp upward angle of the midcallosal body, giving them the convex upward body shape. The cause of this angle is not clear but, if confirmed in other studies, it may be a useful imaging marker for this unusual disorder. Overall, our findings indicate that the appearance of the CC does not simply derive from the pattern of cortical involvement in lissencephalies but is likely the result of impaired neuronal and axonal migration at some step.
This study contains a number of assumptions and limitations. It is limited by the small number of cases with established genetic diagnoses. An attempt was made to increase this number by classifying studies as having a “presumed” genetic classification based upon characteristic MRI features and their correlation with known pathology, such as cell-sparse zones, associated cerebellar anomalies, and cortical thickness. In a previous study, we showed that the genetically-proven and presumed groups showed considerable homogeneity of MRI morphology (10). Thus, we believe that this classification as “presumed” mutations was both useful and justified. Many patients in the vLIS group were classified as ND because of lack of part or total clinical information. Some of these were likely to be the two-layered lissencephaly described by Forman (2005) or a result of TUBA1A mutations (41–44). We did not presume the diagnosis of TUBA1A mutation in any patient because the phenotypes associated with this mutation were not disclosed at the time of the study and are still not fully established. From current literature, it appears that TUBA1A mutations may result in either cLIS or vLIS patterns (41–44). It may be useful to reassess these cases in several years when these and other new causes of lissencephaly are better established. Despite these obvious deficiencies, this study has yielded important information for physicians and scientists interested in corticogenesis by adding to the knowledge of associated malformations.
CONCLUSION
Anomalies of the cerebral commissures are common in the lissencephalies and likely result from impairment of migration of cortical neurons and of navigation of their axons through the developing cerebrum. Looking at the commissures in lissencephalies may help to differentiate among lissencephaly phenotypes and hopefully, in the future, among genotypes. The information provided by our study will hopefully lead to further studies of the molecular disorders involved in brain anomalies associated with agyria and pachygyria and, ultimately, a better understanding of the mechanisms of normal and abnormal brain development.
Figure 3.

Acknowledgments
The authors would like to acknowledge Drs. Christopher Walsh and William Dobyns, who referred many of the MRI scans reviewed for this study.
Abbreviations
- cLIS
Classical lissencephaly
- vLIS
Variant lissencephaly
- CBSC
Cobblestone complex
- LIS1
lissencephaly with mutated LIS1 gene
- DCX
lissencephaly with mutated DCX gene
- ARX-XLAG
lissencephaly with ARX mutation, and an absent callosum, ambiguous genitalia
- RELN
lissencephaly with RELN mutation
- TUBA1A
lissencephaly with TUBA1A mutation
- VLDLR
lissencephaly with VLDLR mutation
- CMD
Congenital muscular dystrophies
- WWS
Walker-Warburg syndrome
- MEB
Muscle-eye-brain disease
- FCMD
Fukuyama congenital muscular dystrophy
- FKRP
lissencephaly with FKRP mutation
- LARGE
lissencephaly with LARGE mutation
- POMT1, POMT2, and POMGnT1
lissencephalies with POMT1, POMT2, POMGnT1 mutations
- (p)
Presumed
- ND
Not determined
- ACC
Agenesis of the corpus callosum
- CC
Corpus callosum
- AC
Anterior commissure
- HC
Hippocampal commissure
Footnotes
Statistics: The first author conducted the statistical analysis.
References
- 1.Barkovich AJ. Pediatric Neuroimaging. 4. Lippincott Williams & Wilkins; Philadelphia: 2005. Chapter 5. Congenital malformations of the brain and skull; pp. 341–352. [Google Scholar]
- 2.Caspi M, Atlas R, Kantor A, Sapir T, Reiner O. Interaction between LIS1 and doublecortin, two lissencephaly gene products. Human Molecular Genetics. 2000;9:2205–22. doi: 10.1093/oxfordjournals.hmg.a018911. [DOI] [PubMed] [Google Scholar]
- 3.Kato M, Dobyns WB. Lissencephaly and the molecular basis of neuronal migration. Human Molecular Genetics. 2003;12:89–96. doi: 10.1093/hmg/ddg086. Review. [DOI] [PubMed] [Google Scholar]; Kiernan ThJA. The Human Nervous System. 7. Lippincott-Raven; Philadelphia: 1998. p. 305. [Google Scholar]
- 4.Barkovich AJ, Kuzniecky RI, Jackson GD, et al. A developmental and genetic classification for malformations of cortical development. Neurology. 2005 Dec 27;65(12):1873–87. doi: 10.1212/01.wnl.0000183747.05269.2d. Epub 2005 Sep 28. Review. [DOI] [PubMed] [Google Scholar]
- 5.Dubeau F, Dulac O, Guerrini R, et al. X-linked malformations of neuronal migration. Neurology. 1996;47:331–339. doi: 10.1212/wnl.47.2.331. [DOI] [PubMed] [Google Scholar]
- 6.Walsh CA. Genetic malformations of the human cerebral cortex. Neuron. 1999;23:19–29. doi: 10.1016/s0896-6273(00)80749-7. [DOI] [PubMed] [Google Scholar]
- 7.Dobyns WB, Berry-Kravis E, Havernick NJ, et al. X-linked lissencephaly with absent corpus callosum and ambiguous genitalia. Am J Med Genet. 1999;86:331–337. [PubMed] [Google Scholar]
- 8.Forman MS, Squier W, Dobyns WB, et al. Genotypically defined Lissencephalies show distinct pathologies. J Neuropathol Exp Neurol. 2005;64(10):847–57. doi: 10.1097/01.jnen.0000182978.56612.41. [DOI] [PubMed] [Google Scholar]
- 9.Clement E, Mercuri E, Godfrey C, et al. Brain involvement in muscular dystrophies with defective dystroglycan glycosylation. Ann Neurol. 2008 Nov;64(5):573–82. doi: 10.1002/ana.21482. [DOI] [PubMed] [Google Scholar]
- 10.Jissendi-Tchofo P, Kara S, Barkovich AJ. Midbrain-hindbrain involvement in lissencephalies. Neurology. 2009 Feb 3;72(5):410–8. doi: 10.1212/01.wnl.0000333256.74903.94. Epub 2008 Nov 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fukuyama Y, Osawa M, Suzuki H. Congenital progressive muscular dystrophy of the Fukuyama type - clinical, genetic and pathological considerations. Brain Dev. 1981;3:1–29. doi: 10.1016/s0387-7604(81)80002-2. [DOI] [PubMed] [Google Scholar]
- 12.Dobyns WB, Stratton RF, Greenburg F. Syndromes with lissencephaly. I. Miller-Dieker and Norman-Roberts syndromes and isolated lissencephaly. Am J Med Genet. 1984;8:509–526. doi: 10.1002/ajmg.1320180320. [DOI] [PubMed] [Google Scholar]
- 13.Williams RS, Swisher CN, Jennings M, et al. Cerebro-ocular dysgenesis (Walker-Warburg syndrome): neuropathologic and etiologic analysis. Neurology. 1984 Dec;34(12):1531–41. doi: 10.1212/wnl.34.12.1531. [DOI] [PubMed] [Google Scholar]
- 14.Dobyns WB, Kirkpatrick JB, Hittner HM, et al. Syndromes with lissencephaly. II: Walker-Warburg and cerebro-oculomuscular syndromes and a new syndrome with type II lissencephaly. Am J Med Genet. 1985;22:157–195. doi: 10.1002/ajmg.1320220118. [DOI] [PubMed] [Google Scholar]
- 15.Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195–210. doi: 10.1002/ajmg.1320320213. [DOI] [PubMed] [Google Scholar]
- 16.Reiner O, Carrozzo R, Shen Y, et al. Isolation of a Miller–Dieker lissencephaly gene containing G protein beta-subunit-like repeats. Nature. 1993;364:717–721. doi: 10.1038/364717a0. [DOI] [PubMed] [Google Scholar]
- 17.Dobyns WB, Caskey CT, Ledbetter DH. Isolation of a Miller–Dieker lissencephaly gene containing G protein beta-subunit-like repeats. Nature. 1993;364:717–721. doi: 10.1038/364717a0. [DOI] [PubMed] [Google Scholar]
- 18.Barkovich AJ, Guerrini R, Battaglia G, et al. Band heterotopia: correlation of outcome with magnetic resonance imaging parameters. Ann Neurol. 1994;36:609–617. doi: 10.1002/ana.410360409. [DOI] [PubMed] [Google Scholar]
- 19.Hattori M, Adachi H, Tsujimoto M, et al. Miller–Dieker lissencephaly gene encodes a subunit of brain platelet-activating factor acetylhydrolase. Nature. 1994;70:216– 218. doi: 10.1038/370216a0. [DOI] [PubMed] [Google Scholar]
- 20.Ramer JC, Lin AE, Dobyns WB, et al. Previously apparently undescribed syndrome: Shallow orbits, ptosis, coloboma, trigonocephaly, gyral malformations, and mental and growth retardation. Am J Med Genet. 1995;57:403–9. doi: 10.1002/ajmg.1320570308. [DOI] [PubMed] [Google Scholar]
- 21.Dobyns WB, Andermann E, Andermann F, et al. X-linked malformations of neuronal migration. Neurology. 1996;47:331–339. doi: 10.1212/wnl.47.2.331. [DOI] [PubMed] [Google Scholar]
- 22.Miura H, Yanazawa M, Kato K, et al. Expression of a novel aristaless related homeobox gene ‘Arx’ in the vertebrate telencephalon, diencephalon and floor plate. Mech Dev. 1997;65:99–109. doi: 10.1016/s0925-4773(97)00062-2. [DOI] [PubMed] [Google Scholar]
- 23.van der Knaap MS, Smit LM, Barth PG, et al. Magnetic resonance imaging in classification of congenital muscular dystrophies with brain abnormalities. Ann Neurol. 1997 Jul;42(1):50–9. doi: 10.1002/ana.410420110. [DOI] [PubMed] [Google Scholar]
- 24.Pilz DT, Matsumoto N, Minnerath S, et al. LIS1 and XLIS (DCX) mutations cause most classical lissencephaly, but different patterns of malformation. Hum Mol Genet. 1998;7:2029–2037. doi: 10.1093/hmg/7.13.2029. [DOI] [PubMed] [Google Scholar]
- 25.Dobyns WB, Truwit CL, Ross ME, et al. Differences in the gyral pattern distinguish chromosome 17-linked and X-linked lissencephaly. Neurology. 1999;53:270–277. doi: 10.1212/wnl.53.2.270. [DOI] [PubMed] [Google Scholar]
- 26.Barkovich AJ, Kuzniecky RI. Gray matter heterotopia. Neurology. 2000;12;55(11):1603. doi: 10.1212/wnl.55.11.1603. [DOI] [PubMed] [Google Scholar]
- 27.Hong SE, Shugart YY, Huang DT, et al. Autosomal recessive lissencephaly with cerebellar hypoplasia is associated with human RELN mutations. Nature genetics. 2000;26:93–6. doi: 10.1038/79246. [DOI] [PubMed] [Google Scholar]
- 28.Golden JA. Cell migration and cerebral cortical development. Neuropathology and Applied Neurobiology. 2001;27:22–28. doi: 10.1046/j.0305-1846.2001.00307.x. [DOI] [PubMed] [Google Scholar]
- 29.Ross ME, Swanson K, Dobyns WB. Lissencephaly with cerebellar hypoplasia (LCH): a heterogeneous group of cortical malformations. Neuropediatrics. 2001;32:256–263. doi: 10.1055/s-2001-19120. [DOI] [PubMed] [Google Scholar]
- 30.Hoffmann B, Zuo W, Liu A, et al. The LIS1-related protein NUDF of Aspergillus nidulans and its interaction partner NUDE bind directly to specific subunits of dynein and dynactin and to alpha- and gamma-tubulin. J Biol Chem. 2001;276:38877– 38884. doi: 10.1074/jbc.M106610200. [DOI] [PubMed] [Google Scholar]
- 31.Bonneau D, Toutain A, Laquerriere A, et al. X-linked lissencephaly with absent corpus callosum and ambiguous genitalia (XLAG): clinical, magnetic resonance imaging, and neuropathological findings. Ann Neurol. 2002;51:340–349. doi: 10.1002/ana.10119. [DOI] [PubMed] [Google Scholar]
- 32.Sicca F, Kelemen A, Genton P, et al. Mosaic mutations of the LIS1 gene cause subcortical band heterotopia. Neurology. 2003;61:1042–46. doi: 10.1212/wnl.61.8.1042. [DOI] [PubMed] [Google Scholar]
- 33.Miyata H, Chute DJ, Fink J, et al. Lissencephaly with agenesis of corpus callosum and rudimentary dysplastic cerebellum: a subtype of lissencephaly with cerebellar hypoplasia. Acta Neuropathol. 2004;107:69–81. 26. doi: 10.1007/s00401-003-0776-0. [DOI] [PubMed] [Google Scholar]
- 34.van Reeuwijk J, Maugenre S, van den Elzen C, et al. The expanding phenotype of POMT1 mutations: from Walker-Warburg syndrome to congenital muscular dystrophy, microcephaly, and mental retardation. Hum Mutat. 2006 May;27(5):453–9. doi: 10.1002/humu.20313. [DOI] [PubMed] [Google Scholar]
- 35.van Reeuwijk J, Grewal PK, Salih MA, et al. Intragenic deletion in the LARGE gene causes Walker-Warburg syndrome. Hum Genet. 2007 Jul;121(6):685–90. doi: 10.1007/s00439-007-0362-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barkovich AJ. Pediatric Neuroimaging. 4. Lippincott Williams & Wilkins; Philadelphia: 2005. Chapter 2. Normal Development of the Neonatal and Infant Brain, Skull and Spine; pp. 17–41. [Google Scholar]
- 37.Gambello MJ, Darling DL, Yingling J, et al. Multiple dose-dependent effects of Lis1 on cerebral cortical development. J Neurosci. 2003;23:1719–1729. doi: 10.1523/JNEUROSCI.23-05-01719.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Richards LJ, Plachez C, Ren T. Mechanisms regulating the development of the corpus callosum and its agenesis in mouse and human. Clin Genet. 2004;66:276–289. doi: 10.1111/j.1399-0004.2004.00354.x. [DOI] [PubMed] [Google Scholar]
- 39.Ren T, Anderson A, Shen W-B, et al. Imaging, anatomical, and molecular analysis of callosal formation in the developing human fetal brain. Anat Rec A. 2006;288A:191–204. doi: 10.1002/ar.a.20282. [DOI] [PubMed] [Google Scholar]
- 40.Rakic P, Yakovlev PI. Development of the corpus callosum and cavum septae in man. J Comp Neurol. 1968;132:45–72. doi: 10.1002/cne.901320103. [DOI] [PubMed] [Google Scholar]
- 41.Poirier K, Keays DA, Francis F, et al. Large spectrum of lissencephaly and pachygyria phenotypes resulting from de novo missense mutations in tubulin alpha 1A (TUBA1A) Hum Mutat. 2007 Nov;(28):11, 1055–64. doi: 10.1002/humu.20572. [DOI] [PubMed] [Google Scholar]
- 42.Bahi-Buisson N, Poirier K, Boddaert N, et al. Refinement of cortical dysgeneses spectrum associated with TUBA1A mutations. J Med Genet. 2008 Oct;45(10):647–53. doi: 10.1136/jmg.2008.058073. Epub 2008 Aug 26. [DOI] [PubMed] [Google Scholar]
- 43.Morris-Rosendahl DJ, Najm J, Lachmeijer AM, et al. Refining the phenotype of alpha-1a Tubulin (TUBA1A) mutation in patients with classical lissencephaly. Clin Genet. 2008 Nov;74(5):425–33. doi: 10.1111/j.1399-0004.2008.01093.x. [DOI] [PubMed] [Google Scholar]
- 44.Fallet-Bianco, Loeuillet L, Poirier K. Neuropathological phenotype of a distinct form of lissencephaly associated with mutations in TUBA1A. Brain. 2008 Sep;131(Pt 9):2304–20. doi: 10.1093/brain/awn155. Epub 2008 Jul 18. [DOI] [PubMed] [Google Scholar]


