Abstract
Objectives
We assessed a school-based intervention designed to promote tobacco control among teachers in the Indian state of Bihar.
Methods
We used a cluster-randomized design to test the intervention, which comprised educational efforts, tobacco control policies, and cessation support and was tailored to the local social context. In 2009 to 2011, we randomly selected 72 schools from participating school districts and randomly assigned them in blocks (rural or urban) to intervention or delayed-intervention control conditions.
Results
Immediately after the intervention, the 30-day quit rate was 50% in the intervention and 15% in the control group (P = .001). At the 9-month postintervention survey, the adjusted 6-month quit rate was 19% in the intervention and 7% in the control group (P = .06). Among teachers employed for the entire academic year of the intervention, the adjusted 6-month abstinence rates were 20% and 5%, respectively, for the intervention and control groups (P = .04).
Conclusions
These findings demonstrate the potent impact of an intervention that took advantage of social resources among teachers, who can serve as role models for tobacco control in their communities.
The global burden of tobacco is rapidly shifting to the developing world. According to the World Health Organization, it is expected that by 2030 more than 8 million people globally will die from tobacco-related causes, 80% of them in low- and middle-income countries.1 As part of growing attention to this issue, the United Nations General Assembly included support for tobacco control in its initiative to reduce noncommunicable diseases.2,3 The World Health Organization created MPOWER as a resource for countries to implement tobacco control efforts4 and negotiated the Framework Convention on Tobacco Control, the first international treaty negotiated under the organization’s auspices.5 These efforts underscore the ongoing significant need for effective strategies that take into account the challenges of resource-poor situations.6
India faces particular challenges because multiple forms of tobacco are in widespread use and limited resources are available for tobacco control.7 An estimated 1 million deaths in 2010 alone were attributable to tobacco-related causes in India, with increases projected in the future.8 The prevalence of tobacco use is 48% among men and 20% among women.7 Tobacco-related cancers constitute about half the total cancer incidence among men and about 20% among women.9,10 India also has the highest oral cancer rate in the world.11,12
Although India was an early signatory to the Framework Convention on Tobacco Control, few resources are available in India to support tobacco use cessation,13–19 quitting tobacco use is not common practice, and few social norms support quitting.7 Indeed, little attention has been paid to studying, developing, and delivering effective interventions for cessation. Prevalence of former tobacco use is much lower in India than in the United States (3% vs 21%–25%).7,20–23
Successful, evidence-based interventions with the potential for widespread implementation, beginning with opinion leaders who contribute to shaping social norms regarding tobacco use, are urgently needed.24 Teachers represent an important vanguard population for tobacco control efforts in India; they are role models for community norms generally and can be instrumental in school-based tobacco control efforts, which are often a community’s first step toward a broad-based control program.25–27
We tested the efficacy of a school-based intervention designed to promote tobacco control among teachers in the Indian state of Bihar, where rates of tobacco use are among the highest in the country. In 2000, the Global School Personnel Survey found that 78% of teachers in Bihar used some form of tobacco.28 We randomly assigned schools to either an intervention or a delayed-intervention control condition. We tested the hypothesis that teachers in intervention schools who used tobacco would be more likely than teachers in control schools to (1) have quit for at least 30 days by immediately after the intervention and (2) have quit for 6 months or more by 9 months after the intervention.
METHODS
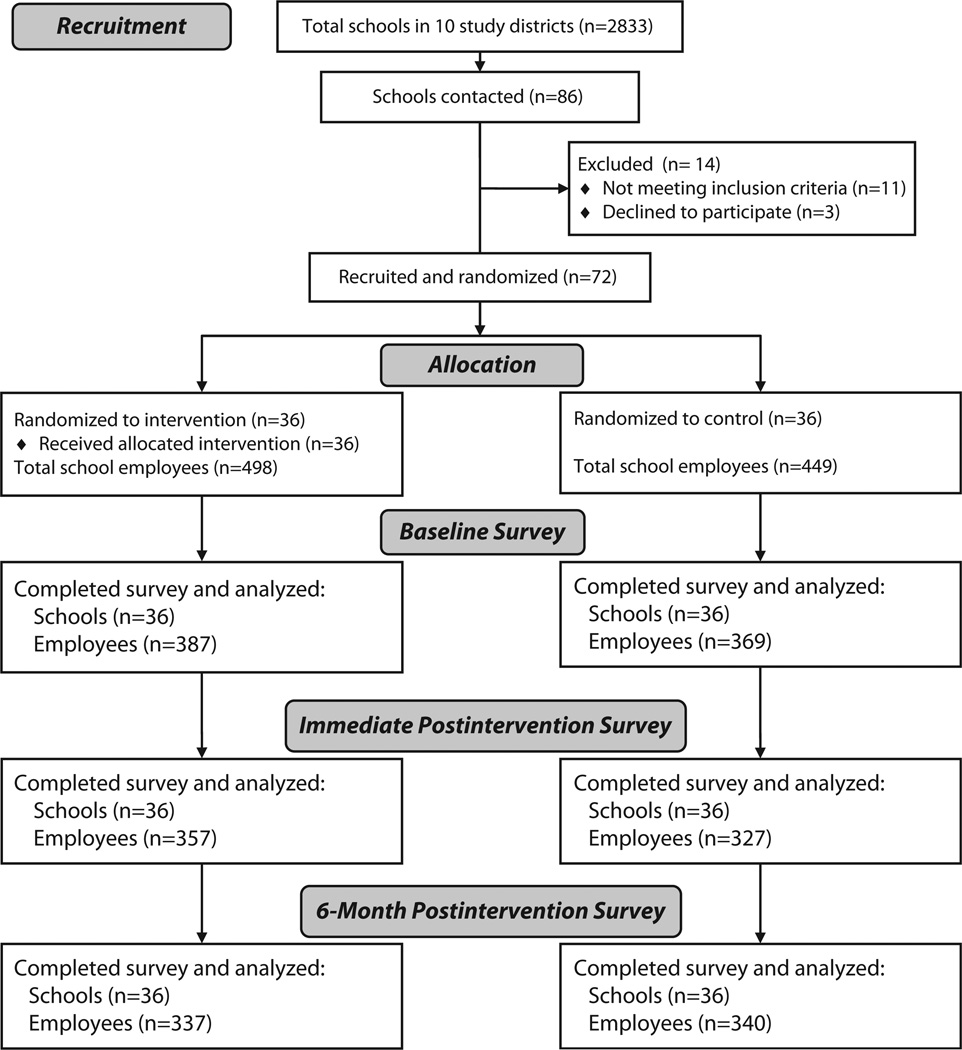
The Bihar School Teachers Study developed and tested a comprehensive school-based tobacco control intervention in 72 schools. The intervention, which had a cluster-randomized design and was called the Tobacco-Free Teachers/Tobacco-Free Society Program, focused on tobacco control policies, educational efforts, and cessation support. We randomly selected schools in participating school districts and randomly assigned selected schools within blocks (rural or urban) to either an intervention or a delayed-intervention control condition (Figure 1). We conducted the study over 2 waves that encompassed 2 separate academic years (2009–2010 and 2010–2011), each with 36 schools. The school served as the unit of intervention and randomization. The study was a collaboration among the Healis–Sekhsaria Institute for Public Health in Mumbai and Patna, India, and the Dana–Farber Cancer Institute and Harvard School of Public Health, Boston, Massachusetts.
Figure 1.
Flow diagram of random selection of tobacco control intervention and control schools: Bihar School Teachers Study, Bihar, India, 2009–2011.
Sample
Bihar, situated in northeast India on the border with Nepal, had fewer social and financial resources than much of India at the time of our study. In 2001, only 4% of Bihar households had tap drinking water (national average = 37%), and 10% had electricity as a source of lighting (56% nationwide).29 Tobacco use was prevalent in Bihar (66% of men in 2009–2010 vs 50% nationwide).7
We randomly selected 72 government schools with grades 8 to 10 from 10 school districts in Bihar. Eligible schools had at least 8 teachers. We excluded school districts located in flood zones because school closures would make intervention delivery unfeasible.
We collected baseline school characteristics on 66 of the 72 participating schools. Average distance from the study office located in the capital, Patna, was 99 kilometers (range = 6–400 km). Common modes of transportation to the schools were bus, auto rickshaw, train, and jeep; for 7 schools, study staff also had to walk an average distance of 5 kilometers. Only 41% of schools had an electric supply, 78% of which were located in urban areas.
Intervention
Our intervention design was informed by the social contextual model for health behavior change, and we developed a systematic plan of formative research, including focus groups and message testing.30,31 The intervention aimed to promote change in 5 mediating mechanisms: risk perceptions, motivation to change, social norms and role models supporting tobacco control, self-efficacy and skills for quitting, and support to quit. We incorporated central findings from our formative research, such as teachers’ beliefs in the importance of serving as role models for students, the central value of family, and the need to establish awareness of risks related to tobacco use. We pilot-tested the intervention in 2 schools and revised accordingly. We learned, for example, that it was important to place the intervention for teachers in the broader context of their role in society and to design specific intervention elements to engage nonusers.30
We framed the intervention around 6 themes linked to the mediating mechanisms, which were addressed in a stepwise manner over 7 months (September–March), with approximately 1 theme addressed per month. Intervention activities and materials aimed to
emphasize teachers as role models,
increase understanding of the risks related to tobacco,
increase motivation to quit,
build skills for quitting,
address ways to cope with withdrawal, and
promote skills for maintenance.
The overarching goal was to build a supportive normative climate for not using tobacco.
Trained study health educators delivered the intervention in close collaboration with each school. Each school appointed a lead teacher, who was trained to facilitate the program on-site during a 2-day training provided by wave in a centralized location. Health educators offered ongoing technical support for the lead teachers through monthly school visits, phone support, and a midyear meeting with lead teachers from other intervention schools. The intervention protocol specified that health educators would conduct 1 visit per month to each school, for a total of 6 visits over the 7 months of intervention delivery. During each visit, health educators met with the principal and lead teacher and conducted a group discussion with the teachers and other school personnel. The lead teacher also conducted 6 to 8 group discussions with the other teachers in the school, addressing the topic defined for that month.
Each school implemented a tobacco policy, painted directly on the walls of the school in large, bold writing, as is common practice for posting messages in India. The policy prohibited tobacco use on school property, banned tobacco advertising or endorsement of tobacco in the school, and supported regulations against sale of tobacco products within a radius of 100 yards of the school. Posters addressing the intervention themes further communicated intervention messages. The intervention provided support for tobacco use cessation through discussions and written materials.
Data Collection
We conducted 3 surveys of teachers within each wave: at baseline at the beginning of the school year (June–July; response rate = 80%; n = 756), immediately after the intervention at the end of the school year (March–April; response rate = 72%; n = 684), and 9 months after the intervention (December–January; response rate = 71%; n = 677). Although the original plan was to collect final data 6 months after intervention, data collection was unavoidably delayed by holidays and school business.
Teachers self-administered surveys in Hindi, the language commonly spoken in Bihar, at the school during visits from data collection project staff. We invited all teachers and clerical staff in each school to participate in each survey. We assigned respondents a study identification number to track individual respondents across surveys.
In addition, we tracked implementation of the intervention protocol. After each intervention visit, health educators completed a process tracking form that documented time spent in meetings with the principal, lead teacher, and other teachers; the total number of teachers present; and the topics addressed in the discussion. Health educators collected similar information from lead teachers after each discussion these teachers led.
Measures
Tobacco use cessation
We measured tobacco use cessation, defined as stopping use of any tobacco product, by self-report on standard items.32,33 Immediately after the intervention, we measured the 30-day tobacco quit rate, defined as the number of participants who quit using tobacco after the beginning of the intervention and had not used in the past 30 days, divided by the number of participants who reported using tobacco at any time during the intervention. We also measured 6-month continuous abstinence from tobacco use at the 9-month postintervention survey among all respondents who reported they were ever-users and who had quit not more than 18 months ago (i.e., prior to the beginning of the intervention). We defined 6-month quitters as tobacco users who had quit in the past 18 months and had not used tobacco in the past 6 months.
Covariates
We measured sociodemographic variables with standard items: age, gender, occupation or position, religion, marital status, and education. We also asked respondents the date they began work in the study school.
Statistical Analyses
We controlled for the clustering of teachers in schools in all analyses. Preliminary analysis assessed balance in the 2 conditions with respect to age, gender, occupation or position, religion, marital status, education, urban or rural location, and wave through mixed-effects linear modeling methods with intervention as a fixed effect and school as a random effect. For analysis of the intervention effect, we used mixed-effects logistic regression analysis of quit status on intervention group (fixed effect) and controlled for school (random effect). We also controlled for wave and urban or rural location and the interaction of intervention and location (fixed effects).
None of those effects was statistically significant, and controlling for them did not change the estimated effect of intervention, so we reported analyses with adjustment only for school. We excluded teachers who started work at the study schools after the beginning of the intervention school year from secondary analyses.
RESULTS
At baseline, the sociodemographic characteristics and tobacco use patterns were comparable among participants in the intervention and control groups (Table 1). About one third of the sample used smokeless tobacco products, and about 7% smoked. The prevalence of any tobacco use at baseline was approximately 33% in the intervention and 38% in the control group. Although the numbers of urban and rural schools were similar in the 2 conditions (18 urban and 18 rural intervention schools; 19 urban and 17 rural control schools), the number of participants differed; approximately 57% of teachers who received the intervention and 45% of control participants worked in urban schools. We also compared these sociodemographic characteristics among those who participated in the baseline survey and those who participated in each of the follow-up surveys and found no differences between surveys (data not shown).
TABLE 1.
Baseline Characteristics of Tobacco Control Intervention and Control Participants: Bihar School Teachers Study, Bihar, India, 2009–2011
| Characteristic | Intervention Group (n = 387), No. (%) or Mean ±SD |
Control Group (n = 369), No. (%) or Mean ±SD |
P |
|---|---|---|---|
| Age, y | 45.1 ±10.7 | 45.8 ±9.9 | .6 |
| Wave | .96 | ||
| 1 (2009–2010) | 200 (50.2) | 175 (47.4) | |
| 2 (2010–2011) | 187 (49.8) | 194 (52.6) | |
| Location | .68 | ||
| Rural | 138 (42.7) | 177 (54.6) | |
| Urban | 249 (57.3) | 192 (45.4) | |
| Gender | .54 | ||
| Male | 259 (71.5) | 236 (67.4) | |
| Female | 128 (28.5) | 133 (32.6) | |
| Occupation/position | .8a | ||
| Principal/headmaster | 31 (8.0) | 34 (9.2) | |
| Teacher | 331 (85.5) | 318 (86.2) | |
| Other (e.g., clerical, nurse) | 25 (6.4) | 17 (4.6) | |
| Religion | .46 | ||
| Hindu | 334 (89.9) | 330 (92.3) | |
| Other | 49 (10.1) | 37 (7.7) | |
| Marital status | .69 | ||
| Not married | 43 (11.3) | 38 (10.3) | |
| Married | 339 (88.7) | 329 (89.7) | |
| Education | .12 | ||
| ≤ college | 241 (64.9) | 260 (73.1) | |
| > college | 143 (35.1) | 107 (26.9) | |
| Current use of any tobacco | .38 | ||
| No | 258 (66.8) | 229 (62.1) | |
| Yes | 128 (33.2) | 140 (37.9) | |
| Current smoker | .48 | ||
| No | 360 (93.5) | 339 (92.1) | |
| Yes | 25 (6.5) | 29 (7.9) | |
| Current use of smokeless tobacco | .13 | ||
| No | 263 (68.2) | 232 (63.0) | |
| Yes | 123 (31.8) | 137 (37.0) |
Note. Results adjusted for clustering of teachers in schools.
Comparison of teachers with all others.
Process-tracking data showed that 98% of the schools implemented all health educator discussions, and 96%of schools implemented all lead teacher discussions. All 36 intervention schools fully implemented the wall paintings, posters, and cessation support. Each school received approximately 22 hours of intervention (health educator visits and lead teacher meetings) over the 7-month period (1339 minutes).
Among the 684 employees who completed the immediate postintervention survey in the 72 study schools, 177 were tobacco users (mean = 2.5/school). The unadjusted 30-day quit rate was approximately 50% in the intervention and 15% in the control group (Table 2). Control for school effects and restriction of the analysis to teachers who worked in the school for the entire intervention period (n = 175) did not change quit rates (both, P < .001).
TABLE 2.
Postintervention Abstinence From Tobacco Products: Bihar School Teachers Study, Bihar, India, 2009–2011
| Variable | Intervention Group, No. or % |
Control Group, No. or % |
P |
|---|---|---|---|
| Immediate postintervention survey, 30-d abstinencea | |||
| Total tobacco users | 99 | 78 | |
| Quit count | 49 | 12 | |
| Unadjusted quit rate | 49.5 | 15.4 | |
| Adjusted quit rateb | 49.6 | 15.4 | < .001 |
| Follow-up survey 9 mo after intervention, 6-mo abstinencec | |||
| Total tobacco users | 69 | 81 | |
| Quit count | 12 | 6 | |
| Unadjusted quit rate | 17.4 | 7.4 | |
| Adjusted quit rateb | 18.5 | 7.3 | .06 |
All tobacco users who quit during the intervention and had not used tobacco for the past 30 days.
Adjusted for random school effect.
All tobacco users who quit after intervention began and had not used tobacco for the past 6 months.
Among the 677 employees who completed the 9-month postintervention survey, 150 were tobacco users (mean = 2.1/school). The unadjusted 6-month quit rate was approximately 17% in the intervention and 7% in the control group (Table 2). After adjustment for school effects, the rates were approximately 19% and 7% in the intervention and control groups, respectively (P = .06). When we restricted the analysis to participants who had been employed in the school for the entire intervention period (n = 123), the adjusted 6-month abstinence rates were approximately 20% in the intervention and 6% in the control group (P = .04).
DISCUSSION
Evidence-based interventions are urgently needed to address the rising public health epidemic of tobacco use in the developing world. We used a cluster-randomized design to test the efficacy of a school-based intervention designed to promote tobacco control among teachers in the Indian state of Bihar. We hypothesized that the intervention would result in more tobacco use cessation among teachers in schools randomly assigned to receive the intervention than in the control group, both immediately after the intervention and 9 months later. At the conclusion of the intervention period, we found dramatic between-group differences in cessation, with half of baseline tobacco users in the intervention and only 15% in the control group reporting quitting. Although the magnitude of the between-group differences remained large 9 months later, rates of sustained cessation declined in both groups. Among all survey respondents, more than twice as many users in the intervention as in the control group quit (19% vs 7%). Although this difference was of borderline statistical significance, the effect was statistically significant among those present for the entire intervention period (20% vs 5%; P = .04).
Little research has examined the efficacy of tobacco use cessation efforts for adults in India. Ours was among the first randomized controlled studies in India to demonstrate the efficacy of a community-based tobacco use cessation initiative. Several early nonrandomized community-based intervention studies have shown promise in adults.16,34,35 More recently, a randomized study of a community-based tobacco control intervention in rural Tamil Nadu found abstinence rates 2 months after an intervention of14% in the intervention group and 7% in the control group (P = .02).19 Another study used a nonrandomized design to test a comprehensive cardiovascular disease risk factor reduction program, including tobacco control, in Indian industrial sites and found greater reductions in tobacco use prevalence immediately after an intervention in the intervention than in the comparison group (38.8%–28.7%; P < .001 vs 17.2%–19.8%; P = .08).36 These studies provide important initial direction for community-based tobacco use cessation support. In our study we observed a larger effect size maintained over 6 months.
Limitations
Our statistical power was lower than expected. We designed the study to be implemented in 100 schools, 50 per condition. Budget and feasibility constraints reduced our sample size to 72 schools, 36 in each condition. We based our sample size estimates on the results of the 2000 Global School Personnel Survey, which found that 78% of teachers in Bihar used some form of tobacco, regardless of gender.28 In our sample, only 35% of teachers reported using tobacco in the baseline surveys conducted in 2009 and 2010. Post hoc power calculations indicated that our study had 45% power to detect the difference observed. Nonetheless, the magnitude of the effect we observed was substantial and larger than expected.
The reduction in tobacco use prevalence between the 2000 Global School Personnel Survey and our data from 2009 and 2010 may reflect actual change as well as possible misreporting. Awareness of the detrimental effects of tobacco use has likely increased in India since the 2000 survey, with a possible result that an increase in social desirability or other bias may have influenced the responses to our baseline survey in all schools. It is also possible that tobacco use prevalence may have decreased substantially. This decrease may reflect at least in part the elimination of tobacco from a dentifrice commonly used in Bihar, Lal dantmanjan; earlier reporting of tobacco use likely reflected use of tobacco included in this tooth powder. Randomization of schools to intervention or control condition occurred after the baseline surveys were completed, so any response bias at baseline could not be attributable to school assignment.
We took numerous precautions to minimize reporting bias: surveys were anonymous, teachers were told in advance that the results would only be communicated in the aggregate, and intervention and survey staff were separate. We also explored collection of cotinine in a pilot test. We requested samples from all survey respondents to avoid appearing to question the veracity of self-report. Unfortunately, cotinine validation proved not to be feasible. We used urinary rather than salivary cotinine because the latter was culturally inappropriate. Not surprisingly, with inconsistent availability of toilet facilities in schools, women were significantly less likely than men to provide urine samples. We selected a rapid screening test because of the lack of available laboratories for testing in Bihar and other logistical issues. Our test samples may have been compromised by exposure to excessively high temperatures. We were unable to convey results confidentially in some school settings. Both false positive and false negative results were high but were equally distributed across the 2 conditions, suggesting high error rates and low sensitivity and specificity. Others have similarly raised concerns about the use of urinary cotinine in India and have noted low sensitivity in detecting use of smokeless tobacco, which is especially prevalent in this population.37,38
Conclusions
We implemented our study in a poor region of India with high prevalence of tobacco use and therefore urgent need for tobacco control interventions. We selected schools randomly, to provide a representative sample that reflected the likely implementation of this intervention in this state. We used a rigorous cluster-randomized design and controlled for the clustering of respondents in schools. Our results demonstrated the feasibility of implementing a school-based intervention for teachers, not only in urban areas but also in hard-to-access rural areas, where passable roads are not consistently available. Local conditions created challenges for intervention delivery—lack of electricity, poor roads that made travel to and from schools arduous and long, and weather conditions that ranged from very hot in summers (> 40°C) to very wet in the monsoon season. Despite these challenges, health educators were able to deliver the intervention fully; all schools implemented a tobacco control policy, 96% of the lead teacher discussions were conducted, and support for cessation was consistently provided. The magnitude of the effect size and the significant result among teachers present for the full intervention period demonstrated the effectiveness of this program.
The Tobacco-Free Teachers/Tobacco-Free Society intervention resulted in a doubling of cessation among all survey respondents and a quadrupling of quit rates among those present for the entire intervention period. Our findings suggest that this program is an innovative and effective response to the rising need for evidence-based tobacco control interventions in India. Few evidence-based approaches are available to inform the creation of an infrastructure to support tobacco use cessation. Our study provides such evidence from one of the first community-based cluster-randomized trials conducted in India. Situating this research in Bihar was significant because of the high prevalence of tobacco use and the lack of sufficient resources to adequately respond to this growing public health problem. Our findings demonstrate the potent and meaningful impact of this intervention, which was designed in response to the local social context and built on the social resources among teachers, who can serve as opinion leaders and role models for tobacco control in their communities.
Acknowledgments
This work was supported by the National Cancer Institute (grants 5R01 CA120958, and 5 K05 CA108663).
The authors thank the numerous investigators and staff members in India and the United States who contributed to this study, including Quayyim Ansari, Lauren Becker, Linnea Benson-Whelan, Ellen Connorton, Caitlin Eicher Caspi, Joshua Gagne, Adam Gerberick, Christopher Kenwood, Neha Mathur, Amruta Miland, Shree Mukesh, Claudia R. Pischke, Divya Ramamurthi, David Rothfarb, Laura Shulman, Melanie Silverman, Gupteshwar Singh, Manibala Singh, and Lorraine Wallace. In addition, this work could not have been completed without the participation of the 72 government schools in Bihar and the Health Educators and staff at the School of Preventive Oncology in Patna, Bihar. Lastly, the authors also thank the Education Department of the Bihar State Government for its support of this study.
Footnotes
Contributors
G. Sorensen is the principal investigator for the Bihar School Teachers’ Study; she led study conceptualization and design and writing of the article and oversaw evaluation. M. S. Pednekar oversaw study implementation in India and was responsible for study evaluation. D. N. Sinha directed all aspects of study implementation in Bihar, including directing all contacts with participating schools. A. M. Stoddard led evaluation design and data analysis. E. Nagler led the design of the intervention and training protocol. M. B. Aghi led collection and analyses of qualitative data and contributed to intervention design. H. A. Lando contributed to the intervention design, particularly cessation methodology, and provided guidance on the cotinine pilot. K. Viswanath led the design of the health communications. P. Pawar led the collection and analyses of the process evaluation. P. C. Gupta is the lead investigator in India and oversaw all aspects of the study in India. M. S. Pednekar, D. N. Sinha, A.M. Stoddard, E. Nagler, and H. A. Lando helped write the article, and all authors approved the final version.
Human Participant Protection
This study was approved by the Healis–Sekhsaria Institute for Public Health and Harvard School of Public Health institutional review boards, as well as by the Indian Council of Medical Research. This study has been registered with clinicaltrials.gov.
Contributor Information
Glorian Sorensen, Dana–Farber Cancer Institute, and the Harvard School of Public Health, Boston MA..
Mangesh S. Pednekar, Healis–Sekhsaria Institute of Public Health, Navi-Mumbai, India..
Dhirendra N. Sinha, School of Preventive Oncology, Patna, Bihar, India..
Anne M. Stoddard, New England Research Institutes, Watertown, MA..
Eve Nagler, Dana–Farber Cancer Institute, and the Harvard School of Public Health, Boston MA..
Mira B. Aghi, Consulting behavioral scientist, New Delhi, India..
Harry A. Lando, Division of Epidemiology and Community Health, University of Minnesota, Minneapolis..
Kasisomayajula Viswanath, Dana–Farber Cancer Institute, and the Harvard School of Public Health, Boston MA..
Pratibha Pawar, Healis–Sekhsaria Institute for Public Health, Navi-Mumbai, India..
Prakash C. Gupta, Healis–Sekhsaria Institute of Public Health, Navi-Mumbai, India..
References
- 1.World Health Organization. WHO report on the global tobacco epidemic, 2011. [Accessed July 9 2012];Executive summary. 2011 Available at: http://whqlibdoc.who.int/hq/2011/WHO_NMH_TFI_11.3_eng.pdf.
- 2.Beaglehole R, Bonita R, Alleyne G, Horton R. NCDs: celebrating success, moving forward. Lancet. 2011;378(9799):1283–1284. doi: 10.1016/S0140-6736(11)61559-6. [DOI] [PubMed] [Google Scholar]
- 3.Beaglehole R, Bonita R, Alleyne G, Horton R. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. WHO report on the global tobacco epidemic, 2008. [Accessed October 3, 2012];the MPOWER package. 2008 Available at: http://www.who.int/tobacco/mpower/mpower_report_full_2008.pdf.
- 5.World Health Organization. Tobacco free initiative. MPower brochures. 2011 Available at: http://www.who.int/tobacco/mpower/publications/en/index.html.
- 6.McMichael C, Waters E, Volmink J. Evidence-based public health: what does it offer developing countries? J Public Health (Oxf) 2005;27(2):215–221. doi: 10.1093/pubmed/fdi024. [DOI] [PubMed] [Google Scholar]
- 7.International Institute for Population Sciences. Global Adult Tobacco Survey (GATS) India 2009–2010. New Delhi, India: Ministry of Health and FamilyWelfare, Government of India; 2010. [Google Scholar]
- 8.Jha P, Jacob B, Gajalakshmi V, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med. 2008;358(11):1137–1147. doi: 10.1056/NEJMsa0707719. [DOI] [PubMed] [Google Scholar]
- 9.Sharma DC. India’s welcome to foreign tobacco giants prompts criticism. Lancet. 1998;352(9135):1204. doi: 10.1016/S0140-6736(05)60546-6. [DOI] [PubMed] [Google Scholar]
- 10.Stewart BW, Kleihues P, editors. World Cancer Report. Lyon, France: IARC Press; 2003. [Google Scholar]
- 11.Tobacco or Health: A Global Status Report: Country Profiles by Region. Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]
- 12.Reddy KS, Gupta PC. Report on Tobacco Control in India. New Delhi, India: Ministry of Health and Family Welfare, Government of India; 2004. [Google Scholar]
- 13.Mehta FS, Gupta MB, Pindborg JJ, Bhonsle RB, Jalnawalla PN, Sinor PN. An intervention study of oral cancer and precancer in rural Indian populations: a preliminary report. Bull World Health Organ. 1982;60(3):441–446. [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta PC, Aghi MB, Bhonsle RB, et al. Intervention study of chewing and smoking habits for primary prevention of oral cancer among 12 212 Indian villagers. In: Zaridze DG, Peto R, editors. Tobacco: A Major International Health Hazard. Lyon, France: International Agency for Research on Cancer; 1986. [Google Scholar]
- 15.Gupta PC, Mehta FS, Pindborg JJ, et al. A primary prevention study of oral cancer among Indian villagers: eight-year follow-up results. In: Hakama M, Beral V, Culln JW, Parkin DM, editors. Evaluating Effectiveness of Primary Prevention of Cancer. Lyon, France: International Agency for Research on Cancer; 1990. pp. 149–156. [PubMed] [Google Scholar]
- 16.Gupta PC, Mehta FS, Pindborg JJ, et al. Primary prevention trial of oral cancer in India: a ten-year follow-up study. J Oral Pathol Med. 1992;21(10):433–439. doi: 10.1111/j.1600-0714.1992.tb00970.x. [DOI] [PubMed] [Google Scholar]
- 17.Gupta PC, Mehta FS, Pindborg JJ, Bhonsle RB, Murti PR, Aghi MB. A ten-year follow-up study for primary prevention of oral cancer among Indian villagers. In: Gupta PC, Hamner JE, Murti PR, editors. Control of Tobacco-Related Cancers and Other Diseases: Proceedings of an International Symposium, January 15–19, 1990. Bombay, India: Oxford University Press; 1992. pp. 307–313. [Google Scholar]
- 18.Anantha N, Nandakumar A, Vishwanath N, et al. Efficacy of an anti-tobacco community education program in India. Cancer Causes Control. 1995;6(2):119–129. doi: 10.1007/BF00052772. [DOI] [PubMed] [Google Scholar]
- 19.Kumar MS, Sarma PS, Thankappan KR. Community-based group intervention for tobacco cessation in rural Tamil Nadu, India: a cluster randomized trial. J Subst Abuse Treat. 2012;43(1):53–60. doi: 10.1016/j.jsat.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. National Center for Health Statistics. [Accessed January 17, 2012];Health data interactive: risk factors and disease prevention. 2012 Available at: http://www.cdc.gov/nchs/hdi.htm.
- 21.Centers for Disease Control and Prevention. [Accessed May 6, 2013];Behavioral Risk Factor Surveillance System survey data. 2009 Available at: http://www.cdc.gov/brfss/annual_data/annual_2009.htm.
- 22.Caban-Martinez AJ, Davila EP, Zhao W, et al. Disparities in hypertension control advice according to smoking status. Prev Med. 2010;51(3–4):302–306. doi: 10.1016/j.ypmed.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vander Weg MW, Howren MB, Cai X. Use of routine clinical preventive services among daily smokers, non-daily smokers, former smokers, and never-smokers. Nicotine Tob Res. 2012;14(2):123–130. doi: 10.1093/ntr/ntr141. [DOI] [PubMed] [Google Scholar]
- 24.Rogers EM. Diffusion of Innovations. New York, NY: Free Press; 1995. [Google Scholar]
- 25.Pertschuk M. Engaging Doctors in Tobacco Control. Atlanta, GA: American Cancer Society; 2003. [Google Scholar]
- 26.Mishra A, Arora M, Stigler MH, et al. Indian youth speak about tobacco: results of focus group discussions with school students. Health Educ Behav. 2005;32(3):363–379. doi: 10.1177/1090198104272332. [DOI] [PubMed] [Google Scholar]
- 27.Sorensen G, Gupta PC, Sinha DN, et al. Teacher tobacco use and tobacco use prevention in two regions in India: qualitative research findings. Prev Med. 2005;41(2):424–432. doi: 10.1016/j.ypmed.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 28.Sorensen G, Gupta PC, Sinha DN, et al. Teacher tobacco use and tobacco use prevention in two regions in India: results of the Global School Personnel Survey. Prev Med. 2005;41(2):417–423. doi: 10.1016/j.ypmed.2004.09.048. [DOI] [PubMed] [Google Scholar]
- 29.Government of India. [Accessed October 24, 2010];Census of India. 2001 Available at: http://www.censusindia.gov.in.
- 30.Nagler EM, Pednekar MS, Viswanath K, et al. Designing in the social context: using the social contextual model of health behavior change to develop a tobacco control intervention for teachers in India. Health Educ Res. 2013;28(1):113–129. doi: 10.1093/her/cys060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pischke CR, Galarce EM, Nagler EM, et al. Message formats and their influence on tobacco use risk perception: a pilot formative research project in India. Health Educ Res. 2013;28(2):326–338. doi: 10.1093/her/cys112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gutmann LB, Sobell LC, Prevo MH, et al. Outcomes research methodology of smoking cessation trials (1994–1998) Addict Behav. 2004;29(3):441–463. doi: 10.1016/j.addbeh.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 33.Office on Smoking and Health. Reducing the Health Consequences of Smoking: 25 Years of Progress: A Report of the Surgeon General. Vol. 89. Rockville, MD: Centers for Disease Control and Prevention, Center for Chronic Disease Prevention and Health Promotion; 1989. p. 8411. DHHS (CDC) [Google Scholar]
- 34.Gupta PC, Mehta FS, Pindborg JJ, et al. Intervention study for primary prevention of oral cancer among 36 000 Indian tobacco users. Lancet. 1986;1(8492):1235–1239. doi: 10.1016/s0140-6736(86)91386-3. [DOI] [PubMed] [Google Scholar]
- 35.Vaidya SG, Viadya NS, Naik UD. Epidemiology of tobacco habits in Goa, India. In: Gupta PC, Hamner JC, Murti PR, editors. Control of Tobacco-Related Cancers and Other Diseases: Proceedings of an International Symposium, January 15–19, 1990. Bombay, India: Oxford University Press; 1992. pp. 315–320. [Google Scholar]
- 36.Prabhakaran D, Jeemon P, Goenka S, et al. Impact of a worksite intervention program on cardiovascular risk factors: a demonstration project in an Indian industrial population. J Am Coll Cardiol. 2009;53(18):1718–1728. doi: 10.1016/j.jacc.2008.12.062. [DOI] [PubMed] [Google Scholar]
- 37.Balhara YP, Jain R, Sundar AS, Sagar R. Use of cotinine urinalysis to verify self-reported tobacco use among male psychiatric out-patients. Lung India. 2012;29(3):217–220. doi: 10.4103/0970-2113.99102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dhavan P, Bassi S, Stigler MH, et al. Using salivary cotinine to validate self-reports of tobacco use by Indian youth living in low-income neighborhoods. Asian Pac J Cancer Prev. 2011;12(10):2551–2554. [PMC free article] [PubMed] [Google Scholar]