Abstract
Objectives
We examined whether neighborhood social characteristics (income distribution and family fragmentation) and physical characteristics (clean sidewalks and dilapidated housing) were associated with the risk of fatalities caused by analgesic overdose.
Methods
In a case-control study, we compared 447 unintentional analgesic opioid overdose fatalities (cases) with 3436 unintentional nonoverdose fatalities and 2530 heroin overdose fatalities (controls) occurring in 59 New York City neighborhoods between 2000 and 2006.
Results
Analgesic overdose fatalities were less likely than nonoverdose unintentional fatalities to have occurred in higher-income neighborhoods (odds ratio [OR] = 0.82; 95% confidence interval [CI] = 0.70, 0.96) and more likely to have occurred in fragmented neighborhoods (OR = 1.35; 95% CI = 1.05, 1.72). They were more likely than heroin overdose fatalities to have occurred in higher-income (OR = 1.31; 95% CI = 1.12, 1.54) and less fragmented (OR = 0.71; 95% CI = 0.55, 0.92) neighborhoods.
Conclusions
Analgesic overdose fatalities exhibit spatial patterns that are distinct from those of heroin and nonoverdose unintentional fatalities. Whereas analgesic fatalities typically occur in lower-income, more fragmented neighborhoods than nonoverdose fatalities, they tend to occur in higher-income, less unequal, and less fragmented neighborhoods than heroin fatalities.
Rates of fatal overdoses caused by analgesic opioids have increased dramatically in the United States, particularly over the past 5 years.1–3 The prevalence of nonmedical analgesic drug abuse is second only to that of marijuana abuse, and currently the number of fatal overdoses attributed to opioid analgesics, such as oxycodone, hydrocodone, and codeine, is greater than the number attributed to heroin and cocaine combined.4
Urban areas have long been associated with elevated risks of substance abuse and subsequent mortality from unintentional drug poisoning. From 1997 to 2002, the number of overdose deaths involving opioid analgesics increased 97% in urban areas during a time when the rate of overdose from all drugs increased 27%.5 From a public health burden standpoint, understanding the determinants of analgesic overdose mortality in large urban areas is critical to help stem the tide of mortality from analgesics, as all available data suggest that analgesic overdose mortality in these areas will continue to increase in the coming years.6
Extant epidemiological research in the area has predominantly been concerned with the role of individual characteristics in explaining the prevalence of analgesic overdose throughout the United States.5,7–12 Analgesic opiate overdose decedents have been reported to be primarily White, male, and adult (ranging in age from 25 to 54 years) and to exhibit a high prevalence of concurrent psychotherapeutic drug use.5,7–10 However, several organizing frameworks in the field (principally rooted in ecosocial theory) suggest that environments operate jointly with individual factors to influence the risk of substance use.13–15
In addition to individual characteristics such as psychiatric morbidity, genetic vulnerability, gender, and age,16–20 these frameworks suggest that interconnected components of influence shape drug use. These components include social policies and regulations that affect the allocation of social and health resources21–26; social and physical features of the neighborhood environment that structure the availability of drugs, influence norms around use, and generate sources of stress that contribute to drug use13,14,27–37; and interpersonal characteristics, such as social support and social networks, that mediate the relationship between the neighborhood environment and drug use.28,31,38–42 Despite this conceptual orientation, few studies have attempted to provide an understanding of the contextual factors that may explain the geographic distribution of analgesic overdose in an urban environment.
Of particular interest in the urban context are the features of neighborhoods that can shape drug overdose. Established conceptual frameworks suggest 2 such features: primary determinants of infrastructure, employment, education, and health care resources, including residential segregation, income distribution, and neighborhood deprivation, and secondary determinants that are consequences of these fundamental conditions and may mediate their impact on drug use, including the quality of the built environment, social norms around drug use, and family fragmentation.15 Drawing on this framework, we examined 3 features of the neighborhood environment that have been previously linked with drug overdose: income distribution, quality of the built environment, and family fragmentation.35,37,43,44
First, neighborhood income distribution has been consistently linked to drug abuse or overdose fatalities.27,35,44,45 For example, research has shown that in New York City neighborhoods with more unequal income distributions, drug overdoses are more likely than other causes to lead to unintentional deaths.35,44 The erosion of social capital and greater mistrust of authority found in more unequal neighborhoods may lead to a greater reluctance to seek medical help in cases of overdose.46 Furthermore, underinvestment in health and social resources could contribute to longer response times on the part of para-medics and limited access to substance abuse treatment. It is plausible that these same processes may drive a higher risk for analgesic opiate overdose in more unequal neighborhoods.
Second, studies have shown a positive association between poor quality of the built environment (dilapidated buildings, vandalism of public property, and littering) and risk of drug overdose.43,44,46 Deterioration of the built environment has been linked with higher levels of distress.47 In turn, people with higher levels of distress may be more vulnerable to drug abuse and overdose than people low in distress.48,49 Moreover, reduced social capital reflected in a vandalized and littered built environment may discourage neighborhood residents from interacting with each other and from developing relationships that would enable to them to intervene to prevent the development of drug distribution networks in the neighborhood.50
Third, family fragmentation (e.g., a high prevalence of divorced, separated, or single-parent families) represents a social mechanism through which neighborhoods may influence analgesic overdose. Disruption of the neighborhood social fabric may manifest in personal forms of disorganization within adult relationships.51,52 Studies of crime have shown that family disruption influences the collective ability of local residents to promote adult and youth conformity to local norms and laws.53–55 A high prevalence of fragmented families in a neighborhood reduces the neighborhood’s ability to monitor young people and respond to delinquency and crime.56 Such disorganization may have direct consequences in terms of access to and consumption of analgesics, given that the formation of drug-selling and drug-consuming networks may be more likely in neighborhoods where residents do not monitor delinquent activity consistently.57
Furthermore, disrupted families may be less likely to exert informal control over the abuse of analgesics by other family members.57 Given that consumption of analgesics occurs most frequently at home,58 the absence of a family support and control net is particularly problematic.
This study had 2 aims. First, we examined the roles that the 3 features of the neighborhood social and physical environment just described—income distribution, the quality of the built environment, and family fragmentation—play in the risk of unintentional death from analgesic overdose in New York City. Second, we examined whether analgesic opiate overdoses in New York City are driven by distinct neighborhood factors than heroin overdose, the historically most prevalent form of illicit opiate overdose in urban areas.59,60
METHODS
Demographic and mortality data were obtained from the Office of the Chief Medical Examiner of New York City (OCME), which is responsible for determining the cause of death for all individuals believed to have died from nonnatural causes in New York City. Through a manual review of OCME medical files, we identified all cases of non–overdose-related fatal accidents (classified under International Classification of Diseases, 10th Revision [ICD-10]61 codes V01–X39, X45–X59, and Y85–Y86) and unintentional poisoning deaths (ICD-10 codes X40–X44 and T40.0–T40.2) involving adults aged 15 to 64 years in New York City during the period 2000 through 2006. Because of our focus on this short time period, it is likely that factors such as the OCME’s classification of cases and toxicology remained consistent over the study period.
Trained abstractors used a standardized protocol and data collection forms developed by the OCME to collect data on cause of death, circumstances of death, and toxicology from the OCME files. OCME investigators used the decedent’s medical history, the circumstances and environment of the death, autopsy findings, and laboratory data to attribute cause of death for each case reviewed. Hence, classification of cause of death differed from the simple presence or absence of a drug in a toxicological screen. Deaths involving positive screens for an analgesic will not necessarily be classified as analgesic-induced deaths. The OCME’s attributions of drugs as a cause of death are not mutually exclusive: an overdose death may be attributed to more than one drug. We included only cases in which unintentional poisoning by drugs was listed as the primary cause of death.
OCME files also included information on decedents’ age, gender, race/ethnicity, and place of residence. Information derived from medical examiner databases has shown high sensitivity, specificity, and positive predictive value with respect to identifying external causes of death.62–64 Further details on collection of data on overdoses have been provided by Galea et al.65
We conducted a pair of case–control analyses. In the first analysis, unintentional deaths in which poisoning caused by analgesic opioids was cited as a cause of death were identified as cases, and deaths from other nonoverdose unintentional causes were considered controls. Analgesic opioids included codeine, fentanyl, hydromorphone, hydrocodone, meperidine, morphine, orphenadrine, oxycodone, and propoxyphene. Nonoverdose unintentional deaths included those caused by firearms, drownings, falls, stabbings, poisonings, and other accidents.
In the second analysis, we compared deaths in which poisoning from analgesic opioids was cited as a cause of death and heroin poisoning was not cited as an additional cause with deaths in which poisoning from heroin was cited as a cause of death but analgesic opioid poisoning was not cited as an additional cause. Hence, overlapping cases of analgesic and heroin poisoning (representing 38.4% of analgesic overdose cases and 6.3% of heroin overdose controls) were excluded from this analysis.
Geocoding and Neighborhood Identifiers
We geocoded data on participants’ site of injury into community district neighborhood designations. New York City is divided into 59 community districts (hereafter “neighborhoods”) that represent meaningful neighborhoods within the city; they include, for example, the neighborhoods of Central Harlem (community district 10 in Manhattan) and Bedford Stuyvesant (community district 3 in Brooklyn).
Neighborhood-Level Measures
We measured income distribution as absolute income (median income) and income inequality (according to the Gini coefficient). The Gini coefficient reflected the extent of inequality based on the income distribution within each of the city’s 59 neighborhoods.35,36,66 We obtained data on household incomes in each of the 5 New York City boroughs from Summary File 3 of the 2000 census.67 We included 25 household income categories, and we used the direct method (see Galea et al.36 for further details) to calculate the Gini co-efficient for each neighborhood and each year. A Gini coefficient of 0 represents total equality, whereas a coefficient of 1 represents maximum inequality. Data were collected at the census tract level and aggregated up to the neighborhood level, weighted by the proportion of overlap between each census tract and neighborhood. A New York City neighborhood contains approximately 31.7 census tracts, although tracts may cross neighborhood boundaries.
We assessed quality of the built environment in 2 ways: as the proportion of dilapidated housing structures in a neighborhood, to reflect physical deterioration of the built environment,43,44 and as the proportion of acceptably clean sidewalks, to reflect the level of social order or disorder.68 Data on dilapidated housing structures were derived from the 1999 New York City Housing and Vacancy Survey. An average of 15 550 housing structures were appraised in the survey and considered in our analyses.69 Data on sidewalk cleanliness in 2000 were obtained from the New York City mayor’s management report.70 The proportion of sidewalks in the neighborhood that met an acceptable standard of cleanliness was based on a 7-point picture-based rating scale designed to reflect public perceptions of acceptable cleanliness levels; values represent the annual neighborhood average of twice-monthly ratings of a citywide street sample.70
We defined family fragmentation according to the proportion of individuals divorced or separated in each neighborhood and the proportion of children younger than 18 years living in single-parent households, as measured in the 2000 census. The 2 measures were highly correlated (r = 0.80) and were combined into a single index via a principal components factor analysis.
Covariates
We derived data on racial/ethnic composition, represented as the proportion of Black residents in a given neighborhood, from the 2000 census. We used the proportion of accidental nonoverdose decedents who had positive toxicological screens for opiates to represent the level of opiate drug use in the neighborhood.35,36,68,71
At the individual level, we controlled for decedents’ age, gender, and race/ethnicity. These data were recorded in the OMCE files.
Statistical Analysis
Only cases without missing address of injury were retained in the analysis: 447 of 477 cases and 3436 of 3871 controls were retained for the analgesic versus accidents analysis, and 276 of 294 cases and 2530 of 2725 controls were retained for the analgesic versus heroin analysis. Cases in which address of injury data were missing were not appreciably different from the retained cases in terms of demographic variables. We used listwise deletion to address missing covariate data.
First, we identified the spatial distribution of analgesic opiate overdose deaths in 2000 through 2006 across New York City neighborhoods. Overdose deaths were calculated as age-adjusted rates of analgesic overdose per 100 000 residents per neighborhood over the study period. Maps were created with ArcMap 10.0.72 Rates (classified in quartiles) were smoothed via an empirical Bayes technique to improve stability in areas with large populations and very few cases.73 We used a spatial weights matrix created from the nearest-neighbors algorithm (via the 4-neighbor specification) to calculate Moran’s I statistic for empirical Bayes rates.73 Statistical significance for Moran’s I was estimated with a permutation procedure, and pseudo-significance values are reported.74 To provide a descriptive overview of spatial patterns of mortality and neighborhood characteristics, we also constructed maps of the neighborhood-level measures of interest and estimated the spatial correlations between these measures and analgesic overdose death rates. We used GeoDa 1.20 in estimating all spatial statistics.75
Second, we assessed bivariate relationships between individual covariates and neighborhood-level indicators separately in the 2 case–control analyses. Analgesic overdose fatalities were placed on the y-axis, and each neighborhood-level indicator was placed on the x-axis. We conducted χ2 and t tests to assess statistical significance.
Finally, we constructed separate multilevel logistic hierarchical models to determine the relationship between neighborhood-level indicators and likelihood of death from analgesic overdose relative to likelihood of death from a control condition. Statistical analyses were conducted with HLM 7 (Scientific Software International, Lincolnwood, IL). All odds ratios (ORs) and 95% confidence intervals (CIs) were based on population average model estimates76,77 to enable us to make population-level inferences about the relationships between neighborhood characteristics and the odds of analgesic-induced overdose deaths. In these models, all neighborhood-level variables were standardized to a mean of 0 and a standard deviation of 1.
We constructed the models in a similar manner for each analysis. We initially assessed the relationship of each neighborhood-level variable with the odds of death from analgesic overdose in a separate model, controlling only for the individual-level covariates. We then added indicators of income distribution, racial/ethnic composition, and neighborhood drug use to address neighborhood-level structural sources of confounding. Measures of the quality of the built environment and family fragmentation were included in separate models to avoid multicollinearity issues.
RESULTS
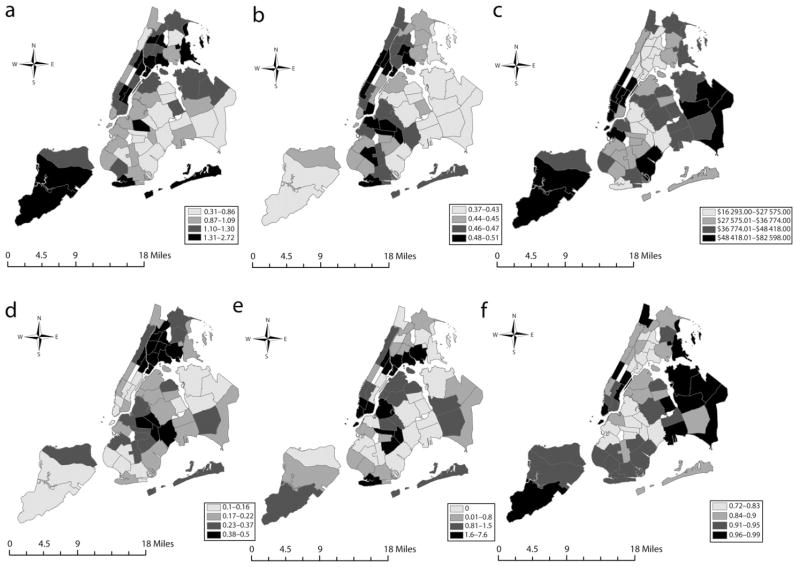
Risk of death from analgesic opiate overdose was concentrated in certain neighborhoods of New York City. The Moran’s I statistic was 0.15 (P < .05), indicating moderate spatial clustering of analgesic overdose fatalities. Figure 1 presents a series of maps depicting the spatial distributions of analgesic overdose fatalities, median incomes, income inequality, family disruption, percentages of dilapidated housing structures, and percentages of acceptably clean sidewalks. The highest rates of analgesic fatalities occurred in neighborhoods in northern Manhattan (East Harlem), Queens (Rockaway–Broadway Channel), and the Bronx (Throgs Neck–Co-op City, Belmont–East Tremont, Hunts Point–Longwood); these neighborhoods are characterized by low median incomes, low-quality built environments, and high levels of family fragmentation.
FIGURE 1.
Distribution by community district of (a) analgesic-induced overdose deaths (2000–2006), (b) income inequality (2000), (c) median household income (2000), (d) family disruption (2000), (e) proportion of houses in dilapidated condition (1999), and (f) proportion of sidewalks rated acceptably clean (2000): New York City.
Note. There are a total of 59 community districts. Analgesic-induced overdose deaths are per 100 000.
The spatial correlations between income inequality and analgesic overdose (I = 0.17; P = .02), family fragmentation and analgesic overdose (I = 0.14; P = .04), and housing dilapidation and analgesic overdose (I = 0.18; P = .02) were moderate and significant. We did not find a spatial correlation between median income or sidewalk cleanliness and analgesic overdose fatalities.
Table 1 presents data on the demographic characteristics of analgesic overdose decedents relative to those of individuals whose unintentional deaths were not attributed to drug overdose. Analgesic overdose decedents were older and more likely to be White and female, and overdose fatalities were more likely to occur in neighborhoods with low concentrations of Black residents and high rates of opiate use.
TABLE 1.
Demographic Data on Analgesic-Induced Deaths and Nonoverdose Unintentional Deaths: New York City, 2000–2006
| Individual or Neighborhood Characteristic | Analgesic Deaths,a No. (%)or Mean ±SD | Unintentional Deaths,b No. (%)or Mean ±SD | P |
|---|---|---|---|
| Age, y | <.001 | ||
| 15–24 | 35 (7.8) | 595 (17.3) | |
| 25–34 | 74 (16.6) | 636 (18.5) | |
| 35–44 | 161 (36.0) | 698 (20.3) | |
| 45–54 | 144 (32.2) | 777 (22.6) | |
| 55–64 | 33 (7.4) | 728 (21.1) | |
| Gender | .003 | ||
| Male | 314 (70.2) | 2634 (76.7) | |
| Female | 133 (29.8) | 802 (23.3) | |
| Race/ethnicity | <.001 | ||
| White | 272 (61.8) | 1183 (37.6) | |
| Black | 65 (14.8) | 1019 (32.4) | |
| Hispanic | 103 (23.4) | 943 (39.0) | |
| Median neighborhood income, $ | 39 820 ±39 977 | 40 259 ±15 802 | .8 |
| Income inequalityc | 0.5 ±0.03 | 0.5 6±0.03 | .3 |
| Black residents, % | 22.0 ±21.0 | 26.0 ±26.0 | .003 |
| Opiate use, % | 10.3 ±9.0 | 9.1 ±8.7 | .01 |
| Other drug use, % | 8.5 ±7.4 | 9.0 ±7.4 | .3 |
| Acceptably clean sidewalks, % | 89.0 ±7.0 | 88.0 ±7.0 | .5 |
| Dilapidated housing structures, % | 0.9 ±1.4 | 0.9 ±1.4 | .9 |
| Fragmented families, %d | 25.0 ±13.0 | 25.0 ±12.0 | .8 |
Note. As a result of missing data, counts for age distribution and race/ethnicity do not necessarily sum to the total counts.
447 deaths in 58 neighborhoods.
3436 in 59 neighborhoods.
According to the Gini coefficient (0 = perfectly equitable income distribution, 1 = complete inequality).
Percentage of individuals divorced and separated and percentage of children living in single-parent households.
Table 2 compares the demographic variables associated with nonoverlapping cases of analgesic and heroin overdose deaths. Analgesic overdose decedents were more likely to be White and female than heroin decedents, and analgesic overdose deaths were concentrated in neighborhoods with lower concentrations of Black residents, higher median incomes, higher proportions of clean sidewalks, and lower concentrations of dilapidated housing structures and family fragmentation.
TABLE 2.
Demographic Data on Analgesic-Induced Deaths and Heroin-Induced Deaths: New York City, 2000–2006
| Individual or Neighborhood Characteristic | Analgesic Deaths,a No. (%)or Mean ±SD | Heroin Deaths,b No. (%)or Mean ±SD | P |
|---|---|---|---|
| Age, y | .44 | ||
| 15–24 | 26 (9.4) | 171 (6.7) | |
| 25–34 | 48 (17.4) | 487 (19.3) | |
| 35–44 | 95 (34.4) | 920 (36.4) | |
| 45–54 | 84 (30.4) | 771 (30.5) | |
| 55–64 | 23 (8.3) | 180 (7.1) | |
| Gender | <.001 | ||
| Male | 190 (68.8) | 2045 (80.8) | |
| Female | 86 (31.2) | 485 (19.2) | |
| Race/ethnicity | <.001 | ||
| White | 180 (66.7) | 1082 (43.3) | |
| Black | 40 (14.8) | 563 (22.5) | |
| Hispanic | 50 (18.5) | 857 (34.2) | |
| Median neighborhood income, $ | 43 039 ±17 106 | 35 694 ±15 934 | <.001 |
| Income inequalityc | 0.5 ±0.03 | 0.5 ±0.03 | <.001 |
| Black residents, % | 20.0 ±22.0 | 25.0 ±23.0 | .001 |
| Opiate use, % | 9.9 ±9.0 | 11.0 ±9.3 | .05 |
| Other drug use, % | 8.0 ±6.5 | 9.2 ±7.5 | .01 |
| Acceptably clean sidewalks, % | 90.0 ±7.0 | 86.0 ±7.0 | <.001 |
| Dilapidated housing structures, % | 0.9 ±1.3 | 1.2 ±1.6 | .002 |
| Fragmented families, %d | 23.0 ±11.0 | 29.0 ±12.0 | <.001 |
Note. As a result of missing data, counts for age distribution and race/ethnicity do not necessarily sum to the total counts.
276 deaths in 56 neighborhoods.
2530 deaths in 59 neighborhoods.
According to the Gini coefficient (0 = perfectly equitable income distribution, 1 = complete inequality).
Percentage of individuals divorced and separated and percentage of children living in single-parent households.
Few differences emerged between analgesic overdoses and nonoverdose unintentional injuries with respect to neighborhood characteristics associated with the odds of death (Table 3). Controlling only for individual decedent characteristics, a higher median income was associated with lower odds of dying from an analgesic overdose than from a nonoverdose unintentional injury (OR = 0.83; 95% CI = 0.71, 0.97), whereas a higher level of family fragmentation was associated with a higher risk of death from analgesic overdose (OR = 1.30; 95% CI = 1.13, 1.50). The association between median income and analgesic overdose decreased in magnitude and became nonsignificant once we controlled for family fragmentation (Table 3, model 4). Income inequality and dilapidated housing were marginally and positively associated with analgesic overdose, whereas sidewalk cleanliness was marginally and negatively associated with overdose. However, these associations became null once we controlled for confounders (models 1–3).
TABLE 3.
Hierarchical Logistic Models of the Relationships Between Neighborhood Characteristics and the Odds of Analgesic-Induced Deaths vs Nonoverdose Unintentional Deaths: New York City, 2000–2006
| Crude OR (95% CI) | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) | Model 4 OR (95% CI) | |
|---|---|---|---|---|---|
|
|
|||||
| Median income | 0.83 (0.71, 0.97) | 0.82 (0.70, 0.96) | 0.78 (0.65, 0.94) | 0.81 (0.69, 0.95) | 0.96 (0.80, 1.16) |
| Income inequalitya | 1.14 (0.99, 1.33) | 0.99 (0.86, 1.15) | 1.02 (0.88, 1.17) | 1.00 (0.87, 1.16) | 0.97 (0.84, 1.12) |
| Acceptably clean sidewalks | 0.86 (0.74, 1.01) | … | 1.09 (0.90, 1.32) | … | … |
| Dilapidated housing structures | 1.08 (0.99, 1.18) | … | … | 0.94 (0.84, 1.07) | … |
| Family fragmentationb | 1.30 (1.13, 1.50) | … | … | … | 1.35 (1.05, 1.72) |
Note. CI = confidence interval; OR = odds ratio. All models controlled for decedents’ age, gender, and race/ethnicity; percentage of Black residents; and percentage of opiate use.
According to the Gini coefficient (0 = perfectly equitable income distribution, 1 = complete inequality).
Percentage of individuals divorced and separated and percentage of children living in single-parent households.
Analgesic opiate and heroin overdose fatalities occurred in distinct types of neighborhoods (Table 4). After control for individual decedent characteristics, higher median incomes (OR = 1.40; 95% CI = 1.20, 1.65) and higher concentrations of clean sidewalks (OR = 1.48; 95% CI = 1.22, 1.79) were associated with higher odds of dying from an analgesic versus a heroin overdose. By contrast, higher levels of income inequality (OR = 0.74; 95% CI = 0.61, 0.91) and family fragmentation (OR = 0.65; 95% CI = 0.55, 0.78) were associated with lower odds of dying from an analgesic versus a heroin overdose. Income inequality and concentration of clean sidewalks became marginally significant once we adjusted for confounders (models 1 and 2). Median income became nonsignificant once we adjusted for family fragmentation.
TABLE 4.
Hierarchical Logistic Models of the Relationships Between Neighborhood Characteristics and the Odds of Analgesic-Induced Deaths vs Heroin-Induced Deaths: New York City, 2000–2006
| Crude OR (95% CI) | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) | Model 4 OR (95% CI) | |
|---|---|---|---|---|---|
|
|
|||||
| Median income | 1.40 (1.20, 1.65) | 1.31 (1.12, 1.54) | 1.20 (0.98, 1.47) | 1.31 (1.11, 1.54) | 1.11 (0.89, 1.39) |
| Income inequalitya | 0.74 (0.61, 0.91) | 0.83 (0.68, 1.01) | 0.86 (0.70, 1.04) | 0.83 (0.67, 1.02) | 0.86 (0.70, 1.04) |
| Acceptably clean sidewalks | 1.48 (1.22, 1.79) | … | 1.18 (0.94, 1.49) | … | … |
| Dilapidated housing structures | 0.86 (0.70, 1.06) | … | … | 0.99 (0.81, 1.23) | … |
| Family fragmentationb | 0.65 (0.55, 0.78) | … | … | … | 0.71 (0.55, 0.92) |
Note. CI = confidence interval; OR = odds ratio. All models controlled for decedents’ age, gender, and race/ethnicity; percentage of Black residents; and percentage of opiate use.
According to the Gini coefficient (0 = perfectly equitable income distribution, 1 = complete inequality).
Percentage of individuals divorced and separated and percentage of children living in single-parent households.
DISCUSSION
Two key conclusions emerge from this study. First, neighborhood economic disadvantage is associated with higher odds of analgesic overdose fatalities than nonoverdose unintentional fatalities.13,27 Neighborhood level of family fragmentation partially explained this association. Second, analgesic overdose fatalities occur in different neighborhoods than the neighborhoods where heroin overdose fatalities occur. Whereas analgesic overdose fatalities tend to occur in lower-income, more fragmented neighborhoods than nonoverdose unintentional fatalities, they typically occur in higher-income, less unequal, and less fragmented neighborhoods than heroin overdose fatalities.
The relationship observed between neighborhood income and analgesic drug overdose is consistent with the findings of previous studies on illicit drug overdose.35,78,79 Lower-income neighborhoods may shape the risk of drug overdose through a variety of mechanisms, including disproportionate exposure of residents to psychosocial stress, eroded social trust and social capital, and limited access to health and social services.
The particular role of family disruption as a mechanism through which lower-income neighborhoods shape the risk of analgesic overdose53–55 may be attributable to several factors. Neighborhoods where fragmented families are common may have lower levels of collective social control and oversight of delinquent activity, and thus a larger pool of one’s peers are involved in delinquent activities such as use of recreational analgesic opiates.57 Larger drug-using networks are a documented risk factor for drug use.40 Limited collective oversight may also provide the opportunity for the diversion and trafficking of analgesics obtained from legitimate prescription users.80 Finally, socially disrupted contexts may inhibit residents from intervening or calling for help when witnessing an overdose.15,44
Analgesic overdose fatalities occurred in different neighborhoods than overdose fatalities caused by heroin, the main type of illicit opiate. The concentration of analgesic overdoses in higher-income, less fragmented neighborhoods may be attributable to several factors. First, higher-income neighborhoods offer a formal supply of analgesics, through pharmacies and physicians, that is not present in highly disadvantaged, primarily minority neighborhoods where heroin may be the drug of choice. Indeed, several studies, including one conducted in New York City, have shown that pharmacies in disadvantaged, non-White neighborhoods do not have sufficient analgesic supplies to meet legitimate demand.81–83
Second, a certain level of family cohesion may facilitate the informal diffusion of analgesics through friend and kinship networks. Several studies indicate that a key source of illicit analgesics is diversion of prescriptions legitimately filled by parents, relatives, friends, or acquaintances.84–89
Third, neighborhoods with higher concentrations of legitimate analgesic users may have more favorable social norms supporting the use of analgesics. A key motivation for nonmedical analgesic drug use (rather than use of illicit drugs) seems to be the belief that such drugs are less stigmatizing, less dangerous, and less affected by legal consequences than illicit drugs.41,84
Fourth, price may shape drug-specific patterns of demand across neighborhoods90: the lower price of heroin relative to analgesics may create an economic disincentive to consume analgesics in lower-income neighborhoods. Future studies need to examine whether increased access to legal sources of analgesics, weak ties among potential providers (i.e., the elderly and patients with pain) and nonmedical consumers of analgesic opiates, and social norms supportive of nonmedical analgesic drug use contribute to the specific contextual risk of analgesic rather than illicit drug overdose.
Limitations
This study was limited by the nature of our data. First, we used mortality data from OCME files that enumerate all unintentional deaths in New York City. The OCME applies uniform guidelines to its reporting of cases to ensure that causes of death are consistently determined.91 This indicates that the mortality data we used were a valid representation of the causes of death in New York City. We also believe that our data represent a complete count of unintentional mortality cases, given the expectation that all unexpected deaths are reported to the OCME. At the same time, our mortality data did not include information on decedents’ socioeconomic or marital status; residual cross-level confounding according to individual socioeconomic characteristics could thus explain some of the associations observed between neighborhood characteristics and type of death.
Second, we used large geographic areas designated as community districts as proxies for neighborhoods, which may have led to the exclusion of smaller-area heterogeneity in neighborhood characteristics. Given this modifiable areal unit problem, findings may have differed had we chosen a different type of neighborhood boundary.92
Third, we used proportion of accidental nonoverdose deaths with positive opiate toxicology findings to represent opiate use in a given neighborhood. It is possible that the factors contributing to mortality differed from those contributing to drug use. However, the lack of variation in the risk of accidental non-overdose death across neighborhoods allays the concern that such a difference in contributing factors led to bias.
Finally, comparisons between analgesic and heroin overdose fatalities excluded overlapping cases that involved both types of drugs. Had we included such fatalities within the analgesic case definition, we would have found greater similarity between the neighborhoods inhabited by analgesic and heroin overdose decedents.
Conclusions
Notwithstanding the limitations just described, our study indicates that neighborhood family fragmentation may be a key mechanism that facilitates the concentration of analgesic opiate fatalities in lower-income neighborhoods. The distinct geographic patterns of analgesic versus heroin fatalities suggest that analgesic overdose may be shaped by different neighborhood factors than illicit drug overdose.
The occurrence of analgesic overdose fatalities in higher-income, less fragmented neighborhoods than heroin overdose fatalities points to several mechanisms of influence, including pharmacy and physician sources of access to analgesics, the role of kinship and friend networks in diffusing diverted analgesics, and social norms supportive of nonmedical analgesic use. Given the increasing rates of analgesic overdose fatalities1–3 and the systematic distribution of overdose risk across urban neighborhoods,58 there is a critical need for research identifying the particular neighborhood mechanisms that may distinguish the risk of analgesic overdose from that of illicit drug overdose.
Acknowledgments
Funding for this work was provided in part by the National Institutes of Health (grants 1K01DA030449-01, DA06534, and 1 R49 CE002096-01).
Footnotes
Reprints can be ordered at http://www.ajph.org by clicking on the “Reprints” link
Contributors
M. Cerdá designed the analysis, conducted the literature review, and wrote the article. Y. Ransome collaborated on the design of the analysis, implemented the analysis, and provided input on the article. K. M. Keyes and K. C. Koenen collaborated on the analysis plan and literature review and substantially edited all sections of the article. K. Tardiff and D. Vlahov collaborated on the design and implementation of the study and edited all sections of the article. S. Galea collaborated on the design and implementation of the study, as well as on the design of the analysis, and substantially edited all sections of the article.
Human Participant Protection
This study was approved by the institutional review boards of the New York Academy of Medicine and the University of Michigan. Informed consent was not needed because we used mortality records.
Contributor Information
Magdalena Cerdá, Department of Epidemiology, Columbia University Mailman School of Public Health, New York, NY.
Yusuf Ransome, Department of Sociomedical Sciences, Columbia University Mailman School of Public Health.
Katherine M. Keyes, Department of Epidemiology, Columbia University Mailman School of Public Health, New York, NY.
Karestan C. Koenen, Department of Epidemiology, Columbia University Mailman School of Public Health, New York, NY.
Kenneth Tardiff, Department of Psychiatry, Weill Cornell Medical College, New York, NY.
David Vlahov, School of Nursing, University of California, San Francisco.
Sandro Galea, Department of Epidemiology, Columbia University Mailman School of Public Health, New York, NY.
References
- 1.Hanson K. A pill problem: prescription drug abuse is the fastest growing form of substance abuse. State Legis. 2010;36(3):22–25. [PubMed] [Google Scholar]
- 2.Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363(21):1981–1985. doi: 10.1056/NEJMp1011512. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics. [Accessed May 24, 2013];Deaths: final data for 2006. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf.
- 4.National Vital Statistics System. Multiple Cause of Death Dataset: 2007. Atlanta, GA: Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 5.Paulozzi LJ. Opioid analgesic involvement in drug abuse deaths in American metropolitan areas. Am J Public Health. 2006;96(10):1755–1757. doi: 10.2105/AJPH.2005.071647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Opioid Analgesics in New York City: Misuse, Morbidity and Mortality Update. New York, NY: New York City Department of Health and Mental Hygiene; 2011. [Google Scholar]
- 7.Green TC, Grau LE, Carver HW, Kinzly M, Heimer R. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997–2007. Drug Alcohol Depend. 2011;115(3):221–228. doi: 10.1016/j.drugalcdep.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 9.Paulozzi LJ, Logan JE, Hall AJ, McKinstry E, Kaplan JA, Crosby AE. A comparison of drug overdose deaths involving methadone and other opioid analgesics in West Virginia. Addiction. 2009;104(9):1541–1548. doi: 10.1111/j.1360-0443.2009.02650.x. [DOI] [PubMed] [Google Scholar]
- 10.Shah NG, Lathrop SL, Reichard RR, Landen MG. Unintentional drug overdose death trends in New Mexico, USA, 1990–2005: combinations of heroin, cocaine, prescription opioids and alcohol. Addiction. 2008;103(1):126–136. doi: 10.1111/j.1360-0443.2007.02054.x. [DOI] [PubMed] [Google Scholar]
- 11.Martins SS, Fenton MC, Keyes KM, Blanco C, Zhu H, Storr CL. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol Med. 2012;42(6):1261–1272. doi: 10.1017/S0033291711002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pletcher MJ, Kertesz SG, Sidney S, Kiefe CI, Hulley SB. Incidence and antecedents of nonmedical prescription opioid use in four US communities: the Coronary Artery Risk Development in Young Adults (CARDIA) prospective cohort study. Drug Alcohol Depend. 2006;85(2):171–176. doi: 10.1016/j.drugalcdep.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Galea S, Ahern J, Vlahov D. Contextual determinants of drug use risk behavior: a theoretic framework. J Urban Health. 2003;80(suppl 3):iii50–iii58. doi: 10.1093/jurban/jtg082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 15.Galea S, Rudenstine S, Vlahov D. Drug use, misuse, and the urban environment. Drug Alcohol Rev. 2005;24(2):127–136. doi: 10.1080/09595230500102509. [DOI] [PubMed] [Google Scholar]
- 16.Agrawal A, Lynskey M. Are there genetic influences on addiction: evidence from family, adoption and twin studies. Addiction. 2008;103(7):1069–1081. doi: 10.1111/j.1360-0443.2008.02213.x. [DOI] [PubMed] [Google Scholar]
- 17.Dick D, Agrawal A. The genetics of alcohol and other drug dependence. Alcohol Res Health. 2008;31(2):111–118. [PMC free article] [PubMed] [Google Scholar]
- 18.Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol. 2002;111(3):411–424. [PubMed] [Google Scholar]
- 19.Niaura R, Bock B, Lloyd EE, Brown R, Lipsitt LP, Buka S. Maternal transmission of nicotine dependence: psychiatric, neurocognitive and prenatal factors. Am J Addict. 2001;10(1):16–29. doi: 10.1080/105504901750160420. [DOI] [PubMed] [Google Scholar]
- 20.Urban N, Martinez D. Neurobiology of addiction: insight from neurochemical imaging. Psychiatr Clin North Am. 2012;35(2):521–541. doi: 10.1016/j.psc.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Gruenewald PJ. The spatial ecology of alcohol problems: niche theory and assortative drinking. Addiction. 2007;102(6):870–878. doi: 10.1111/j.1360-0443.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- 22.Kuo M, Wechsler H, Greenberg P, Lee H. The marketing of alcohol to college students: the role of low prices and special promotions. Am J Prev Med. 2003;25(3):204–211. doi: 10.1016/s0749-3797(03)00200-9. [DOI] [PubMed] [Google Scholar]
- 23.Cerdá M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120(1–3):22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McClure AC, Stoolmiller M, Tanski SE, Worth KA, Sargent JD. Alcohol-branded merchandise and its association with drinking attitudes and outcomes in US adolescents. Arch Pediatr Adolesc Med. 2009;163(3):211–217. doi: 10.1001/archpediatrics.2008.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peterson NA, Lowe JB, Reid RJ. Tobacco outlet density, cigarette smoking prevalence, and demographics at the county level of analysis. Subst Use Misuse. 2005;40(11):1627–1635. doi: 10.1080/10826080500222685. [DOI] [PubMed] [Google Scholar]
- 26.Ponicki WR, Gruenewald PJ, LaScala EA. Joint impacts of minimum legal drinking age and beer taxes on US youth traffic fatalities, 1975 to 2001. Alcohol Clin Exp Res. 2007;31(5):804–813. doi: 10.1111/j.1530-0277.2007.00363.x. [DOI] [PubMed] [Google Scholar]
- 27.Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav. 2001;42(2):151–165. [PubMed] [Google Scholar]
- 28.Schroeder JR, Latkin CA, Hoover DR, Curry AD, Knowlton AR, Celentano DD. Illicit drug use in one’s social network and in one’s neighborhood predicts individual heroin and cocaine use. Ann Epidemiol. 2001;11(6):389–394. doi: 10.1016/s1047-2797(01)00225-3. [DOI] [PubMed] [Google Scholar]
- 29.Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug Alcohol Depend. 1996;43(3):155–161. doi: 10.1016/s0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- 30.Ennett ST, Flewelling RL, Lindrooth RC, Norton EC. School and neighborhood characteristics associated with school rates of alcohol, cigarette, and marijuana use. J Health Soc Behav. 1997;38(1):55–71. [PubMed] [Google Scholar]
- 31.Fuller CM, Borrell LN, Latkin CA, et al. Effects of race, neighborhood, and social network on age at initiation of injection drug use. Am J Public Health. 2005;95 (4):689–695. doi: 10.2105/AJPH.2003.02178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prev Sci. 2002;3(2):125–133. doi: 10.1023/a:1015483317310. [DOI] [PubMed] [Google Scholar]
- 33.Latkin CA, Williams CT, Wang J, Curry AD. Neighborhood social disorder as a determinant of drug injection behaviors: a structural equation modeling approach. Health Psychol. 2005;24(1):96–100. doi: 10.1037/0278-6133.24.1.96. [DOI] [PubMed] [Google Scholar]
- 34.Brook JS, Nomura C, Cohen P. A network of influences on adolescent drug involvement: neighborhood, school, peer, and family. Genet Soc Gen Psychol Monogr. 1989;115(1):123–145. [PubMed] [Google Scholar]
- 35.Galea S, Ahern J, Vlahov D, et al. Income distribution and risk of fatal drug overdose in New York City neighborhoods. Drug Alcohol Depend. 2003;70(2):139–148. doi: 10.1016/s0376-8716(02)00342-3. [DOI] [PubMed] [Google Scholar]
- 36.Galea S, Ahern J, Tracy M, Vlahov D. Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am J Prev Med. 2007;32 (suppl 6):S195–S202. doi: 10.1016/j.amepre.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bohnert AS, Nandi A, Tracy M, et al. Policing and risk of overdose mortality in urban neighborhoods. Drug Alcohol Depend. 2011;113(1):62–68. doi: 10.1016/j.drugalcdep.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ali MM, Dwyer DS. Social network effects in alcohol consumption among adolescents. Addict Behav. 2010;35 (4):337–342. doi: 10.1016/j.addbeh.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 39.James SE, Johnson J, Raghavan C. I couldn’t go anywhere”—contextualizing violence and drug abuse: a social network study. Violence Against Women. 2004;10(9):991–1014. [Google Scholar]
- 40.Latkin CA, Hua W, Tobin K. Social network correlates of self-reported non-fatal overdose. Drug Alcohol Depend. 2004;73(1):61–67. doi: 10.1016/j.drugalcdep.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 41.Lord S, Brevard J, Budman S. Connecting to young adults: an online social network survey of beliefs and attitudes associated with prescription opioid misuse among college students. Subst Use Misuse. 2011;46(1):66–76. doi: 10.3109/10826084.2011.521371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mundt MP. The impact of peer social networks on adolescent alcohol use initiation. Acad Pediatr. 2011;11 (5):414–421. doi: 10.1016/j.acap.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hembree C, Galea S, Ahern J, et al. The urban built environment and overdose mortality in New York City neighborhoods. Health Place. 2005;11(2):147–156. doi: 10.1016/j.healthplace.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 44.Nandi A, Galea S, Ahern J, Bucciarelli A, Vlahov D, Tardiff K. What explains the association between neighborhood-level income inequality and the risk of fatal overdose in New York City? Soc Sci Med. 2006;63(3):662–674. doi: 10.1016/j.socscimed.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 45.Hannon L, Cuddy MM. Neighborhood ecology and drug dependence mortality: an analysis of New York City census tracts. Am J Drug Alcohol Abuse. 2006;32 (3):453–463. doi: 10.1080/00952990600753966. [DOI] [PubMed] [Google Scholar]
- 46.Ross CE, Jang SJ. Neighborhood disorder, fear, and mistrust: the buffering role of social ties with neighbors. Am J Community Psychol. 2000;28(4):401–420. doi: 10.1023/a:1005137713332. [DOI] [PubMed] [Google Scholar]
- 47.Weich S, Blanchard M, Prince M, Burton E, Erens B, Sproston K. Mental health and the built environment: cross-sectional survey of individual and contextual risk factors for depression. Br J Psychiatry. 2002;180:428–433. doi: 10.1192/bjp.180.5.428. [DOI] [PubMed] [Google Scholar]
- 48.Perdue T, Hagan H, Thiede H, Valleroy L. Depression and HIV risk behavior among Seattle-area injection drug users and young men who have sex with men. AIDS Educ Prev. 2003;15(1):81–92. doi: 10.1521/aeap.15.1.81.23842. [DOI] [PubMed] [Google Scholar]
- 49.Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl) 2001;158 (4):343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- 50.Cohen DA, Farley TA, Mason K. Why is poverty unhealthy? Social and physical mediators. Soc Sci Med. 2003;57(9):1631–1641. doi: 10.1016/s0277-9536(03)00015-7. [DOI] [PubMed] [Google Scholar]
- 51.Shihadeh ES, Steffensmeier DJ. Economic inequality, family disruption, and urban black violence: cities as units of stratification and social control. Soc Forces. 1994;73(2):729–751. [Google Scholar]
- 52.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blau JR, Blau PM. The cost of inequality—metropolitan structure and violent crime. Am Sociol Rev. 1982;47(1):114–129. [Google Scholar]
- 54.Sampson RJ. Urban black violence—the effect of male joblessness and family disruption. Am J Sociol. 1987;93(2):348–382. [Google Scholar]
- 55.Sampson RJ, Groves WB. Community structure and crime: testing social-disorganization theory. Am J Sociol. 1989;94(4):774–802. [Google Scholar]
- 56.Sampson R, Wilson W. Toward a theory of race, crime, and urban inequality. In: Hagan J, Peterson R, editors. Crime and Inequality. Stanford, CA: Stanford University Press; 1990. pp. 37–54. [Google Scholar]
- 57.Bernburg JG, Thorlindsson T, Sigfusdottir ID. The neighborhood effects of disrupted family processes on adolescent substance use. Soc Sci Med. 2009;69(1):129–137. doi: 10.1016/j.socscimed.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 58.Cerdá M, Ransome Y, Keyes K, et al. Prescription opiate mortality trends in New York City, 1990–2006: examining the emergence of an epidemic. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2012.12.027. published online ahead of print January 25, 2013. doi: 10.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bryant WK, Galea S, Tracy M, Piper TM, Tardiff KJ, Vlahov D. Overdose deaths attributed to methadone and heroin in New York City, 1990–1998. Addiction. 2004;99(7):846–854. doi: 10.1111/j.1360-0443.2004.00693.x. [DOI] [PubMed] [Google Scholar]
- 60.Frank B. An overview of heroin trends in New York City: past, present and future. Mt Sinai J Med. 2000;67 (5–6):340–346. [PubMed] [Google Scholar]
- 61.International Classification of Diseases, 10th Revision. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 62.Comstock RD, Mallonee S, Jordan F. A comparison of two surveillance systems for deaths related to violent injury. Inj Prev. 2005;11(1):58–63. doi: 10.1136/ip.2004.007567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Landen MG, Castle S, Nolte KB, et al. Methodological issues in the surveillance of poisoning, illicit drug overdose, and heroin overdose deaths in New Mexico. Am J Epidemiol. 2003;157(3):273–278. doi: 10.1093/aje/kwf196. [DOI] [PubMed] [Google Scholar]
- 64.Sternfeld I, Perras N, Culross PL. Development of a coroner-based surveillance system for drug-related deaths in Los Angeles County. J Urban Health. 2010;87 (4):656–669. doi: 10.1007/s11524-010-9455-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Galea S, Ahern J, Tardiff K, et al. Racial/ethnic disparities in overdose mortality trends in New York City, 1990–1998. J Urban Health. 2003;80(2):201–211. doi: 10.1093/jurban/jtg023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Miller JR, Piper TM, Ahern J, et al. Income inequality and risk of suicide in New York City neighborhoods: a multilevel case-control study. Suicide Life Threat Behav. 2005;35(4):448–459. doi: 10.1521/suli.2005.35.4.448. [DOI] [PubMed] [Google Scholar]
- 67.2000 SF3 Sample Data. Washington, DC: US Census Bureau; 2012. [Google Scholar]
- 68.Cerdá M, Tracy M, Messner SF, Vlahov D, Tardiff K, Galea S. Misdemeanor policing, physical disorder, and gun-related homicide in New York City: a spatial analytic test of “broken windows” theory. Epidemiology. 2009;20 (4):533–541. doi: 10.1097/EDE.0b013e3181a48a99. [DOI] [PubMed] [Google Scholar]
- 69.New York City Housing and Vacancy Survey. Washington, DC: US Bureau of the Census; 1999. [Google Scholar]
- 70.Citywide Performance Report. New York, NY: New York City Mayor’s Office of Operations; 2012. [Google Scholar]
- 71.Messner SF, Galea S, Tardiff KJ, et al. Policing, drugs, and the homicide decline in New York City in the 1990s. Criminology. 2007;45(2):385–413. [Google Scholar]
- 72.ArcGIS Desktop: Release 10. Redlands, CA: Environmental Systems Research Institute; 2011. [Google Scholar]
- 73.Pfeiffer D. Spatial Analysis in Epidemiology. Oxford, UK: Oxford University Press; 2008. [Google Scholar]
- 74.Anselin L. An Introduction to Spatial Autocorrelation Analysis with GeoDa. Urbana, IL: Spatial Analysis Laboratory, Department of Agricultural and Consumer Economics; 2003. [Google Scholar]
- 75.OpenGeoDa for Windows Version 1.20. Tempe, AZ: GeoDa Center for Geospatial Analysis and Computation, Arizona State University; 2012. [Google Scholar]
- 76.Neuhaus JM, Kalbfleisch JD, Hauck WW. A comparison of cluster-specific and population-averaged approaches for analyzing correlated binary data. Int Stat Rev. 1991;59:25–35. [Google Scholar]
- 77.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 78.Gotsens M, Mari-Dell’Olmo M, Martinez-Beneitod MA, et al. Socioeconomic inequalities in mortality due to injuries in small areas of ten cities in Spain (MEDEA Project) Accid Anal Prev. 2011;43(5):1802–1810. doi: 10.1016/j.aap.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 79.Marzuk PM, Tardiff K, Leon AC, et al. Poverty and fatal accidental drug overdoses of cocaine and opiates in New York City: an ecological study. Am J Drug Alcohol Abuse. 1997;23(2):221–228. doi: 10.3109/00952999709040943. [DOI] [PubMed] [Google Scholar]
- 80.Davis WR, Johnson BD. Prescription opioid use, misuse, and diversion among street drug users in New York City. Drug Alcohol Depend. 2008;92(1–3):267–276. doi: 10.1016/j.drugalcdep.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mayer JD, Kirlin B, Rehm CD, Loeser JD. Opioid availability in outpatient pharmacies in Washington State. Clin J Pain. 2008;24(2):120–123. doi: 10.1097/AJP.0b013e3181590d4f. [DOI] [PubMed] [Google Scholar]
- 82.Green CR, Ndao-Brumblay SK, West B, Washington T. Differences in prescription opioid analgesic availability: comparing minority and white pharmacies across Michigan. J Pain. 2005;6(10):689–699. doi: 10.1016/j.jpain.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 83.Morrison RS, Wallenstein S, Natale DK, Senzel RS, Huang LL. We don’t carry that”: failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. N Engl J Med. 2000;342(14):1023–1026. doi: 10.1056/NEJM200004063421406. [DOI] [PubMed] [Google Scholar]
- 84.Inciardi JA, Surratt HL, Cicero TJ, Beard RA. Prescription opioid abuse and diversion in an urban community: the results of an ultrarapid assessment. Pain Med. 2009;10(3):537–548. doi: 10.1111/j.1526-4637.2009.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Inciardi JA, Surratt HL, Cicero TJ, Kurtz SP, Martin SS, Parrino MW. The “black box” of prescription drug diversion. J Addict Dis. 2009;28(4):332–347. doi: 10.1080/10550880903182986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ward L, Patel NM, Hanlon A, Eldakar-Hein S, Sherlinski K, Ward SH. Prescription medication borrowing among adult patients at an urban medical center. J Urban Health. 2011;88(6):997–1014. doi: 10.1007/s11524-011-9589-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Carise D, Dugosh KL, McLellan AT, Camilleri A, Woody GE, Lynch KG. Prescription OxyContin abuse among patients entering addiction treatment. Am J Psychiatry. 2007;164(11):1750–1756. doi: 10.1176/appi.ajp.07050252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Green TC, Grimes Serrano JM, Licari A, Budman SH, Butler SF. Women who abuse prescription opioids: findings from the Addiction Severity Index-Multimedia Version Connect prescription opioid database. Drug Alcohol Depend. 2009;103(1–2):65–73. doi: 10.1016/j.drugalcdep.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the Internet: who are the end users? Drug Alcohol Depend. 2010;110(1–2):21–29. doi: 10.1016/j.drugalcdep.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Greenwald MK, Hursh SR. Behavioral economic analysis of opioid consumption in heroin-dependent individuals: effects of unit price and pre-session drug supply. Drug Alcohol Depend. 2006;85(1):35–48. doi: 10.1016/j.drugalcdep.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 91.Tardiff K, Marzuk PM, Leon AC, et al. Accidental fatal drug overdoses in New York City: 1990–1992. Am J Drug Alcohol Abuse. 1996;22(2):135–146. doi: 10.3109/00952999609001650. [DOI] [PubMed] [Google Scholar]
- 92.Mobley LR, Kuo TM, Andrews L. How sensitive are multilevel regression findings to defined area of context?: a case study of mammography use in California. Med Care Res Rev. 2008;65(3):315–337. doi: 10.1177/1077558707312501. [DOI] [PMC free article] [PubMed] [Google Scholar]