SUMMARY
The aim of the present study was to test the hypothesis that increasing kidney tissue epoxyeicosatrienoic acids (EETs) concentration by preventing their degradation to the biologically inactive dihydroxyeicosatrienoic acids (DHETEs) using blockade of soluble epoxide hydrolase (sEH), would attenuate the progression of chronic kidney disease (CKD). Ren-2 transgenic rats (TGR) after 5/6 renal mass reduction (5/6 NX) served as a model of CKD associated with angiotensin II (ANG II)-dependent hypertension. sEH was inhibited using cis-4-[4-(3-adamantan-1-yl-ureido)cyclohexyloxy]benzoic acid (c-AUCB, 3 mg/l of drinking water) for 20 weeks after 5/6 NX. Sham-operated normotensive transgene-negative Hannover Sprague-Dawley (HanSD) rats served as controls. c-AUCB treatment when applied in TGR subjected to 5/6 NX improved the rats’ survival rate, prevented the increase in blood pressure, retarded the progression of cardiac hypertrophy, reduced proteinuria and the degree of glomerular and tubulointerstitial injury, and reduced the glomerular volume, All these organ-protective actions were associated with normalization of the intrarenal EETs/DHETEs ratio, an index of availability of biologically active EETs, to levels observed in sham-operated HanSD rats. There were no significant concurrent alterations of increased intrarenal ANG II content. Taken together, these results show that, first, 5/6 NX TGR exhibit a profound deficiency of intrarenal availability of active epoxygenase metabolites (EETs), which probably contributes to the progression of CKD in this model of ANG II-dependent hypertension. Second, restoration of intrarenal availability of EETs using long-term c-AUCB treatment exhibits substantial renoprotective actions.
Keywords: chronic kidney disease (CKD), 5/6 nephrectomy, end-organ damage, hypertension, cytochrome P450 enzymes, epoxyeicosatrienoic acids, soluble epoxide hydrolase (sEH), renin-angiotensin system (RAS)
INTRODUCTION
Chronic kidney disease (CKD) represents a serious problem of current nephrology and its incidence has been increasing steadily.1 The recognition that CKD tends to progress to end-stage renal disease (ESRD), regardless of the initial cause, has initiated extensive research of the underlying mechanism(s) and of potential therapeutic strategies aimed to interrupt or at least slow-down the progression of CKD to ESRD 2–4. To this purpose, a model of 5/6 renal mass reduction (5/6 NX), consisting in unilateral nephrectomy combined with surgical removal of 2/3 of the contralateral kidney, has been widely used. Despite extensive investigation conducted over the past 40 years, mechanism(s) responsible for the progression of CKD to ESRD remain poorly understood. However, it is clear that different renal diseases exhibit common pathomorphological signs such as tubulointerstitial fibrosis and tubular atrophy, followed by glomerulosclerosis 4–7. The studies employing the 5/6 NX model have demonstrated that hypertension and inappropriately activated renin-angiotensin system (RAS) are two critical determinants of the progression rate of CKD to ESRD 3,8–13. In addition, both experimental and clinical studies have shown that RAS blocking agents such as angiotensin converting enzyme (ACE) inhibitors (ACEis) and angiotensin II (ANG II) receptor blockers (ARBs), are highly effective inhibitors of the progression of CKD (renoprotective action) 8,14–17. Therefore, antihypertensive therapeutic regime involving direct inhibition of RAS is currently accepted as a golden standard in the therapy.
However, the effectiveness of renoprotective action of RAS inhibition is limited, especially in advanced CKD 18–20. This points to the need for more complex pharmacologic strategies which would possibly target also control systems other than RAS. Considerable attention has been focused on the role of active metabolites of arachidonic acid (ARA), those generated by cytochrome P450 (CYP)-dependent enzymes. An evidence indicates that ARA is metabolized by CYP epoxygenases to produce epoxyeicosatrienoic acids (EETs), which are important regulators of cardiovascular and renal function 21–23. It has been shown that increasing kidney tissue EETs by preventing their degradation to biologically inactive dihydroxyeicosatrienoic acids (DHETEs), as achieved by blockade of soluble epoxide hydrolase (sEH), displays antihypertensive, cardio- and renoprotective actions 24–32. Therefore, increasing bioavailability of EETs in kidney could be a new strategy to prevent progression of CKD to ESRD. However, recent studies addressing this issue yielded opposed results. A study that employed overexpression of CYP2J2, an enzyme that produces EETs, demonstrated important renoprotective effects in 5/6 NX rats 33, while the other study that pharmacologically inhibited sEH failed to elicit renoprotective actions and increased the rate of progression of CKD in 5/6 NX mice 34.
Considering this striking controversy and also in view of the established knowledge that hypertension and increased intrarenal RAS are the critical determinants of hypertension-associated end-organ damage and progression of CKD, we examined whether long-term treatment with an sEH inhibitor would retard the progression of CKD in 5/6 NX Ren-2 renin transgenic rats (TGR). In addition, application of this well-defined monogenetic model of angiotensin II (ANG II)-dependent hypertension with endogenous activation of RAS35 appeared well-suited for the purpose.
RESULTS
Series 1: Assessment concentrations of ANG II, EETs, DHETEs and 20-hydroxyeicosatrienoic acid (20-HETE) and Western blot analysis of renal cortical CYP protein expression in the early phase after 5/6 NX
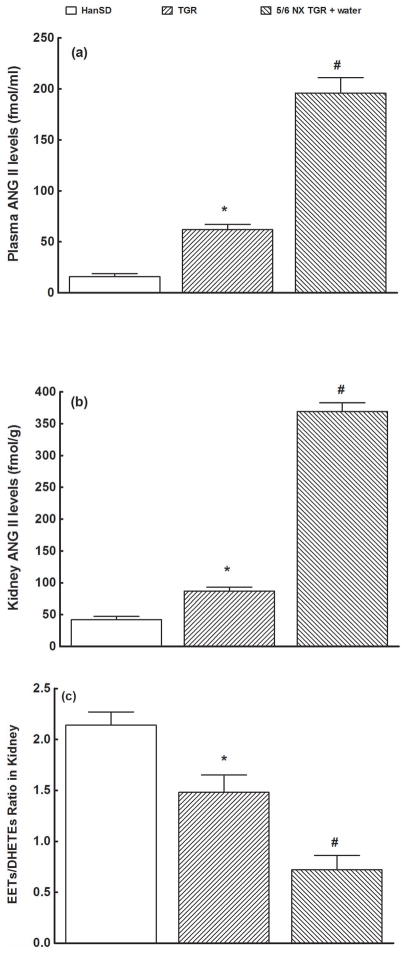
As shown in Figure 1a, plasma ANG II levels in sham-operated TGR were significantly higher compared with sham-operated HanSD (62 ± 5 vs. 16 ± 3 fmol/ml, p<0.05), and 5/6 NX elicited in the early phase substantial increases in plasma ANG II compared with sham-operated TGR (196 ± 15 vs. 62 ± 5 fmol/ml, p<0.05). Likewise, total kidney ANG II concentrations in sham-operated TGR were significantly higher than in sham-operated HanSD, and in the early phase 5/6 NX caused a further increase to concentrations that were much higher compared with those in sham-operated TGR (369 ± 14 vs. 87 ± 6 fmol/g, p<0.05) (Figure 1b). As shown in Figure 1c, the intrarenal availability of biologically active epoxygenase metabolites, expressed as the EETs/DHETEs ratio, was in sham-operated TGR significantly lower than in sham-operated HanSD rats, and already in the early phase 5/6 NX elicited a further profound decrease in the EETs/DHETEs ratio compared with sham-operated TGR (0.72 ± 0.14 vs. 1.48 ± 0.17, p<0.05).
Figure 1.
Plasma (a) and kidney (b) angiotensin II (ANG II) concentrations (b), and the epoxyeicosatrienoic acids (EETs)/dihydroxyeicosatrienoic acids (DHETEs) concentration ratio (c)) measured 4 weeks after 5/6 NX (early phase) in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats, in heterozygous Ren-2 transgenic rats (TGR), and in untreated (water vehicle) 5/6 NX TGR rats.
* P<0.05 compared with sham-operated HanSD rats. # P<0.05 compared with sham-operated TGR.
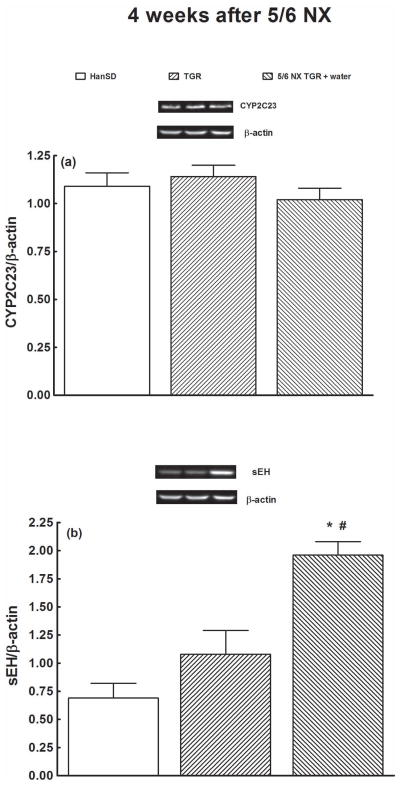
As shown in Figure 2, densitometric analysis revealed no significant differences in CYP2C3 or sEH protein expression in the renal cortex between HanSD rats and TGR (data normalized for β-actin). In the case of sEH, protein expression tended to be higher in TGR compared with HanSD rat (not significant, Figure 2b). 5/6 NX in the early phase did not alter protein expression for CYP2C3 but significantly increased that for sEH.
Figure 2.
CYP2C3 protein expression (a) and soluble epoxide hydrolase (sEH) (b) in kidney cortex measured 4 weeks after 5/6 NX in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats, in heterozygous Ren-2 transgenic rats (TGR), and in untreated (water) 5/6 NX TGR rats.
* P<0.05 compared with sham-operated HanSD rats. # P<0.05 compared with sham-operated TGR at the same time point.
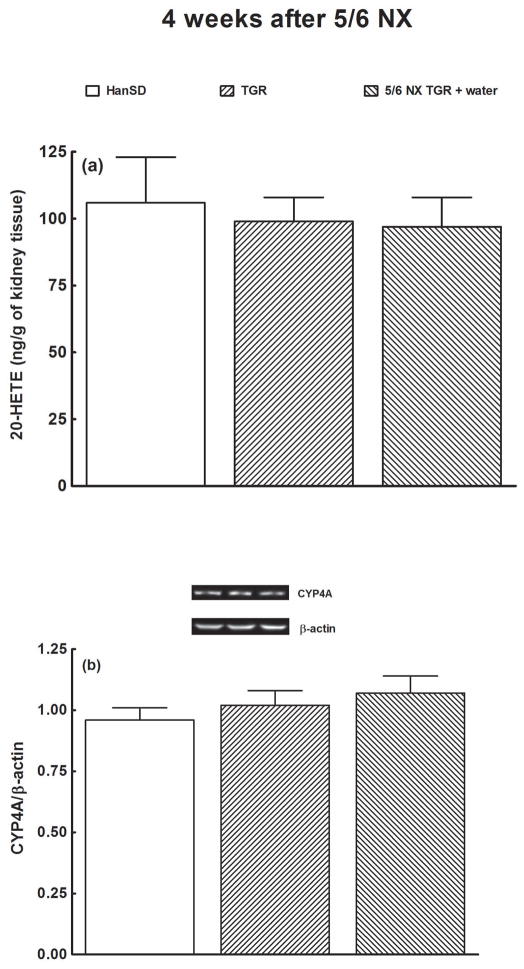
As shown in Figure 3, there were no significant differences in CYP4A protein expression and 20-HETE concentrations in the renal cortex between HanSD rats and TGR, and 5/6 NX did not alter either value.
Figure 3.
Concentrations of 20- hydroxyeicosatrienoic acid (20-HETE) (a) and CYP4A protein expression (b) in the kidney cortex, measured 4 weeks after 5/6 NX in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats, in heterozygous Ren-2 transgenic rats (TGR), and in untreated (water) 5/6 NX TGR rats.
Series 2: Effects of RAS blockade and sEHi on survival rate and signs of end-organ damage
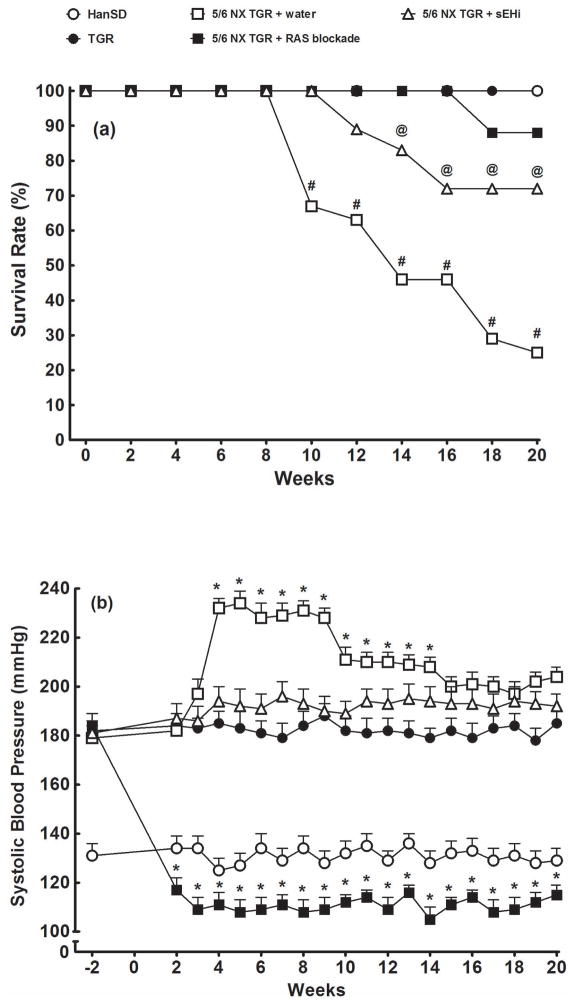
All sham-operated TGR and HanSD rats survived until the end of experiment. As shown in Figure 4a, untreated 5/6 NX TGR began to die at week 9 after 5/6 NX, with the final survival rate of 25 %. Both therapeutical regimes, i.e. RAS blockade and sEH inhibition, substantially improved post-5/6 NX survival rates in TGR, however, the former regime was more efficient (88 vs. 72 %, p<0.05).
Figure 4.
Survival rates (a) and systolic blood pressure (b) values in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats and in heterozygous Ren-2 transgenic rats (TGR), and in 5/6 nephrectomized (5/6 NX) TGR rats, untreated (water) or receiving, combined renin-angiotensin system (RAS) blockade with trandolapril, an angiotensin converting enzyme inhibitor and losartan, an angiotensin II receptor blocker. Alternatively, 5/6 NX TGR were treated with soluble epoxide hydrolase inhibitor (sEHi). * P<0.05 compared with baseline values. # P<0.05 compared with sham-operated TGR at the same time point. @ P<0.05 compared with 5/6 NX TGR + RAS blockade at the same time point.
As shown in Figure 4b, sham-operated HanSD rats remained normotensive and sham-operated TGR were considerably hypertensive, without any significant alterations in SBP during the experiment. In TGR, 5/6 NX caused further significant increase in SBP above the initial SBP of 179 ± 5 mmHg, with the maximum reached at week 8 after 5/6 NX (231 ± 4 mmHg, p<0.05). sEHi treatment prevented this increase and SBP remained at the same level as observed in sham-operated TGR. In contrast, RAS blockade not only prevented an increase in SBP in TGR after 5/6 NX, but rapidly reduced it, even below the levels observed in sham-operated HanSD rats (115 ± 4 vs. 129 ± 4 mmHg, p<0.05).
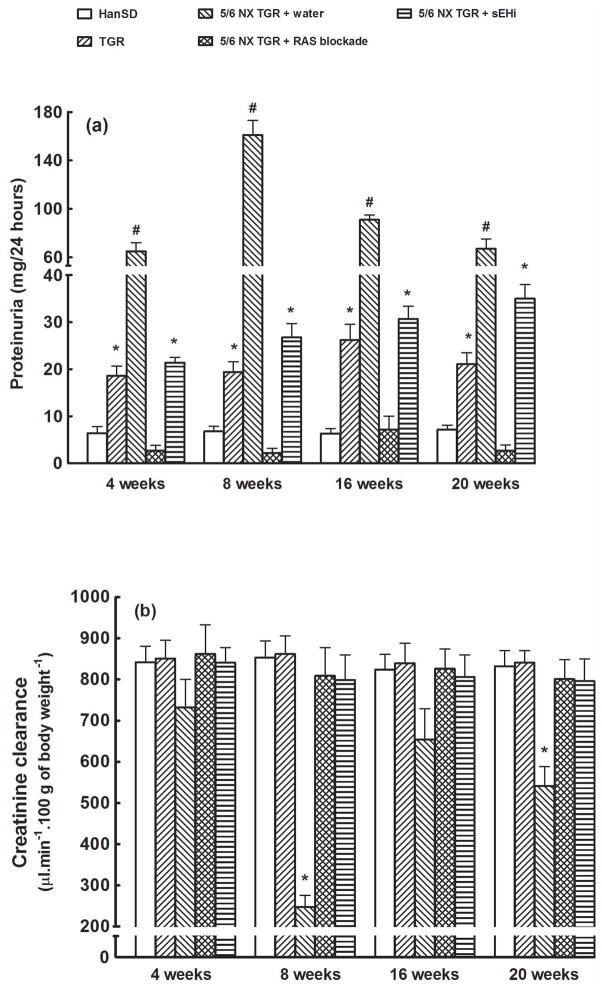
As shown in Figure 5a, sham-operated HanSD rats exhibited minimal proteinuria throughout the experiment (at the end: 7.2 ± 0.9 mg/24 h). Sham-operated TGR revealed pronounced proteinuria, more than 3-fold higher than that observed in sham-operated HanSD rats, throughout the experiment. Untreated 5/6 NX TGR showed a marked increase in proteinuria reaching the maximum 8 weeks after 5/6 NX (161 ± 12 mg/24 h, p<0.05 vs. all the other corresponding values). RAS blockade prevented the increase in proteinuria that occurred after 5/6 NX in TGR and until end of the experiment the proteinuria was even lower than observed in sham-operated HanSD rats (2.7 ± 1.2 vs. 7.2 ± 0.9 mg/24 h, p<0.05). sEHi treatment attenuated the increase in proteinuria in 5/6 NX TGR and 16 weeks after 5/6 NX the values observed were similar as those in sham-operated TGR; subsequently (at week 20 after 5/6 NX), proteinuria was higher than observed in sham-operated TGR, but still significantly lower than that in untreated 5/6 NX TGR (35 ± 3 vs. 67 ± 8 mg/24 h, p<0.05).
Figure 5.
Proteinuria (a) and creatinine clearance (b) in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats, in heterozygous Ren-2 transgenic rats (TGR), in 5/6 nephrectomized (5/6 NX) TGR rats {untreated (water) or under combined RAS blockade (trandolapril and losartan)}, and in 5/6 NX TGR treated with soluble epoxide hydrolase inhibitor (sEHi). * P<0.05 compared with sham-operated HanSD rats at the same time point. # P<0.05 compared with sham-operated TGR at the same time point
As shown in Figure 5b, there were no significant differences in creatinine clearance between sham-operated HanSD rats and sham-operated TGR rats throughout the experimental period, indicating that despite severe hypertension, marked proteinuria and some degree of renal glomerular damage (see below) at the age of 8 months sham-operated TGR did not reveal a significant impairment of renal function. These findings are in accordance with previous studies showing that heterozygous TGR with exposition to no intervention (e.g. high salt or 5/6 NX) exhibit high resistance to the development of hypertension-induced renal damage 11,12. In contrast, untreated 5/6 NX TGR exhibited significantly lower creatinine clearance (especially 8 weeks after 5/6 NX, just before first rats began to die) as compared with sham-operated TGR. Both treatment regimens prevented decreases in creatinine clearance in 5/6 NX TGR.
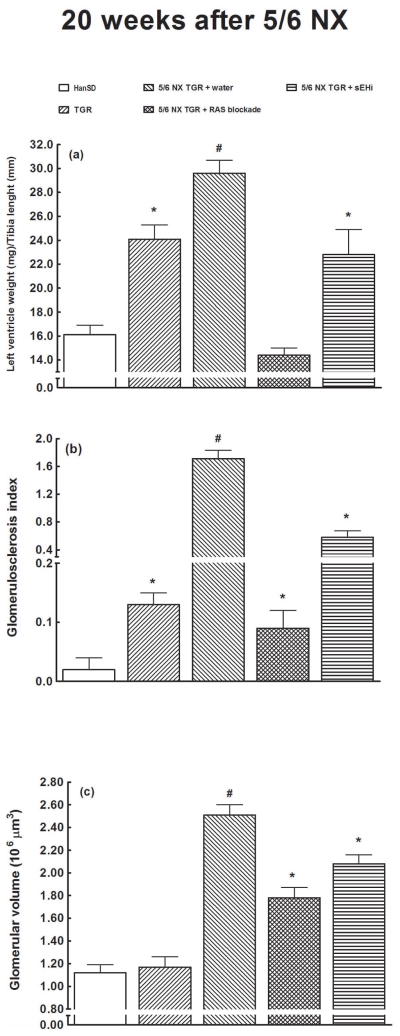
As shown in Figure 6a, sham-operated TGR clearly showed cardiac hypertrophy (measured as the LVW/TL ratio) when compared with sham-operated HanSD rats. In TGR, 5/6 NX induced a marked increase in LVW/TL above the values seen in sham-operated TGR (29.6 ± 1.1 vs. 24.1 ± 1.2, p<0.05). RAS blockade not only prevented the increase in LVW/TL in 5/6 NX TGR but even decreased it below values observed in sham-operated HanSD rats (14.4 ± 0.6 vs. 16.1 ± 0.8, p<0.05). sEH blockade prevented the increase in LVW/TL observed in TGR after 5/6 NX.
Figure 6.
The left ventricle weight to tibia length ratio (a), glomerulosclerosis index (b) and glomerular volume (c) in the late phase (i.e. 20 weeks after 5/6 NX) in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats, in heterozygous Ren-2 transgenic rats (TGR), in 5/6 nephrectomized (5/6 NX) TGR rats {untreated (water) or under combined RAS blockade (trandolapril and losartan)}, and in 5/6 NX TGR treated with soluble epoxide hydrolase inhibitor (sEHi). * P<0.05 compared with sham-operated HanSD rats. # P<0.05 compared with sham-operated TGR.
Sham-operated HanSD rats showed only minimal glomerulosclerosis (measured as GSI) (Fig. 6B). After 5/6 NX, TGR showed a substantial increase in GSI (1.71 ± 0.12 vs. 0.13 ± 0.02 in sham-operated TGR, p<0.05). RAS blockade in 5/6 NX TGR normalized GSI to values observed in sham-operated TGR. sEH inhibition substantially attenuated the increase in GSI after 5/6 NX, but it still remained markedly higher than in sham-operated TGR. The pattern of kidney tubulointerstitial injury closely resembled that of GSI in all groups (data not shown).
As shown in Figure 6c, there was no significant difference between the glomerular volume in sham-operated HanSD rats and sham-operated TGR. Untreated 5/6 NX TGR showed a substantial increase in the glomerular volume compared with the level seen in sham-operated TGR (2.51 ± 0.09 × 106 vs. 1.17 ± 0.09 × 106 μm3, p<0.05). Each of the two therapeutical regimes significantly reduced the glomerular volume in 5/6 NX TGR, but RAS blockade was more effective than sEH inhibition (1.78 ± 0.09 × 106 vs. 2.08 ± 0.08 × 106 μm3, p<0.05).
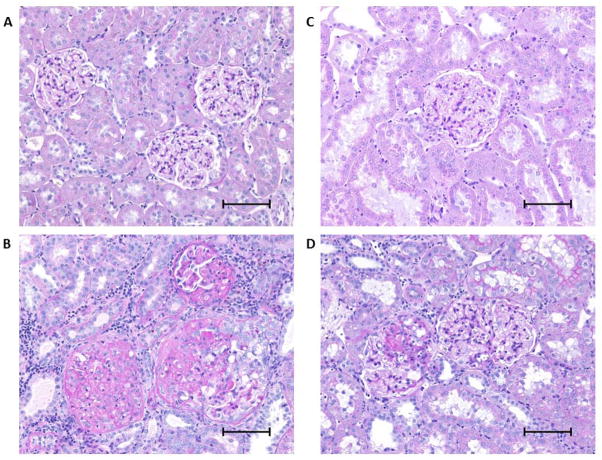
Representative slices of renal tissue stained with periodic acid-Schiff reaction (PAS) of sham-operated HanSD (a), untreated 5/6 NX TGR (b), 5/6 NX TGR treated with RAS blockade (c) and 5/6 NX TGR treated with sEHi (d) are shown in Figure 7.
Figure 7.
Representative renal parenchyma images in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats (A), in 5/6 nephrectomized (5/6 NX) TGR rats, untreated (water) (B) or under RAS blockade (trandolapril and losartan) (C). Alternatively, 5/6 NX TGR were treated with soluble epoxide hydrolase inhibitor (sEHi) (D). Scale bar = 100 μm.
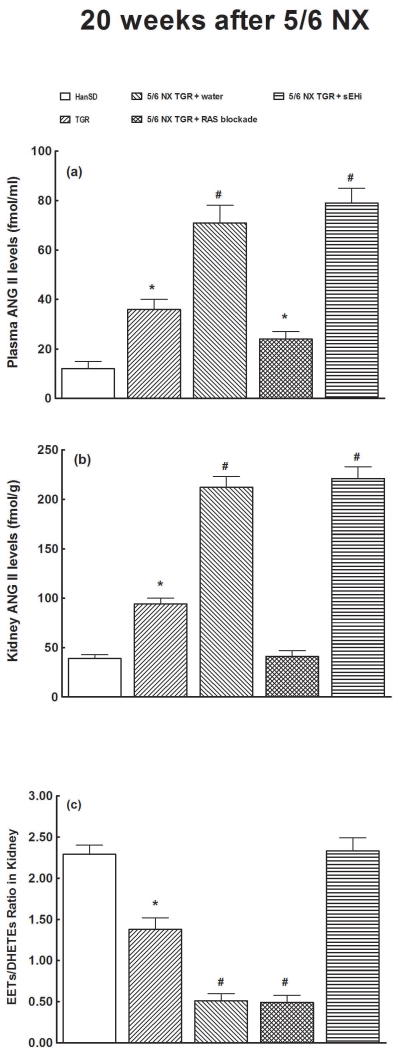
As shown in Figure 8a, plasma ANG II levels were significantly higher in sham-operated TGR than in sham-operated HanSD rats, and 5/6 NX caused, also in the late phase, further increases in plasma ANG II levels in TGR as compared with sham-operated TGR (71 ± 6 vs. 36 ± 4 fmol/ml, p<0.05). Long-term sEH inhibition did not significantly change plasma ANG II levels in 5/6 NX TGR. In contrast, in 5/6 NX TGR, RAS blockade caused significant decrease in plasma ANG II levels to values observed in sham-operated TGR.
Figure 8.
Plasma (a) and kidney (b) angiotensin II (ANG II) concentrations and the epoxyeicosatrienoic acids (EETs)/dihydroxyeicosatrienoic acids (DHETEs) concentration ratio (c) in the late phase (i.e. 20 weeks after 5/6 NX) in sham-operated Hannover Sprague-Dawley (HanSD, transgene-negative) rats, in heterozygous Ren-2 transgenic rats (TGR), and in 5/6 nephrectomized (5/6 NX) TGR rats, untreated (water) or under combined RAS blockade. Alternatively, 5/6 NX TGR were treated with soluble epoxide hydrolase inhibitor (sEHi). * P<0.05 compared with sham-operated HanSD rats. # P<0.05 compared with sham-operated TGR.
Likewise, kidney ANG II concentrations were significantly higher in sham-operated TGR than in sham-operated HanSD rats. After 5/6 NX, the kidney ANG II concenetrations in TGR further increased to a level substantially higher than that seen in sham-operated TGR (212 ± 11 vs. 94 ± 6 fmol/g, p<0.05). In 5/6 NX TGR, RAS blockade decreased kidney ANG II to values that were not significantly different from those in sham-operated HanSD rats (41 ± 6 vs. 39 ± 4 fmol/g). In contrast, sEH blockade did not alter kidney ANG II concentration in 5/6 NX TGR (Figure 8b). As shown in Figure 8c, the intrarenal availability of biologically active epoxygenase metabolites, expressed as the EETs/DHETEs ratio, was in sham-operated TGR significantly lower than in sham-operated HanSD rats. In untreated 5/6 NX TGR the ratio was much lower than in sham-operated TGR (0.51 ± 0.09 vs. 1.28 ± 0.14, p<0.05). RAS blockade in 5/6 NX TGR did not significantly change the ratio, in contrast, sEH inhibition significantly increased it to levels observed in sham-operated HanSD rats.
METHODS
Ethical approval and animals
The studies were performed in accordance with guidelines and practices established by the Animal Care and Use Committee of the Institute for Clinical and Experimental Medicine, Prague, which accord with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes. All animals used in the present study were bred at the Center of Experimental Medicine of this Institute, from stock animals supplied by the Max Delbrück Center for Molecular Medicine, Berlin, Germany, which is accredited by the Czech Association for Accreditation of Laboratory Animal Care. Heterozygous TGR were generated by breeding male homozygous TGR with female homozygous Hannover-Sprague Dawley (HanSD) rats as described in the original study 35, age-matched HanSD rats served as transgene-negative normotensive controls. The animals were kept on a 12-hour/12-hour light/dark cycle. Throughout the experiments rats were fed a normal salt, normal protein diet (0.45% NaCl, 19–21% protein) produced by SEMED (Prague, Czech Republic) and had free access to tap water.
Chemicals
The sEH inhibitor (sEHi), cis-4-[4-(3-adamantan-1-yl-ureido)cyclohexyloxy]benzoic acid (c-AUCB), was prepared freshly and given in drinking water at 3 mg/L 27–32. The dose of c-AUCB was selected based on our recent study where it elicited substantial increases in tissue concentrations of EETs without altering RAS activity 29. We purposely chose the dose of c-AUCB that only blocks sEH activity without altering plasma and tissue ANG II levels, because the major aim of this treatment regime was to evaluate the effects of pharmacologically-induced EETs concentrations on the progression of CKD in 5/6 NX TGR. The activity of RAS can be pharmacologically altered at various levels. We and others 12,36–38 have demonstrated that the pharmacological blockade using combination of ACEi and ARB at high doses provides a cardio- and renoprotection superior to that achieved with routine dosage. Thus, similarly as in our recent studies 11,12, for the “RAS blockade” a combination of trandolapril (6 mg/L drinking water, Gopten; Abbot, Prague, Czech Republic), and of lozap (100 mg/L drinking water, Zentiva, Prague, Czech Republic), was used.
Experimental design
Series 1: Assessment of concentration of ANG II, EETs, DHETEs and 20-hydroxyeicosatrienoic acid (20-HETE), and Western blot analysis of renal cortical CYP protein expression in the early phase after 5/6 NX
The aim of this series was to evaluate the degree of activation of the RAS system and of the synthesis rate at the two CYP dependent enzymatic pathways: epoxygenase and ω-hydroxylase..
Male HanSD rats and TGR, aged nine weeks, were anesthetized (tiletamine + zolazepam, Virbac SA, Carros Cedex, France, 8 mg/kg; and xylasine, Spofa, Czech Republic, 4 mg/kg intramuscularly) and 5/6 NX was performed as described previously 11,12. Sham-operated HanSD rats served as healthy normotensive controls. It is well-recognized that ANG II is the major active product of the RAS and a reliable marker of the the system’s activity 39. Therefore, at the end of experiments, rats were decapitated (without anesthesia), and plasma and tissue ANG II levels were measured by radioimmuassay. This approach was used because we have demonstrated recently that the measured ANG II levels are altered by anaesthesia 40,41. Moreover, we were able to compare the present results with those from our earlier studies of the role of the RAS in the pathophysiology of hypertension 11,12,40–44. In addition, the levels of EETs and DHETEs in the kidney cortex were measured. The samples were extracted, the extracts were separated by reverse-phase high performance liquid chromatography, and analysed by negative-mode electrospray ionization and tandem mass spectroscopy as described previously 27–32,45. Specifically, 8,9-EETs; 11,12-EETs and 14,15-EETs were measured separately and then pooled and presented jointly. These metabolites are the most active products formed in the CYP epoxygenase enzymatic pathway 22,23. The EETs/DHETES ratio was obtained with total concentrations of EETs and of DHETEs. Western blot analysis for protein expression of CYP2C23, the enzyme that is predominantly responsible for the formation of EETs in the kidney, and sEH, the enzyme responsible for the conversion of EETs to DHETEs, in the renal cortex were performed as described previously 29,45, with levels normalized against β-actin. In addition, 20-HETE and protein expression for CYP4A, the enzyme responsible for the formation of 20-HETE, were analysed in the renal cortex as described previously 28.
The following experimental groups were investigated:
-
1
Sham-operated HanSD + water vehicle (n = 7)
-
2
Sham-operated TGR + water (n = 7)
-
3
5/6 NX TGR + water (n = 9)
Series 2: Effects of RAS blockade and sEHi on survival rate and signs of end-organ damage
Male HanSD rats and TGR aged eight weeks, derived from several litters, were randomly assigned to experimental groups to make sure that the animals from a single litter did not prevail in any group. In order to detect inter-group differences in systolic blood pressure (SBP) over time, SBP was measured in accordance with recommendations for blood pressure (BP) measurements in conscious animals, by tail-plethysmography, using a tail-cuff apparatus (MC 4000; Hatteras Instruments Co. and RTBP 1007; Kent Scientific Co.) 46. Three days before starting actual measurements, rats were accustomed to the indirect tail-cuff SBP measurement procedure. This method, regularly employed in our laboratory 11,12, was previously validated and a close correlation was found between these values and those yielded by direct blood pressure (BP) measurements in conscious rats using an indwelling aortic catheter. Measurements of SBP were started 14 days before 5/6 NX and performed at three-day intervals until the end of the experiment. On day 0 (age 9 weeks), 5/6 NX was performed as described above. After 72 hours’ recovery, either appropriate treatment was initiated or rats were left with no treatment. The following experimental groups were investigated:
-
4
Sham-operated HanSD + water (initial n = 10)
-
5
Sham-operated TGR + water (initial n = 10)
-
6
5/6 NX TGR + water (initial n = 24)
-
7
5/6 NX TGR + RAS blockade (initial n = 17)
-
8
5/6 NX TGR + sEHi (initial n = 18)
The follow-up period was 20 weeks. At weeks 4, 8, 16 and 20 after day 0, after appropriate habituation training, the animals were placed in individual metabolic cages and their 24-hour urine was collected for determination of protein and creatinine. Blood samples from the tail vein were taken and plasma creatinine concentrations were measured by picric acid colorimetric method using a commercially available kit (Lachema, Brno, Czech Republic). This approach was previously validated and is regularly used in our studies 11,12. At the end of experiments, rats were decapitated (without anesthesia), ANG II, EETs and DHETEs levels were assessed as described for series 1.
The samples from the second half of kidney were used to assess renal glomerular damage. The kidneys were fixed in 4% formaldehyde, dehydrated and embedded in paraffin. The sections stained with hematoxylin–eosin and PAS (periodic acid, for Schiff reaction) were examined and evaluated in a blind-test fashion. Fifty glomeruli in each kidney were examined on a semi-quantitative scale as described previously 47: grade 0, all glomeruli normal; grade 1, sclerotic area up to 25% (minimal sclerosis); grade 2, sclerotic area 25 to 50% (moderate sclerosis); grade 3, sclerotic area 50 to 75% (moderate-to-severe sclerosis); grade 4, and sclerotic area 75 to 100% (severe sclerosis). The glomerulosclerosis index (GSI) was calculated using the following formula: , where nx is the number of glomeruli in each grade of glomerulosclerosis.
Renal cortical tubulointerstitial injury was evaluated as defined by Nakano et al. 47 and as used in our recent studies 11,12, to determine inflammatory cell infiltration, tubular dilatation, atrophy, or interstitial fibrosis. The injury was graded semi-quantitatively using the following scale of lesions: grade 0, no abnormal findings; 1, mild (<25 % of the cortex); 2, moderate (25 – 50 % of the cortex); 3, severe (>50 % of the cortex). The lesions were assessed in at least 30 random and non-overlapping fields in the renal cortex.
Morphometric evaluation of the glomerular volume was made in the same kidney sections that were examined for morphological changes, using the method validated by Lane et al. 47 and employed in our recent studies 11,12,48, using Nikon NIS-Elements AR 3.1 morphometric programme (Nikon, Tokyo, Japan).
Based on our previous experience 42,43, the ratio of left ventricle weight (LVW) to tibial length (TL), LVW/TL, was employed to determine the degree of cardiac hypertrophy.
Statistical analysis
Statistical analysis of the data was performed using Graph-Pad Prism software (Graph Pad Software, San Diego, California, USA). ANOVA for repeated measurements, followed by Student-Newman-Keuls test, was performed for analysis of BP changes within the groups. Statistical comparison of other results was made by Student’s t-test or one-way ANOVA. Unless noted, values are expressed as mean ± S.E.M. and n represents the number of animals. A p value less than 0.05 was considered statistically significant. For clarity of presentation, statistical evaluation of only two comparisons are marked in figures: first, against the values in sham-operated HanSD rats (the main control group) and, second, the values in 5/6 NX in TGR (the model of CKD) against those in sham-operated TGR
DISCUSSION
This study evaluated the effectiveness of chronic EET activity, achieved by blockade of soluble epoxygenase hydrolase using sEHi, on the progression of CKD induced by 5/6 NX in TGR rats, a unique monogenetic model of RAS-dependent hypertension. This was compared with the effectiveness of a thorough two-level RAS blockade which is currently accepted as a golden standard therapy used to retard the progression of CKD to ESRD 8,11,12,14–17,38.
The first important finding was that the 5/6 NX applied in TGR not only increased circulating and kidney ANG II concentrations, as reported in our recent study 12, but elicited a profound decrease in the intrarenal availability of biologically active epoxygenase metabolites, as evidenced by the decrease in the EETs/DHETEs ratio in the early as well as late phase after 5/6 NX. Since the renal generation of EETs is in TGR after 5/6 NX apparently in normal range, as indicated by unaltered protein expression of the CYP2C23 enzyme, the reduced intrarenal availability of biologically active epoxygenase metabolites is likely a result of increased conversion of EETs to DHETEs, as indicated by distinctly increased renal protein expression of sEH in 5/6 NX TGR. Furthermore, our data show that intrarenal formation of 20-HETE was unaltered in 5/6 NX TGR compared with sham-operated HanSD rats as well as with sham-operated TGR. This finding is of special importance, because it is now well recognized that abnormalities in CYP hydroxylase pathway play an important role in the pathophysiology of hypertension and hypertension-associated end-organ damage in various experimental models 49,50. In addition, sEH inhibition with c-AUCB when applied in TGR subjected to 5/6 NX substantially improved the rats’ survival rate, prevented the BP increase, retarded the progression of cardiac hypertrophy, reduced proteinuria and the degree of glomerular and tubulointerstitial injury, prevented decreases in clearance of endogenous creatinine and reduced the glomerular volume. All these organ-protective actions were associated with normalization of the intrarenal EETs/DHETEs ratio to levels observed in sham-operated HanSD rats but no significant alteration of increased intrarenal ANG II. Remarkably, our finding that the dose of c-AUCB applied substantially increased tissue concentrations of EETs without altering intrarenal ANG II levels in the remnant kidney indicates that all beneficial effects of long-term treatment with sEHi in 5/6 NX TGR should be ascribed to increased intrarenal EETs bioavailability.
Taken together, the findings support the notion that the deficiency of the intrarenal availability of biologically active epoxygenase metabolites contributes to the progression of CKD and development of ESRD in 5/6 NX TGR. This view is in accordance with previous studies reporting that net intrarenal deficiency of EETs contributes to the pathophysiology of certain forms of ANG II-dependent hypertension 22,24–32. It is particularly noteworthy that c-AUCB treatment at a dose that distinctly increased intrarenal EETs/DHETEs ratio but did not alter the elevated circulating and renal RAS activity was still able to attenuate the development of ANG II-dependent malignant hypertension and of hypertension-induced end-organ damage 29,31,32.
Nevertheless, it is important to note that in a recent study with 5/6 NX mice by Jung et al. 34 demonstrated that long-term c-AUCB treatment at almost identical dosage did not prevent the progression of CKD (no effect on SBP, no improvement of the survival rate, and no attenuation of renal glomerular and tubulointerstitial injury) and tended to accelerate rather than retard (vide augmented albuminuria) the course of CKD. There is no satisfactory explanation of these results which contradict our present and earlier findings showing beneficial effects of sEHi treatment on the progression of end-organ damage 25,26,29,31. However, it should be noticed that in the aforementioned study the 5/6 NX mice exhibited suppression of sEH expression and elevation of EETs levels 34, just the opposite to findings in ANG II-dependent hypertension models in rats, where increased expression and activity of sEH with consequent reduction of biologically active EETs were found 29,31,51,52. Apparently, blockade of sEH is antihypertensive and renoprotective only under conditions of increased sEH activity and reduced EETs bioavailability 22–24. The reasons for the suppression of sEH expression in 5/6 NX mice remain unclear; a species difference between rats and mice possibly involving different regulation of sEH expression/activity should be considered
What were the mechanisms underlying renoprotective actions of sEHi treatment in 5/6 NX TGR? It will be recalled that the first theory explaining the mechanism of the progression of CKD, truly a milestone in nephrologic research, was formulated by Brenner 2 On the basis of micropuncture studies with remnant kidneys of 5/6 NX rats 5 he proposed that glomerular hyperfiltration and hypertension represented a compensatory response to a reduction of nephron number, which, however, results in a damage of the healthy remnant glomeruli. The compensation is in fact maladaptive, and within the vicious circle glomerulosclerosis progresses, leading ultimately to ESRD. According to this “hemodynamic” theory, all renoprotective measures applied in CKD should focus on the correction of abnormal glomerular hemodynamics 2,4,5. However, subsequent studies employing serial micropuncture technique in remnant kidneys of 5/6 rats revealed that, on the one hand, hemodynamic abnormalities which developed in the remnant glomeruli had no correlation to the degree of sclerosis subsequently developing in the same glomerulus 53,54, on the other hand, an unequivocal correlation between glomerular hypertrophy and glomerulosclerosis was found 55,56. Based on those studies, it had to be recognized that glomerular hypertrophy is an additional independent risk factor for the development of glomerulosclerosis, which in accordance with the “Laplace law” (tension = radius x pressure), leads to an increase in wall tension and glomerular capillary damage, but also to podocyte injury and depletion, the latter also identified as one of major causes of glomerulosclerosis 7,55–57. Considering this “hypertrophy” theory, of particular interest is our finding that sEHi treatment significantly reduced the glomerular volume in 5/6 NX TGR.
When our present findings are considered in the context of the earlier studies and theories, we suggest that the mechanism underlying renoprotective effects of long-term sEHi treatment in 5/6 NX TGR is related to attenuation of maladaptive compensatory glomerular growth, which in these animals is mediated through anti-proliferative effects of normalized intrarenal EETs levels. Nevertheless, it is known that renal fibrosis is an important factor in the progression of CKD 7,58 and it has been documented that increased renal expression of fibronectin and collagen is a characteristic feature of 5/6 NX rats. 59 Therefore, the lack of measurement of expression of these factors is an obvious limitation of our present study. Another limitation becomes apparent with the current evidence that oxidative stress is an important contributor to pathogenesis of renal fibrosis 60. Since TGR, an ANG II-dependent model of hypertension, exhibits increased generation of superoxide (O2−) 61, the role of oxidative stress in the progression of CKD in this model should also be considered and investigated. These two limitations inevitably narrow our insight into the complex mechanisms responsible for the renoprotective actions of sEHi treatment in 5/6 NX TGR.
Another important finding of the present study is that in 5/6 NX TGR antihypertensive regime based on combined RAS blockade dramatically improved survival rate, and normalized BP, cardiac hypertrophy and proteinuria, moreover, the treatment prevented the development of renal glomerular and tubulointerstitial injury and decreases in clearance of endogenous creatinine. Furthermore, combined RAS blockade not only prevented the rise in kidney ANG II concentration but even decreased it to levels observed in sham-operated HanSD rats. All these findings are in good agreement with our recent study showing that hypertension and increased intrarenal RAS are two critical determinants of the rate of progression of CKD in 5/6 NX TGR 12 and with studies suggesting the crucial role of intrarenal RAS in the pathophysiology of hypertension-associated end-organ damage 39,42–44. Nevertheless, our present results indicate that effectiveness of renoprotective action of RAS blockade is limited during the late stage of CKD. Even though hypertension and intrarenal RAS activity were effectively controlled, some 5/6 NX TGR under RAS blockade began to die at week 18 (two out of 17 animals), which was was preceded by a transient exacerbation of proteinuria. Taken together, our current findings further support the notion that even if antihypertensive regime based on RAS blockade is a key component of the treatment strategy aimed at slowing-down the progression of CKD 8,11,12,14–17,36–38, there is a need to target vasoactive systems other than RAS.
In view of our current encouraging findings indicating renoprotective effects of normalization of intrarenal EETs bioavailability on the progression of CKD, it seems logical and desirable to investigate whether the combined sEH inhibition and RAS blockade might have additive beneficial effects in this model of CKD. However, it this regard it is important to emphasize that renoprotective action of RAS blockade was much less successful in the late phase of CKD 18–20 and, in agreement with the present results, we found previously that in TGR the two-level RAS inhibition provided complete renoprotection when applied no later than 16 weeks after 5/6 NX 11,12. Therefore, it is reasonable to assume that potentially superior renoprotection of combined sEH inhibition and RAS blockade can possibly be demonstrated in the very long-term studies only. Therefore, a relevant research project would require a follow-up period substantially longer than is usually employed in studies with 5/6 NX rats 11,12,37.
It will also be noticed that we demonstrated recently that in HanSD rats, originally normotensive and with normal plasma and kidney ANG II levels, 5/6 NX led to the development of hypertension and marked activation of intrarenal RAS in the remnant kidney, and these factors were dominant determinants of the rate of progression of CKD. 12 Therefore one could reasonable assume that 5/6 NX HanSD rats would also exhibit a decreased EETs availability in the remnant kidney and that sEH inhibition could also exhibit renoprotective actions and retard the progression of CKD in initially normotensive HanSD rats subjected to renal mass reduction. However, this study was designed to address first the role of intrarenal biologically active epoxygenase metabolites in the progression of CKD in hypertensive animals with already augmented RAS activity; the reason was that, previous studies 22–24,27–32 provided a good rationale for the use of sEH inhibition as the new therapeutic strategy to slow the progression of CKD in ANG II-dependent hypertensive model. Nevertheless, the present findings expose the need to establish if renoprotective effects of long-term treatment with sEH inhibitor would also be demonstrable in 5/6 NX animals with originally normal blood pressure and without inappropriate activation of RAS. This would make a desirable target of a future, hopefully more conclusive study.
In conclusion, the results of the present study show that, first, hypertensive TGR subjected to 5/6 renal mass reduction exhibit a profound decrease in the intrarenal EETs/DHETEs ratio, which strongly suggests that the deficiency of intrarenal active epoxygenase metabolites accelerates the progression of CKD in this ANG II-dependent hypertensive model. Second, long-term restoration of intrarenal biologically active EETs, achieved by pharmacologic sEH inhibition, provided important renoprotective effect. The finding that normalization of intrarenal availability of active epoxygenase products substantially attenuates the progression of CKD in 5/6 NX TGR should be considered in attempts to develop new pharmacologic strategies aimed at slowing-down the progression of CKD to ESRD.
Acknowledgments
This study was supported by grant No. NT/14012-3 awarded by the Internal Grant Agency of the Ministry of Health of the Czech Republic to L.Č. Z.H. is supported by a grant of the Ministry of Health within the project for the development of research organization 00023001 (IKEM) – institutional support. The Center for Experimental Medicine (IKEM) received financial support from the European Commission within the Operational Program Prague–Competitiveness; project “CEVKOON” (#CZ.2.16/3.1.00/22126). L.Č. was a recipient of grant No. MŠMT-Kontakt LH 11116 from the Ministry of Education, Youth and Sports for the support of the international research cooperation and it supported the cooperation with K.K. and A.N. from Department of Pharmacology, Kagawa University, Kagawa, Japan. J.D.I. is supported by grant from NIHDK38226. S.H.H. was supported in part by NIEHS grant ES02710, NIEHS Superfund grant P42 ES04699, NIHLB grant HL059699 and the CounterACT Program, National Institutes of Health Office of the Director, and the National Institute of Neurological Disorders and Stroke, Grant Number U54 NS079202 awarded to B.D.H. B.D.H. is a George and Judy Marcus Senior Fellow of the American Asthma Foundation.
References
- 1.U.S. Renal Data System: USEDS. 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2012. [Google Scholar]
- 2.Brenner BM. Nephron adaptation to renal injury or ablation. Am J Physiol. 1985;249:F324–F337. doi: 10.1152/ajprenal.1985.249.3.F324. [DOI] [PubMed] [Google Scholar]
- 3.Zoja C, Abbate M, Remuzzi G. Progression of chronic kidney disease: insight from animal models. Curr Opin Nephrol Hypertens. 2006;15:250–257. doi: 10.1097/01.mnh.0000222691.53970.83. [DOI] [PubMed] [Google Scholar]
- 4.Hostetter TH. Hyperfiltration and glomerulosclerosis. Semin Nephrol. 2003;23:194–199. doi: 10.1053/anep.2003.50017. [DOI] [PubMed] [Google Scholar]
- 5.Hostetter TH, Olson JL, Rennke HG, Ventatachalam MA, Brenner BM. Hyperfiltration in remnant nephrons: a potentially adverse response to ablation. Am J Physiol. 1981;241:F85–F93. doi: 10.1152/ajprenal.1981.241.1.F85. [DOI] [PubMed] [Google Scholar]
- 6.Shimamura T, Morrison AB. A progressive glomerulosclerosis occurring in partial five–sixths nephrectomized rats. Am J Pathol. 1975;79:95–106. [PMC free article] [PubMed] [Google Scholar]
- 7.Kriz W. Podocyte is the major culprit accounting for the progression of chronic renal disease. Micros Res Tech. 2002;57:189–195. doi: 10.1002/jemt.10072. [DOI] [PubMed] [Google Scholar]
- 8.Macconi D. Targeting the renin angiotensin system for remission/regression of chronic kidney disease. Histol Histopathol. 2010;25:655–668. doi: 10.14670/HH-25.655. [DOI] [PubMed] [Google Scholar]
- 9.Kohan DE. Endothelin, hypertension and chronic kidney disease: new insight. Curr Opin Nephrol Hypertens. 2010;19:134–139. doi: 10.1097/MNH.0b013e328335f91f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briet M, Burns KD. Chronic kidney disease and vascular remodeling: molecular mechanisms and clinical implications. Clin Sci. 2012;123:399–416. doi: 10.1042/CS20120074. [DOI] [PubMed] [Google Scholar]
- 11.Vaněčková I, Kujal P, Husková Z, et al. Effects of combined endothelin A receptor and renin-angiotensin system blockade on the course of end-organ damage in 5/6 nephrectomized Ren-2 hypertensive rats. Kidney Blood Press Res. 2012;35:382–392. doi: 10.1159/000336823. [DOI] [PubMed] [Google Scholar]
- 12.Kujal P, Certíková Chábová V, Vernerova Z, et al. Similar renoprotection after renin-angiotensin-dependent and -independent antihypertensive therapy in 5/6-nephrectomized Ren-2 transgenic rats: are there blood pressure-independent effects? Clin Exp Pharmacol Physiol. 2010;37:1159–1169. doi: 10.1111/j.1440-1681.2010.05453.x. [DOI] [PubMed] [Google Scholar]
- 13.Bidani AK, Polichnowski AJ, Loutzenhiser R, Griffin KA. Renal microvascular dysfunction, hypertension and CKD progression. Curr Opin Nephrol Hypertens. 2013;22:1–9. doi: 10.1097/MNH.0b013e32835b36c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ptinopolou AG, Pikilidou MI, Lasaridis N. The effect of antihypertensive drugs on chronic kidney disease: a comprehensive review. Hypertens Res. 2013;36:91–101. doi: 10.1038/hr.2012.157. [DOI] [PubMed] [Google Scholar]
- 15.Turner JM, Bauer C, Abramowitz MK, Melamed ML, Hostetter TH. Treatment of chronic kidney disease. Kidney Int. 2012;81:351–362. doi: 10.1038/ki.2011.380. [DOI] [PubMed] [Google Scholar]
- 16.Rüster C, Wolf G. Renin-angiotensin-aldosterone system and progression of renal disease. J Am Soc Nephrol. 2006;17:2985–2991. doi: 10.1681/ASN.2006040356. [DOI] [PubMed] [Google Scholar]
- 17.Berl T. Renal protection by inhibition of the renin-angiotensin-aldosterone system. J Renin Angiotensin Aldosterone Syst. 2009;10:1–8. doi: 10.1177/1470320309102747. [DOI] [PubMed] [Google Scholar]
- 18.Perico N, Amuchastegui SC, Colosio V, Sonzogni G, Bertani T, Remuzzi G. Evidence that an angiotensin-converting enzyme inhibitor has a different effect on glomerular injury according to the different phase of the disease at which the treatment is started. J Am Soc Nephrol. 1994;5:1139–1146. doi: 10.1681/ASN.V541139. [DOI] [PubMed] [Google Scholar]
- 19.Gordon J, Kopp JB. Off the beaten renin-angiotensin-aldosterone system pathway: new perspectives on antiproteinuric therapy. Adv Chronic Kidney Dis. 2011;18:300–311. doi: 10.1053/j.ackd.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lattanzio MR, Weir MR. Does blockade of the renin-angiotensin-aldosterone system slow progression of all forms of kidney disease? Curr Hypertens Rep. 2010;12:369–377. doi: 10.1007/s11906-010-0142-2. [DOI] [PubMed] [Google Scholar]
- 21.Campbell WB, Fleming I. Epoxyeicosatrienoic acids and endothelium-dependent response. Pfugers Arch. 2010;459:881–895. doi: 10.1007/s00424-010-0804-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Imig JD. Epoxides and soluble epoxide hydrolase in cardiovascular physiology. Physiol Rev. 2012;92:101–130. doi: 10.1152/physrev.00021.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Capdevilla J, Wang W. Role of cytochrome P450 epoxygenase in regulating renal membrane transport and hypertension. Curr Opin Nephrol Hypertens. 2013;22:163–169. doi: 10.1097/MNH.0b013e32835d911e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elmarakby AA. Reno-protective mechanisms of epoxyeicosatrienoic acids in cardiovascular disease. Am J Physiol. 2012;302:R321–R330. doi: 10.1152/ajpregu.00606.2011. [DOI] [PubMed] [Google Scholar]
- 25.Li J, Carroll MA, Chander PN, Falck JR, Sangras B, Stier CT. Soluble epoxide hydrolase inhibitor, AUDA, prevents early salt-sensitive hypertension. Front Biosci. 2008;13:3480–3487. doi: 10.2741/2942. [DOI] [PubMed] [Google Scholar]
- 26.Huang H, Morisseau C, Wang JF, et al. Increasing or stabilizing renal epoxyeicosatrienoic acid production attenuates abnormal renal function and hypertension in obese rats. Am J Physiol. 2007;293:F342–F349. doi: 10.1152/ajprenal.00004.2007. [DOI] [PubMed] [Google Scholar]
- 27.Sporková A, Kopkan L, Varcabová A, et al. Role of cytochrome P450 metabolites in the regulation of renal function and blood pressure in 2-kidney, 1-clip hypertensive rats. Am J Physiol. 2011;300:R1468–R1475. doi: 10.1152/ajpregu.00215.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neckář J, Kopkan L, Husková Z, et al. Inhibition of soluble epoxide hydrolase by cis-4-[4-(3-adamantan-I-ylureido)cyclohexyl-oxy]benzoic acid exhibits antihypertensive and cardioprotective actions in transgenic rats with angiotensin II-dependent hypertension. Clin Sci. 2012;122:513–525. doi: 10.1042/CS20110622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Honetschlägerová Z, Husková Z, Vaňourková Z, et al. Renal mechanisms contributing to the antihypertensive action of soluble epoxide hydrolase inhibition in Ren-2 transgenic rats with inducible hypertension. J Physiol. 2011;589:207–219. doi: 10.1113/jphysiol.2010.199505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kopkan L, Husková Z, Sporková A, et al. Soluble epoxide hydrolase inhibition exhibits antihypertensive actions independently of nitric oxide in mice with renovascular hypertension. Kidney Blood Press Res. 2012;35:595–607. doi: 10.1159/000339883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Honetschlägerová Z, Sporková A, Kopkan L, et al. Inhibition of soluble epoxide hydrolase improves the impaired pressure-natriuresis relationship and attenuates the development of hypertension and hypertension-associated end-organ damage in Cyp1a1-Ren-2 transgenic rats. J Hypertens. 2011;29:1590–1601. doi: 10.1097/HJH.0b013e328349062f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Honetschlägerová Z, Kitada K, Husková Z, et al. Antihypertensive and renoprotective actions of soluble epoxide hydrolase inhibition in ANG II-dependent malignant hypertension are abolished by pretreatment with L-NAME. J Hypertens. 2013;31:321–332. doi: 10.1097/HJH.0b013e32835b50aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao G, Tu L, Li X, et al. Delivery of AAV2-CYP2J2 protects remnant kidney in the 5/6-nephrectomized rat via inhibition of apoptosis and fibrosis. Hum Gene Ther. 2012;23:688–699. doi: 10.1089/hum.2011.135. [DOI] [PubMed] [Google Scholar]
- 34.Jung O, Jansen F, Mieth A, et al. Inhibition of the soluble epoxide hydrolase promotes albuminuria in mice with progressive renal disease. PloS One. 2010;5:e11979. doi: 10.1371/journal.pone.0011979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mullins JJ, Peters J, Ganten D. Fulminant hypertension in transgenic rats harbouring the mouse Ren-2 gene. Nature. 1990;344:541–544. doi: 10.1038/344541a0. [DOI] [PubMed] [Google Scholar]
- 36.Cao Z, Bonnet F, Davis B, Allen TJ, Cooper ME. Additive and anti-albuminuric effects of angiotensin-converting enzyme inhibition and angiotensin receptor antagonism in diabetic spontaneously hypertensive rats. Clin Sci. 2001;100:591–599. [PubMed] [Google Scholar]
- 37.Fujihara CK, Velho M, Malheiros DM, Zatz R. An extremely high dose of losartan affords superior renoprotection in the remnant model. Kidney Int. 2005;67:1913–1924. doi: 10.1111/j.1523-1755.2005.00290.x. [DOI] [PubMed] [Google Scholar]
- 38.Ripley E. Complementary effects of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in slowing the progression of chronic kidney disease. Am Heart J. 2009;157:S7–S16. doi: 10.1016/j.ahj.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 39.Kobori H, Nangaku M, Navar LG, Nishiyama A. The intrarenal renin-angiotensin system: from physiology to the pathobiology of hypertension and kidney disease. Pharmacol Rev. 2007;59:251–287. doi: 10.1124/pr.59.3.3. [DOI] [PubMed] [Google Scholar]
- 40.Huskova Z, Kramer HJ, Thumova M, et al. Effects of anesthesia on plasma and kidney ANG II levels in normotensive and ANG II-dependent hypertensive rats. Kidney Blood Press Res. 2006;29:74–83. doi: 10.1159/000092981. [DOI] [PubMed] [Google Scholar]
- 41.Husková Z, Kramer HJ, Vaňourková Z, Červenka L. Effects of changes in sodium balance on plasma and kidney angiotensin II levels in anesthetized and conscious Ren-2 transgenic rats. J Hypertens. 2006;24:517–527. doi: 10.1097/01.hjh.0000209988.51606.c7. [DOI] [PubMed] [Google Scholar]
- 42.Husková Z, Vaňourková Z, Erbanová M, et al. Inappropriately high circulating and intrarenal angiotensin II levels during dietary salt loading exacerbate hypertension in Cyp1a1-Ren-2 transgenic rats. J Hypertens. 2010;28:495–509. doi: 10.1097/HJH.0b013e3283345d69. [DOI] [PubMed] [Google Scholar]
- 43.Vaňourková Z, Kramer HJ, Husková Z, et al. AT1 receptor blockade is superior to conventional triple therapy in protecting against end-organ damage Cyp1a1-Ren-2 transgenic rats with inducible hypertension. J Hypertens. 2006;24:2465–2472. doi: 10.1097/01.hjh.0000251909.00923.22. [DOI] [PubMed] [Google Scholar]
- 44.Červenka L, Vaněčková I, Husková Z, et al. Pivotal role of AT1A receptors in the development of two-kidney, one-clip hypertension: study in AT1A receptor knockout mice. J Hypertens. 2008;26:1379–1389. doi: 10.1097/HJH.0b013e3282fe6eaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Varcabova S, Huskova Z, Kramer HJ, et al. Antihypertensive action of soluble epoxide hydrolase inhibition in Ren-2 transgenic rats is mediated by suppression of the intrarenal renin-angiotensin system. Clin Exp Pharmacol Physiol. 2013;40:273–281. doi: 10.1111/1440-1681.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kurtz TW, Griffin KA, Bidani AK, Davisson RL, Hall JE. Recommendations for blood pressure measurements in humans and experimental animals. Part 2: Blood pressure measurements in experimental animals. Hypertension. 2005;45:299–310. doi: 10.1161/01.HYP.0000150857.39919.cb. [DOI] [PubMed] [Google Scholar]
- 47.Nakano Y, Hirano T, Uehara K, et al. New rat model induced by anti-glomerular basement membrane antibody shows severe glomerular adhesion in early stage and quickly progress to end-stage renal failure. Pathol Int. 2008;58:361–370. doi: 10.1111/j.1440-1827.2008.02237.x. [DOI] [PubMed] [Google Scholar]
- 48.Lane PH, Steffes MW, Mauer MS. Estimation of glomerular volume: a comparison of four methods. Kidney Int. 1992;41:1085–1089. doi: 10.1038/ki.1992.165. [DOI] [PubMed] [Google Scholar]
- 49.Čertíková Chábová V, Walkowska A, Kompanowska-Jezierska E, et al. Combined inhibition of 20-hydroxyeicosatetraenoic acid formation and epoxyeicosatrienoic acids degradation attenuates hypertension and hypertension-induced end-organ damage in Ren-2 transgenic rats. Clin Sci. 2010;118:617–632. doi: 10.1042/CS20090459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams JM, Murphy S, Burke M, Roman RJ. 20-hydroxyeicosatetraenoic acid: a new target for the treatment of hypertension. J Cardiovasc Pharmacol. 2010;56:336–344. doi: 10.1097/FJC.0b013e3181f04b1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ai D, Fu Y, Guo D, et al. Angiotensin II up-regulates soluble epoxide hydrolase in vascular endothelium in vitro and in vivo. Proc Natl Acad Sci. 2007;104:9018–9023. doi: 10.1073/pnas.0703229104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ai D, Shyy JYY, Zhu Y. Linking an insect enzyme to hypertension: angiotensin II-epoxide hydrolase interactions. Kidney Int. 2010;77:88–92. doi: 10.1038/ki.2009.349. [DOI] [PubMed] [Google Scholar]
- 53.Yoshida Y, Fogo A, Shiraga H, Glick AD, Ichikawa I. Serial micropuncture analysis of single nephron function in subtotal renal ablation. Kidney Int. 1988;33:855–867. doi: 10.1038/ki.1988.77. [DOI] [PubMed] [Google Scholar]
- 54.Fogo A, Yoshida Y, Glick AD, Homma T, Ichikawa I. Serial micropuncture analysis of glomerular function in two rat models of glomerular sclerosis. J Clin Invest. 1988;82:322–330. doi: 10.1172/JCI113590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yoshida Y, Fogo A, Ichikawa I. Glomerular hemodynamic changes vs. Hypertrophy in experimental glomerular sclerosis. Kidney Int. 1989;35:654–660. doi: 10.1038/ki.1989.35. [DOI] [PubMed] [Google Scholar]
- 56.Yoshida Y, Kawamura T, Ikoma M, Fogo A, Ichikawa I. Effects of antihypertensive drugs on glomerular morphology. Kidney Int. 1989;36:626–635. doi: 10.1038/ki.1989.239. [DOI] [PubMed] [Google Scholar]
- 57.Fukuda A, Wickman LT, Vekatareddy MP, et al. Angiotensin II-dependent persistent podocyte loss from destabilized glomeruli causes progression of end-stage kidney disease. Kidney Int. 2012;81:40–55. doi: 10.1038/ki.2011.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Guarino M, Tosoni A, Nebuloni M. Direct contribution of epithelium to organ fibrosis: epithelial-mesenchymal transition. Hum Pathol. 2009;40:1365–1376. doi: 10.1016/j.humpath.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 59.Ni H, Chen J, Pan M, et al. FTY720 prevents progression of renal fibrosis by inhibiting renal microvasculature endothelial dysfunction in a rat model of chronic kidney disease. J Mol Hist. 2013 doi: 10.1007/s10735-013-9521-8. in press. [DOI] [PubMed] [Google Scholar]
- 60.Barnes JL, Gorin Y. Myofibroblast differention during fibrosis: role of NAD(P)H oxidases. Kidney Int. 2011;79:944–956. doi: 10.1038/ki.2010.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kopkan L, Husková Z, Vaňourková Z, et al. Reduction of oxidative stress does not attenuate the development of angiotensin II-dependent hypertension in Ren-2 transgenic rats. Vasc Pharmacol. 2009;51:175–181. doi: 10.1016/j.vph.2009.06.001. [DOI] [PubMed] [Google Scholar]