Abstract
Objectives
We sought to determine if and to what extent a woman’s exposure to stressful life events prior to conception (PSLEs) were associated with subsequent infant birth weight by using a nationally representative sample of US women.
Methods
We examined 9350 mothers and infants participating in the first wave of the Early Childhood Longitudinal Study-Birth Cohort in 2001. Weighted regressions estimated the effect of exposure on very low and low birth weight, adjusting for maternal sociodemographic and health factors and stress during pregnancy.
Results
Twenty percent of women experienced any PSLE. In adjusted analyses, exposed women were 38% more likely to have a very low birth weight infant than nonexposed women. Furthermore, the accumulation of PSLEs was associated with reduced infant birth weight.
Conclusions
This was the first nationally representative study to our knowledge to investigate the impact of PSLEs on very low and low birth weight in the United States. Interventions aimed to improve birth outcomes will need to shift the clinical practice paradigm upstream to the preconception period to reduce women’s exposure to stress over the life course and improve the long-term health of children.
Disorders related to very low birth weight and low birth weight (LBW) are the leading cause of all neonatal deaths in the United States1 and contribute substantially to childhood and adult morbidity and mortality.2–5 Reducing the prevalence of very LBW and LBW, which occurs in approximately 8.2% of births in the United States,6 has significant implications for the future health and well-being of children and families, and is a national health priority.7 However, despite extensive research, practice, and public health efforts devoted to reducing the number of children born with LBW, the prevalence of very LBW and LBW in the United States remains unacceptably high, suggesting that additional risk factors must be identified to improve outcomes.
Maternal exposure to stress during pregnancy is an important contributor to LBW.8–14 Furthermore, Danish population-based evidence suggests that exposure to stressors before pregnancy (i.e., severe life events, such as death or serious health problems of a relative) may also be associated with reduced infant birth weight.15 This finding empirically supports theoretical literature that suggests that the accumulation of stress across the life course results in increased allostatic load or “weathering,” leading to a decline in reproductive health.16,17 Other studies have linked affective states (e.g., depression), which has been hypothesized to be the result of acute or chronic stress,18 during pregnancy to reduced fetal growth and birth weight.19 Moreover, poor preconception mental health has been associated with an increased risk of LBW among a nationally representative cohort of US women and their babies.20 However, to our knowledge, no study has investigated stressful life events prior to conception (PSLEs) as possible predictors of birth weight in a national sample of women living in the United States.
Therefore, we used population-based data available from the Early Childhood Longitudinal Study, Birth Cohort (ECLS-B) to determine if and to what extent a woman’s exposure to PSLEs were associated with having a very LBW or LBW infant. Findings from this study will provide critical information about preconception predictors of birth weight and have significant implications for approaches to preconception, interconception, and primary care. Understanding these pathways might also shift the focus of clinical practice earlier in the life course and inform upstream interventions to improve birth outcomes.
METHODS
Data were from the first wave of ECLS-B, a nationally representative cohort of children born in 2001 and their parents. The ECLS-B used a clustered, list-frame design to select a probability sample of the approximately 4 million children born in 2001, with oversampling of children from minority groups, twins, and children born very LBW and LBW.21 Children born to mothers younger than 15 years, those who were adopted after the birth certificate was issued, and those who did not survive until 9 months of age were excluded from the sampling frame.22 Registered births were sampled within primary sampling units (counties or groups of contiguous counties) from the National Center for Health Statistics vital statistics system. The ECLS-B sampled more than 14 000 births and contacted their parents. The final study cohort consisted of participants who completed the first interview, when the children were approximately 9 months of age (n = 10 700). We obtained restricted data with permission and approval from the Institute for Education Sciences Data Security Office of the US Department of Education, National Center for Education Statistics. In accordance with National Center for Education Statistics guidelines, all reported un-weighted sample sizes were rounded to the nearest 50.21
Participants were eligible for this study if the main survey respondent was the infant’s biological mother (n = 10 550); 450 records missing birth certificate data were subsequently excluded. ECLS-B included individual records for each child within twin pairs identified through oversampling; for this analysis, we randomly selected 1 twin from each pair to retain in the sample. For other multiples in the sample (i.e., not explicitly recruited as part of the oversampling), only 1 infant from the household was surveyed. Our final sample contained 9350 mother–child dyads.
Measures
The first wave of the study occurred when the child was approximately 9 months old. Data were collected from the infant’s birth certificate, computer-assisted personal interviews, and parental self-administered questionnaires.
Birth weight
The infant’s birth weight in grams was derived from the birth certificate and categorized as very low (very LBW; < 1500 g), low (LBW; 1500–2499 g), normal (2500–3999 g), or high (≥ 4000 g).
Stressful life events prior to conception
We derived the date of conception using information from the birth certificate on the length of gestation and the infant’s date of birth. Women were coded as having experienced a PSLE if they indicated that 1 or more of the following events occurred prior to conception:
death of the respondent’s mother,
death of the respondent’s father,
death of a previous live born child,
divorce,
separation from partner,
death of a spouse, or
fertility problems.
All of these experiences were considered stressful life events in previous research.23–26 Death of a previous live born child was collected from the birth certificate and was assumed to have occurred prior to conception. To examine this assumption, we tested alternate specifications of our PSLE measure, with death of a child removed and with death of a child included as a pregnancy event. These modifications did not substantially change our findings; therefore, we presented the results from the model, including death of a child as a PSLE.
Prenatal health and stress
Birth certificate data determined if women had experienced any of the following pregnancy complications: anemia, diabetes, (oligo) hydramnios, hypertension during pregnancy, eclampsia, incompetent cervix, Rh sensitization or uterine bleeding, premature rupture of membranes, placental abruption, or placenta previa (birth certificate data were from the 1989 revision of the US Standard Certificate of Live Birth [see http://www.cdc.gov/nchs/data/techap99.pdf]). Data from the birth certificate also identified whether women had previously given birth to a preterm or small-for-gestational age (SGA) infant and women with chronic conditions, including cardiac disease, lung disease, genital herpes, hemoglobinopathy, chronic hypertension, renal disease, or other medical risk factors. Prepregnancy body mass index (BMI, defined as weight in kilograms divided by the square of height in meters) was calculated from the respondent’s measured height and self-reported weight prior to pregnancy (< 18.5 kg/m2 [underweight]; 18.5–24.9 kg/m2 [normal]; 25–29.9 kg/m2 [overweight]; ≥ 30 kg/m2 [obese]; and unknown).7 In addition, we evaluated the following: the timing of the initiation of prenatal care (in the first trimester, in the second or third trimester, or did not receive prenatal care), plurality (whether the index child was a singleton or multiple birth), and parity (data from the birth certificate, coded as number of prior live births: nulliparous, primiparous, or multiparous). Finally, women were coded as having experienced a stressful life event during pregnancy if they indicated that 1 or more of the following events occurred during their pregnancy:
death of the respondent’s mother,
death of the respondent’s father,
divorce,
separation from partner, or
death of a spouse.
Maternal sociodemographic factors
We examined the following maternal sociodemographic factors: race/ethnicity (White [non-Hispanic], Black [non-Hispanic]; Asian/Pacific Islander [non-Hispanic], Hispanic, or other race [non-Hispanic]); age (15–19, 20–24, 25–29, 30–34, or ≥ 35 years), marital status at the infant’s birth (married or living with partner, separated, divorced, widowed, or never married), health insurance coverage during pregnancy (no health insurance, any publicly funded insurance, or private health insurance coverage only), US region of residence (Northeast, Midwest, South, or West),27 and socioeconomic status. Socioeconomic status was defined using a 5-category composite index (quintiles) generated by the National Center for Education Statistics that incorporated
father’s or male guardian’s education,
mother’s or female guardian’s education,
father’s or male guardian’s occupation,
mother’s or female guardian’s occupation, and
household income.21
Statistical Analyses
Analyses were conducted using survey procedures from SAS version 9.2 (SAS Institute, Cary, NC). The standard errors were corrected for clustering within strata and the primary sampling unit, and survey weights were applied to produce estimates accounting for the complex survey design, unequal probabilities of selection, and survey nonresponse.
Summary statistics were generated to describe sample characteristics; the χ2 test was used to determine significant differences in sociodemographic characteristics between women who did and did not experience any PSLE and by infant birth weight status.
Staged multivariable logistic regression models examined the impact of maternal exposure to PSLEs on the infant’s birth weight status. Model 1 adjusted for exposure to any stressful life event during pregnancy, having a previous preterm or SGA baby, maternal chronic conditions, prepregnancy BMI, initiation of prenatal care, plurality, parity, maternal race/ethnicity, maternal age, marital status at birth, health insurance coverage, region of residence, and socioeconomic status. Model 2 included pregnancy complications. Adjusted odds ratios (AORs) and 95% confidence intervals (CIs) comparing birth weight statuses of infants born to women exposed and not exposed to PSLEs were estimated from these multivariable models. In addition, the models were tested removing multiples from the sample; because this did not influence our findings, results from the full sample were presented. The results presented compared very LBW and LBW to normal birth weight; the results for high birth weight are available as a supplement to the online version of this article at http://www.ajph.org.
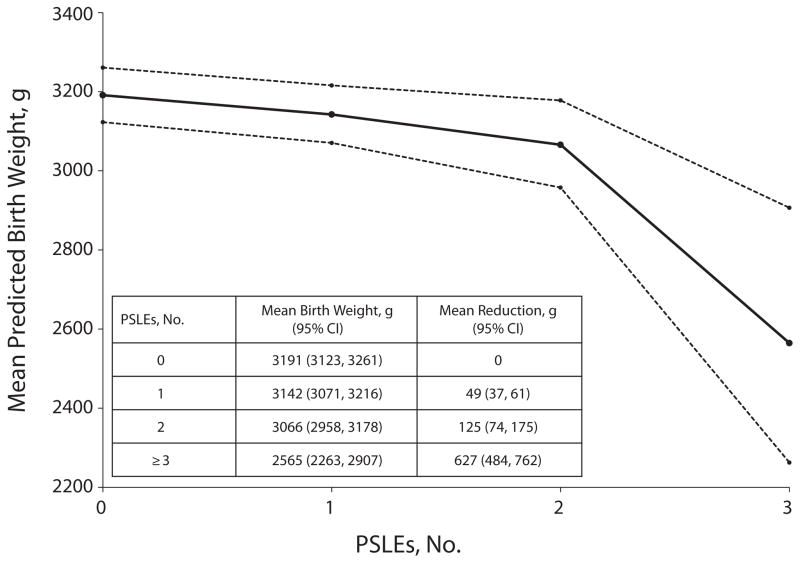
To evaluate the cumulative effect of PSLEs and quantify the magnitude of the change in birth weight associated with PSLEs, we also used weighted, multivariable generalized linear regression to evaluate the association between continuous birth weight (natural log transformed) and the count of PSLEs, adjusting for the previously mentioned covariates. Mothers delivering high birth weight babies were not included in these analyses. We calculated individual predictions of birth weight (and standard errors) from this model, and averaged them across the 4 categories of PSLEs (i.e., 0, 1, 2, and ≥ 3) to generate mean predicted birth weights depicted in Figure 1.
FIGURE 1. Mean predicted birth weight by stressful life events prior to conception (PSLEs): Early Childhood Longitudinal Study, Birth Cohort, 2001.
Note. The solid line represents the relationship between mean predicted birth weight as a function of PSLEs. The dashed lines represent the 95% confidence interval (CI) for the mean predicted birth weight; calculated standard errors of the prediction were used to generate the CIs. The inset table displays the mean values and 95% CIs for each point, in addition to the difference in means (i.e., mean reduction) compared with the mean for women with no PSLEs; analysis of variance was performed to generate the mean reduction and 95% CIs for predicted birth weight. Each mean is statistically significantly different from all other means at P < .01.
Sensitivity analyses examined the effect of exposure to PSLEs on infant birth weight within 3 nonmutually exclusive time frames: (1) within 1 year prior to conception, (2) greater than or equal to 1 year prior to conception, and (3) prior to conception with an unknown time window.
RESULTS
PSLEs were experienced by 19.7% of mothers (Table 1). The most common PSLE was divorce, occurring in 10.4% of the sample, followed by death of the respondent’s father (5.6%) and mother (2.8%). Mean birth weight of the cohort was 3333 grams (Table 2). Women who reported any PSLE were also older and more likely to be privately insured than were women who did not report PSLEs. Compared with women who did not report PSLEs, women who reported PSLEs were less likely to be never married, Hispanic, of low socioeconomic status, or nulliparous. Women who reported PSLEs were more likely to have experienced a pregnancy complication or to have had previous preterm or SGA infant, but less likely to have had singleton birth or to report experiencing a stressful life event during pregnancy than were women who did not report PSLEs.
TABLE 1.
Type and Timing of Stressful Life Events Prior to Conception (PSLEs): Early Childhood Longitudinal Study-Birth Cohort, 2001
| Variable | % |
|---|---|
| PSLEs | |
| None | 80.3 |
| Any | 19.7 |
| 1 | 17.3 |
| 2 | 2.2 |
| ≥ 3 | 0.2 |
| Types of PSLEs | |
| Experienced fertility problems | |
| Never | 99.6 |
| Ever | 0.4 |
| Death of mother | |
| No, not prior to conception | 97.2 |
| Yes, prior to conception | 2.8 |
| Death of father | |
| No, not prior to conception | 94.4 |
| Yes, prior to conception | 5.6 |
| Experienced death of a child | |
| Never | 98.8 |
| Ever | 1.2 |
| Divorced prior to conception | |
| No, not prior to conception | 89.6 |
| Yes, prior to conception | 10.4 |
| Separated prior to conception | |
| No, not prior to conception | 98.3 |
| Yes, prior to conception | 1.7 |
| Widowed prior to conception | |
| No, not prior to conception | 99.8 |
| Yes, prior to conception | 0.2 |
| Timing of PSLEs | |
| Unknown timing prior to conceptiona | |
| None | 98.1 |
| Any | 1.9 |
| Within 1 y prior to conceptionb | |
| None | 95.7 |
| Any | 4.3 |
| ≥ 1 y prior to conceptionb | |
| None | 85.1 |
| Any | 14.9 |
Note. Data are weighted percentages. Total (weighted) n = 3 774 441; total (unweighted) n = 9350. National Center for Education Statistics rounding rules applied to unweighted numbers.
Stressful life events for which an exact event date was not available, including fertility problems or death of a child.
Stressful life events for which an exact event date was available, including death of mother or father, divorce, marital separation, or widowed.
TABLE 2.
Descriptive Statistics by Maternal Stressful Life Events Prior to Conception (PSLEs) and Infant Birth Weight Status: Early Childhood Longitudinal Study-Birth Cohort, 2001
| Variable | Total | PSLEs
|
Infant Birth Weight Statusa
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| None | Any | P | Very Low | Low | Normal | High | P | ||
| Total (weighted) | 3 774 441 | 3 029 554 | 744 887 | 44 755 | 208 987 | 3 160 613 | 360 085 | ||
| % | 100 | 80.3 | 19.7 | 1.2 | 5.5 | 83.7 | 9.5 | ||
| Total (unweighted) | 9350 | 7350 | 1950 | 1000 | 1200 | 6500 | 650 | ||
| Birth weight (g) | .201 | < .001 | |||||||
| Mean (SD) | 3333 (583) | 3337 (566) | 3316 (651) | 1044 (828) | 2190 (398) | 3334 (332) | 4270 (204) | ||
| Median | 3373 | 3373 | 3373 | 1036 | 2266 | 3344 | 4196 | ||
| Stress and obstetric factors | |||||||||
| PSLEs | < .001 | ||||||||
| None, % | 80.3 | … | … | 71.3 | 76.1 | 81.1 | 76.9 | ||
| Any, % | 19.7 | … | … | 28.7 | 23.9 | 18.9 | 23.1 | ||
| Mean (SD) | 0.22 (0.48) | 0.00 (−) | 1.13 (0.38) | < .001 | 0.36 (1.91) | 0.29 (0.86) | 0.21 (0.42) | 0.27 (0.45) | < .001 |
| Stressful life events during pregnancy, % | .001 | < .001 | |||||||
| None | 94.2 | 93.8 | 96.0 | 93.5 | 91.8 | 94.2 | 96.2 | ||
| Any | 5.8 | 6.2 | 4.0 | 6.5 | 8.2 | 5.8 | 3.8 | ||
| Pregnancy complications, % | .026 | < .001 | |||||||
| None | 86.4 | 86.9 | 84.6 | 57.5 | 70.1 | 87.9 | 86.4 | ||
| Any | 13.6 | 13.1 | 15.4 | 42.5 | 29.9 | 12.1 | 13.6 | ||
| Maternal chronic conditions, % | .098 | < .001 | |||||||
| None | 79.4 | 79.9 | 77.6 | 60.0 | 69.5 | 80.5 | 78.5 | ||
| Any | 20.6 | 20.1 | 22.4 | 40.0 | 30.5 | 19.5 | 21.5 | ||
| Prior child born preterm or SGA, % | < .001 | < .001 | |||||||
| No | 99.0 | 99.2 | 98.0 | 95.9 | 96.7 | 99.1 | 99.4 | ||
| Yes | 1.0 | 0.8 | 2.0 | 4.1 | 3.3 | 0.9 | 0.6 | ||
| Prepregnancy BMI, kg/m2, % | .369 | < .001 | |||||||
| < 18.5 | 3.3 | 3.3 | 3.5 | 6.1 | 5.1 | 3.4 | 1.3 | *** | |
| 18.5–24.9 | 49.5 | 50.2 | 46.7 | 42.6 | 53.0 | 50.6 | 38.5 | *** | |
| 25–29.9 | 26.8 | 26.6 | 27.6 | 25.1 | 21.8 | 26.8 | 30.1 | * | |
| ≥ 30 | 17.9 | 17.4 | 19.7 | 23.5 | 16.9 | 16.9 | 26.4 | *** | |
| Unknown | 2.5 | 2.5 | 10.6 | 2.8 | 3.2 | 2.3 | 3.8 | ||
| Initiation of prenatal care, % | .246 | <.001 | |||||||
| In the first trimester | 95.5 | 95.5 | 95.8 | 94.0 | 93.0 | 95.6 | 96.3 | * | |
| In the second or third trimester | 4.2 | 4.3 | 3.7 | 4.2 | 6.2 | 4.1 | 3.7 | ||
| Did not receive prenatal care | 0.3 | 0.3 | 0.5 | 1.8 | 0.9 | 0.3 | 0.0 | ** | |
| No. of children born, % | < .001 | < .001 | |||||||
| Singleton | 98.3 | 98.7 | 96.5 | 81.3 | 86.2 | 99.1 | 100.0 | ||
| Multiple | 1.7 | 1.3 | 3.5 | 18.7 | 13.8 | 0.9 | 0.0 | ||
| Parity,b % | < .001 | < .001 | |||||||
| Nulliparous | 40.7 | 44.7 | 24.5 | *** | 46.0 | 46.0 | 41.1 | 33.5 | *** |
| Primaparous | 32.8 | 32.6 | 33.8 | 25.7 | 27.2 | 32.9 | 36.2 | *** | |
| Multiparous | 26.5 | 22.8 | 41.6 | *** | 28.3 | 26.7 | 26.0 | 30.3 | ** |
| Maternal sociodemographic factors | |||||||||
| Age, y, % | < .001 | < .001 | |||||||
| 15–19 | 7.5 | 9.0 | 1.3 | *** | 8.9 | 10.7 | 7.3 | 6.7 | * |
| 20–24 | 24.2 | 27.4 | 11.4 | *** | 25.0 | 27.6 | 24.9 | 16.1 | *** |
| 25–29 | 26.2 | 27.1 | 22.7 | ** | 22.0 | 20.9 | 26.5 | 27.1 | * |
| 30–34 | 25.0 | 23.7 | 30.1 | *** | 26.8 | 20.6 | 24.8 | 28.8 | ** |
| ≥ 35 | 17.1 | 12.9 | 34.4 | *** | 17.3 | 20.2 | 16.4 | 21.3 | ** |
| Race/ethnicity, % | .001 | < .001 | |||||||
| White (non-Hispanic) | 57.4 | 56.4 | 61.3 | ** | 45.9 | 49.8 | 56.9 | 67.4 | *** |
| Black (non-Hispanic) | 14.1 | 14.2 | 13.6 | 27.5 | 23.5 | 14.0 | 7.5 | *** | |
| Asian/Pacific Islander (non-Hispanic) | 3.5 | 3.6 | 3.0 | * | 2.5 | 3.6 | 3.7 | 1.7 | *** |
| Other | 2.5 | 2.4 | 2.8 | 1.9 | 2.3 | 2.6 | 1.6 | ||
| Hispanic | 22.6 | 23.4 | 19.3 | ** | 22.2 | 20.8 | 22.8 | 21.7 | |
| Marital status (at birth), % | < .001 | < .001 | |||||||
| Married or living with partner | 83.4 | 82.9 | 85.5 | * | 77.1 | 75.9 | 83.4 | 88.9 | *** |
| Separated/divorced/widowed | 3.1 | 2.5 | 5.3 | *** | 3.0 | 3.2 | 3.1 | 2.3 | |
| Never married | 13.5 | 14.6 | 9.2 | *** | 19.9 | 20.9 | 13.5 | 8.8 | *** |
| Health insurance status, % | .008 | < .001 | |||||||
| Private Only | 59.1 | 58.2 | 62.9 | *** | 52.0 | 50.4 | 58.8 | 68.0 | *** |
| Any Public | 37.4 | 38.4 | 33.5 | ** | 43.6 | 45.9 | 37.8 | 29.0 | *** |
| None | 3.4 | 3.4 | 3.5 | 4.3 | 3.8 | 3.4 | 3.0 | ||
| Socioeconomic status, % | < .001 | < .001 | |||||||
| First quintile (lowest) | 19.7 | 20.6 | 15.8 | *** | 23.9 | 24.8 | 19.7 | 16.2 | *** |
| Second quintile | 20.0 | 20.1 | 19.7 | 24.0 | 24.1 | 20.2 | 15.6 | ** | |
| Third quintile | 20.1 | 19.6 | 21.8 | 20.9 | 20.2 | 19.9 | 21.1 | ||
| Fourth quintile | 20.2 | 19.4 | 23.1 | * | 16.8 | 16.1 | 20.2 | 22.2 | * |
| Fifth quintile (highest) | 20.1 | 20.2 | 19.7 | 14.3 | 14.7 | 20.0 | 24.8 | *** | |
| Region of residence, % | .208 | .124 | |||||||
| Northeast | 17.1 | 17.3 | 16.2 | 17.7 | 15.3 | 16.8 | 20.1 | ||
| Midwest | 22.3 | 22.4 | 21.7 | 21.5 | 22.0 | 22.2 | 23.4 | ||
| South | 36.9 | 36.2 | 39.6 | 41.4 | 40.0 | 36.9 | 34.8 | ||
| West | 23.8 | 24.1 | 22.5 | 19.4 | 22.7 | 24.1 | 21.7 | ||
Note. BMI = body mass index; SGA = small for gestational age. Data are weighted percentages or means with standard deviations (SDs). National Center for Education Statistics rounding rules applied to unweighted numbers; unweighted subgroup numbers may not add to the total because of rounding error.
Birth weight defined as very low (< 1500 g), low (1500–2499 g), normal (2500–3999 g), or high (≥ 4000 g).
Parity of the mother not including her most recent live birth.
P < .05;
P < .01;
P < .001.
Very Low Birth Weight
Very LBW infants were delivered by 1.2% of mothers (Table 2). Exposure to PSLEs was more common among women with very LBW infants than among those with normal birth weight infants (very LBW, 28.7% vs normal birth weight, 18.9%; overall P < .001).
In adjusted analyses, women exposed to any PSLE had 44% higher odds of having a very LBW baby than did women who were not exposed (AOR = 1.44; 95% CI = 1.17, 1.76; Table 3). Pregnancy complications did not affect the relationship between PSLEs and the odds of having a very LBW baby (Table 3, model 2; AOR = 1.38; 95% CI = 1.13, 1.69), but they were an independent predictor of very LBW (AOR = 4.84; 95% CI = 4.09, 5.74). Stressful life events during pregnancy were not independently associated with very LBW. There were significant disparities in the odds of having a very LBW infant by key maternal and family sociodemographic and health characteristics (data available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 3.
Staged Multinomial Logistic Regression Predicting Very Low and Low Birth Weight: Early Childhood Longitudinal Study-Birth Cohort, 2001
| Variable | Model 1, AOR (95% CI)
|
Model 2, AOR (95% CI)
|
||
|---|---|---|---|---|
| Very Low Birth Weighta | Low Birth Weighta | Very Low Birth Weighta | Low Birth Weighta | |
| PSLEs | ||||
| None (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Any | 1.44 (1.17, 1.76) | 1.17 (0.93, 1.47) | 1.38 (1.13, 1.69) | 1.14 (0.91, 1.43) |
| Stressful life events during pregnancy | ||||
| None (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Any | 1.05 (0.69, 1.60) | 1.40 (0.95, 2.07) | 1.04 (0.67, 1.64) | 1.36 (0.91, 2.04) |
| Pregnancy complications | ||||
| None (Ref) | 1.00 | 1.00 | ||
| Any | 4.84 (4.09, 5.74) | 3.00 (2.44, 3.70) | ||
Note. AOR = adjusted odds ratio; CI = confidence interval; PSLEs = stressful life events prior to conception. Models also control for maternal chronic conditions, having a prior preterm or small-for-gestational-age baby, prepregnancy body mass index, initiation of prenatal care, plurality, parity, maternal age, maternal race/ethnicity, marital status at birth, health insurance coverage, socioeconomic status, and region of residence. All models account for complex sampling design of the Early Childhood Longitudinal Study, Birth Cohort. Full regression models are available as a supplement to the online version of this article at http://www.ajph.org.
Versus normal birth weight.
Low Birth Weight
Low birth weight infants were delivered by 5.5% of mothers. Exposure to PSLEs was more common among women with LBW infants than among those with normal birth weight infants (LBW, 23.9% vs normal birth weight, 18.9%; overall P < .001).
Our adjusted analyses did not support an association between maternal exposure to PSLEs or stressful life events during pregnancy and the odds of having a LBW baby. Pregnancy complications were significantly and independently associated with higher odds of having a LBW baby (AOR = 3.00; 95% CI = 2.44, 3.70). There were significant disparities in the odds of having a LBW infant by key maternal and family sociodemographic and health characteristics (data available as a supplement to the online version of this article at http://www.ajph.org).
A cumulative effect was observed of PSLEs on birth weight, such that each PSLE exerted an additional negative effect on infant birth weight (Figure 1).
Sensitivity Analyses
The association between PSLEs and birth weight varied by the timing of exposure, such that PSLEs that occurred 1 year or more prior to conception increased the odds of having a very LBW baby (AOR = 1.31; 95% CI = 1.07, 1.61), whereas PSLEs within 1 year prior to conception increased the odds of having a high birth weight baby (AOR = 1.50; 95% CI = 1.02, 2.20), but not a LBW or very LBW baby. Women who experienced PSLEs at an unknown time prior to conception had increased odds of having a very LBW (AOR = 2.50; 95% CI = 1.72, 3.63) or LBW baby (AOR = 1.83; 95% CI = 1.24, 2.68; data available upon request).
DISCUSSION
This was the first population-based study, to our knowledge, to investigate the relationship between PSLEs and infant birth weight in the United States. Our findings indicate that mothers who experienced any PSLE were more likely to give birth to a very LBW infant. Furthermore, there was a reduction in infant birth weight for each additional PSLE, suggesting that the effect of exposure to PSLEs might accumulate over a woman’s life course to increase her risk of having a lower birth weight infant. These novel findings are discussed in this section with respect to their implications for research, policy, and practice.
We know of only 3 other studies that examined the impact of stress or stressors prior to pregnancy on infant birth weight.15,27,28 Notably, Khashan et al.15 demonstrated that Danish women who reported the death or serious illness of a relative within the 6 months prior to or during pregnancy had lower birth weight infants. However, that study did not examine the independent effect of events prior to pregnancy controlling for events during pregnancy; rather, these periods were examined as mutually exclusive categories compared with an unexposed group. Specifically, women were recorded as having a stressful life event (1) during the first trimester, (2) before pregnancy, (3) during the second trimester, or (4) during the third trimester. Women who experienced a stressful life event in more than 1 time period were categorized into 1 of these groups based on this a priori hierarchy. Although these studies provide compelling evidence for the significant role of PSLEs in predicting LBW, to our knowledge, we are the first to investigate the independent effects of events prior to conception and during pregnancy, which allowed us to isolate the effects of these stressors at these different time periods. Importantly, we found that the relationship between PSLEs and very LBW remained significant even after accounting for events during pregnancy.
Additionally, we found evidence that the accumulation of exposure to PSLEs might increase women’s risk for having lower birth weight babies. In turn, these infants might be set on an adverse health trajectory, with greater risks for morbidity and mortality over their life course.2,4,29–34 Future work examining stressors prior to and during pregnancy is needed to confirm our findings and determine the independent, cumulative, or interactive roles of PSLEs on obstetric outcomes.
Our findings also suggest that the type and timing of exposure to PSLEs exerted differential effects on birth weight. Previous research has focused on a relatively narrow time window preceding pregnancy (e.g., up to 17 months) and has found significant associations with poor birth outcomes.15,35–37 Our findings, which examined a larger time window prior to pregnancy, suggest that the experience of stressful life events throughout a woman’s life span might exert lasting effects on her reproductive health and obstetric outcomes. Furthermore, the effect of events that occurred 1 year or more prior to conception had a stronger association with very LBW than did events that occurred within a year prior to conception. Interestingly, Precht et al.36 found that events occurring 12 to 17 months prior to pregnancy were not associated with having a SGA infant, although this subgroup was small. Future research should strive to extend the exposure window when investigating the antecedents of adverse obstetric outcomes to confirm the findings from the present study and to better understand how the timing of events might influence birth outcomes.
By contrast, exposure to events occurring within a year prior to conception was associated with an increased risk for high birth weight. It is possible that the effects of stressors acted through different physiological or behavioral pathways depending on the time period, and therefore, influenced birth outcomes differentially. For example, PSLEs and subsequent psychological stress occurring within a year prior to conception might have contributed to changes in diet that led to higher prepregnancy BMI,38,39 a known risk factor for high birth weight.40,41 Future epidemiological and basic research will be needed to fully understand these relationships.
PSLEs with unknown timing were primarily composed of women who had lost a child or experienced fertility problems. These events might be particularly traumatic for women, which might explain the strong association, irrespective of timing. However, it is also possible that genetic factors could explain this relationship, especially if the death of a previous child occurred during the neonatal or early infancy periods. Although additional research is needed, our results suggest that stressful life events that occurr across a women’s life course, and potentially 1 year or more before conception, might have a lasting effect on women’s obstetric health.
Several mechanisms might explain the relationship between PSLEs and very LBW. Theory suggests that stress affects obstetric outcomes when environmental stimuli (e.g., PSLEs) overwhelm an individual’s coping resources,42 leading to subsequent physiological and behavioral responses.18,43,44 Maternal stress contributes to neuroendocrine, immune and inflammatory processes that are associated with poor birth outcomes18,44; moreover, women exposed to stressors might be more likely to engage in negative health behaviors known to affect infant birth weight.45 Although our study only examined PSLEs and not other domains of the stress process, exposures to PSLEs might activate the stress process and trigger negative physiological responses. If such physiological consequences persist throughout a woman’s life or increase her vulnerability to future stressors, then PSLEs might be far more influential in affecting obstetric outcomes than events occurring only during pregnancy, when there may be less time to elicit substantial physiological costs.17 As such, the preconception period might be a crucial time for interventions to improve birth outcomes.
Limitations
Several potential limitations should be considered when interpreting our results. First, children who died before 9 months of age were not eligible to participate in the ECLS-B. Our study therefore likely excluded the children with the worst birth outcomes, which was a potential survival bias leading to conservative estimates of the effect of PSLEs on infant birth weight.46 Second, the data were collected approximately 9 months postpartum and might be subject to recall bias. Specifically, if events were systematically underreported by mothers of very LBW and LBW infants, or mothers of normal birth weight infants, our findings could be biased toward or away from the null, respectively. In addition, birth certificate data might have been underreported or incorrectly reported some information (e.g., pregnancy complications).6 However, underreporting these data would lead to conservative estimates. Similarly, we relied on self-reported data for factors like prepregnancy BMI, which might have biased our estimates in an unknown direction.
ECLS-B collected limited data on stressful life events and might not have comprehensively captured the spectrum of stressors some women experience.47–51 Failing to capture additional events (including adverse childhood experiences) might have resulted in misclassification. Although there is a rich literature on adverse childhood experiences and adult outcomes,52 only 1 study has investigated the relationship between adverse childhood experiences and reproductive outcomes.53 Clearly, more research into the nexus of adverse childhood experiences and women’s reproductive health is warranted. Moreover, the number of individuals who endorsed specific events was small; therefore, we were unable to conduct analyses examining the independent effect of each type of event on infant birth weight. Furthermore, some of these events were mutually exclusive (i.e., could only happen before or during pregnancy), and future work should examine a broader spectrum of stressors and daily stress in order to confirm and better understand our findings.
To date, the majority of research and policy efforts to improve birth outcomes have focused on identifying and monitoring maternal risk factors during pregnancy. However, interventions that solely address prenatal risk factors inadequately account for the broader, contextual, and life course factors that influence women’s risk for adverse obstetric outcomes. Increasing evidence demonstrates that interventions administered prior to pregnancy improve birth outcomes,54 and recent recommendations from the Maternal and Child Health Bureau, Institutes of Medicine, Centers for Disease Control and Prevention, and Healthy People 2020 have focused on improving women’s health during this critical pre-conception period.45,55–57 Our findings provide empirical evidence to support these calls to action.
This work has implications for practice, policy, and future research. First, our findings suggest that it might be important to shift the clinical paradigm upstream to the preconception period. This work supports efforts to deliver preconception care that encompasses reproductive awareness, risk screening and counseling, and health care for families55 in an effort to improve maternal and child health. Second, research should determine whether screening for these PSLEs in the clinical setting identifies women at risk for very LBW. Third, interventions that focus on reducing the deleterious effects of stressors, such as those that promote coping skills, build resiliency and increase social support, might be an important way to improve infant birth weight. Finally, although preconception care is a top priority, there is also a valuable opportunity during early pregnancy to identify high-risk women (i.e., those with a history of PSLEs) to ensure that supportive interventions can be put in place to decrease the risk of poor birth outcomes.
Conclusions
Our population-based findings indicate that exposure to any PSLE increased a woman’s risk of having a very LBW infant. Furthermore, the accumulation of PSLEs significantly contributed to decreasing infant birth weight. This suggests that PSLEs, especially the accumulation of multiple PSLEs, might have a physiological impact on women with far-reaching implications for their obstetric health. Clinical, programmatic, and policy interventions might need to shift their focus to addressing stressful life events prior to conception, especially for reproductive-aged women, to improve birth outcomes and the health trajectories of their children.
Supplementary Material
Acknowledgments
This work was supported in whole or in part by federal funds from the US Department of Health and Human Services, Health Resources and Services Administration (grant R40MC23625; PI, W. P. W.). Additional funding for this research was provided by a grant from the Health Disparities Research Scholars Program (FW:T32HD049302; PI, G. Sarto).
We would also like to thank the anonymous reviewers for their helpful comments and suggestions.
Footnotes
Contributors
W. P. Witt made substantial contributions to the study design, acquisition of data, interpretation of data, and drafting the article and was ultimately responsible for overseeing the data analysis and article preparation. E. R. Cheng helped with the study design, data interpretation, and drafting of the article. L. E. Wisk assisted with the study design, data preparation and analysis, interpretation of data, and drafting of the article. K. Litzelman contributed to the interpretation of the data and drafting of the article. D. Chatterjee assisted in interpreting the study data, summarizing study results, editing and refining the article, and the conceptualization of the overall analytical plan. K. Mandell helped edit and refine the article and assisted with conceptualization of the overall analytical plan. F. Wakeel assisted with the study design, conceptualization of variables, interpretation of the data, and writing and editing of the article.
Human Participant Protection
The University of Wisconsin-Madison Health Sciences institutional review board considered this study exempt from review.
References
- 1.Heron M. National vital statistics reports. 6. Vol. 60. Hyattsville, MD: National Center for Health Statistics; 2012. Deaths: leading causes for 2008. [PubMed] [Google Scholar]
- 2.Risnes KR, Vatten LJ, Baker JL, et al. Birthweight and mortality in adulthood: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):647–661. doi: 10.1093/ije/dyq267. [DOI] [PubMed] [Google Scholar]
- 3.Bhushan V, Paneth N, Kiely JL. Impact of improved survival of very low birth weight infants on recent secular trends in the prevalence of cerebral palsy. Pediatrics. 1993;91(6):1094–1100. [PubMed] [Google Scholar]
- 4.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312(2):82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 5.Osmond C, Barker D. Fetal, infant, and childhood growth are predictors of coronary heart disease, diabetes, and hypertension in adult men and women. Environ Health Perspect. 2000;108(suppl 3):545–553. doi: 10.1289/ehp.00108s3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin J, Hamilton B, Ventura S, Osterman M, Wilson E, Mathews T. Births: final data for 2010. National vital statistics reports. 1. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 7.North American Association for the Study of Obesity. National Heart, Lung, and Blood Institute. The Practical Guide: Identification, Evaluation, and Treatment for Overweight and Obesity in Adults. Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute; 2000. [Google Scholar]
- 8.Carmichael SL, Shaw GM. Maternal life event stress and congenital anomalies. Epidemiology. 2000;11(1):30–35. doi: 10.1097/00001648-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Hedegaard M, Henriksen TB, Secher NJ, Hatch MC, Sabroe S. Do stressful life events affect duration of gestation and risk of preterm delivery? Epidemiology. 1996;7(4):339–345. doi: 10.1097/00001648-199607000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Lu MC, Chen B. Racial and ethnic disparities in preterm birth: the role of stressful life events. Am J Obstet Gynecol. 2004;191(3):691–699. doi: 10.1016/j.ajog.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 11.Maric NP, Dunjic B, Stojiljkovic DJ, Britvic D, Jasovic-Gasic M. Prenatal stress during the 1999 bombing associated with lower birth weight—a study of 3,815 births from Belgrade. Arch Womens Ment Health. 2010;13(1):83–89. doi: 10.1007/s00737-009-0099-9. [DOI] [PubMed] [Google Scholar]
- 12.Sable MR, Wilkinson DS. Impact of perceived stress, major life events and pregnancy attitudes on low birth weight. Fam Plann Perspect. 2000;32(6):288–294. [PubMed] [Google Scholar]
- 13.Whitehead N, Hill HA, Brogan DJ, Blackmore-Prince C. Exploration of threshold analysis in the relation between stressful life events and preterm delivery. Am J Epidemiol. 2002;155(2):117–124. doi: 10.1093/aje/155.2.117. [DOI] [PubMed] [Google Scholar]
- 14.Zhu P, Tao F, Hao J, Sun Y, Jiang X. Prenatal life events stress: implications for preterm birth and infant birthweight. Am J Obstet Gynecol. 2010;203(1):34, e1–8. doi: 10.1016/j.ajog.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 15.Khashan AS, McNamee R, Abel KM, et al. Reduced infant birthweight consequent upon maternal exposure to severe life events. Psychosom Med. 2008;70(6):688–694. doi: 10.1097/PSY.0b013e318177940d. [DOI] [PubMed] [Google Scholar]
- 16.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42(4):589–597. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- 17.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 18.Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 19.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon W. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Witt WP, Wisk LE, Cheng ER, Hampton JM, Hagen EW. Preconception mental health predicts pregnancy complications and adverse birth outcomes: a national population-based study. Matern Child Health J. 2012;16(7):1525–1541. doi: 10.1007/s10995-011-0916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United States Department of Education. Early Childhood Longitudinal Study, Birth Cohort, Nine-Month Data Collection. Washington, DC: US Department of Education, National Center for Education Statistics; 2001. [Google Scholar]
- 22.Snow K, Derecho A, Wheeless S, et al. Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), Kindergarten 2006 and 2007 Data File User’s Manual (2010-010) Washington, DC: National Center for Education Statistics, Institute of Education Sciences, US Department of Education; 2009. [Google Scholar]
- 23.Eugster A, Vingerhoets A. Psychological aspects of in vitro fertilization: a review. Soc Sci Med. 1999;48 (5):575–589. doi: 10.1016/s0277-9536(98)00386-4. [DOI] [PubMed] [Google Scholar]
- 24.Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 25.Rahe RH, Arthur DRJ. Life change and illness studies: past history and future directions. J Human Stress. 1978;4(1):3–15. doi: 10.1080/0097840X.1978.9934972. [DOI] [PubMed] [Google Scholar]
- 26.Rahe RH, Veach TL, Tolles RL, Murakami K. The stress and coping inventory: an educational and research instrument. Stress Med. 2000;16(4):199–208. [Google Scholar]
- 27.Hisham TJ, Moawed SA. The relation of low birth weight to psychosocial stress and maternal anthropometric measurements. Saudi Med J. 2000;21(7):649–654. [PubMed] [Google Scholar]
- 28.Dominguez TP, Dunkel-Schetter C, Glynn LM, Hobel C, Sandman CA. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychol. 2008;27(2):194–203. doi: 10.1037/0278-6133.27.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anderson P, Doyle LW. Neurobehavioral outcomes of school-age children born extremely low birth weight or very preterm in the 1990s. JAMA. 2003;289(24):3264–3272. doi: 10.1001/jama.289.24.3264. [DOI] [PubMed] [Google Scholar]
- 30.Hack M, Klein N, Taylor H. School-age outcomes of children of extremely low birth weight and gestational age. Semin Neonatol. 1996;1(4):277–288. [Google Scholar]
- 31.Hack M, Klein NK, Taylor HG. Long-term developmental outcomes of low birth weight infants. Future Child. 1995;5(1):176–196. [PubMed] [Google Scholar]
- 32.Paneth NS. The problem of low birth weight. Future Child. 1995;5(1):19–34. [PubMed] [Google Scholar]
- 33.Whincup PH, Kaye SJ, Owen CG, et al. Birth weight and risk of type 2 diabetes. JAMA. 2008;300(24):2886–2897. doi: 10.1001/jama.2008.886. [DOI] [PubMed] [Google Scholar]
- 34.Cheung YB. Early origins and adult correlates of psychosomatic distress. Soc Sci Med. 2002;55(6):937–948. doi: 10.1016/s0277-9536(01)00225-8. [DOI] [PubMed] [Google Scholar]
- 35.Khashan AS, McNamee R, Abel K, et al. Rates of preterm birth following antenatal maternal exposure to severe life events: a population-based cohort study. Hum Reprod. 2009;24(2):429–437. doi: 10.1093/humrep/den418. [DOI] [PubMed] [Google Scholar]
- 36.Precht DH, Andersen PK, Olsen J. Severe life events and impaired fetal growth: a nation-wide study with complete follow-up. Acta Obstet Gynecol Scand. 2007;86 (3):266–275. doi: 10.1080/00016340601088406. [DOI] [PubMed] [Google Scholar]
- 37.Witt WP, Litzelman K, Cheng ER, Wakeel F, Barker ES. Measuring stress before and during pregnancy: a review of population-based studies of obstetric outcomes. Matern Child Health J. 2013 doi: 10.1007/s10995-013-1233-x. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts C, Troop N, Connan F, Treasure J, Campbell IC. The effects of stress on body weight: biological and psychological predictors of change in BMI. Obesity (Silver Spring) 2007;15(12):3045–3055. doi: 10.1038/oby.2007.363. [DOI] [PubMed] [Google Scholar]
- 39.Barry D, Petry N. Gender differences in associations between stressful life events and body mass index. Prev Med. 2008;47(5):498–503. doi: 10.1016/j.ypmed.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kramer MS, Morin I, Yang H, et al. Why are babies getting bigger? Temporal trends in fetal growth and its determinants. J Pediatr. 2002;141(4):538–542. doi: 10.1067/mpd.2002.128029. [DOI] [PubMed] [Google Scholar]
- 41.Nohr EA, Vaeth M, Baker JL, Sørensen TI, Olsen J, Rasmussen KM. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am J Clin Nutr. 2008;87(6):1750–1759. doi: 10.1093/ajcn/87.6.1750. [DOI] [PubMed] [Google Scholar]
- 42.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage Publications; 1987. pp. 31–49. [Google Scholar]
- 43.McEwen BS. Stress, adaptation, and disease: allo-stasis and allostatic load. Ann N Y Acad Sci. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 44.Wadhwa PD, Culhane JF, Rauh V, et al. Stress, infection and preterm birth: a biobehavioural perspective. Paediatr Perinat Epidemiol. 2001;15(suppl 2):17–29. doi: 10.1046/j.1365-3016.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- 45.Valero De Bernabé J, Soriano T, Albaladejo R, et al. Risk factors for low birth weight: a review. Eur J Obstet Gynecol Reprod Biol. 2004;116(1):3–15. doi: 10.1016/j.ejogrb.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 46.Class QA, Khashan AS, Lichtenstein P, Långström N, D’Onofrio BM. Maternal stress and infant mortality: the importance of the preconception period. Psychol Sci. 2013;24(7):1309–1316. doi: 10.1177/0956797612468010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Collins JW, Jr, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94(12):2132–2138. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Collins JW, Jr, David RJ, Symons R, Handler A, Wall SN, Dwyer L. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology. 2000;11(3):337–339. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 49.Elo IT, Culhane JF, Kohler IV, et al. Neighbourhood deprivation and small-for-gestational-age term births in the United States. Paediatr Perinat Epidemiol. 2009;23 (1):87–96. doi: 10.1111/j.1365-3016.2008.00991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roberts EM. Neighborhood social environments and the distribution of low birthweight in Chicago. Am J Public Health. 1997;87(4):597–603. doi: 10.2105/ajph.87.4.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Caetano R, Cunradi CB, Schafer J, Clark CL. Intimate partner violence and drinking patterns among white, black, and Hispanic couples in the US. J Subst Abuse. 2000;11(2):123–138. doi: 10.1016/s0899-3289(00)00015-8. [DOI] [PubMed] [Google Scholar]
- 52.Felitti VJ. The relation between adverse childhood experiences and adult health: turning gold into lead. Z Psychosom Med Psychother. 2002;6(1):44–47. doi: 10.13109/zptm.2002.48.4.359. [DOI] [PubMed] [Google Scholar]
- 53.Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004;113(2):320–327. doi: 10.1542/peds.113.2.320. [DOI] [PubMed] [Google Scholar]
- 54.Atrash HK, Johnson K, Adams M, Cordero JF, Howse J. Preconception care for improving perinatal outcomes: the time to act. Matern Child Health J. 2006;10(5 Suppl):S3–11. doi: 10.1007/s10995-006-0100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cheng TL, Kotelchuck M, Guyer B. Preconception women’s health and pediatrics: an opportunity to address infant mortality and family health. Acad Pediatr. 2012;12(5):357–359. doi: 10.1016/j.acap.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fine A, Kotelchuck M. Rethinking MCH: the MCH life course model as an organizing framework. US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau; 2010. [Accessed November 27, 2012.]. Available at: http://mchb.hrsa.gov/lifecourse/rethinkingmchlifecourse.pdf. [Google Scholar]
- 57.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care—United States. MMWR Recomm Rep. 2006;55 (RR-6):1–23. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.