Abstract
Objectives
We examined factors associated with readiness to coordinate mental health, public health, and HIV testing among community-based addiction health services programs.
Methods
We analyzed client and program data collected in 2011 from publicly funded addiction health services treatment programs in Los Angeles County, California. We analyzed a sample of 14 379 clients nested in 104 programs by using logistic regressions examining odds of service coordination with mental health and public health providers. We conducted a separate analysis to examine the percentage of clients receiving HIV testing in each program.
Results
Motivational readiness and organizational climate for change were associated with higher odds of coordination with mental health and public health services. Programs with professional accreditation had higher odds of coordinating with mental health services, whereas programs receiving public funding and methadone and residential programs (compared with outpatient) had a higher percentage of clients receiving coordinated HIV testing.
Conclusions
These findings provide an evidentiary base for the role of motivational readiness, organizational climate, and external regulation and funding in improving the capacity of addiction health services programs to develop integrated care.
Providers of addiction health services (AHS) face an unprecedented challenge to implement integrated care services to respond to the complex health care conditions of racial- and ethnic-minority populations entering addiction treatment.1–3 Increased access to integrated addiction, mental health, and medical care has been associated with reduced health care costs and positive health outcomes among minority populations.4–8 Yet AHS providers face significant barriers to integrating or collaborating with mental health or medical care providers to address the needs of clients with co-occurring problems.6–11 Because the Affordable Care Act promotes delivery of community-based integrated care for vulnerable populations, out-patient AHS located in low-income and ethnic-minority communities are poised to become significant intervention points for the diagnosis and treatment of sexually transmitted infections and other mental health and physical conditions if they integrate services.12–14 We examined the organizational capacity (funding, regulation, readiness for change, and leadership) of community-based AHS to coordinate mental health, public health, and HIV-testing services in low-income, urban, and ethnic-minority communities in Los Angeles County, California.
Despite significant efforts to increase service coordination and integration in health care settings during the past 50 years, there is limited and inconsistent evidence regarding the most effective approaches to implementing integrated practices.15 Service integration refers to the effective coordination of specific services to holistically respond to the health care needs of individuals.16 The extant literature has revealed multiple system and organizational barriers to integration, including the bureaucratic process of service delivery, professional and philosophical differences among providers, and inadequate resources.10,17 More specifically, effective coordination is generally affected by limited funding and infrastructure for communication among providers to establish effective coordination of services across agencies18 and build necessary partnerships.19–21
Because more than 44% of clients entering AHS report dual substance use and mental health or physical disorders,9 providers have made ongoing efforts to coordinate care.22–26 Yet, besides entering service agreements across agencies, providers with fewer resources (e.g., limited time for training, access to computer terminals, or supervision) struggle to invest in coordination practices, such as dual-diagnosis training and medical staffing, as well as clinical processes to effectively diagnose, treat, or triage mental, physical,27,28 and HIV-related conditions.29–31 Extensive research has shown that public funding increases safety-net services (child care, job readiness, and other ancillary and social services) and HIV preventive care among AHS providers,30,32–36 and state-licensed and professionally accredited facilities are more likely to test for HIV/AIDS.33,37,38 However, little is known about how these external funding and regulatory factors, in combination with internal program factors, enable program staff to coordinate with mental health, public health, and HIV-prevention programs to ensure integrated care.
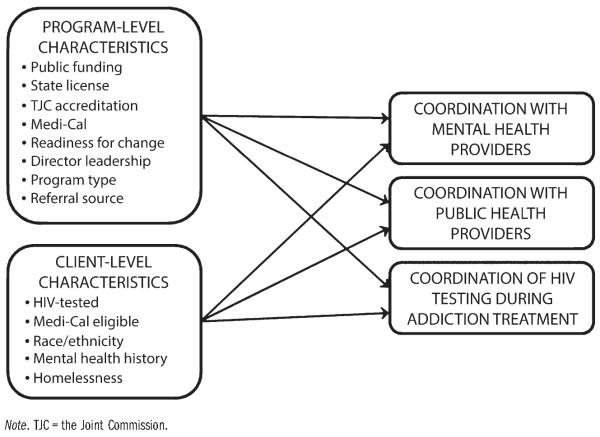
To examine the capacity of AHS programs to integrate care in the addictions system, which is generally characterized by unstable funding, passive leadership, high staff turnover,32,39,40 and limited technical resources to conduct complex clinical operations and support effective decision-making,41 we relied on Shortell’s42 conceptual model of organizational change. This model examines whether system factors (e.g., public funding, regulation, and professional accreditation) and the organizational structure, strategy, coordination, knowledge, and skills of providers (e.g., readiness for change and leadership) are associated with the implementation of changes in service delivery (e.g., coordinated mental and public health care and HIV testing). As shown in Figure 1, we proposed that both program and client characteristics in AHS are likely to affect coordination with mental health, public health, and HIV testing services.
FIGURE 1.
Conceptual model of the effects of program and client characteristics on coordination of mental health, public health, and HIV testing services: Los Angeles County, CA, 2010-2011.
The readiness-for-change framework is commonly used to assess program resources and climate as well as staff motivation and attributes to explain the process of exposing, adopting, implementing, and sustaining new practices.43,44 Attributes such as positive peer influence, opportunities for professional growth, and a strong organizational culture and mission have been associated with increased use of cognitive–behavioral treatment approaches,45,46 and staff training and external pressure from regulation and funding were found to be related to the uptake of mental health practices in AHS.47 Furthermore, leadership is an emerging focal point in efforts to increase the uptake of evidence-based practices and improve the quality of care in behavioral health.48,49 In particular, transactional orientation (guiding performance) and transformational approaches (leading by example and motivating self-growth) have been essential components of leadership associated with fostering change.50 In AHS organizations, these components have been associated with staff satisfaction, a critical aspect of the implementation process.51
As small community-based AHS programs seek to respond to Affordable Care Act funding and regulatory expectations for integrated care and fulfill their mission of improving public health, this conceptual framework highlights the importance of public funding, and professional and state regulation, as well as internal factors such as director’s leadership, program resources, and staff attitudes and skills to delivering coordinated care. Hence, we posited the following hypotheses:
Hypothesis 1: Percentage of public funding, state licensure, and professional accreditation among AHS programs would be positively associated with (1) coordination with mental health, (2) coordination with public health, and (3) the percentage of clients receiving HIV testing.
Hypothesis 2: The 4 components of readiness for change (program resources, program climate, staff motivational readiness, and staff attributes) would be positively associated with (1) coordination with mental health, (2) coordination with public health, and (3) the percentage of clients receiving HIV testing. Hypothesis 3: Director’s leadership would be positively associated with (1) coordination with mental health, (2) coordination with public health, and (3) the percentage of clients receiving HIV testing.
METHODS
We used a fully concatenated program and client data set collected from 2010 to 2011 (full procedures are described in detail elsewhere52). We drew the sampling frame for program data from the Los Angeles County Participant Reporting System. This ongoing systemwide survey, completed by each publicly funded program, captures the treatment experiences and immediate outcomes of a racially and ethnically diverse client population in one of the largest addiction treatment systems in the United States. Of the 141 items in the Los Angeles County Participant Reporting System, more than half are standardized scales and questions related to admission, discharge, and health derived from state (California Outcome Measure System) and federal (Treatment Episode Data Set) measurement systems.53 Client data included 15 100 client treatment episodes collected from July 1, 2010, to December 30, 2011.
The principal investigator and 2 research assistants also collected data via a confidential online survey. We collected data from a random sample of 147 publicly funded and nonprofit programs from the 350 programs located in communities with a population of 40% or more Latino or African American residents in Los Angeles County (78% of Los Angeles County). We defined a program as a treatment unit in which substance abuse treatment constituted at least 75% of services. To enhance parameter estimation and improve representativeness of the average AHS community-based program, we excluded military and nontraditional organizational structures—for instance, solo practitioners and programs operated by the criminal justice system (e.g., drug treatment in prisons, jails, and detention centers).
Clinical supervisors served as key informants for program survey measures. Most programs reported having only 1 supervisor, and in cases where there was more than 1, the investigative team selected the respondent randomly after reviewing a list of staff. The investigative team also relied on additional sources of data to cross-validate survey measures during follow-up site visits with 91% of the sample. Consistent information from at least 2 of the 3 sources of data was necessary for inclusion of each program in the analytic sample: (1) a review of program characteristics and service delivery information reported to the funding organization (Los Angeles County Department of Public Health), (2) qualitative reports from 1 counselor per program, and (3) a review of printed material available at each provider site (e.g., brochures, online information, and posted signs on integration of mental health and public health services). For instance, we checked data from brochures and Web sites to verify provision of mental health services, and referrals to public health providers, including HIV prevention and intervention services.
The final sample consisted of 104 programs and 14 379 treatment episodes with full and verified information. The final analytic sample decreased from 147 to 104 programs because 12 programs did not respond to the survey, 10 programs reported inconsistent data, 10 programs did not serve county clients in 2010 to 2011, and 11 programs had closed before data collection. The 43 excluded programs did not differ from the sample in terms of main independent variables (P > .05). Missing data were less than 8% across all survey measures.
Study Variables
Dependent variables
We examined 3 dependent variables: coordination with mental health providers, coordination with public health providers, and coordination of on-site and off-site HIV testing during addiction treatment. The first measure asked clinical supervisors how frequently their AHS program collaborated with mental health and psychiatric providers to coordinate care for clients with dual disorders. The second measure asked clinical supervisors a similar question about their work with public health providers in community-based settings. The 5 possible responses ranged from never to always. These 2 measures reported bimodal distributions in the never, almost never, and always categories; thus, we transformed them to dichotomous scales. Fifty-three percent of the sample reported high coordination with mental health providers and 21% of supervisors reported high coordination with public health providers. The third outcome measure asked clinical supervisors about coordination of on-site or off-site HIV testing that resulted in clients receiving HIV testing while receiving treatment.
Independent variables
Independent variables in the study included percentage of public funding, state licensure, accreditation, acceptance of Medi-Cal payment, 4 measures of organizational readiness for change, and a measure of director’s leadership. The public funding variable measured the percentage of public funding obtained during the past fiscal year, and regulation variables were dichotomous measures of state licensing and accreditation by the Joint Commission.
We used the Organizational Readiness for Change Scale to measure program readiness to implement new practices with 67 items divided in several subscales: motivational readiness (3 scales, average α = 0.80), resources (2 scales, average α = 0.74), staff attributes (2 scales, average α = 0.86), and organizational climate (4 scales, average α = 0.78).43,44 We rated all items on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree); higher scores represented higher readiness.
The leadership scale consists of 9 items assessing agency or program director leadership capacity. This measure included 2 subscales associated with implementation of evidence-based practices: transformational leadership characterized by intellectual stimulation, support for innovation, and integrity (7 items); and transactional leadership related to delegation and job expectations (2 items; α = 0.96).51 Clinical supervisors rated their directors’ leadership on a 5-point scale (1= strongly disagree to 5 = strongly agree), and scores were totaled as suggested by the measure’s authors.51 Higher scores represented higher levels of leadership capacity among directors as reported by clinical supervisors.
Control variables
Controls included several organizational characteristics associated with implementation of new service delivery practices in AHS programs. These characteristics included program type (i.e., whether the program was primarily outpatient, methadone, or residential) and referral source (i.e., self-referral, community, Proposition 36, drug court, or social services), because referrals may exert pressure on programs to provide integrated care.
At the client level, we also accounted for several characteristics associated with implementation of new practices.32,39,54 Dichotomous variables included client reports on HIV testing, Medi-Cal eligibility, race and ethnicity, mental health history, and homelessness status. Table 1 shows descriptive statistics and response format for scales and measures.
TABLE 1.
Program (n = 104) and Client (n = 14 379) Variables in Community-Based Addiction Health Services Providers: Los Angeles County, CA, 2010-2011
| Variables | Mean (SD) or % | Response Format |
|---|---|---|
| Program characteristics | ||
| Mental health services | 53.29 | On-site or off-site coordination with mental health services |
| Public health services | 21.67 | On-site or off-site coordination with public health services |
| HIV testing service | 31.83 (28.23) | Percentage of clients who received on-site or off-site HIV testing |
| Public funding | 42.52 (42.68) | Percentage of public funding in total funding during previous fiscal year |
| Program license | 97.09 | Licensed by state |
| TJC accreditation | 32.19 | Accredited by TJC |
| Medi-Cal acceptance | 81.91 | Accepts Medi-Cal reimbursement |
| Readiness for change | ||
| Motivational readiness | 3.11 (0.61) | 21 itemsa (e.g., Your program needs more training for effective implementation of EBPs.) |
| Resources | 3.76 (0.56) | 12 items (e.g., Clinical management decisions for your program are well planned.) |
| Staff attributes | 4.16 (0.43) | 8 items (e.g., You are able to adapt quickly when you have to make changes.) |
| Organizational climate | 3.50 (0.56) | 16 items (e.g., You fell encouraged to try new and different techniques.) |
| Directorial leadership | 3.90 (0.69) | 9 itemsa (e.g., Your director inspires others with plans for facility’s future.) |
| Program typeb | ||
| Outpatient | 61.30 | Primarily outpatient services |
| Methadone | 4.21 | Primarily methadone maintenance services |
| Residential | 34.46 | Primarily residential services |
| Referral sourceb | ||
| Self | 4.38 | Self-referred |
| Community | 17.46 | Referred by community-based organization |
| Proposition 36 | 13.14 | Referred by court via Proposition 36 in lieu of incarceration |
| Drug court | 5.99 | Referred by drug court |
| Social services | 20.03 | Referred by social services or county agency |
| Client characteristics | ||
| HIV-tested | 51.55 | Tested for HIV in past |
| Medi-Cal eligible | 42.88 | Eligible for Medi-Cal |
| Race/ethnicity | ||
| White | 30.71 | Self-identified as White |
| Black | 21.17 | Self-identified as Black |
| Latino | 42.80 | Self-identified as Latino |
| Other | 5.32 | Self-identified as Asian or other |
| History of mental health issues | 24.74 | Diagnosed with mental health issue in past |
| Homeless | 16.23 | Unstable housing status |
Note. EBP = evidence-based practice; TJC = the Joint Commission.
Ranges from 10 = not at all to 40 = often.
Client-reported characteristics.
Data Analysis
We used Stata/SE version 12 (StataCorp LP, College Station, TX) to conduct all analyses. We used multiple imputation to fill in missing values because data were assumed to be missing at random.55 This assumption was supported by showing that the probability of having a missing value for a main explanatory variable was not associated with the 3 dependent variables, as suggested by experts on modeling missing data.56 We replaced each missing value with 20 plausible values by using the Markov Chain Monte Carlo method.57 We conducted imputation for program variables and client variables independently. The highest rate of missing data for any variable in the sample was approximately 8%. We developed, merged, and analyzed 20 imputed data sets with Stata’s MI IMPUTE and MI ESTIMATE commands.
We also relied on Stata to conduct multilevel logistic regression analyses using MI ESTIMATE: LOGIT with a log link function for dichotomous outcomes (e.g., programs with high mental and public health collaboration). We analyzed the continuous outcome, percentage of clients tested for HIV, by using MI ESTIMATE: REGRESSION. We analyzed these regressions by using the CLUSTER command to account for the multilevel structure of the data (clients nested in facilities) and to obtain more accurate estimates of standard errors58 as suggested in other research on multilevel program and client disparities.3,59 The intraclass correlation between client and program measures was statistically significant (r > 0.18; P < .01) and justified consideration of both in the analysis. However, programs served as the unit of analysis.
RESULTS
Results from 3 regression analyses, 1 per outcome, are presented in Table 2. Findings provided partial support for hypothesis 1, which posited that percentage of public funding, state license, and professional accreditation would be positively associated with coordination with mental and public health care providers and the percentage of clients receiving HIV testing. Programs accredited by the Joint Commission were more likely to coordinate with mental health services (odds ratio [OR] = 7.664; 95% confidence interval [CI] = 1.490, 9.423), representing the largest positive effect in the study. In addition, clients in programs with more public funding were more likely to be tested for HIV (B = 1.002; P < .001).
TABLE 2.
Logistic and Ordinary Least Squares Regressions on Coordination With Mental Health, Public Health, and HIV Testing Services in Addiction Health Services, Los Angeles County, California, 2010-2011
| Mental Health |
Public Health |
HIV Testing |
||||
|---|---|---|---|---|---|---|
| independent Variables | OR (95% CI) | SE | OR (95% CI) | SE | B (95% CI) | SE |
| Program characteristics | ||||||
| Public funding | 1.004 (0.990, 1.019) | 0.007 | 0.990 (0.975, 1.005) | 0.008 | 1.002*** (1.001, 1.003) | 0.001 |
| State license | 3.648 (0.115, 115.530) | 6.432 | 0.894 (0.046, 17.357) | 1.353 | 1.004 (0.790, 1.277) | 0.122 |
| TJC accreditation | 7.664** (1.490, 9.423) | 6.404 | 0.477 (0.078, 2.901) | 0.439 | 1.057 (0.931, 1.201) | 0.068 |
| Medi-Cal acceptance | 1.146 (0.290, 4.534) | 0.804 | 1.305* (1.001, 1.521) | 0.113 | 1.012 (0.884, 1.159) | 0.069 |
| Readiness for change | ||||||
| Motivational readiness | 1.163** (1.037, 1.305) | 0.068 | 1.136* (1.001, 1.306) | 0.081 | 1.007 (0.995, 1.019) | 0.006 |
| Resources | 0.872 (0.726, 1.048) | 0.082 | 0.847 (0.687, 1.045) | 0.090 | 1.012* (1.001, 1.033) | 0.008 |
| Staff attributes | 1.078 (0.870, 1.334) | 0.118 | 0.946 (0.759, 1.181) | 0.107 | 0.994 (0.978, 1.011) | 0.008 |
| Organizational climate | 1.518*** (1.153, 1.999) | 0.213 | 1.364*** (1.087, 1.710) | 0.158 | 1.003 (0.980, 1.026) | 0.012 |
| Directorial leadership | 0.983 (0.846, 1.143) | 0.075 | 1.030 (0.881, 1.203) | 0.082 | 0.995 (0.980, 1.010) | 0.007 |
| Program typea | ||||||
| Methadone | 0.012*** (0.001, 0.119) | 0.014 | 1.769 (0.234, 7.122) | 1.128 | 1.384** (1.072, 1.786) | 0.178 |
| Residential | 1.624 (0.407, 6.482) | 1.147 | 1.880 (0.476, 7.427) | 1.318 | 1.103* (1.002, 1.224) | 0.058 |
| Referral sourceb | ||||||
| Community | 1.343 (0.426, 4.233) | 0.787 | 1.668 (0.710, 3.922) | 0.728 | 0.962 (0.902, 1.025) | 0.031 |
| Proposition 36 | 1.542 (0.642, 3.705) | 0.690 | 1.316 (0.537, 3.227) | 0.602 | 0.974 (0.906, 1.046) | 0.035 |
| Drug court | 0.846 (0.376, 1.904) | 0.350 | 3.121*** (1.388, 7.015) | 1.290 | 1.035 (0.917, 1.169) | 0.063 |
| Social services | 1.011 (0.522, 1.958) | 0.341 | 1.323 (0.709, 2.467) | 0.421 | 0.998 (0.950, 1.049) | 0.025 |
| Client characteristics | ||||||
| HiV-tested | … | … | … | … | 1.013 (0.967, 1.062) | 0.024 |
| Medi-Cal eligible | 0.900 (0.391, 2.072) | 0.383 | 2.465* (1.002, 6.497) | 1.219 | 1.036 (0.943, 1.138) | 0.049 |
| Race/ethnicityc | ||||||
| Black | 0.986 (0.510, 1.905) | 0.331 | 0.901 (0.438, 1.852) | 0.331 | 1.011 (0.950, 1.076) | 0.032 |
| Latino | 0.941 (0.585, 1.514) | 0.228 | 1.009 (0.617, 1.649) | 0.253 | 1.016 (0.975, 1.058) | 0.021 |
| Other | 1.070 (0.729, 1.571) | 0.210 | 0.991 (0.677, 1.450) | 0.192 | 1.011 (0.970, 1.052) | 0.021 |
| History of mental health issues | 1.806 (0.699, 4.665) | 0.874 | 1.617 (0.788, 3.318) | 0.593 | 0.980 (0.934, 1.029) | 0.024 |
| Homeless | 1.096 (0.699, 1.719) | 0.252 | 1.568 (0.826, 2.979) | 0.513 | 1.051* (1.001, 1.109) | 0.028 |
| Constant | 0.001*** (0.001, 0.001) | 0.001 | 0.001* (0.001, 2.713) | 0.001 | 2.317** (1.095, 4.904) | 0.876 |
Note. CI = confidence interval; OR = odds ratio; TJC = the Joint Commission. Program observations n = 104; client observations n = 14 379.
Outpatient is the reference category.
Self-referral is the reference category.
White is the reference category.
P < .05;
P < .01;
P < .001.
Findings provided partial support for hypothesis 2. Motivational readiness was associated with increased odds of coordination with both mental health (OR = 1.163; 95% CI = 1.037, 1.305) and public health services (OR = 1.136; 95% CI = 1.001, 1.306). In addition, organizational climate was associated with increased odds of coordination with mental health (OR = 1.518; 95% CI = 1.153, 1.999) and public health services (OR = 1.364; 95% CI = 1.087, 1.710). Finally, organizational resources were positively associated with the percentage of clients who received HIV testing services (B = 1.012; P < .05).
Findings provided no support for hypothesis 3, which posited that director’s leadership would be positively associated with coordination of mental and public health care and the percentage of clients receiving HIV testing. However, we found strong and statistically significant relationships among relevant control variables. Clients referred by drug court (OR = 3.121; 95% CI = 1.388, 7.015) and those eligible for Medi-Cal (OR = 2.465; 95% CI = 1.002, 6.497) reported the largest effects in terms of coordination with public health services. Finally, methadone-based (B = 1.384; P < .001) and residential (B = 1.103; P < .05) treatment programs, compared with outpatient providers, were associated with a higher percentage of clients tested for HIV.
DISCUSSION
We examined the impact of program and client characteristics on coordination of AHS providers with mental health, public health, and HIV testing services. We found that components of program capacity for change in service delivery such as public funding, professional accreditation, and organizational readiness for change play a significant role in the coordination of mental health, public health, and HIV testing in community-based AHS programs in Los Angeles County. In these relatively small community-based programs, external incentives from professional regulation and public funding sources were associated with greater service delivery capacity. This is consistent with other addiction treatment studies.30,33,38,39,60 Public funding and professional accreditation generally provided community-based AHS programs with the necessary financial resources, professional incentives, and guidance to respond to the multiple service needs of clients suffering from co-occurring conditions. However, it is important to note that the only significant relationship between public funding and service coordination was related to HIV testing and the effect size was small. This suggests that other more malleable factors may have more influence on service coordination.
Programs with higher motivational readiness and an organizational climate supportive of change were more likely to coordinate with mental health and public health care. This finding suggests that intervening to improve program readiness and a climate for change may be a fruitful direction for future work. For example, research has shown that organizational climates focused on a specific strategic imperative (e.g., safety, customer service) can improve the targeted outcomes.61–63 Such an approach could be applied to improve numerous outcomes in AHS, including coordination with mental health, public health, and HIV services.
Although director’s leadership was not significantly associated with any of the outcomes, we believe leaders can have a direct influence on developing motivation and a climate of change in organizations and service teams. The literature on leadership in behavioral health has suggested that upper-level managers initiate, promote, and help sustain staffing and service delivery changes.46,64–66 However, analysis of leadership may need to focus on more involved practices (e.g., task-oriented leadership vs transformational leadership) to be relevant to initiating and implementing service integration changes. Regardless, these findings highlight the need for leaders to invest in staff attitudes and a work environment that enables change to better coordinate mental and public health care in community-based AHS.
In addition, coordination of integrated care differed across program type, referral source, and Medicaid eligibility. Compared with out-patient providers, methadone programs were less likely to collaborate with mental health services. Methadone programs in this sample reported fewer resources (funding and services) than regular outpatient programs and thus are less able to establish high coordination of care with mental health agencies. By contrast, HIV testing was more likely in methadone and residential programs and more frequently offered to homeless individuals. Compared with regular outpatient, HIV testing is less controversial in methadone programs, and considering the high risk among drug-injecting individuals, funding and regulatory institutions have invested in providing HIV testing in this setting.
In addition, compared with self-referrals, referrals from drug court were related to programs reporting high coordination with public health services. Collaboration with public health services was also more likely in programs that accepted Medicaid insurance and those with more Medicaid-eligible clients. Overall, these findings underscore the importance of external and internal program capacity factors to deliver integrated care in outpatient AHS programs. Because more than 70% of admissions to AHS involve community-based outpatient care,67 these outpatient programs are key allies to identify, prevent, and treat co-occurring mental and physical health conditions in racial and ethnic minority communities.
Findings also have important implications for delivering integrated care in the current era of health care reform. As the Affordable Care Act expands public insurance to more low-income individuals and promotes community-based prevention and integrated care, AHS organizations represent critical intervention points for the diagnosis and treatment of co-occurring substance abuse and mental and physical health conditions. Small AHS organizations located in minority communities can improve standards of care for clients with dual disorders if they develop an effective system of collaboration and increased coordination to address priorities, such as reducing the spread of HIV and addressing the harmful effects of co-occurring disorders.68,69
Limitations
Some limitations of the present study should be noted. First, all measures were cross-sectional, preventing us from establishing causality. However, the large multilevel sample offered robust estimates. Future prospective studies should be conducted to explore causality as a function of policy, system, and organizational change. Second, control measures of client history of mental health and HIV testing likely underreported actual prevalence of these variables. However, we mitigated this concern by using auxiliary variables such as use of psychiatric medication, hospitalization, and sexual risk behaviors to support validity and improve modeling of mental health status and HIV testing. Another limitation was the potential for social desirability associated with supervisors reporting on program characteristics. To address this concern, we corroborated supervisor responses with program materials (e.g., marketing of integrated care) and verified the reliability and consistency of data with counselors during site visits. We did not include 14 programs because of significant inconsistencies among responses by supervisors and counselors.
Finally, our analyses only allowed us to generalize findings about service delivery to our sampling frame and not to other service systems. Nonetheless, this issue was somewhat mitigated by our large sample of 104 publicly funded AHS programs serving communities with a population of 40% or more Latino or African American residents, representing approximately 7.7 million residents in Los Angeles County.
Conclusions
This study demonstrates the importance of both external and internal program factors in the expansion of service delivery in AHS and the role these factors play in coordinating the delivery of mental health, public health, and HIV testing services in low-income, predominately ethnic-minority communities. Different forms of support are necessary to integrate services. It remains to be seen whether Affordable Care Act–related changes, from the expansion of Medicaid and increased regulation to implementation of preventive care, facilitate increased coordination of HIV testing and public health practices among AHS programs.
The results of this study also raise questions regarding at what level officials should intervene to improve coordination of care. In frameworks and approaches to implementation of change, it is important to consider not only various external factors (e.g., structures, processes) in terms of policy and interorganizational networks, but also the interplay of factors in the inner organizational context (e.g., motivational readiness) that may be more or less amenable to change.60,70 For example, in the external context, coordination improvement strategies might include building referral or data-sharing systems to facilitate coordination across service systems.71 In the inner context of individual programs, developing strategic imperatives and performance targets focused on coordination of care may help communicate to staff the importance of facilitating care coordination to permit greater client access to a broader array of services.
These findings are also important for health care management policy that seeks to empower leaders of community-based health organization to motivate staff change and promote a climate of service integration that leads to increased coordination with community providers and greater access to integrated care in low-income minority communities. System and organization leaders must consider and develop practical solutions to enhance the mission of improving care across systems and organizations to meet the complex public health needs of diverse individuals. This approach has the potential to increase the cost-effectiveness of integrated care and decrease health disparities in ethnic-minority communities.
Acknowledgments
Funding for this study was provided by the National Institute on Drug Abuse (R21DA035634-01) and the Hamovitch Center for Science in the Human Services at the School of Social Work, University of Southern California.
We thank Director John Viernes, Ben Lee, and Tina Kim and her research staff at Los Angeles County, Substance Abuse Prevention and Control, who kindly provided the client data necessary for our analysis, as well as feedback on the final draft. We also appreciate all treatment providers who kindly provided the program data for our study. Finally, we thank Eric Lindberg, who assisted with the preparation and proofreading of the article.
Note. The National Institute on Drug Abuse and the Hamovitch Center for Science in the Human Services at the School of Social Work, University of Southern California, had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the article; nor in the decision to submit the article for publication.
Footnotes
Contributors E. G. Guerrero reviewed the research literature, framed the scope of the article, provided primary statistical analyses, and was the primary text author. G. A. Aarons provided additional literature review, critical review, and support in writing the article, including revisions. L. A. Palinkas provided critical review and support for all revisions. All authors reviewed and approved the final draft.
Human Participant Protection The institutional review board at University of Southern California approved the study, and all participants gave informed consent.
Contributor Information
Erick G. Guerrero, School of Social Work, University of Southern California, Los Angeles.
Gregory A. Aarons, Department of Psychiatry, University of California, San Diego.
Lawrence A. Palinkas, School of Social Work, University of Southern California, Los Angeles.
References
- 1.Alegría M, Page JB, Hansen H, et al. Improving drug treatment services for Hispanics: research gaps and scientific opportunities. Drug Alcohol Depend. 2006;84(suppl 1):S76–S84. doi: 10.1016/j.drugalcdep.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Amaro H, Arévalo S, Gonzalez G, Szapocznik J, Iguchi MY. Needs and scientific opportunities for research on substance abuse treatment among Hispanic adults. Drug Alcohol Depend. 2006;84(suppl 1):S64–S75. doi: 10.1016/j.drugalcdep.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Marsh JC, Cao D, Guerrero E, Shin HC. Need–service matching in substance abuse treatment: racial/ethnic differences. Eval Program Plann. 2009;32(1):43–51. doi: 10.1016/j.evalprogplan.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butler M, Kane RL, McAlpine D, et al. Integration of Mental Health/Substance Abuse and Primary Care. Agency for Healthcare Research and Quality; Rockville, MD: 2008. AHRQ publication 09-E003. [Google Scholar]
- 5.Chalk M, Dilonardo J, Rinaldo SG, Oehlmann P. Integrating Appropriate Services for Substance Use Conditions in Health Care Settings: An Issue Brief on Lessons Learned and Challenges Ahead. Treatment Research Institute; Philadelphia, PA: 2010. [Google Scholar]
- 6.Grella CE, Stein JA, Weisner C, Chi F, Moos R. Predictors of longitudinal substance use and mental health outcomes for patients in two integrated service delivery systems. Drug Alcohol Depend. 2010;110(1-2):92–100. doi: 10.1016/j.drugalcdep.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. JAMA. 2001;286(14):1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grella CE, Gilmore J. Improving service delivery to the dually diagnosed in Los Angeles County. J Subst Abuse Treat. 2002;23(2):115–122. doi: 10.1016/s0740-5472(02)00254-4. [DOI] [PubMed] [Google Scholar]
- 9.Rawson R, McLellan T. Health reform and treatment changes in organization, financing, and standards of care. Presented orally at: Los Angeles County Public Health Department; Los Angeles, CA. February 15, 2010. [Google Scholar]
- 10.Grella CE, Gil-Rivas V, Cooper L. Perceptions of mental health and substance abuse program administrators and staff on service delivery to persons with co-occurring substance abuse and mental health disorders. J Behav Health Serv Res. 2004;31(1):38–49. doi: 10.1007/BF02287337. [DOI] [PubMed] [Google Scholar]
- 11.McGovern MP. [Accessed June 12, 2011];Overview of substance abuse and co-occurring disorders. 2010 Available at: http://www.saprp.org/knowledgeassets/Knowledge_detail.cfm?KAID=12.
- 12.Chalk M. Healthcare reform and treatment: changes in organization, financing, and standards of care. Presented orally at: Quarterly Meeting of the County Alcohol and Drug Program Administrators Association of California; Sacramento, CA. January 16, 2010. [Google Scholar]
- 13.Andrulis DP, Siddiqui NJ, Purtle JP, Duchon L. Patient Protection and Affordable Care Act of 2010: Advancing Health Equity for Racially and Ethnically Diverse Populations. Joint Center for Political and Economic Studies; Washington, DC: 2010. [Google Scholar]
- 14.Jarvis D. [Accessed June 12, 2011];Paying for integrated services: FQHC, Medi-Cal and other funding strategies. 2010 Available at: http://www.uclaisap.org/affordable-care-act/assets/documents/health%20care%20reform/Financing/Paying%20for%20Integrated%20Services-%20FQHC,%20Medi-Cal%20and%20other%20Funding%20Strategies.pdf.
- 15.Lehman WEK, Fletcher BW, Wexler HK, Melnick G. Organizational factors and collaboration and integration activities in criminal justice and drug abuse treatment agencies. Drug Alcohol Depend. 2009;103(suppl 1):S65–S72. doi: 10.1016/j.drugalcdep.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Burt MR, Resnick G, Matheson N. Comprehensive Service Integration Programs for At-Risk Youth. Urban Institute; Washington, DC: 1992. [Google Scholar]
- 17.Kusserow RP. Services Integration: A Twenty-Year Retrospective. Office of Inspector General; Washington, DC: 1991. [Google Scholar]
- 18.Taxman FS, Bouffard JA. The importance of systems in improving offender outcomes: new frontiers in treatment integrity. Justice Res Policy. 2000;2(2):37–58. [Google Scholar]
- 19.Axelsson R, Axelsson SB. Integration and collaboration in public health: a conceptual framework. Int J Health Plann Manage. 2006;21(1):75–88. doi: 10.1002/hpm.826. [DOI] [PubMed] [Google Scholar]
- 20.Banaszak-Holl J, Allen S, Mor V, Schott T. Organizational characteristics associated with agency position in community care networks. J Health Soc Behav. 1998;39(4):368–385. [PubMed] [Google Scholar]
- 21.Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Q. 2001;79(2):179–205. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fletcher B, Lehman W, Wexler H, Melnick G, Taxman F, Young D. Measuring collaboration and integration activities in criminal justice and substance abuse treatment agencies. Drug Alcohol Depend. 2009;103(suppl 1):S54–S64. doi: 10.1016/j.drugalcdep.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Turner S, Longshore D, Wenzel S, et al. A decade of drug treatment court research. Subst Use Misuse. 2002;37(12-13):1489–1527. doi: 10.1081/ja-120014420. [DOI] [PubMed] [Google Scholar]
- 24.Rapp CA, Goscha RJ. The principles of effective case management of mental health services. Psychiatr Rehabil J. 2004;27(4):319–333. doi: 10.2975/27.2004.319.333. [DOI] [PubMed] [Google Scholar]
- 25.Grudzinskas AJ, Clayfield JC, Roy-Bujnowski K, Fisher WH, Richardson MH. Integrating the criminal justice system into mental health service delivery: the Worcester Diversion experience. Behav Sci Law. 2005;23(2):277–293. doi: 10.1002/bsl.648. [DOI] [PubMed] [Google Scholar]
- 26.Steadman HJ. Boundary spanners: a key component for the effective interactions of the justice and mental health systems. Law Hum Behav. 1992;16(1):75–87. [Google Scholar]
- 27.McGovern MP, Matzkin AL, Giard J. Assessing the dual diagnosis capability of addiction treatment services: the Dual Diagnosis Capability in Addiction Treatment (DDCAT) index. J Dual Diagn. 2007;3(2):111–123. [Google Scholar]
- 28.McGovern MP, Becker K, Lambert-Harris C, Acquilano S, Matzkin A, Giard J. The dual diagnosis capability in addiction treatment (DDCAT) index: a six state collaborative to enhance policy and implement evidence based practices for persons with co-occurring disorders. Paper presented orally at: Substance Abuse Policy Research Program Annual Grantee Meeting; Amelia Island, FL. June 20, 2008. [Google Scholar]
- 29.Guerrero EG, Cederbaum JA. Adoption and utilization of sexually transmitted infections testing in outpatient substance abuse treatment facilities serving high risk populations in the US. Int J Drug Policy. 2011;22(1):41–48. doi: 10.1016/j.drugpo.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pollack HA, D’Aunno T, Lamar B. Outpatient substance abuse treatment and HIV prevention: an update. J Subst Abuse Treat. 2006;30(1):39–47. doi: 10.1016/j.jsat.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 31.Drake RE, Essock SM, Shaner A, et al. Implementing dual diagnosis services for clients with severe mental illness. Psychiatr Serv. 2001;52(4):469–476. doi: 10.1176/appi.ps.52.4.469. [DOI] [PubMed] [Google Scholar]
- 32.Roman PM, Ducharme LJ, Knudsen HK. Patterns of organization and management in private and public substance abuse treatment programs. J Subst Abuse Treat. 2006;31(3):235–243. doi: 10.1016/j.jsat.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 33.D’Aunno T, Vaughn TE, McElroy P. An institutional analysis of HIV prevention efforts by the nation’s out-patient drug abuse treatment units. J Health Soc Behav. 1999;40(2):175–192. [PubMed] [Google Scholar]
- 34.Campbell CI, Alexander JA, Lemak CH. Organizational determinants of outpatient substance abuse treatment duration in women. J Subst Abuse Treat. 2009;37(1):64–72. doi: 10.1016/j.jsat.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ducharme LJ, Mello HL, Roman PM, Knudsen HK, Johnson JA. Service delivery in substance abuse treatment: re-examining “comprehensive” care. J Behav Health Serv Res. 2007;34(2):121–136. doi: 10.1007/s11414-007-9061-7. [DOI] [PubMed] [Google Scholar]
- 36.Durkin EM. An organizational analysis of psychosocial and medical services in outpatient drug abuse treatment programs. Soc Serv Rev. 2002;76(3):406–429. [Google Scholar]
- 37.Chriqui JF, Terry-McElrath Y, McBride DC, Eidson SS. State policies matter: the case of outpatient drug treatment program practices. J Subst Abuse Treat. 2008;35(1):13–21. doi: 10.1016/j.jsat.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 38.D’Aunno T, Pollack HA. Changes in methadone treatment practices: results from a national panel study, 1988–2000. JAMA. 2002;288(7):850–856. doi: 10.1001/jama.288.7.850. [DOI] [PubMed] [Google Scholar]
- 39.D’Aunno T. The role of organization and management in substance abuse treatment: review and roadmap. J Subst Abuse Treat. 2006;31(3):221–233. doi: 10.1016/j.jsat.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 40.Office of Applied Studies . Substance Abuse Treatment Facilities Provide Programs to Fit Clients. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2007. [Google Scholar]
- 41.McLellan AT, Carise D, Kleber HD. Can the national addiction treatment infrastructure support the public’s demand for quality care? J Subst Abuse Treat. 2003;25(2):117–121. [PubMed] [Google Scholar]
- 42.Shortell SM. Increasing value: a research agenda for addressing the managerial and organizational challenges facing health care delivery in the United States. Med Care Res Rev. 2004;61(3 suppl):12S–30S. doi: 10.1177/1077558704266768. [DOI] [PubMed] [Google Scholar]
- 43.Simpson DD, Flynn PM. Moving innovations into treatment: a stage-based approach to program change. J Subst Abuse Treat. 2007;33(2):111–120. doi: 10.1016/j.jsat.2006.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lehman WEK, Greener JM, Simpson DD. Assessing organizational readiness for change. J Subst Abuse Treat. 2002;22(4):197–209. doi: 10.1016/s0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- 45.Broome KM, Flynn PM, Knight DK, Simpson DD. Program structure, staff perceptions, and client engagement in treatment. J Subst Abuse Treat. 2007;33(2):149–158. doi: 10.1016/j.jsat.2006.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fuller BE, Rieckmann T, Nunes EV, et al. Organizational readiness for change and opinions toward treatment innovations. J Subst Abuse Treat. 2007;33(2):183–192. doi: 10.1016/j.jsat.2006.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gotham HJ, Claus RE, Selig K, Homer AL. Increasing program capability to provide treatment for co-occurring substance use and mental disorders: organizational characteristics. J Subst Abuse Treat. 2010;38(2):160–169. doi: 10.1016/j.jsat.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 48.Guerrero EG. Managerial capacity and adoption of culturally competent practices in outpatient substance abuse treatment organizations. J Subst Abuse Treat. 2010;39(4):329–339. doi: 10.1016/j.jsat.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guerrero E, Andrews CM. Cultural competence in outpatient substance abuse treatment: measurement and relationship to wait time and retention. Drug Alcohol Depend. 2011;119(1-2):e13–e22. doi: 10.1016/j.drugalcdep.2011.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Avolio BJ, Bass BM, Jung DI. Re-examining the components of transformational and transactional leadership using the Multifactor Leadership Questionnaire. J Occup Organ Psychol. 1999;72(4):441–462. [Google Scholar]
- 51.Edwards JR, Knight DK, Broome KM, Flynn PM. The development and validation of a transformational leadership survey for substance use treatment programs. Subst Use Misuse. 2010;45(9):1279–1302. doi: 10.3109/10826081003682834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guerrero EG. Enhancing access and retention in substance abuse treatment: the role of Medicaid payment acceptance and cultural competence. Drug Alcohol Depend. 2013 doi: 10.1016/j.drugalcdep.2013.04.005. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 53.Office of Applied Studies . The TEDS Report: Predictors of Substance Abuse Treatment Completion or Transfer to Further Treatment, by Service Type. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. [Google Scholar]
- 54.Guerrero E. Organizational characteristics that foster early adoption of cultural and linguistic competence in outpatient substance abuse treatment in the United States. Eval Program Plann. 2012;35(1):9–15. doi: 10.1016/j.evalprogplan.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rubin DB. Multiple Imputation for Non-Response in Surveys. John Wiley & Sons; New York, NY: 1987. [Google Scholar]
- 56.Allison PD. Missing Data. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- 57.Shafer JL. Analysis of Incomplete Multivariate Data. Chapman & Hall/CRC; Boca Raton, FL: 1997. [Google Scholar]
- 58.Blakely TA, Woodward AJ. Ecological effects in multi-level studies. J Epidemiol Community Health. 2000;54(5):367–374. doi: 10.1136/jech.54.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guerrero EG, Marsh JC, Duan L, Oh C, Perron BE, Lee B. Disparities in completion of substance abuse treatment between and within racial and ethnic groups. Health Serv Res. 2013;48(4):1450–1467. doi: 10.1111/1475-6773.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wells R, Lemak CH, D’Aunno TA. Insights from a national survey into why substance abuse treatment units add prevention and outreach services. Subst Abuse Treat Prev Policy. 2006;1:21. doi: 10.1186/1747-597X-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aarons GA, Horowitz J, Dlugosz L, Ehrhart M. The role of organizational process in dissemination and implementation research. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. Oxford University Press; New York, NY: 2012. pp. 128–153. [Google Scholar]
- 62.Zohar D. Safety climate in industrial organizations: theoretical and applied implications. J Appl Psychol. 1980;65(1):96–102. [PubMed] [Google Scholar]
- 63.Zohar D. Modifying supervisory practices to improve subunit safety: a leadership-based intervention model. J Appl Psychol. 2002;87(1):156–163. doi: 10.1037/0021-9010.87.1.156. [DOI] [PubMed] [Google Scholar]
- 64.Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health. 2011;38(1):4–23. doi: 10.1007/s10488-010-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Friedmann PD, Jiang L, Alexander JA. Top manager effects on buprenorphine adoption in outpatient substance abuse treatment programs. J Behav Health Serv Res. 2010;37(3):322–337. doi: 10.1007/s11414-009-9169-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guerrero EG. Workforce diversity in outpatient substance abuse treatment: the role of leaders’ characteristics. J Subst Abuse Treat. 2013;44(2):208–215. doi: 10.1016/j.jsat.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Office of Applied Studies [Accessed December 7, 2009];Results From the 2008 National Survey on Drug Use and Health: National Findings. 2009 Available at: http://www.oas.samhsa.gov/nsduh/2k8nsduh/2k8Results.cfm.
- 68.US Preventive Services Task Force Behavioral counseling to prevent sexually transmitted infections: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(7):491–496. doi: 10.7326/0003-4819-149-7-200810070-00010. [DOI] [PubMed] [Google Scholar]
- 69.Guerrero EG, Cepeda A, Duan L, Kim T. Disparities in completion of substance abuse treatment completion among Latino subgroups in Los Angeles County, CA. Addict Behav. 2012;37(10):1162–1166. doi: 10.1016/j.addbeh.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 70.Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q. 2001;79(2):281–315. doi: 10.1111/1468-0009.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hurlburt MS, Leslie LK, Landsverk J, et al. Contextual predictors of mental health service use among children open to child welfare. Arch Gen Psychiatry. 2004;61(12):1217–1224. doi: 10.1001/archpsyc.61.12.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]