Abstract
Objectives
We compared admission rates, outcomes, and performance of the CURB-65 mortality prediction score of homeless patients and nonhomeless patients with community-acquired pneumonia (CAP).
Methods
We compared homeless (n = 172) and nonhomeless (n = 1897) patients presenting to a Salt Lake City, Utah, emergency department with CAP from 1996 to 2006. In the homeless cohort, we measured referral from and follow-up with the local homeless health care clinic and arrangement of medical housing.
Results
Homeless patients were younger (44 vs 59 years; P < .001) and had lower CURB-65 scores and higher hospitalization risk (severity-adjusted odds ratio = 1.89; 95% confidence interval = 1.33, 2.69) than did nonhomeless patients and a similar length of stay, median inpatient cost, and median outpatient cost, even after severity adjustment. Of homeless patients, 22% were referred from the homeless health care clinic to the emergency department; 54% of outpatients and 51% of hospital patients were referred back to the clinic, and medical housing was arranged for 23%.
Conclusions
A large cohort of homeless patients with CAP demonstrated higher hospitalization risk than but similar length of stay and costs as nonhomeless patients. The strong relationship between the hospital and homeless health care clinic may have contributed to this finding. (Am J Public Health. Published online ahead of print October 22, 2013: e1-e5. doi:10.2105/AJPH.2013.301342)
Community-acquired pneumonia (CAP) is the most common infectious cause of death in the developed world1 and a frequent cause of death in homeless populations, even in younger age groups.2,3 Determining the most appropriate site of care is a major decision in the management of pneumonia and depends on estimated severity.4 Mortality prediction tools such as the Pneumonia Severity Index5 and the CURB-656 can guide clinicians in the triage of CAP patients.
The CURB-65 estimates 30-day mortality on the basis of new-onset confusion, uremia (blood urea nitrogen ‡ 20 mg/dL), respiratory rate (> 30 breaths/min), systolic blood pressure (< 90 mm Hg) or diastolic blood pressure (< 60 mm Hg), and age (‡ 65 years); contains objective features available in the electronic medical record (EMR); and is simple to calculate. However, the utility of traditional severity assessment for the management of homeless populations is unclear. A previous study of CAP at a public hospital found a high rate of admission despite low severity scores, citing homelessness, mental illness, and substance abuse as reasons for admission not captured in traditional pneumonia mortality prediction.7 Patients experiencing homelessness or lower socioeconomic status have typically demon-strated higher rates of acute admissions and longer hospitalizations.8,9 For homeless individuals, locally available case management and medical housing after discharge may reduce length and costs of hospitalizations.10
We compared rates of hospital admission and outcomes of a large cohort of homeless patients with those of nonhomeless patients seen in the emergency department (ED) with CAP. We also assessed the accuracy of CURB-65 in predicting 30-day mortality and hospital admission in homeless patients versus nonhomeless patients. In the homeless cohort, we performed a manual chart review to evaluate the rate of involvement with the local homeless clinic, including referral to and from the ED and use of the community medical housing network. We also evaluated relationships between cost of hospital inpatient care and involvement with the local homeless clinic.
METHODS
The study was performed at LDS Hospital, a university-affiliated community teaching hospital in Salt Lake City, Utah, with 520 total beds. During the study period, LDS served as the primary referral hospital for the Fourth Street Clinic, a nonprofit community health center that provides ambulatory care services to approximately 5000 homeless individuals in Salt Lake City annually. Fourth Street Clinic is a federally qualified health center and is the only health-care-for-homeless grantee from the Health Resources and Services Administration’s Bureau of Primary Health Care in the Salt Lake City area. To meet the needs of homeless patients with acute illnesses, the Fourth Street Clinic Respite Program provides medical housing through a shelter-based day bed program, temporary emergency motel housing, tuberculosis housing, or nursing home services.11
Study Population
Our methodology of patient selection has previously been described.12 Briefly, we electronically identified patients older than 18 years evaluated in the ED at LDS Hospital from 1996 to 2006 with International Classification of Diseases, Ninth Revision13 codes specific to a primary diagnosis of pneumonia (480---487.5) or with respiratory failure or sepsis asthe primary diagnosis with pneumonia as a secondary diagnosis. We excluded patients diagnosed with aspiration pneumonia, immune-compromised conditions including AIDS or HIV with receipt of antiretroviral therapy, solid organ transplants, and hematologic malignancies and those meeting criteria for health care---associated pneumonia.4 We manually reviewed all initial chest x-ray and computerized tomography reports and excluded patients lacking radiographic evidence of pneumonia.
Homeless individuals were identified by a computer search on the term “homeless” in all hospital admission and ED reports and by electronic screening for home addresses matching all shelters in the community and LDS Hospital. We then confirmed homelessness by manual review of initially screened charts; homeless individuals were identified as those indicated in the medical chart to be lacking fixed or adequate nighttime housing, including those residing in shelters, in emergency housing, or on the street.14
Manual Chart Review of Homeless Population
For all patients identified as homeless, we performed a manual chart review of dictated ED reports, admission history and physicals, and hospital discharge summaries for the following information: history of chronic obstructive pulmonary disorder or asthma; use of tobacco, alcohol, or illicit substances; and referral from Fourth Street Clinic. We manually reviewed microbiology culture results from blood and respiratory sources. Discharge summaries and ED reports were also reviewed for follow-up at the Fourth Street Clinic or another primary care clinic and arrangement of medical housing.
Electronic Medical Record Data Extraction
As previously described,12 we extracted initial vital signs and orientation status (entered routinely in the EMR during the initial nursing assessment), electrolytes, and complete blood count from the EMR. We measured 30-day all-cause mortality using the Utah Population Database.15 Hospital admission, length of stay (LOS), and cost of care were extracted from the EMR. For all patients initially discharged from the ED, we measured return to the ED and rehospitalization within 7 days; for all patients initially hospitalized, we measured rehospitalization within 30 days.
Analysis
We tested categorical associations by comparing homeless and nonhomeless individuals using the Fisher exact test, and we tested continuous associations with an independent-samples t test or Wilcoxon rank-sum test, as appropriate. We compared receiver operating characteristic curves and P values for the CURB-65. Severity was adjusted for outcomes using eCURB, a continuous, weighted, electronic version of CURB-65 that is more accurate.12 All statistical analyses were performed using the R statistical package version 2.15.1 (http://www.r-project.org; Statistics Department, University of Auckland, New Zealand).
RESULTS
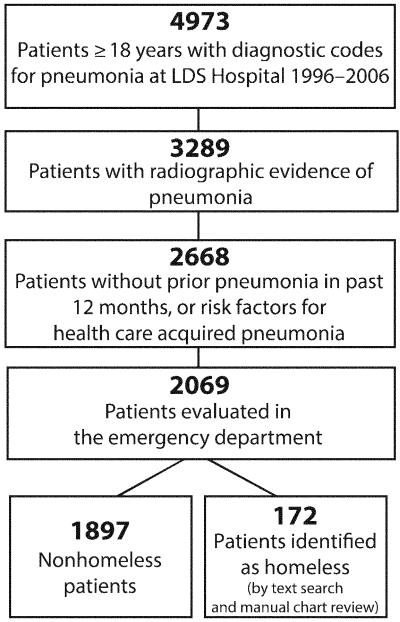
Of 2069 patients evaluated in the ED with CAP, we identified 172 as homeless (Figure 1). Homeless patients were younger and more likely to be uninsured and presented with significantly lower CURB-65 scores than were nonhomeless patients (Table 1). Although the admission rate was similar to that of non-homeless patients (61% vs 58%; P = .42), homeless patients were more likely to be admitted than nonhomeless patients after severity adjustment (odds ratio [OR] = 1.89; 95% confidence interval [CI] = 1.33, 2.69). The median LOS for all patients hospitalized with CAP was 3.0 days; median cost of hospitalization was 7 times that of outpatient management ($3906 vs $554). The LOS, inpatient cost, and outpatient cost were no different for homeless patients compared with nonhomeless patients, even after adjusting for severity.
FIGURE 1. Patient population: Salt Lake City, UT, 1996-2006.
TABLE 1. Patient Characteristics, Admission Decisions, and Outcomes of Community-Acquired Pneumonia in the Homeless and Nonhomeless Population in an Urban Community Hospital: Salt Lake City, UT, 1996-2006.
| Variable | Homeless (n = 172) | Nonhomeless (n = 1897) | P |
|---|---|---|---|
| Age, y, median (95% CI) | 44 (38, 50) | 59 (40, 76) | < .001 |
| Female, % | 22 | 51 | < .001 |
| Minority, % | 34 | 19 | < .001 |
| Uninsured, % | 60 | 16 | < .001 |
| Admission statistics | |||
| % admitted | 61 | 58 | .42 |
| OR (95% CI)a | 1.89 (1.33, 2.69) | 1.00 (Ref) | < .001 |
| ICU, % | 14 | 16 | .57 |
| Patients with empyema, no. (%) | 2(1) | 11 (0.5) | .29 |
| Length of stay,b d, median (95% CI) | 3 (2, 5) | 3 (2, 5) | .99a |
| Readmission rate, % (95% CI) | |||
| 7-dc | 5 (2, 9) | 9 (8, 10) | .06 |
| 30-db | 5.7 (1.9, 12.9) | 4.3 (3.4, 5.3) | >.999 |
| Cost of care, $, median (95% CI) | |||
| Outpatient | 529 (432, 755) | 557 (421, 667) | .72a |
| Inpatient | 3926 (2612, 6581) | 3899 (2754, 6557) | .93a |
| No. patients with CURB-65 score, % (95% CI) | |||
| 0 | 58 (50, 65) | 41 (39, 43) | < .001 |
| ≥3 | 1 (0, 3) | 10 (9, 12) | < .001 |
| CURB-65 of admitted patients, mean (median ±SE) | 0.7 (0.7 ±0.08) | 1.4 (1.4 ±0.03) | < .001 |
| 30-d mortality, % (95% CI) | 2.9% (1.0, 6.7) | 4.3 (3.4, 5.3) | .54 |
Note. CI = confidence interval; ICU = intensive care unit; OR = odds ratio. CURB-65 is a clinical prediction rule used to estimate 30-day mortality for patients with community-acquired pneumonia on the basis of confusion, uremia (blood urea nitrogen ≥ 20 mg/dL), respiratory rate (> 30 breaths/minute), systolic blood pressure (< 90 mm Hg) or diastolic blood pressure (< 60 mm Hg), and age (≥ 65 years).
Adjusted for illness severity using eCURB.
Of hospitalized patients.
Of patients initially managed as outpatients.
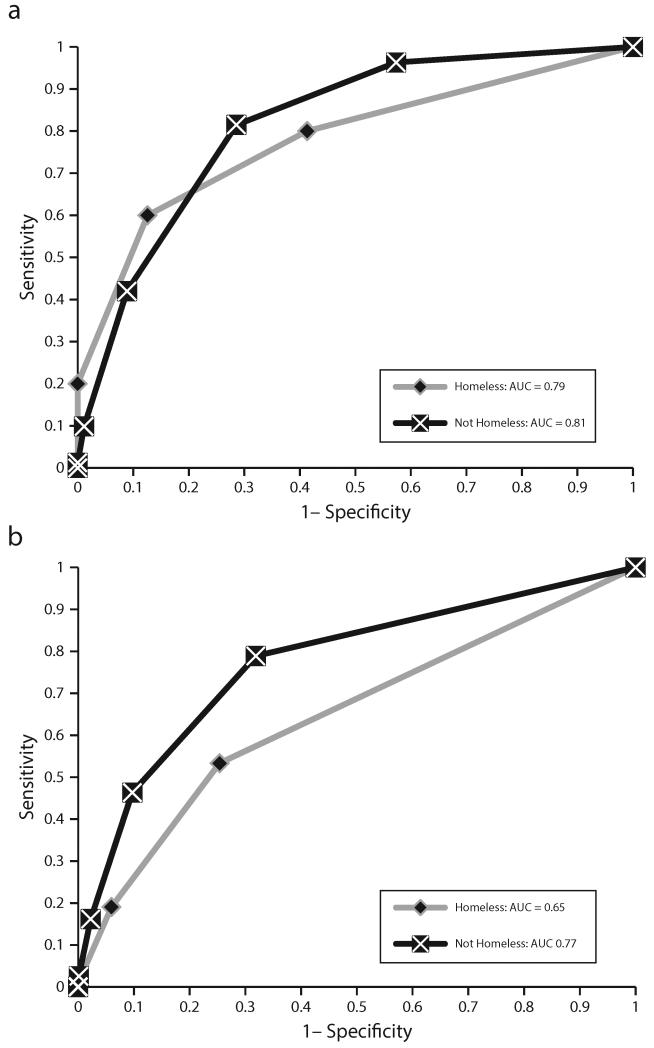
Figure 2 demonstrates receiver operating characteristic curves for the CURB-65 score versus 30-day mortality and admission. We found no difference in CURB-65’s ability to predict 30-day mortality for homeless patients (area under the curve = 0.79 vs 0.81; P = .77). However, CURB-65’s ability to predict hospital admission in the homeless patients was significantly lower (area under the curve = 0.65 vs 0.77; P = .001).
FIGURE 2. Receiver operating characteristic curves for the CURB-65 score vs (a) mortality and (b) admission: Salt Lake City, UT, 1996-2006.
Within the homeless cohort, 72% (n = 124) had a history of tobacco use; 40% (n = 68), ongoing alcohol abuse; 29% (n = 51), illicit substance use; and 23% (n = 40), chronic obstructive pulmonary disorder or asthma. We saw higher rates of admission for patients with ongoing alcohol abuse (87% vs 44%; P < .001), illicit substance use (75% vs 55%; P = .026), and tobacco use (66% vs 48%; P = .028); we found a nonsignificant increase in admission rate for patients with lung disease (68% vs 59%; P = .36). Fourteen percent (n = 24) had a culture-identified pathogen, with 18 patients testing positive for Streptococcus pneumoniae, 3 for Mycobacterium tuberculosis, 2 for methicillin-sensitive Staphylococcus aureus, and 1 for methicillin-resistant S. aureus. After its introduction in January 2000, urinary testing identified Legionella pneumophila in 2.6% of all tested cases (8 of 283); after its introduction in 2003, urinary testing identified pneumococcal pneumonia in 12.5% of tested cases (17 of 136). We found no significant difference in the rate of positive S. pneumoniae or L. pneumophila urinary antigen tests between homeless and nonhomeless individuals, although the study was not powered adequately to rule out a significant difference.
Of all homeless patients, 22% (n = 38) had been referred to the ED from the Fourth StreetClinic. Of outpatients, 54% (36 of 67) were referred to the Fourth Street Clinic for followup, and 51% of inpatients (53 of 105) were referred on discharge. Twenty-four additional patients were referred to clinics other than the Fourth Street Clinic, including the hospital’s internal medicine clinic (n = 18), US Department of Veterans Affairs clinics (n = 2), and specialty clinics (n = 4). Medical housing was arranged for 23% of all patients (34 received housing; 6 placed in nursing facilities); of these patients, 75% (n = 30) followed up at the Fourth Street Clinic. Hospitalized patients were more likely to have medical housing arranged after discharge than were ED patients (29% vs 13%; P = .016) Patients discharged from the ED with follow-up at the Fourth Street Clinic demonstrated significantly lower cost of care than homeless patients not referred (median cost = $483 vs $674; P < .001) with no observed increase in 7-day readmission, 30-day rehospitalization, or mortality. Among hospitalized patients, we found a nonsignificant reduction in hospital LOS for patients with medical housing arranged (median LOS = 2.7 vs 3.1 days; P = .85); we found no significant difference in LOS or cost for patients referred to the Fourth Street Clinic or medical housing.
DISCUSSION
In a large cohort of homeless patients presenting to an ED with CAP, hospitalization risk was higher than among nonhomeless individuals, and traditional severity assessment with the CURB-65 did not predict admission well for homeless individuals compared with non-homeless individuals. These findings are consistent with previous studies in under-served populations,7 suggesting that the admission decision for pneumonia is often influenced by patient characteristics not measured by traditional mortality prediction scores. Homeless patients with ongoing alcohol, illicit substance, and tobacco use demonstrated higher admission rates, suggesting that these features, which are often difficult to measure objectively, contributed to the admission decision. Three patients were also found to have M. tuberculosis, highlighting the importance of considering this pathogen in homeless populations with pneumonia. The disconnect between traditional severity measurement and management observed in this population suggests a need for sensitivity to less measurable clinical features in lower socioeconomic populations, especially if professional societies, insurers, and medical advisory boards place greater emphasis on objective severity assessment in clinical decision-making and quality measurement.
The finding that hospitalized homeless individuals had no difference in LOS or cost of care compared with nonhomeless patients, even after adjustment for severity, differed from those of previous studies,8,9 which cited lack of public housing and access to primary care as possible causes of longer hospitalizations. Housing and case management programs have been proposed as a means to improve long-term outcomes and reduce overall costs of care in chronically ill homeless patients.10,16 During the study period, LDS Hospital had a close relationship with the Fourth Street Clinic. Intermountain Healthcare (the parent organization of LDS Hospital) provides the clinic with approximately $1 billion annually in charity care and has sponsored annual grants to support the Fourth Street Clinic since 1996. The multidisciplinary approach to acute illnesses for homeless individuals may have contributed to the observed shorter hospital stays and reduced cost in our population. Although the study was underpowered to show statistical difference, the observed reduction of LOS for hospitalized patients who were provided medical housing after discharge suggests that providing patients with betterpopulation-sensitive outpatient services could improve outcomes and reduce cost in patients with acute illnesses, especially in vulnerable populations.
Limitations
Our study has several limitations. Because the study was limited to hospital and ED records, we did not follow patients prospectively to confirm follow-up with primary care or study long-term outcomes other than 30-day mortality. We did not distinguish between chronic and acute homelessness. We included hospitalized patients who left against medical advice (although we found only 3 in the homeless cohort, with an average LOS of 2 days). We excluded 20 patients with health care---acquired pneumonia and 5 patients with AIDS (reflecting the low burden of HIV in Salt Lake City). Homeless veterans were also likely underrepresented because of the presence of a large US Department of Veterans Affairs hospital in the area. Small numbers of severely ill patients and subgroups within the homeless cohort limited our power to detect significant differences in 30-day mortality or readmission rates.
Conclusions
Homeless patients with CAP presented to the ED with significantly lower 30-day mortality risk than those of nonhomeless individuals and demonstrated higher rates of admission after adjustment of severity. CURB-65 correlated less well with hospital admission for homeless patients, suggesting that additional clinical or demographic features were considered in the admission decision for homeless patients. Despite the higher admission risk, we found no difference in LOS or cost of hospital care, even after adjustment for illness severity; this finding may be related to the strong affiliation between LDS Hospital and the Fourth Street Clinic during the study period. As the United States faces rising health care costs and an increase in homelessness resulting from foreclosures and unemployment, we need more programs that effectively establish a strong relationship between primary care providers, community housing, and acute care facilities for homeless patients.
Acknowledgments
B. Jones is supported by a training grant from the National Institutes of Health (5T32 HL 105321-2). S. M. Brown is supported by a grant from National Institute of General Medical Sciences (K23GM094465). A. V. Gundlapalli is supported by a grant from the US Department of Veterans Affairs (Grant HIR 10-002). The study was funded by a grant from the Intermountain Research and Medical Foundation.
We thank Al Jephson for database management, David Tomer for chart review, and the Fourth Street Clinic for their continued dedication to quality health care for the homeless of Salt Lake City.
Note. The views expressed herein are those of the authors and do not necessarily reflect the views of the authors’ funding institutions.
Footnotes
Note. The views expressed herein are those of the authors and do not necessarily reflect the views of the LDS Hospital, the University of Utah, or the Department of Veterans Affairs.
Contributors
B. Jones cotributed to study design, data collection, statistical analysis, and article preparation. A. V. Gundlapalli contributed to study design and article preparation. J. P. Jones contributed to statistical analysis and study design. S. M. Brown contributed to data collection and article preparation. N. C. Dean contributed to study design, data collection, and article preparation.
Human Participant Protection
The study was approved by the institutional review board of Intermountain Health Care (Urban Central Region).
Contributor Information
Barbara Jones, Divisions of Pulmonary and Critical Care Medicine, University of Utah, Salt Lake City.
Adi V. Gundlapalli, Division of Epidemiology, University of Utah, and the Department of Veterans Affairs, Salt Lake City..
Jason P. Jones, Kaiser Permanente, Pasadena, CA, and Intermountain Medical Center, Murray.
Samuel M. Brown, Divisions of Pulmonary and Critical Care Medicine, University of Utah, Salt Lake City; Intermountain Medical Center, Murray, UT.
Nathan C. Dean, Divisions of Pulmonary and Critical Care Medicine, University of Utah, Salt Lake City; Intermountain Medical Center, Murray, UT.
References
- 1.Armstrong GL, Conn LA, Pinner RW. Trends in infectious disease mortality in the United States during the 20th century. JAMA. 1999;281(1):61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- 2.Hawke W, Davis M, Erlenbusch B. [Accessed October 2, 2012];Dying without dignity: homeless deaths in Los Angeles County. 2000---2007 Available at: http://www.nationalhomeless.org/publications/dyingwithoutdignity/dyingwithoutdignity.pdf.
- 3.Hwang SW, Orav J, O'Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med. 1997;126(8):625–628. doi: 10.7326/0003-4819-126-8-199704150-00007. [DOI] [PubMed] [Google Scholar]
- 4.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336(4):243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 6.Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goss CH, Rubenfeld GD, Park DR, et al. Cost and incidence of social comorbidities in low-risk patients with community-acquired pneumonia admitted to a public hospital. Chest. 2003;124(6):2148–2155. doi: 10.1378/chest.124.6.2148. [DOI] [PubMed] [Google Scholar]
- 8.Hwang SW, Weaver J, Aubry T, Hoch JS. Hospital costs and length of stay among homeless patients admitted to medical, surgical, and psychiatric services. Med Care. 2011;49(4):350–354. doi: 10.1097/MLR.0b013e318206c50d. [DOI] [PubMed] [Google Scholar]
- 9.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 10.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 11.Gundlapalli A, Hanks M, Stevens SM, et al. It takes a village: a multidisciplinary model for the acute illness aftercare of individuals experiencing homelessness. J Health Care Poor Underserved. 2005;16(2):257–272. doi: 10.1353/hpu.2005.0033. [DOI] [PubMed] [Google Scholar]
- 12.Jones BE, Jones J, Bewick T, et al. CURB-65 pneumonia severity assessment adapted for electronic decision support. Chest. 2011;140(1):156–163. doi: 10.1378/chest.10-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Classification of Diseases, Ninth Revision. World Health Organization; Geneva, Switzerland: 1980. [Google Scholar]
- 14.US Department of Housing and Urban Development [Accessed December 15, 2012];Homelessness definition. 2001 Available at: http://portal.hud.gov/hudportal/HUD?src=/topics/homelessness/definition.
- 15.Skolnick M. The Utah genealogical database: a resource for genetic epidemiology. In: Cairns JL, Skolnick M, editors. Banbury Report No 4: Cancer Incidence in Defined Populations. Cold Spring Harbor Laboratory; New York, NY: 1980. pp. 285–297. [Google Scholar]
- 16.Basu A, Kee R, Buchanan D, Sadowski LS. Comparative cost analysis of housing and case management program for chronically ill homeless adults compared to usual care. Health Serv Res. 2012;47(1 pt 2):523–543. doi: 10.1111/j.1475-6773.2011.01350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]