Abstract
Highly active antiretroviral therapy (HAART) has been successful in reducing HIV-1-associated morbidity and mortality since its introduction in 1996. It, however, fails to eradicate HIV-1 infection thoroughly. The high cost of life-long HAART and the emergence of drug resistance among HIV-1-infected individuals have brought renewed pressure for the discovery of novel antivirals and alternative medicines. Traditional Chinese medicine (TCM) is one of the mainstreams of complementary and alternative medicine, and serves as rich resources for new drug development. Despite almost 100 plant-derived compounds are in clinical trials, few target HIV-1 infection. In this study, we discovered that extract of Sanguisorba officinalis (SOE) has anti-HIV-1 activities. Using a cell-based assay and single-cycle luciferase reporter viruses pseudotyped with envelopes from HIV-1 or control viruses, we found that SOE exhibited significant inhibitory ability against both CCR5 and CXCR4 tropic HIV-1 (ADA and HXB2) with respective IC50 values of 1.91±0.16 μg/ml and 3.70±0.53 μg/ml. Interestingly, SOE also inhibited SIV infection but failed to block vesicular stomatitis virus (VSV), SARS-CoV and influeunza H5N1 pseudoviruses. Furthermore, we showed that SOE had no effects on post-entry events of HIV-1 replication. It blocked entry by acting on viral envelope directly because SOE pre-treatment with the virus but not with cell lines expressing viral receptors showed the maximal inhibitory activity. In addition, SOE was able to inhibit reverse-transcription-inhibitor-resistant viruses (K103N, Y188L, and K103N/Y188L/G190A) and a protease-inhibitor-resistant strain (PI-2840). Our findings demonstrated SOE as a novel and specific entry inhibitor, which shed lights on the discovery of anti-HIV-1 drugs from traditional herbal medicines.
Keywords: Sanguisorba officinalis, HAART, HIV, Traditional Chinese Medicine, Entry Inhibitor
Introduction
Traditional Chinese medicine (TCM) includes various forms of herbal medicine, acupuncture, moxibustion, massage, Qi exercise, meditation and dietary therapy. TCM was developed in China as a personalized medical practice based on a tradition of more than 5,000 years. As a result, thousands of plants have been used as herbal medicines for treating different types of diseases. For example, one of the most famous drugs namely artemisinin was originally extracted from plant Artemisia annua and is now a standard treatment worldwide for P. falciparum malaria [1]. During the recent decade, the use of TCM has increased globally as one of the mainstreams of complementary and alternative medicine. Meantime, it serves as a rich resource for new drug development.
Before the availability of highly active antiretroviral therapy (HAART), people with HIV/AIDS often seek for herbal therapy in China. This situation maintains nowadays because HAART is still not readily accessible or affordable especially in rural areas, where the majority of patients reside. Interestingly, even in the era of HAART, HIV-infected people who used herbal therapy at a high rate attempted more frequent visits to TCM providers and reported helpful improvement with the treatment [2, 3]. In most cases, however, it remains unknown whether or not the herb used has any anti-HIV activities, and therefore regarded as the enhancement of patients' immune function or the treatment of HIV-related symptoms or the management of HAART-related side effects [4]. In recent years, we and others have demonstrated that compounds extracted from herbal plants have their biochemical activity elucidated with evidence-based research, revealing anti-tumor activity in some cases and anti-HIV activity in others [5–9]. Some herbal compounds have been moved forward into clinical trials [6, 7, 10]. Before this study, however, it remains elusive if Sanguisorba officinalis has any anti-HIV activity.
Sanguisorba officinalis (also called Great Burnet) is a plant in the family Rosaceae, subfamily Rosoideae. It is easily found in northern regions of China and has been used as a TCM for thousands of years to treat hemostasis and inflammation [11]. Some other functions that have been discovered in recent years include its antioxidant and anti-tumor properties [12–14]. Here, to the best of our knowledge we are the first group to study the anti-HIV-1 activities of the extract of Sanguisorba officinalis (SOE). Our findings have implications in exploring TCM for new antiviral discovery.
Materials and methods
Preparation of extracts from Sanguisorba officinalis
The stem of Sanguisorba officinalis was cut into small pieces and immersed in distilled water. The mixture was treated by ultrasound for 1hr followed by boiling at 100°C for 30 minutes twice. After filtration, the supernatant was concentrated by a rotary evaporator under reduced pressure and then followed by lyophilization for 48 hours to obtain the aqueous extract powder (SOE). The yield of SOE was 9.9–11.2%. HPLC analysis of SOE was conducted on a Ultimate AQ-C18 column (250 mm×4.6 mm, 5 mm). The mobile phase consisted of acetonitrile (A) and 0.2% formic acid (B) in water, using a gradient elution of 5%–15% A at 0–10 min, 15%–25% A at 10–25 min, 25%–30% A at 25–35 min, 30%–70% A at 35–45 min, 70%–95% A at 45–50 min and 95% A at 50–60 min. The solvent velocity of flow was 1.0 mL min−1 and the column was at room temperature. The detection wavelength was set at 254 nm. The contents of each component were controlled between 1.25–1.35% and 1.69–1.80%, respectively. The extract powder was dissolved in phosphate buffer solution and passed through 0.45 μm filter for sterilization. SOE was dissolved in dimethyl sulfoxide (DMSO) at a concentration of 40 mg/mL followed by gentle vortex at room temperature. The supernatants were carefully collected after centrifugation at 4000 rpm for 5 min and filtered through 0.22 μm Millipore syringe filter for experiments.
Cell culture and virus generation
293T, MDCK and HEK293T-ACE2 were cultured in DMEM (Dulbecco's modified Eagle medium) with 10% inactivated fetal bovine serum (FBS) (Invitrogen), 100 units/ml penicillin, and 100ug/ml streptomycin sulfate (Invitrogen). GHOST(3)-CD4-CCR5/CXCR4 cells were obtained from the NIH AIDS Research and Reference Reagent Program and cultured in DMEM with 10% FBS, 100 u/mL penicillin, 100 μg/ml streptomycin sulfate, 100μg/ml hygromycin B, 500 μg/ml G418 and 1 μg/ml puromycin (Sigma). Single-cycle luciferase HIVADA, HIVHXB2, SIVmac239, SIVmac1a11 VSV, H5N1anhui and SARS-CoV pseudoviruses were constructed as described [9, 15–17]. Briefly, pseudoviruses were generated by co-transfection of (using polyethylenimine [PEI]; Polysciences Inc., Warrington, PA) 293T cells with NL4-3 E−V− Luc+ and envelope protein from different strain of viruses. All NNRTI mutant constructs were generated based on a molecular clone backbone NL4-3 E−V− Luc+ as we previously described[8]. PI resistant strain was obtained from NIH (resistant to multiple anti-HIV protease drugs; 2840, carrying L10R, M46I, L63P, V82T, and I84V). Cell-free supernatant was collected 48 h post transfection and frozen at −80°C. The 50% tissue culture infective dose (TCID50) was calculated as described previously[8]
Cell viability assay
The GHOST(3)-CD4-CCR5/CXCR4 cells were incubated in the presence or absence of serially diluted SOE at 37° C in 5% CO2 for 48 hours. Cells viability was then measured using commercially available kit (CellTiter-Glo® Luminescent Cell Viability Assay kit, Promega, USA).
Antiviral assay
The inhibitory activities of the SOE against viruses are evaluated as described previously [8]. Briefly, a serial diluted drug was tested against 100TCID50 virus infection. GHOST(3)-CD4-CCR5/CXCR4 were used for HIVADA and HIVHXB2, SIVmac239, SIVmac1a11, whereas MDCK and HEK293T-ACE2 were used for H5N1 and SARS-CoV pseudoviruses infection, respectively. The viral infection was determined on day 3 by measuring the reporter luciferase activity in target cells post-infection using commercially available kits. Antiviral data are reported as the quantity of drug required to inhibit viral production by 50% (EC50).
Fractionation of aqueous extract of Sanguisorba officinalis
Different polar solvents were used to obtain sub-fractions from SOE yielding petroleum-ether-partitioned extract (PE), ethyl-acetate-partitioned extract (EtOAc), n-butanol-partitioned extract (BuOH) and water residues (RE). These sub-fractions were then concentrated in vacuum dryer for later testing.
Results
Anti-viral activity of aqueous extract of Sanguisorba officinalis (SOE)
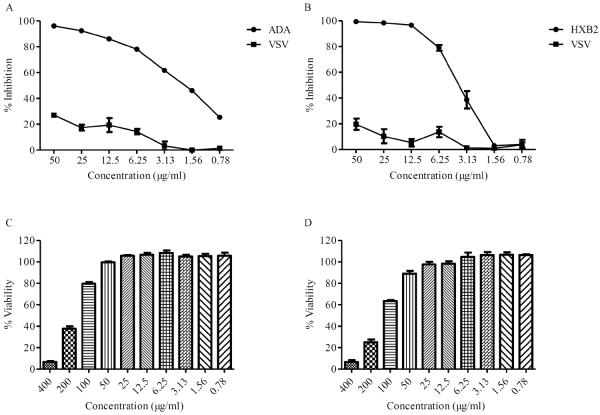
To determine the antiviral activity of SOE, GHOST-CCR5 and GHOST-CXCR4 cells were infected with CCR5-tropic HIV-1ADA and CXCR4-tropic HIV-1HXB2, respectively, in the presence of serial diluted SOE. As a control, VSV pseudovirus was included in parallel experiments. As shown in Fig. 1A and B, SOE displayed an EC50 of 1.91+0.16 μg/ml and 3.70+0.53 μg/ml in the inhibition of HIV-1 replication of both tropic without cell toxicity observed (Fig. 1C and D). In contrast, when SOE was tested against VSV psuedovirus infection, no inhibition was observed. Because ADA, HXB2 and VSV pseudoviruses share the same HIV backbone and differ only in their glycolproteins expressed on the viral surface, this result suggested that SOE acts specifically in inhibiting HIV-1 replication at an early stage of viral entry.
Fig. 1.
Activity of SOE against HIV-1ADA, HIVHXB2 and HIVVSV. Serially diluted SOE was added to GHOST-CCR5 and GHOST-CXCR4 infected with HIV-1ADA (A) and HIVHXB2 (B), respectively. HIVVSV was tested as a negative control (A and B). The luciferase level was measured 2 days PI. All results are means standard errors of the means from three independent experiments. To test SOE cytotoxicity, the GHOST(3)-CD4-CCR5 (C) and The GHOST(3)-CD4-CXCR4 (D) cells were cultured in serially diluted SOE at 37° C for 48 hours in 5% CO2. Cells viability was then measured using the Promega CellTiter-Glo® Luminescent Cell Viability Assay kit. The data represent the mean ± SD of triplicate experiments.
No effect of SOE on HIV-1 post-entry
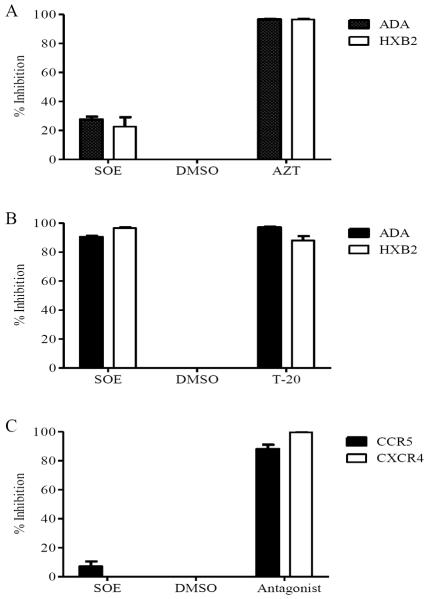
To confirm that SOE antagonizes viral entry rather than post-entry events, we testes the same panel of viruses but with a modified experimental schedule. Target cells were first co-incubated with pseudovirus for 2 hrs, washed, and then treated with the presence of 50ug/ml SOE or 1uM AZT, which is a potent NRTI, for 48 hours. As shown in Figures 2A, with this experimental schedule SOE does not strongly inhibit HIV-1 anymore as compared with AZT. This result supports the finding that inhibition of SOE on HIV-1 replication is not due to the blockade at the post entry step (e.g. reverse transcription) but rather at an entry step.
Fig. 2.
SOE inhibits HIV-1 infection by binding to viruses envelope snd block the entry. A. Post-entry assay. GHOST-CD4-CCR5 or CXCR4 cells was co-incubated with pseudovirus for 2 hrs, washed, and then treated with the presence of 50ug/ml SOE, DMSO as negative control and 1uM AZT as positive control for 48 hours. SOE does not inhibit either HIV-1ADA or HIVHXB2 virus gene replication after viral entry is achieved. B. SOE-virus interaction assay. HIV-1ADA and HIVHXB2 pseudovirus pre-treated with 50ug/ml SOE or DMSO as a negative control and entry inhibitor T20 as a positive control. SOE pre-treatment inhibited both HIVADA and HIVHXB2 pseudovirus infection to a similar degree as T-20. C. SOE-cell binding assays. GHOST cells was pre-treatment with SOE or the CCR5 antagonist Marvaroc (MVC) and the CXCR4 antagonist JM2987 as positive controls, and DMSO as negative control for 1 hour at 37°C before being infected with HIV-1ADA or HIV-1HXB2. SOE pre-treatment with the cells had no antiviral effect, while MVC and JM2987 pre-treatment showed strong inhibition against HIV-1 ADA and HXB2 pseudoviruses at 1μM as expected. The data represent the mean ±SD of triplicate experiments.
SOE inhibits HIV-1 directly
To further determine whether SOE inhibits virus entry by directly inactivating HIV-1 or binding to its receptor on target cells, SOE-virus binding and SOE-cell binding assays were performed. In the SOE-virus binding assay, pseudovirus was pre-treated with 50ug/ml SOE first. Meantime, dilution solution DMSO was used as a negative control and entry inhibitor T20 as a positive control. The viruses were then recover by ultracentrifugation and subjected to infect target cells. We found that SOE inhibited both ADA and HXB2 pseudovirus infection to a similar degree as T-20, which blocks HIV-1 fusion (Figure 2B). Subsequently, the SOE-cell binding assays were performed by pre-treating the target GHOST cells with SOE or with the CCR5 antagonist Marvaroc (MVC) and the CXCR4 antagonist JM2987 as positive controls for 1 hour at 37°C. After washing by PBS, cells were incubated with HIV-1ADA or HIV-1HXB2 for 2 hours, washed, and cultured at 37°C for 48hrs [18]. We found that pre-treating the target cells with SOE had virtually no antiviral effect, while MVC and JM2987 showed strong inhibition against the respective ADA and HXB2 pseudoviruses at 1μM as expected (Figures 2 C). This body of evidence demonstrates that SOE inhibits HIV-1 infection by actions on the viral envelope glycoprotein gp160, which mediates the viral entry into the host target cells.
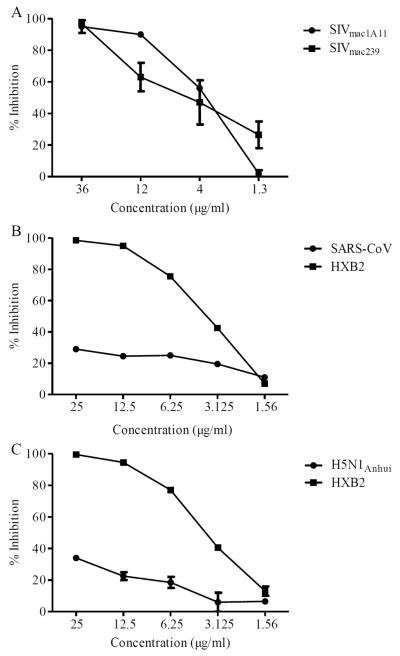
Antiviral activity of SOE against SIV, influenza H5N1 and SARS-CoV pseudoviruses
To further confirm whether SOE is a HIV-1-specific entry inhibitor, we tested two SIV, one influenza H5N1 and one SARS-CoV pseudoviral strains, respectively. A previous study indicated that there are residue peptides discovered as potent inhibitor of virus entry against both HIV-1 and SIV envelope glycoproteins [23]. Interestingly, SOE inhibited both SIV strains mac239 and mac1A11, but neither influenza H5N1 nor SARS-CoV (Figure 3). These results suggest that SOE has a broad and specific reactivity against diverse AIDS viruses, which is rather interesting.
Fig. 3.
Activity of SOE against SIV, influenza and SARS-CoV. Serially diluted SOE was added to GHOST-CCR5 infected with HIVHXB2, SIVmac239 and SIVmac1A11 (A), 293T-ACE2 infected with SARS-CoV (B) and MDCK cells infected with H5N1Anhui (C), respectively. HIVHXB2 was tested as a positive control (B and C). The luciferase level was measured 2 days PI. All results are means standard errors of the means from three independent experiments.
Antiviral activity of SOE against drug resistant HIV-1 strains
The rapid emergence of drug resistant strains in patients is one of the major obstacles to successful antiretroviral treatment. Therefore, the experiment of anti-HIV resistant viruses was carried out, in which four HIV-1 drug resistant strains were tested including three NNRTI resistant viruses (K103N, Y188L, and K103N/Y188L/G190A) and one protease inhibitor resistant virus (PI-2840)[8]. As expected, SOE inhibited all four drug-resistant strains (Figure 4A), demonstrating greater breadth of inhibition when compared to Nevirapine (NVP), which is an FDA-approved NNRTI. Consistent to previous publications, NVP did not inhibit HIV-1 resistant strains harboring Y188L or K103N/Y188L/G190A mutations (Figure 4B). Since viral entry precedes reverse transcription, these results provide further support for SOE as an entry inhibitor against live replicating HIV-1 strains.
Fig. 4.
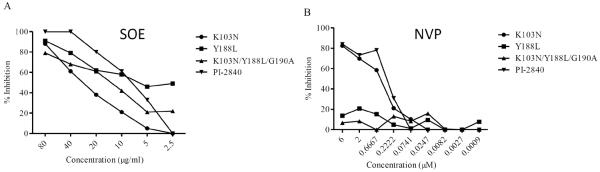
Activity of SOE against NNRTI mutant pseudovirus and a PI resistant strain. Serially diluted SOE was added to GHOST-CCR5 and GHOST-CXCR4 infected with NNRTI mutant pseudoviruses (K103N, Y188L and K103N/Y188L/G190A) and a PI resistant strain (PI-2840), respectively (A). Nevirapine (NVP) was included as control (B). All NNRTI mutant constructs were generated based on a molecular clone backbone, pNL4-3LucEnvVpr. The PI resistant strain (resistant to multiple anti-HIV protease drugs; 2840) carries L10R, M46I, L63P, V82T, and I84V. The luciferase level was measured 2 days PI. All results are means standard errors of the means from three independent experiments.
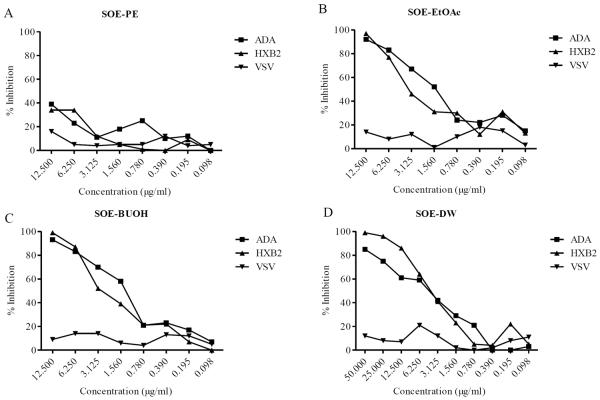
Anti-HIV activities fractionation of SOE
To further characterize the anti-HIV activity of SO aqueous extract, SOE were subjected to different polar solvents to obtain petroleum-ether-partitioned extracts (PE), ethyl-acetate-partitioned extracts (EtOAc), n-butanol-partitioned extracts (BuOH) and water residues (RE). Each fraction was vacuum dried and then screened for anti-HIV-1 activity. Interestingly, the EtOAc and BuUOH subfractions strongly diminished HIV-1 infection of target cell lines similar to SOE (Figure 1 and 5A–D). However, the PE subfraction did not show any inhibition of HIV-1. These results indicate that the solubility of SOE is dependent on the polarity of the solvent and provide direction for future isolation of small molecule HIV-1 entry inhibitor from these sub-fractions.
Fig. 5.
Activity of fractions of SOE against HIV-1ADA, HIVHXB2 and HIVVSV. Serially diluted PE (A), EtOAc (B), BuOH (C) or DW (D) fractions was added to GHOST-CCR5 and GHOST-CXCR4 infected with HIV-1ADA, HIVHXB2, and HIVVSV. The luciferase level was measured 2 days PI. All results are means standard errors of the means from three independent experiments.
Discussion
In this study, we demonstrated that SOE blocks the entry of both CCR5- and CXCR4-tropic strains of HIV-1. This blockade is HIV-1-specific because SOE does not exhibit any activities against HIV-Luc+ viruses pseudotyped with envelopes of VSV, SARS-CoV and Influenza. Interestingly, SOE acts directly on HIV-1 instead of cellular receptor or co-receptor. It also exhibits potency against replication competent HIV-1 strains resistant to specific drugs targeting protease (PI) and reverse transcriptase (RT). Our findings, therefore, provide scientific evidence for the potential use of SOE in the prevention and treatment of HIV-1 infection as well as for the search of ingredient small molecular compounds as specific entry inhibitor.
Closing the door for HIV-1 to enter target cells is a critical strategy for both prevention and treatment [22, 24]. Till now, there are only two drugs in this category approved by FDA for clinical use in the market: Maraviroc and Enfuvirtide (T-20). Maraviroc binds to the host CCR5 co-receptor to prevent binding with gp120, while T-20 interacts with gp41 to interrupt membrane fusion between HIV-1 and the host target cell plasma membrane. Enfuvirtide is part of the repertoire of antiretroviral drugs that have been used in combination therapy to treat HIV-1 infection [25]. Although effective, Enfuvirtide has to be administrated by injection whereas Maraviroc requires the screening of patients to exclude strains of CXCR4-tropism. It is, therefore, useful to identify new types of HIV-1 entry inhibitors. To this end, it is of very interesting to discover that SOE is capable of inhibiting entry of both CCR5- and CXCR4-tropic HIV-1 ADA and HXB2 strains as well as of SIVmac1A11 and SIVmac239 by binding viral envelope glycoproteins directly. We and others previously showed that despite a significant level of sequence diversity, HIV-1 and SIV share a series of events during virus entry including binding of gp120 to CD4 and chemokine coreceptor, and fusion between virus and cell membranes [19–22]. SOE probably acts upon such a highly conserved element of HIV-1 and SIV envelope glycoproteins, which still requires future investigation [19, 20, 26–28]. Because SIVmac1A11 enters target cells in a CD4-independent way [16], SOE likely inhibits virus entry through other mechanisms rather than blocking CD4 binding site directly. Critically, the proofed anti-HIV-1 specificity together with the lack of antiviral effects against VSV, SARS-CoV and influenza also rule out the possibility that SOE simply inactivate HIV-1 virus by acts on viral lipids like a disinfectant. In support of our findings, several small molecules isolated from plant have been reported to have some moderate inhibitory ability against HIV-1 entry. For example, tea polyphenols found in green tea likely interrupt membrane fusion between HIV-1 and the host cell plasma membrane [29]. Further investigations, however, are necessary to reveal the mode of SOE action, which may lead to the identification of new drug target on HIV-1 envelope.
With the enhanced efforts of treatment as prevention, there are also issues of rapid emergence of drug resistant strains of HIV-1 especially in developing countries [30]. Although several extracts of herbal medicines have been investigated for their anti-HIV activities, inhibition of anti-HIV drug resistant strains was rarely studied [7, 31–34]. We recently reported that plant-derived calanolide A and their analogues have unique advantaged overcoming the existing drug resistant viruses [8, 9]. Using the same methods, we showed here that SOE inhibited not only RT inhibitor resistant viruses (K103N, Y188L, and K103N/Y188L/G190A) but also a PR-inhibitor-resistant primary strain (PI-2840). Since reverse transcriptase and protease act after HIV entry, these results are consistent with SOE as new entry inhibitor. To explore the potential of SOE for treating AIDS patients, a future well-designed clinical trial should be conducted for in vivo efficacy evaluation. It is also necessary to purify the small molecule compound from SOE with anti-HIV-1 activity.
Conclusion
In this study, we demonstrated that SOE blocks the entry of both CCR5- and CXCR4-tropic strains of HIV-1. This blockade is HIV-1-specific because SOE does not exhibit any activities against HIV-Luc+ viruses pseudotyped with envelopes of VSV, SARS-CoV and Influenza. Interestingly, SOE acts directly on HIV-1 instead of cellular receptor or co-receptor. It also exhibits potency against replication competent HIV-1 strains resistant to specific drugs targeting protease (PI) and reverse transcriptase (RT). Our findings, therefore, provide scientific evidence for the potential use of SOE in the prevention and treatment of HIV-1 infection as well as for the search of ingredient small molecular compounds as specific entry inhibitor.
References
- 1.White NJ. Assessment of the pharmacodynamic properties of antimalarial drugs in vivo. Antimicrobial agents and chemotherapy. 1997;41(7):1413–1422. doi: 10.1128/aac.41.7.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zou W, Liu Y, Wang J, Li H, Liao X. Traditional Chinese Herbal Medicines for Treating HIV Infections and AIDS. Evidence-based complementary and alternative medicine : eCAM. 2012;2012:950757. doi: 10.1155/2012/950757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu JP. The use of herbal medicines in early drug development for the treatment of HIV infections and AIDS. Expert opinion on investigational drugs. 2007;16(9):1355–1364. doi: 10.1517/13543784.16.9.1355. [DOI] [PubMed] [Google Scholar]
- 4.Cui M, Li J, Li H, Song C. Herbal compatibility of traditional Chinese medical formulas for acquired immunodeficiency syndrome. Journal of traditional Chinese medicine = Chung i tsa chih ying wen pan / sponsored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine. 2012;32(3):329–334. doi: 10.1016/s0254-6272(13)60033-3. [DOI] [PubMed] [Google Scholar]
- 5.Man S, Gao W, Wei C, Liu C. Anticancer Drugs from Traditional Toxic Chinese Medicines. Phytotherapy research : PTR. 2012 doi: 10.1002/ptr.4609. [DOI] [PubMed] [Google Scholar]
- 6.Wang J, Zou W. Practices, challenges, and opportunities: HIV/AIDS treatment with traditional Chinese medicine in China. Frontiers of medicine. 2011;5(2):123–126. doi: 10.1007/s11684-011-0124-z. [DOI] [PubMed] [Google Scholar]
- 7.Chu Y, Liu H. Advances of research on anti-HIV agents from traditional Chinese herbs. Advances in dental research. 2011;23(1):67–75. doi: 10.1177/0022034511399912. [DOI] [PubMed] [Google Scholar]
- 8.Lu X, Liu L, Zhang X, Lau TC, Tsui SK, Kang Y, Zheng P, Zheng B, Liu G, Chen Z. F18, a novel small-molecule nonnucleoside reverse transcriptase inhibitor, inhibits HIV-1 replication using distinct binding motifs as demonstrated by resistance selection and docking analysis. Antimicrobial agents and chemotherapy. 2012;56(1):341–351. doi: 10.1128/AAC.05537-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma T, Liu L, Xue H, Li L, Han C, Wang L, Chen Z, Liu G. Chemical library and structure-activity relationships of 11-demethyl-12-oxo calanolide A analogues as anti-HIV-1 agents. Journal of medicinal chemistry. 2008;51(5):1432–1446. doi: 10.1021/jm701405p. [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Zou W. Recent advances of HIV/AIDS treatment with traditional Chinese medicine in China. Journal of traditional Chinese medicine = Chung i tsa chih ying wen pan / sponsored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine. 2010;30(4):305–308. doi: 10.1016/s0254-6272(10)60062-3. [DOI] [PubMed] [Google Scholar]
- 11.Zhang S, Liu X, Zhang ZL, He L, Wang Z, Wang GS. Isolation and identification of the phenolic compounds from the roots of Sanguisorba officinalis L. and their antioxidant activities. Molecules. 2012;17(12):13917–13922. doi: 10.3390/molecules171213917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goun EA, Petrichenko VM, Solodnikov SU, Suhinina TV, Kline MA, Cunningham G, Nguyen C, Miles H. Anticancer and antithrombin activity of Russian plants. Journal of ethnopharmacology. 2002;81(3):337–342. doi: 10.1016/s0378-8741(02)00116-2. [DOI] [PubMed] [Google Scholar]
- 13.Zberts VL, Plakhova NB. Application of burnet (Sanguisorba officinalis) in treatment of dysentery in children. Sovetskaia meditsina. 1951;4:27–29. [PubMed] [Google Scholar]
- 14.Wang Z, Loo WT, Wang N, Chow LW, Wang D, Han F, Zheng X, Chen JP. Effect of Sanguisorba officinalis L on breast cancer growth and angiogenesis. Expert opinion on therapeutic targets. 2012;16(Suppl 1):S79–89. doi: 10.1517/14728222.2011.642371. [DOI] [PubMed] [Google Scholar]
- 15.Liu L, Fang Q, Deng F, Wang H, Yi CE, Ba L, Yu W, Lin RD, Li T, Hu Z, et al. Natural mutations in the receptor binding domain of spike glycoprotein determine the reactivity of cross-neutralization between palm civet coronavirus and severe acute respiratory syndrome coronavirus. Journal of virology. 2007;81(9):4694–4700. doi: 10.1128/JVI.02389-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun C, Chen Z, Tang X, Zhang Y, Feng L, Du Y, Xiao L, Liu L, Zhu W, Chen L, et al. Mucosal priming with a replicating-vaccinia virus-based vaccine elicits protective immunity to simian immunodeficiency virus challenge in rhesus monkeys. Journal of virology. 2013;87(10):5669–5677. doi: 10.1128/JVI.03247-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen MW, Cheng TJ, Huang Y, Jan JT, Ma SH, Yu AL, Wong CH, Ho DD. A consensus-hemagglutinin-based DNA vaccine that protects mice against divergent H5N1 influenza viruses. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(36):13538–13543. doi: 10.1073/pnas.0806901105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rapista A, Ding J, Benito B, Lo YT, Neiditch MB, Lu W, Chang TL. Human defensins 5 and 6 enhance HIV-1 infectivity through promoting HIV attachment. Retrovirology. 8:45. doi: 10.1186/1742-4690-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen Z, Telfer P, Reed P, Zhang L, Getti A, Ho DD, Marx PA. Isolation and characterization of the first simian immunodeficiency virus from a feral sooty mangabey (Cercocebus atys) in West Africa. Journal of medical primatology. 1995;24(3):108–115. doi: 10.1111/j.1600-0684.1995.tb00155.x. [DOI] [PubMed] [Google Scholar]
- 20.Chen Z, Zhou P, Ho DD, Landau NR, Marx PA. Genetically divergent strains of simian immunodeficiency virus use CCR5 as a coreceptor for entry. Journal of virology. 1997;71(4):2705–2714. doi: 10.1128/jvi.71.4.2705-2714.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang L, He T, Huang Y, Chen Z, Guo Y, Wu S, Kunstman KJ, Brown RC, Phair JP, Neumann AU, et al. Chemokine coreceptor usage by diverse primary isolates of human immunodeficiency virus type 1. Journal of virology. 1998;72(11):9307–9312. doi: 10.1128/jvi.72.11.9307-9312.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kang Y, Wu Z, Lau TC, Lu X, Liu L, Cheung AK, Tan Z, Ng J, Liang J, Wang H, et al. CCR5 antagonist TD-0680 uses a novel mechanism for enhanced potency against HIV-1 entry, cell-mediated infection, and a resistant variant. The Journal of biological chemistry. 2012;287(20):16499–16509. doi: 10.1074/jbc.M112.354084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gustchina E, Hummer G, Bewley CA, Clore GM. Differential inhibition of HIV-1 and SIV envelope-mediated cell fusion by C34 peptides derived from the C-terminal heptad repeat of gp41 from diverse strains of HIV-1, HIV-2, and SIV. Journal of medicinal chemistry. 2005;48(8):3036–3044. doi: 10.1021/jm049026h. [DOI] [PubMed] [Google Scholar]
- 24.Kang Y, Guo J, Chen Z. Closing the door to human immunodeficiency virus. Protein & cell. 2013;4(2):86–102. doi: 10.1007/s13238-012-2111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biswas P, Tambussi G, Lazzarin A. Access denied? The status of co-receptor inhibition to counter HIV entry. Expert opinion on pharmacotherapy. 2007;8(7):923–933. doi: 10.1517/14656566.8.7.923. [DOI] [PubMed] [Google Scholar]
- 26.Moriuchi M, Moriuchi H, Turner W, Fauci AS. Cloning and analysis of the promoter region of CXCR4, a coreceptor for HIV-1 entry. J Immunol. 1997;159(9):4322–4329. [PubMed] [Google Scholar]
- 27.Samson M, Labbe O, Mollereau C, Vassart G, Parmentier M. Molecular cloning and functional expression of a new human CC-chemokine receptor gene. Biochemistry. 1996;35(11):3362–3367. doi: 10.1021/bi952950g. [DOI] [PubMed] [Google Scholar]
- 28.Chen Z, Telfier P, Gettie A, Reed P, Zhang L, Ho DD, Marx PA. Genetic characterization of new West African simian immunodeficiency virus SIVsm: geographic clustering of household-derived SIV strains with human immunodeficiency virus type 2 subtypes and genetically diverse viruses from a single feral sooty mangabey troop. Journal of virology. 1996;70(6):3617–3627. doi: 10.1128/jvi.70.6.3617-3627.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu S, Lu H, Zhao Q, He Y, Niu J, Debnath AK, Wu S, Jiang S. Theaflavin derivatives in black tea and catechin derivatives in green tea inhibit HIV-1 entry by targeting gp41. Biochimica et biophysica acta. 2005;1723(1–3):270–281. doi: 10.1016/j.bbagen.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 30.Perelson AS, Ribeiro RM. Estimating drug efficacy and viral dynamic parameters: HIV and HCV. Statistics in medicine. 2008;27(23):4647–4657. doi: 10.1002/sim.3116. [DOI] [PubMed] [Google Scholar]
- 31.Han H, He W, Wang W, Gao B. Inhibitory effect of aqueous Dandelion extract on HIV-1 replication and reverse transcriptase activity. BMC complementary and alternative medicine. 2011;11:112. doi: 10.1186/1472-6882-11-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park IW, Han C, Song X, Green LA, Wang T, Liu Y, Cen C, Yang B, Chen G, He JJ. Inhibition of HIV-1 entry by extracts derived from traditional Chinese medicinal herbal plants. BMC complementary and alternative medicine. 2009;9:29. doi: 10.1186/1472-6882-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Au TK, Lam TL, Ng TB, Fong WP, Wan DC. A comparison of HIV-1 integrase inhibition by aqueous and methanol extracts of Chinese medicinal herbs. Life sciences. 2001;68(14):1687–1694. doi: 10.1016/s0024-3205(01)00945-6. [DOI] [PubMed] [Google Scholar]
- 34.Liu J. The use of herbal medicines in early drug development for the treatment of HIV infections and AIDS. Expert opinion on investigational drugs. 2007;16(9):1355–1364. doi: 10.1517/13543784.16.9.1355. [DOI] [PubMed] [Google Scholar]