Abstract
Objectives
We investigated outcomes of third molar removal or retention in adolescents and young adults.
Methods
We recruited patients aged 16 to 22 years from a dental practice–based research network in the Pacific Northwest from May 2009 through September 2010 who had at least 1 third molar present and had never undergone third molar removal. Data were acquired via questionnaire and clinical examination at baseline, periodic online questionnaires, and clinical examination at 24 months.
Results
A total of 801 patients participated. Among patients undergoing third molar removal, rates of paresthesia and jaw joint symptoms lasting more than 1 month were 6.3 and 34.3 per 100 person-years, respectively. Among patients not undergoing removal, corresponding rates were 0.7 and 8.8. Periodontal attachment loss at distal sites of second molars did not significantly differ by third molar removal status. Incident caries at the distal surfaces of second molars occurred in fewer than 1% of all sites.
Conclusions
Rates of paresthesia and temporomandibular joint disorder were higher after third molar removal. Periodontal attachment loss and incident caries at the distal sites of second molars were not affected by extraction status.
Third molar removal is one of the most common dental surgical procedures in the United States, representing 95% of all extractions among patients aged 16 to 21 years in an insured population.1 Although the risks associated with third molar removal are generally minor, such as pain and swelling, some complications may be more serious, such as injury to the temporomandibular joint (TMJ) or permanent paresthesia. Because many third molars are surgically removed, the costs associated with this procedure can be significant. One report estimated that more than $3 billion is spent annually in the United States for third molar removal.2 Because decisions regarding removal or retention of third molars are often made in late adolescence and early adulthood, understanding the risks and benefits of removal or retention during this time period is important.
The prophylactic removal of asymptomatic third molars has been the subject of considerable controversy. On one hand, some have advocated early removal of third molars as beneficial to patients to prevent the risk of future pathology and to minimize operative and postoperative risks.3–6 Another common argument for third molar removal is prevention of crowding of lower incisors. In the past decade, prevention of periodontal pathology has been proposed as a reason to prophylactically remove third molars.7,8 This theory suggests that periodontal pathology initiates in third molars and is more likely to proceed when third molars are retained. Additionally, if left unaddressed, the periodontal pathology may lead to negative cardiovascular, obstetric, metabolic, and renal health outcomes.9
On the other hand, third molar removal can result in various types of morbidity, such as pain, swelling, bleeding, infection, dry socket, trismus, paresthesia, and temporomandibular joint disorder (TMD).8 Most of these complications resolve, but some, such as paresthesia or TMD, may persist and become chronic or permanent conditions. The overall rate of complications from third molar removal varies considerably, with values reported from 4.6%10 to 21%.4 Thus, some feel that monitoring asymptomatic third molars is the appropriate strategy.11–13 In fact, the American Public Health Association and the United Kingdom’s National Health Service currently recommend against the removal of asymptomatic third molars.14,15 Nevertheless, about 50% of insured individuals in the United States will have their third molars removed by the time they are 20.16
Many studies have reported on the short-term complications of third molar removal, but few have compared outcomes for patients who do and do not elect to have third molars removed for an intermediate period of time (≤ 2 years). Therefore, we investigated the sequela of third molar removal or retention over a 2-year period. This time frame allowed the identification of sequela that were becoming persistent or chronic after third molar removal, as well as the assessment of conditions related to retained third molars during a period when they are erupting. Our specific aims were to compare the rates of paresthesia, TMD, and caries, as well as periodontal attachment loss. A companion article reports on general dentists’ recommendations for retention or removal of third molars and patient compliance with the recommendations.17
METHODS
We conducted a prospective cohort study on third molar removal and retention in the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (Northwest PRECEDENT), a dental practice–based research network. Network dentists interested in participating in this study underwent formal enrollment and training. Patients were recruited from May 2009 through September 2010 at the offices of participating general dentists and were followed until April 2012. The methods for this clinical portion of the study are described in our companion article.17 Briefly, though, patients aged 16 to 22 years were invited to participate if they had at least 1 third molar present and had never undergone third molar removal. We acquired data by means of a baseline questionnaire and clinical examination. At 8-month intervals, patients were asked to complete online questionnaires describing their third molar status. All patients who reached at least 18 months of follow-up time were invited to return for a final clinical examination (n = 400).
The primary exposure of interest was third molar removal. The primary outcomes were TMJ signs and symptoms, paresthesia, caries, and attachment loss.
The main self-reported outcomes were TMJ signs and symptoms (jaw clicking and popping, pain on wide opening, and pain in temples, jaw joint, or jaw muscles) and paresthesia of the lower lip, tongue, or both. We performed the analyses for these outcomes at the patient level. Patients who had at least one third molar removed were categorized in the removal (exposed) group, and patients without any removals were categorized in the retention group. Because we ascertained removal or retention status by means of multiple surveys over the course of follow-up, a patient could contribute person-years of follow-up to both the removal and the retention groups. For the retention group, follow-up started at the baseline examination and ended at the last follow-up assessment before report of an extraction (if any). For the removal group, follow-up started at the first extraction and ended at the last follow-up. Because all the self-report outcomes were incident events, we did not include additional follow-up after a patient reported an outcome in the respective analysis. Patients were considered to have TMD if they reported pain on wide opening or pain in the temple, jaw joint, or jaw muscles.
The main clinical outcomes were incident dental caries and change in attachment loss (in mm/year). Patients who attended the baseline and final clinical examinations were included in these analyses. We analyzed these outcomes at the surface or periodontal site level. A surface or site was considered to be in the removal (exposure) group if the adjacent third molar was extracted during follow-up. The follow-up time for each surface or site was the time between the 2 clinical examinations. We defined incident dental caries as a new carious lesion or restoration on a surface that was judged as disease free at baseline and calculated change in attachment loss as the difference in attachment loss at the distal surfaces of the second molars between the initial and final clinical examinations. We evaluated rate of pericoronitis, as indicated by dentist diagnosis, as a clinical outcome at the baseline and final clinical examinations, and it was reported at the patient level (i.e., any visible third molar with pericoronitis).
We estimated annual rates, means, and incidence rate ratios (when numbers of events were sufficient) using log-linear regression models for TMD signs and symptoms, pares-thesia, dental caries, and pericoronitis and a linear regression model for rate of progression in attachment loss. We used generalized estimating equations to account for possible lack of independence between observations from the same practice. We performed analyses using IBM SPSS Statistics for Windows, version 19.0.0 (IBM Corporation, Armonk, NY).
RESULTS
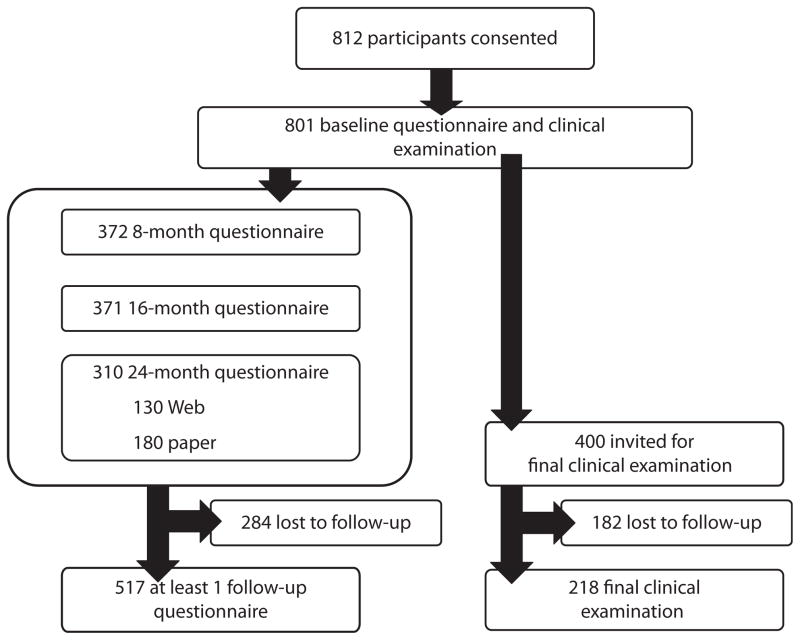
Of 801 participants enrolled at baseline, 517 completed at least 1 follow-up questionnaire, and they were followed for an average of 19.7 months (SD = 5.3). Participants enrolled at least 18 months (n=400) were invited for the final clinical examination, of whom 218 (55%) underwent the final examination (Figure 1). The average time between baseline and follow-up examinations was 21.9 months. The characteristics of patients who underwent the final clinical examination did not differ significantly from the characteristics of the eligible sample, except for age and frequency of dental cleanings. Participants who returned for the final examination were younger (mean age = 17.7 years vs 18.2 years) and had more frequent dental cleanings (79% vs 59% reported twice-annual cleanings) than targeted participants who did not return for final examination.
FIGURE 1.
Study flowchart: Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry; 2009–2012.
At baseline, 49% of the participants were female, 68% were aged 16 to 18 years, and 90% were White (Table 1). The majority of patients had private dental insurance (79%), and 65% had routine dental visits at least twice per year. Of the participants, 30% had at least 1 visible third molar (partially or fully erupted). Six percent of the participants had dental caries at the distal surface of the second molars, and 63 participants had dental caries on third molars (8% of all participants, or 26% of the participants with visible third molars). Of the participants, 27% reported clicking or popping in their TMJ, 13% had jaw pain on wide opening, and 17% had pain in their temples, jaw joint, or jaw muscles. The mean attachment loss at baseline was 0.75 millimeter (Table 1).
TABLE 1.
Baseline Characteristics of the Participants by Removal Status at Follow-Up: Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry, Pacific Northwest, 2009–2012
| Characteristic | Total (n = 801), % or Mean (SD) | Third Molar Removal Status at
Follow-Up,a % or
Mean (SD) |
|
|---|---|---|---|
| Third Molar Removal (≥ 1; n = 201) | Third Molar Retention (All Existing; n = 316) | ||
| Gender | |||
| Female | 49 | 51 | 51 |
| Male | 51 | 49 | 49 |
| Age, y | |||
| 16 | 24 | 28 | 23 |
| 17 | 23 | 23 | 20 |
| 18 | 21 | 20 | 21 |
| 19 | 12 | 12 | 13 |
| 20 | 9 | 7 | 11 |
| 21–22 | 11 | 9 | 13 |
| Raceb | |||
| White | 90 | 92 | 91 |
| Other | 8 | 7 | 8 |
| Dental insurance | |||
| No insurance | 10 | 12 | 9 |
| Medicaid | 11 | 6 | 7 |
| Private insurance | 79 | 82 | 84 |
| Frequency of dental cleanings | |||
| ≥ 2/y | 65 | 72 | 67 |
| 1/y | 23 | 22 | 23 |
| < 1/y | 12 | 7 | 9 |
| Current smoking | |||
| No | 94 | 95 | 97 |
| Yes | 6 | 6 | 3 |
| Eruption status of third molars | |||
| None visible in mouth | 70 | 72 | 70 |
| ≥ 1 visible | 30 | 29 | 30 |
| Angulation (highest in patient) | |||
| ≤ 35° | 51 | 45 | 53 |
| > 35° | 49 | 55 | 47 |
| Pain or discomfort around third molarsc | |||
| No | 85 | 82 | 90 |
| Yes | 15 | 19 | 10 |
| Dental caries at distal of second molar | |||
| No | 94 | 96 | 96 |
| Yes | 6 | 4 | 4 |
| Dental caries on third molars | |||
| No | 92 | 94 | 92 |
| Yes | 8 | 6 | 8 |
| Paresthesia | |||
| No | 99.6 | 99 | 99.7 |
| Yes | 0.4 | 1 | 0.3 |
| Pericoronitis | |||
| No | 94 | 94 | 95 |
| Yes | 6 | 7 | 5 |
| TMD signs and symptoms (categories not exclusive) | |||
| None | 64 | 63 | 62 |
| Popping or clicking | 27 | 27 | 29 |
| Jaw pain on wide opening | 13 | 13 | 9 |
| Pain in temples, jaw joint, or jaw muscles | 17 | 20 | 16 |
| Maximum pocket depth at distal of second molarc | |||
| < 4 mm | 41 | 31 | 50 |
| ≥ 4 mm | 59 | 69 | 50 |
| Attachment loss at distal of second molar, mm | 0.75 (1.09) | 0.82 (1.11) | 0.57 (0.90) |
Note. TMD = temporomandibular joint disorder.
284 participants were lost to follow-up, and third molar removal status is unknown.
14 participants did not report race.
P < .05 between removal and retention group from bivariate generalized estimating equations logistic regression.
Of the 517 participants with follow-up data, 720 third molars were extracted from 201 (39%) participants. They were extracted on average 7.7 months after study entry (SD = 5.8 months). The majority of participants had all third molars extracted by an oral surgeon (73%) in a single visit (97%). Of the participants, 68% reported that intravenous sedation or general anesthesia was used, and 30% reported nitrous oxide was used. Participants who had at least 1 third molar extracted during follow-up were more likely to have pain or discomfort around third molars and periodontal pockets of 4 millimeters or more at the distal of second molars at baseline (Table 1).
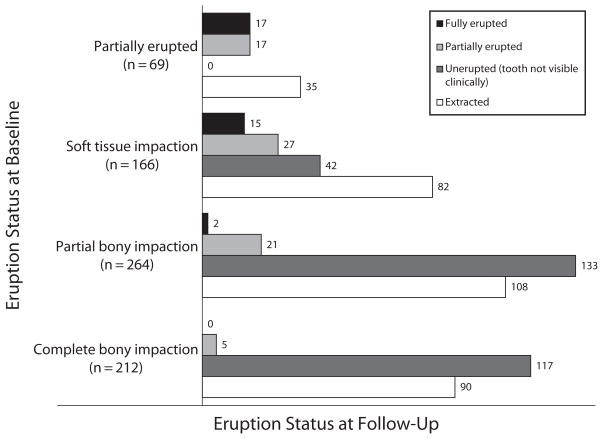
Among the 517 participants with follow-up data, 316 (61%) retained all existing molars during follow-up. Among the 218 participants who returned for the final examination, a general trend toward continued eruption of the third molars was evident (Figure 2). The more advanced the eruption status was at baseline, the more likely those teeth were to reach full eruption in the subsequent 2-year period. At final clinical examination, 26% of the retained third molars were partially or fully erupted.
FIGURE 2.
Change between baseline and study end in eruption status of third molars not fully erupted at baseline: Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry, Pacific Northwest, 2009–2012.
At baseline, 48 participants had 1 or more teeth diagnosed by the general dentist with pericoronitis (6% of all participants, or 20% of the participants with visible third molars). At final clinical examination, 9 participants had 1 or more teeth diagnosed with pericoronitis (4% of all participants, or 15% of the participants with visible third molars). Of 19 third molars with pericoronitis at baseline that were also assessed at the final clinical examination, 11 were extracted, and 1 had a second diagnosis of pericoronitis.
During follow-up, the incidence of self-reported TMJ clicking or popping was not significantly different between participants who did (11.7 per 100 person-years) and did not (15.4 per 100 person-years) undergo third molar removal (Table 2). However, the rates of TMD (jaw pain on wide opening and pain in the temples, jaw joint, or jaw muscles) were significantly higher after third molar removal (29.0 and 14.0 per 100 person-years, respectively) when compared with those not undergoing third molar removal (5.5 and 6.3 per 100 person-years). After adjustment for age and gender, the adjusted incidence risk ratios for pain on wide opening and pain in temples, jaw joint, or jaw muscles indicated 5.2 and 2.2 times higher risks in patients who underwent third molar removal than in patients who did not (95% confidence interval [CI] = 3.3, 8.3 and 1.2, 4.1, respectively; Table 3).
TABLE 2.
Outcomes of Third Molar Removal or Retention—Incidence Rates: Northwest Practice-based Research Collaborative in Evidence-based DENTistry, Pacific Northwest, 2009–2012
| Variable | Third Molar Removal
|
Third Molar Retention
|
||||
|---|---|---|---|---|---|---|
| No. Cases | Total, Person-Years | Rate per 100 Person-Years (95% CI) | No. Cases | Total, Person-Years | Rate per 100 Person-Years (95% CI) | |
| TMD | ||||||
| Jaw clicking or popping | 16 | 137 | 11.7 (7.2, 19.0) | 56 | 363 | 15.4 (12.3, 19.4) |
| Jaw pain on opening | 38 | 131 | 29.0 (20.5, 41.1) | 24 | 435 | 5.5 (3.8, 7.9) |
| Pain in temples, jaw joint, or jaw muscles | 19 | 135 | 14.0 (8.2, 23.9) | 27 | 431 | 6.3 (4.1, 9.6) |
| Either type of TMD pain symptoms | 43 | 126 | 34.3 (24.0, 48.9) | 38 | 431 | 8.8 (6.4, 12.2) |
| Paresthesia | ||||||
| Paresthesia of lips | 11 | 190 | 5.8 (3.0, 11.3) | 2 | 549 | 0.4 (0.1, 1.4) |
| Paresthesia of tongue | 8 | 191 | 4.2 (1.9, 9.1) | 3 | 546 | 0.5 (0.2, 1.7) |
| Paresthesia of lips, tongue, or both | 12 | 190 | 6.3 (3.4, 11.8) | 4 | 548 | 0.7 (0.3, 1.9) |
| Dental cariesa | ||||||
| Dental caries at distal of second molars | 1 | 528 | 0.2 (0.0, 1.4) | 4 | 678 | 0.6 (0.2, 1.5) |
| Dental caries at occlusal of third molars | NA | 9 | 275 | 3.3 (1.6, 6.8) | ||
| Dental caries at all other surfaces of third molars | NA | 3 | 1226 | 0.2 (0.1, 1.1) | ||
| Dental caries on third molars, overall | NA | 12 | 1501 | 0.8 (0.4, 1.7) | ||
Note. CI = confidence interval; NA = not applicable; TMD = temporomandibular joint disorder.
Dental caries are reported in surface-years
TABLE 3.
Association of Third Molar Removal Status and TMD—Adjusted Incidence Rate Ratio: Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry; Pacific Northwest; 2009–2012
| TMD Symptoms | Adjusted Incidence Rate Ratioa (95% CI) | P |
|---|---|---|
| Jaw clicking or popping | 0.8 (0.4, 1.3) | .32 |
| Jaw pain on wide opening | 5.2 (3.3, 8.3) | < .001 |
| Pain in temples, jaw joint, or jaw muscles | 2.2 (1.2, 4.1) | .014 |
| Either type of TMD pain symptoms | 3.8 (2.5, 5.7) | < .001 |
Note. CI = confidence interval; TMD = temporomandibular joint disorder.
Adjusted for age and gender.
The rates of self-reported paresthesia of the lip and tongue were also higher in those who had third molar removal (5.8 and 4.2 per 100 person-years, respectively) than in those who did not (0.4 and 0.5 per 100 person-years, respectively). When combined, the rate for paresthesia during this 2-year follow-up period was 6.3 per 100 person-years for the removal group and 0.7 per 100 person-years for the retention group (Table 2).
The rate of incident dental caries on the distal surfaces of second molars was 0.2 per 100 surface-years for those teeth adjacent to removed third molars and 0.6 per 100 surface-years for those teeth adjacent to retained third molars (Table 2). The rate of incident dental caries on third molars was 3.3 per 100 surface-years for the occlusal surfaces and 0.2 per 100 surface-years for non-occlusal surfaces.
The mean changes in attachment loss at the distal surfaces of the second molars during the follow-up period were 0.23 millimeter per year (95% CI = 0.03, 0.43) in sites adjacent to retained third molars and 0.12 millimeter per year (95% CI = −0.08, 0.32) in sites adjacent to removed third molars. When stratified by maxillary or mandibular arch, the results for attachment loss were essentially the same. After adjustment for age, gender, frequency of dental cleanings, and current smoking, the adjusted mean difference between the extraction and nonextraction adjacent sites was not statistically significant (0.06; 95% CI = −0.16, 0.28).
DISCUSSION
Because third molars are often removed prophylactically, it can be challenging to compare the sequela of removal versus retention over several years. This project was a natural history study in which patients were provided with third molar recommendations and then left to choose retention or removal. As stated previously, our interests were not in the immediate postsurgical period, because this interval has been well documented in the literature. Rather, we were most interested in medium-term outcomes, such as dental caries, periodontal disease progression, paresthesia, and TMJ symptoms.
Paresthesia has been reported to occur in about 1% to 5% of patients undergoing third molar removal.3,4,18 The rate of paresthesia for patients in our study (about 6%) is not far from the upper bounds of past reports.
The rate of TMJ symptoms reported by patients who had undergone third molar removal was much higher than expected (> 30% for either joint pain or muscular pain). The relative risk for TMD (3.8) was also quite high—more than double that reported in a prior retrospective study.16 A growing body of evidence has indicated that third molar removal may result in TMJ symptoms,16,19,20 and in fact the 2012 American Association of Oral and Maxillofacial Surgeons’8 Parameters of Care state that third molar removal may cause or exacerbate TMJ symptoms.
Many articles have stressed the importance of prophylactic removal of third molars to prevent periodontal pathology and the potential systemic health problems associated with periodontal disease.7,9,21–23 However, much of this research has been conducted by 1 group of investigators using 4-millimeter or deeper pockets as indicative of periodontal pathology. Obviously, a 4-millimeter pocket in the second and third molar area may be influenced by the eruption status of the third molar, and it is unclear whether a 4-millimeter pocket is always indicative of periodontal disease, which is usually based on attachment loss and the presence of inflammation rather than just pocket depth.24 Additionally, some recent publications have not indicated a causal relationship between periodontal disease and systemic health.25,26
Although attachment loss, rather than pocket depth, was the primary periodontal outcome in our study, we conducted a post hoc analysis of pocket depth change to allow for comparison with a prior study.27 We found that fewer than 3% of all second molar distal sites with 4 millimeters or more pocket depth at baseline had increases in pocket depth of 2 millimeters or more during the follow-up period, regardless of third molar removal. This previous study reported that 38% of second molar distal sites with 4 millimeters or more pocket depth at baseline had increases in pocket depth of 2 millimeters or more during the follow-up period of 2.2 years.27 These rates are considerably higher than what we observed in our study. However, it is difficult to directly compare our study with this previous study because their patients were on average 7 years older, with most third molars partially or fully erupted.
At the patient level, 1 in 5 participants with visible third molars at baseline had evidence of pericoronitis. The low occurrence of repeated diagnosis of pericoronitis at baseline and follow-up might suggest that spontaneous resolution is common. However, another possibility is that teeth with pericoronitis might be preferentially removed, thus masking a higher rate of recurrence. Our results from a companion article are consistent with this theory.17
The incidence of caries on the distal surfaces of second molars was extremely low, whether third molars were removed or retained. In the patients who returned for a 2-year follow-up examination, fewer than 0.5% of surfaces displayed evidence of incident caries overall. It is possible that this low rate of new lesions was related to the low rate of prevalent decay noted at baseline. Only 6% of our patients exhibited evidence of decay at distal of second molars at enrollment. This rate compares with rates as high as 13% to 20% in other studies.28,29 The proportion of patients with decay or restoration in at least 1 third molar at baseline was 8%, which compares with a previous study reporting that 9% of third molars in participants younger than 25 years had caries.30 In the present study, almost all incident caries observed on third molars was on the occlusal surface. Although restoring third molars can be challenging, occlusal surfaces are usually the most accessible to dentists. Sealants may be beneficial if these teeth are being considered for retention.
On average, third molars that were not extracted displayed continued eruption over the 2-year period. In fact, we found it surprising that 50% of all third molars that were classified as partially erupted at the time of enrollment were classified as fully erupted at the end of the study. Even 18% of teeth classified as soft tissue impactions at baseline were considered fully erupted 2 years later. This information is generally in line with research conducted by Venta et al.,31 who reported on eruption for patients in their early 20s. Obviously, the favorable rates of eruption observed in this study may be affected by the possibility that teeth with poor eruption potential were preferentially targeted for removal. This issue highlights 1 major limitation of observational studies: the potential for confounding by indication.
This study also had other limitations. Patients were obviously influenced by the recommendations of their dentists, most of whom indicated that they favored third molar removal for prophylactic reasons. Regardless of their dentists’ recommendations, patients were allowed to self-select whether they would or would not undergo third molar removal, and certainly many factors, such as availability of insurance coverage and patient symptoms, influenced the decision. It is likely that this self-selection resulted in nonequivalence of the extraction and nonextraction groups for various potentially confounding factors, many of which would be difficult to address. However, randomizing patients to retain or remove third molars prophylactically could present a patient acceptance challenge. Another limitation was the 2-year follow-up period. It would be desirable to follow these patients for longer than 2 years, perhaps for as long as a decade until patients neared their 30s. The response rate for the questionnaires, which ranged from 40% to 50% for the 3 time points, was lower than anticipated, even though we offered incentives and facilitated access to questionnaires with embedded links in e-mails. Perhaps the low rates should not be unexpected given the age of our patients and the fact that many transitioned into college or the workforce during the 2-year follow-up period. We also fell short of our target of 300 participants for the 24-month follow-up examinations. One positive factor is that the characteristics of patients who did return questionnaires and did undergo the final examination were relatively similar to the characteristics of the entire sample at baseline. Strengths of this study are the multisite structure of the network, which improves generalizability to broader populations.
The debate on third molar management has existed for many decades. A PubMed search conducted in January 2013 using the term “third molar” resulted in more than 7000 articles, and restricting the search to systematic reviews still netted almost 100 references. With all this literature available in peer-reviewed journals, it is interesting to cite a recent systematic review that was conducted under the auspices of the Cochrane Collaboration.32 This systematic review investigated randomized clinical trials on surgical removal versus retention for the management of asymptomatic third molars. After an extensive search, Mettes et al. identified only 1 trial that met their inclusion criteria, and the only outcome reported in that trial was that third molar removal or retention did not appear to be associated with lower incisor crowding. Their conclusion was that the evidence to “support or refute routine removal of asymptomatic impacted wisdom teeth in adults” is insufficient.32(p2) This systematic review highlights the need for better research on the topic of third molars.
Surely, some third molars, perhaps many third molars, should be removed because of insufficient space, poor eruption paths, recurrent pericoronitis, periodontal disease, or other pathology. However, it also seems likely that in some individuals, third molars might have sufficient space and exist for a lifetime as healthy, functional teeth. Our charge, as dentists, is to thoroughly assess a patient’s unique circumstances, to educate our patients on their condition, to utilize the existing evidence, and to provide our best advice and care for the management of their particular oral condition. Third-molar decisions should be no different.
In summary, our study provides information on a 2-year observation period of patients in their late teens and early 20s when decisions are often made regarding third molar removal. The network setting allowed the recruitment of a large number of participants, and we were able to investigate conditions related to both retention and removal. We report the following conclusions in a population of patients, 79% of whom were covered by dental insurance.
The rates of paresthesia and TMD symptoms were significantly higher in patients who underwent third molar removal, and these effects lasted longer than the immediate postsurgical period.
The average rate of attachment loss at distal sites of second molars was minimal over a 2-year period, regardless of third molar retention or removal.
The incidence of caries on the distal surface of the second molars was less than 1%. For third molars, the caries rate was approximately 3.3% on the occlusal surfaces.
When third molars were not removed, considerable eruption occurred during the 2-year period.
Acknowledgments
This article was submitted on behalf of the Northwest PRECEDENT network, with support from the National Institute of Dental and Craniofacial Research (DE016750 and DE016752), National Institutes of Health, Bethesda, MD.
We thank the dentist-investigator members of Northwest PRECEDENT and their staff for their invaluable contributions.
Footnotes
Reprints can be ordered at http://www.ajph.org by clicking the “Reprints” link.
Contributors
G. J. Huang conceptualized the study, developed the protocol with the study team, supervised the conduct of the study, interpreted the data, and wrote the first draft of the article. J. Cunha-Cruz developed the protocol and clinical research forms with the study team, assisted in study supervision and conduct, interpreted the data, and assisted with article preparation. M. Rothen was the lead regional coordinator for Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (PRECEDENT) and assisted in study supervision and conduct, as well as article preparation. C. Spiekerman conducted the data analysis and assisted with article preparation. M. Drangsholt assisted in developing the protocol and with article preparation. L. Anderson and G. A. Roset collected data and assisted with article preparation.
Human Participant Protection
The institutional review board at the University of Washington reviewed and approved the study protocol. All participants provided informed consent.
Contributor Information
Greg J. Huang, Department of Orthodontics, School of Dentistry, University of Washington, Seattle.
Joana Cunha-Cruz, Department of Oral Health Sciences, School of Dentistry, University of Washington, Seattle.
Marilynn Rothen, Regional Clinical Dental Research Center, School of Dentistry, University of Washington, Seattle.
Charles Spiekerman, Department of Oral Health Sciences, School of Dentistry, University of Washington, Seattle.
Mark Drangsholt, Department of Oral Medicine, School of Dentistry, University of Washington, Seattle.
Loren Anderson, Private practice, Kennewick, WA.
Gayle A. Roset, Private practice, Billings, MT.
References
- 1.Eklund SA, Pittman JL. Third-molar removal patterns in an insured population. J Am Dent Assoc. 2001;132(4):469–475. doi: 10.14219/jada.archive.2001.0209. [DOI] [PubMed] [Google Scholar]
- 2.Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J Public Health. 2007;97(9):1554–1559. doi: 10.2105/AJPH.2006.100271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Osborn TP, Frederickson G, Jr, Small IA, Torgerson TS. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg. 1985;43(10):767–769. doi: 10.1016/0278-2391(85)90331-3. [DOI] [PubMed] [Google Scholar]
- 4.Bruce RA, Frederickson GC, Small GS. Age of patients and morbidity associated with mandibular third molar surgery. J Am Dent Assoc. 1980;101(2):240–245. doi: 10.14219/jada.archive.1980.0183. [DOI] [PubMed] [Google Scholar]
- 5.de Boer MP, Raghoebar GM, Stegenga B, Schoen PJ, Boering G. Complications after mandibular third molar extraction. Quintessence Int. 1995;26(11):779–784. [PubMed] [Google Scholar]
- 6.Phillips C, White RP, Jr, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg. 2003;61(12):1436–1448. doi: 10.1016/j.joms.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Blakey GH, Hull DJ, Haug RH, Offenbacher S, Phillips C, White RP., Jr Changes in third molar and non-third molar periodontal pathology over time. J Oral Maxillofac Surg. 2007;65(8):1577–1583. doi: 10.1016/j.joms.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 8.American Association of Oral and Maxillofacial Surgeons. [Accessed February 6, 2013];Parameters of care: clinical and practice guidelines for oral and maxillofacial surgery. 2012 Available at: http://www.mfch.cz/doc/ParCare2012%20Complete.pdf.
- 9.White RP., Jr Progress report on third molar clinical trials. J Oral Maxillofac Surg. 2007;65(3):377–383. doi: 10.1016/j.joms.2006.10.054. [DOI] [PubMed] [Google Scholar]
- 10.Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003;61(12):1379–1389. doi: 10.1016/j.joms.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Edwards MJ, Brickley MR, Goodey RD, Shepherd JP. The cost, effectiveness and cost effectiveness of removal and retention of asymptomatic, disease free third molars. Br Dent J. 1999;187(7):380–384. doi: 10.1038/sj.bdj.4800285. [DOI] [PubMed] [Google Scholar]
- 12.Tulloch JFC, Antczak-Bouckoms AA, Ung N. Evaluation of the costs and relative effectiveness of alternative strategies for the removal of mandibular third molars. Int J Technol Assess Health Care. 1990;6(4):505–515. doi: 10.1017/s0266462300004177. [DOI] [PubMed] [Google Scholar]
- 13.Song F, O’Meara S, Wilson P, Golder S, Kleijnen J. The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth. Health Technol Assess. 2000;4(15):1–55. [PubMed] [Google Scholar]
- 14.American Public Health Association. [Accessed July 15, 2013];Opposition to prophylactic removal of third molars (policy no. 20085) 2008 Available at: http://www.apha.org/advocacy/policy/policysearch/default.htm?id=1371.
- 15.Morant H. NICE issues guidelines on wisdom teeth. BMJ. 2000;320(7239):890. [PubMed] [Google Scholar]
- 16.Huang GJ, Rue TC. Third-molar extraction as a risk factor for temporomandibular disorder. J Am Dent Assoc. 2006;137(11):1547–1554. doi: 10.14219/jada.archive.2006.0090. [DOI] [PubMed] [Google Scholar]
- 17.Cunha-Cruz J, Rothen M, Spiekerman C, et al. Recommendations for third molar removal: a practice based cohort study. Am J Public Health. 2014;104(4):735–743. doi: 10.2105/AJPH.2013.301652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldberg MH, Nemarich AN, Marco WP., 2nd Complications after mandibular third molar surgery: a statistical analysis of 500 consecutive procedures in private practice. J Am Dent Assoc. 1985;111(2):277–279. doi: 10.14219/jada.archive.1985.0098. [DOI] [PubMed] [Google Scholar]
- 19.Juhl GI, Jensen TS, Norholt SE, Svensson P. Incidence of symptoms and signs of TMD following third molar surgery: a controlled, prospective study. J Oral Rehabil. 2009;36(3):199–209. doi: 10.1111/j.1365-2842.2008.01925.x. [DOI] [PubMed] [Google Scholar]
- 20.Akhter R, Hassan NM, Ohkubo R, Tsukazaki T, Aida J, Morita M. The relationship between jaw injury, third molar removal, and orthodontic treatment and TMD symptoms in university students in Japan. J Orofac Pain. 2008;22(1):50–56. [PubMed] [Google Scholar]
- 21.Offenbacher S, Jared HL, O’Reilly PG, et al. Potential pathogenic mechanisms of periodontitis associated pregnancy complications. Ann Periodontol. 1998;3(1):233–250. doi: 10.1902/annals.1998.3.1.233. [DOI] [PubMed] [Google Scholar]
- 22.Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Periodontal disease and cardiovascular disease. J Periodontol. 1996;67(10 suppl):1123–1137. doi: 10.1902/jop.1996.67.10s.1123. [DOI] [PubMed] [Google Scholar]
- 23.Briggs JE, McKeown PP, Crawford VL, et al. Angiographically confirmed coronary heart disease and periodontal disease in middle-aged males. J Periodontol. 2006;77(1):95–102. doi: 10.1902/jop.2006.77.1.95. [DOI] [PubMed] [Google Scholar]
- 24.Michalowicz BS, Hodges JS, Pihlstrom BL. Is change in probing depth a reliable predictor of change in clinical attachment loss? J Am Dent Assoc. 2013;144(2):171–178. doi: 10.14219/jada.archive.2013.0096. [DOI] [PubMed] [Google Scholar]
- 25.Lockhart PB, Bolger AF, Papapanou PN, et al. Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association? A scientific statement from the American Heart Association. Circulation. 2012;125(20):2520–2544. doi: 10.1161/CIR.0b013e31825719f3. [DOI] [PubMed] [Google Scholar]
- 26.Baccaglini L. A meta-analysis of randomized controlled trials shows no evidence that periodontal treatment during pregnancy prevents adverse pregnancy outcomes. J Am Dent Assoc. 2011;142(10):1192–1193. doi: 10.14219/jada.archive.2011.0089. [DOI] [PubMed] [Google Scholar]
- 27.Blakey GH, Jacks MT, Offenbacher S, et al. Progression of periodontal disease in the second/third molar region in participants with asymptomatic third molars. J Oral Maxillofac Surg. 2006;64(2):189–193. doi: 10.1016/j.joms.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 28.Falci SG, de Castro CR, Santos RC, et al. Association between the presence of a partially erupted mandibular third molar and the existence of caries in the distal of the second molars. Int J Oral Maxillofac Surg. 2012;41(10):1270–1274. doi: 10.1016/j.ijom.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 29.Ozeç I, Herguner Siso S, Tasdemir U, Ezirganli S, Goktolga G. Prevalence and factors affecting the formation of second molar distal caries in a Turkish population. Int J Oral Maxillofac Surg. 2009;38(12):1279–1282. doi: 10.1016/j.ijom.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 30.Shugars DA, Elter JR, Jacks MT, et al. Incidence of occlusal dental caries in asymptomatic third molars. J Oral Maxillofac Surg. 2005;63(3):341–346. doi: 10.1016/j.joms.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 31.Ventä I, Murtomaa H, Turtola L, Meurman J, Ylipaavalniemi P. Clinical follow-up study of third molar eruption from ages 20 to 26 years. Oral Surg Oral Med Oral Pathol. 1991;72(2):150–153. doi: 10.1016/0030-4220(91)90154-5. [DOI] [PubMed] [Google Scholar]
- 32.Mettes TD, Ghaeminia H, Nienhuijs ME, Perry J, van der Sanden WJ, Plasschaert A. Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth. Cochrane Database Syst Rev. 2012;6:CD003879. doi: 10.1002/14651858.CD003879.pub3. [DOI] [PubMed] [Google Scholar]