Abstract
Most of immunomodulatory materials (e.g., vaccine adjuvants such as alum) modulate adaptive immunity, and yet little effort has focused on developing materials to regulate innate immunity, which get mentioned only when inflammation affects the biocompatibility of biomaterials. Traditionally considered as short-lived effector cells from innate immunity primarily for the clearance of invading microorganisms without specificity, neutrophils exhibit key role in launching and shaping the immune response. Here we show that the incorporation of unnatural amino acids into a well-known chemoattractant—N-formyl-L-methionyl-L-leucyl-L-phenylalanine (fMLF)—offers a facile approach to create a de novo, multifunctional chemoattractant that self-assembles to form supramolecular nanofibrils and hydrogels. This de novo chemoattractant not only exhibits preserved cross-species chemoattractant activity to human and murine neutrophils, but also effectively resists proteolysis. Thus, its hydrogel, in vivo, releases the chemoattractant and attracts neutrophils to the desired location in a sustainable manner. As a novel and general approach to generate a new class of biomaterials for modulating innate immunity, this work offers a prolonged acute inflammation model for developing various new applications.
Keywords: Chemoattractant, fMLF, supramolecular hydrogels, controlled release, peptides, pharmaceutical formulation
Upon the breaching of the host physical barrier by intruding microorganisms, neutrophils, among all the leukocytes, are the first to influx into a focus of bacterial invasion for host defense.(1) Neutrophils used to be considered to function exclusively as the effector cells in the innate phase of the immune response. However, the old view was challenged since a growing body of evidence that neutrophils play a crucial role in framing immune response, both innate and adaptive immunity.(2, 3) For example, neutrophils are found to have a B cells-helper neutrophil population in the splenic marginal zone and these neutrophils can activate marginal zone B cells to secrete immunoglobulins against T cell-independent antigens.(4)
The efficient recruitment of neutrophils depends on many signals, including N-formyl peptides, chemokines, complement components and leukotrienes.(1) As the by-products of protein translation in the invading bacteria, N-formyl peptides form molecular gradients originating from the bacteria in the infected tissue. And the gradients of N-formyl peptides signal neutrophils to migrate (i.e., chemotaxis) towards their targets while overriding other minor signals, such as IL-8 and MIP-2.(1) Proposed in 1965 and confirmed in 1984, fMLF represents the best-known N-formyl peptide and one of the most well-established chemoattractants for neutrophils (Scheme 1).(5) Having a well-defined molecular structure, fMLF offers an opportunity for chemical modifications and for precise control and accurate understanding of immunomodulation at the molecular level. Recognized for its potential as a useful reagent to induce acute inflammation in vivo, fMLF, in the form of aqueous solution, has been injected subcutaneously,(6) intravenously,(7) intraplantarly,(8) intradermally,(9) or just topically applied on the microvasculature(10) to study the biology of neutrophils for various applications. Although the aqueous solution of fMLF is able to induce the accumulation of neutrophils, its effect is relatively weak and transient (2–6 hr.).11
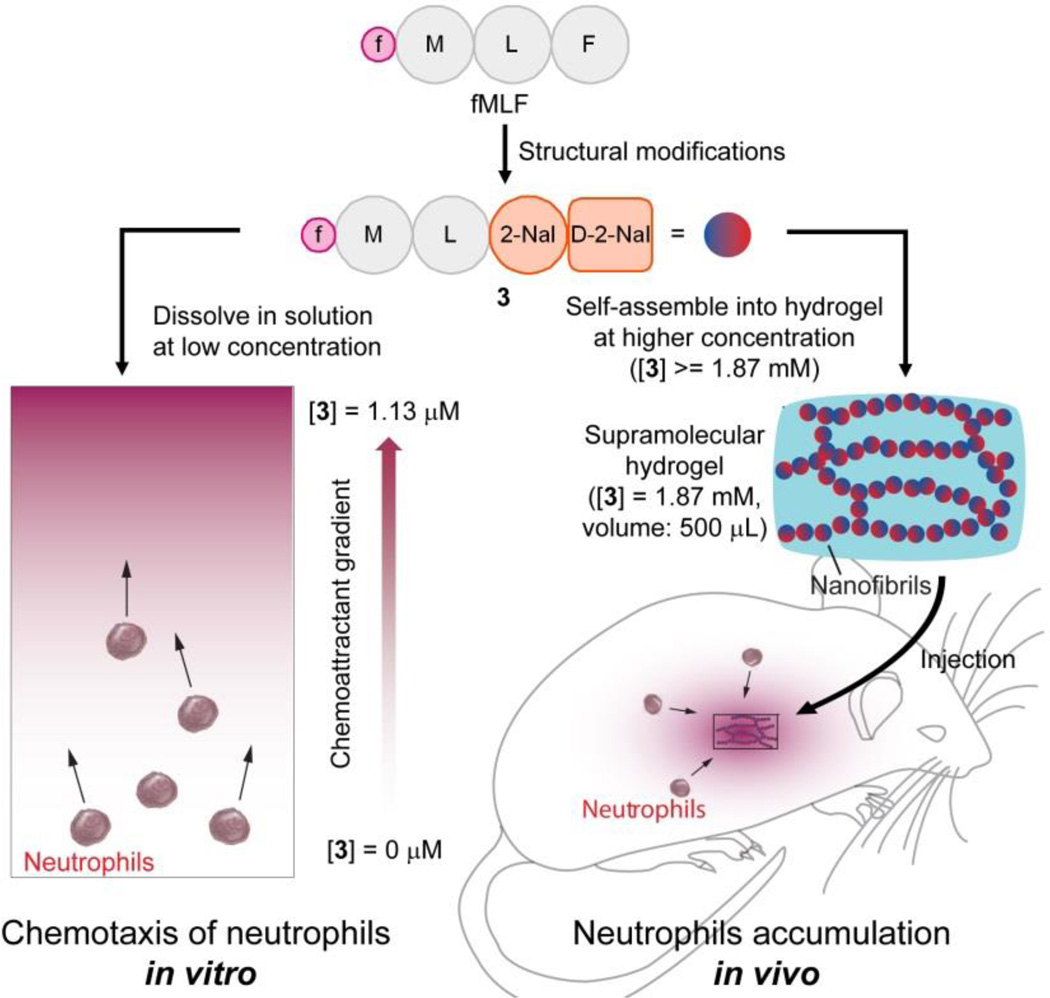
Scheme 1. The illustration of converting fMLF to a fMLF-based hydrogelator (3) to induce the chemotaxis of neutrophils in vitro and accumulation of neutrophils in vivo.
In vitro assay: 3 induces chemotaxis of murine and human neutrophils at the minimum effective concentrations of 1.13 µM and 11.3 nM, respectively. In vivo assay: the hydrogel of 3 slowly releases 3 for attracting neutrophils to the location of the hydrogel (at the dosage of 0.935 µmole per mouse). Denotation: f = formyl, M = l-methionyl residue, L = l-leucyl residue, F = l-phenylalaninyl residue, 2-Nal = l-3-(2–naphthyl)-alaninyl residue and d-2-Nal = d-3-(2–naphthyl)-alaninyl residue.
Instead of weak and transient acute inflammation, sometimes reagents that can elicit inflammation with a longer period are highly desired. However, the field of biomaterials concerning neutrophils and inflammation has been concerted on suppressing inflammation as the foreign body response to biomaterials.(12) Most recently, material scientist has started to pay attention to regulation of innate immunity and neutrophils, still focus on inflammation imaging(13) and suppression(14). Demonstrated in a recent work, the intratumoral injection of fMLF solution every two days after the inoculation of tumor cells slows the tumor growth in a xenograft tumor model.15 Similarly, the daily intratumoral injection of another chemoattractant, chemerin, decreases the tumor growth.16 In order to maintain a meaningful local concentration of the chemoattractants, both studies required frequent intratumoral injections.15, 16 Therefore, a formulation of chemoattractant (e.g., fMLF) for prolonged release, not only acts as a useful tool to study the biology of neutrophils over long duration, but also holds promises for therapeutic applications, like cancer treatment. This potential has already led to explorations of different formulations of fMLF,17–19 such as particles of fMLF in suspensions produced by sonication for studying neutrophil infiltration into pulmonary alveoli during murine pneumococcal pneumonia,(17) physically encapsulated N-formyl peptides in poly(lactic-co-glycolic acid) (PLGA) microbeads for inducing chemotaxis of neutrophils(18) or human monocytes and monocyte-derived dendritic cells (DCs)(19) in vitro. Based on the same idea of physically encapsulation by polymers, chemoattraction of regulatory T cells in vivo has been achieved by releasing CCL22 from PLGA particles.(20, 21) Despite this progress, heterogeneous suspensions of fMLF particles are far from ideal for in vivo applications due to differences between batches, and physical encapsulation using polymeric materials suffers from several limitations, such as burst release, low capacity for payload, and slow bioresorption of the polymeric materials, along with its inherent problem as mixtures of molecules with different molecular weight. These limitations demand the development of new approaches to attract neutrophil in vivo.
As an alternative, learning from nature, we chose to develop a biomimetic approach for sustained release of fMLF in vivo. Away from the dominant drug delivery idea of drug loading onto vehicles, such as biodegradable polymers, nature has provided a strategy, of which natural peptides and proteins self-assemble to form functional amyloids for sustained release.(22) Certain hormones such as prolactin and growth hormone form amyloids for storage, which dissolve slowly as a way for sustained or regulated hormone secretion.(23) This principle and mechanism has led to the development of supramolecular nanofibrils and hydrogels(24–26) of bioactive molecules as "self-delivery drugs".(22) In fact, a hydrogel of lanreotide acetate (i.e., Somatuline Depot),(27) based on this mechanism, has found clinical applications for treating acromegaly. This success has stimulated the development of supramolecular hydrogels as a unique depot for controlled release.(22, 27–29) However, existing examples of using self-assembly of peptides as releasing depot are almost all discovered by accident. The self-assembly property was not included in the molecular design of small molecular drug, which was discovered afterwards. However, a real challenge for “releasing depot” is how to modify existing bioactive molecules into the derivatives with preserved bioactivities while gaining the new function of self-assembly into nanofibrils. Intrigued by the simplicity and effectiveness of the "self-delivery drugs", also from the perspectives of peptide engineering and peptide formulation, we hypothesized that, by rational chemical derivatization, fMLF-derived peptides would form supramolecular hydrogels without compromising the biological efficacy of fMLF, and the corresponding hydrogels would deliver long-term efficacy for local accumulation of neutrophils by sustained release of the chemotactic hydrogelators (Scheme 1).
To demonstrate the concept illustrated in Scheme 1, we designed, synthesized, and evaluated several fMLF-derived molecules. And we obtained N-formyl-l-methionyl-l-leucyl-l-3-(2–naphthyl)-alaninyl-d-3-(2–naphthyl)-alanine (i.e., fMet-Leu-(2–Nal)-(d-2-Nal) shown as 3 in Scheme 1). In addition to behaving as a hydrogelator, 3 exhibits three advantageous features: ability to form a hydrogel efficiently (minimum gelation concentration (MGC) = 0.125 % w/v in DPBS buffer), enhanced stability against proteolysis, and preserved activity to both mouse and human neutrophils. Moreover, the hydrogel of 3, in the murine peritonitis model, stimulates a much longer-lasting pro-inflammatory phase than fMLF solution does, and exhibits a two orders of magnitude increase in neutrophil accumulation compared with that of fMLF solution. This work, for the first time, not only offers a facile approach to convert chemoattractants into hydrogels with exceptional biostability and tailored activity for controlled accumulation of neutrophils in vivo, but also validates the concept of the supramolecular hydrogelators acting as chemoattractants for homing cells in a sustainable manner. Besides being a useful tool to study the biology of innate immunity, this prolonged inflammation model holds promises for various potential therapeutic applications(30, 31) (e.g., inhibiting tumor growth,(15, 16) decreasing mortality caused by lethal sepsis after microbial infection(32) and acting as a basis for vaccine adjuvants(33)). Furthermore, the same principle can apply to the design of molecular hydrogels of formyl peptide receptor (FPR) antagonists, which finds direct applications in controlling pain caused by microbial infection.(34)
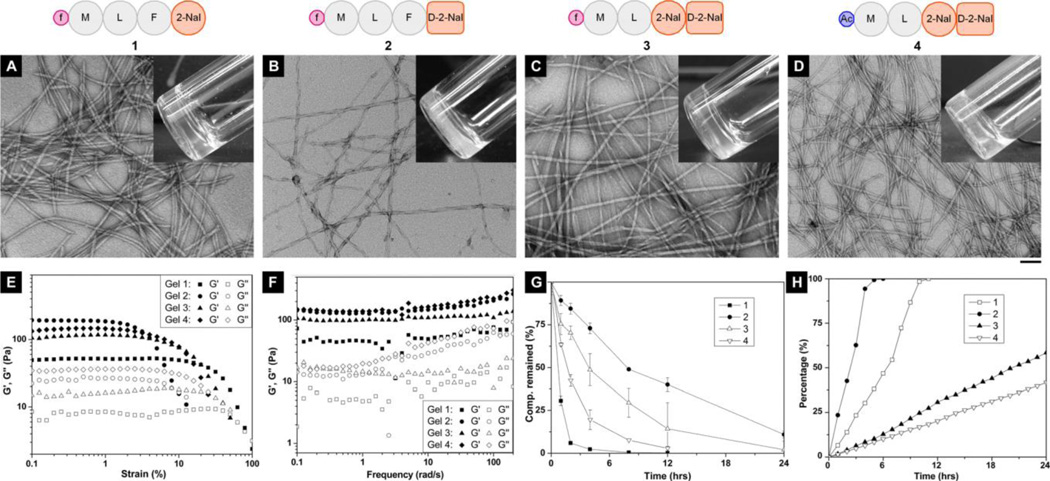
Figure 1 shows the schematic representation of the fMLF-derived peptides that self-assemble in water and form hydrogels and their characterizations (e.g., TEM, rheological properties, proteolytic stability, and the release profiles). The chemical structures are shown in Figure S1. Based on the structure of fMLF, we mainly modified fMLF at the C-terminus.(35, 36) Since naphthyl group promotes small peptides to form hydrogels,(27, 28) we connected a unnatural amino acid with naphthyl group (2–Nal) to fMLF to obtain fMLF-(2–Nal) (1). 1 self-assembles in Dulbecco's Phosphate-Buffered Saline (DPBS) buffer to form a supramolecular hydrogel at concentration of 0.2 w/v% (Figure 1A, inset). Transmission electron microscopy (TEM) reveals the network of nanofibrils (around 16 nm in diameters) (Figure 1A) in the hydrogel of 1 (0.2 w/v%), which shows the storage modulus (G’) of around 50 Pa and the critical strain of about 10.0 % (Figure 1E, F). As shown in Figure 1G, being incubated with a powerful protease (e.g., proteinase K), more than 90% of 1 undergoes hydrolysis in the first 2 hr. The release of 1 from its hydrogel finishes in about 8 hr. (Figure 1H).
Figure 1. Characterization of fMLF-derived hydrogelators (1, 2, 3) and a control peptide (4) and the hydrogels.
(A-D) The typical TEM images of negatively-stained fibrils of (A) the hydrogels of 1 (0.20 w/v%), (B) 2 (0.40 w/v%), (C) 3 (0.125 w/v%), and (D) 4 (0.075 w/v%), respectively, with the molecular representation on top (all hydrogels are at pH = 7.4 in DPBS buffer; the scale bar is 100 nm; denotation: Ac = acetyl; inset: the optical images of the hydrogels ). (E) Strain sweep and (F) frequency sweep of the hydrogels with the same concentrations as the hydrogels prepared for optical images and TEM. (G) The digestions of 1, 2 and 3, respectively, in 3.5 mL HEPES buffer solution of 1.4 mg (0.4 mg/mL) by adding 2.8 µL of proteinase K solution at 37°C. (H) The release profiles of the monomers from the hydrogels of 1, 2, 3 and 4 (0.4 w/v%) at 37°C.
To improve the stability of the hydrogelator against proteolytic enzymes, we replaced the 4th L-amino acid residue to the corresponding D-amino acid residue(37) to obtain a new peptide, fMLF-(d-2-Nal) (2), which still forms a hydrogel (Figure 1B, inset) but at a higher concentration (MGC: 0.4 w/v%) than that of 1. As shown in the TEM images, the nanofibrils in the hydrogel of 2 have diameters around 22 nm (Figure 1B). Rheology measurement shows the storage modulus and the critical strain of the hydrogel of 2 to be around 200 Pa and about 1.0 %, respectively (Figure 1E, F). The incorporation of a D-amino acid, indeed, substantially enhances proteolytic stability of 2 in comparison with that of 1. For example, in the presence of proteinase K, more than 80% and 40% of 2 remains after 2 hr. and after 12 hr., respectively (Figure 1G). The hydrogel of 2 collapses within the first 4 hr. and completely dissolves after 6 hr. in DPBS buffer at 37°C (Figure 1H), suggesting the relatively loose molecular packing in the hydrogel of 2.
Therefore, to obtain the fMLF derivative that has better gelation property, we changed the 3rd amino acid residue on 2 from Phe to 2-Nal, which gave the peptide fML-(2–Nal)-(d-2-Nal) (3). This simple change boosts intermolecular aromatic-aromatic interaction that promotes molecular self-assembly in water for hydrogelation, so 3 exhibits excellent gelation property with a MGC of 0.125 w/v% (Figure 1C, inset). The hydrogel prepared at the concentration of 0.125 w/v% has nanofibrils with diameters around 18 nm (Figure 1C), storage modulus around 100 Pa, and critical strain around 2.0 % (Figure 1E, F). 3 not only maintains the resistance to the proteinase K proteolysis (Figure 1G), but the improved gelation property also results in a longer sustained release of 3 in vitro. The hydrogel of 3 releases about 60 % of 3 after 24 hr. incubation at 37°C (Figure 1H).
The importance of the formyl group for the activities of the N-formyl peptides has been well documented and the replacement of formyl group by acetyl group in fMLF causes a 1000 to 10000 fold activity drop.(38, 39) Therefore, We also synthesized a control molecule of 3, AcML-(2–Nal)-(d-2-Nal) (4). It forms hydrogel (Figure 1D, inset) at a low concentration (MGC = 0.075 w/v%). The hydrogel of 4 contains the nanofibrils with diameters around 17 nm (Figure 1D), and has a storage modulus around 140 Pa and a critical strain around 2.0 % (Figure 1E, F). 4 is less stable against proteolytic digestion by proteinase K than 3. Matching with its excellent gelation property, the hydrogel of 4 also gradually releases 4 (with 40 % release at the first 24 hr.) (Figure 1H).
These four hydrogels, prepared at the MGCs of the hydrogelators, exhibit comparable storage moduli (G’), loss moduli (G’’), and critical strains (Figure 1E, F). Together with that the moduli of these hydrogels depend little on the frequency and the nanofibrils that serve as the matrices of the hydrogels have close diameters (16–22 nm), these results suggest the hydrogels of fMLF-based molecules share similar morphological and rheological properties. In addition, the MGC values of the hydrogelators correlate well with the release profiles of the hydrogelators. For example, the order of the hydrogelators having MGCs from high to low is 2, 1, 3 and 4, which is the same as the order of the hydrogelator release rates (Figure 1H). This trend suggests that molecular engineering of the hydrogelators to control the MGC values should be effective and useful for tailoring the release profiles of the chemoattractants.
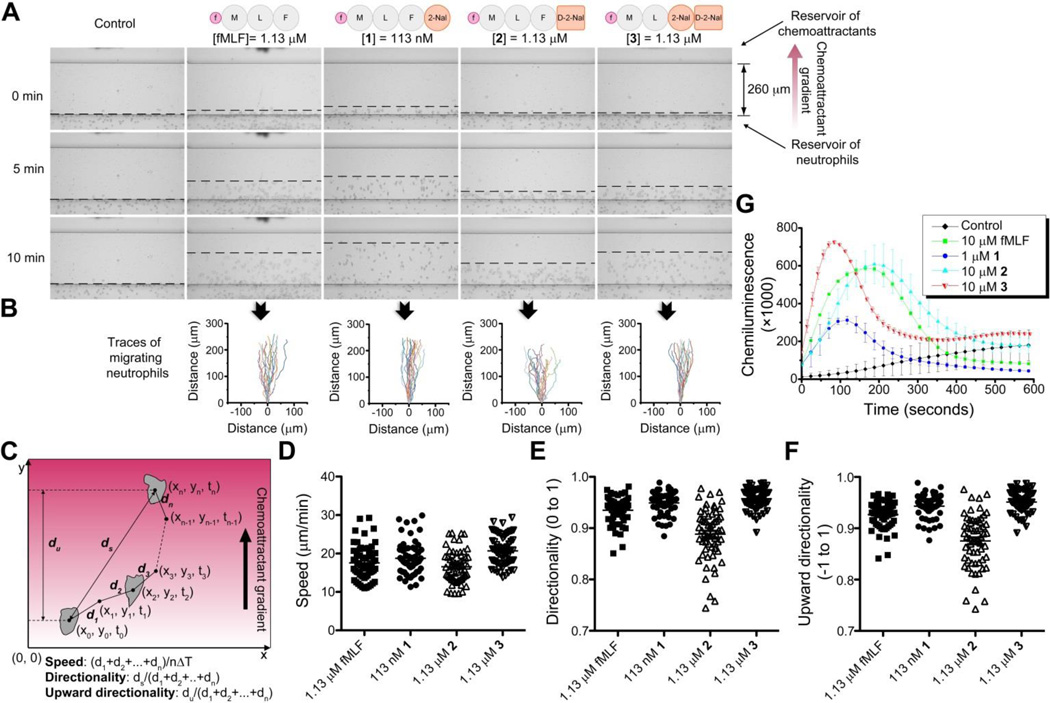
After confirming that the fMLF derivatives act as hydrogelators and exhibit proteolytic stability, we determined their activities to murine neutrophils by measuring chemotaxis and ROS production. Figure 2A shows the frames of the chemotaxis (performed on the EZ-TAXIScan(40)) induced by different molecules at 0, 5 and 10 min. to determine the minimum effective concentrations of the fMLF derivatives. The recorded frames of the first 20 minutes serve as the traces of cell migration (Figure 2B), which, being analyzed by the algorithm shown in Figure 2C, provide three important parameters for neutrophil chemotaxis: migration speed (Figure 2D), directionality (0 to 1) (Figure 2E), and upward directionality (−1 to 1) (Figure 2F) to characterize, respectively, how fast the neutrophils move, how straight they migrate, and how faithfully they follow the gradients of the chemoattractants. Chemoattratants will also induce the production of reactive oxygen species (ROS) by the NADPH oxidase assembled on the plasma membrane and phagosome.(1) Thereby the quantification of ROS production using isoluminol also indicates the activities of the chemoattractants. According to the Figure 2A-G, at its minimum effective concentration (1.13 µM), which is about 1000 times lower than the minimum gelation concentration, 3 not only induces chemotaxis of murine neutrophils as effectively as fMLF (i.e., the almost identical migration speed (Figure 2D) and directionality (Figure 2E), and slightly better upward directionality (Figure 2F)), but also exhibits slightly more potent activity for generation of ROS than that of fMLF (Figure 2G). The reason for the faster ROS production activated by 3 is currently unknown, which might be related to its interaction with formyl peptide receptors (FPRs). Interestingly, 1, at 113 nM, exhibits similar chemotactic activities as that of fMLF at 1.13 µM (Figure 2A), but generates only half as much ROS as fMLF (Figure 2G). 2 exhibits drops in the chemotactic activity and the ROS production when compared with fMLF, which matches the previously reported results that the D enantiomer is a less active chemoattractant than the L enantiomer.(41, 42) 4 failed to induced the chemotaxis even at 113 µM, a 100 fold of the minimum effective concentration of 3 (Figure S2), which matches the 1000 to 10000 fold activity drop reported in the literature.(38, 39) Therefore, 4 is considered having no chemotactic activity, and the hydrogel of 4 can be used as a control for the hydrogel of 3.
Figure 2. Induction of chemotaxis and ROS production of murine neutrophils by fMLF-derived hydrogelators (1, 2 and 3) in vitro.
(A) Snapshots of chemotaxis of murine neutrophils at 0, 5 and 10 minutes induced by the gradient of fMLF, 1, 2 and 3 performed on EZ-TAXIScan,(40) with the blank control. (B) The traces of 20 typical migrating neutrophils corresponding to different chemoattractants in the first 20 minutes. (C) The scheme and formulas for the calculation of the migration parameters. (D) The migration speed, (E) directionality, and (F) upward directionality of the murine neutrophils during chemotaxis from three independent samples, and each sample has 20 cell traces. (G) ROS production in the neutrophils (5 × 105) after stimulation with DMSO (0.1 v/v%, as the negative control), fMLF (10 µM), 1 (1 µM), 2 (10 µM), and 3 (10 µM).
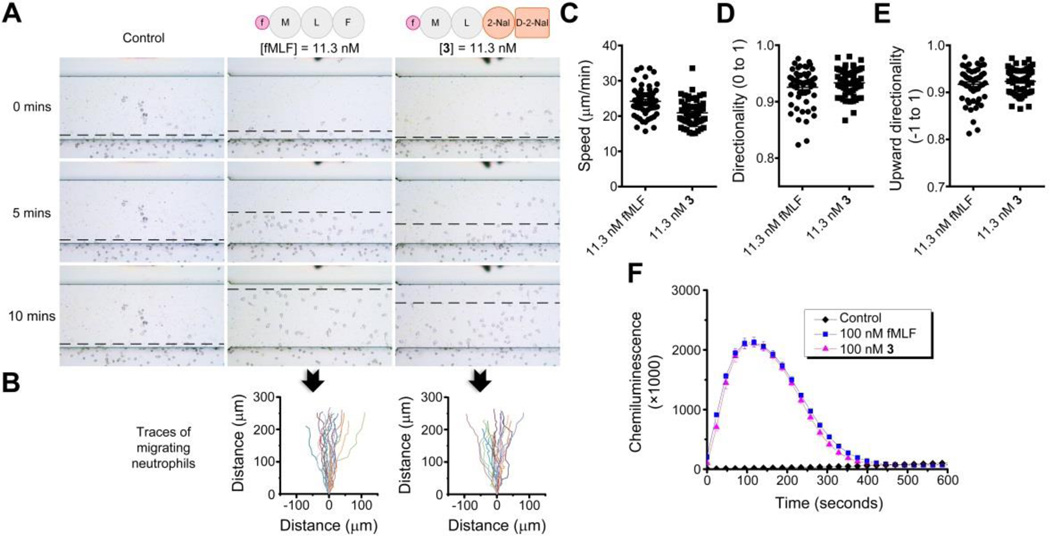
The above results clearly show that 3 fulfills all three criteria of the molecular design: excellent gelation property for the purpose of sustained release, fair stability against proteolysis, and well preserved chemotactic activity to murine neutrophils. Encouraged by the in vitro activity of 3 to attract murine neutrophils, we also investigated the activity of 3 on human neutrophils. As shown in Figure 3A, the minimum effective concentration of fMLF to human neutrophils is 11.3 nM determined by a ten-fold serial dilution, which is 100 times lower than the minimum effective concentration of fMLF to murine neutrophils (1.13 µM). This result agrees with the observation that fMLF’s activity to murine FPR is 100–10,000-fold less than to human and rabbit FPRs.(43) Moreover, 3, at 11.3 nM, exhibits the same effectiveness as fMLF to human neutrophils, as evidenced by the indistinguishable migration traces (Figure 3B), similar migration parameters (Figure 3C, 3D and 3E), and essentially identical ROS production (Figure 3F). Although the binding pockets of the mouse and human FPRs might be quite different, which is suggested by fMLF’s significantly different activities to FPRs,(43) the well preserved chemotactic activity of 3 to both mouse and human neutrophils indicates that 3 maintains the binding to both human and murine FPRs. How the modification can satisfy the binding to the two seemingly quite different pockets is surprisingly interesting and certainly deserves further exploration.
Figure 3. Induction of chemotaxis and ROS production of human neutrophils by 3 in vitro.
(A) Snapshots of chemotaxis of purified neutrophils from healthy human donors at 0, 5 and 10 minutes induced by fMLF, 3, and PBS (as the control) performed on EZ-TAXIScan. (B) The traces of 20 typical migrating neutrophils corresponding to different chemoattractants. (C) The migration speed, (D) directionality and (E) upward directionality of the human neutrophils during chemotaxis from three independent samples, and each sample has 20 cell migration traces. (F) ROS production in the neutrophils (5 × 105) after the addition of fMLF (100 nM), 3 (100 nM), and PBS (as the blank control).
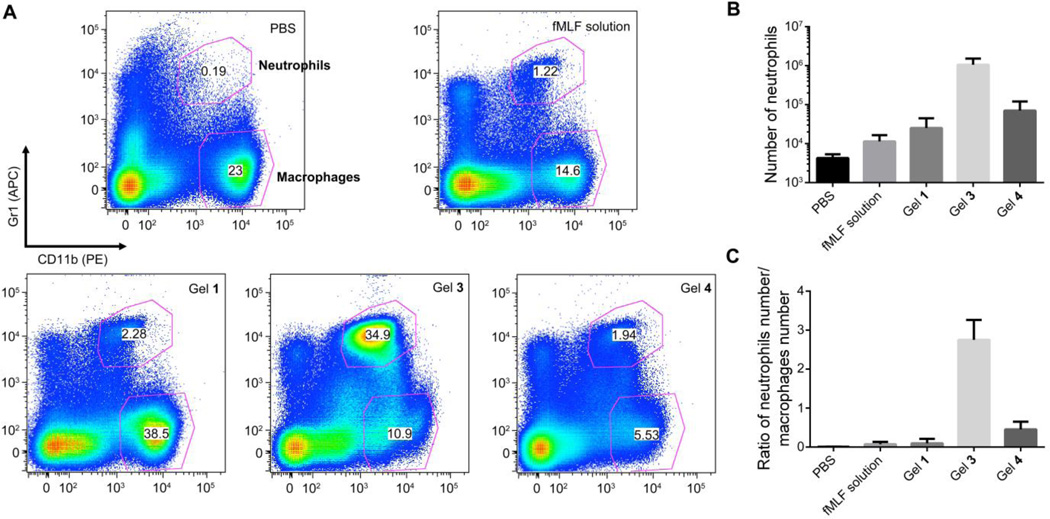
After successfully demonstrating the in vitro properties (i.e., gelation property for sustained release, stability, and the chemotactic activity to both mouse and human neutrophils) of 3, we used in vivo murine model to determine whether the hydrogel of 3 achieves a longer proinflammatory effect for attracting neutrophils than the solution of fMLF. We collected peritoneal lavages for flow cytometry 24 hr. after the injection of DPBS solution, fMLF solution, and the gels of 1, 3, and 4 into mice, respectively. In the representative flow cytometry plots (Figure 4A) using the markers Gr1 and CD11b, the double positive (Gr1+CD11b+) corresponds to neutrophils and the Gr1−CD11b+ are macrophages. The acute inflammation starts with the rapid influx of neutrophils and switches to monocyte-derived inflammatory macrophages, both from the blood. Although there’s not clear cut, the initial influx with a high percentage of neutrophils is considered as pro-inflammatory phase and the later stage with dominant macrophages is the resolution phase. Therefore, the ratio of neutrophils to macrophages is the indicator of the phase of inflammation.(44) As shown in Figure 4A, while the effect of the solution of fMLF almost disappears 24 hr after the injection, the hydrogel of 3, having the same amount of N-formyl peptides as the fMLF solution, still attracts high counts of neutrophils. According to the quantification (Figure 4B), the neutrophil number attracted by the hydrogel of 3 is two orders of magnitude higher than that of the solution of fMLF. Moreover, the ratio of the number of neutrophils vs the number of macrophages (Figure 4C) suggests that the inflammation of peritoneum (peritonitis) induced by the hydrogel of 3 is in a much earlier phase than the solution of fMLF, which is in the resolution phase of the inflammation. Although the hydrogel of 4 also results in stronger accumulation of neutrophils than the solution of fMLF does, the total number of neutrophils is still one order of magnitude lower than that induced by the hydrogel of 3 (Figure 4B). In addition, the ratio of neutrophils to macrophages (Figure 4C) clearly shows that the inflammation induced by the hydrogel of 4 is also close to the resolution phase. These results agree with the chemotactic activities of the hydrogelators 3 and 4, and suggest the accumulation of neutrophils caused by the hydrogel of 4 probably due to the inflammatory response toward stable foreign materials.
Figure 4. Hydrogels stimulate prolonged accumulation of murine neutrophils in vivo.
(A) Representative flow cytometry plots showing the neutrophils (Gr1+CD11b+) and the macrophages (Gr1−CD11b+) from the cells collected from the peritoneal lavage of wild-type mice 24 hr. after receiving the intraperitoneal injections (IP injections) of 500 µL of PBS (as the control), the solution of fMLF and the hydrogels of 1, 3 and 4 containing 0.935 µmole of peptides. (B) The number of neutrophils and (C) the ratio of the number of neutrophils vs the number of macrophages according to the FACS quantification from three independent experiments.
As the other control, the hydrogel of 1 results in similar results as the solution of fMLF: low total number of neutrophils and low ratio of neutrophils to macrophages 24 hr. after the injections (Figure 4B and 4C). Although 1 is roughly 10 times more chemotactically active as 3 (Figure 2), the hydrogel of 1 release faster than the hydrogel of 3, and 1 is less stable than 3. Therefore, the stronger accumulation of neutrophils induced by the hydrogel of 3 than by the hydrogel of 1 likely is not only due to the inflammatory response to stable foreign materials (as the case of the hydrogel of 4), but also originates from the sustained release of more stable chemoattractive hydrogelators. This result suggests that it is feasible to modulate inflammation by controlling the rheological properties of the hydrogels, the release profiles, and the stabilities of the hydrogelators.
Because neutrophils, as short-lived cells,(1) have a half-life of 1.5 hr. in the circulation in mice, the accumulation of neutrophils in this murine model is different from the other cell accumulations where the attracted cells remain alive. Therefore, the results, shown in Figure 4, could not be interpreted as the explosive accumulation of neutrophils induced at first couple of hr. all at once and then no activity follows. Instead, the results from 24 hr. strongly support that the accumulation of neutrophils is due to a constant attraction by the sustained release of the hydrogelators from the hydrogel of 3.
48 hr. after injections (Figure S3), the number of neutrophils attracted by the hydrogel of 3 is 1.1±0.3 X104 and the ratio of neutrophils to macrophages is 0.05±0.03, which shows that the peritonitis induced by the hydrogel of 3 also moves into the resolution phase, suggesting that the controlled release exhausts between 24 hr. and 48 hr. This might be related to the watery environment of peritoneum due to peritoneal fluid.
In summary, this study illustrates the evolution of multifunctional molecular hydrogelators for attracting neutrophils in vitro and in vivo. As the new class of “self-delivery” biomaterials, supramolecular hydrogels are only at its infancy for immunomodulation, with some initial but exciting explorations on vaccines for adaptive immunity.(45) Our work is the first example of using molecular self-assembly for the construction of immunomodulatory materials for innate immunity. The self-assembled hydrogel of fMLF-derived peptides, as a unique tool, can be very useful to researchers that need to induce sustained innate immune recruitment, which was unavailable before. Furthermore, this hydrogel also holds therapeutic potentials that have yet to be explored. More broadly, besides fMLF, there are many small biological peptides, playing essential roles in diverse biological functions. However, our preliminary study on the attracting neutrophils to the tumor sites on a B16-F10 melanoma model indicates that the peritumoral injection of the gel of 3 or the solution of fMLF affects little on the growth of the tumor. This result suggests more extensive study on this observation is needed. The concept illustrated in this work along with other work has the potential to modify those peptides to form supramolecular hydrogel without compromising the bioactivities. And the insight of molecular design gained from this work can be very useful. The general concept of using supramolecular hydrogel of bioactive small molecules as “self-delivery” system, thus, provides a novel approach to therapeutics and an attractive and validated alternative to the traditional drug delivery system.
Supplementary Material
Acknowledgements
The authors acknowledge the National Institute of Health (CA142746, B. X.; HL085100, AI076471, HL092020 and GM076084, H. R. L.), start-up fund of Brandeis (B. X.) and Chinese Council Scholarship (J. L. and J. S.). We thank Brandeis EM facility for the help on EM experiment, Isaac M. Chiu for the helpful discussions on the manuscript, and Subhanjan Mondal, Chunbao Guo and Hongmei Li for their help on mice experiment.
References
- 1.Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13:159–175. doi: 10.1038/nri3399. [DOI] [PubMed] [Google Scholar]
- 2.Nathan C. Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol. 2006;6:173–182. doi: 10.1038/nri1785. [DOI] [PubMed] [Google Scholar]
- 3.Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol. 2011;11:519–531. doi: 10.1038/nri3024. [DOI] [PubMed] [Google Scholar]
- 4.Puga I, Cols M, Barra CM, He B, Cassis L, Gentile M, Comerma L, Chorny A, Shan M, Xu W, Magri G, Knowles DM, Tam W, Chiu A, Bussel JB, Serrano S, Lorente JA, Bellosillo B, Lloreta J, Juanpere N, Alameda F, Baro T, de Heredia CD, Toran N, Catala A, Torrebadell M, Fortuny C, Cusi V, Carreras C, Diaz GA, Blander JM, Farber C-M, Silvestri G, Cunningham-Rundles C, Calvillo M, Dufour C, Notarangelo LD, Lougaris V, Plebani A, Casanova J-L, Ganal SC, Diefenbach A, Arostegui JI, Juan M, Yague J, Mahlaoui N, Donadieu J, Chen K, Cerutti A. B cell-helper neutrophils stimulate the diversification and production of immunoglobulin in the marginal zone of the spleen. Nat Immunol. 2012;13:170–180. doi: 10.1038/ni.2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ye RD, Boulay F, Wang JM, Dahlgren C, Gerard C, Parmentier M, Serhan CN, Murphy PM. International Union of Basic and Clinical Pharmacology. LXXIII. Nomenclature for the Formyl Peptide Receptor (FPR) Family. Pharmacological Reviews. 2009;61:119–161. doi: 10.1124/pr.109.001578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao J-L, Lee EJ, Murphy PM. Impaired Antibacterial Host Defense in Mice Lacking the N-formylpeptide Receptor. The Journal of Experimental Medicine. 1999;189:657–662. doi: 10.1084/jem.189.4.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jagels M, Chambers J, Arfors K, Hugli T. C5a- and tumor necrosis factor-alpha-induced leukocytosis occurs independently of beta 2 integrins and L-selectin: differential effects on neutrophil adhesion molecule expression in vivo. Blood. 1995;85:2900–2909. [PubMed] [Google Scholar]
- 8.Rittner HL, Hackel D, Voigt P, Mousa S, Stolz A, Labuz D, Schäfer M, Schaefer M, Stein C, Brack A. Mycobacteria Attenuate Nociceptive Responses by Formyl Peptide Receptor Triggered Opioid Peptide Release from Neutrophils. PLoS Pathog. 2009;5:e1000362. doi: 10.1371/journal.ppat.1000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng D, Nagy JA, Pyne K, Dvorak HF, Dvorak AM. Neutrophils Emigrate from Venules by a Transendothelial Cell Pathway in Response to FMLP. The Journal of Experimental Medicine. 1998;187:903–915. doi: 10.1084/jem.187.6.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oda T, Katori M. Inhibition site of dexamethasone on extravasation of polymorphonuclear leukocytes in the hamster cheek pouch microcirculation. Journal of Leukocyte Biology. 1992;52:337–342. doi: 10.1002/jlb.52.3.337. [DOI] [PubMed] [Google Scholar]
- 11.Colditz IG, Movat HZ. Kinetics of neutrophil accumulation in acute inflammatory lesions induced by chemotaxins and chemotaxinigens. The Journal of Immunology. 1984;133:2169–2173. [PubMed] [Google Scholar]
- 12.Williams DF. On the mechanisms of biocompatibility. Biomaterials. 2008;29:2941–2953. doi: 10.1016/j.biomaterials.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 13.Chen X, Wong R, Khalidov I, Wang AY, Leelawattanachai J, Wang Y, Jin MM. Inflamed leukocyte-mimetic nanoparticles for molecular imaging of inflammation. Biomaterials. 2011;32:7651–7661. doi: 10.1016/j.biomaterials.2011.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Z, Li J, Cho J, Malik AB. Prevention of vascular inflammation by nanoparticle targeting of adherent neutrophils. Nat. Nano. 2014;9:204–210. doi: 10.1038/nnano.2014.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang L, Khayat A, Cheng HS, Graves DT. The pattern of monocyte recruitment in tumors is modulated by MCP-1 expression and influences the rate of tumor growth. Laboratory Investigation. 1997;76:579–590. [PubMed] [Google Scholar]
- 16.Pachynski RK, Zabel BA, Kohrt HE, Tejeda NM, Monnier J, Swanson CD, Holzer AK, Gentles AJ, Sperinde GV, Edalati A, Hadeiba HA, Alizadeh AA, Butcher EC. The chemoattractant chemerin suppresses melanoma by recruiting natural killer cell antitumor defenses. The Journal of Experimental Medicine. 2012;209:1427–1435. doi: 10.1084/jem.20112124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gauthier J-F, Fortin A, Bergeron Y, Dumas M-C, Champagne M-E, Bergeron MG. Differential Contribution of Bacterial N-Formyl-Methionyl-Leucyl- Phenylalanine and Host-Derived CXC Chemokines to Neutrophil Infiltration into Pulmonary Alveoli during Murine Pneumococcal Pneumonia. Infection and Immunity. 2007;75:5361–5367. doi: 10.1128/IAI.02008-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kress H, Park J-G, Mejean CO, Forster JD, Park J, Walse SS, Zhang Y, Wu D, Weiner OD, Fahmy TM, Dufresne ER. Cell stimulation with optically manipulated microsources. Nat Meth. 2009;6:905–909. doi: 10.1038/nmeth.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao X, Jain S, Benjamin Larman H, Gonzalez S, Irvine DJ. Directed cell migration via chemoattractants released from degradable microspheres. Biomaterials. 2005;26:5048–5063. doi: 10.1016/j.biomaterials.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Jhunjhunwala S, Raimondi G, Glowacki AJ, Hall SJ, Maskarinec D, Thorne SH, Thomson AW, Little SR. Bioinspired Controlled Release of CCL22 Recruits Regulatory T Cells In Vivo. Advanced Materials. 2012;24:4735–4738. doi: 10.1002/adma.201202513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glowacki AJ, Yoshizawa S, Jhunjhunwala S, Vieira AE, Garlet GP, Sfeir C, Little SR. Prevention of inflammation-mediated bone loss in murine and canine periodontal disease via recruitment of regulatory lymphocytes. Proceedings of the National Academy of Sciences. 2013;110:18525–18530. doi: 10.1073/pnas.1302829110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao F, Ma ML, Xu B. Molecular hydrogels of therapeutic agents. Chemical Society Reviews. 2009;38:883–891. doi: 10.1039/b806410p. [DOI] [PubMed] [Google Scholar]
- 23.Maji SK, Perrin MH, Sawaya MR, Jessberger S, Vadodaria K, Rissman RA, Singru PS, Nilsson KPR, Simon R, Schubert D, Eisenberg D, Rivier J, Sawchenko P, Vale W, Riek R. Functional Amyloids As Natural Storage of Peptide Hormones in Pituitary Secretory Granules. Science. 2009;325:328–332. doi: 10.1126/science.1173155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Estroff LA, Hamilton AD. Water Gelation by Small Organic Molecules. Chemical Reviews. 2004;104:1201–1218. doi: 10.1021/cr0302049. [DOI] [PubMed] [Google Scholar]
- 25.Aida T, Meijer EW, Stupp SI. Functional Supramolecular Polymers. Science. 2012;335:813–817. doi: 10.1126/science.1205962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Branco MC, Sigano DM, Schneider JP. Materials from peptide assembly: towards the treatment of cancer and transmittable disease. Current Opinion in Chemical Biology. 2011;15:427–434. doi: 10.1016/j.cbpa.2011.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cherif-Cheikh R, Bismuth F, Torres ML, Alloza R, Bosch MT, Montes M, Fuster E, Valles J, Cordero JA, Peraire C, Obach R, Antonijoan R. Autogel™: a new lanreotide prolonged release formulation. Proc. Int. Symp. Control. Rel. Bioact. Mater. 1998;25:798–799. [Google Scholar]
- 28.Maji SK, Schubert D, Rivier C, Lee S, Rivier JE, Riek R. Amyloid as a Depot for the Formulation of Long-Acting Drugs. PLoS Biol. 2008;6:e17. doi: 10.1371/journal.pbio.0060017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vemula PK, Cruikshank GA, Karp JM, John G. Self-assembled prodrugs: An enzymatically triggered drug-delivery platform. Biomaterials. 2009;30:383–393. doi: 10.1016/j.biomaterials.2008.09.045. [DOI] [PubMed] [Google Scholar]
- 30.Dufton N, Perretti M. Therapeutic anti-inflammatory potential of formyl-peptide receptor agonists. Pharmacol. Ther. 2010;127:175–188. doi: 10.1016/j.pharmthera.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 31.Gavins FNE. Are formyl peptide receptors novel targets for therapeutic intervention in ischaemia–reperfusion injury? Trends Pharmacol. Sci. 2010;31:266–276. doi: 10.1016/j.tips.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim SD, Kim Y-K, Lee HY, Kim Y-S, Jeon SG, Baek S-H, Song D-K, Ryu SH, Bae Y-S. The Agonists of Formyl Peptide Receptors Prevent Development of Severe Sepsis after Microbial Infection. The Journal of Immunology. 2010;185:4302–4310. doi: 10.4049/jimmunol.1001310. [DOI] [PubMed] [Google Scholar]
- 33.Kurosaka K, Chen Q, Yarovinsky F, Oppenheim JJ, Yang D. Mouse Cathelin-Related Antimicrobial Peptide Chemoattracts Leukocytes Using Formyl Peptide Receptor-Like 1/Mouse Formyl Peptide Receptor-Like 2 as the Receptor and Acts as an Immune Adjuvant. J. Immunol. 2005;174:6257–6265. doi: 10.4049/jimmunol.174.10.6257. [DOI] [PubMed] [Google Scholar]
- 34.Chiu IM, Heesters BA, Ghasemlou N, Von Hehn CA, Zhao F, Tran J, Wainger B, Strominger A, Muralidharan S, Horswill AR, Wardenburg JB, Hwang SW, Carroll MC, Woolf CJ. Bacteria activate sensory neurons that modulate pain and inflammation. Nature. 2013;501:52–57. doi: 10.1038/nature12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sklar LA, Fay SP, Seligmann BE, Freer RJ, Muthukumaraswamy N, Mueller H. Fluorescence analysis of the size of a binding pocket of a peptide receptor at natural abundance. Biochemistry. 1990;29:313–316. doi: 10.1021/bi00454a002. [DOI] [PubMed] [Google Scholar]
- 36.Freer RJ, Day AR, Muthukumaraswamy N, Pinon D, Wu A, Showell HJ, Becker EL. Formyl peptide chemoattractants: a model of the receptor on rabbit neutrophils. Biochemistry. 1982;21:257–263. doi: 10.1021/bi00531a009. [DOI] [PubMed] [Google Scholar]
- 37.Powell M, Stewart T, Otvos L, Urge L, Gaeta F, Sette A, Arrhenius T, Thomson D, Soda K, Colon S. Peptide Stability in Drug Development. II. Effect of Single Amino Acid Substitution and Glycosylation on Peptide Reactivity in Human Serum. Pharm. Res. 1993;10:1268–1273. doi: 10.1023/a:1018953309913. [DOI] [PubMed] [Google Scholar]
- 38.Marasco WA, Showell HJ, Freer RJ, Becker EL. Anti-f Met-Leu-Phe: similarities in fine specificity with the formyl peptide chemotaxis receptor of the neutrophil. The Journal of Immunology. 1982;128:956–962. [PubMed] [Google Scholar]
- 39.Freer RJ, Day AR, Radding JA, Schiffmann E, Aswanikumar S, Showell HJ, Becker EL. Further studies on the structural requirements for synthetic peptide chemoattractants. Biochemistry. 1980;19:2404–2410. doi: 10.1021/bi00552a019. [DOI] [PubMed] [Google Scholar]
- 40.Kanegasaki S, Nomura Y, Nitta N, Akiyama S, Tamatani T, Goshoh Y, Yoshida T, Sato T, Kikuchi Y. A novel optical assay system for the quantitative measurement of chemotaxis. Journal of Immunological Methods. 2003;282:1–11. doi: 10.1016/j.jim.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 41.Vyas JM, Shawar SM, Rodgers JR, Cook RG, Rich RR. Biochemical specificity of H-2M3a. Stereospecificity and space-filling requirements at position 1 maintain N-formyl peptide binding. J. Immunol. 1992;149:3605–3611. [PubMed] [Google Scholar]
- 42.Aswanikumar S, Schiffmann E, Corcoran BA, Pert CB, Morell JL, Gross E. Antibiotics and peptides with agonist and antagonist chemotactic activity. Biochem. Biophys. Res. Commun. 1978;80:464–471. doi: 10.1016/0006-291x(78)90700-3. [DOI] [PubMed] [Google Scholar]
- 43.Gao JL, Murphy PM. Species and subtype variants of the N-formyl peptide chemotactic receptor reveal multiple important functional domains. Journal of Biological Chemistry. 1993;268:25395–25401. [PubMed] [Google Scholar]
- 44.Nathan C. Points of control in inflammation. Nature. 2002;420:846–852. doi: 10.1038/nature01320. [DOI] [PubMed] [Google Scholar]
- 45.Rudra JS, Tian YF, Jung JP, Collier JH. A self-assembling peptide acting as an immune adjuvant. Proceedings of the National Academy of Sciences. 2010;107:622–627. doi: 10.1073/pnas.0912124107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.