Abstract
We describe health and psychosocial outcomes of HIV+ Young transgender women (YTW) engaged in care across the United States. When compared to other behaviorally infected youth (BIY), YTW reported higher rates of unemployment (25% vs 19%), limited educational (42% vs 13%), and suboptimal ART adherence (51% vs 30%). There was no difference in likelihood of having a detectable viral load (38% vs 39%) between groups. However, particular isolating psychosocial factors (unstable housing, depression, and lack of social support for attending appointments) increased predicted probability of viral detection to a greater extent among YTW which may have important health implications for this marginalized youth population.
Keywords: HIV/AIDS, Transgender, LGBT Youth, Gender Identity, Access to Care
Background
Male-to-female transgender youth or young transgender women (YTW) face many challenges to their physical and emotional well-being, including high rates of homelessness, joblessness, victimization, suicide, and alarming rates of HIV infection.1–3 It is clear that social determinants play an important role in health outcomes for gender minority youth particularly including factors such as exclusion, isolation and fear.4,5 The increased prevalence of HIV infection among adult transgender women, is reported to be approximately 28% according to one meta-analysis,2 and has been attributed to several factors, including higher rates of sex work, risky sexual behaviors, substance abuse, and barriers to culturally appropriate gender-affirming healthcare including limited evidence for biomedical treatments, few trained providers, and high costs of essential medical, surgical and mental health treatments.1,3,6–12 While several studies indicate that YTW are a marginalized population at increased risk for HIV infection, little is known about psychosocial and health outcomes for HIV+ transgender individuals engaged in care.
The few studies to date of adult HIV+ transgender women have reported conflicting results regarding HIV-related health outcomes. In 2009, Melendez et al. showed that significantly fewer transgender women reported receiving ART and having an undetectable viral load when compared to HIV+ controls and Sevelius et al demonstrated higher rates of self-reported poor adherence among HIV+ transgender women when compared to other HIV+ adults.13,14 However, a more recent study with a large representative U.S.-based sample suggests that transgender adults have comparable rates of retention in care, receipt of ART, and achieving viral suppression to other HIV+ individuals.15 To date, there are limited data about specific risk behaviors and health outcomes among transgender youth living with HIV who are receiving regular HIV-related medical care. Additionally, recent studies have shown that multiple co-occurring psychosocial problems, particularly those that lead to social isolation and marginalization, have an additive effect on HIV risk behavior among YTW.8,16 However, it is unknown how these isolating psychosocial factors such as homelessness, depression, and lack of social support, that have been shown to impact health outcomes for transgender and HIV+ individuals in general,17–19 relate to disease specific outcomes among HIV+ YTW.
The purpose of this study was to: (1) describe HIV-related health and psychosocial outcomes of HIV+ YTW engaged in care compared to their behaviorally infected youth (BIY) counterparts; (2) compare the likelihood of viral suppression between HIV+ YTW and other BIY when controlling for other risk factors; and (3) examine whether particular isolating psychosocial risk factors (unstable housing status, depression, and lack of social support for engaging in medical care) modify the likelihood of having a detectable viral load among HIV+ YTW compared to matched BIY.
Methods
Participants, Setting, and Procedures
This study is a secondary data analysis of a multisite study conducted at 20 Adolescent Medicine Trials Units (AMTUs) participating in the Adolescent Trials Network (ATN), representing 15 cities across all geographic regions of the U.S. and Puerto Rico. The goal of this large cross-sectional study (N=2,200) was to describe behavioral risk factors and current health status in a sample of youth living with HIV across the U.S.20 The present study was based on the sub-sample of youth who were behaviorally infected and 12–24 years of age. Participants completed a psychosocial assessment using audio-computer assisted self-interviews (ACASI). Biomedical data (i.e. viral load levels, CD4 counts) were abstracted from medical records.
Measures
The following demographic information and other psychosocial data from the ACASI were used in this analysis:
Demographic Variables
Age, birth sex, current identified gender, race/ethnicity, route of HIV infection, educational attainment, and employment status were included.
Mental Health
The Brief Symptom Inventory (BSI) was used to assess mental health issues.21 Depression was defined by the clinical cut-off of T score ≥63. Individual items which assessed suicidal ideation and attempts, and mental health medications use in the last year were also included.
Substance Use
CRAFFT was used to assess substance use behaviors22 and scores of 2 or greater are suggestive of problem substance use, abuse or dependence.
Sexual Behavior
This study used the following measures developed by ATN scientists to assess aspects of sexual behavior:
Sexual Activity Measure
In this 38-item questionnaire, participants report protected and unprotected oral, vaginal, and anal sexual activity with HIV+ and HIV-/unknown status partners during the past 3 months.
Substance Use with Sexual Activity
In this 9-item questionnaire, participants report unprotected vaginal or anal sexual activity in the past three months after using alcohol or other drugs.
Adherence
Participants were asked to report the number of missed doses in the last 7 days and adherence rates were calculated as a proportion of the number of expected doses.
Biomedical Chart Abstraction
The most recent HIV-1 viral load and CD4 count were included. Viral load was dichotomized as detectable or not since assays with different lower limits of detection were used at different sites.
Subject Selection
Our total sample consisted of the 1,584 BIY who met inclusion criteria. Sixty-six youth were classified as transgender women because they selected “transgender” or “female” as their current gender and reported their birth sex to be male. Because the transgender youth comprised only 4% of the total sample, we matched each transgender participant randomly to 4 controls across strata of non-modifiable factors that included age, race and time since diagnosis. We incorporated sampling weights for controls as an inverse of the number of controls selected for each transgender subject, which equated to 0.25 for each control.
Analysis
We used weighted bivariate analysis using chi-square statistics to describe psychosocial, behavioral, and disease specific outcomes among YTW compared to all other BIY and randomly matched BIY. Across the independent variables, missingness was of greatest concern for the depression measure (aggregate missingness 5% across the composite scores of the BSI). Missing data were imputed using multiple imputation methods performed in SAS 9.3. Imputation models inclusive of the dependent variable and all independent variables available for multivariable regression were used to create five imputed datasets. Estimates were combined across individual datasets according to Rubin’s methodology23 using Stata mi commands (Stata 12.0, College Station, Texas). Survey-weighted logistic regression then determined the association of modifiable factors with the likelihood of unsuppressed viral load between YTW and matched BIY. Factors were selected for possible inclusion in the multivariable model if they were considered modifiable and if a trend (p<0.10) was detected in the unadjusted association with being transgender or not. Separately, because of limitations in transgender sample size, we also explored interactions of isolating psychosocial factors present (unstable housing, lack of social support for engagement in care, depression) that would modify the likelihood of unsuppressed viral load between HIV+ YTW and matched BIY. Each isolating factor was added to a regression model testing its association with detectable viral load, while controlling for the other independent variables selected for regression analysis (substance abuse, education and employment status). Results were then expressed as probabilities of detectable viral load by isolating factor and standardized by the other variables in the model.
Results
Mean age was 21.07 years (sd= 2.216) and there were no YTW under age 18. Most participants were African American (51%) and diagnosed for at least one year. See table 1 for bivariate comparison of demographics, psychosocial and disease related outcomes among HIV+ YTW compared to all BIY and matched controls. Of note, approximately two-thirds of YTW were unemployed compared to about one-third of other BIY. YTW were more than twice as likely than other BIY (42% vs 13%) to have not graduated from high school and one-quarter reported being homeless or unstably housed. No significant differences were seen in mental health and substance use. While there were no overall differences in sexual behavior, a higher proportion of YTW (15%) reported having more than 9 sexual partners in the last 3 months. In terms of health outcomes, there were no differences in disease-specific markers including viral suppression, although YTW were more likely to report sub-optimal ART adherence.
Table 1.
Bivariate comparison of demographics, psychosocial and disease related outcomes
| YTW (%) | All other BIY (%) | p-value | Matched BIY (%) | p-value | |
|---|---|---|---|---|---|
| Unstable housing | 25.0 | 16.7 | 0.054 | 18.8 | 0.270 |
| Low educational achievement (less than HS graduate) | 42.2 | 16.0 | 0.000 | 13.3 | 0.000 |
| Unemployed | 64.1 | 33.6 | 0.000 | 32.0 | 0.000 |
| Potential of a significant problem with Alcohol/Other Drug Abuse; CRAFFT ≥2 | 65.6 | 62.1 | 0.568 | 64.1 | 0.815 |
| Unprotected sex under influence of any alcohol/drug in the past 3 months | 18.0 | 25.4 | 0.444 | 23.2 | 0.471 |
| Depression; BSI >63 | 18.2 | 15.4 | 0.574 | 15.7 | 0.646 |
| Mental health medication use in past 12 months | 21.9 | 14.7 | 0.064 | 14.1 | 0.124 |
| Considered suicide in the past 12 months | 15.6 | 16.6 | 0.837 | 19.1 | 0.517 |
| Attempted suicide in the past 12 months | 7.8 | 6.7 | 0.723 | 7.8 | 1.000 |
| Disclosed HIV Status | 84.1 | 86.0 | 0.684 | 87.8 | 0.431 |
| Health Outcomes | |||||
| HIV classification: AIDS (CD4 count <200) | 23.4 | 24.6 | 0.952 | 27.0 | 0.568 |
| Other sexually transmitted disease diagnosis | 35.7 | 47.3 | 0.132 | 48.6 | 0.214 |
| Currently on ART medications | 51.6 | 49.6 | 0.950 | 50.0 | 0.823 |
| Ever on ART medications | 53.1 | 51.4 | 0.983 | 51.6 | 0.823 |
| Low (< 90%) medication adherence | 51.5 | 36.0 | 0.070 | 30.0 | 0.020 |
| Viral load undetectable | 37.5 | 35.8 | 0.932 | 39.2 | 0.801 |
| Provider Connection: I feel my provider | |||||
| Provides me with choices and options | 93.7 | 89.5 | 0.486 | 87.4 | 0.162 |
| Understands me | 95.2 | 89.0 | 0.242 | 88.7 | 0.128 |
| Conveys confidence in my ability to make changes | 92.2 | 88.6 | 0.581 | 87.1 | 0.261 |
| Encourages me to ask questions | 90.6 | 91.8 | 0.462 | 91.8 | 0.763 |
| Tries to understand how I see things before suggesting a new way to do things | 93.8 | 88.0 | 0.288 | 87.5 | 0.154 |
| Social Support: There are people in my life that are supportive about | |||||
| Keeping medical appointments | 75.0 | 84.1 | 0.028 | 81.6 | 0.238 |
| Taking HIV medication | 74.2 | 79.5 | 0.212 | 82.1 | 0.156 |
| Using condoms | 85.9 | 90.3 | 0.135 | 89.5 | 0.426 |
| Telling my partner about my HIV status | 59.0 | 71.6 | 0.021 | 73.6 | 0.024 |
| Avoiding drug use | 73.4 | 82.9 | 0.028 | 83.5 | 0.065 |
| Avoiding alcohol use | 71.9 | 74.4 | 0.508 | 69.0 | 0.657 |
| Number of male sexual partners in the last 3 months: | 0.057 | 0.053 | |||
| 0 Partners | 17.2 | 18.8 | -- | 13.0 | -- |
| 1 Partner | 18.8 | 27.6 | -- | 30.5 | -- |
| 2–9 Partners | 48.4 | 46.4 | -- | 50.0 | -- |
| >9 Partners | 15.6 | 7.2 | -- | 6.5 | -- |
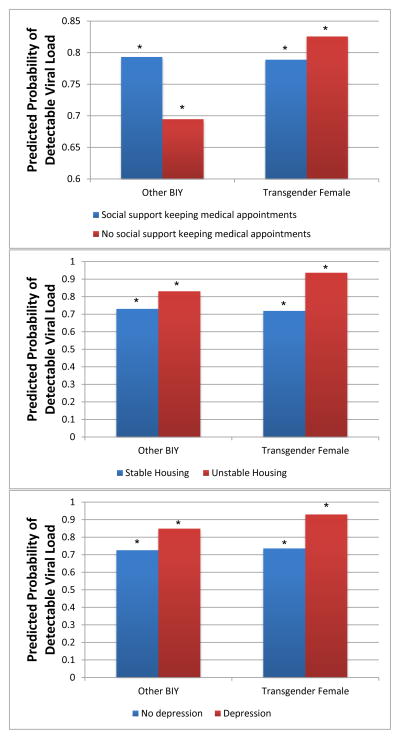
In the survey-weighted logistic regression when controlling for education, housing, substance use, lack of social support for keeping medical appointments, and depression there was no difference in likelihood of viral suppression among YTW versus matched BIY. However, when exploring interactions, figure 1 shows the predicted probability of detectable viral load by isolating factor. For YTW, there was a 19% increase (73.6% vs 92.9%) in the probability of having a detectable viral load among those who met clinical criteria for depression while there was a much smaller increase among other BIY (73.6% vs 84.8%). Similarly for housing status there was a 20% increase in probability of having a detectable viral load for YTW with unstable housing compared to only a 10% increase among other BIY. There was also a small but significant increase in the likelihood of viral detection among those YTW who lacked social support for engaging in medical care.
Figure 1.
Predicted Probability of Detectable Viral Load by isolating psychosoical factor
Discussion
Overall, the findings of this study are consistent with recent reports of HIV+ adults in care, indicating that health outcomes including rates of ART prescription and viral suppression are similar for HIV+ YTW when compared to their behaviorally infected counterparts.15 In terms of psychosocial risk profile, transgender youth in this sample were more likely to have low educational achievement and to be unemployed. YTW were also significantly more likely to have more than 9 sexual partners in the last 3 months which may suggest higher rates of sex work or survival sex. These findings are not surprising given the high rates of psychosocial problems reported among YTW previously.1,9
Interestingly, despite reporting significantly lower adherence rates to ART, in addition to other psychosocial risk factors, YTW were equally as likely to have achieved viral suppression when compared to their behaviorally infected counterparts. However, when exploring interactions we found that isolating psychosocial factors including depression and lack of stable housing were associated with a higher predicted probability of detectable viral load among YTW. The reasons for these findings are unclear. In the context of syndemic theory, as it has been used to describe risk for poor health outcomes among both transgender individuals and YMSM, it is possible that those transgender youth who are most marginalized are particularly sensitive to multiple co-occurring problems.16 The findings of no difference in viral suppression with lower reported adherence despite more isolating psychosocial factors suggests a particular resiliency in this subset of HIV+ YTW in care. The resilience in this population of HIV+ YTW in care is also supported by the low rates of suicidal ideation and attempts in the last 12 months among the YTW, 15.6% and 7.8% respectively, rates similar to the general adolescent population and much lower than previously reported for transgender youth.24,25 Another possible explanation is that YTW are benefiting more from culturally competent care than their counterparts. A recent qualitative study of adult HIV+ transgender women identified healthcare provider cultural competence as a key factor in facilitating HIV care engagement and treatment adherence.26 In our study, on measures that assessed patient-provider relationship, all BIY highly rated their providers, but there was a trend toward even higher ratings among YTW, perhaps suggesting that they may be deriving even greater benefit from relationships with clinicians who may possibly affirm their gender and better understand their medical/psychosocial needs.
This study has several limitations. First, the sample size is relatively small, albeit larger than has ever been described previously of HIV+ YTW engaged in care. Second, our cross-sectional data is insufficient to identify causal relationships, so the results are therefore hypothesis-generating. Third, these results may not be generalizable to all HIV+ transgender youth; particularly those not engaged in HIV care, a group about which relatively little is known.1,16
Despite these limitations, to our knowledge, this is among the first and largest studies of a national sample of HIV+ YTW engaged in care in the U.S. and shows similar rates of ART prescription and viral suppression when compared with other BIY in care. Additionally, by using statistical methods similar to Reisner et al,27 we were able, despite a small number of transgender subjects, to show that virologic outcomes for HIV+ YTW may be particularly negatively affected by certain isolating psychosocial factors in comparison to other BIY. Therefore, health and social service providers should specifically screen for these factors such as housing homelessness, depression, and limited social support for adherence to HIV-related medical treatment as these youth may be more likely to benefit from structural or behavioral interventions that address such factors. Future research and program development should add to the success of recently developed HIV prevention interventions for YTW like LifeSkills.28 Specifically, providers and researchers should consider addressing the factors identified in this study in potential adaptation of interventions like LifeSkills across the HIV care continuum with the ultimate goal of increasing the proportion of HIV+ YTW who achieve viral suppression. Finally, further work is needed to understand protective factors that may lead to the resiliency of HIV+ YTW engaged in care found in this study and particularly examining the role of culturally appropriate medical care, where multidisciplinary teams providers are trained to provide both gender-affirming and HIV care.
Acknowledgments
This work was supported by The Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) from the National Institutes of Health [U01 HD 040533 and U01 HD 040474] through the National Institute of Child Health and Human Development (B. Kapogiannis, S. Lee), with supplemental funding from the National Institutes on Drug Abuse (K. Davenny, S. Kahana) and Mental Health (P. Brouwers, S. Allison). The study was scientifically reviewed by the ATN’s Behavioral Leadership Group. Network, scientific and logistical support was provided by the ATN Coordinating Center (C. Wilson, C. Partlow) at The University of Alabama at Birmingham. Network operations and data management support was provided by the ATN Data and Operations Center at Westat, Inc. (J. Korelitz, B. Driver). We acknowledge the contribution of the investigators and staff at the following sites that participated in this study: University of South Florida, Tampa (Emmanuel, Lujan-Zilbermann, Julian), Children’s Hospital of Los Angeles (Belzer, Flores, Tucker), Children’s National Medical Center (D’Angelo, Hagler, Trexler), Children’s Hospital of Philadelphia (Douglas, Tanney, DiBenedetto), John H. Stroger Jr. Hospital of Cook County and the Ruth M. Rothstein CORE Center (Martinez, Bojan, Jackson), University of Puerto Rico (Febo, Ayala-Flores, Fuentes-Gomez), Montefiore Medical Center (Futterman, Enriquez-Bruce, Campos), Mount Sinai Medical Center (Steever, Geiger), University of California-San Francisco (Moscicki, Auerswald, Irish), Tulane University Health Sciences Center (Abdalian, Kozina, Baker), University of Maryland (Peralta, Gorle), University of Miami School of Medicine (Friedman, Maturo, Major-Wilson), Children’s Diagnostic and Treatment Center (Puga, Leonard, Inman), St. Jude’s Children’s Research Hospital (Flynn, Dillard), Children’s Memorial Hospital (Garofalo, Brennan, Flanagan), Baylor College of Medicine (Paul, Calles, Cooper), Wayne State University (Secord, Cromer, Green-Jones), Johns Hopkins University (Agwu, Anderson, Park), Fenway Community Health Center, Inc. (Mayer, George, Dormitzer), University of Colorado Denver (Reirden, Hahn, Witte). The investigators are grateful to the members of the local youth Community Advisory Boards for their insight and counsel and are particularly indebted to the youth who participated in this study. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of NIDA or any of the sponsoring organizations, agencies, or the U.S. government. This work was also supported by NIH K23MH102128 (Dowshen) and the Penn Mental Health AIDS Research Center (PMHARC) Pilot Award (Dowshen), an NIH-funded program (P30 MH 097488).
Footnotes
Author Disclosure Statement
Nadia Dowshen: No competing financial interests exist.
Meredith Matone: No competing financial interests exist.
Xianqun Luan: No competing financial interests exist.
Susan Lee: No competing financial interests exist.
Marvin Belzer: No competing financial interests exist.
Maria Isabel Fernandez: No competing financial interests exist.
David Rubin: No competing financial interests exist.
Contributor Information
Meredith Matone, Email: MatoneM@email.chop.edu.
Xianqun Luan, Email: LUAN@email.chop.edu.
Susan Lee, Email: lees8@email.chop.edu.
Marvin Belzer, Email: mbelzer@chla.usc.edu.
Maria Isabel Fernandez, Email: mariafer@nova.edu.
David Rubin, Email: RUBIN@email.chop.edu.
References
- 1.Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adolesc Health. 2006 Mar;38(3):230–236. doi: 10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 2.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008 Jan;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 3.Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. Am J Public Health. 2009 Apr;99(4):713–719. doi: 10.2105/AJPH.2007.132035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer GR, Hammond R, Travers R, Kaay M, Hohenadel KM, Boyce M. I don’t think this is theoretical; this is our lives”: how erasure impacts health care for transgender people. J Assoc Nurses AIDS Care. 2009 Sep-Oct;20(5):348–361. doi: 10.1016/j.jana.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Dysart-Gale D. Social justice and social determinants of health: lesbian, gay, bisexual, transgendered, intersexed, and queer youth in Canada. J Child Adolesc Psychiatr Nurs. 2010 Feb;23(1):23–28. doi: 10.1111/j.1744-6171.2009.00213.x. [DOI] [PubMed] [Google Scholar]
- 6.Melendez RM, Exner TA, Ehrhardt AA, et al. Health and health care among male-to-female transgender persons who are HIV positive. Am J Public Health. 2006 Jun;96(6):1034–1037. doi: 10.2105/AJPH.2004.042010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nemoto T, Operario D, Keatley J, Han L, Soma T. HIV risk behaviors among male-to-female transgender persons of color in San Francisco. Am J Public Health. 2004 Jul;94(7):1193–1199. doi: 10.2105/ajph.94.7.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sevelius JM, Reznick OG, Hart SL, Schwarcz S. Informing interventions: the importance of contextual factors in the prediction of sexual risk behaviors among transgender women. AIDS Educ Prev. 2009 Apr;21(2):113–127. doi: 10.1521/aeap.2009.21.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson EC, Garofalo R, Harris RD, et al. Transgender female youth and sex work: HIV risk and a comparison of life factors related to engagement in sex work. AIDS Behav. 2009 Oct;13(5):902–913. doi: 10.1007/s10461-008-9508-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2008 May 1;48(1):97–103. doi: 10.1097/QAI.0b013e31816e3971. [DOI] [PubMed] [Google Scholar]
- 11.Grossman AH, D’Augelli AR. Transgender youth: invisible and vulnerable. J Homosex. 2006;51(1):111–128. doi: 10.1300/J082v51n01_06. [DOI] [PubMed] [Google Scholar]
- 12.Mayer KH, Bradford JB, Makadon HJ, Stall R, Goldhammer H, Landers S. Sexual and gender minority health: what we know and what needs to be done. Am J Public Health. 2008 Jun;98(6):989–995. doi: 10.2105/AJPH.2007.127811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melendez RM, Pinto RM. HIV prevention and primary care for transgender women in a community-based clinic. J Assoc Nurses AIDS Care. 2009 Sep-Oct;20(5):387–397. doi: 10.1016/j.jana.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sevelius JM, Carrico A, Johnson MO. Antiretroviral therapy adherence among transgender women living with HIV. J Assoc Nurses AIDS Care. 2010 May-Jun;21(3):256–264. doi: 10.1016/j.jana.2010.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yehia BR, Fleishman JA, Moore RD, Gebo KA. Retention in care and health outcomes of transgender persons living with HIV. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2013 Sep;57(5):774–776. doi: 10.1093/cid/cit363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012 Sep;102(9):1751–1757. doi: 10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. J Homosex. 2006;51(3):53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- 18.Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007 Nov;11(6 Suppl):85–100. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- 19.Pinto RM, Melendez RM, Spector AY. Male-to-Female Transgender Individuals Building Social Support and Capital From Within a Gender-Focused Network. J Gay Lesbian Soc Serv. 2008 Sep 1;20(3):203–220. doi: 10.1080/10538720802235179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacDonell K, Naar-King S, Huszti H, Belzer M. Barriers to medication adherence in behaviorally and perinatally infected youth living with HIV. AIDS Behav. 2013 Jan;17(1):86–93. doi: 10.1007/s10461-012-0364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 22.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Archives of pediatrics & adolescent medicine. 2002 Jun;156(6):607–614. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 23.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999 Mar;8(1):3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 24.Grossman AH, D’Augelli AR. Transgender youth and life-threatening behaviors. Suicide Life Threat Behav. 2007 Oct;37(5):527–537. doi: 10.1521/suli.2007.37.5.527. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) [Accessed 2/10, 2014];Suicide Prevention: Youth Suicide. 2014 http://www.cdc.gov/violenceprevention/pub/youth_suicide.html.
- 26.Sevelius JM, Patouhas E, Keatley JG, Johnson MO. Barriers and Facilitators to Engagement and Retention in Care among Transgender Women Living with Human Immunodeficiency Virus. Ann Behav Med. 2013 Dec 7; doi: 10.1007/s12160-013-9565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reisner SL, White JM, Bradford JB, Mimiaga MJ. Transgender Health Disparities: Comparing Full Cohort and Nested Matched-Pair Study Designs in a Community Health Center. LGBT Health. 2014 doi: 10.1089/lgbt.2014.0009. Online Ahead of Print: April 10, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garofalo R, Johnson AK, Kuhns LM, Cotten C, Joseph H, Margolis A. Life skills: evaluation of a theory-driven behavioral HIV prevention intervention for young transgender women. J Urban Health. 2012 Jun;89(3):419–431. doi: 10.1007/s11524-011-9638-6. [DOI] [PMC free article] [PubMed] [Google Scholar]