Abstract
Objectives
Although schools and neighborhoods influence health outcomes, little is known about their relative importance, or the influence of one context after accounting for the other. Our objective was to simultaneously examine the influence of each setting on levels of depressive symptoms among adolescents.
Methods
Analyzing cross-sectional data from the National Longitudinal Study of Adolescent Health (Add Health), we used cross-classified multilevel modeling (CCMM) to examine between-level variation (random effects) and individual-, school-, and neighborhood-level predictors of adolescent depressive symptoms (fixed effects). We also compared CCMM results to results from a multilevel model (MLM) where either school or neighborhood was ignored.
Results
In CCMMs examining each context simultaneously, the school-level random effect was statistically significant and more than three times the neighborhood-level random effect, even after accounting for individual-level characteristics. While individual-level indicators (e.g., race/ethnicity, gender, socioeconomic status) were significantly associated with depressive symptoms, neither school- nor neighborhood-level fixed effects were. CCMM results showed that the between-level variance in depressive symptoms was driven largely by the school (ICC=3.0%) and not by the neighborhood (ICC=0.8%), as suggested by the school- (ICC=3.6%) and neighborhood-only (ICC=3.2%) MLM.
Conclusions
Schools appear more salient than neighborhoods in explaining variation in depressive symptoms. However, the school-level demographic variables examined were not determinants of youth depression. Future work using CCMM is needed to better understand the relative effect of schools and neighborhoods on youth mental health. These findings also underscore the need for CCMM over MLM when youth are nested in more than one context.
Depression is one of the most serious public health problems among adolescents in the United States. Large epidemiological studies estimate that 12% of youth meet lifetime diagnostic criteria for major depression or dysthymia (1) and that 29% of high school students report feeling sad or hopeless nearly every day in the past two weeks (2). Given that adolescent-onset depression is associated with many short- and long-term consequences, including suicidal thoughts and behaviors (3, 4), cigarette, alcohol, and drug use (5–7), and recurrent episodes of depression in adulthood (8, 9), there is an urgent need to understand the etiology of depression in adolescence.
Interest in the social determinants of depression – or how features of the broader social context in which adolescents are embedded affect their risk for depression – has received increased attention in the past decade. Neighborhood social environments have been primarily examined to date (10–14). This research suggests the racial/ethnic and socioeconomic composition and culture of the neighborhood (e.g. levels of social cohesion; norms related to relationships between neighbors) are associated with individual mental health outcomes, even after accounting for individual-level factors. Though schools are gaining more interest by public health researchers (15, 16), research on the role of schools in depression is lacking outside of a small number of studies. These studies have primarily focused on school connectedness and school socioeconomic status and found that higher levels of each are associated with lower levels of depressive symptoms in students (17–25). Additionally, most school-related studies have focused on individual-level, rather than multilevel associations (26–32).
Not only are schools understudied on their own, but their role in relation to neighborhoods is also poorly understood (33). Studies using cross-classified multilevel modeling techniques (CCMM), which explicitly allow researchers to disentangle the unique impact of multiple non-nested contexts—such as school and neighborhood environments—on health (34, 35), are rare. This is especially true for mental health outcomes. As a result, it remains unclear whether each context is important independent of the other and, if so, whether schools or neighborhoods are equally important determinants of adolescent depression or one context is more salient than the other.
A case could be made for the importance of either schools or neighborhoods. Schools are likely important determinants of depression because they serve more than 95% of the nation’s young people for approximately 6 hours per day (or upwards of 40% of student’s waking time during the school year) and at least 11 continuous years of their lives (36). Schools are also well-defined social institutions providing access to a range of supportive relationships that promote mental health (30, 37, 38). Neighborhoods, on the other hand, may be important because they are the setting where unstructured social activity occurs outside of school and during the summer (39, 40). Neighborhoods may also have a more direct influence on parents’ capacity to raise their children through shaping community norms, supervision/monitoring, collective efficacy, and reducing the burdens and stressors associated with caregiving (41, 42).
Studies that examine the salience of schools compared to neighborhoods (and vice versa) are needed, as schools and neighborhoods have increasingly become non-nested contexts in the United States. Indeed, a growing number of young people are attending schools outside of their neighborhoods, as a result of the popularity of school choice (e.g., charter schools; federal vouchers to attend private school) and the desire to close low performing schools (43, 44). Thus, schools and neighborhoods are no longer hierarchically nested for many youth, leading youth to experience non-neighborhood based schools, which may have different demographic features relative to their neighborhood of residence.
The objective of our study was to address these gaps in the literature by understanding the relative importance of neighborhoods and schools in youth depression. Specifically, we set out to: (1) determine the unique proportion of variance in depressive symptoms attributable to schools and neighborhoods (i.e., random effects of each context); and (2) examine the association between sociodemographic characteristics (e.g., socioeconomic status, race/ethnicity) at the individual-, school-, and neighborhood-level (i.e., fixed effects) on youth depression.
METHODS
Data
Data came from Wave I of the National Longitudinal Study of Adolescent Health (Add Health), one of the only nationally-representative longitudinal surveys of US adolescents that examines health and health-related behaviors and includes information about both school and neighborhood environments (45). Adolescents in grades 7–12 were recruited through school-based sampling and were first interviewed in 1994–1995 (Wave I) (18). A systematic random sample of high schools along with feeder schools (i.e., middle schools whose students matriculate at the selected high school) was selected. A total of 134 schools (79%) participated. An in-school survey was completed by 90,118 students. A random sample of these 90,118 students (as well as all students who were eligible to complete the in-school survey, but were absent on the day of administration) was invited to complete a more detailed in-home interview. 20,745 students completed the in-home interview (over 75% of those asked to participate did so). In addition, 17,670 caregivers (for 85% of in-home respondents) provided information at Wave I.
These cross-sectional analyses were based on an analytic sample of 16,172 students nested in 128 schools (median of 103.5 students per school ranging from 18 to 1,018) and 2,118 neighborhoods (median of 2 students per neighborhood ranging from 1 to 262, defined by census-tracts). This analytic sample was derived after eliminating youth (n=660) in the non-nationally-representative sample (i.e., who attended schools sampled for genetic analyses) or from schools that did not provide demographic data. We also excluded youth who were missing data on the outcome measure (n=38) or predictors and covariates (n=1,404). We restricted the analysis to youth who were White, Black, or Hispanic, given that students in other racial/ethnic groups were not sufficiently represented in Add Health to obtain robust group estimates (Native Americans n=105, <1%; Asians n=1189, 6%; Other n=1,177, 6%). Although Add Health is a longitudinal study, we pursued a cross-sectional analysis here because the majority of respondents resided in the same neighborhood and school in Wave II as they did in Wave I, and because Wave III and Wave IV were conducted when most respondents had graduated from high school.
Measures
Outcome: depressive symptoms
Depressive symptoms were assessed at Wave I using a 19-item adaptation of the Center for Epidemiological Studies of Depression Scale (CES-D) (46), a widely-used instrument to capture symptoms of depression. Youth reported how often they experienced each symptom in the past week, with responses ranging from “never or rarely” to “most or all of the time.” The adapted CES-D had good internal consistency reliability in this sample (Cronbach’s alpha=0.87). CES-D scores were slightly skewed towards lower values; as skew and kurtosis values were within reasonable limits (skew=1.15, kurtosis=1.89 (47)), and linear regression is robust to minor violations of normality (48), we did not conduct any transformations of the data.
We also examined the following predictors.
Socioeconomic Status (SES)
SES was obtained at the individual-, school-, and neighborhood-level using measures of parent education and parental receipt of public assistance. At the individual-level, highest level of parent education (defined as the highest level of education by the resident mother, resident father, or resident step-father/partner) was determined using items from the caregiver interview (or when missing, (in 12% of youth), the in-home version of the youth interview). We used responses to these items to create a binary variable (1=at least one parent graduated college; 0=neither parent graduated college). Parent receipt of public assistance at the individual-level was also determined from either the in-school youth or in-home caregiver surveys (1=either parent currently receiving public assistance; 0=not). The school-level SES predictors were calculated from the proportion of students within each school with a parent receiving public assistance and the proportion of students with at least one parent who had received a college degree. The aggregation of individual-level data was required as information about school-level SES was not directly available. At the neighborhood level, we used data from the 1990 Census to create neighborhood-level SES measures indicating the proportion of residents within each neighborhood who had received public assistance or had a college degree.
Racial/Ethnic Composition
Race/ethnicity was measured at the individual-, school-, and neighborhood-level. At the individual-level, we used a self-reported measure of race/ethnicity (1=non-Hispanic white; 2=non-Hispanic black; 3=Hispanic). We limited our analyses to these groups given the smaller number of participants from other racial/ethnic groups. We created a school-level measure by calculating the proportion of students within each school who were non-Hispanic white based on the in-school interview. At the neighborhood level, 1990 Census data were used to create a measure of the proportion of residents in the neighborhood who were non-Hispanic white.
Covariates
Adjusted models controlled for age (continuous) and sex (male=0; female=1).
Analysis
Our analyses proceeded in five steps. First, we estimated three sets of null or random intercept only multilevel models: (a) a school-only multilevel model (MLM), where adolescents were clustered in schools; (b) a neighborhood-only MLM, where adolescents were clustered in neighborhoods; and (c) a cross-classified multilevel model (CCMM), where adolescents simultaneously belong to both a school and neighborhood. These null models (Models 1A – 1C) allowed us to partition the variance in depressive symptoms into within and between components and estimate an intraclass correlation coefficient (ICC, i.e., the proportion of variation in the outcome that was due to differences across schools or neighborhoods, rather than differences across students). Second, we estimated a CCMM that contained individual-level predictors and covariates (Model 2) with the random effects of both schools and neighborhoods simultaneously accounted for. By including individual-level variables, we were able to evaluate the extent to which the between-level variance estimates for both schools and neighborhoods (i.e., random effect parameters) were due to the observed composition (i.e., the characteristics of individuals in a given school or neighborhood). Next, we added to Model 2 the school-level variables (Model 3) and neighborhood-level predictors (Model 4). Fourth, we fit a CCMM containing all individual-, school-, and neighborhood-level variables of interest (Model 5).
All analyses were conducted in MLwiN version 2.26 with Bayesian estimation procedures as implemented via Markov Chain Monte Carlo (MCMC) methods using Metropolis-Hastings algorithm (49). Parameter estimates (betas) and 95% confidence intervals (CI) are presented for fixed effect parameters. For random effect parameters, we present variance estimates and 95% CIs. We examined residual plots at each level of analysis to evaluate model diagnostics on the variance parameter; this enabled us to test model assumptions, detect outliers and influence points on model fit. Two-tailed p-values are presented for fixed effect parameters. One-tailed p-values are presented for residual variance terms, as values less than zero are implausible. Analyses were conducted using unweighted data, as weighting techniques for CCMM have not been established (50). A non-weighted analysis is appropriate as our emphasis was on tests of association, rather than deriving nationally representative estimates, and we adjusted our analyses for sample characteristics and thus reduced the heterogeneity in the sample (51).
RESULTS
Descriptive Analyses
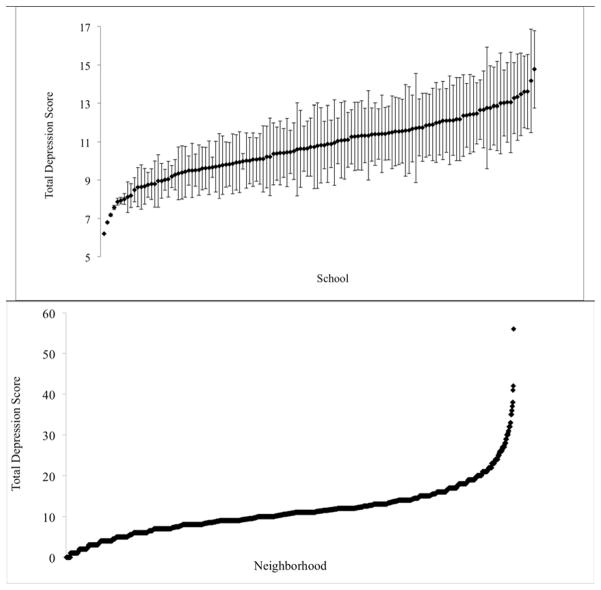
The sample was predominately white (58%), balanced by gender (51% female), and consisted largely of youth in mid-adolescence (mean age=15.6; SD=1.7). The sample was modestly disadvantaged, as 70% of adolescents had no parent with a college degree and 10% had at least one parent who was currently receiving public assistance. Youth reported an average depression score of 11.1 (SD=7.5; minimum=0, maximum=56). The average depressive symptoms score was similar across neighborhoods (neighborhood mean=11.2; SD=6.1) and schools (school mean=10.8; SD=1.6) yet there was marked variation within schools and neighborhoods (Figure 1). Average SES was similar across schools and neighborhoods. Specifically, the school percentage of parents on public assistance was 10.4% (SD=9.4; minimum=0; maximum=45.4%) and the neighborhood percentage of residents on public assistance was 10.7% (SD=10.0; minimum=0; maximum=67.5%). Similarly, the school percentage of parents who had less than a college degree was 68.3% (SD=16.9; minimum=8.8; maximum=94.5%) and the neighborhood percentage of parents who had less than a college degree was 76.6% (SD=14.6; minimum=17.5; maximum=100%).
Figure 1. Distribution of Depressive Symptoms Within and Between Schools (N=128) and Neighborhoods (N=2,118).
Dots represent the mean total depression score within the school. 95% bounds around the mean based on the standard deviation (SD) of total depression score in the school are also presented; these values are excluded for the neighborhood due to the high number of neighborhoods present in the data. Values are sorted from left to right by lowest school or neighborhood mean. Average depressive symptoms scores across schools ranged from 6.2 to 14.8. Average depressive symptoms scores across neighborhoods ranged from 0 to 56.
Multilevel-Cross Classified Models
Table 1 presents the results of the school-only and neighborhood-only MLM, and CCMM. In these null models with schools and neighborhoods examined in separate MLM (Model 1), the random effect for the school ( ) and neighborhood ( ) were similar. ICC values were comparable for the school (3.6%) and neighborhood (3.2%). However, the CCMM showed that the between-level variance in depressive symptoms was driven largely by the school ( ) and not by the neighborhood ( ) (ICC school=3.0%; ICC neighborhood=0.8%). Adding individual-level covariates to the CCMM (Model 2) attenuated the between-level variance for schools ( ) and neighborhoods ( ), though the individual-level residual variance was largely unchanged (ICC school=1.3%; ICC neighborhood=0.4%). This decline suggests that the between-level variation in depressive symptoms was due largely to compositional effects (i.e., characteristics of adolescents in these contexts) though this was more striking in neighborhoods. Results of this model also suggest that depressive symptom scores were higher among females (β=1.97), both Black (β=1.00) and Hispanic adolescents (β=1.52), students of an older age (β=0.40), students who had a parent on public assistance (β=1.70), and students for whom at least one parent completed a college degree (β=−1.46).
Table 1.
Nested Models Describing Association between Predictors and Depressive Symptoms in the National Longitudinal Study of Adolescent Health (N=16,172)
| Fixed Effect Estimates | Model 1 (Null Models) | Model 2 (Individual-Level Predictors) | ||
|---|---|---|---|---|
|
| ||||
| A. School Only MLM | B. Neighborhood Only MLM | C. Cross-Classified Multilevel Model | Cross Classified Multilevel Model | |
|
|
||||
| Intercept (SE) | 11.2 (0.09)* | 11.1 (0.08)* | 10.8 (0.14)* | 3.6 (0.61)* |
| Individual-level | ||||
| Age | - | - | - | 0.40 (0.32, 0.47)* |
| Female | - | - | - | 1.97 (1.74, 2.21)* |
| Public Assistance | - | - | - | 1.70 (1.31, 2.09)* |
| College degree (parent) | - | - | - | −1.46 (−1.72, −1.20)* |
| Race | ||||
| White | - | - | - | Ref. |
| Black | - | - | - | 1.00 (0.66, 1.35)* |
| Hispanic | - | - | - | 1.52 (1.13, 1.91)* |
| Random Effect Estimates | ||||
| U3 neighborhood (CI) | - | 1.84 (1.32, 2.37)* | 0.45 (0.10, 0.79)* | 0.19 (−0.02, 0.39)* |
| U2 school (CI) | 2.05 (1.5, 2.61)* | - | 1.69 (1.10, 2.28)* | 0.70 (0.37, 1.02)* |
| U1 individual (CI) | 54.65 (53.43, 55.86)* | 55.04 (53.81, 56.27)* | 54.68 (53.48, 55.89)* | 52.81 (51.64, 53.99)* |
| Fit Statistics | ||||
| DIC | - | - | 110788 | 110169 |
|
| ||||
| ICC estimates | ||||
| Neighborhood | - | 3.2% | 0.8% | 0.4% |
| School | 3.6% | - | 3.0% | 1.3% |
For the fixed effect estimates, cell entries are parameter (beta) estimates and confidence intervals. All other entries are estimates and confidence intervals. DIC refers to Deviance Information Criterion, a measure of model fit and is only reported for the cross-classified multilevel models. Higher DIC values indicate a poorer fitting model. Two-sided tests were performed for fixed effects while one-sided tests were performed for random effects (as negative variance estimates are not plausible). Significant fixed and random effects are indicated by * (p<0.05). ICC refers to the intraclass correlation coefficient, or the proportion of variance in the outcome attributable to neighborhoods (after adjusting for schools) or attributable to schools (after adjusting for neighborhoods).
Table 2 presents the results of the CCMM including school- and neighborhood-level predictors. In Model 3, which introduced the school-level covariates into Model 2, the residual variance terms for the school ( ), neighborhood ( ), and student-level ( ) were largely unchanged. Consistent with this finding, we also detected no statistically significant fixed effects for the percentage of students in the school with a parent receiving public assistance (β=0.02), the percentage of students with at least one parent with a college degree (β=−0.01), or the percentage of students in the school who were white (β=−0.01).
Table 2.
Nested Cross-Classified Multilevel Models (CCMM) Describing Association Between Predictors and Depressive Symptoms in the National Longitudinal Study of Adolescent Health (N=16,172)
| Fixed Effect Estimates | Model 3 (School-Level Predictors) | Model 4 (Neighborhood-Level Predictors) | Model 5 (School- and Neighborhood-Level Predictors |
|---|---|---|---|
|
|
|||
| Intercept (SE) | 3.91 (0.8)* | 4.01 (0.8)* | 3.98 (0.9)* |
| Individual-level | |||
| Age | 0.40 (0.33, 0.48)* | 0.39 (0.32, 0.47)* | 0.40 (0.32, 0.48)* |
| Female | 1.97 (1.74, 2.20)* | 1.97 (1.74, 2.20)* | 1.97 (1.75, 2.20)* |
| Public Assistance | 1.63 (1.23, 2.04)* | 1.60 (1.19, 2.00)* | 1.57 (1.17, 1.97)* |
| College degree (parent) | −1.41 (−1.68, −1.14)* | −1.37 (−1.64, −1.09)* | −1.36 (−1.62, −1.09)* |
| Race | |||
| White | Ref. | Ref. | Ref. |
| Black | 0.84 (0.46, 1.22)* | 0.72 (0.30, 1.13)* | 0.68 (0.27, 1.09)* |
| Hispanic | 1.37 (0.95, 1.79)* | 1.41 (1.02, 1.81)* | 1.33 (0.92, 1.74)* |
| School-level | |||
| % Public Assistance | 0.02 (−0.02, 0.05) | - | 0.01 (−0.03, 0.04) |
| % College degree | −0.01 (−0.02, 0.01) | - | 0.00 (−0.02, 0.02) |
| % White | −0.01 (−0.02, 0.00) | - | −0.01 (−0.02, 0.01) |
| Neighborhood-level | |||
| % Public Assistance | - | 0.02 (0.00, 0.05) | 0.02 (−0.01, 0.05) |
| % College degree | - | −0.01 (−0.02, 0.00) | −0.01 (−0.03, 0.00) |
| % White | - | 0.00 (0.00, 0.01) | 0.00 (−0.01, 0.01) |
| Random Effect Estimates | |||
| U3 neighborhood (95% CI) | 0.20 (−0.02, 0.42)* | 0.15 (−0.03, 0.33) | 0.15 (−0.02, 0.31) |
| U2 school (95% CI) | 0.65 (0.33, 0.96)* | 0.73 (0.40, 1.05)* | 0.73 (0.38, 1.08)* |
| U1 individual (95% CI) | 52.82 (51.6, 54.0)* | 52.80 (51.62, 53.98)* | 52.80 (51.63, 53.98)* |
| Fit Statistics | |||
| DIC | 110168 | 110157 | 110158 |
|
| |||
| ICC estimates | |||
| Neighborhood | 0.4% | 0.3% | 0.3% |
| School | 1.2% | 1.4% | 1.4% |
For the fixed effect estimates, cell entries are parameter (beta) estimates and confidence intervals. All other entries are estimates and confidence intervals. DIC refers to Deviance Information Criterion, a measure of model fit and is only reported for the cross-classified models. Higher DIC values indicate a poorer fitting model. Two-sided tests were performed for fixed effects while one-sided tests were performed for random effects (as negative variance estimates are not plausible). Significant fixed and random effects are indicated by * (p<0.05).
Model 4, which introduced the neighborhood-level covariates into Model 2, was similar to Model 3. The residual variance terms for the school ( ), neighborhood ( ), and student-level ( ) were largely unchanged. Similarly, no statistically significant fixed effects were detected for the percentage of residents in the neighborhood who received public assistance (β=0.02), the percentage of residents in the neighborhood who had a college degree (β=−0.01), or the percentage of residents in the neighborhood who were white (β=−0.01). Results of Model 5, which contained all individual, school, and neighborhood factors, were similar to previous models, with only individual fixed effects being significant and the school random effect remaining significant.
DISCUSSION
This study used CCMM to disentangle the effect of schools from neighborhoods on adolescent risk for depression. Three major findings emerged from this research. First, we found that schools appeared to drive the between-level variance in depressive symptoms more than neighborhoods. After accounting for individual-level (or compositional) characteristics, the school-level random effect was statistically significant and more than three times the neighborhood-level random effect. These findings suggest that schools may be more salient than neighborhoods for influencing depressive symptoms in youth. Although the magnitude of these school effects (e.g., ICC estimates) is small, with the majority of variation in depressive symptoms being due to differences between adolescents, our findings suggest that schools appear to contribute to variation in levels of depressive symptoms. Therefore, schools may be an important context for reducing the population-level burden of depression by targeting school-level predictors, including school-based interventions. These findings also underscore the need to use CCMM, as these findings would have been missed had we used traditional MLM (34, 52).
Second, we found that only student-level factors (i.e., sex, race/ethnicity, age, parental SES) were significantly associated with depressive symptoms. We did not find that any of the school-level predictors (% on public assistance, % of students with at least one parent with a college degree, and % White) or neighborhood-level predictors (% on public assistance, % of residents without a college degree, % White) were associated with depressive symptoms in any of the models. Our results did differ from previous findings (10–14), including studies using Add Health that examined either the school- or neighborhood context alone using a multilevel model (24, 53–56). These differences were unsurprising given that there have been substantially different approaches used to tests these questions in Add Health and other datasets (e.g., different predictors, covariates, samples). However, even after running additional CCMM analyses to more closely mimic prior work in Add Health, for example, focusing on income as the measure of socioeconomic status, we still reached the same substantive conclusions (results available from the author). Future studies are therefore needed to replicate and extend these findings, focusing especially on comparing the results of analyses focusing on MLM to CCMM. Future studies are also needed to understand what aspects of the school may contribute to between-school variation in adolescent depression, as none of the variables we examined here appeared to be large contributors.
To our knowledge, only one previous study used CCMM to examine the simultaneous contribution of neighborhoods and schools on adolescent self-reported wellbeing. In a study of 9107 high school students in New Zealand, Aminzadeh and colleagues found that 1.16% of the variance in wellbeing was attributed to neighborhoods after accounting for schools, compared to only 0.14% for schools after accounting for neighborhoods (57). The differences in results between our study and the Aminzadeh study is interesting, particularly as both studies sampled students using school-based sampling approaches. These differences could be due to numerous factors, including differences in school and neighborhood salience between the United States and New Zealand and differences in school and neighborhood salience between outcomes. Given the lack of prior research on CCMM, additional studies are needed to disentangle the unique impact of school and neighborhood environments. Knowledge generated from such studies can help guide policymakers in determining where to apply limited funds to most effectively shape youth development and reduce risk for mental health problems like depression.
Why might schools be more important than neighborhoods for shaping adolescent’s risk for depression? First, schools are the one setting where students spend a majority of time outside of their home and where there are high levels of adult monitoring of student behavior during the day. Second, schools are no longer solely formal educational institutions, but instead are the settings where numerous health- and development-promoting interventions take place (58–60) and student’s acquire knowledge and learn health-promoting skills in both cognitive and social-emotional domains (e.g., problem-solving, coping, cognitive restructuring) (61–63). Moreover, schools also have formal opportunities, through mental health screening, health services, and educational mandates, to monitor youth behavior and intervene with those at-risk (64, 65). Thus, schools may be contributing more to the variance in depressive symptoms because they are the setting where students are exposed to a range of possible risk or protective factors that influence the onset of depressive symptoms or are a setting for addressing depressive symptoms once they emerge. Examination of these types of characteristics, along with other social characteristics of schools (e.g., social climate of the school; levels of student connectedness to the school) may be important to better understand the effect of schools on youth risk for depression.
Our study had several limitations that must be noted when interpreting the results. First, and most importantly, the analyses are based on a nationally representative sample of adolescents who were selected using school-based sampling. Whether our findings are an artifact of the sampling strategy remains unknown. It is possible our results reflect the greater number of individuals per school rather than neighborhood. We think this is unlikely, however, as preliminary analyses we conducted in Add Health using CCMM to examine other health outcomes did find meaningful effects for neighborhoods; neighborhoods contributed more than schools to the variance in female body mass index for example. Moreover, when we conducted sensitivity analyses to eliminate neighborhoods with less than 5 respondents, our results were similar (results available from the author). Although these findings are reassuring, simulation studies and studies using CCMM in the context of neighborhood-based sampling designs are needed to determine the extent to which sampling influences cross-classified results. Second, Add Health Wave I data were collected almost twenty years ago. Although these data are older, Add Health remains the only nationally representative sample of adolescents in the US and thus is one of the only large-scale studies available to test our research questions. Third, our outcome measure was based on symptoms of depression during the past week, rather than a diagnostic interview or depressive symptoms measured over a longer period of time. However, the current measure has been widely used in epidemiological studies and demonstrates good reliability and validity (46). Fourth, our use of binary indicators, particularly of socioeconomic status, may result in some possible misclassification of respondents and therefore residual confounding. However, when we ran these analyses using continuous measures the results were similar. Finally, given that we defined neighborhoods based on Census Tract, it is also possible that there was misclassification of individuals by neighborhoods. Although Census Tracts are an imperfect measure to define “neighborhoods”, they are most commonly used in multilevel research (66). Future studies may wish to expand upon traditional boundaries of neighborhoods, as well as schools, to focus comparisons on “activity spaces,” or the spaces where students travel during the course of their day-to-day activities (67). Despite these limitations, these results suggest that schools might have a unique potential to affect, at a population-level, the prevalence of depression among youth. Further, this study provides a good demonstration of the ability of CCMM to answer questions related to differential effects of schools and neighborhoods, which are sorely needed given the dearth of studies using CCMM. Future studies using CCMM are needed to guide the investment of limited public health resources and identify in which settings (schools, neighborhoods, or both) public health policies and interventions can have the greatest impacts.
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) under Award Number K01HD058042.
Footnotes
Contributor Statement -
Erin C. Dunn: Dr. Dunn conceptualized the analytic plan, oversaw the analysis, interpreted results, drafted the manuscript, and approved the final version.
Carly E. Milliren: Ms. Milliren carried out the analyses, helped with interpretation of results, edited the early manuscripts, and approved the final version.
Clare Rosenfeld Evans: Ms. Evans helped with interpretation of results and edited and approved the final manuscript version.
S.V. Subramanian: Dr. Subramanian worked with Dr. Dunn to conceptualize the original study design, reviewed and aided in interpreting early results, and approved the final version.
Tracy K. Richmond: Dr. Richmond helped Dr. Dunn conceptualize the original study design, met regularly to review results, reviewed and edited the early draft of the manuscript, and approved the final version.
Human Participant Protection – This project was approved by the Boston Children’s Hospital Institutional Review Board.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. SVS was supported in part by the RWJ Investigator Award in Health Policy Research.
References
- 1.Merikangas KR, He S, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2011;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, et al. Youth risk behavior surveillance - United States, 2011. Morbidity and Mortality Weekly. 2012;61(SS-4):1–168. [PubMed] [Google Scholar]
- 3.Hallfors DD, Waller MW, Ford CA, Halpern CT, Brodish PH, Iritani B. Adolescent depression and suicide risk: Association with sex and drug behavior. American Journal of Preventive Medicine. 2004;27(3):224–230. doi: 10.1016/j.amepre.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Harrington R. Depression, suicide, and deliberate self-harm in adolescence. British Medical Journal. 2001;57:47–60. doi: 10.1093/bmb/57.1.47. [DOI] [PubMed] [Google Scholar]
- 5.Escobedo LG, Reddy M, Giovino GA. The relationship between and cigarette smoking in depressive symptoms U S adolescents. Addiction. 1998;93(3):433–440. doi: 10.1046/j.1360-0443.1998.93343311.x. [DOI] [PubMed] [Google Scholar]
- 6.Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: A critical review of the literature. Tobacco Control. 1998;7:409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinberg NZ, Rahdert E, Colliver JD, Glantz MD. Adolescent substance abuse: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(3):252–261. doi: 10.1097/00004583-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. American Journal of Psychiatry. 2000;157:1584–1591. doi: 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- 9.Rao U, Ryan ND, Birmaher B, Dahl RE, Williamson DE, Kaufman J, et al. Unipolar depression in adolescents: Clinical outcome in adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(5):566–578. doi: 10.1097/00004583-199505000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Mair CF, Diez Roux AV, Galea S. Are neighborhood characterisics associated with depressive symptoms? A critical review. Journal of Epidemiology and Community Health. 2008;62(11):940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 11.Truong Kd, Ma S. A systematic review of relations between neighborhoods and mental health. The Journal of Mental Health Policy and Economics. 2006;9:134–154. [PubMed] [Google Scholar]
- 12.Xue Y, Leventhal T, Brooks-Gunn J, Earls FJ. Neighborhood residence and mental health problems of 5- to 11-year olds. Archives of General Psychiatry. 2005;62:554–563. doi: 10.1001/archpsyc.62.5.554. [DOI] [PubMed] [Google Scholar]
- 13.Leventhal T, Brooks-Gunn J. Moving to opportunity: An experimental study of neighborhood effects on mental health. American Journal of Public Health. 2003;93(9):1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim D. Blues from the neighborhood? Neighborhood characteristics and depression Epidemiologic Reviews. 2008;30:101–117. doi: 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- 15.Virtanen M, Ervasti J, Oksanen T, Kivimaki M, Vahtera J. Social capital in schools. In: Kawachi I, Takao S, Subramanian SV, editors. Global perspectives on social capital and health. New York, NY: Springer New York Heidelberg Dordrecht London; 2013. pp. 65–85. [Google Scholar]
- 16.Kidger J, Araya R, Donovan J, Gunnell D. The effect of the school environment on the emotional health of adolescents: A systematic review. Pediatrics. 2012;129:925–949. doi: 10.1542/peds.2011-2248. [DOI] [PubMed] [Google Scholar]
- 17.Kuperminc GP, Leadbeater BJ, Blatt SJ. School social climate and individual differences in vulnerability to psychopathology among middle school students. Journal of School Psychology. 2001;39(2):141–159. [Google Scholar]
- 18.Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm: Findings from the National Longitudinal Study on Adolescent Health. Journal of the American Medical Association. 1997;278:823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 19.Jacobson KC, Rowe DC. Genetic and environmental influences on the relationship between family connectedness, school connectedness and adolescent depressed mood: Sex differences. Developmental Psychology. 1999;35:926–939. doi: 10.1037//0012-1649.35.4.926. [DOI] [PubMed] [Google Scholar]
- 20.Kasen S, Johnson J, Cohen P. The impact of school emotional climate on student psychopathology. Journal of Abnormal Child Psychology. 1990;18(2):165–177. doi: 10.1007/BF00910728. [DOI] [PubMed] [Google Scholar]
- 21.Bond L, Butler H, Thomas L, Carlin J, Glover S, Bowes G, et al. Social and school connectedness in early secondary schools as predictors of late teenage substance use, mental health, and academic outcomes. Journal of Adolescent Health. 2007;40(357):e9–357. e18. doi: 10.1016/j.jadohealth.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 22.Way N, Reddy R, Rhodes J. Students’ perceptions of school climate during the middle school years: Associations with trajectories of psychological and behavioral adjustment. American Journal of Community Psychology. 2007;40:194–213. doi: 10.1007/s10464-007-9143-y. [DOI] [PubMed] [Google Scholar]
- 23.Anderman EM. School effects on psychological outcomes during adolescence. Journal of Educational Psychology. 2002;94(4):795–809. [Google Scholar]
- 24.Goodman E, Huang B, Wade TJ, Kahn RS. A multilevel analysis of the relation of socioeconomic status to adolescent depressive symptoms: Does school context matter? Journal of Pediatrics. 2003;143:451–456. doi: 10.1067/S0022-3476(03)00456-6. [DOI] [PubMed] [Google Scholar]
- 25.Briere FN, Pascal S, Dupere V, Janosz M. School environment and adolescent depressive symptoms: A multilevel longitudinal study. Pediatrics. 2013;131:e702–e708. doi: 10.1542/peds.2012-2172. [DOI] [PubMed] [Google Scholar]
- 26.Catalano RF, Haggerty KP, Oesterle S, Fleming CB, Hawkins JD. The importance of bonding to school for healthy development: Findings from the Social Development Research Group. Journal of School Health. 2004;74:252–262. doi: 10.1111/j.1746-1561.2004.tb08281.x. [DOI] [PubMed] [Google Scholar]
- 27.Sellstrom E, Bremberg S. Is there a “school effect” on pupil outcomes? A review of multilevel studies. Journal of Epidemiology and Community Health. 2006;60:149–155. doi: 10.1136/jech.2005.036707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reis J, Trockel M, Mulhall P. Individual and school predictors of middle school agression. Youth and Society. 2007;38(3):322–347. [Google Scholar]
- 29.Green JG, Dunn EC, Johnson RM, Molnar BE. A multi-level investigation of the association between school context and adolescent non-physical bully victimization. Journal of School Violence. 2011;10(2):133–149. doi: 10.1080/15388220.2010.539165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roeser RW, Eccles JS, Sameroff AJ. School as a context of early adolescent’ academic and social-emotional development: A summary of research findings. The Elementary School Journal. 2000;100(5):443–471. [Google Scholar]
- 31.Hoge DR, Smit EK, Hanson SL. School experiences predicting changes in self-esteem of sixth and seventh-grade students. Journal of Educational Psychology. 1990;82:117–127. [Google Scholar]
- 32.Dunn EC, Grief Green J, Johnson RM. The modified depression scale (MDS): A brief, no-cost assessment tool to estimate the level of depressive symptoms in students and schools. School Mental Health. 2012;4(1):34–45. doi: 10.1007/s12310-011-9066-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: The effects of neighborhood residence on child and adolescent outcomes. Psychological Bulletin. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 34.Beretvas SN. Cross-classified and multiple-membership models. In: Hox JJ, Roberts JK, editors. Handbook of advanced multilevel analysis. New York, NY: Routledge; 2011. pp. 313–334. [Google Scholar]
- 35.Goldstein H. Multilevel cross-classified models. Sociological Methods and Research. 1994;22:364–375. [Google Scholar]
- 36.Aud S, Hussar W, Planty M, Snyder T, Bianco K, Fox M, et al. The condition of education 2010 (NCES 2010–028) Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education; 2010. [Google Scholar]
- 37.Roeser RW, Eccles JS, editors. Schooling and mental health. New York, NY: Kluwer Academic/Plenum Publishers; 2000. [Google Scholar]
- 38.Gershoff ET, Aber JL, editors. Neighborhoods and schools: Contexts and consequences for the mental health and risk behaviors of children and youth. New York, NY: Psychology Press; 2006. [Google Scholar]
- 39.Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, Peters S, McCaslin C, Joyce R, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: The role of built, socioeconomic, and social environments. Social Science and Medicine. 2013;95:106–114. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Macintyre S, Ellaway A, editors. Ecological approaches: Rediscovering the role of the physical and social environment. New York, NY: Oxbord University Press; 2000. [Google Scholar]
- 41.Tendulkar SA, Buka S, Dunn EC, Subramanian SV, Koenen KC. A multilevel investigation of neighborhood effects on parental warmth. Journal of Community Psychology. 2010;38(5):557–573. [Google Scholar]
- 42.Sampson RJ, Raudenbush S, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 43.Grady S, Bielick S. Trends in the use of school choice: 1993 to 2007 (NCES 2010–004) Washington, DC: 2010. [Google Scholar]
- 44.Snyder TD, Dillow SA. Digest of Education Statistics, 2012 (NCES 2014–2015) Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education; 2013. [Google Scholar]
- 45.Harris KM. The Add Health Study: Design and accomplishments. Carolina Population Center, University of North Carolina; Chapel Hill: 2013. [Google Scholar]
- 46.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 47.Tabachnick BG, Fidell LS. Using multivariate statistics. 6. Boston, MA: Allyn and Bacon; 2013. [Google Scholar]
- 48.van Belle G. STRUTS: Statistical rules of thumb. New York, NY: John Wiley and Sons; 2002. [Google Scholar]
- 49.Browne NJ. MCMC estimation in MLwiN version 2.0. London, UK: Centre for Multilevel Modeling, Institute of Education; 2004. [Google Scholar]
- 50.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis method. 2. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 51.Lee ES, Forthofer RN. Analyzing complex survey data. Thousand Oaks: Sage; 2006. [Google Scholar]
- 52.Dunn EC, Richmond TK, Milliren CE, Subramanian SV. Avoiding confounded contexts: Using cross-classified multilevel models to disentangle school and neighborhood effects: An example focusing on smoking behaviors among adolescents in the United States. under review. doi: 10.1016/j.healthplace.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wight RG, Aneshensel CS, Botticello AL, Sepulveda JE. A multilevel analysis of ethnic variation in depressive symptoms among adolescents in the United States. Social Science and Medicine. 2005;60:2073–2084. doi: 10.1016/j.socscimed.2004.08.065. [DOI] [PubMed] [Google Scholar]
- 54.Wickrama KAS, Bryant CM. Community context of social resources and adolescent mental health. Journal of Marriage and Family. 2003;65:850–866. [Google Scholar]
- 55.Hull P, Kilbourne B, Reece M, Husaini B. Community involvement and adolescent mental health: Moderating effects of race/ethnicity and neighborhood disadvantage. Journal of Community Psychology. 2008;36(4):534–551. [Google Scholar]
- 56.Wight RG, Botticello AL, Aneshensel CS. Socioeconomic context, scial support, and adolescent mental health: A multilevel investigation. Journal of Youth and Adolescence. 2006;35(1):115–126. [Google Scholar]
- 57.Aminzadeh K, Denny S, Utter J, Milfont TL, Ameratunga S, Teevale T, et al. Neighbourhood social capital and adolescent self-reported wellbeing in New Zealand: a multilevel analysis. Soc Sci Med. 2013;84:13–21. doi: 10.1016/j.socscimed.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 58.Mellanby AR, Rees JB, Tripp JH. Peer-led and adult-led school health education: A critical review of available comparative research. Health Education Research. 2000;15(5):533–545. doi: 10.1093/her/15.5.533. [DOI] [PubMed] [Google Scholar]
- 59.Rones M, Hoagwood K. School-based mental health services: A research review. Clinical Child and Family Psychology Review. 2000;3(4):223–241. doi: 10.1023/a:1026425104386. [DOI] [PubMed] [Google Scholar]
- 60.Greenberg MT, Weissberg RP, O’Brien MU, Zins JE, Fredericks L, Resnik H, et al. Enhancing school-based prevention and youth development through coordinated social, emotional, and academic learning. American Psychologist. 2003;58(6–7):466–474. doi: 10.1037/0003-066x.58.6-7.466. [DOI] [PubMed] [Google Scholar]
- 61.Eccles JS, Roeser RW. School and community influences on human development. In: Bornstein MH, Lamb ME, editors. Developmental science: An advanced textbook. 6. New York, NY: Psychology Press; 2011. pp. 571–643. [Google Scholar]
- 62.Jones SM, Brown JL, Aber JL. Two-year impacts of a universal school-based social-emotional and literacy intervention: An experiment in translational developmental research. Child Development. 2011;82(2):533–554. doi: 10.1111/j.1467-8624.2010.01560.x. [DOI] [PubMed] [Google Scholar]
- 63.Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74(3):401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- 64.Weist MD, Evans SW, Lever NA, editors. Handbook of school mental health: Advancing practice and research. New York, NY: Kluwer Academic/Plenum Publishers; 2003. [Google Scholar]
- 65.Ringeisen H, Henderson K, Hoagwood K. Context matters: schools and the “research to practice gap” in children’s mental health. School Psychology Review. 2003;32(2):153–168. [Google Scholar]
- 66.Dunn EC, Masyn KE, Yudron M, Jones SM, Subramanian SV. Translating multilevel theory into multilevel research: Challenge and opportunities for understanding the social determinants of psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology. 2014;49:859–872. doi: 10.1007/s00127-013-0809-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vallee J, Cadot E, Roustit C, Parizot I, Chauvin P. The role of daily mobility in mental health inequalities: The interactive influence of activity space and neighbourhood of residence on depression. Social Science and Medicine. 2011;73(8):1133–1144. doi: 10.1016/j.socscimed.2011.08.009. [DOI] [PubMed] [Google Scholar]