Abstract
Introduction
This systematic review was conducted to analyze the impact and describe simulation-based training and the acquisition of laparoscopic surgery skills during medical school and residency programs.
Methods
This systematic review focused on the published literature that used randomized controlled trials to examine the effectiveness of simulation-based training to develop laparoscopic surgery skills. Searching PubMed from the inception of the databases to May 1, 2014 and specific hand journal searches identified the studies. This current review of the literature addresses the question of whether laparoscopic simulation translates the acquisition of surgical skills to the operating room (OR).
Results
This systematic review of simulation-based training and laparoscopic surgery found that specific skills could be translatable to the OR. Twenty-one studies reported learning outcomes measured in five behavioral categories: economy of movement (8 studies); suturing (3 studies); performance time (13 studies); error rates (7 studies), and global rating (7 studies).
Conclusion
Simulation-based training can lead to demonstrable benefits of surgical skills in the OR environment. This review suggests that simulation-based training is an effective way to teach laparoscopic surgery skills, increase translation of laparoscopic surgery skills to the OR, and increase patient safety; however, more research should be conducted to determine if and how simulation can become apart of surgical curriculum.
Keywords: laparoscopic surgery, simulation, medical education, systematic review, skill transfer, translation, randomized clinical trials
1. Introduction
Laparoscopic surgery has become the “gold standard” for common surgical procedures such as cholecystectomies and appendectomies (Bennett, Birch, Menzes, Vizhul, & Karmali, 2011; Richardson, Carter, Fuhrman, Bolton, & Bowen, 2000), and is associated with less surgical trauma, faster postoperative recovery, shorter hospital stays, and better cosmetic results (Munz, Kumar, Moorthy, Bann, & Darzi, 2004; Johnson & Walsh, 2009). There is a general understanding that simulation-based training improves knowledge (McGaghie, Siddall, Mazmanian, & Myers, 2009; Ehdaie, Tracy, Reynolds, Cung, Thomas, Floyd, & Schenkman, 2011) and that training outside the operating room (OR) reduces the risk of adverse surgical events (Hyltander, Liljegren, Rhodin, & Lönroth, 2002; Andreatta et al., 2006; Aggarwal, Ward, Balasundaram, Sains, Athanasiou, & Darzi, 2007).
As the health care community creates and maintains new teaching methods to train competent surgeons, learning opportunities that exist outside the OR are becoming a recommended method for developing laparoscopic surgery skills (Ahlberg et al., 2007; Jordan, Gallagher, McGuigan, McGlade, & McClure, 2000; Verdaasdonk, Dankelman, Lange, & Stassen, 2008). Training outside the OR reduces the risk of adverse surgical events (Hyltander, Liljegren, Rhodin, & Lönroth, 2002; Aggarwal, Ward, Balasundaram, Sains, Athanasiou, & Darzi, 2007; Ahlberg, Heikkinen, Iselius, Leijonmarck, Rutqvist, & Arvidsson, 2002). Simulation-based surgical skills and procedures allows inexperienced surgeons to acquire skills through repetitive practice in a safe, nonthreatening environment, prior to encountering the risk and time pressures inherent in the OR (Andreatta et al., 2006; Miskovic, Wyles, Ni, Darzi, & Hanna, 2010). Those responsible for designing simulation facilities work with limited evidence to resolve complex questions relating to education, translation of skills learned, and patient safety with regard to teaching laparoscopic surgery.
In a systematic review conducted in 2006, researchers found that learners acquire similar clinical results as surgeons in laparoscopic colorectal surgery, if supervised by an expert during training (Sutherland, Middleton, Anthony, Hamdorf, Cregan, Scott, & Maddern, 2006); however, this review was limited only to colorectal surgeries. In a different systematic review, investigators reported that simulation training may not be a better method than patients, cadavers, and animals for teaching surgical skills (Sutherland et al., 2006), but the skills learned by simulation-based training appeared to be transferable to the OR. This review conducted by Strum and researchers (Sturm, Windsor, Cosman, Cregan, Hewett, & Maddern, 2008) was limited to 11 published studies and was conducted in 2008. Gurusamy and colleagues (Gurusamy, Aggarwal, Palanivelu, & Davidson, 2008) found that virtual reality training can supplement laparoscopic surgery training, but variability across research designs and conflicting findings in the published studies prevented the confirmation of clear best practices. More recently, Cook and colleagues (Cook et al., 2001) studied technology-enhanced simulation training and concluded that simulation training is associated with large effects on clinician behaviors and moderate effects on patient care.
This current review of the literature addresses the question of whether laparoscopic simulation translates the acquisition of surgical skills to the OR. The conceptual framework for this manuscript is focused on the importance and relevance related to the education of surgical skills, the translation of surgical skills acquired outside of the OR, and improvements focused on safety for patients. A review of published research was completed to describe the impact of simulation-based training on the acquisition of laparoscopic surgery skills and the translation of these skills to the OR. Skills acquisition was assessed for performance time, global rating, suturing, cutting, and cautery skills; errors, and economy of movement.
2. Methods
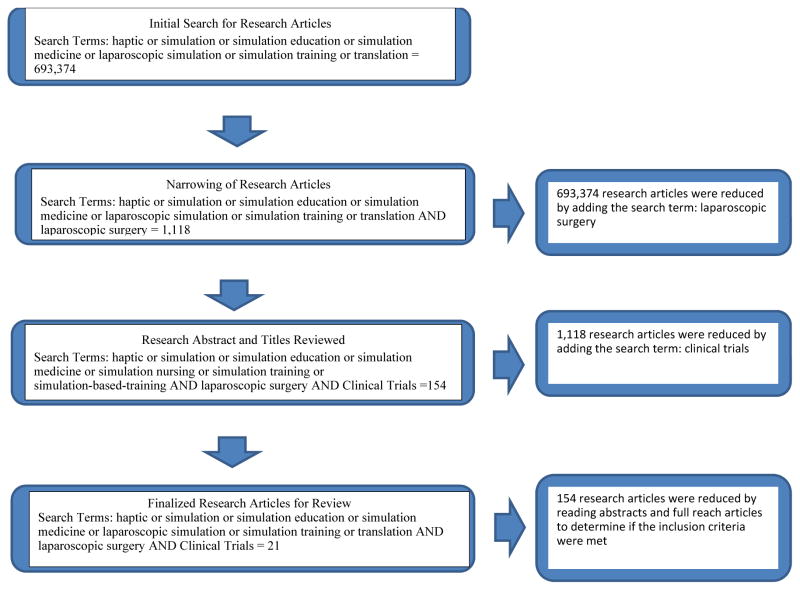
This review focused on published literature that examines the effectiveness of simulation-based training to develop laparoscopic surgery skills translation into the OR. The studies reviewed were identified by searching PubMed from the inception of the database to April 1, 2014 and hand searching: Simulation in Health Care, Annals of Surgery, Journal American Surgery, International Journal of Surgery, Surgery, Archives of Surgery, and The British Journal of Surgery from 2000 – May 2014. Multiple combinations of several relevant key words were used to identify articles for review (haptic or simulation or simulation education or simulation medicine or laparoscopic simulation or simulation training or translation AND laparoscopic surgery). Figure 1 demonstrates the elimination of articles that came up during the search process.
Figure 1.
Flow chart for research article search in May 2014
2.1 Inclusion and Exclusion Criteria
Inclusion criteria required that studies: (a) use a randomized controlled design that includes at least one intervention group and one control group that either received no training or traditional training in the operating room, (b) single-group pretest-posttest, (c) two group nonrandomized, (d) parallel-group (e) crossover designs, (f) use simulation-based training as the educational intervention for teaching laparoscopic surgery skills, and (e) translation of skills was measured into the OR setting. Simulation-based training was defined broadly to include equipment that replicated the task environment with sufficient realism to serve as a training tool. Examples of the simulators included in this systematic review were box trainers, computer software, virtual reality simulators, task trainers, and high fidelity and static mannequins. The exclusion criteria were: (a) studies that did not use simulation as the educational intervention for teaching laparoscopic surgery skills, (b) literature reviews, and (c) translation of skills was not measured into the OR setting.
An adopted coding framework based on PRISMA (Liberati et al., 2001) and Cochrane handbook (Higgins, 2012) was used to review the literature. The first author independently coded each of the articles discovered through the literature search. When reviewing the literature some abstracts provided enough detail and information related to the methods to determine if the inclusion criteria were met; if not, the full manuscript was read to determine if the methods met the inclusion criteria. The manuscripts were eliminated because the methods did not meet the inclusion criteria.
3. Results
The results reported in this section are based on the 20 articles we determined met our inclusion criteria. Table 1 describes the types of simulators implemented in the 21 studies, manufacturers for the simulators, definitions for the simulators, and performance skills the simulators provide. A total of 21 studies were analyzed; the specific simulators, participants, assessments, and details of the 21 studies are provided in Tables 2 and 3. All post-training assessment were translational to either a porcine model or the OR, 9 (43%) studies conducted the posttest in a Porcine Model, 12 (57%) studies conducted the posttest in the OR with patients.
Table 1.
Laparoscopic training tools, definitions, manufacturers, and procedures commonly trained in surgery
| Type of Simulation | Definition | Manufacturer | Camera Navigation | Clipping & Cutting | Suturing & Knot Tying | Lifting & Grasping | Dissection |
|---|---|---|---|---|---|---|---|
| Box Trainer | A box that incorporates conventional laparoscopic equipment to perform basic skills, is versatile, and enables training on animal parts as well as synthetic inanimate models | Simulab Corporation | X | X | X | X | X |
| Task Trainer | A partial component of a simulator or simulation modality, for example, an arm, leg, or torso. | Limbs and Things | X | X | X | ||
| MIST-VR | A virtual reality simulator with six different tasks to simulate maneuvers performed during laparoscopic cholecystectomy in a computerized environment. | Mentice AB | X | X | X | X | |
| LapMentor/LapMentor II | A virtual reality simulator consisting of a camera and two calibrated working instruments for which the motion of the instruments is translated to a two-dimensional computer screen for student practices. | Simbionix Ltd. | X | X | X | X | X |
| LapSim | A computer-based simulator creating a virtual laparoscopic setting through a computer operating system, a video monitor, a laparoscopic interface containing two pistol-grip instruments, and a diathermy pedal without haptic feedback | Surgical Science | X | X | X | X | X |
| EndoTower | EndoTower software consists of an angled telescope simulator composed of rotating camera and telescopic components. | Verefi Technologies, INC. | X | X | |||
| MISTELS/FLS trainer | McGill Inanimate System for Training and Evaluation of Laparoscopic Skills – this inexpensive, portable, and flexible system allows students to practice in a virtual Endotrainer box. | SAGES | X | X | X | ||
| SIMENDO VR | Computer software used to train eye-hand coordination skills by camera navigation and basic drills. | Delta Tech | X | X | X | ||
| URO Mentor | A hybrid simulator, consisting of a personal computer based system linked to a mannequin with real endoscopes. Cytoscopic and ureterosciopic procedures are performed using either flexible or semi rigid endoscopes | Simbionix Ltd. | X | X | X | X | |
| Da Vinci Skills Simulator | A portable simulator containing a variety of exercises and scenarios specifically designed to give users the opportunity to improve their proficiency with surgical controls. | Intuitive Surgical | X | X | X | X | X |
Table 2.
Study participants, pre-study data, simulation, features of training procedures, and assessment
| Citation | Participants | Pre-study data collected |
Simulation intervention |
Additional training |
Time between initial assessment and final assessment |
Training time | Training tasks |
|---|---|---|---|---|---|---|---|
| Aggarwal et al., 2007 |
|
|
|
|
|
|
|
| Ahlberg et al., 2007 |
|
|
|
|
|
|
|
| Ahlberg et al., 2002 |
|
|
|
|
|
|
|
| Andreatta et al., 2006 |
|
|
|
|
|
|
|
| Banks et al., 2007 |
|
|
|
|
|
|
|
| Bennet et al. 2011 |
|
|
|
|
|
|
|
| Gala et al., 2013 |
|
|
|
|
|
|
|
| Ganai et al., 2007 |
|
|
|
|
|
|
|
| Grantcharov et al., 2004 |
|
|
|
|
|
|
|
| Hogle et al., 2009 |
|
|
|
|
|
|
|
| Hung et al., 2012 |
|
|
|
|
|
|
|
| Korndorffer et al., 2005 |
|
|
|
|
|
|
|
| Larsen et al., 2009 |
|
|
|
|
|
|
|
| Seymour et al., 2002 | 16 PGY1-4 surgical residents |
|
|
|
|
|
|
| Stefanidis et al., 2008 |
|
|
|
|
|
|
|
| Stefanidis et al., 2007 |
|
|
|
|
|
|
|
| Sroka et al., 2010 |
|
|
|
|
|
|
|
| Van Sickle et al. 2008 |
|
|
|
|
|
|
|
| Verdaasdonk et al., 2008 |
|
|
|
|
|
|
|
| Zendejas et al., 2011 |
|
|
|
|
|
|
|
Note:
Indicates articles that are unclear or do not supply an explanation of information.
Table 3.
Published reference, context of final assessment, source of assessment, skills assessed post-training, and results from studies
| Citation | Contextual setting for final assessment | Source of final assessment ratings | Skills assessed post training | Results from research studies |
|---|---|---|---|---|
| Aggarwal et al., 2007 | Porcine Model (pre on box trainer) | 2 observers (OSATS global rating and a motion tracking device) |
|
|
|
| ||||
| Ahlberg et al., 2007 | Porcine Model |
|
||
|
| ||||
| Ahlberg et al., 2002 | Patients in OR (pre on a simulator) | 2 observers (reliability greater .98) |
|
|
|
| ||||
| Andreatta et al., 2006 | Porcine Model | 2 surgeons (.99 reliability) |
|
|
| Banks et al., 2007 | Patients in OR (post only. Pre assess was done on simulator and then the training group performed on the simulator again before being evaluated in the OR) | Observers |
|
|
|
| ||||
| Bennet et al., 2011 | Patients in OR (post only) | Observers |
|
|
|
| ||||
| Gala et al., 2013 | Patients in OR | Observers |
|
|
|
| ||||
| Ganai et al., 2007 | Porcine Model (pre and post) | 3 External observers (90%) and from Endo Tower simulator |
|
|
|
| ||||
| Grantcharov et al., 2004 | Patients in OR | 2 Senior surgeons rated 1 surgery (cohen’s kappa .71) |
|
|
|
| ||||
| Hogle et al., 2009 | Study 1: OR Patients Study 3: Porcine Model (pre and post) |
Study 1: Attending surgeon Study 3: Observer |
|
|
|
| ||||
| Hung et al., 2012 | Porcine Model | 3 expert robotic surgeons blinded |
|
|
|
| ||||
| Korndorffer, et al., 2007 | Porcine Model (pre and post) | Observers |
|
|
|
| ||||
| Larsen et al., 2009 | Patients in OR (post only, pre was on a VR Simulator) | Observers |
|
|
|
| ||||
| Seymour et al., 2002 | Patients in OR (post only, pre was only ability tests) | Observers |
|
|
|
| ||||
| Stefanidis et al., 2008 | Porcine Model (pre and post) | Objective scores based on time and errors using a published formula |
|
|
|
| ||||
| Stefanidis et al., 2007 | Porcine Model (pre and post) A posttest was taken right after training was done, and then a retention test was taken after 5 months |
Observers |
|
|
| Sroka et al., 2010 | MISTELS and Box Trainer on Patients in the OR | Attending surgeon or external evaluator |
|
FLS scores
|
|
| ||||
| Van Sickle et al., 2008 | Patients in OR (post only) | 2 surgeons (agreement > .80) |
|
|
|
| ||||
| Verdaasdonk et al., 2008 | Porcine Model (post only) | 2 Expert laparoscopic surgeons |
|
|
| Zendejas et al., 2011 | OR (pre and post) | Observers and medical records |
|
|
Note:
Indicates articles that are unclear or do not supply an explanation of information.
3.1 Performance Time (n = 13 Studies) (Bennett et al., 2011; Andreatta et al., 2006; Aggarwal et al., 2007; Ahlberg et al., 2007; Gala et al., 2013; Larsen et al., 2009; Grantcharov et al., 2004; Clevin & Grantcharov, 2008; Hiemstra et al., 2011; Ganai et al., 2007; Stefanidis et al., 2008; Stefanidis et al., 2007)
Performance time was reported as the amount of time taken to perform the laparoscopic procedure of interest at the posttest evaluation. Of the 13 (62%) studies that assessed whether the training intervention resulted in the improvement of performance time, thirteen studies reported statistically significant improvement. For example, in one study researchers reported that the control group took 58% longer to perform the surgery (Ahlberg et al., 2007) and in another study investigators reported that the control group, on average, performed the surgery twice as long as the intervention group (24 minutes as compared to 12 minutes, P < .001) (Van Sickle et al., 2008). In yet another study the intervention group was 29% faster in dissecting the gallbladder during a cholecystectomy than the control group (Van Sickle et al., 2008). On the other hand, two studies (Bennett et al., 2011; Gala et al., 2013) reported no significant changes in time between the intervention and control groups when performance time was measured.
3.2 Global Ratings (n =7 studies) (Aggarwal et al., 2007; Verdaasdonk et al., 2008; Hogle et al., 2009; Sroka et al., 2010; Seymour et al., 2002; Zendejas et al., 2011; Grantcharov et al., 2004)
Global assessments were conducted using the Objective Structured Assessment of Technical Skill (Lucas, Tuncel, Bensalah, Zeltser, Jenkins, Pearle, & Cadeddu, 2008) (OSATS) rating scale, The OSATS evaluation tool evaluates participants on respect for tissue handling, time and motion, instrument handling, knowledge of instruments, flow of operation, use of assistant, and knowledge of procedure. GOALS rating scale (Watterson, Beiko, Kuan, & Denstedt, 2002) measures performance in 5 domains; three of the domains are specific to laparoscopic surgery (e.g., depth perception, bimanual dexterity and tissue handling) and 2 of the domains are generic (e.g., efficiency and autonomy). The standard Fundamentals of Laparoscopic Surgery (FLS) metrics (Larsen et al., 2009). FLS are the basic psychomotor skills necessary prior to learning how to perform and develop a laparoscopic surgical case. A different study reported that global assessment scores increased and their standard deviation decreased in the intervention group as compared to the non-trained group (P =.004) (Hogle, Chang, Strong, Welcome, Sinaan, Bailey, & Fowler, 2009). Moreover, in the same study 100% of intervention participants reached the passing score level where as only 37.5% of the control group. Investigators did not find any statistical significance between the two groups; however, the participants with low baseline performance increased their scores significantly after simulation training (Hung et al., 2012).
3.3 Suturing, Cutting and Cautery Skills (n = 3 Studies) (Andreatta et al., 2006; Ahlberg et al., 2002; Van Sickle et al., 2008)
Three (14%) of the 21 studies reported significant improvement on suturing, cutting, and cautery skills in the trained group as compared to the control group. Investigators reported that the trained participants outperformed the control participants in the performance of safe electrocautery (P < .01) (Andreatta et al., 2006).
Errors (n = 7 Studies) (Ahlberg et al., 2007; Verdaasdonk et al., 2008; Clevin & Grantcharov, 2008; Hiemstra et al., 2011; Korndorffer Jr et al., 2005; Stefanidis, Acker,& Heniford, 2008; Stefanidis et al., 2007)
Seven (33%) of the studies assessed whether simulation-based training resulted in a decrease in errors. Errors were reported as clipping errors, dissection errors, tissue damage, incorrect plane for dissection, lack of progress, and instrument out of view. All seven-research articles reported statistical findings that the intervention decreased the amount of errors that occurred. For example, investigators that the intervention group made significantly fewer errors related to tissue division (P=.008) and dissection (P=.03) with the control group producing three times as many errors (Ahlberg et al., 2007).
3.4 Economy of Movement (n = 8 Studies) (Bennett et al., 2011; Andreatta et al., 2006; Aggarwal et al., 2007; Ahlberg et al., 2002; Gala et al., 2013; Hogle et al., 2009; Zendejas et al., 2011; Torkington et al., 2001)
Eight of the studies assessed if simulation-based training resulted in an increase in the economy of movement. Economy of movement was reported as camera navigation, efficiency of instrument, total path length, number of movements, navigation, and bimanual dexterity. The eight studies (38%) reported statistical findings that the intervention increased the economy of movement. More specifically, training was significantly related to path length (P<.001) and total number of movements (P =.009) (Aggarwal et al., 2007). In contrast, investigators found no difference in economy of movement between the control and intervention groups (P =.40) (Bennett et al., 2011). In two different studies, researchers found that the control groups did not show significant differences compared to the intervention group as related to economy of movement (Bennett et al., 2011; Hogle et al., 2009).
4. Discussion
This review of laparoscopic literature and translation of skills summarizes the evidence for the simulation-based training studies and supports skill transfer in a safe and effective way for novice surgeons to learn to perform procedures on patients in the OR (Table 3). Those responsible for teaching and assessing surgical performance should consider implications of these findings in three major areas: (1) education for competence or improved skills practiced in a controlled setting, (2) translation of new knowledge into performance outside the simulated setting, and (3) safety for patients.
5. Education
Laparoscopic surgery curricula may be modified or supplemented with the implementation of simulation-based training. Simulation can lead to improved assessment, improved training, error reduction, and the development of technical skills in laparoscopic surgery necessary to operate on real patients (Van Sickle et al., 2008). Residents in the intervention group made fewer errors and were less likely to injure the gallbladder or to burn non-target tissue on real patients (Van Sickle et al., 2008). Simulation-based training allows for repeated practice of standardized tasks under reproducible conditions and enables the use of objective measures for assessment purposes (Sroka, Feldman, Vassiliou, Kaneva, Fayez, & Fried, 2010) and student feedback. A simulation-based training curriculum has the potential to shorten the learning time for laparoscopic procedures compared to traditional teaching methods in laparoscopic surgery (Seymour et al., 2002).
Surgical residents who received simulation-based training curriculum significantly outperformed surgical residents who received the standard curriculum on knot tying (Zendejas et al., 2011). Additionally, surgical residents who received simulation-based training performed the suturing task faster, made fewer errors, and were more efficient in handling the suture (Zendejas et al., 2011). Overall, participants who received simulation based skills training demonstrated faster attainment of those skills than their peers from the control group in a high stakes environment (Grantcharov et al., 2004). Training curriculum related to laparoscopic surgery skills allows for more learning opportunities for novice surgeons to practice with simulation-based training prior to entering OR environment; thus, allowing for the potential of skills translating into the OR.
Finally, the studies in this review show that simulation-based training should be incorporated into surgical curricula specifically targeting novice learners. Presently, simulation-based training programs are generally offered as a supplement to traditional surgical training and are voluntary (Graber, Wyatt, Kasparek, & Xu, 2005). Currently, there is not a standard or universal specific surgical curriculum in place in surgical educational programs; however, there has been a recent change, FES (Fundamentals of Endoscopic Surgery) was approved in March, 2014 as an additional requirement for residents graduating in 2018 and after this is a simulation-based training program.
Further research is needed to determine the best longitudinal curriculum for basic and advanced skills acquisition and transfer to the OR environment. Simulation-based training will allow for the novice to learn the psychomotor skills and spatial judgments necessary for laparoscopic surgical skills allowing them to focus more on learning operative strategies and handling intraoperative complications while in the OR (Torkington, Smith, Rees, & Darzi, 2001). Training in proficiency-based skills should be incorporated into a comprehensive surgical training and assessment curriculum for residents prior to operating on real patients (Banks, Chudnoff, Karmin, Wang, & Pardanani, 2007). The pressure to make surgical training more efficient and safer for patients is substantial, and simulation-based training has the potential to improve surgical curricula (Clevin & Grantcharov, 2008).
6. Translation
Translational impact was achieved in the OR with live patients when simulation-based training was used for the educational intervention. Researchers found that training in a simulated environment led to improved surgical performance on either animals or humans (Ahlberg et al., 2007; Verdaasdonk et al., 2008; Ahlberg et al., 2002; Van Sickle et al., 2008; Seymour et al., 2002; Zendejas et al., 2011; Banks et al., 2007; Clevin & Grantcharov, 2008; Crochet et al., 2011). Simulation-based training, influences the translation of laparoscopic surgery skills to the OR. As a result of these findings, simulation-based training has the potential to provide the foundational skills necessary for future surgeons to learn in a controlled environment and translate those acquired skills to the OR. With increases in technology and the need for a standard surgical curricula there is potential with simulation as an educational tool to further the translation of laparoscopic surgical skills into the OR. More specifically, typical skills that translate into the OR are suturing, camera navigation, and the manipulation of equipment.
7. Patient Safety
Simulation-based training has the potential to lead to an increase in patient safety. Residents who trained with simulation had fewer errors than control groups (Van Sickle et al., 2008; Hiemstra et al., 2011) while in the OR. Participants in the intervention group had fewer incidents of the supervising surgeon taking over the procedure. These types of events can significantly affect clinical outcomes because they represent potential errors in technique compromising patient safety (Ahlberg et al., 2002).
Using simulation for training surgical skills can benefit the larger goal of improved patient safety in several ways. With simulation, learners can repeat a procedure or even a specific element of a procedure until competency is demonstrated. Novice surgeons enter the OR more apt to produce favorable patient outcomes and are better prepared to participate in surgical cases with live patients in the OR if they previously trained on a simulator. Simulation can also provide more opportunities for remedial training to reduce skill decay (Sroka et al., 2010). Laparoscopic surgical simulators provide opportunities to train other concepts central to patient safety. For example, teamwork skills can be trained through surgeons interacting with camera navigators or nurses in a simulated OR. Simulating laparoscopic surgical equipment and interfaces can even be used to introduce, test, and train new equipment or protocols before they are implemented in the OR, leading to identification of potential latent threats to safety and avoidance of medical errors due to poor human systems integrations.
8. Limitations
As with any literature review, our review and results are limited by the data provided in the original studies. Our findings are limited by the lack of descriptions of the data collection process and interventions of the included studies. In particular, it was difficult to discern many of the potential covariates that were used in the data analyses as well as the timing between pre- and post-tests once the interventions were implemented. Moreover, a majority of the studies that reported statistical results reported the results using p-values. The lack of effect size reporting contributes to the difficulty in truly understanding the magnitude of the effect of these interventions on the acquisition of surgical skills.
Another limitation to this study is this was only one database was used to identify all literature, data, or studies related to a specific topic. Therefore, potentially, excluding conference presentations, other online search engines, and contacting colleagues within the field to identify any potential missing studies that may not have been included. Furthermore, not all surgical journals were hand searched, just those identified by one author as to be key surgery journals within the field.
The scope of our review is both a strength and limitation. Restricting our scope to only randomized control trials increased the stability of the findings reported in the original studies. However, it is not possible to draw firm conclusions about the effectiveness of the different types of simulation based on our findings as many of the RCTs did not conduct comparative analyses between varying types of simulations. Nonetheless, we argue that our review does provide useful insight into the literature that examines the effectiveness of simulation based laparoscopic training interventions. The need for more robust comparisons of these training interventions is needed to be able to provide an unequivocal conclusion to the impact on surgical skills.
9. Conclusion
Simulation-based training can lead to demonstrable benefits of surgical skills in the OR. These benefits include decreased procedural errors as well as other effects on overall patient safety. This review suggests that simulation-based training is an effective way to teach laparoscopic surgery skills, increase translation of laparoscopic surgical skills to the OR and increase patient safety. However, more research should be conducted to determine if and how simulation can become apart of the surgical curriculum.
Acknowledgments
Funding/Support
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Drs. DiazGranados and Feldman are supported by award number UL1TR000058 from the National Center for Research Resources and NIH Roadmap for Medical Research, National Institutes of Health. The contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Footnotes
Other Disclosures
None.
Ethical Approval
N/A.
Disclaimer
The contents are solely the opinions of the authors.
Previous Presentations
None.
References
- Aggarwal R, Ward J, Balasundaram I, Sains P, Athanasiou T, Darzi A. Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Annals of surgery. 2007;246(5):771–779. doi: 10.1097/SLA.0b013e3180f61b09. [DOI] [PubMed] [Google Scholar]
- Ahlberg G, Enochsson L, Gallagher AG, Hedman L, Hogman C, McClusky DA, III, Arvidsson D. Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. The American journal of surgery. 2007;193(6):797–804. doi: 10.1016/j.amjsurg.2006.06.050. [DOI] [PubMed] [Google Scholar]
- Ahlberg G, Heikkinen T, Iselius L, Leijonmarck CE, Rutqvist J, Arvidsson D. Does training in a virtual reality simulator improve surgical performance? Surgical Endoscopy and Other Interventional Techniques. 2002;16(1):126–129. doi: 10.1007/s00464-001-9025-6. [DOI] [PubMed] [Google Scholar]
- Andreatta PB, Woodrum DT, Birkmeyer JD, Yellamanchilli RK, Doherty GM, Gauger PG, Minter RM. Laparoscopic skills are improved with LapMentor™ training: results of a randomized, double-blinded study. Annals of surgery. 2006;243(6):854. doi: 10.1097/01.sla.0000219641.79092.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks EH, Chudnoff S, Karmin I, Wang C, Pardanani S. Does a surgical simulator improve resident operative performance of laparoscopic tubal ligation? American journal of obstetrics and gynecology. 2007;197(5):541–e1. doi: 10.1016/j.ajog.2007.07.028. [DOI] [PubMed] [Google Scholar]
- Bennett A, Birch DW, Menzes C, Vizhul A, Karmali S. Assessment of medical student laparoscopic camera skills and the impact of formal camera training. The American journal of surgery. 2011;201(5):655–659. doi: 10.1016/j.amjsurg.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Clevin L, Grantcharov TP. Does box model training improve surgical dexterity and economy of movement during virtual reality laparoscopy? A randomized trial. Obstetrical & Gynecological Survey. 2008;63(5):301–303. doi: 10.1080/00016340701789929. http://dx.doi.org/10.1080/00016340701789929. [DOI] [PubMed] [Google Scholar]
- Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Hamstra SJ. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. Jama. 2011;306(9):978–988. doi: 10.1001/jama.2011.1234. [DOI] [PubMed] [Google Scholar]
- Crochet P, Aggarwal R, Dubb SS, Ziprin P, Rajaretnam N, Grantcharov T, Darzi A. Deliberate practice on a virtual reality laparoscopic simulator enhances the quality of surgical technical skills. Annals of surgery. 2011;253(6):1216–1222. doi: 10.1097/SLA.0b013e3182197016. http://dx.doi.org/10.1097/SLA.0b013e3182197016. [DOI] [PubMed] [Google Scholar]
- Ehdaie B, Tracy C, Reynolds C, Cung B, Thomas K, Floyd T, Schenkman N. Evaluation of laparoscopic curricula in American urology residency training. Journal of Endourology. 2011;25(11):1805–1810. doi: 10.1089/end.2011.0213. [DOI] [PubMed] [Google Scholar]
- Gala R, Orejuela F, Gerten K, Lockrow E, Kilpatrick C, Chohan L, Schaffer J. Effect of validated skills simulation on operating room performance in obstetrics and gynecology residents: a randomized controlled trial. Obstetrics & Gynecology. 2013;121(3):578–584. doi: 10.1097/AOG.0b013e318283578b. http://dx.doi.org/10.1097/AOG.0b013e318283578b. [DOI] [PubMed] [Google Scholar]
- Ganai S, Donroe JA, St Louis MR, Lewis GM, Seymour NE. Virtual-reality training improves angled telescope skills in novice laparoscopists. The American journal of surgery. 2007;193(2):260–265. doi: 10.1016/j.amjsurg.2005.11.019. http://dx.doi.org/10.1016/j.amjsurg.2005.11.019. [DOI] [PubMed] [Google Scholar]
- Graber MA, Wyatt C, Kasparek L, Xu Y. Does simulator training for medical students change patient opinions and attitudes toward medical student procedures in the emergency department? Academic emergency medicine. 2005;12(7):635–639. doi: 10.1197/j.aem.2005.01.009. http://dx.doi.org/10.1111/j.1553-2712.2005.tb00920.x. [DOI] [PubMed] [Google Scholar]
- Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. British Journal of Surgery. 2004;91(2):146–150. doi: 10.1002/bjs.4407. http://dx.doi.org/10.1002/bjs.4407. [DOI] [PubMed] [Google Scholar]
- Gurusamy K, Aggarwal R, Palanivelu L, Davidson BR. Systematic review of randomized controlled trials on the effectiveness of virtual reality training for laparoscopic surgery. British Journal of Surgery. 2008;95(9):1088–1097. doi: 10.1002/bjs.6344. [DOI] [PubMed] [Google Scholar]
- Hiemstra E, Terveer EM, Chmarra MK, Dankelman J, Jansen FW. Virtual reality in laparoscopic skills training: Is haptic feedback replaceable? Minimally Invasive Therapy & Allied Technologies. 2011;20(3):179–184. doi: 10.3109/13645706.2010.532502. http://dx.doi.org/10.3109/13645706.2010.532502. [DOI] [PubMed] [Google Scholar]
- Higgins JPT. Green S. Cochrane handbook for systematic reviews of interventions Version 5.1. 0 [updated March 2011] The Cochrane Collaboration. 2012;2011 www.cochrane-handbook.Org. [Google Scholar]
- Hogle NJ, Chang L, Strong VEM, Welcome AOU, Sinaan M, Bailey R, Fowler DL. Validation of laparoscopic surgical skills training outside the operating room: a long road. Surgical endoscopy. 2009;23(7):1476–1482. doi: 10.1007/s00464-009-0379-5. http://dx.doi.org/10.1007/s00464-009-0379-5. [DOI] [PubMed] [Google Scholar]
- Hung AJ, Patil MB, Zehnder P, Cai J, Ng CK, Aron M, Desai MM. Concurrent and predictive validation of a novel robotic surgery simulator: a prospective, randomized study. The Journal of urology. 2012;187(2):630–637. doi: 10.1016/j.juro.2011.09.154. http://dx.doi.org/10.1016/j.juro.2011.09.154. [DOI] [PubMed] [Google Scholar]
- Hyltander A, Liljegren E, Rhodin PH, Lönroth H. The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surgical Endoscopy and Other Interventional Techniques. 2002;16(9):1324–1328. doi: 10.1007/s00464-001-9184-5. [DOI] [PubMed] [Google Scholar]
- Johnson MD, Walsh RM. Current therapies to shorten postoperative ileus. Cleveland Clinic journal of medicine. 2009;76(11):641–648. doi: 10.3949/ccjm.76a.09051. [DOI] [PubMed] [Google Scholar]
- Jordan JA, Gallagher AG, McGuigan J, McGlade K, McClure N. A comparison between randomly alternating imaging, normal laparoscopic imaging, and virtual reality training in laparoscopic psychomotor skill acquisition. The American journal of surgery. 2000;180(3):208–211. doi: 10.1016/s0002-9610(00)00469-4. [DOI] [PubMed] [Google Scholar]
- Korndorffer JR, Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ. Simulator training for laparoscopic suturing using performance goals translates to the operating room. Journal of the American College of Surgeons. 2005;201(1):23–29. doi: 10.1016/j.jamcollsurg.2005.02.021. http://dx.doi.org/10.1016/j.jamcollsurg.2005.02.021. [DOI] [PubMed] [Google Scholar]
- Larsen CR, Soerensen JL, Grantcharov TP, Dalsgaard T, Schouenborg L, Ottosen C, Ottesen BS. Effect of virtual reality training on laparoscopic surgery: randomised controlled trial. Bmj. 2009;338 doi: 10.1136/bmj.b1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-anlyses of studies that evaluate healthcare interventions: exploration and elaboration. Br Med J. 2009:339. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas S, Tuncel A, Bensalah K, Zeltser I, Jenkins A, Pearle M, Cadeddu J. Virtual reality training improves simulated laparoscopic surgery performance in laparoscopy naive medical students. Journal of Endourology. 2008;22(5):1047–1052. doi: 10.1089/end.2007.0366. http://dx.doi.org/10.1089/end.2007.0366. [DOI] [PubMed] [Google Scholar]
- McGaghie WC, Siddall VJ, Mazmanian PE, Myers J. American College of Chest Physicians Health and Science Policy Committee. Lessons for continuing medical education from simulation research in undergraduate and graduate medical education: effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest. 2009;135(3 Suppl):62S–68S. doi: 10.1378/chest.08-2521. [DOI] [PubMed] [Google Scholar]
- Miskovic D, Wyles SM, Ni M, Darzi AW, Hanna GB. Systematic review on mentoring and simulation in laparoscopic colorectal surgery. Annals of surgery. 2010;252(6):943–951. doi: 10.1097/SLA.0b013e3181f662e5. [DOI] [PubMed] [Google Scholar]
- Munz Y, Kumar BD, Moorthy K, Bann S, Darzi A. Laparoscopic virtual reality and box trainers: is one superior to the other? Surgical Endoscopy And Other Interventional Techniques. 2004;18(3):485–494. doi: 10.1007/s00464-003-9043-7. [DOI] [PubMed] [Google Scholar]
- Richardson WS, Carter KM, Fuhrman GM, Bolton JS, Bowen JC. Minimally Invasive Abdominal Surgery. The Ochsner Journal. 2000;2(3):153–157. [PMC free article] [PubMed] [Google Scholar]
- Seropian M, Lavey R. Design considerations for healthcare simulation facilities. Simulation in Healthcare. 2010;5(6):338–345. doi: 10.1097/SIH.0b013e3181ec8f60. [DOI] [PubMed] [Google Scholar]
- Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Annals of surgery. 2002;236(4):458. doi: 10.1097/00000658-200210000-00008. http://dx.doi.org/10.1097/00000658-200210000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM. Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room—a randomized controlled trial. The American journal of surgery. 2010;199(1):115–120. doi: 10.1016/j.amjsurg.2009.07.035. http://dx.doi.org/10.1016/j.amjsurg.2009.07.035. [DOI] [PubMed] [Google Scholar]
- Stefanidis D, Acker C, Heniford BT. Proficiency-based laparoscopic simulator training leads to improved operating room skill that is resistant to decay. Surgical innovation. 2008;15(1):69–73. doi: 10.1177/1553350608316683. http://dx.doi.org/10.1177/1553350608316683. [DOI] [PubMed] [Google Scholar]
- Stefanidis D, Korndorffer JR, Jr, Markley S, Sierra R, Heniford BT, Scott DJ. Closing the gap in operative performance between novices and experts: does harder mean better for laparoscopic simulator training? Journal of the American College of Surgeons. 2007;205(2):307–313. doi: 10.1016/j.jamcollsurg.2007.02.080. http://dx.doi.org/10.1016/j.jamcollsurg.2007.02.080. [DOI] [PubMed] [Google Scholar]
- Sturm LP, Windsor JA, Cosman PH, Cregan P, Hewett PJ, Maddern GJ. A systematic review of skills transfer after surgical simulation training. Annals of surgery. 2008;248(2):166–179. doi: 10.1097/SLA.0b013e318176bf24. [DOI] [PubMed] [Google Scholar]
- Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D, Maddern GJ. Surgical simulation: a systematic review. Annals of surgery. 2006;243(3):291. doi: 10.1097/01.sla.0000200839.93965.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torkington J, Smith SGT, Rees BI, Darzi A. Skill transfer from virtual reality to a real laparoscopic task. Surgical endoscopy. 2001;15(10):1076–1079. doi: 10.1007/s004640000233. http://dx.doi.org/10.1007/s004640000233. [DOI] [PubMed] [Google Scholar]
- Van Sickle KR, Ritter EM, Baghai M, Goldenberg AE, Huang IP, Gallagher AG, Smith CD. Prospective, randomized, double-blind trial of curriculum-based training for intracorporeal suturing and knot tying. Journal of the American College of Surgeons. 2008;207(4):560–568. doi: 10.1016/j.jamcollsurg.2008.05.007. http://dx.doi.org/10.1016/j.jamcollsurg.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Verdaasdonk EGG, Dankelman J, Lange JF, Stassen LPS. Transfer validity of laparoscopic knot-tying training on a VR simulator to a realistic environment: a randomized controlled trial. Surgical endoscopy. 2008;22(7):1636–1642. doi: 10.1007/s00464-007-9672-3. [DOI] [PubMed] [Google Scholar]
- Watterson JD, Beiko DT, Kuan JK, Denstedt JD. A randomized prospective blinded study validating acquistion of ureteroscopy skills using a computer based virtual reality endourological simulator. The Journal of urology. 2002;168(5):1928–1932. doi: 10.1016/S0022-5347(05)64265-6. http://dx.doi.org/10.1016/S0022-5347(05)64265-6. [DOI] [PubMed] [Google Scholar]
- Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG, Farley DR. Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Annals of surgery. 2011;254(3):502–511. doi: 10.1097/SLA.0b013e31822c6994. http://dx.doi.org/10.1097/SLA.0b013e31822c6994. [DOI] [PubMed] [Google Scholar]