Abstract
Community engagement is recommended to ensure the public health impact of NIH-funded science. To understand the prevalence of community-engaged research and faculty interest in and needs around this, from 2012–2013, an online survey (n=3,022) was sent to UCLA Clinical and Translational Science Institute faculty. Among respondents, 45% reported community-engaged project participation in the last year and 64% an interest in learning about community-engaged research. Over 50% indicated career development and pilot grants would increase participation in community-engaged research. A greater percentage of pre-tenure than tenured faculty (pre-tenure 54.9%, tenured 42.2%, p=0008) noted faculty promotion criteria incentivizing community-engaged research would increase participation. In adjusted analyses, African American (OR 4.06, CI 1.68–9.82, p=0.002) and Latino (OR 1.91, CI 1.10–3.33, p=0.022) faculty had higher odds of prior participation in community-engaged projects than Whites. Female faculty had greater odds of interest (OR 1.40, CI 1.02–1.93, p=0.038) in learning about community-engaged research than males. African American (OR 4.31, CI 1.42–13.08, p=0.010) and Asian/Pacific Islander (OR 2.24, CI 1.52–3.28, p<0.001) faculty had greater interest in learning about community-engaged research than Whites. To build community-engaged faculty research capacity, CTSAs’ may need to focus resources on female and minority faculty development.
INTRODUCTION
The National Institutes of Health (NIH) Clinical and Translational Science Awards (CTSAs) are a biomedical research infrastructure supporting the rapid translation of science into public health impact.1 Community engagement, “the process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people” is recommended in all CTSA components to enhance translation. In fact, strengthening community engagement’s integration throughout the translational science spectrum is recognized as a powerful approach to reach underserved populations, local community organizations, and healthcare providers to ensure that medical advances are reaching people in need.3,4
Despite its potential to enhance the real world impact of science, a recent Institute of Medicine report evaluating the CTSAs noted a paucity of investigation regarding the prevalence and effectiveness of community engagement in research.1,5 To better understand where and how to build on existing CTSAs’ community engagement capacity, several institutions have conducted surveys to evaluate existing community engagement efforts with NIH-funded research and investigators.6,7
The mission of the UCLA Clinical and Translational Science Institute’s (CTSI), comprised of UCLA, Cedars-Sinai Medical Center, Charles R. Drew University (CDU), and Los Angeles Biomedical Research Institute (LA Biomed)/Harbor-UCLA Medical Center, is “to create a borderless institute that brings UCLA resources and innovations to bear on the greatest health needs of Los Angeles.”8 Within the UCLA CTSI, the Community Engagement and Research Program (CERP) facilitates research collaborations between faculty and community stakeholders.9 To better understand the prevalence of community-engaged research and faculty interest in and needs around this research, CERP conducted a survey of all UCLA CTSI faculty. This paper adds to the existing literature on community-engaged research in CTSAs by using, multivariable analyses to examine factors associated with participation in and interest in community-engaged research in a large multi-institutional CTSA.
METHODS
Survey Sample and Administration
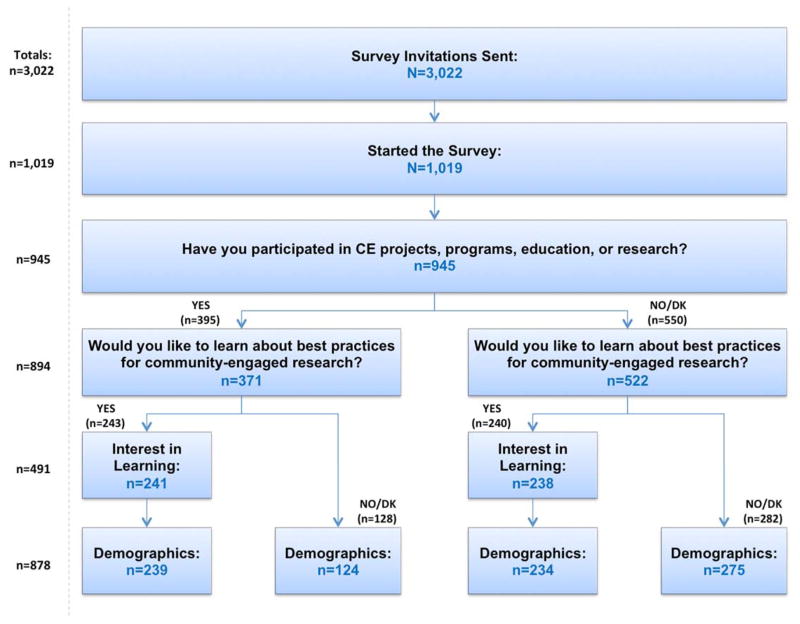
An online survey was sent to 10,305 persons from the following categories: (1) UCLA David Geffen School of Medicine (DGSOM), UCLA Health System (UCLA Health), and UCLA School of Dentistry students, residents, clinical fellows, post-graduate researchers, staff, and faculty; (2) UCLA CTSI affiliated institutions’ faculty and staff (3) UCLA School of Nursing faculty; and (4) UCLA Health providers, staff, and administrators without academic appointments. Eligible participants for this report were the 3,022 with faculty appointments at UCLA DGSOM, Schools of Dentistry and Nursing (UCLA Westwood, UCLA Santa Monica Hospital, Harbor-UCLA Medical Center, CDU, Cedars-Sinai, Olive View Medical Center, Greater Los Angeles Veterans Administration Healthcare System) and for individuals without UCLA appointments at the three UCLA CTSI-affiliated institutions (Cedars-Sinai, CDU, LA Biomed/Harbor-UCLA Medical Center) at the time of the survey. With the exception of the UCLA School of Nursing, the survey was not anonymous and was distributed in 3 waves from 2012–2013 via e-mail using a UCLA developed, open-source, survey software (Web-based Interactive Survey Environment), tracking non-responders, partial completers, and completers. Each survey wave was deployed over six weeks with up to six reminder e-mails sent to partial completers and non-responders. A one-time survey link was e-mailed by the UCLA School of Nursing Dean’s Office to their faculty. All respondents completing the survey were enrolled in a weekly raffle for an iPad. Of 3,022 faculty sent invitations, 33.7% (n=1,019) started the survey. Survey item response rates in this manuscript ranged from 92.7% (n=945/1,019) to 86.1% (n=878/945). (Figure 1)
Figure 1.
Faculty Survey Profile
Measures
The survey collected data on prior participation in community-engaged programs; interest in learning about best practices for community-engaged research; projected hours an individual would be able to commit in community-engaged research in a year; incentives that would increase the likelihood a respondent would participate in opportunities to learn about community-engaged research, demographic characteristics, and primary academic affiliation. (Figure 1) The NIH definition of community-engagement prior was provided in the survey introduction.2
The Institutional Review Boards of UCLA and VA Greater Los Angeles Healthcare System determined that the survey was not human subjects research.
Data Analysis
Categorical variables were summarized by frequencies and percentages of non-missing values, and continuous variables were summarized by means and standard deviations. Due to varying survey item response rates for different questions, we report the number of respondents selecting one or more responses for each survey item. Survey respondents were stratified by faculty rank into clinical instructor, assistant professor, associate professor, and professor. We report unadjusted comparisons of each item between pre-tenure (clinical instructor, assistant professor) and tenured (associate and full professor) faculty using chi-squared and fisher’s exact tests where appropriate. Analyses were not adjusted by site (e.g. hospital, School of Nursing), because we did not expect site differences due to UCLA CTSI faculty being within the same system. Logistic regression models were used to identify characteristics associated with past participation in community-engaged research, as well as interest in learning about best practices. Models were adjusted for gender, age, race/ethnicity, education level, discipline, and faculty rank. All covariates included a category for non-response to include incomplete cases in the analysis. Odds ratios and 95% confidence intervals for each covariate were reported. A p-value < 0.05 was considered statistically significant. We conducted sensitivity analyses using faculty rank instead of tenure status in the unadjusted and adjusted models. All analyses were performed using SAS v. 9.3 (SAS Institute, Cary, NC).
RESULTS
Demographics
Of 923 faculty completing the demographics section (Table 1), 13.0% (n=120/923) were clinical instructors/lecturers, 32.5% (n=300/923) were assistant professors, 21.6% (n=200/923) were associate professors, and 32.8% (n=303/923) were full professors. Slightly more than half were male. Almost all, 98.2% had a doctoral degree (e.g. MD, DDS, DrPH, or PhD). Over 60% of respondents were physicians, about 10% dentists, and 18.6% scientists from basic and social science or statistics. Of note, 12 (1.3%) were allied health professionals without doctoral degrees such as dental hygienists.
Table 1.
Demographic Characteristics by Faculty Rank
| N (%) | All Faculty | Clinical Instructor/Lecturer | Assistant Professor | Associate Professor | Full Professor |
|---|---|---|---|---|---|
|
| |||||
| (N=923) | (N=120) | (N=300) | (N=200) | (N=303) | |
| Age (n=852) | |||||
| 20–30 | 11 (1.3) | 10 (8.7) | 1 (0.4) | 0 | 0 |
| 31–40 | 253 (29.7) | 61 (53.0) | 173 (61.6) | 18 (9.7) | 1 (0.4) |
| 41–50 | 280 (32.9) | 20 (17.4) | 89 (31.7) | 113 (61.1) | 58 (21.4) |
| 51–60 | 192 (22.5) | 17 (14.8) | 14 (5.0) | 41 (22.2) | 120 (44.3) |
| 61–70 | 91 (10.7) | 4 (3.5) | 4 (1.4) | 11 (6.0) | 72 (26.6) |
| 71 and over | 25 (2.9) | 3 (2.6) | 0 | 2 (1.1) | 20 (7.4) |
| Female (n=921) | 403 (43.8) | 60 (50.0) | 153 (51.2) | 89 (44.7) | 101 (33.3) |
| Ethnicity (n=918) | |||||
| White | 580 (63.2) | 71 (59.2) | 162 (54.4) | 122 (61.6) | 225 (74.5) |
| Asian/Pacific Islander | 249 (27.1) | 35 (29.2) | 100 (33.6) | 59 (29.8) | 55 (18.2) |
| Hispanic/Latino | 59 (6.4) | 8 (6.7) | 27 (9.1) | 11 (5.6) | 13 (4.3) |
| African American | 30 (3.3) | 6 (5.0) | 9 (3.0) | 6 (3.0) | 9 (3.0) |
| Education (n=921) | |||||
| Less than master’s degree | 5 (0.5) | 3 (2.5) | 1 (0.3) | 0 | 1 (0.3) |
| Master’s degree | 12 (1.3) | 5 (4.2) | 3 (1.0) | 3 (1.5) | 1 (0.3) |
| DrPH or PhD | 255 (27.7) | 7 (5.8) | 93 (31.1) | 60 (30.2) | 95 (31.4) |
| DDS or MD | 649 (70.5) | 105 (87.5) | 202 (67.6) | 136 (68.3) | 206 (68.0) |
| Discipline (n=919) | |||||
| Physician | 585 (63.7) | 55 (46.2) | 202 (67.6) | 132 (66.7) | 196 (64.7) |
| Basic/social science, statistics | 171 (18.6) | 1 (0.8) | 64 (21.4) | 50 (25.3) | 56 (18.5) |
| Dentistry | 91 (9.9) | 57 (47.9) | 9 (3.0) | 5 (2.5) | 20 (6.6) |
| Psychology | 52 (5.7) | 4 (3.4) | 16 (5.4) | 9 (4.6) | 23 (7.6) |
| Allied health professional | 12 (1.3) | 2 (1.7) | 6 (2.0) | 0 | 4 (1.3) |
| Health system administrator | 8 (0.9) | 0 | 2 (0.7) | 2 (1.0) | 4 (1.3) |
Prior experience in community-engaged projects
Slightly less than half, 45.5% (n=395/923) of respondents had prior experience with community-engaged projects, programs, education, or research (Table 2). A significantly lower percentage of pre-tenure had prior experience in community-engaged work than tenured faculty (pre-tenure 39.7%, n=156/420; tenured 50.3%, n=239/503; p=0.002). More than half (64.2%, n=483/923) expressed interest in learning about community-engaged research with no significant differences by tenure status.
Table 2.
Prior experience in community-engaged projects and interest in and preferred training approaches for learning about community-engaged research by faculty tenure status*
| N (%) | All Faculty | Pre-Tenure+ | Tenured‡ | P |
|---|---|---|---|---|
|
| ||||
| (N=923) | (N=420) | (N=503) | ||
| From January 1, 2011 to present, have you participated in community-engaged projects, programs, education, or research? (n=868), n(%) | 395 (45.5) | 156 (39.7) | 239 (50.3) | 0.002 |
| Would you like to learn about best practices for community-engaged research? (n=752), n(%) | 483 (64.2) | 210 (62.5) | 273 (65.6) | 0.374 |
| What would be the best delivery mode for you to learn about community-engaged research? Select all that apply. (n=475)§, n(%) | ||||
| Seminar, grand rounds, conference, self- directed online learning opportunities | 436 (91.8) | 188 (89.5) | 248 (93.6) | 0.109 |
| Participation in current community partnered research projects, meeting community partners, formal mentorship, consultation | 247 (52.0) | 114 (54.3) | 133 (50.2) | 0.375 |
| What are your barriers to conducting community- engaged research? Select all that apply. (n=458) §, n(%) | ||||
| Lack of time | 337 (73.6) | 157 (75.5) | 180 (72.0) | 0.400 |
| Lack of capacity/skill | 98 (21.4) | 42 (20.2) | 56 (22.4) | 0.566 |
| Lack of funding (opportunities) | 268 (58.5) | 115 (55.3) | 153 (61.2) | 0.201 |
| Lack of access to community partners | 128 (27.9) | 62 (29.8) | 66 (26.4) | 0.418 |
| Lack of incentive/reward structure | 106 (23.1) | 58 (27.9) | 48 (19.2) | 0.028 |
| What would increase the likelihood you would participate in opportunities to learn about community-engaged research? Select all that apply. (n=439) §, n(%) | ||||
| Career development grants that would protect time to conduct research | 253 (57.6) | 133 (68.2) | 120 (49.2) | <0.001 |
| Convenience of learning opportunities on how to conduct community engaged research | 257 (58.5) | 116 (59.5) | 141 (57.8) | 0.719 |
| Pilot grant awards in community engaged research | 277 (63.1) | 121 (62.1) | 156 (63.9) | 0.685 |
| Improved access to community partners | 209 (47.6) | 97 (49.7) | 112 (45.9) | 0.423 |
| Faculty promotion criteria that incentivize community engaged research | 210 (47.8) | 107 (54.9) | 103 (42.2) | 0.008 |
| How many hours would you be open to committing to learning about community- engaged research per year? (n=380) | 0.020 | |||
| Mean (SD) | 24.8 (43.1) | 30.9 (54.0) | 20.0 (31.1) | |
| Median (Min-Max) | 10 (0.5–480) | 12 (0.5–480) | 10 (1–200) | |
Data are presented as No. (%) or mean (SD). Chi-square and fisher’s exact tests were used for comparing two groups.
Pre-tenure: Clinical Instructor, Assistant Professor, Associate Professor;
Tenured: Associate Professor, Professor.
“n” indicates the number of respondents selecting one or more survey item response options.
Best mode and incentives to learn community-engaged research
Of the 475 faculty providing at least one response to the survey item asking what the best modes for learning about community engaged research, 91.8% (n=436/475) selected seminars, grand rounds, self-directed online learning opportunities and 52.0% (n=247/475) selected participation in community partnered research project, meeting community partners, formal mentorship and consultation with no significant differences by tenure status. About 15% (15.6%, n=74/475) selected one, 33.7% (n=160/475) two, and 16.4% (n=78/475) selected three response options (not in tables).
Of 458 faculty providing at least one response to the survey item asking what were the barriers to conducting community-engaged research, 73.6% (n=337/458) selected lack of time, 21.4% (n=98/458) funding, 27.9% (n=128/458) access to community partners, and 23.1% incentive/reward structure. A significantly greater percentage of pre-tenure than tenured faculty endorsed lack of inventive/reward structure as a barrier (27.9% vs. 19.2% respectively, p=0.028). Forty percent (n=183/458) selected one, 28.4% two, 22.3% (n=102/458) three, 5.9% (n=27/458) four, and 3.5% (n=16/458) selected five response options (not in tables).
Of 439 faculty providing at least one response to the survey item asking what would increase the likelihood of participating in opportunities to learn about community-engaged research across all faculty, 73.6% (n=337/439) noted career development awards to protect time; 58.5% (n=257/439) convenience of learning opportunities, 63.1% (n=277/439) pilot grants, 47.6% (n=209/439) improved access to community partners; and 47.8% (n=210/439) cited faculty promotion criteria. A significantly greater percentage of pre-tenure than tenured faculty noted career development grants (68.2% vs. 49.2% respectively, p<0.001) and faculty promotion criteria incentivizing community-engaged research (54.9% vs. 42.2% respectively, p=0008) would increase the likelihood of participating in learning opportunities. One-fifth (n=88/439) selected one, 26.7% (n=113/439) two, and 26.0% (n=114/439), 15.9% (n=70/439) four, and 12.3% (n=54/439) selected all five responses (not in tables). Faculty indicated that being open to an average of 24.8 hours/year (range 0.5 – 480 hours/year) to learn about community-engaged research.
Logistic regression models for past participation and interest in learning about CE best practices
In adjusted analyses, African American (OR 4.06, CI 1.68–9.82, p=0.002) and Latino (OR 1.91, CI 1.10–3.33, p=0.022) faculty had higher odds of prior participation in community-engaged projects compared to Whites. Basic scientists, social scientists, and statisticians had lower odds of prior participation (OR 0.54, CI 0.32–0.91, p=0.020) than physicians, dentists, psychologists, health systems administrators, and allied health professionals. There was a trend toward tenured faculties’ odds of prior participation in community-engaged projects to exceed pre-tenure faculty, but it did not reach statistical significance (OR 1.44, CI 1.00 –2.07, p=0.052).
Female faculty had greater odds of interest (OR 1.40, CI 1.02–1.93, p=0.038) in learning about best practices in community-engaged research than males. African American (OR 4.31, CI 1.42–13.08, p=0.010) and Asian or Pacific Islander (OR 2.24, CI 1.52–3.28, p<0.001) faculty had greater interest in learning about community-engaged research than Whites. Tenured faculty had greater interest (OR 1.70, CI 1.11–2.06, p=0.014) in learning about community-engaged research than pre-tenured faculty.
DISCUSSION
Although reports have noted the need to enhance NIH CTSAs’ capacity for community-engaged research, few publications provide evidence on the prevalence and scope of community-engaged research activity and interests within CTSAs.1,10 Our report adds important information on the capacity for and interests in community-engaged research within the UCLA CTSI. Overall, slightly more than 40% of faculty respondents reported prior experience in community-engaged projects, programs, education, or research, while over half had interest in learning about community-engaged research, similar to Ohio State’s CTSA (42.6%),7 though lower than the Harvard CTSA (58%).6 Unlike our study, both reports surveyed a select subset of CTSA investigators. Regardless of past experience, about half of UCLA respondents expressed interest in learning about community-engaged research—levels similar to Harvard Catalyst. With over 800 respondents, our study has a substantially larger sample than prior reports and is the only study to our knowledge with sufficient diversity to explore racial/ethnic and tenure track differences in participation and interest in community engagement.
UCLA CTSI minority faculty were more likely than Whites to have interest in and to have participated in community-engaged research. Specifically, African American and Latinos had over four times and nearly two times higher odds, respectively, of prior participation in community-engaged projects than Whites. Similarly, African American and Asian American faculty had greater interest in learning about community-engaged research than Whites. Since translational research with a focus on community engagement is a key strategy for reducing racial and ethnic health disparities, our findings of increased interests by minority faculty are consistent with observations that minority researchers are more likely to study minority health issues. 11
Developing the necessary infrastructure to conduct high quality community-engaged research requires training approaches compatible with faculty preferences and offering incentives to address existing barriers.12 Although community-engaged research training opportunities are increasing, faculty interested in this research face persistent challenges. 6,12–15 Our survey found that over 90% of the UCLA CTSI faculty preferred traditional approaches to training, such as seminars, grand rounds, and self-directed online learning opportunities. Over half indicated a preference for more intensive approaches, such as participation in current community partnered research projects, meeting community partners, and formal mentorship/consultation. Our results suggest that CTSAs may need to offer a range of training options from low intensity, open to all faculty, to more intensive/formal training opportunities for selected faculty.
Prior reports have noted that an additional challenge, particularly for junior faculty, is that timelines for community-engaged research may not be aligned with tenure review timelines.13–16 For all faculty, including NIH funded researchers, the length of time required to develop community partnerships and collect primary data, often in non randomized controlled trial (RCT) designs, may not be compatible with timelines for achieving traditional academic benchmarks of “progress” and accepted products, specifically high impact, peer-reviewed RCT publications and grants.10,13,16–18 Consistent with prior work,10,13,16–18 our survey revealed that about three-quarters of faculty noted lack of time, about half noted lack of funding as barriers to conducting community-engaged research, while slightly more than one-fifth listed lack of capacity/skill and access to community partners as barriers. As in prior reports describing low to moderate levels of support in valuing community-engaged research in the faculty promotion process at CTSAs, a significantly greater percentage of pre-tenure (27.9%) than tenured faculty (19.2%) indicated lack of incentives was a barrier to learning about community-engaged research. Also, our findings revealed that over 60% of pre-tenure faculty indicated that faculty promotion criteria and over half noted career development grants would increase community-engaged research training participation.
There were several limitations to our report. A significant limitation was the relatively low overall response rates and high rates of missing responses to individual survey items. However, our survey response rates are consistent with other surveys of health professionals, CTSAs, and university-wide community engagement surveys. This limitation may be mitigated in part by our report’s sample being larger than similar studies. Because our survey was limited to one large, multi-institutional CTSA, our findings may not be generalizable to other CTSAs. Another potential limitation is that our report also included community-engaged projects in education and health services delivery in contrast to prior reports describing community engagement within existing NIH-funded research. However, our survey included this approach because CTSAs may consider leveraging existing community-academic partnerships to accelerate community-engaged research across the other traditional missions in university-based health sciences such as education and patient care. Although the UCLA CTSI faculty are more diverse than many other CTSAs,19 we still had relatively small numbers of Latino and African American respondents.
CONCLUSION
These limitations notwithstanding, our report adds to the literature examining the prevalence of community-engaged research within CTSAs and offer insights on how to build capacity in this area. Our findings suggest that levels of experience with and interest in community-engaged research within the UCLA CTSI vary by faculty characteristics, including race/ethnicity and rank. Further, faculty members who are interested in learning more about community engagement endorse multifaceted approaches to obtaining additional low and high intensity training opportunities in addition to endorsing increased funding to help investigators build or strengthen partnerships to conduct partnered research. To address barriers to promotion for junior faculty who are interested in or who are conducting this research, committees on academic promotions should develop and disseminate clear guidelines for advancement among investigators who emphasize community-engaged research.20 Additional qualitative work is needed to explore these issues in greater depth, perhaps with an option for anonymous responses to promote increased candor in participant responses. Finally, future work should follow-up on our report’s novel observation that female and minority faculty are more likely to participate in community-engaged research and training opportunities than male and White faculty in order to build CTSA capacity for translational, community-engaged research may require focusing resources on minority and female faculty development.
Table 3.
Logistic regression models for past participation in community-engaged (CE) projects, and interest in learning about CE best practices
| Participation in CE projects: N=862, AUC=0.608 | Interest in Learning: N=748, AUC=0.646 | |||
|---|---|---|---|---|
|
| ||||
| OR (95% CI) | P | OR (95% CI) | P | |
| Gender (Ref=Male) | ||||
| Female | 1.23 (0.93, 1.63) | 0.152 | 1.40 (1.02, 1.93) | 0.038 |
| Age (Ref≤40) | ||||
| 41–50 | 1.26 (0.84, 1.90) | 0.271 | 0.87 (0.55, 1.38) | 0.555 |
| 51–60 | 1.27 (0.78, 2.07) | 0.333 | 0.66 (0.38, 1.15) | 0.146 |
| 60+ | 1.30 (0.74, 2.28) | 0.363 | 0.57 (0.31, 1.06) | 0.077 |
| Unknown | 1.30 (0.71, 2.38) | 0.394 | 0.52 (0.21, 1.31) | 0.164 |
| Race/Ethnicity (Ref=White) | ||||
| Black/African American | 4.06 (1.68, 9.82) | 0.002 | 4.31 (1.42, 13.08) | 0.010 |
| Hispanic/Latino | 1.91 (1.10, 3.33) | 0.022 | 1.88 (0.97, 3.63) | 0.061 |
| Asian or Pacific Islander | 1.05 (0.76, 1.45) | 0.786 | 2.24 (1.52, 3.28) | <0.001 |
| Education (Ref=DDS or MD) | ||||
| HS Diploma, Bachelor’s Degree or Master’s Degree | 0.90 (0.32, 2.55) | 0.845 | 0.63 (0.21, 1.95) | 0.427 |
| DrPH or PhD | 1.38 (0.89, 2.16) | 0.153 | 1.66 (0.98, 2.81) | 0.061 |
| Discipline (Ref=Physician, Dentist, Psychologist, HSA or AHP) | ||||
| Basic or Social Scientist, Statistician | 0.54 (0.32, 0.91) | 0.020 | 0.61 (0.34, 1.11) | 0.107 |
| Faculty Rank (Ref=Pre-Tenure*) | ||||
| Tenure+ | 1.44 (1.00, 2.07) | 0.052 | 1.70 (1.11, 2.60) | 0.014 |
Pre-tenure: Clinical Instructor, Assistant Professor, Associate Professor;
Tenured: Associate Professor, Professor
Acknowledgments
NIH:
Article based in research wholly or partially by one or more of the bodies listed (None NIH, HHMI): NIH
Financial support for this manuscript were provided by the UCLA Clinical and Translational Science Institute through the NIH/National Center for Advancing Translational Science Grant Number UL1TR000124, the UCLA Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30-AG021684, Office of the Dean, David Geffen School of Medicine at UCLA.
Contributor Information
Bowen Chung, Center for Health Services & Society, Semel Institute for Neuroscience.
Keith Norris, UCLA, Medicine.
Carol Mangione, UCLA, Medicine.
Homero del Pino, Charles R. Drew University.
Loretta Jones, Healthy African American Families II.
Daniel Castro, Harbor-UCLA Medical Center/Los Angeles Biomedical Research Institute, Family Practice.
Christina Wang, Harbor-UCLA Medical Center/Los Angeles Biomedical Research Institute, Medicine.
Douglas Bell, UCLA, Medicine.
Sitaram Vangala, UCLA, Medicine.
Katherine Kahn, UCLA, Medicine.
Arleen Brown, University of California, GIM and HSR.
References
- 1.Committee to Review the Clinical and Translational Science Awards Program at the National Center for Advancing Translational Science, Institute of Medicine. The CTSA Program at NIH. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 2.Agency for Toxic Substances and Disease Registry. CTSA community engagement key function committee task force on the principals of community engagement. (2) 2011 Retrieved December 15, 2013, from http://www.atsdr.cdc.gov/communityengagement/pce_ctsa.html, 2013.
- 3.Israel BA, Eng E, Schulz AJ, et al. Introduction to methods in community-based participatory research for health. Methods in community-based participatory research for health. 2005:3–26. [Google Scholar]
- 4.Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. JAMA. 2007;297(4):407–410. doi: 10.1001/jama.297.4.407. [DOI] [PubMed] [Google Scholar]
- 5.Zerhouni EA. Transl Res. Moving Discovery to Practice. Clinical Pharmacology and Therapeutics. 2007 Jan;81(1):126–128. doi: 10.1038/sj.clpt.6100029. [DOI] [PubMed] [Google Scholar]
- 6.DiGirolamo A, Geller AC, Tendulkar SA, et al. Community-based participatory research skills and training needs in a sample of academic researchers from a clinical and translational science center in the Northeast. Clin Trans Sci Jun. 2012;5(3):301–305. doi: 10.1111/j.1752-8062.2012.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hood NE, Brewer T, Jackson R, Wewers ME. Survey of Community Engagement in NIH-funded Research. Clin Transl Sci Feb. 2010;3(1):19–22. doi: 10.1111/j.1752-8062.2010.00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.UCLA Clinical and Translational Science Institute. Retrieved March 2, 2015 https://www.ctsi.ucla.edu/about/pages/leadership.
- 9.UCLA Clinical and Translational Science Institute Community Engagement and Research Program. Retrieved on March 2, 2015 http://www.ctsi.ucla.edu/patients-community/pages/
- 10.A Working Group of the NCATS Advisory Council to the Director. NCATS Advisory Council Working Group Report on the IOM Report: The CTSA Program at NIH Draft Report. 2014 May 16; Retrieved on February 18, 2015 at http://www.ncats.nih.gov/files/CTSA-IOM-WG-Draft-Report.pdf.
- 11.Committee on Institutional and Policy-Level Strategies for Increasing the Diversity of the U.S. Health Care Workforce, Board on Health Sciences Policy, Institute of Medicine. In the Nation’s Compelling Interest: Ensuring Diversity in the Health-care Workforce. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 12.Holzer J, Kass N. Understanding the Supports of and Challenges to Community Engagement in the CTSAs. Clin Transl Sci. 2014 Sep 8; doi: 10.1111/cts.12205. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nokes KM, Nelson DA, McDonald MA, Hacker K, Gosse J, Sandford AA, Opel S. Faculty Perceptions of How Community-Engaged Research is Valued in Tenure, Promotion, and Retention Decisions. Clin Transl Sci. 2013 Aug;6(4):259–66. doi: 10.1111/cts.12077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carter-Edwards L, Cook JL, McDonald MA, Weaver SM, Chukwuka K, Eder MM. Clin Transl Sci. 2013 Feb 6;6(1):34–9. doi: 10.1111/cts.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The Clinical and Translational Science Award (CTSA) Consortium’s Community Engagement Key Function Committee, CTSA Community Engagement Workshop Planning Committee. Researchers and Their Communities: The Challenge of Meaningful Community Engagement. Bethesda, MD: National Center for Research Resources; 2009. [Google Scholar]
- 16.Marrero DG, Hardwick EJ, Staten LK, Savaiano DA, Odell JD, Comer KF, Saha C. Promotion and tenure for community-engaged research: an examination of promotion and tenure support for community-engaged research at three universities collaborating through a Clinical and Translational Science Award. Clin Transl Sci. 2013 Jun;6(3):204–8. doi: 10.1111/cts.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldberg-Freeman C, Kass N, Gielen A, et al. Faculty beliefs, perceptions, and level of community involvement in their research: a survey at one urban academic institution. J Empir Res Hum Res Ethics Dec. 2010;5(4):65–76. doi: 10.1525/jer.2010.5.4.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nyden P. Academic Incentives for faculty participation in community based participatory research. J Gen Intern Med. 2003 Jul;18(7):576–85. doi: 10.1046/j.1525-1497.2003.20350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Striving for Excellence, Faculty Diversity in Medical Education, American Association of Medical Colleges. Table 2: Count of Full-time Faculty by Medical School, Race/Hispanic Origin, and Sex for 2008. 2008 Retrieved on March 5, 2015 at https://members.aamc.org/eweb/DynamicPage.aspx?Action=Add&ObjectKeyFrom=1A83491A-9853-4C87-86A4-F7D95601C2E2&WebCode=PubDetailAdd&DoNotSave=yes&ParentObject=CentralizedOrderEntry&ParentDataObject=Invoice%20Detail&ivd_formkey=69202792-63d7-4ba2-bf4e-a0da41270555&ivd_prc_prd_key=DDFD9DA5-723A-4FCE-A980-55DD0EF845B2.
- 20.Community-Engaged Scholarship for Health Collaborative. Community-Engaged Scholarship Review, Promotion, and Tenure Package. Community-Campus Partnerships for Health; Retrieved on March 5, 2015 at http://depts.washington.edu/ccph/pdf_files/CES_RPT_Package.pdf. [Google Scholar]