Abstract
Background
Suicide is a leading cause of death for young people. Children living in sub-Saharan Africa, where HIV rates are disproportionately high, may be at increased risk.
Aims
To identify predictors, including HIV-status, of suicidal ideation and behavior in Rwandan children ages 10–17.
Method
Matched case-control study of 683 HIV-positive, HIV-affected (seronegative children with an HIV-positive caregiver), and unaffected children and their caregivers.
Results
Over 20% of HIV-positive and affected children engaged in suicidal behavior in the previous six months, compared to 13% of unaffected children. Children were at increased risk if they met criteria for depression, were at high-risk for conduct disorder, reported poor parenting, or had caregivers with mental health problems.
Conclusions
Policies and programs that address mental health concerns and support positive parenting may prevent suicidal ideation and behavior in children at increased risk related to HIV.
Declaration of interest
The authors have no conflicts to report.
Introduction
Across 90 countries, suicide has been found to be the third leading cause of death for females and the fourth leading cause for males ages 15–19 years old, accounting for more than 9% of the deaths of young people (1). Younger adolescents are also affected, with suicide being the 10th leading cause of death for adolescents 10–14 years old (2). A cross-national survey of adults estimated lifetime prevalence rates of suicidal ideation at 9.2% and suicide attempt at 2.7%, with the strongest risk factors comprising being female, less educated, and having a mental health disorder (3). While suicide risk has been understudied in sub-Saharan Africa (SSA), there is some evidence to suggest that rates of suicidal ideation and attempt might be higher among individuals living in SSA, with studies finding rates of suicidal behavior among school children ranging from 19.6% in Uganda to a high of 31.9% in Zambia (4). One study in South Africa found that more than one in five adolescents ages 13–19 reported having attempted suicide in the last six months (5). These observed elevated rates of suicidal ideation and behavior in youth in SSA may be due in part to disproportionately high rates of stressors with known associations to suicidality, such as HIV, which has been observed to increase psychosocial stress and hopelessness (6–8). Additionally, children affected by HIV have been found to be at increased risk for mental health problems due in part to parental loss and disrupted parent-child relationships, increased risk of family conflict, stigma and community rejection, economic insecurity, poor educational outcomes, caregiver depression, and physical impairment (9–15); some of these factors have been associated with increased suicide risk in youth in SSA (16).
Many countries in SSA, including Rwanda, have made significant progress in improving the health outcomes of individuals who are living with HIV (17–19). With increasing access to antiretroviral therapy (ART) (18, 19), HIV is rapidly becoming a chronic illness in many countries. However the broader consequences of HIV on individuals and within families, including possible increased risk for suicide, remain largely unaddressed. As global attention to children directly and indirectly affected by HIV/AIDS expands, greater understanding is needed on suicide risk among children living with HIV, children affected by HIV (children with an HIV-positive (HIV+) caregiver or a caregiver who died due to AIDS), and those unaffected by HIV, and the risk and protective factors that may influence this risk. This study is a secondary analysis of existing data from a case-control study conducted to compare mental health problems among children living with HIV, children affected by HIV, and children unaffected by HIV (15). The matched nature of the design allows us to examine suicidal ideation and behavior and how these experiences may be associated with HIV status. Furthermore, the study aims to understand how differences in demographics, mental health, parenting, harsh discipline, community social support and stigma predict suicidal ideation and behavior while accounting for the influence of HIV.
Method
Population and study design
This study was conducted by the Harvard School of Public Health, the Rwandan Ministry of Health, and Partners In Health/Inshuti Mu Buzima (PIH/IMB), a non-governmental organization supporting health system strengthening in Rwanda. The study was conducted within the catchment area of two district hospitals located in southern Kayonza and Kirehe Districts, which serve as referral hubs for 24 health centers that provide routine HIV services (18, 20). In the catchment area of these hospitals, an electronic medical record (EMR) system is maintained for patients receiving HIV care.
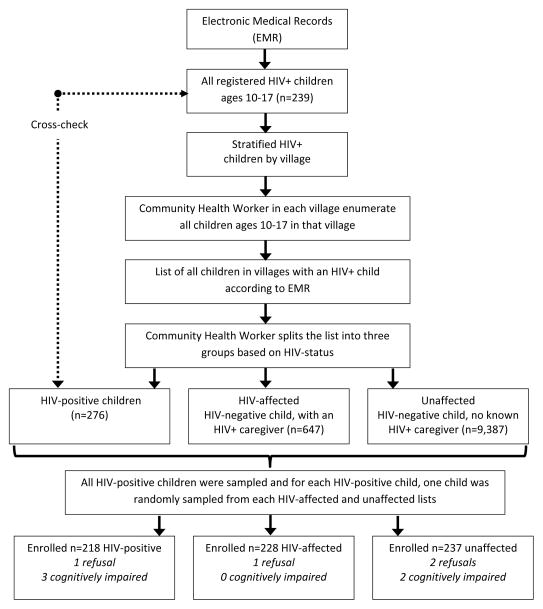
A case-control study design was used to enroll a sample of N=683 children stratified by HIV status from March to December 2012 (15). Sampling followed a multiple-step process (see Figure 1). First, the EMR identified children living with HIV aged 10–17 who were then stratified by village. For each village with an EMR-identified child living with HIV, a community health worker (CHW) compiled lists of all children aged 10–17. Rwandan CHWs track approximately 50 households per village making this procedure feasible. Second, specialized CHWs knowledgeable of all residents in their assigned villages who have were living with HIV stratified the lists by HIV status which revealed 37 additional children living with HIV who were added to the final HIV+ list. Children residing with a caregiver living with HIV or a caregiver who died due to AIDS made up the list of HIV-affected children. The remaining children confirmed by CHWs to be neither living with HIV or affected by HIV in their family made up the list of unaffected children. If the index child from the HIV+ list consented to participate, a random number generator was used to select HIV-affected and unaffected children in the same village. If the child or their caregivers did not provide assent/consent, a different participant was randomly sampled and invited to participate. This procedure allowed for a case-control design matched on village to control for geographic differences. Matching on age and gender was not necessary or logistically feasible given the relatively large sample size, which led to approximately equal distribution of demographic variables across groups.
Figure 1.
Sampling procedure
A target sample size of 250 subjects per group (n=750) was estimated to yield 82% power to detect standardized expected group mean differences equivalent to .25 SD at α =.05 (21). The number of eligible children living with HIV fell just short of this target, with 683 children and one of their caregivers participating in the study (participation rate over 95%). Children living with HIV were ineligible if they moved outside the study area, had since tested HIV-negative, were under 10 years of age, or lived in a child-headed household. Eligible children were aged 10–17 years and had lived in Kayonza or Kirehe Districts for at least one month. For each child, a cohabiting adult caregiver (selected as “knowing the child best”) reported on their mental health, the child’s mental health, family and community relationships, and family socio-economic status (SES). Exclusion criteria were active psychosis or severe cognitive impairment in the invited child (as identified by study psychologists). Although no exclusions were made due to cognitive impairment, five of the younger children were not able to fully complete the self-report due to poor comprehension of the items; for two of these children, caregivers completed caregiver reports. During data collection, local psychologists traveled with the research team to respond to serious risk of harm situations (e.g., suicidality) and make referrals to the health system and local service programs as appropriate. Overall, 5% of the sample received additional referral to mental health services due to such immediate risk of harm issues.
This study received approval from the Harvard School of Public Health Office of Human Research Administration and the Rwanda National Ethics Committee. Independent parental/guardian informed consent and child assent was obtained for all study participants.
Procedures
Rwandan research assistants orally conducted all assessments in Kinyarwanda, the local language, with oversight from the study field coordinators and investigators. Children and caregivers were assessed for mental health problems as well as protective and risk factors. Research assistants received two-weeks of training in research ethics, data collection methods, and interviewing children and parents. Interviews were carried out in participants’ homes, with child and caregiver interviews conducted separately. All data were collected on Android smart phones using DataDyne’s EpiSurveyor. De-identified data was uploaded to DataDyne’s secure website where it was accessed for analysis.
Measures
All measures were subjected to rigorous translation procedures, and measures of suicidal ideation and behavior, child mental health, good parenting, and social support were locally validated with 378 child-caregiver dyads (22–24).
Demographics
Children reported their sex, age, whether they were currently attending school and had experienced the death of a caregiver. Caregivers reported on whether they were a single caregiver (typically a female headed household), and family SES, which was measured using the wealth index (25) from the Rwanda Demographic and Health Survey (26).
Child mental health
Children and their caregivers reported on child depression and conduct problems. The 20-item Center for Epidemiologic Studies Depression Scale for Children (CES-DC) (27) assessed symptoms of depression and was scored 0 (never) to 3 (often), and the scale score was the sum. The CES-DC was validated in this population using a process described previously, which identified a cut-off score of 30 as being optimally able to identify children with a clinical depression diagnosis (23), and so children with scores greater than or equal to 30 were classified as likely having depression. The scale demonstrated good internal consistency (α = .88). Conduct Problems were measured using the short form of the Youth Conduct Problems Scale-Rwanda (YCPS-R), a locally-derived scale based on qualitative data (24), as standardized measures of conduct disorder did not match well with the local construct (28). The scale contains 11 items scored 0 (never) to 3 (often) and was scored as the sum. The internal reliability in this sample was excellent (α=.89). A validity study of the YCPS-R identified scores of five for the child report, nine for the caregiver report on females, and 14 for the caregiver report on males as being the cut-off scores best able to identify children diagnosed with conduct disorder (24); these were used as cut-off scores for conduct problems. While the YCPS-R questions used in the validity study were the same as those used in this study, the time frame during the validity study was one week, while the one used in this study was six months, and so in this study, the YCPS-R cut-offs should be viewed as identifying children at higher risk of conduct disorder, rather than children scoring above the diagnostic threshold.
Parenting
Children and caregivers reported on the good parenting and severe physical punishment the children received, and caregivers reported on caregiver mental health. Good parenting, a protective factor derived from previous qualitative research (29), was assessed by 16 locally-derived items and 16 items from the Parental Acceptance and Rejection Questionnaire (30). Parenting was scored on four-point Likert scale 0 (never) to 3 (every day) and the scale score was the mean. The local parenting scale performed well in validity testing (α=.94, test-retest r=.87) and the combined scale had excellent internal reliability in this sample (α=.93). Severe physical punishment was measured using the severe physical punishment subscale of UNICEF’s Multiple Indicator Cluster Survey’s Child Discipline module (31) which includes two items (“You were slapped in the face, in the head, or in the ears,” and “You were severely beaten”) scored 0=No, 1=Yes, and the scale was scored as a binary variable of whether or not the child reported either form of punishment in the past month. Caregiver mental health was assessed using the Hopkins Symptom Checklist (HSCL-25) (32), a 25-item measure of depression and anxiety previously tested and validated for use in Rwanda (α = .94 in this sample) (33).
Community support and HIV-related stigma
Children and caregivers reported on the community support and HIV-related stigma received and experienced by the child. Community support was measured using an adapted Inventory of Socially Supportive Behaviors (ISSB) (34). The ISSB assesses how often an individual receives informational, instrumental, and emotional support on a five-point Likert scale (0–4) ranging from “never” to “nearly all the time.” The adapted Rwandan scale contains 33 items (23 from the original ISSB and 10 drawn from qualitative data). The scale demonstrated good internal consistency (α = .95). HIV-related stigma was measured by 13 items adapted from the Young Carer’s Project (35). Frequency of experiencing interpersonal interactions indicative of stigma was reported on a three-point Likert scale (0–2) of “never,” “sometimes,” or “often/a lot.” When a stigma item was endorsed, children were then asked to report why they thought it happened. If children endorsed HIV as the reason for experiencing any of the stigma items, then they received a score of one, all other children received a score of zero.
Suicidal ideation and behavior
Children and caregivers responded to two items from the Youth Self-Report (YSR) Internalizing Subscale (36) to assess child suicidal ideation and behavior during the previous six months. Suicidal ideation was assessed by “You thought about killing yourself,” and suicidal behavior was assessed by “You deliberately tried to hurt or kill yourself.” If either the child or caregiver endorsed these items, children were deemed to have had suicidal ideation or behavior. While only two items from the YSR were used in this analysis, the complete YSR Internalizing Subscale had 16 items and it demonstrated strong internal reliability (α = .89) in this sample.
Analyses
Summary statistics were computed for each outcome and predictor variable. Univariate logistic regressions were run to assess the relationship between each predictor variable (including HIV-status) and suicidal ideation and behavior in the past six months. Multicollinearity between predictor variables was assessed by examination of the correlation matrix and by computing the variance inflation factors (VIF) using the Stata version 12 command COLLIN (37). If predictor variables were not multicollinear, they were included in multiple logistic regressions predicting suicidal ideation and behavior. All analyses were conducted using Stata version 12 (38).
Results
Demographics
The final sample contained a total of N=683 children, 218 of whom were living with HIV, 228 HIV-affected, and 237 unaffected by HIV in their family. The mean age of the children was 13.60 (SD=2.19), and 51.54% were females. Half of the children (52.05%) were being raised by a single caregiver, almost one-third (28.97%) had experienced the death of a caregiver, but 90.40% were currently attending school. Mental health problems were common in the sample, with 25.70% of children scoring above the diagnostic threshold for depression, and 30.10% of children scoring in the high-risk range for conduct problems. See Table 1 for summary statistics of all study variables.
Table 1.
Univariate logistic regressions predicting suicidal ideation and behavior in past six months
| Suicidal Ideation | Suicidal Behavior | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Total n=683 |
Yes n=141 20.64% |
No n=542 79.36% |
Unadj. OR (95% CI) | Yes n=125 18.30% |
No n=558 81.70% |
Unadj. OR (95% CI) | |
| HIV-Status, No. (%)a | |||||||
| HIV-unaffected | 237 (34.70) | 44 (18.57) | 193 (81.43) | reference | 30 (12.66) | 207 (87.34) | reference |
| HIV-affected | 228 (33.38) | 51 (22.37) | 177 (77.63) | 1.26 (.80–1.99) | 49 (21.49) | 179 (78.51) | 1.89* (1.15–3.10) |
| HIV+ | 218 (31.92) | 46 (21.10) | 172 (78.90) | 1.17 (.74–1.86) | 46 (21.10) | 172 (78.90) | 1.85* (1.12–3.05) |
| Demographics, No. (%) | |||||||
| Femalec | 351 (51.54) | 75 (21.37) | 276 (78.63) | 1.09 (.75–1.58) | 69 (19.66) | 282 (80.34) | 1.20 (.81–1.77) |
| Age,c mean (SD) | 13.60 (2.19) | 14.12 (2.08) | 13.47 (2.20) | 1.15** (1.05–1.25) | 14.25 (2.19) | 13.46 (2.20) | 1.18*** (1.08–1.29) |
| Death of Caregiverf | 195 (28.97) | 44 (22.56) | 151 (77.44) | 1.17 (.78–1.76) | 42 (21.54) | 153 (78.46) | 1.41 (.93–2.14) |
| Single Caregiverb | 355 (52.05) | 87 (24.51) | 268 (75.49) | 1.64** (1.12–2.40) | 81 (22.82) | 274 (77.18) | 1.90** (1.27–2.84) |
| Not in Schoole | 65 (9.60) | 22 (33.85) | 43 (66.15) | 2.19** (1.26–3.80) | 19 (29.23) | 46 (70.77) | 2.04* (1.15–3.63) |
| SES,c mean (SD) | <.001 (1.00) | −.06 (1.05) | .02 (.99) | .92 (.76–1.12) | −.16 (.92) | .04 (1.02) | .81* (65–1.00) |
| Child Mental Health, No. (%) | |||||||
| Depression-Chc | 175 (25.70) | 78 (44.57) | 97 (55.43) | 5.65*** (3.80–8.42) | 60 (34.29) | 115 (65.71) | 3.54*** (2.36–5.32) |
| Depression-Cgd | 164 (24.15) | 60 (36.59) | 104 (63.41) | 3.14*** (2.11–4.67) | 55 (33.54) | 109 (66.46) | 3.26*** (2.16–4.92) |
| Conduct Problems-Chc | 205 (30.10) | 80 (39.02) | 125 (60.98) | 4.35*** (2.95–6.42) | 66 (32.30) | 139 (67.80) | 3.36*** (2.25–5.01) |
| Conduct Problems-Cga | 123 (18.06) | 47 (38.21) | 76 (61.79) | 3.05*** (1.99–4.67) | 49 (39.84) | 74 (60.16) | 4.20*** (2.72–6.49) |
| Parenting, mean (SD) | |||||||
| Caregiver Mental Healtha | 1.09 (.63) | 1.34 (.66) | 1.02 (.61) | 2.21*** (1.64–2.99) | 1.23 (.64) | 1.06 (.62) | 1.53** (1.13–2.08) |
| Good Parenting-Chc | 2.38 (.55) | 2.07 (.63) | 2.46 (.49) | .30*** (.22–.42) | 2.01 (.66) | 2.47 (.48) | .26*** (.18–.37) |
| Good Parenting-Cgb | 2.58 (.33) | 2.46 (.33) | 2.60 (.30) | .31*** (.18–.52) | 2.45 (.39) | 2.60 (.31) | .30*** (.18–.51) |
| SPP-Ch,a No, (%) | 161 (23.57) | 41 (25.47) | 120 (74.53) | 2.42*** (1.62–3.61) | 41 (25.47) | 120 (74.53) | 1.78** (1.17–2.72) |
| SPP-Ca,a No, (%) | 68 (9.96) | 24 (35.39) | 44 (64.71) | 2.32** (1.36–3.97) | 18 (26.47) | 50 (73.53) | 1.71 (.96–3.05) |
| Community Support, mean (SD) and HIV-Related Stigma, No. (%) | |||||||
| Community Support-Chc | 1.90 (.76) | 1.64 (.73) | 1.97 (.75) | .56*** (.43–.72) | 1.59 (.79) | 1.97 (.74) | .51*** (.39–.67) |
| Community Support-Cga | 1.56 (.69) | 1.46 (.70) | 1.58 (.69) | .76* (.58–1.00) | 1.42 (.76) | 1.59 (.67) | .69* (.52–.93) |
| Stigma-Cha | 110 (16.11) | 35 (31.82) | 75 (68.18) | 2.06** (1.31–3.23) | 28 (25.45) | 82 (74.55) | 1.68* (1.04–2.71) |
| Stigma-Cga | 188 (27.53) | 42 (22.34) | 146 (77.66) | 1.15 (.77–1.73) | 41 (21.81) | 147 (78.19) | 1.36 (.90–2.07) |
Ch=Child reported; Cg=Caregiver reported; SPP=Severe Physical Punishment
n = a683, b682, c681, d679, e677, f673
p<.05,
p<.01,
p<.001
Suicidal Ideation and behavior and HIV-status
Of the 683 children, 141 (20.64%) had reported suicidal ideation and 125 (18.30%) had reportedly engaged in intentional self-harm or attempted suicide during the previous six months. As hypothesized, children who were living with HIV (OR=1.85, 95% CI=1.12–3.05) or HIV-affected (OR=1.90, 95% CI=1.16–3.12) were at greater risk of suicidal behavior compared to children who were not affected by HIV, with 21.10% of those living with HIV and 21.49% of HIV-affected children endorsing suicidal behavior compared to 12.66% of children not affected by HIV. HIV-status was not significantly predictive of suicidal ideation.
Predictors of suicidal ideation and behavior: Unadjusted logistic regression results
Results of the univariate logistic regressions indicated that older children, those with a single caregiver, and those not in school were at increased risk for suicidal ideation and behavior, while those living in families with higher SES were at decreased risk for suicidal behavior (see Table 1 for all logistic regression results). Neither sex nor having a caregiver die predicted suicidal ideation or behavior. Child depression and conduct problems both substantially increased the risk of suicidal ideation and behavior.
Children with self-reported depression scores above diagnostic cut-off were 5.65 times more likely to have suicidal ideation and 3.54 times more likely to have suicidal behavior than those below clinical cut-off. Children whose caregivers reported that their depression scores were above the diagnostic cut-off were more than 3 times more likely to have suicidal ideation and behavior. Children at high risk for conduct problems were also much more likely to have suicidal ideation and behavior, with increased odds of 3.05 and 4.35 respectively (p<.001).
Good parenting was associated with decreased risk of ideation (OR=.30, p<.001) and behavior (OR=.26, p<.001), while children who reported experiencing severe physical punishment had more then double the risk of suicidal ideation (OR=2.42, p<.001) and almost double the risk of suicidal behavior (OR=1.78, p=.008). Children whose caregivers reported more mental health problems themselves were also at increased risk for suicidal ideation (OR=2.21, p<.001) and behavior (OR=1.53, p=.006). Finally, community support predicted less suicidal ideation (OR=.56, p<.001) and behavior (OR=.51, p<.001) while child-reported HIV-related stigma was associated with significantly increased risk of ideation (OR=2.06, p=.002) and behavior (OR=1.68, p=.04).
Predictors of suicidal ideation and behavior: Multiple logistic regression results
Results of the mulicollinearity analysis found no evidence of collinearity between predictors, as the highest correlation was r=−.48 between the dummy codes for those living with HIV and HIV-affected, and the mean VIF was 1.31, with the highest VIF being 2.07. Results of the multiple regressions are presented in Table 2. Results indicated that child mental health symptoms significantly increased the odds of suicidal ideation and behavior, while child report of good parenting decreased the odds. Caregiver mental health symptoms increased the odds of child suicidal ideation, but not behavior. After accounting for these factors, none of the other predictors were significantly associated with suicidal ideation or behavior.
Table 2.
Multiple logistic regressions predicting suicidal ideation and behavior in past six months
| Suicidal Ideation | Suicidal Behavior | |||||
|---|---|---|---|---|---|---|
| Adj. OR | 95% CI | p | Adj. OR | 95% CI | p | |
| HIV-Status | ||||||
| HIV-affected | .86 | .49–1.53 | .62 | 1.62 | .88–2.98 | .12 |
| HIV+ | 1.04 | .52–2.08 | .91 | 1.80 | .87–3.69 | .11 |
| Demographics | ||||||
| Female | 1.00 | .63–1.57 | .99 | 1.28 | .80–2.05 | .30 |
| Age | 1.05 | .94–1.17 | .41 | 1.11 | .99–1.25 | .08 |
| Death of Caregiver | 1.01 | .59–1.73 | .97 | 1.05 | .61–1.81 | .86 |
| Single caregiver | 1.03 | .64–1.68 | .90 | 1.14 | .69–1.87 | .61 |
| Not in School | 1.22 | .57–2.63 | .61 | .92 | .43–1.98 | .83 |
| SES | 1.26 | 1.00–1.59 | .06 | 1.09 | .84–1.40 | .52 |
| Child Mental Health | ||||||
| Depression-Ch | 3.16 | 1.97–5.09 | <.001 | 1.78 | 1.07–2.97 | .03 |
| Depression-Cg | 1.93 | 1.15–3.23 | .01 | 2.02 | 1.19–3.44 | .009 |
| Conduct Problems-Ch | 2.45 | 1.52–3.95 | <.001 | 1.75 | 1.06–2.89 | .03 |
| Conduct Problems-Cg | 1.18 | .67–2.09 | .57 | 2.38 | 1.36–4.19 | .003 |
| Parenting | ||||||
| Caregiver Mental Health | 1.54 | 1.03–2.29 | .03 | .90 | .60–1.37 | .64 |
| Good Parenting-Ch | .60 | .38–.95 | .03 | .44 | .27–.71 | .001 |
| Good Parenting-Cg | .65 | .32–1.31 | .22 | .70 | .34–1.41 | .32 |
| Severe Physical Punishment-Ch | 1.26 | .75–2.12 | .37 | 1.01 | .58–1.77 | .97 |
| Severe Physical Punishment-Cg | 1.31 | .65–2.64 | .45 | .86 | .40–1.83 | .69 |
| Community Support & HIV-Related Stigma | ||||||
| Community Support-Ch | .86 | .60–1.22 | .40 | .85 | .59–1.23 | .39 |
| Community Support-Cg | .79 | .56–1.13 | .20 | .75 | .52–1.09 | .13 |
| HIV-Related Stigma-Ch | 1.11 | .58–2.13 | .76 | .70 | .36–1.38 | .31 |
| HIV-Related Stigma-Cg | .81 | .03–8.07 | .65 | 1.01 | .58–1.77 | .97 |
Ch=Child reported; Cg=Caregiver reported
Child mental health
Results of the multiple logistic regression found that children who self-reported and whose caregivers reported depression symptoms above the diagnostic threshold were two to three times more likely to have suicidal ideation and two times more likely to have suicidal behavior than those with depression symptoms below the diagnostic threshold. Moreover, children who were at high-risk for conduct problems were 2.5 times more likely to have suicidal ideation and 1.75 times more likely to have suicidal behavior. Children whose caregivers reported that they were high risk for conduct problems were more than twice as likely to have suicidal behavior, but were no more likely to have suicidal ideation compared to those at low risk for conduct problems.
Parenting
Child report of good parenting was associated with decreased risk of suicidal ideation (OR=.60, p=.03) and behavior (OR=.44, p=.001), however caregiver report of good parenting was not associated with any differences in suicide risk. Caregiver mental health problems increased the risk of suicidal ideation (OR=1.54, p=.03), but was not associated with risk for suicidal behavior.
Discussion
Throughout the world suicidal ideation and behavior, particularly by children, is often hidden, unrecognized, and misunderstood. However, suicidal behavior in children demands attention, as the results of this study found alarmingly high rates of suicidal ideation and behavior in this sample in SSA, particularly among youth who are living with HIV and who have a caregiver living with HIV – more than one in five of these children reported a previous suicide or self-harm attempt in the last six months. Children who are living with HIV or who are affected by HIV may be at higher risk of suicide due to higher rates of mental health concerns, poorer parenting, and caregivers with their own mental health concerns. These risk factors seem to put children at higher risk regardless of HIV-status and may also make it much harder for these children to access care and support.
Attention to mental health globally is sparse, particularly in much of SSA and other low- and middle-income country settings where mental health services and human resources for mental health care are extremely limited and risk factors, such as poverty, are high. Child and caregiver mental health and parenting factors remained the strongest predictors of suicidal ideation and behavior even after accounting for other risk factors such as SES, death of caregivers, and social support and HIV-related stigma. The results of this study demonstrate the importance of tackling child and adult mental health concerns and supporting positive parenting skills with families in low- and middle-income countries (LMICs), in addition to addressing poverty and social support.
Study limitations must be acknowledged, including no ability to conduct clinical testing at the time of data collection in order to confirm HIV-status biomarkers for children and their caregivers. However, the CHWs in Rwanda provide directly observed therapy to all patients living with HIV in the PIH/IMB supported districts, and so we are confident in the correct categorization of children by HIV-status. Additionally, reports of suicidal ideation and behavior, child mental health, and risk and protective factors such as good parenting, social support, HIV-related stigma and harsh punishment were collected through retrospective self-reports, and may be subject to recall and reporting bias. However, we believe a strength of the study is that this information was reported by both the child and one of their caregivers, which may help to offset some of the self-reporting concerns. Additionally, many of the measures including those for mental health, good parenting, and social support were previously validated in Rwanda, increasing the likelihood of valid and reliable results.
Effective suicide prevention is a societal challenge that would benefit from coordinated responses by family, educational, and community partners, in addition to health service providers and systems. Suicide prevention public health campaigns that seek to broaden awareness of, and sensitivity to, mental health needs and suicide risk factors and behavior is needed at the individual, family, and community levels, as many people may be unaware of the risk of suicidal ideation in children and ways to prevent and address it. Moreover, national health systems may need to provide training and assistance to local community providers, such as CHWs, to develop and maintain case identification, referral, and service delivery programs for children and adults with mental health concerns that can be sustained in low-resource settings (39). In addition, prevention interventions such as the Family Strengthening Intervention (40) which seeks to improve parenting skills and prevent child mental health problems in families affected by HIV in Rwanda may help address some of these needs.
Acknowledgments
This work was made possible by the collaboration and dedication of the Rwandan Ministry of Health and Partners In Health/Inshuti Mu Buzima. We are endlessly grateful to the local research team who carried out these interviews and to the study participants and their families who shared their experiences with us. No authors have any financial interest or conflicts of interest to report. Dr. Lauren Ng wrote the manuscript and conducted the data analyses. Catherine Kirk contributed significantly to writing and data interpretation. Fredrick Kanyanganzi, Justin Bizimana, Evelyne Shema, and Dr. Vincent Sezibera contributed to study implementation and provided significant intellectual contributions. Drs. Felix Cyamatare and Mary Smith Fawzi contributed significantly to study design and implementation and provided input and feedback on the manuscript. All authors revised the article for intellectual content and approved the final version. Dr. Theresa Betancourt had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was primarily funded by the Harvard University Center for AIDS Research (CFAR) Grant# P30 AI060354, which supported design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Additional funding was from Grant#1K01MH07724601 A2 from the National Institute of Mental Health, the Peter C. Alderman Foundation, the Harvard Center for the Developing Child, the François-Xavier Bagnoud Center for Health and Human Rights, the Harvard School of Public Health Career Incubator Fund, and the Julie Henry Family Development Fund.
References
- 1.Wasserman D, Cheng Q, Jiang G-X. Global suicide rates among young people aged 15–19. World Psychiatry. 2005;4(2):114. [PMC free article] [PubMed] [Google Scholar]
- 2.Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009;374(9693):881–92. doi: 10.1016/S0140-6736(09)60741-8. [DOI] [PubMed] [Google Scholar]
- 3.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swahn M, Bossarte R, Elimam DM, Gaylor E, Jayaraman S. Prevalence and correlates of suicidal ideation and physical fighting: a comparison between students in Botswana, Kenya, Uganda, Zambia and the USA. Int Public Health J. 2010;2(2):195–206. [Google Scholar]
- 5.Shilubane HN, Ruiter RA, van den Borne B, Sewpaul R, James S, Reddy PS. Suicide and related health risk behaviours among school learners in South Africa: results from the 2002 and 2008 national youth risk behaviour surveys. BMC Public Health. 2013;13(1):926. doi: 10.1186/1471-2458-13-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooperman NA, Simoni JM. Suicidal ideation and attempted suicide among women living with HIV/AIDS. J Behav Med. 2005;28(2):149–56. doi: 10.1007/s10865-005-3664-3. [DOI] [PubMed] [Google Scholar]
- 7.Komiti A, Judd F, Grech P, Mijch A, Hoy J, Lloyd JH, et al. Suicidal behaviour in people with HIV/AIDS: a review. Aust N Z J Psychiatry. 2001;35(6):747–57. doi: 10.1046/j.1440-1614.2001.00943.x. [DOI] [PubMed] [Google Scholar]
- 8.Gielen AC, McDonnell KA, O’Campo PJ, Burke JG. Suicide risk and mental health indicators: Do they differ by abuse and HIV status? Womens Health Issues. 2005;15(2):89–95. doi: 10.1016/j.whi.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Doku P. Parental HIV/AIDS status and death, and children’s psychological wellbeing. Inte J Ment Health Syst. 2009;3(1):26. doi: 10.1186/1752-4458-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy DA, Greenwell L, Mouttapa M, Brecht ML, Schuster MA. Physical health of mothers with HIV/AIDS and the mental health of their children. J Dev Behav Pediatr. 2006;27(5):386–95. doi: 10.1097/00004703-200610000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lester P, Jane Rotheram-Borus M, Lee S-J, Comulada S, Cantwell S, Wu N, et al. Rates and predictors of anxiety and depressive disorders in adolescents of parents with HIV. Vuln Child Youth Stud. 2006;1(1):81–101. [Google Scholar]
- 12.Smith Fawzi MC, Eustache E, Oswald C, Surkan P, Louis E, Scanlan F, et al. Psychosocial functioning among HIV-affected youth and their caregivers in Haiti: implications for family-focused service provision in high HIV burden settings. AIDS Patient Care STDS. 2010;24(3):147–58. doi: 10.1089/apc.2009.0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cluver LD, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. J Child Psychol Psychiatry. 2012;53(4):363–70. doi: 10.1111/j.1469-7610.2011.02459.x. [DOI] [PubMed] [Google Scholar]
- 14.Gadow KD, Angelidou K, Chernoff M, Williams PL, Heston J, Hodge J, et al. Longitudinal study of emerging mental health concerns in youth perinatally infected with HIV and peer comparisons. J Dev Behav Pediatr. 2012;33(6):456. doi: 10.1097/DBP.0b013e31825b8482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Betancourt T, Scorza P, Kanyanganzi F, Fawzi MCS, Sezibera V, Cyamatare F, et al. HIV and child mental health: a case-control study in Rwanda. Pediatrics. 2014;134(2):e464–e72. doi: 10.1542/peds.2013-2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swahn MH, Palmier JB, Kasirye R, Yao H. Correlates of suicide ideation and attempt among youth living in the slums of Kampala. Int J Environ Res Public Health. 2012;9(2):596–609. doi: 10.3390/ijerph9020596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farmer P, Nutt C, Wagner CM, Sekabaraga C, Nuthulanganti T, Weigel JL, et al. Reduced premature mortality in Rwanda: lessons from success. BMJ. 2013:346. doi: 10.1136/bmj.f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rich ML, Miller AC, Niyigena P, Franke MF, Niyonzima JB, Socci A, et al. Excellent Clinical Outcomes and High Retention in Care Among Adults in a Community-Based HIV Treatment Program in Rural Rwanda. J Acquir Immune Defic Syndr. 2012;59:e35–e42. doi: 10.1097/QAI.0b013e31824476c4. [DOI] [PubMed] [Google Scholar]
- 19.UNAIDS. Country Progress Report: Rwanda. 2012. [Google Scholar]
- 20.Merkel E, Gupta N, Nyirimana A, Niyonsenga SP, Nahimana E, Stulac SN, et al. Clinical Outcomes Among HIV-Positive Adolescents Attending an Integrated and Comprehensive Adolescent-Focused HIV Care Program in Rural Rwanda. J HIV/AIDS Soc Serv. 2013;12(3–4):437–50. [Google Scholar]
- 21.Forsyth BW, Damour L, Nagler S, Adnopoz J. The psychological effects of parental human immunodeficiency virus infection on uninfected children. Arch Pediatr Adolesc Med. 1996;150(10):1015–20. doi: 10.1001/archpedi.1996.02170350017002. [DOI] [PubMed] [Google Scholar]
- 22.Scorza P, Stevenson A, Canino G, Mushashi C, Kanyanganzi F, Munyanah M, et al. Validation of the “World Health Organization Disability Assessment Schedule for Children, WHODAS-Child” in Rwanda. PLoS One. 2013;8(3):e57725. doi: 10.1371/journal.pone.0057725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betancourt T, Scorza P, Meyers-Ohki S, Mushashi C, Kayiteshonga Y, Binagwaho A, et al. Validating the center for epidemiological studies depression scale for children in Rwanda. J Am Acad Child Adolesc Psychiatry. 2012;51(12):1284–92. doi: 10.1016/j.jaac.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ng LC, Kanyanganzi F, Munyanah M, Mushashi C, Betancourt TS. Developing and Validating the Youth Conduct Problems Scale-Rwanda: A Mixed Methods Approach. PLoS One. 2014;9(6):e100549. doi: 10.1371/journal.pone.0100549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rutstein SO, Johnson K. ORC Macro. 2004. The DHS Wealth Index. [Google Scholar]
- 26.Ministry of Health, ICF International. Rwanda Demographic and Health Survey. Ministry of Health; 2012. [Google Scholar]
- 27.Radloff LS. The Use of the Center for Epidemiological Studies Depression Scale in Adolescents and Young Adults. J Youth Adolesc. 1991;20(2):149–66. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 28.Betancourt TS, Rubin-Smith JE, Beardslee WR, Stulac SN, Fayida I, Safren S. Understanding locally, culturally, and contextually relevant mental health problems among Rwandan children and adolescents affected by HIV/AIDS. AIDS Care. 2011;23(4):401–12. doi: 10.1080/09540121.2010.516333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Betancourt TS, Meyers-Ohki SE, Stulac SN, Barrera AE, Mushashi C, Beardslee WR. Nothing can defeat combined hands (Abashize hamwe ntakibananira): Protective processes and resilience in Rwandan children and families affected by HIV/AIDS. Soc Sci Med. 2011 doi: 10.1016/j.socscimed.2011.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rohner RP, Saavedra JM, Granum EO. Development and validation of the parental acceptance and rejection questionnaire: Test manual. JSAS Catalog of Selected Documents in Psychology (Manuscript 1635) 1978;8(7–8) [Google Scholar]
- 31.UNICEF. Child Disciplinary Practices at Home: Evidence from a Range of Low- and Middle-Income Countries. 2010. [Google Scholar]
- 32.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 33.Bolton P. Cross-cultural validity and reliability testing of a standard psychiatric assessment instrument without a gold standard. J Nerv Ment Dis. 2001;189(4):238–42. doi: 10.1097/00005053-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Barerra M, Sandler IN, Ramsay TB. Inventory of Socially Supportive Behaviors (ISSB) 1983. [Google Scholar]
- 35.Boyes ME, Mason SJ, Cluver LD. Validation of a brief stigma-by-association scale for use with HIV/AIDS-affected youth in South Africa. AIDS Care. 2013;25(2):215–22. doi: 10.1080/09540121.2012.699668. [DOI] [PubMed] [Google Scholar]
- 36.Achenbach TM. Manual for the Youth Self-Report and 1991 profile. University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 37.Ender P. SCa Consulting, editor. Collinearity Diagnostics. UCLA Office of Academic Computing; 2010. [Google Scholar]
- 38.StataCorp. Stata Statistical Software: Release 12. StataCorp LP; 2011. [Google Scholar]
- 39.Betancourt TS, Beardslee WR, Kirk CM, Hann K, Zombo M, Mushashi C, et al. Working with vulnerable populations: Examples from trials with children and families in adversity due to war and HIV/AIDS. In: Thornicroft G, Patel V, editors. Global Mental Health Trials. Oxford University Press; 2014. [Google Scholar]
- 40.Betancourt TS, Ng L, Kirk CM, Munyanah M, Mushashi C, Ingabire C, et al. Family-based prevention of mental health problems in children affected by HIV and AIDS: an open trial. AIDS. 2014;28(Suppl 3):S359–S68. doi: 10.1097/QAD.0000000000000336. [DOI] [PMC free article] [PubMed] [Google Scholar]