Abstract
Background
A large body of evidence demonstrates dose-response relationships of cumulative coal mine dust exposure with lung function impairment and with small opacity profusion. However, medical literature generally holds that simple coal workers’ pneumoconiosis (CWP) is not associated with lung function impairment. This study examines the relationship between small opacity profusion and lung function in U.S. underground coal miners with simple CWP.
Methods
Miners were examined during 2005–2013 as part of the Enhanced Coal Workers’ Health Surveillance Program. Work histories were obtained, and chest radiographs and spirometry were administered. For those with multiple Program encounters, the most recent visit was used. Lung parenchymal abnormalities consistent with CWP were classified according to International Labour Organization guidelines, and reference values for FEV1 and FVC were calculated using reference equations derived from the 3rd National Health and Nutrition Examination Survey. Differences in lung function were evaluated by opacity profusion, and regression models were fit to characterize associations between profusion and lung function.
Results
A total of 8,230 miners were eligible for analysis; 269 had category 1 or 2 simple CWP. Decrements in FEV1 percent predicted were nearly consistent across profusion subcategories. Clear decrements in FVC percent predicted and FEV1/FVC were also observed, although these were less consistent. Controlling for smoking status, BMI, and mining tenure, each one-unit subcategory increase in profusion was associated with decreases of 1.5% (95% CI 1.0% to 1.9%), 1.0% (95% CI 0.6% to 1.3%), and 0.6% (95% CI 0.4% to 0.8%) in FEV1 percent predicted, FVC percent predicted, and FEV1/FVC, respectively.
Conclusions
We observed progressively lower lung function across the range of small opacity profusion. These findings address a longstanding question in occupational medicine, and point to the importance of medical surveillance and respiratory disease prevention in this workforce.
Introduction
In 1969, the U.S. Congress passed the Federal Coal Mine Health and Safety Act (Coal Act) “to prevent death and serious physical harm, and in order to prevent occupational disease” caused by work in the Nation’s coal mines.1 Since 1972, the permissible exposure limit (PEL) for respirable coal mine dust has been 2 mg/m3. This enforceable standard was adopted to protect underground coal miners from disability and premature mortality that accompanies severe coal workers’ pneumoconiosis (CWP).2,3 In the decades following enactment of the PEL there was a clear and substantial decline in the prevalence of CWP among active miners as reported by the National Institute for Occupational Safety and Health (NIOSH) Coal Workers’ Health Surveillance Program (CWHSP), but a resurgence of the disease has been observed, most notably in the central Appalachian region.4–8
During Congressional hearings before passage of the Coal Act, scientists and lawmakers acknowledged that implementation of the 2 mg/m3 PEL, which had been derived from British research, would not completely prevent the occurrence of new cases of CWP;9 simple CWP [International Labour Organization (ILO) small opacity profusion ≥1/0 in the absence of large opacities on chest radiograph] would continue to occur among long-tenured miners, although at a lower prevalence.10 At the time most available evidence suggested that, as long as miners worked under dust conditions consistent with the 2 mg/m3 PEL, there would be many fewer newly incident simple CWP cases, simple CWP cases would not be expected to advance to progressive massive fibrosis (PMF), and miners would no longer become disabled or suffer premature mortality as a result of the disease.3,10 Officials focused regulatory and public health efforts on preventing PMF among coal miners, based on the widespread belief that, in contrast with PMF, simple CWP was not associated with clinically significant lung function impairment. Research from the United Kingdom’s Medical Research Council Pneumoconiosis Research Unit during the 1950s and 1960s generally reported no association between increasing profusion of small opacities and worse lung function among those with simple CWP,11–13 as did later studies of U.S. coal miners.14–17 Medical textbooks have tended to perpetuate the early view,18–21 despite much of that early work having been called into question,22,23 and a number of international studies of coal miners in Britain,24,25 China, 26 South Africa,27 and Turkey28 reporting lung function impairment among coal miners with simple CWP.
A large body of evidence demonstrates dose-response relationships of cumulative coal mine dust exposure with lung function impairment and also with small opacity profusion.29–37 However, the association between profusion of small opacities in simple CWP and lung function has not been thoroughly investigated in U.S. coal miners. Recently, a study using data from the NIOSH Enhanced Coal Worker’s Health Surveillance Program (ECWHSP) identified similar geographic distributions of spirometric abnormalities (findings below lower limits of normal using U.S. population prediction equations) and radiographic CWP, in addition to associations between small opacity profusion category and certain lung function measures.38 We have expanded this work, using four additional years of data, by examining the relationship of radiographic profusion of opacities by subcategory with lung function in active and former underground coal miners with simple CWP.
Methods
In the ECWHSP, NIOSH staff visit mine sites or nearby communities to provide examinations at no cost to coal miners. The emphasis of the ECWHSP has been active coal miners, but former miners are welcome to participate. As a surveillance program, the ECWHSP has been granted a non-research designation by the NIOSH Institutional Review Board (11-DRDS-NR03). Trained technicians obtain written informed consent from participating miners, collect work histories, take posterior-anterior chest radiographs, and administer spirometry.39 Each chest radiograph is independently classified by a minimum of two physicians, at least one of whom is certified by NIOSH as a B Reader.40 All radiographs first classified by an A or B Reader are then submitted by NIOSH to a B Reader. If there is agreement between the two classifications, the result is final. If not, NIOSH requests a third classification from a panel of B Readers. If there is not agreement among the three classifications, two additional independent B Reader classifications are obtained, and the final determination is the median profusion category of the five classifications. Lung parenchymal abnormalities consistent with CWP are classified according to ILO guidelines.41 A final determination of small opacity profusion subcategory 1/0 or greater (range: 0/− to– 3/+) or large opacity category A, B, or C is considered evidence of CWP.42 Lung function testing is conducted using a SensorMedics dry-rolling seal volume spirometer integrated with Occupational Marketing Inc (Houston, TX) spirometry software. Spirometry calibration, performance, and results are interpreted according to American Thoracic Society and European Respiratory Society guidelines.43,44 Reference values and lower limits of normal for forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and FEV1/FVC are calculated using gender and race-specific reference equations derived from the 3rd National Health and Nutrition Examination Survey.45 Measured height (without shoes), measured weight, age, underground mining tenure, and smoking status (current, former, never) are recorded for each participant.
We evaluated differences in miner characteristics and lung function values (percent predicted FEV1, percent predicted FVC, and FEV1/FVC) across the range of profusion subcategories for small opacities. We used SAS® software version 9.3 (Cary, North Carolina) to fit linear regression models, with lung function values as continuous outcomes and profusion subcategory as an ordinal predictor, while controlling for smoking status (ever/never), body mass index (continuous BMI), and underground mining tenure (used as a surrogate for dust exposure, in years). Because we were interested in the association between profusion and lung function among those with simple CWP, participants with PMF were excluded from descriptive statistics and regression models; we report lung function values for PMF cases separately.
Results
At the time of analysis, records for 10,017 ECWHSP examinations of active and former underground coal miners were available for the time period September 2005 through December 2013. Of these, we excluded participants who did not perform spirometry (n = 1,361) and those with fewer than two acceptable and repeatable spirometry curves (n = 278). A total of 68 miners with PMF and acceptable spirometry were excluded from analysis. Fewer than ten miners had category 3 simple CWP; these participants were also excluded (rationale below). Among those with multiple ECWHSP visits during the study period, we restricted analysis to the most recent encounter, leaving 8,230 miners (7,864 active and 366 former) eligible for analysis.
The mean age was 46.8 years (range: 18 to 84) and 95.6% were white; males comprised 98.4% of the population. Mean underground coal mining tenure was 19 years (range: 0 to 51 years), mean BMI was 30.2 kg/m2, and 50.7% of participants reported ever smoking. Demographic differences by profusion subcategory are presented in e-Table 1.
Of the miners included in analysis, 269 (3.3%) had a determination of category 1 or 2 simple CWP; 210 had category 1 CWP (59 with 1/0, 95 with 1/1, and 56 with 1/2) and 59 had category 2 CWP (17 with 2/1, 23 with 2/2, and 19 with 2/3). The remaining 7,961 miners had either 0/0 or 0/1 determinations. Because fewer than ten miners had category 3 disease, these cases were excluded from analysis due to potential for instability in subcategory mean values and because a majority had evidence suggesting coalescence of small opacities (i.e., a radiographic appearance just short of PMF). Thus, our unadjusted subcategory and linear regression analyses were limited to miners with evidence of simple CWP and profusion scores within the range 0/0 through 2/3.
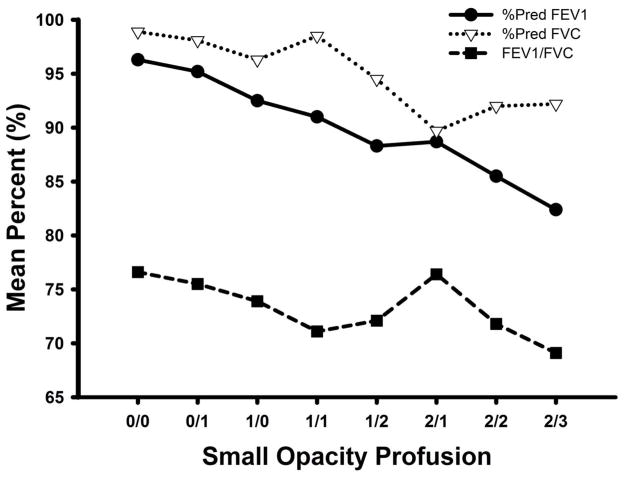
Figure 1 presents unadjusted mean percent predicted values for FEV1 (FEV1%) and FVC (FVC%), and mean percentages for FEV1/FVC, stratified by profusion subcategory. Omnibus F-tests for differences in means were statistically significant (p < 0.001) for each lung function measure. Differences in means as determined by the Waller-Duncan t-test are noted in e-Table 2; the k-ratio was set to 100 to approximate α = 0.05. Decrements in mean FEV1% were nearly consistent across profusion subcategories; mean FEV1% was 96.3% among miners with 0/0 profusion compared to 82.4% among those with 2/3 profusion. Additionally, there were statistically significant differences in mean FEV1% within the range of simple CWP (e.g., the 2/2 and 2/3 profusion subgroups had significantly lower mean FEV1% than the 1/0 profusion subgroup). Decrements in mean FVC% were less consistent, but were still evident. Miners with 0/0 profusion had a mean FVC% of 98.9% compared to 92.2% among those with 2/3 profusion. Within the range of simple CWP, the 2/1 profusion subgroup had significantly lower mean FVC% than the 1/0 and 1/1 subgroups. We observed a mean FEV1/FVC of 76.6% among miners with 0/0 profusion, compared to 69.1% among those with 2/3 profusion. The 2/3 profusion subgroup had significantly lower mean FEV1/FVC than the 1/0 subgroup, suggesting an association between higher radiographic profusion of simple CWP and obstructive impairment. Among participants with category 3 simple CWP, mean FEV1% was 85.6%, mean FVC% was 91.7%, and mean FEV1/FVC was 72.6%. Among the 68 with PMF, mean FEV1% was 80.3%, mean FVC% was 90.9%, and mean FEV1/FVC was 68.6%.
Figure 1.
Mean spirometric lung function values among underground coal miners participating in the Enhanced Coal Workers’ Health Surveillance Program, by small opacity profusion category, 2005–2013, n = 8,230
Table 1 summarizes the results of linear regression models of the relationship between small opacity profusion and the three lung function measures. Controlling for smoking status, BMI, and underground mining tenure (natural log transformed to approximate normal distribution), each one unit subcategory increase in profusion was associated with a decrease of 1.5% (95% CI 1.0% to 1.9%) in FEV1%. Adjusting for the same covariates, each unit increase in profusion was associated with decreases of 1.0% (95% CI 0.6% to 1.3%) and a 0.6% (95% CI 0.4% to 0.8%) in FVC% and FEV1/FVC, respectively. In the FEV1% and FVC% models, history of smoking, higher BMI, and longer underground mining tenures were each associated with lower mean lung function values. In the FEV1/FVC model, smoking and longer tenure were risk factors, while higher BMI appeared to be mildly protective.
Table 1.
Results of multiple linear regression analysis of associations between spirometric lung function values and radiographic profusion among underground coal miners participating in the Enhanced Coal Workers’ Health Surveillance Program, 2005–2013, n = 8,230
| Beta | Lower 95% CI | Upper 95% CI | |
|---|---|---|---|
| % Predicted FEV1 | |||
| Profusion (0/0 to 2/3)a | −1.46 | −1.88 | −1.04 |
| Smoking status (never/ever) | −4.09 | −4.71 | −3.47 |
| Body mass index (cont.) | −0.31 | −0.37 | −0.25 |
| Underground tenure (years) | −1.02 | −1.30 | −0.73 |
| % Predicted FVC | |||
| Profusion | −0.97 | −1.34 | −0.60 |
| Smoking status | −0.59 | −1.13 | −0.04 |
| Body mass index | −0.49 | −0.54 | −0.44 |
| Underground tenure | −0.67 | −0.92 | −0.42 |
| FEV1/FVC | |||
| Profusion | −0.59 | −0.80 | −0.37 |
| Smoking status | −3.15 | −3.46 | −2.83 |
| Body mass index | 0.10 | 0.07 | 0.14 |
| Underground tenure | −1.46 | −1.61 | −1.32 |
CI, Confidence interval; FEV1, Forced expiratory volume in 1 second; FVC, Forced vital capacity; cont., continuous variable
Profusion of small pneumoconiotic opacities, per International Labor Office (ILO) guidelines
Discussion
Simple CWP is not an inconsequential condition—we observed progressively lower lung function across the range of increasing small opacity profusion for each of the three spirometry measures. The effect was most apparent for FEV1%, the most important resting spirometric measure of lung function, and less consistent for FVC% and FEV1/FVC. In multiple regression models, this association between higher radiographic profusion and increasing impairment of lung function remained after controlling for smoking status, BMI, and underground mining tenure. Past studies have demonstrated an association between cumulative coal mine dust exposure and lung function impairment,29,31–33,35,37 as well as dust exposure and radiographic category of CWP.30,34,36 The current findings differ from the widely held historical literature and modern medical text dictums that there is no relationship between radiographic profusion and lung function in those with simple CWP.11–21 International studies have reported similar results,24–28 but these findings build on the work of Wang and colleagues38 by classifying small opacity profusion using ILO subcategories and by focusing on a modern sample of U.S. coal miners.
It is biologically plausible that increasing scarring of the lungs could be associated with progressive impairment of lung function, even if this may be difficult to demonstrate using categorical lower limits of normal as the criterion for defining outcomes. Meaningful physiologic changes may be associated with increasing small opacity profusion even if spirometric measures marking those changes in an affected individual don’t fall below lower limits of normal. For example, a miner could lose one-third of lung function, declining from high normal (e.g., 120% of predicted)—common in healthy industrial workers46,47—to low normal (e.g., 80% of predicted), but still have ‘normal’ lung function.
Exposure to coal mine dust causes lung function impairment through a variety of pathologies, including interstitial fibrosis, chronic bronchitis, emphysema, and small airways disease,48 but only the former is consistently evident as opacities on chest radiographs. In the current study the association between radiographic profusion and lung function remained after controlling for underground mining tenure, perhaps indicating that miners who are more susceptible to the scarring effects of coal mine dust may also be more susceptible to dust-induced lung function impairment. We noted lower FVC% and FEV1/FVC associated with higher profusion of small parenchymal opacities. It may be that increased scarring is associated not only with reductions in vital capacity, a restrictive pattern that would be expected, but also with obstructive deficits, perhaps through scar emphysema or small airways disease.48–50 Higher BMI appeared to be mildly but significantly protective in the FEV1/FVC model. This would be expected because higher BMI would lower an individual’s FVC and therefore increase the ratio value, assuming FEV1 remains static.
This study may be subject to healthy worker selection bias because about 95% of participants were actively working in coal mines and we had limited representation from former coal miners. If this effect were present it would likely lead to an underestimate of the degree of impairment because sicker individuals would be more likely to have left active mining, and sick individuals who were diagnosed and/or compensated previously would be less likely to participate in ongoing surveillance. There could be participation bias because ECWHSP participation is voluntary, but this would not be expected to affect the relationship between chest radiograph profusion and respiratory physiology. Additionally, it is quite possible that individuals in the early stages of disease are unaware they have CWP, because outward symptoms may be subtle or absent. A recent study found the concern of participation bias in this particular population to be largely unfounded.51 Of the groups included in analysis, the 2/1 subcategory had the smallest sample size within the simple CWP profusion range, and was the closest to what one could consider an outlier in the FVC% and FEV1/FVC trend lines in Figure 1. If a few participants had FVC measures markedly lower than the rest of those with the same profusion determination, the effect would be to depress the mean FVC% and inflate the mean ratio value. The low number of participants with category 3 determinations kept us from reliably assessing lung function differences across the entire range of simple CWP. Recent regulatory developments, summarized below, will likely increase the number of miners from which NIOSH obtains chest radiographs and spirometry, which could help address limitations related to small sample size in future analyses. Although the ECWHSP collects information on smoking status, it doesn’t include pack-year data. Individuals with more cumulative smoking would be more likely to have lower lung function, and the binary covariate used in this study doesn’t fully capture differences in smoking exposure among this group. We did not have coal mine dust exposure information and were limited to the use of self-reported tenure data. This precluded a more direct assessment of lung function impairment related to radiographic abnormality after adjusting for the separate effect of dust exposure.
In 1995, based on a comprehensive review of the literature examining adverse health effects of coal mine dust exposure, NIOSH recommended reducing the PEL for respirable coal mine dust from 2 to 1 mg/m3.52 The literature was reviewed again in 2011 and the recommendation was reaffirmed.3 This became part of the scientific basis for a final Mine Safety and Health Administration (MSHA) rule designed to reduce miners’ exposure to respirable coal mine dust, which was issued on May 1st, 2014.53 Components of the MSHA rule are being phased in between August 1st, 2014 and August 1st, 2016. The rule lowers the PEL to 1.5 mg/m3 (effective August 2016). It also institutes dust sampling changes to more accurately assess exposures and requires use of continuous personal dust monitors for high-risk positions. In accordance with the MSHA rule, NIOSH issued an interim final rule on August 1st, 2014 expanding all CWHSP medical surveillance beyond occupational history and chest radiography to include respiratory symptom assessment and spirometry screening for the early stages of lung function impairment among coal miners, and to expand the target population beyond those employed by underground coal mines to include those employed by surface coal mines and mining contractors.54
The results of our analysis point to progressive lung function impairment across the range of radiographic profusion of simple CWP, addressing a longstanding question in the field of occupational respiratory disease. Taken in concert with recent studies reporting a resurgence of CWP in U.S. coal miners,8,55–58 they highlight the importance of primary prevention and medical surveillance in this workforce. The CWHSP has a history spanning nearly half a century, and is the only nationwide surveillance system monitoring respiratory disease for the workforce of an entire industry. Until recently, only the ECWHSP—which has accounted for approximately one-third of the radiographs in the CWHSP—included spirometry. The new changes in the CWHSP will not only enhance our capacity to track the occurrence of radiographically evident pneumoconiosis throughout the coal mining industry, but will also enable us to better understand the factors which contribute to lung function impairment in coal miners.
Supplementary Material
Acknowledgments
Funding information: Dr. Cohen’s work was supported in part by funding from the Alpha Foundation for the Improvement of Mining Safety and Health.
D.B. designed the study; analyzed and interpreted the data; led writing of the manuscript; and is responsible for its content. A.L. participated in study design, data interpretation, and in writing the manuscript. C.H. assisted with statistical software coding, data interpretation, and participated in writing the manuscript. R.C. proposed the study, provided guidance during study design and data interpretation, and participated in writing the manuscript. All authors approved the submitted version and are accountable for the work.
The authors report no potential conflicts of interest. Dr. Cohen’s work was supported in part by funding from the Alpha Foundation for the Improvement of Mining Safety and Health. The Alpha Foundation played no role in the development of the study or the manuscript.
The authors would like to acknowledge the work of Anita Wolfe and the Coal Workers’ Health Surveillance Program staff.
Abbreviations list
- BMI
Body mass index
- CWHSP
Coal Workers’ Health Surveillance Program
- CWP
Coal workers’ pneumoconiosis
- ECWHSP
Enhanced Coal Worker’s Health Surveillance Program
- FEV1
Forced expiratory volume in one second
- FVC
Forced vital capacity
- ILO
International Labour Organization
- MSHA
Mine Safety and Health Administration
- NIOSH
National Institute for Occupational Safety and Health
- FEV1%
Percent predicted FEV1
- FVC%
Percent predicted FVC
- PEL
Permissible exposure limit
- PMF
Progressive massive fibrosis
Footnotes
Conflict of interest statement: The authors report no potential conflicts of interest.
Prior presentation: These findings have not been published or presented.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health or the Centers for Disease Control and Prevention (CDC). Mention of a specific product or company does not constitute an endorsement by the authors or by CDC.
References
- 1.United States Congress. Federal Coal Mine Health and Safety Act of 1969. Public Law 1969:91–173.
- 2.American College of Occupational and Environmental Medicine. Lung Disorders Committee. 2011. Comments of the ACOEM, U.S. Mine Safety and Health Administration, Lowering miner’s exposure to respirable coal mine dust, including continuous personal dust (RIN 1219–AB64) [Google Scholar]
- 3.Attfield M, Hale J, Suarthana E, Wang ML, Castranova V, Clough Thomas K. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. Current Intelligence Bulletin 64: Coal Mine Dust Exposures and Associated Health Outcomes, a Review of Information Published Since 1995. Cincinnati, OH: 2011. pp. 1–38. [Google Scholar]
- 4.Percentage of examined underground miners with coal workers’ pneumoconiosis (ILO category 1/0+) by tenure in mining, 1970–2009. 2011 at http://www2a.cdc.gov/drds/worldreportdata/SectionDetails.asp?ArchiveID=1&SectionTitleID=2.
- 5.Laney AS, Attfield MD. Coal workers’ pneumoconiosis and progressive massive fibrosis are increasingly more prevalent among workers in small underground coal mines in the United States. Occup Environ Med. 2010;67:428–31. doi: 10.1136/oem.2009.050757. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin S, Attfield MD. Temporal trends in coal workers’ pneumoconiosis prevalence: validating the national coal study results. Occup Environ Med. 1998;40:1065–71. doi: 10.1097/00043764-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Occupational Respiratory Disease Surveillance, Coal Workers’ Health Surveillance Program. National Institute for Occupational Safety and Health; [Accessed May 8, 2014]. at http://www.cdc.gov/niosh/topics/surveillance/ords/CoalWorkersHealthSurvProgram.html. [Google Scholar]
- 8.Blackley DJ, Halldin CN, Laney AS. Resurgence of a debilitating and entirely preventable respiratory disease among working coal miners. Am J Respir Crit Care Med. 2014;190:708–9. doi: 10.1164/rccm.201407-1286LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bayer R. The Health and safety of workers: case studies in the politics of professional responsibility. Oxford University Press; USA: 1988. [Google Scholar]
- 10.Jacobsen M, Rae S, Walton WH, Rogan JM. The relation between pneumoconiosis and dust-exposure in British coal mines. Inhaled particles. 1970;2:903. [PubMed] [Google Scholar]
- 11.Higgins ITT, Oldham PD. Ventilatory capacity in miners. A five-year follow-up study. Br J Ind Med. 1962;19:65–76. doi: 10.1136/oem.19.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cochrane AL, Higgins ITT, Thomas J. Pulmonary ventilatory functions of coalminers in various areas in relation to the x-ray category of pneumoconiosis. Br J Prev Soc Med. 1961;15:1–11. doi: 10.1136/jech.15.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carpenter RG, Cochrane AL, Gilson JC, Higgins ITT. The relationship between ventilatory capacity and simple pneumoconiosis in coalworkers: the effect of population selection. Br J Ind Med. 1956;13:166. doi: 10.1136/oem.13.3.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgan WKC. On dust, disability, and death. Am Rev Respir Dis. 1986;134:639–41. doi: 10.1164/arrd.1986.134.4.639. [DOI] [PubMed] [Google Scholar]
- 15.Morgan WKC, Handelsman L, Kibelstis J, Lapp NL, Reger R. Ventilatory capacity and lung volumes of US coal miners. Arch Environ Health. 1974;28:182–9. doi: 10.1080/00039896.1974.10666466. [DOI] [PubMed] [Google Scholar]
- 16.Morgan WKC, Lapp NL, Seaton D. Respiratory disability in coal miners. JAMA. 1980;243:2401–4. [PubMed] [Google Scholar]
- 17.Morgan WKC. Coal workers’ pneumoconiosis. Am Ind Hyg Assoc J. 1971;32:29–34. doi: 10.1080/0002889718506403. [DOI] [PubMed] [Google Scholar]
- 18.Bourke SJ, Burns GP. Lecture Notes: Respiratory Medicine. John Wiley & Sons; 2011. [Google Scholar]
- 19.Mason RJ, Broaddus VC, Martin T, et al. Murray and Nadel’s Textbook of Respiratory Medicine. Elsevier Health Sciences; 2010. [Google Scholar]
- 20.Hendrick DJ. Occupational Disorders of the Lung: Recognition, Management and Prevention. Saunders; 2002. [Google Scholar]
- 21.Baum G, Wolinsky E. Textbook of Pulmonary Diseases. 1994;2 [Google Scholar]
- 22.Rudd R. Coal miners’ respiratory disease litigation. Thorax. 1998;53:337–40. doi: 10.1136/thx.53.5.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Griffiths & Ors v British Coal Corp & Anor England and Wales High Court. Queen’s Bench Division; 1998. [Google Scholar]
- 24.Lyons J, Campbell H. Evolution of disability in coalworkers’ pneumoconiosis. Thorax. 1976;31:527–33. doi: 10.1136/thx.31.5.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rogan JM, Ashford J, Chapman P, Duffield D, Fay J, Rae S. Pneumoconiosis and respiratory symptoms in miners at eight collieries. Brit Med J. 1961;1:1337. doi: 10.1136/bmj.1.5236.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, Yu IT, Wong TW, Yano E. Respiratory symptoms and pulmonary function in coal miners: looking into the effects of simple pneumoconiosis. Am J Ind Med. 1999;35:124–31. doi: 10.1002/(sici)1097-0274(199902)35:2<124::aid-ajim3>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 27.Naidoo RN, Robins TG, Solomon A, White N, Franzblau A. Radiographic outcomes among South African coal miners. Int Arch Occup Environ Health. 2004;77:471–81. doi: 10.1007/s00420-004-0532-3. [DOI] [PubMed] [Google Scholar]
- 28.Akkoca Yildiz O, Eris Gulbay B, Saryal S, Karabiyikoglu G. Evaluation of the relationship between radiological abnormalities and both pulmonary function and pulmonary hypertension in coal workers’ pneumoconiosis. Respirology. 2007;12:420–6. doi: 10.1111/j.1440-1843.2007.01031.x. [DOI] [PubMed] [Google Scholar]
- 29.Coggon D, Taylor AN. Coal mining and chronic obstructive pulmonary disease: a review of the evidence. Thorax. 1998;53:398–407. doi: 10.1136/thx.53.5.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Attfield MD, Seixas NS. Prevalence of pneumoconiosis and its relationship to dust exposure in a cohort of US Bituminous coal miners and ex-miners. Am J Ind Med. 1995;27:137–51. doi: 10.1002/ajim.4700270113. [DOI] [PubMed] [Google Scholar]
- 31.Seixas NS, Robins TG, Attfield MD, Moulton L. Longitudinal and cross sectional analyses of exposure to coal mine dust and pulmonary function in new miners. Br J Ind Med. 1993;50:929–37. doi: 10.1136/oem.50.10.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oxman AD, Muir DC, Shannon HS, Stock SR, Hnizdo E, Lange H. Occupational dust exposure and chronic obstructive pulmonary disease: a systematic overview of the evidence. Am Rev Respir Dis. 1993;148:38–48. doi: 10.1164/ajrccm/148.1.38. [DOI] [PubMed] [Google Scholar]
- 33.Attfield MD, Hodous TK. Pulmonary function of US coal miners related to dust exposure estimates. Am Rev Respir Dis. 1992;145:605–9. doi: 10.1164/ajrccm/145.3.605. [DOI] [PubMed] [Google Scholar]
- 34.Attfield M, Morring K. An investigation into the relationship between coal workers’ pneumoconiosis and dust exposure in coal miners. Am Ind Hyg Assoc J. 1992;53:486–92. doi: 10.1080/15298669291360012. [DOI] [PubMed] [Google Scholar]
- 35.Marine WM, Gurr D, Jacobsen M. Clinically important respiratory effects of dust exposure and smoking in British coal miners. Am J Respir Crit Care Med. 1988;137:106–12. doi: 10.1164/ajrccm/137.1.106. [DOI] [PubMed] [Google Scholar]
- 36.Hurley J, Alexander W, Hazledine D, Jacobsen M, Maclaren W. Exposure to respirable coalmine dust and incidence of progressive massive fibrosis. Br J Ind Med. 1987;44:661–72. doi: 10.1136/oem.44.10.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rogan J, Attfield M, Jacobsen M, Rae S, Walker D, Walton W. Role of dust in the working environment in development of chronic bronchitis in British coal miners. Br J Ind Med. 1973;30:217–26. doi: 10.1136/oem.30.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang ML, Beeckman-Wagner L-A, Wolfe AL, Syamlal G, Petsonk EL. Lung-function impairment among US underground coal miners, 2005 to 2009: geographic patterns and association with coal workers’ pneumoconiosis. J Occup Environ Med. 2013;55:846–50. doi: 10.1097/JOM.0b013e31828dc985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National Institute for Occupational Safety and Health. Enhanced Coal Workers’ Health Surveillance Program (ECWHSP) Mar, 2011. [Google Scholar]
- 40. [Accessed January, 2015];The NIOSH B Reader Program. 2011 at http://www.cdc.gov/niosh/topics/chestradiography/breader.html.
- 41.International Labour Office. Guidelines for the use of the ILO international classification of radiographs of pneumoconioses. Geneva: International Labour Office; 2011. [Google Scholar]
- 42.Centers for Disease Control and Prevention. Pneumoconiosis prevalence among working coal miners examined in federal chest radiograph surveillance programs--United States, 1996–2002. MMWR Morb Mortal Wkly Rep. 2003;52:336–40. [PubMed] [Google Scholar]
- 43.Miller M, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 44.Pellegrino R, Viegi G, Brusasco V, et al. Interpretive strategies for lung function tests. Eur Respir J. 2005;26:948–68. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 45.Hankinson J, Odencrantz J, Fedan K. Spirometric reference values from a sample of the general U.S population. Am J Respir Crit Care Med. 1999;159:179–87. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 46.Becklake MR, White N. Sources of variation in spirometric measurements. Identifying the signal and dealing with noise. Occup Med. 1993;8:241–64. [PubMed] [Google Scholar]
- 47.Kauffmann F, Drouet D, Lellouch J, Brille D. Occupational exposure and 12-year spirometric changes among Paris area workers. Br J Ind Med. 1982;39:221–32. doi: 10.1136/oem.39.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stansbury RC, Beeckman-Wagner LAF, Wang ML, Hogg JP, Petsonk EL. Rapid decline in lung function in coal miners: Evidence of disease in small airways. Am J Ind Med. 2013;56:1107–12. doi: 10.1002/ajim.22211. [DOI] [PubMed] [Google Scholar]
- 49.Kuempel ED, Wheeler MW, Smith RJ, Vallyathan V, Green FH. Contributions of dust exposure and cigarette smoking to emphysema severity in coal miners in the United States. Am J Respir Crit Care Med. 2009;180:257–64. doi: 10.1164/rccm.200806-840OC. [DOI] [PubMed] [Google Scholar]
- 50.Vallyathan V, Landsittel DP, Petsonk EL, et al. The influence of dust standards on the prevalence and severity of coal worker’s pneumoconiosis at autopsy in the United States of America. Arch Pathol Lab Med. 2011;135:1550–6. doi: 10.5858/arpa.2010-0393-OA. [DOI] [PubMed] [Google Scholar]
- 51.Laney A, Attfield M. Examination of potential sources of bias in the US Coal Workers’ Health Surveillance Program. Am J of Public Health. 2013;104:165–70. doi: 10.2105/AJPH.2012.301051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Institute for Occupational Safety and Health, editor. Criteria for a Recommended Standard: Occupational Exposure to Respirable Coal Mine Dust. Cincinnati, Ohio: U.S. Government Printing Office; 1995. p. 360. [Google Scholar]
- 53.U.S. Department of Labor. Lowering Miners’ Exposure to Respirable Coal Mine Dust, Including Continuous Personal Dust Monitors. Federal Register. 2014;79(84) [Google Scholar]
- 54.U.S. Department of Health and Human Services, editor. Specifications for Medical Examinations of Coal Miners. 2014. [Google Scholar]
- 55.Pon M, Roper R, Petsonk E, et al. Pneumoconiosis Prevalence Among Working Coal Miners Examined In Federal Chest Radiograph Surveillance Programs-United States, 1996–2002. MMWR Morb Mortal Wkly Rep. 2003;52:336–40. [PubMed] [Google Scholar]
- 56. [Accessed January, 2015];Coal Workers’ Pneumoconiosis: Morbidity. 2011 at http://wwwn.cdc.gov/eworld/Data/CWXSP_Percentage_of_examined_underground_miners_with_coal_workers_pneumoconiosis_ILO_category_10_by_tenure_in_mining_1970-2009/558.
- 57.Blackley DJ, Halldin CN, Wang ML, Laney AS. Small mine size is associated with lung function abnormality and pneumoconiosis among underground coal miners in Kentucky, Virginia and West Virginia. Occup Environ Med. 2014;71:690–94. doi: 10.1136/oemed-2014-102224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Laney AS, Weissman DN. Respiratory diseases caused by coal mine dust. J Occup Environ Med. 2014;56(Suppl 10):S18–22. doi: 10.1097/JOM.0000000000000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.