Abstract
BACKGROUND
The course of denim sandblasting silicosis is unknown. We aimed to reevaluate former sandblasters studied in 2007 for incident silicosis, radiographic progression, pulmonary function loss, and mortality and to examine any associations between these outcomes and previously demonstrated risk factors for silicosis.
METHODS
We defined silicosis on chest radiograph as category 1/0 small opacity profusion using the International Labor Organization classification. We defined radiographic progression as a profusion increase of two or more subcategories, development of a new large opacity, or an increase in large opacity category. We defined pulmonary function loss as a ≥ 12% decrease in FVC.
RESULTS
Among the 145 former sandblasters studied in 2007, 83 were reassessed in 2011. In the 4-year follow-up period, nine (6.2%) had died at a mean age of 24 years. Of the 74 living sandblasters available for reexamination, the prevalence of silicosis increased from 55.4% to 95.9%. Radiographic progression, observed in 82%, was associated with younger age, never smoking, foreman work, and sleeping at the workplace. Pulmonary function loss, seen in 66%, was positively associated with never smoking and higher initial FVC % predicted. Death was associated with never smoking, foreman work, number of different denim-sandblasting places of work, sleeping at the workplace, and lower pulmonary function, of which only the number of different places worked remained in multivariate analyses.
CONCLUSIONS
This 4-year follow-up suggests that almost all former denim sandblasters may develop silicosis, despite short exposures and latency.
Denim-jean sandblasting is a recognized cause of silicosis, and many cases, some with fatal outcomes, have been reported from different centers in Turkey.1-7 Our previous work demonstrated that among former denim sandblasters who were exposed to silica for at least 1 month and who had a latency period of at least 10 months, 77 of 145 subjects (53%) had silicosis in 2007,6 based on the International Labor Organization (ILO) classification of radiographs of pneumoconioses.8
In the current study, our primary aim was to reevaluate these former sandblasters who had terminated occupational exposure to silica dust prior to 2007, to determine whether the number of cases meeting diagnostic criteria for silicosis had increased in the absence of continued exposure. Second, we aimed to investigate other health outcomes (radiographic progression, pulmonary function loss, and mortality) among the subjects and to examine associations between these health outcomes and risk factors that had been individually associated with silicosis in the earlier cross-sectional study,6 including exposure duration, foreman status at work (a marker of higher exposure than apprentices), and number of denim-sandblasting workplaces in which they worked.
Materials and Methods
Study Population
The source population of this study consisted of the 145 former denim sandblasters who had interpretable chest radiographs and spirometry tests when studied in 2007.6 In 2011, a temporary national law in Turkey gave a right to compensation to all uninsured patients with silicosis. Thus, we invited all the denim sandblasters in our source population, regardless of a prior silicosis diagnosis, to our tertiary-care university hospital to participate in our follow-up study. We offered assistance in preparing an official application for compensation. For the nonrespondents to our follow-up, we ascertained vital status with our hospital records and the online Death Declaration System of the Turkish Health Ministry. We included those who died between 2007 and 2011 in this study. All living participants gave their written informed consent, and the local ethics committee approved the study protocol (registration number 2011/37).
Study Procedures
For baseline evaluation, we used the findings of the 2007 study.6 In a 2011 medical interview, we confirmed that all participants being reevaluated had no further exposure to silica dust. The same technician conducted pulmonary function tests in 2007 and 2011 using the same computerized spirometer (Vmax22; SensorMedics Corp),6 recording the best FEV1, FVC, and FEV1/FVC ratio among three acceptable efforts. We calculated FEV1 % predicted and FVC for age, sex, and height.9
Standard posteroanterior chest radiographs of all living participants were taken at maximal inspiration and evaluated according to the ILO classification.8 Three experts independently evaluated 2011 chest radiographs, blinded to the 2007 ILO reading and clinical data of the participants. Any disagreement was resolved by consensus. Small-opacity profusion was classified into four main categories (0 to 3) and 12 subcategories, and the ILO categories and subcategories were used as indices of disease severity.
We defined silicosis on chest radiograph as a profusion of small pneumoconiotic opacities of ILO category 1/0 or higher.8 We defined radiographic progression as (1) an increase in small-opacity profusion of two or more subcategories (ie, from 0/0 to 1/0 or from 1/2 to 2/2), or (2) the appearance of one or more new large opacities (A, B, C), or (3) an increase in large-opacity category (from A to B or from B to C).8 Pulmonary function loss was defined as a ≥ 12% decrease in FVC, with guidance from longitudinal interstitial lung disease research,10,11 between 2007 and 2011. All deaths were attributed to silicosis or related complications.
Statistical Analysis
We used SPSS Statistics soft ware, version 20 for Mac (IBM Corporation), for statistical analyses. The Pearson χ2 test and the Mann-Whitney U test were used to compare categorical and numeric values, respectively. We used binary logistic regression to test for associations with predetermined risk factors. A P value < .05 was considered statistically significant.
Results
Of the 145 denim sandblasters studied in 2007, the follow-up study included 83 men (57.2%), of whom 74 had both interpretable chest radiographs and valid spirometry in 2011 and nine (6.2%) had died (Fig 1). In comparison with the nonparticipants in 2011, the study group had less history of working as a foreman, history of sleeping at the sandblasting work places, and smoking pack-years (Table 1). Nonparticipants and participants had similar pulmonary function in 2007, but living participants tended to have more small and large pneumoconiotic opacities on their 2007 chest radiograph (Table 2). The mean age (± SD) of living participants was 27 ± 6 years in 2011. The mean age at death of the nine who had died during the follow-up period was 24 years (range, 18-29 years).
Figure 1. Flowchart. The 83 former sandblasters reported in the current study included 74 living participants who had new chest radiographs and pulmonary function tests in 2011 and nine who were deceased.
TABLE 1.
Characteristics in 2007 of Denim Sandblasters by Nonparticipants and Those Whose Vital Status and Medical Tests Were Reassessed in 2011
| Characteristics in 2007 | Nonparticipants (n = 62) |
Reassessed in 2011 (n = 83) |
|---|---|---|
| Age at first admission, y | 23 ± 5 | 23 ± 6 |
| First exposure age, y | 17 ± 6 | 17 ± 5 |
| Ever smoker | 46 (74) | 58 (70) |
| Smoking, pack-ya | 7.1 ± 4.6 | 5.0 ± 4.9 |
| Exposure duration, mo | 35 ± 24 | 41 ± 27 |
| Time since first exposure, mo |
78 ± 35 | 81 ± 37 |
| Working as a foremana | 57 (92) | 58 (70) |
| Months as a foreman | 32 ± 28 | 31 ± 29 |
| Places of work, No. | 3 ± 2 | 2 ± 1 |
| Sandblasting devices, No. |
4 ± 1 | 4 ± 1 |
| Sleeping at workplacea | 57 (92) | 51 (61) |
| FVC, L | 4.37 ± 0.96 | 4.47 ± 1.08 |
| FVC, % predicted | 93.6 ± 22.8 | 95.6 ± 21.9 |
| FEV1, L | 3.82 ± 0.90 | 3.83 ± 1.00 |
| FEV1, % predicted | 94.5 ± 23.1 | 95.9 ± 25.4 |
| FEV1/FVC % | 86.8 ± 9.4 | 86.4 ± 9.5 |
Data presented as mean ± SD or No. (%) unless otherwise stated.
P < .05.
TABLE 2.
Chest Radiograph ILO Categorization by Nonparticipants, Decedents, and Participants by Year of Examinationa
| ILO Category | Nonparticipantsb (n = 62) | Decedentsc (n = 9) | Participants (n = 74) | |
|---|---|---|---|---|
| Year of data | 2007 | 2007 | 2007 | 2011 |
| Category 0 | 35 (56.5) | … | 33 (44.6) | 3 (4.1) |
| 0/− | 27 | … | 25 | … |
| 0/0 | 1 | … | 2 | 1 |
| 0/1 | 7 | … | 6 | 2 |
| Category 1 | 14 (22.6) | 1 (11.1) | 20 (27.0) | 24 (32.4) |
| 1/0 | 5 | … | 14 | 4 |
| 1/1 | 5 | … | 4 | 10 |
| 1/2 | 4 | 1 | 2 | 11 |
| Category 2 | 8 (12.9) | … | 8 (10.8) | 22 (29.7) |
| 2/1 | 1 | … | 3 | 4 |
| 2/2 | 0 | … | 2 | 9 |
| 2/3 | 7 | … | 3 | 9 |
| Category 3 | 5 (8.1) | 8 (88.9) | 13 (17.6) | 25 (33.8) |
| 3/2 | 3 | 1 | 4 | 6 |
| 3/3 | 2 | 1 | 3 | 7 |
| 3/+ | … | 6 | 6 | 20 |
| Large opacities | 2 (3.2) | 4 (44.4) | 8 (10.8) | 18 (24.3) |
| Type A | … | 2 | 4 | 3 |
| Type B | … | 0 | 3 | 3 |
| Type C | 2 | 2 | 1 | 13 |
Overall category data given as No. (%); subcategory data given as No. ILO = International Labor Organization.
The small-opacity profusion category and the presence of large opacities were both statistically significantly different between decedents and both participants (P < .01) and nonparticipants (P < .001) and within participants studied in 2007 (P < .001) and reevaluated in 2011 (P < .001).
Participants from the 2007 study who were not included in the 2011 follow-up. Data listed from these participants are from the 2007 study. These participants were not included in the follow-up because they had no new chest radiograph or pulmonary function test to evaluate.
Participants from the 2007 study who were deceased at the time of the 2011 follow-up.
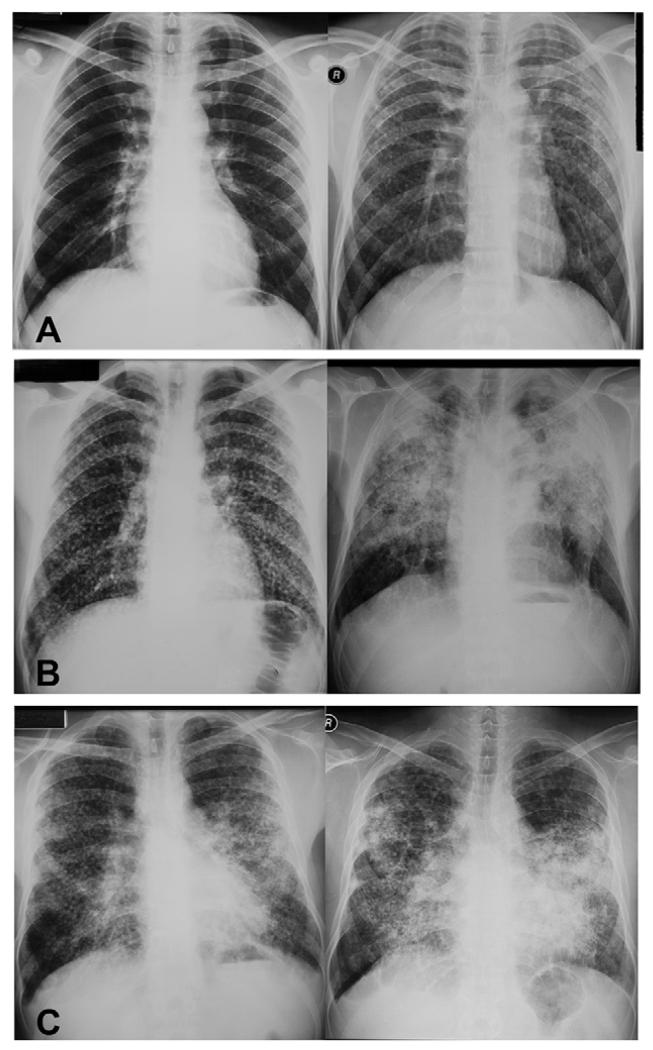
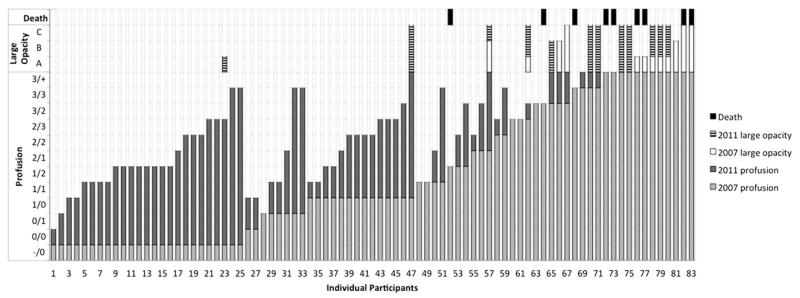
The proportion of living participants with silicosis increased from 55.4% to 95.9%. Radiographic progression and 12% pulmonary function loss were observed in 82% (n = 61) and 66% (n = 49) of participants, respectively. Between 2007 and 2011, both the small-opacity profusion and the presence of large opacities increased significantly. Three examples of radiographic progression are shown in Figure 2. ILO classifications in 2007 and 2011 are shown in Figure 3 for each participant. Table 2 presents the 2007 classification results for nonparticipants, those who had died, and living participants, along with 2011 classification results for living participants. Eight of nine decedents (88.9%) had severe ILO category 3 disease in 2007, significantly higher than both nonparticipants (P < .001) and living participants (P < .001). Decedents were also more likely to have had large opacities in 2007 compared with those who were restudied in 2011 (44.4% vs 10.8%, P < .01), as well as nonparticipants (44.4% vs 3.2%, P < .001).
Figure 2. A-C, Chest radiographs showing progression in three different cases. A, Incident small opacities to International Labor Organization subcategory 3/2. B, Incident small opacities to category C large opacity. C, Progression of large opacities from category A to category B.
Figure 3. Radiographic progression during the follow-up period by individual participants showing International Labor Organization small-opacity profusion and large-opacity category on the vertical axis. Large-opacity categories A, B, and C are indicated by bars of lengths 1, 2, and 3 units, respectively. Decedents are indicated in the top row on top of the appropriate histogram bar.
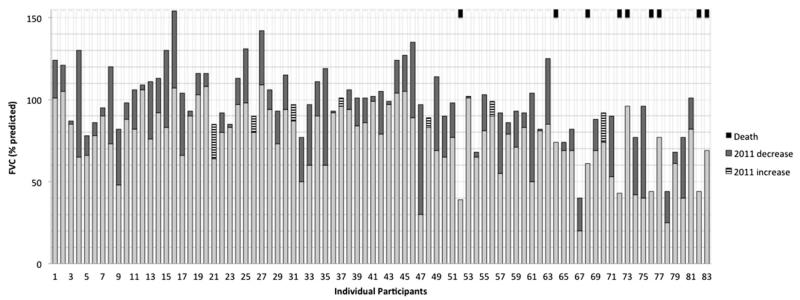
Data on FVC % predicted in 2007, along with the change measured in 2011 for the living participants, are shown by participant in Figure 4. All but eight participants had a decrease in FVC % predicted (89%), and the mean change in FVC % predicted for the 74 was −19.7, with a range of −67.0% to 21.0% predicted. For FEV1, all but six had a decrease in FEV1 % predicted, and the mean change in FEV1 % predicted was −25.3, with a range of −86.0% to 25.2%. For living participants, the mean FEV1 % predicted (± SD) was 100.3% ± 22.1 in 2007 and 74.9% ± 24.4 in 2011. The comparable mean values for FVC % predicted (± SD) were 98.7% ± 20.6 in 2007 and 79.0% ± 20.7 in 2011.
Figure 4. Pulmonary functions (FVC % predicted values) by individual participants in the study group, with the same numbering system as used in Figure 3. Light gray bars indicate the 2007 value for decedents, indicated in the top row above the appropriate histogram bar. Hatched bars indicate a 2011 increase in the 2007 value. Dark gray bars indicate the magnitude of decrease of pulmonary function in 2011 compared with the 2007 value, the latter being the sum of light gray and dark gray bars.
Comparison of 2007 characteristics of the participants by radiographic progression, 12% loss of pulmonary function, and death is shown in Table 3. In multivariate analyses, the only statistically significant relation we found for any of the health outcomes and for the predetermined risk factors for silicosis found cross sectionally in our 2007 study was between mortality and number of sandblasting places of work (OR, 3.16; 95% CI, 1.46-6.85). The other predetermined risk factors—exposure duration and foreman work status—did not enter multivariate models for any of the health outcomes.
TABLE 3.
Demographics, Pulmonary Function Indexes, and Exposure Characteristics in 2007 of 83 Former Sandblasters Assessed in 2011 by Radiographic Progression, 12% Pulmonary Function Loss, and Death
| Characteristic | Radiographic Progression | Pulmonary Function Loss | Death | |||
|---|---|---|---|---|---|---|
| No Progression (n = 13) | Progression (n = 61) | No Loss (n = 25) | Loss (n = 49) | Alive (n = 74) | Dead (n = 9) | |
| Age in 2007, y | 26.9 ± 7.4a | 23.1 ± 5.2a | 24.2 ± 4.3 | 23.5 ± 6.3 | 23.7 ± 5.7 | 20.9 ± 2.5 |
| Age at first exposure, y | 19.5 ± 6.5a | 16.3 ± 5.3a | 17.0 ± 5.4 | 16.8 ± 5.7 | 16.9 ± 5.6 | 15.1 ± 1.9 |
| Ever smoker, No. (%) | 10 (76.9)a | 44 (72.1)a | 22 (88.0)a | 32 (65.3)a | 54 (73.0) | 4 (44.4)a |
| Smoking pack-y | 5.8 ± 4.8 | 5.3 ± 5.0 | 6.6 ± 4.5 | 4.7 ± 5.1 | 5.4 ± 4.9a | 2.0 ± 3.0a |
| Exposure duration, mo | 35.0 ± 34.7 | 41.8 ± 27.2 | 44.2 ± 23.4 | 38.8 ± 30.9 | 40.6 ± 28.5 | 40.1 ± 13.5 |
| Time since first exposure, mo | 88.6 ± 45.8 | 81.1 ± 36.4 | 85.4 ± 42.2 | 80.8 ± 36.1 | 82.4 ± 38.0 | 65.3 ± 29.8 |
| Work as a foreman, No. (%) | 6 (46.2)a | 45 (73.8)a | 20 (80.0)a | 31 (63.3)a | 51 (68.9)a | 7 (77.8) |
| Months as a foreman | 24.9 ± 38.3 | 31.9 ± 28.3 | 34.2 ± 27.6 | 28.8 ± 31.4 | 30.6 ± 30.1 | 29.8 ± 18.0 |
| Places of work, No. | 2.2 ± 1.4 | 2.2 ± 1.1 | 2.3 ± 0.9 | 2.1 ± 1.3 | 2.2 ± 1.2a | 3.3 ± 0.7 |
| Sandblasting devices, No. | 3.3 ± 0.8 | 3.8 ± 1.5 | 4.3 ± 1.9a | 3.5 ± 0.9a | 3.7 ± 1.4 | 3.6 ± 0.5 |
| Sleeping at workplace, No. (%) | 7 (53.8)a | 36 (59.0)a | 18 (72.0)a | 25 (51.0)a | 43 (58.1)a | 8 (88.9)a |
| Height, cm | 172.2 ± 3.9 | 170.3 ± 6.3 | 170.4 ± 5.6 | 170.7 ± 6.2 | 170.6 ± 6.0 | 168.4 ± 4.3 |
| FVC, L | 5.16 ± 0.65 | 4.58 ± 0.90 | 4.42 ± 0.73a | 4.82 ± 0.93a | 4.68 ± 0.89a | 2.71 ± 0.95a |
| FVC, % predicted | 104.3 ± 14.1 | 97.5 ± 21.7 | 88.3 ± 12.8a | 104.0 ± 21.9a | 98.7 ± 20.6a | 60.8 ± 19.7a |
| FEV1, L | 4.33 ± 0.55 | 3.96 ± 0.89 | 3.92 ± 0.77 | 4.07 ± 0.89 | 4.02 ± 0.85a | 2.32 ± 0.88a |
| FEV1, % predicted | 104.1 ± 16.1 | 99.5 ± 23.3 | 95.3 ± 18.6 | 102.8 ± 23.5 | 100.3 ± 22.1a | 59.8 ± 21.9a |
| FEV1/FVC % | 86.9 ± 11.5 | 86.3 ± 9.5 | 88.6 ± 8.3 | 85.3 ± 10.4 | 86.4 ± 9.8 | 86.0 ± 7.2 |
Data are presented as mean ± SD unless otherwise indicated.
Statistically significant.
Discussion
The most important findings of our study were the high incidence of silicosis and progression of silicosis without further exposure to silica dust among the former denim sandblasters. The silicosis prevalence rate for the 83 subjects with follow-up testing or vital status determination in 2011 increased from 60.2% (n = 50) to 96.4% (n = 80) in a 4-year period, after mean occupational exposure of < 3.5 years and a mean latency since first exposure within 11 years. Of those who did not die of silicosis, most had two-subcategory radiographic progression (82%) or pulmonary function loss ≥ 12% in the FVC (66%). In fact, of the 74 surviving participants, only one had neither any progression of radiologic abnormality nor any pulmonary function loss.
Our study is unique in describing the radiographic course of silicosis in denim sandblasters and having a 4-year follow-up period. The only other follow-up study of denim sandblasters, at 29 (SD, ± 20 months), showed all pulmonary function test and % predicted values declined in acute and accelerated silicosis and only diffusing capacity of the lung to carbon monoxide declined in chronic silicosis cases.12 Our findings extend what is known about pneumoconiosis radiographic progression and pulmonary functions over time without further exposure and about impairment of lung function with radiographic progression.13-16 Although we had diagnosed some patients with acute silicosis among the former denim sandblasters in the past, they died before the 2007 study3,6; thus, this study only includes cases with accelerated silicosis.
In univariate analyses, we determined that younger age and younger age at first silica exposure were significantly associated with radiographic progression. Because smoking history and smoking pack-years were associated with older age (data not shown), those with progression in radiographic and pulmonary function indexes and those who died were less likely to have ever smoked; those who died had significantly fewer mean pack-years of smoking. Radiographic and 12% pulmonary function deterioration, and mortality were associated with working as a foreman and with sleeping at the workplace, during which workers had passive silica exposure, resulting in around-the-clock exposure. Mortality also increased with number of places in which they had worked, which may reflect turnover from workplaces with poorer conditions.
In addition to silicosis, this sandblaster population has contributed to studies of other health conditions associated with silica exposure and affecting their quality of life. These include eye and upper airway problems17; pneumothorax, even bilateral18,19; and TB.20 Also, psychologic problems are common,21,22 in that many patients have relatives or friends who have died of silicosis, and they know that there is no long-term curative treatment of the disease except for lung transplantation.23
Producing fashionable worn-out jeans by sandblasting of denim began in Turkey after 1992 and reached its peak around 2000.6 Following the death of the first two cases and emergence of other silicosis cases,1-6 the public started to realize the magnitude of the problem and most of the workers quit their jobs. In response to public indignation, the government provided patients with silicosis free access to health care and banned the process of sandblasting with silica abrasives in 2009. Since many patients with silicosis had no health insurance and were too impaired to work, the government provided compensation via a temporary law valid for a 3-month period for workers who had previously worked in companies in which ≥ 15% of the workforce had developed silicosis. This law did not cover the families of workers who had previously died or workers who had not progressed to silicotic impairment at the time of the law’s passage. Of the applicants with a valid application for compensation and diagnosed with silicosis in 2011, only 48% received disability compensation.24 Our study shows that silicosis progresses with time in the absence of exposure and that such temporary laws will not cover all the workers at risk who have not yet developed impairment from the disease.
Although Turkey banned sandblasting of denim jeans, the occupational health consequences are global as long as sandblasted jeans are sold, because production has shifted to other countries, including Bangladesh.25 Another preventive approach would be for clothing manufacturers to clarify their policies on purchasing sandblasted denim in light of the mortality and morbidity from silicosis associated with this process in the global supply chain.25
Our study was limited in that we were not able to recruit 62 of the 145 workers evaluated in 2007. Some of the nonparticipants may have sought evaluation at other academic medical centers; one is equidistant from their village. The nonparticipants differed from study subjects in having higher proportions of foremen (92%) and those who slept in the sandblasting workplaces (92%), both characteristics associated with worse health outcomes among those who were reassessed in 2011. We conclude that our participant sample may have underestimated the burden of silicosis and its progression in the entire cohort evaluated in 2007. With the small numbers of decedents and participants, we had limited statistical power to demonstrate differences in determinants of health outcome, if they existed, in several indices of exposure risk, such as exposure duration and time since first exposure.
Another limitation of our study was the lack of clinical laboratory evidence of the prevalence of mycobacterial infection in this population. Without sputum smear and culture results, we could not be confident of radiologic differentiation between silicosis and pulmonary TB. Some participants had past physician misdiagnoses of TB before physicians became aware of possible silica exposure in these patients. For this reason, we did not seek participant report of prior TB diagnosis and cannot evaluate any influence of mycobacterial infection on disease progression.
The strengths of the study lie in the comparability of measurements at the 4-year interval. The same technician used the same pulmonary function equipment to assess progression of respiratory impairment. Two of the three physicians providing ILO classifications of radiographs had previously read the 2007 chest radiographs and performed the 2011 readings independent of each other and without reference to the earlier reading or physiology. Vital status determination was robust, using national resources. Finally, the community-based recruitment of former sandblasters in 20076 allowed a composite picture of morbidity from silica exposure in many workshops, substantiating an industry-wide risk. Indeed, mortality was associated with the number of workplaces in which sandblasting had been performed, likely reflecting variable work conditions across the industry that may have motivated former sandblasters to move from poorer establishments to somewhat better ones.
Conclusions
Our results suggest that almost all former denim sandblasters will develop silicosis, and that progression of impairment to disability is expected over time. Thus, temporary compensation is insufficient in Turkey, and global measures to prevent silicosis of workers in this industry are needed.
Acknowledgments
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
Other contributions: The authors thank the American Thoracic Society’s Methods in Epidemiologic, Clinical and Operations Research Program. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the US National Institute for Occupational Safety and Health.
ABBREVIATIONS
- ILO
International Labor Organization
Footnotes
Author contributions: M. A. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. M. A., O. A., E. Y. U., A. K., and F. A. contributed to study design; M. A., O. A., E. Y. U., A. K., F. A., M. G., and K. K. contributed to data analysis and writing the manuscript; M. A., F. A., M. G., and K. K. contributed to revising the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
References
- 1.Akgun M, Gorguner M, Meral M, et al. Silicosis caused by sandblasting of jeans in Turkey: a report of two concomitant cases. J Occup Health. 2005;47(4):346–349. doi: 10.1539/joh.47.346. [DOI] [PubMed] [Google Scholar]
- 2.Gur A, Kiyik M, Kilic L, et al. Silicosis in denim sandblasting textile workers (two case reports) Eur Respir J. 2005;26(suppl 49):147s. [Google Scholar]
- 3.Akgun M, Mirici A, Ucar EY, Kantarci M, Araz O, Gorguner M. Silicosis in Turkish denim sandblasters. Occup Med (Lond) 2006;56(8):554–558. doi: 10.1093/occmed/kql094. [DOI] [PubMed] [Google Scholar]
- 4.Cimrin A. ‘Silicosis’ over again; causes and responsibilities. Tuberk Toraks. 2007;55(1):118–122. [PubMed] [Google Scholar]
- 5.Sahbaz S, Inönü H, Ocal S, et al. Denim sandblasting and silicosis two new subsequent cases in Turkey. Tuberk Toraks. 2007;55(1):87–91. [PubMed] [Google Scholar]
- 6.Akgun M, Araz O, Akkurt I, et al. An epidemic of silicosis among former denim sandblasters. Eur Respir J. 2008;32(5):1295–1303. doi: 10.1183/09031936.00093507. [DOI] [PubMed] [Google Scholar]
- 7.Yilmaz S, Bogatekin G, Senyigit A, Buyukbayram H, Senyigit A. Silicosis due to denim sandblasting: four cases. Turkiye Klinikleri J Med Sci. 2009;29(3):765–770. [Google Scholar]
- 8.International Labour Office (ILO) Guidelines for the Use of the ILO International Classification of Radiographs of Pneumoconioses. Revised edition, 2000. International Labour Office; Geneva, Switzerland: 2000. ILO Occupational Safety and Health Series No. 22. [Google Scholar]
- 9.Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Official Statement of the European Respiratory Society. Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, European Community for Steel and Coal. Official statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:5–40. [PubMed] [Google Scholar]
- 10.Cottin V. Changing the idiopathic pulmonary fibrosis treatment approach and improving patient outcomes. Eur Respir Rev. 2012;21(124):161–167. doi: 10.1183/09059180.00001112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taniguchi H, Ebina M, Kondoh Y, et al. Pirfenidone Clinical Study Group in Japan. Pirfenidone in idiopathic pulmonary fibrosis. Eur Respir J. 2010;35(4):821–829. doi: 10.1183/09031936.00005209. [DOI] [PubMed] [Google Scholar]
- 12.Bakan ND, Özkan G, Çamsari G, et al. Silicosis in denim sandblasters. Chest. 2011;140(5):1300–1304. doi: 10.1378/chest.10-1856. [DOI] [PubMed] [Google Scholar]
- 13.Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease. New lessons from old exposure. Am J Respir Crit Care Med. 2013;187(11):1178–1185. doi: 10.1164/rccm.201301-0042CI. [DOI] [PubMed] [Google Scholar]
- 14.Laney AS, Petsonk EL, Attfield MD. Pneumoconiosis among underground bituminous coal miners in the United States: is silicosis becoming more frequent? Occup Environ Med. 2010;67(10):652–656. doi: 10.1136/oem.2009.047126. [DOI] [PubMed] [Google Scholar]
- 15.Carneiro AP, Barreto SM, Siqueira AL, Cavariani F, Forastiere F. Continued exposure to silica after diagnosis of silicosis in Brazilian gold miners. Am J Ind Med. 2006;49(10):811–818. doi: 10.1002/ajim.20379. [DOI] [PubMed] [Google Scholar]
- 16.Kreiss K, Zhen B. Risk of silicosis in a Colorado mining community. Am J Ind Med. 1996;30(5):529–539. doi: 10.1002/(SICI)1097-0274(199611)30:5<529::AID-AJIM2>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 17.Yoruk O, Ates O, Araz O, et al. The effects of silica exposure on upper airways and eyes in denim sandblasters. Rhinology. 2008;46(4):328–333. [PubMed] [Google Scholar]
- 18.Aydin Y, Turkyilmaz A, İntepe YS, Eroglu A. Simultaneous bilateral spontaneous pneumothorax: a rare emergency clinical condition. Eurasian J Med. 2010;42:5–8. doi: 10.5152/eajm.2010.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaynar H, Aydın Y, Akgün M, Türkyılmaz A, Eroğlu A. Pneumothorax in the cases with silicosis due to denim sandblasting. Türk Göğüs Kalp Damar Cerrahisi Dergisi. 2012;20(2):291–294. [Google Scholar]
- 20.Ozden K, Araz O, Yilmazel Ucar E, Alper F, Akgun M. Co-existence of tuberculous meningitis and pulmonary tuberculosis in a denim sandblaster. Eurasian J Med. 2012;44:54–57. doi: 10.5152/eajm.2012.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yildiz T, Eşsizoğlu A, Onal S, et al. Quality of life, depression and anxiety in young male patients with silicosis due to denim sandblasting. Tuberk Toraks. 2011;59(2):120–125. doi: 10.5578/tt.1606. [DOI] [PubMed] [Google Scholar]
- 22.Sunal A, Sunal O, Yasin F. A comparison of workers employed in hazardous job in terms of job satisfaction, perceived job risk and stress: Turkish jean sandblasting workers, dock workers, factory workers and miners. Soc Indic Res. 2011;102(2):265–273. [Google Scholar]
- 23.Helvaci A, Meydan B, Akin O, et al. A single lung transplantation for silicosis: the first successful lung transplantation case in Turkey. Türk Göğüs Kalp Damar Cerrahisi Dergisi. 2011;19(3):455–462. [Google Scholar]
- 24.Uzunoğlu ÖB, Özkara Ş , Ökmen M, Aritürk O, Tüzün D, Arantaş K. Determining silicosis patients without insurance with temporary law. Turkish Thoracic J. 2013;14(2 suppl 1):0916. [Google Scholar]
- 25.Hobson J. To die for? The health and safety of fast fashion. Occup Med (Lond) 2013;63(5):317–319. doi: 10.1093/occmed/kqt079. [DOI] [PubMed] [Google Scholar]