Abstract
Therapeutic nanoparticles (TNPs) aim to deliver drugs more safely and effectively to cancers, yet clinical results have been unpredictable owing to limited in vivo understanding. Here we use single-cell imaging of intratumoral TNP pharmacokinetics and pharmacodynamics to better comprehend their heterogeneous behavior. Model TNPs comprised of a fluorescent platinum(IV) pro-drug and a clinically-tested polymer platform (PLGA-b-PEG) promote long drug circulation and alter accumulation by directing cellular uptake toward tumor associated macrophages (TAMs). Simultaneous imaging of TNP vehicle, its drug payload, and single-cell DNA damage response reveals that TAMs serve as a local drug depot that accumulates significant vehicle from which DNA damaging Pt payload gradually releases to neighboring tumor cells. Correspondingly, TAM depletion reduces intratumoral TNP accumulation and efficacy. Thus, nanotherapeutics co-opt TAMs for drug delivery, which has implications for TNP design and for selecting patients into trials.
INTRODUCTION
Approximately half of all cancer patients who receive chemotherapy are treated with one of three clinically approved platinum (Pt) drugs — cisplatin, carboplatin, and oxaliplatin1. These Pt compounds are first-line agents in ovarian, lung, head and neck and testicular cancers, among others, and development of combination therapies using Pt compounds is an active area of research2. Unfortunately, most cancers either exhibit intrinsic Pt resistance or ultimately develop resistance to treatment through mechanisms including reduced drug uptake, altered cellular metabolism, increased DNA repair, chemoprotective niche formation, and/or activation of oncogenic and anti-apoptotic pathways3. Dose escalation and combination drug regimens help overcome resistance. However, Pt-related toxic side-effects including neurotoxicity and nephrotoxicity limit some of these approaches, indicating the need for new strategies.
To circumvent these problems, specialized drug-delivery mechanisms such as nanoparticles (NPs) have been introduced to enhance local drug accumulation in tumors while simultaneously mitigating systemic toxicities4,5. Non-encapsulated Pt compounds in particular are often plagued by poor pharmacokinetic (PK) properties. They generally must be intravenously administered over a prolonged period (sometimes over 24 hr) because promiscuous Pt reactivity causes side effects and the covalent binding to plasma proteins such as albumin consequently neutralizing its activity. Recent work has demonstrated the possibility of using NPs to encapsulate Pt pro-drugs, thereby i) extending the circulating half-life of the unreacted Pt compound and enabling controlled drug release6; ii) facilitating precisely engineered Pt-based combination therapies through co-encapsulation with additional drugs7 (or siRNA treatments8); iii) enabling the administration of more lipophilic and newer-generation Pt compounds9 and iv) modifying tissue distribution and enhancing intratumoral accumulation6,8. The last is thought to occur through enhanced permeability and retention (EPR) effects and has been termed “passive NP targeting” 10. In theory, enhanced permeability of the abnormal tumor microvasculature (TMV) should allow TNPs to enter the tumor interstitial space, while suppressed lymphatic filtration and increased cellular uptake should allow them to stay there11. Although therapeutic nanoparticles (TNPs) of Pt-based anticancer agents have advanced to clinical trials12,13, results have been mixed, presumably due to heterogeneous EPR effects in different tumors combined with limited experimental data from patients on the effectiveness of this mechanism as related to enhanced drug accumulation14. Furthermore, the inter-related in vivo pharmacokinetics and pharmacodynamics (PK/PD) of TNPs are more difficult to understand than those of the unencapsulated drug. TNP drug delivery is inherently a multi-step process, defined by PK of the TNP vehicle, drug release dynamics that may change depending on the in vivo environmental context, and PK of the Pt payload itself. Little experimental evidence exists that describes how this multi-step drug delivery sequence performs in vivo and within tumors, despite its critical importance to overall therapeutic outcome. This lack of understanding clearly represents a bottleneck in the design and development of more efficacious therapies.
Here we use high-resolution microscopic imaging in live tumor-bearing mice to test the hypothesis that therapeutic nano-encapsulation not only affects traditional bulk PK properties, but also significantly influences heterogeneous drug uptake and response at the single-cell level within tumors15,16. We engineer a platform that for the first time allows simultaneous imaging of both a ~100-nm TNP vehicle as well as its Pt payload, in addition to monitoring DNA damage at the single cell level in real time. As expected, our results show that nano-encapsulated Pt exhibits a longer circulating half-life than traditional unencapsulated Pt compounds. However, we quite unexpectedly find that TNP accumulate at high levels within tumor-associated macrophages (TAMs), and that TAMs serve as “cellular drug reservoirs”. Indeed, TAMs release the Pt payload into neighboring tumor cells over time. Depletion of macrophages significantly decreases intratumoral Pt accumulation and correspondingly increases tumor growth. Overall, this work establishes a paradigm for nanoparticle drug delivery based on the principle that TAMs can sequester TNP payload and gradually release it into the surrounding tissue, thereby serving as “drug depots.”
RESULTS
Dual imaging shows congruent vehicle and payload kinetics
For clinical applicability and generalizability, TNPs in this study were designed to incorporate desirable properties of previously described polymeric nano-formulations that have entered clinical trials5, especially those of materials that have received FDA approval. TNPs were formulated by combining three compounds (compounds 1-3, Fig. 1A) via nano-precipitation, using spectrally complementary derivatives of BODIPYs as ideal fluorophores for efficient nano-encapsulation that convey lipophilicity and robust in vivo imaging arising from in vivo structural stability, environmentally robust fluorescence, high brightness, and high photostability15,17-19. Compound 3 (PLGA-b-PEG) self-assembles to form the hydrophobic PLGA core of the nanoparticle and hydrophilic PEG outer shell. For the cytotoxic payload, we used a novel Pt(IV) pro-drug (c,c,t-Pt(NH3)2Cl2(hexadecylcarbamate)[4-((2-(4,4-difluoro-1,3,5,7-tetramethyl-4-dora-3a,4adiaza-s-Indacene)ethyl)amino)-4-oxobutanoate]) with a C16 aliphatic carbon chain and a BODIPY (λex = 498 nm, λem = 543 nm; Supplementary Fig. 1a) as the two lipophilic ligands axially coordinated to the Pt(IV) center. Nanoparticles were similar in size (135 ± 1 nm; S.E.M. across n=12; Supplementary Fig. 1b-c), polydispersity (PDI = 0.18 ± 0.01; S.E.M. across n=12), and drug release rates (t1/2 release = 15 hr; n=2; Supplementary Fig. 1d) compared to previously published Pt(IV) nano-formulations6,8, and were stable in physiological saline (Supplementary Fig. 1e). Free carboxylic acid terminal groups on the PEG gave TNPs a slight negative charge (zeta-potential = −23 ± 1.4 mV; S.E.M. across n=4), which has been shown in some cases to benefit tumoral accumulation20-23 and mirrors TNPs in the clinic5. C16-Pt(IV) remains relatively stable in whole blood24. However, upon reduction to the active Pt(II) compound cisplatin, dissociated BODIPY increases fluorescence by seven-fold owing to loss of quenching by Pt(IV)(Supplementary Fig. 1f-g). BODIPY fluorescence thus serves as an effective indicator of both pro-drug delivery and activation. Overall, these properties enable clearly distinguishable imaging of both the TNP vehicle and its payload, in a stable and clinically relevant nano-formulation platform.
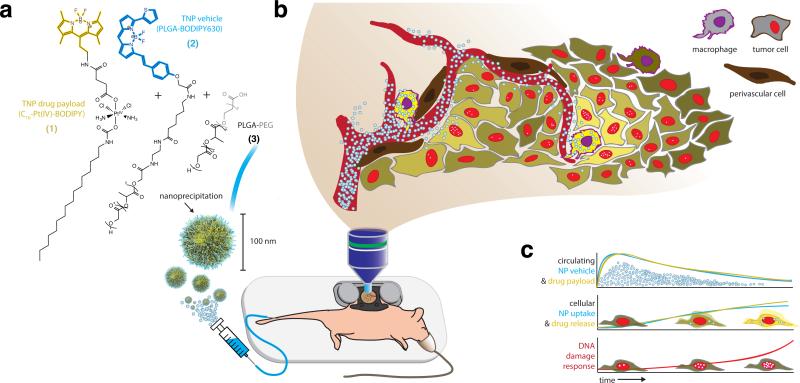
Figure 1. Overview schematic of intravital nanoparticle imaging for pharmacokinetic and pharmacodynamic analysis.
Nanoparticles (a) were injected by tail-vein catheter and imaged in real time within the tumor using a dorsal window chamber (b). Imaging results enable simultaneous monitoring of circulating pharmacokinetics within the TMV (c, top); single-cell uptake of the nanoparticle vehicle and its drug payload (c, middle); and DNA damage response in tumor cells, monitored by 53BP1 puncta formation (c, bottom).
We performed a series of in vitro experiments to characterize TNP behavior in tumor cell culture (Supplementary Fig. 2a). Co-localization studies with fluorescent compartmentally localized proteins showed that the TNP vehicle moved from early to late endosomes over the course of 24 hr (Supplementary Fig. 2b). Compared to the TNP vehicle, the TNP payload exhibited more diffuse intracellular localization, and co-localization peaked in the late endosome 24 hr post-treatment (Supplementary Fig. 2c). Payload fluorescence increased over time owing to Pt reduction and BODIPY de-quenching (Supplementary Fig. 2d). Yet despite this de-quenching, dose-response TNP treatment indicated that intracellular fluorescence correlates well with overall Pt uptake (R2 > 0.99) and resulting DNA damage (Supplementary Fig. 3), thereby validating the use of fluorescence as a surrogate marker of cellular payload content. Together, these results provide evidence that over the course of 24 hr, TNPs accumulate in endosomes and lysosomal compartments, where the Pt pro-drug is activated through reduction to form cisplatin.
TNPs exhibit long TMV half-life and perivascular cell uptake
We first used time-lapse intravital imaging to characterize PK within a xenograft tumor model often used for intravital studies (Fig. 1)15,25-27. Tumors were generated from subcutaneously implanted HT1080 cells expressing a fluorescently-tagged DNA damage response protein, 53BP1, which localizes to the nucleus28,29. TNPs reached the TMV within 10-15 minutes of intravenous injection, and at early time-points (t < 30 min) the vehicle and its payload exhibited strong co-localization within vessels (Fig. 2a; intravascular Pearson's correlation ρ = 0.8 ± 0.02, S.E.M. across n=4; Mander's M1 & M2 > 0.95). Both the vehicle and its payload showed initial vascular PK similar to each other (Fig. 2b; t1/2 vehicle = 55 ± 5 min; t1/2 payload = 61 ± 6 min; S.E.M. across n = 6), to previous studies using similar nano-formulations entering the clinic5,6,30, and to clinical nanoparticle formulations such as PEGylated liposomal doxorubicin (DOXIL; t1/2 initial < 5.2 hr in humans and 2 hr in rats31,32). Immediately as the TNPs reached the TMV, roughly 10% of the payload diffused into the surrounding tumor tissue. Such an initial burst of drug release was also observed in vitro (Supplementary Fig. 1d) and with similar previously described nano-formulations33,34, characterized by significantly faster release kinetics at initial phases followed by a later phase of slower release. Notably, pharmacokinetic imaging of BODIPY-labeled Pt compounds that were not nano-encapsulated revealed much more rapid vascular PK (t1/2 unencapsulated = 10 ± 5 min28). Therefore, despite an initial burst of Pt release seen both in vitro (Supplementary Fig. 1d) and in vivo (Fig. 2), nano-encapsulation conferred a relatively long circulation half-life.
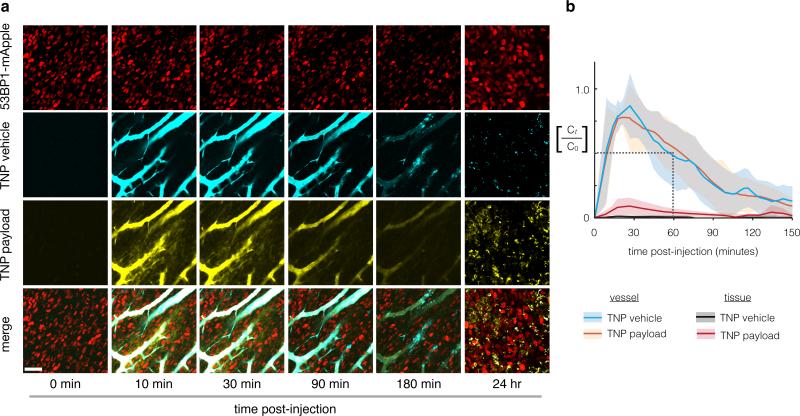
Figure 2. Pharmacokinetic analysis of nanoparticle shows extended microvasculature half-life and heterogeneous tissue accumulation.
(a) Nanoparticle concentrations are monitored (a) and quantified (b) using time-lapse confocal fluorescence microscopy in the dorsal window chamber model. Nanoencapsulation extends the TMV half-life to 55 min, a > 5-fold increase compared to unencapsulated Pt(II) compounds in the same animal model28. Scale bar = 50μm. Thick lines and shading denote means ± S.E.M. (n=6).
Over the course of several hours, TNPs moved from the TMV (t < 1 hr) specifically to peritumoral host cells (1 - 3 hr) adjacent to, or even extending processes into the TMV. Uptake of TNPs by tumor cells themselves occurred more gradually and to a lesser degree compared to these perivascular host cells. By 24 hr TNPs were undetectable in vessels and had accumulated primarily in a heterogeneous mix of tumor cells and host cells, with host-cell uptake characterized by high local accumulation within cell-sized (7 ± 1 μm; S.E.M. across n=4 tumors) diameters. At 24 hr post-injection, the TNP payload also co-localized with the TNP vehicle in these host cells (Pearson's correlation within tumor tissue: ρ = 0.7 ± 0.08; Mander's M1 & M2 > 0.6 ± 0.05; S.E.M. across n=4). Compared to the TNP vehicle, however, the payload accumulated more diffusely throughout the bulk tumor tissue, suggesting some payload release from the TNP vehicle (Supplementary Fig. 4a). We quantified these observations by measuring the coefficient of variation (CV) across cells within the tumor tissue (Supplementary Fig. 4b). The payloads exhibited > 40% decrease in CV compared to the TNP vehicle, indicating more homogeneous distribution. In contrast to TNPs, naked BODIPY-labeled Pt that was injected in the absence of an encapsulating NP vehicle showed a substantially more homogeneous distribution within tumor tissue, with little preferential accumulation in any particular cell type (Supplementary Fig. 4; 60% reduction in CV). In summary, these data show that i) nano-encapsulation enables a relatively long circulating half-life of the Pt(IV) pro-drug; ii) nano-encapsulation influences spatial distribution within the bulk tumor tissue, and iii) TNPs primarily accumulate in perivascular host cells and, to a lesser extent, tumor cells.
TNPs cause mitotic arrest and localized DNA damage
In addition to PK analysis, high-resolution intravital imaging allowed for simultaneous monitoring of the cellular response to TNPs at the molecular level. Fluorescently tagged 53BP1 is a key member of the non-homologous end-joining pathway that forms visible puncta at sites of DNA double-strand breaks28,35. Based on the hypothesis that treatment with a cisplatin pro-drug would lead to increased DNA damage in tumors cells, we imaged 53BP1 puncta in response to TNP and quantitated the DNA damage response across populations of individual tumor cells at various time points (Fig. 3a). The results show a dose- and time-dependent increase in the fraction of tumor cells exhibiting high levels of DNA damage (Fig. 3b). We next tested whether there was an observable relationship between local payload accumulation and resulting single-cell DNA damage response. We used automated 3D segmentation software to quantify TNP vehicle and payload accumulation within individual tumor nuclei, and correlated this information with DNA damage response in those cells. The results showed that cells exhibiting high levels of DNA damage also had a roughly 300% higher local payload concentration (Fig. 3c). Rather than TNP payload, local concentration of TNP vehicle also correlated with DNA damage, but to a lesser degree (Fig. 3c). DNA damage elicited by Pt treatment generally induces mitotic arrest in vitro24, but it has been difficult to directly observe this response in vivo, where anti-mitotics often behave much differently25. To determine TNP effects on cell growth, we used time-lapse intravital imaging to track individual tumor cells and mitotic events over the first 3 hr following TNP injection in the HT1080 model (Supplementary Fig. 5) and found that TNP indeed caused a substantial reduction in tumor cell division (Fig. 3d). To test generalizability in another tumor model, we next examined local drug accumulation and DNA damage in an orthotopic model of disseminated ovarian cancer (OVCA)36. Human A2780CP OVCA cells were intraperitoneally injected in nu/nu mice, and 6 weeks later (once palpable tumors and/or ascites had developed), animals received TNP treatment. The following day, tumors were excised and imaged for TNP accumulation and DNA damage. Imaging shows similar TNP localization patterns as observed with the HT1080 model (Fig. 4a). We also found similar statistically significant correlation between local TNP payload levels and tumor cell DNA damage (Fig. 4b). Taken together, these results demonstrate that TNPs elicit substantial DNA damage response activity and corresponding growth arrest in vivo. In both the subcutaneous and orthotopic OVCA tumor models, the correlation between local drug accumulation and DNA damage response implies that nanoparticle-mediated drug delivery plays a significant role in governing such pharmacodynamics.
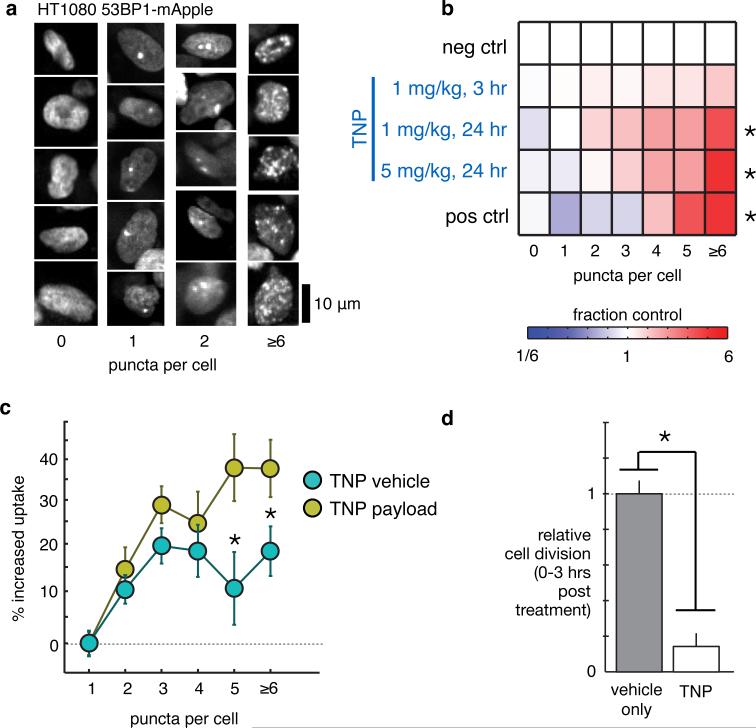
Figure 3. TNP causes mitotic arrest and DNA damage in a spatially defined dose-dependent manner.
(a) Example images of 53BP1 puncta, 24 hr post-treatment with 1 mg kg−1 TNP, scale bar 10 μm. (b) TNP treatment increases the fraction of cells exhibiting many 53BP1 puncta, measured across n≥3 animals and n>2000 cells (*p<0.01, two-tailed t-test). Pos. ctrl.: 24 hr supra-therapeutic cisplatin, 9 mg kg−1. (c) Heterogeneous local TNP vehicle and payload accumulation within 5 μm of single-cell nuclei correlate with corresponding DNA damage response in those cells (one-way ANOVA; n>6000 cells across n=5 animals; p<10−21 for both vehicle and payload); the local TNP payload correlates better with response compared to TNP vehicle (*p<0.05; two-tailed t-test). (d) Cell division events were quantified from time-lapse movies across n>1000 cells (*p=0.001; two-tailed t-test; n=3 animals). All dosages in mg of Pt. Data are means ± S.E.M.
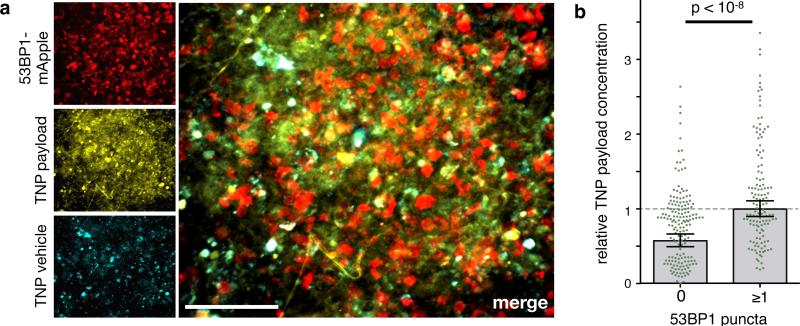
Figure 4. Local TNP payload accumulation correlates with DNA damage in OVCA.
(a) Single-cell DNA damage response correlates with local TNP payload levels in a model of disseminated metastatic OVCA. A2780CP OVCA cells were injected intraperitoneally; 6 weeks later, TNP was i.v. injected, and the following day intraperitoneal lesions were excised and imaged for DNA damage response (using 53BP1 puncta) and TNP uptake. Scale bar = 50μm. (b) OVCA cells exhibiting detectable DNA damage by 53BP1-puncta have higher TNP payload levels, compared to those without (*two-tailed t-test; S.E.M. across n=3 animals).
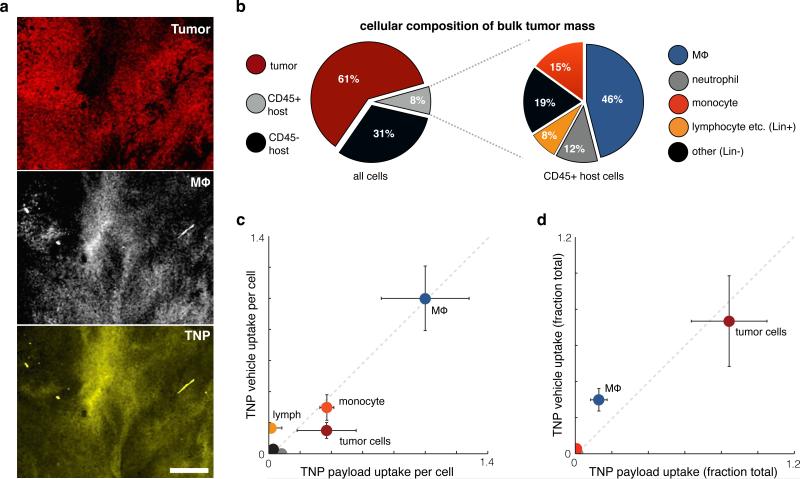
Identification of cell populations with drug in steady state
We next performed a combination of intravital imaging, flow cytometry, and histology studies to determine in which immunologically defined cell populations the TNP vehicle and its payload accumulated within the bulk tumor mass at 24 hr, after TNPs had largely cleared the circulation. With the same HT1080 xenograft model used in the previous imaging experiments, we labeled tumor-associated macrophages (TAMs) with a fluorescent dextran-coated nanoparticle15 and found significant TNP uptake in TAM-rich regions of the bulk tumor mass (Fig. 5a). For more detailed immunological examination, we next performed flow cytometry analysis of HT1080 tumors. Results show that tumor cells made up 61% of the bulk tumor; 31% of the cells within the bulk tumor were CD45- host cells (erythrocytes, tumor associated fibroblasts, endothelium, and others); and the remaining 8% were CD45+ leukocytes (Fig. 5b). TAMs made up the largest population of leukocytes within the bulk tumor and also accumulated the highest levels of both TNP vehicle and payload on a per-cell basis (Fig. 5c). Because tumor cells far outnumbered TAMs in the HT1080 xenograft model, the majority of TNP vehicle and payload within the bulk tumor still resided in tumor cells themselves (Fig. 5d). Nonetheless, even though TAMs comprised only 4% of cells within the total tumor mass, they accumulated more than 40% of the total injected TNPs relative to tumor cells, and 30% of the total TNP overall.
Figure 5. TNPs primarily accumulate in tumor cells and tumor-associated macrophages in steady state.
(a) Intravital imaging of subcutaneous HT1080-53BP1-mApple tumors 24 hr post-injection with TNP (payload shown in yellow). TAMs (white) were labeled by dextran-coated nanoparticles injected 24 hr prior. Scale bar = 100 μm. (b) Single-cell suspensions of the bulk tumor mass were immunostained and gated into various cell-populations, quantified here as fractions of the total number of cells analyzed. (c) Macrophages accumulate the most TNP per cell. Using flow cytometry, uptake of both the TNP vehicle and its payload were quantified by fluorescence for each of the cell populations shown in b, 24 hr post-injection. CD45- host cells, neutrophils, and “other” CD45+ leukocytes did not accumulate significant TNP vehicle or payload. Fluorescence values normalized to the average macrophage values, after subtracting background autofluorescence of each cell population measured from control-treated tumors. (d) Most TNP accumulates in tumor cells and macrophages within the bulk tumor mass. TNP uptake measurements from c were weighted against the relative prevalence of each cell population in b to calculate the total fraction of TNP uptake within each cell population. For b-d, error bars denote standard error (n≥4).
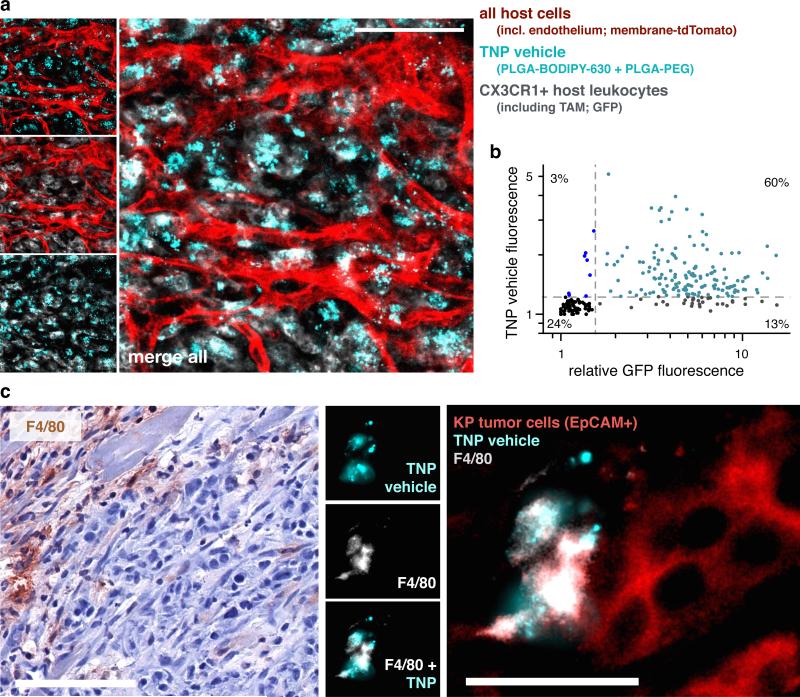
To directly visualize genetically-defined tumor associated host leukocytes, we imaged TNP vehicle uptake in tumor-bearing fractalkine Cx3cr1GFP/+ reporter mice, which are known to contain GFP+ macrophages37. In this model, KRAS mutant p53−/− (KP) cells derived from autochthonous lung tumors38 were subcutaneously implanted into immunocompetent Cx3cr1GFP/+ reporter mice, and TNP vehicle (without the green-fluorescent payload) was intravenously administered. The vast majority of TNP vehicle accumulated within these GFP+ host leukocytes, especially near TMV (Fig. 6a-b). Using the above described KP lung cancer and intraperitoneal OVCA xenografts, we confirmed by histology that high levels of TNP vehicle accumulate in F4/80+ host phagocytes in these disease models as well (Fig. 6c; Supplementary Fig. 6). These analyses ultimately corroborate results from the intravital imaging data showing uptake of TNPs in tumor cells but also host cells, which are confirmed here as TAMs.
Figure 6. Tumor-associated CX3CR1+ and F4/80+ host phagocytes accumulate TNP vehicle in a syngeneic model of lung cancer.
Kras mutant p53−/− (KP) lung cancer cells were subcutaneously implanted into Cx3cr1GFP/+ reporter mice for directly visualizing GFP+ monocytes, dendritic cells, and TAMs. Tumor-adjacent stromal regions were imaged 24 hr following i.v. injection with TNP vehicle. Reporter mice expressed membrane-anchored tdTomato in all host cells, most visibly here with endothelium. Scale bar = 50μm. (b) Fluorescence intensities of GFP and TNP vehicle were quantified across single-cells based on a, showing most stromal cells that accumulate TNP vehicle were also GFP+ (n=4 animals, n=250 cells). (c) Histological analysis of F4/80+ host phagocytes, 24 hr post-injection with TNP vehicle. Immunohistochemistry (left) shows tumors stained with hematoxylin and F4/80 (brown ; scale bar = 100μm), and corresponds with immunofluorescence (right) showing F4/80+ host phagocytes, EpCAM+ KP tumor cells, and local accumulation of TNP vehicle (scale bar = 25 μm). F4/80 labels a subset of GFP+ cells in Cx3cr1GFP/+ reporter mice37 (namely, macrophages).
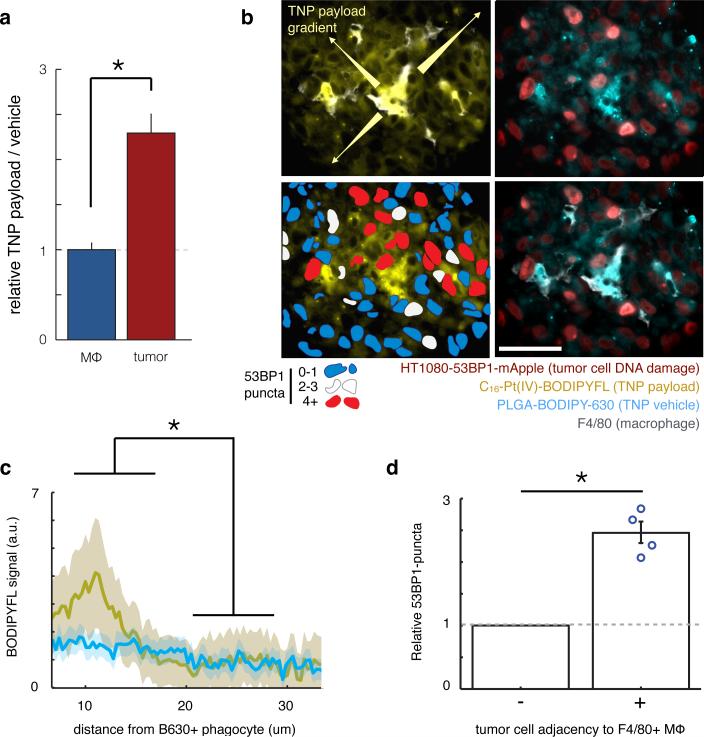
TNP payload spatially redistributes from TAMs to tumor cells
Based on intravital imaging evidence showing that the Pt(IV)-payload was more diffusely distributed within tumor tissue compared to its TNP vehicle (Supplementary Fig. 4), we next quantified the extent of payload redistribution and its effect on drug response. Using flow-cytometry data, we confirmed that tumor cells exhibited more than twice the amount of payload accumulation as a ratio of vehicle accumulation, compared to TAMs (Fig. 7a), thereby suggesting that payload may transfer from TAMs to tumor cells. We hypothesized that local payload release from TAMs into neighboring tumor cells would lead to elevated payload concentration in these tumor cells, which would in turn enhance DNA damage. By histology we also measured greater than threefold elevated payload concentrations within roughly one cell-length (15 μm) of TAMs (Fig. 7b-c), and analysis of intravital imaging data provided further evidence that relevant payload concentration gradients occur over length-scales of < 25 μm (Supplementary Fig. 7a). One explanation for these observations is that TAMs induce neighboring tumor cells to take up more TNP directly; however, the TNP vehicle itself was not similarly elevated in the same neighboring region (Fig. 7c). Tumor cells within the same phagocyte-neighboring region also exhibited higher DNA damage on average, as determined by histology (Fig. 7d) and supported by corroborating intravital imaging analysis (Supplementary Fig. 7b). These analyses cumulatively show local payload redistribution from TAMs to neighboring tumor cells exhibiting elevated DNA damage.
Figure 7. DNA-damaging TNP payload redistributes from TAMs to neighboring tumor cells.
(a) Compared to TAMs, tumor cells exhibit elevated TNP payload as a fraction of TNP vehicle (measured by flow-cytometry), suggesting payload redistribution (p=0.005; two-tailed t-test; n≥4 per group). (b) Example immunofluorescence showing TNP vehicle uptake by F4/80+ macrophages and payload diffusion into surrounding tumor tissue. In lower left panel, red pseudo-color indicates tumor cells with high levels of 53BP1 puncta. Of note, these cells are also adjacent to F4/80+ macrophages and contain elevated TNP payload. Scale bar = 50 μm. (c) By histological analysis, TNP payload but not vehicle is present at elevated levels within a 15-μm range of host phagocytes (p=0.047, two-tailed t-test; n=3 animals). (d) By histological analysis, tumor cells immediately adjacent to F4/80+ macrophages exhibit elevated DNA damage response, compared to average DNA damage response seen in non-adjacent tumor cells for each of 4 animals shown by individual data points (p=0.007; matched two-tailed t-test).
We next performed a series of in vitro experiments to directly test whether macrophages could release functional, DNA-damaging TNP payload into their surrounding environment. Similar to in vivo observations, we found that in vitro macrophagesaccumulated TNPs more rapidly and to a greater degree than tumor cells (Supplementary Fig. 8a). Once taken up by macrophages, Pt-payload was released at high levels into the extracellular supernatant. In fact, over the course of 24 hr, more Pt was found in the supernatant than in the macrophages themselves (Supplementary Fig. 8b-c). The Pt-containing macrophage supernatant was both DNA damaging (Supplementary Fig. 8d) and cytotoxic (Supplementary Fig. 8e). In contrast, supernatant from macrophages treated with unencapsulated cisplatin at concentrations ranging from 1-300 μM was not cytotoxic to tumor cells (Supplementary Fig. 8e). For supernatant from TNP-treated macrophages, filtration with molecular-weight cutoff filters (3 kDa and 100 kDa) did not reduce its potency, which indicated that cytotoxic effects were independent of macrophage-derived cytokines or other signaling proteins (Supplementary Fig. 8f). In addition, Pt-containing macrophage supernatant exhibited 50% inhibitory effect on tumor cell viability/cytotoxicity at Pt concentrations of 1.5 ± 0.5 μM (S.E.M. across n= 3) within the macrophage supernatant (Supplementary Fig. 7e), which is comparable to the potency of the Pt-payload when TNP was directly applied to tumor cells (IC50 = 1.7 ± 0.02 μM; S.E.M. across n=2; Supplementary Table 1). Taken together, these combined in vitro and in vivo data further confirmed that TAMs can serve as drug depots that accumulate high levels of TNPs and then release their DNA-damaging cytotoxic payload to the surrounding tumor tissue.
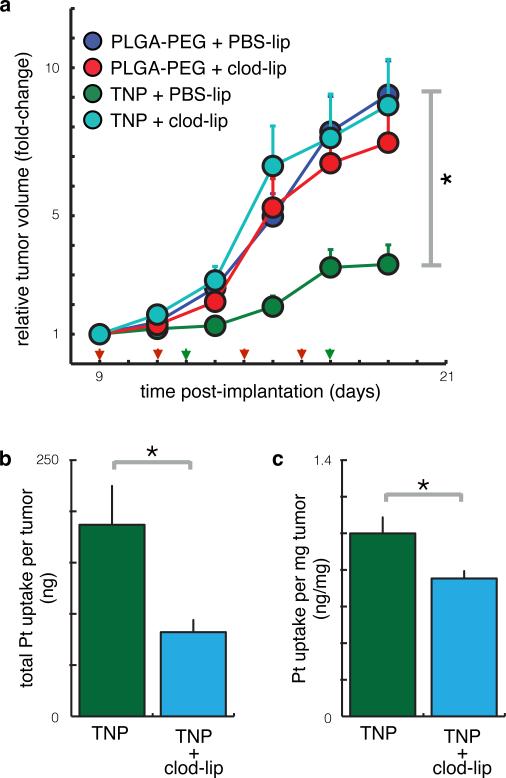
TAM depletion reduces TNP accumulation and efficacy
Finally, we tested whether TAM depletion would reduce the therapeutic efficacy of TNP in cancers. Macrophages were systemically depleted by pre-treatment with clodronate liposomes (clod-lip) 39 before TNP injection. In this tumor model, macrophage depletion itself had no detectable impact on tumor growth (p=0.2; two-tailed two-way ANOVA; n=38 mice). However, it substantially reduced the degree to which TNP treatment was able to slow tumor growth (Fig. 8a). Direct measurement of intratumoral TNP accumulation confirmed that macrophages play a key role in mediating drug delivery: macrophage-depleted tumors exhibited both lower total intratumoral Pt (Fig. 8b) and a lower concentration of Pt (Fig. 8c) compared to macrophage-containing tumors, 24 hr post-administration of TNP, at which time no TNP remained circulating in the TMV of any tumor. The 25% decrease in Pt concentration (from 5 μM to 3.8 μM; Fig. 8c after converting to molarity) correlates well with the flow cytometry-based estimate that TAMs accumulate 30% of the total intratumoral TNP. It also correlates with the observation that unencapsulated Pt exhibits 37% lower intratumoral accumulation than nano-encapsulated Pt (Supplementary Table 1)8. This decrease disproportionately impacted TNP effects on tumor growth, probably because intratumoral Pt concentrations were near the threshold at which HT1080 tumor cells respond (in vitro IC50 = 3.7 ± 0.1 μM for unencapsulated Pt(IV) payload; S.E.M. across n=2). TNP clearance kinetics, TMV leakiness, and other EPR factors all may influence drug accumulation within the tumor; nonetheless, the experiments here show that all things being equal, macrophage uptake substantially contributes both to the delivery of TNP to the tumor and, consequently, to the therapeutic impact on tumor growth.
Figure 8. Macrophage depletion reduces intratumoral accumulation and efficacy of TNP.
(a) TNP reduces tumor growth in a macrophage-dependent manner. Animals were treated with TNP (green arrows) and clodronate liposomes (red arrows) to systemically deplete macrophages. TNP significantly reduced tumor growth (p=0.039) while clodronate liposomes did not (p=0.21); however, clodronate liposomes significantly reduced the impact of TNP (p=0.039 interaction term; all p-values used the two-tailed two-way ANOVA, total n=38 animals). (b-c) Macrophage depletion using liposomal clodronate reduced the total amount (b) and concentration (c) of intratumoral Pt, measured using AAS (p=0.02 and p=0.03 respectively, two-tailed t-test; total n=22).
Liver TNP uptake is well tolerated and blocks metastasis
Given our evidence for TAMs in mediating TNP delivery, we next investigated TNP effects in the liver, which is a prominent site of the mononuclear phagocyte system and is known to accumulate NPs6. Despite substantial liver accumulation (Supplementary Fig. 9a), TNPs did not significantly impact animal body weight (Supplementary Fig. 9b) and did not cause changes outside of the normal range in blood markers of renal or liver toxicity at the therapeutic dose (Supplementary Fig. 9c). Within the bone marrow, another important site of the mononuclear phagocyte system, TNP payload concentrations were much lower (Supplementary Fig. 9d-e). While clinically-relevant doses of un-encapsulated cisplatin caused a significant reduction in the number of nucleated cells in the bone marrow, TNP effects were not statistically significant (Supplementary Fig. 9f-g). Overall, these results demonstrate a positive safety profile despite liver accumulation.
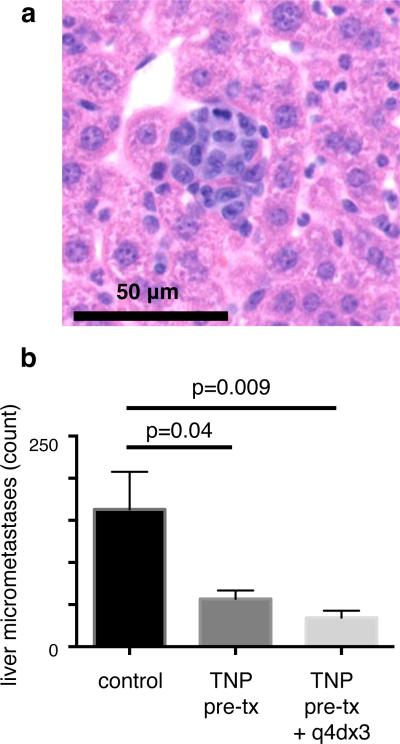
We next tested whether TNP treatment could block the development of liver micro-metastases in a model of hematogenous breast cancer dissemination. 4T1 murine breast cancer cells were intravenously injected into immunocompetent balb/c mice, thus forming tumors in the liver, lung, and other organs. To primarily deliver TNPs to host phagocytes rather than tumor cells, we pre-treated naive mice with TNPs, waited 6 hr for a majority of the drug to clear circulation, and then injected a single-cell suspension of 4T1 cells. Two weeks later, livers were excised and analyzed by histology for tumor burden. Results show that pre-treatment with TNPs reduced development of micro-metastases by over 65%, and repeated TNP doses caused a slightly greater reduction of 80% (Fig. 9). No treatment impacted tumor burden in the lung (two-tailed t-test; n≥5). Taken together, these results demonstrate that TNPs can safely accumulate in host cells of the liver, thus allowing TNP payload to block the development of local metastases from hematogenously disseminated cancer cells.
Figure 9. TNP delivery to the liver blocks development of micro-metastases.
(a) Representative liver micro-metastasis, 2 weeks after i.v. injection of 4T1 breast cancer cells (H&E staining of FFPE tissue section). (b) TNP reduces liver micro-metastasis development in the 4T1 model of hematogenous metastasis (*two-tailed t-test; shown as mean ± S.E.M.; n ≥ 5). To initially deliver TNPs to host phagocytes (rather than tumor cells), TNPs were i.v. administered (1 mg kg−1) 6 hr before i.v. injection of 4T1 cancer cells, such that TNP largely cleared the circulation at the time of cancer cell administration. 1/3 of the cohort received subsequent TNP treatments as indicated.
DISCUSSION
This work presents a new paradigm for employing TAMs as “drug depots” for local delivery of nanotherapeutics to neighboring tumor cells. Key to the development of this model was new technology for the in vivo visualization of multi-step drug delivery and the corresponding single-cell pharmacodynamic response at high spatiotemporal resolution. With this approach we demonstrated that nano-encapsulation allows for long circulating drug half-life and guides the delivery of drugs to TAMs, from which their functional cytotoxic payloads locally transfer to and damage neighboring tumor cells. This paradigm most likely extends to other nano-encapsulated therapeutics and non-cancer disease indications in which macrophages accumulate near the target tissue. The clinically tested TNP platform used here13 can encapsulate other therapeutics including paclitaxel, doxorubicin, and irinotecan, which exhibit release rates similar to the Pt(IV) payload5-7. Of relevance is that local macrophage accumulation occurs in multiple diseases including type I diabetes40, rheumatoid arthritis41, endometriosis42, and cardiovascular diseases such as atherosclerosis and myocardial infarction43,44. The imaging approach we describe may thus apply to these other pathologies, especially where intravital microscopy has already been successfully used45. Although macrophages themselves are often pharmacological targets46, concomitant drug delivery to surrounding tissue may be advantageous47. Overall, the drug delivery paradigm presented here, along with the complementary imaging technology, portend broad applicability to other TNP strategies and disease indications.
Tumor associated macrophages have been extensively studied and targeted for their roles in disease development, progression, and therapeutic response47,48. Nonetheless, TAMs have received less consideration in the context of novel nanotherapeutics entering the clinic. Because of their secretion of growth factors, cytokines, and proteases, TAMs have been implicated in supporting disease progression by enhancing angiogenesis, metastasis, and cancer stem cell niche formation, all while suppressing anti-cancer immune responses. In multiple indications, high TAM accumulation at tumor sites correlates with poor prognosis49,50. Although TAM-mediated tumor neo-vascularization can increase vascular leakage and corresponding therapeutic delivery51, TAMs also provide chemoprotective cues to tumor cells, and TAM infiltration following chemotherapy correlates with poor treatment response51,52. For these reasons, therapeutic TAM killing or TAM re-polarization into an anti-cancer phenotype represents an active area of development, for example by targeting colony stimulating factor 1 receptor (CSF1R)53-55. In several examples, blocking leukocyte infiltration via CSF1R inhibition or chemokine receptor type 2 (CCR2) ablation enhances response to chemotherapeutics including cisplatin51. However, very little experimental data describes how TAM depletion affects the response to nanotherapeutic formulations, and evidence presented here suggests that complete TAM elimination would be undesirable in such contexts.
In contrast to previous reports that focus chiefly on traditional unencapsulated cytotoxic therapies, we show here that TAMs are critical mediators of drug action for nano-encapsulated therapeutics. TAMs and other leukocytes are implicated in taking up a wide range of clinically relevant nanotherapeutics, including liposomal56, polymeric57, and albumin-binding58 formulations. Nonetheless, in the past, imaging capabilities have generally not allowed detailed insight into the kinetics of drug uptake, payload redistribution, and corresponding pharmacodynamic responses at the single-cell or subcellular level to be determined for these compounds56,59. Compared to polymeric NPs such as those used here, liposomal formulations generally are associated with slower payload release and decreased payload bioavailability, and there is little evidence that doxorubicin is released from TAMs after they have taken up liposomes56,60. In fact, previous failures to develop liposomal cisplatin have been attributed to insufficiently fast drug release12. By contrast, polymeric nano-formulations can be designed to release payloads at prescribed rates5 and even at programmed environmental (e.g., pH) conditions61. Here, TNPs were engineered to release their payload over a slightly longer time scale (50% drug release at 15 hr; Supplementary Fig. 1d) relative to the observed pharmacokinetics of cellular uptake (TAM uptake observable at 1 hr and gradually increases by 24 hr), and therefore were ideally suited for TAM-mediated drug delivery as described herein. Overall, this work builds on previous studies that implicate macrophages in TNP uptake; however, through engineered drug release and fluorescence imaging strategies we demonstrate how the TNP payload can redistribute to neighboring tumor cells at the site of local TAM accumulation in a therapeutically beneficial manner.
The results presented have implications for future development and clinical use of TNPs. Given that TNPs accumulate in TAMs at high levels, it follows that one criterion for selecting patients into TNP trials may be the degree of peritumoral TAM content, which can be assessed by MRI using clinically approved nanoparticle contrast agents such as ferumoxytol (Feraheme®)62 or experimental theranostics including drug-conjugated ferumoxytol derivatives63,64. TAM content is especially important in the context of therapies that either increase or decrease infiltration of macrophages to tumors. For instance, doxorubicin51 and CD40 agonist antibodies65 enhance macrophage infiltration, whereas CSF1R inhibitors55 and the clinically approved trabectedin66 decrease TAM accumulation. The paradigm of TAM-mediated drug delivery presented offers a compelling case for consideration of competing drug effects on TAM recruitment, and highlights the potential use of TNP vehicles for more efficient (via improved kinetics and/or targeting subsets) targeting of both TAMs and their neighboring tumor cells.
Methods
C16-Pt(IV)-BODIPY synthesis
A 0.2 mL DMF solution of cis,cis,trans-[Pt(NH3)2Cl2(O2CCH2CH2COOH)(OCONH(CH2)15CH3)] (15 mg, 21 μmol) and HATU (8 mg, 21 μmol) was stirred at R.T. for 15 min. To the clear solution was added a 0.4 mL DMF suspension of the amino BODIPY (4,4-difluoro-5,7-di- methyl-4-bora-3a,4a-daizas-indacene) (6 mg, 21 μmol), and the orange suspension was stirred at R.T. for 30 min. Finally, a 4 μL portion of DIPEA was added to the mixture and the resulting orange solution was stirred at R.T. for 5 hr. A 5 mL volume of saturated aqueous NaCl was added to the reaction mixture and a red precipitate was obtained. The precipitate was washed with 3 × 3 mL water. The resulting orange solid was dried in the vacuum overnight and the product was isolated by silica chromatography (acetone, Rf = 0.5). Yield: 7 mg (30 %). 1H NMR (400 MHz, acetone-d6): δ: 7.73 (s, 1H, NHCH2CH2-BODIPY), 6.54 (m, 6H, NH3), 6.18 (s, 1H, BODIPY), 5.80 (s, 1H, NHcarbamate), 3.42 (m, 2H, NHCH2CH2-BODIPY), 3.29 (m, 2H, NHCH2CH2-BODIPY), 3.01 (m, 2H, CH2(CH2)14CH3), 2.45 (s, 6H, BODIPY), 2.21 (m, 10H, BODIPY, succinate), 1.20 (m, 28H, CH (CH2)14CH3), 0.8(t, 3H, CH2(CH2)14CH3). 13C NMR (100 MHz, DMSO-d6): δ: 180.4, 172.1, 164.4, 153.9, 143.0, 142.0, 131.5, 122.3, 41.5, 40.9, 31.9, 31.8, 30.3, 29.5, 29.4, 29.2, 29.1, 22.6, 16.5, 14.6, 14.4. 195Pt NMR (86 MHz, DMSO-d6): δ: 1240.1. HRESI-MS (Positive mode) for C36H63BCl2F2N6O5Pt: m/z [M - H]− calcd: 975.4020; obsd: 975.4001.
Polymer materials
Unless otherwise stated, all chemical reagents were purchased from Sigma-Aldrich. PLGA(55:45 lactide:glycolide)35.2kDa-PEG3.5kDa was purchased from Advanced Polymer Materials, Inc. (Montreal, QC, Canada; Cat. #13-01-CX-55/45-35.2k/3.5k; lot 14-02-169). From the vender, gel permeation chromatography (GPC) indicated Mn = 38.8 kDa, Mw = 58.8 kDa, and PI = 1.52. PEG weight fraction (8.7% ± 0.3%) and molecular weight were confirmed by 1H NMR peak integration values, which were also used to calculate the lactide:glycolide ratio. 1H NMR in CDCl3: δ (in ppm) 5.12-5.28 (m, (-OCH(CH3)CO)), 4.66-4.9 (m, (-OCH2COO-)), 3.64( s, -OCH2CH2O-), 1.52-1.62 (m, (-OCH(CH3)CO-). Differential scanning calorimetry (DSC) was performed (Q10; TA Instruments), heating from −60°C to 100°C at 10°C min−1, with no apparent crystallization or melting temperature (Tm); glass temperature (Tg) was observed at 39.5°C. BODIPY-630-NH2 (Life Technologies; 2.8 mg, 0.0046 mmol) was conjugated to PLGA(50:50 lactide:glycolide)30-60kDa (100mg, ca. 0.0023 mmol; Sigma) using previously published procedures26, by stirring at r.t. under Ar for 10 min, adding EDCI (4.4 mg, 0.023 mmol) and DMAP (2.8 mg, 0.023 mmol) in CH2Cl2 (0.5 mL), and stirring overnight. Polymer was precipitated in cold 1:1 MeOH:Et2O, centrifuged (2,700xg, 10 min) and repeatedly washed in minimal CH2Cl2, followed by MeOH:Et2O precipitation and centrifugation. The resulting blue precipitate was dried under vacuum.
Nanoparticle synthesis and characterization
TNPs were prepared by nano-precipitation. Briefly, the following reagents were dissolved in 50:50 v/v DMF:ACN at the indicated concentrations: PLGA-BODIPY-630 (0.17 mg mL−1), C16-Pt(IV)-BODIPY (0.17 mg mL−1), and PLGA-PEG (0.83 mg mL−1). The resulting solution was then mixed and added drop-wise to nuclease-free H2O while maintaining a ratio of 20:1 H2O to organic solvent. TNPs were stirred overnight and filtered through sterile 0.45 μm syringe filters (regenerated cellulose, 17 mm, Cole Palmer). The TNPs were concentrated by centrifugation using centrifugal filter units (Amicon; Millipore; MWCO 100KDa). The concentrated TNPs were washed twice with de-ionized H2O and re-suspended in 1 mL of nuclease-free H2O. TNPs were diluted 10 times in H2O and characterized by size using dynamic light scattering (DLS; Malvern Zetasizer). Zeta-potential was also measured by DLS in dI-H2O (−25 ± 2.5 mV) and phosphate buffered saline, pH 7.4 (−23 ± 1.4 mV). Although the buffered solution produced a slightly higher zeta-potential, measurements were not statistically different from each other (two-tailed t-test; α=0.05). The Pt concentration was determined by graphite furnace flameless atomic absorption spectroscopy (AAS). BODIPY-630 concentration was determined by a microplate fluorimeter after diluting TNPs in DMF and using pure BODIPY-630 for a standard curve. Transmission electron microscopy (TEM) experiments were performed on a JEOL 1011 electron microscope. The TEM sample was prepared by depositing 10 μL of TNPs (5 mg mL−1) onto a carbon-coated copper grid. The excess solution was blotted, and the grids were immersed in a solution of phosphotungstic acid stain. The stain was blotted, and the dried grids were immediately used for imaging. To characterize payload release from TNPs (Supplementary Fig. 1d), they were incubated in PBS at 37°C, filtered using 100 kDa MWCO centrifugal filters (Amicon; Millipore) at the indicated time-points and resuspended in fresh PBS. Filtrate was frozen for later analysis by AAS. After 72 hr, both the TNPs and the filtrate were analyzed by AAS to quantify the remaining Pt. Based on the above procedure, < 5% of total PLGA-BODIPY-630 was released from TNPs over the course of 48 hr.
Animal models
All animal research was performed in accordance with guidelines from the Institutional Subcommittee on Research Animal Care (Massachusetts General Hospital). All experiments were performed using female mice that were 5-7 weeks old at the start of the experiment. For experiments with HT1080 tumors, 2 million cells in PBS were subcutaneously implanted into nu/nu mice; roughly 2-3 weeks later (once tumors reached approximately 8 mm diameter), imaging experiments were initiated. For the experimental model of hematogenous metastatic dissemination, 0.25 million 4T1 breast cancer cells suspended in phosphate-buffered saline (PBS) were i.v. injected into balb/c mice; roughly 2 weeks later tumors were excised for histological quantification of liver and lung tumor burden in FFPE, hematoxylin and eosin (H&E) stained sections. For intraperitoneal OVCA imaging, 10 million A2780CP cells suspended in PBS were intraperitoneally injected into nu/nu mice. TNP injection and imaging were performed once ascites or tumor masses became evident (roughly 6 weeks later). For histology and imaging experiments using KP cells, 1 million cells were subcutaneously implanted into C57Bl/6 background animals (all JAX), including Cx3cr1GFP/+ R26mT-mG/+ dual-reporter mice. For dual reporter mice generation, Cx3cr1GFP/GFP animals were crossed with R26mT-mG/mT-mG animals that ubiquitously express membrane-anchored tdTomato69. The resulting Cx3cr1GFP/+ R26mT-mG/+ animals can be used to visualize GFP+ tdTomato+ macrophages, monocytes, and dendritic cells, as well as tdTomato+ stroma and endothelium.
Cell lines
With some exceptions, cell lines were obtained from ATCC and routinely cultured according to the manufacturer's guidelines. OVCA-429 were a kind gift from Dr. Michael Birrer (MGH), and A2780CP were from Sigma. The murine lung adenocarcinoma cell line KP1.9 was generated from lung tumor cells of KrasLSL-G12D/+;p53fl/fl mice (C57/Bl6 background), which develop lung adenocarcinoma after infection with an adenovirus expressing Cre recombinase by intratracheal administration38. KP cells were maintained in Iscove's DMEM media supplemented with 10% fetal bovine serum (FBS) and 5% penicillin/streptomycin. All cell lines were routinely tested for contamination using mouse antibody production (MAP) testing (VRL Laboratories) and assaying for mycoplasma (VRL Laboratories; Lonza MycoAlert). The fluorescent protein mApple was subcloned into the pLVX vector using restriction enzymes AfeI and NotI. We inserted a XhoI site at in the 5′ end of the pLVX-mApple multiple cloning site using QuikChange site-directed mutagenesis (Agilent). The pDsRed-Monomer-Mem membrane targeting sequence (Clontech) was PCR amplified for In-Fusion® cloning to construct pLVX-Mem-mApple. PCR product was then ligated into pLVX-Apple after AfeI and XhoI digestion, and fully sequenced. Lentiviral particles were produced using Lenti-X HTX Packaging System (Clontech) for transduction into HT1080 and A2780CP cells, which were then selected using 3 μg mL−1 puromycin. HT1080-53BP1-mApple and A2780CP-53BP1-mApple were developed as previously described28.
Intravital microscopic imaging
TNPs were injected at the indicated dose (1 mg kg−1 unless otherwise stated) via tail-vein catheter immediately after mixing to a final 1x phosphate-buffered saline (PBS) solution, at a final volume of 100 μl. Intravital microscopy was performed on an Olympus FV1000 multiphoton imaging system using a XLUMPLFLN 20x water immersion objective (NA 1.0; Olympus America). Images were scanned sequentially using 405-nm, 473-nm, 559-nm and 633-nm diode lasers in combination with a DM405/488/559/635-nm dichroic beam splitter. Emitted light was then separated and collected using appropriate combinations of beam splitters (SDM473, SDM560 and/or SDM 640) and emission filters BA490-540, BA575-620, BA575-675 and/or BA655-755 (all Olympus America). Dextran pacific blue (λex = 405 nm) was injected to initially image TMV as previously described28. Briefly, 500 kDa amino-dextran (Thermo) was labeled with Pacific Blue succinimidyl ester (Thermo), purified using 30 kDa MWCO centrifugal filtration (Amicon), and 250 μg intravenously injected 10 min prior to imaging. Dorsal window chamber imaging was performed following previously described procedures28,67,68. Briefly, 2 million HT1080-53BP1-mApple cells were suspended in 50 μl PBS and injected under the fascia of nu/nu mice (Cox7, MGH) 30 min following surgical chamber implantation, and imaged two weeks later.
Histology
Excised tumors were embedded in optimal cutting temperature (OCT) compound, flash-frozen, sectioned using a Leica CM1900 Rapid Sectioning Cryostat, stained using anti-mouse F4/80 antigen eFluor 450 (clone BM8; eBioscience), and imaged using an upright Olympus BX63 microscope and a 100x oil-immersion objective. For immunohistochemistry, a biotinylated anti-rat IgG antibody was applied, and VECTASTAIN ABC kit (Vector Laboratories Inc.) along with a 3-amino-9-ethylcarbazole substrate (Dako) were used for color development. The sections were counterstained with Harris hematoxylin solution (Sigma-Aldrich) and scanned by using Nanozoomer 2.0RS (Hamamatsu, Japan). For immunofluorescence, anti-rat IgG-Alexa Fluor 405 (Abcam) as a secondary antibody and anti-mouse CD326 (EpCAM)-PE antibody (clone: G8.8, eBioscience) were used.
In vitro nanoparticle characterization
For cytotoxicity assays (Supplementary Table 1), 5,000 cells per well were plated in 96-well plates, treated the next day with Pt-compound or the appropriate buffer control (DMF or drug-free PLGA-PEG nanoparticles, as appropriate), and assessed for viability 72 hr later using PrestoBlue (Life Technologies) following the manufacturer's protocol. IC50 values for each compound were calculated by interpolating from an 11-point dose-response curve.
For live-cell in vitro microscopy of TNP uptake (Supplementary Fig. 2a), HT1080-53BP1-mApple cells were seeded on an optical-bottom 96-well plate (Ibidi; Applied Biophysics), treated the following day with 1 μM TNP for 24 hr, washed in warm medium, and immediately imaged on a DeltaVision (Applied Precision) modified Olympus BX63 microscopy system with an environmental chamber. Dose-response analysis of TNP uptake (Supplementary Fig. 3) followed the same protocol. Corresponding measurements of intracellular Pt uptake (Supplementary Fig. 3d) were performed by treating 80% confluent cells in 6-well plates for 24 hr with TNP, rinsing with PBS, trypsinizing, centrifuging the cell pellet for 300xg for 5 min, re-suspending the pellet in 50 μL fresh PBS, and freezing it for subsequent AAS analysis.
CellLight BacMam (Life Technologies) fluorescent protein-signal peptide fusions, delivered using baculovirus, were used for subcellular compartment co-localization experiments (Supplementary Fig. 2b). Briefly, 10,000 HT1080 cells were treated overnight with 20 μL CellLight reagent in 12-well dishes, plated the next day on collagen-I-coated glass coverslips in 6-well dishes, and the following day were treated with 0.5 μM TNP for either 3 or 24 hr. Following treatment, cells were counterstained with Hoechst 33342 and immediately imaged. Collagen-coating was performed by treating coverslips with 100 μg mL−1 rat-tail collagen-I (BD Biosciences) overnight and then rinsing with PBS.
To analyze de-quenching of the C16-Pt(IV)-BODIPY compound (Supplementary Fig. 2d), TNPs were added at 1 μM to full serum medium (DMEM + 10% FBS + 1% pen/strep) in the presence or absence of 90% confluent HT1080 in 96-well plates. Fluorescence was monitored by a Tecan Safire 2 fluorescence plate reader. For monitoring TNP uptake kinetics (Supplementary Fig. 8a), equal numbers of RAW macrophages or HT1080 cells were plated in 96-well plates and incubated with 1 μM TNP. At the indicated time points, medium was temporarily transferred to empty wells and replaced with fresh media on cells. Cells were then immediately measured using a plate reader for BODIPY-630 fluorescence, and the TNP-containing media was replaced onto the cells again.
To analyze Pt uptake and release into supernatant by macrophages (Supplementary Fig. 8c), confluent 10 cm tissue-culture dishes of RAW macrophages were treated with 62 μM TNP for 24 hr, rinsed in PBS, treated with fresh media, incubated for another 24 hr, and then analyzed for Pt content by AAS. The supernatant was clarified by centrifugation (300xg for 5 min) prior to AAS analysis. Cells were harvested by trypsinization, centrifugation (300xg for 5 min), resuspension of the cell pellet in 50 μL PBS, and freezing for subsequent AAS analysis.
To analyze whether the Pt-containing macrophage supernatant could invoke a DNA damage response in tumor cells (Supplementary Fig. 8d), RAW macrophages were treated for 6 hr with 15 μM TNP, then rinsed and incubated in fresh media. After 24 hr, media were clarified by centrifugation (300xg for 5 min), transferred to HT1080-53BP1-mApple cells plated on optical-bottom 96-well plates (Ibidi; Applied Biophysics), and incubated overnight. The following day cells were rinsed and immediately imaged.
To analyze whether Pt-containing macrophage supernatant cause cytotoxic effects on tumor cells (Supplementary Fig. 8e), RAW macrophages were treated for 24 hr with either TNP or unencapsulated C16-Pt(IV)-BODIPY (the latter to achieve high Pt concentrations), then rinsed and incubated in fresh media. After 24 hr, media were clarified by centrifugation (300xg for 5 min), then transferred to 5000 HT1080 cells per well of a 96-well plate. After 72 hr the cell count was determined by the PrestoBlue assay (Life Technologies).
To analyze whether the above cytotoxic effects depend on proteins in the Pt-containing macrophage supernatant (Supplementary Fig. 8f), RAW macrophages were treated for 16 hr with 60 μM TNP, then rinsed and incubated in fresh media. After an additional 16 hr, media were clarified by centrifugation (300xg for 5 min), filtered using MWCO centrifugal filters (Amicon; Millipore), and transferred to 5000 HT1080 cells per well of a 96-well plate. After an additional 72 hr the cell count was determined by the PrestoBlue assay (Life Technologies).
Tumor growth
Subcutaneous tumors were implanted in 7 week old female nu/nu mice (Cox7, MGH), injected in four quadrant animal flanks as 1 million HT1080 cells suspended in 50 μL PBS. Nine days later, animals were ranked and sorted into groups of four based on tumor size. According to predefined protocol guidelines, mice were sacrificed when tumor burden reached more than 1 cm in diameter, or 2 cm in diameter if only one tumor was present. Tumor volumes were measured two to three times per week, estimated using the spherical tumor volume formula V = 4/3Πr3, where r is averaged from four caliper measurements performed by two blinded researchers. Each size-group was randomly distributed to the four treatment-groups such that final treatment-groups exhibited roughly equal distribution in tumor size, with 9-10 mice per group. Groups received 150 μL of clodronate liposomes (clod-lip) or PBS liposomes as a vehicle control, intraperitoneally, on the indicated days (Fig. 8a). Liposomes were from ClodLip BV (Haarlem, The Netherlands), with clodronate at a concentration of 5 mg mL−1. As separate intravenous injections on indicated days (Fig. 8a), groups received 1 mg kg−1 Pt of either TNP or the TNP without Pt(IV) as a vehicle control. TNPs for this experiment were formulated as described above, using PLGA8kDa-PEG5kDa and non-fluorescent PLGA30-60kDa rather than PLGA30-60kDa-BODIPY-630. TNP formulations were made fresh before each injection, and batches were tested for size and monodispersity by dynamic light scattering and transmission electron microscopy. Pt loading was measured by AAS, and appropriate drug release was measured as previously described. At 19 days post-implantation, tumors were excised, rinsed in PBS, and processed for histology by freezing in OCT compound, or alternatively processed for AAS analysis by blotting tissue to remove excess water and freezing. One of 38 animals was prematurely sacrificed owing to biting and cachexia.
Flow cytometry
Subcutaneous tumors (HT1080 cells) were harvested from nu/nu mice three weeks post-implantation, cut into small pieces, and incubated in RPMI 1640 medium containing 0.2mg mL−1 collagenase type I (Worthington Biochemical Corporation) for 1 hr at 37°C while shaking (250 rpm). Digested tumors were filtered through a 70 μm cell strainer (BD Falcon). The resulting single-cell suspensions were washed and resuspended in PBS with 0.5% BSA and 2mM EDTA. Cell labeling was performed with appropriate antibodies as indicated below for 45 min at 4°C. The following cell types were identified by flow cytometry (LSRII, BD Biosciences) depending on cell marker expression: tumor cells (hCD29+), macrophages (CD45+CD11b+Ly6C−Lin−CD11c+F4/80+), neutrophils (CD45+CD11b+Ly6C+Lin+) and lymphocyte-like cells (CD45+Lin+CD11b−Ly6G−). The anti-human CD29 antibody (clone MAR4) was from BD, and the following anti-mouse antibodies used were from Biolegend: CD45 (clone 30-F11), F4/80 (clone BM8), CD11c (clone N418), Ly6C (clone HK1.4). CD11b (clone M1/70) was from BD Biosciences, along with all antibodies used in the lineage (Lin) mixture: anti-CD90.2 (clone 53-2.1), anti-B220 (clone RA3-6B2), anti-NK1.1 (clone PK136), anti-CD49b (clone DX5), anti-Ter119 (cloneTER-119) and anti-Ly6G (clone 1A8). To exclude dead cells, 7-aminoactinomycin D (7-AAD, Sigma-Aldrich) was used. Data were analyzed using FlowJo v.8.8.7 (Tree Star, Inc.) and MATLAB. BODIPY-630 and amino-BODIPY fluorescence was assessed by using an LSRII flow cytometer and the mean fluorescence intensity (MFI) of the different cell populations was determined. Background autofluorescence for each immunologically defined cell population was measured from control-treated animals that were injected with non-fluorescent PLGAPEG vehicle; this value was subtracted from the data for the fluorescent TNP-treated animals.
Computational image analysis
Intravital microscopy images were analyzed using either Matlab (Mathworks) or ImageJ and were pre-processed using background subtraction based on data acquired immediately prior to TNP injection. For vascular half-life calculations, fluorescence time-lapse values from multiple vessels across multiple animals were recorded, averaged, and fit to an exponential decay model using nonlinear regression in MATLAB. Single-cell 3D segmentation for image cytometry analysis was performed using a custom MATLAB pipeline. Briefly, a previously described 3D nuclear-segmentation algorithm was modified to measure the mean fluorescence intensity of TNP vehicle and its payload within a given radius of each nucleus. These measurements were then correlated with observed 53BP1-puncta in each individual nucleus, validated by eye (Fig. 3c). Throughout the manuscript, data falling >2 standard deviations from the mean were excluded as outliers from the statistical calculations. For calculation of spatial heterogeneity, measured by the coefficient of variation (CV; Supplementary Fig. 4), cell-sized regions of interest within images were quantified for mean fluorescence intensity. CV for TNP and unencapsulated Pt (CP-11; 28) were measured >20 half-lives post-injection as an approximation of steady-state tissue distribution (5 hr and 24 hr, respectively).
Liver and BM analysis
Pt concentrations in the liver and bone marrow were determined by AAS and fluorescence imaging. Briefly, naive female nu/nu mice 8 weeks old were i.v. injected with TNP at a dose of 1 mg kg−1 Pt. 24 hr later, animals were perfused with PBS by intracardiac injection before dissection. For fluorescence quantification of TNP payload, livers were excised and frozen in OCT compound for later sectioning. Femoral BM was flushed using PBS and smeared on a glass slide for immediate imaging. Un-injected control animals were used to measure background signal for each organ, which was baseline-subtracted in the quantification. For AAS analysis of Pt content, livers were excised, patted dry, and frozen. BM was flushed using PBS, centrifuged at 16,000 x g to pellet cells, and frozen. Tissue was then dissolved in 70% nitric acid and analyzed as with the HT1080 tumors (Fig. 8). For quantification of BM cellularity, femurs were excised 24 hr post-injection with TNP, formalin fixed overnight, decalcified in EDTA, and processed for FFPE sectioning. Immunohistochemistry was performed for apoptosis analysis by terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL), using Apoptag Peroxidase In Situ Apoptosis Detection Kit (Millipore), counterstaining with Harris hematoxylin solution (Sigma-Aldrich), and scanning with a Nanozoomer 2.0RS (Hamamatsu, Japan).
Metastasis burden in lung and liver was quantified by morphological assessment in H&E stained liver FFPE sections that had been imaged using Nanozoomer 2.0RS, with organ excision at time of animal euthanasia according to institutional guidelines (body condition score of 2) or 20 days post-cancer injection, whichever came first. No statistically significant difference was observed in animal survival, body weight loss, or lung tumor burden across the groups. One mouse from the group receiving repeated TNP dosing was excluded from analysis since no lung tumors (and very few liver tumors) were found by histology, presumably due to failed initial intravenous injection.
Clinical chemistry measurements in Swiss albino mice were performed using previously described TNP and methods6. Graphically re-plotted here for context (Supplementary Fig. 9a), bio-distribution of Pt in male rats was measured as described previously6.
Supplementary Material
Acknowledgements
This work was supported in part by the US National Institutes of Health (NIH) grants RO1-CA164448, P50-CA086355, PO1-CA139980, U54-CA151884 (to RW) and RO1-CA034992 from the National Cancer Institute (to SJL). CP is supported by the Deutsche Forschungsgemeinschaft (DFG) PF809/1-1. The authors thank Dr. Kevin King, Dr. Julia Kalow, Dr. Basit Yameen, Alex Zaltsman, Matthew Sebas, Greg Wojtkiewicz, David Pirovich, and Olivier Kister for technical assistance, and Dr. Melissa Sprachman for helpful discussions.
Footnotes
Author contributions: M.A.M., Y.Z., S.G., C.P., D.J., G.D., M.P., S.J.L., O.C.F., and R.W. developed the concepts and designed the experiments; M.A.M., S.G., and H.Z. synthesized and characterized TNPs; Y.Z. and B.A. synthesized and characterized C16-Pt(IV)-BODIPY; M.A.M., C.P., and C.E. performed and analyzed the FACS experiments; M.A.M. and R.H.K. performed imaging experiments; M.A.M. and K.S.Y. generated the cell lines; M.A.M. and D.R.J. developed and performed the image processing; M.A.M. and Y.I. performed and analyzed the histology; M.A.M. and Y.Z. performed and analyzed the AAS experiments; M.A.M. performed all tissue culture experiments; M.A.M. and R.W. wrote the paper; all authors analyzed results, wrote the methods section, and edited the manuscript.
Conflict of interest statement: O.C.F. has a financial interest in BIND Biosciences, BLEND Therapeutics and Selecta Biosciences, biotechnology companies developing nanoparticle technologies for medical applications. S.J.L. discloses a financial interest in BLEND Therapeutics. The remaining authors declare no competing financial interests.
References
- 1.Kelland L. The resurgence of platinum-based cancer chemotherapy. Nat Rev Cancer. 2007;7:573–584. doi: 10.1038/nrc2167. [DOI] [PubMed] [Google Scholar]
- 2.O'Shaughnessy J, et al. Phase III Study of Iniparib Plus Gemcitabine and Carboplatin Versus Gemcitabine and Carboplatin in Patients With Metastatic Triple-Negative Breast Cancer. J Clin Oncol. 2014 doi: 10.1200/JCO.2014.55.2984. [DOI] [PubMed] [Google Scholar]
- 3.Cooke SL, Brenton JD. Evolution of platinum resistance in high-grade serous ovarian cancer. Lancet Oncol. 2011;12:1169–1174. doi: 10.1016/S1470-2045(11)70123-1. [DOI] [PubMed] [Google Scholar]
- 4.Bertrand N, Wu J, Xu X, Kamaly N, Farokhzad OC. Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Adv Drug Deliv Rev. 2014;66:2–25. doi: 10.1016/j.addr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hrkach J, et al. Preclinical development and clinical translation of a PSMA-targeted docetaxel nanoparticle with a differentiated pharmacological profile. Sci Transl Med. 2012;4:128ra39. doi: 10.1126/scitranslmed.3003651. [DOI] [PubMed] [Google Scholar]
- 6.Dhar S, Kolishetti N, Lippard SJ, Farokhzad OC. Targeted delivery of a cisplatin prodrug for safer and more effective prostate cancer therapy in vivo. Proc Natl Acad Sci U S A. 2011;108:1850–1855. doi: 10.1073/pnas.1011379108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valencia PM, et al. Synergistic cytotoxicity of irinotecan and cisplatin in dual-drug targeted polymeric nanoparticles. Nanomedicine (Lond) 2013;8:687–698. doi: 10.2217/nnm.12.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu X, et al. Enhancing tumor cell response to chemotherapy through nanoparticle-mediated codelivery of siRNA and cisplatin prodrug. Proc Natl Acad Sci U S A. 2013;110:18638–18643. doi: 10.1073/pnas.1303958110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnstone TC, et al. Nanoparticle encapsulation of mitaplatin and the effect thereof on in vivo properties. ACS Nano. 2013;7:5675–5683. doi: 10.1021/nn401905g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prabhakar U, et al. Challenges and key considerations of the enhanced permeability and retention effect for nanomedicine drug delivery in oncology. Cancer Res. 2013;73:2412–2417. doi: 10.1158/0008-5472.CAN-12-4561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maeda H, Nakamura H, Fang J. The EPR effect for macromolecular drug delivery to solid tumors: Improvement of tumor uptake, lowering of systemic toxicity, and distinct tumor imaging in vivo. Adv Drug Deliv Rev. 2013;65:71–79. doi: 10.1016/j.addr.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Harrington KJ, et al. Phase I-II study of pegylated liposomal cisplatin (SPI-077) in patients with inoperable head and neck cancer. Ann Oncol. 2001;12:493–496. doi: 10.1023/a:1011199028318. [DOI] [PubMed] [Google Scholar]
- 13.Wright J. Nanotechnology: Deliver on a promise. Nature. 2014;509:S58–S59. doi: 10.1038/509S58a. [DOI] [PubMed] [Google Scholar]
- 14.Caron WP, Song G, Kumar P, Rawal S, Zamboni WC. Interpatient pharmacokinetic and pharmacodynamic variability of carrier-mediated anticancer agents. Clin Pharmacol Ther. 2012;91:802–812. doi: 10.1038/clpt.2012.12. [DOI] [PubMed] [Google Scholar]
- 15.Thurber GM, et al. Single-cell and subcellular pharmacokinetic imaging allows insight into drug action in vivo. Nat Commun. 2013;4:1504. doi: 10.1038/ncomms2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamamoto N, et al. Cellular dynamics visualized in live cells in vitro and in vivo by differential dual-color nuclear-cytoplasmic fluorescent-protein expression. Cancer Res. 2004;64:4251–4256. doi: 10.1158/0008-5472.CAN-04-0643. [DOI] [PubMed] [Google Scholar]
- 17.Hinkeldey B, Schmitt A, Jung G. Comparative photostability studies of BODIPY and fluorescein dyes by using fluorescence correlation spectroscopy. Chemphyschem. 2008;9:2019–2027. doi: 10.1002/cphc.200800299. [DOI] [PubMed] [Google Scholar]
- 18.Karolin J, Johansson LB-A, Strandberg L, Ny T. Fluorescence and absorption spectroscopic properties of dipyrrometheneboron difluoride (BODIPY) derivatives in liquids, lipid membranes, and proteins. J Am Chem Soc. 1994;116:7801–7806. [Google Scholar]
- 19.Ulrich G, Ziessel R, Harriman A. The chemistry of fluorescent bodipy dyes: versatility unsurpassed. Angew Chem Int Ed Engl. 2008;47:1184–1201. doi: 10.1002/anie.200702070. [DOI] [PubMed] [Google Scholar]
- 20.Xiao K, et al. The effect of surface charge on in vivo biodistribution of PEG-oligocholic acid based micellar nanoparticles. Biomaterials. 2011;32:3435–3446. doi: 10.1016/j.biomaterials.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He C, Hu Y, Yin L, Tang C, Yin C. Effects of particle size and surface charge on cellular uptake and biodistribution of polymeric nanoparticles. Biomaterials. 2010;31:3657–3666. doi: 10.1016/j.biomaterials.2010.01.065. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto Y, Nagasaki Y, Kato Y, Sugiyama Y, Kataoka K. Long-circulating poly(ethylene glycol)-poly(D,L-lactide) block copolymer micelles with modulated surface charge. J Control Release. 2001;77:27–38. doi: 10.1016/s0168-3659(01)00451-5. [DOI] [PubMed] [Google Scholar]
- 23.Kommareddy S, Amiji M. Biodistribution and pharmacokinetic analysis of long-circulating thiolated gelatin nanoparticles following systemic administration in breast cancer-bearing mice. J Pharm Sci. 2007;96:397–407. doi: 10.1002/jps.20813. [DOI] [PubMed] [Google Scholar]
- 24.Zheng YR, et al. Pt(IV) prodrugs designed to bind non-covalently to human serum albumin for drug delivery. J Am Chem Soc. 2014;136:8790–8798. doi: 10.1021/ja5038269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orth JD, et al. Analysis of mitosis and antimitotic drug responses in tumors by in vivo microscopy and single-cell pharmacodynamics. Cancer Res. 2011;71:4608–4616. doi: 10.1158/0008-5472.CAN-11-0412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laughney AM, et al. Single-cell pharmacokinetic imaging reveals a therapeutic strategy to overcome drug resistance to the microtubule inhibitor eribulin. Sci. Transl. Med. 2014;6:261ra152. doi: 10.1126/scitranslmed.3009318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang M, Jiang P, Hoffman RM. Whole-body subcellular multicolor imaging of tumor-host interaction and drug response in real time. Cancer Res. 2007;67:5195–5200. doi: 10.1158/0008-5472.CAN-06-4590. [DOI] [PubMed] [Google Scholar]
- 28.Miller MA, Askevold B, Yang KS, Kohler RH, Weissleder R. Platinum compounds for high-resolution in vivo cancer imaging. ChemMedChem. 2014;9:1131–1135. doi: 10.1002/cmdc.201300502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miwa S, et al. Imaging UVC-induced DNA damage response in models of minimal cancer. J Cell Biochem. 2013;114:2493–2499. doi: 10.1002/jcb.24599. [DOI] [PubMed] [Google Scholar]
- 30.Beletsi A, Panagi Z, Avgoustakis K. Biodistribution properties of nanoparticles based on mixtures of PLGA with PLGA-PEG diblock copolymers. Int J Pharm. 2005;298:233–241. doi: 10.1016/j.ijpharm.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 31.Doxil . Janssen Products, LP; Horsham, PA: 2015. [Google Scholar]
- 32.Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal Doxorubicin: review of animal and human studies. Clin Pharmacokinet. 2003;42:419–436. doi: 10.2165/00003088-200342050-00002. [DOI] [PubMed] [Google Scholar]
- 33.Kolishetti N, et al. Engineering of self-assembled nanoparticle platform for precisely controlled combination drug therapy. Proc Natl Acad Sci U S A. 2010;107:17939–17944. doi: 10.1073/pnas.1011368107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dhar S, Gu FX, Langer R, Farokhzad OC, Lippard SJ. Targeted delivery of cisplatin to prostate cancer cells by aptamer functionalized Pt(IV) prodrug-PLGA-PEG nanoparticles. Proc Natl Acad Sci U S A. 2008;105:17356–17361. doi: 10.1073/pnas.0809154105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karanam K, Kafri R, Loewer A, Lahav G. Quantitative live cell imaging reveals a gradual shift between DNA repair mechanisms and a maximal use of HR in mid S phase. Mol Cell. 2012;47:320–329. doi: 10.1016/j.molcel.2012.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shaw TJ, Senterman MK, Dawson K, Crane CA, Vanderhyden BC. Characterization of intraperitoneal, orthotopic, and metastatic xenograft models of human ovarian cancer. Mol Ther. 2004;10:1032–1042. doi: 10.1016/j.ymthe.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 37.Ginhoux F, et al. Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science. 2010;330:841–845. doi: 10.1126/science.1194637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DuPage M, Dooley AL, Jacks T. Conditional mouse lung cancer models using adenoviral or lentiviral delivery of Cre recombinase. Nat Protoc. 2009;4:1064–1072. doi: 10.1038/nprot.2009.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zeisberger SM, et al. Clodronate-liposome-mediated depletion of tumour-associated macrophages: a new and highly effective antiangiogenic therapy approach. Br J Cancer. 2006;95:272–281. doi: 10.1038/sj.bjc.6603240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Denis MC, Mahmood U, Benoist C, Mathis D, Weissleder R. Imaging inflammation of the pancreatic islets in type 1 diabetes. Proc Natl Acad Sci U S A. 2004;101:12634–12639. doi: 10.1073/pnas.0404307101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365:2205–2219. doi: 10.1056/NEJMra1004965. [DOI] [PubMed] [Google Scholar]
- 42.Beste MT, et al. Molecular network analysis of endometriosis reveals a role for c-Jun-regulated macrophage activation. Sci Transl Med. 2014;6:222ra16. doi: 10.1126/scitranslmed.3007988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Cell. 2011;145:341–355. doi: 10.1016/j.cell.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frantz S, Nahrendorf M. Cardiac macrophages and their role in ischaemic heart disease. Cardiovasc Res. 2014;102:240–248. doi: 10.1093/cvr/cvu025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weissleder R, Nahrendorf M, Pittet MJ. Imaging macrophages with nanoparticles. Nat Mater. 2014;13:125–138. doi: 10.1038/nmat3780. [DOI] [PubMed] [Google Scholar]
- 46.Aouadi M, et al. Orally delivered siRNA targeting macrophage Map4k4 suppresses systemic inflammation. Nature. 2009;458:1180–1184. doi: 10.1038/nature07774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.De Palma M, Lewis CE. Macrophage regulation of tumor responses to anticancer therapies. Cancer Cell. 2013;23:277–286. doi: 10.1016/j.ccr.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 48.Cortez-Retamozo V, et al. Origins of tumor-associated macrophages and neutrophils. Proc Natl Acad Sci U S A. 2012;109:2491–2496. doi: 10.1073/pnas.1113744109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steidl C, et al. Tumor-associated macrophages and survival in classic Hodgkin's lymphoma. N Engl J Med. 2010;362:875–885. doi: 10.1056/NEJMoa0905680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang QW, et al. Prognostic significance of tumor-associated macrophages in solid tumor: a meta-analysis of the literature. PLoS One. 2012;7:e50946. doi: 10.1371/journal.pone.0050946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nakasone ES, et al. Imaging tumor-stroma interactions during chemotherapy reveals contributions of the microenvironment to resistance. Cancer Cell. 2012;21:488–503. doi: 10.1016/j.ccr.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang W, et al. Depletion of tumor-associated macrophages enhances the effect of sorafenib in metastatic liver cancer models by antimetastatic and antiangiogenic effects. Clin Cancer Res. 2010;16:3420–3430. doi: 10.1158/1078-0432.CCR-09-2904. [DOI] [PubMed] [Google Scholar]
- 53.Pyonteck SM, et al. CSF-1R inhibition alters macrophage polarization and blocks glioma progression. Nat Med. 2013;19:1264–1272. doi: 10.1038/nm.3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhu Y, et al. CSF1/CSF1R Blockade Reprograms Tumor-Infiltrating Macrophages and Improves Response to T-cell Checkpoint Immunotherapy in Pancreatic Cancer Models. Cancer Res. 2014;74:5057–5069. doi: 10.1158/0008-5472.CAN-13-3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ries CH, et al. Targeting tumor-associated macrophages with anti-CSF-1R antibody reveals a strategy for cancer therapy. Cancer Cell. 2014;25:846–859. doi: 10.1016/j.ccr.2014.05.016. [DOI] [PubMed] [Google Scholar]
- 56.Mayer LD, Dougherty G, Harasym TO, Bally MB. The role of tumor-associated macrophages in the delivery of liposomal doxorubicin to solid murine fibrosarcoma tumors. J Pharmacol Exp Ther. 1997;280:1406–1414. [PubMed] [Google Scholar]
- 57.Hirota K, et al. Optimum conditions for efficient phagocytosis of rifampicin-loaded PLGA microspheres by alveolar macrophages. J Control Release. 2007;119:69–76. doi: 10.1016/j.jconrel.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 58.Liu H, et al. Structure-based programming of lymph-node targeting in molecular vaccines. Nature. 2014;507:519–522. doi: 10.1038/nature12978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kirpotin DB, et al. Antibody targeting of long-circulating lipidic nanoparticles does not increase tumor localization but does increase internalization in animal models. Cancer Res. 2006;66:6732–6740. doi: 10.1158/0008-5472.CAN-05-4199. [DOI] [PubMed] [Google Scholar]
- 60.Venkatraman SS, Ma LL, Natarajan JV, Chattopadhyay S. Polymer- and liposome-based nanoparticles in targeted drug delivery. Front Biosci (Schol Ed) 2010;2:801–814. doi: 10.2741/s103. [DOI] [PubMed] [Google Scholar]
- 61.She W, et al. The potential of self-assembled, pH-responsive nanoparticles of mPEGylated peptide dendron-doxorubicin conjugates for cancer therapy. Biomaterials. 2013;34:1613–1623. doi: 10.1016/j.biomaterials.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 62.Harisinghani M, Ross RW, Guimaraes AR, Weissleder R. Utility of a new bolusinjectable nanoparticle for clinical cancer staging. Neoplasia. 2007;9:1160–1165. doi: 10.1593/neo.07940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ansari C, et al. Development of novel tumor-targeted theranostic nanoparticles activated by membrane-type matrix metalloproteinases for combined cancer magnetic resonance imaging and therapy. Small. 2014;10:566–75. 417. doi: 10.1002/smll.201301456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kaittanis C, et al. Environment-responsive nanophores for therapy and treatment monitoring via molecular MRI quenching. Nat Commun. 2014;5:3384. doi: 10.1038/ncomms4384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beatty GL, et al. CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science. 2011;331:1612–1616. doi: 10.1126/science.1198443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Germano G, et al. Role of macrophage targeting in the antitumor activity of trabectedin. Cancer Cell. 2013;23:249–262. doi: 10.1016/j.ccr.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 67.Alieva M, Ritsma L, Giedt RJ, Weissleder R, van Rheenen J. Imaging windows for long-term intravital imaging. IntraVital. 2014;3 doi: 10.4161/intv.29917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Turetsky A, Kim E, Kohler RH, Miller MA, Weissleder R. Single cell imaging of Bruton's tyrosine kinase using an irreversible inhibitor. Sci Rep. 2014;4:4782. doi: 10.1038/srep04782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Muzumdar MD, Tasic B, Miyamichi K, Li L, Luo L. A global double-fluorescent Cre reporter mouse. Genesis. 2007;45:593–605. doi: 10.1002/dvg.20335. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.