Abstract
Objectives
We sought to evaluate the effect of ratifying the World Health Organization Framework Convention on Tobacco Control (FCTC) on countries enacting smoke-free laws covering indoor workplaces, restaurants, and bars.
Methods
We compared adoption of smoke-free indoor workplace, restaurant, and bar laws in countries that did versus did not ratify the FCTC, accounting for years since the ratification of the FCTC and for countries’ World Bank income group.
Results
Ratification of the FCTC significantly (P < .001) increased the probability of smoke-free laws. This effect faded with time, with a half-life of 3.1 years for indoor workplaces and 3.8 years for restaurants and bars. Compared with high-income countries, upper-middle–income countries had a significantly higher probability of smoke-free indoor workplace laws.
Conclusions
The FCTC accelerated the adoption of smoke-free indoor workplace, restaurant, and bar laws, with the greatest effect in the years immediately following ratification. The policy implication is that health advocates must increase efforts to secure implementation of FCTC smoke-free provisions in countries that have not done so.
Smoke-free laws improve health by reducing exposure to secondhand smoke and the associated heart disease, cancer, and other disease.1-3 The World Health Organization’s (WHO’s) Framework Convention on Tobacco Control4 (FCTC), in force since 2005, commits the countries that have adopted the treaty to implement tobacco-control measures including smoke-free environments, strong health warning labels, increased tobacco taxes, and safeguarding the policymaking process against the tobacco industry. Article 8 of the FCTC commits countries to
adopt and implement … measures, providing for protection from exposure to tobacco smoke in indoor workplaces, public transport, indoor public places and, as appropriate, other public places.4(p8)
As of April 2015, 180 countries were parties to the FCTC.5 The FCTC has already been shown to improve the chances for certain tobacco-control policies, such as its role in accelerating the adoption of FCTC-compliant warning labels on tobacco products.6,7 Countries that previously had voluntary warning label agreements with tobacco companies starting in the 1990s,6 along with poorer countries with less state capacity,7 were less likely to have such labels. The FCTC states that countries should pursue graphic health warning labels within 3 years of ratifying the treaty and within 5 years for some other policies, but does not specify a timeframe for smoke-free laws and has no external means of enforcement. In the first 5 years after ratifying the treaty, 24 (14%) of the 175 parties as of 2012 had passed smoke-free indoor workplace laws.8
We evaluated the effect of ratifying the FCTC on countries enacting national smoke-free laws. We focused on indoor workplaces, restaurants, and bars because these are the venues for which the tobacco industry internationally has fought strongly to prevent smoke-free environments.9-12
METHODS
We evaluated the effect of the FCTC on national smoke-free laws through quantitative methods.
We obtained data on national smoking restriction laws from the tobacco industry–created International Tobacco Documentation Centre’s Smoking Issues Status Book13 for 1997 (workplaces, cafes and restaurants, and bars and nightclubs) and from the WHO report on the global tobacco epidemic in 2013, with its accompanying published data set,8 which gives the status of smoke-free environments for 2007, 2010, and 2012 (indoor offices, restaurants, and pubs and bars). Twenty-two jurisdictions listed in the WHO data set were not included in the 1997 tobacco industry Smoking Issues Status Book. These places were primarily Pacific or Caribbean island countries with small populations or were not independent in 1997 (Cook Islands, Dominica, Equatorial Guinea, Eritrea, Federated States of Micronesia, Grenada, Kiribati, Macedonia, Marshall Islands, Monaco, Nauru, Niue, Palau, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Solomon Islands, Timor-Leste, Tonga, Tuvalu, Vanuatu, and West Bank and Gaza Strip). Because we used the WHO data set, our data did not include polities (such as Taiwan) that were ineligible to be WHO members, regardless of smoke-free laws in place.
The Smoking Issues Status Book had no information on smoking law status for 12 countries (Albania, Antigua and Barbuda, Bahamas, Belize, Bosnia and Herzegovina, Cambodia, Georgia, Laos, Namibia, Samoa, San Marino, and Seychelles). The Smoking Issues Status Book also listed 9 jurisdictions, mostly autonomous territories of European countries, that the WHO data set did not list. We excluded all these places from the analysis. Finally, some countries split apart after 1997 (such as Serbia and Montenegro); for these cases, we applied the 1997 data to each successor country.
Because the first available time point in the WHO data was for policies in 2007,14 the smoke-free laws that countries passed before and up to 2007 were represented as occurring in 2007. Likewise, smoke-free laws passed in 2008 through 2010 were represented as 2010, and laws passed in 2011 through 2012 were represented as 2012. To provide a more accurate characterization of the years that countries passed smoke-free laws, we also used a list of national smoke-free laws compiled by the Campaign for Tobacco-Free Kids (electronic communication from Ernesto Sebrié of Campaign for Tobacco-Free Kids, April 6, 2015). From this list, we identified 34 countries with comprehensive nationwide smoke-free laws that listed the years that the laws passed. For these countries, we used the year identified in the Campaign for Tobacco-Free Kids’ list rather than 2007, 2010, or 2012. In addition, we excluded countries with populations of fewer than 1 million, leaving 166 countries for which we had data from 1997 through 2012.
Coding Laws
For each country, we assigned smoke-free policies for indoor workplaces, restaurants, and bars 1 of 4 statuses: (1) 100% smoke-free by law, (2) partial restrictions by law, (3) voluntary restrictions not by legislation, or (4) no restrictions. Two coders (R. U. and H. H.) independently coded each venue in each country, and then reached agreement.
We checked some of the smoke-free claims made by the International Tobacco Documentation Centre’s Smoking Issues Status Book for 1997, and reclassified 15 cases of smoke-free indoor workplaces, restaurants, or bars. The Smoking Issues Status Book claimed smoke-free indoor workplaces for 12 former Soviet republics (Armenia, Azerbaijan, Belarus, Estonia, Kazakhstan, Kyrgyzstan, Moldova, Russia, Tajikistan, Turkmenistan, Ukraine, and Uzbekistan), citing a 1980 law15 that in actuality only restricted smoking in offices. The Smoking Issues Status Book also claimed smoke-free workplaces for Mongolia, citing a 1993 law that applied in actuality to government and administrative offices.16 (Three other republics—Georgia, Latvia, and Lithuania—were listed as having partial restrictions or listed as having no information.) We reclassified all these cases as partial restrictions, rather than smoke-free. The Smoking Issues Status Book, in addition, claimed smoke-free bars for Mongolia by citing the 1993 law, which in actuality prohibited smoking in places of entertainment but not bars, and claimed smoke-free restaurants for North Korea without citing a law. We reclassified these countries as not restricted. With these cases reclassified, our sample from the Smoking Issues Status Book had zero cases of smoke-free indoor workplaces, restaurants, and bars.
For the WHO reports, we classified as smoke-free all the cases marked in the reports as “yes” being smoke-free, meaning that the law mandated complete smoke-free spaces, and classified the cases listed as “no” in the reports as not smoke-free. The reports listed some venues (in 2012, in 12 countries) as allowing designated smoking rooms. We classified these as not smoke-free.17
The first national smoke-free law covering indoor workplaces, restaurants, or bars came into force in Ireland in 2004,18,19 so we used the Smoking Issues Status Book data to represent the state of policies in 2003, the year countries began to ratify the FCTC. We scored cases with missing data as no restrictions, and then collapsed the 4 smoking status categories into 2 categories: 100% prohibition of smoking by legislation (FCTC-compliant) and all other categories (not FCTC-compliant).
Other Variables
In our preliminary analysis, we considered but discarded several potential independent variables: state capacity measured by the state fragility index,20 whether the country was a member of the Organization for Economic Cooperation and Development, whether English was the official language, whether there was a common law system, the number of years since universal suffrage was introduced, the number of years since formal independence, the WHO region (with Europe as the reference group), and the World Bank income group (with high-income countries as the reference group). We assessed the influence of each of these potential independent variables on having such laws in place by 2012, with logistic regression. None of these variables except World Bank income group were statistically significant. The lowest P value for any of these variables, except income group and region, was .16. One region (Americas) had P = .012 for indoor workplaces, which became .076 in a model including income group; the P value for the Americas region for both restaurants and bars was .206. Therefore, we dropped all but income group from the subsequent analysis.
We also assessed, in preliminary analysis, the impact of having had voluntary smoking restriction policies without any legislation, as measured by our coding from the Smoking Issues Status Book. We further assessed the impact of having partial restrictions by law. Neither of these variables was statistically significant, so we dropped these from the analysis.
Analysis
We examined the pace of transitions from not smoke-free to smoke-free in each of the periods for which we had data as endpoints (2003–2007, 2007–2010, and 2010–2012). For each time period, we calculated the number of countries that transitioned from not smoke-free to smoke-free; the number of countries, if any, that transitioned in the opposite direction from smoke-free to not smoke-free; as well as those countries that, during each period, started not smoke-free and remained that way, or started and remained smoke-free.
We used Cox proportional hazards models to quantify the effect of the FCTC on the 3 types of smoke-free laws as a function of years since FCTC ratification and World Bank income group. We quantified years between FCTC ratification and passing a smoke-free law for indoor workplaces, restaurants, or bars, counting starting from the year of ratification. For example, if a country ratified the FCTC in 2007 and passed a national smoke-free workplace law that same year, we classified workplaces in that country as reaching FCTC compliance in year 1; if it passed a smoke-free restaurant law by 2010, we classified restaurants as reaching FCTC compliance in year 4. Some groups (years 1–3 and 10) were based on very few cases: for years 1 to 3 there were as few as 4 to 9 cases, and for year 10 there were only 1 to 2 cases, depending on which of the venues (indoor workplaces, restaurants, bars) that we considered.
World Health Organization member countries that had not ratified the FCTC by the end of 2012 (Andorra, Argentina, Cuba, Dominican Republic, El Salvador, Eritrea, Ethiopia, Haiti, Indonesia, Malawi, Monaco, Morocco, Mozambique, Somalia, South Sudan, Switzerland, Tajikistan, the United States, and Zimbabwe) had years since ratification set to 0.
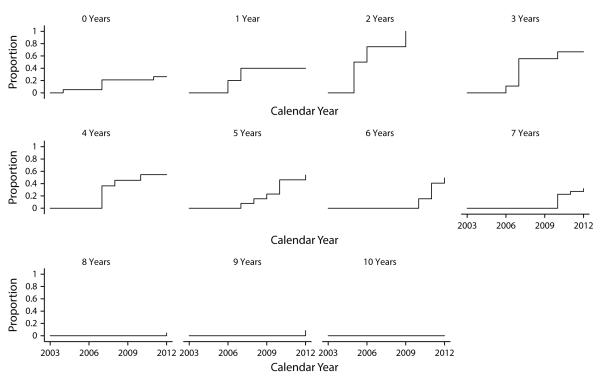
Preliminary analysis that simply included time since FCTC ratification as an independent variable in a Cox proportional hazards regression indicated that FCTC ratification was associated with a significantly lower likelihood of enacting smoke-free laws (Figure 1). Examination of the data (Figure 2 and Appendix Figure A1, available as a supplement to the online version of this article at http://www.ajph.org) suggested that there was an acceleration of passing smoke-free laws soon after FCTC ratification, but that this effect faded over time. To model this effect, we tested models with time after FCTC ratification entered as t (the original model), 1/t, , and , as well as exponential decay models e−(t-1)/τ with τ from 0.5 to 7.0, in 0.5-year increments. In all these models, we entered time (or the transformed time variable) as 0 for countries that had not yet ratified the FCTC. The Akaike information criterion and Bayesian information criterion revealed that an exponential decay model, entering time as e−(t-1)/τ with a time constant of τ = 4.5 years, provided the best description of the data for indoor workplaces, and using a time constant of τ = 5.5 years provided the best description of the data for restaurants and bars. Differences in Akaike information criterion and Bayesian information criterion were small near the optimal values of τ.
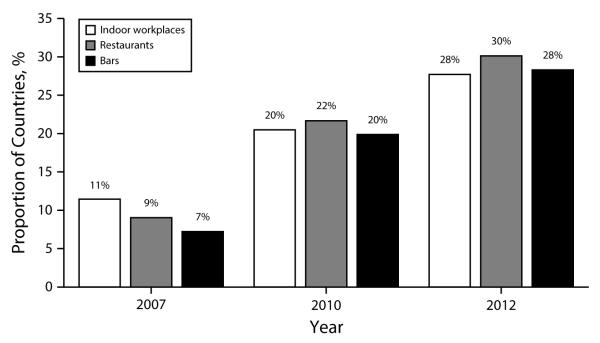
FIGURE 1. Proportion of countries with Framework Convention on Tobacco Control–compliant smoke-free indoor workplaces, restaurants, and bars: 2012.
Note. These numbers are for the 166 countries in our sample, which excludes countries with less than 1 million population. The number of countries with Framework Convention on Tobacco Control–compliant smoke-free indoor workplaces, restaurants, and bars increased over time, but as of 2012 less than one third of the parties to the treaty had enacted national legislation to implement it.
FIGURE 2. Smoke-free workplace law passage estimates for countries grouped by years since ratifying the Framework Convention on Tobacco Control: 2002–2012.
Note. The Framework Convention on Tobacco Control’s effects were strongest in earlier years following ratification, as shown by the cumulative success function for smoke-free indoor laws. See file available as a supplement to the online version of this article at http://www.ajph.org for comparable plots for restaurant and bar laws.
We used Stata version 12.1 (StataCorp LP, College Station, TX) for the analysis.
RESULTS
Within our sample of 166 countries, the number of countries with an FCTC-compliant smoke-free law for restaurants and bars increased most rapidly between 2007 and 2012 (Figure 1). Roughly similar total numbers of transitions from not smoke-free to smoke-free occurred among the periods 2003 to 2007 (transitions to smoke-free: 19 for workplaces, 15 for restaurants, 12 for bars), 2007 to 2010 (16 for workplaces, 21 for restaurants, 21 for bars), and 2010 to 2012 (12 for workplaces, 15 for restaurants, 14 for bars). Except for 2 countries (workplaces in Latvia from 2007–2010 and restaurants in Guinea from 2010–2012, which went from smoke-free to not smoke-free) transitions were from not smoke-free to smoke-free.
As of 2012, upper-middle–income countries were the income group with the most smoke-free indoor workplace, restaurant, and bar laws (Table 1). Of the 166 countries in this analysis, 44 countries fell under the World Bank classification of upper-middle income (gross domestic product per capita of $4036 to $12 475 for the year 2012). Among the upper-middle–income countries in our sample, 18 countries (40.9%) had smoke-free indoor workplace laws, 21 countries (47.7%) had smoke-free restaurant laws, and 22 countries (50%) had smoke-free bar laws. By contrast, of the 41 countries classified as high-income, only 11 countries (26.8%) had a national smoke-free bar law.
TABLE 1.
Smoke-Free Workplace, Restaurant, and Bar Laws by Country Income Group Following Adoption of the World Health Organization Framework Convention on Tobacco Control: 2012
| Country Income Statusa | Indoor Workplaces, No. (%) | Restaurants, No. (%) | Bars, No. (%) |
|---|---|---|---|
| Low income (n = 36) | 6 (16.7) | 3 (8.3) | 3 (8.3) |
| Lower-middle income (n = 45) | 15 (33.3) | 14 (31.1) | 11 (24.4) |
| Upper-middle income (n = 44) | 18 (40.9) | 21 (47.7) | 22 (50.0) |
| High income (n = 41) | 7 (17.1) | 12 (29.3) | 11 (26.8) |
| Total countries (n = 166) | 46 (27.7) | 50 (30.1) | 47 (28.3) |
According to World Bank income group.
Ratifying the FCTC was associated with an increased probability of passing smoke-free indoor workplace, restaurant, and bar laws, with the strongest effect in the years immediately after ratification. Figure 2 shows the cumulative success function for passing indoor workplace, restaurant, and bar laws, with countries grouped by year since ratifying the FCTC. In the years immediately following ratification of the FCTC, the probability of a country adopting a smoke-free indoor workplace law increased strongly. The Cox proportional hazards regression showed that the FCTC significantly increased the probability of a country enacting smoke-free laws (Table 2 and Figure 2) in the years immediately following FCTC ratification, with the effect diminishing over time. The effect of the FCTC decayed slightly faster for indoor workplaces (τ = 4.5 years) than for restaurants and bars (τ = 5.5 years). These time constants correspond to half-lives, t1/2, of 3.1 and 3.8 years, respectively. This finding suggests that the effect of the FCTC is cut by half 3 to 4 years after ratification, and by three quarters after 6 to 8 years.
TABLE 2.
Effect of the World Health Organization Framework Convention on Tobacco Control Ratification on Smoke-Free Laws by Country Income Level: 2002–2012
| Indoor Workplaces (Half Lifea = 3.1 Y) |
Restaurants (Half Lifea = 3.8 Y) |
Bars (Half Lifea = 3.8 Y) |
||||
|---|---|---|---|---|---|---|
| Predictors | HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P |
| Income groupb | ||||||
| Low | 1.00 (0.33, 2.97) | .994 | 0.38 (0.12, 1.19) | .096 | 0.32 (0.09, 1.15) | .08 |
| Lower-middle | 1.77 (0.72, 4.36) | .217 | 0.96 (0.44, 2.08) | .914 | 0.82 (0.36, 1.90) | .65 |
| Upper-middle | 2.66 (1.12, 6.34) | .027 | 1.68 (0.83, 3.43) | .151 | 1.94 (0.94, 4.00) | .075 |
| High (Ref) | 1.00 | . . . | 1.00 | . . . | 1.00 | . . . |
| Time since ratifying the treaty, e−(t-1)/τ c |
19.38 (6.61, 56.84) | < .001 | 23.35 (7.69, 70.94) | < .001 | 23.50 (7.05, 78.32) | < .001 |
Note. CI = confidence interval; HR = hazard ratio.
The half-life of effect (t1/2) corresponds to the time constants, τ, of 4.5 years for indoor workplaces, and 5.5 years for restaurants and bars.
According to World Bank income group.
Time t set to 0 when countries had not yet ratified the Framework Convention on Tobacco Control. Hazard ratios correspond to a change in e−(t-1)/τ from 1 to 0.
Upper-middle–income countries had a greater probability of adopting smoke-free indoor workplace laws, independent of FCTC ratification. Compared with high-income countries, being an upper-middle–income country was associated with 2.66 times the odds of reaching FCTC compliance for indoor workplaces (Table 2). For restaurants and bars, income group was not significantly associated with enacting smoke-free laws.
DISCUSSION
Our results show that ratification of the FCTC, a public health treaty without an external means of enforcement and without a specified deadline for smoke-free areas, was associated with increased enactment of smoke-free indoor workplace, restaurant, and bar laws, compared with countries that did not ratify. These findings are similar to studies on the FCTC and graphic health warning labels for cigarette packages, showing that the FCTC accelerated adoption of such laws.6,7 These findings contrast, however, with the research on health warning labels, which found that the effect of the FCTC increased with time since ratification, although our use of a transformed time variable makes it more difficult to make comparisons with hazard ratios found in such research.6 Perhaps these differences are attributable to graphic health warning labels being a newer public health policy that emerged along the same time as the FCTC, whereas smoke-free legislation has been attempted around the world for decades.
This study, along with the previous studies on warning labels,6,7 shows that the FCTC, an international treaty, helped change countries’ domestic policies, accelerating policies to protect public health. These findings are in agreement with studies showing that treaties can change domestic policies in other issue areas, such as human rights and economic policy21–24; such studies find that treaties often do so by altering the policy discourse and activating key constituencies.21,22 In addition, as we found that many countries had not passed smoke-free laws even many years after FCTC ratification, our findings counter the perspective that treaties are often merely signed in cases where such policies are already planned.23,24 The FCTC did not lead every country to pass comprehensive smoke-free laws by 2012, but FCTC ratification still increased the odds of passing such laws.
In addition, independently of the FCTC, upper-middle–income countries also experienced a greater probability than high-income countries of adopting smoke-free indoor workplace laws. In lower- and middle-income countries, health advocates and authorities are frequently outmatched for resources by the tobacco industry.25 In past decades, tobacco-control efforts were most successful in high-income countries, but by the decade of the 2000s many upper-middle–income countries may have developed the resources to achieve such laws. The reduced probability of smoke-free laws among high-income countries, relative to upper-middle–income countries, may also be attributable to concentrated tobacco industry activities against smoke-free laws in high-income countries,10,26,27 including promoting ineffectual voluntary policies to forestall legislation, communications tactics such as “accommodation” of smoking, and policy diversion tactics such as promoting ventilated smoking areas.10–12 These tactics resulted in laws in several European countries that allowed smoking in designated smoking areas or ventilated areas rather than being smoke-free.28 Likewise, the lack of clear evidence for increased law passage for restaurants and bars in upper-middle–income countries may be the result of tobacco industry efforts to block such legislation by attempting to court the hospitality industry.9
For several tobacco-control provisions, the FCTC calls for countries to adopt measures by between 2 and 5 years after adoption.4 Although the FCTC does not specify a time frame for adopting smoke-free laws, this analysis suggests that most countries that adopted smoke-free laws for indoor workplaces, restaurants, and bars did so within 5 years after ratification. Although this study did not analyze smoke-free laws for outdoor areas, it may plausibly apply to outdoor areas as such laws develop.29 Yet, the fading of the effect of the FCTC over time suggests that if smoke-free laws do not pass in the years immediately after adoption of the FCTC, it may reflect strong tobacco industry influence beyond the impact of the treaty. It may also reflect a weakening of health advocates’ efforts in cases in which smoke-free legislation stalls. Health advocates should push for smoke-free legislation when countries adopt the FCTC, and should continue to push against tobacco industry influence in cases in which new legislation does not immediately pass.
Some countries may have passed FCTC-compliant smoke-free laws in anticipation of FCTC ratification. If this is the case, our estimates of the FCTC’s effect for the years immediately following ratification are probably biased downward.
The FCTC accelerated the adoption of smoke-free indoor workplace, restaurant, and bar laws, with the greatest effect in the years immediately following ratification of the convention. The effect faded as time passed, suggesting a need for a renewed effort by public health advocates to see that Article 8 of the FCTC is implemented in the 134 countries that, as of 2012, had ratified the FCTC but had not come into compliance with its provisions requiring protection of people from exposure to secondhand smoke.
Supplementary Material
Acknowledgments
This work was funded by National Cancer Institute grant CA-87472.
Note. The funding agency played no role in the selection of the research question, data collection and analysis, or preparation of the article. H. Hiilamo served without remuneration as an expert witness for a plaintiff in tobacco litigation, Salminen v. Amer Sports Oyj and BAT Finland in 2008 and in 2009.
Footnotes
Contributors
R. Uang conducted the analysis, verified the data, and drafted the article. H. Hiilamo had the idea for the article and did the initial data collection. S. A. Glantz helped design the analysis. All authors contributed to writing the article.
Human Participant Protection
Human participant protection was not required because the study did not involve human participants.
Contributor Information
Randy Uang, University of California San Francisco Center for Tobacco Control Research and Education, San Francisco, CA..
Heikki Hiilamo, Faculty of Social Sciences at Helsinki University, Helsinki, Finland..
Stanton A. Glantz, University of California San Francisco Center for Tobacco Control Research and Education, San Francisco, CA..
References
- 1.Tan CE, Glantz SA. Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation. 2012;126(18):2177–2183. doi: 10.1161/CIRCULATIONAHA.112.121301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services [Accessed January 23, 2015];The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Available at: http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf.
- 3.World Health Organization [Accessed January 23, 2015];Literature review on the health effects of smoke-free policies in light of the WHO FCTC. Available at: http://www.who.int/fctc/publications/Smoke_free_policies_FINAL_09052014.pdf.
- 4.World Health Organization [Accessed March 24, 2015];Framework Convention on Tobacco Control. Available at: http://whqlibdoc.who.int/publications/2003/9241591013.pdf.
- 5.World Health Organization [Accessed April 3, 2015];Parties to the Framework Convention on Tobacco Control. Available at: http://www.who.int/fctc/signatories_parties/en.
- 6.Sanders-Jackson AN, Song AV, Hiilamo H, Glantz SA. Effect of the Framework Convention on Tobacco Control and voluntary industry health warning labels on passage of mandated cigarette warning labels from 1965 to 2012: transition probability and event history analyses. Am J Public Health. 2013;103(11):2041–2047. doi: 10.2105/AJPH.2013.301324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hiilamo H, Glantz SA. Implementation of effective cigarette health warning labels among low and middle income countries: state capacity, path-dependency and tobacco industry activity. Soc Sci Med. 2015;124:241–245. doi: 10.1016/j.socscimed.2014.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . Tobacco Free Initiative; [Accessed April 9, 2015]. WHO Report on the Global Tobacco Epidemic, 2013: enforcing bans on tobacco advertising, promotion and sponsorship. Published data set. Available at: http://www.who.int/tobacco. [Google Scholar]
- 9.Dearlove JV, Bialous SA, Glantz SA. Tobacco industry manipulation of the hospitality industry to maintain smoking in public places. Tob Control. 2002;11(2):94–104. doi: 10.1136/tc.11.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez M, Glantz SA. Failure of policy regarding smoke-free bars in the Netherlands. Eur J Public Health. 2013;23(1):139–145. doi: 10.1093/eurpub/ckr173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mandel LL, Glantz SA. Hedging their bets: tobacco and gambling industries work against smoke-free policies. Tob Control. 2004;13(3):268–276. doi: 10.1136/tc.2004.007484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drope J, Bialous SA, Glantz SA. Tobacco industry efforts to present ventilation as an alternative to smoke-free environments in North America. Tob Control. 2004;13(suppl 1):i41–i47. doi: 10.1136/tc.2003.004101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Tobacco Documentation Centre . British American Tobacco; [Accessed June 25, 2014]. 1997. Smoking Issues Status Book (SISB): Public Smoking. Bates no. 800444612-800445178. Available at: http://legacy.library.ucsf.edu/tid/ipq53a99. [Google Scholar]
- 14.World Health Organization [Accessed April 3, 2015];WHO Report on the Global Tobacco Epidemic, 2008: the MPOWER package. Appendix II - Global tobacco control policy data. Available at: http://www.who.int/entity/tobacco/mpower/mpower_report_policy_data_2008.pdf.
- 15.Council of Ministers of the Soviet Union [Accessed March 4, 2015];Law 706, June 12, 1980, Measures to strengthen the struggle against smoking [in Russian] Available at: http://russia.bestpravo.ru/ussr/data02/tex13685.htm.
- 16.Tobacco Merchants Association . British American Tobacco; [Accessed March 4, 2015]. World alert. January 1, 1995. Bates no. 600031818-600031821. Available at: http://legacy.library.ucsf.edu/tid/hia60a99. [Google Scholar]
- 17.World Health Organization [Accessed April 3, 2015];WHO Report on the Global Tobacco Epidemic, 2013: enforcing bans on tobacco advertising, promotion and sponsorship. Appendix VI - Table 6.1: Public places with smoke-free legislation. Available at: http://www.who.int/entity/tobacco/global_report/2013/appendix_vi_table_6_1.pdf.
- 18.Hyland A, Barnoya J, Corral JE. Smoke-free air policies: past, present and future. Tob Control. 2012;21(2):154–161. doi: 10.1136/tobaccocontrol-2011-050389. [DOI] [PubMed] [Google Scholar]
- 19.Framework Convention Alliance [Accessed October 19, 2015];Nations at international tobacco control conference seize opportunity to protect people from secondhand smoke and save lives. 2007 Available at: http://www.fctc.org/publications/bulletins/doc_download/87-nations-at-international-tobacco-control-conference-seize-opportunity-to-protect-people-from-second.
- 20.Marshall MG, Cole BR. [Accessed April 9, 2015];State fragility index and matrix 2012. Available at: http://www.systemicpeace.org.
- 21.Simmons BA. Mobilizing for Human Rights: International Law in Domestic Politics. Cambridge University Press; Cambridge, England: 2009. [Google Scholar]
- 22.Dai X. Why comply? The domestic constituency mechanism. Int Organ. 2005;59(2):363–398. [Google Scholar]
- 23.Hathaway O. Why do countries commit to human rights treaties? J Conflict Resolut. 2007;51:588–621. [Google Scholar]
- 24.Von Stein J. Do treaties constrain or screen? Selection bias and treaty compliance. Am Polit Sci Rev. 2005;99(4):611–622. [Google Scholar]
- 25.Lee S, Ling PM, Glantz SA. The vector of the tobacco epidemic: tobacco industry practices in low and middle-income countries. Cancer Causes Control. 2012;23(suppl 1):117–129. doi: 10.1007/s10552-012-9914-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saloojee Y, Dagli E. Tobacco industry tactics for resisting public policy on health. Bull World Health Organ. 2000;78(7):902–910. [PMC free article] [PubMed] [Google Scholar]
- 27.Kashiwabara M, Armada F. Mind your “smoking manners”: the tobacco industry tactics to normalize smoking in Japan. Kobe J Med Sci. 2013;59(4):E132–E140. [PubMed] [Google Scholar]
- 28.Martínez C, Martinez-Sanchez JM, Robinson G, Bethke C, Fernandez E. Protection from secondhand smoke in countries belonging to the WHO European Region: an assessment of legislation. Tob Control. 2014;23(5):403–411. doi: 10.1136/tobaccocontrol-2012-050715. [DOI] [PubMed] [Google Scholar]
- 29.Martínez C, Guydish J, Robinson G, Martinez-Sanchez JM, Fernandez E. Assessment of the smoke-free outdoor regulation in the WHO European Region. Prev Med. 2014;64:37–40. doi: 10.1016/j.ypmed.2014.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.