Abstract
Compound muscle action potential (CMAP) and motor unit number estimation (MUNE) are electrophysiological techniques that can be used to monitor the functional status of a motor unit pool in vivo. These measures can provide insight into the normal development and degeneration of the neuromuscular system. These measures have clear translational potential because they are routinely applied in diagnostic and clinical human studies. We present electrophysiological techniques similar to those employed in humans to allow recordings of mouse sciatic nerve function. The CMAP response represents the electrophysiological output from a muscle or group of muscles following supramaximal stimulation of a peripheral nerve. MUNE is an electrophysiological technique that is based on modifications of the CMAP response. MUNE is a calculated value that represents the estimated number of motor neurons or axons (motor control input) supplying the muscle or group of muscles being tested. We present methods for recording CMAP responses from the proximal leg muscles using surface recording electrodes following the stimulation of the sciatic nerve in mice. An incremental MUNE technique is described using submaximal stimuli to determine the average single motor unit potential (SMUP) size. MUNE is calculated by dividing the CMAP amplitude (peak-to-peak) by the SMUP amplitude (peak-to-peak). These electrophysiological techniques allow repeated measures in both neonatal and adult mice in such a manner that facilitates rapid analysis and data collection while reducing the number of animals required for experimental testing. Furthermore, these measures are similar to those recorded in human studies allowing more direct comparisons.
Keywords: Behavior, Issue 103, neuromuscular diseases, compound muscle action potential, motor unit number estimation, electrophysiology, electrodiagnosis, sciatic nerve, mouse
Introduction
Motor unit number estimation (MUNE) was originally described by McComas et al. over three decades ago1. The original technique was a modification of the compound muscle action potential (CMAP) recording technique that employed a gradual increase of stimulation to obtain submaximal increments. These increments were summed and averaged to determine an estimated size of a single motor unit potential (SMUP). This size was divided into the CMAP response to estimate the number of motor units innervating the muscle being tested. Following the original description, numerous variations using both electrophysiological responses and incremental force (mechanical) measurements have been used in both human studies and animal models2. The MUNE technique was modified by Shefner and colleagues to investigate mouse models of Amyotrophic Lateral Sclerosis (ALS)3, 4.
In the current description, we detail simplified modifications of the MUNE techniques that are rapid to perform. Importantly, CMAP and MUNE allow reliable measures in both neonatal and adult mice5–8. Experienced individuals can perform these measures in 10–20 min per animal, and repeated measures are feasible which permits the acquisition of longitudinal data5. In the current studies, we employ a clinical electrodiagnostic system. In our experience, clinical electrodiagnostic systems are optimized for rapid and efficient capture of electrophysiological data in vivo, nevertheless standard electrophysiological rigs can easily be adapted for this application.
Protocol
This protocol was approved by and adheres to the animal care and ethics guidelines of the Ohio State University Wexner Medical Center.
1. Animal Preparation and Anesthesia
Wear gloves while handling mice.
- Anesthetize mice with inhaled isoflurane and place in the prone position. Induce anesthesia using 3–5% isoflurane and 1 L per minute O2 flow rate. Following induction of anesthesia, maintain anesthesia at 2–3% and 1 L per minute O2 flow rate.
- Adjust O2 flow and isoflurane percentage for adequate anesthesia according to animal’s disease state, age, and respiration rate. Smaller or weaker animals may require less isoflurane for adequate anesthesia (i.e.1.5–2.5% isoflurane).
- Confirm adequate anesthesia by applying light hindlimb footpad pressure with an object such as forceps to demonstrate a lack of withdrawal response.
Maintain temperature at 37 °C surface temperature with a thermostatic warming plate as variation in temperature can affect CMAP size and duration.
Apply veterinarian petroleum-based ointment to eyes to prevent dryness. Monitor level of anesthesia observing respiration rate and assessing for withdrawal responses following pressure applied to the foot pad via forceps. 5. Remove hair from the hindlimb to be studied using clippers. After removal of hair from the hindlimb(s) to be studied, lightly extend the hindlimbs at the knee, abduct at the hips and affix to the working surface using adhesive tape (as shown in Figure 1).
Following the CMAP and MUNE recordings and discontinuation of anesthesia, do not leave animal unattended until it has regained sufficient consciousness to maintain sternal recumbency. Do not return animal to the company of other animals until fully recovered.
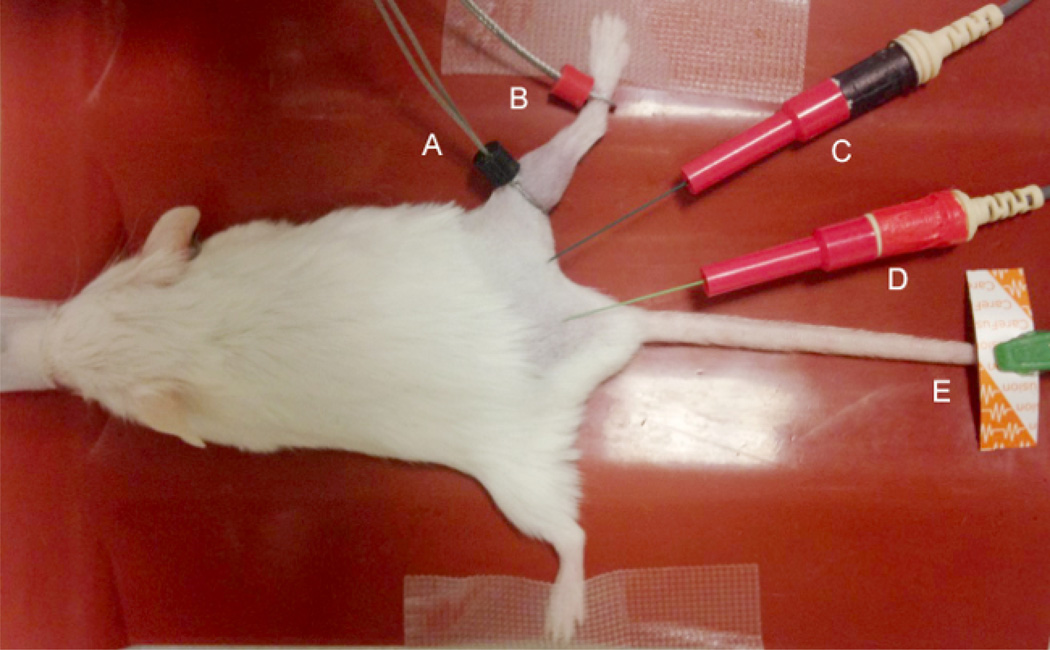
Figure 1. Electrode Placement.
The black (E1) “active” electrode (A) and red (E2) “reference” recording electrode (B) are placed over the gastrocnemius at the proximal portion of the gastrocnemius at the knee. The stimulating cathode (black) (C) and anode (red) (D) are inserted subcutaneously proximal to the recording electrodes to generate distal responses. A disposable disk electrode (D) is placed on the hind limb, tail or sacrum as a ground to minimize artifact.
2. Recording Setup and Equipment
Place the electrodes for the CMAP and MUNE recordings as pictured in Figure 1.
- Use two fine ring electrodes for the recording electrodes.
- Place the active (E1) ring electrode on the skin overlying the proximal portion of the gastrocnemius muscle of the hind limb, at the knee joint, and the reference (E2) ring electrode on the skin over mid-metatarsal portion of the foot.
- In order to reduce impedance, coat the skin underlying the ring electrodes with gel to sufficiently saturate residual hair and maximize electrode-skin contact. Avoid excessive application of electrode gel as this may cause an electrical bridge between electrodes and could prevent accurate recording.
- For stimulation of the sciatic nerve at the proximal hind limb, use two insulated 28 G monopolar needles as the cathode and anode. Insert the cathode at the region of the proximal hind limb and insert the anode more proximally in the subcutaneous tissue overlying the sacrum.
- Avoid inserting the stimulating electrodes overly close to the sciatic nerve or too deep that it would directly injury the sciatic nerve or other structure. Figure 1 illustrates electrode placement.
For the ground electrode, place a disposable surface electrode on the contralateral hind limb or tail.
3. Data Acquisition
- Sciatic CMAP
- Obtain sciatic CMAP responses by stimulating the sciatic nerve with square-wave pulses of 0.1 ms duration and intensity ranging from 1–10 mA.
- Acquire CMAP responses with increasing stimulus intensity until the amplitude of the response no longer increases. Then, in order to ensure supramaximal stimulation, increase the stimulation to ~120% of the stimulus intensity utilized to obtain a maximal response and obtain an additional response. If there is no further increase in the CMAP size, record this response as the maximal CMAP.
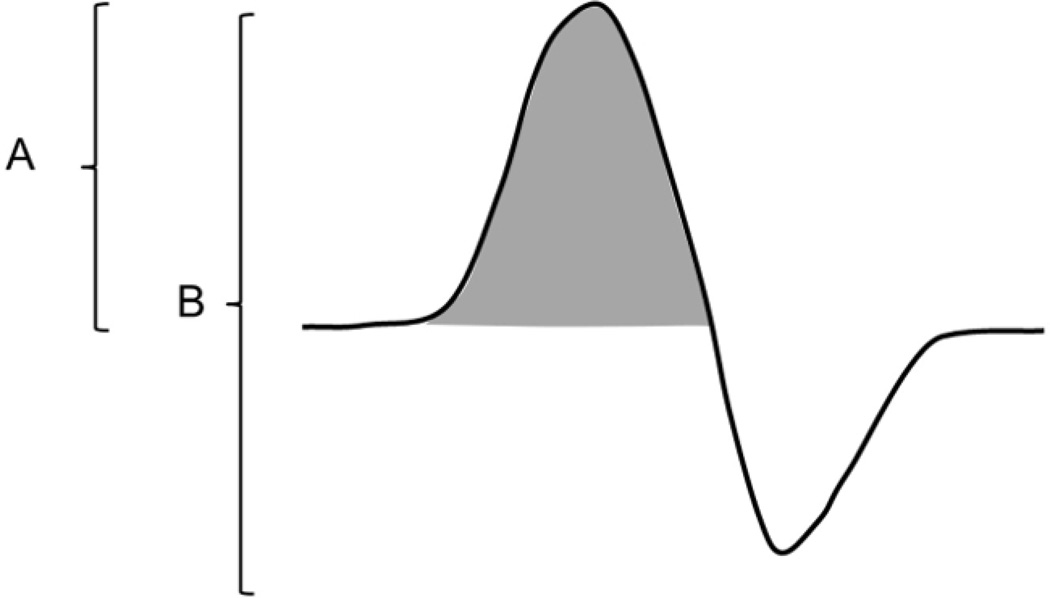
- Record baseline-to-peak and peak-to-peak CMAP amplitudes in mV (Figure 2).
- Average Single Motor Unit Potential (SMUP) Size and MUNE Calculation
- Determine the average single motor unit potential (SMUP) size with an incremental stimulation technique1. To obtain incremental responses, deliver submaximal stimulation of 0.1 ms duration at a frequency of 1 Hz while increasing the intensity in 0.03 mA steps to obtain the minimal all-or-none responses. Obtain the initial response with stimulus intensity between 0.21 mA and 0.70 mA.
- If the initial response does not occur with stimulus intensity between 0.21 mA and 0.70 mA, adjust the stimulating cathode position either closer or farther away from the position of the sciatic nerve in the proximal thigh to decrease or increase the required stimulus intensity, respectively.
- If the initial incremental response is obtained with a stimulus intensity between 0.21 mA and 0.70 mA and fulfills the criteria noted below (3.2.2), store and record additional increments with increasing stimulus intensities adjusting by steps of 0.03 mA to obtain a total of 9 additional increments that meet the established criteria.
- During measurements of the incremental responses, ensure that each increment meets the following criteria.
- Ensure that the initial negative peak of the incremental responses is aligned temporally within the negative peak of the maximal CMAP response shown as the shaded portion of the CMAP illustration in Figure 2.
-
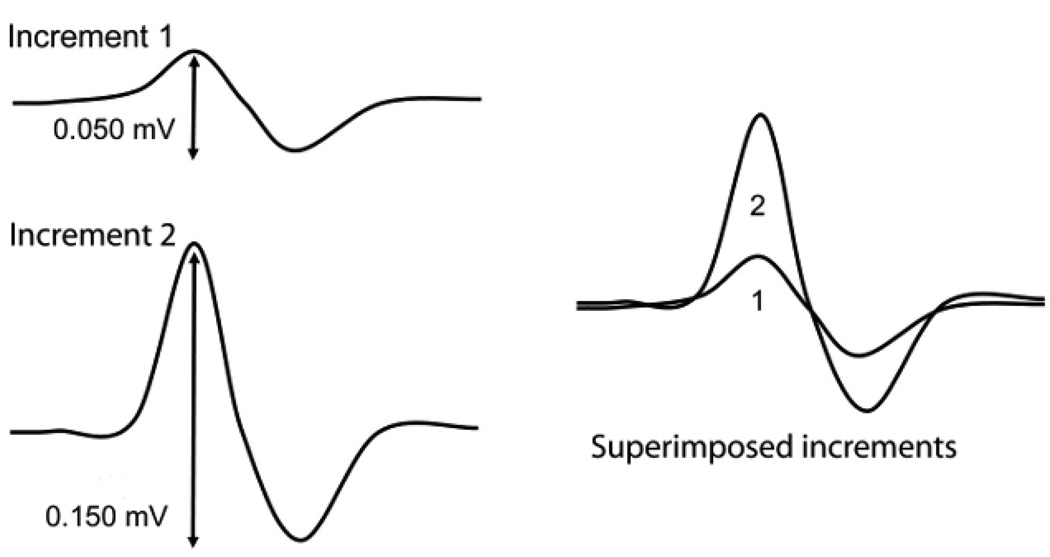
Ensure that each incremental response is stable and without fractionation, established by observing three duplicate responses. Distinguish visually incremental responses in real-time (superimposed on the previously recorded increments).Note: Each increment should be visually distinct and larger compared with the preceding response (Figure 3). Analysis in real-time allows recognition of larger amplitude (incremental) responses compared to prior responses, and small changes attributable to background noise can be disregarded. A superimposed view of 10 increments is shown in Figure 4 (B and D) to further illustrate this point.
- After visually confirming each increment, ensure that the measured amplitude difference (confirmed response-amplitude of the prior response=amplitude difference) is at least 25 µV.
- If the increment is less than 25 µV, discard and re-measure the response. After recording 10 incremental responses, assess the increments to ensure that the amplitude of each individual incremental response is not greater than 1/3 of the sum of all ten increments (i.e. the total amplitude of the final response). If this condition is not met, re-measure the incremental responses.
-
Average the 10 incremental values to give an estimation of the average single motor unit potential (SMUP) amplitude (Figure 3). Note: Figure 3 details the basis of the average SMUP calculation, but the average SMUP amplitude can be simply calculated by dividing the entire amplitude of the final incremental response by the total number of increments (i.e., 10).
Example individual SMUP calculations (illustrated in Figure 3):- SMUP 1=peak-to-peak amplitude of increment 1
- SMUP 1=0.050 mV
- SMUP 2= (peak-to-peak amplitude of increment 2) – (peak-to-peak amplitude of increment 1)
- SMUP 2=0.150 mV-0.050 mV=0.100 mV
- Calculate each subsequent increment (up to a total of 10), and make an average of the ten increments.
Calculate MUNE by dividing the maximum CMAP amplitude (peak-to-peak) by the average SMUP amplitude (peak-to-peak). (MUNE=CMAP/average SMUP). In some electrophysiological systems, the SMUP increments are measured in µV whereas CMAP is typically provided in mV. When necessary, convert CMAP and SMUP results to similar units prior to MUNE calculation.
Figure 2. Compound Muscle Action Potential.
Pictured is an illustration of a representative CMAP response. (A) The baseline-to-peak amplitude is measured from the isoelectric baseline to the initial negative peak (negative voltage is depicted above the baseline). (B) The peak-to-peak amplitude is measured from negative peak voltage to positive peak voltage. The grey-shaded area denotes the negative peak area.
Figure 3. Incremental responses.
Two representative incremental responses are shown superimposed and in isolation. For MUNE calculation amplitudes of each increment are measured peak-to-peak. Increment #1 is the initial all-or-none response recorded and represents a single motor unit potential (SMUP). Each subsequent increment (#2–10) represents a quantal increase superimposed on the prior response. Therefore to obtain the SMUP amplitudes for increments 2–10, the amplitude of the prior response is subtracted from the amplitude of the increment obtained.
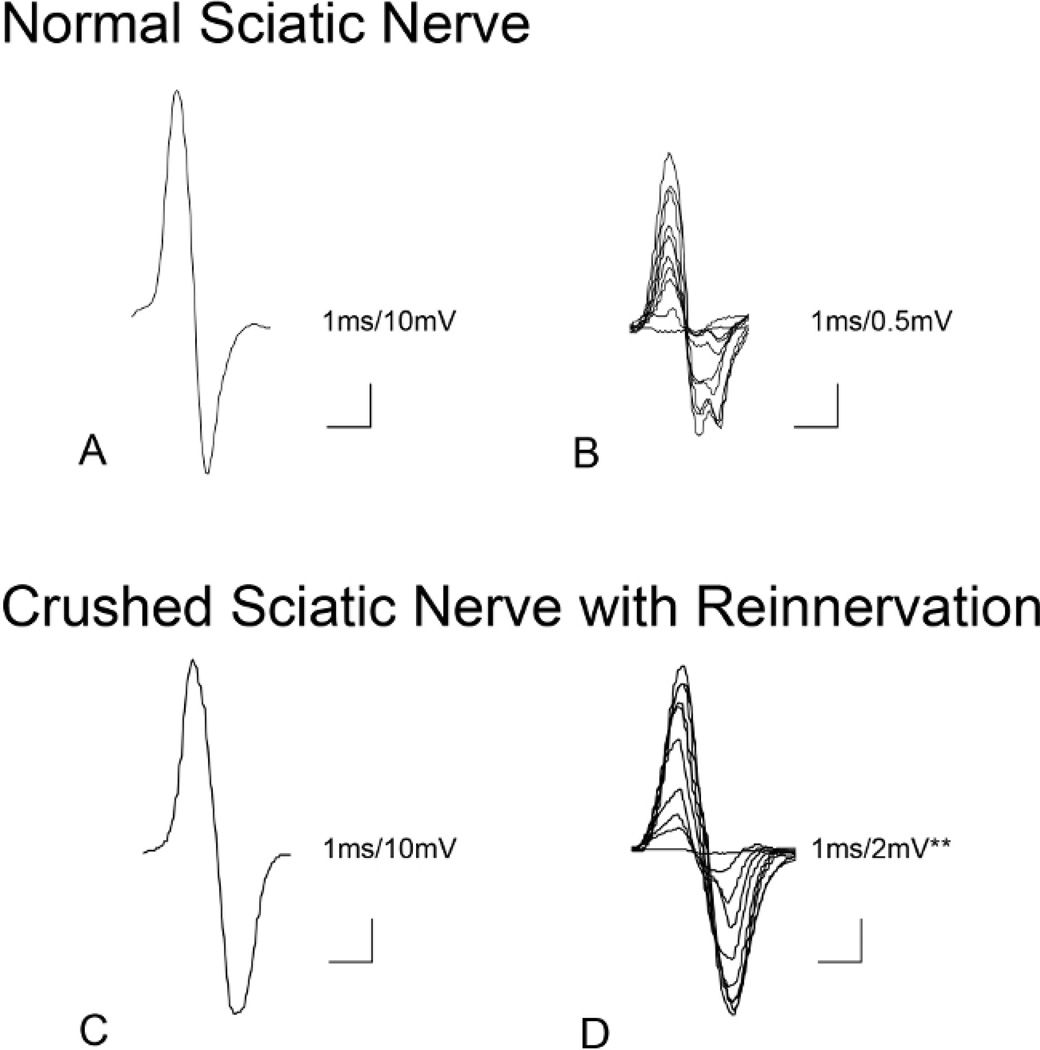
Figure 4. Example Sciatic CMAP and MUNE.
(A) Sciatic compound muscle action potential (CMAP) in an adult (6 months of age) control mouse with baseline-to-peak amplitude of 49.0 mV and peak-to-peak amplitude of 84.2 mV. Screen sensitivity=10 mV per division and screen duration 10 ms. (B) Ten corresponding incremental responses (in the control mouse) with total amplitude of 3.028 mV are divided by 10 to determine average SMUP size (0.3028 mV). Screen sensitivity=0.5 mV and sweep speed of 1 ms per division. Calculated MUNE=278 (MUNE=CMAP/average SMUP(84.2 mV/ 0.3028 mV)) (C) Sciatic CMAP 11 weeks following sciatic nerve crush in an adult mouse (6 months of age) showing mildly reduced baseline-to-peak amplitude (39.6 mV) and peak-to-peak amplitude (74.9 mV). Screen sensitivity=10 mV per division and sweep speed of 1 ms per division. (D) Ten corresponding incremental responses (in the mouse with nerve crush) with total peak–to–peak amplitude of 14.923 mV divided by 10 to obtain an average SMUP size of 1.4923 mV. Screen sensitivity=2 mV per division and a sweep speed of 1 ms per division. Calculated MUNE=50 (MUNE=CMAP/average SMUP (74.9 mV/1.4923 mV)). (**Note the different sensitivity for the incremental responses of the sciatic crush mouse).
Representative Results
The techniques of CMAP and MUNE described in this report allow recording of neuromuscular function of the sciatic innervated hind limb muscles utilizing minimally invasive electrode placement (Figure 1). Supramaximal CMAP size, which represents the total output from a muscle group, can be described using the parameters of amplitude and area (Figure 2), however, in the current methods, we use amplitude to quantify the CMAP and the SMUP sizes. Since the CMAP response measures summated depolarization of muscle fibers within a muscle, pathology anywhere from the motor neuron to the muscle fiber can result in reduction in CMAP size. Therefore, CMAP gives an excellent measure of the total functional status. As expected, CMAP size will increase during development5. Due to compensatory changes that can occur following denervation (i.e. collateral sprouting), CMAP size may be maintained despite processes of motor neuron or motor axonal loss. Therefore, the technique of MUNE is required to determine the motor neuron or axon input to the muscle or group of muscles being tested. Recording of individual increments (Figure 3) allows estimation of the average output of single motor units (SMUP size) to give more detailed information about functional status of motor units.
CMAP and MUNE can be utilized to measure neuromuscular function in various mouse models of neuromuscular disease. In Figure 4, findings in an adult control mouse and an adult mouse 11 weeks following sciatic nerve crush are contrasted. Following sciatic nerve crush, MUNE is severely reduced at 50 estimated functional motor units compared with normal findings of 278 functional motor units in the control mouse. In contrast, the CMAP amplitude in the crushed animal (39.6 mV baseline-to-peak, 74.9 mV peak-to-peak) shows only mild reduction compared to control (49.0 mV baseline-to-peak, 84.2 mV peak-to-peak) due to collateral sprouting.
Discussion
MUNE and CMAP are clinically relevant measures frequently utilized in research studies and in monitoring patients with neuromuscular disorders such as ALS and spinal muscular atrophy (SMA)9, 10. For instance, in SMA, CMAP and MUNE correlate well with age, severity and clinical measures of function10–14. Both measures are minimally invasive and allow assessment of function longitudinally in the same individual. Importantly, these measures cannot measure activation or recruitment of the motor unit by cortical motor neurons, but they provide a clinicallyrelevant assessment of the integrity of the motor neuron and its functional counterpart, the motor unit.
Animal models of neuromuscular disease are critical to an understanding of pathogenic mechanisms of human disease and to the preclinical development of potentially effective therapeutic agents. The ability to translate outcome measures and biomarkers that can be utilized across species can facilitate and hasten the translation of promising preclinical findings to human clinical trials. Several groups have previously utilized both electrophysiological and force (mechanical) measurements to estimate motor unit function in mouse models2–4, 15–22. Due to the relative complexity of the measures, we have refined these techniques in a visual format to allow more widespread use and implementation in mice.
The format of video demonstration and instruction, allows key steps of the procedure to be highlighted and potential pitfalls to be addressed. The application of these techniques to preclinical testing of potential therapies in motor neuron diseases may improve the translation of putative therapies from mice to human disease.
There are several critical steps in the process of acquiring the CMAP and MUNE responses. Proper and consistent recording electrode placement and sufficient electrode contact with the hind limb are critical for reproducible measurement of amplitude and to decrease background noise. Therefore, close contact between hind limb skin and electrodes should be consistently confirmed. We have found that surface electrodes offer more consistent CMAP and MUNE recordings than needle electrodes. Due to very thin subcutaneous tissues, small movements of needle recording surface may lead to wide variation in CMAP amplitudes. Additionally, the more invasive nature of needle electrodes is not optimal for neonatal mice or longitudinal studies due to potential muscle disruption and injury. One potential drawback of non-selective, surface electrode recordings relates to the possibility of diminished phenotype resolution if a particular muscle is more or less involved compared with another, and this has been reported in an ALS mouse model21.
Acquiring the average SMUP size is technically more challenging compared to the CMAP. Due to the smaller response size (in the range of µV rather than mV) background noise can be more problematic. Background noise can be reduced by adjusting the ground electrode, cathode, anode, and checking other electrical equipment near the experimental setup. A Faraday cage, typically used for intracellular electrophysiology applications, is not required. Visual determination of the individual SMUP responses is the most difficult skill to acquire and takes practice for consistent results with adequate repeatability. It is important to ensure that the SMUPs that are being recorded initiate within the duration of the maximal CMAP response. We have defined criteria for acceptance of individual incremental responses to make this process more straightforward to perform and to increase intra- and inter-rater reliability.
One potential drawback of the incremental MUNE technique includes the possibility of overestimating the number of functional motor units due to alternation of motor units. We have used a technique similar to Shefner et al. in that each response should be reproducibly seen a total of 3 times to reduce the impact of this phenomenon3.
In our experience, clinical electrodiagnostic systems are optimized for the studies described herein due to improved examiner-electrodiagnostic system interface ergonomics allowing ease of control. The two-channel system utilized in our lab is equipped with two non-switched amplifier channels using an amplifier with 24 bit Analog to Digital Converter and a sampling rate of 48 kHz per channel. Hardware gain can be adjusted from 10nV to 100 mV/division. The low frequency filter has a range from 0.2 Hz-5 kHz, and the high frequency filter settings range from 30 Hz-10 kHz. A constant-current stimulator is used (intensity: 0–100 mA; duration: 0.02–1 ms). Most clinical systems have similar appropriate features and can be adjusted to adequately record CMAP and MUNE responses. Additionally, standard electrophysiological rigs can be assembled to adequately record CMAP and MUNE, but the interface may need to be adjusted for ease of stimulation adjustment and rapid identification of CMAP and SMUP responses.
We have previously utilized the techniques of CMAP and MUNE described here to allow rapid and reproducible assessment of the sciatic innervated muscle of the hind limb in mice during the early postnatal period to adulthood5. These techniques allow assessment in mouse models when behavioral testing for motor function is not feasible or is less reliable. Application of this technique to neonatal mice facilitates the study of motor unit development and has the potential to expand our understanding of motor neuron innervation and pruning. For instance, we have shown that the number of functional motor units recorded with MUNE will increase during pruning from polyneuronal to mononeuronal innervation during the first two weeks of life in neonatal mice5. The ability to test mice over long periods of time with this technique lends itself to the study of motor unit response to peripheral nerve injury, hereditary neuromuscular disorders and aging.
Acknowledgements
WDA is supported by grant funding from NIH-NICHD (5K12HD001097-17) and Cure SMA. SJK is supported by grant funding from NINDS (K08NS067282 and U01NS079163).
Footnotes
Video Link
The video component of this article can be found at http://www.jove.com/video/52899/
Disclosures
The authors have nothing to disclose.
References
- 1.McComas AJ, Fawcett PR, Campbell MJ, Sica RE. Electrophysiological estimation of the number of motor units within a human muscle. Journal of neurology, neurosurgery, and psychiatry. 1971;34(2):121–123. doi: 10.1136/jnnp.34.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shefner JM. Motor unit number estimation in human neurological diseases and animal models. Clinical Neurophysiology. 2001;112(6):955–964. doi: 10.1016/s1388-2457(01)00520-x. [DOI] [PubMed] [Google Scholar]
- 3.Shefner JM, Cudkowicz ME, Brown RH. Comparison of incremental with multipoint MUNE methods in transgenic ALS mice. Muscle & Nerve. 2002;25(1):39–42. doi: 10.1002/mus.10000. [DOI] [PubMed] [Google Scholar]
- 4.Shefner JM, Cudkowicz M, Brown RH., Jr Motor unit number estimation predicts disease onset and survival in a transgenic mouse model of amyotrophic lateral sclerosis. Muscle Nerve. 2006;34(5):603–607. doi: 10.1002/mus.20628. [DOI] [PubMed] [Google Scholar]
- 5.Arnold WD, et al. Electrophysiological Biomarkers in Spinal Muscular Atrophy: Preclinical Proof of Concept. A. nnals of clinical and translational neurology. 2014;1(1):34–44. doi: 10.1002/acn3.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li J, et al. A comparison of three electrophysiological methods for the assessment of disease status in a mild spinal muscular atrophy mouse model. PloS one. 2014;9(10):e111428. doi: 10.1371/journal.pone.0111428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Srivastava AK, et al. Mutant HSPB1 overexpression in neurons is sufficient to cause age-related motor neuronopathy in mice. Neurobiology of disease. 2012;47(2):163–173. doi: 10.1016/j.nbd.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yalvac ME, Arnold WD, Hussain SR, et al. VIP-expressing dendritic cells protect against spontaneous autoimmune peripheral polyneuropathy. Molecular therapy: the journal of the American Society of Gene Therapy. 2014;22(7):1353–1363. doi: 10.1038/mt.2014.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gooch CL, et al. Motor unit number estimation: A technology and literature review. Muscle Nerve. 2014;50(6):884–893. doi: 10.1002/mus.24442. [DOI] [PubMed] [Google Scholar]
- 10.Arnold WD, Kassar D, Kissel JT. Spinal muscular atrophy: diagnosis and management in a new therapeutic era. Muscle Nerve. 2014 doi: 10.1002/mus.24497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Swoboda KJ, et al. Natural history of denervation in SMA: Relation to age, SMN2 copy number, and function. Annals of Neurology. 2005;57(5):704–712. doi: 10.1002/ana.20473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finkel RS. Electrophysiological and motor function scale association in a pre-symptomatic infant with spinal muscular atrophy type I. Neuromuscular Disorders. 2013;23(2):112–115. doi: 10.1016/j.nmd.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Kaufmann P, et al. Prospective cohort study of spinal muscular atrophy types 2 and 3. Neurology. 2012;79(18):1889–1897. doi: 10.1212/WNL.0b013e318271f7e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arnold WD, Burghes AH. Spinal muscular atrophy: The development and implementation of potential treatments. Annals of Neurology. 2013;74(3):348–362. doi: 10.1002/ana.23995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li J, Sung M, Rutkove SB. Electrophysiologic biomarkers for assessing disease progression and the effect of riluzole in SOD1 G93A ALS mice. PloS one. 2013;8(6):e65976. doi: 10.1371/journal.pone.0065976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngo ST, et al. The relationship between Bayesian motor unit number estimation and histological measurements of motor neurons in wild-type and SOD1 (G93A) mice. Clin Neurophysiol. 2012;123(10):2080–2091. doi: 10.1016/j.clinph.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 17.Shefner JM. Recent MUNE studies in animal models of motor neuron disease. Supplements to Clinical neurophysiology. 2009;60:203–208. doi: 10.1016/s1567-424x(08)00021-4. [DOI] [PubMed] [Google Scholar]
- 18.Souayah N, Potian JG, Garcia CC, et al. Motor unit number estimate as a predictor of motor dysfunction in an animal model of type 1 diabetes. American journal of physiology Endocrinology and metabolism. 2009;297(3):E602–E608. doi: 10.1152/ajpendo.00245.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou C, et al. A method comparison in monitoring disease progression of G93A mouse model of ALS. Amyotrophic lateral sclerosis: official publication of the World Federation of Neurology Research Group on Motor Neuron Diseases. 2007;8(6):366–372. doi: 10.1080/17482960701538759. [DOI] [PubMed] [Google Scholar]
- 20.Feng XH, Yuan W, Peng Y, Liu MSs, Cui LY. Therapeutic effects of dl-3-n-butylphthalide in a transgenic mouse model of amyotrophic lateral sclerosis. Chinese medical journal. 2012;125(10):1760–1766. [PubMed] [Google Scholar]
- 21.Mancuso R, Santos-Nogueira E, Osta R, Navarro X. Electrophysiological analysis of a murine model of motoneuron disease. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2011;122(8):1660–1670. doi: 10.1016/j.clinph.2011.01.045. [DOI] [PubMed] [Google Scholar]
- 22.Lee Yi, Mikesh M, Smith I, Rimer M, Thompson W. Muscles in a mouse model of spinal muscular atrophy show profound defects in neuromuscular development even in the absence of failure in neuromuscular transmission or loss of motor neurons. Developmental biology. 2011;356(2):432–444. doi: 10.1016/j.ydbio.2011.05.667. [DOI] [PMC free article] [PubMed] [Google Scholar]