Abstract
Background
Previous studies of Long QT Syndrome (LQTS) have focused primarily on the clinical course of affected patients up to 40 years of age to avoid the confounding influence of acquired heart disease on LQTS-related cardiac events in this genetic disorder.
Methods
Patients were identified as having coronary disease if they had a history of hospitalization for myocardial infarction, coronary angioplasty, coronary artery bypass graft surgery, or were treated with medication for angina. LQTS-related cardiac events included the first occurrence of syncope, aborted cardiac arrest, or sudden cardiac death without evidence suggestive of an acute coronary event. Cox proportional hazards regression modeling was used to analyze the independent contribution of coronary disease to LQTS-related cardiac events.
Results
Time-dependent coronary disease was associated with an increased risk of LQTS-related cardiac events (hazard ratio 2.24, 95% confidence interval 1.23–4.07, p=0.008) after adjustment for syncopal history before age 40, QTc, and gender. Factors such as diabetes and hypertension that increase the risk for coronary disease were not associated with an increased risk for LQTS-related cardiac events.
Conclusions
This is the first study to demonstrate that coronary disease augments the risk for LQTS-related cardiac events in LQTS. The findings highlight the need for more focused preventive therapy in LQTS patients above the age of 40.
Keywords: Long QT Syndrome, Cardiac Events, Coronary Disease
The Long QT Syndrome (LQTS) is a genetic disorder characterized by delayed ventricular repolarization that is manifest on the ECG as QTc prolongation. Affected patients have an increased propensity for syncope due to transient ventricular tachyarrythmias (torsades de pointes) and for sudden cardiac death due to ventricular fibrillation.1 Previous research has identified ten LQTS genotypes, with most mutations affecting either potassium or sodium ion channels.2 Over 95% of known mutations involve just three genes: KCNQ1 (LQT1), HERG (LQT2), and SCN5A (LQT3). Monogenetic mutations in these LQTS genes exhibit autosomal dominant inheritance with variable penetrance.
Previous studies on LQTS have focused primarily on the clinical course of affected patients within the first four decades of life.3–6 These studies have identified the following risk factors for LQTS-related cardiac events: QTc prolongation, male gender before adolescence, female gender after adolescence, prior syncope, and the post-partum period after pregnancy in childbearing women. Beta-blockers (BB) have been shown to be effective in reducing risk in patients affected with LQTS.7 This study looks at the relatively unexplored age group of LQTS patients over 40 years of age, with investigation of the influence of coronary disease (CD) on LQTS-related cardiac events.
METHODS
Study population
The study population was drawn from the International Long QT Registry.5 All active patients enrolled in the Registry provided informed consent, and the University of Rochester Medical Center Research Subjects Review Board approved the study. Subjects in the Registry over 40 years of age were selected for investigation, as overt CD is rare before age 40. Selection criteria required survival beyond age 40 in LQTS Registry subjects who had an ECG with QTc ≥450ms and answered a prospective follow-up questionnaire regarding the age of non-LQTS-related comorbidities related to coronary disease, hypertension, and diabetes mellitus. A total of 641 patients met the QTc entry criteria. Genetic studies identified 282 subjects with an LQTS-related mutation using standard genetic tests.
Clinical data were collected on prospectively designed forms that included patient demographics, patient and family history, cardiac events, and start and termination dates of specific LQTS therapies. Copies of ECGs were obtained at enrollment, with the earliest one being designated as baseline. The QT interval was corrected for heart rate by Bazett’s formula.8
Patients were identified as having CD if they indicated on the medical questionnaire the date when they had been hospitalized for a myocardial infarction, coronary angioplasty, coronary artery bypass graft surgery, or were prescribed medication for the treatment of angina pectoris.
LQTS end points included syncope manifest by transient loss of consciousness that was sudden in onset and offset; aborted cardiac arrest (ACA) that required external defibrillation during resuscitation; or LQTS-related sudden cardiac death (SCD) that was unexpected, exclusive of a known cause, and not associated with chest pain or clinical evidence suggestive of a coronary event. The clinical information surrounding each end point was collected as part of our prospective Registry and categorized according to prespecified criteria.
Statistical analysis
Graphical display of the time to the LQTS end point before and after experiencing a coronary event utilized the Mantel-Byar method.9 Cox proportional hazards regression modeling was used to analyze the independent contribution of the first CD diagnosis to the likelihood of experiencing an LQTS-related end point.10 The age at which coronary heart disease was first diagnosed was handled as a time-dependent covariate in the Cox model. Beta-blocker therapy was included in the Cox model as a time-dependent covariate using the dates when this therapy was initiated and stopped. The Cox model was stratified by the decade in which study patients were born to account for changes in the baseline hazard function for different calendar time-periods. The four stratification periods used were dates of births before 1930, 1930–1939, 1940–1949, 1950–1959, and 1960 and later. This approach was used to help account for changes over time, especially in the use of beta-blocker therapy. Interaction of time-dependent beta-blocker therapy in patients with and without prior syncope and in those with and without CD was evaluated. All tests were 2-sided, and statistical significance was set at the 0.05 level. The statistical software used for Cox models was SAS version 9.13 (SAS Institute, Inc, Cary, NC).
RESULTS
Clinical characteristics of the study population are presented in Table 1. LQTS patients with CD were more likely to be males with longer QTc intervals, had a higher frequency of diabetes mellitus and hypertension, and had a greater probability of being treated with beta-blockers and implanted defibrillators.
Table 1.
Clinical Characteristics of the LQTS Study Population
| Parameters | Total Population n=641 | No Coronary Disease n=554 | Coronary Disease n=87 |
|---|---|---|---|
| Female | 451 (70) | 397 (72) | 54 (62) |
| Age range (yrs) | 41–92 | 41–92 | 41–83 |
| Mean age at baseline ECG | |||
| Baseline QTc findings | |||
| QTc (ms) | 489 ± 43 | 488 ± 43 | 491 ± 41 |
| 450–499 ms | 452 (71) | 396 (71) | 56 (64) |
| ≥500 ms | 189 (29) | 158 (29) | 31 (36) |
| Syncope before age 40 | 213 (33) | 185 (33) | 28 (32) |
| Genotype positive | 282 | 244 | 38 |
| LQT1 | 135 (48) | 120 (50) | 15 (39) |
| LQT2 | 128 (46) | 107 (44) | 21 (55) |
| LQT3 | 19 (7) | 17 (7) | 2 (5) |
| Co-morbidity | |||
| Diabetes mellitus | 44 (7) | 27 (5) | 17 (20) |
| Hypertension | 192 (30) | 143 (26) | 49 (56) |
| Cardiac therapy, any time | |||
| Beta-blockers | 413 (64) | 340 (61) | 73 (84) |
| Implantable defibrillator | 107 (17) | 81 (15) | 26 (30) |
| Pacemaker | 59 (9) | 47 (8) | 12 (14) |
| Left sympathetic ganglionectomy | 14 (2) | 11 (2) | 3 (3) |
| 1st diagnosis of coronary disease | 87 (14) | - | 87 (100) |
| Angina pectoris | 41 (6) | - | 41 (47) |
| Coronary angioplasty | 20 (3) | - | 20 (23) |
| Coronary artery bypass surgery | 10 (2) | - | 10 (11) |
| Myocardial infarction | 16 (2) | - | 16 (18) |
| 1st LQTS-related cardiac event | 98 (15) | 83 (15) | 15 (17) |
| Syncope | 88 (14) | 76 (14) | 12 (14) |
| Aborted cardiac arrest | 9 (1) | 6 (1) | 3 (3) |
| Sudden cardiac death | 1 (0.1) | 1 (0.2) | 0 (0) |
Values in parentheses are percentages.
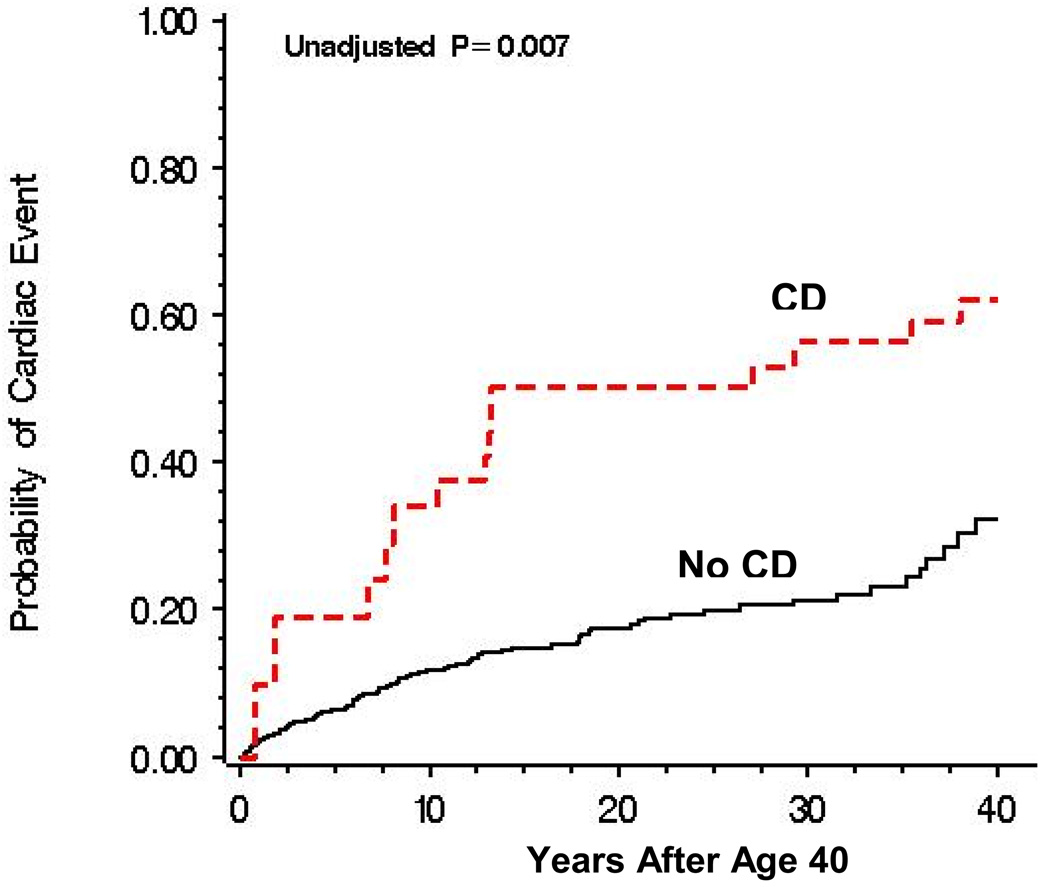
The probability of an LQTS-related cardiac event for those who did and did not develop CD after age 40 is presented in Figure 1. Patients with CD had a significantly higher event rate than those without CD, and the increased risk from CD for LQTS-related cardiac events occurred largely between age 40 and 60 years.
Figure 1. Mantel-Byar Analysis of Outcome by Coronary Disease Status.
Graphic presentation of the probability of a 1st time-dependent LQTS-related cardiac event before and after the development of symptomatic coronary disease (CD) in LQTS patients 41 to 80 years of age with QTc ≥ 450ms.
The results from the Cox analysis for the LQTS patients are presented in Table 2. Time-dependent CD and prior syncope make significant and independent contributions to the risk for LQTS events while adjusting for known LQTS risk factors (QTc>500ms, females, and syncope before age 40). Beta-blockers, when added to the risk model as a time-dependent covariate, did not make a significant contribution to the risk model (p = 0.24). Neither time-dependent hypertension nor time-dependent diabetes made a significant contribution to the risk model. The overall findings were very similar when analysis was restricted to the 282 genotype-positive patients. The event rates in each of the three genotype-positive patient groups were too low to evaluate the risk of CD on LQTS-related cardiac events by specific genotype.
Table 2.
Cox model: Factors Associated with Risk for a 1st LQTS-related Cardiac Event in 641 Patients Older than 40 years of Age with QTc ≥ 450ms
| Variable | Hazard Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|
| Time-dependent coronary disease | 2.24 | 1.23 – 4.07 | 0.008 |
| QTc ≥ 500ms | 1.22 | 0.83 – 1.81 | 0.31 |
| Females | 1.19 | 0.77 – 1.84 | 0.44 |
| Prior Syncope | 3.72 | 2.44 – 5.67 | < 0.0001 |
| Time-dependent beta-blockers | 0.76 | 0.48 – 1.20 | 0.24 |
Note: QTc≥500ms, female gender, and time-dependent beta-blockers were forced into the model. Neither diabetes mellitus or hypertension made a significant contribution to the model. Time-dependent beta-blockers utilized decade stratification of patients by date of birth (see Methods).
Time-dependent beta-blocker therapy had a significant effect in reducing LQTS events in patients with prior syncope (HR 0.56, 95% CI 0.32 – 0.97; p value = 0.04), but no meaningful effect in those patients without prior syncope (HR 1.27 95% CI 0.66 – 2.44; p = 0.47). This bidirectional effect of beta-blockers on LQTS events in those with and without a history of syncope before age 40 reflects an interaction that approaches significance (p=0.052). No meaningful interaction was evident between beta-blockers and CD for LQTS events.
DISCUSSION
We found that in LQTS patients over age 40 years, development of CD is an independent and significant risk factor for LQTS-related cardiac events. Syncope before age 40 is an independent and significant risk factor. Factors such as diabetes and hypertension that increase the risk for CD were not associated with an increased risk for LQTS-related cardiac events.
The altered substrate in CD (ischemia, scar, and possibly reduced ejection fraction) may lower the threshold for afterdepolarization in LQTS, a critical factor in the initiation of torsade de pointes that is thought to be the arrhythmogenic mechanism in LQTS-related cardiac events.11 Only one patient died suddenly in this study population. It is unclear whether the use of implantable cardioverter defibrillators in 15% of the patients without CD and 30% of the patients with CD contributed to this low sudden cardiac death rate. We do not have information on the frequency of life-saving appropriate shock therapy in these defibrillator-treated patients. However, when these defibrillator patients were excluded from the analysis, the findings in the Cox risk model were essentially unchanged.
Beta-blockers were utilized in a majority of the patients, and this medication was not associated with a significant reduction in cardiac events in the overall study population (Table 2). However, beta-blockers were associated with a significant reduction in cardiac events in the higher-risk patients who had syncope before age 40 (hazard ratio=0.56, p=0.04). This finding is consistent with our prior experience in younger LQTS patients in which beta-blocker efficacy was evident only in higher-risk patients.3,4
An important question relates to the accuracy of the diagnosis of CD in this study population. We relied exclusively on data from a prespecified medical questionnaire that was completed by all study participants older than 40 years of age. Patient recall is generally quite good for hospitalizations related to acute myocardial infarction, coronary angioplasty, or coronary artery bypass surgery. The diagnosis of angina is a bit softer, but we required for this diagnosis that the patient had physician-prescribed antianginal sublingual nitrate therapy for treatment of chest pain. We feel confident that the diagnosis of CD was accurate in these patients, but we may have missed the diagnosis of CD in a small percentage of patients who experienced coronary symptoms but responded negatively to the questionnaire. Unfortunately, we do not have information from hospital records or coronary angiographic data to verify the diagnosis of CD, and we have no data on the severity of the coronary disease or associated myocardial dysfunction.
Since CD can produce cardiac arrhythmias that result in syncope, aborted cardiac arrest, and sudden cardiac death, is it appropriate to categorize these events as LQTS-related cardiac end points, especially in the over 40 age group? Syncope is a frequent event in LQTS and relatively infrequent in CD, and syncope dominated the events in this study and accounted for more than 50% of the end points (Table 1), much like the findings in several of our prior LQTS studies in patients younger than 40 years of age.3,4
This is the first study to investigate the influence of CD on LQTS risk in older LQTS patients. The development of CD is associated with increased risk for LQTS-related cardiac events, especially syncope, and this finding highlights the need for more effective preventive therapy when coronary disease develops in older LQTS patients.
Acknowledgments
Supported in part by research grants HL-33843 and HL-51618 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD.
REFERENCES
- 1.Moss AJ. Long QT Syndrome. JAMA. 2003;289:2041–2044. doi: 10.1001/jama.289.16.2041. [DOI] [PubMed] [Google Scholar]
- 2.Splawski I, Shen J, Timothy KW, et al. Spectrum of mutations in long-QT syndrome genes. KVLQT1, HERG, SCN5A, KCNE1, and KCNE2. Circulation. 2000;102:1178–1185. doi: 10.1161/01.cir.102.10.1178. [DOI] [PubMed] [Google Scholar]
- 3.Hobbs JB, Peterson DR, Moss AJ, et al. Risk of aborted cardiac arrest or sudden cardiac death during adolescence in the long-QT syndrome. Jama. 2006;296:1249–1254. doi: 10.1001/jama.296.10.1249. [DOI] [PubMed] [Google Scholar]
- 4.Sauer AJ, Moss AJ, McNitt S, et al. Long QT syndrome in adults. J Am Coll Cardiol. 2007;49:329–337. doi: 10.1016/j.jacc.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 5.Moss AJ, Schwartz PJ, Crampton RS, et al. The long QT syndrome. Prospective longitudinal study of 328 families. Circulation. 1991;84:1136–1144. doi: 10.1161/01.cir.84.3.1136. [DOI] [PubMed] [Google Scholar]
- 6.Priori SG, Schwartz PJ, Napolitano C, et al. Risk stratification in the long-QT syndrome. N Engl J Med. 2003;348:1866–1874. doi: 10.1056/NEJMoa022147. [DOI] [PubMed] [Google Scholar]
- 7.Moss AJ, Zareba W, Hall WJ, et al. Effectiveness and limitations of beta-blocker therapy in congenital long-QT syndrome. Circulation. 2000;101:616–623. doi: 10.1161/01.cir.101.6.616. [DOI] [PubMed] [Google Scholar]
- 8.Bazett JC. An analysis of the time relations of electrocardiograms. Heart. 1920;7:353–367. [Google Scholar]
- 9.Byar DP, Mantel N. Some interrelationships among the regression coefficient estimates arising in a class of models appropriate to response-time data. Biometrics. 1975;31:943–947. [PubMed] [Google Scholar]
- 10.Cox DR. Regression models and life-tables. J Stat Soc [B] 1972;34:187–220. [Google Scholar]
- 11.Kass RS, Moss AJ. Long QT syndrome: novel insights into the mechanisms of cardiac arrhythmias. J Clin Invest. 2003;112:810–815. doi: 10.1172/JCI19844. [DOI] [PMC free article] [PubMed] [Google Scholar]