Abstract
Objective
To examine associations between food insecurity, excess body weight, psychosocial factors and food behaviors among low-income African-American (AA) families.
Design
Cross-sectional survey of participants in the baseline evaluation of the B’More Healthy Communities for Kids (BHCK) obesity prevention trial. We collected data on socioeconomic factors, food source destinations, acquiring food, preparation methods, psychosocial factors, beliefs and attitudes, participation in food assistance programs, anthropometry and food security. We used principal component analysis to identify patterns of food source destinations and logistic regression to examine associations.
Setting
Fourteen low-income, predominantly AA neighborhoods in Baltimore City.
Subjects
298 adult caregiver-child (10–14 years old) dyads.
Results
41.6% of households had some level of food insecurity, and 12.4% experienced some level of hunger. Food insecure participants with hunger were significantly more likely to be unemployed and to have lower incomes. We found high rates of excess body weight (overweight and obese) among adults and children (82.8% and 37.9% food insecure without hunger; 89.2% and 45.9% with hunger, respectively), although there were no significant differences by security status. Food source usage patterns, food acquisition, preparation, knowledge, self-efficacy and intentions did not differ by food security. Food security was associated with perceptions that healthy foods are affordable and convenient. Greater caregiver body satisfaction was associated with food insecurity and excess body weight.
Conclusions
In this setting, obesity and food insecurity are major problems. For many food insecure families, perceptions of healthy foods may serve as additional barriers to their purchase and consumption.
Keywords: African American, Food insecurity, Obesity, Behavioral intentions, Perceptions
INTRODUCTION
The coexistence of food insecurity and obesity has been identified in diverse ethnic minorities and low-income settings (1; 2; 3; 4; 5; 6). African-American (AA) populations living in urban areas in United States have high rates of obesity (45.0%) and related chronic diseases (7). Compared to the general population, AAs also have a higher prevalence of food insecurity (1;8; 9), with 24.6% of AA households experiencing food insecurity in 2012, compared to 14.5% of US households overall (8). Poverty exacerbates these associations (8).
A possible explanation for the association between food insecurity and obesity is that families in limited resource conditions may compromise dietary quality in exchange for calories (2;10; 11; 12). Budgetary constraints may result in increased purchasing of low-cost, non-nutrient rich and energy-dense foods, and decreased consumption of healthy foods, such as fruit and vegetable (1;2;3; 4; 11;12). Likewise, federal food assistance programs that target hunger and food insecurity seem to play a key role in this phenomenon (1;3;9; 13;14). Food insecurity is defined as a household-level economic and social condition of limited or uncertain access to adequate food, whereas hunger is an individual-level physiological condition caused by a lack of food (15). Participation in the Supplemental Nutrition Assistance Program (SNAP) has been directly associated with obesity in women (3;16), and with unhealthier food patterns for AA populations, especially at the beginning and end of the monthly benefit cycle (12;13;17).
Differential food access is another possible explanation for the link between food insecurity and less healthy food choices among ethnic minority populations (9;11;14;18;19;20). Urban neighborhoods that are both low-income and predominantly AA tend to have limited access to healthy food sources (e.g., supermarkets) (18;21), as well as greater access to corner stores and other types of convenience stores that are associated with higher obesity and chronic disease rates (19;21;22).
The majority of studies on the relationship between food security and obesity have focused on socioeconomic factors (1;3; 4; 10; 17; 23; 24) and energy and nutrient intake (12; 13; 24; 25), and little is known about other factors influencing food decisions made by minority populations (4;26). In Baltimore City, AA food insecure households have shown greater healthy eating self-efficacy and healthier food acquisition compared to food secure households, even though they were less likely to adopt healthy cooking methods (26). The literature is conflicting regarding the relationship between food-related psychological factors (1;26;27), access to food in the context of food insecurity (4;11;20), and food-related behaviors, such as the allocation of economic resources (2;28). Additionally, to date few studies have investigated how beliefs and attitudes towards health and body weight influence food security and nutritional status.(2;3)
In the current study, we conjectured that adult caregivers who reported higher levels of food insecurity will show poorer household food acquisition patterns, be less likely to buy foods at grocery stores and fresh produce markets, be more likely to visit local convenience stores, and be less likely to show positive psychosocial factors (such as higher knowledge, intentions and self-efficacy) for making healthier food choices and performing healthful cooking practices, and show more reserved attitudes towards healthier eating and body weight satisfaction for themselves and their children. We address the following questions:
How do child and adult overweight and obesity differ by food security status among our sample?
What are the relationships between adult food-related attitudes, psychosocial factors and behaviors with household food insecurity and child and adult excess body weight?
METHODS
Study Setting and Design
A cross-sectional survey was administered to participants in the baseline phase of B’More Healthy Communities for Kids (BHCK), an ongoing five-year obesity prevention trial that aims to increase the demand for and access to healthy and affordable foods through integrated interventions at the individual, family, youth-leader, recreation center, food store, carryout restaurant, wholesaler, and policy levels (19).
The study sample came from 14 low-income and predominantly AA neighborhoods in Baltimore City that were considered food deserts (29) i.e. a geographic area where the distance to a supermarket is more than one quarter of a mile; the median household income is at or below 185 percent of the federal poverty level; over 40% of households have no vehicle available; and the average Healthy Food Availability Index score for supermarkets, convenience and corner stores is lower than that of the food sources located in areas where the majority of the population is white. Fourteen recreation centers were selected as central points from which to define the geographic zones.
Sampling
Households were recruited from within low-income AA neighborhoods as part of baseline data collection for the parent study. To be eligible the family needed to: 1) reside within a mile and a half radius of a recreation center; 2) have at least one child between 10–14 years old; 3) have no intention of moving within two years; 4) have a caregiver who was the primary food shopper for the household willing to participate. Among households recruited and screened as eligible, 24 were selected to be interviewed in each recreation zone (a description of the randomization method can be found elsewhere (19)). If a selected household was unable to complete the interview, then the next eligible one was chosen from a recruitment list of 2250 eligible households.
We obtained an average of 21 household interviews per recreation zone (n= 298). 13% of households approached agreed to be part of the study.
This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB). Families signed the written informed consent and received $50 (total) in gift cards for participation. Parents provided consent for their child to participate and children provided written assent.
Measures
The 176-item Adult Impact Questionnaire (AIQ) included items to measure demographics and household socioeconomic information (sex, education, marital status, employment status, and household income, and housing arrangement), food source purchasing, acquisition of non-prepared foods for the household, food preparation methods, psychosocial factors, household participation in food assistance programs, anthropometry and food security.
The data were collected between June 2013 and June 2014, through interviews with the adult caregiver primarily responsible for household food purchasing and preparation. Interviews lasted on average 90 minutes. Data collectors were public health students and staff who underwent extensive training and received certification on the study instruments. Data were checked for errors and missing information by the interviewer and a second party following each interview, after which they were entered and cleaned by a third party.
Food source destinations
We assessed the most common food sources used in the past 30 days (How many times did you purchase or get foods from the following locations?). Food sources were categorized: farmers’ market in the city; local or urban farm stand; mobile produce cart; street food vendor; public market; the Virtual Supermarket Program; local corner store; supermarket or grocery store; wholesale food store; local carryout; fast food chain restaurant; specialty store (i.e., bakery, African store, coffee shop); sit-down restaurant, bar or pub; convenience store; food pantry; church or community center; family and/or friends).
Food acquisition patterns
Food acquisition, preparation, health beliefs and attitudes and psychosocial factors scales were developed and assessed for internal consistency reliability using Cronbach’s alpha.
Household food acquisition patterns were determined based on how often the household acquired selected foods over the past 30 days (How many times did you get these foods?). It is important to note that food acquisition encompasses food that was purchased outright, purchased with food safety net program benefits (SNAP, WIC), and food that was obtained for free. A 54-food item list was designed: (1) based on previous research done in this community (26;27) (2) formative research with the population of interest(19) and (3) to reflect items that would be promoted during the BHCK intervention. The healthier food acquisition score was the sum of the frequency of obtaining 27 healthy foods for each respondent (n=296). Additive scores ranged from 2 to 315 with a mean of 39.31 (SD = 30.54, alpha = 0.79). Similarly, the less-healthy food acquisition score was a sum of the frequency of acquiring 27 less-healthy foods during the same recall period (n=294). Scores ranged from 6 to 311 with a mean of 54.47 (SD = 39.77, α = 0.78). High scores indicate that foods were obtained more frequently. The healthier and less-healthy food items are presented in the Box 1 (supplementary material).
Healthy Food Preparation
We asked participants to rank the top three most common cooking methods used when they prepared meats (e.g. fish, chicken, turkey, pork, beef, including bacon and ground meat); eggs; greens (except lettuce) and potatoes. Cooking methods were assigned scores as follows: deep fry, or pan fry with butter or margarine (−2); pan fry with oil, or not prepared at home (−1); pan fry, drained (0); broiled, boiled, grilled, steamed, microwaved, baked without added fat, pan fry without oil, pan fry with water, raw, use of cooking spray, pan fry, drained and rinsed with hot water (+2). The healthy food preparation score was calculated by the weighted mean score for each food, taking into account the following proportion: 60% (first method), 30% (second method), and 10% (third method). Finally, the scores for all 8 foods were calculated and totaled to obtain an overall score for each household (n=290). Total healthiness of food preparation scores ranged from −2.67 to +4.93 with a mean of 1.38 (SD = 1.45, α = 0.54).
Healthy food beliefs and attitudes
Using a 5-item Likert scale, we developed four subscales to represent different dimensions about beliefs and attitudes towards healthy food: Affordability (three items); Convenience (three items); Importance (three items); and Taste (one item). We also developed a Body Image and Health subscale (three items). The subscale items are presented in the Box 2 (supplementary material). The level of agreement or disagreement with each of the six positive statements were coded as: strongly disagree (1), disagree (2), undecided (3), agree (4) or strongly agree (5); and inversely coded for the remaining seven negative statements. Total scores ranged from 3 to 15 with a mean of 9.67 (SD = 2.92, α = 0.76) for Affordability; from 3 to 15 with a mean of 10.08 (SD = 2.00, α = 0.42) for Convenience; from 4 to 15 with a mean of 12.44 (SD = 1.88, α = 0.59) for Importance; and from 1 to 5 with a mean of 3.93 (SD = 0.94) for Taste. Higher beliefs and attitudes scores on healthy foods reflect that the respondent showed a positive predisposition to behave consistently favorably towards healthy food choices because they believe that they are affordable, convenient, important to family’s health and palatable. Total scores ranged from 3 to 15 with a mean of 8.87 (SD = 2.78, α = 0.61) for the body image and health subscale. Higher belief and attitude scores on body image reflected caregiver body weight satisfaction for themselves and their children.
Food-related psychosocial factors
Psychosocial constructs were based on Social Cognitive Theory (See Box 3 in the supplementary material).(30) Eleven questions assessed the level of caregiver food and nutrition knowledge related to food purchasing, food preparation and understanding of information from nutrition facts labels. Food knowledge scores were calculated for each household by summing the number of correct responses to questions (n=297). The range for these scores was 2 to 11 with a mean of 7.08 (SD = 1.76, α = 0.42).
Ten questions about intentions for healthy eating focused on how respondents intend to purchase and prepare food for themselves and their children. The responses were scored by assigning 2 points to the healthiest option, 1 point to a less healthy choice, and 0 to the least healthy choice. Scores ranged from 2 to 20 with a mean of 11.31 (SD = 4.16, α = 0.72; n=293). Higher healthy eating intention scores indicated that the respondent had a positive inclination toward healthy eating.
Ten self-efficacy questions elicited the respondent’s level of confidence in performing daily food-related activities, such as making healthier food choices, using nutrition facts labels and performing healthful cooking practices. The responses were based on the options: would be very easy, somewhat difficult, very difficult, or impossible to do regularly, and responses were scored from 3 to 0, respectively. Total scores ranged from 11 to 30 with a mean of 24.82 (SD = 3.82, α = 0.68; n=298).
We had missing data values for some of the scales (healthier food acquisition 2; less-healthy acquisition, 4; food preparing, 8; knowledge, 1; intention, 5). We handled the missing data by dropping those participants from the analyses.
Anthropometric measures
We directly measured weights and heights of 298 adults/caregivers and 283 eligible children in the same household, using a Seca 213 Portable Measuring Rod stadiometer and a Tanita BF697W Duo Scale. Respondents were weighed and measured barefoot, in their clothes, removing only heavy outerwear. Body Mass Index (BMI) was obtained calculating kg/m². Overweight was defined for adults as BMI between 25 and 29.99 kg/m² and obesity as BMI greater than or equal to 30 kg/m². BMI for children up to 14 years old was assessed using BMI-for-age, according to WHO Child Growth Standards (31). Overweight was defined as a BMI-for-age ≥ 1 and < 2 z-score and obesity ≥ 2 z-scores for children of the same age and sex.
Household food security status
Food security was assessed by the 18-item USDA Household Food Security Scale for households with children under 18 years old (8;32). Household food security was determined by the number of food insecure conditions and reported behaviors reported in the past 12 months. The questions measured a cluster of situations related to the experience of food availability and the physiological state of hunger; perceptions that the food eaten by adults or children was inadequate in quality; instances of reduced food intake, or consequences of reduced intake; and instances of reduced food intake or its consequences for children. Responses to each question were coded as either affirmative (yes, sometimes true, often true, almost every month, some months but not every month) or negative (no, never true, only one or two months). We coded food security according to the methods of Bickel et al (32). Food security status was coded using recommended scale values (32). For the analysis, food insecure households with moderate and severe hunger were combined.
Data analysis
Descriptive statistics were calculated for demographic characteristics, attitudinal, psychosocial and behavioral variables, food security and excess body weight status. One-way ANOVA, Chi-square tests (2-sided) and Fisher’s Exact Test were used to compare the groups by food security status. For all analyses p ≤ 0.05 was the level of significance.
We performed a Principal Component Analysis (PCA) to derive patterns of food source use by adults, reducing the list of 17 types of food source destinations to a few key patterns. For better interpretation of the factors obtained (patterns), these were submitted to orthogonal rotation using the Varimax. We used eigenvalues >1.0 to establish the number of factors to be retained and assessments of proportion of variance accounted for by these factors. In interpreting the rotated factor pattern, a selected food source was considered to load on a given factor if the factor loading (FL) was > 0.6 (33). The retained set of factor scores were saved as continuous variables, and mean scores were calculated by food security status.
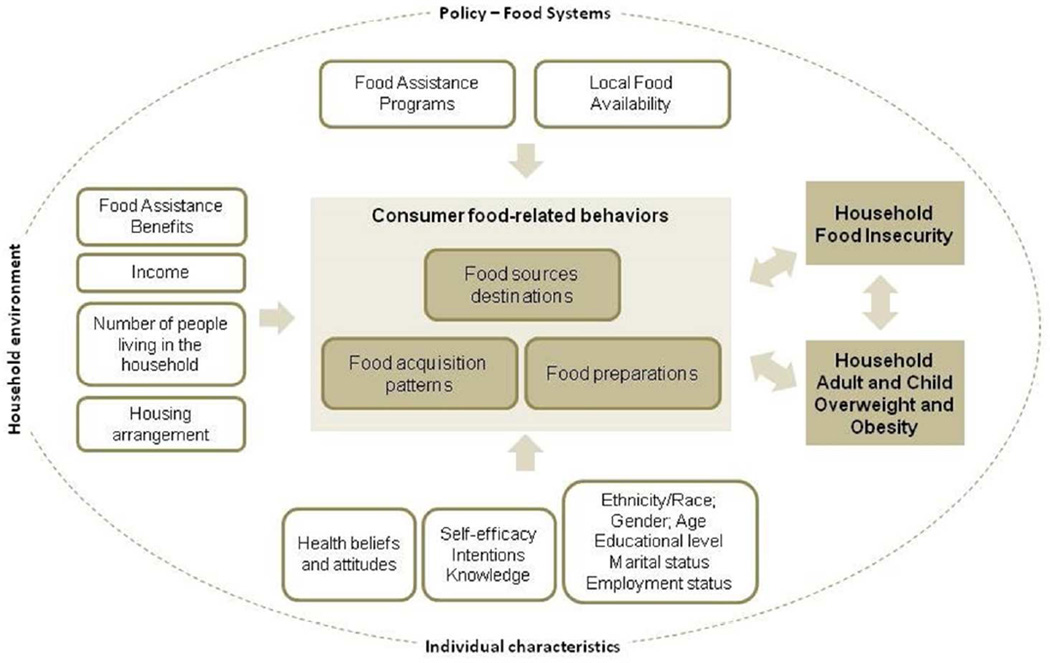
We used logistic regression analysis to assess the association between attitudinal, psychosocial and behavioral variables (which were each dichotomized with a median-split to compare higher versus lower levels) with two dichotomous outcomes at the household level: (I) food insecurity (food insecure without hunger, food insecure with moderate hunger and food insecure with severe hunger combined and compared to those who were food secure) and (II) excess body weight (adult and/or child overweight and obese at the same home). On the basis of our conceptual framework (Figure 1) and hypothesis, we first examined the unadjusted models for the following independent variables: patterns of food source destinations (rotated factors generated by PCA), psychosocial scores (knowledge, intentions, and self-efficacy), attitudinal scores (affordability, convenience, importance, taste and body image), healthier and less-healthy food acquisition scores and food preparation score. Finally, we examined all models adjusted for the following sociodemographic covariates caregiver age (continuous), gender, education (high school completed or high school not completed), marital status (indicator variables: never married; divorced/separated or widowed; married), employment status (indicator variables: unemployed or looking for work; student or seasonal work; employed full or part time), housing arrangement (indicator variables: transitional housing/shelter/group house/other; live with family who own/rent the property; rent or own property), number of people and children living in the household, and food assistance benefits received in the past 12 months (SNAP and Special Supplemental Nutrition Program for Women and Infants and Children - WIC). Alpha was set at p<0.05. All analyses were performed using SPSS software (version 16.0, SPSS Inc., Chicago, IL, USA).
Figure 1.
Conceptual framework to understand the relationship between consumer food-related behaviors, household food insecurity and excess of body weight
Our primary models for excess body weight were defined by both the child and the adult caregiver in the same household being overweight or obese. In sensitivity analyses, we assessed whether results would be substantively different had we analyzed adult and child overweight/obesity in separate models.
RESULTS
Description of the study sample
We found that 41.6% of households had some level of food insecurity, with 12.4% reporting having experienced moderate or severe hunger in the previous year (Table 1). The majority of adult respondents were female who were never married and had completed at least 12 years of formal education.
Table 1.
Socioeconomic characteristics of the BHCK adult study sample by household food security status (n=298)
| Food security status |
|||
|---|---|---|---|
| Food Secure (n=174) |
Food Insecure |
||
| without hunger (n=87) |
with hunger (n=37) |
||
| Individual characteristics | |||
| Age (years), mean (SD)‡ | 39.2 (9.8) | 38.8 (9.0) | 37.7 (10.2) |
| Female (%)§ | 83.9 | 88.5 | 89.2 |
| Education >12 years (%)∥ | 83.8 | 72.4 | 75.7 |
| Marital status (%)∥ | |||
| Never married | 58.8 | 63.2 | 54.1 |
| Married | 25.3 | 19.5 | 18.9 |
| Separated and divorced | 12.9 | 12.6 | 27.0 |
| Employment status (%)∥ | |||
| Employed (full-time or part-time) | 56.3* | 53.3† | 35.1* † |
| Seasonal and student | 10.9* | 3.5* † | 16.2† |
| Unemployed/looking for work | 6.3* † | 17.4* | 21.6† |
|
Participation in food assistance programs in the past 12 months (%) |
|||
| SNAP§ | 73.6 | 78.2 | 81.1 |
| WIC§ | 25.9 | 16.1 | 21.6 |
| Free or reduced cost school breakfast ∥ | 86.8 | 89.7 | 86.5 |
| Free or reduced cost school lunch ∥ | 87.4 | 92.0 | 89.2 |
| Head Start or daycare assistance ∥ | 12.1 | 10.3 | 8.1 |
| Household characteristics | |||
| Housing arrangement (%)∥ | |||
| Own property | 21.3 | 12.6 | 10.8 |
| Rent | 69.0 | 75.9 | 73.0 |
| Live with family who own/rent the property |
8.0 | 8.0 | 8.1 |
| Transitional housing, shelter or group house |
1.7 | 3.4 | 8.1 |
| Number of people living in the household, mean (SD)‡ |
4.5 (1.5)* | 5.1 (1.9)* † | 4.2 (1.6) † |
| Number of children under 18 years of age, mean (SD)‡ |
2.6 (1.4)* | 3.2 (1.6)* † | 2.4 (1.5) † |
| Annual household income less than $20,000 (%)§ |
44.2* | 54.8 | 62.9* |
| Income-to-poverty ratio¶ < 1.00§ | 57.1 | 67.5 | 60.0 |
One-way ANOVA with Bonferroni post hoc test to compare the groups
Pearson Chi-square to compare the groups (2-sided)
Fisher’s Exact Test to compare the groups (2-sided)
Source: U.S. Census Bureau, Weighted Average Poverty Thresholds, 2012.
Significant differences between groups (p-value < 0.05)
Sociodemographic associations with food security
Food insecure households with hunger were significantly less likely to have full-time or part-time employment (35.1%) compared to food insecure without hunger (53.3%) and food secure households (56.3%). Seasonal jobs and student status were more prevalent among both food secure (10.9%) and food insecure households with hunger (16.2%) compared to those that were food secure without hunger. We also observed a significantly higher number of family members (mean=5.1, SD=1.9) and children (mean=3.2, SD=1.6) among food insecure households without hunger compared to food secure (mean=4.5, SD=1.5; mean=2.6, SD=1.4, respectively) and food insecure with hunger (mean=4.2, SD=1.6; mean=2.4, SD=1.5, respectively). Most of the food insecure households with hunger had annual household income less than $20,000 (62.9%), and this proportion was significantly lower for food secure households (44.2%). A high proportion of food secure (57.1%) and insecure households (without hunger, n=67.5%; and with hunger, n=60.0%) showed an income-to-poverty ratio under 1.0, indicating that their average income for respective family size is below the official definition of poverty.
Excess body weight and food security status
We found marginally higher rates of adult and child overweight in our sample among low-income food secure AA households, but higher proportions of adult and child obesity for those with food insecurity with hunger, even though differences were not statistically significant across the groups (Table 2). The proportions of overweight or obese among individuals living in food insecure households with hunger were 89.2% for adults and 40.5% for children.
Table 2.
Proportion of overweight and obesity by food security status among low-income AA households in Baltimore City
| Food security status †* |
|||
|---|---|---|---|
| Food Secure | Food Insecure |
||
| without hunger | with hunger | ||
| Adult (%) (n=298) | |||
| Overweight‡ | 20.1 | 18.4 | 16.2 |
| Obesity§ | 66.1 | 64.4 | 73.0 |
| Child (%) (n=283) | |||
| Overweight ∥ | 28.7 | 20.7 | 21.6 |
| Obesity¶ | 14.4 | 16.1 | 18.9 |
| Household** (%) (n=283) | |||
| Overweight ‡,∥ | 4.0 | 5.7 | 2.7 |
| Obesity§,¶ | 10.9 | 11.5 | 16.2 |
Pearson Chi-square to compare the groups (2-sided)
BMI 25 – 29.99 (kg/m²) (WHO)
BMI ≥30 (kg/m²) (WHO)
BMI-for-age ≥ 1 and < 2 z-score for children of the same age and sex (WHO Child Growth Standards)
BMI-for-age ≥ 2 z-score for children of the same age and sex (WHO Child Growth Standards)
Adult and child overweight and obese in the same household
No significant differences were found between groups (p-value < 0.05)
Food-related behaviors and psychosocial factors associated with food security status
Table 3 shows the seven patterns of food sources destinations used to acquire food in the past month. Factor 1 was labeled “Convenience store shopping” – and reflects a purchasing pattern based on the habit of getting foods at corner stores and prepared foods from restaurants, such as carry-outs and fast-food restaurants. Factor 2 – “Grocery store shopping” – indicates acquiring foods at supermarkets, grocery and wholesale food stores. The use of street food vendors and the support from family members and friends to acquire foods for the household are exhibited by Factor 3, named “Social support and local shopping”. Factor 4 – “Eating out and online grocery shopping” – corresponds to the use of sit-down restaurants and the Virtual Supermarket program (a city-run free grocery delivery program for food desserts) to buy food. Acquiring food at public markets and specialty stores comprises Factor 5, entitled “Covered market shopping”. The habit of buying fresh produce at a local or urban farm stand contributes inversely (FL= −0.74) to the Factor 6 (“Farmers market shopping”), but this healthy habit also shows a positive relation to Factor 7 (“Mobile produce market shopping”) reflecting frequent use of Arabber or mobile produce cart (FL=0.63). No significant differences of means between the food security groups were found by food source use pattern.
Table 3.
Patterns of use of food sources destinations most often used for household food acquisition among low-income AA households in Baltimore City (n=298)
| Households | Food sources destinations |
||||||
|---|---|---|---|---|---|---|---|
| Factor 1† | Factor 2† | Factor 3† | Factor 4† | Factor 5† | Factor 6† | Factor 7† | |
| Total | local carry-out (0.85) |
supermarket or grocery store (0.77) |
street food vendor (0.80) |
sit-down restaurant, bar or pubs (0.64) |
public market (0.75) |
local or urban farm stand (−0.74) |
Arabber or m obile produce cart (0.63) |
| chain fast-food restaurant (0.74) |
wholesale food store (0.62) |
family and friends (0.70) |
Virtual Supermarket program (0.63) |
specialty store (0.74) |
Food pantry (−0.66) |
||
| local corner store (0.69) |
|||||||
| Variance‡ | 11.06% | 9.43% | 9.06% | 8.06% | 7.88% | 6.63% | 6.50% |
| Mean (SD) § * | |||||||
| Food Secure (n=174) |
−0.01 (1.04) | 0.03 (1.03) | 0.04 (1.20) | 0.03 (1.00) | −0.01 (1.10) | 0.04 (0.79) | −0.09 (0.94) |
| Food Insecure without hunger (n=87) |
−0.00 (0.99) | −0.11 (0.88) | −0.03 (0.63) | −0.19 (0.80) | 0.03 (0.90) | −0.10 (1.39) | 0.07 (0.69) |
| Food Insecure with hunger (n=37) |
0.05 (0.87) | 0.01 (0.90) | −0.13 (0.64) | 0.67 (1.31) | −0.03 (0.73) | 0.03 (0.85) | 0.29 (1.64) |
Factors extracted by Principal Component Analysis adopting eigenvalues >1.0 criterion. Factor loading (FL) value according to patterns extracted using rotation method Varimax with Kaiser Normalization. FL (in brackets) value >0.6 were maintained in the pattern.
Variance explained (%) of each factor retained. Cumulative variance of the 7 obtained factors: 58.61%.
One-way ANOVA with Bonferroni post hoc test to compare the groups
No significant differences were found between groups (p-value < 0.05)
No associations between participation in food assistance programs and food-related psychosocial factors and behaviors were found (results not shown).
In unadjusted and adjusted models, no significant differences were observed in food source usage pattern, frequency of food acquisition and healthiness of food preparation method by food security groups (Table 3 & Table 5).
Table 5.
Factors associated with food insecurity and excess of body weight among low-income urban African-American families with children
| Household | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Food Insecurity† | Excess Body Weight‡ | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unadjusted model | Adjusted model§ | Unadjusted model | Adjusted model§ | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| OR | (95%CI) | OR | (95%CI) | OR | (95%CI) | OR | (95%CI) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Patterns of food sources destinations ∥ | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Convenience store shopping (factor 1) | 0.79 | (0.49–1.27) | 0.79 | (0.41–1.54) | 1.21 | (0.75–1.94) | 1.51 | (0.81–2.81) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Grocery store shopping (factor 2) | 0.66 | (0.41–1.06) | 0.69 | (0.35–1.36) | 0.90 | (0.56–1.45) | 1.06 | (0.56–1.99) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Social support and local shopping (factor 3) | 1.02 | (0.64–1.64) | 1.02 | (0.53–1.98) | 0.73 | (0.45–1.17) | 0.72 | (0.39–1.35) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Eating out and online grocery shopping (factor 4) | 0.91 | (0.57–1.46) | 0.79 | (0.40–1.55) | 0.92 | (0.57–1.48) | 1.05 | (0.55–2.00) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Covered market shopping (factor 5) | 1.20 | (0.75–1.93) | 1.24 | (0.63–2.44) | 1.37 | (0.85–2.21) | 1.42 | (0.75–2.71) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Farmers market shopping (factor 6) | 0.88 | (0.55–1.41) | 0.80 | (0.41–1.54) | 0.89 | (0.55–1.43) | 0.73 | (0.39–1.37) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mobile produce market shopping (factor 7) | 1.00 | (0.62–1.60) | 0.90 | (0.46–1.76) | 0.82 | (0.51–1.32) | 0.72 | (0.38–1.36) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Food-related behaviors ∥ | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Healthier food acquisition | 1.03 | (0.64–1.65) | 1.09 | (0.56–2.11) | 0.93 | (0.58–1.50) | 1.04 | (0.55–1.96) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Less-healthy food acquisition | 1.08 | (0.67–1.73) | 1.19 | (0.62–2.28) | 0.98 | (0.61–1.57) | 0.98 | (0.53–1.82) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Healthy food preparation | 0.83 | (0.51–1.34) | 0.84 | (0.43–1.62) | 1.10 | (0.68–1.79) | 0.97 | (0.52–1.83) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Healthy Food Beliefs and Attitudes ∥ | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Affordable | 0.34 | (0.20–0.58)* | 0.16 | (0.07–0.35)* | 0.80 | (0.49–1.30) | 0.88 | (0.46–1.67) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Convenient | 0.59 | (0.36–0.98)* | 0.50 | (0.25–1.01) * | 0.63 | (0.38–1.05) | 0.43 | (0.21–0.85)* | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Important | 0.88 | (0.55–1.41) | 0.84 | (0.44–1.61) | 1.28 | (0.80–2.07) | 1.36 | (0.73–2.56) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Tastes good | 0.76 | (0.43–1.34) | 0.62 | (0.28–1.36) | 0.95 | (0.54–1.66) | 0.80 | (0.38–1.67) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Body image satisfaction | 0.55 | (0.34–0.89)* | 0.78 | (0.40–1.53) | 0.59 | (0.37–0.96)* | 0.51 | (0.26–0.97)* | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Food-related psychosocial factors ∥ | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Food and nutrition knowledge | 0.63 | (0.39–1.01) | 0.81 | (0.42–1.59) | 0.83 | (0.51–1.34) | 0.67 | (0.35–1.25) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Intentions on healthy eating | 0.89 | (0.55–1.44) | 0.85 | (0.43–1.68) | 1.24 | (0.77–2.00) | 1.03 | (0.54–1.96) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Healthy eating self-efficacy | 0.93 | (0.57–1.50) | 0.74 | (0.37–1.45) | 1.48 | (0.90–2.41) | 1.50 | (0.78–2.87) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
OR – odds ratio; CI – confidence interval
Three categories of Food Insecurity: without hunger; with moderate hunger; and with severe hunger.
Adult and child overweight and/or obese in the same household.
Adjusted for caregiver age, caregiver education, caregiver gender, marital status, employment status, participation in food assistance programs (SNAP and WIC), housing arrangement, number of people, number of children, and income-to-poverty ratio.
Higher score: > 50th percentile (v. ≤ 50th percentile)
p-value < 0.05
Regarding psychosocial factors, we did not find significant differences between food secure and insecure respondents in unadjusted or adjusted models (Table 4 & Table 5).
Table 4.
Food-related behaviors, attitudinal and psychosocial factors by household food security status among low-income urban African American families (n=298)
| Food security status ‡ mean score (SD) |
|||
|---|---|---|---|
| Food Secure (n=174) |
Food Insecure |
||
| without hunger (n=87) |
with hunger (n=37) |
||
| Food-related Behaviors | |||
| Healthier food acquisition | 39.26 (32.99) | 37.30 (24.20) | 41.89 (29.23) |
| Less-healthy food acquisition | 54.10 (40.93) | 54.17 (36.93) | 55.73 (41.48) |
| Healthy food preparation | 1.39 (1.38) | 1.48 (1.62) | 1.08 (1.38) |
| Healthy Food Beliefs and Attitudes | |||
| Affordable | 10.46 (2.42)* † | 8.90 (3.12)* | 7.81 (3.28)† |
| Convenient | 10.47 (1.92)* | 9.48 (1.96)* | 9.68 (2.07) |
| Important | 12.54 (1.74) | 12.26 (1.96) | 12.41 (2.31) |
| Tastes good | 4.05 (0.84) | 3.79 (0.98) | 3.70 (1.22) |
| Body Image Satisfaction | 9.20 (2.85)* | 8.33 (2.41)* | 8.57 (3.07) |
| Food-related Psychosocial factors | |||
| Food and nutrition knowledge score |
7.14 (1.80) | 6.99 (1.76) | 6.97 (1.61) |
| Intentions on healthy eating score | 11.71 (4.21) | 10.79 (4.01) | 10.57 (4.19) |
| Healthy eating self-efficacy score | 24.88 (3.70) | 25.05 (3.76) | 23.89 (4.49) |
One-way ANOVA with Bonferroni post hoc test to compare the food security groups
Significant differences between groups (p-value < 0.05)
Health beliefs and attitudes associated with food security status
In unadjusted models, we found that food secure respondents showed a higher level of agreement with healthy food as being affordable, compared to both food insecurity groups. Food insecure respondents without hunger tended to consider healthy foods less accessible and less convenient to buy in the neighborhood and to prepare at home (Table 4). Each of these results remained significant in the models adjusted for sociodemographic characteristics (Table 5), with more food secure households perceiving healthy food as being affordable and convenient, associated with 0.18 (95% CI 0.09–0.39) and 0.49 (95% IC 0.24–0.95) odds of household food insecurity, respectively.
Caregiver body weight satisfaction score was lower in the food insecurity without hunger, compared to food security (Table 4). However, upon adjustment for covariates, this relationship was no longer statistically significant.
Factors associated with excess body weight
In the adjusted models (Table 5), a higher perception of healthy food as being convenient was associated with a 57% decrease in odds of caregiver and child excess body weight. We also found that higher satisfaction scores on beliefs about body image were associated with a 47% decrease in odds of caregiver overweight or obesity and child overweight or obesity (adjusted model). We did not find significant associations between food-related behaviors, psychosocial factors (as exposures) and household food insecurity and excess body weight (as outcomes).
The sensitivity models that examined child and adult overweight/obesity in separate models were substantively similar with the exceptions that in models examining only adult overweight/obesity as the outcome, we find that the factor variable characterized by shopping frequently at a covered market was associated with higher odds of overweight/obesity (OR=2.51; 95% CI 1.07–5.91), and higher nutrition knowledge was marginally statistically significantly associated with lower odds of overweight/obesity (p=0.097) (results not shown).
DISCUSSION
This is the first study to examine the associations between food security status, excess body weight, and consumer food-related behaviors and perceptions among low-income AA families with children living in Baltimore City. We found very high rates of adult and child overweight and/or obesity, as well as a high prevalence of families that had recently experienced food insecurity. Living in a food secure household was associated with the perception that healthy foods are affordable and convenient. Not being an overweight/obese caregiver and not having an overweight/obese child was associated with the caregiver body satisfaction and the perception that healthy foods are convenient. Nevertheless, we did not find significant differences regarding food-related behaviors and psychosocial factors across levels of food security.
Prevalence of overweight and obesity in our sample of food insecure households with hunger was 89.2% for adults and 45.9% for children. There is a growing body of research corroborating the relationship between obesity and food insecurity (1; 2; 3; 12; 23; 34), with clearer associations for women (1; 3; 35), but still mixed results for children (36). Our findings were consistent in direction, but there was not a statistically significant relationship between food insecurity and overweight or obesity among women or children. This may be attributable to either limited variation in the socioeconomic and community demographics of our sample, or potentially to the extremely high prevalence of overweight and obesity. Additionally, perceptions and attitudes towards body size may vary by social and cultural group (37).
Our data indicate that in our Baltimore sample, food insecurity rates (41.6%) are 1.7 times that of households headed by individuals who are non-Hispanic black nationwide and approximately three times the levels in the general US population (8). Since all the households included were drawn from low-income neighborhoods with high poverty rates (19), higher rates of food insecurity were expected. Also, this result is consistent with other studies that have found significant disparities in food insecurity among ethnic minorities (1; 4; 14; 24). A similar prevalence of household food insecurity has been found among American-Indian families (45%). (4).
In terms of sociodemographic factors associated with food insecurity, many of our results are in the expected direction and consistent with other studies. We found that caregivers from food insecure households with hunger were significantly more likely to be unemployed and have lower incomes compared to those who are food secure. Also, there was a higher prevalence of food insecure families without hunger (67.5%) who had income below the poverty threshold, though the differences between the groups were not significant. Similarly, Suratkar et al (2010) also observed in a low-income AA in Baltimore City sample, significantly lower employment among food insecure households (26). Unemployment or other events that stress household budgets may influence food security as income is clearly a critical economic determinant of food insecurity and hunger (1; 4; 17; 24; 25).
Our study adds to the literature by examining consumer food decisions made by low-income caregivers who are at high risk for being food insecure and overweight or obese. In this context, we found that food source destination, food acquisition behaviors and food-related psychosocial factors were not associated with food security status. On the other hand, certain health beliefs and attitudes were associated with food security status and overweight/obesity status. Specifically, believing that healthy foods are affordable and convenient as well as having a positive body image was related to lower odds of food insecurity. In line with that, food secure respondents showed higher food and nutrition knowledge and intentions for healthy eating compared to food insecure households, although this trend was not statistically significant. Having a positive body image and believing that healthy foods are convenient to buy and prepare were also related to lower odds of overweight or obesity.
Our findings around perceived affordability are consistent with previous work that has found that perceiving healthy foods as unaffordable and being less satisfying (vs. energy-dense foods) was negatively associated with the consumption of fruits and vegetables by food insecure populations (3; 25). Investigating different theoretical constructs as predictors of food-related behaviors, such as those based on Health Belief Model and Social Cognitive Theory, are useful to develop appropriate strategies focusing on consumer food choices and dietary practices to foster low-income families’ health promotion and obesity prevention, especially food program recipients (10; 30; 37). Yet to our knowledge, no studies investigating associations between food assistance program use, perceptions of food access and food-related psychosocial factors exist. Therefore, the BHCK program has focused on working with wholesalers, local corner stores and carryout restaurants in Baltimore city to increase access to healthy foods and promotes these foods through point-of-purchase activities, such as cooking demonstration, taste tests and educational materials aiming to improve food-related perceptions, and promote food selection and preparation behaviors among low-income AA youths and their caregivers (19).
Although we found extremely high excess body weight in the entire sample, we also observed higher levels of body weight and body image satisfaction among food secure caregivers (for themselves and their children), compared to food insecure. It is worthwhile to note that ethnicity and culture influence body size preference (37; 38). Having a positive body image was associated with a 45% lower odds of being food insecure. Body image satisfaction may mediate the relationship between food security and food-related psychosocial factors, such as intentions and self-efficacy to eat healthier foods (38). We are unaware of any other studies that have examined body image in relation to food insecurity. Being overweight or obese was also associated with having a more negative body image in our sample. James et al (2012) identified that AA women are aware of health risks of obesity, and believe that culture and genetics made them more susceptible to obesity (37). Motivators to lose weight include having a health problem, improving one’s physical appearance and saving money on clothes (37).
We were expecting to find associations between food security status and food source destinations, but the lack of significant differences for preferred food stores and food acquisition patterns between the groups may be due to the similarities in the local food environment and access to food sources among low-income AA living in urban areas of Baltimore City (21; 29; 39). Factors including fourteen types of food source destinations accounted for the most variance explained, which allow us to infer that the three food sources destinations not retained (farmer’s market, convenience stores, and specialty stores) were not frequently used by our sample. In this setting, the “Convenience store shopping” (Factor 1) reveals that local carry-out, chain fast-food restaurant and local corner store are important food venues for low-income AA adults. Corner stores are typically small stores with limited space that stock primarily high-fat, high-sugar and high-salt foods, and have been documented as the most frequently used food source by AA youth (28) and the second most by AA adults living in low-income neighborhoods (21).
The current study has some limitations. First, it uses a cross-sectional design making it impossible to determine how food insecurity may be associated with increased weight gain over time. Second, given there are multiple scales to evaluate household food insecurity that rely on different assumptions and metrics, comparability with other studies is difficult. Third, our survey was administered to self-identified caregivers under the assumption that they purchase most of the food and cook for other family members in the household, though the extent of this practice could vary among low-income AA families. Fourth, given we investigated food-related psychosocial factors and behaviors, performing a complementary qualitative approach could have helped to identify and contextualize these constructs. Future studies should include methods to better understand which factors influence decision-making regarding household food acquisition and eating patterns (e.g. exploring affordability, accessibility and other food access dimensions) and their relationship with food insecurity and obesity. Further, food acquisition scores were based only on frequency of items acquired, but did not take into account their quantity and size. The food acquisition score also did not identify the participant’s primary food shopping/acquiring source (i.e. a participant might go to a corner store everyday for small items – for example, a can of soda – but still do their primary shopping at a supermarket) and our measure would not be able to differentiate these behaviors. In order to establish more direct associations between household food acquisition dynamics, food security and obesity, researchers should evaluate portion size, total quantity consumed, or other factors that reflect the overall dietary quality of each family member.
CONCLUSIONS
In summary, our findings suggest that obesity and food insecurity are major problems among adults living in food deserts in Baltimore City. In this context, food insecurity was associated with employment status, family size and income. Beliefs and attitudes towards healthy food as being affordable and convenient were negatively associated with household food insecurity. Overweight and obesity in the same family was associated with the caregivers’ perception that healthy foods are less convenient and with a negative body image. Given that the households interviewed exhibited a similar pattern of food source destination, food acquisition, preparation and psychosocial factors regardless of their food security status, further qualitative research should be done to contextualize behaviors, beliefs and experiences of food insecurity. Food-related consumer behaviors are key to empowering families with children to make healthier decisions and overcome constraints in the food environment regarding access to healthy foods. The BHCK, as a sequence to these baseline data, will provide an opportunity to identify strategies to increase nutrition knowledge, self-efficacy, intentions, and skills for behavior change that have the potential to address obesity and food insecurity. Additionally, the study’s findings could inform policy decisions and food assistance program initiatives focused on food insecurity, given that low-income and food insecure minorities are especially vulnerable to obesity.
Supplementary Material
Acknowledgments
Disclosure statements
We thankful to and acknowledge the students, staff and volunteers of the Johns Hopkins Bloomberg School of Public Health who contributed with data collection and the BHCK families who contributed to this research.
Financial Support
Research reported in this publication was supported by the Global Obesity Prevention Center (GOPC) at Johns Hopkins, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Office of the Director, National Institutes of Health (OD) under award number U54HD070725. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest
None.
Authorship
Gabriela M. Vedovato was involved in formulating the research questions, designing the study, analyzing and interpreting the data.
Pamela J. Surkan was involved in interpreting the data and the article revision.
Jessica Jones-Smith was involved in interpreting the data and the article revision.
Elizabeth Anderson Steeves was involved in interpreting the data and the article revision.
Eunkyung Han was involved in interpreting the data and the article revision.
Angela C.B. Trude was involved in interpreting the data and the article revision.
Anna Y. Kharmats was involved in interpreting the data and the article revision.
Joel Gittelsohn is the Principal Investigator and was involved in formulating the research questions, designing the study, interpreting the data and article revision.
All authors were involved in writing this article.
Ethical Standards Disclosure
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB). Written informed consent was obtained from all subjects/patients.
References
- 1.Dinour LM, Bergen D, Yeh M-C. The food insecurity-obesity paradox: A review of the literature and the role food stamps may play. Journal of the American Dietetic Association. 2007;107:1952–1961. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Crawford PB, Webb KL. Unraveling the Paradox of Concurrent Food Insecurity and Obesity. American Journal of Preventive Medicine. 2011;40:274–275. doi: 10.1016/j.amepre.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Larson NI, Story MT. Food Insecurity and Weight Status Among US Children and Families A Review of the Literature. American Journal of Preventive Medicine. 2011;40:166–173. doi: 10.1016/j.amepre.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 4.Mullany B, Neault N, Tsingine D, et al. Food insecurity and household eating patterns among vulnerable American-Indian families: associations with caregiver and food consumption characteristics. Public Health Nutrition. 2013;16:752–760. doi: 10.1017/S136898001200300X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pardilla M, Prasad D, Suratkar S, et al. High levels of household food insecurity on the Navajo Nation. Public Health Nutrition. 2014;17:58–65. doi: 10.1017/S1368980012005630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kac G, Velasquez-Melendez G, Schluessel MM, et al. Severe food insecurity is associated with obesity among Brazilian adolescent females. Public Health Nutrition. 2012;15:1854–1860. doi: 10.1017/S1368980011003582. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y, Beydoun MA. The obesity epidemic in the United States - Gender, age, socioeconomic, Racial/Ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiologic Reviews. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 8.Coleman-Jensen A, Nord M, Singh A. Household Food Security in the United States in 2012: U.S. Department of Agriculture, Economic Research Service. 2013. [Google Scholar]
- 9.Bonanno A, Li J. Food Insecurity and Food Access in U.S. Metropolitan Areas. Applied Economic Perspectives and Policy first published online December 3. 2014 [Google Scholar]
- 10.Franklin B, Jones A, Love D, et al. Exploring Mediators of Food Insecurity and Obesity: A Review of Recent Literature. Journal of Community Health. 2012;37:253–264. doi: 10.1007/s10900-011-9420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zachary DA, Palmer AM, Beckham SW, et al. A Framework for Understanding Grocery Purchasing in a Low-Income Urban Environment. Qualitative Health Research. 2013;23:665–678. doi: 10.1177/1049732313479451. [DOI] [PubMed] [Google Scholar]
- 12.Leung CW, Epel ES, Ritchie LD, et al. Food Insecurity Is Inversely Associated with Diet Quality of Lower-Income Adults. J Acad Nutr Diet. 2014 doi: 10.1016/j.jand.2014.06.353. [DOI] [PubMed] [Google Scholar]
- 13.Kharmats AY, Jones-Smith JC, Cheah YS, et al. Relation between the Supplemental Nutritional Assistance Program cycle and dietary quality in low-income African Americans in Baltimore, Maryland. Am J Clin Nutr. 2014;99:1006–1014. doi: 10.3945/ajcn.113.075994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayer VL, Hillier A, Bachhuber MA, et al. Food insecurity, neighborhood food access, and food assistance in Philadelphia. Journal of urban health : bulletin of the New York Academy of Medicine. 2014;91:1087–1097. doi: 10.1007/s11524-014-9887-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.USDA. [accessed July 20 2015];Definitions of Food Security. 2006 http://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx.
- 16.Meyerhoefer CD, Yang M. The Relationship between Food Assistance and Health: A Review of the Literature and Empirical Strategies for Identifying Program Effects. Applied Economic Perspectives and Policy. 2011;33:304–344. [Google Scholar]
- 17.Leung CW, Villamor E. Is participation in food and income assistance programmes associated with obesity in California adults? Results from a state-wide survey. Public Health Nutrition. 2011;14:645–652. doi: 10.1017/S1368980010002090. [DOI] [PubMed] [Google Scholar]
- 18.Powell LM, Slater S, Mirtcheva D, et al. Food store availability and neighborhood characteristics in the United States. Preventive Medicine. 2007;44:189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Gittelsohn J, Steeves EA, Mui Y, et al. B’More healthy communities for kids: design of a multi-level intervention for obesity prevention for low-income African American children. Bmc Public Health. 2014;14 doi: 10.1186/1471-2458-14-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carter MA, Dubois L, Tremblay MS. Place and food insecurity: a critical review and synthesis of the literature. Public Health Nutrition. 2014;17:94–112. doi: 10.1017/S1368980013000633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.D’Angelo H, Suratkar S, Song H-J, et al. Access to food source and food source use are associated with healthy and unhealthy food-purchasing behaviours among low-income African-American adults in Baltimore City. Public Health Nutrition. 2011;14:1632–1639. doi: 10.1017/S1368980011000498. [DOI] [PubMed] [Google Scholar]
- 22.Lee SH, Rowan MT, Powell LM, et al. Characteristics of Prepared Food Sources in Low-Income Neighborhoods of Baltimore City. Ecology of Food and Nutrition. 2010;49:409–430. doi: 10.1080/03670244.2010.524102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leung CW, Williams DR, Villamor E. Very low food security predicts obesity predominantly in California Hispanic men and women. Public Health Nutr. 2012;15:2228–2236. doi: 10.1017/S1368980012000857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramsey R, Giskes K, Turrell G, et al. Food insecurity among adults residing in disadvantaged urban areas: potential health and dietary consequences. Public Health Nutrition. 2012;15:227–237. doi: 10.1017/S1368980011001996. [DOI] [PubMed] [Google Scholar]
- 25.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. American Journal of Clinical Nutrition. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 26.Suratkar S, Gittelsohn J, Song HJ, et al. Food insecurity is associated with food-related psychosocial factors and behaviors among low-income African American adults in Baltimore City. Journal of Hunger & Environmental Nutrition. 2010;5:100–119. [Google Scholar]
- 27.Surkan PJ, Coutinho AJ, Christiansen K, et al. Healthy food purchasing among African American youth: associations with child gender, adult caregiver characteristics and the home food environment. Public Health Nutrition. 2011;14:670–677. doi: 10.1017/S136898001000251X. [DOI] [PubMed] [Google Scholar]
- 28.Dennisuk LA, Coutinho AJ, Suratkar S, et al. Food expenditures and food purchasing among low-income, urban, African-American youth. Am J Prev Med. 2011;40:625–628. doi: 10.1016/j.amepre.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 29.Center for a Livable Future JHSoPHF. The Baltimore City Food Environment. 2010 [Google Scholar]
- 30.McAlister AL, Perr CL, Parcel GS. How individuals, environments and health behavior interact. Social Cognitive Theory. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education Theory, Research and Practice. 4th. San Fracisco: Jossey-Bass; 2008. pp. 167–185. [Google Scholar]
- 31.WHO. Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: World Health Organization; 2006. p. 312. [Google Scholar]
- 32.Bickel G, Nord M, Price C, et al. Guide to Measuring Household Food Security, Revised 2000. March, 2000. US Department of Agriculture, Food and Nutrition Service Alexandria VA. 2000 [Google Scholar]
- 33.Hair J, Black W, Babin B, et al. Multivariate data analysis. 6th. Pearson Education, Inc.; 2009. [Google Scholar]
- 34.Leung CW, Williams DR, Villamor E. Very low food security predicts obesity predominantly in California Hispanic men and women. Public Health Nutrition. 2012;15:2228–2236. doi: 10.1017/S1368980012000857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanson KL, Sobal J, Frongillo EA. Gender and marital status clarify associations between food insecurity and body weight. Journal of Nutrition. 2007;137:1460–1465. doi: 10.1093/jn/137.6.1460. [DOI] [PubMed] [Google Scholar]
- 36.Eisenmann JC, Gundersen C, Lohman BJ, et al. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obesity Reviews. 2011;12:e73–e83. doi: 10.1111/j.1467-789X.2010.00820.x. [DOI] [PubMed] [Google Scholar]
- 37.James DCS, Pobee JW, Oxidine Dl, et al. Using the Health Belief Model to Develop Culturally Appropriate Weight-Management Materials for African-American Women. Journal of the Academy of Nutrition and Dietetics. 2012;112:664–670. doi: 10.1016/j.jand.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Chen X, Wang Y. Is ideal body image related to obesity and lifestyle behaviours in African American adolescents? Child Care Health and Development. 2012;38:219–228. doi: 10.1111/j.1365-2214.2011.01227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Franco M, Roux AVD, Glass TA, et al. Neighborhood Characteristics and Availability of Healthy Foods in Baltimore. American Journal of Preventive Medicine. 2008;35:561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.