Abstract
The prevalence of masked hypertension, out-of-clinic daytime systolic/diastolic blood pressure (SBP/DBP)≥135/85 mmHg on ambulatory blood pressure monitoring (ABPM) among adults with clinic SBP/DBP<140/90 mmHg, is high. It is unclear who should be screened for masked hypertension. We derived a clinic blood pressure (CBP) index to identify populations for masked hypertension screening. Index cut-points corresponding to 75% to 99% sensitivity and prehypertension were evaluated as ABPM testing criterion. In a derivation cohort (n=695), the index was clinic SBP+1.3*clinic DBP. In an external validation cohort (n=675), the sensitivity for masked hypertension using an index ≥190 mmHg and ≥217 mmHg and prehypertension status was 98.5%, 71.5% and 82.5%, respectively. Using NHANES data (n=11,778), we estimated that these thresholds would refer 118.6, 44.4 and 59.3 million US adults, respectively, to ABPM screening for masked hypertension. In conclusion, the CBP index provides a useful approach to identify candidates for masked hypertension screening using ABPM.
Keywords: masked hypertension, clinic blood pressure, ambulatory blood pressure monitoring
INTRODUCTION
In 2002, Pickering introduced the term masked hypertension, referring to individuals not taking antihypertensive medication who have non-elevated clinic-measured blood pressure (BP) but elevated daytime BP when assessed outside of the clinic by ambulatory blood pressure monitoring (ABPM).1 Masked daytime hypertension has been reported to be common among individuals with non-elevated clinic BP (CBP) with prevalence estimates ranging from 15% to 30% in population-based studies.2 Compared with sustained normotension, defined as non-elevated CBP with non-elevated daytime BP on ABPM, masked daytime hypertension is associated with increased risk for target-organ damage, cardiovascular disease and mortality.3,4
Some guidelines and position papers recommend ABPM to detect masked hypertension.5–7 However, it is unclear which populations to screen with ABPM to detect masked hypertension.5–21 One approach would be to offer ABPM to all adults with non-elevated CBP to identify those with masked hypertension.2 However, population-wide screening for masked hypertension is not practical. Another approach is to offer ABPM to individuals with prehypertension, defined as clinic systolic BP (SBP) of 120–139 mmHg or clinic diastolic BP (DBP) of 80–89 mmHg, due to the substantial overlap that exists between prehypertension and masked hypertension.22,23 This too may result in a substantial proportion of US adults undergoing ABPM. A third approach is to develop an equation to identify individuals for ABPM screening.
In this study, we derived and validated a CBP diagnostic index for detecting masked hypertension among adults with non-elevated CBP who were not taking antihypertensive medication. Test characteristics for the identification of masked hypertension using this index, including sensitivity, specificity, and positive and negative predictive values, were calculated and compared with the test characteristics associated with using prehypertension. Data from the National Health and Nutrition Examination Survey (NHANES) 2009–2012 were used to estimate the number of US adults who would be recommended having ABPM to detect masked hypertension using each of these approaches.
METHODS
Study Populations
The current analyses used data from four studies. The Masked Hypertension (MHT) Study (n=1,010) was used to derive an equation, the CBP diagnostic index, for identifying masked daytime hypertension.22 We pooled the Improving the Detection of Hypertension (IDH) Study (n=408) and the Jackson Heart Study (JHS; n=5,301; n=1,148 who completed ABPM) to externally validate the CBP diagnostic index in samples having a high number of Hispanics and African Americans. NHANES 2009–2010 and 2011–2012 (n=11,778) were used to estimate the number of US adults ≥20 years old that would be recommended ABPM screening to identify masked hypertension with the approaches being compared.
Each of the studies used for the current analysis have been described in detail previously.22,24–26 In brief, the MHT Study is a worksite-based study comprised of adult employees from Stony Brook University, University Hospital at Stony Brook, Columbia University, and a private hedge fund management organization in New York who work >20 hours per week and on at least two consecutive days. The goal of the MHT Study is to estimate the prevalence, predictors, and prognosis of masked hypertension.22 The IDH Study enrolled a community-based sample of adults, primarily from upper Manhattan, New York City.24 It was designed to compare the cost-effectiveness of different strategies for diagnosing ambulatory hypertension. The JHS is a prospective population-based study comprised exclusively of African Americans from the tri-county (Hinds, Madison and Rankin counties) area of Jackson, MS.25 The purpose of the JHS is to evaluate cardiovascular disease risk among African Americans.27 The aim of the NHANES is to assess the health and nutritional status of adults and children in the US. The NHANES enrolled a multistage probability sample of non-institutionalized U.S. civilians and can be used to calculate nationally representative estimates of disease prevalence. It is conducted in 2 year cycles and these cycles can be pooled to provide stable prevalence estimates in population sub-groups.
For the current analyses, the MHT Study, the IDH Study and the JHS were restricted to participants who met criteria for a complete ABPM (defined below) and who had non-elevated CBP and were not taking antihypertensive medication (MHT Study: n=695; IDH Study: n=344; JHS: n=331). The NHANES sample was restricted to participants ≥20 years of age who had non-elevated CBP and were not taking antihypertensive medication (n=6,835). ABPM was not performed in the NHANES. Additional details on each study are available in the online eSupplement. The current study was approved by all appropriate Institutional Review Boards and is in agreement with the Declaration of Helsinki. All participants provided written informed consent.
Data collection
The MHT and IDH studies collected data using self-administered questionnaires during a clinic examination and through ABPM. The JHS collected data using interviewer-administered questionnaires during a clinic examination and through ABPM. In each study, trained technicians measured height, weight and CBP during a clinic examination. Questionnaires were used to document information on demographics (i.e., age, sex, race/ethnicity), smoking status, current use of antihypertensive medication and self-reported diabetes status. In the NHANES, interviewer-administered questionnaires were used during the in-home interview to collect demographic information and data on antihypertensive medication use.
Clinic blood pressure in the MHT Study, IDH Study, JHS and NHANES
In all four studies, CBP was measured by trained staff following a standardized protocol. Prior to CBP measurements, participants sat quietly for at least 5 minutes in an upright position with their back and arms supported, feet flat on the floor and legs uncrossed. During the CBP measurements, an appropriately-sized cuff, determined by measuring the mid-arm circumference, was used.28,29 One-to-two minutes elapsed between the readings in the MHT Study, IDH Study and JHS; there was a 30-second interval between the readings in the NHANES. In the MHT Study, IDH Study and NHANES, three CBP measurements were obtained using a mercury sphygmomanometer. In the JHS, two CBP measurements were obtained using a random zero mercury sphygmomanometer. For each participant, the CBP measurements were averaged. Non-elevated CBP was defined as clinic SBP<140 mmHg and clinic DBP<90 mmHg. Prehypertension was defined as clinic SBP of 120–139 mmHg or clinic DBP of 80–89 mmHg.
Ambulatory blood pressure monitoring in the MHT Study, IDH Study and JHS
ABPM was conducted in the MHT Study, IDH Study and JHS using Spacelabs Model 90207 (Snoqualmie, WA). For each study, participants were fitted with an appropriately-sized ABPM arm cuff. BP on ABPM was recorded every 28 minutes in the MHT Study, every 30 minutes in the IDH Study and every 20 minutes in the JHS. For the current analysis, we defined diurnal periods using International Database on ABPM in relation to Cardiovascular Outcomes (IDACO) criteria. Daytime was defined as the time period from 10:00 to 20:00 and nighttime as 00:00 to 06:00.30 Participants were considered to have a complete ABPM if they had ≥10 daytime and ≥5 nighttime SBP and DBP measurements.
The ABPM recordings were analyzed to obtain mean daytime and nighttime SBP and DBP. Daytime hypertension was defined as a mean SBP ≥ 135 mmHg or mean DBP ≥ 85 mmHg based on the daytime measurements, and nocturnal hypertension was defined as a mean SBP ≥ 120 mmHg or mean DBP ≥ 70 mmHg based on the nighttime measurements.5,31,32 Since the current analysis was restricted to participants with non-elevated CBP, those with daytime and nocturnal hypertension had masked daytime hypertension and masked nocturnal hypertension, respectively.
Statistical Analyses
In the MHT Study, the c-statistic was calculated for three logistic regression models to identify factors that discriminated participants with and without masked daytime hypertension, defined as a mean daytime SBP ≥ 135 mmHg or mean daytime DBP ≥ 85 mmHg in participants with non-elevated CBP (SBP/DBP <140/90 mmHg; Supplemental eTable 1).33 In these analyses, masked daytime hypertension was the dependent variable. The independent variables were clinic SBP and DBP in Model 1; age, sex, body mass index, race, ethnicity, diabetes and current smoking in Model 2; and all variables from Models 1 and 2 in Model 3. As described below, Model 1 discriminated masked daytime hypertension better than Model 2. Discrimination was better in Model 3 versus Model 1. Model 1 was chosen for the diagnostic index as it provides a simple method using CBP alone and may be more easily implemented in practice.
A receiver operating characteristic curve was plotted to determine the CBP diagnostic index cut-point with 99%, 95%, 90%, 85%, 80% and 75% sensitivity (Supplemental eFigure 1). The CBP diagnostic index cut-point for masked daytime hypertension corresponding to the respective sensitivity level was subsequently applied in the diagnostic index equation from the selected logistic regression model (Model 1) to derive the cut-points. The online eSupplement provides further details on the derivation of the CBP diagnostic index.
In the pooled IDH/JHS validation cohort, the c-statistic and the Hosmer-Lemeshow Goodness-of-Fit for deciles were calculated to determine the discrimination and calibration, respectively, of the diagnostic index. The external validity of the CBP diagnostic index was determined by taking the cut-points associated with 99%, 95%, 90%, 85%, 80% and 75% sensitivity from the MHT Study and calculating the test characteristics for detecting masked daytime hypertension in the pooled IDH/JHS validation cohort. As the 2013 European Society of Hypertension (ESH) position paper on ABPM recommends including nocturnal hypertension as a criterion for the definition of masked hypertension, we evaluated the test characteristics of the CBP diagnostic index for identifying masked daytime or masked nocturnal hypertension in a secondary analysis.5 For comparison, test characteristics were calculated for prehypertension and the upper range of prehypertension (i.e., clinic SBP 130–139 mmHg or clinic DBP 85–89 mmHg). The upper range of prehypertension was selected for an a priori analysis as studies have reported that the prevalence of masked hypertension is very high in this range of CBP.4,22,34
Finally, using the NHANES 2009–2012 data, the number and percentage of US adults ≥20 years old who would be recommended testing with ABPM was estimated for individuals with an elevated CBP diagnostic index, prehypertension, and the upper range of prehypertension, separately. Estimates were calculated for the overall population and in sub-groups defined by age (i.e., <40, 40–59, ≥60 years), race/ethnicity (i.e., non-Hispanic white, non-Hispanic black, Hispanic, other) and sex. NHANES analyses were conducted taking into account the study’s complex multistage sampling design and were weighted to produce US population estimates. Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC) and SUDAAN 10.1 (Research Triangle Institute, Research Triangle Park, NC).
RESULTS
Participant characteristics
Compared with the derivation cohort (i.e., MHT Study), the pooled validation cohort (i.e., IDH/JHS) had a higher percentage of participants who were aged 60 years or older, and black and Hispanic (Table 1). Participants with prehypertension and the upper range of prehypertension comprised 39.9% and 12.8% of the derivation cohort, respectively, and 47.4% and 19.3% of the pooled validation cohort, respectively. Whereas masked daytime and masked nocturnal hypertension was present in 19.3% and 20.0% of the derivation cohort, respectively, the prevalence was 20.3% and 32.9%, respectively, in the pooled IDH/JHS cohort. Also, 30.2% and 37.6% of the MHT and pooled IDH/JHS cohort participants, respectively, had masked daytime and/or nocturnal hypertension.
Table 1.
Characteristics of the Masked Hypertension Study, Improving the Detection of Hypertension Study and Jackson Heart Study participants.
| MHT Study (derivation cohort) |
IDH/JHS (pooled validation cohort) |
|
|---|---|---|
| (n=695) | (n=675) | |
| Age categories | ||
| < 40 years | 213 (30.7%) | 212 (31.4%) |
| 40 to 59 years | 435 (62.6%) | 324 (48.0%) |
| ≥ 60 years | 47 (6.8%) | 139 (20.6%) |
| Male | 275 (39.6%) | 241 (35.9%) |
| Black race | 47 (6.8%) | 5415 (61.5%) |
| Hispanic ethnicity | 87 (12.5%) | 216 (32.0%) |
| Body mass index, kg/m2 | 27.4 (5.4%) | 28.5 (6.0) |
| Diabetes | 25 (3.8%) | 37 (5.5%) |
| Current smoker | 49 (7.4%) | 62 (9.3%) |
| Clinic blood pressure | ||
| Systolic, mmHg | 113.8 (10.7) | 115.0 (11.8) |
| Diastolic, mmHg | 74.4 (7.5) | 74.3 (8.0) |
| Prehypertensiona | 277 (39.9%) | 320 (47.4%) |
| Upper range of prehypertensionb | 89 (12.8%) | 130 (19.3%) |
| Ambulatory blood pressure | ||
| Daytime period | ||
| Systolic, mmHg | 122.6 (10.1) | 118.6 (12.1) |
| Diastolic, mmHg | 77.2 (7.5) | 71.8 (9.4) |
| Masked daytime hypertensionc | 134 (19.3%) | 137 (20.3%) |
| Nighttime period | ||
| Systolic, mmHg | 106.2 (10.7) | 108.6 (11.1) |
| Diastolic, mmHg | 62.3 (7.9) | 63.5 (7.7) |
| Masked nocturnal hypertensiond | 139 (20.0%) | 222 (32.9%) |
| Masked daytimec and/or nocturnald hypertension | 210 (30.2%) | 254 (37.6%) |
Numbers in the table are number (percentage) or mean (standard deviation).
MHT: Masked Hypertension Study.
IDH: Improving the Detection of Hypertension Study.
JHS: Jackson Heart Study.
Prehypertension: Among adults with non-elevated clinic blood pressure (i.e., systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg), clinic systolic blood pressure ≥ 120 mmHg and < 140 mmHg or clinic diastolic blood pressure ≥ 80 mmHg and < 90 mmHg.
Upper range of prehypertension: Among adults with non-elevated clinic blood pressure (i.e., systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg), clinic systolic blood pressure ≥ 130 mmHg and < 140 mmHg or clinic diastolic blood pressure ≥ 85 mmHg and < 90 mmHg.
Masked daytime hypertension: Clinic systolic/diastolic blood pressure < 140/90 mmHg with mean ambulatory daytime systolic/diastolic blood pressure ≥ 135/85 mmHg.
Masked nocturnal hypertension: Clinic systolic blood pressure < 140/90 mmHg with mean ambulatory nocturnal systolic/diastolic blood pressure ≥ 120/70 mmHg.
Derivation of the clinic blood pressure diagnostic index in the Masked Hypertension Study
The c-statistic (95% confidence interval [CI]) for masked daytime hypertension was 0.78 (95% CI 0.74–0.82) for a model including only clinic SBP and DBP (Model 1) and 0.72 (95% CI 0.66–0.77) for a model that included age, sex, body mass index, race, ethnicity, diabetes, and current smoking status (Model 2; Supplemental eTable 1). In a model including all of the variables from Models 1 and 2 (Model 3), the c-statistic was 0.81 (95% CI 0.77–0.85). Using Model 1, the CBP diagnostic index was defined as: clinic SBP + 1.3*clinic DBP.
A scatterplot of each participant’s clinic SBP and DBP in the MHT Study is shown in Supplemental eFigure 2. The lines in the figure correspond to the CBP diagnostic index equation for sensitivity levels of 99%, 95%, 90%, 85%, 80% and 75%. Using the CBP diagnostic index equation, the cut-point for detecting masked daytime hypertension with 99% sensitivity was 190 mmHg. The cut-point for 95% sensitivity was 201 mmHg, 90% sensitivity was 207 mmHg, 85% sensitivity was 212 mmHg, 80% sensitivity was 214 mmHg and 75% sensitivity was 217 mmHg. The specificity and positive and negative predictive values for each level of sensitivity are provided in Supplemental eTable 2.
Validation of the clinic blood pressure diagnostic index in the pooled IDH/JHS cohorts
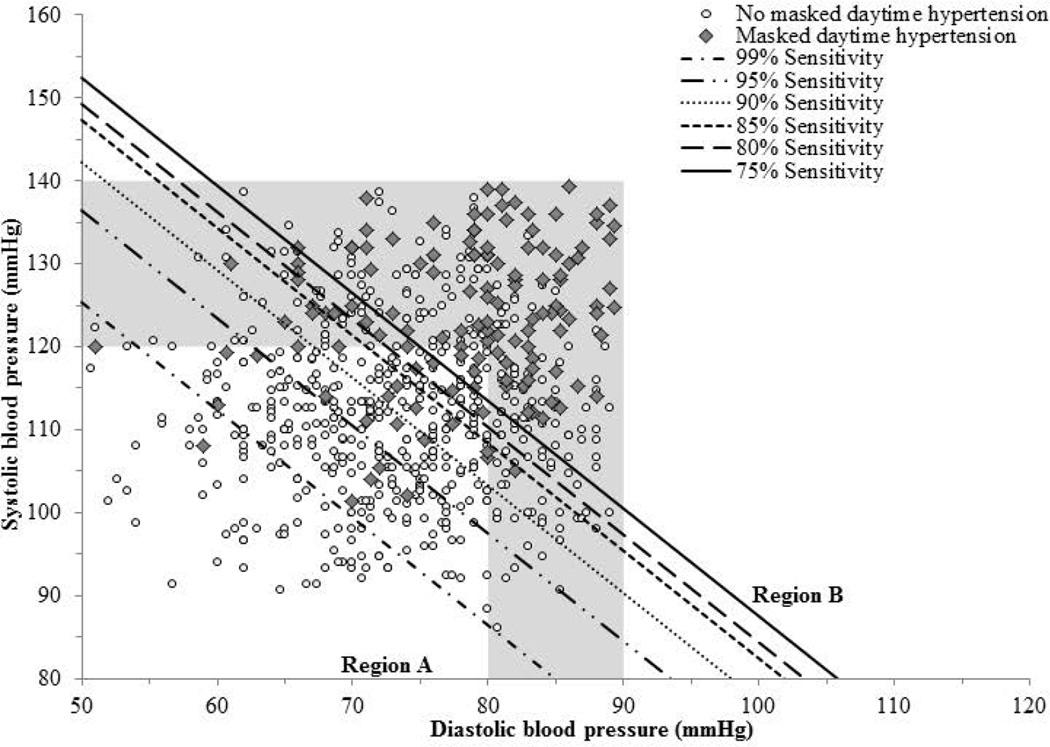
In the validation cohort, the c-statistic (95% confidence interval [CI]) for masked daytime hypertension was 0.77 (95% CI 0.73–0.81). The CBP diagnostic index was well calibrated in the validation cohort (Hosmer-Lemeshow Goodness-of-Fit chi-square for deciles with 8 degrees of freedom: 9.78; p=0.281). A scatterplot of IDH and JHS participants’ clinic SBP and DBP readings and the boundary lines representing 99%, 95%, 90%, 85%, 80% and 75% sensitivity for detecting masked daytime hypertension using the CBP diagnostic index are plotted in Figure 1. In the pooled IDH/JHS cohort, the sensitivity for detecting masked daytime hypertension using the cut-points on the CBP diagnostic index from the MHT study ranged from 98.5% to 71.5% and the specificity ranged from 18.8% to 64.1%, respectively (CBP diagnostic index ≥190 mmHg to ≥217 mmHg, respectively; Table 2, top panel). The sensitivity and specificity for detecting masked daytime hypertension was 82.5% and 61.5% for prehypertension and 42.3% and 86.6% for the upper range of prehypertension, respectively. The sensitivity for detecting masked daytime or nocturnal hypertension ranged from 97.2% to 64.6% (CBP diagnostic index ≥190 mmHg to ≥217 mmHg, respectively) using the CBP diagnostic index and was 71.3% for prehypertension and 34.3% for the upper range of prehypertension (Table 2, bottom panel).
Figure 1.
Scatterplot of clinic systolic versus diastolic blood pressure demonstrating derived cut-points corresponding with specified sensitivity levels for detecting masked daytime hypertension using the clinic blood pressure index equation in the pooled validation cohort of Improving the Detection of Hypertension Study and Jackson Heart Study participants (n=675).
The shaded region represents the clinic blood pressure values corresponding with prehypertension defined as systolic blood pressure ≥ 120 mmHg and < 140 mmHg and/or diastolic blood pressure ≥ 80 mmHg and < 90 mmHg.
Region A: The clinic blood pressure diagnostic index, defined as systolic clinic blood pressure + 1.3*diastolic clinic blood pressure, was categorized as normal (i.e., below the cut-point corresponding with the specified sensitivity level).
Region B: The clinic blood pressure diagnostic index, defined as systolic clinic blood pressure + 1.3*diastolic clinic blood pressure, was categorized as elevated (i.e., at or above the cut-point corresponding with the specified sensitivity level).
- Sensitivity 99%: ≥ 190 mmHg.
- Sensitivity 95%: ≥ 201 mmHg.
- Sensitivity 90%: ≥ 207 mmHg.
- Sensitivity 85%: ≥ 212 mmHg.
- Sensitivity 80%: ≥ 214 mmHg.
- Sensitivity 75%: ≥ 217 mmHg.
Table 2.
Test characteristics for detecting masked daytime hypertension (n=137; top panel) and masked daytime and/or nocturnal hypertension (n=254; bottom panel) associated with prehypertension, upper range of prehypertension, and an elevated clinic blood pressure diagnostic index in the pooled validation cohort of the Improving the Detection of Hypertension Study and Jackson Heart Study participants (n=675).
| Prehypertensiona | Upper range of prehypertensionb |
Elevated clinic blood pressure diagnostic index using different derived cut-pointsc |
||||||
|---|---|---|---|---|---|---|---|---|
| ≥ 190 mmHg |
≥ 201 mmHg |
≥ 207 mmHg |
≥ 212 mmHg |
≥ 214 mmHg |
≥ 217 mmHg |
|||
| N=320 | N=130 | N=572 | N=472 | N=415 | N=351 | N=330 | N=291 | |
| Masked daytime hypertension | ||||||||
| Sensitivity | 82.5% (113 / 137) |
42.3% (58 / 137) |
98.5% (135 / 137) |
93.4% (128 / 137) |
89.8% (123 / 137) |
81.0% (111 / 137) |
78.8% (108 / 137) |
71.5% (98 / 137) |
| Specificity | 61.5% (331 / 538) |
86.6% (466 / 538) |
18.8% (101 / 538) |
36.1% (194 / 538) |
45.7% (246 / 538) |
55.4% (298 / 538) |
58.7% (316 / 538) |
64.1% (345 / 538) |
| PPV | 35.3% (113 / 320) |
44.6% (58 / 130) |
23.6% (135 / 572) |
27.1% (128 / 472) |
29.6% (123 / 415) |
31.6% (111 / 351) |
32.7% (108 / 330) |
33.7% (98 / 291) |
| NPV | 93.2% (331 / 355) |
85.5% (466 / 545) |
98.1% (101 / 103) |
95.6% (194 / 203) |
94.6% (246 / 260) |
92.0% (298 / 324) |
91.6% (316 / 345) |
89.8% (345 / 384) |
| Masked daytime and/or nocturnal hypertensiond | ||||||||
| Sensitivity | 71.3% (181 / 254) |
34.3% (87 / 254) |
97.2% (247 / 254) |
90.6% (230 / 254) |
83.9% (213 / 254) |
73.2% (186 / 254) |
71.3% (181 / 254) |
64.6% (164 / 254) |
| Specificity | 67.0% (282 / 421) |
89.8% (378 / 421) |
22.8% (96 / 421) |
42.5% (179 / 421) |
52.0% (219 / 421) |
60.8% (256 / 421) |
64.6% (272 / 421) |
69.8% (294 / 421) |
| PPV | 56.6% (181 / 320) |
66.9% (87 / 130) |
43.2% (247 / 572) |
48.7% (230 / 472) |
51.3% (213 / 415) |
53.0% (186 / 351) |
54.8% (181 / 330) |
56.4% (164 / 291) |
| NPV | 79.4% (282 / 355) |
69.4% (378 / 545) |
93.2% (96 / 103) |
88.2% (179 / 203) |
84.2% (219 / 260) |
79.0% (256 / 324) |
78.8% (272 / 345) |
76.6% (294 / 384) |
PPV: positive predictive value.
NPV: negative predictive value.
Prehypertension: Among adults with non-elevated clinic blood pressure (i.e., systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg), clinic systolic blood pressure ≥ 120 mmHg and < 140 mmHg or clinic diastolic blood pressure ≥ 80 mmHg and < 90 mmHg.
Upper range of prehypertension: Among adults with non-elevated clinic blood pressure (i.e., systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg), clinic systolic blood pressure ≥ 130 mmHg and < 140 mmHg or clinic diastolic blood pressure ≥ 85 mmHg and < 90 mmHg.
Clinic blood pressure diagnostic index cut-points associated with 99% (190 mmHg), 95% (201 mmHg), 90% (207 mmHg), 85% (212 mmHg), 80% (214 mmHg), and 75% (217 mmHg) sensitivity.
Masked daytime and/or nocturnal hypertension: Clinic systolic/diastolic blood pressure < 140/90 mmHg and daytime hypertension (i.e., mean daytime systolic blood pressure ≥ 135 mmHg or mean diastolic blood pressure ≥ 85 mmHg) and/or nocturnal hypertension (i.e., mean nighttime systolic blood pressure ≥ 120 mmHg or mean diastolic blood pressure ≥ 70 mmHg).
Testing for masked daytime hypertension in the US population
In 2009–2012, an estimated 152.7 million US adults had non-elevated CBP and were not taking antihypertensive medication (Table 3). Using the CBP diagnostic index, the number of US adults recommended ABPM to detect masked daytime hypertension ranged from 44.4 million using a cut-point of 217 mmHg to 118.6 million using a cut-point of 190 mmHg. Using prehypertension as the criterion for ABPM would result in referring 59.3 million US adults for ABPM. There would be 20.3 million US adults referred for ABPM if the upper range of prehypertension is used.
Table 3.
Number in millions and percentage of US adult with non-elevated clinic blood pressurea not taking antihypertensive medication that would be referred for ambulatory blood pressure monitoring using prehypertension, the upper range of prehypertension and cut-points derived using the clinic blood pressure diagnostic index.
| Prehypertensionb | Upper range of prehypertensionc |
Elevated clinic blood pressure diagnostic index using different derived cut-pointsd |
||||||
|---|---|---|---|---|---|---|---|---|
| ≥ 190 mmHg |
≥ 201 mmHg |
≥ 207 mmHg |
≥ 212 mmHg |
≥ 214 mmHg |
≥ 217 mmHg |
|||
| Number in millions (percentage) of US adultse | ||||||||
| Overall | 59.3 (39.1%) |
20.3 (14.0%) |
118.6 (76.5%) |
90.4 (58.1%) |
73.1 (46.8%) |
58.3 (37.4%) |
53.0 (34.0%) |
44.4 (28.5%) |
| Age categories | ||||||||
| < 40 years | 22.3 (29.0%) |
6.4 (8.4%) |
53.7 (69.8%) |
38.0 (49.5%) |
29.0 (37.8%) |
22.0 (28.4%) |
19.2 (25.2%) |
15.9 (20.6%) |
| 40 – 59 years | 26.5 (45.3%) |
8.7 (15.3%) |
49.2 (83.9%) |
39.7 (67.4%) |
33.7 (56.7%) |
27.9 (47.4%) |
26.2 (43.9%) |
22.2 (37.5%) |
| ≥ 60 years | 10.5 (57.4%) |
5.3 (28.8%) |
15.7 (81.1%) |
12.7 (65.0%) |
10.4 (53.3%) |
8.4 (43.8%) |
7.7 (40.0%) |
6.3 (33.4%) |
| Race / ethnicity | ||||||||
| Non-Hispanic White | 40.1 (39.2%) |
13.7 (14.0%) |
79.8 (77.5%) |
61.5 (59.4%) |
49.9 (47.5%) |
39.6 (37.3%) |
36.1 (34.2%) |
30.3 (28.5%) |
| Non-Hispanic Black | 6.6 (46.1%) |
2.6 (18.3%) |
11.6 (78.5%) |
9.1 (61.4%) |
7.4 (50.9%) |
6.1 (41.6%) |
5.5 (38.1%) |
4.7 (32.5%) |
| Hispanic | 9.1 (35.0%) |
3.2 (12.9%) |
20.6 (76.4%) |
15.6 (59.7%) |
12.4 (48.9%) |
10.1 (41.0%) |
9.1 (37.3%) |
7.8 (32.4%) |
| Other Race | 4.5 (34.7%) |
1.3 (10.6%) |
9.2 (75.6%) |
6.7 (55.8%) |
5.5 (45.7%) |
4.6 (37.4%) |
4.3 (34.7%) |
3.5 (28.9%) |
| Sex | ||||||||
| Female | 24.0 (29.9%) |
8.4 (10.6%) |
55.2 (67.6%) |
39.4 (48.1%) |
30.7 (37.2%) |
23.4 (28.5%) |
21.3 (25.6%) |
17.7 (21.5%) |
| Male | 35.3 (48.6%) |
11.9 (17.5%) |
63.4 (85.7%) |
50.9 (68.5%) |
42.3 (56.7%) |
34.8 (46.7%) |
31.7 (42.8%) |
26.7 (35.7%) |
Non-elevated clinic blood pressure: clinic systolic blood pressure < 140 mmHg and clinic diastolic blood pressure < 90 mmHg.
Prehypertension: Among adults with non-elevated clinic blood pressure (i.e., systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg), clinic systolic blood pressure ≥ 120 mmHg and < 140 mmHg or clinic diastolic blood pressure ≥ 80 mmHg and < 90 mmHg.
Upper range of prehypertension: Among adults with non-elevated clinic blood pressure (i.e., systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg), clinic systolic blood pressure ≥ 130 mmHg and < 140 mmHg or clinic diastolic blood pressure ≥ 85 mmHg and < 90 mmHg.
Clinic blood pressure diagnostic index cut-points associated with 99% (190 mmHg), 95% (201 mmHg), 90% (207 mmHg), 85% (212 mmHg), 80% (214 mmHg), and 75% (217 mmHg) sensitivity.
Number and percentage of US adults were derived from the National Health and Nutrition Examination Survey 2009–2012. There were approximately 152.7 million US adults with non-elevated clinic blood pressure who were not taking antihypertensive medication.
DISCUSSION
In the current study, we developed and validated a CBP diagnostic index that identifies adults as having masked daytime hypertension. We externally validated cut-points for identifying masked daytime hypertension using the CBP diagnostic index with sensitivity ranging from 75% to 99%. Although the CBP diagnostic index can be used to identify almost all adults with masked hypertension (i.e., approximately 99% sensitivity), this would require that 118.6 of the 152.7 million US adults with non-elevated CBP undergo ABPM. By choosing a cut-point associated with lower sensitivity, specificity would be higher and ABPM would be required for far fewer US adults. For example, using a cut-point that identified 89.8% of individuals with masked daytime hypertension would require testing 73.1 million US adults. For comparison, using prehypertension as a criterion to screen for masked daytime hypertension provides 82.5% sensitivity and would require 59.3 million US adults undergo ABPM. While the upper range of prehypertension would only require screening 20.3 million US adults, less than 50% of masked daytime hypertension cases (42.3% sensitivity) would be referred to ABPM.
Guidelines and position papers recommend ABPM to detect masked hypertension but agreement has not been reached on who should be offered ABPM.2,5–21 The current study provides evidence that it is impractical to perform ABPM on all US adults (approximately 153 million) with non-elevated CBP who were not taking antihypertensive medication. A more reasonable approach would be to test adults with a CBP diagnostic index above a specified cut-point. For any selected cut-point, there is a balance between sensitivity to detect masked daytime hypertension and the number of US adults requiring testing with ABPM. Using a low cut-point provides high sensitivity and almost all adults with masked daytime hypertension would be detected. However, this would result in performing ABPM on a majority of US adults with non-elevated CBP. In contrast, using a higher cut-point on the CBP diagnostic index, the sensitivity will be lower but substantially fewer US adults would need to undergo ABPM.
There are proponents of offering ABPM to adults with prehypertension in order to detect masked hypertension.22,34 Supporting this approach are prior studies that have examined the overlap of prehypertension with masked daytime hypertension.22 In the MHT Study, 35.0% of participants with prehypertension but only 8.9% of those with normal CBP had masked daytime hypertension.22 Similarly, masked daytime hypertension was more common among IDH/JHS participants with prehypertension (35.3%) compared to normal CBP (6.8%).35 In the MHT Study, masked daytime hypertension was almost twice as common in adults with CBP in the upper versus lower range of prehypertension (i.e. clinic SBP/DBP 130–139/85–89 mmHg versus 120–129/80–84 mmHg): 51.7% versus 26.5%.22 These studies may be interpreted as recommending ABPM for adults with CBP in the upper range of prehypertension may be an appropriate approach for detecting masked hypertension. Although these prior studies demonstrate high positive predictive value of prehypertension to identify masked daytime hypertension, the current study shows the upper range of prehypertension has low sensitivity for detecting masked daytime hypertension. Therefore, referring only individuals with CBP in the upper range of prehypertension for ABPM would miss the majority of individuals with masked daytime hypertension.
Increasing evidence suggests that CVD risk is higher for individuals with compared to without elevated nighttime BP.36 The 2013 European Society of Hypertension ABPM position paper incorporates elevated nighttime BP as a criterion for masked hypertension. The current study suggests that the cut-points from the CBP diagnostic index chosen for detecting masked daytime hypertension may also be useful for detecting masked daytime or nocturnal hypertension.
ABPM and home blood pressure monitoring (HBPM) can also be used to identify masked hypertension. Some evidence suggests that some individuals have masked hypertension on ABPM or HBPM, but not by both approaches. It is unclear whether the current results apply to masked hypertension identified by HBPM.
The current study has several strengths. First, there were four cohorts available for analysis. This allowed us to derive the CBP diagnostic index, externally validate it and estimate the number of US adults that would be recommended for ABPM across a range of cut-points on the index. The large number of participants from each cohort with non-elevated CBP provided large samples to derive and externally validate the CBP diagnostic index. Furthermore, these cohorts allowed us to compare test characteristics for cut-points on the CBP diagnostic index with prehypertension and the upper range of prehypertension. Additionally, the pooled validation cohort had a high representation of minorities including Hispanics in IDH and African Americans in the JHS.
Several limitations should be considered when interpreting the current results. Although the CBP diagnostic index was validated in a pooled cohort of IDH Study and JHS participants, it may not be generalizable to other populations. Masked hypertension was diagnosed using one 24-hour ABPM period. While some individuals with masked daytime and/or nocturnal hypertension on a single ABPM may not have it when repeated, conducting only one 24-hour ABPM period is common clinical practice.24 The cut-points may be different if an oscillometric device were used to measure CBP. Also, while all four studies used trained staff who followed standardized protocols to measure CBP, the effect of different intervals on successive CBP measurements (e.g., 30-seconds in the NHANES versus 1–2 minutes in other studies) is unclear. Further, CBP was measured following a research protocol in each of the individual studies. However, CBP measured in clinical practice is generally of poorer quality. Last, a possible limitation of the use of ABPM in clinical practice is that self-reported sleep disturbances are relatively common among those who undergo ABPM.
There are approximately 153 million adults with non-elevated CBP who are not taking antihypertensive medication in the US. Performing ABPM on all of these people in order to detect masked hypertension is not practical. Using the CBP diagnostic index, developed and validated in the current study, provides a simple approach to identify a sub-group of individuals for whom ABPM is better targeted. If identifying all individuals with masked hypertension is viewed as necessary, a cut-point of 190 mmHg on the CBP diagnostic index could be used. NHANES data indicate that 118.6 million US adults would be referred for ABPM under this approach. In contrast, fewer US adults would be referred to ABPM using higher cut-points on the CBP diagnostic index, but at the expense of lower sensitivity. The use of the upper range of prehypertension as screening criteria would result in masked hypertension not being identified in many people. In conclusion, the current study provides empirical data on various approaches for identifying masked hypertension in untreated adults with non-elevated CBP.
Supplementary Material
Acknowledgments
Study conception and design: JNBIII, PM, KMD, JES, DS; Acquisition, analysis or interpretation of data: JNBIII, PM, KMD, JES, DS; Statistical analysis: JNBIII, PM, DS; Drafting of the manuscript: JNBIII; Critical revision of the manuscript: JNBIII, PM, KMD, AJV, NB, JES, DS; Critical revision of the manuscript for important intellectual content: JNBIII, PM, KMD, AJV, NB, JS, DS, JNBIII, KMD, JES and DS had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding Sources: JNBIII: receives support through F31 HL129701 from the National Heart Lung and Blood Institute; PM: receives research support from NIH grant R01 HL080477 and Amgen, Inc.; KMD: receives support through R01 HL116470-02S1 from the National Heart Lung and Blood Institute; AJV: receives support through grant R01-HL098604; JES: receives support through grant P01-HL047540; DS: receives support through grants P01-HL047540, R01 HL117323-01, and K24-HL125704 from the National Heart Lung and Blood Institute.
Dr. Muntner received an institutional grant from Amgen Inc. Dr. Viera has served on the Medical Advisory Board for Suntech Medical, a manufacturer of a brand of ambulatory blood pressure monitor.
Footnotes
Disclosures: There are no other conflicts of interest.
References
- 1.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002 Dec;40(6):795–796. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- 2.Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens. 2014 Sep;28(9):521–528. doi: 10.1038/jhh.2014.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hansen TW, Kikuya M, Thijs L, et al. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007 Aug;25(8):1554–1564. doi: 10.1097/HJH.0b013e3281c49da5. [DOI] [PubMed] [Google Scholar]
- 4.Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, Determinants, and Clinical Significance of Masked Hypertension in a Population-Based Sample of African Americans: The Jackson Heart Study. Am J Hypertens. 2015 Jul;28(7):900–908. doi: 10.1093/ajh/hpu241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Brien E, Parati G, Stergiou G, et al. European society of hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013 Sep;31(9):1731–1768. doi: 10.1097/HJH.0b013e328363e964. [DOI] [PubMed] [Google Scholar]
- 6.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B, Guideline Development G. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891. [DOI] [PubMed] [Google Scholar]
- 7.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013 Jul;34(28):2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 8.O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003 May;21(5):821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 9.O'Brien E, Coats A, Owens P, et al. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British hypertension society. BMJ. 2000 Apr 22;320(7242):1128–1134. doi: 10.1136/bmj.320.7242.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003 Dec;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 11.Mancia G, De Backer G, Dominiczak A, et al. 2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens. 2007 Sep;25(9):1751–1762. doi: 10.1097/HJH.0b013e3282f0580f. [DOI] [PubMed] [Google Scholar]
- 12.Head GA, McGrath BP, Mihailidou AS, et al. Ambulatory blood pressure monitoring in Australia: 2011 consensus position statement. J Hypertens. 2012 Feb;30(2):253–266. doi: 10.1097/HJH.0b013e32834de621. [DOI] [PubMed] [Google Scholar]
- 13.Verdecchia P, O'Brien E, Pickering T, et al. When can the practicing physician suspect white coat hypertension? Statement from the Working Group on Blood Pressure Monitoring of the European Society of Hypertension. Am J Hypertens. 2003 Jan;16(1):87–91. doi: 10.1016/s0895-7061(02)03150-3. [DOI] [PubMed] [Google Scholar]
- 14.Williams B, Poulter NR, Brown MJ, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens. 2004 Mar;18(3):139–185. doi: 10.1038/sj.jhh.1001683. [DOI] [PubMed] [Google Scholar]
- 15.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005 Jan;45(1):142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 16.Alessi A, Brandao AA, Pierin A, et al. [IV Guideline for ambulatory blood pressure monitoring. II Guideline for home blood pressure monitoring. IV ABPM/II HBPM] Arq Bras Cardiol. 2005 Jul;85(Suppl 2):1–18. doi: 10.1590/S0066-782X2005002100001. [DOI] [PubMed] [Google Scholar]
- 17.Parati G, Omboni S, Palatini P, et al. Italian society of hypertension guidelines for conventional and automated blood pressure measurement in the office, at home and over 24 hours. High Blood Press Cardiovasc Prev. 2008 Oct;15(4):283–310. doi: 10.2165/0151642-200815040-00008. [DOI] [PubMed] [Google Scholar]
- 18.Ogihara T, Kikuchi K, Matsuoka H, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009) Hypertens Res. 2009 Jan;32(1):3–107. [PubMed] [Google Scholar]
- 19.Daskalopoulou SS, Khan NA, Quinn RR, et al. The 2012 Canadian hypertension education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol. 2012 May;28(3):270–287. doi: 10.1016/j.cjca.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 20.Seedat YK, Rayner BL Southern African Hypertension S. South African hypertension guideline 2011. S Afr Med J. 2012 Jan;102(1 Pt 2):57–83. [PubMed] [Google Scholar]
- 21.Group JCSJW. Guidelines for the clinical use of 24 hour ambulatory blood pressure monitoring (ABPM) (JCS 2010): - digest version. Circ J. 2012;76(2):508–519. doi: 10.1253/circj.cj-88-0020. [DOI] [PubMed] [Google Scholar]
- 22.Shimbo D, Newman JD, Schwartz JE. Masked hypertension and prehypertension: diagnostic overlap and interrelationships with left ventricular mass: the Masked Hypertension Study. Am J Hypertens. 2012 Jun;25(6):664–671. doi: 10.1038/ajh.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elliott WJ, Black HR. Prehypertension. Nat Clin Pract Cardiovasc Med. 2007 Oct;4(10):538–548. doi: 10.1038/ncpcardio0989. [DOI] [PubMed] [Google Scholar]
- 24.Abdalla M, Goldsmith J, Muntner P, et al. Is Isolated Nocturnal Hypertension A Reproducible Phenotype? Am J Hypertens. 2015 Apr 22; doi: 10.1093/ajh/hpv058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor HA, Jr, Wilson JG, Jones DW, et al. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005 Autumn;15(4 Suppl 6) S6-4-17. [PubMed] [Google Scholar]
- 26.NCHS Statistics. National Health and Nutrition Examination Survey: Center for Disease Control and Prevention. [Accessed Acessed September 10, 2015]; http://www.cdc.gov/nchs/nhanes.htm.
- 27.Wilson JG, Rotimi CN, Ekunwe L, et al. Study design for genetic analysis in the Jackson Heart Study. Ethn Dis. 2005 Autumn;15(4 Suppl 6) S6-30-37. [PubMed] [Google Scholar]
- 28.Barker MH, Erlanger J, Meakins J, et al. Standard method for taking and recording blood pressure readings. Journal of the American Medical Association. 1939;113:294–297. [Google Scholar]
- 29.Investigators. TJHS. Jackson Heart Study Protocol Manual 4: Blood Pressure, Visit 1. 2001 Feb 18; 2001. [Google Scholar]
- 30.Thijs L, Hansen TW, Kikuya M, et al. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007 Aug;12(4):255–262. doi: 10.1097/mbp.0b013e3280f813bc. [DOI] [PubMed] [Google Scholar]
- 31.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005 Feb 8;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 32.Fan HQ, Li Y, Thijs L, et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens. 2010 Oct;28(10):2036–2045. doi: 10.1097/HJH.0b013e32833b49fe. [DOI] [PubMed] [Google Scholar]
- 33.Shimbo D, Kuruvilla S, Haas D, Pickering TG, Schwartz JE, Gerin W. Preventing misdiagnosis of ambulatory hypertension: algorithm using office and home blood pressures. J Hypertens. 2009 Sep;27(9):1775–1783. doi: 10.1097/HJH.0b013e32832db8b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pickering TG. The natural history of hypertension: prehypertension or masked hypertension? J Clin Hypertens (Greenwich) 2007 Oct;9(10):807–810. doi: 10.1111/j.1751-7176.2007.tb00011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Redmond N, Booth JN, III, Tanner RM, et al. Associations of Masked Hypertension and Prehypertension with Subclinical Cardiovascular Disease in African Americans: Results from the Jackson Heart Study. doi: 10.1161/JAHA.115.002284. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fagard RH, Celis H, Thijs L, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008 Jan;51(1):55–61. doi: 10.1161/HYPERTENSIONAHA.107.100727. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.