Summary
Objective
Acutely restricting sleep worsens insulin sensitivity in healthy individuals whose usual sleep is normal in duration and pattern. The effect of recovery or weekend ‘catch-up’ sleep on insulin sensitivity and metabolically active hormones in individuals with chronic sleep restriction who regularly ‘catch-up’ on sleep at weekends is as yet unstudied.
Design
19 men (mean ± SEM age 28.6±2.0years, BMI 26.0±0.8kg/m2) with at least 6 months’ history (5.1±0.9years) of lifestyle driven, restricted sleep during the working week (373±6.6 min/night) with regular weekend ‘catch up’ sleep (weekend sleep extension 37.4±2.3%) completed an in-laboratory, randomised, cross-over study comprising 2 of 3 conditions, stratified by age. Conditions were 3 weekend nights of 10 hours, 6 hours or 10 hours time-in-bed with slow wave sleep suppression using targeted acoustic stimuli.
Measurements
Insulin sensitivity was measured in the morning following the 3rd intervention night by minimal modelling of 19 samples collected during a 2 hour oral glucose tolerance test. Glucose, insulin, c-peptide, leptin, peptide YY, ghrelin, cortisol, testosterone and luteinising hormone (LH) were measured from daily fasting blood samples; HOMA-IR, HOMA-β and QUICKI were calculated.
Results
Insulin sensitivity was higher following 3 nights of sleep extension compared to sustained sleep restriction. Fasting insulin, c-peptide, HOMA-IR, HOMA-β, leptin and PYY decreased with ‘catch-up’ sleep, QUICKI and testosterone increased, while morning cortisol and LH did not change. Targeted acoustic stimuli reduced SWS by 23%, but did not alter insulin sensitivity.
Conclusions
Three nights of ‘catch-up’ sleep improved insulin sensitivity in men with chronic, repetitive sleep restriction. Methods to improve metabolic health by optimising sleep are plausible.
Keywords: chronic sleep restriction, insulin sensitivity, ‘catch-up’ sleep, recovery sleep
Introduction
Chronic, lifestyle-driven sleep restriction is common in many modern ‘24/7’ societies, with about 40% of individuals relying on discretional time on weekends to ‘catch-up’ on sleep curtailment during the working week1, 2. The prevalence of obesity and type 2 diabetes mellitus is increasing to epidemic proportions, particularly in developing nations, in line with increasing globalisation, changes in nutrition and sedentary lifestyles3. Epidemiological, interventional and molecular experiments provide a strong rationale linking sleep restriction with these metabolic disorders. Recent large epidemiological studies have associated sleep loss to the development of both obesity4 and diabetes mellitus1, and short sleep duration to increased subcutaneous fat5. Experimentally restricting or perturbing sleep for 1 to 14 nights in duration worsens insulin sensitivity in healthy individuals whose usual sleep is normal in duration and pattern1. Molecular experiments show that adipocytes from sleep restricted individuals are resistant to insulin’s effects on phosphorylated Akt, a mediator in the insulin-signalling pathway6. Together, these data indicate that acute sleep restriction is metabolically harmful.
Although 40% of individuals ‘catch-up’ on sleep over the weekend, the metabolic effects of catch-up sleep is relatively understudied with no interventional studies to date. Cross-sectional epidemiological studies in children show that weekend ‘catch-up’ sleep is associated with a decreased risk of being overweight compared to perpetual short sleepers7–9. In adults, an hour of weekend ‘catchup’ sleep was associated with a 39% decreased risk of hypertension10. Given these epidemiological data, we therefore examined whether three nights of a saturating amount of ‘catch-up’ sleep following regular weekday sleep curtailment would improve insulin sensitivity in those with a history of such sleep patterns, compared to sustained sleep restriction. We also tried to unravel mechanisms. An exploratory aim was to examine the effect of targeted acoustic perturbation of slow-wave sleep (SWS) on insulin sensitivity since SWS has been implicated mechanistically in glucose homeostasis11. Finally, we also explored the effect of both sleep restriction and experimental perturbation of SWS on other hormones known to modify insulin sensitivity and food intake.
Methods
Study protocol
The study complied with Good Clinical Practice guidelines, applicable regulatory requirements and the Declaration of Helsinki. All participants provided written informed consent to participate in the study, which was approved by the Sydney South West Area Health Service Human Research and Ethics Committee (Concord Zone). The study is registered with the Australia New Zealand Clinical Trials Network, www.anzctr.org.au, number ACTRN12609000123246.
Screening and participants
Healthy male subjects aged between 18 and 50 years were recruited through local advertising. Inclusion criteria included regular sleep-wake patterns as per the description below and being agreeable to spend two weekends at the research institute. Exclusions included shift-workers, habitual napping (more than once per month from history), diabetes mellitus, a history of, or symptoms suggesting, a co-existing sleep disorder, including insomnia, obstructive sleep apnoea, parasomnias or restless legs syndrome. Those with uncontrolled medical conditions or a history of psychiatric disorders or drug abuse, including use of any sedative or neuroactive medications, or indeed any medication that might affect sleep, were also excluded. Subjects could not have crossed time-zones within one month of the study visits.
Screening included a full medical history, physical examination and detailed explanation of the study protocol. No subject had type 2 diabetes mellitus from history, confirmed by oral glucose tolerance test. Habitual sleep-wake patterns were objectively assessed over 2 weeks with at-home actigraphy incorporating sleep diary verification of sleep onset and wake up times (Actiwatch™, Philips/Respironics, PA, USA), analysed by two investigators. Subjects were included if mean weekday nightly sleep period over 2 weeks, between Monday and Thursday nights inclusive, was less than 6.5 hours(h)/night and mean nightly weekend sleep period, Friday and Saturday nights, was greater than 25% of the weekday mean. Sleep disordered breathing was excluded by three nights assessment with a portable single channel nasal flow recording device (Flow Wizard™, DiagnoseIT, Sydney, Australia)12.
Randomisation
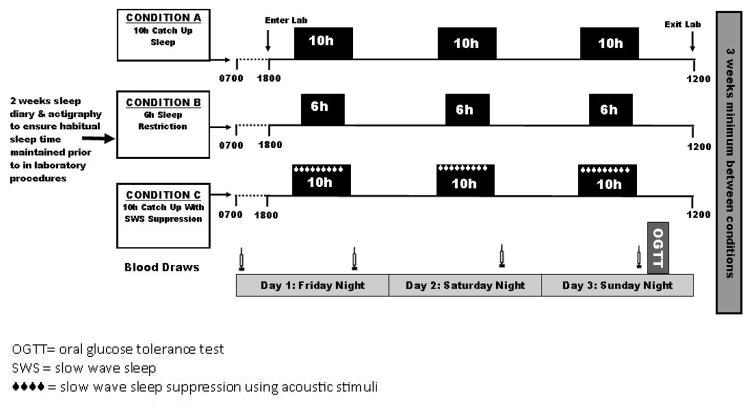
All participants underwent 2 out of 2 or 3 potential study conditions, in a randomised order, two period crossover design. The three potential study conditions were 3 weekend nights (Friday night to Monday morning) of: (A) 10h time in bed (TIB) each night, (B) 6h TIB each night or (C) 10h TIB with SWS suppression by acoustic stimuli (10h↓SWS) each night-Figure 1. Those aged ≤35 years (group 1) could be randomised to any 2 of the 3 conditions. Those >35 years (group 2) could only be randomised to Condition A (6h TIB) or Condition B (10h TIB). Men >35 years were not randomised to Condition C (10h↓SWS) because SWS is already reduced in this age group. Two separate randomisation lists for young and older men were computer-generated in blocks of 4. There was a minimum of 3 weeks wash-out between each study visit.
Figure 1.
Study design. Subjects were randomised to undergo 2 of 3 (young men) or 2 (older men) conditions in random order: i.e. AB, BA, AC, CA, BC or CB in young men; or, AB or BA in older men. There was 3 weeks washout between conditions.
Study visits
General
For 2 weeks prior to a study weekend visit, subjects were asked to maintain their regular ‘catch-up’ sleep-wake schedules at home and this was verified by inspection of actigraphy and sleep diaries, with any deviation resulting in a study weekend being rescheduled. Subjects were asked to restrict caffeine and alcohol to two or less drinks or units per day at home. The study was conducted within the chronobiology laboratory in the research institute. Subjects were encouraged to be sedentary, not to sleep outside of scheduled times, and had their own bedroom with ensuite with access to a shared living area. Ambient lighting was kept at less than 50 lux for the duration of the study visit to minimise any phase shift. Subjects were not permitted to exercise or leave the chronobiology laboratory. Study staff ensured subjects did not nap, through continuous camera or direct visual surveillance.
Sleep scheduling
Time of lights out was calculated by the subject’s screening actigraphy. The weekday (Monday to Thursday nights inclusive) mean sleep centre-point for each subject was calculated and lights-on and lights-off times were individually centred on that time for each condition. Subjects were only told of their lights-off time immediately prior to bed on the first evening. They were instructed that if they woke prior to lights on, they should remain in bed attempting further sleep until the lights were switched on. Loudspeakers were present in all bedrooms, irrespective of whether used or not.
Study schedule
Figure 1 shows the study visit schedule. Subjects arrived fasted on Friday morning for blood sampling (glucose, insulin, c-peptide, leptin, peptide YY (PYY), total ghrelin, cortisol, total testosterone and luteinising hormone (LH)), verification of their sleep compliance with actigraphy data and to answer the Epworth Sleepiness Score (ESS)13 and Horne-Ostberg Morningness-Eveningness Questionnaire (MEQ)14. Height and weight were measured by standard methods. Subjects were asked to refrain from caffeine completely from that time. They returned to the facility on Friday from 5pm and then did not leave the facility until after tests were completed on Monday morning. Following each night of the study condition, fasting blood samples were taken immediately after wake-up (for glucose, insulin, c-peptide, leptin, PYY, total ghrelin, cortisol, testosterone and LH). On Monday morning within 30–60 minutes of wake-up, subjects underwent a frequently sampled (19 samples), two hour, oral glucose tolerance test to determine insulin sensitivity. After baseline fasting hormone levels were taken through an intravenous cannula, 75g of glucose was administered orally, then samples were taken after 5, 10, 15, 20, 25, 30, 35, 40, 45, 50, 55, 60, 70, 80, 90, 100, 110 and 120 minutes for insulin, c-peptide and glucose measurements. Samples were centrifuged immediately and frozen to minus 80 degrees Celsius until assayed. Detailed hormonal assay methodology can be found in Supplementary table S1. Insulin sensitivity was determined by minimal model analysis15, 16. Area-under-the-curve (AUC) for glucose and insulin was calculated using the trapezoid rule. HOMA-IR, HOMA-β17 and QUICKI18 indices of insulin sensitivity were calculated.
Polysomnography and slow wave sleep suppression
Polysomnography was recorded each night using standard electrode placement (Sandman Elite V.9.2, Tyco Healthcare, Denver, Colorado, USA). Leads were referenced to the contralateral mastoid position. Sleep stages were scored using standardised criteria 19 by one scorer, with strict attention to delta wave voltage criteria. SWS was suppressed using acoustic stimuli on all three weekend nights of Condition C. Delta waves were recognised visually in real-time on the central leads of the electroencephalogram (EEG) by the researchers. When two or more consecutive delta waves were seen, a mixed frequency ramped tone was played through bilateral loudspeakers next to the subject’s bed, ramping from 40dB to 95dB (measured at the approximate location of the subject’s head), until delta activity was suppressed. If the maximum volume tone did not control delta activity, the researchers would go into the bedroom, gently disturb the subject and say their name.
Power Spectral Analysis
Power spectral analysis was performed on a central lead of the EEG to determine non-rapid eye movement (NREM) mean delta power, NREM relative delta power density (% delta power/total power across all frequency bands) and total NREM delta power (mean delta power x number of 30 second epochs x2) after removal of EEG artefact using an automated method with visual verification20. If noise artefact was present in over 25% of the channel, it was discarded from analysis (10/114 studies). Lead C3-M2 was utilised unless the signal quality was suboptimal, whereby C4-M1 was substituted for all 6 nights for that subject (n=4). Fast Fourier transformation was performed on five second epochs over the entire frequency bands, with the delta range (0.75–4.5Hz) the primary focus for analysis20.
Food intake and exercise
Meals were chosen from a menu which included healthy balanced frozen meals for breakfast, lunch and dinner, with snacks available. Quantity of food was not restricted over the 1st weekend visit. During the 2nd weekend study visit, each subject was served exactly the same meals and snacks they had consumed during the first weekend, to ensure dietary intake was standardised over both weekends. Food intake for each individual was summed from the available nutritional information. No caffeine, alcohol or chocolate was available. Breakfast was served 30 minutes after the subject’s wake-up time, lunch at 12.30pm and dinner at 6.30pm. All subjects obliged with the dietary instructions and minimal deviation occurred, except occasionally for food availability, when a similar meal was provided. Diet was not monitored in between study visits.
Statistical analysis
Our primary aim was to determine if ‘catch-up’ sleep would improve insulin sensitivity, and our exploratory aim was to unravel potential mechanisms by which this might occur, such as through changes in SWS and/or hormones known to be metabolically active. The primary outcome was the difference in insulin sensitivity, determined by minimal modelling, after three nights of each sleep condition. Secondary outcomes were disposition index and hormones (leptin, PYY, ghrelin, cortisol, testosterone, LH). Tertiary outcomes were insulin sensitivity measured by HOMA and QUICKI, fasting and/or AUC glucose, insulin and c-peptide. The polysomnographic findings are not outcomes – these variables were analysed to verify that the intervention (i.e. catch-up sleep, slow wave sleep suppression) altered sleep duration and architecture as expected. Data were analysed using SAS version 9.2 (SAS Institute) using paired t tests and mixed model analysis for repeated measures where appropriate incorporating ‘condition’, ‘day’ and interaction terms, with two-tailed p values <0.05 considered significant. Normality of data or of residuals was assessed, as appropriate. Data transformation was not required. Period and crossover effects were excluded from available baseline data of each weekend21. Results were assessed separately for group 1 compared to overall, and a ‘group*condition’ term was utilised to assess for any age interaction of the older group on the overall results. Data are described as means and standard errors, or differences and 95% confidence intervals as appropriate.
Results
Demographics
315 people responded to advertising; 49 attended full screening, of which 21 men were randomised: 18 in group 1 (≤ 35 years) and 3 in group 2 (>35 years), with 19 subjects completing both weekend visits. The main reasons for screen failures were not exhibiting sufficient sleep restriction during the working week (n=9 of 28; 32%), or not reaching the criteria set of 25% catch-up sleep on weekends (n=6 of 28; 22%). In group 1; one subject was randomised who did not undergo either weekend visit and another subject withdrew following one weekend due to needle phobia. Due to within-person study design, neither individual could be analysed. The following participants completed each of the 3 possible condition pairings:
10h TIB/6h TIB: n=8
10h TIB/10h↓SWS: n=6
6h TIB/10h↓SWS TIB: n=5
Screening characteristics are shown in Table 1; demonstrating subjects were sleep restricted during the working work (6h 12min/night±7min). All men showed a significant increase in weekend sleep compared to weekday sleep (mean weekend sleep extension 37.3%±2.4)-Supplementary Figure S1. Hence, a 6h sleep opportunity was almost identical to the average time spent asleep during weekdays, whereas a 10h sleep opportunity exceeded the time each slept during weekends-Supplementary Figure S1. All subjects had habituated to these sleep patterns regularly at home for at least six months and on average 5.1years±0.9. The most common reason for these sleep patterns was working long hours, alongside studying and time commuting to and from work and/or study. MEQ excluded preference for morning or evening (mean 47.3± 1.5; ‘neither type’ category range 42–5814). Other than age and BMI being higher, descriptively the older group did not alter the overall mean demographics. ESS was within the normal range, excluding subjective sleepiness. No significant differences in BMI or sleep parameters by actigraphy for the 2 weeks leading up to study visits were found between the two weekends-Supplementary Table S2.
Table 1.
Screening characteristics (means ± SEM)
| n=19 | Mean ± SEM | Range |
|---|---|---|
| Age (yrs) | 28.6±2.0 | 19–49 |
| Midweek sleep1 | 6h 12m±7m | 5h 18m–6h 54m |
| Weekend sleep2 | 8h 30m±9m | 6h 59m–9h 39m |
| Weekend sleep extension3 (%) | 37.3±2.4 | 19–56 |
| Duration of catch-up sleep patterns (yrs) | 5.1±0.9 | 0.5–15 |
| MEQ score4 | 47.1±1.5 | 34–58 |
Defined as average rest period Monday to Thursday inclusive over 2 weeks screening by actigraphy and diaries
Defined as average rest period Friday and Saturday over 2 weeks screening
Defined as % more weekend sleep compared to midweek sleep over 2 weeks screening
MEQ- Horne-Ostberg Morningness-Eveningness Questionnaire (definite evening type 16–30; moderate evening type 31–41; neither type 42–58; moderate morning type 59–69; definite morning type 70–86)
Sleep parameters- the intervention
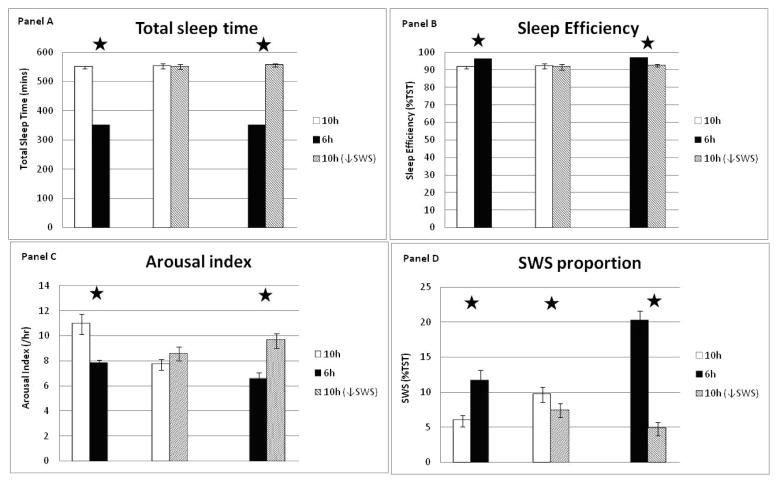
PSG sleep parameters and power spectral analysis results are shown in Figure 2 and Supplementary Figures S2. Across the pairs of conditions, expected significant differences were seen in total sleep time (TST)-Figure 2A, sleep efficiency (percentage time asleep during time in bed)-Figure 2B and sleep latency-Supplementary Figure 2A. Notably sleep efficiency exceeded 90% for all conditions, and the 10h↓SWS condition compared to 10h did not significantly reduce TST nor sleep efficiency, despite the acoustic stimuli-Figure 2A, B. The 6h condition had a significantly reduced arousal index compared to 10h (p<0.001) or 10h↓SWS (p<0.001), consistent with maintaining a more consolidated sleep with sustained sleep restriction-Figure 2C. Arousal index in the 10h↓SWS condition compared to 10h although higher, did not reach significance (p=0.09). The 10h↓SWS condition reduced SWS quantity by 23% (− 12.6min, −23.4 to −1.8, p=0.02) compared to 10h and by 62% compared to 6h (−43.6min, −55.0 to −32.3, p<0.001), as expected by the experimental protocol-Supplementary Figure S2B. The 6h condition had the highest SWS proportion (%TST) across all pairs of conditions (compared to 10h, p<0.001; compared to 10h↓SWS, p<0.001)-Figure 2D.
Figure 2.
Polysomnographic sleep parameters between pairs of conditions averaged over 3 experimental nights.
Panels: A- TST (mins), B- sleep efficiency (%TST), C-arousal index (events/hr), D- SWS proportion (%TST)
10h/6h n=8, 10h/10h↓SWS n=6, 6h/10h↓SWS n=5. Error bars are SEM.
* represents significance p<0.05
In examining the delta power of the EEG, 10h↓SWS reduced mean NREM delta power by 10% (−41.7 μV2, −69.3 to −13.9, p=0.005) and relative delta power compared to 10h (p=0.0002), as anticipated by the acoustic stimuli protocol-Supplementary Figure S2E, F. The 6h condition had significantly higher mean NREM delta power and relative delta power compared to either 10h (p<0.001) or 10h↓SWS (p<0.001), as expected with sustained sleep restriction-Supplementary Figure S2E, F.
Metabolic outcomes-insulin sensitivity
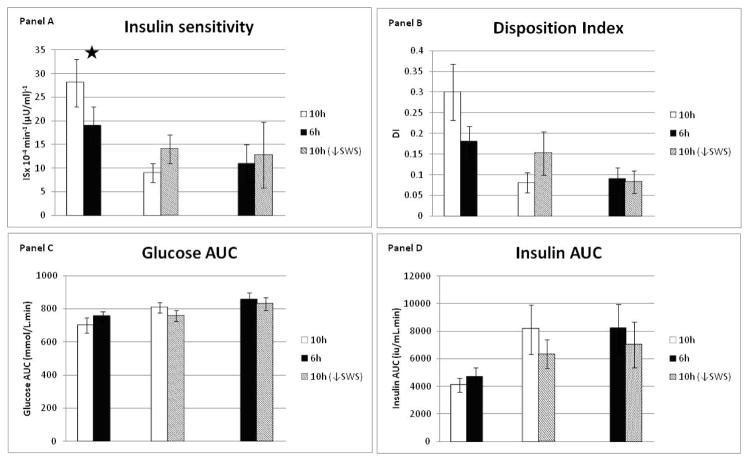
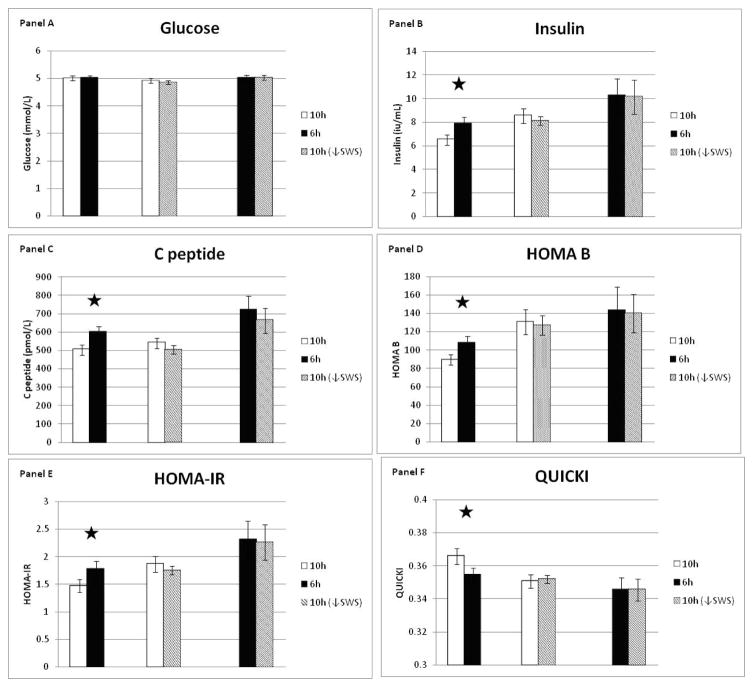
Results for the main metabolic parameters are shown in Figures 3 & 4. Period and carryover effects were excluded by analysing Friday baseline values where available. Insulin sensitivity (ISx) was significantly increased following 3 nights of ‘catch-up’ sleep (10h) compared to continuing sleep restriction (6h) (8.57×10−4 min−1 (μU/ml)−1, 1.1 to 16.1×10−4, p=0.03)-Figure 3A. There were no significant differences between 10h↓SWS and either 10h (p=0.17) or 6h (p=0.6). Changes of similar magnitude and direction were seen for disposition index (DI), but these were not statistically significant-Figure 3B. Glucose AUC was significantly lower in 10h compared to 6h in the younger men (−69.2 mmol.min.L−1 CI −119.7, −18.6), p=0.02), but not in the young and old men together (p=0.14)-Figure 3C. Insulin AUC differences were not significant-Figure 3D. Daily fasting morning hormone levels showed significant reductions in fasting insulin, c-peptide, HOMA-IR, HOMA-β and an increase in QUICKI following 10h compared to 6h-Figure 4- all consistent with improvements. Only 1% of insulin, c-peptide and glucose values were missing. Certain results showed an age effect, with the older subjects having higher C-peptide, glucose and leptin levels, however this did not alter the overall significances of differences when an age factor was applied to the model.
Figure 3.
Metabolic outcomes between pairs of conditions from minimal model of an oral glucose tolerance test performed on Monday after 3 nights of each condition.
Panels: A-insulin sensitivity (min−1 (μU/mL)−1), B-disposition index, C-glucose area-under-the-curve (AUC- mmol/L.min), D-insulin AUC (iu/mL.min).
10h/6h n=8, 10h/10h↓SWS n=6, 6h/10h↓SWS n=5. Error bars are SEM.
* represents significance p<0.05
Figure 4.
Metabolic outcomes between pairs of conditions from daily fasting blood samples showing mean values across Sat/Sun/Mon.
Panels: A-glucose (mmol/L), B-insulin (iu/ml), C- c peptide (pmol/L), D-HOMA-β, E- HOMA-IR, F- QUICKI.
10h/6h n=8, 10h/10h↓SWS n=6, 6h/10h↓SWS n=5. Error bars are SEM.
* represents significance p<0.05
Metabolic outcomes-appetite hormones, cortisol, testosterone
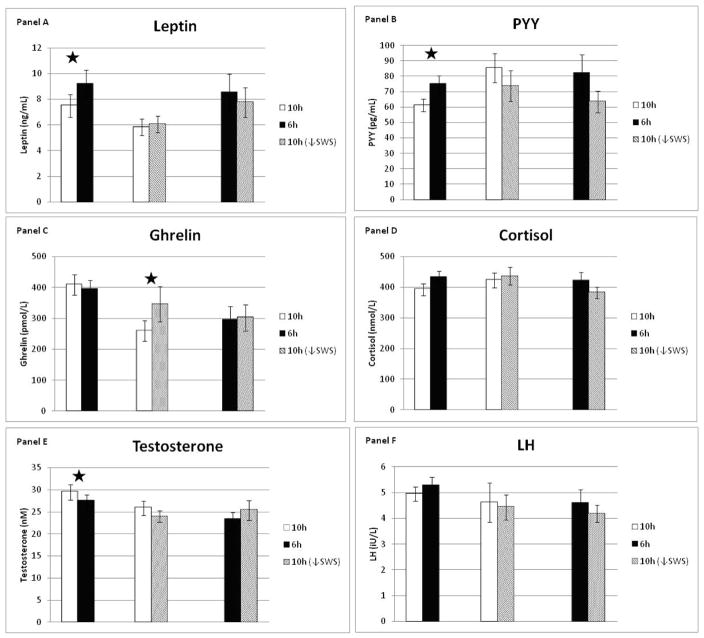
Leptin was significantly reduced following 10h ‘catch-up’ sleep compared to 6h (−1.69ng/mL (−0.6, −2.8); p=0.003), along with a corresponding reduction in PYY (−12.7pg/mL (−2.1, −23.3); p=0.02), but no change was seen in total ghrelin (p=0.59)-Figure 5A–C. There was no significant change in fasting morning cortisol levels between any of the condition pairings-Figure 5D.
Figure 5.
Metabolic outcomes between pairs of conditions from daily fasting blood samples showing mean values across Sat/Sun/Mon.
Panels: A-leptin (ng/ml), B- PYY (pg/mL), C-ghrelin (pmol/L), D-cortisol (nmol/L), E-testosterone (nM), F-lutenising hormone (LH-iU/L).
10h/6h n=8, 10h/10h↓SWS n=6, 6h/10h↓SWS n=5. Error bars are SEM.
* represents significance p<0.05
The amount of food consumed between weekend visits was not significantly different for each individual (1st weekend=6230kcal, 2nd weekend= 6291kcal; p=n/s). Nor was there any significant difference between the amount of energy intake between sleep conditions, when specifically looking at only the first weekend chronologically when food choices were made, independent of condition pairing (10h = 6394kcal, 6h=5845kcal, 10h↓SWS = 6426kcal; p=n/s). Only food choices from the first weekend were analysed because subjects were not allowed to rechoose on the second weekend. Furthermore when exploring only those in the 10h/6h condition pairing, no significant difference was seen between food choice as determined by energy intake on the first weekend (10h = 6250kcal, 6h= 5844kcal; p=n/s). Fasting morning testosterone levels were significantly higher following 10h compared to 6h (2.2nM (0.2, 4.2); p=0.03) in both the group as a whole (n=8) and in the younger group alone (n=5)-Figure 5E. The older men (n=3) had lower levels compared to the younger men, as expected with ageing (p=0.01). LH was not significantly different between any of the condition pairings-Figure 5F.
Discussion
‘Catch-up’ sleep is highly prevalent with >40% of working aged adults sleeping more on weekends compared to weekdays2. Understanding the metabolic implications of these lifestyle choices is therefore highly relevant. We show that men who regularly adopt lifestyle-driven, chronic, repetitive sleep restriction with weekend ‘catch-up’ sleep, significantly improved insulin sensitivity by 45% following three nights of a saturating sleep compared to ongoing sleep restriction, as measured by minimal model after an oral glucose challenge. HOMA-IR decreased and QUICKI increased. Accordingly, 3 separate measures of ISx all showed improved insulin sensitivity with ‘catch-up’ sleep. These data are novel and together attest to the veracity of this finding. Previous studies have shown that sleep restriction of 1 night to 2 weeks has a negative impact on markers of glucose homeostasis22–25, but have examined subjects with regular sleep patterns, unlike those in our study. Our finding of a 45% improvement in ISx with ‘catch-up’ sleep is complementary and consistent with previous studies showing a 20–25% worsening of ISx with sleep restriction1.
‘Catch-up’ sleep decreased fasting insulin, c-peptide and HOMA-β, likely reflecting the concomitant improvement in ISx. ‘Catch-up’ sleep increased morning testosterone and did not change morning cortisol. These findings are consistent with other studies of sleep restriction26, 27. Randomised controlled trials directly show that testosterone treatment improves ISx in men who are obese28, as well as in men with disrupted and reduced sleep from obstructive sleep apnoea29. Testosterone improves glycaemic control in men with type 2 diabetes mellitus30 and reduces obesity and metabolic syndrome31. Meta-analyses show significant reductions in fasting plasma glucose, fat mass and triglycerides with testosterone therapy in men with type 2 diabetes mellitus30. Previous studies have shown that sleep restriction can increase evening, but not morning, cortisol22, 24–26, with no change in mean cortisol across 24 hours1. Interventional studies conclusively show that increased afternoon/evening cortisol worsens insulin resistance in humans32 and rodents33. These findings occur because maintaining cortisol concentrations during the 4–6 hours of the circadian nadir (early evening) is important to avoid effects of glucocorticoid excess on peripheral tissues33. Whether or not sleep impacts insulin sensitivity through these hormonal changes is plausible, but remains to be determined.
We examined satiety and hunger hormones released by adipose tissue (leptin-satiety signal), small intestine (PYY-satiety) and stomach (ghrelin-hunger) as secondary outcomes. ‘Catch-up’ sleep decreased leptin and PYY compared with continued sleep restriction, but did not alter ghrelin or food choice determined by energy intake. Studies have shown conflicting changes in appetite hormones with sleep restriction due to differing food intake, energy balance at time of assessment, gender differences and possible changes in circadian rhythm1, 26, 34. However, our subjects ate the same meals across both weekends, albeit ad libitum during the first weekend. Energy expenditure was not measured, however exercise was not allowed. Circadian shift was minimised, as sleep opportunity was centred individually to home sleep patterns and lighting was <50 lux. Although decreased leptin and PYY should decrease satiety, we did not observe a change in energy intake. Although surprising, these data are consistent with recent data showing sleep restriction increased leptin and PYY, and decreased ghrelin in a carefully conducted study utilising 24h assessment of these hormones34. We found no change in ghrelin with ‘catch-up’ sleep, although decreasing SWS increased ghrelin. This novel finding requires replication in other studies since we did not adjust for multiple testing for this or any of the other secondary outcomes.
SWS is a metabolically active sleep stage and others have shown that disrupting SWS can worsen ISx 11. In our hands, targeted acoustic stimuli significantly disrupted SWS and reduced delta power, but the absolute effect, although significant, was small in magnitude. ISx was not altered, in contrast with previous studies11, 35. This discrepancy could be explained if a minimal reduction in SWS required to worsen ISx was not achieved in our chronically sleep restricted subjects, or if other factors such as sleep fragmentation and/or arousals per se are ultimately responsible35. On the other hand, our study was likely underpowered to show an effect of SWS suppression on ISx, in part because both baseline SWS and ability to suppress SWS were highly variable in our study population and also because it proved to be much more difficult to suppress SWS in a population that is chronically sleep deprived than we had originally anticipated.
These experimental findings exploring chronic repetitive sleep restriction are highly relevant because such sleep patterns are common in modern society and it has been suggested that chronic sleep restriction leads to the development of obesity and diabetes mellitus36, in addition to other cardiometabolic consequences37. Over a prolonged period of time (years or decades) this improvement in insulin sensitivity could be highly relevant in delaying or even preventing prediabetes or type 2 diabetes mellitus in a relatively healthy young individual. In a population of millions of individuals, this change in insulin sensitivity would translate to decreased prediabetes and diabetes mellitus in the community. Furthermore, interventional studies now show that sleep restriction increases weight38 and decreases fat proportion lost in those trying to lose weight through planned negative energy balance1. Studies attempting to manipulate sleep in the home setting have not been adequately powered to show changes in ISx given the increased variability that can occur in an uncontrolled non-laboratory environment. Nevertheless, larger community based sleep extension trials are required, but need to be sufficiently large to account for variable adherence to the sleep intervention, the introduction of confounders outside of the laboratory and possibly for a between-group study design.
Indeed, this wide variability in ISx is one potential limitation for our investigation. This variability was readily observed by examining the inter-individual differences in response to 10h of sleep repletion (Figure 3A), and could be related to age, lifetime duration of chronic sleep deprivation, degree of at-home sleep restriction or many other variables. In fact, these factors may contribute to the wide variability observed in ISx in the general population. Our sample size was too small for us to determine these factors, but the goal of the study was to determine effects of recovery ‘catch-up’ sleep on ISx and here, the crossover study design allowed a paired statistical analysis to examine the effect of sleep repletion within the same person, using 57 measurements (19 measurements each for insulin, C-peptide and glucose) to precisely measure ISx, thereby negating the impact of inter-individual differences in ISx among individuals. Indeed, paired student t-tests, as we implemented, remain valid without an increase in type 1 error over 0.05 even with these sample sizes39 and Student’s original paper utilised a sample size of 440. Another possible limitation is that 3, not 2, nights of ‘catch-up’ sleep was tested, whereas the latter might be more consistent with a weekday/weekend pattern. However, our proof-of-concept study of 3 nights ‘catch-up’ sleep is still feasible in the community, wherein additional sleep on the 3rd (Sunday) night could be achieved with an earlier bedtime. Nevertheless further studies of 1 and 2 nights of sleep repletion are needed to explore the chronology of metabolic recovery. Our population was specifically in individuals with ‘catch-up’ sleep patterns, and may not be generalisable to the other populations including those with other sleep disorders such as obstructive sleep apnea.
Our study examines, for the first time, a population regularly using ‘catch-up’ sleep. We show that ‘catch-up’ sleep improved ISx over continued sleep restriction, thereby confirming that extending sleep is potentially beneficial at least in non-diabetic men with long-standing chronic, repetitive sleep restriction. Critically, our intervention of 10h sleep opportunity translated to actual sleep since sleep efficiencies >90% and exceeded the usual amount of sleep extension of every participant, raising the possibility that their habitual attempts at ‘catch-up’ sleep were suboptimal. These data suggest that many in our society should sleep more, but further studies will be required to determine how much more sleep is needed in which specific individuals and whether planning to consistently sleep more every night is, in the long-run, ultimately superior to the occasional 1, 2 or 3 nights of ‘catch-up’ sleep.
Supplementary Material
Supplementary Figure S1: Screening sleep period times - weekend sleep period (mean minutes/night of Fri/Sat inclusive) versus midweek (mean minutes/night Mon to Thurs inclusive). White triangles indicate subjects who were randomised to condition pairing 10h/6h only. Straight lines indicate the experimental conditions of 6h or 10h sleep opportunities.
Supplementary Figure S2: Additional polysomnographic sleep parameters and power spectral analysis results between pairs of conditions averaged over 3 experimental nights.
Panels: A- Sleep latency (mins), B-SWS mins, C-NREM proportion (%TST), D-REM proportion (%TST), E-NREM mean delta power by power spectral analysis (μV2), F- NREM relative delta power (% total power).
10h/6h n=8, 10h/10h↓SWS n=6, 6h/10h↓SWS n=5. Error bars are SEM.
* represents significance p<0.05
Supplementary Table S1: Methodology- Detailed Hormonal Assay Information
Supplementary Table S2: Baseline characteristics between study visits
Acknowledgments
This project was supported by the National Health and Medical Research Council of Australia (NHMRC) through seed funding from the Centre for Integrated Research and Understanding of Sleep (CIRUS). RK was supported by an NHMRC scholarship (633161) and CIRUS scholarship, CMH by an NHMRC scholarship (512057) and CIRUS post-doctoral fellowship, KM by an NHMRC scholarship (633166), PYL by a NHMRC Senior Research Fellowship (1025248), R01 HL124211 and by the National Center for Advancing Translational Sciences through UCLA CTSI Grant UL1TR000124.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NHMRC or NIH.
The authors have no conflict of interests to declare.
The study is registered with the Australia New Zealand Clinical Trials Network, www.anzctr.org.au, number ACTRN12609000123246.
References
- 1.Killick R, Banks S, Liu PY. Implications of sleep restriction and recovery on metabolic outcomes. J Clin Endocrinol Metab. 2012;97:3876–3890. doi: 10.1210/jc.2012-1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Sleep Foundation. International Bedroom Poll. National Sleep Foundation; 2013. [Google Scholar]
- 3.Lam DW, LeRoith D. The worldwide diabetes epidemic. Curr Opin Endocrinol Diabetes Obes. 2012;19:93–96. doi: 10.1097/MED.0b013e328350583a. [DOI] [PubMed] [Google Scholar]
- 4.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yi S, Nakagawa T, Yamamoto S, Mizoue T, Takahashi Y, Noda M, Matsushita Y. Short sleep duration in association with CT-scanned abdominal fat areas: the Hitachi Health Study. Int J Obes (Lond) 2013;37:129–134. doi: 10.1038/ijo.2012.17. [DOI] [PubMed] [Google Scholar]
- 6.Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction: a randomized, crossover study. Ann Intern Med. 2012;157:549–557. doi: 10.7326/0003-4819-157-8-201210160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim CW, Choi MK, Im HJ, Kim OH, Lee HJ, Song J, Kang JH, Park KH. Weekend catch-up sleep is associated with decreased risk of being overweight among fifth-grade students with short sleep duration. J Sleep Res. 2012;21:546–551. doi: 10.1111/j.1365-2869.2012.01013.x. [DOI] [PubMed] [Google Scholar]
- 8.Wing YK, Li SX, Li AM, Zhang J, Kong AP. The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics. 2009;124:e994–e1000. doi: 10.1542/peds.2008-3602. [DOI] [PubMed] [Google Scholar]
- 9.Stone MR, Stevens D, Faulkner GE. Maintaining recommended sleep throughout the week is associated with increased physical activity in children. Prev Med. 2013;56:112–117. doi: 10.1016/j.ypmed.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Hwangbo Y, Kim WJ, Chu MK, Yun CH, Yang KI. Association between weekend catch-up sleep duration and hypertension in Korean adults. Sleep Med. 2013;14:549–554. doi: 10.1016/j.sleep.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105:1044–1049. doi: 10.1073/pnas.0706446105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rofail LM, Wong KK, Unger G, Marks GB, Grunstein RR. The utility of single-channel nasal airflow pressure transducer in the diagnosis of OSA at home. Sleep. 2010;33:1097–1105. doi: 10.1093/sleep/33.8.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 14.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 15.Dalla Man C, Caumo A, Cobelli C. The oral glucose minimal model: estimation of insulin sensitivity from a meal test. IEEE Trans Biomed Eng. 2002;49:419–429. doi: 10.1109/10.995680. [DOI] [PubMed] [Google Scholar]
- 16.Dalla Man C, Campioni M, Polonsky KS, Basu R, Rizza RA, Toffolo G, Cobelli C. Two-hour seven-sample oral glucose tolerance test and meal protocol: minimal model assessment of beta-cell responsivity and insulin sensitivity in nondiabetic individuals. Diabetes. 2005;54:3265–3273. doi: 10.2337/diabetes.54.11.3265. [DOI] [PubMed] [Google Scholar]
- 17.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 18.Trout KK, Homko C, Tkacs NC. Methods of measuring insulin sensitivity. Biol Res Nurs. 2007;8:305–318. doi: 10.1177/1099800406298775. [DOI] [PubMed] [Google Scholar]
- 19.Rechtschaffen A, Kales A. A manual of standardized terminology, technique and scoring system for sleep stages of human subjects. Brain Information Service/Brain Research Institute, University of California Los Angeles; Los Angeles, California: 1968. [Google Scholar]
- 20.D’Rozario AL, Dungan GC, 2nd, Banks S, Liu PY, Wong KK, Killick R, Grunstein RR, Kim JW. An automated algorithm to identify and reject artefacts for quantitative EEG analysis during sleep in patients with sleep-disordered breathing. Sleep Breath. 2014 doi: 10.1007/s11325-014-1056-z. [DOI] [PubMed] [Google Scholar]
- 21.Pocock S. Clinical Trials: A Practical Approach 1983 [Google Scholar]
- 22.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 23.Donga E, van Dijk M, van Dijk JG, Biermasz NR, Lammers GJ, van Kralingen KW, Corssmit EP, Romijn JA. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010;95:2963–2968. doi: 10.1210/jc.2009-2430. [DOI] [PubMed] [Google Scholar]
- 24.Nedeltcheva AV, Kessler L, Imperial J, Penev PD. Exposure to recurrent sleep restriction in the setting of high caloric intake and physical inactivity results in increased insulin resistance and reduced glucose tolerance. J Clin Endocrinol Metab. 2009;94:3242–3250. doi: 10.1210/jc.2009-0483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010;59:2126–2133. doi: 10.2337/db09-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reynolds AC, Dorrian J, Liu PY, Van Dongen HP, Wittert GA, Harmer LJ, Banks S. Impact of five nights of sleep restriction on glucose metabolism, leptin and testosterone in young adult men. PLoS One. 2012;7:e41218. doi: 10.1371/journal.pone.0041218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leproult R, Van Cauter E. Effect of 1 week of sleep restriction on testosterone levels in young healthy men. JAMA. 2011;305:2173–2174. doi: 10.1001/jama.2011.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marin P, Oden B, Bjorntorp P. Assimilation and mobilization of triglycerides in subcutaneous abdominal and femoral adipose tissue in vivo in men: effects of androgens. J Clin Endocrinol Metab. 1995;80:239–243. doi: 10.1210/jcem.80.1.7829619. [DOI] [PubMed] [Google Scholar]
- 29.Hoyos CM, Yee BJ, Phillips CL, Machan EA, Grunstein RR, Liu PY. Body compositional and cardiometabolic effects of testosterone therapy in obese men with severe obstructive sleep apnoea: a randomised placebo-controlled trial. Eur J Endocrinol. 2012;167:531–541. doi: 10.1530/EJE-12-0525. [DOI] [PubMed] [Google Scholar]
- 30.Corona G, Monami M, Rastrelli G, Aversa A, Sforza A, Lenzi A, Forti G, Mannucci E, Maggi M. Type 2 diabetes mellitus and testosterone: a meta-analysis study. Int J Androl. 2011;34:528–540. doi: 10.1111/j.1365-2605.2010.01117.x. [DOI] [PubMed] [Google Scholar]
- 31.Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F, Lenzi A, Forti G, Mannucci E, Maggi M. Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med. 2011;8:272–283. doi: 10.1111/j.1743-6109.2010.01991.x. [DOI] [PubMed] [Google Scholar]
- 32.Plat L, Leproult R, L’Hermite-Baleriaux M, Fery F, Mockel J, Polonsky KS, Van Cauter E. Metabolic effects of short-term elevations of plasma cortisol are more pronounced in the evening than in the morning. J Clin Endocrinol Metab. 1999;84:3082–3092. doi: 10.1210/jcem.84.9.5978. [DOI] [PubMed] [Google Scholar]
- 33.Jacobson L. Hypothalamic-pituitary-adrenocortical axis regulation. Endocrinol Metab Clin North Am. 2005;34:271–292. vii. doi: 10.1016/j.ecl.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Markwald RR, Melanson EL, Smith MR, Higgins J, Perreault L, Eckel RH, Wright KP., Jr Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci U S A. 2013;110:5695–5700. doi: 10.1073/pnas.1216951110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stamatakis KA, Punjabi NM. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest. 2010;137:95–101. doi: 10.1378/chest.09-0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cappuccio FP, Miller MA. Is prolonged lack of sleep associated with obesity? BMJ. 2011;342:d3306. doi: 10.1136/bmj.d3306. [DOI] [PubMed] [Google Scholar]
- 37.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spaeth AM, Dinges DF, Goel N. Effects of Experimental Sleep Restriction on Weight Gain, Caloric Intake, and Meal Timing in Healthy Adults. Sleep. 2013;36:981–990. doi: 10.5665/sleep.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Winter JCF. Using the Student’s t-test with extremely small sample sizes. Practical Assessment, Research & Evaluation. 2013:18. [Google Scholar]
- 40.Student. The Probable Error Of A Mean. Biometrika. 1908;6:1–25. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1: Screening sleep period times - weekend sleep period (mean minutes/night of Fri/Sat inclusive) versus midweek (mean minutes/night Mon to Thurs inclusive). White triangles indicate subjects who were randomised to condition pairing 10h/6h only. Straight lines indicate the experimental conditions of 6h or 10h sleep opportunities.
Supplementary Figure S2: Additional polysomnographic sleep parameters and power spectral analysis results between pairs of conditions averaged over 3 experimental nights.
Panels: A- Sleep latency (mins), B-SWS mins, C-NREM proportion (%TST), D-REM proportion (%TST), E-NREM mean delta power by power spectral analysis (μV2), F- NREM relative delta power (% total power).
10h/6h n=8, 10h/10h↓SWS n=6, 6h/10h↓SWS n=5. Error bars are SEM.
* represents significance p<0.05
Supplementary Table S1: Methodology- Detailed Hormonal Assay Information
Supplementary Table S2: Baseline characteristics between study visits