Abstract
Purpose
Providing long-acting reversible contraception (LARC) in the immediate postpartum period is an evidence-based strategy for expanding women’s access to highly effective contraception and for reducing unintended and rapid repeat pregnancy. The purpose of this article is to demonstrate the application of implementation science methodology to study the complexities of rolling-out policies that promote immediate postpartum LARC use across states.
Description
The Immediate Postpartum LARC Learning Community, sponsored by the Association of State and Territorial Health Officials (ASTHO), is made up of multi-disciplinary, multi-agency teams from 13 early-adopting states with Medicaid reimbursement policies promoting immediate postpartum LARC. Partners include federal agencies and maternal and child health organizations. The Learning Community discussed barriers, opportunities, strategies, and promising practices at an in-person meeting. Implementation science theory and methods, including the Consolidated Framework for Implementation Research (CFIR), and a recent compilation of implementation strategies, provide useful tools for studying the complexities of implementing immediate postpartum LARC policies in birthing facilities across early adopting states.
Assessment
To demonstrate the utility of this framework for guiding the expansion of immediate postpartum LARC policies, illustrative examples of barriers and strategies discussed during the in-person ASTHO Learning Community meeting are organized by the five CFIR domains—intervention characteristics, outer setting, inner setting, characteristics of the individuals involved, and process.
Conclusion
States considering adopting policies can learn from ASTHO’s Immediate Postpartum LARC Learning Community. Applying implementation science principles may lead to more effective statewide scale-up of immediate postpartum LARC and other evidence-based strategies to improve women and children’s health.
Keywords: Implementation science, Long-acting reversible contraception, Learning collaborative, Postpartum, Medicaid policy
Purpose
Nationally, 51 % of all U.S. births in 2010 were paid for by public insurance through Medicaid, the Children’s Health Insurance Program and the Indian Health Service. Of the 2 million publicly-funded births, half were unplanned [17]. Long-acting reversible contraceptives (LARC), which include implants and intrauterine devices (IUDs), are evidence-based methods for preventing unintended and rapid repeat pregnancies (i.e., pregnancies within 12–18 months after delivery), given their failure rate of <1 % [20].
While the most common time for receiving LARC after childbirth is during the 4–6 week postpartum visit, offering LARC immediately after delivery provides an additional opportunity for obtaining LARC in a setting that is convenient for women and providers [16, 2]. There are no contraindications to immediate postpartum implant insertion, and recent evidence also supports IUD placement in the first 48 h post-delivery, ideally within 10 min of placental delivery to minimize expulsion rates [1, 7]. A recent study estimated that immediate postpartum IUD placement resulted in 88 fewer unintended pregnancies per 1000 women over 2 years compared with routine IUD placement at the postpartum visit, leading to cost savings of $282,540 per 1000 women [19].
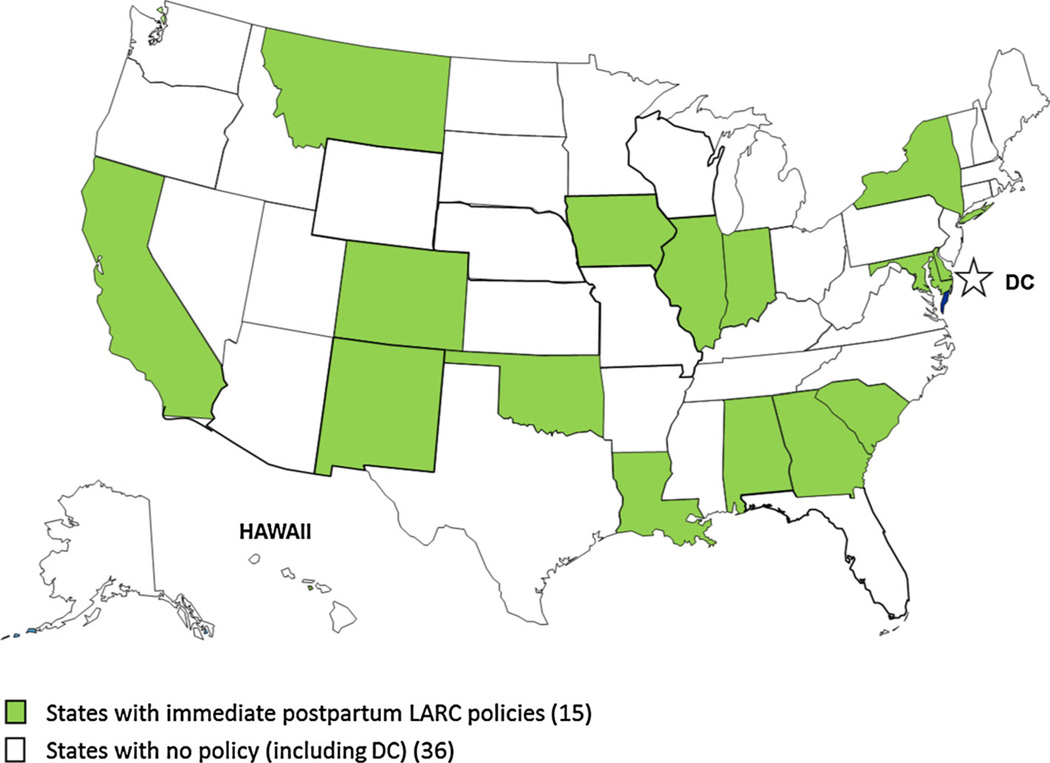
Although providing immediate postpartum LARC has potential for increasing women’s access to effective contraception, barriers have prevented widespread adoption across birthing facilities. The cost of the expensive LARC devices and associated procedures (e.g., LARC insertion and removal) are not fully reimbursed by many payers when placed immediately postpartum [16]. To address this barrier, several state Medicaid agencies have recently changed reimbursement policies for immediate postpartum LARC [3]. While hospitals bill for all labor and delivery costs using a single bundled Diagnosis-Related Group (DRG) code, immediate postpartum LARC policies allow hospitals to be reimbursed for the device, and in some states, the procedure, in addition to the DRG [13]. Currently, 15 states have implemented policies on immediate postpartum LARC with accompanying coding documentation and guidance for billing (Fig. 1) [3, 2].
Fig. 1.
Fifteen states have implemented Medicaid policies for immediate postpartum long-acting reversible contraception with accompanying coding documentation and guidance for billing
The experiences of early adopting states demonstrate that reimbursement policy change alone is insufficient for overcoming access barriers. Several other systems challenges must be addressed to fully integrate immediate postpartum LARC in birthing facilities across states. To address implementation challenges, the Association of State and Territorial Health Officials (ASTHO) convened a multi-state Immediate Postpartum LARC Learning Community, in partnership with multiple federal agencies and maternal and child health organizations. The Learning Community aims to improve state capacity for successfully implementing immediate postpartum LARC policies by supporting cross-state collaboration to overcome barriers and providing technical assistance, as needed [4].
Implementation science is a rapidly-growing field with useful tools for guiding and evaluating the integration of evidence-based interventions with standard practice. Conceptual frameworks for implementation encompass barriers and facilitators across different contexts at multiple levels. Methodologists in the field also have developed a compilation of implementation strategies, defined as “methods or techniques used to enhance the adoption, implementation, and sustainability of a clinical program or practice” [15], that can be applied to enhance implementation across a wide range of evidence-based practices and contexts. The purpose of this article is to illustrate some ways in which implementation science methodology can be applied to the implementation of immediate postpartum LARC policies, using examples from states participating in the ASTHO Immediate Postpartum LARC Learning Community.
Description
ASTHO Immediate Postpartum LARC Learning Community
The ASTHO Immediate Postpartum LARC Learning Community includes multi-disciplinary, multi-agency teams of state health officials, payers, providers, state health department staff, and other stakeholders from 13 states with immediate postpartum LARC reimbursement policies. ASTHO, with support from the Centers for Disease Control and Prevention (CDC), convened an in-person meeting of the Learning Community states in October 2015 to discuss states’ successes, challenges, and technical assistance needs. Over 70 participants attended the meeting, representing Colorado, Delaware, Georgia, Indiana, Iowa, Louisiana, Maryland, Massachusetts, Montana, New Mexico, Oklahoma, South Carolina, and Texas, as well as national partners, including CDC, Centers for Medicare and Medicaid Services, Office of Population Affairs, American Congress of Obstetricians and Gynecologists, National Family Planning and Reproductive Health Association, and Association of Maternal and Child Health Programs. ASTHO staff presented on eight technical assistance domains impacting implementation of immediate postpartum LARC implementation including training, reimbursement, consent, stocking and supply, outreach, measurement and evaluation, stakeholders and partnerships, and service location [12]. Each state team presented its immediate postpartum LARC activities and plans, including successes, barriers, challenges and lessons learned to date, and goals for the next year. Open discussions followed each presentation.
The state teams convened into six topical groups that included patient and provider outreach, Medicaid reimbursement policies and procedures, service location, leadership and systems, and two groups for logistical challenges to implementation to discuss common issues and opportunities for partnerships. Topical group meetings were followed by a facilitated discussion of all participants to synthesize information from all of the groups.
State teams subsequently reconvened to identify steps for increasing immediate postpartum LARC provision in their states and to conduct a strengths, weaknesses, opportunities, threats (SWOT) analysis, to inform later action planning. States were then paired to discuss technical assistance needs, propose ways teams can support each other, and identify promising practices for moving forward. Presentations and discussions from this in-person Learning Community meeting provide the illustrative examples described in the Assessment section below.
Consolidated Framework for Implementation Research
Implementation science is dedicated to understanding how to effectively introduce and integrate evidence-based practices into the standard of care. It involves studying facilitators and barriers that support or diminish the uptake and/or effectiveness of evidence-based practices, and identifying implementation strategies to overcome barriers [6]. Applying conceptual models in implementation science ensures a systematic approach to developing and implementing complex interventions, and enhances the usefulness of findings [18]. The Consolidated Framework for Implementation Research (CFIR) synthesizes the concepts of several available models into five inter-related domains: (1) intervention characteristics, (2) outer setting, (3) inner setting, (4) characteristics of the individuals involved, and (5) process of implementation [9].
The CFIR is well-suited for studying the implementation of immediate postpartum LARC policies, since this is an example of an evidence-based strategy requiring adaptation for different contexts (i.e., inner and outer settings), an important construct in the CFIR. Also important is the role of individuals in influencing implementation efforts, including policy implementers and other stakeholders. The CFIR also describes the often non-linear process of implementation, which has been observed in states implementing immediate postpartum LARC policies.
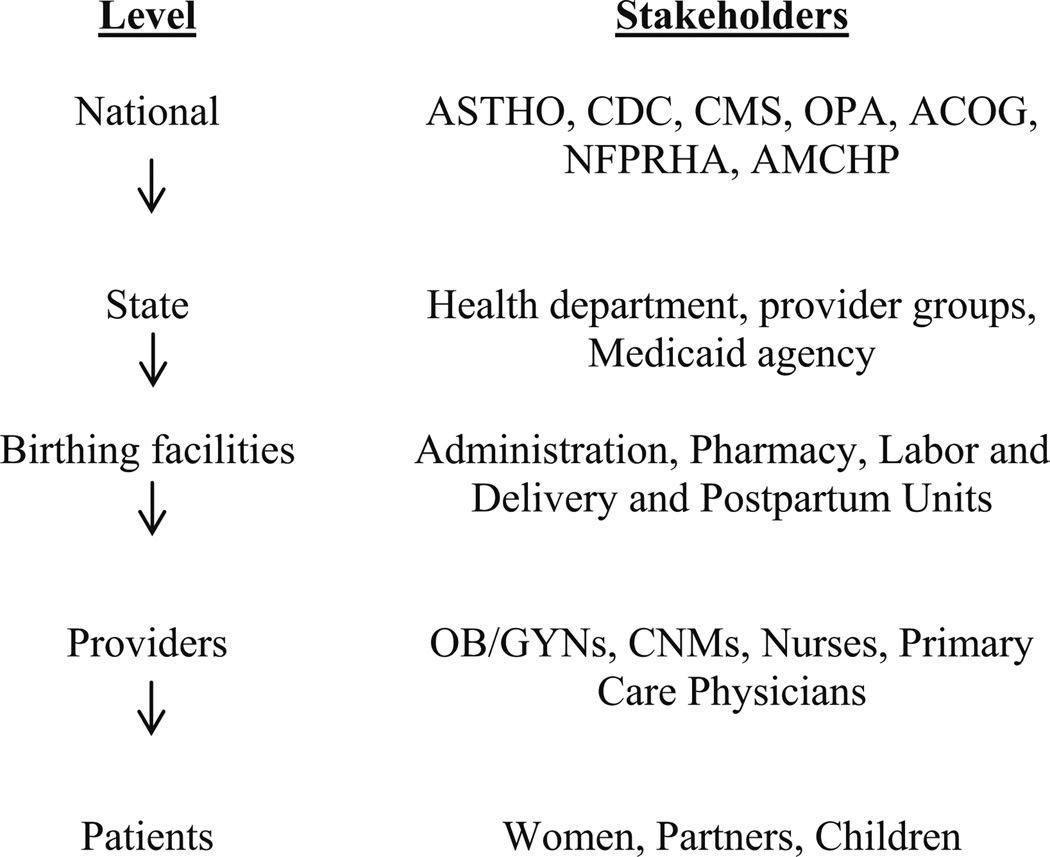
To appreciate the complexity of immediate postpartum LARC policy implementation within the five CFIR domains, one must understand the multi-level structure of implementation efforts and the stakeholders involved at each level, as displayed in Fig. 2. For the purposes of this example, the “inner setting” is the birthing facility because LARC provision occurs at that level.
Fig. 2.
Multilevel framework for immediate postpartum LARC implementation with stakeholders at each level. ASTHO Association of State and Territorial Health Officials, CDC Centers for Disease Control and Prevention, CMS Centers for Medicare and Medicaid Services, OPA Office of Population Affairs, ACOG American Congress of Obstetricians and Gynecologists, NFPHRA National Family Planning and Reproductive Health Association, AMCHP Association of Maternal and Child Health Programs, OB/GYN, obstetricians/gynecologists, CNM Certified Nurse Midwife
Below, we introduce constructs within each CFIR domain and provide illustrative examples of each that are relevant for immediate postpartum LARC implementation, as described by participants at the recent ASTHO Learning Community meeting. Each construct is accompanied by a complementary implementation strategy for immediate postpartum LARC, defined according to a list of strategies recently compiled by a panel of implementation science experts [14]. CFIR constructs and IPP LARC examples are summarized in Table 1.
Table 1.
Summary of illustrative examples of immediate postpartum LARC implementation in domains of the Consolidated Framework for Implementation Research (CFIR) and associated implementation strategies
| CFIR domain | CFIR construct within domain |
Immediate postpartum LARC example | Associated implementation strategy | Implementation strategy label [14] |
|---|---|---|---|---|
| Intervention characteristics |
Evidence strength and quality |
Strong evidence of safety and efficacy of immediate postpartum LARC; provider misperceptions about the impact of expulsion rates and interference with lactation |
Provider outreach and education at provider professional meetings |
Conduct educational meetings |
| Outer setting | External policies and incentives |
State reimbursement strategies differ from typical reimbursement practices |
ASTHO Multi-State Learning Community for immediate postpartum LARC |
Create a learning collaborative |
| Inner setting | Readiness for implementation |
Lack of devices stocked at facilities | Stocking devices in secured, automated medication dispensing system on labor and delivery floor; bed-side tackle boxes stocked and available on postpartum floor |
Change physical structure and equipment |
| Characteristics of individuals |
Personal Attributes of Patients |
Women’s knowledge, preferences, and prior experiences with healthcare and contraception |
Incorporate women’s perspectives about implementation efforts, specifically counseling and consent |
Involve patients/consumers; obtain and use patient/consumer feedback |
| Provider Self- efficacy |
Lack of provider skills to insert immediate postpartum IUDs |
Outreach trainings to perinatal centers with special pelvic models for hands- on training |
Conduct educational outreach visits; make training dynamic |
|
| Process | Planning | Facility-specific protocols for immediate postpartum LARC are needed to support implementation |
Develop toolkits to facilitate implementation in birthing facilities |
Identify and prepare provider champions |
Assessment
CFIR Domain #1: Intervention Characteristics
The intervention is defined as inserting an IUD or implant immediately postpartum, before a woman is discharged from her delivery hospitalization. One CFIR construct in the domain of Intervention Characteristics is “evidence strength and quality” [9]. While the scientific literature describing the safety and efficacy of immediate postpartum LARC [1] is an important part of this construct, stakeholders’ knowledge and perceptions about the quality and validity of that evidence are also important. Learning Community participants described hesitancy among many providers due to concerns that higher expulsion rates of IUDs placed immediately postpartum would lead to increases in unintended pregnancy, or that LARC devices would interfere with lactation [5], neither of which is supported by the evidence [1, 11]. However, these misperceptions influence implementation efforts if they prevent providers from offering their patients LARC in the immediate postpartum period.
One implementation strategy employed by Learning Community states to address provider knowledge gaps and misperceptions is described by Powell et al. [14] as “conducting educational meetings.” In venues such as professional meetings of OB/GYNs, midwives, primary care providers, or other provider groups, trusted peer experts disseminate evidence supporting the safety of placing LARC immediately postpartum, and refuting common misperceptions.
CFIR Domain #2: Outer Setting
The outer setting describes influences external to birthing facilities that affect implementation. One construct within the outer setting is “external policies and incentives” [9]. State reimbursement policies that address ease of billing generate external motivation for birthing facilities to offer LARC in the immediate postpartum period.
Reimbursement policies vary across states, with some state Medicaid agencies reimbursing for LARC devices and procedures through increases to payment for the “bundled” labor and delivery billing code (i.e., DRG code). Other states provide payment for LARC devices and procedures, in addition to the DRG code. Reimbursement for devices and procedures outside the DRG code is uncommon for state Medicaid agencies, and therefore can be complex to implement for providers and coders at the facility level, as well as for claims-system programmers at the state level [5]. As a result, several states experienced barriers to reimbursing providers, often stemming from automated claims systems rejecting payments for LARC placement during the same inpatient stay as the DRG code for labor and delivery.
The ASTHO Immediate Postpartum LARC Learning Community itself is an implementation strategy initiated at the national level, facilitating information sharing within each state (e.g., between the health department and Medicaid agency) and across states to address barriers and develop promising solutions regarding reimbursement and payment processes. Termed “create a learning collaborative” by Powell et al. [14], this strategy fosters a collaborative learning environment supportive of implementation in varied state settings.
CFIR Domain #3: Inner Setting
Birthing facility “readiness for implementation” is an important descriptor of the Inner Setting domain. Readiness includes indicators of commitment to adopting interventions such as leadership engagement, available resources, and access to information and knowledge [9]. One facet of available resources for birthing facilities is the ability to stock and supply LARC devices. This requires commitment from hospital administrators and pharmacy directors to pre-pay for devices with the assurance of later reimbursement (i.e., “buy and bill”), or developing alternate financial strategies for supplying devices. Devices must then be readily available and conveniently located in facilities for providers to place them at the appropriate time during the immediate postpartum period. This is especially challenging for IUDs, which are optimally placed in the first 10 min post-placental delivery [1].
Powell et al. [14] suggest a strategy called “change physical structure and equipment” to remove barriers by adapting physical configurations that most effectively support the intervention. Some facilities located in Learning Community states employ this strategy by stocking IUDs in a secured, automated medication dispensing system on the labor and delivery floor for providers to easily access when needed. Other facilities construct ‘tackle boxes’ filled with supplies necessary for implant placement at the bedside. Staff members in the unit are assigned to ensure that tackle boxes are stocked and ready for implant placement. These strategies provide increased opportunity for inserting LARC immediately postpartum.
CFIR Construct #4: Characteristics of Individuals
Implementation efforts generally involve numerous individuals, from the advocates and change agents at the national level to the patients who are ultimately impacted by the evidence-based intervention. With respect to immediate postpartum LARC, a woman’s knowledge, preferences, prior experiences with the healthcare delivery system, and contraceptive history, among other factors, may influence her decisions about contraception in the immediate postpartum period. Strategies such as “involve patients/consumers” and “obtain and use patients/consumers feedback” [14], especially with respect to preferred timing and location of counseling and consent, place value on women’s perspectives about immediate postpartum LARC and associated implementation efforts.
Providers also greatly influence implementation of immediate postpartum LARC through their direct role in contraceptive counseling and delivering the intervention. One of the individual characteristics described by Damschroder et al. [9] is “self-efficacy,” which is defined as a belief in one’s capabilities to perform actions within a specific context to meet implementation goals. Provider self-efficacy in inserting LARC in general, and specifically in placing IUDs immediately postpartum when the uterus is much larger than normal, is an important factor influencing immediate postpartum LARC implementation. Learning Community teams cite a lack of delivery providers in their states who have these skills as a barrier to moving forward with implementation.
“Conduct educational outreach visits” [14], “make training dynamic,” and “provide ongoing consultation” are complementary implementation strategies being used to build provider skills and, subsequently, self-efficacy. In one Learning Community state, a Care Management Organization (CMO) funds the OB/GYN Society to conduct trainings at regional perinatal centers. These trainings are delivered by a provider champion and a CMO representative who jointly present the evidence for immediate postpartum LARC and answer billing questions for providers. Trainings are dynamic because providers practice IUD insertions using a pelvic model specially designed to mimic a postpartum uterus, allowing them to build self-efficacy, and consultation with the provider champion is available beyond the visit to reinforce skills.
CFIR Construct #5: Process
The final CFIR domain focuses on process, and includes planning, engaging, executing, reflecting and evaluating [9]. Developing a toolkit is an example of planning for implementation across birthing facilities. Learning Community state teams have been developing toolkits that include training materials for providers, answers to frequently asked questions about billing, informational handouts for patients, and other implementation resources [10]. Facility staff may then use the toolkit as guide for developing a facility-level protocol that is adapted to match the context of their facility.
To effectively disseminate toolkits in facilities and encourage adoption and adaptation, provider champions at each facility are needed to advance implementation effort progress. Powell et al. [14] highlight “identifying and preparing champions” as a strategy for overcoming internal resistance to change across CFIR domains.
Conclusion
Implementation science methodology, specifically the CFIR and implementation strategy compilations, can be successfully applied to guide and evaluate immediate postpartum LARC policy implementation in state Medicaid programs. Information exchange within the ASTHO Learning Community has led to the adoption of best practices and identification of successful strategies for overcoming barriers related to billing and cost-reimbursement, stocking and supply, physician training, and patient education. Since Medicaid covers approximately 50 % of U.S. deliveries [8] and Medicaid policies are often later adopted by private insurance plans, successful implementation of this policy has the potential to increase access to immediate postpartum LARC for all women who desire it. Continued application of implementation science principles to this implementation process may lead to more effective implementation in Learning Community states, and may inform future efforts in other states and among private insurers. Furthermore, implementation science and the multi-agency clinical and public health partnerships fostered through the Learning Community could be applied more broadly to the implementation of other evidence-based practices to improve health services and outcomes for women, infants, and children.
Significance.
What is already known on this subject?
Immediate postpartum long-acting reversible contraception (LARC) insertion is an evidence-based approach for increasing access to highly effective contraception for women before they leave the hospital after delivery. However, barriers have prevented widespread adoption across birthing facilities.
What this study adds?
Implementation science provides useful tools for guiding the implementation of immediate postpartum LARC Medicaid policies in states.
Acknowledgments
The authors would like to acknowledge and thank the state teams in the ASTHO Immediate Postpartum LARC Learning Community for their contributions at the meeting. The authors would also like to thank ASTHO’s Chief Program Officer of Community Health and Prevention Lisa Waddell, MD, MPH for her continued leadership and Lekisha Daniel-Robinson, CMCS, CMS, for representing her agency and providing technical assistance to state teams. Dr. Loretta Gavin of OPA and Dr. Melissa Kottke of Emory University and the Jane Fonda Center for Adolescent Reproductive Health reviewed and commented on this manuscript, for which the authors are grateful. Finally, the authors would like to recognize all of the national partners who have contributed to these efforts: CMCS, CMS, OPA, ACOG, AMCHP, and NFPRHA.
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the Association of State and Territorial Health Officials.
References
- 1.American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstetrics and Gynecology. 2011;118(1):184–196. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 2.American Congress of Obstetricians and Gynecologists. Long acting reversible contraception program. 2015 Retrieved from http://www.acog.org/About-ACOG/ACOG-Departments/Long-Acting-Reversible-Contraception. [Google Scholar]
- 3.ASTHO. Long-acting reversible contraception (LARC) Medicaid Policies, Codes, and Guidance. 2015a Retrieved from http://www.astho.org/Programs/Maternal-and-Child-Health/Long-Acting-Reversible-Contraception-LARC/Medicaid-Policies/ [Google Scholar]
- 4.ASTHO. Maternal and child health: Long-acting reversible contraception. 2015b Retrieved from http://www.astho.org/Programs/Maternal-and-Child-Health/Long-Acting-Reversible-Contraception-LARC/ [Google Scholar]
- 5.ASTHO Immediate Postpartum LARC Learning Community. Year 2 Kick-Off Meeting. VA: Arlington; 2015. [Google Scholar]
- 6.Brownson RC, Colditz GA, Proctor EK. Dissemination and implementation research in health: Translating science to practice. Oxford, New York: Oxford University Press; 2012. [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) U.S. medical eligibility criteria for contraceptive use, 2010. MMWR, Recommendations and reports. 2010:1–6. June 18, 2010/59(RR04), Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5904a1.htm?s_cid=rr5904a1_e. [PubMed]
- 8.Curtin SC, Osterman MJ, Uddin SF, Sutton SR, Reed PR. Source of payment for the delivery: Births in a 33-state and district of columbia reporting area, 2010. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2013;62(5):1–20. [PubMed] [Google Scholar]
- 9.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heberlein E, Billings DL, Mattison-Faye A, Giese BZ. The South Carolina Postpartum LARC Toolkit. Choose Well Initiative and the South Carolina Birth Outcomes Initiative. 2015 Retrieved from http://www.choosewellsc.org/SC_Postpartum_LARC_Toolkit.pdf. [Google Scholar]
- 11.Kapp N, Curtis KM. Intrauterine device insertion during the postpartum period: A systematic review. Contraception. 2009;80(4):327–336. doi: 10.1016/j.contraception.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 12.Kroelinger CD, Waddell LF, Goodman DA, Pliska E, Rudolph C, Ahmed E, Addison D. Working with state health departments on emerging issues in maternal and child health: Immediate postpartum long-acting reversible contraceptives. Journal of Women’s Health. 2015;24(9):693–701. doi: 10.1089/jwh.2015.5401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moniz MH, Dalton VK, Davis MM, Forman J, Iott B, Landgraf J, Chang T. Characterization of Medicaid policy for immediate postpartum contraception. Contraception. 2015;92(6):523–531. doi: 10.1016/j.contraception.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 14.Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, Kirchner JE. A refined compilation of implementation strategies: Results from the expert recommendations for implementing change (ERIC) project. Implementation Science. 2015 doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Proctor EK, Powell BJ, McMillen JC. Implementation strategies: Recommendations for specifying and reporting. Implementation Science. 2013 doi: 10.1186/1748-5908-8-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodriguez MI, Evans M, Espey E. Advocating for immediate postpartum LARC: Increasing access, improving outcomes, and decreasing cost. Contraception. 2014;90(5):468–471. doi: 10.1016/j.contraception.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 17.Sonfield A, Kost K. Public costs from unintended pregnancies and the role of public insurance programs in paying for pregnancy-related care: National and state estimates for 2010. New York: Guttmacher Institute; 2015. 2015. Retrieved from http://www.guttmacher.org/pubs/public-costs-of-UP-2010.pdf. [Google Scholar]
- 18.Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: Models for dissemination and implementation research. American Journal of Preventive Medicine. 2012;43(3):337–350. doi: 10.1016/j.amepre.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Washington CI, Jamshidi R, Thung SF, Nayeri UA, Caughey AB, Werner EF. Timing of postpartum intrauterine device placement: A cost-effectiveness analysis. Fertility and Sterility. 2015;103(1):131–137. doi: 10.1016/j.fertnstert.2014.09.032. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization Department of Reproductive Health and Research and Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs, Knowledge for Health Project. Family planning: A global handbook for providers (2011 update) Baltimore and Geneva: CCP and WHO; 2011. [Google Scholar]