Abstract
We estimated overweight and obesity (OWOB) prevalence of children in US-Affiliated Pacific jurisdictions (USAP) of the Children's Healthy Living Program compared with the contiguous United States.
We searched peer-reviewed literature and government reports (January 2001–April 2014) for OWOB prevalence of children aged 2 to 8 years in the USAP and found 24 sources. We used 3 articles from National Health and Nutrition Examination Surveys for comparison. Mixed models regressed OWOB prevalence on an age polynomial to compare trends (n = 246 data points).
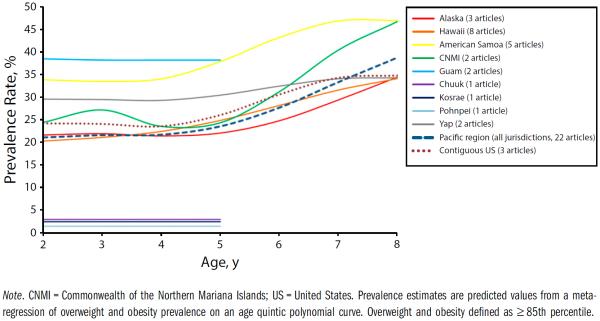
In the USAP, OWOB prevalence estimates increased with age, from 21% at age 2 years to 39% at age 8 years, increasing markedly at age 5 years; the proportion obese increased from 10% at age 2 years to 23% at age 8 years. The highest prevalence was in American Samoa and Guam.
THERE ARE FEW DATA ON overweight and obesity (OWOB) of children in the US-Affiliated Pacific Islands, Hawaii, and Alaska, collectively referred to as the US-Affiliated Pacific region (USAP) in this article (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). The USAP has not been included in the National Health and Nutrition Examination Survey (NHANES) or other national surveillance systems with measured anthropometric data.1,2 Native ethnic populations (Native Hawaiians, Pacific Islanders, Alaska Natives) of the USAP have not been reported on in national surveillance,3 yet Native Hawaiians and other Pacific Islanders constitute 1.2 million people (0.4% of the total US population) and have increased 40% in the past decade,4 and Native Alaskans constitute another quarter million people.5 The USAP has political ties to the United States (Table A, available as a supplement to the online version of this article at http://www.ajph.org).4
The high prevalence of obesity and noncommunicable diseases in USAP adult populations6 and consequent state of emergency declared7 underpins the urgency of obesity prevention, starting with children. The mean OWOB prevalence for children aged 5 to 8 years in Hawaii was 33% (13% overweight and 20% obese) and the risk for OWOB varied by ethnicity, from 2-fold in Asians to 17-fold in Samoans, compared with Whites.8,9 Data from the Commonwealth of the Northern Mariana Islands (CNMI) showed similar OWOB prevalence.10
Aggregating prevalence estimates for the region and by jurisdiction will allow programs to target their activities and policies. The purpose of this article is to (1) estimate prevalence of OWOB of children aged 2 to 8 years living in the USAP and (2) determine how that prevalence compares with children aged 2 to 8 years living in the 48 contiguous states.
METHODS
Investigators from the Children's Healthy Living for the Remote Underserved Minority Populations of the Pacific Program searched peer-reviewed literature and publicly available agency data for OWOB prevalence rates in the USAP relative to the Centers for Disease Control and Prevention (CDC) body mass index (BMI; defined as weight in kilograms divided by the square of height in meters) reference, as is reported by NHANES and has been used in past reports for the USAP.9,11,12
Study Selection
Peer-reviewed literature
For our primary data sources, we searched electronic databases (PubMed, US National Library of Medicine; EBSCO Publishing; and Web of Science) for articles published between January 2001 and April 2014 with the following search terms: child, obesity, overweight, Pacific, Alaska, Samoa, Micronesia, Hawaii, Marshall Islands, Mariana, Palau, Guam. We found 323 articles; 223 were unique and we reviewed these for other inclusion criteria.
Publicly available government agency data
For our secondary data sources, we located other reports on OWOB from the USAP by Internet search engine (Google) with the same search terms. We further limited search hits in excess of 1 million to government agencies that focused on the 2- to 8-year-old age group (e.g., Head Start, Department of Education, Department of Health and Human Services, Special Supplemental Feeding Program for Women, Infants, and Children [WIC]). In addition, we contacted child obesity experts in the Pacific region for the relevant government agency reports. We found 14 reports and reviewed these for other inclusion criteria.
The other inclusion criteria included (1) English language, the main language used for business in the region; (2) children aged 2 to 8 years were included in the report; and (3) OWOB prevalence (%) in the USAP defined with CDC body mass index criteria13–15 (≥ 85th percentile and < 95th percentile for age and sex was labeled “overweight”; ≥ 95th percentile was labeled “obese”16).
Data Extraction and Synthesis
One experienced reviewer (M. K. F.)17 independently identified eligible data sets and recorded study year, authors, publication year, location, racial/ethnic group(s), ages, sample size, OWOB prevalence, and notes on OWOB criteria (list of eligible data sets available on request). A second reviewer (F. L.) confirmed the data.
We identified 11 primary and 14 secondary data sources from 2001 to 2014 from Alaska, American Samoa, CNMI, Federated States of Micronesia (FSM; Yap, Kosrae, Pohnpei, and Chuuk), Guam, and Hawaii (Table 1). Because 2 primary data sources18,19 reported on the same data set, we dropped 1, yielding 10. We found no data sources for the Marshall Islands or Palau. We used data from NHANES from 2009 to 2010, 2007 to 2008, and 2003 to 200611,37,38 as a reference data set from the 48 contiguous states.
TABLE 1.
Sources of Overweight, Obesity, or Both With Prevalence (%) Data Used in the Meta-analysis for the US-Affiliated Pacific Region and the 48 Contiguous United States, in Literature Published January 2001–April 2014
| Author | Region | Age, y | Sexa | No. of children | Racial/Ethnic Group(s) | Study Source and Cohort (Year of Data Collection) | Sampling Frame | Ref. Cutoff, CDC Criteriab | Age Group, % |
|---|---|---|---|---|---|---|---|---|---|
| Peer-reviewed literature (n = 10c) | |||||||||
| Bruss et al.10 | CNMI | 8–9 | Both sexes | 407 | Pacific Islander (Chamorro, Carolinian, Micronesian), Asian | Project Familia Giya Marianas—Children from 12 public schools in the CNMI (2005) | Caregivers from 12 public schools were invited to participate | ≥ 85th percentile | 47 |
| ≥ 95th percentile | 32 | ||||||||
| Paulino et al.18 | CNMI | 1–10 | Both sexes | 393 | Pacific Islander (Chamorro, Carolinian), mixed or other, Asian | Children randomly selected from 16 villages on Rota, Saipan, and Tinian (2005) | Random cluster survey sampling proportionate to 2000 US Census population estimate | ≥ 85th percentile | 2–3 y = 25 |
| 4–6 y = 26 | |||||||||
| 7–10 y = 45 | |||||||||
| 85th–94th percentile | 2–3 y = 12 | ||||||||
| 2–3 y = 83 | 4–6 y = 13 | ||||||||
| 4–6 y = 127 | 7–10 y = 18 | ||||||||
| 7–10 y = 136 | ≥ 95th percentile | 2–3 y = 13 | |||||||
| 2–10 y = 346 | 4–6 y = 13 | ||||||||
| 7–10 y = 27 | |||||||||
| ≥ 85th percentile | 34 | ||||||||
| 85th–94th percentile | 15 | ||||||||
| ≥ 95th percentile | 19 | ||||||||
| Novotny et al.19 | Hawaii | 2–10 | Both sexes | 554 | Native Hawaiian, Pacific Islander, Asian, White, other | Children who accessed one of the health maintenance organization's (Kaiser Permanente's) 10 Oahu clinics for a physical examination (2003) | Stratified random sample | 85th–94th percentile | 13 (all) |
| 15 males, 10 females | |||||||||
| 2–3 y = 10 | |||||||||
| 4–5 y = 14 | |||||||||
| 6–10 y = 13 | |||||||||
| Native Hawaiian = 11 | |||||||||
| Pacific Islander = 18 | |||||||||
| Filipino = 11 | |||||||||
| ≥ 95th percentile | 19 (all) | ||||||||
| 22 males, 15 females | |||||||||
| 2–3 y = 7 | |||||||||
| 4–5 y = 20 | |||||||||
| 6–10 y = 29 | |||||||||
| Native Hawaiian = 19 | |||||||||
| Pacific Islander = 40 | |||||||||
| Filipino = 19 | |||||||||
| Baruffi et al.8 | Hawaii | 2–4 | Both sexes | 12 709 | Asian, Black, White, Filipino, Native Hawaiian, Hispanic, Samoan, other | WIC (1997–1998) | Data with complete date, age, sex, weight, and height information | ≥ 95th percentile | 2–4 y = 11.4 |
| Native Hawaiian = 11.3 | |||||||||
| Samoan = 27 | |||||||||
| Filipino = 12.4 | |||||||||
| Pobutsky et al.20 | Hawaii | 4–6 | Both sexes | 10 199 | Multiple racial/ethnic groups (children who entered kindergarten in the Hawaii public school system) | Public elementary schools (2002–2003) | All student health records with complete age, sex, weight, and height information and plausible anthropometric values | ≥ 85th percentile | 28.5 |
| 85th–94th percentile | 14.1 | ||||||||
| ≥ 95th percentile | 14.4 | ||||||||
| Novotny et al.9 | Hawaii | 5–8 | Both sexes | 4608 (with ethnic information) | White, Asian, Filipino, Native Hawaiian, Native Hawaiian-Asian, Samoan, other mixed, other | Health maintenance organization (Kaiser Permanente; 2010) | Cross-sectional study design of electronic medical record data with complete weight and height information | ≥ 85th percentile | 32.6 (with ethnic information) |
| 29.4 (with and without ethnic information) | |||||||||
| 85th–94th percentile | 12.9 (with ethnic information) | ||||||||
| ≥ 95th percentile | 19.7 (with ethnic information) | ||||||||
| Chai et al.21 | Hawaii | 6–17 | Males only and females only | 1437 | Native Hawaiian, Asian, Filipino, Portuguese, White, other | Public school students in a Hawaii district with a higher population of residents of Native Hawaiian ancestry (1992–1996) | Five years of semilongitudinal data from a cohort of students in grades 1–12 | ≥ 95th percentile | males = Native Hawaiian (6–11 y), 29.3 |
| females = Native Hawaiian (6–11 y), 23.7 | |||||||||
| both = Native Hawaiian (6–11 y), 26.5 | |||||||||
| males = non-Native Hawaiian (6–11 y), 25.1 | |||||||||
| females = non-Native Hawaiian (6–11 y), 16.3 | |||||||||
| both = non-Native Hawaiian (6–11 y), 20.7 | |||||||||
| Okihiro et al.22 | Hawaii | 4–5 | Both sexes | 389 | Native Hawaiian, Samoan, Filipino | Children from 2 rural and impoverished communities who utilized Hawaii's largest federally qualified CHC | Retrospective study of children: (1) Native Hawaiian, Samoan or Filipino; (2) lived in the CHC zip code; (3) born during 1 of 4 periods: 1981–1983, 1986–1988, 1991–1993, and 1996–1998; (4) attended the CHC for their well-child care; and (5) had a prekindergarten physical examination at the CHC | ≥ 95th percentile | 22.7 |
| 85th–94th percentile | 20.1 | ||||||||
| ≥ 85th percentile | 42.8 | ||||||||
| Manea23 | Hawaii | 4–5 | Both sexes | 586 | Unspecified | Kauai public elementary school 1st graders (2003) | Student health records of all Kauai children enrolled in the first grade during the period from August to December | ≥ 85th percentile | 4 y = 41.6 males, 27.9 females |
| 5 y = 38.8 males, 37.3 females | |||||||||
| 4 y = 316 (144 males, 172 females) | 4–5 y = 36 | ||||||||
| 85th–94th percentile | 4 y = 19.4 males, 8.7 females | ||||||||
| 5 y = 15.9 males, 15.1 females | |||||||||
| 5 y = 270 (144 males, 126 females) | 4–5 y = 14.5 | ||||||||
| ≥ 95th percentile | 4 y = 22.2 males, 19.2 females | ||||||||
| 5 y = 22.9 males, 22.2 females | |||||||||
| 4–5 y = 21.5 | |||||||||
| Ichiho et al.24 | Federated States of Micronesia, Yap | 2–14 | Both sexes | 1948 | Unspecified | Yap State Cancer Prevention and Control Program—Outer Island Household Survey (2008–2009) | Household survey | 85th–94th percentile | 15.6 |
| ≥ 85th percentile | 33.8 | ||||||||
| ≥ 95th percentile | 18.2 | ||||||||
| Agency literature (n = 14) | |||||||||
| Boles et al.25 | Alaska | 3–19 | Both sexes | 5902 | White, Alaska Native/American Indian, Asian, Black/African American, Pacific Islander/Native Hawaiian, Hispanic/Latino, mixed | Kenai Peninsula Borough school district (2011) | All student records with valid height and weight measures from the electronic student information system | ≥ 85th percentile | 3–6 y = 32.9 |
| 7–10 y = 34.2 | |||||||||
| 85th–94th percentile | 3–6 y = 19.7 | ||||||||
| 7–10 y = 17.8 | |||||||||
| ≥ 95th percentile | 3–6 y = 13.1 | ||||||||
| 7–10 y = 16.4 | |||||||||
| Alaska Special Supplemental Nutrition Program for Women, Infants, and Children26 | Alaska | 2–5 | Both sexes | 16 525 (2012) | Unspecified | Alaska WIC (2005–2012) | Data with complete age, sex, weight, and height information | ≥ 85th percentile | 22 (2012) |
| 16 192 (2011) | 21.42 (2011) | ||||||||
| 17 273 (2010) | 21.52 (2010) | ||||||||
| 16 462 (2009) | 21.69 (2009) | ||||||||
| 15 662 (2008) | 21.54 (2008) | ||||||||
| 15 579 (2007) | 21.60 (2007) | ||||||||
| 15 667 (2006) | 21.7 (2006) | ||||||||
| 17 128 (2005) | 22.1 (2005) | ||||||||
| Eberling27 | Alaska | 5–8 | Males only, females only, and both sexes | 650 (334 males, 316 females) | White, American Indian/Alaska Native, Black/African American, Hispanic/Latino, Asian, Native Hawaiian/ Pacific Islander, mixed, unknown | Representative sample of kindergarten students at selected elementary schools (2010–2011) | A consent form and questionnaire was sent home to parents and guardians | ≥ 85th percentile | 35 both, 37 males, 32 females |
| 85th–94th percentile | 19 both, 20 males, 17 females | ||||||||
| ≥ 95th percentile | 16 both, 17 males, 15 females | ||||||||
| Vargo28 | American Samoa | 4–20 | Males only and females only | 5390 | Unspecified | A sample of public and private school children attending grades K, 3, 6, 9, and 12 (2006–2007) | School-based measurement | ≥ 85th percentile | males = 46 (kindergarten) |
| K–5: 1015 (524 males, 491 females) | males = 46 (3rd grade) | ||||||||
| females = 42 (kindergarten) | |||||||||
| females = 45 (3rd grade) | |||||||||
| 3rd grade: 1189 (615 males, 574 females) | 85th–94th percentile | males = 21.4 (kindergarten) | |||||||
| males = 17.4 (3rd grade) | |||||||||
| females = 21.4 (kindergarten) | |||||||||
| females = 17.8 (3rd grade) | |||||||||
| ≥ 95th percentile | males = 25.4 (kindergarten) | ||||||||
| males = 29.4 (3rd grade) | |||||||||
| females = 20.8 (kindergarten) | |||||||||
| females = 27.4 (3rd grade) | |||||||||
| Vargo29 | American Samoa | 5–18 | Males only and females only | 4214 | Unspecified | Students in grades K through 12 at public and private schools (2007–2008) | School-based measurement | ≥ 85th percentile | 5 y = 36.05 males, 41.4 females |
| 5 y = 213 (114 males, 99 females) | 6 y = 38.4 males, 34.9 females | ||||||||
| 7 y = 51.1 males, 47.6 females | |||||||||
| 8 y = 50 males, 39 females | |||||||||
| 6 y = 264 (138 males, 126 females) | 9 y = 42 males, 51.4 females | ||||||||
| 10 y = 54.2 males, 54.7 females | |||||||||
| 85th–94th percentile | 5y = 21.1 males, 18.2 females | ||||||||
| 7 y = 263 (135 males, 128 females) | 6 y = 18.1 males, 22.2 females | ||||||||
| 7 y = 18.5 males, 14.8 females | |||||||||
| 8 y = 19.1 males, 15.8 females | |||||||||
| 8 y = 256 (136 males, 120 females) | 9 y = 16.2 males, 15.5 females | ||||||||
| 10 y = 16.1 males, 25.0 females | |||||||||
| ≥ 95th percentile | 34.4 males, 36.3 females | ||||||||
| 9 y = 284 (142 males, 142 females) | 5 y = 14.9 males, 23.2 females | ||||||||
| 6 y = 20.3 males, 12.7 females | |||||||||
| 7 y = 32.6 males, 32.8 females | |||||||||
| 10 y = 246 (118 males, 128 females) | 8 y = 30.9 males, 23.4 females | ||||||||
| 9 y = 26.1 males, 35.9 females | |||||||||
| 10 y = 38.1 males, 29.7 females | |||||||||
| Vargo30 | American Samoa | 2–20 | Males only and females only | 3478 | Unspecified | Students in grades 2, 5, and 8 from each of the 23 public elementary schools and juniors from each of the 6 public high schools (2008–2009) | School-based measurement | ≥ 85th percentile | 20 males, 23.5 females |
| 6–11 y = 47.7 males, 46.8 females (2008–2009) | |||||||||
| 48.5 males, 47.4 females (2007–2008) | |||||||||
| 52.4 males, 50.1 females (2006–2007) | |||||||||
| ≥ 95th percentile | 33.6 males, 34.3 females | ||||||||
| 6–11 y = 29.2 males, 25.1 females (2008–2009) | |||||||||
| 30.2 males, 27.8 females (2007–2008) | |||||||||
| 33.5 males, 31.3 females (2006–2007) | |||||||||
| American Samoa Maternal and Child Health Program31 | American Samoa | 2–5 | Both sexes | 4225 | Unspecified | American Samoa WIC (2009) | Data with complete date, age, sex, weight, and height information | ≥ 85th percentile | 33.7 |
| 85th–94th percentile | 19.1 | ||||||||
| ≥ 95th percentile | 14.6 | ||||||||
| American Samoa Maternal and Child Health Program31 | American Samoa | 2–4 | Both sexes | 576 | Unspecified | Tafuna Health Center and Leone Health Center (2010) | Data with complete date, age, sex, weight, and height information | ≥ 85th percentile | 35.1 |
| 85th–94th percentile | 19.1 | ||||||||
| ≥ 95th percentile | 16 | ||||||||
| Federated States of Micronesia Maternal and Child Health Program32 | Federated States of Micronesia | 2–5 | Both sexes | 800 (Chk) | Unspecified | Maternal and Child Health data collection in Chuuk, Kosrae, Pohnpei, and Yap (2010) | School-based measurement | ≥ 85th percentile | 3 (Chuuk) |
| 812 (Kos) | 2.5 (Kosrae) | ||||||||
| 580 (Poh) | 1.5 (Pohnpei) | ||||||||
| 205 (Yap) | 14 (Yap) | ||||||||
| Department of Education33 | Guam | 3–5 | Both sexes | 576 | Unspecified | Guam Headstart Program (2011–2012) | School-based measurement | 85th–94th percentile | 13 |
| ≥ 95th percentile | 14.2 | ||||||||
| Department of Public Health and Social Services34 | Guam | 2–5 | Both sexes | 4410 | Unspecified | WICd (2006–2009) | Data with complete date, age, sex, weight, and height information | ≥ 85th percentile | 52.7 (2009) |
| 4029 | 34.9 (2008) | ||||||||
| 2653 | 26.8 (2007) | ||||||||
| 3369 | 31.8 (2006) | ||||||||
| Hawaii Special Supplemental Nutrition Program for Women, Infants, and Children35 | Hawaii | 2–5 | Both sexes | 1766 (2010) | Unspecified | Hilo WICd (2008–2010) | Data with complete date, age, sex, weight, and height information | 85th–94th percentile | 15.7 (2010) |
| 1748 (2009) | 14.9 (2009) | ||||||||
| 1531 (2008) | 15.7 (2008) | ||||||||
| ≥ 95th percentile | 10.6 (2010) | ||||||||
| 11.6 (2009) | |||||||||
| 10.3 (2008) | |||||||||
| Hawaii Special Supplemental Nutrition Program for Women, Infants, and Children35 | Hawaii | 2–5 | Both sexes | 731 (2010) | Unspecified | Kona WICd (2008–2010) | Data with complete date, age, sex, weight, and height information | 85th–95th percentile | 13.3 (2010) |
| 650 (2009) | 13.8 (2009) | ||||||||
| 650 (2008) | 15.5 (2008) | ||||||||
| ≥ 95th percentile | 10.8 (2010) | ||||||||
| 8.5 (2009) | |||||||||
| 8.8 (2008) | |||||||||
| Centers for Disease Control and Prevention36 | Hawaii | 2–5 | Both sexes | 17 879 | Unspecified | Pediatric Nutrition Surveillance System data (2011) | WIC data with complete date, age, sex, weight, and height information | ≥ 85th percentile | 21.5 |
| 85th–94th percentile | 12.3 | ||||||||
| ≥ 95th percentile | 9.2 | ||||||||
| Reference data (n = 3) | |||||||||
| Ogden et al.11 | Contiguous US | 0–19 | Both sexes | 4111 | White, Hispanic, Black, Mexican American | NHANES 2009–2010 | Cross-sectional analyses of all children and adolescents with measured heights and weights from NHANES | ≥ 85th percentile | 2–5 y = 26.7 |
| 0 to < 2 y = 703; | 6–11 y = 32.6 | ||||||||
| 2–5 y = 903; | ≥ 95th percentile | 2–5 y = 12.1 | |||||||
| 6–11 y = 1213; | 6–11 y = 18.0 | ||||||||
| 12–19 y = 1292 | |||||||||
| Ogden et al.37 | Contiguous US | 0–19 | Both sexes | 4000 | White, Hispanic, Black, Mexican American (beginning in 2007, all Hispanics were oversampled while allowing for a sufficient no. of Mexican Americans) | NHANES 2007–2008 | Cross-sectional analyses of all children and adolescents with measured heights and weights from NHANES | ≥ 85th percentile | 2–5 y = 21.2 |
| 0 to < 2 y = 719 | 6–11 y = 35.5 | ||||||||
| 2–5 y = 885 | ≥ 95th percentile | 2–5 y = 10.4 | |||||||
| 6–11 y = 1197 | 6–11 y = 19.6 | ||||||||
| 12–19 y = 1199 | |||||||||
| Ogden et al.38 | Contiguous US | 2–19 | Both sexes | 8165 | White, Black, Mexican American, and other (in 2005–2006 survey, Mexican Americans were oversampled) | NHANES 2003–2006 | Cross-sectional analyses of all children and adolescents with measured heights and weights from NHANES | ≥ 85th percentile | 2–5 y = 24.4 |
| 2–5 y = 1770 | 6–11 y = 33.3 | ||||||||
| 6–11 y = 2095 | ≥ 95th percentile | 2–5 y = 12.4 | |||||||
| 12–19 y = 4300 | 6–11 y = 17.0 |
Note. CDC = Centers for Disease Control and Prevention; CHC = community health center; Chk = Chuuk; CNMI = Commonwealth of the Northern Mariana Islands; K = kindergarten; Kos = Kosrae; Poh = Pohnpei; NHANES = National Health and Nutrition Examination Survey; US = United States; WIC = Supplemental Nutrition Program for Women, Infants, and Children.
Males only, females only, or both sexes combined.
85th–95th percentile defined as overweight (previously defined as at risk for overweight), ≥ 95 percentile defined as obese (previously defined as overweight).13
Analytic Methods
We used regression to estimate OWOB prevalence for each single age by jurisdiction (USAP state or territory or contiguous United States). The prevalence estimates in the 24 USAP sources and 3 NHANES sources were given for age groups, rather than for single ages. For the regression to provide a smooth curve of estimates across all ages from 2 to 8 years, we needed estimates for single ages. The estimate for the age group is the best estimate available for any particular single age; for instance, if the prevalence was 10% for children aged 2 to 4 years, the best estimate of the probability of obesity for a 2-year-old child is 10%. Therefore, a record was created for each single age in the age group with the age group–specific prevalence and an equal proportion of the sample size (e.g., a prevalence estimate for the age group aged 2 to 4 years would lead to 3 records). One investigator (L. R. W.) entered data into a spreadsheet and a separate investigator (F. L.) reviewed the data. We performed an inverse variance–weighted, fixed-effect meta-regression39 to produce curves for OWOB prevalence by single ages. A mixed model regressed the OWOB prevalence on a polynomial of age (years) accounting for the variance of the prevalence estimates,40 with polynomials up to the fifth power. As the power functions were correlated, we used orthogonal polynomials41 to determine the significance of each independent power component (linear, squared, cubic, etc.) and the maximum degree needed to fit the curve. We also performed random models and the results were similar to the fixed-effect model results; however, the random effects models were not as stable, so only the fixed-effects models are presented.
In addition to the inverse variance weighting that accounted for precision of the individual prevalence estimates, in the analysis for the overall USAP region, further weighting was performed so that the contribution of data from a single jurisdiction to the overall estimate was equal to the proportion of children younger than 10 years from the USAP (based on census data) that it contributes. This ensures that overall estimates were not overly influenced by jurisdictions with more publications. The weights were adjusted so that the total sample size n, defined as the sum of the weights, equaled the number of children included in the model to maintain the correct type I and II errors. Thus, for estimation of the overall USAP prevalence, each jurisdiction was assigned a sample size of pJ n, where pJ is the number of children younger than 10 years in the 2010 census of jurisdiction (J) divided by the total number of children younger than 10 years across jurisdictions included in the model.42,43 This poststratification weighting44 allows for the overall USAP estimate to reflect the distribution of children across jurisdictions as in a simple random sample.
We used one set of models to predict prevalence by single ages for each jurisdiction within the USAP and to test for differences between jurisdictions using a global F test of all age power components. We used another model to predict prevalence by single ages for the USAP region overall and to compare the overall USAP and contiguous US curves across ages with a global F test. We computed separate models for overweight, obesity, and OWOB combined.
To ensure that the published prevalence data that were being aggregated within each USAP jurisdiction were homogeneous, we performed models with and without inclusion of a random effect for manuscript number for each jurisdiction with 3 or more data sources. There was no evidence of heterogeneity for any jurisdiction (all Ps > .1). We used a bootstrap analysis to determine the effect of the variability of the included manuscripts on the results. The bootstrap analysis performed 500 iterations in which a random selection of data sources with replacement was made within jurisdiction maintaining the number of data sources per jurisdiction at each iteration. We performed further subgroup analyses (based on jurisdiction, year, source of data, and type of sampling) as sensitivity analyses. To test disaggregation of published estimates of age groups into single ages, we did analysis of variance modelling of prevalence by age group, using the same weighting scheme as described previously and assigning each data source to age group 2 to 5 years or 6 to 8 years; we assigned estimates to one of these categories.
RESULTS
Two hundred forty-six single-year data points resulted from 27 data sources: 3 from the contiguous states (27 data points for single ages),11,37,38 3 from Alaska,25–27 5 from American Samoa,28–31 2 from CNMI,10,18 2 from Guam,33,34 10 from Hawaii,8,9,20–23,35–37,45 and 2 from the FSM.24,32 The 24 USAP sources contributed 219 data points of prevalence for single ages. The adjusted sample size per age group for each USAP jurisdiction is presented in Table B (available as a supplement to the online version of this article at http://www.ajph.org). When we added NHANES reference data, the total sample size was 230 515 children with OWOB data. Sample sizes per jurisdiction and for the contiguous states are presented in Table 2.
TABLE 2.
Sample Size per Jurisdiction of the US–Affiliated Pacific Region and the 48 Contiguous United States in Literature on Prevalence of Young Child Overweight and Obesity, Published January 2001–April 2014
| Jurisdiction | No. Aged 0–9 Years in 2010 Census | No. Articles or Reports Included | No. Children Measured Aged 2–10 Years Since 2000 | No. With Proportional Weighting |
|---|---|---|---|---|
| Alaska | 104 883 | 3 | 137 040.0 | 594.7 |
| American Samoa | 13 146 | 5 | 11 429.3 | 73.8 |
| Chuuk | 11 733 | 1a | 800 | 66.8 |
| CNMI | 9440 | 2 | 753.0 | 53.0 |
| Contiguous US | 40 223 509 | 3 | 7312.2 | 228 474.6 |
| Guam | 28 273 | 2 | 15 037.0 | 161.4 |
| Hawaii | 170 768 | 10 | 55 197.5 | 970.5 |
| Kosrae | 1587 | 1a | 812.0 | 9.2 |
| Pohnpei | 8298 | 1a | 580.0 | 46.1 |
| Yap | 11 376 | 2a | 1553.6 | 64.5 |
| Sum | 40 583 013 | 27 | 230 514.6 | 230 514.6 |
Note. CNMI = Commonwealth of the Northern Mariana Islands; US = United States. The sample sizes were adjusted to be proportional to the jurisdiction census counts of children aged 10 years and younger and so that the total sample size equals the number of children across publications included in the model. The jurisdiction adjusted counts were divided into ages proportionally based on the observed counts.
Yap had a total of 2 data sources, of which one is a shared data source with Chuuk, Kosrae, and Pohnpei.
Most data sets targeted children aged 2 to 5 years. Only data for this age group were available for Guam and for the states of Chuuk, Kosrae, and Pohnpei of the FSM. Sample sizes varied slightly between models. Two of the 24 sources from the USAP only reported obesity prevalence8,21 leaving 22 sources that contributed 206 data points for the overweight plus obesity analyses. Four sources did not provide a separate prevalence of obesity26,32,34,35; thus, the model predicting obesity included 143 data points from 20 USAP sources. Six sources did not separate prevalence of overweight from overweight plus obesity8,21,26,32,34,35; thus, 18 USAP sources contributed 130 data points for the model predicting overall overweight prevalence. The vast majority of the data sources for the USAP were from census or near censuses of children who were members of government organizations, such as schools, health care organizations, and WIC programs. For 2- to 5-year-old children, WIC was the major contributor to data, and for 6- to 8-year-old children, schools were major contributors to data (Table 1).
Predicted Overweight and Obesity Prevalence
Overall US-Affiliated Pacific jurisdictions
Predicted curves are given in Figure 1, and regression coefficients for age for each of the models in Table C (available as a supplement to the online version of this article at http://www.ajph.org). The OWOB estimate increased by year of age from 21% at age 2 years to 39% at age 8 years and the trend of OWOB increased sharply at age 5 years. After the removal of the data from FSM states, where the prevalence estimates are much lower and generally only data through age 4 years are available, the pattern was unchanged, because of the small contribution of the FSM states to the overall population size of the USAP. The trend of OWOB was also unchanged by the removal of American Samoa where prevalence estimates are much higher, also because of the small population sizes of American Samoa. Removal of Hawaii, the jurisdiction contributing the largest population of children, led to a similar prevalence curve, with a steeper increase at age 5 years. Separate analyses of data collected in 2007 and earlier and collected in 2008 and later showed a similar trend in OWOB for the USAP. The prevalence curve was unchanged when the data were limited to WIC and school sources only.
FIGURE 1.
Predicted prevalence of overweight, obesity, and overweight or obesity for ages 2–8 years among all US-Affiliated Pacific jurisdictions combined, in literature published January 2001–April 2014.
The trend was mirrored in the obesity prevalence data, in which the estimates did not change in early ages, but increased significantly in later ages (5–8 years), from 10% at age 2 years to 23% at age 8 years. None of the age terms reached significance in the overweight model and the overall prevalence was stable from ages 2 years (13%) to 8 years (15%).
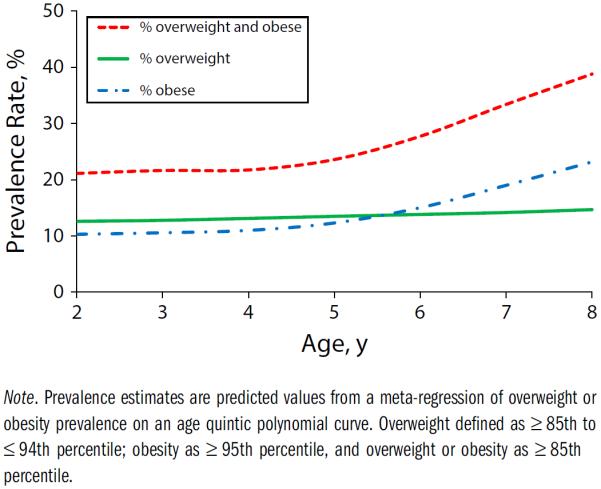
Individual jurisdictions within the US-Affiliated Pacific jurisdictions
For Alaska, American Samoa, CNMI, Hawaii, and Yap, prevalence of OWOB was predicted for ages 2 to 8 years. For Guam and the FSM states of Chuuk, Kosrae, and Pohnpei, prevalence of OWOB was only predicted for ages 2 to 5 years because of lack of data in children aged 5 to 8 years. Separate prevalence estimates of overweight and obesity were not reported because of small sample sizes by jurisdiction.
Figure 2 shows the prevalence curves for each USAP jurisdiction; regression coefficients for models are given in Table D (available as a supplement to the online version of this article at http://www.ajph.org). Based on jurisdictions with data beyond age 5 years, the OWOB prevalence estimates were relatively flat until that time and then increased yearly up to age 8 years. The overall curves were found to differ across jurisdictions (P < .001 for the global F test). There were 3 general patterns across the jurisdictions. One pattern was defined by high OWOB prevalence. The prevalence was highest in Guam and American Samoa, followed by Yap. For Guam, OWOB prevalence was 39% at age 2 years and 38% from age 3 to 5 years. For American Samoa, the OWOB prevalence increased from 34% at age 2 years to 47% at 8 years. In another pattern, Alaska, Hawaii, and CNMI had lower, although still substantial, OWOB prevalence estimates. From ages 5 to 8 years, CNMI showed a much steeper increase. For Alaska, OWOB prevalence increased from 22% at age 2 years to 35% at 8 years, for Hawaii from 20% at 2 years to 34% at 8 years, and for CNMI from 25% at 2 years to 47% at 8 years. In the third pattern, 3 states of the FSM showed low OWOB prevalence up to age 5 years—Chuuk, Kosrae, and Pohnpei. With only 1 data source, the prevalence was constant across ages and was 2% for Pohnpei, and 3% for Chuuk and Kosrae. For Yap, an FSM state with more available data, the estimated OWOB prevalence was higher and remained similar across ages, from 30% at age 2 years to 34% at age 8 years.
FIGURE 2.
Predicted prevalence of overweight and obesity, ages 2–8 years, for the US-Affiliated Pacific region (USAP) combined, individual USAP jurisdictions, and the 48 contiguous United States, in literature published January 2001–April 2014.
The 48 contiguous states
Figure 2 displays the prevalence curve for the 48 contiguous states. The pattern of stable prevalence in early ages and increase thereafter was displayed for the contiguous United States as well. However, an increase occurred at age 4 years and the prevalence plateaued at age 7 years. The OWOB prevalence increased from 24% at age 2 years to 35% at 8 years.
We compared the contiguous US curve with a USAP curve aggregated across jurisdictions. We included only jurisdictions with data from children aged 2 to 8 years (Alaska, American Samoa, CNMI, and Hawaii) in the overall USAP comparison curve, created within the model as a weighted average across jurisdictions, where the weights were proportional to the size of the jurisdiction population and adjusted to sum to the overall sample size (Table B, available as a supplement to the online version of this article at http://www.ajph.org). The estimated prevalence curve of the USAP differed from that of the contiguous states (P < .001; F test). The prevalence at younger ages was lower in the USAP than the contiguous United States, and the increase in OWOB was steeper after age 5 years in the USAP. Significant differences between USAP and the contiguous United States persisted when we removed the jurisdictions of American Samoa or Hawaii from the USAP estimate. Also, each of the USAP jurisdiction-specific curves for Alaska, American Samoa, CNMI, and Hawaii differed significantly from the contiguous US curve (all Ps < .001).
Sensitivity Analysis
We performed several sensitivity analyses to determine the robustness of our estimation procedure. The prevalence curve was similar when we removed the jurisdiction with the highest prevalence (American Samoa) or with the largest contribution to sample size (Hawaii), or when stratified by data collection year. We found a significant difference, at P < .001, between the curve for the US Pacific region and that from the contiguous United States for each iteration of the bootstrap analysis. Also, the 95% confidence intervals for the prevalence curves predicted from the bootstrap analysis were similar in shape to that in Figure 1. The prevalence curve pattern was maintained when we limited the data to WIC and to school sources, which represent census or near census data. Thus, the prevalence curve is quite robust to the variation in the data sources.
We found the same pattern in the analysis of variance (Figure B, available as a supplement to the online version of this article at http://www.ajph.org)—the prevalence of overweight and obesity rose between the group aged 2 to 5 years and the group aged 6 to 8 years for both the USAP and the contiguous United States, and the prevalence was higher at ages 6 to 8 years in the USAP (P < .001).
DISCUSSION
At first contact with Europeans, Pacific people were described as strong, muscular, slim, and healthy.46 Traditional foods were nutritionally adequate.47 Globalization48 and trade policies placed pressures on food security.48,49 The introduction of a cash economy50 and other social, economic, and political changes contributed to a nutritional and epidemiological transition that resulted in an increase in chronic diseases.
The estimated prevalence of OWOB in the USAP varied in the present study from 21% at age 2 years to 39% at age 8 years and in the contiguous United States from 24% at age 2 years to 35% at age 8 years. The prevalence of OWOB was lower at younger ages in the USAP but increased at a faster rate. The prevalence of OWOB increased sharply at age 5 years in the USAP, and at age 4 years in the 48 contiguous states. The start of the abrupt increase in OWOB at age 4 or 5 years in the USAP and the US contiguous states could be an artifact of the 0-to-5–year and 6-to-10–year age grouping of samples that were available. Also, fewer data were available for children aged 6 to 8 years, and this age group could be biased by the inclusion of 9- to 10-year-old children in only some of the samples. Also, older age groups were sampled from schools with relatively comprehensive sampling whereas younger age groups were sampled from agencies that could represent lower socioeconomic subsets of populations (e.g., WIC). However, these sources of data are likely comparable as USAP populations are generally in lower income brackets. Also, the OWOB prevalence of children was found to be similar between WIC participants and nonparticipants in NHANES data,51 although nonparticipants in the highest income level were found to have lower BMI. If this confounding of age and data source introduces a bias in the present study, it would be expected that the prevalence at younger ages would be overestimated.
The increase in obesity in the older age group could also reflect the lifestyle transition to attending elementary school, and the food and physical activity environment at elementary schools warrants further exploration. Early life influences, as early as fetal life and infancy, could also have set a growth trajectory from malnutrition attributable to either lack of energy and nutrients, or excess.52 Fetal programming and metabolic changes can optimize for energy storage, and in a mismatched postnatal obesogenic environment can lead to childhood obesity.53
The states of Chuuk, Pohnpei, and Kosrae have lower income, according to the World Bank,54 and may have more undernutrition than obesity in children aged 0 to 5 years. Public health messages should focus on sustainable diets, healthy eating, and physical activity,55 rather than on weight reduction, particularly where undernutrition and obesity coexist.56
We defined OWOB for this study on the basis of CDC criteria. Definitions of OWOB vary across countries.57 In the 48 contiguous US states, including in NHANES, CDC growth charts are used for children aged 2 to 19 years.58,59 These charts were developed from the noninstitutionalized population of the contiguous states.13 There is a need for global comparisons. The International Obesity Task Force used 6 large nationally representative samples (Brazil, Great Britain, Hong Kong, the Netherlands, and Singapore) to develop global centile curves for children aged 2 to 18 years that are linked to the adult BMI cut-points of 25 kg/m2 and 30 kg/m2.15 World Health Organization (WHO) reference data for children aged 0 to 5 years are from samples of healthy children in Brazil, Ghana, India, Norway, Oman, and the United States,60 and define overweight as greater than 1 standard deviation and obesity as greater than 2 standard deviations above the mean.60,61 The WHO reference is an international multiethnic standard for how children should grow, rather than how children are growing, in an environment where they may or may not be healthy.
Further examination of USAP data with global references should be pursued where data are available to do so, to help interpret health implications of body size among the region's diverse ethnic groups. For example, evidence suggests that definitions of OWOB do not adequately correspond to body fat levels in children of diverse ethnic backgrounds,62 especially among Pacific people.63 Several studies have developed ethnic-specific BMI cut-points,64,65 including for Pacific Islanders from the South Pacific,63 though these studies have focused on adults. Such cut-points may provide additional insight into the interpretation of the data. However, with the high prevalence of mixed ethnicity (e.g., Pacific Islander and Asian groups) in the Pacific,9 the application of different cut-points or reference data (e.g., WHO, International Obesity Task Force, or CDC) for different ethnic groups would not allow comparison across these population groups.
Although the prevalence of OWOB in this study cannot be directly compared with the global prevalence of 7% for preschool children,66 based on WHO reference data and cut-points, the estimates are substantially higher among young children in the USAP. At 21% at age 2 years, the overall OWOB prevalence in the USAP was already in excess of the 15% expected in a normal distribution (> 85th percentile). Furthermore, American Samoa and Guam rates were an additional 10 to 15 percentile points higher. Thus, factors before age 2 years, during infancy and the intrauterine period, may contribute to excess OWOB in the USAP, especially in American Samoa and Guam, and deserve further study.
Ethnicity varies substantially across the USAP, with Alaska Natives, the natives of Hawaii and American Samoa of Polynesian ancestry, and natives of the FSM, Guam, and CNMI of Micronesian ancestry. Body attributes vary, with Polynesians historically showing especially large heights and weights.67 The proportion of native ethnic population also varies within each jurisdiction, and among individuals in many cases, with a history of colonization by and immigration from a number of Asian and non-Hispanic White populations.68 Mixing and migration of ethnic populations in the Pacific is very high,69 and increasing elsewhere in the world as well.70
It must be noted that we do not have ethnic identifiers in our data sets and proportion of the population that is native in each jurisdiction varies substantially from 19% Alaska Native or Native American71 to 28% Native Hawaiian in Hawaii71 to 89% Samoan in American Samoa.72 In Hawaii and Alaska, less than half of the jurisdiction's populations is native, and native ethnic groups show higher rates of OWOB compared with jurisdiction means,9,73 implying that OWOB among native populations of the Pacific is higher than the estimates in the current analysis. Interestingly, mixed ethnic children have shown higher risk of OWOB than is expected from a mean of the 2 component ethnicities.9 Reasons for this are not known, but might be related to retaining favored (energy-dense) foods of component cultures. In the nutrition transition continuum, the USAP jurisdictions with higher OWOB are further along in the transition. Some features of this transition include US military presence, imported US food, and presence of US fast-food restaurants.
As each of the USAP jurisdictions has a different environment and a different pattern of OWOB for children and adults, the results are discussed separately by jurisdiction. The estimated prevalence of OWOB among young children in Alaska was high. Although data were drawn from many regions and subpopulations in Alaska, they cannot be considered representative of Alaska Natives, as they were not specifically sampled.74 Alaska Natives constitute approximately 15% of the population in Alaska and are disproportionately young.73 Regions within Alaska also differ by a number of socioeconomic, cultural, and geographic factors that affect risk for OWOB. Data were collected as part of health screenings and a standardized protocol was not followed. Despite these limitations, findings highlight the importance of identifying effective preventive interventions that address the root causes of OWOB.
As early as 1952, American Samoan (Polynesian) infants showed high weight-for-age in the first year of life, trending near the 75th percentile of US children regardless of feeding pattern. High birth weight was common.75 The present data show that the American Samoan children already display higher BMI than children of the contiguous states at age 2 years. American Samoan parents have attributed the high prevalence of OWOB in children and adolescents to high bone tissue and lean tissue, rather than high body fat tissue.76 Still, American Samoan adolescent mean BMIs increased between 1978 and 2007.77 The high prevalence of obesity-driven noncommunicable diseases among American Samoan adults implies that population-level BMI is higher than is healthy.78
At age 2 years, CNMI children showed a relatively high prevalence of OWOB (25%) with a rapid increase to 47% at 8 years, the most rapid increase in OWOB prevalence between age groups among all jurisdictions studied. On Guam, the prevalence of OWOB among children was high and remained stable in the younger ages, from ages 2 years (39%) to 5 years (38%).
The Hawaii OWOB prevalence increased from about one fifth of 2-year-old children to about one third of 8-year-old children, resembling rates of Alaska and the contiguous states, but lower than Guam, CNMI, and American Samoa. Because of the ethnic diversity in Hawaii, which includes substantial proportions of Asians and non-Hispanic Whites in addition to Native Hawaiians and other Pacific Islanders,42 disaggregating the Hawaii data would likely show different OWOB prevalence among the ethnic groups in Hawaii, as has been shown before,79 and which has implications for resource allocation targeting at-risk groups.9
Data from the FSM Maternal and Child Health (MCH) Program report32 present a different view of OWOB prevalence. Chuuk, Kosrae, and Pohnpei were low at 2% to 3%, and Yap was higher, closer to the expected normal distribution of 15%. Generally, these data were from children who visited MCH centers in urban centers and may not be representative of all children in FSM. Sick children may be more likely to attend MCH centers. Furthermore, the data may not represent unique children, because children may attend MCH centers more than once, especially if sick. The second paper from Yap was from an outer island and also may not be representative of Yap. Yap was not expected to show such a large difference in comparison with the 3 other states of FSM. It is difficult to gauge the quality of the anthropometric data and there were no quality control assurances. The small sample also limits the ability to draw robust conclusions. Nonetheless, the FSM data suggest that the prevalence of OWOB children in 3 states of the FSM may be much lower than in other jurisdictions of the USAP, despite high levels of OWOB and obesity-related diseases among adults in these populations.6 Formal studies utilizing standard measuring protocols should be implemented to confirm these findings.
The results reflect all data available on OWOB prevalence in the USAP, and results are likely relatively generalizable to children in the USAP. The jurisdiction-specific estimates are aggregates of homogeneous data sources and also likely represent their jurisdictions, apart from the concerns raised previously. However, the prevalence estimates will not be representative of native populations as described previously. A fuller understanding of the patterns of OWOB in the Freely Associated States of Micronesia will require additional data from FSM, and inclusion of Palau and the Republic of the Marshall Islands.
Despite containing among the fastest growing racial/ethnic groups in the United States in 2000 to 2010,4 the USAP is underrepresented and not reported in US health surveillance reports. The 2-fold increase in obesity from ages 2 to 8 years in USAP children shown here is a public health concern. Disparities in health status, including by race and ethnicity, have widened80 in the USAP. Availability of data on USAP populations are limited or scattered at best (Table 1). Additional data are needed among young children, especially in Palau and the Marshall Islands. Institutions that collect infant and child BMI data are encouraged to publish their findings as this would add to the sparse pool of published data available on children in the region. Policymakers, public health workers, and the USAP community are encouraged to generate and use available data to develop monitoring systems and formulate policies that will improve the health status of USAP children and adults.
Supplementary Material
Acknowledgments
This study was supported by US Department of Agriculture/Agriculture and Food Research Initiative/National Institute of Food and Agriculture grant 2011-68001-30335, Children's Healthy Living Program for Remote Underserved Minority Populations of the Pacific (P. Novotny, PI).
Footnotes
Reprints can be ordered at http://www.ajph.org by clicking the “Reprints” link.
Contributors R. Novotny led the study concept, interpretation of data, and writing of the article, and oversaw and had primary responsibility for the final article. M. K. Fialkowski led data abstraction, drafted discussions on nutrition and epidemiological transition and overweight and obesity global definitions, and compiled the article. F. Li conducted statistical analysis, reported results, and had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. Y. Paulino participated in design and interpretation of Guam data, and drafted the data systems discussion. D. Vargo participated in design and led interpretation of American Samoa data. R. Jim and J. Deenik participated in design and interpretation of Federated States (Yap, Kosrae, Pohnpei, and Chuuk) of Micronesia data. P. Coleman and J. H. Kim participated in design and interpretation of Commonwealth of the Northern Marianas data. A. Bersamin participated in design and interpretation of Alaska data. C. R. Nigg participated in design and interpretation of Hawaii data. R. T. L. Guerrero participated in design and interpretation of Guam data. L. R. Wilkens led the meta-regression and had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors critically reviewed and approved the final article.
An abstract of this study was presented at Experimental Biology 2014; April 26–30, 2014; San Diego, CA.
Jodi Leslie contributed to the writing of the abstract and article.
Human Participant Protection This study used secondary data sources with no individual identifiers and, thus, human participant protection was not needed.
References
- 1.Murphy SP. Collection and analysis of intake data from the integrated survey. J Nutr. 2003;133(2):585S–589S. doi: 10.1093/jn/133.2.585S. [DOI] [PubMed] [Google Scholar]
- 2.Peterkin BB. Nationwide food consumption survey, 1977–1978. Prog Clin Biol Res. 1981;67:59–69. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. National Center for Health Statistics [Accessed April 12, 2013];National Health and Nutrition Examination Survey: note on 2007–2010 sampling methodology. 2011 Available at: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/sampling_0708.htm.
- 4.Hixson L, Hepler BB, Kim MO. The Native Hawaiian and Other Pacific Islander Population: 2010. US Census Bureau; Washington, DC: 2012. [Google Scholar]
- 5.Department of Labor and Workforce Development [Accessed January 5, 2014];Alaska 2010 census demographic profiles. 2010 Available at: http://live.laborstats.alaska.gov/cen/dp.cfm.
- 6.Secretariat of the Pacific Community [Accessed June 26, 2013];NCD statistics for the Pacific Islands countries and territories. 2010 Available at: http://www.spc.int/hpl/index.php?option=com_docman&task=doc_details&gid=67&Itemid=99999999.
- 7.Board resolution #48-01: the burden of NCDs. Pacific Islands Health Officers Association; Honolulu, HI: 2010. [Google Scholar]
- 8.Baruffi G, Hardy CJ, Waslien CI, Uyehara SJ, Krupitsky D. Ethnic differences in the prevalence of overweight among young children in Hawaii. J Am Diet Assoc. 2004;104(11):1701–1707. doi: 10.1016/j.jada.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 9.Novotny R, Oshiro CE, Wilkens LR. Prevalence of childhood obesity among young multiethnic children from a health maintenance organization in Hawaii. Child Obes. 2013;9(1):35–42. doi: 10.1089/chi.2012.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruss MB, Michael TJ, Morris JR, et al. Childhood obesity prevention: an intervention targeting primary caregivers of school children. Obesity (Silver Spring) 2010;18(1):99–107. doi: 10.1038/oby.2009.111. [DOI] [PubMed] [Google Scholar]
- 11.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Novotny R. Nutrition and Health Status of Children in the CNMI. University of Hawaii, Northern Marianas College, Department of Public Health; Honolulu, HI: 2006. [Google Scholar]
- 13.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Hyattsville, MD: National Center for Health Statistics. 2002;11(246) [PubMed] [Google Scholar]
- 14.Frisancho AR. Anthropometric Standards for the Assessment of Growth and Nutritional Status. University of Michigan Press; Ann Arbor, MI: 1990. [Google Scholar]
- 15.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flegal KM, Tabak CJ, Ogden CL. Overweight in children: definitions and interpretation. Health Educ Res. 2006;21(6):755–760. doi: 10.1093/her/cyl128. [DOI] [PubMed] [Google Scholar]
- 17.Fialkowski MK, Okoror TA, Boushey CJ. The relevancy of community-based methods: using diet within Native American and Alaska Native adult populations as an example. Clin Transl Sci. 2012;5(3):295–300. doi: 10.1111/j.1752-8062.2011.00364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paulino YC, Coleman P, Davison NH, et al. Nutritional characteristics and body mass index of children in the Commonwealth of the Northern Mariana Islands. J Am Diet Assoc. 2008;108(12):2100–2104. doi: 10.1016/j.jada.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Novotny R, Coleman P, Tenorio L, et al. Breastfeeding is associated with lower body mass index among children of the Commonwealth of the Northern Mariana Islands. J Am Diet Assoc. 2007;107(10):1743–1746. doi: 10.1016/j.jada.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 20.Pobutsky AM, Hirokawa R, Zou L, Huang T, Rosen L, Wood B. Overweight and at-risk for overweight among Hawai'i public school students entering kindergarten, 2002–2003. Hawaii Med J. 2006;65(10):283–287. [PubMed] [Google Scholar]
- 21.Chai D, Kaluhiokalani N, Little J, et al. Childhood overweight problem in a selected school district in Hawaii. Am J Hum Biol. 2003;15(2):164–177. doi: 10.1002/ajhb.10134. [DOI] [PubMed] [Google Scholar]
- 22.Okihiro M, Davis J, White L, Derauf C. Rapid growth from 12 to 23 months of life predicts obesity in a population of Pacific Island children. Ethn Dis. 2012;22(4):439–444. [PMC free article] [PubMed] [Google Scholar]
- 23.Manea SJ. Overweight among Kauai first-graders. Hawaii Med J. 2005;64(9):244–245. [PubMed] [Google Scholar]
- 24.Ichiho HM, Yurow J, Lippwe K, Aitaoto N. An assessment of noncommunicable diseases, diabetes, and related risk factors in the Federated States of Micronesia, State of Yap: a systems perspective. Hawaii J Med Public Health. 2013;72(5):57–67. [PMC free article] [PubMed] [Google Scholar]
- 25.Boles M, Fenaughty AM, Fink K, Utermohle C. Prevalence of overweight and obesity among students in the Kenai Peninsula borough school district, 2011–2012. Chronic Dis Prev Health Promotion. 2012;4(3):1–12. [Google Scholar]
- 26.Alaska Special Supplemental Nutrition Program for Women Infants and Children . National performance measures. Alaska Department of Health and Social Services; Anchorage, AK: 2012. WIC Program, Report 340. [Google Scholar]
- 27.Eberling S. Results of the 2010/2011 Survey of Alaskan Kindergarten Children: Alaska Oral Health Basic Screening Survey. Alaska Department of Health and Social Services; Anchorage, AK: 2011. [Google Scholar]
- 28.Vargo D. Prevalence of Overweight in American Samoan Schoolchildren. American Samoa Community College; Pago Pago, American Samoa: 2007. [Google Scholar]
- 29.Vargo D. Prevalence of Overweight in American Samoan Schoolchildren (2007/2008 School Year) American Samoa Community College; Pago Pago, American Samoa: 2008. [Google Scholar]
- 30.Vargo D. Prevalence of Obesity in American Samoan Schoolchildren (2008/2009 School Year) American Samoa Community College; Pago Pago, American Samoa: 2009. [Google Scholar]
- 31.US Department of Health and Human Services, Health Resources and Services Administration [Accessed September 19, 2014];American Samoa Maternal and Child Health Program. Assets and needs assessment—2010. 2010 Available at: https://mchdata.hrsa.gov/tvisreports/Documents/NeedsAssessments/2011/AS-NeedsAssessment.pdf.
- 32.US Department of Health and Human Services, Health Resources and Services Administration [Accessed September 19, 2014];Federated States of Micronesia Maternal and Child Health Programs. MCH Program needs assessment for 2010–2015. 2010 Available at: https://mchdata.hrsa.gov/tvisreports/Documents/NeedsAssessments/2011/FM-NeedsAssessment.pdf.
- 33.Guam Department of Education . 2011–2012 Head Start program information report: Guam. Guam Head Start Progam; Hagatna, Guam: 2012. [Google Scholar]
- 34.Guam Department of Public Health and Social Services. Guam Division of Public Health. Bureau of Family Health and Nursing Services. Maternal and Child Health Program [Accessed September 19, 2014];Guam's Title V Maternal and Child Health 2010 needs assessment. 2010 Available at: https://mchdata.hrsa.gov/tvisreports/Documents/NeedsAssessments/2011/GU-NeedsAssessment.pdf.
- 35.Hawaii Special Supplemental Nutrition Program for Women Infants and Children. Nutrition Services Plan (NSP) FFY; Hilo/Kona WIC agencies; Hawaii WIC: Hilo, HI: 2012. 2012. [Google Scholar]
- 36.Centers for Disease Control and Prevention [Accessed September 19, 2014];Table 6D: 2011 pediatric nutrition surveillance: national comparison of growth and anemia indicators by contributor children aged < 5 years. 2011 Available at: http://www.cdc.gov/pednss/pednss_tables/pdf/national_table6.pdf.
- 37.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 38.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 39.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 40.Sheu C-F, Suzuki S. Meta-analysis using linear mixed models. Behav Res Methods Instrum Comput. 2001;33(2):102–107. doi: 10.3758/bf03195354. [DOI] [PubMed] [Google Scholar]
- 41.Snedecor G, Cochran W. Statistical Methods. Iowa State University Press; Ames, IA: 1989. [Google Scholar]
- 42.US Census . US Census Bureau; Jeffersonville, IN: 2010. 2010. [Google Scholar]
- 43.Summary Analysis of Key Indicators From the FSM 2010 Census of Population and Housing. Federated States of Micronesia: FSM Division of Statistics; Pohnpei: 2010. [Google Scholar]
- 44.Rossi PH, Wright JD, Anderson AB. Handbook of Survey Research: Quantitative Studies in Social Relations. Academic Press; New York, NY: 1985. [Google Scholar]
- 45.Stark MJ, Niederhauser VP, Camacho JM, Shirai L. The prevalence of overweight and obesity in children at a health maintenance organization in Hawai'i. Hawaii Med J. 2011;70(7, suppl 1):27–31. [PMC free article] [PubMed] [Google Scholar]
- 46.Miller CD. In: The influence of foods and food habits upon the stature and teeth of ancient Hawaiians. Snow CE, editor. Kentucky Press; Early Hawaiians. Lexington, KY: 1974. pp. 167–175. [Google Scholar]
- 47.Fujita R, Braun KL, Hughes CK. The traditional Hawaiian diet: a review of the literature. Pac Health Dialog. 2004;11(2):250–259. [PubMed] [Google Scholar]
- 48.Hughes RG, Lawrence MA. Globalization, food and health in Pacific Island countries. Asia Pac J Clin Nutr. 2005;14(4):298–306. [PubMed] [Google Scholar]
- 49.Thow AM, Heywood P, Schultz J, Quested C, Jan S, Colagiuri S. Trade and the nutrition transition: strengthening policy for health in the Pacific. Ecol Food Nutr. 2011;50(1):18–42. doi: 10.1080/03670244.2010.524104. [DOI] [PubMed] [Google Scholar]
- 50.Evans M, Sinclair RC, Fusimalohi C, Liava'a V. Diet, health and the nutrition transition: some impacts of economic and socio-economic factors on food consumption patterns in the Kingdom of Tonga. Pac Health Dialog. 2002;9(2):309–315. [PubMed] [Google Scholar]
- 51.Ver Ploeg M, Mancino L, Lin BH, Guthrie J. US Food assistance programs and trends in children's weight. Int J Pediatr Obes. 2008;3(1):22–30. doi: 10.1080/17477160701520231. [DOI] [PubMed] [Google Scholar]
- 52.Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353(17):1802–1809. doi: 10.1056/NEJMoa044160. [DOI] [PubMed] [Google Scholar]
- 53.Monasta L, Batty G, Cattaneo A, et al. Early life determinants of overweight and obesity: a review of systematic reviews. Obes Rev. 2010;11(10):695–708. doi: 10.1111/j.1467-789X.2010.00735.x. [DOI] [PubMed] [Google Scholar]
- 54.The Little Data Book 2012. The World Bank; Washington, DC: 2012. [Google Scholar]
- 55.Johns T, Eyzaguirre PB. Linking biodiversity, diet and health in policy and practice. Proc Nutr Soc. 2006;65(2):182–189. doi: 10.1079/pns2006494. [DOI] [PubMed] [Google Scholar]
- 56.Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. Int J Obes (Lond) 2005;29(1):129–136. doi: 10.1038/sj.ijo.0802824. [DOI] [PubMed] [Google Scholar]
- 57.Flegal KM, Ogden CL. Childhood obesity: are we all speaking the same language? Adv Nutr. 2011;2(2):159S–166S. doi: 10.3945/an.111.000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ogden CL. Defining overweight in children using growth charts. Md Med. 2004;5(3):19–21. [PubMed] [Google Scholar]
- 59.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 2010;(25):1–5. [PubMed] [Google Scholar]
- 60.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.World Health Organization [Accessed April 30, 2013];BMI-for-age (5-19 years) Growth reference 5-19 years. 2007 Available at: http://www.who.int/growthref/who2007_bmi_for_age/en.
- 62.Deurenberg P, Deurenberg-Yap M. Differences in body-composition assumptions across ethnic groups: practical consequences. Curr Opin Clin Nutr Metab Care. 2001;4(5):377–383. doi: 10.1097/00075197-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 63.The Native Hawaiian and Other Pacific Islander Population: 2010. US Census Bureau; Washington, DC: 2012. [Google Scholar]
- 64.Kim E, Hwang JY, Woo EK, Kim SS, Jo SA, Jo I. Body mass index cutoffs for underweight, overweight, and obesity in South Korean schoolgirls. Obes Res. 2005;13(9):1510–1514. doi: 10.1038/oby.2005.183. [DOI] [PubMed] [Google Scholar]
- 65.Hosseini M, Carpenter RG, Mohammad K, Jones ME. Standardized percentile curves of body mass index of Iranian children compared to the US population reference. Int J Obes Relat Metab Disord. 1999;23(8):783–786. doi: 10.1038/sj.ijo.0800924. [DOI] [PubMed] [Google Scholar]
- 66.de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92(5):1257–1264. doi: 10.3945/ajcn.2010.29786. [DOI] [PubMed] [Google Scholar]
- 67.Wallace A. The Polynesians and their migrations. In: Samuelson J, Crookes W, editors. The Quarterly Journal of Science. John Churchill and Sons; London, England: 1867. pp. 164–166. [Google Scholar]
- 68.Parkman M, Sawyer J. Dimensions of ethnic intermarriage in Hawaii. Am Sociol Rev. 1967;32(4):593–607. [Google Scholar]
- 69.Wasem C. U.S. affiliated Pacific basin jurisdictions: legal, geographic, and demographic information. Office of Pacific Health and Human Services - Region IX Office of the Regional Health Administrator, Department of Health and Human Services; Honolulu, HI: 2004. [Google Scholar]
- 70.Absatova M, Nurpeisova T, Tektibayeva D, Mamytbekova L. Scientific-theoretical basis of polycultural education development in polyethnic medium. World Appl Sci J. 2013;23(10):1360–1365. [Google Scholar]
- 71.US Census Bureau . Facts for features: American Indian and Alaska Native Heritage Month: November 2013. US Department of Commerce; Washington, DC: 2013. [Google Scholar]
- 72.Profile of General Demographic Characteristics: 2010. US Census Bureau; Washington, DC: 2010. 2010 American Samoa demographic profile data. [Google Scholar]
- 73.Alaska Native Epidemiology Center . Alaska Native Health Status Report. Alaska Native Tribal Health Consortium; Anchorage, AK: 2009. [Google Scholar]
- 74.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163(4):344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 75.Rush EC, Paterson J, Obolonkin VV, Puniani K. Application of the 2006 WHO growth standard from birth to 4 years to Pacific Island children. Int J Obes (Lond) 2008;32(3):567–572. doi: 10.1038/sj.ijo.0803751. [DOI] [PubMed] [Google Scholar]
- 76.Gittelsohn J, Lee-Kwan SH, Batorsky B. Community-based interventions in prepared-food sources: a systematic review. Prev Chronic Dis. 2013;10:E180. doi: 10.5888/pcd10.130073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Davison N, Fanolua S, Rosaine M, Vargo DL. Assessing overweight and obesity in American Samoan adolescents. Pac Health Dialog. 2007;14(2):55–61. [PubMed] [Google Scholar]
- 78.Ichiho HM, Roby FT, Ponausuia ES, Aitaoto N. An assessment of noncommunicable diseases, diabetes, and related risk factors in the territory of American Samoa: a systems perspective. Hawaii J Med Public Health. 2013;72(5):10–18. [PMC free article] [PubMed] [Google Scholar]
- 79.Crowell DH, Rudoy R, Nigg CR, Sharma S, Baruffi G. Perspective on racial/ethnic birth weight. Hawaii Med J. 2010;69(9):216–220. [PMC free article] [PubMed] [Google Scholar]
- 80.Hosey G, Ichiho H, Satterfield D, et al. Chronic disease surveillance systems within the US Associated Pacific Island jurisdictions. Prev Chronic Dis. 2011;8(4):A86. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.