Abstract
In 2009, a preliminary framework for how climate change could affect worker safety and health was described. That framework was based on a literature search from 1988–2008 that supported seven categories of climate-related occupational hazards: (1) increased ambient temperature; (2) air pollution; (3) ultraviolet exposure; (4) extreme weather; (5) vector-borne diseases and expanded habitats; (6) industrial transitions and emerging industries; and (7) changes in the built environment. This paper reviews the published literature from 2008–2014 in each of the seven categories. Additionally, three new topics related to occupational safety and health are considered: mental health effects, economic burden, and potential work safety and health impacts associated with the nascent field of climate intervention (geoengineering).
Beyond updating the literature, the paper also identifies key priorities for action to better characterize and understand how occupational safety and health may be associated with climate change events and ensure that worker health and safety issues are anticipated, recognized, evaluated, and mitigated. These key priorities include research, surveillance, risk assessment, risk management, and policy development. Strong evidence indicates that climate change will continue to present occupational safety and health hazards, and this framework may be a useful tool for preventing adverse effects to workers.
Keywords: occupational safety and health, temperature, extreme weather, risk assessment
INTRODUCTION
Workers have received inadequate attention in the literature on climate-change and public health.(1) To address this deficit, in 2009, a preliminary framework for how climate change could affect worker safety and health was developed.(2) That framework was based on an assessment of the scientific literature published from 1988–2008. Seven categories of climate-related hazards were identified: (1) increased ambient temperature; (2) air pollution; (3) ultraviolet exposure; (4) extreme weather; (5) vector-borne diseases and expanded habitats; (6) industrial transitions and emerging industries; and (7) changes in the built environment. In addition to identifying these seven categories, the framework charted areas where the occupational safety and health field could address occupational hazards of climate change. These areas included alteration of standards, modification and improvement of hazard controls including personal protective equipment (PPE), development of acclimatization procedures, new research directions, development of new hazard control guidance and hazard communications, development of early warning systems and surveillance, and increased emphasis on prevention through design.(2)
This paper updates and strengthens the 2009 framework with a review and assessment of the peer-reviewed literature from 2008–2014 for each of the seven-climate related occupational safety and health hazard categories. Recent examples of hazards in each of the climate-related categories are provided. Some recent reports from authoritative organizations on environmental and public health issues of climate change now include workers as vulnerable populations.(3–8) However, awareness of the potential work-relatedness of hazards with climate change is not widely known and needs further emphasis.(1)
The update of the literature supporting the framework involved searches of the following information and data bases for English language articles: ABI/Inform; Compendex; Embase; Environment Abstracts; Environmental Science Journals; Global Health; Health & Safety Science Journals; NIOSHTIC-2; PubMed; Risk Abstracts; Scopus; Toxicology Abstracts; Toxline; and Web of Science. The seven categories of climate-related occupational hazards identified in the 2009 framework were used as the search terms.(2) In addition, literature was searched relevant to the topics of mental health implications, economic burden, and the potential impact on workers of geoengineering (climate intervention).
Beyond increased awareness, there is need for more strategic thinking about actions that prevent or reduce risk to workers resulting from climate change. While there are still uncertainties about climate change models, climate change is likely to result in increasing prevalence, distribution, and severity of known occupational hazards, and new unanticipated hazards may emerge.(2–8) Employment increases are likely in jobs intended to mitigate or respond to consequences of climate change. Workers may consequently be exposed to extreme conditions that the general public can elect to avoid. Impacts to workers will include the direct effects of climate change-potentiated occupational hazards such as increased ambient temperatures. Indirect climate-change-associated occupational hazards are also likely to occur from industrial transitions, emerging industries, and changes in the built environment. How to address these anticipated impacts is an important question. Identification of gaps related to specific hazards, their severity, and location of populations at risk and identification of information and communication tools that will protect workers are also needed. This paper provides priorities for action to address these issues.
OCCUPATIONAL HEALTH HAZARDS AND EFFECTS RELATED TO CLIMATE CHANGE: 2008–2014
Increased Ambient Temperatures
The global mean earth surface air temperature has increased during the past 100 years and the resultant deleterious heat-related effects including deaths in workers have been well established.(9,10) Many workers spend their entire work shift in a variety of indoor and outdoor hot environments that may become hotter because of ambient rising temperatures, increases in extreme heat events, or shifting and expanding hot seasons. For many workers, occupational exposures to heat and humidity may be more hazardous than community exposures because workers generally have less control of exposures in their work activities.(11,12)
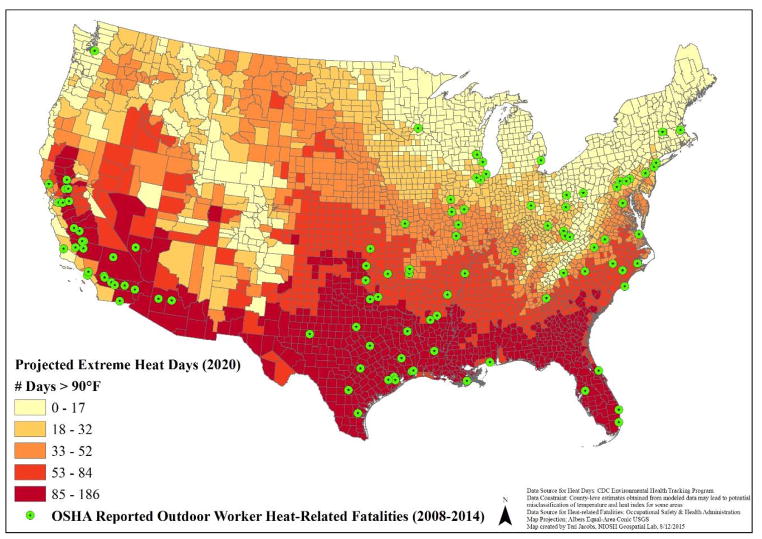
Outdoor workers in particular have been considered at high risk of adverse impacts in part because of their increased exposure to heat and humidity and work that may involve heavy exertion.(13,14) The Occupational Safety and Health Administration conducted a limited assessment of outdoor heat-related fatalities and identified 106 deaths in the United States from 2008–2014 (https://www.osha.gov/SLTC/heatillness/map.html). In Figure 1, the locations of these deaths are mapped along with the projected number of days/year in 2020 with temperatures that exceed 90 °F. The number of days with temperatures above 90 °F is projected to increase. Since most fatalities between 2008 and 2014 occurred in areas that are projected to have increased number of days above 90°F it is likely that more fatalities may occur in the future. For workers who may have second jobs or live in homes that lack efficient cooling or have high humidity, heat stress and susceptibility to heat-related illnesses may be even higher, and may be further complicated by the urban heat island effect (i.e., built-up areas releasing heat absorbed during the day and night).(14) Some workers who perform heavy labor in outdoor and indoor hot environments and are paid a piece rate (like many transient or immigrant farm workers), and those who have poor health and economic conditions with few or non-existent bargaining possibilities, may also be particularly vulnerable to adverse effects. These workers may choose to decline rest and water breaks if they negatively affect their income.(11,15) Also, unacclimatized new workers or workers with less employment tenure have been shown to have proportionally more heat-related illness.(16)
FIGURE 1.
Individual outdoor heat-related fatalities 2008–2014 on projection of number of days above 90 °F in 2020
Heat stress (i.e., the sum of metabolic heat plus environmental heat, minus the heat lost from the body to the environment) can result in heat-related illnesses such as heat stroke, heat exhaustion, heat syncope, heat cramps, heat rash, or death. Heat exposures can also increase the risk of workplace injuries, such as those caused by sweaty palms, fogged-up safety glasses, dizziness, and reduced brain function.(17) Excess heat reduces work capacity and productivity in heat-exposed jobs, and may result in the loss of income, leading to adverse mental health and economic effects.(18–23) On average, working capacity of heat-exposed workers is expected to decrease globally over the rest of this century.(12) For some workers, like those in healthcare or emergency response, the need to work at maximum capacity during extreme heat events or natural disasters, often while wearing personal protective clothing or equipment, may cause additional mental and physical strain.(24)
Changes to the body’s core temperature can alter the absorption, distribution, metabolism, and excretion of toxicants such as, pesticides.(25) Increases in respiration can lead to additional toxicant exposure through inhalation, and increases in sweat and skin blood flow can lead to more efficient transcutaneous absorption of toxicants.(25,26) High temperatures may also accelerate dispersion of pesticides and increase the density of airborne particles. Some workers may be more likely to not use PPE, or not use it correctly because of discomfort from the heat.(26) In addition to pesticides, other airborne pollutants may put additional strain or have exacerbated health effects in exposed workers in hot environments.(24,27) Bourbannais et al. (28) identified 136 occupations with high potential of simultaneous exposure to heat and chemicals. Workers in metal manufacturing and roofing and firefighters were in the highest risk category.
There is a substantial history of standards and guidance related to heat stress and hot environments.(17,31,33) In recent years, a number of new efforts have occurred, such as updated regulation from the California Department of Industrial Relations (https://www.dir.ca.gov/title8/3395.html); interest in a risk assessment strategy that considers the link between meteorological conditions and International Organization for Standardization heat stress standards; the development of a Thermal Climate Index based on a model of human thermoregulation;(34,35) and an updated NIOSH heat stress criteria document.(17) This new guidance from the National Institute for Occupational Safety and Health (NIOSH) reaffirms the 1986 recommended exposure limit/recommended alert limits and reflects increased awareness about physiological changes that result from heat stress, specifically involving better understanding of the central nervous system, circulatory regulation, the sweating mechanism, water and electrolyte balance, and dietary factors. Recent literature supported updates and updated guidance on hydration, the definition of exertional heat stroke, risk factors associated with heat-related illness, and the effects of heat on toxicological responses.(17)
Air Pollution
Air pollution and climate change have complex interrelationships. In a reciprocal interplay, various air pollutants increase global warming and global warming leads to formation of various pollutants.(36–38) Climate change resulting in rising temperatures and an increased wildland fire season, unless mitigated, is projected to have the following effects on national air quality levels: produce 2–8 part per billion increases in summertime average ground-level ozone concentrations in many regions in the United States; further exacerbate ozone concentrations on days when weather is already conducive to high ozone concentrations; lengthen the “ozone season”, and produce increases and decreases in particle pollution over different regions in the United States.(37)
The impact of ambient air pollution on workers has not been assessed comprehensively, but information on the number of premature deaths related to ozone and PM2.5, may make it possible to distinguish general population risk areas by state and geographic regions to infer risks to workers.(39)
Outdoor work in hot environments have increased respiratory rates and thus may be more affected by air pollution than other members of the general population. Since 2008, the role of climate change and air pollution has been better defined and characterized although many questions still remain.(40–42) In addition to other hazards, wildland firefighters’ exposures to air pollution continues to be an area of research and concern.(43) The base camps in which these firefighters live may contribute to their particulate matter exposures via vehicle emissions, dust, and generator use.(44) Climate change is thought to contribute to the recent increase in intensity and duration of wildland fires and this is expected to continue.(45)
Temperature increases associated with climate change can also affect indoor workers exposure to air pollution during their work and non-work times, while traveling to and from work, and from pollutants in their work environment.
Ultraviolet Exposure
The complex interaction of green-house gases, climate change, and stratospheric ozone depletion, results in increased ultraviolet (UV) radiation that can affect all people, particularly outdoor workers.(46) However, while at present UV levels are still increased relative to the 1960s, terrestrial UV radiation is projected to decrease in the 21st century.(47) This change is in part due to the decrease in ozone-depleting chemicals in the atmosphere. Even though the Montreal protocol of 1987 led to reduction of these gases, they still have long lifetimes and “normal” ozone levels are not likely to occur for several decades.(48) Moreover, the recovery may be longer in northern latitudes and in the Arctic.(48,49) Because increased numbers of workers are projected to be working in the Arctic, more will be at risk of UV-related health effects (http://live.laborstats.alaska.gov/occfcst/index.cfm). Additionally, by the year 2100, “models predict that UV radiation will have increased in the tropics (where current UV radiation is already intense) and to have decreased at polar latitudes …”(45) There is a strong interaction between stratospheric ozone-depletion and change in climate induced by greenhouse gas-induced climate change.(50,51) The risks from these interactions are unknown and still require investigation.(46,47) Overexposure to UV radiation can increase the risk of eye damage (e.g., cataracts and photokeratitis), skin and other cancers, sunburn, and immune suppression.(51) It is therefore likely that outdoor workers will have higher exposure to UV radiation as a result of climate change and will be at higher risk for adverse health effects for decades.(48) To the extent that climate change and planetary warming increase temperatures, more fair-skinned people may be exposed to UV radiation and be at risk of skin cancers.(52–57)
Airline pilots’ UV exposure will increase to the extent to which human activity and climate-change affects stratospheric ozone layers. A few studies have demonstrated that airline pilots are at a risk of adverse health effects in their eyes from exposure to UV radiation. Hammer et al. (53) noted some evidence of increased melanoma occurrence in professional pilots. Chorley et al. (196) concluded that pilots flying in daylight hours are exposed to solar radiation that is 2 or 3 times greater at cruising altitudes compared to exposures at sea level. Though pilots are protected by the aircraft windshield which blocks most UVB radiation, there is no standard for the optical transmission properties of the aircraft windshields. Development of such a standard is important to protect pilots from UV radiation. It is known that UV radiation increases by 10%–12% every 1,000 meters of altitude and thereby subsequently affects pilots.(56) Therefore, UV radiation at 10,000 meters of altitude for commercial aircraft may be 2–3 times higher than at ground level.
Extreme Weather
Weather events such as storms, floods, landslides, droughts, and wildfires have been linked to climate change and are likely to present hazards to outdoor workers, particularly emergency responders and others involved in response, rescue, clean-up, and remediation.(2,58) In recent decades, extreme weather, such as hurricanes and wildfires, have increased in frequency and severity amplifying occupational risks.(58–62)
From 1992 to 2006, a total of 307 workers died from natural disasters. Wildfires (80), hurricanes (72), and floods (62) accounted for most of these occupational weather-related fatalities.(45) Fatal injuries were associated with different phases of the response for each of these disaster types. For wildland fires, 80% of the 80 deaths affected workers who were attempting to put out or divert the fires, whereas for hurricanes, more than 60% of the 72 deaths occurred after the disaster event and affected workers involved in clean up, restorative construction, and restoration of public utilities. For flooding events, 45% of all 62 workers who died were operating or riding in a motor vehicle at the time of the injury.(45) Models predict lightning strikes in the United States to increase 12 ±5% per degree Celsius and occur at about 50% greater frequency over the 21st century.(63) Fifteen percent of lightning fatalities from a 2006–2013 dataset occurred during work-related activities.(64)
The increased intensity and duration of the wildland fire season due to drought can also result in more exposure of wildland firefighter’s to smoke and a reduced firefighter recovery time between fire seasons. Additionally, firefighters and other natural resource workers can be exposed to naturally occurring asbestos and/or erionite, fibrous mineral fibers that are potent carcinogens associated with high rates of malignant mesothelioma, during trail and forest road maintenance, timber stand grading, cutting fire lines, and while fighting fires.(65,66)
Extreme weather events may also force workers to remain at the worksite and prolong work hours until replacements arrive, triggering mental fatigue that increases the risk of accidents. The potential for increased rates of morbidity and mortality due to extreme weather hazards is a strong rationale for conducting hazard and vulnerability assessments to expand knowledge and target at-risk worker populations for mitigation and adaption efforts.(67) Modelling future weather-related occupational health risks requires understanding the risks from current weather, recent variations and trends, and the climate-health relationship.(68,69) In addition, Fayard(45) recommends researching how demographic, social, and environmental factors influence disaster outcomes to promote greater disaster preparation which should further protect worker health.
Vector-borne Diseases and Other Biological Hazards
Considerable research regarding the impact of climate change on vector-borne disease and other biological hazards (venomous insects and reptiles, water-borne disease, non-vector-borne pathogens, and poisonous plants) has been conducted since 2008.(5,7,8,70–84) However, literature specifically addressing the occupational implications of those hazards to specific workers is much more limited because of the number of workers and diversity of occupations that may be affected by biological hazards. Outdoor workers are primarily at risk, including those in construction, landscaping, forestry, brush clearing, land surveying, farming, oil field and utility work, natural resources management, and wildland firefighters.(6,72,83,85–90) This increased risk stems from heightened exposure to vectors such as mosquitoes, ticks, and fleas that can transmit parasites, viruses, or bacteria.(6,8,83) In the United States, many vector-borne diseases could directly affect workers (e.g., Lyme disease).(6–8,74,82,92)
Climate effects such as temperature influence vector transmission through their effects on range, vector growth cycles, pathogen development within the vector and subsequent introduction of new diseases into the United States.(8,70,71,73,75,75,78,82,93,95–97) Although some uncertainties remain, the evidence that climate change has contributed to the expanded range of certain vectors is considerable.(70,71,73,75,76,78,82,93,95–106) For example, in 2014, the first locally-acquired case of Chikungunya, a vector-borne viral disease, was documented in the United States.(33,107–111,196) While the introduction of Chikungunya is not thought to be due to climate change, the possibility of establishment and subsequent spread could be influenced by this process. Outdoor workers have up to a five times higher risk for Lyme disease than indoor workers.(106,112–114) The numbers of high-risk counties for Lyme disease in the United States has increased over the last 20 years by >320% in the northeastern states and >250% in the north-central states.(115) Climate change is thought to be one factor that could be contributing to this spread.(115) West Nile and Zika viruses, other known vector-borne hazards to outdoor workers, may increase because of climate change. Recommendations to protect workers exposed to vector-borne diseases have been published.(100,108,110,116–118,199)
Along with increasing vector range, climate change has also extended the habitat or reach of organisms that cause adverse health effects. For example, the incidence of coccidioidomycosis, a fungal disease endemic in the Southwest United States has been associated with a number of outdoor occupations and has increased substantially from 1998–2011.(89,92,119–130) Drought-ridden areas may lead to outdoor workers breathing more windborne dusts with various toxicities and possibly containing harmful vectors.
Some common allergic diseases are climate sensitive. Warmer conditions favor airborne allergens (e.g., fungal spores, plant pollen, and mold). Since 1995, the ragweed pollen season has grown longer at 10 of 11 locations studied.(7,8,80) Expanded ranges for poisonous plants such as poison ivy have significant implications for outdoor workers.(8) Waterborne diarrheal disease is sensitive to climate variability, which can affect workers in occupations such as fishing and natural resource management.(77,79,96,131)
Because of increased growth, range, and duration of growth of pests and weeds, pesticide use is expected to increase, including use in areas where specific pesticides were not previously necessary, thus putting applicators and other workers at increased risk of exposure.(96,132–135) A secondary effect of expanded pest range is illustrated by the expansion of the Mountain Pine beetle in Western states and subsequent build-up of fuels from trees killed by beetles. An increase in wildland fires would put fire-fighters at increased risk.(136,137,200)
Industrial Transitions and Emerging Industries
As society experiences, responds to, and attempts to prevent the effects of climate change industrial transitions will occur. ‘Green’ industries including renewable energy production and the development and use of low-carbon technologies will see substantial growth.(138) In addition, some traditional industries, such as construction, are seeing a transition towards ‘green activities’ such as retrofitting buildings for energy conservation.(139) The US Bureau of Labor Statistics estimates that in 2011 there were 3.4 million ‘Green Goods and Services’ jobs (2.6% of total US employment) and greener industries are projected to experience greater job growth than less green industries.(138,140) Negative impacts of climate change are expected in other traditional industries such as agriculture and fishing, potentially leading to contraction of the workforce or modification of work practices.(141–143) Changes in the industry distributions of employment opportunities as industries experience climate change related disruption, expansion, or adaptation might lead to exposure to traditional hazards in new occupations and/or industries (e.g. slips, trips and falls, musculoskeletal disorders, chemical exposures), or the emergence of previously unidentified hazards. The transition period might be associated with job insecurity, job loss, economic migration, and additional training needs, as workers and employers adapt to the new economic environment.
Renewable Energy
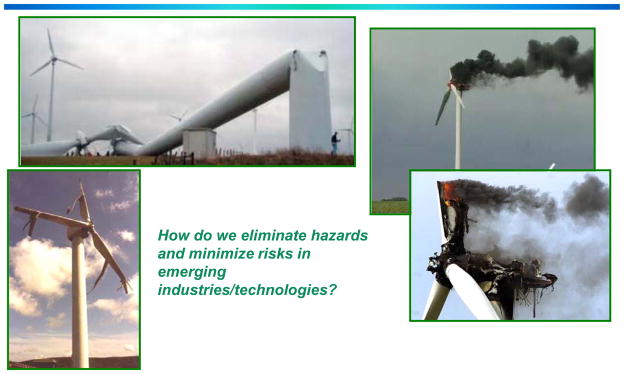
In the U.S., solar and wind energy production have seen rapid growth, as has biofuel production, and hydropower continues to contribute substantially to overall electrical energy generation.(144) While it has been suggested that renewable energy production may result in fewer occupational injuries and fatalities than fossil fuel extraction and processing, each type of renewable energy production process presents unique occupational hazards in the construction, operation, and maintenance of the facilities (Figure 2). (138) (145) Research on worker safety, particularly long-term occupational health effects, in renewable energy industries is limited. Worker safety standards and activities are often based on experience from other industries that are assumed to have similar hazards.(144) It has also been noted that as some alternative energy production industries, such as biofuel production, grow without clear and specific health and safety standards in place, workers may be exposed to unnecessary hazards.(146.147)
FIGURE 2.
Illustration that new “green” technologies, such as wind energy production, are not hazard free(199)
Recycling
One of the potential responses to climate change is an increase in recycling which may reduce energy needs. In 2013, over 87 million tons of municipal solid waste was recycled or composted in the US, which the US Environmental Protection Agency estimates as resulting in an annual reduction of more than 186 million tons of carbon dioxide equivalent emissions — comparable to removing the emissions from over 39 million passenger vehicles from the road for a year.(148) Although the environmental benefits of recycling (also known as materials recovery) are clear, recycling workers are exposed to a wide variety of occupational hazards. In the US during 2011–2013 there were 17 occupational fatalities among workers in materials recovery facilities. The rate of non-fatal injury in materials recovery facility workers in 2012 was 8.5 per 100 workers, compared with 5.1 per 100 for all waste management and remediation services workers, and 3.5 per 100 for all industries.(149) Specific hazards that have been identified include: acute injury in recycling center workers;(150) elevated exposures to heavy metals, polybrominated diphenyl ethers, and flame retardants in electronic waste recycling workers;(151–154) an increase in symptoms likely related to organic dust exposure in industrial composting facility workers;(158) and, exposure to biological agents in recycling of domestic waste including plastics, textiles and paper products.(153) Research to assess the occupational hazards in the recycling industry is often limited by the lack of sufficiently detailed data to separate recycling workers from other waste management workers.(150)
Tracking the occupational injuries and illnesses associated with climate change related industrial transition, emerging industries, and the growth of ‘green jobs’ is needed so more detailed research can be planned. To appropriately safeguard workers, research is needed to: better understand where it is reasonable to apply existing knowledge and safety standards in emerging industries; identify previously unrecognized hazards associated with new technologies and emerging industries; develop safer materials for ‘green’ product construction; and assess the need for new hazardous substance exposure limits. Rapid growth and extensive construction in emerging industries also provides an opportunity to encourage the incorporation of Prevention through Design (PtD) principles to design out worker hazards in facility construction and technology development.(156)
Changes in the Built Environment
Climate change has implications for the built environment and the workers involved with it. Climate change resulting in sealed buildings will continue to affect exposure to air pollutants in buildings that include by-products of combustion, radon, and volatile and semi-volatile organic compounds and biological organisms such as mold.(157,158) Since 2008, the literature has introduced new topics and ideas related to occupational safety and health risks due to changes in the built environment including the green building movement. Studies have shown that effects of climate change can be contained or even reversed with improvements to building standards and energy consumption can be reduced with building improvements.(159) Additionally, it is likely there will be increased construction of hard structures to protect many coastal areas from flooding.(160) However, ecologists are concerned that building such structures (e.g., dikes) will destroy tidal wetlands and diminish the supply of organisms in the oceans as well as eliminating wetlands’ ability to buffer storms.(161) Nevertheless, construction workers may experience new types of settings and unfamiliar hazards as demand and incentives increase to build “green buildings”. (138) The construction industry will be called upon for mitigation of a broad range of climate change problems.(158,162–165)
Programs have emerged to enhance building design to lessen the impact on the environment as well as to avoid adversely affecting the health of the occupants. For example, the Leadership in Energy and Environmental Design (LEED), developed in 2000, is a rating system that addresses environmental and building design concerns. The goal of LEED is to “make sure the performance of each building meets the environmental needs of the community as well as the building, itself, maintaining a more eco-friendly design” (http://leedcert.com/, accessed March 28, 2015). Buildings receive credits for criteria such as location near public transit and energy efficiency. The higher the number of credits, the more sustainable the building is considered. The LEED rating system was established by the U.S. Green Building Council (http://www.usgbc.org/leed, accessed, October 1, 2015). NIOSH successfully recommended the inclusion of worker protection standards in the LEED criteria such as improved indoor air quality, fall protection, and safe access for maintenance workers and others. Building on LEED, workers can be protected through all stages of the building life by considering Life Cycle Safety. Life Cycle Safety addresses the safety and health of workers who may be at risk during construction, maintenance, and ultimately demolition of the building (http://www.cdc.gov/niosh/topics/greenconstruction/pdfs/lifecyclesafety2.pdf, accessed March 28, 2015). Other aspects of the built environment include such activities as urban and landscape design. No literature was found indicating climate-related hazards to workers beyond what might be seen in construction, forestry, and landscaping.
ADDITIONAL CONSIDERATIONS
Mental Health Effects of Climate-Related Occupational Hazards
Although this topic was identified in the initial framework,(2) there continues to be an absence of literature on the mental health effects of climate change in workers.(166) However, the link between extreme weather disasters such as floods, forest fires, heat waves, cyclones, and extreme anxiety reactions such as post-traumatic stress disorder is well established.(167.168) Climate change may present acute and chronic stressors that may have severe mental health effects.(166) Also, direct and indirect effects of climate change on mental health have been hypothesized.(166.168,169) Workers may also be subject to the mental health effects of climate change in general; these may interact with work-related hazards. For example, workers in a drought area may have combined psychological stress from the weather in general as well as from psychological effects of heat exposure in their jobs.(20,72) Or the loss of workers’ homes and property in floods could affect a worker’s ability to concentrate and do work tasks safely. Long periods of high temperatures, heat, and drought put significant stress on communities that will be felt by workers in their jobs. Moreover, the loss of work capacity due to increasing heat exposure and the resulting loss of income is likely to cause mental health stresses in some workers.(18,20)
Economic Burden of Climate-Related Occupational Safety and Health Hazards
Literature on economic costs or losses related to the exposure of workers to climate changing conditions is limited but provides some useful observations. Individual, local, national, and regional economic productivity may be affected by workers slowing down and reducing their physical exertion in an attempt to prevent heat-related illness.(14) For example, Hsiang(170) illustrated that in 28 Caribbean-basin countries, the response of economic output to increased temperatures is structurally similar to the response of labor productivity to high temperatures. The study also specified that the similarity among such factors as the influence of temperature and tropical cyclones is mostly neglected in economic models predicting impacts of climate change.(170)
Similarly, Kjellstrom(171) found that in Southeast Asia about 15% to 20% of annual work hours may be lost in heat-exposed jobs, which may double by 2050 because of global climate change. Also, the annual cost of reduced labor productivity due to climate change at country level in 2030 can be several percent of gross domestic product, accounting for billions of United States dollars for medium-size countries.(171)
Some investigators have attempted to model the economic burden of diseases associated with climate change, including the economic effects of climate change on the working population. Some of these studies developed quantitative models to predict effects of different climate conditions in the future.(198,172,173) These models also address the integration of climate change adaptation into public health practice to increase future resilience and the associated economic evaluations.(12,198,172,173)
Although researchers have demonstrated the importance of the economic impact of reduced labor productivity because of limited work hours imposed to reduce exposures to excessive heat, few studies provide a comprehensive picture of the different economic issues related to these exposures. Additionally, there is little published research on the efficacy of interventions to reduce risks and hence economic costs of exposures of workers to the climate changing conditions. More research is needed to produce the comprehensive data to estimate the economic burden.
Geoengineering and the Potential for Worker Hazards
Geoengineering, also referred to as “climate intervention” or “climate engineering,” is defined as the intentional large-scale human manipulation of the environment.(174) It is increasingly mentioned as a way to artificially cool the planet as the threshold for CO2-induced irreversible climate change approaches. Geoengineering, generally based upon predictive models, is a highly controversial topic. A recent National Academy of Sciences report states that no climate interventions are substitutes for cutting emissions of CO2 and greenhouse gases.(174,175)
Some potential positive benefits of geoengineering such as cooling of the planet that would reduce the adverse human health impacts of excessive heat, flooding, droughts, influenza, malaria, etc. that result in high rates of global morbidity and mortality may be possible. However, the predictive models have indicated that a number of adverse effects associated with carbon capture storage and/or solar radiation management geoengineering could occur.(176–181) The Ocean Studies Board reports concluded that “there is significant potential for unanticipated, unimaginable, and regrettable consequences in multiple human dimensions from climate change modification”.(174,175) The extent to which geoengineering would create hazards and risks for workers is unknown. One way to begin to address potential worker hazards is to develop scenarios for geoengineering and identify job tasks that would be included in those scenarios and the hazards that might arise. Hazard and operability studies, fault-tree analyses, and other risk assessment methods can be used for this purpose.
PRIORITIES FOR ACTION
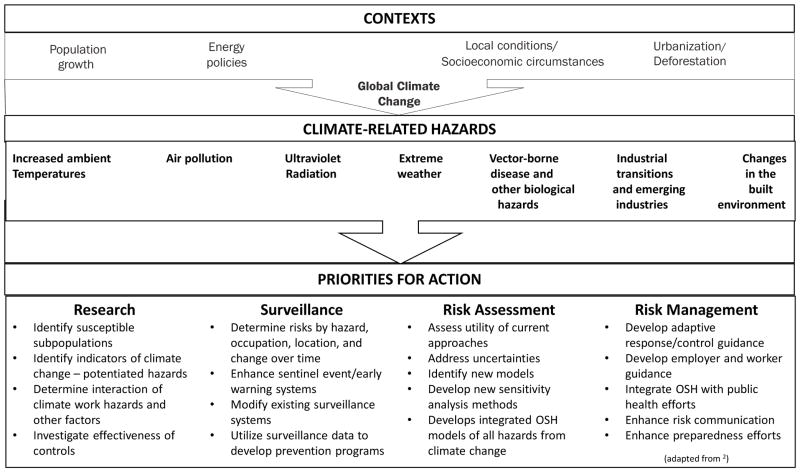
Based on a synthesis of all the information available for each of the climate-related hazards described above, four priority areas for action were identified for the occupational safety and health community to help protect workers from climate-related hazards. Figure 3 illustrates the climatic-related hazards and corresponding priorities for action: research, surveillance, risk assessment, and risk management policy.
FIGURE 3.
Priorities for action to address climate-related occupational safety and health hazards
Research
Research is needed to increase the knowledge of climate change effects on workers and improve the options for an effective occupational safety and health response. Table 1 shows specific research needs in each of these categories for the specific climate-related hazards. The following steps may assist with identifying occupational safety and health research priorities.
TABLE 1.
Framework for Climate Change and Occupational Safety and Health
| Research Needs
| ||||
|---|---|---|---|---|
| Climate-related Occupational Hazards | Research | Surveillance | Risk Assessment | Risk Management |
|
| ||||
| Increased ambient temperature |
|
|
|
|
| Air pollution |
|
|
|
|
| Ultraviolet radiation |
|
|
|
|
| Extreme weather |
|
|
|
|
| Vector-borne disease and other biological hazards1 |
|
|
|
|
| Industrial transitions and emerging industries |
|
|
|
|
| Changes in the built environment2 |
|
|
|
|
Name modified to include other biological hazards
Includes geoengineering
Identify the most vulnerable workers. Changes in the environment could result in increased prevalence of heat stress, respiratory, and cardiovascular disease among certain worker populations. Outdoor workers are often the first to be exposed to the effects of climate change and are affected by temperature extremes and disease vectors for long durations and at high intensity. Extreme weather events can also put emergency, rescue, and clean-up workers in situations involving exposure to hazardous agents as well as physical and psychological risks.(2) Multidisciplinary research (atmospheric science, occupational and environmental health, epidemiology, geography, medicine, emergency preparedness, and other fields) will help quantify and forecast workers at risk by hazard, occupation, and geographic location.
Identify indicators of climate change effects on workers. Indicators of occupational health status and well-being may help identify potential emerging issues and assist in determining priorities for the prevention of work-related injuries and illnesses.(182,183) Economic and other indicators relevant to climate change and occupational safety and health studied by Kjellstrom et al.(19) may be useful to measure the burden of occupational injury and illness and drive future research activities.
Determine interactions between climate, work hazards and other factors. Assessing the interactions of climate, occupational hazards, and worker vulnerability is an important new area of research. To adequately understand the combined impact of environmental factors on workers’ health requires the collaboration and expertise of researchers in atmospheric science, environmental health, epidemiology, psychology, medicine, and other fields.(184)
Investigate the effectiveness of mitigation strategies and hazard controls. Controls developed and implemented to reduce the likelihood or impact of adverse worker health outcomes potentially associated with climate change should be systematically investigated and evaluated to determine if they are effective and practical mechanisms for reducing climate change related worker safety and health hazards. The need to design and evaluate PPE for use in high heat and humidity and in extreme weather events is critical.
Surveillance
Surveillance is important in identifying and prioritizing occupational safety and health hazards related to climate-change, establishing research priorities, targeting interventions, and evaluating implemented interventions and other prevention strategies to reduce work related morbidity and mortality associated with climate change events.
Determine risk by hazard, occupation, and location. The impact on occupational safety and health of climate change events such as extreme weather differs from one geographic location to another and involve factors such as local ecology, geography, water supply, worker population, and primary work activities.(185,186) If appropriately designed and implemented, surveillance activities can assist with identifying climate change related hazards by occupation and location, and can guide prevention and intervention efforts to reduce occupational morbidity and mortality.
Enhance sentinel event/early warning systems. Early warning systems use environmental and public health data to identify and forecast regional health risks. For example, environmental variables have been used to predict outbreaks of malaria in Botswana.(187) Early warning and sentinel surveillance systems can assist with identifying, predicting, and assessing trends regarding work-related injury and illness, exposures, and other hazards. Few if any current surveillance systems can directly detect climate-related occupational illness or monitor a report, or respond to users.(1) For example, the incidence of occupational heat-related illness in the United States is not known.(11)
Modify existing surveillance systems. Analysis of the National Center for Health Statistics’ Compressed Mortality File showed that between 1979 and 2004, extreme cold or heat accounted for 75% of climate-related deaths. These deaths may be more preventable than those caused by earth movements, floods, and storms.(188) Existing surveillance systems could possibly be modified to incorporate leading and lagging indicators, non-temperature related climate hazards (e.g., disease vectors, air pollution), reliable tracking, and health data collection systems to assist with monitoring for increased morbidity and mortality among workers associated with climate change.(189)
Risk Assessment
The following steps may assist with ensuring occupational safety and health hazard and risk assessment activities are considered and incorporated into climate change action plans.
Identify new models. The utility of current approaches to risk assessment are likely useful for climate change models but this should be assessed. Meanwhile new forecasting and risk assessment models that integrate occupational safety and health and climate data are needed to evaluate the vulnerability of health care, public health, and emergency responder systems, and to conduct workforce health impact assessments. Programs such as the Chicago Extreme Weather Operations Plan can serve as a model for activating and coordinating a response to climate-related hazards.(188)
Consider uncertainties. Risk assessment involves decision-making when there are uncertainties and limited data. One source of uncertainty pertains to factors that result in variability of response to climate-related hazards. Some of these susceptibility factors include: age, immunologic status, physical condition, use of prescription drugs, degree of acclimatization, and genetics. Sensitivity analyses should be conducted utilizing these and other variables. Ultimately, risk assessment will involve the extent to which workers are exposed to climate-related hazards given these various sources of variability.
Risk Management and Policy Development
Research, surveillance and risk assessment activities can inform climate change risk management programs and policy development. The following steps can help ensure that risk management programs and policies incorporate occupational safety and health.
Develop adaptive response/control guidance. Since climate change presents new occupational hazards and exposures, public health and occupational safety and health professionals must adapt and respond to the issues as they emerge.(67) For example, the knowledge about the specific occupational safety and health hazards encountered in green jobs has significant gaps. If hazards unique to green jobs are identified, effective prevention campaigns, such as Prevention through Design, can be implemented as technology is developed.(156)
Develop employer and worker guidance. In the United States, employers are responsible, to the extent possible, for providing workplaces free of recognized hazards and mitigating risk to workers from hazards that cannot be eliminated. However, as Roelofs and Wegman(1) noted, “Employers may not be sufficiently prepared, empowered, educated, concerned, or compelled to protect their employees from the health impacts of climate change.” Most hazards of climate change are known and the means to protect the workforce are known as well (2, 13, 19, 28, 58, 68, 116). Worker guidance and educational materials are also needed to allow workers to protect themselves and advocate for employer action.
Incorporate consideration of worker risks into planning. For the most part, hazard prevention programs for the workforce have not been a specific part of any state’s climate-change action plan. Occupational safety and health should be considered a core component of any public health climate change plan. Occupational safety and health professionals should be part of the planning process and play an important role in preparing for conditions that may affect public health and in communicating the need for climate change policies that address occupational safety and health to policymakers and the public.
Integrate occupational safety and health with public health efforts. Climate change is an issue where the health concerns of workers and the public at large clearly intersect. The health and productivity of the workforce reflects the health of the general population. Climate change is an issue for workers, not only because they can be affected in their current workplace, but also because the people who are expected to be responsible for first response and recovery are workers and volunteers. Climate change models must be scaled to identify vulnerable areas and populations, locally and regionally, and identify and address vulnerable worker subpopulations.
Improve risk communication. Enhancing integration of climate action networks with health communication and surveillance tools is a requirement for effective risk communication. For example, in an effort to reduce heat-related events, the Occupational Safety and Health Administration partnered with the National Oceanic and Atmospheric Administration on weather service alerts that incorporate worker safety precautions and worker safety information (https://www.osha.gov/SLTC/heatillness/index.html).
Enhance preparedness efforts. Anticipating hazards and future risks to workers is the basis for preparation to prevent or minimize them. Preparedness also requires assessment of capacity for developing and implementing prevention, mitigation, adaptation, and resilience programs for workers.(190–193) These efforts may require working with state and local health and labor departments. Preparedness related to workers should have outdoor workers as a primary focus. To enhance preparedness, increased awareness among authorities, decision-makers, occupational safety and health practitioners, employers and workers about climate-related hazards to workers is needed. An Executive Order 13514 on sustainability performance goals issued in 2009 (and since revoked) is one example of an attempt to raise this awareness at the Federal level.(191)
Next Steps
The recent scientific literature indicates that climate change is presenting and will continue to present occupational safety and health hazards to workers. The information available about each of the climate-related hazards has grown, leading to the identification of new priorities for action. However, numerous critical questions still need to be resolved regarding specific hazards, appropriate sentinel events, risk assessment, and preventive actions. Additional surveillance, research, and risk assessment activities are needed to better characterize and understand how occupational safety and health may be associated with climate change events. Nonetheless, useful prevention actions can be taken while these characterization activities are carried out.
Integrating climate change and occupational health information into a comprehensive adaptation planning process may yield the largest health improvements and savings.(194,195) Tools to enable this include checklists for scenarios involving increased prevalence, severity, or distribution of occupational safety and health hazards; inventories and maps of resources, capacity and vulnerability; partnerships between decision makers and occupational safety and health resource groups; and regional or national symposia to discuss strategies and identify collaborative opportunities. This updated framework and priorities for action provide additional tools to assist the occupational safety and health and public health communities to protect workers from potential hazards and adverse impacts.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.Roelofs C, Wegman D. Workers: the Climate Canaries. Am J Publ Health. 2014;104(10):1799–1801. doi: 10.2105/AJPH.2014.302145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schulte PA, Chun H. Climate change and occupational safety and health: establishing a preliminary framework. J Occup Environ Hyg. 2009;6(9):542–554. doi: 10.1080/15459620903066008. [DOI] [PubMed] [Google Scholar]
- 3.Portier C. A Human Health Perspective on Climate Change: A Report Outlining the Research Needs on the Human Health Effects of Climate Change. 22 April 2010. Research Triangle Park, NC: Environmental Health Perspectives/National Institute of Environmental Health Sciences; 2010. [Google Scholar]
- 4.Garfin G, Jardine A, Merideth R, Black M, LeRoy S. Assessment of Climate Change in the Southwest United States: A Report Prepared for the National Climate Assessment. NCA Regional Input Reports. 2013 [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];World Health Day – Vector-Borne Diseases. 2014a Available at http://www.cdc.gov/features/worldhealthday2014/
- 6.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Climate change and occupational safety and health. 2014b Available at http://www.cdc.gov/niosh/topics/climate/default.html.
- 7.Melillo JM, Richmond T, Yohe GW. Climate change impacts in the United States: the third national climate assessment. US Global Change Research Program. 2014;841 [Google Scholar]
- 8.Smith K, Woodward A, Campbell-Lendrum D, Chadee D, Honda Y, LQ, et al. Human health: impacts, adaptation, and co-benefits. In: FCB, Barros V, Dokken D, Mach K, Mastrandrea M, Bilir T, Chatterjee M, Ebi K, Estrada Y, Genova R, Girma B, Kissel E, Levy A, MacCracken S, Mastrandrea P, White L, editors. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom, and New York, NY: Cambridge University Press; 2014. pp. 709–754. [Google Scholar]
- 9.Centers for Disease Control Prevention. Heat-related deaths among crop workers--United States, 1992--2006. MMWR. 2008;57(24):649–653. [PubMed] [Google Scholar]
- 10.IPCC Climate Change. "The Physical Science Basis. [accessed September 22, 2015];Working Group I Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. 2013 Available at http://www.ipcc.ch/report/ar5/wg1/
- 11.Gubernot DM, Anderson GB, Hunting KL. The epidemiology of occupational heat exposure in the United States: a review of the literature and assessment of research needs in a changing climate. Int J Biometeorol. 2014;58(8):1779–1788. doi: 10.1007/s00484-013-0752-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunne JP, Stouffer RJ, John JG. Reductions in labour capacity from heat stress under climate warming. Nat Clim Chang. 2013;3(6):563–566. [Google Scholar]
- 13.Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009;51(1):33–37. doi: 10.1097/JOM.0b013e318193e12e. [DOI] [PubMed] [Google Scholar]
- 14.Lundgren K, Kuklane K, Gao C, Holmér I. Effects of heat stress on working populations when facing climate change. Indust Health. 2013;51(1):3–15. doi: 10.2486/indhealth.2012-0089. [DOI] [PubMed] [Google Scholar]
- 15.Nilsson M, Kjellstrom T. Climate change impacts on working people: how to develop prevention policies. Global Health Action. 2010;3 doi: 10.3402/gha.v3403i3400.5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fortune MK, Mustard CA, Etches JJ, Chambers AG. Work-attributed Illness Arising From Excess Heat Exposure in Ontario, 2004–2010. Can J Public Health. 2013;104(5):e420–e426. doi: 10.17269/cjph.104.3984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacklitsch B, Williams W, Musolin K, Turner N, Coca A, Kim J-H, editors. National Institute for Occupational Safety and Health (NIOSH) Criteria for a recommended standard: Occupational exposure to heat and hot environments. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2016. [Google Scholar]
- 18.Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle-income countries. Global Health Action. 2009;2(1):1–3. doi: 10.3402/gha.v2i0.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kjellstrom T, Kovats RS, Lloyd SJ, Holt T, Tol RS. The direct impact of climate change on regional labor productivity. Arch Environ Occup Health. 2009;64(4):217–227. doi: 10.1080/19338240903352776. [DOI] [PubMed] [Google Scholar]
- 20.Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. 2010;55(2):123–132. doi: 10.1007/s00038-009-0112-0. [DOI] [PubMed] [Google Scholar]
- 21.Kjellstrom T, Butler AJ, Lucas RM, Bonita R. Public health impact of global heating due to climate change: potential effects on chronic non–communicable diseases. Int J Public Health. 2010;55(2):97–103. doi: 10.1007/s00038-009-0090-2. [DOI] [PubMed] [Google Scholar]
- 22.Tawatsupa B, Lim LL, Kjellstrom T, Seubsman S-a, Sleigh A T.C.S. Team. The association between overall health, psychological distress, and occupational heat stress among a large national cohort of 40,913 Thai workers. Global Health Action. 2010;3 doi: 10.3402/gha.v3i0.5034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McMichael AJ. Globalization, climate change, and human health. N Engl J Med. 2013;369(1):96. doi: 10.1056/NEJMc1305749. [DOI] [PubMed] [Google Scholar]
- 24.Hanna EG, Kjellstrom T, Bennett C, Dear K. Climate change and rising heat: Population health implications for working people in Australia. Asia Pac J Public Health. 2011;23(2 Suppl):14S–26S. doi: 10.1177/1010539510391457. [DOI] [PubMed] [Google Scholar]
- 25.Leon LR. Thermoregulatory responses to environmental toxicants: The interaction of thermal stress and toxicant exposure. Toxicol Appl Pharmacol. 2008;233(1):146–161. doi: 10.1016/j.taap.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 26.Gordon CJ. Role of environmental stress in the physiological response to chemical toxicants. Environ Res. 2003;92(1):1–7. doi: 10.1016/s0013-9351(02)00008-7. [DOI] [PubMed] [Google Scholar]
- 27.Katsouyanni K, Pantazopoulou A, Touloumi G, Tselepidaki I, Moustris K, Asimakopoulos D, et al. Evidence for interaction between air pollution and high temperature in the causation of excess mortality. Arch Environ Health. 1993;48(4):235–242. doi: 10.1080/00039896.1993.9940365. [DOI] [PubMed] [Google Scholar]
- 28.Bourbonnais R, Zayed J, Levesque M, Busque MA, Duguay P, Truchon G. Identification of workers exposed concomitantly to heat stress and chemicals. Ind Health. 2013;51(1):25–33. doi: 10.2486/indhealth.2012-0095. [DOI] [PubMed] [Google Scholar]
- 29.Leithead CS, Lind AR. Heat Stress and Heat Disorders. Philadelphia, PA: F.A. Davis Company; 1964. [Google Scholar]
- 30.ISO. Hot environments-Estimation of heat stress on working man, based on the WBGT-index (wet bulb globe temperature) Geneva: International Standards Organization; 1989. (ISO 7243) [Google Scholar]
- 31.American Conference of Governmental Industrial Hygienists (ACGIH) 1985 [Google Scholar]
- 32.National Institute for Occupational Safety and Health (NIOSH) Revised criteria 1986. C. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 1986. Criteria for a recommended standard: Occupational exposure to hot environments. [Google Scholar]
- 33.Occupational Safety and Health Administration (OSHA) OSHA Directive TED 01-00-015 (TED 1-OSH) Washington, DC: US Department of Labor; 1998. OSHA Technical Manual. [Google Scholar]
- 34.Fiala D, Havenith G, Bröde P, Kampmann B, Jendritzky G. UTCI-Fiala multi-node model of human heat transfer and temperature regulation. Int J Biometeorol. 2012;56(3):429–441. doi: 10.1007/s00484-011-0424-7. [DOI] [PubMed] [Google Scholar]
- 35.Jendritzky G, de Dear R, Havenith G. UTCI—Why another thermal index? Int J Biometeorol. 2012;56(3):421–428. doi: 10.1007/s00484-011-0513-7. [DOI] [PubMed] [Google Scholar]
- 36.Kinney PL. Climate change, air quality, and human health. Am J Prev Med. 2008;35(5):459–467. doi: 10.1016/j.amepre.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 37.US Environmental Protection Agency (EPA) Assessment of the impacts of global change on regional US air quality: a synthesis of climate change impacts on ground-level ozone. Research Triangle Park, NC: Office of Research and Development, National Center for Environmental Assessment; 2009. [Google Scholar]
- 38.Tibbetts J. Air quality and climate change: a delicate balance. Environ Health Perspect. 2015;123(6):A148–153. doi: 10.1289/ehp.123-A148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dedoussi IC, Barrett SR. Air pollution and early deaths in the United States. Part II: Attribution of PM 2.5 exposure to emissions species, time, location and sector. Atmospher Environ. 2014;99:610–617. [Google Scholar]
- 40.Cattaneo A, Taronna M, Consonni D, Angius S, Costamagna P, Cavallo DM. Personal exposure of traffic police officers to particulate matter, carbon monoxide, and benzene in the city of Milan, Italy. J Occup Environ Hyg. 2010;7(6):342–351. doi: 10.1080/15459621003729966. [DOI] [PubMed] [Google Scholar]
- 41.Chiarelli PS, Pereira LAA, do Nascimento Saldiva PH, Ferreira Filho C, Garcia MLB, Braga ALF, et al. The association between air pollution and blood pressure in traffic controllers in Santo André, São Paulo, Brazil. Environ Res. 2011;111(5):650–655. doi: 10.1016/j.envres.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 42.Tomei F, Ciarrocca M, Rosati M, Casale T, Di Pastena C, Nieto H, et al. Relationship between occupational exposure to cadmium, transaminases and γ-GT in workers exposed to urban stressors. Ann Ig. 2012;25(4):353–363. doi: 10.7416/ai.2013.1937. [DOI] [PubMed] [Google Scholar]
- 43.Adetona O, Dunn K, Hall DB, Achtemeier G, Stock A, Naeher LP. Personal PM2. 5 exposure among wildland firefighters working at prescribed forest burns in southeastern United States. J Occup Environ Hyg. 2011;8(8):503–511. doi: 10.1080/15459624.2011.595257. [DOI] [PubMed] [Google Scholar]
- 44.McNamara ML, Semmens EO, Gaskill S, Palmer C, Noonan CW, Ward TJ. Base camp personnel exposure to particulate matter during wildland fire suppression activities. J Occup Environ Hyg. 2012;9(3):149–156. doi: 10.1080/15459624.2011.652934. [DOI] [PubMed] [Google Scholar]
- 45.Fayard GM. Fatal work injuries involving natural disasters, 1992–2006. Disaster Med Public Health Prep. 2009;3(04):201–209. doi: 10.1097/DMP.0b013e3181b65895. [DOI] [PubMed] [Google Scholar]
- 46.Williamson CE, Zepp RG, Lucas RM, Madronich S, Austin AT, Ballaré CL, et al. Solar ultraviolet radiation in a changing climate. Nat Climate Change. 2014;4(6):434–441. [Google Scholar]
- 47.Bais A, Tourpali K, Kazantzidis A, Akiyoshi H, Bekki S, Braesicke P, et al. Projections of UV radiation changes in the 21st century: impact of ozone recovery and cloud effects. Atmos Chem Phys. 2011;11(15):7533–7545. [Google Scholar]
- 48.Arctic Climate Impact Assessment (ACIA) Impacts of a Warming Arctic-Arctic Climate Impact Assessment, by Arctic Climate Impact Assessment. 2004 Vol. 1. Cambridge, UK: Cambridge University Press; Dec, 2004. p. 144. [Google Scholar]
- 49.World Meterological Organization (WMO); Global Ozone Research and Monitoring Project, editor. 1998 WMO Ozone Report 44. Geneva, Switzerland: 1999. Scientific assessment of ozone depletion: 1998. [Google Scholar]
- 50.McKenzie LM, Witter RZ, Newman LS, Adgate JL. Human health risk assessment of air emissions from development of unconventional natural gas resources. Sci Total Environ. 2012;424:79–87. doi: 10.1016/j.scitotenv.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 51.Jaggernath J, Haslam D, Naidoo KS. Climate change: Impact of increased ultraviolet radiation and water changes on eye health. Health. 2013;5(05):921. [Google Scholar]
- 52.World Health Organization. Artificial tanning sunbeds: risks and guidance. World Health Organization; 2003. [Google Scholar]
- 53.Hammer GP, Blettner M, Zeeb H. Epidemiological studies of cancer in aircrew. Radiat Prot Dosimetry. 2009;136:232–239. doi: 10.1093/rpd/ncp125. [DOI] [PubMed] [Google Scholar]
- 54.D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV Radiation and the Skin. Int J Mol Sci. 2013;14(6):12222–12248. doi: 10.3390/ijms140612222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reinau D, Weiss M, Meier C, Diepgen T, Surber C. Outdoor workers’ sun-related knowledge, attitudes and protective behaviours: a systematic review of cross-sectional and interventional studies. Br J Dermatol. 2013;168(5):928–940. doi: 10.1111/bjd.12160. [DOI] [PubMed] [Google Scholar]
- 56.Chorley A, Higlett M, Baczynska K, Hunter R, Khazova M. Measurements of Pilots’ Occupational Solar UV Exposure. Photochem Photobiol. 2014;90(4):935–940. doi: 10.1111/php.12269. [DOI] [PubMed] [Google Scholar]
- 57.Kozma B, Eide MJ. Photocarcinogenesis: An Epidemiologic Perspective on Ultraviolet Light and Skin Cancer. Dermatol Clin. 2014;32(3):301–313. doi: 10.1016/j.det.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 58.IPCC Climate Change. [accessed September 21, 2015];Managing the risks of extreme events and disasters to advance climate change adaption. 2012 doi: 10.1136/jech-2012-201045. Available at https://www.ipcc.ch/pdf/special-reports/srex/SREX_Full_Report.pdf. [DOI] [PubMed]
- 59.Bender MA, Knutson TR, Tuleya RE, Sirutis JJ, Vecchi GA, Garner ST, et al. Modeled impact of anthropogenic warming on the frequency of intense Atlantic hurricanes. Science. 2010;327(5964):454–458. doi: 10.1126/science.1180568. [DOI] [PubMed] [Google Scholar]
- 60.Done JM, Holland GJ, Bruyère CL, Leung LR, Suzuki-Parker A. Modeling high-impact weather and climate: lessons from a tropical cyclone perspective. Clim Change. 2013;129(3–4):381–395. [Google Scholar]
- 61.Holland G, Bruyère CL. Recent intense hurricane response to global climate change. Clim Dyn. 2014;42(3–4):617–627. [Google Scholar]
- 62.Westerling A, Brown T, Schoennagel T, Swetnam T, Turner M, Veblen T. Briefing: Climate and wildfire in western US forests. 2014 [Google Scholar]
- 63.Romps DM, Seeley JT, Vollaro D, Molinari J. Projected increase in lightning strikes in the United States due to global warming. Science. 2014;346(6211):851–854. doi: 10.1126/science.1259100. [DOI] [PubMed] [Google Scholar]
- 64.Jensenius JS., Jr [accessed September 21, 2015];A detailed analysis of lightning deaths in the United States from 2006 through 2013. 2015 Available at http://www.lightningsafety.noaa.gov/resources/RecentLightningDeaths.pdf.
- 65.Levin M. Peril in the West - After three decades, officials ponder action on cancer-causing erionite. 2011 Available at http://www.fairwarning.org/2011/10/peril-in-the-west/
- 66.Weissman D, Keifer M. National Institute for Occupational Safety and Health; [accessed September 21, 2015]. 2011. Erionite–an emerging North American hazard. NIOSH Science Blog. Available at http://blogs.cdc.gov/niosh-science-blog/2011/11/erionite. [Google Scholar]
- 67.Adam-Poupart A, Labr, Egrave, Che F, Smargiassi A, Duguay P, et al. Climate Change and Occupational Health and Safety in a Temperate Climate: Potential Impacts and Research Priorities in Quebec, Canada. Indust Health. 2013;51(1):68–78. doi: 10.2486/indhealth.2012-0100. [DOI] [PubMed] [Google Scholar]
- 68.McMichael AJ, Lindgren E. Climate change: present and future risks to health, and necessary responses. J Intern Med. 2011;270(5):401–413. doi: 10.1111/j.1365-2796.2011.02415.x. [DOI] [PubMed] [Google Scholar]
- 69.The Royal Society. [accessed September 21, 2015];Resilience to Extreme Weather. 2014 Available at https://royalsociety.org/topics-policy/projects/resilience-extreme-weather/
- 70.Lafferty KD. The ecology of climate change and infectious diseases. Ecol. 2009;90(4):888–900. doi: 10.1890/08-0079.1. [DOI] [PubMed] [Google Scholar]
- 71.Russell RC. Mosquito-borne disease and climate change in Australia: time for a reality check. Aust J Entomol. 2009;48(1):1–7. [Google Scholar]
- 72.Bennett CM, McMichael AJ. Non-heat related impacts of climate change on working populations. Global Health Action. 2010;3 doi: 10.3402/gha.v3i0.5640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Epstein P. The ecology of climate change and infectious diseases: comment. Ecol. 2010;91(3):925–928. doi: 10.1890/09-0761.1. [DOI] [PubMed] [Google Scholar]
- 74.Shuman EK. Global climate change and infectious diseases. N Engl J Med. 2010;362(12):1061–1063. doi: 10.1056/NEJMp0912931. [DOI] [PubMed] [Google Scholar]
- 75.Mills JN, Gage KL, Khan AS. Potential influence of climate change on vector-borne and zoonotic diseases: a review and proposed research plan. Environ Health Perspect. 2010;118(1):1507–1514. doi: 10.1289/ehp.0901389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tabachnick W. Challenges in predicting climate and environmental effects on vector-borne disease episystems in a changing world. J Exp Biol. 2010;213(6):946–954. doi: 10.1242/jeb.037564. [DOI] [PubMed] [Google Scholar]
- 77.Semenza JC, Suk JE, Estevez V, Ebi KL, Lindgren E. Mapping climate change vulnerabilities to infectious diseases in Europe. Environ Health Perspect. 2012;120(3):385. doi: 10.1289/ehp.1103805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McGregor GR. Human biometeorology. Prog Phys Geogr. 2012;36(1):93–109. [Google Scholar]
- 79.European Centre for Disease Prevention and Control. Assessing the potential impacts of climate change on food- and waterborne diseases in Europe. Stockholm: ECDC; 2012. [Google Scholar]
- 80.US Environmental Protection Agency (EPA) Climate Change Indicators in the United States, 2014. 2014 [Online] Available at www.epa.gov/climatechange/indicators.
- 81.Institute of Medicine (IOM) The influence of global environmental change on infectious disease dynamics. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 82.Luber G, Knowlton K, Balbus JM, Frumkin H, Hayden M, Hess JJ, et al. Ch.9: Human Health. In: Melillo Jerry M, Richmond TC, Yohe GW, editors. Climate Change Impacts in the United States: The Third National Climate Assessment. US Global Change Research Program; 2014. pp. 220–256. [Google Scholar]
- 83.Patz JA, Frumkin H, Holloway T, Vimont DJ, Haines A. Climate change: challenges and opportunities for global health. JAMA. 2014;312(15):1565–1580. doi: 10.1001/jama.2014.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Parham PE, Waldock J, Christophides GK, Michael E. Climate change and vector-borne diseases of humans. Philos Trans R Soc Lond B Biol Sci. 2015;370(1665) doi: 10.1098/rstb.2014.0377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Insects and Scorpions. 2012a Available at http://www.cdc.gov/niosh/topics/insects/
- 86.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Tick-Borne Diseases. 2012b Available at http://www.cdc.gov/niosh/topics/tick-borne/
- 87.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Poisinous Plants. 2012c Available at http://www.cdc.gov/niosh/topics/plants/
- 88.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Venomous Spiders. 2012d Available at http://www.cdc.gov/niosh/topics/spiders/
- 89.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Valley Fever (Coccidioidomycosis) 2014c Available at http://www.cdc.gov/fungal/diseases/coccidioidomycosis/index.html.
- 90.Cozzetto K, Nania J, Gillette N. Human Health. In: Jania J, Cozzetto J, editors. Considerations for climate change and variability adaptation on the Navajo Nation. Boulder, CO: 2014. [Google Scholar]
- 91.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Venomous Snakes. 2012e Available at http://www.cdc.gov/niosh/topics/snakes/
- 92.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];West Nile Virus. 2015 Available at http://www.cdc.gov/westnile/index.html/
- 93.Rosenthal J. Climate change and the geographic distribution of infectious diseases. Ecohealth. 2009;6(4):489–495. doi: 10.1007/s10393-010-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Degallier N, Favier C, Menkes C, Lengaigne M, Ramalho WM, Souza R, et al. Toward an early warning system for dengue prevention: modeling climate impact on dengue transmission. Clim Change. 2010;98(3–4):581–592. [Google Scholar]
- 95.Moore SM, Eisen RJ, Monaghan A, Mead P. Meteorological influences on the seasonality of Lyme disease in the United States. J Trop Med Hyg. 2014;90(3):486–496. doi: 10.4269/ajtmh.13-0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Levy S. Warming trend: how climate shapes Vibrio ecology. Environ Health Perspect. 2015;123(4):A82. doi: 10.1289/ehp.123-A82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Monaghan AJ, Moore SM, Sampson KM, Beard CB, Eisen RJ. Climate change influences on the annual onset of Lyme disease in the United States. Ticks and Tick-borne Dis. 2015;6:615–622. doi: 10.1016/j.ttbdis.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Danielová V, Schwarzová L, Materna J, Daniel M, Metelka L, Holubová J, et al. Tick-borne encephalitis virus expansion to higher altitudes correlated with climate warming. Internat J Med Microbio. 2008;298:68–72. [Google Scholar]
- 99.Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H. The emergence of Lyme disease in Canada. Can Med Assoc J. 2009;180(12):1221–1224. doi: 10.1503/cmaj.080148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Lyme Disease. 2011 Available at http://www.cdc.gov/niosh/topics/lyme/
- 101.Colón-González FJ, Fezzi C, Lake IR, Hunter PR. The effects of weather and climate change on dengue. PLoS Negl Trop Dis. 2013;7(11):e2503. doi: 10.1371/journal.pntd.0002503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.World Health Organization (WHO) [accessed November 12, 2015];Impact of Dengue. 2013 Available at www.who.int/csr/disease/dengue/impact/en/
- 103.Yamana TK, Eltahir EA. Projected impacts of climate change on environmental suitability for malaria transmission in West Africa. Environ Health Perspect. 2013;121(10):1179–1186. doi: 10.1289/ehp.1206174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ogden NH, Radojevic M, Wu X, Duvvuri VR, Leighton PA, Wu J. Estimated effects of projected climate change on the basic reproductive number of the Lyme disease vector Ixodes scapularis. Environ Health Perspect. 2014;122(6):631–638. doi: 10.1289/ehp.1307799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Siraj A, Santos-Vega M, Bouma M, Yadeta D, Carrascal DR, Pascual M. Altitudinal changes in malaria incidence in highlands of Ethiopia and Colombia. Science. 2014;343(6175):1154–1158. doi: 10.1126/science.1244325. [DOI] [PubMed] [Google Scholar]
- 106.Ostfeld RS, Brunner JL. Climate change and Ixodes tick-borne diseases of humans. Philos Trans R Soc Lond B Biol Sci. 2015;370(1665):20140051. doi: 10.1098/rstb.2014.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Staples JE, Breiman RF, Powers AM. Chikungunya fever: an epidemiological review of a re-emerging infectious disease. Clin Infect Dis. 2009;49(6):942–948. doi: 10.1086/605496. [DOI] [PubMed] [Google Scholar]
- 108.NIOSH Mosquito-borne disease web page.
- 109.Kuehn BM. Chikungunya virus transmission found in the United States: US health authorities brace for wider spread. JAMA. 2014;312(8):776–777. doi: 10.1001/jama.2014.9916. [DOI] [PubMed] [Google Scholar]
- 110.Morens DM, Fauci AS. Chikungunya at the door—Déjà vu all over again? N Engl J Med. 2014;371(10):885–887. doi: 10.1056/NEJMp1408509. [DOI] [PubMed] [Google Scholar]
- 111.Weaver S. Arrival of chikungunya virus in the new world: prospects for spread and impact on public health. PLoS Neglected Tropical Diseases. 2014;8(6):e2921–e2921. doi: 10.1371/journal.pntd.0002921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bowen GS, Schulze TL, Hayne C, Parkin WE. A Focus Of Lyme Disease In Monmoutei County, New Jersey. Am J Epidemiol. 1984;120(3):387–394. doi: 10.1093/oxfordjournals.aje.a113903. [DOI] [PubMed] [Google Scholar]
- 113.Goldstein MD, Schwartz BS, Friedmann C, Maccarillo B, Borbi M, Tuccillo R. Lyme disease in New Jersey outdoor workers: a statewide survey of seroprevalence and tick exposure. Am J Public Health. 1990;80(10):1225–1229. doi: 10.2105/ajph.80.10.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Schwartz BS, Goldstein MD. Lyme disease in outdoor workers: risk factors, preventive measures, and tick removal methods. Am J Epidemiol. 1990;131(5):877–885. doi: 10.1093/oxfordjournals.aje.a115578. [DOI] [PubMed] [Google Scholar]
- 115.Kugeler KJ, Farley GM, Forrester JD, Mead PS. Geographic distribution and expansion of human Lyme disease, United States. Emerg Infect Dis. 2015;21:1455–1457. doi: 10.3201/eid2108.141878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.National Institute for Occupational Safety and Health (NIOSH) NIOSH fast facts: Protecting yourself from ticks and mosquitoes. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2010. pp. NIOSH Publication No. 2010–2119. [Google Scholar]
- 117.Morin CW, Comrie AC. Regional and seasonal response of a West Nile virus vector to climate change. Proc Natl Acad Sci. 2013;110(39):15620–15625. doi: 10.1073/pnas.1307135110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Paz S. Climate change impacts on West Nile virus transmission in a global context. Philosophical Transactions of the Royal Society of London B: Biolog Sci. 2015;370(1665):20130561. doi: 10.1098/rstb.2013.0561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cummings K, McDowell A, Wheeler C, McNary J, Das R, Vugia D, et al. Point-source outbreak of coccidioidomycosis in construction workers. Epidemiol Infect. 2010;138(04):507–511. doi: 10.1017/S0950268809990999. [DOI] [PubMed] [Google Scholar]
- 120.Tsang CA, Anderson SM, Imholte SB, Erhart LM, Chen S, Park BJ, et al. Enhanced surveillance of coccidioidomycosis, Arizona, USA, 2007–2008. Emerg Infect Dis. 2010;16(11):1738. doi: 10.3201/eid1611.100475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.California Correctional Health Care Services (CCHCS) California Correctional Health Care Services. 2012. Public health and quality management units. Coccidioidomycosis in California’s adult prisons 2006–2010. [Google Scholar]
- 122.Das R, McNary J, Fitzsimmons K, Dobraca D, Cummings K, Mohle-Boetani J, et al. Occupational coccidioidomycosis in California: outbreak investigation, respirator recommendations, and surveillance findings. J Occup Environ Med. 2012;54(5):564–571. doi: 10.1097/JOM.0b013e3182480556. [DOI] [PubMed] [Google Scholar]
- 123.Brown J, Benedict K, Park BJ, Thompson GR., III Coccidioidomycosis: epidemiology. Clin Epidemiol. 2013;5:185. doi: 10.2147/CLEP.S34434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Centers for Disease Control Prevention (CDC) Increase in reported coccidioidomycosis--United States, 1998–2011. MMWR. 2013;62(12):217. [PMC free article] [PubMed] [Google Scholar]
- 125.California Department of Public Health (CDPH) [accessed November 10, 2015];Preventing work-related coccidioidomycosis (valley fever) 2013 Available at http://www.cdph.ca.gov/programs/ohb/pages/cocci.aspx.
- 126.Nguyen C, Barker BM, Hoover S, Nix DE, Ampel NM, Frelinger JA, et al. Recent advances in our understanding of the environmental, epidemiological, immunological, and clinical dimensions of coccidioidomycosis. Clin Microbiol Rev. 2013;26(3):505–525. doi: 10.1128/CMR.00005-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sondermeyer G, Lee L, Gilliss D, Tabnak F, Vugia D. Coccidioidomycosis-associated hospitalizations, California, USA, 2000–2011. Emerg Infect Dis. 2013;19(10):1590–1597. doi: 10.3201/eid1910.130427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Centers for Disease Control and Prevention (CDC) Coccidioidomycosis among cast and crew members at an outdoor television filming event--California. MMWR. 2014d;63(15):321–324. [PMC free article] [PubMed] [Google Scholar]
- 129.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Coccidioidomycosis (Valley Fever) 2014e Available at http://www.cdc.gov/niosh/topics/valleyfever/default.html.
- 130.de Perio MA, Burr GA, editors. National Institute for Occupational Safety and Health (NIOSH) Hazard evaluation and technical assistance report: Evaluation of Coccidioides Exposures and Coccidioidomycosis Infections among Prison Employees. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2014. [Google Scholar]
- 131.Hu W, Mengersen K, Fu SY, Tong S. The use of ZIP and CART to model cryptosporidiosis in relation to climatic variables. Int J Biometeorol. 2010;54(4):433–440. doi: 10.1007/s00484-009-0294-4. [DOI] [PubMed] [Google Scholar]
- 132.Gregory PJ, Johnson SN, Newton AC, Ingram JS. Integrating pests and pathogens into the climate change/food security debate. J Exp Bot. 2009;60(10):2827–2838. doi: 10.1093/jxb/erp080. [DOI] [PubMed] [Google Scholar]
- 133.Koleva NG, Schneider UA. The impact of climate change on the external cost of pesticide applications in US agriculture. Int J Agricul Sustain. 2009;7(3):203–216. [Google Scholar]
- 134.McDonald A, Riha S, DiTommaso A, DeGaetano A. Climate change and the geography of weed damage: analysis of US maize systems suggests the potential for significant range transformations. Agric Ecosyst Environ. 2009;130(3):131–140. [Google Scholar]
- 135.Chakraborty S, Newton AC. Climate change, plant diseases and food security: an overview. Plant Pathol. 2011;60(1):2–14. [Google Scholar]
- 136.Bentz BJ. [accessed September 21, 2015];Western US bark beetles and climate change. 2008 Available at http://www.fs.fed.us/ccrc/topics/bark-beetles.shtml.
- 137.Hart SJ, Schoennagel T, Veblen TT, Chapman TB. Area burned in the western United States is unaffected by recent mountain pine beetle outbreaks. Proc Natl Acad Sci. 2015;112(14):4375–4380. doi: 10.1073/pnas.1424037112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Pollack E. Economic Policy Institute. 2012. Counting up to green: assessing the green economy and its implications for growth and equity. [Google Scholar]
- 139.Schulte PA, Heidel D, Okun A, Branche C. Making green jobs safe. Indust Health. 2010;48(4):377–379. doi: 10.2486/indhealth.ms4804ed. [DOI] [PubMed] [Google Scholar]
- 140.Bureau of Labor Statistics (BLS) [accessed September 22, 2015];GGS News, Green Goods and Services. 2013 Available at http://www.bls.gov/ggs/#news.
- 141.Hatfield J, Takle G, Grotjahn R, Holden P, Izaurralde RC, Mader T, Marshall E, Liverman D. Agriculture. Climate Change Impacts in the United States. The Third National Climate Assessment. In: Melillo JM, Richmond Terese TC, Yohe GW, editors. US Global Change Research Program. 2014. pp. 150–174. [Google Scholar]
- 142.Malcolm S, Marshall E, Aillery M, Heisey P, Livingston M, Day-Rubenstein K. Agricultural adaptation to a changing climate: economic and environmental implications vary by US region. USDA-ERS Economic Research Report. 2012;(136) [Google Scholar]
- 143.Shelton C. Fisheries and Aquaculture Circular No. 1088. Rome: FAO; 2014. Climate change adaptation in fisheries and aquaculture–compilation of initial examples; p. 34. [Google Scholar]
- 144.Mulloy KB, Sumner SA, Rose C, Conway GA, Reynolds SJ, Davidson ME, et al. Renewable energy and occupational health and safety research directions: A white paper from the Energy Summit, Denver Colorado, April 11–13, 2011. Am J Indust Med. 2013;56(11):1359–1370. doi: 10.1002/ajim.22184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sumner SA, Layde PM. Expansion of renewable energy industries and implications for occupational health. JAMA. 2009;302(7):787–789. doi: 10.1001/jama.2009.1214. [DOI] [PubMed] [Google Scholar]
- 146.Law BF, Pearce T, Siegel PD. Case Study: Safety and Chemical Exposure Evaluation at a Small Biodiesel Production Facility. J Occup Environ Hyg. 2011;8(7):D68–D72. doi: 10.1080/15459624.2011.584841. [DOI] [PubMed] [Google Scholar]
- 147.Travis N. Breathing easier? The known impacts of biodiesel on air quality. Biofuels. 2012;3(3):285–291. doi: 10.4155/bfs.12.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.US Environmental Protection Agency (EPA) [accessed September 22, 2015];Advancing Sustainable Materials Management: Facts and Figures 2013. 2015 Available at http://www.epa.gov/epawaste/nonhaz/municipal/pubs/2013_advncng_smm_rpt.pdf.
- 149.Graham T, Tessler J, Orris P, Shimek J, Wilson M, Witt H. [accessed September 22, 2015];Sustainable and safe recycling: protecting workers who protect the planet. 2015 Available at http://www.coshnetwork.org/sites/default/files/SafeRecyclingReport.pdf.
- 150.Engkvist IL, Svensson R, Eklund J. Reported occupational injuries at Swedish recycling centres–based on official statistics. Ergonomics. 2011;54(4):357–366. doi: 10.1080/00140139.2011.556261. [DOI] [PubMed] [Google Scholar]
- 151.Schecter A, Colacino JA, Harris TR, Shah N, Brummitt SI. A newly recognized occupational hazard for US electronic recycling facility workers: polybrominated diphenyl ethers. J Occup Environ Med. 2009;51(4):435–440. doi: 10.1097/JOM.0b013e31819b8c09. [DOI] [PubMed] [Google Scholar]
- 152.Tsydenova O, Bengtsson M. Chemical hazards associated with treatment of waste electrical and electronic equipment. Waste Manag. 2011;31(1):45–58. doi: 10.1016/j.wasman.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 153.Hebisch R, Linsel G. Workers exposure to hazardous substances and biological agents in recycling enterprises. Arbeitsplatzbelastung. 2012;72(4):163–169. [Google Scholar]
- 154.Julander A, Lundgren L, Skare L, Grandér M, Palm B, Vahter M, et al. Formal recycling of e-waste leads to increased exposure to toxic metals: An occupational exposure study from Sweden. Environ Int. 2014;73:243–251. doi: 10.1016/j.envint.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 155.Hambach R, Droste J, François G, Weyler J, Van Soom U, De Schryver A, et al. Work-related health symptoms among compost facility workers: a cross-sectional study. Arch Public Health. 2012;70(13):0778–0736. doi: 10.1186/0778-7367-70-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Schulte PA, Rinehart R, Okun A, Geraci CL, Heidel DS. National Prevention through Design (PtD) Initiative. J Saf Res. 2008;39(2):115–121. doi: 10.1016/j.jsr.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 157.Institute of Medicine (IOM) Climate Change, the Indoor Environment, and Health. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 158.Spengler J. Climate Change and Indoor Environments. Epidemiol. 2011;22(1):S143–S144. [Google Scholar]
- 159.Chow DHC. The potential impact of climate change on heating and cooling loads for office buildings in the Yangtze River Delta. Int J Low-Carbon Technol. 2012;7(3):234–247. [Google Scholar]
- 160.Hinkel J, Lincke D, Vafeidis AT, Perrette M, Nicholls RJ, Tol RS, et al. Coastal flood damage and adaptation costs under 21st century sea-level rise. Proc Natl Acad Sci. 2014;111(9):3292–3297. doi: 10.1073/pnas.1222469111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mattheus CR, Rodriguez AB, McKee BA, Currin CA. Impact of land-use change and hard structures on the evolution of fringing marsh shorelines. Estuarine, Coastal and Shelf Sci. 2010;88(3):365–376. [Google Scholar]
- 162.Stone B, Hess JJ, Frumkin H. Urban form and extreme heat events: Are sprawling cities more vulnerable to climate change than compact cities? Environ Health Perspect. 2010;118(10):1425–1428. doi: 10.1289/ehp.0901879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Mallick FH, Mourshed M. Adapting buildings to climate change. Open House International. 2012;37(4):14–18. [Google Scholar]
- 164.Hrabovszky-Horváth S, Pálvölgyi T, Csoknyai T, Talamon A. Generalized residential building typology for urban climate change mitigation and adaptation strategies: The case of Hungary. Energy Build. 2013;62:475–485. [Google Scholar]
- 165.Talamon A. Adapting building sector to climate change: The case of Hungary. IYCE 2013 - 4th International Youth Conference on Energy; 2013. [Google Scholar]
- 166.Clayton S, Manning C, Hodge C. Beyond storms & droughts: The psychological impacts of climate change. Washington, DC: American Psychological Association and ecoAmerica; 2014. [Google Scholar]
- 167.Salcioglu E, Basoglu M, Livanou M. Post-traumatic stress disorder and comorbid depression among survivors of the 1999 earthquake in Turkey. Disasters. 2007;31(2):115–129. doi: 10.1111/j.1467-7717.2007.01000.x. [DOI] [PubMed] [Google Scholar]
- 168.Berry HL, Kelly BJ, Hanigan IC, Coates JH, McMichael AJ, Welsh JA, et al. Commissioned report for the Garnaut Climate Change Review. Canberra: The Australian National University; 2008. Rural mental health impacts of climate change. [Google Scholar]
- 169.Fritze JG, Blashki GA, Burke S, Wiseman J. International Journal of Mental Health Systems. Int J Ment Health Syst. 2008;2:13. doi: 10.1186/1752-4458-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Hsiang SM. Temperatures and cyclones strongly associated with economic production in the Caribbean and Central America. Proc Natl Acad Sci. 2010;107(35):15367–15372. doi: 10.1073/pnas.1009510107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Kjellstrom T. Impact of Climate Conditions on Occupational Health and Related Economic Losses A New Feature of Global and Urban Health in the Context of Climate Change. Asia Pac J Public Health. 2015 doi: 10.1177/1010539514568711. 1010539514568711. [DOI] [PubMed] [Google Scholar]
- 172.Grasso M, Manera M, Chiabai A, Markandya A. The health effects of climate change: A survey of recent quantitative research. Int J Environ Res Public Health. 2012;9(5):1523–1547. doi: 10.3390/ijerph9051523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Huang C, Barnett AG, Xu Z, Chu C, Wang X, Turner LR, et al. Managing the health effects of temperature in response to climate change: challenges ahead. Environ Health Perspect. 2013;121(4):415. doi: 10.1289/ehp.1206025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ocean Studies Board. Climate Intervention:: Carbon Dioxide Removal and Reliable Sequestration. Washington, DC: National Academies Press; 2015a. [Google Scholar]
- 175.Ocean Studies Board. Climate intervention: Reflecting sunlight to cool the earth. Washington, DC: National Academies Press; 2015b. [Google Scholar]
- 176.Lenton TM, Vaughan NE. The radiative forcing potential of different climate geoengineering options. Atmos Chem Phys. 2009;9(15):5539–5561. [Google Scholar]
- 177.Robock A, Marquardt A, Kravitz B, Stenchikov G. Benefits, risks, and costs of stratospheric geoengineering. Geophys Res Lett. 2009;36(19) [Google Scholar]
- 178.Buck JH. Geoengineering: Re-making Climate for Profit or Humanitarian Intervention? Dev Change. 2012;43(1):253–270. doi: 10.1111/j.1467-7660.2011.01744.x. [DOI] [PubMed] [Google Scholar]
- 179.Schmidt H, Alterskjær K, Bou Karam D, Boucher O, Jones A, Kristjánsson J, et al. Solar irradiance reduction to counteract radiative forcing from a quadrupling of CO2: climate responses simulated by four earth system models. Earth System Dynamics. 2012;3:63–78. [Google Scholar]
- 180.Caldeira K, Bala G, Cao L. The science of geoengineering. Annu Rev Earth Planet Sci. 2013;41:231–256. [Google Scholar]
- 181.Robock A. Stratospheric Aerosol Geoengineering. Geoengineering of the Climate System. 2014;38:162. [Google Scholar]
- 182.Thomsen C, McClain J, Rosenman K, Davis L. Indicators for occupational health surveillance. MMWR Recomm Rep. 2007:1–7. [PubMed] [Google Scholar]
- 183.Arbury S, Jacklitsch B, Farquah O, Hodgson M, Lamson G, Martin H, et al. Heat illness and death among workers — United States, 2012–2013. MMWR. 2014;(31):661–665. [PMC free article] [PubMed] [Google Scholar]
- 184.Spector JT, Sheffield PE. Re-evaluating Occupational Heat Stress in a Changing Climate. Ann Occup Hyg. 2014;58(8):936–942. doi: 10.1093/annhyg/meu073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Zhang Y, Bi P, Hiller J. Climate change and disability-adjusted life years. J Environ Health. 2007;70(3):32–36. [PubMed] [Google Scholar]
- 186.Crider KG, Maples EH, Gohlke JM. Incorporating occupational risk in heat stress vulnerability mapping. J Environ Health. 2014;77(1):16–22. [PMC free article] [PubMed] [Google Scholar]
- 187.American Public Health Association. Climate Change: Mastering the Public Health Role: a Practical Guidebook. Washington, DC: American Public Health Association; 2011. [Google Scholar]
- 188.Thacker MT, Lee R, Sabogal RI, Henderson A. Overview of deaths associated with natural events, United States, 1979–2004. Disasters. 2008;32(2):303–315. doi: 10.1111/j.1467-7717.2008.01041.x. [DOI] [PubMed] [Google Scholar]
- 189.Wilson ML, Anker M. 10 Disease surveillance in the context of climate stressors: needs and opportunities. In: Ebi KL, Smith J, Ian Burton, editors. Integration of Public Health with Adaptation to Climate Change: Lessons Learned and New Directions. London: Taylor & Francis; 2005. pp. 191–214. [Google Scholar]; Ebi KL, Burton I. Identifying practical adaptation options: an approach to address climate change-related health risks. Environ Sci Policy. 2008;11(4):359–369. [Google Scholar]
- 190.Hess JJ, Schramm PJ, Luber G. Public health and climate change adaptation at the federal level: one agency’s response to executive order 13514. Am J Public Health. 2014;104(3):e22–e30. doi: 10.2105/AJPH.2013.301796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Manangan AP, Uejio CK, Saha S, Schramm PJ, Marinucci GD, Brown CL, et al. Climate health Technical Report Series. Atlanta, GA: Centers for Disease Control and Prevention; 2014. Assessing Health Vulnerability to Climate Change. [Google Scholar]
- 192.Schramm PJ, Uejio CK, Hess JJ, Marinucci GD, Luber G. Climate Models and the Use of Climate Projections. 2014. [Google Scholar]
- 193.Letcher TM. Climate change: observed impacts on planet Earth. Amsterdam; Boston: Elsevier; 2009. [Google Scholar]
- 194.Bloom AJ. Global climate change: Convergence of disciplines. University of California at Davis: Sinauer Associates; 2010. [Google Scholar]
- 195.Centers for Disease Control and Prevention (CDC) [accessed August 31, 2015];Chikungunya virus. 2014f Available at http://www.cdc.gov/chikungunya/
- 196.Chorley AC, Evans BJ, Benwell MJ. Civilian pilot exposure to ultraviolet and blue light and pilot use of sunglasses. Aviat Space Environ Med. 2011;82(9):895–900. doi: 10.3357/asem.3034.2011. [DOI] [PubMed] [Google Scholar]
- 197.NYDOH. [accessed September 22, 2015];Fact sheet for outdoor workers: West Nile Virus Information. 2013 Available at http://www.health.ny.gov/publications/2742/
- 198.Kjellstrom T, Lemke B, Otto M, Hyatt O, Briggs D, Freyberg C. Climate Change and increasing heat impacts on labor productivity. 2015. [Google Scholar]
- 199.Heidel DS. Prevention through Design Making Green Jobs Safe. Presentation to ORC Worldwide Western OSH Meeting; June 19, 2008.Dana Point, California: ORC Worldwide; [Google Scholar]
- 200.Massey N. [accessed September 21, 2015];Colorado fire follows in pine beetles and climate change. 2012 Available at http://www.scientificamerican.com/article/colorado-fire-follows-pine-beetles-tracks/