Abstract
Parents/caregivers require specialized education in order to care for their child with a newly diagnosed cancer. Currently, no evidence-based guidelines exist to identify content essential for inclusion in patient/family education prior to a child’s initial discharge home; this study used Delphi methodology to obtain multidisciplinary consensus regarding essential content amongst pediatric oncology experts from the Children’s Oncology Group. Three questionnaire rounds were employed to identify essential content, evaluate the importance of the educational topics identified, and gain expert consensus regarding the final ranking of topics identified and whether or not each topic was considered mandatory for inclusion in education for newly diagnosed patients. Disease-specific topics were also identified for patients with leukemia, solid tumors and CNS tumors. The results of this study provide, for the first time, multidisciplinary expert consensus regarding key content essential for inclusion in discharge education for newly diagnosed pediatric oncology patients.
Keywords: Delphi study, childhood cancer, educating families, Children’s Oncology Group
Introduction
Parents/caregivers of newly diagnosed pediatric oncology patients require specialized education (patient/family education) in order to provide ongoing care for these children at home (Kelly & Porock, 2005; Pyke-Grimm, Degner, Small, & Mueller, 1999). This education typically includes information about the child’s diagnosis and treatment (Kelly & Porock, 2005), and may require parents/caregivers to master new and challenging cognitive and technical skills, such as central line care, management of complex home medication regimens, and ongoing assessment for potential life-threatening complications that require immediate medical intervention (Aburn & Gott, 2011; Kelly & Porock, 2005). Currently, there are no evidence-based guidelines to inform the selection of essential content for inclusion in education provided to parents/caregivers of newly diagnosed pediatric oncology patients. As a result, there is a lack of standardization across institutions (Withycombe et al., 2016), resulting in considerable variability in the content included in teaching for newly diagnosed patients (Slone, Self, Friedman, & Heiman, 2014). This study addresses variability in educational content provided to newly diagnosed families across COG institutions, by employing Delphi methodology (Hasson, Keeney, & McKenna, 2000; Jones & Hunter, 1995) to attain consensus from a multidisciplinary panel of pediatric oncology experts from the Children’s Oncology Group (COG). We aimed to identify essential informational content for inclusion in parent/caregiver education at the time of an initial pediatric cancer diagnosis, and to determine which topics are mandatory to promote safe care at home following the initial hospital discharge. Topics of importance specific to the three primary subtypes of childhood cancer (leukemia/lymphoma, solid tumors and central nervous system [CNS] tumors) were also identified.
Methods
Delphi methodology utilizes a group facilitation technique involving multistage processes designed to transform expert opinion into group consensus (Dalkey & Helmer, 1963; Jones & Hunter, 1995). Group consensus-building is established through the solicited opinions of experts who are given a series of carefully designed questionnaires. Once the expert opinions are collected, the method employs multiple iterations in which responses are summarized and redistributed to the expert panel to develop consensus concerning a specific topic. During the final iteration, the items achieving consensus in previous rounds are reviewed by the panel and rankings are finalized. Thus, the Delphi method is suitable for exploring topics for which there is limited evidence available (Hasson et al., 2000), and where lack of clarity exists (Iqbal & Pipon-Young, 2009).
This Delphi study employed three questionnaire rounds to gain expert consensus. Participant identifiers were not obtained, ensuring anonymity of all those who completed the study questionnaires. The study was submitted to the Duke University Institutional Review Board (IRB) and determined to be exempt from further review.
Delphi Round 1
The purpose of Round 1 of the Delphi study was to generate the essential content to be reviewed in subsequent rounds. Participants in Round 1 consisted of pediatric oncology professionals and patient advocates who attended a two-hour session focused on patient/family education held in September 2014 during the annual COG meeting in Dallas, Texas. This session featured a panel of pediatric oncology clinical experts (nurses, physicians, psychologists), and patient advocates who were asked a series of three questions related to educating parents/caregivers of newly diagnosed patients (Table 1). All session participants, including panel members, were invited to complete written questionnaires containing the same questions that were addressed by the expert panel during the session. All responses to the Round 1 questionnaires were completed in free-text in order to generate a wide range of initial ideas. Questionnaire completion was voluntary; no identifiers were collected except for professional role (e.g., nurse, physician, parent). Those who chose to complete a questionnaire placed it in a box at the back of the room after the session.
Table 1.
Delphi Round 1 – Questionnaire Items and Number of Responses and Categories
| Questionnaire Item | Initial # of Responses (Free-Text, Raw Data) | Initial # of Categories (Assigned by Working Group) | Final # of Categories (Assigned by Research Team) |
|---|---|---|---|
| 1. What are the five most important topics, in order of importance, which should be discussed with newly diagnosed pediatric oncology patients and families before discharge from the hospital? | 494 | 57 | 20 |
| 2. What specific content within the topics listed above must be covered before the child is discharged from the hospital? | 389 | 49 | 20 |
| 3. Are there specific topics that are related to the child’s diagnosis that should be included in discussions prior to hospital discharge? If so, what are these topics? A. Leukemia/lymphoma |
164 |
42 |
8 |
| B. Solid tumor | 163 | 44 | 7 |
| C. CNS Tumor | 202 | 55 | 12 |
A working group within the research team initially collated, reviewed, and categorized all questionnaire responses. The entire research team then reviewed the raw response data along with the associated categories assigned by the working group, identified similar and duplicate topics, and collapsed these topics into comparable categories. Through an iterative process, the research team reached consensus regarding categorization and generated a final list of 20 topics important in the education of all newly diagnosed patients for inclusion in Round 2. Additionally, important diagnosis-specific topics were identified for patients with leukemia/lymphoma (8 topics), solid tumors (7 topics) and CNS tumors (12 topics).
Delphi Rounds 2 and 3
For Delphi Rounds 2 and 3, 60 pediatric oncology clinicians from the Children’s Oncology Group were selected to comprise the expert panel for this Delphi study. Potential panelists were nominated by the research team, and selection was based on professional role, expertise in specific disease areas, and representation from various sizes/types of institutions across COG. Selected panelists included physicians, nurses, and behavioral scientists who had relevant expertise in pediatric leukemia/lymphoma, solid tumors, and/or CNS tumors and represented small (<75 new patients per year, on average), medium (75–149 new patients per year), and large (>150 new patients per year) COG institutions that were free-standing children’s hospitals, community hospitals, and academic programs. Expert panel members received a link to Rounds 2 and 3 of the Delphi survey via email and were invited to complete each of the electronic surveys online.
Round 2
The purpose of Round 2 was to have the expert panel evaluate the importance of educational topics identified during Round 1. A 5-item survey was administered to expert panel members, who were asked to rate each of the 20 topics on a 7-point Likert scale in relation to its importance for inclusion in education for all newly diagnosed families prior to a first discharge home. Panelists were also asked to separately rate the importance of each of the additional 27 topics specific to educating families of children with leukemia/lymphoma, solid tumors, and CNS tumors. Means, standard deviations, medians, and ranges for each rating were calculated in order to further characterize the importance of each item for inclusion in the final Delphi round. Items were further curated by consensus of the research team and expert panel comments prior to proceeding to Round 3, with some low-rated items removed, and duplicative items collapsed into singular categories.
Round 3
The purpose of Round 3 was to establish expert consensus regarding the final ranking of the remaining 18 general and 23 diagnosis-specific topics from Round 2 that had been identified as important, and to determine the proportion of expert panel members that considered each topic mandatory for inclusion in education prior to a first discharge home. To facilitate consensus-building, panelists were each provided with Round 2 results so that they could gain perspective regarding their own responses in relationship to the responses of other expert panel members. A 9-item survey was then administered to panel members, in which they were asked to rank all topics in order of importance, and to indicate whether or not they believed each topic was mandatory for inclusion in education prior to the initial hospital discharge for all newly diagnosed patients. Panelists were also asked to separately rank and specify mandatory status for the additional educational topics applicable to families of children with leukemia/lymphoma, solid tumors, and CNS tumors. Rank order was determined by awarding points to each topic based on the rank position assigned by each panel member. For example, for the 18 topics considered important for all patients, 18 points were assigned for a first-place rank position, 17 points for second-place, and so on, down through 1 point assigned for a last-place rank. Overall rank order was then assigned based on mean-rank score. Descriptive statistics were used to calculate the proportion of panel members that indicated each topic should be mandatory for inclusion in initial education.
Results
Participant Characteristics
The participation rate for Round 1 was 80% (100/125); 80% of the participants were nurses, 7% psychosocial professionals, 3% patient advocates, 2% physicians, and 8% other oncology healthcare professionals. For the invited expert panel, the participation rate was 93.3% (56/60) for Round 2 and 73.3% (44/60) for Round 3. Of the experts invited, 100% of nurses (36/36), 83.3% (10/12) of physicians and 83.3% (10/12) of psychologists participated in at least one round. The clinical focus of expert panel members included leukemia/lymphoma (69.6%), solid tumors (60.7%) and CNS tumors (55.4%). The large majority of participating expert panel members (87.5%; 49/56) had more than ten years of experience in pediatric oncology.
Round 1: Identification of Important Topics for Inclusion in Discharge Education
The number of questionnaire responses obtained during Round 1, and the associated categorization of these responses, are included in Table 1. Iterative analysis of Round 1 data by the research team identified 20 topics of importance for inclusion in initial discharge education for all newly diagnosed pediatric oncology patients, as well as additional topics of importance for inclusion in discharge education for patients with leukemia/lymphoma (8 topics identified), solid tumors (7 topics), and central nervous system tumors (12 topics). The 20 topics of importance to all pediatric oncology patients (Table 2), and the additional 27 topics pertinent to the 3 diagnostic subgroups (Table 2), were subsequently used to develop the survey items administered to the expert panel in Rounds 2 and 3.
Table 2.
Results of Delphi Round 2 – Likert scale ratings of overall importance of each topic for inclusion in education prior to initial hospital discharge (0=not important at all; 7=most important)
| Topic | Mean | SD | Median | Range |
|---|---|---|---|---|
| FOR ALL NEWLY DIAGNOSED PEDIATRIC ONCOLOGY PATIENTS | ||||
| Diagnosis | 6.91 | 0.44 | 7.0 | 4–7 |
| Fever | 6.89 | 0.31 | 7.0 | 6–7 |
| Treatment plan | 6.89 | 0.45 | 7.0 | 4–7 |
| Who/how to call (e.g., days, nights, weekends) | 6.86 | 0.35 | 7.0 | 6–7 |
| When/why to call treatment team | 6.80 | 0.72 | 7.0 | 2–7 |
| Managing medications | 6.73 | 0.62 | 7.0 | 4–7 |
| Care of the child at home | 6.54 | 0.69 | 7.0 | 4–7 |
| Central line care | 6.29 | 0.91 | 7.0 | 4–7 |
| Follow-up appointments | 6.25 | 1.01 | 7.0 | 3–7 |
| Side effects of treatment | 6.20 | 0.77 | 6.0 | 4–7 |
| Preventing infection | 6.14 | 1.30 | 6.5 | 1–7 |
| Healthcare team (key members) | 5.98 | 1.00 | 6.0 | 3–7 |
| Prognosis | 5.86 | 1.31 | 6.0 | 1–7 |
| Clinical trials | 5.80 | 1.14 | 6.0 | 1–7 |
| Blood counts | 5.77 | 1.21 | 6.0 | 1–7 |
| Supportive care | 5.68 | 1.18 | 6.0 | 1–7 |
| Psychosocial issues | 5.66 | 1.13 | 6.0 | 2–7 |
| Fertility preservation options | 5.64 | 1.33 | 6.0 | 1–7 |
| School | 5.32 | 1.21 | 5.0 | 1–7 |
| Complementary therapy | 4.07 | 1.70 | 5.0 | 0–7 |
| ADDITIONAL TOPICS FOR LEUKEMIA/LYMPHOMA PATIENTS ONLY | ||||
| Medication adherence | 6.77 | 0.54 | 7.0 | 4–7 |
| Steroid side effects | 6.61 | 0.62 | 7.0 | 4–7 |
| Vincristine side effects | 6.46 | 0.63 | 7.0 | 4–7 |
| Neutropenic precautions | 6.38 | 1.11 | 7.0 | 1–7 |
| Bleeding precautions | 5.96 | 1.18 | 6.0 | 1–7 |
| Procedures | 5.79 | 1.22 | 6.0 | 1–7 |
| Anemia | 5.50 | 1.29 | 6.0 | 1–7 |
| Nutrition | 5.48 | 1.08 | 6.0 | 2–7 |
| ADDITIONAL TOPCS FOR SOLID TUMOR PATIENTS ONLY | ||||
| Post-operative/wound care | 6.43 | 0.83 | 7.0 | 4–7 |
| Pain | 6.43 | 0.87 | 7.0 | 4–7 |
| Physical limitations | 5.89 | 1.2 | 6.0 | 1–7 |
| Pegfilgrastim/G–CSF (neupogen) | 5.88 | 1.10 | 6.0 | 2–7 |
| Safety | 5.88 | 1.34 | 6.0 | 2–7 |
| Local Control: Surgery and/or radiation | 5.52 | 1.44 | 6.0 | 1–7 |
| Nutrition | 5.34 | 1.38 | 6.0 | 1–7 |
| ADDITIONAL TOPICS FOR CNS TUMOR PATIENTS ONLY | ||||
| Increased intracranial pressure | 6.48 | 1.31 | 7.0 | 0–7 |
| Seizures | 6.38 | 1.27 | 7.0 | 0–7 |
| Shunt malfunctions | 6.36 | 1.37 | 7.0 | 0–7 |
| Steroid side effects | 6.36 | 0.75 | 6.0 | 4–7 |
| Vomiting | 6.29 | 1.16 | 7.0 | 0–7 |
| Post-operative/wound care | 6.29 | 0.89 | 6.5 | 4–7 |
| Headaches | 6.18 | 0.92 | 6.0 | 4–7 |
| Safety | 6.00 | 1.47 | 7.0 | 0–7 |
| Radiation | 5.77 | 1.29 | 6.0 | 1–7 |
| Physical limitations | 5.66 | 1.21 | 6.0 | 3–7 |
| Rehabilitation | 5.57 | 1.45 | 6.0 | 1–7 |
| Cognitive limitations | 5.32 | 1.45 | 6.0 | 1–7 |
Abbreviation: SD=Standard deviation
Round 2: Rating of Overall Importance of Topics for Inclusion in Discharge Education
During Round 2, the expert panel was asked to rate the importance of 20 topics for inclusion in education for all newly diagnosed patients on a Likert scale from 0 (not important at all) to 7 (most important). The expert panel rated diagnosis, fever, and treatment plan highest (mean ratings, 6.91, 6.89, and 6.89, respectively), and school and complementary therapy lowest (mean ratings 5.32 and 4.07, respectively; Table 2); the two topics with the lowest mean scores were removed from the list prior to Round 3. Using the same Likert scale, the expert panel rated the importance of additional topics for inclusion in education for specific diagnostic subgroups, Medication adherence and steroid side effects were rated as most important for leukemia/lymphoma patients (mean ratings 6.77 and 6.61, respectively), post-operative/wound care and pain as most important for solid tumor patients (mean rating 6.43 for each), and increased intracranial pressure and seizures as most important for CNS tumor patients (mean ratings 6.48 and 6.38, respectively; Table 2). Duplicative items identified by the expert panel for the CNS tumor group were collapsed into singular categories prior to Round 3.
Round 3: Final Ranking of Overall Importance of Topics for Inclusion in Discharge Education and Determination of Recommendations for Mandatory Inclusion of Topics
Education for All Newly Diagnosed Pediatric Oncology Patients
During Round 3, the expert panel was asked to rank the 18 remaining topics from Round 2 from most to least important, for inclusion in education of all newly diagnosed pediatric oncology patients. Panelists ranked diagnosis, treatment plan, and fever as the most important topics, while fertility preservation options and psychosocial issues were ranked least important (Table 3). Panelists were then asked to indicate whether or not they considered each topic mandatory for inclusion in education prior to a first discharge home; over 90% of expert panel members identified 10 topics as mandatory, while the remaining 8 topics were identified as mandatory by 53.5% to 88.6% of panelists (Figure 1). Three topics (fever, who/how to call and when/why to call the treatment team) were considered mandatory by 100% of the expert panel members.
Table 3.
Results of Delphi Round 3 – Overall rank order of topics by importance for inclusion in education prior to initial hospital discharge
| Educational Topic | Rank Order | Mean-Rank Score |
|---|---|---|
|
TOPICS FOR ALL NEWLY DIAGNOSED PEDIATRIC ONCOLOGY PATIENTS (#1=most important; #18=least important) | ||
| Diagnosis | 1 | 16.66 |
| Treatment plan | 2 | 14.18 |
| Fever | 3 | 12.23 |
| Prognosis | 4 | 11.43 |
| Side effects of treatment | 5 | 11.32 |
| Who/how to call (e.g., days, nights, weekends) | 6 | 10.98 |
| When/why to call treatment team | 7 | 10.70 |
| Clinical trials | 8 | 9.91 |
| Managing medications | 9 | 9.34 |
| Central line care | 10 | 8.98 |
| Care of the child at home | 11 | 8.89 |
| Supportive care | 12 | 7.73 |
| Healthcare team (key members) | 12 | 7.73 |
| Preventing infection | 14 | 7.20 |
| Blood counts | 15 | 6.68 |
| Follow-up appointments | 16 | 6.45 |
| Fertility preservation options | 17 | 5.84 |
| Psychosocial issues | 18 | 4.75 |
|
ADDITIONAL TOPICS FOR LEUKEMIA/LYMPHOMA PATIENTS ONLY (#1=most important; #8=least important) | ||
| Neutropenic precautions | 1 | 6.58 |
| Medication adherence | 2 | 6.47 |
| Steroid side effects | 3 | 5.44 |
| Vincristine side effects | 4 | 4.65 |
| Bleeding precautions | 5 | 4.44 |
| Procedures | 6 | 3.72 |
| Nutrition | 7 | 2.40 |
| Anemia | 8 | 2.30 |
|
ADDITIONAL TOPICS FOR SOLID TUMOR PATIENTS ONLY (#1=most important; #7=least important) | ||
| Post-operative/wound care | 1 | 5.59 |
| Pain | 2 | 5.57 |
| Safety | 3 | 4.27 |
| Pegfilgrastim/G-CSF (neupogen) | 4 | 3.57 |
| Physical limitations | 5 | 3.48 |
| Local control: Surgery and/or radiation | 6 | 2.82 |
| Nutrition | 7 | 2.70 |
|
ADDITIONAL TOPICS FOR CNS TUMOR PATIENTS ONLY (#1=most important; #8=least important) | ||
| Increased intracranial pressure | 1 | 7.58 |
| Post-operative/wound care | 2 | 6.03 |
| Safety | 3 | 5.55 |
| Steroid side effects | 4 | 4.61 |
| Physical limitations | 5 | 3.61 |
| Radiation | 6 | 2.97 |
| Cognitive limitations | 7 | 2.92 |
| Rehabilitation | 8 | 2.74 |
Figure 1.
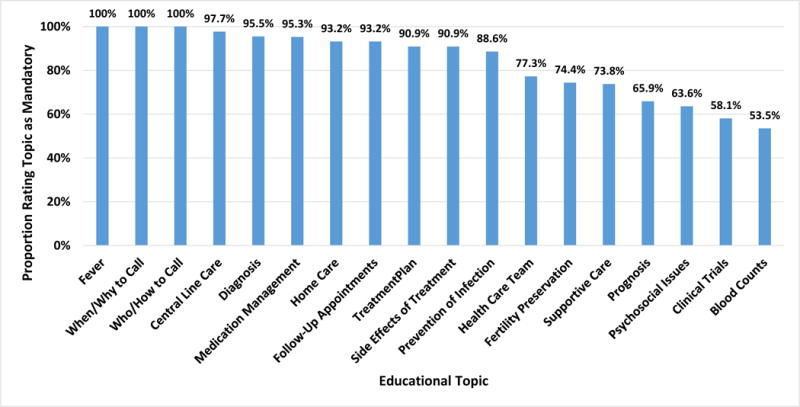
Proportion of expert panel members that considered each topic mandatory for inclusion in education for all newly diagnosed pediatric oncology patients prior to the initial hospital discharge
Education for Newly Diagnosed Leukemia/Lymphoma Patients
Expert panel members were asked to rank the importance of additional topics for inclusion in education for newly diagnosed patients with leukemia/lymphoma. Panelists ranked neutropenic precautions and medication adherence as the most important topics and nutrition and anemia as the least important (Table 3). When asked to indicate whether topics were considered mandatory for newly diagnosed leukemia/lymphoma patients, over 90% of panelists identified 4 topics (neutropenic precautions, medication adherence, bleeding precautions, and steroid side effects) as mandatory, while the remaining 4 topics (nutrition, procedures, anemia, and vincristine side effects) were identified as mandatory by 51.2% to 88.6% of the panelists (Figure 2a).
Figure 2.
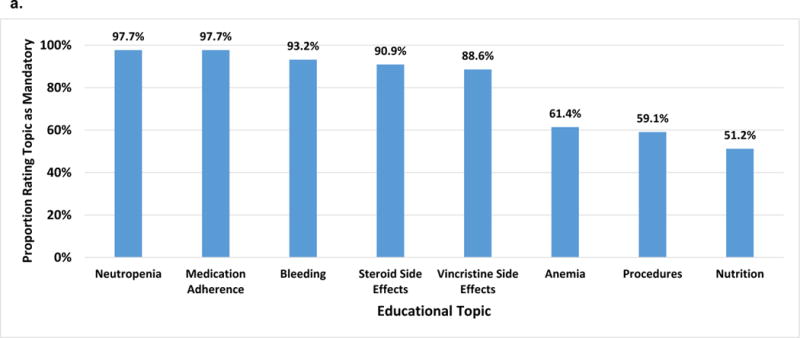
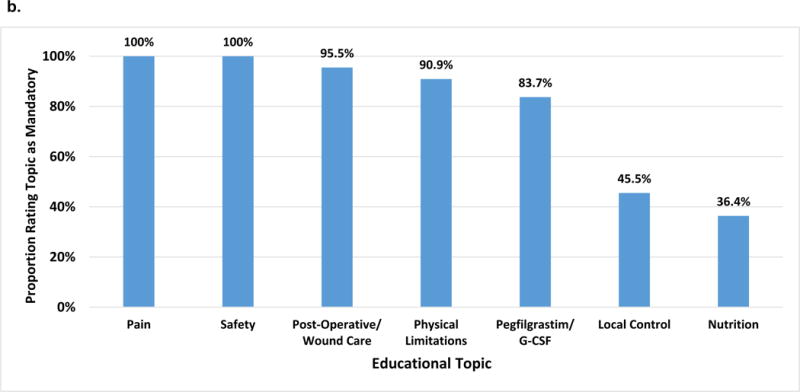
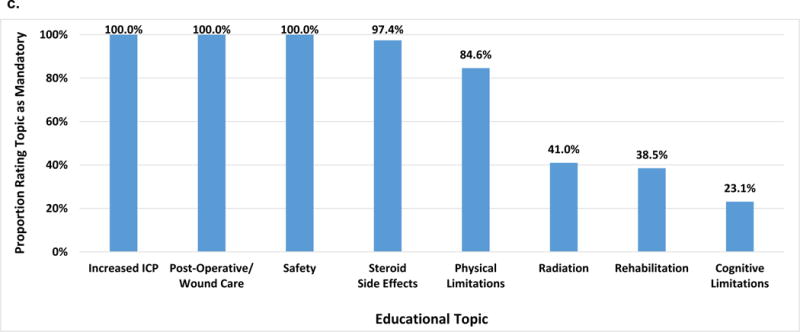
Proportion of expert panel members that considered additional topics mandatory for inclusion in education for newly diagnosed pediatric oncology patients prior to the initial hospital discharge by diagnostic group: (a) Leukemia/lymphoma; (b) Solid tumors; (c) CNS tumors
Education for Newly Diagnosed Solid Tumor Patients
Next, panelists were asked to rank the importance of topics for inclusion in education of newly diagnosed patients with solid tumors; post-operative/wound care and pain were ranked highest and local control and nutrition lowest (Table 3). Over 90% of the expert panelists identified 4 topics (pain, safety, post-operative/wound care, and physical limitations) as mandatory for inclusion in education for newly diagnosed solid tumor patients, while the remaining 3 topics (nutrition, local control, and pegfilgrastim/G-CSF) were identified as mandatory by 36.4% to 83.7% of panelists (Figure 2b). Two topics (pain and safety) were considered mandatory by 100% of the expert panel members.
Education for Newly Diagnosed CNS Tumor Patients
When asked to rank the importance of additional topics for inclusion in education of newly diagnosed patients with CNS tumors, expert panel members ranked increased intracranial pressure, postoperative/wound care and safety highest and cognitive limitations and rehabilitation lowest (Table 3); 100% of the panelists identified increased intracranial pressure, postoperative/wound care and safety as mandatory and 97.4% identified steroid side effects as mandatory, while the remaining 4 topics (cognitive limitations, rehabilitation, radiation, and physical limitations) were identified as mandatory by 23.1.1% to 84.6% of panelists (Figure 2c).
Discussion
The results of this study reflect the consensus of a multidisciplinary expert panel regarding the relative importance of topics for inclusion in discharge education for all newly diagnosed pediatric oncology patients, and additional topics for specific disease subtypes. To our knowledge, this is the first study to establish expert consensus regarding the necessary content for inclusion in discharge education of newly diagnosed pediatric oncology patients and families.
Overall, there was clear consensus among the expert panel with regard to the importance of educating newly diagnosed families about the child’s diagnosis and treatment plan, as well as fever management; these three topics received the highest mean scores in Round 2 and the highest overall rankings in Round 3. One hundred percent of the expert panelists indicated that they considered fever and accessing the treatment team (i.e., who/how to call and when/why to call) as mandatory topics for inclusion in education prior to first discharge. Over 90% of panelists agreed that seven additional topics should be considered mandatory prior to discharge. There was also strong agreement regarding additional topics necessary for inclusion in education provided to specific disease groups. One hundred percent of the expert panel members agreed that increased intracranial pressure, postoperative/wound care and safety were mandatory topics for newly diagnosed CNS tumor patients. There was also 100% agreement among the expert panel members that pain and safety were mandatory topics for newly diagnosed solid tumor patients, and 97.7% agreement that medication adherence and neutropenic precautions were mandatory topics for the leukemia and lymphoma population.
Our study identified fever as a topic of high importance for inclusion in education for all newly diagnosed pediatric oncology patients. Additionally, neutropenia was ranked highly for leukemia and lymphoma patients. Similarly, Kelly & Porock (2005) reported bone marrow suppression as the second most important teaching priority identified by pediatric oncology nurses, and Aburn & Gott (2011) cited fever and neutropenia as topics identified by parents as necessary components of education to be addressed prior to transitioning the child from hospital to home (Aburn & Gott 2011). Our study also identified diagnosis and treatment as high priority topics for inclusion in education for newly diagnosed patients. These findings are consistent with the teaching priorities identified by Kelly & Porock (2005), and findings from studies reporting the information needs of children and adolescents with leukemia (Cavusoglu, 2000), children with brain tumors (Freeman, O’Dell & Meola, 2003), and young adults with cancer (Giacalone, Blandino, Spazzapan & Tirelli, 2005). However, notable differences from a previous study examining nurses’ perceptions of parental educational needs are apparent. Kelly & Porock (2005) reported that nurses identified coping as a high-priority topic for education during the first week following diagnosis; whereas, in our study, the multidisciplinary expert panel ranked psychosocial issues of lowest importance as an educational topic to be addressed prior to the first discharge home.
Results from this study support current literature that suggests targeting educational topics by diagnosis (Kelly & Porock 2005; Aburn & Gott, 2011; Flury et al 2011; Gupta et al 2013). Topics of importance to all patients, as well as additional topics specific to each of the disease subgroups were identified by this Delphi panel. For example, post-operative wound care and pain were ranked highest for solid tumor patients, while neutropenia and medication adherence were ranked highest for newly diagnosed leukemia and lymphoma patients.
The participation rate for each round of our Delphi study was above 70% (Round 1–80%; Round 2–93.3%; Round 3–73.3%), which is generally considered acceptable for Delphi methodology (Iqbal & Pipon-Young, 2009). An advantage of the Delphi technique is that it allows for unification of professional expertise regarding an important area of interest (Hsu & Sanford, 2007). Participants maintained anonymity throughout the process, decreasing the risk of bias. As with similarly designed studies, limitations do exist. Since the focus of this study was on determination of educational content for inclusion in discharge teaching to promote safe care at home, certain topics (e.g., clinical trials, fertility preservation) that may generally be regarded as highly important for discussion with newly diagnosed families may not have received ratings indicative of high importance, given the objective of promoting safe care at home The views were those of the panelists, and it is unknown if these views are representative of the pediatric oncology community as a whole. However, the majority of the multidisciplinary panel had more than 10 years’ of experience in pediatric oncology, and the panel was representative of diverse COG institutional types and geographical locations. Due to sample size considerations, differences between professional disciplines could not be evaluated; further research is needed to examine these potential differences.
The results of this study provide, for the first time, multidisciplinary consensus regarding key content essential for inclusion in discharge education for newly diagnosed pediatric oncology patients. To date, the lack of formal delineation of the information necessary for inclusion in patient/family education for newly diagnosed patients has limited the provision of optimal care for this vulnerable population (Landier, Leonard, & Ruccione, 2013). This study addressed this gap in knowledge by developing expert consensus regarding informational content for inclusion in the initial education for newly diagnosed pediatric oncology patients, setting the stage for establishing standardized educational content for these patients and their families. In addition, the identification of specialized informational needs for specific disease subgroups provides a foundation for disease-based discharge education.
Conclusion
Patient/family education continues to play an increasingly important role in healthcare. Findings from this Delphi Study will contribute to the development of evidence-based intervention programs aimed at standardizing essential informational content and supporting the effective delivery of patient/family education for newly diagnosed pediatric oncology patients.
Acknowledgments
Funding:
Supported by the National Cancer Institute/National Clinical Trials Network Group Operations Center Grant (U10CA180886; PI: Adamson). Presented, in part, at the Children’s Oncology Group’s “State of the Science Symposium: Patient/Family Education in Pediatric Oncology,” on October 6, 2015, in Dallas, TX; Symposium supported by the National Cancer Institute (R13CA196165 PIs-Landier&Hockenberry).
We would like to thank Lu Chen, PhD, for providing statistical review, the Delphi panel participants, and the members of the expert panel from the Fall 2014 COG meeting, who were instrumental in the initial phase of this study: Joan Darling PhD (patient advocate), Beryl Gantt MSW (patient advocate), Ruth Anne Herring PNP, Nina Kadan-Lottick MD, Marcia Leonard PNP, Neyssa Marina, MD, Robert Noll, PhD, and A. Kim Ritchey, MD.
Biographies
Maureen Haugen, RN, MS, CPNP, CPON® is a Pediatric Nurse Practitioner on the Hematologic Malignancy Team and APN Manager in Hematology/Oncology/Stem Cell Transplant at Lurie Children’s Hospital in Chicago, Illinois. She has served as the Chair of the Children’s Oncology Group Nursing Education Subcommittee 2010–2015.
Wendy Landier, PhD, RN, CPNP, CPON® is an Associate Professor in the Division of Pediatric Hematology/Oncology and in the School of Nursing, and a member of the Institute for Cancer Outcomes and Survivorship, at the University of Alabama at Birmingham in Birmingham, Alabama. She serves as Chair of the Children’s Oncology Group Nursing Discipline.
Belinda Mandrell, PhD, RN, CPNP is Director, Division of Nursing Research and Assistant Member, Department of Pediatrics, St. Jude Children’s Research Hospital, Memphis, Tennessee.
Jeneane Sullivan, MSN, RN, CPON® is the Patient/Family Education Specialist for the Division of Oncology at the Children’s Hospital of Philadelphia in Philadelphia, Pennsylvania. She currently serves as the Nursing Member-At-Large for the Children’s Oncology Group.
Courtney Schwartz, MSN, RN, CPHON® is a Registered Nurse, Expert, on the inpatient unit for the Division of Hematology/Oncology/Stem Cell Transplant at Ann & Robert H Lurie Children’s Hospital in Chicago, Illinois. She is an active member of the Children’s Oncology Group and the Association of Pediatric Hematology Oncology Nurses.
Micah A. Skeens, RN, MS, PNP is a Pediatric Nurse Practitioner on the Embryonal Tumor team in the Division of Hematology/Oncology/BMT at Nationwide Children’s Hospital in Columbus, Ohio. She currently serves as the Chair of the Children’s Oncology Group Nursing Clinical Trials Subcommittee.
Marilyn Hockenberry, PhD, RN, PPCNP-BC, FAAN is the Associate Dean for Research and the Bessie Baker Professor at the Duke University School of Nursing. She is the Vice Chair of the Children’s Oncology Group Nursing Discipline and the Chair of the Nursing Research Subcommittee.
References
- Aburn G, Gott M. Education given to parents of children newly diagnosed with acute lymphoblastic leukemia: a narrative review. Journal of Pediatric Oncology Nursing. 2011;28(5):300–305. doi: 10.1177/1043454211409585. [DOI] [PubMed] [Google Scholar]
- Cavusoglu H. Problems related to the diagnosis and treatment of adolescents with leukemia. Issues in Comprehensive Pediatric Nursing. 2000;23:15–26. doi: 10.1080/014608600265183. [DOI] [PubMed] [Google Scholar]
- Dalkey NC, Helmer O. An experimental application of the Delphi method to the use of experts. Management Science. 1963;9(3):458–467. [Google Scholar]
- Flury M, Caflisch U, Ullmann-Bremi A, Spichiger E. Experiences of parents with caring for their child after a cancer diagnosis. Journal of Pediatric Oncology Nursing. 2011;28:143–153. doi: 10.1177/1043454210378015. [DOI] [PubMed] [Google Scholar]
- Freeman K, O’Dell C, Meola C. Childhood brain tumors: Children’s and siblings’ concerns regarding the diagnosis and phase of illness. Journal of Pediatric Oncology Nursing. 2003;20:133–140. doi: 10.1053/jpon.2003.74. [DOI] [PubMed] [Google Scholar]
- Giacalone A, Blandino M, Spazzapan S, Tirelli U. Cancer and aging: are there any differences in the information needs of elderly and younger patients? Results from an Italian observational study. Annals of Oncology. 2005;16:1982–1983. doi: 10.1093/annonc/mdi391. [DOI] [PubMed] [Google Scholar]
- Gupta AA, Edelstein K, Albert-Green A, D’Agostino N. Assessing information and service needs of young adults with cancer at a single institution: the importance of information on cancer diagnosis, fertility preservation, diet, and exercise. Supportive Care in Cancer. 2013;21:2477–2484. doi: 10.1007/s00520-013-1809-4. [DOI] [PubMed] [Google Scholar]
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–1015. doi: 10.1046/j.1365-2648.2000.t01-1-01567.x. [DOI] [PubMed] [Google Scholar]
- Hsu C, Sanford BA. The Delphi technique: Making sense of consensus. Practical Assessment, Research & Evaluation. 2007;12(10):1–9. [Google Scholar]
- Iqbal S, Pipon-Young L. The Delphi method. The Psychologist. 2009;22(7):598–601. [Google Scholar]
- Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly KP, Porock D. A survey of pediatric oncology nurses’ perceptions of parent educational needs. Journal of Pediatric Oncology Nursing. 2005;22(1):58–66. doi: 10.1177/1043454204272537. [DOI] [PubMed] [Google Scholar]
- Landier W, Leonard M, Ruccione KS. Children’s Oncology Group’s 2013 blueprint for research: nursing discipline. Pediatric Blood & Cancer. 2013;60(6):1031–1036. doi: 10.1002/pbc.24415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyke-Grimm KA, Degner L, Small A, Mueller B. Preferences for participation in treatment decision making and information needs of parents of children with cancer: a pilot study. Journal of Pediatric Oncology Nursing. 1999;16(1):13–24. doi: 10.1177/104345429901600103. [DOI] [PubMed] [Google Scholar]
- Slone JS, Self E, Friedman D, Heiman H. Disparities in pediatric oncology patient education and linguistic resources: results of a national survey of pediatric oncologists. Pediatric Blood & Cancer. 2014;61(2):333–336. doi: 10.1002/pbc.24831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Withycombe J, Andam-Mejia R, Dwyer A, Slaven A, Windt K, Landier W. A comprehensive survey of institutional patient/family educational practices for newly diagnosed pediatric oncology patients: A report from the Children’s Oncology Group. Journal of Pediatric Oncology Nursing. 2016 doi: 10.1177/1043454216652857. in review. [DOI] [PMC free article] [PubMed] [Google Scholar]


