Abstract
Objectives
Information has been collected from positron emission tomography/magnetic resonance imaging (PET/MRI) operational sites to identify its present and future applications. This may help to focus discussions on common interests of the PET/MRI community.
Methods
A web-based survey of PET/MRI users was conducted from June to October 2015. The survey was composed of 26 questions related to (A) the PET/MRI center, (B) present utilization and imaging protocols and (C) perspectives on key applications.
Results
Responses were collected from 39 international sites that operated PET/MRI for a median of 30 months (range, 2 to 62 months). Most installations were located in public institutions with an academic focus (n=26, 67%). Systems were primarily operated by Nuclear Medicine Departments (n=13, 33%), jointly by Nuclear Medicine and Radiology (n=11, 28%), and Radiology only (n=10, 26%). PET/MRI operation was equally focused on clinic routine and research (47% vs. 45% of sites respectively). Sites reported a strong focus on oncology (76% of research and 88% of clinical applications). Other applications included neurology (9% clinical, 12% research) and cardiology (3% clinical, 6% research). Perceived superiority over positron emission tomography/computed tomography (PET/CT) was identified as the strongest driver for clinical adoption. Over half the operators expect PET/MRI to excel in clinical routine within three to five years. Emerging key applications for future PET/MRI use were cardiovascular disease and imaging of inflammation.
Conclusion
An international survey of early PET/MR adopters reveals a mixed utilization of this combined imaging modality with a focus on oncology. The future of PET/MRI is seen in expanded application for oncology, neurology, but also cardiovascular disease and inflammation.
Keywords: PET/MRI, survey, imaging protocols
INTRODUCTION
Simultaneous preclinical positron emission tomography/magnetic resonance imaging (PET/MRI) imaging was proposed in 1997 by Cherry’s group at University of California, Los Angeles (1). Since then the concept of combining PET and MRI within a single examination has been refined technologically and methodologically, first in small animals and, as of 2006, in humans (2). This is different from positron emission tomography/computed tomography (PET/CT) that initially addressed a clinical need (3) before being adapted for small animal imaging (4,5). PET/CT is a tremendous success story with more than 5000 systems installed worldwide today. Within the first 3 years following market introduction in 2001 over 500 PET/CT systems had been installed. By comparison, the adoption of PET/MRI has been slow. Following the introduction of the first prototype (designed for brain imaging) in 2007 (6) and the installation of five more units worldwide, the first commercially available whole-body PET/MRI system was introduced in 2011 (7). Two fully-integrated PET/MRI systems were introduced in 2011 (8) and 2014 (9), respectively. Five years after its introduction only around 70 PET/MRI systems have been placed worldwide.
Advantages of PET/MRI integration may include the near-simultaneous acquisition of molecular images and high-resolution anatomical images of high soft tissue contrast as well as the exploitation of functional MRI imaging parameters to aid the development of diagnostic and intermediate endpoint biomarkers. Thus, much has been published about the potential of combined PET/MRI. Yet little clinical evidence is available to support an added value of this modality in comparison to other, established imaging modalities (10,11). Several expert panels have commented on the potential of PET/MRI imaging for clinical specific applications, such as brain or cardiac imaging as well as for research applications that are based on multi-parametric anatometabolic imaging (12,13,14,15,16). While PET/MRI is an innovative technology it has not yet found its place in clinical practice. Current users are early adopters and their PET/MRI utilization patterns may provide insights into current and future key applications. The current survey of international PET/MRI users was conducted to record and document such current utilization patterns in clinical routine and research.
METHODS
Concept
A survey of international PET/MRI users was designed in February 2015 to collect data on existing PET/MRI operations worldwide and to review PET/MRI protocol variations. The idea for this data collection originated from discussions during the recent PET/MRI workshop in Tübingen (16) and a subsequent review of the international survey on PET/CT operations conducted a few years earlier (17). As in this previous study we decided to benefit from the easy, rapid and widespread distribution of web-based questionnaires. Similar to our previous study, we prepared our survey in line with recent recommendations on the structure of surveys that – in theory – help to maximize response rates; this included a personal introductory statement, the offer to make results public, the use of simple headers and textual representation of response categories, and the provision of a relatively short deadline including multiple reminders.
Survey
The electronic questionnaire consisted of 26 questions (see supplemental material section) that could be answered in about 20 minutes. Questions, developed by imaging experts with extensive experience in PET/CT and PET/MRI imaging addressed three issues: (A) the operation of the PET/MRI centers (n=9), (B) current applications and imaging protocols (n=14) and (C) perspectives on future key applications (n=3). Question types were dichotomous, single choice, multiple choice, rating scales, or open ended for number, text comment, or date. The survey was composed in English using an internet-based platform (SurveyMonkey.com). Invitation to the survey was sent in June 2015 to the complete email listing of all active whole-body PET/MRI physicians or researchers (one key user per site) at the time. This list of 69 active sites was composed of feedback we solicited from participants of the most recent PET/MRI expert panel meeting in Tübingen 2015 (16) and the three vendors of whole-body PET/MRI imaging systems: Philips Healthcare, Siemens Healthcare, and GE Healthcare. Three reminders were mailed to all non-responding recipients between 06/2015 and 08/2015. The survey was closed on November 1st 2015.
Statistical Analysis
Responses were collected anonymously and tabulated for each question. We report total number of response per answer option, proportion of response per respective answer option in percent, rank of answer options, or median (range) for quantitative response. Free text response for key applications (questions 23 and 24) was summarized by field of application into five categories (Cardiovascular, Pediatric, Other, Neurology, Oncology) with respective subcategories.
RESULTS
A total of 39 responses were collected from 69 active PET/MRI users between June and October of 2015. All responses were satisfactory in quality and quantity and, therefore, the overall response rate was 57%.
Demographics – PET/MRI Center (Questions 1–9)
The 39 responding sites were located in Europe (62%), North America (23%), and Asia Pacific (16%) (Fig. 1A). Responding sites operated PET/MR systems from Siemens Healthcare (77%), Philips Healthcare (13%), and GE Healthcare (10%) (Fig. 1B), which corresponded well to the known market shares of these companies at time of the survey (72%, 14% and 14%, respectively).
Figure 1.
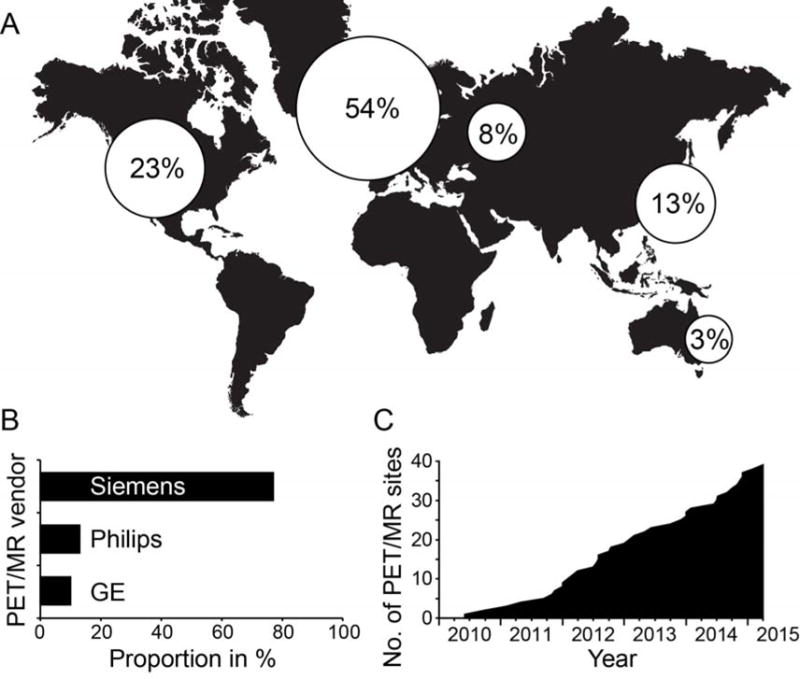
Survey of 39 PET/MRI sites by (A) location, (B) vendor, and (C) first year of operation. PET/MRI location was categorized into (from left to right): North America, Western Europe, Eastern Europe, Asia, and Australia.
The number of active PET/MRI sites grew continuously since 2010 with an average number of 8 sites becoming operational each year (Fig. 1C). Responding sites had operated PET/MRI for a median of 30 months (range, 2 to 62 months) and 23 of 39 (59%) sites had PET/MRI experience for ≥2 years.
Table 1 lists funding and clinical responsibility separate for private and public institutions as well as for different operating Departments. Most PET/MRI systems (26/39, 67%) were placed in public institutions with an academic focus. Systems were operated by Nuclear Medicine (n=13, 33%), jointly between departments (n=11, 28%), or by Radiology (n=10, 26%). Other operators (n=5, 13%) were Departments of Radiation Therapy (n=2) and Research institutions (n=3).
Table 1.
PET/MRI financial resources as well as clinical responsibility separated by provider. Absolute number (%) or median (range) are given.
| All | Private | Public | Joint | Nuc | Rad | Other | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | 39 | 10 | 29 | 11 | 13 | 10 | 5 |
| Funded by | |||||||
| Hospital | 10 (26%) | 3 (30%) | 7 (24%) | 3 (27%) | 3 (23%) | 4 (40%) | 0 |
| Government | 7 (18%) | 0 | 7 (24%) | 3 (27%) | 0 | 1 (10%) | 3 (60%) |
| Private | 11 (28%) | 5 (50%) | 6 (21%) | 3 (27%) | 5 (38%) | 3 (30%) | 0 |
| Res grant | 11 (28%) | 2 (20%) | 9 (31%) | 2 (18%) | 5 (38%) | 2 (20%) | 2 (40%) |
| Reported by | |||||||
| Joint | 30 (77%) | 7 (70%) | 23 (79%) | 10 (91%) | 12 (92%) | 5 (50%) | 3 (60%) |
| Nuc only | 1 (3%) | 1 (10%) | 0 | 0 | 1 (8%) | 0 | 0 |
| Res only | 3 (8%) | 0 | 3 (10%) | 0 | 0 | 1 (10%) | 2 (40%) |
| Rad only | 5 (13%) | 2 (20%) | 3 (10%) | 1 (9%) | 0 | 4 (40%) | 0 |
| MRI only scans | 25 (64%) | 8 (80%) | 17 (59%) | 7 (64%) | 7 (54%) | 7 (70%) | 4 (80%) |
Abbreviations: Nuc = Nuclear Medicine Department, Rad = Radiology Department, Joint = Joint Nuclear Medicine/Radiology Department, Res = research.
Clinical scans were reported jointly by Nuclear Medicine + Radiology in private (7/10, 70%) and public (23/29, 79%) institutions. Interdisciplinary reporting was performed in almost all Nuclear Medicine and jointly operated departments (92% and 91%); however, 40% of reports from PET/MRI clinics operated by Radiology were provided only by radiologists.
Hospital, private, and research funds were almost equally regarded as leading source of financing for the PET/MRI device (26%, 28% and 28% respectively). Governments provided main funds in 18% of sites. Nine of 21 (43%) devices in Western Europe were primarily funded by research grants versus 11% of devices elsewhere. A median of 10 employees participated in PET/MRI operation, including 4 physicians, 2 technicians, 2 physicists, and 2 administrative staff. Median number of staff was lower for public (n=9) versus private (n=15) institutions, and for Joint, Nuclear Medicine, or Other Departments (n=10) as compared to Radiology Departments (n=13). Median number of employees was similar in institutions with PET/MRI interpretation by radiologists or nuclear medicine physicians only (n=11) when compared to the entire group (n=10).
Present Applications (Questions 10–13, 15–16)
Fig. 2 demonstrates most prevalent applications as reported by the survey participants. Forty-seven and 45% of PET/MRI operations focused on clinical and research, respectively. The main applications were oncology (76% of research and 88% of clinical applications) and neurology (12% and 9% respectively). Several centers operated PET/MRI for clinical (13%) or research purpose (19%) only.
Figure 2.
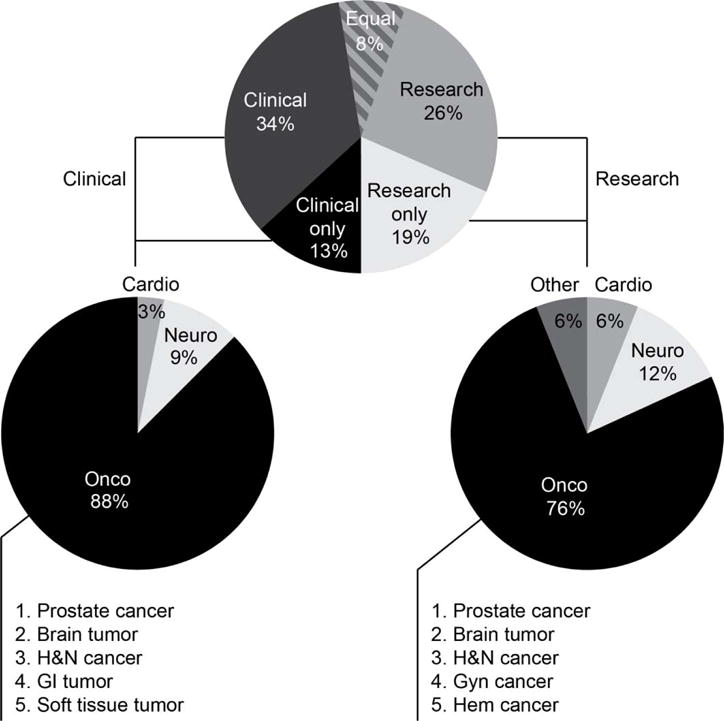
Present clinical and research applications. Most prevalent clinical and research applications have been categorized into cardiology (Cardio), neurology (Neuro), other, or oncology (Onco). Oncology was further subdivided by tumor type. Abbreviations: H&N = head & neck, GI = gastrointestinal, Gyn = gynecologic, Hem = hematologic.
Within both clinical and research oncologic applications, participants ranked prostate cancer, brain tumors, and head & neck cancers highest. Few sites ranked cardiac (n=3 sites) and other applications highest (n=2 sites).
In total, 44706 patients underwent a PET/MRI at the responding sites, which corresponds to an average throughput of about 8 (max. 38) patients per week. This average number, derived from the total number of patients scanned divided by the number of weeks of operation for each site, however, was lower than the present throughput reported by the sites at 12 (max. 35) patients per week.
Variations in Imaging Protocols (Questions 14, 17–22)
Imaging protocols vary widely across active PET/MRI sites (Table 2). Since no PET/MRI standard or guidelines have been published, survey questions regarding typical imaging protocols were phrased more generically. Typical cardiology and oncology imaging protocols were reported to take a median of 60 min, with 30 min minimum and 100 min to 120 min maximum. A typical neurology imaging protocol was somewhat shorter with a reported median of 45 min (range, 10 min to 120 min).
Table 2.
Scan time and tracer separated by field of application. Median (range) is given for typical duration of PET/MRI scans.
| N=39 | Cardio | Neuro | Onco |
|---|---|---|---|
| Typical duration of scan (min) | 60 (30–120) | 45 (10–120) | 60 (30–100) |
| Top three tracer used | |||
| 1 | 18F-FDG | 18F-FDG | 18F-FDG |
| 2 | 13N-NH3 | Other | Other |
| 3 | Other | 18F-FET | PSMA ligands |
The most frequently used PET probe across all categories and applications was 18F-FDG. 13N-NH3 (ranked #2), 18F-FET (ranked #3), and prostate-specific membrane antigen (PSMA) ligands (ranked #3) were also used frequently.
MR protocols were heterogeneous with a certain degree of overlap (Supplemental Table 1). All reported neurology MRI protocols included diffusion weighted imaging (DWI) and/or fluid attenuation inversion recovery in addition to T1- and T2-acquisition. MR protocols for oncology imaging frequently included Dixon (5/8), DWI (4/8), and volumetric interpolated breath-hold examination (VIBE; 3/8) sequences. About two thirds of the sites (25/39, 64%), foremost those from the private sector (80%) and those within Radiology, Radiation Therapy, or Research Departments (70% – 80%), performed MRI-only protocols in addition to PET/MRI imaging (Table 1). Most patients would, in the user’s perspective (25 of 39, 64%), have undergone MRI and PET/CT in case PET/MRI was not available.
Present and future Key Applications (Questions 23–24)
Participants named up to three key applications for present and future use of PET/MRI (Fig. 3). Oncology (n=24) and neurology (n=13) were most frequently mentioned for present key application, followed by pediatric (n=4) and other (n=7) imaging. General oncology and prostate cancer were most prevalent oncology indications; general neurology and dementia imaging were the most prevalent neurology indications.
Figure 3.
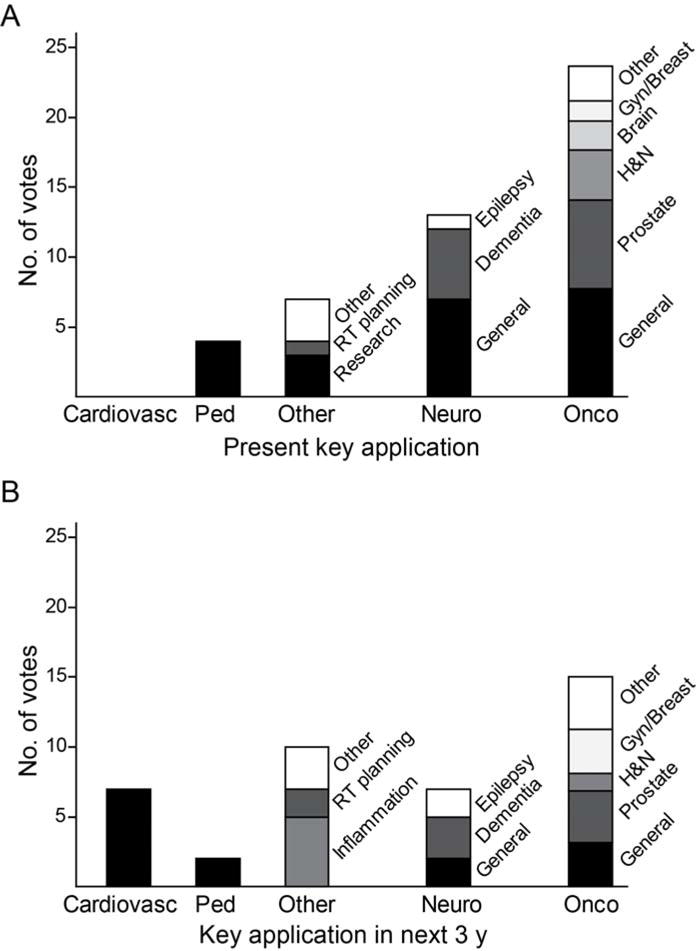
(A) Present and (B) future key applications. Participants listed up to three key applications for present and future PET/MRI use. Abbreviations: RT = radiation therapy, Cardiovasc = cardiovascular, Ped = pediatric, y = years.
None of the participants listed cardiovascular disease at present, however, seven participants included cardiovascular imaging, e.g. for diagnosis of cardiac fibrosis, atherosclerosis, or vasculitis, as future key application of PET/MRI. Furthermore, imaging inflammation was considered a new application within the next years by five participants. Future pediatric, oncology, and neurology PET/MRI had fewer mentions. Further votes for future key applications were casted for musculoskeletal disease (n=1), lymphoma (n=2), soft tissue (n=2) and liver (n=1) tumors.
Clinical Adoption (Questions 25–26)
Table 3 summarizes the user’s perspective on clinical adoption of PET/MRI. Most operators expected increased utilization in the mid-term (approx. 3 to 5 years; 28/39, 72%). “Superiority over PET/CT” and “Unique clinical information” were ranked highest among the anticipated drivers for adoption, followed by “Cost”, “Combined functional MRI and PET” and “Patient throughput” ranked last.
Table 3.
Timeline for clinical adoption of PET/MRI.
| All | Private | Public | |
|---|---|---|---|
|
| |||
| N | 39 | 10 | 29 |
| In how many years will PET/MRI excel in clinical routine? | |||
| 1 | 4 (10%) | 0 | 4 (14%) |
| 3 | 13 (33%) | 5 (50%) | 8 (28%) |
| 5 | 15 (38%) | 2 (20%) | 13 (45%) |
| 10 | 6 (15%) | 3 (30%) | 3 (10%) |
| >10 | 1 (3%) | 0 | 1 (3%) |
DISCUSSION
The aim of this survey was to determine how PET/MRI is used worldwide. This survey follows in its design other surveys on the adoption of PET/CT (17) and single-photon emission computed tomography/computed tomography (SPECT/CT) (18). A decade after the introduction of PET/CT more than 5000 systems from six different vendors have been installed worldwide (17,19). At the time of this survey, about five years into commercialization of whole-body PET/MRI, less than 80 systems from three vendors have been installed at near linear growth rate. The current survey helps to identify strengths and weaknesses of PET/MRI and may provide insights into the reasons for its slow adoption.
First, the duration of a typical PET/MRI protocol (45 to 60 min) was about two times longer and weekly throughput (8 to 12 patients) about 5 times lower than in typical PET/CT operations, despite similar number of staff employed (17). This difference likely reflects a higher complexity of the MRI versus CT component in terms of active operator involvement and integration with PET. Further, most PET/MRI systems were installed in Western Europe after considerable research funding for these sites. The low patient throughput and the amount of public and research funding raises questions about the financial viability of privately operated systems.
Second, protocols are not well-defined, mostly due to varying MRI protocols. Members of the Tübingen PET/MRI expert panels expressed their clear intent to harmonize future PET/MRI operation (15). However, imaging protocols, especially those of the MRI component, remain highly variable as shown in the current survey. Variation of MRI protocols is apparently needed to enable further innovation at this early stage of PET/MRI operation. However in a long-term perspective, harmonization of specific protocols may be of use in demonstrating clinical utility needed to accelerate PET/MRI adoption. The reported selection of PET tracers, however, revealed one clear similarity among the participating sites: 18F-FDG remains the most important tracer for PET/MRI. PSMA ligands were ranked among the top three tracers for oncology, even before choline-analogues or somatostatin-ligands. Such prominent position of a relatively new radioligand further underlines the dominant role of prostate cancer proposed both for present and future use of PET/MRI in cancer patients. 18F-FET was ranked #3 for brain applications, even before compounds for neurodegenerative disease, thus indicating an important role of PET/MRI for neuro-oncology. 13N-NH3 ranked #2 for cardiac applications, however at an overall low volume of cardiovascular examinations.
Third, the interpretation of PET/MRI images is more challenging than that of PET/CT studies. This was reflected in our survey by the fact that interpretation was jointly performed by radiologists and Nuclear Medicine physicians at more than 80% of PET/MRI sites versus only approx. 40% of PET/CT sites in our previous survey (17).
PET/MRI was performed equally often for clinic and research. Oncology was the dominant application of present clinical and research use (88 and 76%; respectively). Cancers that were imaged frequently with stand-alone MRI before the availability of PET/MRI (i.e. patients with prostate cancer, brain tumors, and head & neck cancer) were listed as the top three indications. The focus on these tumor entities, for which MRI may be considered an anatomic modality-of-choice, is reasonable if cost-effectiveness is demonstrated and patient comfort is acceptable. However, this ranking of indications also underlines a current lack of definite new indications for fully-integrated (8,9) PET/MR imaging.
The survey revealed a low current or future proportion of neurologic and cardiovascular PET/MRI examinations. This is surprising as these indications were frequently named as key future applications (2,20). Cardiovascular disease was not mentioned as a key present indication by any of the participants; pediatric imaging was named as a key application by only 4/39 sites and was even less frequently mentioned as a key future indication. This is surprising, given the frequently publicized radiation concerns of the pediatric medical community (21,22). However, imaging of inflammation and cardiovascular diseases was voted first and second most anticipated future indication.
In general, the current survey suggests that both current and future applications might evolve around oncologic entities and questions. Given the high utilization of PET/CT and its acceptable costs in cancer (23) it remains questionable whether this will result in dramatic increases in PET/MRI utilization in cancer patients. However PET/MRI is still at the level of early adoption with a number of unsolved technical, regulatory and funding issues. Utilization patterns of the current respondents might therefore not be representative for the PET/MRI community of the future.
One potential advantage of near-simultaneous data acquisition is the exact temporal and spatial correlation of morphologic, functional, and metabolic information. Exact fusion is needed to combine complementary PET and MRI information of a dynamic system, such as moving organs or transient pathologies. Drzezga et al. proposed a complementary value of brain metabolism (PET) and regional perfusion (MRI) and pointed to a clinical advantage through their simultaneous acquisition (24). However, the clinical benefit of near-simultaneous versus sequential acquisition of such biomarkers has not been confirmed yet (16). PET/MRI applications for which near-simultaneous image acquisitions were proposed as advantageous such as neurodegenerative diseases (24) contributed to less than 10% of the clinical PET/MRI workload.
Despite the lack of novel future applications more than 50% of respondents predict a profound clinical impact of PET/MRI within five years. Interestingly, more than 15% of respondents predict an impact of PET/MRI only after the next decade. Despite the apparent lack of key applications and the obvious need for future development, PET/MRI users expressed their confidence in the potential of this technology by ranking “Superiority over PET/CT” among the top drivers for clinical adoption. Evidence for such superiority, however, is not yet available (11).
CONCLUSION
This survey among early adopters of combined PET/MRI imaging systems demonstrates a mixed perspective on the current and future use-case scenarios of this imaging modality with a focus on oncology, particularly with prostate, brain and head & neck malignancies. Today’s PET/MRI users predict evidence for diagnostic benefits over PET/CT as one of the drivers for clinical transition.
Supplementary Material
Acknowledgments
We thank the participants of this survey for their support.
Footnotes
CONFLICTS OF INTEREST
J.C. is co-founder of Momentum Biosciences, Sofie Biosciences, and Trethera Therapeutics, Los Angeles, USA. T.B. is co-founder and owner of cmi-experts GmbH, Basel, Switzerland and academic collaborator with Siemens Healthcare. K.H. is a consultant of Sofie Biosciences, Los Angeles, USA.
References
- 1.Shao Y, Cherry SR, Farahani K, et al. Simultaneous PET and MR imaging. Phys Med Biol. 1997;42:1965–1970. doi: 10.1088/0031-9155/42/10/010. [DOI] [PubMed] [Google Scholar]
- 2.Schlemmer HP, Pichler BJ, Schmand M, et al. Simultaneous MR/PET imaging of the human brain: feasibility study. Radiology. 2008;248:1028–1035. doi: 10.1148/radiol.2483071927. [DOI] [PubMed] [Google Scholar]
- 3.Beyer T, Townsend DW, Brun T, et al. A combined PET/CT scanner for clinical oncology. J Nucl Med. 2000;41:1369–1379. [PubMed] [Google Scholar]
- 4.Szanda I, Mackewn J, Patay G, et al. National Electrical Manufacturers Association NU-4 performance evaluation of the PET component of the NanoPET/CT preclinical PET/CT scanner. J Nucl Med. 2011;52:1741–1747. doi: 10.2967/jnumed.111.088260. [DOI] [PubMed] [Google Scholar]
- 5.Magota K, Kubo N, Kuge Y, Nishijima K, Zhao S, Tamaki N. Performance characterization of the Inveon preclinical small-animal PET/SPECT/CT system for multimodality imaging. Eur J Nucl Med Mol Imaging. 2011;38:742–752. doi: 10.1007/s00259-010-1683-y. [DOI] [PubMed] [Google Scholar]
- 6.Schmand M, Burbar Z, Corbeil J, et al. BrainPET: First human tomograph for simultaneous (functional) PET and MR imaging. J Nucl Med. 2007;48:45. [Google Scholar]
- 7.Zaidi H, Ojha N, Morich M, et al. Design and performance evaluation of a whole-body Ingenuity TF PET-MRI system. Phys Med Biol. 2011;56:3091–3106. doi: 10.1088/0031-9155/56/10/013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Delso G, Furst S, Jakoby B, et al. Performance measurements of the Siemens mMR integrated whole-body PET/MR scanner. J Nucl Med. 2011;52:1914–1922. doi: 10.2967/jnumed.111.092726. [DOI] [PubMed] [Google Scholar]
- 9.Delso G, Khalighi M, Hofbauer M, Porto M, Veit-Haibach P, von Schulthess G. Preliminary evaluation of image quality in a new clinical ToF-PET/MR scanner. EJNMMI Phys. 2014;1:A41. doi: 10.1186/2197-7364-1-S1-A41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Czernin J, Herrmann K. The potential of PET/MRI imaging in oncology: a comment to a summary report of the first PET/MRI Workshop in Tuebingen in 2012. Mol Imaging Biol. 2013;15:372–373. doi: 10.1007/s11307-013-0642-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spick C, Herrmann K, Czernin J. 18F-FDG PET/CT and PET/MRI perform equally well in cancer patients: Evidence from studies in more than 2300 patients. J Nucl Med. 2016;57:420–30. doi: 10.2967/jnumed.115.158808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wahl RL, Quint LE, Cieslak RD, Aisen AM, Koeppe RA, Meyer CR. “Anatometabolic” tumor imaging: fusion of FDG PET with CT or MRI to localize foci of increased activity. J Nucl Med. 1993;34:1190–1197. [PubMed] [Google Scholar]
- 13.Bailey DL, Antoch G, Bartenstein P, et al. Combined PET/MR: The real Work has just started. Summary Report of the third international Workshop on PET/MR imaging; February 17–21, 2014, Tubingen, Germany. Mol Imaging Biol. 2015;17:297–312. doi: 10.1007/s11307-014-0818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey DL, Barthel H, Beuthin-Baumann B, et al. Combined PET/MR: Where are we now? Summary report of the second international workshop on PET/MR imaging April 8–12, 2013, Tubingen, Germany. Mol Imaging Biol. 2014;16:295–310. doi: 10.1007/s11307-014-0725-4. [DOI] [PubMed] [Google Scholar]
- 15.Bailey DL, Barthel H, Beyer T, et al. Summary report of the first international Workshop on PET/MR imaging, March 19–23, 2012, Tubingen, Germany. Mol Imaging Biol. 2013;15:361–371. doi: 10.1007/s11307-013-0623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey DL, Pichler BJ, Guckel B, et al. Combined PET/MRI: Multi-modality multi-parametric imaging is here: Summary report of the 4th international Workshop on PET/MR imaging; February 23–27, 2015, Tubingen, Germany. Mol Imaging Biol. 2015;17:595–608. doi: 10.1007/s11307-015-0886-9. [DOI] [PubMed] [Google Scholar]
- 17.Beyer T, Czernin J, Freudenberg LS. Variations in clinical PET/CT operations: results of an international survey of active PET/CT users. J Nucl Med. 2011;52:303–310. doi: 10.2967/jnumed.110.079624. [DOI] [PubMed] [Google Scholar]
- 18.Wieder H, Freudenberg LS, Czernin J, Navar BN, Israel O, Beyer T. Variations of clinical SPECT/CT operations: an international survey. Nuklearmedizin. 2012;51:154–160. doi: 10.3413/Nukmed-0467-12-01. [DOI] [PubMed] [Google Scholar]
- 19.Beyer T, Townsend DW, Czernin J, Freudenberg LS. The future of hybrid imaging-part 2: PET/CT. Insights Imaging. 2011;2:225–234. doi: 10.1007/s13244-011-0069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marsden PK, Strul D, Keevil SF, Williams SC, Cash D. Simultaneous PET and NMR. Br J Radiol. 2002;75:S53–S59. doi: 10.1259/bjr.75.suppl_9.750053. [DOI] [PubMed] [Google Scholar]
- 21.Gatidis S, Schmidt H, Gucke B, et al. Comprehensive oncologic imaging in Infants and preschool Children with substantially reduced radiation Exposure using combined simultaneous 18F-Fluorodeoxyglucose Positron Emission Tomography/Magnetic Resonance imaging: A Direct Comparison to 18F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography. Invest Radiol. 2016;51:7–14. doi: 10.1097/RLI.0000000000000200. [DOI] [PubMed] [Google Scholar]
- 22.Purz S, Sabri O, Viehweger A, et al. Potential pediatric Applications of PET/MR. J Nucl Med. 2014;55:32S–39S. doi: 10.2967/jnumed.113.129304. [DOI] [PubMed] [Google Scholar]
- 23.Yang Y, Czernin J. Contribution of imaging to cancer care costs. J Nucl Med. 2011;52(Suppl 2):86S–92S. doi: 10.2967/jnumed.110.085621. [DOI] [PubMed] [Google Scholar]
- 24.Drzezga A, Barthel H, Minoshima S, Sabri O. Potential clinical Applications of PET/MR imaging in neurodegenerative Diseases. J Nucl Med. 2014;55:47S–55S. doi: 10.2967/jnumed.113.129254. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


