Abstract
Objective
To examine where residents in an area with limited access to healthy food (an urban food desert) purchased healthier and less healthy foods.
Design
Food shopping receipts were collected over a one-week period in 2013. These were analyzed to describe where residents shopped for food and what types of food they bought.
Setting
Two low-income, predominantly African-American neighborhoods with limited access to healthy food in Pittsburgh, PA, USA.
Subjects
293 households in which the primary food shoppers were predominantly female (77.8%) and non-Hispanic black (91.1%) adults.
Results
Full-service supermarkets were by far the most common food retail outlet from which food receipts were returned and accounted for a much larger proportion (57.4%) of food and beverage expenditures, both healthy and unhealthy, than other food retail outlets. Although patronized less frequently, convenience stores were notable purveyors of unhealthy food.
Conclusions
Findings highlight the need to implement policies that can help to decrease unhealthy food purchases in full-service supermarkets and convenience stores and increase healthy food purchases in convenience stores.
Keywords: diet, food desert, food receipts, food retail environment
Introduction
Unhealthy diet is a modifiable risk factor for chronic conditions such as diabetes(1), cancer(2), and cardiovascular disease(3), and has been highlighted as a major public health problem(4, 5). Although widespread across the United States, unhealthy diet is more common among low-income populations(6), particularly those who reside in low-income neighborhoods in which access to healthy, affordable food is lacking, i.e., “food deserts”(7).
Guided by the assumption that geographic access is a major factor underlying a poor diet (7), recent policy initiatives have invested hundreds of millions of dollars into food deserts to increase access to healthy food(8). Understanding household food purchasing behavior, i.e., the purchase of foods from a variety of sources, including but not limited to grocery stores, neighborhood and convenience stores, and restaurants(9, 10), could illuminate the role of geographic access in actual dietary intake. Specifically, analysis of where residents purchase healthier (i.e., fruits and vegetables) and less healthy (i.e., high in sugar, salt, or calories) foods can provide a more complete understanding of whether and how the neighborhood food environment might best be modified to improve food purchasing behavior. For example, policies may need to be modified to facilitate purchase of healthy foods in retail outlets where healthy foods are underrepresented and/or stymie purchase of unhealthy foods in outlets where unhealthy foods are overrepresented.
Of the various methods for assessing household food purchasing behavior, including food shopping receipts, home food inventories, Universal Product Code (UPC) bar scanning, and self-reported shopping behavior in surveys, food receipts have some key advantages(9). Food receipts capture food from a wider variety of sources, including both stores and restaurants, whereas home food inventories and UPC bar scanning capture only foods purchased in stores and/or eaten at home. In addition, food receipts are better-suited for assessment of food purchasing behavior over a greater period of time, thereby affording more stable estimates of food purchasing behavior. Food receipts are also advantageous over self-reported shopping behavior in that they do not depend on the accuracy of participants’ recall. Recent empirical research affirms the viability and validity of food receipts as a source of data on household food purchasing behaviors across a variety of food sources(9).
The collection of food receipts to study household food purchasing behavior is a relatively recent development. One of the main recent sources of data on household food purchasing behavior, the 2010 Nielsen Homescan Panel Survey data, suggests that residents of lower-income neighborhoods purchase less healthy food than their higher-income counterparts(11). However, data for this study were collected using the UPC scanning method and supplemented by self-report data. This study has the notable strengths of a large consumer panel and detailed data on food purchases, but the data do not include food purchases from sources other than stores (e.g., restaurants) and underrepresent poor consumers. Other research has analyzed receipts data, but, to our knowledge, none have focused on residents of an urban food desert(10, 12).
We sought to fill these gaps by collecting food receipts data to examine household food purchasing behavior of low-income African Americans residing in a food desert. We present a detailed description of food purchasing patterns in this population, focusing on the types of food retail outlets (e.g., full-service grocery store, convenience store) residents patronized and the kinds of foods and beverages purchased (e.g., fruits, vegetables, sweets, salty snacks) from these venues.
Methods
Design and sample
The food receipts data analyzed for this study were collected as part of the Pittsburgh Hill/Homewood Research on Eating, Shopping, and Health (PHRESH), a 5-year study of residents and their neighborhood environment in two predominantly African American, low-income “food deserts” in Pittsburgh, Pennsylvania. The study sought to understand the effect on residents of eliminating a food desert: in one of the neighborhoods, a new full-service supermarket was slated to open. PHRESH study participants were recruited from a random sample of households drawn from a complete list of residential addresses generated by the Pittsburgh Neighborhood and Community Information System (a detailed description of sampling procedures is provided elsewhere(13)). The final sample consisted of 1,372 households where the primary food shopper in each household was interviewed and administered an in-person baseline questionnaire in their home between May and December 2011. The study protocol was approved by the Institutional Review Board of the institution where the study was conducted.
Approximately two years after completion of the PHRESH baseline interview, data collectors returned to the same households to conduct a different household interview with the same primary household shopper for a separate but related study of physical activity (PHRESH Plus, or the Pittsburgh Hill/Homewood Research on Neighborhoods, Exercise and Health). At the same time this interview was administered, data collectors asked participants to collect their food shopping receipts from all household food purchases, including those in stores and restaurants, and wear an accelerometer to record their physical activity over the course of one week. At the end of the week, data collectors returned to collect the food shopping receipts and accelerometer; participants were compensated an additional $25 (above and beyond $15 compensation for completing the household interview) for participating in this component of the study. These data, including the food receipts, were collected prior to the opening of the new supermarket whose influence was evaluated in the PHRESH study.
Of 1,372 primary household food shoppers who completed the PHRESH baseline interview, 982 (71.6%) also participated in PHRESH Plus, and 644 of these participants returned household food shopping receipts1. Due to the labor-intensive nature of entering food receipts data and constrained resources, we randomly selected 300 participants from the sampling frame of 644 participants. Of the 300 participants, seven were excluded due to incomplete information on the receipts (i.e., food items were undiscernible), resulting in a final analytic sample size of 293 participants in the food receipts data analysis.
Household interviews
Household interviews included questions on participants’ sociodemographic characteristics (e.g., age, gender, race/ethnicity, marital status, educational attainment) and objective measurements of height and weight. Missing values on income were imputed with the software IVEWare in SAS macros (version 0.2, 2009, Software Survey Methodology Program at the University of Michigan’s Survey Research Center, Institute for Social Research, Ann Arbor). Adjusted income was computed as a ratio of household income and size.
Food receipts
Key receipt data elements, including the names and locations of stores and restaurants for which receipts were returned and the names, quantities, and pre-tax costs of food and beverage items purchased, were manually entered by research assistants. To ensure reliable extraction of receipt characteristics, a coding protocol with standard definitions for data elements was created, and all research assistants were trained to follow it. Research assistants were initially required to demonstrate fidelity to the protocol by coding five receipts correctly according to the independent coding done by a researcher or senior research assistant who had already demonstrated fidelity to the protocol. After this initial training period, fidelity to the coding protocol was ensured by having a senior coder check a random sample of 10% of receipts entered by each assistant.
Because of wide variability in the types of foods and beverages purchased and the level of detail reported on receipts across food retail outlets, one food or beverage “item” was generally defined as the smallest packaged unit for purchase. For example, all of the following would have been counted as a single item: a carton of eggs, a bag of potato chips, and an 8-pack of Pepsi cans. Thus, the actual quantity in a single item varies tremendously across different foods and beverages. For the vast majority (80%) of items, specific quantities in a single unit were not listed on the receipt and are thus unknown. In lieu of data on the quantity of food and beverage items, the cost of food and beverage items serves as a rough proxy of the quantity of item(s) purchased.
After raw receipt data elements were recorded, all types of food items purchased in stores were classified into one of several mutually exclusive categories. Because some food items consisted of multiple types of food, items were assigned to a single category according to the following hierarchy: prepackaged or take-away/eating-out entrée; sweetened baked goods; ice cream or gelato; candy; condiments, dips, and gravy; sweets; salty snacks; potatoes; meat; eggs; cheese; yogurt; butter, margarine, or spread; whole grains; other type of grain (refined or not specified); nuts and seeds; fruit; beans and peas; vegetables; other. These categories were later aggregated to form larger categories for analysis: empty calories (sweets, salty snacks, butter, margarine, shortening, condiments, dips, and gravy), protein (meat, eggs, nuts and seeds, beans and peas), grains (whole, refined or not specified), vegetables (including potatoes), fruits, dairy (cheese, yogurt), prepackaged and take-away/eating-out entrees, and other. A similar process was followed for beverages using the following categories: sugar-sweetened beverages, milk, fruit/vegetable juice, water, artificially sweetened or low-calorie beverages, coffee and tea, condiments (e.g., creamer), alcohol, and specialty drinks (e.g., latte, smoothie). Food and beverage items purchased in restaurants were not listed in sufficient detail to permit classification into finer-grained categories.
We initially classified stores into one of 11 categories. Classifications were based on definitions from the Food Marketing Institute (FMI) and the North American Industry Classification System (NAICS) and confirmed with our Community Advisory Boards, comprised of key resident stakeholders within each neighborhood. To simplify, we reduced these categories to the following four categories of stores: (1) full-service supermarkets, which include grocery stores run by nationally or regionally recognized chains; (2) mass merchandising and discount grocery stores, which include supercenters (e.g., Walmart, Target), wholesale clubs (e.g., Sam’s Club, Costco), and discount grocery stores, which offer a large assortment of low-priced food items (e.g., Save A Lot); (3) convenience stores, which include small chain stores such as those at gas stations (e.g., Get Go, AM/PM), neighborhood stores (i.e., small individual/family-owned stores), drug stores, and dollar stores, which offer a limited assortment of low-priced and perishable items (e.g., Family Dollar); and (4) other stores, such as meat or seafood markets and specialty grocery stores (e.g., Whole Foods). Restaurants were also classified into one of the following mutually exclusive categories: fast food restaurant; restaurant with table service; buffet or cafeteria; bar, tavern, or lounge; coffee shop; other.
Statistical analyses
Given the paper’s descriptive purpose, we report univariate descriptive statistics to characterize the sociodemographic and other characteristics of the primary household food shoppers who returned receipts. We then present univariate descriptive statistics for food purchases to characterize where participants did their food shopping, what types of foods and beverages they purchased, and, finally, where they purchased different types of foods and beverages. We did not conduct any tests of significance for two main reasons: 1) we had no particular hypotheses for this descriptive paper, and 2) where we do compare two or more groups descriptively (e.g., amount of household food expenditures on a particular food type in different store types), unbalanced, small sample sizes limited our power to detect statistically significant differences between groups. Analyses were conducted in SAS, version 9.4, of the SAS System for Windows (SAS Institute, Inc., Cary, NC).
Results
Participant characteristics
As shown in Table 1, most participants in the receipts sample were female (77.8%) and non-Hispanic black (91.1%); on average, participants were 55.06 years old (SD = 15.17). Roughly half of the sample had a high school education or less (50.5%). Slightly less than half of the sample reported that a SNAP recipient resided in the household (46.1%), and slightly more than half of the sample reported access to a vehicle when needed (55.0%); on average, per capita annual household income was $13,913.20 (SD = $11,879.80). Most participants were single, divorced, separated or widowed (81.3%) and reported no children residing in the household (75.1%). On average, participants reported having made roughly three visits to the main food store at which they had done their major food shopping in the past month (M = 2.93, SD = 0.83) and having made roughly two visits to other stores (besides the main store) for major food shopping in the past month (M = 1.90, SD = 1.13). Roughly three-quarters (78.8%) of participants were considered to be overweight or obese based on BMI.
Table 1.
Characteristics of primary household food shoppers in the receipts study and parent study, 2013
| Receipts sample* (N = 293) | Parent sample* (N = 982) | |||
|---|---|---|---|---|
|
| ||||
| Characteristic | n | % | n | % |
| Female | 228 | 77.8 | 751 | 76.5 |
| Non-Hispanic black | 267 | 91.1 | 891 | 91.5 |
| Highest level of education completed | ||||
| Less than high school | 38 | 13.0 | 132 | 13.4 |
| High school | 110 | 37.5 | 380 | 38.7 |
| Some college | 98 | 33.5 | 327 | 33.3 |
| College | 47 | 16.0 | 143 | 14.6 |
| SNAP recipient in household | 135 | 46.1 | 512 | 52.1 |
| Owns or has access to a vehicle | 161 | 55.0 | 549 | 56.2 |
| Marital status | ||||
| Married or living with partner | 55 | 18.8 | 171 | 17.5 |
| Single, never married | 106 | 36.2 | 408 | 41.8 |
| Widowed, divorced, or separated | 132 | 45.1 | 398 | 40.7 |
| Children under 18 in household | 73 | 24.9 | 269 | 27.4 |
| Weight status | ||||
| Not overweight or obese (BMI < 25) | 59 | 20.1 | 211 | 21.7 |
| Overweight (BMI 25–29) | 90 | 30.7 | 287 | 29.5 |
| Obese (BMI 30+) | 141 | 48.1 | 475 | 48.8 |
|
| ||||
| M | SD | M | SD | |
|
| ||||
| Age (years) | 55.06 | 15.17 | 54.14 | 16.12 |
| Per capita annual household income (USD) | 13,913.20 | 11,879.80 | 12,790.52 | 12,919.44 |
| Number of main food store visits, past month | 2.93 | 0.83 | 2.87 | 0.85 |
| Number of other food store visits, past month | 1.90 | 1.13 | 1.93 | 1.12 |
SNAP, Supplemental Nutrition Assistance Program; BMI, body mass index; USD, United States dollars.
Participants in the receipts sample are primary household food shoppers whose household food shopping receipts were included in the final analytic sample for this paper. They are a subset of parent study participants, who completed the baseline interviews for both PHRESH and PHRESH Plus and were invited to return food shopping receipts.
To assess response bias, we compared the 293 participants in the final analytic receipts sample with the total sample of 982 participants in the parent study who were eligible for inclusion in the receipts analysis (i.e., had the opportunity to return their food shopping receipts and completed both the PHRESH and PHRESH Plus baseline interviews). As shown in Table 1, the receipts sample very closely resembled the parent study sample on most characteristics. Exceptions were residence of a recipient of Supplemental Nutrition Assistance Program (SNAP) benefits in the household and per capita annual household income: Having a SNAP benefits recipient residing in the household was slightly less common in the receipts sample (46.1%) than in the parent sample (52.1%), and participants in the receipts sample appeared to have slightly higher per capita annual household income (M = $13,913.20, SD = $11,879.80) than those in the parent sample (M = $12,790.52, SD = $12,919.44). In addition, the samples appeared to differ slightly on marital status, such that those in the receipts sample were slightly more likely to have been widowed, divorced, or separated (45.1%) and slightly less likely never to have been married (36.2%) than those in the parent sample (widowed, divorced, or separated: 40.7%; single, never married: 41.8%); however, the samples had very similar proportions of participants who were currently married or living with their partner (receipts sample: 18.8%; parent sample: 17.5%).
Food retail outlets where household food purchases were made
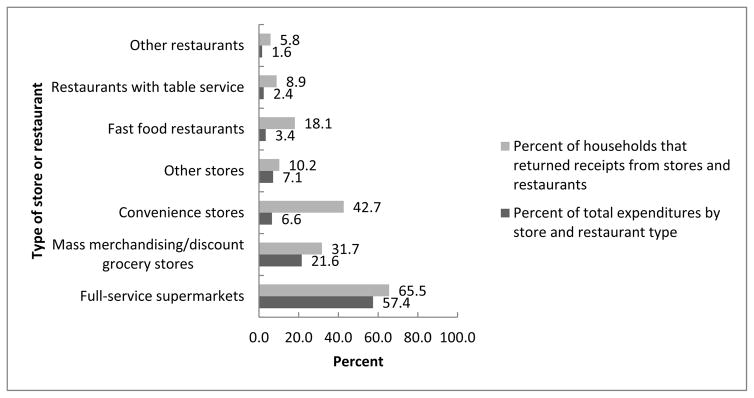
Across the 293 households, 879 receipts were returned. On average, each household returned three receipts (SD = 2.51). As shown in Figure 1, a greater proportion of households returned receipts from stores (93.2%) than restaurants (27.0%). Similarly, at the aggregate level, stores accounted for a much larger proportion of total food and beverage expenditures (92.6%) than restaurants (7.4%).
Fig. 1. Percentages of Total Food Expenditures and Receipts Returned by Store and Restaurant Type among Households in a Food Desert in Pittsburgh, 2013.
The “full-service supermarkets” category includes only full-service supermarkets; “mass merchandising/discount stores” include supercenters, whole sale clubs, and discount grocery stores; “convenience stores” include dollar stores, drug stores, convenience stores, and neighborhood stores; “other” stores include meat or seafood market, specialty grocery stores, and all other types of food stores. The “other” restaurants category includes buffet or cafeteria; bar, tavern, or lounge; coffee shop; and other type of restaurant. Percentages of households that returned at least one receipt from each type of store and restaurant were calculated with the total number of households as the denominator (N = 293). Percentages of total expenditures by store and restaurant type were calculated with the total food and beverage expenditures in all food retail outlets (stores and restaurants) across all households in the sample as the denominator (N = $18,398.10).
Among stores, full-service supermarkets were by far the most common store type from which households returned food receipts (65.5%) and accounted for a much larger proportion of food and beverage expenditures (57.4%) than any other food retail channel. After full-service supermarkets, receipts were most commonly returned from convenience stores (42.7%), followed by mass merchandising/discount grocery stores (31.7%) and other store types (10.2%). After full-service supermarkets, the greatest proportion of total food and beverage expenditures was accounted for by mass merchandising/discount grocery stores (21.6%), followed by other store types (7.1%) and convenience stores (6.6%).
Among restaurants, more households returned receipts from fast-food restaurants (18.1%), followed by restaurants with table service (8.9%) and buffets or cafeterias (5.8%). Paralleling these trends, fast-food restaurants accounted for a greater proportion of food and beverage expenditures (3.4%) than restaurants with table service (2.4%) and other types of restaurants (1.6%).
Types of food and beverage purchased in stores
We also examined the types of food and beverages purchased in stores (see Table 2). The great majority of expenditures in stores were for food (87.9%) rather than beverages (12.1%). More than one-third of household food expenditures were for foods high in protein, e.g., meats (38.0%). Foods that consist primarily of empty calories (e.g., sweets, salty snacks) collectively accounted for the second largest proportion of household food expenditures (22.5%). All other categories represented less than 10% of household food expenditures. We saw a similar pattern when we examined food expenditures on a household level. We observed extensive variability in food expenditures across households.
Table 2.
In-store food and beverage expenditures of households in a food desert in Pittsburgh, 2013
| Food/beverage category | Percent of total expenditures* | Average expenditures, all households (N = 293) † ($) | Average expenditures of households with at least one food or beverage item purchase‡ | Households with at least one food or beverage item purchase | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean | SD | Mean | SD | N | % | ||
| Food | 87.9 | 51.07 | 60.74 | 56.25 | 61.51 | 266 | 90.8 |
| Protein | 38.0 | 19.41 | 28.41 | 26.21 | 30.20 | 217 | 74.1 |
| Salty snacks | 5.1 | 2.59 | 4.08 | 5.31 | 4.43 | 143 | 48.8 |
| Sweets | 11.3 | 5.76 | 8.77 | 8.70 | 9.53 | 194 | 66.2 |
| Other empty calories§ | 6.1 | 3.11 | 5.86 | 6.64 | 7.07 | 137 | 46.8 |
| Grains | 9.2 | 4.69 | 5.90 | 6.95 | 5.99 | 198 | 67.6 |
| Vegetables | 8.6 | 4.37 | 7.46 | 8.42 | 8.56 | 152 | 51.9 |
| Fruit | 7.2 | 3.69 | 5.90 | 6.76 | 6.57 | 160 | 54.6 |
| Prepackaged/takeaway entrees | 6.9 | 3.53 | 7.28 | 9.77 | 9.26 | 106 | 36.2 |
| Dairy | 3.9 | 2.01 | 4.04 | 5.73 | 5.02 | 103 | 35.2 |
| Other | 3.7 | 1.89 | 6.52 | 7.21 | 11.15 | 78 | 26.6 |
| Beverages | 12.1 | 6.99 | 9.65 | 9.25 | 10.12 | 222 | 75.8 |
| Sugar-sweetened beverages | 40.2 | 2.81 | 4.19 | 5.20 | 4.47 | 159 | 54.3 |
| Milk | 16.8 | 1.18 | 2.16 | 3.48 | 2.40 | 99 | 33.8 |
| Fruit/vegetable juice | 11.1 | 0.78 | 2.29 | 4.28 | 3.77 | 53 | 18.1 |
| Water | 7.4 | 0.52 | 1.75 | 4.00 | 3.12 | 38 | 13.0 |
| Coffee/tea | 7.2 | 0.51 | 2.27 | 4.49 | 5.36 | 34 | 11.6 |
| Alcohol | 6.5 | 0.46 | 4.48 | 33.48 | 21.97 | 4 | 1.4 |
| Artificially sweetened and low-calorie | 5.6 | 0.38 | 1.49 | 3.56 | 3.07 | 32 | 10.9 |
| Mean | SD | Mean | SD | N | % | ||
| Condiment (e.g., creamer) | 3.1 | 0.21 | 0.86 | 3.29 | 1.12 | 19 | 6.5 |
| Specialty drinks (e.g., latte) | 2.2 | 0.15 | 1.62 | 7.35 | 9.43 | 6 | 2.1 |
Percentages for both of the overarching food and beverage categories of expenditures were calculated with the total food and beverage expenditures (N = $17,015.48) as the denominator. Percentages for subcategories of food and beverage expenditures were calculated with the total food (N = $14,962.71) and beverage (N = $2,052.77) expenditures, respectively, as the denominators.
The numbers in the “average expenditures, all households” column are the average (mean) amount of money spent on each type of food or beverage across all households during the seven-day period of data collection (N = 293) and the standard deviation.
The numbers in the “average expenditures of households with at least one food or beverage item purchase” columns are the average (mean) amount of money spent on each type of food or beverage of households that purchased at least one food or beverage item in the corresponding category and the standard deviation; for example, the average shown for protein is the average amount of money spent on protein of households that bought at least one protein item during the seven-day period of data collection and the standard deviation. The number and percentage of households that purchased at least one food or beverage item in the corresponding category are shown in the columns to the right.
Other empty calories include butter, margarine, shortening, condiments, dips, and gravy.
In the full sample, sugar-sweetened beverages (SSBs) accounted for the greatest share of household beverage expenditures in stores (40.2%), followed by milk (16.8%) and fruit/vegetable juice (11.1%). All other beverage types represented less than 10% of beverage expenditures. The average household beverage expenditures followed a similar trend, and, like food, the standard deviations for each beverage category indicated substantial variability across households in beverage expenditures.
Store types where healthy and unhealthy foods were purchased
To determine where purchases of unhealthy and healthy foods were made, we conducted a more granular analysis of expenditures for specific types of unhealthy and healthy foods and beverages in different types of stores (see Table 3). For unhealthy foods, we focused on salty snacks, sweets, and SSBs, all of which consist primarily of empty calories; for healthy foods, we focused on fruits and vegetables.
Table 3.
Average household expenditures ($) on each type of food and sugar-sweetened beverages (SSBs) by store type among the subset of households that made at least one purchase of the particular type of food or SSBs in each type of store, 2013
| Store types | Unhealthy foods and beverages | Healthy foods | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Salty snacks | Sweets | SSBs | Fruits | Vegetables | |||||||||||
|
| |||||||||||||||
| n* | Mean† | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | |
| Full-service supermarkets | 67 | 5.24 | 4.75 | 109 | 8.32 | 8.22 | 97 | 5.46 | 4.27 | 113 | 6.15 | 5.91 | 115 | 7.99 | 8.19 |
| Mass merchandisers/discount grocery stores | 41 | 4.19 | 2.53 | 56 | 8.36 | 10.53 | 31 | 3.82 | 2.90 | 50 | 6.15 | 6.56 | 49 | 5.83 | 4.94 |
| Convenience stores | 52 | 3.83 | 3.27 | 76 | 3.29 | 2.74 | 56 | 2.98 | 2.33 | 16 | 2.24 | 1.39 | 5 | 1.40 | 0.49 |
| Other | 10 | 3.72 | 2.25 | 7 | 9.03 | 12.99 | 6 | 1.96 | 1.71 | 7 | 6.21 | 7.83 | 7 | 9.86 | 12.40 |
The numbers shown in all of the “n” columns in the table are the number of households that made at least one purchase of the corresponding type of food or SSB in the store type. For example, n=67 for purchases of salty snacks in full-service supermarkets indicates that 67 households returned receipts showing a purchase of salty snacks in a full-service supermarket.
The numbers shown in the “Mean” columns in the table are the average amount of money spent on the corresponding type of food or SSB in the store type across households among the subset of households that made at least one purchase of the food type or SSB in the store type. For example, the mean of $5.24 shown in the cell corresponding to salty snacks and full-service supermarkets indicates that, on average, the 67 households that purchased salty snacks in full-service supermarkets spent $5.24 on salty snacks in full-service supermarkets.
In general, purchases of both unhealthy and healthy foods were more common in full-service supermarkets than in other stores. For example, 109 households had purchased sweets in full-service supermarkets, whereas purchases of sweets in convenience stores were made by roughly two-thirds as many households (n = 76) and purchases of sweets in mass merchandisers/discount grocery stores were made by roughly half as many households (n = 56); very few households purchased sweets in other stores (n = 7). Similarly, 115 households had purchased vegetables in full-service supermarkets, whereas less than half as many households had purchased vegetables in mass merchandisers/discount grocery stores (n = 49); purchases of vegetables were very rare in other stores (n = 7) and convenience stores (n = 5). Convenience stores were the second most common site of unhealthy food purchases. For example, salty snacks were purchased in full-service supermarkets, convenience stores, and mass merchandisers/discount grocery stores by 67, 52, and 41 households, respectively. Mass merchandisers/discount grocery stores were also the second most common purveyor of healthy food purchases after full-service supermarkets, with 113 and 115 households purchasing fruits and vegetables, respectively, in full-service supermarkets, and less than half as many households purchasing fruits (n = 50), and vegetables (n = 49), respectively, in mass merchandisers/discount grocery stores. Convenience stores and other stores were rarely the site of purchases of fruits (convenience stores: n = 16; other stores: n = 7) and vegetables (convenience stores: n = 5; other stores: n = 7).
Average household food expenditures on both unhealthy and healthy foods were also generally higher in full-service supermarkets. For example, on average, household food shoppers spent more money on salty snacks and vegetables in full-service supermarkets than in mass merchandisers/discount grocery stores (salty snacks: full-service supermarkets [M = $5.24, SD = $4.75], mass merchandisers/discount grocery stores [M = $4.19, SD = $2.53]; vegetables: full-service supermarkets [M = $7.99, SD = $8.19], mass merchandisers/discount grocery stores [M = $5.83, SD = $4.94]. However, among the subgroups of food shoppers who purchased unhealthy food in convenience stores and mass merchandiser/discount grocery stores, average household expenditures on unhealthy food types were generally higher among those who made their purchases in mass merchandisers/discount grocery stores than in convenience stores. For example, the average (mean) amount of money spent on sweets was $8.36 (SD = $10.53) in mass merchandisers/discount grocery stores and $3.29 (SD = $2.74) in convenience stores.
Discussion
The current study dovetails with previous research indicating that residents of food deserts, in spite of not living near full-service supermarkets (by definition), purchase most foods from full-service supermarkets(11). This finding is perhaps not surprising in light of other research showing that the majority of people rarely shop at the supermarket closest to their home(14–16). Our analysis also documents the high demand among this cohort for unhealthy foods such as sweets relative to healthy foods such as fruits and vegetables. Households made most of their food purchases, both healthy and unhealthy, from full-service supermarkets. This is an important point, as research and nutrition policy initiatives emphasize the importance of access to a full-service supermarket in having a healthy diet. Although access to a full-service supermarket is important for facilitating purchases of healthy foods, supermarkets may also facilitate purchases of junk food. Indeed, as Elbel and colleagues noted, in addition to stocking healthy food, supermarkets stock vast quantities of unhealthy food(17). This may help to explain why recent studies of the effects of opening a supermarket in a low-income neighborhood to increase residents’ proximity and access to a supermarket did not find the broad, positive effects on dietary intake that were expected(13, 17–19). Thus, in the absence of policies and practices that curb junk food purchases in full-service supermarkets, the benefits of providing access to a full-service supermarket are unlikely to be fully realized.
Our findings have policy implications for the types of food retail outlets to target and the availability and marketing of unhealthy food in full-service supermarkets. First, nutrition policies will be more impactful to the extent that they focus on the primary site of food shopping among residents, i.e., full-service supermarkets. Policies that overlook this and focus instead on reducing access to other types of food retail outlets that account for a relatively small share of food purchases (e.g., the ban on fast food restaurants in south Los Angeles) are unlikely to have a strong impact on diet. Second, instead of merely subsidizing the opening of full-service supermarkets in low-income or food desert areas, policies should aim to reduce the convenience and salience of low-nutrient foods in full-service supermarkets. For example, in-store marketing practices could be modified to de-emphasize unhealthy food options and emphasize healthy food options.
In addition to underscoring the need for food policy to target full-service supermarkets, the current findings suggest that food policy should also target other types of food retail outlets that predominantly feature unhealthy food. Convenience stores, which encompassed neighborhood stores, dollar stores, and convenience stores, collectively accounted for only seven percent of total food expenditures but were the site of unhealthy food and beverage purchases for roughly 20–25% of households. By contrast, less than six percent of households purchased fruits or vegetables in convenience stores. These findings converge with past research suggesting that convenience stores are notable purveyors of junk food(20). Some communities in Philadelphia, Pennsylvania and Minneapolis, Minnesota are trying to address this imbalance by increasing the selection of healthy foods in corner stores. Initial evaluations of these initiatives suggest that increasing the availability of fruits and vegetables in these stores has been followed by increased sales of fruits and vegetables(21, 22). However, as with full-service supermarkets, simply facilitating access to healthy food in convenience stores is unlikely to be enough to improve diet. Implementing policies that curb unhealthy food purchases is critical to producing meaningful improvements in diet.
Study limitations
One limitation of this research is that we do not know the extent to which the receipts returned represent a complete census of all household food shopping receipts. Thus, our estimates of food purchases might underestimate food purchases over the preceding week. However, our estimate of the average total weekly expenditures in stores very closely resembles that obtained in a recent analysis of national panel data on household food purchasing behavior (i.e., the 2010 Nielsen Homescan Survey) in residents of low-income, low-access areas: Their analysis indicated that an average of $697.50 was spent per quarter (i.e., 12-week period)(11), and our analysis indicated an average of $58.14 spent per week, which translates to $697.68 per quarter (when multiplied by 12). Similarly, the average expenditures on fruits and vegetables in our sample closely resembled their estimates. They reported an average (mean) of $47.4 (SD = 48.2) and $49.3 (SD = 41.5) for expenditures on fruits and vegetables, respectively, over a quarter (i.e., roughly 12 weeks); in comparison, after adjusting for differences in the time periods by multiplying our average expenditures over a week by 12, we obtain average expenditures of $44.28 and $52.44 for fruits and vegetables, respectively. The similarity in these estimates increases confidence that our estimates of total weekly food expenditures reasonably represented actual expenditures.
Another limitation of this study concerns the generalizability of its findings. Although the receipts sample very closely resembled the parent study sample on most sociodemographic characteristics, the receipts sample appeared to be slightly less socioeconomically disadvantaged than the parent study sample: Recipients of SNAP benefits were less commonly residents of households in the receipts sample (46.1%) than the parent study sample (52.1%), and per capita annual household income was slightly higher in the receipts sample (M = $13,913.20, SD = $11.879.80) than in the parent study sample (M = $12,790.52, SD = $12,919.44). Similarly, the receipts sample had a slightly lower proportion of single, never married participants (36.2%) and a slightly higher proportion of widowed, divorced, or separated participants (45.1%) relative to the parent sample (single, never married: 41.8%; widowed, divorced, or separated: 40.7%). While these differences were of modest magnitude, they might nonetheless indicate limited generalizability of the current findings to households that have greater financial need and in which the primary household food shopping is done by single, never married individuals.
Another limitation of the current research is the lack of annotated receipts data, which indicate precise quantities purchased. Cost was used as a rough proxy of quantity, but this likely leads to underestimation of the quantities of types of food that have a lower price per unit (e.g., foods in the empty calories category such as salty snacks and candy) and potentially overestimation of the quantities of types of food that have a higher price per unit (e.g., meats). The lack of annotated receipts also precluded our ability to examine food purchases in restaurants in detail, which is one of the major gaps in this literature. We were able to determine that restaurant food purchases represent a minority of food purchases and that fast food restaurants are the most common type of restaurant at which food purchases were made; however, we lack detailed data on the types of foods and beverages purchased in restaurants. Future research would benefit from having participants annotate receipts using a standardized protocol to permit a more detailed examination of food purchases in both stores and restaurants.
Another limitation concerns the one-week time frame of data collection. Previous validation research suggests a minimum of two weeks to obtain stable estimates of household food purchases(10). Thus, our estimates of household food purchasing behavior might be unstable. However, the similarity between our findings on average weekly household food expenditures and another study’s findings on household food purchases over a three-month period(11) increases confidence in the stability of our estimates.
Conclusions
In sum, these findings reinforce previous calls to implement policies that increase healthy food purchases and decrease junk food purchases(4, 5). In particular, policies should focus on mitigating the convenience and salience of unhealthy food options sold in full-service supermarkets and convenience stores and increasing the convenience and salience of healthy food options in convenience stores.
Acknowledgments
The authors express sincere appreciation and gratitude to La’Vette Wagner, field coordinator of the Pittsburgh Hill/Homewood Research on Eating, Shopping, and Health Study; Elizabeth Steiner, the project coordinator; and Reema Singh, Leslie Mullins, Rachel Ross, and Jacqueline Mauro, who entered data.
Financial Support: Funding for this study was provided by the National Cancer Institute (Grant No. R01CA149105; Tamara Dubowitz, Principal Investigator). The National Cancer Institute had no role in the design, analysis, or writing of this article.
Footnotes
We included receipts only from participants who had completed both the PHRESH and PHRESH Plus baseline interviews so that we would be able to examine household food purchasing behavior based on receipts data in relation to outcomes assessed in both the PHRESH and PHRESH Plus interviews in subsequent studies.
Conflict of Interest: None.
References
- 1.Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345:790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- 2.Key TJ, Allen NE, Spencer EA, et al. The effect of diet on risk of cancer. The Lancet. 2002;360:861–868. doi: 10.1016/S0140-6736(02)09958-0. [DOI] [PubMed] [Google Scholar]
- 3.Hung H-C, Joshipura KJ, Jiang R, et al. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004;96:1577–1584. doi: 10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services, PHS, Office of the Surgeon General; Services U.S.D.o.H.a.H, editor. The Surgeon General’s call to action to prevent and decrease overweight and obesity. U.S. GPO; Rockville, MD: 2001. [PubMed] [Google Scholar]
- 5.Story M, Kaphingst K, Robinson-O’Brien R, et al. Creating healthy food and eating environments: Policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 6.Zenk SN, Schulz AJ, Hollis-Neely T, et al. Fruit and vegetable intake in African Americans: Income and store characteristics. Am J Prev Med. 2005;29:1–9. doi: 10.1016/j.amepre.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966–2007. Prev Chronic Dis: Public Health Res, Practice, and Policy. 2009;6:A105. [PMC free article] [PubMed] [Google Scholar]
- 8.Couzin-Frankel J. Tackling America’s eating habits, one store at a time. Science. 2012;337:1473–1475. doi: 10.1126/science.337.6101.1473. [DOI] [PubMed] [Google Scholar]
- 9.French SA, Shimotsu ST, Wall M, et al. Capturing the spectrum of household food and beverage purchasing behavior. J Am Diet Association. 2008;108:2051–2058. doi: 10.1016/j.jada.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 10.French SA, Wall M, Mitchell NR, et al. Annotated receipts capture household food purchases from a broad range of sources. International J Behavioral Nutr and Physical Activity. 2009;6:1–11. doi: 10.1186/1479-5868-6-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahkovsky I, Snyder S. Food Choices and Store Proximity. US Department of Agriculture ERS; Contract No.: ERR-195. [Google Scholar]
- 12.Cullen K, Baranowski T, Watson K, et al. Food category purchases vary by household education and race/ethnicity: Results from grocery receipts. J Am Diet Association. 2007;107:1747–1752. doi: 10.1016/j.jada.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Dubowitz T, Ghosh-Dastidar M, Cohen D, et al. Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Affairs. 2015;34:1858–1868. doi: 10.1377/hlthaff.2015.0667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drewnowski A, Aggarwal A, Hurvitz PMMP, et al. Obesity and supermarket access: proximity or price? Am J Public Health. 2012;102:e74–e80. doi: 10.2105/AJPH.2012.300660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hillier A, Cannuscio CC, Karpyn A, et al. How far do low-income parents travel to shop for food? Empirical evidence from two urban neighborhoods. Urban Geogr. 2011;32:712–729. [Google Scholar]
- 16.Dubowitz T, Zenk SN, Ghosh-Dastidar B, et al. Healthy food access for urban food desert residents: examination of the food environment, food purchasing practices, diet and BMI. Public Health Nutr. 2014;18:2220–2230. doi: 10.1017/S1368980014002742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elbel B, Moran A, Dixon LB, et al. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutr. 2015;18:2881–2890. doi: 10.1017/S1368980015000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Affairs. 2014;33:283–291. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elbel B, Mijanovich T, Kiszko K, et al. The introduction of a supermarket via tax-credits in a low-income area: The influence on purchasing and consumption. Am J Health Promotion. doi: 10.4278/ajhp.150217-QUAN-733. Published online: 21 September 2015. [DOI] [PubMed] [Google Scholar]
- 20.Cavanaugh E, Mallya G, Brensinger C, et al. Nutrition environments in corner stores in Philadelphia. Prev Med. 2013;56:149–151. doi: 10.1016/j.ypmed.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Almaguer Sandoval B, Law Y, Young C. Healthier Corner Stores: Positive Impacts and Profitable Changes. Philadelphia, PA: The Food Trust; 2014. [Google Scholar]
- 22.Minneapolis Department of Health and Family Support. Healthy Corner Store Program: Making produce more visible, affordable and attractive. Minneapolis, MN: 2012. [Google Scholar]