Abstract
Cross-talk between B and T cells in transplantation is increasingly recognized as being important in the alloimmune response. T cell activation of B cells occurs by a 3-stage pathway, culminating with costimulation signals. We review the distinct T cell subtypes required for B cell activation, and discuss the formation of the Germinal Center (GC) after transplantation, with particular reference to the repopulation of the GC following depletional induction, and the subsequent effect of immunosuppressive manipulation of T-B cell interactions. Additionally, ectopic GCs are seen in transplantation, but their role is not fully understood. Therapeutic options to target T-B cell interactions are of considerable interest, both as immunosuppressive tools, and to aid further understanding of these important alloimmune mechanisms.
1. General introduction
The two major cellular components that constitute the alloimmune response in transplantation, T and B cells, play major roles in graft rejection. In the absence of immunosuppression, organ transplantation elicits intense responses from T and B cells, resulting in cell- and antibody-mediated rejection, respectively. Unsurprisingly, ‘pure’ alloimmune responses, limited exclusively to either type of rejection are infrequent in clinical settings. Increasingly, it is recognised that the role of B cells in transplantation is not restricted to their effector function, the humoral response, alone: antigen presentation of B cells also contributes to the optimal immune response1. Similarly, although graft rejection had been considered largely mediated by T cell effector function, there is growing evidence that B cells and their immunoglobulin products (alloantibody) may play a role in the process2. In this review, we wish to focus on crosstalk between T and B cells in antibody-mediated rejection (ABMR), following transplantation.
2. B cell in Transplantation
2.1. T- cell dependent B cell activation in Transplantation
Following transplantation, there are 3 signaling pathways required for T cell dependent activation of B cells. Initial B cell activation is driven by alloantigen (Figure 1). Alloantigen is delivered to the mature B cell (IgM+IgD+) rich area known as the B cell follicle (cortex) within the secondary lymphoid organ.
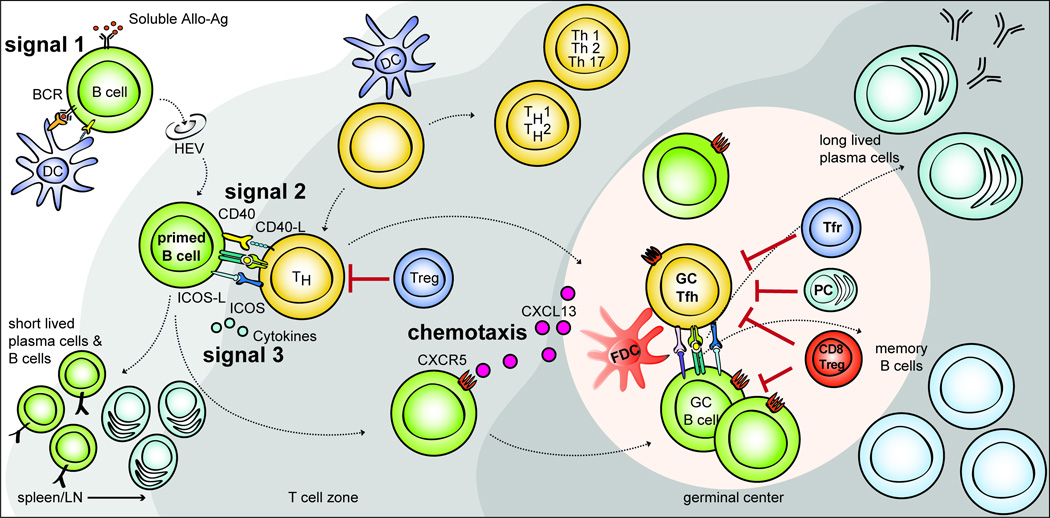
FIGURE 1. T cell dependent B cell activation via Mutiple T-B interations after allostimulation.
Naïve mature B cells are activated through BCR recognition (signal 1) and migrate to the T-B border via HEVs (High Endothelial Venules). Primed B cells receive further signals from costimulation (signal 2), and cytokines (signal 3) in the T-B border. Some activated CD4 T cells can acquire charateristics of Tfh cell lineage and migrate into the B cell follicle via CXCR5. These Tfh cells provide IL-21 and costimulation and induce the proliferation of cognate B cells, isotype switching, and somatic mutation. This massive B cell expansion and differentiation leads to the formation of hyperplastic germinal center in the B cell follicle. Tfr cells and CD8 Treg cells are thought to suppress this germinal center response either directly, by depleting B cells or indirectly by modulating Tfh cells. The germinal center response induces the differentiation of isotype-switched affinity mature B cells into memory B cells or into long-lived plasma cells.
These naïve mature B cells are able to recognize both membrane bound and soluble alloantigens as a function of the B cell receptor (BCR). BCR recognition (signal 1) of the cognate alloantigen provides an activation signal via CD19 complex (which comprises CD19, CD21, CD81 and CD225)3–5. The BCR is also responsible for internalization (endocytosis) of alloantigens derived from the allogeneic cells, which are degraded and presented via MHC II molecules6,7. Primed B cells are translocated into the T cell rich area (T cell zone, paracortex) and only B cells which interact with cognate T helper cells (Tfh) receive further activation signals.
In addition to antigen recognition through the BCR, the second signal for B cell activation is costimulation (signal 2). A cognate interaction between helper T cells and B cells provides multiple costimulation signals for B cell activation. CD40L from T cells has been extensively studied; signaling via CD40 on B cells drives B cell proliferation, antibody affinity maturation and class switch recombination (via activation of NF-kB)8. In mice, deficiency of CD40 or CD40L results in the absence of IgG production, and Ig class switch defects9,10. Corroborating this, targeting CD40 or CD40L in organ transplantation results in a reduction of alloantibody production11,12. Following alloantigen recognition and costimulation, B cell activation requires cytokines (signal 3), produced by various helper T cells including Th1, Th2, and Th17. In support of this various cytokines are known to affect antibody production. Furthermore, numerous cytokines (including IL-6, IL-21, IL-12, IL-23, and IL-27) appear to be capable of inducing enhancing or sustaining Tfh cell-like phenotypes, which become important in the Germinal Center (GC) response. These cytokines act through phosphorylation of STAT1, STAT3 or STAT4 to regulate the Tfh cell –associated gene expression13–15. However, it is now known that BCL-6 is the required transcription factor for Tfh cell differentiation16,17, which implies that the Tfh is a separate lineage of helper T cell. This is supported by the finding that the expression of BCL-6 is suppressed by IL-2 acting through STAT 518, and that BCL-6 expression represses of T-bet (Th1 differentiation) and RORγc (Th17 differentiation)15. More GC-associated cytokines will be discussed later.
2.2. T cell independent Signals for B cell activation
Although B cell activation is predominantly through T cell dependent mechanisms, there is interest in T cell independent mechanisms by which B cell activation might occur in organ transplantation.
Innate immunity
Complement split products, are bound by complement receptors CD21 (C3b, C3dg & C3d) and CD35 (C3b & C4b), which then inactivate them to iC3b and iC4b respectively19. CD21 expression is limited to B cells and follicular dendritic cells, while CD35 is expressed more widely. In cross talk between complement and the adaptive immune system, opsonized alloantigen activates the classical complement pathway and may engage the complement receptor, CD21/CD35, to form a co-receptor with the BCR, thereby lowering the threshold for B cell activation20,21.
Cytokine stimulation
Part of the TNF family of cytokines, the BLyS (B Lymphocyte stimulator) family of ligands (BLyS, BAFF – B cell activating factor) and receptors (BAFFr - B cell activating factor receptor; present on each B cell, TACI - transmembrane activator and calcium modulator and cyclophilin ligand interactor; present on memory B cells & BCMA - B cell maturation antigen; present on plasma cells) are co-stimulators of B cells and necessary for the survival and maturation of B cells to plasma cells22. A proliferation inducing ligand (abbreviated as APRIL), like BAFF, is produced as a transmembrane protein, and then proteolytically cleaved to be released in soluble form23.In mice, BAFF has been shown to independently promote TLR7/9 expression and autoantibody production, in the absence of T cells.24.
Other mechanisms for T cell independent B cell activation include BCR recognition of polysaccharides, and costimulation with TLRs25. Although this is predominantly of importance in bacterial immunity, it may be of relevance in ABO-incompatible or xenotransplantation.
3 Germinal Centre Development
The Germinal center (GC) is a specialized structure containing proliferating antigen-specific B cells that promote antigen-dependent affinity maturation, which is located within B cell follicles of secondary lymphoid organs. The GC response arises from the interaction between follicular helper T cells (Tfh) and B cells. It is now known that Tfh cells and their interaction with B cells are required for GC formation, the generation of long-lasting antibody production26–28, and high-affinity antibody generation.
3.1. Follicular Helper T cell (Tfh) and B cell interaction
Tfh cells upregulate the chemokine receptor 5 (CXCR5) whilst downregulating chemokine receptor 7 (CCR7). This facilitates migration towards B cell follicle29,30. Additional surface molecules including PD-1, ICOS, and SLAM family of receptors are highly expressed by Tfh cells (Figure 2). These molecules are now used for the identification of Tfh cells. It is now known that BCL-6 is the key transcription factor for Tfh cell differentiation15–17. CXCR5+PD-1hiICOS+BCL-6+ CD4 T cells also have been shown to localize to the GCs. Taken together, Tfh cells are a terminally differentiated effector T cell lineage31.
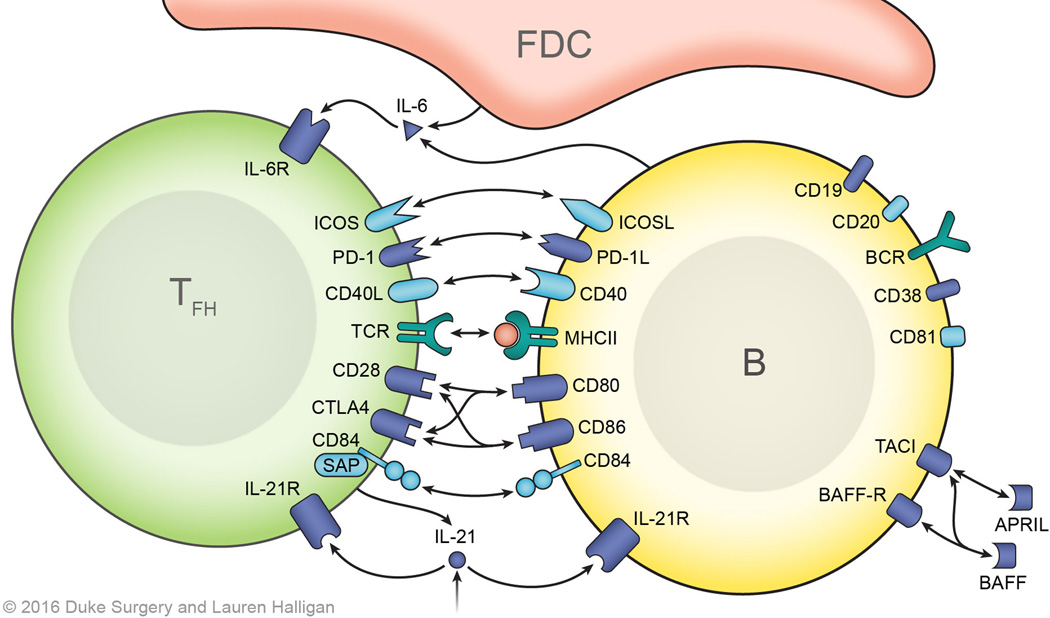
FIGURE 2. T-B cell interactions and signals.
The initial B cell activation signal is provided by cognate BCR-alloantigen interaction and requires the CD19, CD21, CD81 complex for an optimal signaling. Congnate follicular helper T cells provide costimulation following presentation of antigenic peptides in MHC class II by the B cells in the germinal center. T:B interactions, especially ICOS-ICOSL, CD40-CD40L, and CD28-B7 interactions, are central to this process. Members of the SLAM (Signaling lymphocytic activation molecule) family of receptors, particularly CD84, are also important for stable T:B cell interactions, which also contribute to Tfh cell differentiation through SAP (SLAM associated protein)-mediated signaling. Cytokines, IL-6 and IL-21 contribute to Tfh cell differentiation via upregulation of BCL-6. The cross-talk between T and B cells in the GC is bi-directional mediated by ligand-receptor interactions, soluble mediators (cytokines). Biologics targeting these signals can modulate post-transplant humoral response.
As shown in figure 1, the T cells located at the T:B border are considered to be precursors of Tfh cells, which briefly express some of the Tfh cell-associated markers. It is believed that these cells initiate primed B cell proliferation and differentiation. Only once B cells receive the described activation signals, will they proliferate and differentiate along the both follicular and extrafollicular pathway32. While some fully differentiate into short-lived plasma cells and memory B cells (via the extrafollicular pathway) others move through the dark zone (centroblasts; CXCR4+CD83+CD86+) into the light zone of the germinal center (GC) via chemokine receptor CXCR5 (binding its ligand CXCL13; Figure 1). These B cells (known as centrocytes; CXCR4−CD83+CD86+) have already experienced somatic hypermutation (SHM) and interact with follicular dendritic cells (FDC) and Tfh cells. Selected B cell clones, via the cognate interaction with Tfh cells, differentiate into plasma cells (short-lived and long-lived) and memory B cells or, alternatively, some migrate back to the dark zone for further proliferation8,33. It is notable that memory B cells emerge earlier than plasmablast with less Tfh cell requirement34,35. Clonal expansion of these cells, to become the hyperplastic GC, occurs as result of their interaction with cognate-follicular helper T (Tfh: CXCR5+ PD-1hiICOS+ CD4+) cells, via CD40 signaling and IL-2136. Further costimulation signaling, via ICOS and PD-1 interactions with ICOS-L and PD-L1/L2 on the B cell provides optimal signals for hyperplastic GC formation and antibody production37–39. Defects of these surface molecules in human have been shown to result in impaired GC formation and an improper antibody response37,38,40,41.
CD28 and CTLA4 interactions to CD80 or CD86 on B cells are involved in both positive and negative regulation of B cells. Signaling of CD28 via CD86 promotes B cell proliferation and Ig class switching, while interaction of CD28 to CD80 inhibits this response42,43. CTLA4 counteracts the CD28 signal by binding to CD80/86 with higher affinity44. In transplantation, the efficacy of CTLA4-Ig (Belatacept) to suppress the anti-donor humoral response has been demonstrated45–48. However, like to ICOS and PD-1, it is still unclear if this costimulation signal is critical for T-B cell cooperation directly, or whether the mode of action is predominantly by limiting Tfh cell or B cell function/proliferation.
The costimulation interactions described between T & B cells require additional binding to provide physical stabilisation. Initially this is by adhesion molecules, LFA-1 and ICAM, however subsequent maintenance of the T-B conjugation is dependent on SLAM-associated protein interactions, including CD8449. Targeting these interactions with an anti-LFA-1mAb also significantly reduces both alloantibody production as well as the GC formation (manuscript in preparation). Additionally CD84 deficiency has been shown to result in an impaired humoral response in mice49.
Within the germinal center, cytokines (IL-6 and IL-21) remain crucial for further B cell differentiation50. Tfh cells are the major source of IL-21. Both Tfh cells and GC-B cells express IL-21 receptors. IL-21 signaling in GC-B cells promotes proliferation, plasma cell differentiation, and antibody production51–53. IL-21 signaling also stimulates Tfh formation54,55. IL-6 provided by dendritic cells (DC, including Follicular DC) induces IL-21 production from Tfh cells56. Interestingly, IL-6 production from DC is enhanced after IFN-γ activation57. The role of IFN-γ may be very limited since the BCL-6 represses IFN-γ expression. It also has been shown that Tfh cells produce less IFN- γ15,58.From the auto-immune literature, it would appear that IFN-γ promotes BAFF production from myeloid cells that may be indirectly involved in the GC response59. Cancro and colleagues elegantly showed that within the GC, a further role of BAFF produced by Tfh cells for GC B cells60,61. In transplantation, the role of BAFF is a developing field and its effect on Tfh within the GC remains to be fully elucidated.
3.2. Distinct T cell subtypes in the Germinal Centre
Tfh cells are known to be the key helper T cell phenotype however the mechanism of Tfh cells in GC homeostasis is incompletely understood. Here, we briefly outline the other known T cell phenotypes involved in the process:
T follicular regulatory cell (Tfr)
The selection of GC-B cells expressing high affinity variants of BCR via cognate Tfh cells prevents an irrelevant germinal center response. However this does not explain the control of possible cross-reactive GC-B cells which can recognize both target and self-antigen. More recently, CXCR5 expressing T reg (FoxP3+) cells (T follicular regulatory cells; Tfr) have been identified in the germinal center62–64. Like Tfh cells, the high surface expression of CXCR5 is a useful marker to identify the subset of Tfr cells involved in regulation of germinal center in secondary lymphoid organ65. The Tfr cells share a similar genetic profile to Tfh cells and Treg cells including BCL-6, FoxP3, CXCR5, PD-1, ICOS and CTLA-4. An important distinguishing feature is that the Tfr does not express certain molecules necessary for B cell help such as CD40L, IL-4 and IL-2163. A lack of Tfr promotes increased Tfh, GC-B cells, and antibody secreting cells62. However, the relevance of these cells in transplantation is not fully elucidated, and it is still unclear how these Tfr affect the GC response.
CD8 T cells in humoral response
The other notable cell population involved in the GC response is CD8 T cells. It has been shown that a fraction of the CD8 T cell population suppresses B cell response66. More recently, CD8+ regulatory T cells which are crucial for the maintenance of self tolerance in the GC were identified in autoimmune disease models.67 These suppressive CD8 T cells do not share common developmental pathway with CD4 Treg cells. Unlike Tfr, CD8 regulatory cells in the GC express ICOS ligand (ICOS-L) but they do not express ICOS or PD-168. However, they are both dependent on the transcription factor Helios to maintain suppressive phenotype69. In transplantation, Bumgardner and colleagues also observed the role of CD8 T cells in alloantibody reduction70. In their model, allo-primed CD8 T cells targeted allo-primed B cells via perforin and FasL in a antigen specific manner71.
4. Kinetics of GC development after organ transplantation
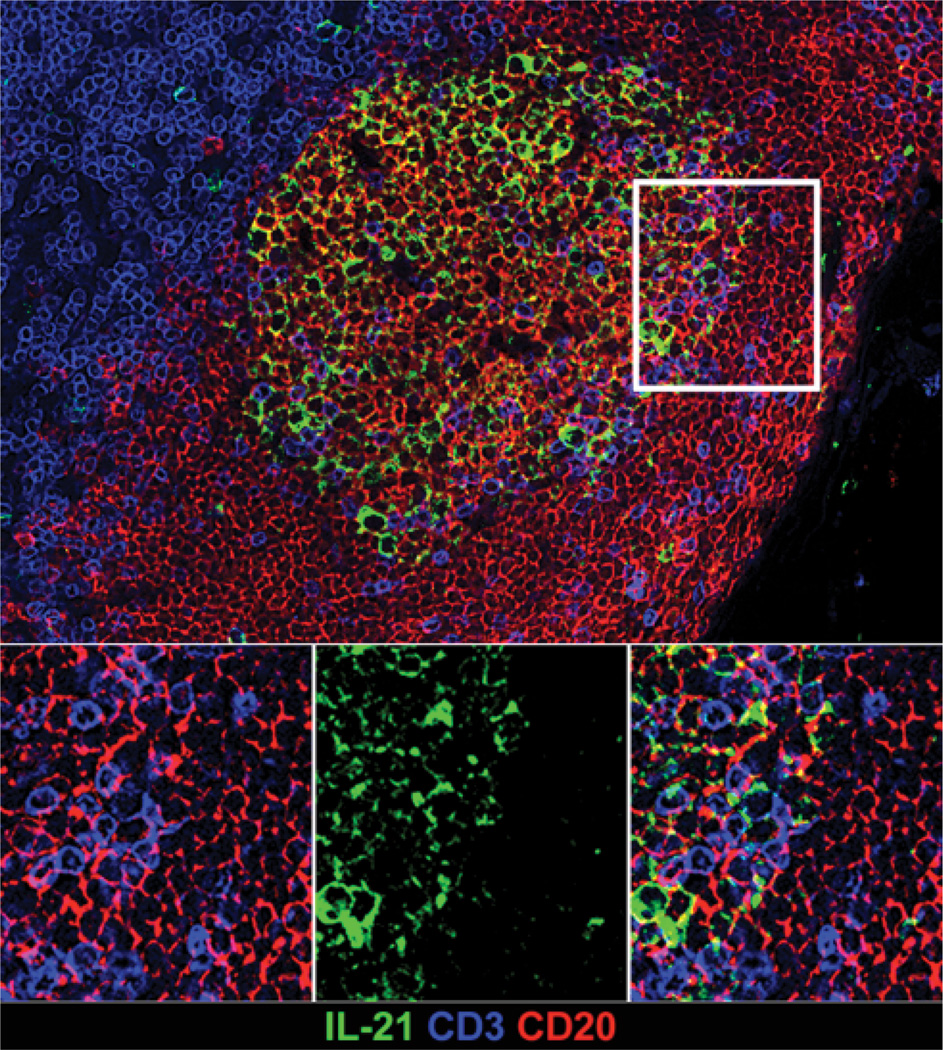
The GC response after organ transplantation has not been fully described, this is mostly due to scarcity of post-transplant samples of secondary lymphoid samples in human patients. The GC is, however, an important site of interaction between T & B cells, which has been investigated more thoroughly in animal models. In nonhuman primate model, we have traced the in vivo GC response with immunohistochemical analysis. The GC-associated Tfh cell has been also visualized via PD-1 and their functional cytokine, IL-21 in rhesus macque (Figure 3)72,73. Interestingly, we did not see an impressive development of GC after skin transplantation in spite of DSA elevation (Data not shown). It is partially because the base line level of GC response is high in monkeys since it is not germ-free animals. The robust Th1 immune reponse, especially IL-2, induced by skin transplantation (without immunosuppression) may also limit the Tfh cell differntiation18. IL-2 represses Tfh cell differentiation by upregulating BLIMP-1, a transcription factor that is mutually antagonistic to BCL-6, which is critical for Tfh cell differentitation..
FIGURE 3. In situ IL-21 staining in the GC.
IL-21 expression is increased in hyperplastic follicles during antibody-mediated rejection. Representative immunofluorescence image of GC staining with CD3 (Blue), CD20 (Red), IL-21 (green) in lymph node of rhesus macaque.
We have developed a NHP AMR model which mimics clinical observations seen with alemtuzumab. Cai et al found that 42% of their alemtuzumab and sirolimus treated renal transplant recipients developed HLA antibodies, 60% of which were donor-specific74. Other studies have observed more frequent occurrences of acute antibody-mediated rejection after renal transplantation with alemtuzumab induction75–78. We treated our monkeys with CD3-Immunotoxin, Alefacept (LFA-3-Ig; anti-CD2 mAb), and tacrolimus79. Comparing this combination therapy to those monkeys treated with CD3-Immunotoxin and tacrolimus alone, we found that Alefacept treatment resulted in significant production of de novo antibody. Since Kirk and colleagues showed that higher CD2 expression on activated (or memory) CD8 T cells80,81, our findings45,79,82, support Bumgardner’s work on the role of CD8 T cells in GC regulation, as previously described.
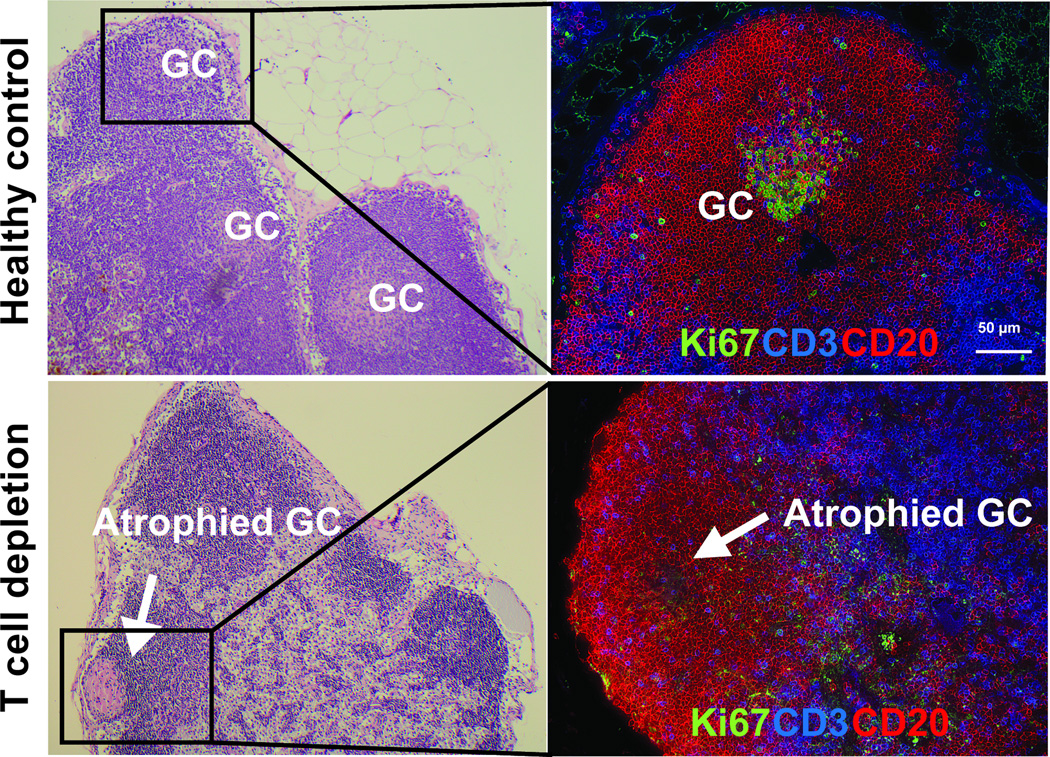
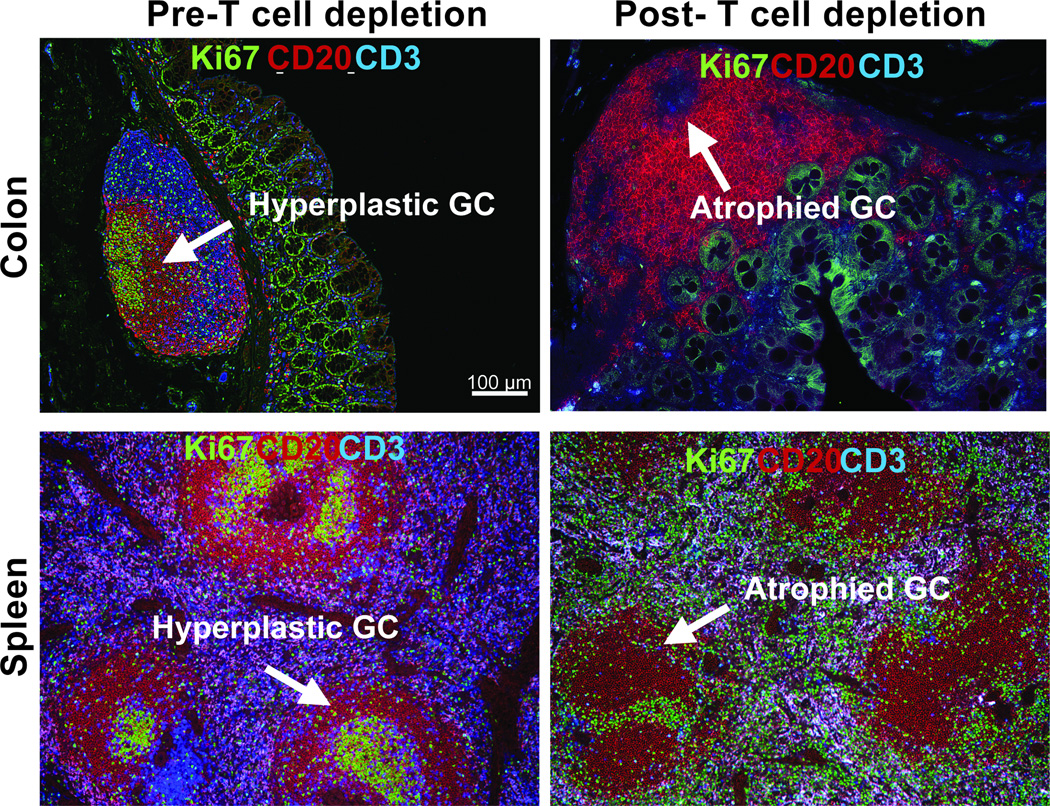
We have also assessed T cell depletion in different immune-compartments and GC of the secondary lymphoid organs following CD3-immunotoxin. We found that GC size and frequency are highly correlated to both DSA production and AMR score45,82. In the AMR-inducing model, T cell depletion allowed us to study the reconstruction of GC after eradication due to the depletional therapy. GC areas containing proliferating B cells (Ki67+) were measured using Hoechst staining of nuclei, demonstrating markedly less focal staining than the smaller marginal B cells72,73. In kidney transplantation, we found that T cell depletion results in elimination of GC in the first week after transplantation (Figure 4). There was also an absence of visible GC in the spleen and peyer’s patches within the gut (Figure 5). In addition, systemic T cell depletion resulted in a reduction in the circulating number of B cells, despite the B cell follicle remaining intact. This suggests that, in the nondepleted steady state, B cells from the GC contribute to circulating B cell numbers45,82.
FIGURE 4. Eradication of GC in the lymph node after T cell depletion.
Representative H&E (left) and immunofluorescence image (right) of GC staining with CD3 (Blue), CD20 (Red), Ki67 (green) in lymph node of rhesus macaque. Upper panels show sections of LN from healthy control with GCs and lower panels show atrophied GC (white arrow) after T cell depletion.
FIGURE 5. Disrupted GC after T cell depletion in spleen and colon.
Representative IHC panels show sections of colon (Upper panel) and Spleen (lower panel) from before and After T cell depletion with large lymphoid aggregation (Peyer’s patch) stained with Ki67, CD20, and CD3 antibodies. (A) Similar to the lymph node, Peyer’s patch and spleen comprises T cell area and B cell follicle with germinal center containing large proliferating B cells. (B) GC in payer’s patch in the descending colon and spleen of rhesus macaques were disrupted after T cell depletion.
Immunohistochemistry within the B cell follicles this early after transplantation with T cell depletion, showed no evidence of T-or proliferating B cells (Ki67). The GC-like structures without cell components may represent the effect of rapid T cell depletion on the GC (Figure 4 and 5). However at this stage, although very few T cells were identified in the B cell follicle, residual T cells in the medulla appear more evident.
By 2–4 weeks post transplantation, the GC shows evidence of rapid reconstruction. Within the medulla, there is clear evidence of T cell presence, with small numbers of T cells detectable in the B cell follicle and germinal center. It would appear that, following T cell depletion, repopulation of the T cell occurs in the LN before the circulation. Supporting this finding, Kirk et al also showed that any remaining T cells after Alemtuzumab treatment are found in the lymph node, specifically the mantle zone83. Of note in the NHP model, T cells are not fully removed by T cell depletion79.
In a mouse model of chronic AMR, using human CD52 transgenic mice84, following alemtuzumab treatment, we also demonstrated eradication of the GC with residual T cells in the LN (MS in preparation). This mouse model also showed that T cells in the LN were more resistant to those in spleen (Data not shown). Like our NHP observations, it is notable that there was more remaining T cells and faster repopulation in the lymph node compartments compared to spleen. We currently don’t know what the driving force of GC reconstruction is, under the current immunosuppressive regimen. We speculate that CNI based regimen does not efficiently suppress Tfh cell during homeostatic repopulation. It might be due to their great efficacy on suppressing Th1 response. It is also possible that Tfh cells are relatively spared by depletional induction due to their physical location (surrounded by densely populated B cells in GC). These remnant Tfh cells (or memory Tfh cells) could repopulate relatively faster under the lack of Th1 immune response. Currently we are further analyzing these T cells in the GC, in order to discover what type of T cell sub-population they represent.
By 30 days after transplantation, recipients treated with CD3-IT with either tacrolimus or rapamycin showed GCs which are similar to the naïve animals. In the spleen and gut, GC reconstruction was negligible. This suggests that it is the residual T cells, following depletion, which contribute to GC reconstruction. In our AMR-model, with considerable immunosuppression, we found that in conjunction with elevated DSA, the rebound increase in GC size and frequency at later time points exceeded baseline. This finding suggests that T-B interactions in the germinal center can be completely eradicated by current cytolytic induction. However, repopulating Tfh cells within the germinal center provide B cell help, despite potent immunosuppression to control T cell mediated rejection.
5. Ectopic GC (Tertiary Structure) in Transplantation
In addition to the changes within hyperplastic Germinal Centre, it is known that germinal center-like structures develop in transplanted organs (kidney, lung tx). These ectopic intragraft GCs (also known as tertiary lymphoid organs) appear during chronic rejection, however, their role in graft rejection is debated. Originally, it was believed that they were related to rejection response by providing both a humoral response85 and/or allo-T cell priming86 directly at the site of alloantigens. Clinically, it is also been suggested that ectopic germinal centers correlate with poor survival87. However, these ectopic GC have also been found in transplanted organs with no evidence of dysfunction88.
In nonhuman primate kidney transplantation model, we have made similar demonstrations of ectopic GCs in kidney transplant recipients in whom immunosuppressive drug therapy has been discontinued after initial long-term treatment. We observed that the tertiary GC structure developed rapidly in conjunction with graft rejection. However, even with well-developed T and B cell zones, there was no evidence of a B cell clonal expansion (Data not shown).
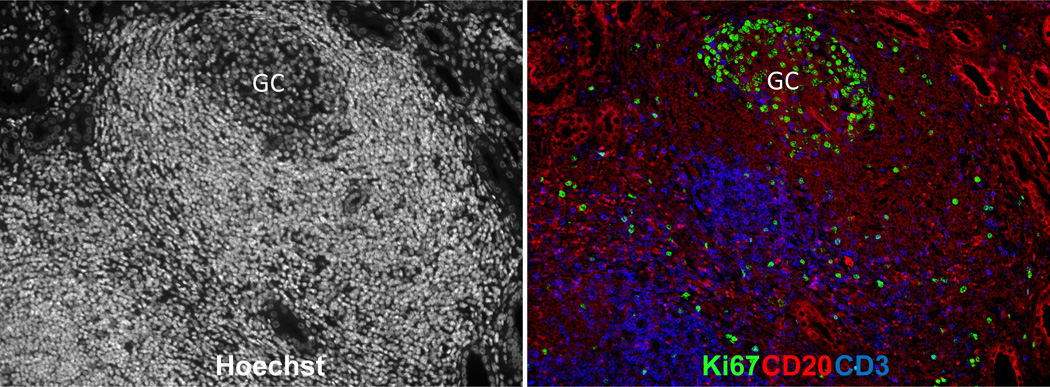
We also found evidence of ectopic GC within a well-functioning graft after drug discontinuation. These ectopic GCs are composed of T and B cells with often hyperplastic GC (showing B cell clonal expansion), although there was no evidence of circulating DSA. As found in other lymphoid organs including lymph nodes, spleen and payer’s patch (figure 4 and 5), GCs in the tertiary lymphoid aggregates are clearly identifiable based on their typical architecture. Staining of ectopic GC within the graft showed Ki67+B cells (Figure 6). We also observed an inverse BAFF staining pattern which suggests a consumption of BAFF in the GC-B cells in the ectopic GC – a finding which was also demonstrated in the hyperplastic GCs (data not shown). It remains unclear which factors mediate the differential GC morphologies in the graft after discontinuation of immunosuppression. Further analysis of T and B cells in the ectopic and hyperplastic GCs in well functioning (tolerant) nonhuman primate kidney recipient is likely to provide an insight on how these structures regulate the alloimmune response in recipients with long-term graft function and survival.
FIGURE 6. Ectopic Germinal Center in well-functioning graft.
Representative GC response in the well-functioning kidney graft. Immunological profiles of Hoechst (left), CD20/CD3/Ki67 positive cells (right) within kidney graft section from renal transplant rhesus recipients. The sections were stained with hoechst dye (white), CD3 (Blue), CD20 (Red), and Ki67 (green) antibodies.
6. Possible drug interventions on T:B cross talk in transplantation
There are a number of drug therapies which have the ability to influence this crosstalk between T and B cells.
6. 1. Costimulation blockade
Co-stimulation pathway blockade has been in use in preclinical and clinical transplantation for some time89. Belatacept is a second generation fusion protein (CTLA4-Ig) which blocks the CD28/CTL4:CD80/86 costimulation axis, and has been licensed for use in transplantation as maintenance therapy since 2011. Clinically, a Cochrane review has found that there is no difference in effectiveness of belatacept, compared to CNI based maintenance, with respect to graft rejection or survival, although it is less nephrotoxic than CNI90. This review however acknowledges that the evidence so far has not fully evaluated the role of belatacept in transplantation, particularly with respect to costimulation blockade resistant rejection. Of pertinent interest, in a recent paper based on an alemtuzumab, belatacept, rapamycin based regimen in human kidney transplantation, it has been shown that, following depletional induction, the rapidly repopulating B cell phenotype is predominantly naïve and regulatory in nature47.
CD40 ligand pathway inhibitors are also currently of interest in preclinical models of transplantation91. In a case report of liver transplantation in a patient with CD40L deficiency, it was been noted that although B cell immunity is severely compromised due to CD40L being required for B cell activation, germinal center formation and class switching, the lack of CD40L on T- and NK-cells did not result in any differences in T cell and NK-cell responses early after transplantation92. In NHP models of transplantation, using CD40L blockade (Chi220) resulted in prolonged graft function, and peripheral B cell depletion, although this was associated with severe systemic CMV infection93. We have investigated CD40L (2C10) blockade, in conjunction with belatacept and, as described above in our AMR inducing model, and noted decreased DSA production, and suppression of the GC response45. To date, no human studies of CD40 inhibition in transplantation are available.
Although anti-LFA1 blockade is appealing, Efalizumab (Anti LFA-1 blocking monoclonal antibody) has been used in a Phase I/II trial human kidney transplantation, where although the graft rejection rates were low, and mild, higher dose treatment was associated with PTLD94. Anti-LFA-1 has been also used in combination with belatacept in an NHP model of renal transplantation where it failed to significantly prolong graft survival95. Efalizumab is also no longer commercially available.
6. 2. Modulation of B cell development via B-lymphocyte stimulator/BAFF or APRIL pathways
Belimumab (Benlysta), is a fully human IgG1 monoclonal antibody directed against circulating B-lymphocyte stimulation factor (BLyS) or B cell activating factor (BAFF) which binds soluble human BLyS is currently in clinical use in autoimmune disease.
Atacicept is a fusion protein which targets not only BLyS, but also APRIL pathways. Again, clinical use to date has been reserved to autoimmune indications, and outcomes have been somewhat controversial96. However, as discussed in our NHP models, in a T cell depletion model, using Taci-Ig, successfully reduced the DSA response82.
Summary.
The role of crosstalk between B & T cells is increasingly recognized as being an important in the activation of the B cell, and development of the humoral response in transplantation. In particular, this cross talk is vital for the development of the Germinal Center. There are multiple pharmaceutical possibilities for intervention, although further studies in preclinical transplant models are necessary to fully evaluate the mechanisms described.
Acknowledgments
We would like to thank Lauren Halligan (Department of Surgery, Duke University) for her contribution creating the illustration in the manuscript.
Funding
The work in this paper is supported in part by grants: NIH U01 AI074635 (SJK), NIH U19 AI051731 (SJK), and AHA Enduring Hearts Foundation Research Award 15SDG25710165 (JK).
Footnotes
Author Contribution
J.K. participated in the concept, manuscript writing, figures drawing. M.M. participated in the concept, manuscript co-writing. E.P, C.B, and J.H. participated in manuscript co-writing. S.J.K participate in the concept, manuscript writing.
Disclosure
The authors of this manuscript have no conflicts of interest to disclose
References
- 1.Lund FF, Randall TD. Effector and regulatory B cells: modulators of CD4+ T cell immunity. Nat Rev Immunol. 2010;10:236–247. doi: 10.1038/nri2729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwun J, Knechtle SJ. Overcoming Chronic Rejection-Can it B? Transplantation. 2009;88:955–961. doi: 10.1097/TP.0b013e3181b96646. [DOI] [PubMed] [Google Scholar]
- 3.van Zelm MC, Reisli I, van der Burg M, et al. An antibody-deficiency syndrome due to mutations in the CD19 gene. N Engl J Med. 2006;354:1901–1912. doi: 10.1056/NEJMoa051568. [DOI] [PubMed] [Google Scholar]
- 4.van Zelm MC, Smet J, Adams B, et al. CD81 gene defect in humans disrupts CD19 complex formation and leads to antibody deficiency. J Clin Invest. 2010;120:1265–1274. doi: 10.1172/JCI39748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thiel J, Kimmig L, Salzer U, et al. Genetic CD21 deficiency is associated with hypogammaglobulinemia. J Allergy Clin Immunol. 2012;129:801–810. e806. doi: 10.1016/j.jaci.2011.09.027. [DOI] [PubMed] [Google Scholar]
- 6.Mitchison A. Latent help to and from H-2 antigens. Eur J Immunol. 1992;22:123–127. doi: 10.1002/eji.1830220119. [DOI] [PubMed] [Google Scholar]
- 7.Mitchison NA. T cell-B-cell cooperation. Nat Rev Immunol. 2004;4:308–312. doi: 10.1038/nri1334. [DOI] [PubMed] [Google Scholar]
- 8.MacLennan IC. Germinal centers. Annu Rev Immunol. 1994;12:117–139. doi: 10.1146/annurev.iy.12.040194.001001. [DOI] [PubMed] [Google Scholar]
- 9.Durandy A, Kracker S, Fischer A. Primary antibody deficiencies. Nat Rev Immunol. 2013;13:519–533. doi: 10.1038/nri3466. [DOI] [PubMed] [Google Scholar]
- 10.van Zelm MC, Bartol SJ, Driessen GJ, et al. Human CD19 and CD40L deficiencies impair antibody selection and differentially affect somatic hypermutation. J Allergy Clin Immunol. 2014;134:135–144. doi: 10.1016/j.jaci.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Yin H, Xu J, et al. Reversing endogenous alloreactive B cell GC responses with anti-CD154 or CTLA-4Ig. Am J Transplant. 2013;13:2280–2292. doi: 10.1111/ajt.12350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haanstra KG, Ringers J, Sick EA, et al. Prevention of kidney allograft rejection using anti-CD40 and anti-CD86 in primates. Transplantation. 2003;75:637–643. doi: 10.1097/01.TP.0000054835.58014.C2. [DOI] [PubMed] [Google Scholar]
- 13.Schmitt N, Morita R, Bourdery L, et al. Human dendritic cells induce the differentiation of interleukin-21-producing T follicular helper-like cells through interleukin-12. Immunity. 2009;31:158–169. doi: 10.1016/j.immuni.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leonard WJ. Cytokines and immunodeficiency diseases. Nat Rev Immunol. 2001;1:200–208. doi: 10.1038/35105066. [DOI] [PubMed] [Google Scholar]
- 15.Yu D, Rao S, Tsai LM, et al. The transcriptional repressor Bcl-6 directs T follicular helper cell lineage commitment. Immunity. 2009;31:457–468. doi: 10.1016/j.immuni.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Johnston RJ, Poholek AC, DiToro D, et al. Bcl6 and Blimp-1 are reciprocal and antagonistic regulators of T follicular helper cell differentiation. Science. 2009;325:1006–1010. doi: 10.1126/science.1175870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nurieva RI, Chung Y, Martinez GJ, et al. Bcl6 mediates the development of T follicular helper cells. Science. 2009;325:1001–1005. doi: 10.1126/science.1176676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ballesteros-Tato A, León B, Graf BA, et al. Interleukin-2 inhibits germinal center formation by limiting T follicular helper cell differentiation. Immunity. 2012;36:847–856. doi: 10.1016/j.immuni.2012.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roozendaal R, Carroll MC. Complement receptors CD21 and CD35 in humoral immunity. Immunological reviews. 2007;219:157–166. doi: 10.1111/j.1600-065X.2007.00556.x. [DOI] [PubMed] [Google Scholar]
- 20.Fearon DT, Locksley RM. The Instructive Role of Innate Immunity in the Acquired Immune Response. Science. 1996;272:50–54. doi: 10.1126/science.272.5258.50. [DOI] [PubMed] [Google Scholar]
- 21.Dempsey PW, Allison MED, Akkaraju S, Goodnow CC, Fearon DT. C3d of Complement as a Molecular Adjuvant: Bridging Innate and Acquired Immunity. Science. 1996;271:348–350. doi: 10.1126/science.271.5247.348. [DOI] [PubMed] [Google Scholar]
- 22.Treml JF, Hao Y, Stadanlick JE, Cancro MP. The BLyS Family: Toward a Molecular Understanding of B Cell Homeostasis. Cell Biochem Biophys. 2009;53:1–16. doi: 10.1007/s12013-008-9036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vincent FB, Saulep-Easton D, Figgett WA, Fairfax KA, Mackay F. The BAFF/APRIL system: emerging functions beyond B cell biology and autoimmunity. Cytokine Growth Factor Rev. 2013;24:203–215. doi: 10.1016/j.cytogfr.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Groom JR, Fletcher CA, Walters SN, et al. BAFF and MyD88 signals promote a lupuslike disease independent of T cells. J Exp Med. 2007;204:1959–1971. doi: 10.1084/jem.20062567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vinuesa CGMICM. Antibody Responses to Polysaccarides. New York: Kluwer Academic; 2003. [Google Scholar]
- 26.Crotty S. Follicular helper CD4 T cells (TFH) Annu Rev Immunol. 2011;29:621–663. doi: 10.1146/annurev-immunol-031210-101400. [DOI] [PubMed] [Google Scholar]
- 27.Tangye SG, Ma CS, Brink R, Deenick EK. The good, the bad and the ugly - TFH cells in human health and disease. Nat Rev Immunol. 2013;13:412–426. doi: 10.1038/nri3447. [DOI] [PubMed] [Google Scholar]
- 28.Haynes NM, Allen CD, Lesley R, et al. Role of CXCR5 and CCR7 in follicular Th cell positioning and appearance of a programmed cell death gene-1high germinal center-associated subpopulation. J Immunol. 2007;179:5099–5108. doi: 10.4049/jimmunol.179.8.5099. [DOI] [PubMed] [Google Scholar]
- 29.Kim CH, Rott LS, Clark-Lewis I, et al. Subspecialization of CXCR5+ T cells: B helper activity is focused in a germinal center-localized subset of CXCR5+ T cells. J Exp Med. 2001;193:1373–1381. doi: 10.1084/jem.193.12.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ansel KM, McHeyzer-Williams LJ, Ngo VN, McHeyzer-Williams MG, Cyster JG. In vivo-activated CD4 T cells upregulate CXC chemokine receptor 5 and reprogram their response to lymphoid chemokines. J Exp Med. 1999;190:1123–1134. doi: 10.1084/jem.190.8.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Linterman MA, Rigby RJ, Wong R, et al. Roquin differentiates the specialized functions of duplicated T cell costimulatory receptor genes CD28 and ICOS. Immunity. 2009;30:228–241. doi: 10.1016/j.immuni.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 32.Lee SK, Rigby RJ, Zotos D, et al. B cell priming for extrafollicular antibody responses requires Bcl-6 expression by T cells. J Exp Med. 2011;208:1377–1388. doi: 10.1084/jem.20102065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Victora GD, Schwickert TA, Fooksman DR, et al. Germinal center dynamics revealed by multiphoton microscopy with a photoactivatable fluorescent reporter. Cell. 2010;143:592–605. doi: 10.1016/j.cell.2010.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shinnakasu R1,2, Inoue T1, Kometani K2, et al. Regulated selection of germinal-center cells into the memory B cell compartment. Nat Immunol. 2016;17:861–869. doi: 10.1038/ni.3460. [DOI] [PubMed] [Google Scholar]
- 35.Weisel FJ, Zuccarino-Catania GV, Chikina M, Shlomchik MJ. A Temporal Switch in the Germinal Center Determines Differential Output of Memory B and Plasma Cells. Immunity. 2016;44:116–130. doi: 10.1016/j.immuni.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chtanova T, Tangye SG, Newton R, et al. T follicular helper cells express a distinctive transcriptional profile, reflecting their role as non-Th1/Th2 effector cells that provide help for B cells. J Immunol. 2004;173:68–78. doi: 10.4049/jimmunol.173.1.68. [DOI] [PubMed] [Google Scholar]
- 37.Good-Jacobson KL, Szumilas CG, Chen L, et al. PD-1 regulates germinal center B cell survival and the formation and affinity of long-lived plasma cells. Nat Immunol. 2010;11:535–542. doi: 10.1038/ni.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kawamoto S, et al. The inhibitory receptor PD-1 regulates IgA selection and bacterial composition in the gut. Science. 2012;336:485–489. doi: 10.1126/science.1217718. [DOI] [PubMed] [Google Scholar]
- 39.Bauquet AT, Jin H, Paterson AM, et al. The costimulatory molecule ICOS regulates the expression of c-Maf and IL-21 in the development of follicular T helper cells and TH-17 cells. Nat Immunol. 2009;10:167–175. doi: 10.1038/ni.1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grimbacher B, Hutloff A, Schlesier M, et al. Homozygous loss of ICOS is associated with adult-onset common variable immunodeficiency. Nat Immunol. 2003;4:261–268. doi: 10.1038/ni902. [DOI] [PubMed] [Google Scholar]
- 41.Warnatz K, Bossaller L, Salzer U, et al. Human ICOS deficiency abrogates the germinal center reaction and provides a monogenic model for common variable immunodeficiency. Blood. 2006;107:3045–3052. doi: 10.1182/blood-2005-07-2955. [DOI] [PubMed] [Google Scholar]
- 42.Jeannin P, Delneste Y, Lecoanet-Henchoz S, et al. CD86 (B7-2) on human B cells. A functional role in proliferation and selective differentiation into IgE- and IgG4-producing cells. J Biol Chem. 1997;272:15613–15619. [Google Scholar]
- 43.Suvas S, Singh V, Sahdev S, Vohra H, Agrewala JN. Distinct role of CD80 and CD86 in the regulation of the activation of B cell and B cell lymphoma. J Biol Chem. 2002;277:7766–7775. doi: 10.1074/jbc.M105902200. [DOI] [PubMed] [Google Scholar]
- 44.Walker LS, Sansom DM. The emerging role of CTLA4 as a cell-extrinsic regulator of T cell responses. Nat Rev Immunol. 2011;11:852–863. doi: 10.1038/nri3108. [DOI] [PubMed] [Google Scholar]
- 45.Kim EJ, Kwun J, Gibby AC, et al. Costimulation blockade alters germinal center responses and prevents antibody-mediated rejection. Am J Transplant. 2014;14:59–69. doi: 10.1111/ajt.12526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Badell IR, Russell MC, Cardona K, et al. CTLA4Ig prevents alloantibody formation following nonhuman primate islet transplantation using the CD40-specific antibody 3A8. Am J Transplant. 2012;12:1918–1923. doi: 10.1111/j.1600-6143.2012.04029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu H, et al. Postdepletion Lymphocyte Reconstitution During Belatacept and Rapamycin Treatment in Kidney Transplant Recipients. Am J Transplant. 2016;16:550–564. doi: 10.1111/ajt.13469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Young JS, Chen J, Miller ML, et al. Delayed Cytotoxic T Lymphocyte-Associated Protein 4-Immunoglobulin Treatment Reverses Ongoing Alloantibody Responses and Rescues Allografts From Acute Rejection. Am J Transplant. 2016;16:2312–2323. doi: 10.1111/ajt.13761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cannons JL, Qi H, Lu KT, et al. Optimal germinal center responses require a multistage T cell:B cell adhesion process involving integrins: SLAM-associated protein, and CD84. Immunity. 2010;32:253–265. doi: 10.1016/j.immuni.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eto D, Lao C, DiToro D, et al. IL-21 and IL-6 are critical for different aspects of B cell immunity and redundantly induce optimal follicular helper CD4 T cell (Tfh) differentiation. PLoS One. 2011;6:e17739. doi: 10.1371/journal.pone.0017739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Recher M, Berglund LJ, Avery DT, et al. IL-21 is the primary common gamma chain-binding cytokine required for human B-cell differentiation in vivo. Blood. 2011;118:6824–6835. doi: 10.1182/blood-2011-06-362533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Linterman MA, Beaton L, Yu D, et al. IL-21 acts directly on B cells to regulate Bcl-6 expression and germinal center responses. J Exp Med. 207:353–363. doi: 10.1084/jem.20091738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zotos D, et al. IL-21 regulates germinal center B cell differentiation and proliferation through a B cell-intrinsic mechanism. J Exp Med. 2010;207:365–378. doi: 10.1084/jem.20091777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nurieva RI, Chung Y, Hwang D, et al. Generation of T follicular helper cells is mediated by interleukin-21 but independent of T helper 1, 2, or 17 cell lineages. Immunity. 2008;29:138–149. doi: 10.1016/j.immuni.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vogelzang A, McGuire HM, Yu D, et al. A fundamental role for interleukin-21 in the generation of T follicular helper cells. Immunity. 2008;29:127–137. doi: 10.1016/j.immuni.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 56.Karnowski A, Chevrier S, Belz GT, et al. B and T cells collaborate in antiviral responses via IL-6, IL-21, and transcriptional activator and coactivator, Oct2 and OBF-1. J Exp Med. 2012;209:2049–2064. doi: 10.1084/jem.20111504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Clark EA, Grabstein KH, Shu GL. Cultured human follicular dendritic cells. Growth characteristics and interactions with B lymphocytes. J Immunol. 1992;148:3327–3335. [PubMed] [Google Scholar]
- 58.Oestreich KJ, Huang AC, Weinmann AS. The lineage-defining factors T-bet and Bcl-6 collaborate to regulate Th1 gene expression patterns. J Exp Med. 2011;208:1001–1013. doi: 10.1084/jem.20102144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harigai M, Kawamoto M, Hara M, et al. Excessive production of IFN-gamma in patients with systemic lupus erythematosus and its contribution to induction of B lymphocyte stimulator/B cell-activating factor/TNF ligand superfamily-13B. J Immunol. 2008;181:2211–2219. doi: 10.4049/jimmunol.181.3.2211. [DOI] [PubMed] [Google Scholar]
- 60.Goenka R, Scholz JL, Sindhava VJ, Cancro MP. New roles for the BLyS/BAFF family in antigen-experienced B cell niches. Cytokine Growth Factor Rev. 2014;25:107–113. doi: 10.1016/j.cytogfr.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Goenka R, et al. Local BLyS production by T follicular cells mediates retention of high affinity B cells during affinity maturation. J Exp Med. 2014;211:45–56. doi: 10.1084/jem.20130505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chung Y, Tanaka S, Chu F, Nurieva RI, et al. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nat Med. 2011;17:983–988. doi: 10.1038/nm.2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Linterman MA, Pierson W, Lee SK, et al. Foxp3+ follicular regulatory T cells control the germinal center response. Nat Med. 2011;17:975–982. doi: 10.1038/nm.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wollenberg I, Agua-Doce A, Hernández A, et al. Regulation of the germinal center reaction by Foxp3+ follicular regulatory T cells. J Immunol. 2011;187:4553–4560. doi: 10.4049/jimmunol.1101328. [DOI] [PubMed] [Google Scholar]
- 65.Yu D, Vinuesa CG. The elusive identity of T follicular helper cells. Trends Immunol. 2010;31:377–383. doi: 10.1016/j.it.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 66.Noble A, Zhao ZS, Cantor H. Suppression of immune responses by CD8 cells. II. Qa-1 on activated B cells stimulates CD8 cell suppression of T helper 2 responses. J Immunol. 1998;160:566–571. [PubMed] [Google Scholar]
- 67.Kim HJ, Verbinnen B, Tang X, Lu L, Cantor H. Inhibition of follicular T-helper cells by CD8(+) regulatory T cells is essential for self tolerance. Nature. 2010;467:328–332. doi: 10.1038/nature09370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim HJ1, Wang X, Radfar S, et al. CD8+ T regulatory cells express the Ly49 Class I MHC receptor and are defective in autoimmune prone B6-Yaa mice. Proc Natl Acad Sci U S A. 2011;108:2010–2015. doi: 10.1073/pnas.1018974108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim HJ, Barnitz RA, Kreslavsky T, et al. Stable inhibitory activity of regulatory T cells requires the transcription factor Helios. Science. 2015;350:334–339. doi: 10.1126/science.aad0616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zimmerer JM, Pham TA, Sanders VM, Bumgardner GL. CD8+ T cells negatively regulate IL-4-dependent, IgG1-dominant posttransplant alloantibody production. J Immunol. 2010;185:7285–7292. doi: 10.4049/jimmunol.1001655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zimmerer JM, Horne PH, Fiessinger LA, et al. Inhibition of recall responses through complementary therapies targeting CD8+ T-cell- and alloantibody-dependent allocytotoxicity in sensitized transplant recipients. Cell Transplant. 2013;22:1157–1169. doi: 10.3727/096368912X657350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hong JJ, Amancha PK, Rogers K, Ansari AA, Villinger F. Spatial alterations between CD4(+) T follicular helper, B, and CD8(+) T cells during simian immunodeficiency virus infection: T/B cell homeostasis, activation, and potential mechanism for viral escape. J Immunol. 2012;188:3247–3256. doi: 10.4049/jimmunol.1103138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hong JJ, Amancha PK, Rogers KA, et al. Early lymphoid responses and germinal center formation correlate with lower viral load set points and better prognosis of simian immunodeficiency virus infection. J Immunol. 2014;193:797–806. doi: 10.4049/jimmunol.1400749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cai J, et al. Correlation between human leukocyte antigen antibody production and serum creatinine in patients receiving sirolimus monotherapy after Campath-1H induction. Transplantation. 2004;78:919–924. doi: 10.1097/01.tp.0000134398.86243.81. [DOI] [PubMed] [Google Scholar]
- 75.Knechtle SJ, Pirsch JD, H Fechner J, Jr, et al. Campath-1H induction plus rapamycin monotherapy for renal transplantation: results of a pilot study. Am J Transplant. 2003;3:722–730. doi: 10.1034/j.1600-6143.2003.00120.x. [DOI] [PubMed] [Google Scholar]
- 76.Willicombe M, Roufosse C, Brookes P, et al. Antibody-mediated rejection after alemtuzumab induction: incidence, risk factors, and predictors of poor outcome. Transplantation. 2011;92:176–182. doi: 10.1097/TP.0b013e318222c9c6. [DOI] [PubMed] [Google Scholar]
- 77.Willicombe M, Brookes P, Santos-Nunez E, et al. Outcome of patients with preformed donor-specific antibodies following alemtuzumab induction and tacrolimus monotherapy. Am J Transplant. 2011;11:470–477. doi: 10.1111/j.1600-6143.2010.03421.x. [DOI] [PubMed] [Google Scholar]
- 78.LaMattina JC, Mezrich JD, Hofmann RM, et al. Alemtuzumab as compared to alternative contemporary induction regimens. Transpl Int. 2012;25:518–526. doi: 10.1111/j.1432-2277.2012.01448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Page EK, Page AJ, Kwun J, et al. Enhanced de novo alloantibody and antibody-mediated injury in rhesus macaques. Am J Transplant. 2012;12:2395–2405. doi: 10.1111/j.1600-6143.2012.04074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Weaver TA, Charafeddine AH, Agarwal A, et al. Alefacept promotes co-stimulation blockade based allograft survival in nonhuman primates. Nat Med. 2009;15:746–749. doi: 10.1038/nm.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lo DJ, Weaver TA, Stempora L, et al. Selective targeting of human alloresponsive CD8+ effector memory T cells based on CD2 expression. Am J Transplant. 2011;11:22–33. doi: 10.1111/j.1600-6143.2010.03317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kwun J, Page E, Hong JJ, et al. Neutralizing BAFF/APRIL with atacicept prevents early DSA formation and AMR development in T cell depletion induced nonhuman primate AMR model. Am J Transplant. 2015;15:815–822. doi: 10.1111/ajt.13045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kirk AD, Hale DA, Mannon RB, et al. Results from a human renal allograft tolerance trial evaluating the humanized CD52-specific monoclonal antibody alemtuzumab (CAMPATH-1H) Transplantation. 2003;76:120–129. doi: 10.1097/01.TP.0000071362.99021.D9. [DOI] [PubMed] [Google Scholar]
- 84.Kwun J, Oh BC, Gibby AC, et al. Patterns of de novo allo B cells and antibody formation in chronic cardiac allograft rejection after alemtuzumab treatment. Am J Transplant. 2012;12:2641–2651. doi: 10.1111/j.1600-6143.2012.04181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Thaunat O, Field AC, Dai J, et al. Lymphoid neogenesis in chronic rejection: evidence for a local humoral alloimmune response. Proc Natl Acad Sci U S A. 2005;102:14723–14728. doi: 10.1073/pnas.0507223102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nasr IW, et al. Tertiary lymphoid tissues generate effector and memory T cells that lead to allograft rejection. Am J Transplant. 2007;7:1071–1079. doi: 10.1111/j.1600-6143.2007.01756.x. [DOI] [PubMed] [Google Scholar]
- 87.Moreso F1, Seron D, O'Valle F, et al. Immunephenotype of glomerular and interstitial infiltrating cells in protocol renal allograft biopsies and histological diagnosis. Am J Transplant. 2007;7:2739–2747. doi: 10.1111/j.1600-6143.2007.02013.x. [DOI] [PubMed] [Google Scholar]
- 88.Brown K, Sacks SH, Wong W. Tertiary lymphoid organs in renal allografts can be associated with donor-specific tolerance rather than rejection. Eur J Immunol. 2011;41:89–96. doi: 10.1002/eji.201040759. [DOI] [PubMed] [Google Scholar]
- 89.Snanoudj R, Zuber J, Legendre C. Co-Stimulation Blockade as a New Strategy in Kidney Transplantation. Drugs. 2012;70:2121–2131. doi: 10.2165/11538140-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 90.Masson P, Henderson L, Chapman JR, Craig JC, Webster AC. Belatacept for kidney transplant recipients. Cochrane Database Syst Rev. 2014;11:CD010699. doi: 10.1002/14651858.CD010699.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Angin M, et al. Gene transfer of human CD40Ig does not prevent rejection in a non-human primate kidney allotransplantation model. Transpl Immunol. 2012;27:139–145. doi: 10.1016/j.trim.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 92.Tseng M, Ge S, Roberts R, et al. Liver Transplantation in a Patient With CD40 Ligand Deficiency and Hyper-IgM Syndrome: Clinical and Immunological Assessments. Am J Transplant. 2016;16(5):1626–1632. doi: 10.1111/ajt.13580. [DOI] [PubMed] [Google Scholar]
- 93.Pearson TC1, Trambley J, Odom K, et al. Anti-CD40 therapy extends renal allograft survival in rhesus macaques. Transplantation. 2002;74:933–940. doi: 10.1097/00007890-200210150-00006. [DOI] [PubMed] [Google Scholar]
- 94.Vincenti F1, Mendez R, Pescovitz M, et al. A phase I/II randomized open-label multicenter trial of efalizumab, a humanized anti-CD11a, anti-LFA-1 in renal transplantation. Am J Tranplant. 2007;7:1770–1777. doi: 10.1111/j.1600-6143.2007.01845.x. [DOI] [PubMed] [Google Scholar]
- 95.Anderson DJ, Lo DJ, Leopardi F, et al. Anti-LFA-1 Therapy in a Nonhuman Primate Renal Transplant Model of Costimulation Blockade Resistant Rejection. Am J Tranplant. 2015;16(5):1456–1464. doi: 10.1111/ajt.13628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cogollo E, Silva MA, Isenberg D. Profile of atacicept and its potential in the treatment of systemic lupus erythematosus. Drug Des Devel Ther. 2015;9:1331–1339. doi: 10.2147/DDDT.S71276. [DOI] [PMC free article] [PubMed] [Google Scholar]