Abstract
Background
Patients with coronary microvascular dysfunction (CMD) often have diastolic dysfunction, representing an important therapeutic target. Ranolazine—a late-sodium current inhibitor—improves diastolic function in animal models, and subjects with obstructive CAD. We hypothesized that ranolazine would beneficially alter diastolic function in CMD.
Methods
To test this hypothesis, we performed retrospective tissue tracking analysis to evaluate systolic/diastolic strain, using cardiac magnetic resonance imaging cine images: a) acquired in a recently completed, randomized, double-blind, placebo-controlled, crossover trial of short-term ranolazine in subjects with CMD, and b) from 43 healthy reference controls.
Results
Diastolic strain rate was impaired in CMD vs. controls (circumferential diastolic strain rate: 99.9 ± 2.5%/s vs. 120.1 ± 4.0%/s, p=0.0003; radial diastolic strain rate: −199.5 ± 5.5%/s vs. −243.1 ± 9.6%/s, p=0.0008, case vs. control). Moreover, peak systolic circumferential (CS) and radial (RS) strain were also impaired in cases vs. controls (CS: −18.8 ± 0.3% vs. −20.7 ± 0.3%; RS: 35.8 ± 0.7% vs. 41.4 ± 0.9%; respectively; both p < 0.0001), despite similar and preserved ejection fraction. In contrast to our hypothesis however, we observed no significant changes in left ventricular diastolic function in CMD cases after two weeks of ranolazine vs. placebo.
Conclusions
The case-control comparison both confirms and extends our prior observations of diastolic dysfunction in CMD. That CMD cases were also found to have sub-clinical systolic dysfunction is a novel finding, highlighting the utility of this retrospective approach. In contrast to previous studies in obstructive CAD, ranolazine did not improve diastolic function in CMD.
Keywords: Coronary microvascular dysfunction, microvascular ischemia, ranolazine, tissue tracking
Introduction
Presentation with signs and symptoms of myocardial ischemia, in the absence of obstructive coronary artery disease (CAD), is more frequent in women, is associated with increased risk of major cardiovascular events in follow up, and is a major burden to the health care system.1–6 The exact mechanism responsible remains incompletely understood, and as a result, effective treatment remains elusive.
Sex-specific research initiatives, including the NHLBI sponsored Women’s Ischemic Syndrome Evaluation (WISE) study, have provided important insight into the pathophysiology of this debilitating disease. For example, data from the WISE study indicate that more than half of the women with signs and symptoms of ischemia, but no obstructive CAD, have coronary microvascular dysfunction (CMD).7–11 We also have observed greater than expected diastolic dysfunction in this cohort,12;13 together with a higher incidence of heart failure hospitalizations1—most notably heart failure with preserved ejection fraction.14 These data, and reports from others, have led to the hypothesis that CMD may be mechanistically linked with diastolic dysfunction in such subjects, and may serve as a precursor to heart failure with preserved ejection fraction. Drug therapies specifically targeting these pathways are therefore of particular interest.
Late sodium current inhibition using ranolazine— an FDA approved medication for treatment of chronic angina— has demonstrated both safety and efficacy as an anti-anginal agent among subjects believed to have obstructive CAD.15–21 Despite a promising pilot trial, suggesting that late sodium channel inhibition may also improve angina symptoms and myocardial perfusion in women with CMD,22 results from our recent Phase III clinical trial suggest only a modest benefit.23 It is possible however that late sodium channel inhibition could improve other aspects of the CMD phenotype. In particular, improving intracellular sodium homeostasis should, in theory, limit calcium influx via the sodium-calcium exchanger, shorten the action potential duration, and improve left ventricular relaxation (i.e. diastolic function). Indeed, this has previously been demonstrated in preclinical rodent studies24;25 and small clinical studies of obstructive CAD.26;27 Whether late sodium current inhibition can similarly improve diastolic function in patients with CMD remains unknown, and is the focus of this investigation. To address this question, we leveraged the cardiac magnetic resonance cine images acquired in our recently completed, randomized, double-blind, placebo-controlled, cross-over trial of ranolazine (NCT01342029), and performed retrospective tissue tracking analysis to evaluate left ventricular strain changes in response to short-term ranolazine administration. In order to characterize strain abnormalities in our cases with CMD, we also performed a case-control comparison in a cohort of healthy controls.
Methods
Subject Population
Cases
Subject data were collected as part of a double-blind placebo-controlled, crossover trial, testing the efficacy of short-term ranolazine (500 mg ranolazine/placebo for 1 week and increased to 1000 mg ranolazine/placebo [as tolerated] for 1 week, twice daily) in subjects with CMD. A detailed description of the methodology has previously been published.23 Institutional Review Boards at Cedars-Sinai Medical Center and the University of Florida, Gainesville approved the study, and all subjects gave written informed consent prior to study participation. Briefly, both men and women with symptoms thought due to ischemia, no obstructive CAD (<50% epicardial coronary stenosis), and preserved LV ejection fraction, who had abnormal coronary reactivity testing (CRT) [coronary flow reserve (CFR) <2.5, or no dilation (≤0% change) with acetylcholine (Ach)], or stress CMRI myocardial perfusion reserve index <2.0, were enrolled. Angina frequency, nitroglycerin diary, and SF-36 were recorded as previously described.23
Reference Controls
To compare left ventricular strain in our CMD cohort to healthy reference controls, 43 women without symptoms, cardiac risk factors or signs suggesting IHD, who had a normal maximal Bruce-protocol exercise treadmill stress test were recruited from the community between September, 2007 and August, 2015. All reference control studies were performed at Cedars-Sinai Medical Center where institutional approval was obtained and all participants provided written informed consent.
Study Design
All CMRI studies were performed on a 1.5 Tesla magnet (Siemens Healthcare, Erlangen, Germany) with ECG-gating and a vendor-provided cardioac-coil using a highly standardized protocol. Cine function images were acquired in 10–12 short-axis slices using a steady-state free precession pulse sequence with electrocardiogram gating during breath hold at end-expiration (flip angle = 80°; resolution: 1.4×1.4 mm2; slice thickness: 8 mm; matrix size: 256×208; receiver bandwidth = 930 Hz/pixel; TE = 1.26 ms). The primary outcome was left ventricular relaxation rate (i.e. circumferential and radial diastolic strain rate), measured by myocardial tissue tracking. Secondary outcome variables included left ventricular systolic strain, also by tissue tracking, along with global morphology and systolic function: left ventricular mass and volume, left atrial volume28 and left ventricular ejection fraction.
To characterize the level of dysfunction present in our subject population, we first compared CMD cases (placebo visit) with our reference controls. Then, to test whether ranolazine improves diastolic function in CMD, we then compared the placebo arm with the treatment arm of the randomized, double-blind, placebo-controlled trial.
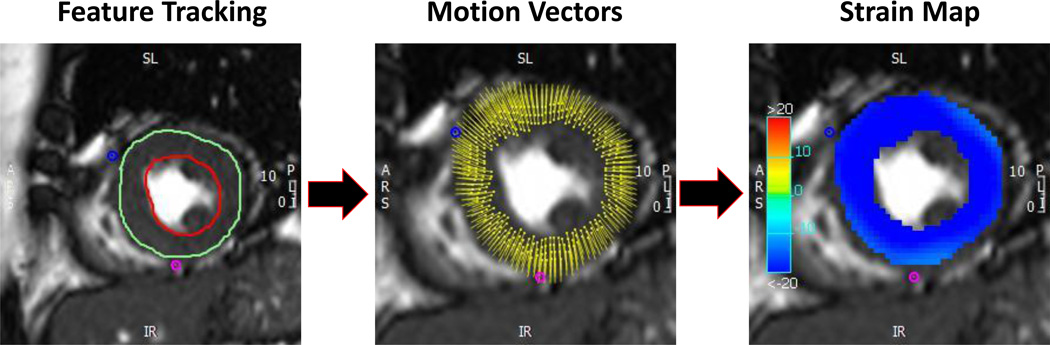
Myocardial Strain Analysis using CMR Tissue Tracking
As illustrated in Figure 1, myocardial tissue tracking was performed offline using previously acquired steady-state free precession cine images, and dedicated software (Circle CVI42, Calgary, AB, Canada). Myocardial tissue tracking is closely related to reference-standard myocardial tissue tagging (Supplemental Figure 1), as described in previous reports.29–31 For each subject and control, masked to patient data and treatment period, a series of short-axis CMR images were chosen, spanning the left ventricle (base-to-apex). Care was taken to avoid: 1) basal slices which included LV outflow tract and/or left atrium, and 2) apical slices without clear delineation of the LV lumen at end-systole. As a general rule, the apical slice was chosen 1–2 cm proximal to luminal obliteration. LV endocardial and epicardial borders were manually delineated at end-diastole. In case of insufficient tracking, defined as apparent deviations of the contours from the endocardial and epicardial borders, contours were manually corrected and the tissue tracking algorithm re-applied. All of the data were analyzed by a single observer, who was blinded to each subject’s medical history and/or treatment order. Our in-lab intra-rater variability, expressed as a co-efficient of variation, for each of the primary endpoints is as follows (mean ± SD): Circumferential Strain, 1 ± 1%; Radial Strain, 3 ± 2%; Circumferential Diastolic Strain Rate, 6 ± 5%; and Radial Diastolic Strain Rate, 7 ± 5%.
Figure 1.
Myocardial tissue tracking in a representative mid-ventricular short axis cine image. Left. Contours are drawn on the endo- and epicardial boarders at a single phase of the cardiac cycle. Middle: Tissue tracking software propagates the contours automatically and follows the motion of the contour throughout the cardiac cycle; displayed as motion vectors across the ventricular wall. Right: Strain (circumferential or radial) can then be displayed in the form of color maps throughout the cardiac cycle. In this case, circumferential strain is displayed. With this data derived, diastolic strain rate is simply calculated as the time derivative of either circumferential or radial strain.
Statistical Analysis
Data are expressed as mean ± standard error, or as absolute frequency and percentage for categorical data, unless otherwise specified. Differences between CMD cases and controls were compared using two sample Student’s t-test or Mann-Whitney U test. Treatment comparisons were paired t-tests on the treatment differences against the null hypothesis of zero difference (Ranolazine-Placebo). Linear regression models were tested using treatment differences and outcomes. A stepwise procedure was used to choose the variables that were significantly associated with the outcomes. Statistical significance was set a priori at p < 0.05.
Results
Pertinent case and control subject characteristics are summarized in Table 1. A total of 128 cases completed the trial with complete and analyzable data from both treatment periods. Although the ages were similar, the controls were on average 4-years older than controls (55 ± 10 vs. 51 ± 10 years, respectively, p = 0.007), with cases having a higher BMI (29.3 ± 7.6 vs. 25.6 ± 3.7 kg/m2, P < 0.01). Heart rate did not differ in cases compared to controls (p = 0.140); however systolic blood pressure was slightly higher in cases compared to controls (p = 0.002), and diastolic blood pressure was slightly lower (p = 0.04).
Table 1.
Baseline demographic and clinical variables
| Variables | Cases | Controls |
|---|---|---|
| n | 128 | 43 |
| Female | 96% | 100% |
| Age, years | 55 ± 10 | 51 ± 10* |
| BMI, kg/m2 | 29.3 ± 7.6 | 25.6 ± 3.7* |
| Race (non-Caucasian) | 31 (24.2%) | 17 (39.5%) |
| Tobacco use | ||
| Current | 2 (1.6%) | 2 (4.7%) |
| Former | 38 (29.7%) | 13 (30.2%) |
| Never | 88(68.8%% | 27 (62.8) |
| History of Hypertension | 69 (53.9%) | 0 |
| History of Diabetes | 23 (18.0%) | 0 |
| History of Hyperlipidaemia | 70 (54.7%) | 1 (2.3%) |
| Family history of premature coronary artery disease |
83 (64.8%) | 13 (30.2%) |
| LV Ejection Fraction, % | 68 ± 8 | 65 ± 6* |
| Heart rate, bpm | 67 ± 12 | 64 ± 11 |
| Systolic Blood Pressure, mmHg | 128 ± 20 | 119 ± 14* |
| Diastolic Blood Pressure, mmHg | 62 ± 13 | 66 ± 9* |
| Medications | ||
| Beta-blockers | 54 (42.2%) | 0 |
| Calcium Channel blockers | 29 (22.7%) | 0 |
| Angiotensin-converting enzyme inhibitors | 13 (10.2%) | 0 |
| Nitrates | 50 (39.1%) | 0 |
| Statins | 74 (57.8%) | 0 |
| Hormone replacement Therapy | 16 (12.5%) | 0 |
Mean ± SD or absolute frequency (%).
indicates P < 0.05
Case-Control Comparison
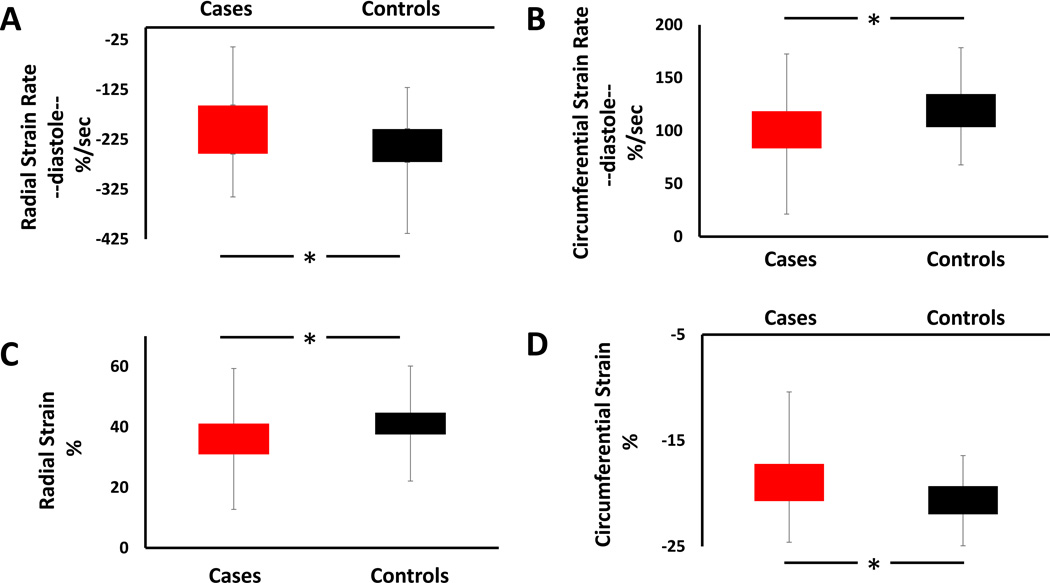
Myocardial tissue tracking confirmed previous observations, demonstrating significant group differences in the rate of early ventricular relaxation in cases compared to controls (Figure 2). In particular, both circumferential and radial diastolic strain rate (CSRd and RSRd, respectively) were significantly reduced in cases compared to reference controls (CSRd: 99.9 ± 2.5 vs. 120.1 ± 4.0, p=0.0003; RSRd: −199.5 ± 5.5 vs. −243.1 ± 9.6, p=0.0008, cases vs. controls), shown in Figure 2A & 2B. Myocardial tissue tracking also revealed, for the first time, systolic strain abnormalities in cases compared to controls (CS: −18.8 ± 0.3 vs. −20.7 ± 0.3; RS: 35.8 ± 0.7 vs. 41.4 ± 0.9; respectively; both p < 0.0001), shown in Figure 2C and 2D, despite similar and preserved left ventricular ejection fractions (LVEF 68 ± 8% vs. 65 ± 6%, case vs. control, p = 0.04). Importantly, these group differences remained after adjusting for age, BMI, and blood pressure. We observed no relationship between myocardial perfusion reserve index and LV diastolic or systolic function. Left atrial volume normalized to body surface area, a secondary measure of left ventricular diastolic function, was not significantly different between cases and controls (39.2 ± 1.0 mL/m2 vs. 41.9 ± 1.5 mL/m2, p=0.104).
Figure 2.
Group strain and strain rate data, comparing cases with coronary microvascular dysfunction (red bars) with healthy matched controls (black bars). Top panels (A and B) illustrate group differences in radial diastolic strain rate (A) and circumferential diastolic strain rate (B). Bottom panels (C and D) illustrate group differences in peak radial (C) and circumferential (D) strain. * indicates P < 0.05.
Influence of late sodium channel inhibition on systolic and diastolic function
In contrast to our hypothesis, short-term late sodium channel inhibition with ranolazine did not improve either left ventricular circumferential diastolic strain rate (ΔCSRd = 2.0 ± 1.7, p=0.25) or radial diastolic strain rate (ΔRSRd = −2.6 ± 4.3, p=0.54). Likewise, systolic circumferential and radial strain also remained unchanged (ΔCS = 0.09 ± 0.15%, p = 0.545; ΔRS = −0.13 ± 0.47%, p = 0.785), as did left atrial volume (Δ left atrial volume normalized to body surface area = 0.62 ± 0.67 mL/m2, p = 0.356) and left ventricular ejection fraction (Δ ejection fraction −0.03 ± 3.33, p=0.92). Moreover, we observed no relationship between the change in myocardial perfusion reserve index and the change in LV function with ranolazine.
Sub-analysis of the subjects with clinically significant limited coronary flow reserve < 2.5 and/or subjects with the lowest diastolic strain rate (i.e. 1 and 2 SD below the mean), also did not reveal any major benefit in left ventricular strain/strain rate with ranolazine. Modeling demonstrated that among subjects with the same change in angina frequency and change in reported depression, usage of nitrates was associated with a higher estimated change in radial diastolic strain rate of 23.2 units (p = 0.013). Use of nitrates also tended to predict the greatest change in radial diastolic strain rate (15.1 %/s), compared to those not on nitrates (p = 0.08), independent of other modeling factors.
Discussion
Women with signs and symptoms of ischemia but no obstructive CAD, often have coronary microvascular dysfunction, and are at increased risk for developing heart failure with preserved ejection fraction. We have previously shown, in two separate small proof-of-concept studies12;13, that the rate of left ventricular relaxation is impaired in women with CMD. The data herein, both confirm and extend those previous observations using novel, retrospective, myocardial tissue tracking in a much larger cohort of cases and controls. First, we confirm that left ventricular relaxation rate is reduced in patients with CMD. Second, we extend our previous work by documenting subclinical left ventricular systolic dysfunction for the first time in this subject population. With this foundation, we tested whether late-sodium channel inhibition could rescue left ventricular dysfunction in CMD. In contrast to previous work in obstructive CAD however, we observed no detectable major benefit with ranolazine on left ventricular relaxation or systolic strain.
Cardiac MRI is the clinical reference-standard imaging tool for the evaluation of left ventricular morphology and function. Notably, MR cine imaging provides excellent intrinsic blood-to-tissue contrast and a high degree of reproducibility. As such, cine imaging is an intrinsic part of every cardiac MRI exam world-wide. Cardiac MRI is also the reference technique for measuring myocardial tissue deformation (i.e. strain), which is increasingly recognized as a more sensitive measure for the detection of left ventricular dysfunction than other, more traditional, cine derived global metrics of left ventricular function.32–34 Conventional strain imaging has not been widely adopted throughout the MR community however, largely due to its associated technical challenges, including difficult and sometimes unavailable imaging sequences, longer and/or additional breath-holds and scanner time, and lack of available post-processing software. Myocardial tissue tracking with MRI, which utilizes standard cine images to assess myocardial deformation, has recently emerged as an exciting new tool for reliably measuring left ventricular strain,29–31 independent of field strength.35 Importantly, this approach to strain measurement does not require any image acquisition beyond the standard routine cardiac MRI procedure.
Application of myocardial tissue tracking to our existing clinical dataset re-establishes diastolic dysfunction as an important clinical phenotype in CMD; confirming observations from two separate small proof-of-concept studies from our laboratory.12;13 Given the increased incidence of heart failure in this subject population,1 of whom the majority of cases have preserved ejection fraction,14 diastolic dysfunction may represent an important therapeutic target. We speculate that interventions aimed at alleviating diastolic dysfunction in patients with CMD may prevent future development of clinical HFpEF. That we also observe subclinical systolic dysfunction in cases compared to controls further strengthens the relationship between CMD and HFpEF. Indeed, left ventricular strain is also impaired in HFpEF,36–38 and associated with a higher risk of heart failure hospitalization, cardiovascular death, and aborted sudden death.36
Ranolazine has been shown to improve diastolic function in subjects with CAD.26;27 To test whether ranolazine is equally effective in subjects with CMD who have no obstructive CAD, we leveraged the recently completed randomized, placebo-controlled trial of late sodium current inhibition with ranolazine in CMD (NCT01342029).23 In line with a recent study in subjects with aortic stenosis39, we observed no major differences in diastolic or systolic function between the placebo arm and the ranolazine arm. While the reason for this negative finding remains unclear, we acknowledge that it may be related to the treatment regimen. For example, in our positive pilot study,22 we administered ranolazine for 4 weeks (2 weeks 500 mg b.i.d. followed by 2 weeks of 1000 mg b.i.d.) resulting in a higher SAQ and a trend towards an improvement in myocardial perfusion reserve index (which was significant in women with CFR <3.0). In the present trial however, subjects were treated for 2 weeks (1 week of 500 mg b.i.d. and 1 week of 1000 mg b.i.d.), which may have at least partially contributed to the present findings.
Limitations
Myocardial tissue tracking uses proprietary modeling algorithms to track the endocardial and epicardial boarders of the left ventricle, providing detailed information about global left ventricular strain. Other more conventional strain imaging modalities derive their measurement of strain very differently. For example, speckle-tracking echocardiography relies on tracking acoustic backscatter within the myocardium itself. Similarly, gold-standard tissue tagging changes the tissue magnetization in such a way that the myocardium is divided into quantifiable square patterns. In both of these methods, regional changes in tissue deformation, spanning the epicardium, mid-wall, and endocardium, can be measured throughout the cardiac cycle. Thus, a major limitation of myocardial tissue tracking is its inability to differentiate and quantify regional deformation changes separately in the epicardium, mid-wall, and endocardium.
Myocardial tissue tracking of short-axis cine images provides quantitative information about circumferential and radial tissue deformation (i.e. strain and strain rate). While left ventricular strain has previously been shown to have important prognostic value,32–34 we acknowledge that the rate of circumferential or radial strain is not a conventional diastolic metric (like Doppler derived mitral inflow, annular tissue velocity, or pulmonary venous velocity). However, we believe the rate of left ventricular tissue deformation more closely reflects changes in myocardial relaxation rate per se, rather than transmitral filling velocities, which can be drastically influenced by changes in filling pressure. This is exemplified in a previous report from our group, in cases with CMD, where we observed diastolic strain abnormalities despite significantly elevated LV filling pressures.13
A fundamental assumption of this investigation is that CMD prolongs the late sodium current, even under resting conditions, such that inhibition of this current would improve intracellular calcium homeostasis. This is indeed an important consideration when interpreting the present results. Future investigations are needed, evaluating the effects of late sodium channel inhibition on diastolic function during periods of physiological stress.
Conclusions
Impaired myocardial deformation, as represented by a reduction in LV circumferential and radial strain and strain rate, provides important insight into the pathophysiology of disease. Here, we used myocardial tissue tracking, a simple non-invasive post-processing tool used to measure myocardial deformation, to both confirm diastolic dysfunction in CMD and extend these observations to subclinical systolic dysfunction for the first time. Application of this technique also afforded the opportunity to test whether short term treatment with the late-sodium channel inhibitor ranolazine could improve left ventricular function in subjects with CMD. Our finding that ranolazine did not improve left ventricular function in subjects with CMD may reflect the non-ischemic state of the resting myocardium in these subjects, and warrants further investigation.
Supplementary Material
Acknowledgments
Conflict of Interest:
MDN reports received research support from Gilead Sciences. C.N.B.M. reports receiving research support from the Gilead Sciences and served on the grant review committee for Gilead. E.M.H. reports receiving research grants from Gilead Sciences. C.L.S. reports receiving research grants from Gilead Sciences. P.K.M. reports receiving research grants from Gilead Sciences. L.E.J.T. reports receiving research grants from Gilead Sciences. C.J.P. reports receiving research grants from Gilead Sciences.
This work was supported by an unrestricted research grant from Gilead and by the American Heart Association (16SDG27260115), the Harry S. Moss Heart Trust, the National Heart, Lung and Blood Institute (N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164), a GCRC grant MO1-RR00425 from the National Center for Research Resources, the National Center for Research Resources, grant UL1RR033176, the NIH/National Center for Advancing Translational Sciences (NCATS), UCLA CTSI grant UL1TR000124 and UF CTSI grant UL1TR001427, grant R01 HL089765, and grants from the Gustavus and Louis Pfeiffer Research Foundation, Denville, New Jersey, the Women's Guild of Cedars-Sinai Medical Center, Los Angeles, California, the Edythe L. Broad Women's Heart Research Fellowship, Cedars-Sinai Medical Center, Los Angeles, California, the Constance Austin Women's Heart Research Fellowship, the Barbra Streisand Women's Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles, and the Erika Glazer Women's Heart Health Project, Cedars-Sinai Medical Center, Los Angeles.
Reference List
- 1.Gulati M, Cooper-DeHoff RM, McClure C, Johnson BD, Shaw LJ, Handberg EM, Zineh I, Kelsey SF, Arnsdorf MF, Black HR, Pepine CJ, Merz CN. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: A report from the women's ischemia syndrome evaluation study and the st james women take heart project. Arch Intern Med. 2009;169:843–850. doi: 10.1001/archinternmed.2009.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jespersen L, Hvelplund A, Abildstrom SZ, Pedersen F, Galatius S, Madsen JK, Jorgensen E, Kelbaek H, Prescott E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734–744. doi: 10.1093/eurheartj/ehr331. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger V, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics 2014 Update: A Report From the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw LJ, Merz CNB, Pepine CJ, et al. The Economic Burden of Angina in Women With Suspected Ischemic Heart Disease: Results From the National Institutes of Health National Heart, Lung, and Blood Institute Sponsored Womens Ischemia Syndrome Evaluation. Circulation. 2006;114:894–904. doi: 10.1161/CIRCULATIONAHA.105.609990. [DOI] [PubMed] [Google Scholar]
- 5.Shaw LJ, Bugiardini R, Merz CNB. Women and Ischemic Heart Disease: Evolving Knowledge. J Am Coll Cardiol. 2009;54:1561–1575. doi: 10.1016/j.jacc.2009.04.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pepine CJ, Ferdinand KC, Shaw LJ, Light-McGroary KA, Shah RU, Gulati M, Duvenoy C, Walsh MN, Bairey Merz CN ACC CVD in Women Committee. Emergence of Nonobstructive Coronary Artery Disease: A Woman's Problem and Need for Change in Definition on Angiography. J Am Coll Cardiol. 2015;66:1918–1933. doi: 10.1016/j.jacc.2015.08.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marroquin OC, Kip KE, Mulukutla SR, Ridker PM, Pepine CJ, Tjandrawan T, Kelsey SF, Mankad S, Rogers WJ, Merz CN, Sopko G, Sharaf BL, Reis SE. Inflammation, endothelial cell activation, and coronary microvascular dysfunction in women with chest pain and no obstructive coronary artery disease. Am Heart J. 2005;150:109–115. doi: 10.1016/j.ahj.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Pepine CJ, Anderson RD, Sharaf BL, Reis SE, Smith KM, Handberg EM, Johnson BD, Sopko G, Bairey Merz CN. Coronary Microvascular Reactivity to Adenosine Predicts Adverse Outcome in Women Evaluated for Suspected Ischemia: Results From the National Heart, Lung and Blood Institute WISE (Women's Ischemia Syndrome Evaluation) Study. J Am Coll Cardiol. 2010;55:2825–2832. doi: 10.1016/j.jacc.2010.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pepine CJ, Petersen JW, Bairey Merz CN. A Microvascular-Myocardial Diastolic Dysfunctional State and Risk for Mental Stress Ischemia: A Revised Concept of Ischemia During Daily LifeΓêù. JACC Cardiovasc Imaging. 2014;7:362–365. doi: 10.1016/j.jcmg.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Thomson LEJ, Wei J, Agarwal M, Haft-Beradaran A, Shufelt C, Mehta PK, Gill E, Johnson BD, Kenkre T, Handberg EM, Li D, Sharif B, Berman DS, Petersen JW, Pepine CJ, Bairey Merz CN. Cardiac Magnetic Resonance Myocardial Perfusion Reserve Index Is Reduced in Women With Coronary Microvascular Dysfunction: A National Heart, Lung, and Blood Institute-Sponsored Study From the Women's Ischemia Syndrome Evaluation. Circ Cardiovasc Imaging. 2015;8:e002481. doi: 10.1161/CIRCIMAGING.114.002481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei J, Mehta PK, Johnson BD, Samuels B, Kar S, Anderson RD, Azarbal B, Peterson J, Handberg E, Shufelt C, Kothawade K, Sopko G, Lerman A, Shaw L, Kelsey SF, Pepine CJ, Bairey Merz CN. Safety of Coronary Reactivity Testing in Women with No Obstructive Coronary Artery Disease: Results from the NHLBI-sponsored Women∍s Ischemia Syndrome Evaluation (WISE) Study. JACC Cardiovasc Interv. 2012;5:646–653. doi: 10.1016/j.jcin.2012.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nelson MD, Szczepaniak LS, Wei J, Haftabaradaren A, Bharadwaj M, Sharif B, Mehta P, Zhang X, Thomson LE, Berman DS, Li D, Bairey Merz CN. Diastolic Dysfunction in Women With Signs and Symptoms of Ischemia in the Absence of Obstructive Coronary Artery Disease: A Hypothesis-Generating Study. Circ Cardiovasc Imaging. 2014;7:510–516. doi: 10.1161/CIRCIMAGING.114.001714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wei J, Nelson MD, Szczepaniak EW, Smith L, Mehta PK, Thomson LEJ, Berman DS, Li D, Bairey Merz CN, Szczepaniak LS. Myocardial steatosis as a possible mechanistic link between diastolic dysfunction and coronary microvascular dysfunction in women. Am J Physiol Heart Circ Physiol. 2016;310:H14–H19. doi: 10.1152/ajpheart.00612.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakir M, Nelson M, Jones E, Li Q, Wei J, Mehta PK, Sharif B, Shufelt C, Sopko G, Pepine CJ, BAirey Merz CN. Heart Failure Hospitalization in Women with Signs and Symptoms of Ischemia: A Report from the Women's Ischemia Syndrome Evaluation Study. Int J Cardiol. doi: 10.1016/j.ijcard.2016.07.301. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Timmis AD, Chaitman BR, Crager M. Effects of ranolazine on exercise tolerance and HbA1c in patients with chronic angina and diabetes. Eur H J. 2005;27:42–48. doi: 10.1093/eurheartj/ehi495. [DOI] [PubMed] [Google Scholar]
- 16.Wenger NK, Chaitman B, Vetrovec GW. Gender Comparison of Efficacy and Safety of Ranolazine for Chronic Angina Pectoris in Four Randomized Clinical Trials. Am J Cardiol. 2007;99:11–18. doi: 10.1016/j.amjcard.2006.07.052. [DOI] [PubMed] [Google Scholar]
- 17.Rousseau MF, Pouleur H, Cocco G, Wolff AA. Comparative efficacy of ranolazine versus atenolol for chronic angina pectoris. Am J Cardiol. 2005;95:311–316. doi: 10.1016/j.amjcard.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 18.Stone PH, Gratsiansky NA, Blokhin A, Huang IZ, Meng L. Antianginal Efficacy of Ranolazine When Added to Treatment With Amlodipine: The ERICA (Efficacy of Ranolazine in Chronic Angina) Trial. J Am Coll Cardiol. 2006;48:566–575. doi: 10.1016/j.jacc.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 19.Chaitman BR, Pepine CJ, Parker JO. Effects of ranolazine with atenolol, amlodipine, or diltiazem on exercise tolerance and angina frequency in patients with severe chronic angina: A randomized controlled trial. JAMA. 2004;291:309–316. doi: 10.1001/jama.291.3.309. [DOI] [PubMed] [Google Scholar]
- 20.Chaitman BR, Skettino SL, Parker JO, Hanley P, Meluzin J, Kuch J, Pepine CJ, Wang W, Nelson JJ, Hebert DA, Wolff AA MARISA Investigators. Anti-ischemic effects and long-term survival during ranolazine monotherapy in patients with chronic severe angina. J Am Coll Cardiol. 2004;43:1375–1382. doi: 10.1016/j.jacc.2003.11.045. [DOI] [PubMed] [Google Scholar]
- 21.Chaitman BR. Ranolazine for the Treatment of Chronic Angina and Potential Use in Other Cardiovascular Conditions. Circulation. 2006;113:2462–2472. doi: 10.1161/CIRCULATIONAHA.105.597500. [DOI] [PubMed] [Google Scholar]
- 22.Mehta PK, Goykhman P, Thomson LEJ, Shufelt C, Wei J, Yang Y, Gill E, Minissian M, Shaw LJ, Slomka PJ, Slivka M, Berman DS, Bairey Merz CN. Ranolazine Improves Angina in Women With Evidence of Myocardial Ischemia But No Obstructive Coronary Artery Disease. JACC: Cardiovasc Imaging. 2011;4:514–522. doi: 10.1016/j.jcmg.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bairey Merz CN, Handberg EM, Shufelt CL, Mehta PK, Minissian MB, Wei J, Thomson LE, Berman DS, Shaw LJ, Petersen JW, Brown GH, Anderson RD, Shuster JJ, Cook-Wiens G, Rogatko A, Pepine CJ. A randomized, placebo-controlled trial of late Na current inhibition (ranolazine) in coronary microvascular dysfunction (CMD): impact on angina and myocardial perfusion reserve. Eur Heart J. 2015 doi: 10.1093/eurheartj/ehv647. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams S, Pourrier M, McAfee D, Lin S, Fedida D. Ranolazine improves diastolic function in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol. 2014;306:H867–H881. doi: 10.1152/ajpheart.00704.2013. [DOI] [PubMed] [Google Scholar]
- 25.Lovelock JD, Monasky MM, Jeong EM, Lardin HA, Liu H, Patel BG, Taglieri DM, Gu L, Kumar P, Pokrel N, Zeng D, Belardinelli L, Sorescu D, Solaro RJ, Dudley SC., Jr Ranolazine Improves Cardiac Diastolic Dysfunction Through Modulation of Myofilament Calcium Sensitivity. Circ Res. 2012;110:841–850. doi: 10.1161/CIRCRESAHA.111.258251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Figueredo VM, Pressman GS, Romero-Corral A, Murdock E, Holderbach P, Morris DL. Improvement in Left Ventricular Systolic and Diastolic Performance During Ranolazine Treatment in Patients With Stable Angina. J Cardiovasc Pharmacol Ther. 2011;16:168–172. doi: 10.1177/1074248410382105. [DOI] [PubMed] [Google Scholar]
- 27.Hayashida W, van Eyll C, Rousseau M, Pouleur H. Effects of ranolazine on left ventricular regional diastolic function in patients with ischemic heart disease. Cardiovasc Drug Ther. 1994;8:741–747. doi: 10.1007/BF00877121. [DOI] [PubMed] [Google Scholar]
- 28.Maceira A, Cosin-Sales J, Roughton M, Prasad S, Pennell D. Reference left atrial dimensions and volumes by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2010;12:65. doi: 10.1186/1532-429X-12-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schuster A, Paul M, Bettencourt N, Morton G, Chiribiri A, Ishida M, Hussain S, Jogiya R, Kutty S, Bigalke B, Perera D, Negel E. Cardiovascular magnetic resonance myocardial feature tracking for quantitative viability assessment in ischemic cardiomyopathy. Int J Cardiol. 2013;166:413–420. doi: 10.1016/j.ijcard.2011.10.137. [DOI] [PubMed] [Google Scholar]
- 30.Hor KN, Gottliebson WM, Carson C, Wash E, Cnota J, Fleck R, Wansapura J, Klimeczek P, Al-Khalidi HR, Chung ES, Benson DW, Mazur W. Comparison of Magnetic Resonance Feature Tracking for Strain Calculation With Harmonic Phase Imaging Analysis. JACC: Cardiovasc Imaging. 3:144–151. doi: 10.1016/j.jcmg.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Augustine D, Lewandowski A, Lazdam M, et al. Global and regional left ventricular myocardial deformation measures by magnetic resonance feature tracking in healthy volunteers: comparison with tagging and relevance of gender. J Cardiovasc Magn Reson. 2013;15:8. doi: 10.1186/1532-429X-15-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Motoki H, Borowski AG, Shrestha K, Troughton RW, Tang WH, Thomas JD, Klein AL. Incremental Prognostic Value of Assessing Left Ventricular Myocardial Mechanics in Patients With Chronic Systolic Heart Failure. J Am Coll Cardiol. 2012;60:2074–2081. doi: 10.1016/j.jacc.2012.07.047. [DOI] [PubMed] [Google Scholar]
- 33.Buss SJ, Emami M, Mereles D, Korosoglou G, Kristen AV, Voss A, Schelberg D, Zugck C, Galuschky C, Giannitsis E, Hegenbart U, Ho AD, Katus HA, Schonland SO, Hardt SE. Longitudinal Left Ventricular Function for Prediction of Survival in Systemic Light-Chain Amyloidosis: Incremental Value Compared With Clinical and Biochemical Markers. J Am Coll Cardiol. 2012;60:1067–1076. doi: 10.1016/j.jacc.2012.04.043. [DOI] [PubMed] [Google Scholar]
- 34.Choi EY, Rosen BD, Fernandes VR, Yan RT, Yoneyama K, Donekal S, Opdahl A, Almeida AL, Wu CO, Gomes AS, Bluemke DA, Lima JA. Prognostic value of myocardial circumferential strain for incident heart failure and cardiovascular events in asymptomatic individuals: the Multi-Ethnic Study of Atherosclerosis. Eur Heart J. 2013;34:2354–2361. doi: 10.1093/eurheartj/eht133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schuster A, Morton G, Hussain ST, Jogiya R, Kutty S, Asrress KN, Makowski MR, Bigalke Bm Perera D, Beerbaum P, Nagel E. The intra-observer reproducibility of cardiovascular magnetic resonance myocardial feature tracking strain assessment is independent of field strength. Eur J Radiol. 2013;82:296–301. doi: 10.1016/j.ejrad.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 36.Shah AM, Claggett B, Sweitzer NK, Shah SJ, Anand IS, Liu L, Pitt B, Pfeffer MA, Solomon SD. Prognostic Importance of Impaired Systolic Function in Heart Failure With Preserved Ejection Fraction and the Impact of Spironolactone. Circulation. 2015;132:402–414. doi: 10.1161/CIRCULATIONAHA.115.015884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hasselberg NE, Haugaa KH, Sarvari SI, Gullestad L, Andreassen AK, Smiseth OA, Edvardsen T. Left ventricular global longitudinal strain is associated with exercise capacity in failing hearts with preserved and reduced ejection fraction. Eur Heart J Cardiovasc Imaging. 2015;16:217–224. doi: 10.1093/ehjci/jeu277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stampehl MR, Mann DL, Nguyen JS, Cota F, Colmenares C, Dokainish H. Speckle Strain Echocardiography Predicts Outcome in Patients with Heart Failure with both Depressed and Preserved Left Ventricular Ejection Fraction. Echocardiography. 2015;32:71–78. doi: 10.1111/echo.12613. [DOI] [PubMed] [Google Scholar]
- 39.Singh A, Steadman CD, Khan JN, Reggiardo G, McCann GP. Effect of late sodium current inhibition on MRI measured diastolic dysfunction in aortic stenosis: a pilot study. BMC Research Notes. 2016;9:1–10. doi: 10.1186/s13104-016-1874-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.