Abstract
Autophagy has broad functions in immunity ranging from cell autonomous defense to coordination of complex multicellular responses. The successful resolution of infection and avoidance of autoimmunity necessitates efficient and timely communication between autophagy and pathways that sense the immune environment. In this article, progress in elucidating mechanisms of crosstalk between autophagy and inflammatory signaling cascades will be reviewed. The recent literature indicates that a variety of immune mediators induce or repress autophagy. It is also becoming increasing clear that immune signaling cascades are subject to regulation by autophagy, and that a return to homeostasis following a robust immune response is critically dependent on this pathway. Importantly, examples of non-canonical forms of autophagy in mediating immunity are pervasive. Improved mechanistic understanding of the autophagy machinery offers hope for treating infectious and inflammatory diseases.
Macroautophagy, more commonly referred to simply as autophagy, is a fundamental cellular process in eukaryotes that is essential for responding and adapting to changes in the environment. In its most common form, autophagy involves sequestration of cytosolic material within a double membrane-bound vesicle termed the autophagosome, and the subsequent fusion of the autophagosome with endolysosomal vesicles leads to degradation and recycling of sequestered substrates. A critical function of autophagy is to breakdown macromolecules such as proteins to provide amino acids and other factors necessary to generate energy and synthesize new proteins. The ability to capture large material distinguishes this pathway from proteasomal degradation, making autophagy critical for maintaining cellular homeostasis in a variety of settings. Many of the substrates found within autophagosomes are those that threaten cell viability, such as damaged organelles, protein aggregates, and intracellular pathogens.
Although autophagosomes are detected under steady-state conditions, their generation is increased substantially in response to stressors, of which nutrient deprivation is the best characterized. Depletion of amino acids or growth factors induces autophagy by inhibiting mechanistic target of rapamycin complex 1 (mTORC1), a master regulator of metabolism that inhibits the ULK1 complex through phosphorylation under nutrient replete conditions (Box 1). Once freed from inhibition, the ULK1 complex phosphorylates beclin-1 to activate the class III PI3K (PI3KC3) complex1, which creates PI3P-rich subdomains at regions associated with the endoplasmic reticulum (ER), such as the ER-Golgi intermediate compartment or ER-mitochondria contact sites2,3. PI3P binding proteins then recruit the ATG16L1 complex to this autophagosome precursor site (isolation membrane)4. The ATG16L1 complex anchors the ubiquitin-like molecule LC3 to the lipid bilayer by conjugating LC3 to phosphatidylethanolamine (PE) (Box 1). Next, LC3-PE mediates membrane tethering and fusion to extend the isolation membrane through recruiting lipids, which are likely derived from multiple membrane sources including endosomal vesicles harboring the transmembrane protein ATG9L1. The growing isolation membrane eventually fuses with itself to form the enclosed double-membrane structure, and class C VPS and SNARE-like proteins mediate fusion with endo-lysosomal vesicles leading to the degradation and recycling of the contents.
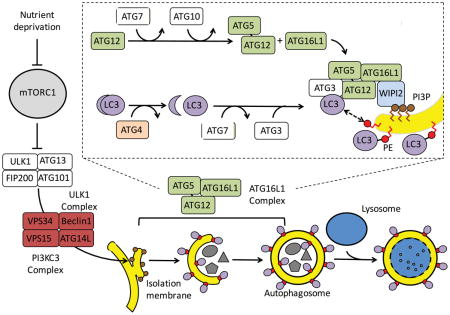
Box 1. Autophagosome biogenesis and autophagy related (ATG) proteins.
The generation of the autophagosome is mediated by the sequential activities of three key protein complexes: the ULK1 complex (ULK1, FIP200, ATG13, and ATG101), the class III phosphatidylinositol 3-OH kinase (PI3KC3) complex (Beclin-1, VPS34, VPS15, and ATG14L), and the ATG16L1 complex (ATG16L1, ATG5, and ATG12). Inhibition of mTORC1, such as through nutrient deprivation, allows the ULK1 complex to activate the PI3KC3 complex (see the figure). The ATG16L1 complex is recruited by the PI3P-binding protein WIPI2 to the autophagosome precursor structure (isolation membrane) when the PI3KC3 complex creates PI3P-rich regions on the surface of the ER-Golgi intermediate compartment or other membranes. The ATG16L1 complex is generated through an ubiquitin-like (UBL) conjugation reaction in which the UBL molecule ATG12 is conjugated to ATG5 by the sequential action of ATG7 and ATG10. ATG16L1 non-covalently binds the ATG5-ATG12 conjugate to form a multimeric complex. In parallel, another UBL molecule, LC3, is processed by the ATG4 protease and subjected to a second UBL conjugation reaction involving ATG7 and ATG3. The ATG16L1 complex conjugates LC3 and phosphatidylethanolamine (PE) to complete the reaction. LC3-PE mediates membrane tethering and fusion to extend the isolation membrane through recruiting membranes from multiple sources, eventually leading to self-fusion and the formation of the autophagosome. Subsequent fusion with the lysosome, mediated by class C VPS and SNARE-like proteins, leads to the degradation of the contents.
In this article, the function and regulation of autophagy in the context of inflammatory signals will be reviewed. It is now appreciated that autophagy function is critical to both cell autonomous defense and multicellular immunity alike, and autophagy dysfunction appears to be a recurring theme in inflammatory disease. First, the general function of autophagy in immunity will be summarized. The focus of the second section will be on specific modes of intersection between autophagy and immune pathways, especially signaling downstream of innate immune sensors. The third section will provide examples of how these mechanisms contribute to multicellular immune responses, with an emphasis on adaptive immunity and inflammatory disease. Finally, the barriers for targeting the autophagy pathway to treat disease will be discussed.
The role of autophagy in immunity
Autophagy can eliminate an infectious threat by promoting xenophagy, whereby intracellular pathogens such as viruses, bacteria, and protozoans are trapped within an autophagosome and targeted to the lysosome for destruction. Xenophagy depends on adaptor molecules that crosslink pathogens with the autophagy machinery. For instance, sequestosome 1 (SQSTM1; also known as p62), nuclear domain 10 protein NDP52, optineurin (OPTN), and TAX1-binding protein 1 (TAX1BP1) bind LC3 along with host molecules associated with damaged Salmonella-containing vacuoles, including ubiquitin and galectin-85. These binding events allow the isolation membrane to grow around Salmonella resulting in its sequestration within the autophagosome. One of the most compelling evidence that autophagy is an important cell-intrinsic defense mechanism is that many invasive pathogens encode virulence factors that counteract the pathway, as exemplified by the LC3-deconjugating enzyme RavZ secreted by Legionella pneumophila6. Also, autophagy enhances cell-to-cell spread of enteroviruses by providing a membrane coat during egress7.
Some pathogens are neutralized by non-canonical functions of the autophagy machinery, hereon referred to as ‘non-canonical autophagy’ (Box 2). For instance, LC3-associated phagocytosis (LAP) mediates phagosome maturation, and requires many of the same proteins as conventional autophagy but occurs independently of autophagosome formation8. Another form of non-canonical autophagy induced by IFNγ restricts norovirus and Toxoplasma gondii replication in macrophages in a lysosome-independent manner9–11. In the case of T. gondii infection, the ATG16L1 complex and LC3 disrupt the parasitophorous vacuole by recruiting p47 immunity-related GTPases (IRGs) and p65 guanylate binding proteins (GBPs)9,12–15. Although it is not always clear whether the classical or an unconventional form of autophagy is involved in host defense, autophagy proteins remain strong candidates as drug targets in infectious disease. Inducing autophagy with a cell permeable beclin-1 peptide protects against multiple pathogens in vitro and in vivo, including chikungunya and West Nile viruses16.
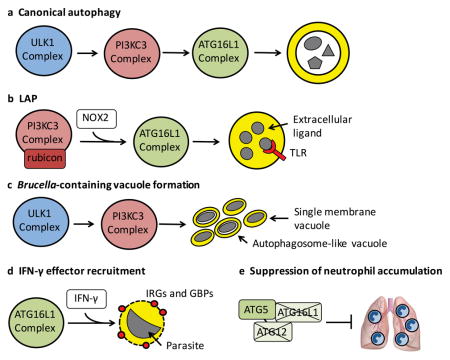
Box 2. Non-canonical autophagy and immunity.
Several processes have been described in which subsets of the canonical autophagy pathway (see box figure, part a) contribute to immune responses, frequently independent of autophagosome formation. LC3-associated phagocytosis (LAP) mediates the maturation of phagosomes containing TLR ligands independently of the ULK1 complex, but requires the association of rubicon with the PI3KC3 complex8 (see box figure, part b). Brucella abortus subverts the ULK1 and PI3KC3 complexes, but not the ATG16L1 complex or LC3, to generate pathogen-containing vacuoles which can either be single or double membrane structures160 (see box figure, part c). The recruitment of IFN-γ effector molecules (IRGs and GBPs) to the parasitophorous vacuole during Toxoplasma gondii infection is dependent on the the ATG16L1 complex but not autophagosome formation or lysosomes11 (see box figure, part d). A similar process is involved in inhibition of norovirus replication by IFN-γ10. ATG5 prevents neutrophil-mediated lung damage during Mycobacterium tuberculosis infection independently of the other ATG16L1 complex members161 (see box figure, part e). It is unclear whether this function of ATG5 represents a type of non-canonical autophagy or a new function of ATG5. There are several other examples not depicted. Coronavirus replication occurs on ER-derived membranes decorated by the unconjugated form of LC3, and does not require the rest of the autophagy machinery162. ATG9L1 represses DNA stimulation of STING independently of the LC3 conjugation machinery. LC3 can be recruited to double-membrane structures containing internalized Salmonella in the absence of ATG9L1 and subunits of the ULK1 and PI3KC3 complexes163. The inhibitory activity of ATG16L1 on NOD1 and NOD2 signaling can occur independently of the autophagy function of this protein164. CD4 T cell recognition of DCs harboring T. gondii was shown to depend on ATG5 and not ATG7165. Thus, the immune function of conserved autophagy proteins often reflects a non-canonical form of autophagy.
Autophagy also reduces damage inflicted by pathogens. During Sindbis virus infection, autophagy protects against neuronal cell death without affecting the degree of viral replication17. Similarly, in the absence of ATG16L1, the beneficial intestinal virus murine norovirus (MNV)18 triggers intestinal pathologies in mice through the cytokines TNFα and IFNγ19. Viral replication is unaltered in these mice19, consistent with a role for autophagy in suppressing the negative impact of inflammatory cytokines produced in responses to an enteric virus. Furthermore, TFEB (HLH-30), a master transcriptional regulator of autophagy and lysosomal genes, protects Caenorhabditis elegans from Staphylococcus aureus infection by promoting a cytoprotective transcriptional response20. Autophagy is also essential for the survival of mice with S. aureus-mediated bacteremia and pneumonia. Instead of reducing bacterial burden in these animals, autophagy promotes the viability of endothelial cells in the presence of a pore-forming toxin produced by widely circulating methicillin resistant S. aureus (MRSA) strains21. The vulnerability of autophagy-deficient cells reflects an increase in the toxin receptor ADAM10 at the protein level21, indicating that the protein turnover function of autophagy can indirectly contribute to infectious disease susceptibility. Therapeutically increasing autophagy also improves survival in a mouse model of sepsis through reducing inflammation in the lung22. Thus, in addition to resistance mechanisms aimed at reducing the number of infectious agents, autophagy facilitates tolerance mechanisms that reduce the adverse effect of an infection23.
A related function of autophagy is to inhibit the production of soluble inflammatory mediators, which can come at the cost of diminishing host defense. Deficiency in autophagy proteins protects against intestinal infection by Citrobacter rodentium, improves survival during lung infection by influenza virus, and prevents reactivation of murine herpesvirus 68 (MHV68) from latency24–26. The enhanced host defense in these models are associated with large scale increases in cytokine levels and/or inflammatory gene expression. Although autophagy inhibition confers a short-term benefit during infection by these specific pathogens, the long-term consequence of this heightened immunity may be chronic inflammatory disease. Additionally, as the above examples with S. aureus, Sindbis virus, and a large number of other studies illustrate, autophagy usually benefits the host during a life-threatening infection. The ultimate function of autophagy in immunity may be to mediate a balanced immune response whereby the greatest number of different types of infectious threats are neutralized with as little damage to the host as possible, thereby staving off long term disease.
Crosstalk between autophagy and immune signaling cascades
Amino acid starvation during bacterial infection can induce autophagy27, raising the possibility that sensing changes in nutrient availability is an ancient mechanism to turn on autophagy in response to infectious threats. As the immune system evolved, autophagy and related pathways have been integrated into the complex signaling networks that coordinate multicellular defense strategies. An array of pathogen and damage associated molecular patterns (PAMPs and DAMPs) induce or inhibit autophagy in specific contexts. Also, autophagy can feedback on the process of PAMP and DAMP recognition to serve a regulatory role of preventing an over exuberant response. This creates a set of feedback loops between autophagy and immune signaling pathways that mediate host defense while limiting damage.
NLRs
NOD-like receptors (NLRs) are cytosolic sensors of PAMPs and DAMPs. Many NLRs are inflammasome subunits that mediate IL-1β and IL-18 production and pyroptosis. The NLRP3 inflammasome, for instance, is activated by diverse stimuli that disrupt mitochondrial integrity, including ATP, bacterial products, and uric acid crystals. Mitophagy, a selective form of autophagy tasked with removing damaged mitochondria, inhibits IL-1β and IL-18 production in response to these stimuli by preventing the accumulation of mitochondria-derived DAMPs, such as reactive oxygen species (ROS) and mitochondrial DNA28–30 (Figure 1). Autophagy also removes or prevents leakage of bacterial products from Shigella or Salmonella-containing vacuoles into the cytoplasm, thereby limiting detection of microbial factors in the cytosol by the caspase-11 inflammasome31,32. This model is consistent with a role for autophagy in repairing damaged pathogen-containing vacuoles33, and the observation that autophagy prevents pyroptosis in the presence of invasive bacteria32,34,35. In addition to these examples in which autophagy limits the availability of inflammasome activators (ROS, mtDNA, LPS) in the cytosol, one study has shown that SQSTM1 can target the inflammasome subunit ASC for incorporation into an autophagosome, leading to its inactivation36. These examples illustrate the critical role of autophagy in suppressing inflammation through the removal of PAMPs, DAMPs, and inflammatory signaling intermediates from the cytosol, a theme that will be reinforced throughout this article.
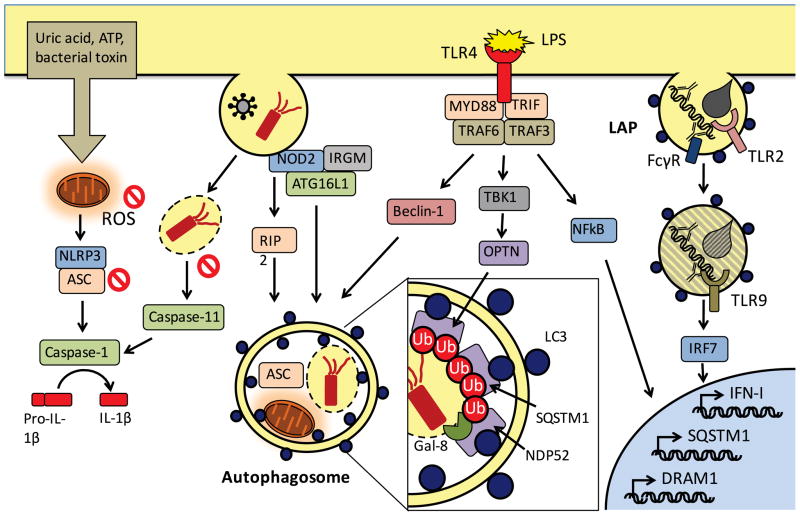
Figure 1. Crosstalk between TLR and NLR signaling and autophagy.
Following LPS activation of TLR4, MYD88 and TRIF signal through TRAF6 and TRAF3 to facilitate autophagy by inducing: (i) the release of Beclin-1 from inhibition by BCL-2, (ii) phosphorylation and activation of optineurin (OPTN) through TBK-1, and (iii) transcription of SQSTM1 and the autophagosome maturation protein DRAM1 downstream of NFκB signaling (see figure). Recognition of internalized fungal glycans and antibody-bound DNA complexes by TLR2 and the Fcγ chain receptor (FcγR) triggers LAP. As the phagosome matures, the fungal pathogen is degraded and TLR9 signals through interferon regulatory factor 7 (IRF7) and type I interferon (IFN-I) transcription. NOD2 in the cytosol recognizes bacterial peptidoglycan or viral RNA from internalized pathogens and subsequently induces autophagy, either by signaling through RIP2 or by directly recruiting ATG16L1 in a complex with IRGM. Incorporation of the bacteria into the autophagosome is achieved by the LC3 binding proteins SQSTM1, OPTN, NDP52, and others, which recognize the damaged vacuole tagged by ubiquitin (Ub) and galectin-8 (Gal-8). In addition to inhibiting pathogen replication, this process reduces leakage of bacterial LPS to prevent activation of the casapse-11 inflammasome. Autophagy also inhibits the NLRP3 inflammasome, which is activated by reactive oxygen species (ROS) and other factors produced by damaged mitochondria following exposure to exogenous agents including uric acid crystals, ATP, and bacterial toxins. The autophagosome sequesters damaged mitochondria and the NLRP3 binding protein ASC to prevent caspase-1 mediated cleavage of pro-IL-1β into its active form.
NLRs also have a role in inducing autophagy in response to the presence of PAMPs and DAMPs in the cytosol. Sensing of uric acid and nigericin by NLRP3, or recognition of poly(dA:dT) double-stranded DNA by AIM2, induces autophagy by triggering nucleotide exchange on the small GTPase RalB36. Amino acid deprivation also signals through RalB to induce autophagy by creating a large multi-protein complex with the exocyst protein Exo84 that links the ULK1 and PI3KC3 complexes37. Interestingly, autophagy induction downstream of GCN2, which senses amino acid depletion, dampens inflammasome-mediated intestinal damage following chemical injury38. Thus, nutrient sensing pathways may have been repurposed for inducing autophagy during inflammatory stress.
NLR activation by infectious agents generally induces autophagy. During L. pneumophila infection of macrophages, flagellin that leaks from the vacuole into the cytosol is recognized by NAIP5 and NLRC4, and the formation of the inflammasome complex induces autophagy by releasing beclin-1 from an inhibitory interaction with NLRC435. Also, the NLRP6 inflammasome regulates the composition of the gut microbiota and is required for autophagosome formation in the intestinal epithelium39. As discussed later, autophagy induction in epithelial cells is critical to the intestinal barrier. These examples indicate that activation of inflammasomes is coupled with induction of autophagy, which most likely reflects the property of inflammasomes as a double-edged sword, where some activity is essential for defense, but excessive cytokine release and pyroptosis cause irreparable damage to the host.
NOD1 and NOD2, the founding members of the NLR family, also induce autophagy. In the presence of bacterial peptidoglycan derivatives, these molecules signal through the adaptor kinase RIP2 to induce NFκB and MAPK signaling. Both NOD1 and NOD2 mediate the recruitment of LC3 to vesicles containing internalized bacteria to initiate xenophagy (Figure 1), although there is disagreement regarding whether this process involves signaling through RIP2 or direct binding between the NLR and ATG16L140–45.
The induction of autophagy following NOD1 and NOD2 activation can dampen the immune response. Specifically, cytokine production by myeloid cells in the presence of bacteria or bacterial ligands that activate NOD2 is increased in the absence of autophagy proteins46–49. NOD2 also recognizes viral RNA, and subsequent RIP2 signaling induces mitophagy through ULK1 phosphorylation. Consequently, NOD2 or RIP2 deficiency increases ROS production by mitochondria and NLRP3 inflammasome activation, which exacerbates lung inflammation during influenza virus infection50. Similarly, NOD2-RIP2 signaling induces autophagy in alveolar macrophages to suppress inflammation caused by the inflammasome during acute lung injury51. Additionally, NOD2 is required for induction of a LAP-like process in dendritic cells (DCs) following internalization of outer-membrane vesicles (OMVs) derived from the commensal bacterium Bacteroides fragillus, a process that mediates regulatory T cell differentiation52. Although the mechanistic contribution of LAP in this setting remains unclear, this study demonstrates a novel role for non-canonical autophagy in suppressing immune reactions at barrier sites where microbial encounters are common. All together, these studies indicate that a major function of autophagy is to keep the immune system in check by counteracting the pro-inflammatory functions of NLRs.
TLRs
Toll-like receptors (TLRs) sense PAMPs at the cell surface or in vesicle lumens, and signal through adaptor proteins MYD88 and/or TRIF to activate TRAF6, which catalyzes lysine 63 (K63) ubiquitination of several signaling intermediates upstream of NFκB and MAPK to induce inflammatory gene expression. Both MYD88 and TRIF signaling promote autophagosome formation (Figure 1), perhaps explaining why a broad range of TLR ligands are capable of inducing autophagy53,54. Upon lipopolysaccharide (LPS) exposure, TLR4 promotes the assembly of the PI3KC3 complex through TRAF6-mediated K63 ubiquitination of beclin-1 to free it from an inhibitory interaction with BCL-255. Signaling through MYD88 and NFκB further increase autophagosome maturation by inducing the expression of DRAM1, a lysosomal transmembrane protein involved in lysosomal acidification56. The ability to target specific substrates to the autophagosome is facilitated by transcriptional induction of SQSTM1 downstream of TLR457. In addition, LPS-induced SQSTM1 recognizes ubiquitin-tagged mitochondria to promote mitophagy-mediated suppression of the NLRP3 inflammasome30 (Figure 1) and thus, the induction of SQSTM1 explains why NFκB signaling is sometimes counter-intuitively anti-inflammatory. TLR4/TRIF activation by Gram-negative bacteria can also induce TRAF3-mediated K63 ubiquitination of TBK1, a kinase that phosphorylates optineurin to increase its binding affinity for LC3, thereby promoting xenophagy by crosslinking LC3 and bacteria bound to optineurin58. These studies indicate that pathogen-sensing by TLRs triggers multiple signaling events that converge on pathogen and organelle-specific autophagy.
Importantly, TLR-mediated induction of autophagy has been validated in vivo. Rift Valley Fever Virus (RVFV) triggers autophagy downstream of TLR7 signaling to restrict viral replication in Drosophila melanogaster59. In mice, MYD88-dependent induction of autophagy in the intestinal epithelium prevents dissemination of Salmonella60. Unlike NLRs in the cytosol, the ability to detect the presence of PAMPs prior to a breach in the membrane may explain why a role for TLR-induced autophagy can be detected as early as 24 hours post-infection in this setting.
Communication between autophagy and TLRs is bidirectional. Autophagy delivers viral RNA to the endosome for TLR7 recognition in plasmacytoid DCs (pDCs)61. In at least some examples, effector functions downstream of TLRs require LC3 recruitment to phagosomes through LAP (Figure 1). When antibody-bound DNA complexes are internalized by pDCs and bind Fcγ receptor (FcγR), LAP mediates the maturation of the phagosome to a vesicle that supports type I interferon (IFN-I) signaling downstream of TLR962. The acidification of phagosomes containing TLR2 ligands in macrophages also occurs through LAP63. Melanin on the cell wall of the fungal pathogen Aspergillus fumigatus inhibits ROS production by the NADPH oxidase, which together with TLR recognition of fungal surface molecules, is a necessary step in recruiting autophagy proteins. However, A. fumigatus is unable to evade LAP upon removal of melanin during germination, and is ultimately degraded8,64. These findings demonstrate how autophagy and LAP support vesicle trafficking events that are critical for TLR-mediated cytokine production and pathogen degradation.
In contrast to the above examples, there are situations in which autophagy proteins and TLRs have an antagonistic relationship. SQSTM1 serves a dual function as both an adaptor molecule for autophagy and a scaffolding protein that binds TRAF6 to mediate NFkB signaling downstream of TLRs65. In keratinocytes, SQSTM1 is targeted for autophagic degradation by virtue of binding to LC3, thereby disrupting TLR4 and TLR2 signaling66. In another example of autophagy and TLR antagonism, MYD88 signaling upon TLR2 recognition of Mycobacterium tuberculosis induces a microRNA (miRNA) that inhibits autophagy by targeting UVRAG, a subunit of the PI3K3C complex, resulting in increased bacterial survival67. Unlike the extensive antagonistic relationship observed between NLRs and autophagy, these situations in which autophagy and TLR signaling inhibit one another have thus far been exceptions and may apply to specific cell types or pathogens.
Antiviral signaling
While autophagy proteins typically promote TLR signaling in the presence of vesicle-bound nucleic acid, autophagy proteins mediate mitophagy to inhibit signaling downstream of cytosolic sensors of viral nucleic acid. RIG-I-like receptors (RLRs) RIG-I and MDA5 sense double-stranded RNA (dsRNA) in the cytosol and signal through the mitochondrial antiviral signaling protein (MAVS), which oligomerizes on the mitochondrial outer-membrane to induce IFN-I expression by activating the transcription factors IRF3 and IRF7. Mitophagy suppresses IFN-I production by removing the platform for RLR signaling and causes degradation of signaling intermediates such as MAVS68–70 (Figure 2a). ROS produced by accumulating mitochondria also contributes to excess IFN-I production when mitophagy is inhibited71. When MAVS signaling is triggered by viral infection, the ATG16L1 complex is recruited to mitochondria by NLRX1, TUFM, and COX5b68,70 (Figure 2a). For this reason, cells deficient in autophagy proteins, NLRX1, or COX5b display enhanced IFN-I production and are better able to restrict the replication of a variety of viruses68–72. Presumably, mitophagy is coupled to detection of cytosolic RNA to prevent sustained pathological IFN-I production, but this model has not been formally demonstrated.
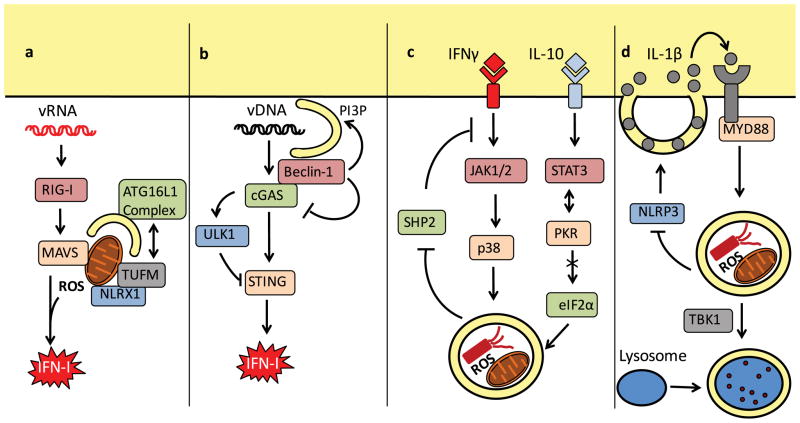
Figure 2. Intersection between autophagy and cytokines.
Several examples have been reported in which autophagy regulates cytokine production, or is subject to regulation by cytokines. Viral RNA (vRNA) recognition by RIG-I induces mitochondrial ROS production and MAVS signaling, leading to IFN-I transcription. Mitophagy following recruitment of the ATG16L1 complex by NLRX1 and TUFM (or COX5B, not shown) inhibits this pathway by removing the MAVS signaling platform and inhibiting ROS production (a). cGAS converts cytosolic DNA (from viruses, bacteria or host) to cGAMP for recognition by STING and subsequent IFN-I signaling. cGAS activates ULK1, which mediates an inhibitory phosphorylation of STING. Also, binding between beclin-1 and cGAS allows beclin-1 to induce autophagy through the PI3KC3 activity to remove the cytosolic DNA and simultaneously inhibits cGAS-dependent IFN-I production (b). IFN-γ induces autophagy through JAK1, JAK2, and p38. This pathway is reinforced by mitophogy because mitochondrial ROS activates SHP-2, an inhibitor of IFN-γ signaling. IL-10 can inhibit autophagy by promoting binding between STAT3 and PKR, which inhibits activation of eIF2α (c). In addition to suppressing IL-1β production by inhibiting the NLRP3 inflammasome, autophagy mediates the secretion of IL-1β. Extracellular IL-1β signals through the IL-1R and MYD88 to induce autophagy, and autophagosome maturation and degradation of engulfed material including intracellular bacteria is dependent on TBK1 (d).
Autophagy also intersects with pathways responsible for sensing cytosolic DNA, which is associated with viral infection, intracellular bacteria, and autoimmunity. Cyclic dinucleotides generated by cyclic GMP-AMP synthase (cGAS) in the presence of dsDNA activate the transmembrane protein stimulator of interferon genes (STING) to induce IFN-I expression. STING colocalizes with autophagy proteins including LC3, and loss of ATG9L1 leads to aberrant STING trafficking and activation73. However, STING function was unaffected by deletion of the E1-like enzyme ATG773, implicating a non-canonical autophagy pathway in membrane trafficking events during dsDNA recognition. Also, ULK1 phosphorylates STING to inhibit IRF3 and aberrant IFN-I expression74 (Figure 2b). Similar to autophagy induction during glucose starvation, cyclic dinucleotides induce AMP-activated protein kinase (AMPK) activation, which leads to phosphorylation and activation of ULK1, thus serving as a negative feedback loop74. During herpes simplex virus-1 (HSV-1) infection, beclin-1 binds and inhibits cGAS. This interaction simultaneously frees beclin-1 from inhibition by rubicon (run domain Beclin-1-interacting and cysteine-rich domain-containing protein) to enhance PI3KC3 activity and autophagy-mediated degradation of viral DNA, thus reducing both the amount of cytosolic DNA and the downstream signaling75 (Figure 2b). Autophagy also prevents pathological STING activation by targeting damaged DNA that leaks from the nucleus to the lysosome where it is degraded by DNASE2a76.
Spontaneous IFN-I signaling occurs upon autophagy inhibition in intestinal tissue and tumor cells24,77,78, indicating that autophagy in some organs or cell types is constitutively suppressing cytokine release. An IFN-I signature in the absence of an infectious trigger could reflect an inappropriate immune response to host nucleic acid, the microbiota, or endogenous retroviruses. Given our growing appreciation of the contribution of IFN-I to cancer and autoimmunity, this autophagy-mediated control of cytokine expression under steady-state conditions is likely relevant to situations beyond infectious disease.
Cytokines
Consistent with the role of autophagy in supporting cellular immunity, the Th1 cytokines interferon-γ (IFNγ) and TNFα generally upregulate xenophagy in target cells79–81. IFNγ induces autophagy through the JAK1/JAK2 and p38 MAPK pathway independently of signal transducer and activator of transcription 1 (STAT1)82. In turn, autophagy promotes IFNγ signaling by limiting ROS production, which if left to accumulate, would activate the JAK/STAT inhibitory phosphatase SHP283 (Figure 2c). In addition to conventional autophagy, IFNγ induces a LAP-like process in hepatocytes infected by the malarial parasite Plasmodium vivax. The deposition of LC3 onto the parasitophorous vacuole leads to the recruitment of lysosomes and killing of the parasite84. As mentioned earlier, IFNγ suppress T. gondii and norovirus replication through an incompletely understood type of non-canonical autophagy9–11. Therefore, IFNγ induces canonical and non-canonical autophagy to inhibit intracellular pathogen replication.
Cytokines that signal through other STAT molecules do not necessarily induce autophagy. Binding of protein kinase R (PKR) by STAT3 prevents PKR-mediated phosphorylation of eIF2α, a stress-responsive regulator of translation that promotes autophagy85 (Figure 2c). As seen with IL-10, any cytokine that activates STAT3 can theoretically interfere with autophagy86. STAT6 signaling downstream of the Th2 cytokines IL-4 and IL-13 also inhibits autophagy induction by IFNγ in macrophages80. However, DCs differentiated in the presence of IL-4 display increased expression of RUFY4, a positive regulator of autophagosome growth and fusion with lysosomes87. The amount of time the cell is exposed to Th2 cytokines, and the presence of other cytokines such as IFNγ and GM-CSF, may explain these contradictory effects of Th2 cytokines on autophagy. These studies establish a link between autophagy and Th2 or regulatory cytokines. How this impacts host defense requires further investigation.
Autophagy inhibits IL-1β production by repressing inflammasome activation, but can facilitate the secretion of this cytokine88. IL-1β does not undergo conventional secretion due to the absence of a signal peptide, but can pass through a permeabilized plasma membrane89. Alternatively, when membrane integrity is intact, IL-1β can be incorporated into the space between the inner- and outer-membrane of the autophagosome, and is released from the cell following autophagosome fusion with the plasma membrane or multivesicular body90 (Figure 2d). IL-1β is ultimately secreted from autophagy-deficient cells, likely because of the permeabilized membrane accompanying increased inflammasome activity and pyroptosis.
Secreted IL-1β, in turn, activates autophagy through TBK191 (Figure 2d). IL-1β (also IL-1α and IFNγ) induces ubiquitination of beclin-1, suggesting that it can also activate autophagy through a mechanism similar to LPS (Figure 1). Finally, secretion of other IL-1 family members, specifically IL-1α and MIF, is increased in autophagy-deficient macrophages as a downstream consequence of mitochondrial ROS accumulation92,93. It is likely that autophagy induction following the engagement of the IL-1R is another mechanism of negative feedback through ROS suppression.
Autophagy may be particularly important for preventing Th17 responses because the cytokines that are suppressed by autophagy are key to inducing IL-17 expression by T cells: IL-1α, IL-1β, IL-18, IL-23, IL-6, TGFβ, and MIF47,92–95. Excess IL-1α released by autophagy-deficient macrophages induces Th17 differentiation and exacerbates lung inflammation during M. tuberculosis infection (Figure 3). Similarly, IL-1β produced downstream of autophagy inhibition in DCs acts in an autocrine manner to mediate IL-23 production, leading to IL-17 secretion by γδT cells94. There is less evidence that Th1 and other branches of adaptive immunity benefit from autophagy-deficiency in macrophages and DCs. One reason may be that IFN-I, which is over-produced upon autophagy-inhibition, is known to inhibit IFNγ activity96. An inflammatory milieu could also cause T cell exhaustion. As discussed later, the role of autophagy in antigen presentation is another variable that requires consideration.
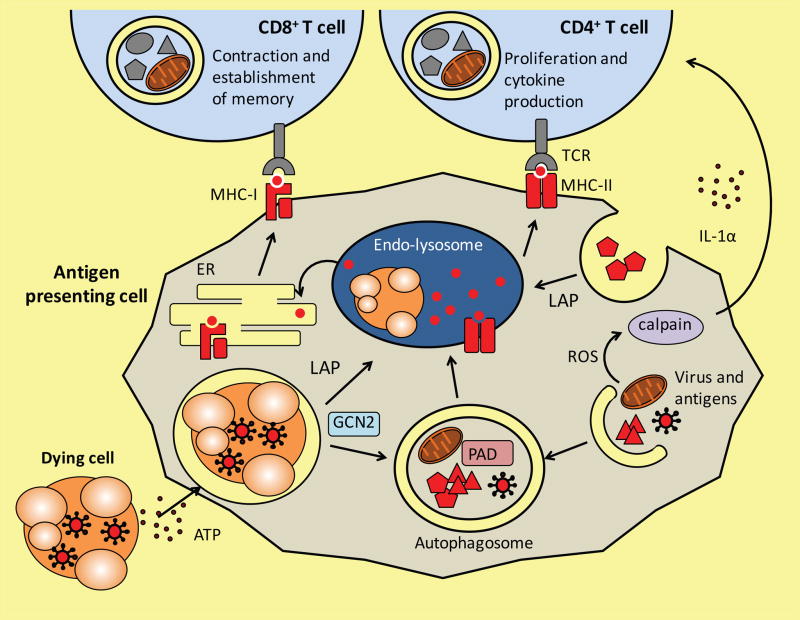
Figure 3. Autophagy coordinates a multicellular adaptive immune response.
Autophagy activity in T cells, antigen presenting cells (APCs), and dying cells affects T cell immunity. Autophagy in APCs such as dendritic cells delivers intracellular and extracellular antigens to endo-lysosomal vesicles where it can intersect the MHC-II presentation pathway and stimulate a CD4+ T cell response. Peptidylarginine deiminases (PADs) in autophagosomes generate citrullinated peptides, thereby affecting the repertoire of antigens being presented. Extracellular antigens can also be delivered to the endoso-lysosome by LAP. Autophagy-mediated release of ATP by dying cells, such as those infected by viruses, leads to engulfment by the APC. Internalized antigens from the dying cell can then be cross-presented on MHC-I molecules to stimulate CD8+ T cells, a process mediated by autophagy or potentially LAP downstream of GCN2 activation. The removal of ROS producing mitochondria inhibits calpain-mediated processing of IL-1α, thereby decreasing Th17 differentiation of CD4+ T cells by secreted IL-1α. Naïve CD4+ T cells require autophagy for survival and proliferation, and cytokine production once activated. The establishment of memory by CD8+ T cells is also dependent on autophagy.
DAMPs
Cell death can lead to extracellular release of DAMPs that are confined within the cell, such as nucleic acids, ATP, high mobility group box 1 (HMGB1), and IL-1β. Autophagy is induced by ATP, and controls the secretion of ATP. Purinergic receptors and transporters that recognize exogenous ATP triggers autophagy through AMPK-mediated mTOR inhibition and dephosphorylation of AKT97–100. Prior to cell death, autophagy regulates the secretion of ATP by mediating the migration of ATP-containing lysosomes towards the plasma membrane101. Due to the importance of ATP as a chemotactic signal, loss of autophagy in tumor cells diminishes the ability of chemotherapeutic agents to trigger a robust anti-tumor immune response (Figure 3)102.
Like IL-1β, autophagy facilitates the release of HMGB1, a chromatin-associated nuclear protein, from stressed or dying tumor cells103. Extracellular HMGB1 is recognized by receptor for advanced glycation end products (RAGE), resulting in decreased mTOR activity and increased autophagy104. Nuclear HMGB1 regulates the expression of heat shock protein b 1 (HSPB1), a chaperone protein that promotes mitophagy105. Also, HMGB1 translocates to the cytosol in the presence of ROS, where it induces autophagy by releasing beclin-1 from inhibition by BCL-2103. Endogenous HMGB1 can also promote autophagy by protecting beclin-1 and ATG5 from calpain-mediated cleavage106. Thus, when HMGB1 is removed from macrophages or intestinal epithelial cells, the balance shifts from autophagy to apoptosis, and favors exaggerated cytokine production to increase inflammation106,107.
To summarize, an extensive amount of crosstalk has been observed between autophagy and immune signaling cascades downstream of the array of receptors that recognize PAMPs, DAMPs, and cytokines. The finding that autophagy is sometimes necessary for IFN-I production (e.g., by functioning together with TLRs in pDCs) but can also dampen IFN-I signaling (e.g., through mitophagy) reinforces the fact that the relationship between autophagy and a given immune pathway is context-dependent and not generalizable. However, one recurring observation is that pathways that induce autophagy are often inhibited by autophagy to prevent sustained activation. This role of autophagy in negative feedback is most obvious in the presence of inflammasome substrates and viral nucleic acids in the cytosol, where autophagy limits the amount of cytokines produced. This function is not mutually exclusive from antimicrobial functions of autophagy such as xenophagy; removing the infectious threat and removing the PAMP that triggers the inflammatory response are both ways to restore homeostasis.
Autophagy in multicellular immunity and inflammatory disease
Autophagy and adaptive immunity
A role for autophagy can be seen in virtually all the cell types that participate in adaptive immunity – lymphocytes, antigen presenting cells (APCs), dying cells, and cells that contribute to the inflammatory milieu (Figure 3). Autophagy, most likely through mitochondrial quality control, is necessary for the survival and proliferation of T cells (CD4, CD8, and NK T cells)108–114, memory responses of CD8 T cells, and activated NK cell maintenance115–119. In effector CD4 T cells, autophagy activity generates the ATP necessary to produce IL-2 and IFN-γ120. Autophagy may have analogous functions in maintaining organelle and metabolic homeostasis in the B cell lineage because Atg5 deletion leads to an absence of B-1a B cells and a defect in antibody production by plasma cells121–123. The induction of autophagy in naïve CD4 T cells following TCR stimulation is dependent on mTOR inhibition downstream of the ubiquitin editing enzyme TNFAIP3 (A20)114. TCR engagement also induces autophagy-mediated degradation of the upstream NFκB signaling molecule BCL-10, thus preventing hyperactivation of effector T cells124. Inhibiting autophagy in regulatory T cells (Tregs) causes apoptosis and lineage instability due to aberrant metabolism, which leads to unrestrained Th2 responses and inflammation at intestinal barrier sites125,126. As expected, the role of autophagy in supporting these various lymphocyte lineages is necessary for optimal immune responses to viruses, parasites, self-antigens, and tumors115,122,125,126.
On the APC side, autophagy affects the repertoire of peptides presented on MHC-II molecules127, including by thymic epithelial cells that mediate selection of developing T cells128. Specific antigens have been shown to depend on autophagy for presentation. Autophagosomes transport peptidylarginine deiminases (PADs) that convert arginine to citrulline, which generates the citrullinated self-peptides implicated in rheumatoid arthritis129 (Figure 3). Autophagy in virally-infected cells generate antigens for presentation to CD4 T cells by delivering cytosolic proteins to the lysosome for antigen processing, such as the Epstein-Barr virus protein EBNA-1130 (Figure 3). In some cases, antigens are generated from ubiquitinated protein aggregates and pathogen-containing vacuoles that are recognized by SQSTM1, which become substrates for either MHC-I or MHC-II presentation131,132. Autophagy can be augmented to enhance antigen presentation through previously discussed signals, such as IFN-γ and NOD2 activation41,131,132. Autophagy or LAP is also critical for the processing of exogenous antigens by mediating the fusion of phagosomes containing TLR ligands or apoptotic corpses with lysosomes in DCs133–135 (Figure 3). This process is necessary for MHC-II presentation that drives the antiviral Th1 response during herpes simplex virus-2 (HSV-2) infection136. It is possible that avoidance of CD4 T cell recognition is a major reason why some pathogens encode proteins that inhibit autophagy. For instance, the HSV-1 protein ICP34.5 binds beclin-1 to inhibit autophagy-mediated MHC-II antigen presentation in DCs137.
DCs can also present exogenous antigens on MHC-I molecules through cross-presentation. Challenge with the yellow fever virus vaccine YF-17D induces autophagy in DCs through induction of the amino acid starvation sensor GCN2. Inhibiting either autophagy proteins or GCN2 impairs the ability of DCs to mediate proliferation of CD8 T cells when co-cultured with infected cells138 (Figure 3), providing a clinically relevant example of autophagy-dependent MHC-I cross-presentation. However, as with certain examples of antigen presentation on MHC-II, the role for autophagy proteins revealed by this study may be more likely to reflect LAP rather than autophagy. Now that the tools are available, future studies will be able to distinguish the role of canonical versus non-canonical forms of autophagy in antigen presentation.
ATG16L1 in Crohn’s disease and graft-versus-host disease
Genetic variants that occur near or within autophagy genes are implicated in several inflammatory disorders (Table 1). One of the first indicators that autophagy dysfunction contributes to inflammatory disease was provided by the genetic link between Crohn’s disease and a common polymorphism in ATG16L1139. The disease polymorphism results in a threonine to alanine coding change (T300A) that destabilizes the ATG16L1 protein product by introducing a caspase-3 cleavage site48,49. The function of autophagy in inhibiting cytokine production is consistent with the idea that this disease stems from an exaggerated immune response directed towards the gut microbiota. Additionally, inhibiting autophagy within the intestinal epithelium causes defects in antimicrobial granule formation by Paneth cells and mucus secretion by goblet cells19,140–142. Together with xenophagy, the role of autophagy in maintaining these secretory cell lineages helps prevent breaches of the epithelial barrier by Salmonella and commensal bacteria60,143. The relevance of these epithelial-specific functions of autophagy is supported by the observation that knock-in mice harboring the ATG16L1T300A disease variant are susceptible to enteric bacterial infections, and display defects in Paneth cells and goblet cells48,49. Also, the crosstalk between the ER stress pathway and autophagy in Paneth cells was shown to have a central role in preventing intestinal inflammation142, directly implicating the organelle homeostasis function of autophagy in this secretory cell type.
Table 1.
Examples of autophagy genetic variants associated with chronic inflammatory disorders.
| Disease | Variant | Proposed mechanism | References |
|---|---|---|---|
| Crohn’s disease | T300A coding variant of ATG16L1 (rs2241880) | Destabilization of ATG16L1 decreases autophagy to cause increased inflammasome activation, defects in secretory lineages of the intestinal epithelium, impaired xenophagy, and failure to induce Treg differentiation, all of which can contribute to an imbalanced relationship with the gut microbiota. | 48,49,52,139,140,166 |
| Graft versus host disease | T300A coding variant of ATG16L1 (rs2241880) | Hyperactive autophagy deficient dendritic cells induce enhanced proliferation of donor-derived T cells in allogeneic HSCT recipients. | 144 |
| Systemic lupus erythematosus | Polymorphism in non-coding region proximal to ATG5 (rs548234) | Increased ATG5 expression, resulting in enhanced autophagy or LAP, facilitates nucleic acid sensing by TLRs. Alternatively, impaired clearance of dead cells can increase systemic cytokine levels downstream of LAP-deficiency. | 62,146,148,150,151 |
| Asthma | Polymorphism in ATG5 promoter region (rs12201458, rs510432) | Increased ATG5 promoter activity augments goblet cell differentiation and mucus production. | 145,147 |
| Vici Syndrome | Loss of function mutations in Epg-5 (recessive coding variants) | EPG-5 mediates the degradative function of autophagy, which is necessary to prevent myopathies. Consistent with the role of autophagy in suppressing cytokine production, EPG-5 deletion creates a heightened state of inflammation, which may be related to the immune dysfunction observed in some patients. | 26,167 |
| Rheumatoid arthritis, type 1 diabetes, and others | Non-coding variants of PTPN22 (rs6679677, rs2476601, rs1893217) and CLEC16A (rs2903692, rs725613, rs17673553) | Variants within or near the PTPN22 and CLEC16A loci are associated with a range of autoimmune diseases including rheumatoid arthritis and type 1 diabetes. Loss of PTPN22 and CLEC16A function inhibits degradation of autophagy substrates, which could contribute to the generation of autoreactive T cells due to impaired antigen presentation by thymic epithelial cells. CLEC16A also maintains pancreatic β cell function through mitophagy. Defective phosphofructokinase activity rather than genetic predisposition may cause autophagy defects in T cells from RA patients. Also, it is unclear how these findings fit with the requirement of autophagy for generating citrullinated peptides recognized by T cells during RA. | 129,166,168–174 |
The same ATG16L1T300A polymorphism increases the risk of death following allogeneic hematopoietic stem cell transplantation (HSCT)144. Autophagy was found to prevent lethal graft-versus-host disease (GVHD) in a preclinical animal model of HSCT by suppressing DC hyperactivity. These autophagy-deficient DCs displayed alterations in the expression of genes implicated in endolysosomal trafficking including those that affect NFκB and MAPK signaling144. The reason why autophagy suppresses rather than promotes the ability of DCs to stimulate T cells in this situation is likely explained by differences between allogeneic and syngeneic T cell activation, where the former has less constraints on the antigen being presented. Given that GVHD frequently affects the gut, it would be interesting to determine whether autophagy in the intestinal epithelium also has a role in preventing disease following HSCT.
ATG5 non-coding variants
Polymorphisms associated with increased ATG5 expression are linked to asthma and systemic lupus erythematosus (SLE)145,146. Although it remains possible that these polymorphisms act through neighboring genes and not ATG5, autophagy contributes to biological processes that are relevant to these disorders including regulation of the cytokine milieu and antigen presentation. In airway epithelial cells, autophagy mediates goblet cell differentiation and mucus secretion in response to IL-13147, suggesting that enhanced autophagy contributes to the pathological overproduction of mucus observed in asthmatic individuals.
Markers of increased autophagy have been observed in B and T lymphocytes from SLE patients148,149, which could reflect genetic predisposition, or an attempt to stem further cytokine production. The multi-organ inflammation observed in SLE is associated with immune complexes consisting of antibodies bound to nucleic acid and histones, which induce aberrant IFN-I production following recognition by the DNA and RNA sensors TLR7 and TLR9. LAP, which is dependent on ATG5, mediates the delivery of such immune complexes in pDCs, resulting in TLR9 activation and IFN-I production62. Also, ATG5 in B cells is necessary for TLR7-dependent generation of autoantibodies and SLE pathologies, hinting at an early role for autophagy proteins in disease progression150. In myeloid cells, ATG5 and other autophagy proteins prevent the production of self-reactive antibodies. Dying cells are not properly degraded by macrophages in LAP-deficient mice, leading to a general increase in serological markers of inflammation and signs of SLE as the animals age151. Of note, among the different LAP-deficient mice used in this study were rubicon knockouts, which display increased autophagy. One interpretation of this result is that loss of LAP in myeloid cells is more significant in the development of SLE (in aged mice) than a potential increase in lymphocyte autophagy. Studies that examine the effect of specifically increasing autophagy in B cells are warranted.
Inflammatory disease accompanied by autophagy dysfunction
The list of immunological diseases accompanied by autophagy dysfunction extends beyond those caused by mutations in autophagy genes. Chronic granulomatous disease (CGD) occurs in individuals harboring loss of function mutations in subunits of the NADPH oxidase, which is necessary for generating ROS and recruiting LC3 to the phagosome152. Monocytes from CGD patients are defective in LAP-mediated control of A. fumigatus64. Similarly, APCs deficient in NAPDH oxidase activity display reduced MHC-I and MHC-II presentation of fungal antigens133,153. Cells from CGD patients also display defects in autophagy-mediated suppression of IL-1β in the presence of the spirochete Borrelia burgdorferi47. This failure of autophagy-mediated control of IL-1β production contributes to Th17-driven colitis in CGD patients, which can be treated with an antibody against IL-1R (anakinra)154.
A defect in pathogen handling through autophagy may also explain why individuals with Niemen-Pick disease type C 1 (NPC1), a lysosomal storage disorder, sometimes develop granulomatous inflammation in the intestine that resembles Crohn’s disease. NPC1 mutation inhibits NOD2-mediated xenophagy155. In another example, cystic fibrosis transmembrane conductance receptor (CFTR) mutation leads to sequestration of the PI3KC3 complex into protein aggregates and downregulation of autophagy156. This block in autophagy potentially contributes to chronic lung inflammation and recurring pulmonary infections characteristic of CF. Indeed, CFTR mutation increases susceptibility of macrophages to Burkholderia cenocepacia infection and exacerbates IL-1β production157. Autophagy inhibition in CF patients is further exacerbated upon treatment with the antibiotic azithromycin, which is associated with increased infection by nontuberculous mycobacteria158. Thus, restoration of autophagy may ameliorate many chronic inflammatory disorders.
Conclusion
Autophagy and related processes regulate intracellular trafficking of pathogens, production of inflammatory mediators, and viability of cells that coordinate immunity. Through these functions, the autophagy machinery controls complex multicellular immune responses at the whole organism level. The literature highlighted in this article reinforces three themes related to how these functions of autophagy are integrated into inflammatory signaling cascades to ensure an appropriate response to environmental threats and a return to homeostasis: (1) pathways that induce autophagy are subject to regulation by autophagy, (2) autophagy can increase and decrease different parts of the same inflammatory signaling cascade in a context-dependent manner, and (3) non-canonical autophagy is pervasive. Although these principles apply to the role of autophagy in other situations, they are perhaps most obvious in the recent literature examining the function of autophagy proteins in host defense and inflammatory disease.
These three themes have implications for the clinical application of autophagy inducers and inhibitors. Short-term induction of autophagy is effective in reducing the burden of intracellular pathogens16, and can simultaneously enhance TLR-mediated cytokine production and antigen presentation by DCs to improve adaptive immunity138. Treating chronic infections is potentially more challenging and will require consideration of the bidirectional communication between autophagy and inflammation. Also, given the regulatory role of autophagy in immunity, it may be reasonable to ask whether autophagy is actually beneficial for host defense. It is important to remind ourselves that the measure of an effective immune response is not how vigorous it is, but how efficiently the threat is neutralized without damaging the host. Therefore, the role of autophagy in reducing inflammation is not necessarily counterproductive to the role of autophagy in reducing pathogen burden.
Treating complex inflammatory disorders by modulating autophagy has similar challenges. Prior to considering this strategy, it is important to identify the physiological situations in which the net effect of autophagy on the level of IL-1β, IFN-I, and other cytokines is positive versus negative. It is also equally necessary to determine the cell types and organs most affected by autophagy activity. Although the discovery of non-canonical forms of autophagy has increased the complexity of the field, we may be able to exploit the subtle differences in the function of different parts of the autophagy machinery. Indeed, deleting some autophagy genes in macrophages leads to a more pronounced inflammatory outcome than others25,151, perhaps indicating that inhibition of certain parts of the pathway can be compensated by other membrane trafficking processes, and that some autophagy proteins have partially redundant functions. It may be possible to target different nodes of the autophagy pathway without broadly affecting all the downstream immune functions of autophagy proteins.
Finally, defects in autophagy coincide with aging, metabolic disease, cancer, myopathies, and neurodegenerative disorders. Indeed, transgenic mice engineered to overexpress Atg5 display increased lifespan, and improvements in glucose sensitivity and motor function159. If humans are to receive autophagy-based treatments for these conditions associated with aging, it will be necessary to understand the effect of altered autophagy on inflammation, which universally accompanies maladies.
Key points.
The cellular degradative process of autophagy participates in multiple aspects of immunity, including cell autonomous defense, innate immune signaling, and antigen presentation.
Extensive crosstalk between autophagy and inflammatory signaling cascades ensures a robust immune response towards pathogens while avoiding collateral damage to the host. Several chronic inflammatory disorders are associated with autophagy dysfunction.
Pathways that induce autophagy, such as those downstream of pattern recognition receptors, are subject to regulation by autophagy.
Autophagy can increase and decrease different parts of the same inflammatory signaling cascade in a context-dependent manner.
Many immune-related functions of conserved autophagy proteins reflect non-canonical forms of autophagy, representing new opportunities for therapeutic intervention.
Acknowledgments
The author would like to thank Victor Torres (New York University School of Medicine) and members of the Cadwell lab for comments on the manuscript. K.C. is supported by NIH grants DK103788, DK093668, HL123340, Stony Wold-Herbert Fund, and philanthropic support from Bernard Levine. K.C. is a Burroughs Wellcome Fund Investigator in the Pathogenesis of Infectious Diseases.
Glossary terms
- Autophagy
An evolutionarily conserved process in which double-membrane vacuoles sequester intracellular contents (such as damaged organelles and macromolecules) and target them for degradation, through fusion to lysosomes
- Xenophagy
A cell-intrinsic defense mechanism involving the selective degradation of microorganisms (such as bacteria, fungi, parasites or viruses) through an autophagy-related mechanism
- Sequestosome 1
A prototypical adaptor protein that targets ubiquitinated proteins for selective autophagy by binding ubiquitin and LC3. Through incorporation into the autophagosome, SQSTM1 itself becomes a substrate for autophagic degradation
- Inflammasome
A multi-protein oligomer that catalyzes the autoactivation of caspase-1, which cleaves pro-IL-1β and pro-IL-18 to produce the active forms of these cytokines
- Pyroptosis
An inflammatory form of programmed cell death that is dependent on inflammasome activation of caspase-1
- Outer membrane vesicles
(OMVs). Vesicles derived from the bacterial outer membrane that mediate communication among bacteria. OMVs can be immunogenic and mediate interaction between commensal or pathogenic bacteria and the host
- Citrullinated self-peptide
A self-peptide that incorporates the amino acid citrulline. These peptides are generated post-translationally by peptidylarginine deiminases. The citrulline moiety is the essential part of the antigenic determinant towards which characteristic autoantibodies in patients with rheumatoid arthritis are generated
- Cross-presentation
The initiation of a CD8+ T cell response to an antigen that is not present within antigen-presenting cells (APCs). This exogenous antigen must be taken up by APCs and then re-routed to the MHC class I pathway of antigen presentation
- Crohn’s disease
Together with ulcerative colitis, Crohn’s disease is one of the two main forms of chronic inflammatory bowel disease (IBD). It most commonly affects the lower portion of the small intestine, resulting in symptoms of abdominal pain, diarrhoea, fever and weight loss. Analysis of the strong genetic predisposition led to the identification of mutations in the NOD2 gene that are particularly strongly associated with ileal disease, but not with ulcerative colitis
- Endoplasmic reticulum stress
(ER stress). A conserved stress response pathway that senses the accumulation of unfolded proteins in the ER
- Hematopoietic stem cell transplantation
(HSCT). A procedure in which HSCs from bone marrow or blood is transplanted to treat leukemia and other disorders
- Graft-versus-host disease
(GVHD). A common complication of HSC transplantation in which allogeneic T cells derived from a non-identical donor attack healthy tissue in the recipient
- Chronic granulomatous disease
An inherited disorder caused by defective oxidase activity in the respiratory burst of phagocytes. It results from mutations in any of four genes that are necessary to generate the superoxide radicals required for neutrophil antimicrobial function. Affected patients suffer from increased susceptibility to recurrent infections.
Biography
Ken Cadwell received his Ph.D. from University of California, Berkeley, and is currently an associate professor in the Skirball Institute at New York University School of Medicine. His laboratory investigates how the immune system avoids collateral damage to the host during an infection. He is a Burroughs Wellcome Fund Investigator in the Pathogenesis of Infectious Diseases.
Footnotes
Competing interest statement
The author declares no competing interests.
References
- 1.Russell RC, et al. ULK1 induces autophagy by phosphorylating Beclin-1 and activating VPS34 lipid kinase. Nat Cell Biol. 2013;15:741–750. doi: 10.1038/ncb2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ge L, Melville D, Zhang M, Schekman R. The ER-Golgi intermediate compartment is a key membrane source for the LC3 lipidation step of autophagosome biogenesis. eLife. 2013;2:e00947. doi: 10.7554/eLife.00947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamasaki M, et al. Autophagosomes form at ER-mitochondria contact sites. Nature. 2013;495:389–393. doi: 10.1038/nature11910. [DOI] [PubMed] [Google Scholar]
- 4.Dooley HC, et al. WIPI2 links LC3 conjugation with PI3P, autophagosome formation, and pathogen clearance by recruiting Atg12-5-16L1. Molecular cell. 2014;55:238–252. doi: 10.1016/j.molcel.2014.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Randow F, Youle RJ. Self and nonself: how autophagy targets mitochondria and bacteria. Cell Host Microbe. 2014;15:403–411. doi: 10.1016/j.chom.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choy A, et al. The Legionella effector RavZ inhibits host autophagy through irreversible Atg8 deconjugation. Science. 2012;338:1072–1076. doi: 10.1126/science.1227026. This study provides an example of how intracellular bacteria evade trafficking to the lysosome by blocking autophagy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen YH, et al. Phosphatidylserine vesicles enable efficient en bloc transmission of enteroviruses. Cell. 2015;160:619–630. doi: 10.1016/j.cell.2015.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martinez J, et al. Molecular characterization of LC3-associated phagocytosis reveals distinct roles for Rubicon, NOX2 and autophagy proteins. Nat Cell Biol. 2015;17:893–906. doi: 10.1038/ncb3192. This study demonstrates that LC3-associated phagocytosis is distinguished from autophagy by its dependence on Rubicon and NOX2. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.Zhao Z, et al. Autophagosome-independent essential function for the autophagy protein Atg5 in cellular immunity to intracellular pathogens. Cell Host Microbe. 2008;4:458–469. doi: 10.1016/j.chom.2008.10.003. S1931-3128(08)00329-6 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang S, et al. Nondegradative role of Atg5-Atg12/Atg16L1 autophagy protein complex in antiviral activity of interferon gamma. Cell host & microbe. 2012;11:397–409. doi: 10.1016/j.chom.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi J, et al. The parasitophorous vacuole membrane of Toxoplasma gondii is targeted for disruption by ubiquitin-like conjugation systems of autophagy. Immunity. 2014;40:924–935. doi: 10.1016/j.immuni.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Selleck EM, et al. A Noncanonical Autophagy Pathway Restricts Toxoplasma gondii Growth in a Strain-Specific Manner in IFN-gamma-Activated Human Cells. mBio. 2015;6:e01157–01115. doi: 10.1128/mBio.01157-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohshima J, et al. Role of mouse and human autophagy proteins in IFN-gamma-induced cell-autonomous responses against Toxoplasma gondii. J Immunol. 2014;192:3328–3335. doi: 10.4049/jimmunol.1302822. [DOI] [PubMed] [Google Scholar]
- 14.Haldar AK, Piro AS, Pilla DM, Yamamoto M, Coers J. The E2-like conjugation enzyme Atg3 promotes binding of IRG and Gbp proteins to Chlamydia- and Toxoplasma-containing vacuoles and host resistance. PLoS One. 2014;9:e86684. doi: 10.1371/journal.pone.0086684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park S, et al. Targeting by AutophaGy proteins (TAG): Targeting of IFNG-inducible GTPases to membranes by the LC3 conjugation system of autophagy. Autophagy. 2016 doi: 10.1080/15548627.2016.1178447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shoji-Kawata S, et al. Identification of a candidate therapeutic autophagy-inducing peptide. Nature. 2013;494:201–206. doi: 10.1038/nature11866. This study shows that a cell permeable beclin-1 peptide induces autophagy to enhance host defense. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orvedahl A, et al. Autophagy protects against Sindbis virus infection of the central nervous system. Cell Host Microbe. 2010;7:115–127. doi: 10.1016/j.chom.2010.01.007. S1931-3128(10)00033-8 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kernbauer E, Ding Y, Cadwell K. An enteric virus can replace the beneficial function of commensal bacteria. Nature. 2014;516:94–98. doi: 10.1038/nature13960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cadwell K, et al. Virus-plus-susceptibility gene interaction determines Crohn’s disease gene Atg16L1 phenotypes in intestine. Cell. 2010;141:1135–1145. doi: 10.1016/j.cell.2010.05.009. S0092-8674(10)00545-3 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Visvikis O, et al. Innate host defense requires TFEB-mediated transcription of cytoprotective and antimicrobial genes. Immunity. 2014;40:896–909. doi: 10.1016/j.immuni.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maurer K, et al. Autophagy Mediates Tolerance to Staphylococcus aureus Alpha-Toxin. Cell Host Microbe. 2015;17:429–440. doi: 10.1016/j.chom.2015.03.001. This study shows that autophagy limits damage caused by a pore-forming toxin from a clinical isolate of Staphylococcus aureus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Figueiredo N, et al. Anthracyclines induce DNA damage response-mediated protection against severe sepsis. Immunity. 2013;39:874–884. doi: 10.1016/j.immuni.2013.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medzhitov R, Schneider DS, Soares MP. Disease tolerance as a defense strategy. Science. 2012;335:936–941. doi: 10.1126/science.1214935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marchiando AM, et al. A deficiency in the autophagy gene Atg16L1 enhances resistance to enteric bacterial infection. Cell Host Microbe. 2013;14:216–224. doi: 10.1016/j.chom.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park S, et al. Autophagy Genes Enhance Murine Gammaherpesvirus 68 Reactivation from Latency by Preventing Virus-Induced Systemic Inflammation. Cell Host Microbe. 2016;19:91–101. doi: 10.1016/j.chom.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu Q, et al. Homeostatic Control of Innate Lung Inflammation by Vici Syndrome Gene Epg5 and Additional Autophagy Genes Promotes Influenza Pathogenesis. Cell Host Microbe. 2016;19:102–113. doi: 10.1016/j.chom.2015.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tattoli I, et al. Amino acid starvation induced by invasive bacterial pathogens triggers an innate host defense program. Cell Host Microbe. 2012;11:563–575. doi: 10.1016/j.chom.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 28.Saitoh T, et al. Loss of the autophagy protein Atg16L1 enhances endotoxin-induced IL-1beta production. Nature. 2008;456:264–268. doi: 10.1038/nature07383. nature07383 [pii] This study is the first to demonstrate the immunosuppressive function of autophagy in limiting the inflammasome. [DOI] [PubMed] [Google Scholar]
- 29.Nakahira K, et al. Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat Immunol. 2011;12:222–230. doi: 10.1038/ni.1980. ni.1980 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhong Z, et al. NF-kappaB Restricts Inflammasome Activation via Elimination of Damaged Mitochondria. Cell. 2016;164:896–910. doi: 10.1016/j.cell.2015.12.057. This study shows that mitophagy inhibits inflammasome activation in the presence of LPS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dupont N, et al. Shigella phagocytic vacuolar membrane remnants participate in the cellular response to pathogen invasion and are regulated by autophagy. Cell Host Microbe. 2009;6:137–149. doi: 10.1016/j.chom.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 32.Meunier E, et al. Caspase-11 activation requires lysis of pathogen-containing vacuoles by IFN-induced GTPases. Nature. 2014;509:366–370. doi: 10.1038/nature13157. [DOI] [PubMed] [Google Scholar]
- 33.Kreibich S, et al. Autophagy Proteins Promote Repair of Endosomal Membranes Damaged by the Salmonella Type Three Secretion System 1. Cell Host Microbe. 2015;18:527–537. doi: 10.1016/j.chom.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 34.Suzuki T, et al. Differential regulation of caspase-1 activation, pyroptosis, and autophagy via Ipaf and ASC in Shigella-infected macrophages. PLoS Pathog. 2007;3:e111. doi: 10.1371/journal.ppat.0030111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Byrne BG, Dubuisson JF, Joshi AD, Persson JJ, Swanson MS. Inflammasome components coordinate autophagy and pyroptosis as macrophage responses to infection. mBio. 2013;4:e00620–00612. doi: 10.1128/mBio.00620-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shi CS, et al. Activation of autophagy by inflammatory signals limits IL-1beta production by targeting ubiquitinated inflammasomes for destruction. Nat Immunol. 2012;13:255–263. doi: 10.1038/ni.2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bodemann BO, et al. RalB and the exocyst mediate the cellular starvation response by direct activation of autophagosome assembly. Cell. 2011;144:253–267. doi: 10.1016/j.cell.2010.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ravindran R, et al. The amino acid sensor GCN2 controls gut inflammation by inhibiting inflammasome activation. Nature. 2016;531:523–527. doi: 10.1038/nature17186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wlodarska M, et al. NLRP6 inflammasome orchestrates the colonic host-microbial interface by regulating goblet cell mucus secretion. Cell. 2014;156:1045–1059. doi: 10.1016/j.cell.2014.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Travassos LH, et al. Nod1 and Nod2 direct autophagy by recruiting ATG16L1 to the plasma membrane at the site of bacterial entry. Nat Immunol. 2010;11:55–62. doi: 10.1038/ni.1823. ni.1823 [pii] [DOI] [PubMed] [Google Scholar]
- 41.Cooney R, et al. NOD2 stimulation induces autophagy in dendritic cells influencing bacterial handling and antigen presentation. Nat Med. 2010;16:90–97. doi: 10.1038/nm.2069. nm.2069 [pii] [DOI] [PubMed] [Google Scholar]
- 42.Homer CR, et al. A Dual Role for Receptor-interacting Protein Kinase 2 (RIP2) Kinase Activity in Nucleotide-binding Oligomerization Domain 2 (NOD2)-dependent Autophagy. The Journal of biological chemistry. 2012;287:25565–25576. doi: 10.1074/jbc.M111.326835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anand PK, et al. TLR2 and RIP2 pathways mediate autophagy of Listeria monocytogenes via extracellular signal-regulated kinase (ERK) activation. J Biol Chem. 2011;286:42981–42991. doi: 10.1074/jbc.M111.310599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Irving AT, et al. The immune receptor NOD1 and kinase RIP2 interact with bacterial peptidoglycan on early endosomes to promote autophagy and inflammatory signaling. Cell Host Microbe. 2014;15:623–635. doi: 10.1016/j.chom.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 45.Chauhan S, Mandell MA, Deretic V. IRGM governs the core autophagy machinery to conduct antimicrobial defense. Molecular cell. 2015;58:507–521. doi: 10.1016/j.molcel.2015.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Plantinga TS, et al. Crohn’s disease-associated ATG16L1 polymorphism modulates pro-inflammatory cytokine responses selectively upon activation of NOD2. Gut. 2011 doi: 10.1136/gut.2010.228908. gut.2010.228908 [pii] [DOI] [PubMed] [Google Scholar]
- 47.Buffen K, et al. Autophagy modulates Borrelia burgdorferi-induced production of interleukin-1beta (IL-1beta) J Biol Chem. 2013;288:8658–8666. doi: 10.1074/jbc.M112.412841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lassen KG, et al. Atg16L1 T300A variant decreases selective autophagy resulting in altered cytokine signaling and decreased antibacterial defense. Proc Natl Acad Sci U S A. 2014;111:7741–7746. doi: 10.1073/pnas.1407001111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murthy A, et al. A Crohn’s disease variant in Atg16l1 enhances its degradation by caspase 3. Nature. 2014 doi: 10.1038/nature13044. [DOI] [PubMed] [Google Scholar]
- 50.Lupfer C, et al. Receptor interacting protein kinase 2-mediated mitophagy regulates inflammasome activation during virus infection. Nat Immunol. 2013;14:480–488. doi: 10.1038/ni.2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wen Z, et al. Neutrophils counteract autophagy-mediated anti-inflammatory mechanisms in alveolar macrophage: role in posthemorrhagic shock acute lung inflammation. J Immunol. 2014;193:4623–4633. doi: 10.4049/jimmunol.1400899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chu H, et al. Gene-microbiota interactions contribute to the pathogenesis of inflammatory bowel disease. Science. 2016;352:1116–1120. doi: 10.1126/science.aad9948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xu Y, et al. Toll-like receptor 4 is a sensor for autophagy associated with innate immunity. Immunity. 2007;27:135–144. doi: 10.1016/j.immuni.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Delgado MA, Elmaoued RA, Davis AS, Kyei G, Deretic V. Toll-like receptors control autophagy. Embo J. 2008;27:1110–1121. doi: 10.1038/emboj.2008.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shi CS, Kehrl JH. TRAF6 and A20 regulate lysine 63-linked ubiquitination of Beclin-1 to control TLR4-induced autophagy. Sci Signal. 2010;3:ra42. doi: 10.1126/scisignal.2000751. 3/123/ra42 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meijer AH, van der Vaart M. DRAM1 promotes the targeting of mycobacteria to selective autophagy. Autophagy. 2014;10:2389–2391. doi: 10.4161/15548627.2014.984280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fujita K, Maeda D, Xiao Q, Srinivasula SM. Nrf2-mediated induction of p62 controls Toll-like receptor-4-driven aggresome-like induced structure formation and autophagic degradation. Proc Natl Acad Sci U S A. 2011;108:1427–1432. doi: 10.1073/pnas.1014156108. 1014156108 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wild P, et al. Phosphorylation of the autophagy receptor optineurin restricts Salmonella growth. Science. 2011;333:228–233. doi: 10.1126/science.1205405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moy RH, et al. Antiviral autophagy restrictsRift Valley fever virus infection and is conserved from flies to mammals. Immunity. 2014;40:51–65. doi: 10.1016/j.immuni.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Benjamin JL, Sumpter R, Jr, Levine B, Hooper LV. Intestinal Epithelial Autophagy Is Essential for Host Defense against Invasive Bacteria. Cell Host Microbe. 2013;13:723–734. doi: 10.1016/j.chom.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee HK, Lund JM, Ramanathan B, Mizushima N, Iwasaki A. Autophagy-dependent viral recognition by plasmacytoid dendritic cells. Science. 2007;315:1398–1401. doi: 10.1126/science.1136880. 1136880 [pii] [DOI] [PubMed] [Google Scholar]
- 62.Henault J, et al. Noncanonical autophagy is required for type I interferon secretion in response to DNA-immune complexes. Immunity. 2012;37:986–997. doi: 10.1016/j.immuni.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sanjuan MA, et al. Toll-like receptor signalling in macrophages links the autophagy pathway to phagocytosis. Nature. 2007;450:1253–1257. doi: 10.1038/nature06421. nature06421 [pii] [DOI] [PubMed] [Google Scholar]
- 64.Akoumianaki T, et al. Aspergillus Cell Wall Melanin Blocks LC3-Associated Phagocytosis to Promote Pathogenicity. Cell Host Microbe. 2016;19:79–90. doi: 10.1016/j.chom.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 65.Katsuragi Y, Ichimura Y, Komatsu M. p62/SQSTM1 functions as a signaling hub and an autophagy adaptor. FEBS J. 2015;282:4672–4678. doi: 10.1111/febs.13540. [DOI] [PubMed] [Google Scholar]
- 66.Lee HM, et al. Autophagy negatively regulates keratinocyte inflammatory responses via scaffolding protein p62/SQSTM1. J Immunol. 2011;186:1248–1258. doi: 10.4049/jimmunol.1001954. [DOI] [PubMed] [Google Scholar]
- 67.Kim JK, et al. MicroRNA-125a Inhibits Autophagy Activation and Antimicrobial Responses during Mycobacterial Infection. J Immunol. 2015;194:5355–5365. doi: 10.4049/jimmunol.1402557. [DOI] [PubMed] [Google Scholar]
- 68.Lei Y, et al. The mitochondrial proteins NLRX1 and TUFM form a complex that regulates type I interferon and autophagy. Immunity. 2012;36:933–946. doi: 10.1016/j.immuni.2012.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xia M, et al. Mitophagy enhances oncolytic measles virus replication by mitigating DDX58/RIG-I-like receptor signaling. J Virol. 2014;88:5152–5164. doi: 10.1128/JVI.03851-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhao Y, et al. COX5B regulates MAVS-mediated antiviral signaling through interaction with ATG5 and repressing ROS production. PLoS Pathog. 2012;8:e1003086. doi: 10.1371/journal.ppat.1003086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tal MC, et al. Absence of autophagy results in reactive oxygen species-dependent amplification of RLR signaling. Proc Natl Acad Sci U S A. 2009;106:2770–2775. doi: 10.1073/pnas.0807694106. 0807694106 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jounai N, et al. The Atg5 Atg12 conjugate associates with innate antiviral immune responses. Proc Natl Acad Sci U S A. 2007;104:14050–14055. doi: 10.1073/pnas.0704014104. 0704014104 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saitoh T, et al. Atg9a controls dsDNA-driven dynamic translocation of STING and the innate immune response. Proc Natl Acad Sci U S A. 2009;106:20842–20846. doi: 10.1073/pnas.0911267106. 0911267106 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Konno H, Konno K, Barber GN. Cyclic dinucleotides trigger ULK1 (ATG1) phosphorylation of STING to prevent sustained innate immune signaling. Cell. 2013;155:688–698. doi: 10.1016/j.cell.2013.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liang Q, et al. Crosstalk between the cGAS DNA sensor and Beclin-1 autophagy protein shapes innate antimicrobial immune responses. Cell Host Microbe. 2014;15:228–238. doi: 10.1016/j.chom.2014.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lan YY, Londono D, Bouley R, Rooney MS, Hacohen N. Dnase2a deficiency uncovers lysosomal clearance of damaged nuclear DNA via autophagy. Cell reports. 2014;9:180–192. doi: 10.1016/j.celrep.2014.08.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mathew R, et al. Functional role of autophagy-mediated proteome remodeling in cell survival signaling and innate immunity. Molecular cell. 2014;55:916–930. doi: 10.1016/j.molcel.2014.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Grimm WA, et al. The Thr300Ala variant in ATG16L1 is associated with improved survival in human colorectal cancer and enhanced production of type I interferon. Gut. 2015 doi: 10.1136/gutjnl-2014-308735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gutierrez MG, et al. Autophagy is a defense mechanism inhibiting BCG and Mycobacterium tuberculosis survival in infected macrophages. Cell. 2004;119:753–766. doi: 10.1016/j.cell.2004.11.038. S0092867404011067 [pii] [DOI] [PubMed] [Google Scholar]
- 80.Harris J, et al. T helper 2 cytokines inhibit autophagic control of intracellular Mycobacterium tuberculosis. Immunity. 2007;27:505–517. doi: 10.1016/j.immuni.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 81.Mostowy S, et al. p62 and NDP52 proteins target intracytosolic Shigella and Listeria to different autophagy pathways. J Biol Chem. 2011;286:26987–26995. doi: 10.1074/jbc.M111.223610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Matsuzawa T, et al. IFN-gamma elicits macrophage autophagy via the p38 MAPK signaling pathway. J Immunol. 2012;189:813–818. doi: 10.4049/jimmunol.1102041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chang YP, et al. Autophagy facilitates IFN-gamma-induced Jak2-STAT1 activation and cellular inflammation. J Biol Chem. 2010;285:28715–28722. doi: 10.1074/jbc.M110.133355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Boonhok R, et al. LAP-like process as an immune mechanism downstream of IFN-gamma in control of the human malaria Plasmodium vivax liver stage. Proc Natl Acad Sci U S A. 2016 doi: 10.1073/pnas.1525606113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shen S, et al. Cytoplasmic STAT3 represses autophagy by inhibiting PKR activity. Molecular cell. 2012;48:667–680. doi: 10.1016/j.molcel.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 86.Van Grol J, et al. HIV-1 inhibits autophagy in bystander macrophage/monocytic cells through Src-Akt and STAT3. PLoS One. 2010;5:e11733. doi: 10.1371/journal.pone.0011733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Terawaki S, et al. RUN and FYVE domain-containing protein 4 enhances autophagy and lysosome tethering in response to Interleukin-4. The Journal of cell biology. 2015;210:1133–1152. doi: 10.1083/jcb.201501059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dupont N, et al. Autophagy-based unconventional secretory pathway for extracellular delivery of IL-1beta. Embo J. 2011;30:4701–4711. doi: 10.1038/emboj.2011.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cullen SP, Kearney CJ, Clancy DM, Martin SJ. Diverse Activators of the NLRP3 Inflammasome Promote IL-1beta Secretion by Triggering Necrosis. Cell reports. 2015;11:1535–1548. doi: 10.1016/j.celrep.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 90.Zhang M, Kenny S, Ge L, Xu K, Schekman R. Translocation of interleukin-1beta into a vesicle intermediate in autophagy-mediated secretion. eLife. 2015;4 doi: 10.7554/eLife.11205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pilli M, et al. TBK-1 promotes autophagy-mediated antimicrobial defense by controlling autophagosome maturation. Immunity. 2012;37:223–234. doi: 10.1016/j.immuni.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Castillo EF, et al. Autophagy protects against active tuberculosis by suppressing bacterial burden and inflammation. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:E3168–3176. doi: 10.1073/pnas.1210500109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lee JP, et al. Loss of autophagy enhances MIF/macrophage migration inhibitory factor release by macrophages. Autophagy. 2016;12:907–916. doi: 10.1080/15548627.2016.1164358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Peral de Castro C, et al. Autophagy regulates IL-23 secretion and innate T cell responses through effects on IL-1 secretion. J Immunol. 2012;189:4144–4153. doi: 10.4049/jimmunol.1201946. [DOI] [PubMed] [Google Scholar]
- 95.Ding Y, et al. Autophagy regulates TGF-beta expression and suppresses kidney fibrosis induced by unilateral ureteral obstruction. J Am Soc Nephrol. 2014;25:2835–2846. doi: 10.1681/ASN.2013101068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Trinchieri G. Type I interferon: friend or foe? J Exp Med. 2010;207:2053–2063. doi: 10.1084/jem.20101664. jem.20101664 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.de Mello PA, et al. Adenosine uptake is the major effector of extracellular ATP toxicity in human cervical cancer cells. Mol Biol Cell. 2014;25:2905–2918. doi: 10.1091/mbc.E14-01-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Biswas D, et al. ATP-induced autophagy is associated with rapid killing of intracellular mycobacteria within human monocytes/macrophages. BMC immunology. 2008;9:35. doi: 10.1186/1471-2172-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Takenouchi T, et al. The activation of P2X7 receptor impairs lysosomal functions and stimulates the release of autophagolysosomes in microglial cells. J Immunol. 2009;182:2051–2062. doi: 10.4049/jimmunol.0802577. [DOI] [PubMed] [Google Scholar]
- 100.Bian S, et al. P2X7 integrates PI3K/AKT and AMPK-PRAS40-mTOR signaling pathways to mediate tumor cell death. PLoS One. 2013;8:e60184. doi: 10.1371/journal.pone.0060184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Martins I, et al. Molecular mechanisms of ATP secretion during immunogenic cell death. Cell death and differentiation. 2014;21:79–91. doi: 10.1038/cdd.2013.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Michaud M, et al. Autophagy-dependent anticancer immune responses induced by chemotherapeutic agents in mice. Science. 2011;334:1573–1577. doi: 10.1126/science.1208347. This study demonstrates that autophagy promotes anticancer immunity by mediating the release of ATP. [DOI] [PubMed] [Google Scholar]
- 103.Tang D, et al. Endogenous HMGB1 regulates autophagy. The Journal of cell biology. 2010;190:881–892. doi: 10.1083/jcb.200911078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kang R, et al. The receptor for advanced glycation end products (RAGE) sustains autophagy and limits apoptosis, promoting pancreatic tumor cell survival. Cell death and differentiation. 2010;17:666–676. doi: 10.1038/cdd.2009.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tang D, et al. High-mobility group box 1 is essential for mitochondrial quality control. Cell metabolism. 2011;13:701–711. doi: 10.1016/j.cmet.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhu X, et al. Cytosolic HMGB1 controls the cellular autophagy/apoptosis checkpoint during inflammation. J Clin Invest. 2015;125:1098–1110. doi: 10.1172/JCI76344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yanai H, et al. Conditional ablation of HMGB1 in mice reveals its protective function against endotoxemia and bacterial infection. Proc Natl Acad Sci U S A. 2013;110:20699–20704. doi: 10.1073/pnas.1320808110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pua HH, Dzhagalov I, Chuck M, Mizushima N, He YW. A critical role for the autophagy gene Atg5 in T cell survival and proliferation. J Exp Med. 2007;204:25–31. doi: 10.1084/jem.20061303. jem.20061303 [pii] This study is the first to demonstrate that deficiency in an autophagy protein leads to defects in lymphocyte survival and proliferation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stephenson LM, et al. Identification of Atg5-dependent transcriptional changes and increases in mitochondrial mass in Atg5-deficient T lymphocytes. Autophagy. 2009;5:625–635. doi: 10.4161/auto.5.5.8133. 8133 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jia W, He YW. Temporal regulation of intracellular organelle homeostasis in T lymphocytes by autophagy. J Immunol. 2011;186:5313–5322. doi: 10.4049/jimmunol.1002404. [DOI] [PubMed] [Google Scholar]
- 111.Kovacs JR, et al. Autophagy promotes T-cell survival through degradation of proteins of the cell death machinery. Cell death and differentiation. 2012;19:144–152. doi: 10.1038/cdd.2011.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Pei B, et al. Invariant NKT cells require autophagy to coordinate proliferation and survival signals during differentiation. J Immunol. 2015;194:5872–5884. doi: 10.4049/jimmunol.1402154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Willinger T, Flavell RA. Canonical autophagy dependent on the class III phosphoinositide-3 kinase Vps34 is required for naive T-cell homeostasis. Proc Natl Acad Sci U S A. 2012;109:8670–8675. doi: 10.1073/pnas.1205305109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Matsuzawa Y, et al. TNFAIP3 promotes survival of CD4 T cells by restricting MTOR and promoting autophagy. Autophagy. 2015;11:1052–1062. doi: 10.1080/15548627.2015.1055439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Xu X, et al. Autophagy is essential for effector CD8(+) T cell survival and memory formation. Nat Immunol. 2014;15:1152–1161. doi: 10.1038/ni.3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.O’Sullivan TE, Johnson LR, Kang HH, Sun JC. BNIP3- and BNIP3L-Mediated Mitophagy Promotes the Generation of Natural Killer Cell Memory. Immunity. 2015;43:331–342. doi: 10.1016/j.immuni.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Puleston DJ, et al. Autophagy is a critical regulator of memory CD8(+) T cell formation. eLife. 2014;3 doi: 10.7554/eLife.03706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Schlie K, et al. Survival of effector CD8+ T cells during influenza infection is dependent on autophagy. J Immunol. 2015;194:4277–4286. doi: 10.4049/jimmunol.1402571. [DOI] [PubMed] [Google Scholar]
- 119.Henson SM, et al. p38 signaling inhibits mTORC1-independent autophagy in senescent human CD8(+) T cells. J Clin Invest. 2014;124:4004–4016. doi: 10.1172/JCI75051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hubbard VM, et al. Macroautophagy regulates energy metabolism during effector T cell activation. J Immunol. 2010;185:7349–7357. doi: 10.4049/jimmunol.1000576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Miller BC, et al. The autophagy gene ATG5 plays an essential role in B lymphocyte development. Autophagy. 2008;4:309–314. doi: 10.4161/auto.5474. 5474 [pii] [DOI] [PubMed] [Google Scholar]
- 122.Conway KL, et al. ATG5 regulates plasma cell differentiation. Autophagy. 2013;9:528–537. doi: 10.4161/auto.23484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pengo N, et al. Plasma cells require autophagy for sustainable immunoglobulin production. Nat Immunol. 2013;14:298–305. doi: 10.1038/ni.2524. [DOI] [PubMed] [Google Scholar]
- 124.Paul S, Kashyap AK, Jia W, He YW, Schaefer BC. Selective autophagy of the adaptor protein Bcl10 modulates T cell receptor activation of NF-kappaB. Immunity. 2012;36:947–958. doi: 10.1016/j.immuni.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wei J, et al. Autophagy enforces functional integrity of regulatory T cells by coupling environmental cues and metabolic homeostasis. Nat Immunol. 2016 doi: 10.1038/ni.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kabat AM, et al. The autophagy gene Atg16l1 differentially regulates Treg and TH2 cells to control intestinal inflammation. eLife. 2016;5 doi: 10.7554/eLife.12444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Dengjel J, et al. Autophagy promotes MHC class II presentation of peptides from intracellular source proteins. Proc Natl Acad Sci U S A. 2005;102:7922–7927. doi: 10.1073/pnas.0501190102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nedjic J, Aichinger M, Emmerich J, Mizushima N, Klein L. Autophagy in thymic epithelium shapes the T-cell repertoire and is essential for tolerance. Nature. 2008;455:396–400. doi: 10.1038/nature07208. [DOI] [PubMed] [Google Scholar]
- 129.Ireland JM, Unanue ER. Autophagy in antigen-presenting cells results in presentation of citrullinated peptides to CD4 T cells. J Exp Med. 2011;208:2625–2632. doi: 10.1084/jem.20110640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Paludan C, et al. Endogenous MHC class II processing of a viral nuclear antigen after autophagy. Science. 2005;307:593–596. doi: 10.1126/science.1104904. [DOI] [PubMed] [Google Scholar]
- 131.Lee Y, et al. p62 Plays a Specific Role in Interferon-gamma-Induced Presentation of a Toxoplasma Vacuolar Antigen. Cell reports. 2015;13:223–233. doi: 10.1016/j.celrep.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 132.Sakowski ET, et al. Ubiquilin 1 Promotes IFN-gamma-Induced Xenophagy of Mycobacterium tuberculosis. PLoS Pathog. 2015;11:e1005076. doi: 10.1371/journal.ppat.1005076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Romao S, et al. Autophagy proteins stabilize pathogen-containing phagosomes for prolonged MHC II antigen processing. The Journal of cell biology. 2013;203:757–766. doi: 10.1083/jcb.201308173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Martinez J, et al. Microtubule-associated protein 1 light chain 3 alpha (LC3)-associated phagocytosis is required for the efficient clearance of dead cells. Proc Natl Acad Sci U S A. 2011;108:17396–17401. doi: 10.1073/pnas.1113421108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Brooks CR, et al. KIM-1-/TIM-1-mediated phagocytosis links ATG5-/ULK1-dependent clearance of apoptotic cells to antigen presentation. Embo J. 2015;34:2441–2464. doi: 10.15252/embj.201489838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lee HK, et al. In vivo requirement for Atg5 in antigen presentation by dendritic cells. Immunity. 2010;32:227–239. doi: 10.1016/j.immuni.2009.12.006. S1074-7613(10)00045-2 [pii] This study demonstrates that the autophagy pathway in dendritic cells is critical for antigen presentation during herpesvirus infection in vivo. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gobeil PA, Leib DA. Herpes simplex virus gamma34.5 interferes with autophagosome maturation and antigen presentation in dendritic cells. mBio. 2012;3:e00267–00212. doi: 10.1128/mBio.00267-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ravindran R, et al. Vaccine activation of the nutrient sensor GCN2 in dendritic cells enhances antigen presentation. Science. 2014;343:313–317. doi: 10.1126/science.1246829. This study shows that autophagy induced by the nutrient sensor GCN2 promotes cross-presentation of viral antigens. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Jostins L, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–124. doi: 10.1038/nature11582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Cadwell K, et al. A key role for autophagy and the autophagy gene Atg16l1 in mouse and human intestinal Paneth cells. Nature. 2008;456:259–263. doi: 10.1038/nature07416. nature07416 [pii] This study identifies a role for the autophagy gene ATG16L1 in supporting intestinal Paneth cells. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Patel KK, et al. Autophagy proteins control goblet cell function by potentiating reactive oxygen species production. Embo J. 2013;32:3130–3144. doi: 10.1038/emboj.2013.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Adolph TE, et al. Paneth cells as a site of origin for intestinal inflammation. Nature. 2013 doi: 10.1038/nature12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Conway KL, et al. Atg16l1 is required for autophagy in intestinal epithelial cells and protection of mice from Salmonella infection. Gastroenterology. 2013;145:1347–1357. doi: 10.1053/j.gastro.2013.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hubbard-Lucey VM, et al. Autophagy gene atg16l1 prevents lethal T cell alloreactivity mediated by dendritic cells. Immunity. 2014;41:579–591. doi: 10.1016/j.immuni.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Martin LJ, et al. Functional variant in the autophagy-related 5 gene promotor is associated with childhood asthma. PLoS One. 2012;7:e33454. doi: 10.1371/journal.pone.0033454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhou XJ, et al. Genetic association of PRDM1-ATG5 intergenic region and autophagy with systemic lupus erythematosus in a Chinese population. Annals of the rheumatic diseases. 2011;70:1330–1337. doi: 10.1136/ard.2010.140111. [DOI] [PubMed] [Google Scholar]
- 147.Dickinson JD, et al. IL13 activates autophagy to regulate secretion in airway epithelial cells. Autophagy. 2015;0 doi: 10.1080/15548627.2015.1056967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Clarke AJ, et al. Autophagy is activated in systemic lupus erythematosus and required for plasmablast development. Annals of the rheumatic diseases. 2015;74:912–920. doi: 10.1136/annrheumdis-2013-204343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Alessandri C, et al. T lymphocytes from patients with systemic lupus erythematosus are resistant to induction of autophagy. FASEB J. 2012;26:4722–4732. doi: 10.1096/fj.12-206060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Weindel CG, et al. B cell autophagy mediates TLR7-dependent autoimmunity and inflammation. Autophagy. 2015;11:1010–1024. doi: 10.1080/15548627.2015.1052206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Martinez J, et al. Noncanonical autophagy inhibits the autoinflammatory, lupus-like response to dying cells. Nature. 2016;533:115–119. doi: 10.1038/nature17950. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 152.Huang J, et al. Activation of antibacterial autophagy by NADPH oxidases. Proc Natl Acad Sci U S A. 2009;106:6226–6231. doi: 10.1073/pnas.0811045106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.De Luca A, et al. CD4(+) T cell vaccination overcomes defective cross-presentation of fungal antigens in a mouse model of chronic granulomatous disease. J Clin Invest. 2012;122:1816–1831. doi: 10.1172/JCI60862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.de Luca A, et al. IL-1 receptor blockade restores autophagy and reduces inflammation in chronic granulomatous disease in mice and in humans. Proc Natl Acad Sci U S A. 2014;111:3526–3531. doi: 10.1073/pnas.1322831111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Schwerd T, et al. Impaired antibacterial autophagy links granulomatous intestinal inflammation in Niemann-Pick disease type C1 and XIAP deficiency with NOD2 variants in Crohn’s disease. Gut. 2016 doi: 10.1136/gutjnl-2015-310382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Luciani A, et al. Defective CFTR induces aggresome formation and lung inflammation in cystic fibrosis through ROS-mediated autophagy inhibition. Nat Cell Biol. 2010;12:863–875. doi: 10.1038/ncb2090. [DOI] [PubMed] [Google Scholar]
- 157.Abdulrahman BA, et al. Autophagy stimulation by rapamycin suppresses lung inflammation and infection by Burkholderia cenocepacia in a model of cystic fibrosis. Autophagy. 2011;7:1359–1370. doi: 10.4161/auto.7.11.17660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Renna M, et al. Azithromycin blocks autophagy and may predispose cystic fibrosis patients to mycobacterial infection. J Clin Invest. 2011;121:3554–3563. doi: 10.1172/JCI46095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Pyo JO, et al. Overexpression of Atg5 in mice activates autophagy and extends lifespan. Nature communications. 2013;4:2300. doi: 10.1038/ncomms3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Starr T, et al. Selective subversion of autophagy complexes facilitates completion of the Brucella intracellular cycle. Cell host & microbe. 2012;11:33–45. doi: 10.1016/j.chom.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kimmey JM, et al. Unique role for ATG5 in neutrophil-mediated immunopathology during M tuberculosis infection. Nature. 2015;528:565–569. doi: 10.1038/nature16451. This study identifies a non-autophagy function of ATG5 in defense against Mycobacterium tuberculosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Reggiori F, et al. Coronaviruses Hijack the LC3-I-positive EDEMosomes, ER-derived vesicles exporting short-lived ERAD regulators, for replication. Cell Host Microbe. 2010;7:500–508. doi: 10.1016/j.chom.2010.05.013. S1931-3128(10)00176-9 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kageyama S, et al. The LC3 recruitment mechanism is separate from Atg9L1-dependent membrane formation in the autophagic response against Salmonella. Mol Biol Cell. 2011;22:2290–2300. doi: 10.1091/mbc.E10-11-0893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Sorbara MT, et al. The protein ATG16L1 suppresses inflammatory cytokines induced by the intracellular sensors Nod1 and Nod2 in an autophagy-independent manner. Immunity. 2013;39:858–873. doi: 10.1016/j.immuni.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 165.Liu E, Van Grol J, Subauste CS. Atg5 but not Atg7 in dendritic cells enhances IL-2 and IFN-gamma production by Toxoplasma gondii-reactive CD4+ T cells. Microbes Infect. 2015;17:275–284. doi: 10.1016/j.micinf.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Consortium TWTCC. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007;447:661–678. doi: 10.1038/nature05911. nature05911 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Cullup T, et al. Recessive mutations in EPG5 cause Vici syndrome, a multisystem disorder with defective autophagy. Nat Genet. 2013;45:83–87. doi: 10.1038/ng.2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Hakonarson H, et al. A genome-wide association study identifies KIAA0350 as a type 1 diabetes gene. Nature. 2007;448:591–594. doi: 10.1038/nature06010. [DOI] [PubMed] [Google Scholar]
- 169.Soleimanpour SA, et al. The diabetes susceptibility gene Clec16a regulates mitophagy. Cell. 2014;157:1577–1590. doi: 10.1016/j.cell.2014.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Schuster C, et al. The Autoimmunity-Associated Gene CLEC16A Modulates Thymic Epithelial Cell Autophagy and Alters T Cell Selection. Immunity. 2015;42:942–952. doi: 10.1016/j.immuni.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Smyth DJ, et al. PTPN22 Trp620 explains the association of chromosome 1p13 with type 1 diabetes and shows a statistical interaction with HLA class II genotypes. Diabetes. 2008;57:1730–1737. doi: 10.2337/db07-1131. [DOI] [PubMed] [Google Scholar]
- 172.Martinez A, et al. Chromosomal region 16p13: further evidence of increased predisposition to immune diseases. Annals of the rheumatic diseases. 2010;69:309–311. doi: 10.1136/ard.2008.098376. [DOI] [PubMed] [Google Scholar]
- 173.Scharl M, et al. Crohn’s disease-associated polymorphism within the PTPN2 gene affects muramyl-dipeptide-induced cytokine secretion and autophagy. Inflamm Bowel Dis. 2012;18:900–912. doi: 10.1002/ibd.21913. [DOI] [PubMed] [Google Scholar]
- 174.Yang Z, Fujii H, Mohan SV, Goronzy JJ, Weyand CM. Phosphofructokinase deficiency impairs ATP generation, autophagy, and redox balance in rheumatoid arthritis T cells. J Exp Med. 2013;210:2119–2134. doi: 10.1084/jem.20130252. [DOI] [PMC free article] [PubMed] [Google Scholar]