Abstract
Importance
There is a significant need to find biomarkers of response to radiation and cetuximab in locally advanced head and neck squamous cell carcinoma (HNSCC), as well as biomarkers predicting altered immunity, thereby enabling personalized treatment.
Objective
To evaluate if the KRAS-variant, a germ-line mutation in a microRNA-binding site in KRAS, is a predictive biomarker of cetuximab response and altered immunity in the setting of radiation and cisplatin treatment. To evaluate the interaction of the KRAS-variant with p16 status and blood-based TGF-β1.
Design
Advanced HNSCC patients from NRG Oncology RTOG 0522, a Phase III trial of cisplatin plus radiation+/−cetuximab, were included in this study, and patients with available samples were genotyped for the KRAS-variant.
Methods
Genomic DNA was tested for the KRAS-variant in a CLIA-certified laboratory. Correlation between the KRAS-variant, p16 positivity, outcome, and TGF-β1 levels was evaluated. Hazard ratios (HR) were estimated by Cox model.
Main Outcomes and Measures
The correlation of KRAS-variant status with cetuximab response and outcome, p16 status, and plasma TGF-β1 levels was tested.
Results
Of 891 RTOG 0522 patients eligible for protocol analyses, 413 had biological samples for KRAS-variant testing, and 376 had plasma for TGF-β1 measurement. Seventy patients (16.9%) had the KRAS-variant. Overall, for KRAS-variant patients, cetuximab improved both progression-free survival (PFS) for the first year (HR 0.31, 95%CI 0.10–0.94, p=0.04) and overall survival (OS) in years 1–2 (HR 0.19, 95%CI 0.04–0.86, p=0.03). There was a significant interaction of the KRAS-variant with p16 status for PFS in patients treated without cetuximab (p=0.04). In p16 positive patients, KRAS-variant patients treated without cetuximab had worse PFS than non-variant patients (HR 2.59, 95%CI 0.91–7.33, p=0.07). There was a significant three-way interaction between the KRAS-variant, p16 status and treatment for OS (p=0.02). KRAS-variant patients had significantly elevated TGF-β1 plasma levels (p=0.03), and a trend for worse treatment-related toxicity.
Conclusion and Relevance
KRAS-variant HNSCC patients significantly benefit from the addition of cetuximab to radiation and cisplatin, and there is a significant interaction between the KRAS-variant and p16 status. Elevated TGF-β1in KRAS-variant patients suggests that cetuximab may help these patients by overcoming TGF-beta induced suppression of antitumor immunity.
Introduction
The current standard of care for the non-surgical management of locally advanced head and neck squamous cell carcinoma (HNSCC) is concurrent platinum-based chemotherapy and radiotherapy. Unfortunately, however, this approach results in an ~ 50% treatment failure rate in unselected patients.1,2 Cetuximab is an anti-EGFR monoclonal antibody that was previously shown to be beneficial for such patients, improving survival when given with definitive radiation, or with cisplatin+5-fluorouracil in recurrent/metastatic HNSCC.3,4 However, a randomized phase III clinical trial (NRG Oncology RTOG 0522) failed to show any improvement in survival with the addition of 8 weeks of cetuximab to cisplatin and radiotherapy.2 To date, beyond EGFR surface expression,5 no predictive biomarker of cetuximab response has been identified for these patients.
Recently, human papillomavirus (HPV), reliably measured by p16 expression, has been established as a prognostic biomarker in HNSCC, with p16-positive patients having a favorable outcome compared to p16-negative patients.1,6,7 One reason for the better prognosis in p16-positive disease is thought to be due to immune mediated mechanisms, as both cisplatin and radiation expose p16-associated antigens, which are immunogenic,8 enabling host-mediated immune tumor killing. Consistent with prior reports, p16-positive patients in RTOG 0522 had improved outcome compared to p16-negative patients.2 However, there was no benefit of cetuximab treatment when p16 status was considered in RTOG 0522. One hypothesis put forward is lower EGFR tumor cell staining in p16-positive patients in 0522 compared to p16-negative tumors (22% vs. 30%).2
Beyond inhibition of EGFR signaling however, cetuximab has also been shown to work through immune-mediated mechanisms, by enhancing adaptive immunity via antibody dependent cell-mediated cytotoxicity (ADCC),9,10 and by better enabling cytotoxic T-lymphocyte (CTL) cross-priming by dendritic cells.11 Recently, cetuximab combined with chemotherapy was further confirmed to trigger immunogenic cell death in mouse models through increased phagocytosis by dendritic cells.12 These immune-based mechanisms of cetuximab efficacy have not yet been studied in the setting of radiation, although radiation also enables antitumor immunity, with the release of danger signals, and dendritic and T cell activation.13–15 Recently, a biomarker of altered immune function, FCGR2A, a polymorphism in an Fcy receptor, was shown to impact response rate to cetuximab for patients with KRAS mutant tumors, 16 indicating that inherited polymorphisms can impact cetuximab response.
In the colon cancer field, response to cetuximab is associated with an inherited biomarker disrupting KRAS, referred to as the KRAS-variant.17 The KRAS-variant is the first microRNA (miRNA) binding site mutation discovered in cancer, and is a functional germ-line mutation in the 3′ untranslated (3′UTR) region of KRAS. While the KRAS-variant is rare in tumors with acquired KRAS mutations, 18 it leads to gene expression patterns consistent with KRAS-addiction across tumor types. 19,20 The KRAS-variant is associated with increased cancer risk,18–20 and the development of multiple cancers,21,22 and more recently has been found to be a predictive biomarker of response to cancer treatment irrespective of tumor type or tumor acquired mutations.23–28 In HNSCC the KRAS-variant is found in 15–32% of patients,29,30 and is therefore highly relevant. HNSCC patients with the KRAS-variant have previously been shown to have a poor response to platinum therapy, similar to findings for KRAS-variant patients with other cancer types.23,29–31
While the mechanisms leading to the predictive power of the KRAS-variant in treatment response have not been fully elucidated, one could hypothesize that the KRAS-variant identifies patients with altered immunity, based on the fact that KRAS signaling and let-7 expression, both universally abnormal in KRAS-variant associated tumors,29,32,33 are both critical in systemic immunity.34–35 In addition, mutant KRAS has been shown to directly inhibit anti-tumor immunity through induction of TGF-β1 secretion, which is known to lead to conversion of conventional T cells into Tregs or Th17 cells.36, 37,38 In the setting of radiation, TGF-β1 is proposed to be a master regulator of treatment response, with high levels preventing radiation induced anti-tumor immunity.39 Interestingly, in cells with high TGF-β1, cetuximab has been found to restore the killing activity of patient NK cells against primary HNSCC cells, via enhanced ADCC, in a dose-dependent manner.40 Cetuximab response has also been shown to overcome TGF-β1 expressing Tregs, known to inhibit NK cell killing 41, providing a potential mechanism of action. The role of altered immunity and TGF-β1 levels as potential mechanisms of cetuximab response in KRAS-variant patients has not been previously evaluated.
Thus, here we sought to test the predictive role of the KRAS-variant for HNSCC patient outcome in the setting of radiation, cisplatin and cetuximab, considering p16 status. We further evaluated immune parameters in KRAS-variant patients through plasma TGF-β1 levels. We show for the first time that the KRAS-variant is a predictive biomarker of cetuximab response for HNSCC patients, and interacts significantly with p16. Furthermore, we find that KRAS-variant patients have significantly elevated plasma TGF-β1 levels, consistent with baseline immune suppression.
Patients and Methods
Protocol and Patients
NRG Oncology RTOG 0522 was a phase III trial testing the addition of cetuximab to radiation therapy with concurrent cisplatin for patients with advanced HNSCC.2 The study was approved by all IRBs where patients were enrolled, and oral informed consent was obtained from all study participants. Race and sex was collected and is reported in Supplemental Table 1. Eligible patients had pathologically proven squamous cell carcinoma of the oropharynx, hypopharynx, or larynx, with selected stage III or IV disease (T2 N2-3 M0 or T3-4 any N M0), Zubrod performance status 0–1, age ≥ 18 years, and adequate bone marrow, hepatic, and renal function. HPV status was evaluated by p16 expression as previously described.1,2 See attached protocol (Supplemental Document 1). Nine-hundred and forty patients were enrolled into NRG Oncology RTOG 0522, of whom 891 (94.8%) were eligible for protocol analyses. 413 of 891 patients had biological samples available for KRAS-variant analysis (46.4%, see Supplemental Figure 1 for a CONSORT Flow Diagram). Patients not tested for the KRAS-variant had significantly lower age (p=0.02) than patients tested for the KRAS-variant, but the difference in medians was only 2 years (56 vs. 58) (Supplemental Table 1). Progression-free survival (PFS) and overall survival (OS) were similar for the patients tested and not tested for the KRAS-variant [PFS hazard ratio 0.92 (95%CI 0.76 to 1.13), p=0.44; OS hazard ratio 0.99 (95%CI 0.78 to 1.25), p=0.93]. At the time of analysis, median follow-up for surviving patients was 4.8 years (range 0.2 to 6.9). Of the 413 study participants tested for the KRAS-variant, 5 (1.2%) were homozygous (GG) and 65 (15.7%) were heterozygous (TG), resulting in an overall prevalence of 16.9%. The prevalence of the KRAS-variant was not significantly different in p16-negative (17.4%) versus p16-positive (16.0%) patients, in agreement with prior studies.42
Of the 70 patients with the KRAS-variant, the cetuximab treated subset had fewer patients of Caucasian race (87.5% vs. 100%, p=0.04). Within the non-variant cohort, the cetuximab treated subset had significantly lower age than the subset not receiving cetuximab, but the difference in medians was only 2 years (59 vs. 57, p=0.05)(Supplemental Table 2).
KRAS-variant testing
Genomic DNA from peripheral blood mononuclear cells or whole blood was isolated as previously described43, and 100ng was analyzed in a CLIA-certified laboratory for the KRAS-variant (Mira Dx). Patients that were homozygous (GG) were grouped with those that were heterozygous (TG) for these analyses.
Statistical methods
Local-regional failure (LRF), distant metastasis (DM), PFS, and OS were as defined in the NRG Oncology RTOG 0522 protocol. LRF and DM rates were estimated by the cumulative incidence method.44 PFS and OS rates were estimated by the Kaplan-Meier method.45 Hazard ratios were estimated by the Cox model.34 Adverse events were graded by Common Terminology Criteria for Adverse Events (CTCAE) version 3.0. Odds ratios were estimated by logistic regression. Patient characteristics were compared by Fisher’s exact test (categorical variables) or Wilcoxon rank-sum test (ordinal or continuous variables). All analyses were performed using SAS version 9.4.
Plasma TGF-β1 levels
Plasma levels of TGF-β1 from 376 patients enrolled on 0522 were measured using multiplex bead assays utilizing reagents from Millipore and the Luminex 100 system as previously described. 46 The assay was run using manufacturer controls to ensure precision. The correlation between KRAS-variant status and plasma TGF-β1 levels was evaluated by Wilcoxon rank-sum test.
Results
The KRAS-variant Predicts Response to Cetuximab
We investigated the association of the KRAS-variant with cetuximab response in HNSCC and found a significant, positive effect of 8 weeks of cetuximab treatment for all KRAS-variant patients. KRAS-variant patients had significantly improved PFS in the first year (hazard ratio 0.31, 95%CI 0.10 to 0.94, p=0.04), but not thereafter (hazard ratio 1.76, 95%CI 0.62 to 4.95, p=0.28)(Figure 1A). The cetuximab treatment effect significantly varied over time (p=0.02 for interaction between treatment and PFS time [>1 year]). In the non-variant group there was no impact of cetuximab on PFS with a treatment effect hazard ratio [cetuximab/no cetuximab] of 1.00 (95%CI 0.72 to 1.38, p=0.98). In multivariate analysis, the interaction between treatment, time (>1 year), and KRAS group remained significant (p=0.02), indicating that there is an interaction between treatment and time in the KRAS-variant group (Table 1).
Figure 1. Progression-free survival (PFS) and overall survival (OS) for HNSCC patients by KRAS-variant status and assigned treatment.
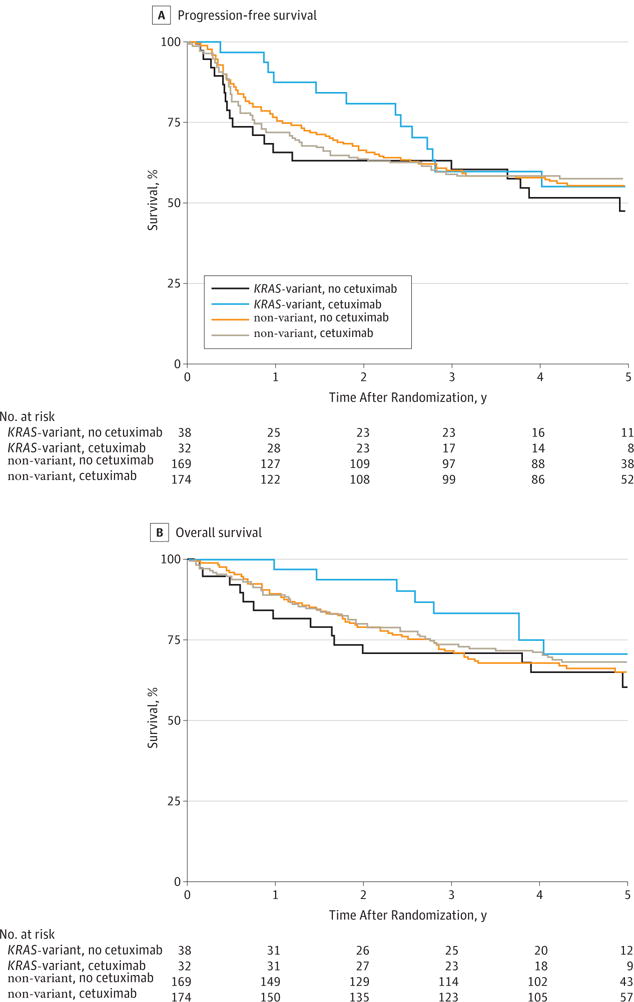
A. PFS In total, 179 of 413 (43.3%) patients experienced a PFS failure: 19 of 38 (50.0%) in the non-cetuximab treated KRAS-variant group, 13 of 32 (40.6%) in the cetuximab treated KRAS-variant group, 74 of 169 (43.8%) in the non-cetuximab treated non-variant group, and 73 of 174 (42.0%) in the cetuximab treated non-variant group. B. OS. In total, 134 of 413 (32.4%) patients have died: 14 of 38 (36.8%) in the non-cetuximab treated KRAS-variant group, 8 of 32 (25.0%) in the cetuximab treated KRAS-variant group, 58 of 169 (34.3%) in the non-variant non-cetuximab treated group, and 54 of 174 (31.0%) in the non- variant cetuximab treated group.
Table 1.
Multivariate analysis of PFS and OS (n=413)
| PFS (179 events) |
OS (134 events) |
|||
|---|---|---|---|---|
| HR (95%CI) | p-value | HR (95%CI) | p-value | |
| Treatment X time X KRAS | – | 0.02 | – | 0.04 |
| Treatment X time, if KRAS-variant | – | 0.10 | – | 0.05 |
| Treatment X time, if non-variant | – | 0.21 | – | 0.80 |
| Treatment X KRAS, if early [1] | – | 0.07 | – | 0.13 |
| Treatment X KRAS, if late | – | 0.36 | – | 0.29 |
| Early treatment effect [1], if KRAS-variant | 0.42 (0.14–1.26) | 0.12 | 0.27 (0.06–1.21) | 0.09 |
| Late treatment effect, if KRAS-variant | 1.22 (0.53–2.80) | 0.64 | 1.47 (0.53–4.03) | 0.46 |
| Early treatment effect [1], if non-variant | 1.20 (0.80–1.80) | 0.39 | 0.89 (0.56–1.41) | 0.62 |
| Late treatment effect, if non-variant | 0.79 (0.47–1.33) | 0.38 | 0.81 (0.45–1.48) | 0.49 |
PFS, progression-free survival; OS, overall survival; HR, hazard ratio; CI, confidence interval.
First year for PFS, first 2 years for OS.
Hazard ratios estimated from Cox models including treatment (cetuximab vs. no cetuximab), treatment X PFS/OS time interaction, KRAS (variant vs. non-variant), treatment X KRAS interaction, treatment X PFS/OS time X KRAS interaction, age, Zubrod performance status (1 vs. 0), primary site (oropharynx vs. others), T stage (T4 vs. T2-3), and N stage (N2b-3 vs. N0-2a).
The pattern of failure in a multivariate analysis suggested that distant metastases (DM) rather than local regional failure (LRF) may be a more likely contributor to the difference in PFS for KRAS-variant patients: in the KRAS-variant group, the treatment effect for DM is 0.45 (95%CI 0.12 to 1.70), and for LRF is 0.84 (95%CI 0.29 to 2.42)(Supplemental Figure 2 and 3). In the non-variant group, the treatment effects for DM and LRF are 0.90 (95%CI 0.48 to 1.70) and 1.24 (95%CI 0.80 to 1.92), respectively.
KRAS-variant patients also had significantly improved OS in the first 2 years (hazard ratio 0.19, 95%CI 0.04 to 0.86, p=0.03), but not thereafter (hazard ratio 2.34, 95%CI 0.58 to 9.41, p=0.23)(Figure 1B). Again, the cetuximab treatment effect significantly varied over time (p=0.02 for interaction between treatment effect and survival time [>2 years]). In the non-variant group, there was no impact of cetuximab treatment on overall survival (treatment effect hazard ratio [cetuximab/no cetuximab] 0.90 (95%CI 0.62 to 1.30, p=0.56). In a multivariate analysis the interaction between treatment, time (>2 years), and KRAS group remained significant (p=0.04)(Table 1), indicating that there is an interaction between treatment and time in the KRAS-variant group. The treatment effect in the first 2 years for the KRAS-variant group is 0.27 (95%CI 0.06–1.21, p=0.09) and 1.47 (95%CI 0.53–4.03, p=0.46) thereafter (p=0.05 for the interaction).
The KRAS-variant interacts with p16 status for PFS
Because p16, a key cell cycle inhibitor, is a known prognostic biomarker in HNSCC, we evaluated outcome in KRAS-variant patients considering p16 status, without or with cetuximab treatment. For PFS, in patients treated without cetuximab, the two-way interaction between KRAS and p16 was significant (p=0.04, Table 2). KRAS-variant/p16-positive patients treated without cetuximab had worse PFS than non-variant/p16 positive patients, of borderline significance (HR 2.59, 95%CI 0.91–7.33, p=0.07, Figure 2A, left panel). However, in cetuximab treated patients, there was no longer a difference in outcome between KRAS-variant/p16-positive patients and non-variant/p16-positive patients (HR 0.89, 95%CI 0.34–2.35, p= 0.82)(Figure 2A, right).
Table 2.
Multivariate analysis of PFS and OS including p16 (n=271)
| PFS (116 events) |
OS (85 events) |
|||
|---|---|---|---|---|
| HR (95%CI) | p-value | HR (95%CI) | p-value | |
| Treatment X KRAS X p16 | – | 0.20 | – | 0.02 |
| Treatment X KRAS, if p16-positive | – | 0.14 | – | 0.05 |
| Treatment X p16, if KRAS-variant | – | 0.51 | – | 0.15 |
| Treatment X p16, if KRAS-non-variant | – | 0.12 | – | 0.01 |
| KRAS X p16, if cetuximab | – | 0.84 | – | 0.11 |
| KRAS X p16, if no cetuximab | – | 0.04 | – | 0.10 |
| Treatment effect, if KRAS-variant and p16-positive | 0.60 (0.17−2.10) | 0.42 | 0.21 (0.02−2.04) | 0.18 |
| Treatment effect, if KRAS-non-variant and p16-positive | 1.74 (0.88−3.42) | 0.11 | 2.36 (0.98−5.67) | 0.05 |
| KRAS effect, if no cetuximab and p16-positive | 2.59 (0.91−7.33) | 0.07 | 2.48 (0.64−9.65) | 0.19 |
| KRAS effect, if cetuximab and p16-positive | 0.89 (0.34−2.35) | 0.82 | 0.22 (0.03−1.66) | 0.14 |
| p16 effect, if cetuximab and KRAS-variant | 0.73 (0.20−2.73) | 0.64 | 0.12 (0.01−1.11) | 0.06 |
| p16 effect, if cetuximab and KRAS-non-variant | 0.63 (0.36−1.11) | 0.11 | 0.80 (0.41−1.54) | 0.50 |
| p16 effect, if no cetuximab and KRAS-variant | 1.34 (0.40−4.44) | 0.64 | 0.86 (0.20−3.64) | 0.84 |
| p16 effect, if no cetuximab and KRAS-non-variant | 0.32 (0.17−0.61) | <0.001 | 0.21 (0.09−0.49) | <0.001 |
PFS, progression-free survival; OS, overall survival; HR, hazard ratio; CI, confidence interval.
Hazard ratios estimated from Cox models including treatment (cetuximab vs. no cetuximab), KRAS (variant vs. non-variant), p16 (positive vs. negative), treatment X KRAS interaction, treatment X p16 interaction, KRAS X p16 interaction, treatment X KRAS X p16 interaction, Zubrod performance status (1 vs. 0), T stage (T4 vs. T2-3), and N stage (N2b-3 vs. N0-2a).
Figure 2. Progression Free Survival (PFS) and Overall Survival (OS) by KRAS Genotype and p16 Status for Patients treated without (left) or with (right) Cetuximab Treatment.
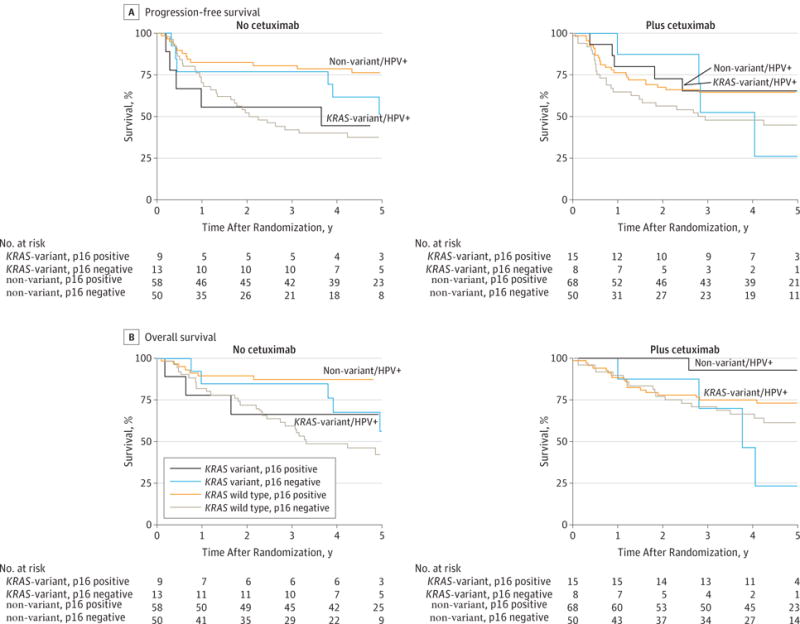
Solid lines, KRAS-variant, dashed lines, non-variant. Black lines p16-positive, red lines p16-negative. A. PFS. There is a significant two way interaction between KRAS and p16 in patients treated without cetuximab (p=0.04). B. OS. There is a significant three-way interaction between cetuximab treatment, KRAS-variant status, and p16 status (p=0.02).
The KRAS-variant interacts with p16 and Treatment for Overall Survival
For OS, there is a significant three-way interaction between cetuximab treatment, KRAS-variant status, and p16 status (p=0.02). There is also a significant two-way interaction between treatment and KRAS for p16-positive patients (p=0.05), and between treatment and p16 status for KRAS-non-variant patients (p=0.01)(Table 2). In patients treated without cetuximab, KRAS-variant/p16-positive patients had a non-significant trend for worse OS than non-variant/p16-positive patients (HR 2.48, 95%CI 0.64–9.65, p=0.19), which appeared to be non-significantly reversed with cetuximab treatment (HR 0.22, 95%CI 0.03–1.66, p=0.14, Figure 2B). In p16-positive patients, the cetuximab treatment effect is 0.21 (95%CI 0.02–2.04, p=0.18) for KRAS-variant patients compared to 2.36 (95%CI 0.98–5.67, p=0.05) for non-variant patients.
KRAS-variant patients’ immunological landscape and toxicity
Based on the differential effect of cetuximab, especially in p16-positive patients, we investigated immune parameters in KRAS-variant patients. We measured plasma TGF-β1 (generally a negative regulator of local immune response) levels in patients from 0522, and found that KRAS-variant patients had significantly higher plasma TGF-β1 levels compared to non-variant patients (Median 23,376 pg/ml versus 18,477 pg/ml, respectively; Wilcoxon rank-sum test, p=0.03; Table 3). TGF-β1 levels were also compared by p16 and KRAS-variant status, but the differences were not statistically significant in this smaller cohort (Supplemental Table 3).
Table 3.
Plasma TGFB1 levels in patients with HNSCC grouped by KRAS-variant status. Wilcoxon rank-sum test p=0.03
| n | Min | Q1 | Median | Q3 | Max | |
|---|---|---|---|---|---|---|
| KRAS-non-variant | 311 | 2261.42 | 8837.00 | 18476.52 | 32379.43 | 123264.70 |
| KRAS-variant | 65 | 5034.35 | 12574.03 | 23376.49 | 44809.10 | 109759.72 |
Based on the known role of TGF-β1 in normal tissue radiation toxicity, we evaluated toxicity in KRAS-variant versus non-variant patients. KRAS-variant patients appeared to have elevated levels of Grade 3–4 mucositis even without cetuximab treatment (47.4% without cetuximab vs 50.0% with, OR 1.11 [95%CI 0.43 to 2.85], p=0.83). In contrast, in non-variant patients the addition of cetuximab significantly increased Grade 3–4 mucositis (37.9% vs 50.6%, OR 1.68 [95%CI 1.09 to 2.58], p=0.02) (Supplemental Table 4). However, a test of the interaction between KRAS-variant status and cetuximab treatment was not significant (p=0.43). KRAS-variant patients also appeared to have elevated levels of Grade 3–4 skin reaction inside the portal even without cetuximab treatment (18.4% without cetuximab vs 15.6% with, OR 0.82 [95%CI 0.23 to 2.89], p=0.76). In contrast, in non-variant patients the addition of cetuximab significantly increased Grade 3–4 skin reactions inside the portal (11.2% vs 21.8%, OR 2.21 [95%CI 1.21 to 4.01], p=0.05), but again a test of interaction was not significant (p=0.16)(Supplemental Table 5). As expected, both non-variant and KRAS-variant patients developed increased skin reaction outside the portal with cetuximab (non-variant OR 50.15, p<0.001; KRAS-variant OR 8.54, p=0.05)(Supplemental Table 6).
To further evaluate if KRAS-variant status and TGF-β1 levels together predict toxicity, we evaluated KRAS-variant patients with known TGF-β1 levels (n=65), and looked at Grade 3–4 mucositis or in-field skin toxicity. We only included patients not treated with cetuximab, as cetuximab is known to be a radiosensitizer. We found that KRAS-variant patients with TGF-β1 levels > versus ≤ the median treated without cetuximab appeared to have an increase in risk of Grade 3–4 toxicity (OR 2.31, 95%CI 0.57–9.41). However, the interaction between KRAS and TGF-β1 was not significant (p=0.4). In contrast, non-variant patients with TGF-β1 levels > versus ≤ the median treated without cetuximab showed little correlation of TGF-β1 levels on toxicity (OR 1.19, 95%CI 0.62–2.25).
Discussion
Advanced HNSCC patients with the KRAS-variant significantly benefit from the addition of cetuximab to radiation and cisplatin therapy, resulting in improved PFS and OS. We found that this benefit fades over time, possibly due to the short course of cetuximab delivered in this study. We further show that there is a significant interaction between the KRAS-variant, p16 status, and cetuximab, with KRAS-variant/p16 patients doing poorly compared to non-variant/p16 patients, a deficit that seems to be overcome by cetuximab. Furthermore, we show that KRAS-variant patients have significantly elevated TGF-β1 expression, suggesting that they may have a baseline immune-deficient and/or anti-tumor immune defective state, which cetuximab in combination with radiation may be helping to overcome.
For HNSCC, while p16 has been shown to be an important prognostic biomarker, it appears that knowledge of both p16 status and KRAS-variant status may be important to determine optimal personalized treatment for these patients. It is particularly notable that KRAS-variant/p16-positive patients had the worst outcomes of all subgroups of HNSCC patients in our study, which appeared to be improved with a short course of cetuximab treatment given with radiation and cisplatin. These patients should perhaps be considered a different entity from non-variant/p16-positive patients, who had excellent outcomes with radiation and cisplatin alone. Work is ongoing to further validate these observations.
Our finding that HNSCC patients with the KRAS-variant may have an altered immune state compared to non-variant patients is novel, but perhaps not surprising, considering that the KRAS-variant is germ-line and, thus, present in all cells, including immune cells. This inherited mutation is known to lead to globally altered gene expression profiles consistent with KRAS-addiction,32,33 as well as altered expression of the let-7 miRNA,43 both of which are known to have significant effects on the immune system.34,35 In addition, our findings here of elevated TGF-β1 in these cancer patients, which has long been known to be involved in immunity37 and immune suppression,47 further supports our hypothesis that KRAS-variant patients are immune suppressed. Baseline differences in immunity could also help explain the increased cancer risk found in KRAS-variant patients. Interestingly, cetuximab has been shown to overcome the impaired NKG2D-dependent functionality of activated natural killer (NK) cells 40,41 in the presence of TGF-β1,48,49 potentially explaining the global benefit of cetuximab treatment seen in KRAS-variant patients. Whether the altered TGF-β1 we see in these patients represents baseline perturbations in homeostasis, or altered responses to tumor challenge, and is a finding that will be found for all KRAS-variant cancer patients, remains unclear, and are the subject of important ongoing investigations.
Although the sample size was small in this study, and a larger study would strengthen the results, our current findings are consistent with prior work with patients with recurrent/metastatic HNSCC treated with cisplatin +/− cetuximab, showing that the addition of cetuximab improved median survival to 3.9 months; however, the interaction with p16 status could not be evaluated previously because of the small sample size.42 Our findings are also consistent with those found in KRAS-variant colon cancer patients, where cetuximab monotherapy is clearly beneficial.16,17 What this study has additionally found is the potential importance of cetuximab delivered in conjunction with radiation therapy for KRAS-variant patients, to seemingly enable them to mount appropriate immunologic responses following tumor-targeted irradiation, diminishing metastatic failures. We also find that patients with the KRAS-variant may have baseline normal tissue radiation sensitivity, possibly through their elevated TGF-β1 levels. Although cetuximab is a known radiosensitizer, there did not appear to be worsened radiosensitivity with the addition of cetuximab for KRAS-variant patients. Studies are ongoing to better understand the mechanisms of radiosensitivity in these patients, to further personalize their treatment.
While a germ-line biomarker that can identify individuals with altered immunity that can be used to direct the best therapeutic combinations is a bold, new concept, the KRAS-variant is unfolding as a true candidate. Based on our findings in this study, defining how anti-cancer agents affecting the tumor-host-immune relationship differently impact KRAS-variant patients is a critical, and pressing need, as this knowledge could help in personalizing developing immune based cancer therapies for all cancer patients.
Supplementary Material
Acknowledgments
We would like to thank James W. Sayre from UCLA for his reading and thoughts on the manuscript and work. Data analysis was completed by NRG statisticians Jonathan Harris and Qiang Zhang. Jonathan Harris had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Research Support:
This trial was conducted by the NRG Oncology Radiation Therapy Oncology Group (NRG/RTOG). The research was supported by grants U10 CA21661 (RTOG-Ops-Stat), U10CA180868 (NRG Oncology Operations) and U10CA180822 (NRG Oncology SDMC), U10CA37422 (CCOP), UG1CA 189867 (NCORP) from the National Cancer Institute (NCI) and Eli Lilly and Aventis Pharmaceuticals. And, in part by SPORE in Head and Neck Cancer at the Johns Hopkins University from the National Institute of Dental & Craniofacial Research (P50DE019032). Dr. Weidhaas was supported by a grant from the NIH (CA157749). Dr. Ferris is supported by R01 DE019727, P50 CA097190, and CA206517. MiraDx genotyped blinded samples for the KRAS-variant, at no cost. This manuscript’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. None of the funding sources were involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Authors Declaration of Potential Conflicts of Interest:
Dr. Weidhaas is a co-inventor of the discovery of the KRAS-variant, which has been patented by Yale University, and licensed to a company that she co-founded, MiraDx. Dr. Chung has served on the Scientific Advisory Board for BMS and Lilly Oncology. Dr. Ferris has served on advisory boards for Amgen, AZ-Medimmune, BMS, Lilly, and Merck. All remaining authors declare no conflicts of interest.
References
- 1.Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ang KK, Zhang Q, Rosenthal DI, et al. Randomized phase III trial of concurrent accelerated radiation plus cisplatin with or without cetuximab for stage III to IV head and neck carcinoma: RTOG 0522. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(27):2940–2950. doi: 10.1200/JCO.2013.53.5633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonner JA, Harari PM, Giralt J, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2006;354(6):567–578. doi: 10.1056/NEJMoa053422. [DOI] [PubMed] [Google Scholar]
- 4.Vermorken JB, Mesia R, Rivera F, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 2008;359(11):1116–1127. doi: 10.1056/NEJMoa0802656. [DOI] [PubMed] [Google Scholar]
- 5.Boeckx C, Baay M, Wouters A, et al. Anti-epidermal growth factor receptor therapy in head ane neck squamous cell carcinoma: focus on potential molecular mechanisms of drug resistance. Oncologist. 2013;18:850–864. doi: 10.1634/theoncologist.2013-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fakhry C, Westra W, Li S, et al. Improved survival of patients with human papillomavirus-positive head ane neck squamous cell carcinoma in a prospective clinical trial. Journal of the National Cancer Institute. 2008;100(4):261–269. doi: 10.1093/jnci/djn011. [DOI] [PubMed] [Google Scholar]
- 7.Chung C, Zhang Q, Kong C, et al. p16 protein expression and human papillomavirus status as a prognostic biomarker of nonoropharygeal head ane neck squamous cell carcinoma. J Clin Oncol. 2014;32:3930–3938. doi: 10.1200/JCO.2013.54.5228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spanos W, Nowicki P, Lee D, et al. Immune Response During Therapy with Cisplatin or Radiation for Human Papillomavirus-Related Head and Neck Cancer. Arch Otolaryngol Head Neck Surg. 2009;135:1137–1146. doi: 10.1001/archoto.2009.159. [DOI] [PubMed] [Google Scholar]
- 9.Srivastava R, Lee S, Andrade Filho P, et al. Cetuximab-activated natural killer and dendritic cells collaborate to trigger tumor antigen-specific T-cell immunity in head and neck cancer patients. Clin Cancer Res. 2013;19:1858–1872. doi: 10.1158/1078-0432.CCR-12-2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stephenson R, Lim C, Mattews M, Dietsch G, Hershberg R, Ferris R. TLR8 stimulation enhances cetuximab-mediated natural killer cell lysis of head and neck cancer cells and dendritic cell cross priming of EGFR-specific CD8+ T cells. Cancer Immunol Immunother. 2013;62:1347–1357. doi: 10.1007/s00262-013-1437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang X, Zhang X, Mortenson E, Radkevich-Brown O, Wang Y, Fu Y-X. Cetuximab-mediated Tumor Regression Depends on Innate and Adaptive Immune Responses. Molecular Therapy. 2012;21:91–100. doi: 10.1038/mt.2012.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pozzi C, Cuomo A, Spadoni I, et al. The EGFR-specific antibody cetuximab combined with chemotherapy triggers immonogenic cell death. Nature Medicine. 2016 doi: 10.1038/nm.4078. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Battacharyya T, Purushothaman K, SPuthiyottil S, Bhattacherjee A, Muttah G. Immunological interaction in radiotherapy - opening a new window of opportunity. Annals of Translational Medicine. 2016;4 doi: 10.3978/j.issn.2305-5839.2015.10.44. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derer A, Frey B, Fietkau R, Gaipl U. Immune-modulating properties of ionizing radiation: rationale for the treatment of cancer by combination radiotherapy and immune checkpoint inhibitors. Cancer Immunol Immunother. 2015 doi: 10.1007/s00262-015-1771-8. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frey B, Rubner Y, Kulzer L, et al. Antitumor immune responses induced by ionizing irradiaiton and further immune stimulation. Cancer Immunol Immunother. 2014;63:29–36. doi: 10.1007/s00262-013-1474-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kjersem J, Skovlund E, Ikdahl T, et al. FCGR2A and FCGR3A polymorphisms and clinical outcome in metastatic colorectal cancer patients treated with first-line 5′fluorouracil/folinic acid and oxaliplatin +/− cetuximab. BMC Cancer. 2014;14:340. doi: 10.1186/1471-2407-14-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saridaki Z, Weidhaas J, Lenz H-J, et al. A let-7 microRNA-binding site polymophism is KRAS predicts improved outcome in metastatic colorectal cancer (mCRC) patients treated with salvage cetuximab/panitumumab monotherapy. Clin Cancer Res. 2014;20(17):4499–4510. doi: 10.1158/1078-0432.CCR-14-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chin L, Ratner E, Leng S, et al. A SNP in a let-7 microRNA complementary site in the KRAS 3′ untranslated region increases non-small cell lung cancer risk. Cancer Res. 2008;68:8535–8540. doi: 10.1158/0008-5472.CAN-08-2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paranjape T, Heneghan H, Lindner R, et al. A 3′-untranslated region KRAS variant and triple-negative breast cancer: a case-control and genetic analysis. Lancet Oncol. 2011;12(4):377–386. doi: 10.1016/S1470-2045(11)70044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ratner E, Lu L, Boeke M, et al. A KRAS-variant in Ovarian Cancer Acts as a Genetic Marker of Cancer Risk. Cancer Research. 2010;15:6509–6515. doi: 10.1158/0008-5472.CAN-10-0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pilarski R, Patel D, Weitzel J, et al. A KRAS-variant is associated with risk of developing double primary breast and ovarian cancer. PLos ONE. 2012;7(5):e37891. doi: 10.1371/journal.pone.0037891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McVeigh T, Jung S-Y, Kerin M, et al. Estrogen Withdrawal, increased Breast Cancer Risk and the KRAS-variant. Cell Cycle. 2015 doi: 10.1080/15384101.2015.1041694. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ratner E, Keane F, Lindner R, et al. A KRAS-variant is a Biomarker of Poor Outcome, Platinum Chemotherapy Resistance and a Potential Target for Therapy in Ovarian Cancer. Oncogene. 2011 Dec 5; doi: 10.1038/onc.2011.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weidhaas J, Kim E, Herbst R, et al. The KRAS-variant and treatment response in BATTLE-1. J Clin Oncol. 2014;32(52) suppl; abstr 8135. [Google Scholar]
- 25.Graziano F, Canestrari E, Loupakis F, et al. Genetic modulation of the Let-7 microRNA binding to KRAS 3′-untranslated region and survival of metastatic colorectal cancer patients treated with salvage cetuximab-irinotecan. Pharmacogenomics J. 2010;10(5):458–464. doi: 10.1038/tpj.2010.9. [DOI] [PubMed] [Google Scholar]
- 26.Zhang W, Winder T, Ning Y, et al. A let-7 microRNA-binding site polymorphism in 3′-untranslated region of KRAS gene predicts response in wild-type KRAS patients with metastatic colorectal cancer treated with cetuximab monotherapy. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO. 2011;22(1):104–109. doi: 10.1093/annonc/mdq315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ganzinelli M, Rulli E, Caiola E, et al. Role of KRAS-LCS6 polymorphism in advanced NSCLC patients treated with erlotinib or docetaxel in second line treatment (TAILOR) Sci Rep. 2015;5:16331. doi: 10.1038/srep16331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sclafani F, Chau I, Cunningham D, et al. Prognostic role of the LCS6 KRAS variant in locally advanced rectal cancer: results of the EXPERT-C trial. Annals of Oncology. 2015;26:9. doi: 10.1093/annonc/mdv285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christensen B, Moyer B, Avissar M, et al. A let-7 microRNA binding site polymorphism in the KRAS 3′UTR is associatied with reduced survival in oral cancers. Carcinogenesis. 2009;30(6):1003–1007. doi: 10.1093/carcin/bgp099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chung CH, Lee JW, Slebos RJ, et al. A 3′-UTR KRAS-variant is associated with cisplatin resistance in patients with recurrent and/or metastatic head and neck squamous cell carcinoma. Ann Oncol. 2014;25(11):2230–2236. doi: 10.1093/annonc/mdu367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Ruyck K, Duprez F, Ferdinande L, et al. A let-7 microRNA polymorphism in the KRAS 3′UTR is prognostic in oropharyngeal cancer. Cancer Epidemiol. 2014;38:591–598. doi: 10.1016/j.canep.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 32.Paranjape T, Heneghan H, Lindner R, et al. A 3′-untranslated region KRAS variant and triple-negative breast cancer: a case-control and genetic analysis. Lancet Oncology. 2011;12(4):377–386. doi: 10.1016/S1470-2045(11)70044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ratner E, Keane F, Lindner R, et al. A KRAS variant is a biomarker of poor outcome, platinum chemotherapy resistance and a potential target for therapy in ovarian cancer. Oncogene. 2012;31(42):4559–4566. doi: 10.1038/onc.2011.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smakman N, Veenendaal L, van Diest P, et al. Duel effect of KRAS(K12) knockdown on tumorigenesis: increased immune-mediated tumor clearance and abrogation of tumor malignancy. Oncogene. 2005;24:8338–8342. doi: 10.1038/sj.onc.1208995. [DOI] [PubMed] [Google Scholar]
- 35.Sathe A, Ayyar K, Reddy K. MicroRNA let-7 in the spotlight: Role in innate immunity. Inflammation & Cell Signaling. 2014;e109:1–8. [Google Scholar]
- 36.Zdanov S, Mandeapathil M, Abu Eid R, et al. Mutant KRAS Conversion of Conventional T Cells into Regulatory T Cells. Cancer Immunol Res. 2016;4:354–365. doi: 10.1158/2326-6066.CIR-15-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li M, Wan Y, Sanjabi S, Robertson A, Flavell R. Transforing growth factor-beta regulation of immune responses. Annu Rev Immunol. 2006;24:99–146. doi: 10.1146/annurev.immunol.24.021605.090737. [DOI] [PubMed] [Google Scholar]
- 38.Gutcher I, MK D, Ma Q, Rudensky A, Flavell R, Li M. Autocrine Transforming Growth Factor-B1 Promotes in vivo Th17 Cell Differentiation. Immunity. 2011;34:396–408. doi: 10.1016/j.immuni.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vanpouille-Box C, Diamond J, Pilones K, et al. TGFB Is a Master Regulator of Radiation Therapy-Induced Antitumor Immunity. Cancer Res. 2015;75:2232–2242. doi: 10.1158/0008-5472.CAN-14-3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kloss S, Chambron N, Gardlowski T, et al. Cetuximab Reconstitutes Pro-Inflammatory Cytokine Secretions and Tumor-Infiltrating Capabilities of sMICA-Inhibited NK Cells in HNSCC Tumor Spheroids. Front Immunol. 2015;6:543. doi: 10.3389/fimmu.2015.00543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jie H, Schuler P, Lee S, et al. CTLA-4+ Regulatory T Cells Increased in Cetuximab-Treated Head and Neck Cancer Patients SUppress NK Cell Cytotoxicity and Correlate with Poor Prognosis. Cancer Res. 2015;75:2200–2210. doi: 10.1158/0008-5472.CAN-14-2788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chung CH, Lee JW, Slebos RJ, et al. A 3′UTR KRAS variant is associated with cisplatin resistance in patients with recurrent and/or metastatic head and neck squamous cell carcinoma. Ann Oncol. 2014 doi: 10.1093/annonc/mdu367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chin L, Ratner E, Leng S, et al. A SNP in a let-7 microRNA complementary site in the KRAS 3′UTR Increases Non-Small Cell Cancer Risk. Cancer Research. 2008;68:8535–8540. doi: 10.1158/0008-5472.CAN-08-2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kalbfleisch J, Prentice R. The Statistical Analysis of Failure Time Data. New York: Wiley; 1980. [Google Scholar]
- 45.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Amer Stat Assoc. 1958;53:457–481. [Google Scholar]
- 46.Byers L, Holsinger F, Kies M, et al. Serum signature of hypoxia-regulated factors is associated with progression after induction therapy in head and neck squamous cell cancer. Molecular cancer therapeutics. 2010;9:1755–1763. doi: 10.1158/1535-7163.MCT-09-1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yoshimura A, Muto G. TGF-B function in immune suppression. Curr Top Microbiol Immunol. 2011;350:127–147. doi: 10.1007/82_2010_87. [DOI] [PubMed] [Google Scholar]
- 48.Guo S, Du Y, Liu X. Platelet-derived TGF-B1 mediates the down-modulation of NKG2D expression and may be responsible for impaired natural killer (NK) cytotoxicity in women with endometriosis. Hum Reprod. 2016 doi: 10.1093/humrep/dew057. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 49.Klob S, Chambron N, Gardlowski T, et al. Increased sMICA and TGFB1 levels in HNSCC patients impair NKG2D-dependent functionality of activated NK cells. Oncoimmunology. 2015;4(11):e1055993. doi: 10.1080/2162402X.2015.1055993. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


