Introduction
Fear and anxiety have been implicated in many aspects of pain, including experimentally-induced pain intensity (George, Dannecker, & Robinson, 2006; Parr, Borsa, Fillingim, Tillman, Tillman, Gregory, & George, 2012), pain during dental care (van Wijk & Hoogstraten, 2009), chronic pain behavior (McCracken, Gross, Aikens, & Carnkike Jr., 1996; Vlaeyen, de Johng, Geilen, Heuts, & van Breuklen, 2001; Turk, Robinson, & Burwinkle, 2004), and pain-related disability (Crombez, Vlaeyen, Heuts, & Lysens, 1999; Buer & Linton, 2002; Lee, Chiu, & Lam, 2007). As fear and anxiety, along with depression, are integral to understanding pain, valid and time-efficient assessments of such phenomena are needed. Currently available instruments are useful, but due to mounting pressures in healthcare to improve efficiency and see more patients in increasingly shorter periods of time (Okie, 2012; Bodenheimer & Smith, 2013), briefer assessments are needed.
One such widely used and studied fear of pain instrument is the Fear of Pain Questionnaire-III (FPQ-III; McNeil & Rainwater, 1998). Although a few studies have identified limitations (e.g., Asmundson, Bovell, Carleton, & McWilliams, 2007), the original FPQ-III factor structure and items have continued to be widely used and validated (e.g., Hursey & Jacks, 1992; Osman, Breitenstein, Barrios, Gutierrez, & Kipper, 2002; Roelofs, Peters, Deutz, Spijker, & Vlaeen, 2005). In addition, the FPQ-III has been translated and used in other languages such as French and Dutch (Albaret, Sastre, Cottencin, & Mullet, 2004; van Wijk & Hoogstraten, 2006).
In addition to the FPQ-III, there are several other published instruments which assess fear and anxiety associated with pain, each with a different focus. Regardless of the scale (or subscale) name, all of them assess both fear and anxiety, as disentangling those constructs for measurement is extraordinarily difficult. The Pain Anxiety Symptoms Scale (PASS; McCracken, Zayfert, & Gross, 1992) is a 40-item measure that assesses pain-related fear and anxiety; it is used in this study and so is more fully described under Methods. The Fear Avoidance Beliefs Questionnaire (FABQ) is a 16-item measure that assesses beliefs about how work and physical activity affect pain, and is particularly well suited for assessing degree of work-related disability in chronic pain patients. Finally, the Tampa Kinesiophobia Scale (TSK) is a 17-item measure that assesses pain-related fear of re-injury, which also is available in a shortened version of 11 items.
The aim of this study was to develop and establish a shortened version of the FPQ-III that could reduce time and staff demands in clinical and research settings, reduce respondent fatigue, and possibly be used as a screening instrument. The Fear of Pain Questionnaire-9 (FPQ-9) was designed to mirror its parent version (i.e., to use existing items and to maintain its three-factor structure). The purpose of this study was to develop and test a short (i.e., nine items) assessment instrument that paralleled the original FPQ-III (McNeil & Rainwater, 1998). This paper describes the process of testing the FPQ-9 as a brief, reliable, and valid assessment of fear and anxiety associated with pain, for clinical and research purposes.
Data and Methods
Instruments
Fear of Pain Questionnaire-III (FPQ-III)
The FPQ-III is a 30-item self-report questionnaire composed of three subscales: Fear of Severe Pain, Fear of Minor Pain, and Fear of Medical/Dental Pain (McNeil & Rainwater, 1998). Using a 5-point Likert-type scale, higher scores indicated more fear. The scale has high test-retest reliability (r = .92) and high internal consistency (α = .74), as do each of the subscales (McNeil & Rainwater, 1998). Other researchers have confirmed the original three-factor structure and high internal consistency of the FPQ-III (Osman, Breitenstein, Barrios, Gutierrez, & Kopper, 2002; Roelofs, Peters, Deutz, Spijker, & Vlaeen, 2005). The FPQ-III has been used to help identify patients with pain-related fear and anxiety that is high enough to negatively impact their experience of medical and dental procedures and their overall quality of life (Sperry-Clark, McNeil, & Ciano-Federoff, 1999; McNeil, Au, Zvolensky, McKee, Klineberg, & Ho, 2001; LeMay, Wilson, Buenger, Jarvis, Fitzgibbon, Bhimji, & Dobkin, 2011). The FPQ-III also has been used in basic research on the effects of fear on acute pain (Carter, McNeil, Vowles, Sorrell, Turk, Ries, & Hopko, 2002; Hirsh, George, Bialosky, & Robinson, 2008). Asmundson, Bovell, Carleton, and McWilliams (2008) developed a different revised and shortened form of the original FPQ-III with the purpose to evaluate alternative factorial models; however, their final questionnaire still had 23 items, only seven fewer than the original scale. Parr and colleagues (2012) used the present 9-item shortened version of the FPQ-III, in its unpublished format and with permission from the test developers (McNeil & Rainwater, 1998), to determine the relation between fear of pain and pain intensity. The FPQ-9 demonstrated high internal consistency (ICC = .83–.87, compared with .94–.95 for the 30-item version), and was highly correlated with the original FPQ-III (r = .94–.97), as well as participant report of pain intensity (r = .29), severity of disability (r = .16), scores on the Pain Catastrophizing Scale (r = .35), and scores on the Tampa Kinesiophobia Scale (r = .34). The Parr study, however, did not address other psychometric properties of the FPQ-9, utilized only total score with no attention paid to subscales and the factor structure of the instrument, and did not include a clinical sample; thus, the present study aimed to present the FPQ-9 more comprehensively and with richer psychometric analyses.
Pain Anxiety Symptoms Scale (PASS)
The PASS (McCracken et al., 1992) is a 40-item self-report measure that assesses pain-related fear and anxiety, and consists of four subscales: Cognitive Anxiety, Fear, Escape/Avoidance, and Physiological Anxiety. Using a 5-point Likert-type scale, higher scores are indicative of more anxiety and fear. McCracken and Dhingra (2002) developed a shortened PASS, but still consisting of 20 items; it has been criticized for having wordy items and “uncertain” (p. 46) psychometric properties (Grimmer-Somers, Vipond, Kumar, & Hall, 2009).
Dental Fear Survey (DFS)
The DFS (Kleinknect, Klepac, & Alexander, 1973) is a 20-item self-report measure that assess dental care-related anxiety and fear on a continuum (McNeil & Randall, 2014). With a 5-point Likert-type scale, higher scores reflect greater fear and anxiety. The DFS consists of three factorially-derived subscales: Behavioral Avoidance, Physiological Responses, and Fear of Specific Stimuli (McGlynn, McNeil, Gallagher, & Vrana, 1987). There has been extensive psychometric testing of the DFS, confirming its reliability, validity, and utility (e.g., Heaton, Carlson, Smith, Baer, & de Leeuw , 2007; McNeil & Randall, 2014).
Participants
Patients with chronic pain
FPQ-III data previously were collected (Sperry-Clark et al., 1999) on 275 outpatients (112 males and 163 females; M age = 45.6 years, SD = 12.0) with chronic pain at the West Virginia Pain Treatment Center in Morgantown, WV, and so served as part of an archival dataset. (This sample was collected to match the undergraduate group, detailed subsequently, in terms of total number and gender distribution.) These data, along with a second, new sample of 100 outpatients with chronic pain seeking outpatient treatment (43 males, 50 females, 7 unknown gender) with complete data from the aforementioned facility, were utilized in this study. Newly acquired participants were between the ages of 18 and 65 with a mean age of 48.5 (SD = 13.7). Institutional Review Board (IRB) approval was secured for data collection; all participants provided written and oral informed consent.
To collect data from a new sample of participants with chronic pain, individuals were approached in the waiting room of the West Virginia Pain Treatment Center. These 100 new participants were randomly divided into two groups. Group 1 (n = 55) provided demographic information and completed the existing FPQ-III directly before the appointment. Immediately following the appointment, these participants in Group 1 (25 males, 25 females, and 5 unknown gender) completed the new FPQ-9. Group 2 (n = 45), which consisted of 18 males, 25 females, and 2 participants of unknown gender, followed the same procedure except with reversal of presentation of the FPQ-III and the FPQ-9. Along with the FPQ-9 and demographic questionnaire, each chronic pain outpatient in the new sample also completed an omnibus fear item (i.e., #20) from the Dental Fear Survey (DFS; Kleinknecht, Klepac, & Alexander, 1973): “All things considered, how fearful are you of having dental work done?”.
Students
Archival FPQ-III data from 275 undergraduates (112 males and 163 females; M age = 19.7 years, SD = 3.2) from Oklahoma State University were used in this study (McNeil & Rainwater, 1998). (This sample was matched with the 275 chronic pain patients in terms of total number and gender distribution.) In addition, a new sample of 190 college students (70 males and 120 females) with a mean age of 20.1 (SD = 3.5) were obtained from the West Virginia University Department of Psychology. As for data collection with the chronic pain patient samples, IRB approval was obtained and all participants provided written and oral informed consent.
Data collection with the new sample of West Virginia University undergraduates took place over the course of two sessions at the conclusion of an academic class period, in classrooms that seated approximately 60 students. In total, there were 190 volunteer undergraduate students (70 males and 120 females); they received extra credit in their introductory psychology course for their participation. Undergraduate participants completed a demographic questionnaire, and then were randomly assigned to either Group 1 (n = 97) or Group 2 (n = 93). Order of measures were counterbalanced such that during the first data collection session, Group 1 completed the FPQ-III, and Group 2 was given the FPQ-9, the PASS (McCracken et al., 1992), and the entire 20-item DFS (Kleinknecht et al., 1973; McGlynn, 1998). One week later, these same students returned and completed the other tests; Group 1 (38 males and 59 females) received the FPQ-9, PASS, and the DFS, while Group 2 (32 males and 61 females) was given the existing FPQ-III.
Analytic approach
Item selection
Literature on scale development suggests that any single factor or subscale include at least three items to avoid them being poorly-defined (Brown, 2015). Thus, in order to maintain the original FPQ-III three-factor structure, and to equate the number of items across each of the three factors, a nine-item scale was the goal. Quantitative information was used to determine which items to include in the brief form as outlined in the following sections, along with theoretically-based judgments to mimic broad representation of the constructs.
Item-total correlations
Data from all 30 items of the FPQ-III available from the 550 respondents in the archival dataset (275 chronic pain outpatients and 275 undergraduates) were subjected to item-total correlation analysis. Separate item-total correlations calculated for the pain patients and the undergraduates were essentially the same, so only combined data are reported. Items first were considered based upon their correlation value (see Table 1). After considering the individual items’ correlation value, three items were selected from each of the original subscales (i.e., Fear of Severe Pain, Fear of Minor Pain, and Fear of Medical/Dental Pain) that most comprehensively and broadly represented the factors in the parent scale, from a theoretical perspective.
Table 1.
Item-Total Correlations for the Subscales of the FPQ-III
| Fear of Medical/Dental Pain | ||
|
| ||
| FPQ-III Item # and Item: | r | |
| I FEAR THE PAIN ASSOCIATED WITH: | ||
| 8. | Having a blood sample drawn with a hypodermic needle. | .63 |
| 11. | Receiving an injection in your arm. | .62 |
| 14. | Receiving an injection in you hip/buttocks. | .68 |
| 15. | Having a deep splinter in the sole of your foot probed and removed with tweezers. | .64 |
| 16. | Having an eye doctor remove a foreign particle stuck in your eye. | .51 |
| 17. | Receiving an injection in your mouth. | .69 |
| 20. | Receiving stitches in your lip. | .67 |
| 21. | Having a foot doctor remove a wart from your foot with a sharp instrument. | .66 |
| 26. | Having a tooth pulled. | .65 |
| 29. | Having one of your teeth drilled. | .66 |
|
| ||
| Fear of Minor Pain | ||
|
| ||
| FPQ-III Item # and Item: | r | |
| I FEAR THE PAIN ASSOCIATED WITH: | ||
| 2. | Biting your tongue while eating. | .56 |
| 4. | Cutting your tongue licking an envelope. | .59 |
| 7. | Hitting a sensitive bone in your elbow-your “funny” bone. | .64 |
| 12. | Burning your fingers with a match. | .58 |
| 19. | Getting a paper-cut on your finger. | .70 |
| 22. | Cutting yourself while shaving with a sharp razor. | .64 |
| 23. | Gulping a hot drink before it has cooled. | .67 |
| 24. | Getting strong soap in both your eyes while bathing or showering. | .69 |
| 28. | Having sand or dust blow into your eyes. | .63 |
| 30. | Having a muscle cramp. | .57 |
|
| ||
| Fear of Severe Pain | ||
|
| ||
| FPQ-III Item # and Item: | r | |
| I FEAR THE PAIN ASSOCIATED WITH: | ||
| 1. | Being in an automobile accident. | .64 |
| 3. | Breaking your arm. | .75 |
| 5. | Having a heavy object hit you in the head. | .76 |
| 6. | Breaking your leg. | .80 |
| 9. | Having someone slam a heavy car door on your hand. | .81 |
| 10. | Falling down a flight of concrete stairs. | .77 |
| 13. | Breaking your neck. | .79 |
| 18. | Being burned on your face by a lit cigarette. | .70 |
| 25. | Having a terminal illness that causes you daily pain. | .69 |
| 27. | Vomiting repeatedly because of food poisoning. | .63 |
Note. n = 550 (275 chronic pain patients and 275 undergraduates).
After item selection, an exploratory factor analysis (EFA) on the archival data (n = 550) and a confirmatory factor analyses (CFA) on the new data (i.e., 100 pain patients and 190 undergraduates) were used to test the decisions described previously. Conducting the EFA and CFA on different datasets allowed for cross-validation of the assumed factor structure and model fit.
Exploratory factor analysis
The exploratory factor analysis (EFA) was conducted using Mplus 7.4 (Muthén & Muthén, 1999–2015). The EFA first was conducted with the assumption that the Likert-type items were continuous and then as categorical. The EFA included a full information maximum likelihood estimator (MLR) for the continuous analysis and the WMSLV estimator for the categorical analysis. The Mplus default—a geomin, oblique rotation method—provided estimated factor loadings for each item.
Confirmatory factor analysis
Utilizing the new data set (n = 290), the CFA was conducted with the items as categorical and continuous; the model with continuous items fit the data markedly better. Because of improved model fit, the full information likelihood (MLR) estimator was used in subsequent analyses. Based on modification indices reported in Mplus, a second CFA included a ‘WITH’ statement for items 14 and 17 (which allowed the items to be correlated) and improved model fit.
Reliability
To test for internal consistency, coefficient alpha was calculated for each of the subscales individually as well as for the total score. Alpha was chosen because of its familiarity in the literature and because, with a short-form assessment, it is not susceptible to the same downfalls as longer assessments (e.g., inflated reliability as a function of length, similar grammar/statement structure; DeVellis, 2017). The heuristic cutoff of alpha ≥ .70 was used in determining adequate reliability (Nunnally, 1978).
Validity
In addition to factor validity, which was assessed vis-à-vis model fit indices, convergent validity was examined by correlating the FPQ-9 total score with PASS scores derived from the 190 participants in the new data set. Concurrent validity was tested with respondents who completed both the FPQ-9 and FPQ-III. Convergent validity also was evaluated comparing FPQ-9 responses to those of the PASS and the DFS. The DFS was chosen for analysis of convergent validity given that fear of pain has been shown to be a primary component (McNeil & Berryman, 1989) and strong predictor (e.g., Randall et al., 2016) of dental care-related fear, and because dental care-related fear is prevalent, with wide variability, among the general population (Milgrom, Weinstein, & Heaton, 2009). Moreover, the DFS can simultaneously be used for the analysis of convergent and divergent validity across FPQ-9 subscales, given that the FPQ-9 has a subscale assessing fear of medical/dental pain (with expected large associations with DFS scores) and two subscales that are not specifically related to medical/dental pain (each with expected smaller associations with DFS scores).
Results
Item-total correlations
The item-total correlations are reported in Table 1 and were used to determine how each item from the original FPQ-III correlated with its intended subscale or factor (i.e., Fear of Severe Pain, Fear of Minor Pain, Fear of Medical/Dental Pain). Item-total correlation coefficients, theoretical, and pragmatic justifications were used in choosing three items for each of the three subscales, to mirror the parent FPQ-III and its structure of three factors, each consisting of an equal number of 10 items.
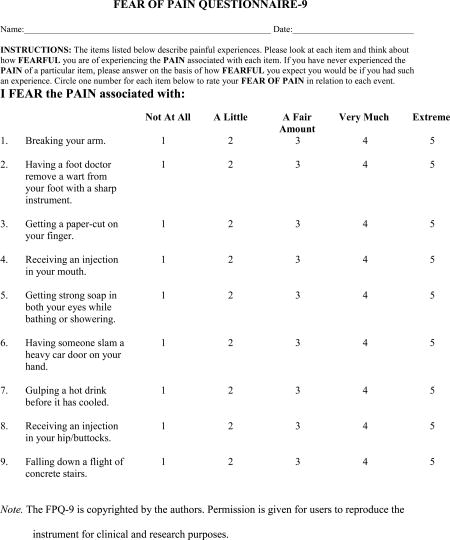
For all selected items, the Flesch Reading Ease statistic is 70.0 and the Flesch-Kincaid Grade Level is 6.3, suggesting appropriate readability. The final measure has a public domain copyright and is included in Appendix A, with scoring criteria in Appendix B.
Exploratory factor analyses
The factor loading results of the EFA using the archival data (i.e., 275 outpatients and 275 undergraduates) are described in Table 2. All items loaded successfully on their intended factor, with factor loadings of above .40 and without cross-loading within .15, with the exception of item 21 (“I fear the pain associated with having a foot doctor remove a wart from your foot with a sharp instrument”) from the original FPQ-III scale. This item cross-loaded on two different factors, but was retained as an attempt to maintain the original factor structure of the parent instrument and because it did not prevent excellent model fit. This justification led to retention of that item and allowed proceeding to the confirmatory factor analysis phase to assess if the factor structure and model fit held in a different sample.
Table 2.
Exploratory Factor Analysis Geomin Rotated Factor Loadings for Three-Factor Model
| FPQ-III Item | Fear of Severe Pain | Fear of Moderate Pain | Fear of Medical Pain |
|---|---|---|---|
| 3. | 0.761* | −0.042 | −0.004 |
| 9. | 0.852* | 0.026 | 0.006 |
| 10. | 0.914* | 0.000 | −0.166 |
| 14. | −0.005 | 0.856* | −0.133 |
| 17. | 0.042 | 0.688* | 0.002 |
| 19. | 0.000 | 0.107 | 0.583* |
| 21. | 0.377* | 0.351* | 0.089 |
| 23. | 0.015 | −0.004 | 0.770* |
| 24. | −.005 | 0.001 | 0.784* |
Note.
p < .05.
Model fit statistics from the EFA are reported in Table 3. As mentioned previously, a three-factor structure produced good to excellent fit. This finding served as reason to proceed to the CFA phase of the analysis. As the EFA revealed no significant difference when the variables were treated as categorical compared to continuous ones, results for handling the data as continuous variables are reported.
Table 3.
Model Fit when Extracting Various Factor Structures from the Exploratory Factor Analysis
| # of factors extracted |
RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|
| One-factor | 0.176 | 0.763 | 0.683 | 0.090 |
| Two-factor | 0.121 | 0.921 | 0.851 | 0.052 |
| Three-factor | 0.034 | 0.996 | 0.988 | 0.012 |
Note. RMSEA = Root Mean Square Error of Approximation; CFI = Confirmatory Fit Index; TLI = Tucker-Lewis Index; SRMR = Standardized Root Mean Square Residual.
Confirmatory factor analysis
Using the new data (n = 290; 190 undergraduates and 100 outpatient pain patients), two CFA models were tested. The first CFA was performed with the items as categorical and the second with items as continuous. The continuous CFA produced better model fit (see Table 4) and subsequently was used for the final CFA. Utilizing the modification indices function in MPlus, two of the items (14 and 17) in the Fear of Medical/Dental Pain subscale were allowed to be correlated, which subsequently produced a well-fitting model as seen in Table 4.
Table 4.
Model Fit Indices Produced by Confirmatory Factor Analyses
| Model | RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|
| Three-factor (categorical) | 0.118 | 0.954 | 0.931 | 1.005 |
| Three-factor (continuous) | 0.072 | 0.950 | 0.925 | 0.048 |
| Three-factor (continuous) and 14 & 17 correlated | 0.000 | 1.000 | 1.000 | 0.027 |
Note. The three-factor model was categorical and fit statistic was WRMR instead of SRMR. RMSEA = Root Mean Square Error of Approximation; CFI = Confirmatory Fit Index; TLI = Tucker-Lewis Index; SRMR = Standardized Root Mean Square Residual.
Examination of Possible Order Effects
To assess possible order effects across two instruments of differing lengths, a mean single-item rating was derived for each of the forms of the FPQ. No differences were observed across FPQ-III (M = 2.5, SD = .71) and FPQ-9 scores (M = 2.5, SD = .74), t(289) = .25, p = .80. Also, a t-test was conducted between the mean score for whichever test was first administered (M = 2.5, SD = .71) and the mean score for whichever test was administered second (M = 2.5, SD = .74), similarly yielding no differences, t(289) = .24, p = .81.
Psychometric Properties of the FPQ-9
Internal consistency
Cronbach’s alpha was calculated for the FPQ-9 total score and three subscales, yielding values from .72 to .94. Table 5 presents these results.
Table 5.
Alpha Coefficients for FPQ-9 and FPQ-III Subscales and Total Scores
| FPQ-9 | FPQ-III | |
|---|---|---|
| Subscale | ||
| Fear of Severe Pain | 0.84 | 0.92 |
| Fear of Minor Pain | 0.72 | 0.89 |
| Fear of Medical/Dental Pain | 0.73 | 0.89 |
| Total Score | 0.83 | 0.94 |
Note. FPQ-9 Fear of Pain Questionnaire – 9; FPQ-III – Fear of Pain Questionnaire – III; n = 290.
Validity
As a measure of concurrent validity, correlations were conducted between the FPQ-III and FPQ-9 subscale and total scores for the new data (i.e., 100 pain patients and 190 undergraduates). Correlations were strong for all scale scores, with p < .01 for each analysis: Total score – r = .77; Fear of Severe Pain - r = .73; Fear of Minor Pain - r = .67; and Fear of Medical/Dental Pain - r = .76. Additionally, as a measure of convergent validity, correlations were conducted between the DFS’ omnibus fear item #20 with the FPQ-9 scores. For the undergraduates, these scores also were compared with the full-length DFS total and subscale scores. Table 6 presents these results. As expected, the FPQ-9 subscale with the highest correlations (all moderate to high) with DFS total score, subscale scores, and Item #20 score was the Fear of Medical/Dental Pain subscale, an indication of convergent validity. Lower correlations between the Fear of Severe Pain subscale of the FPQ-9 and DFS total score, subscale scores, and Item #20 score, also expected, suggest divergent validity. Correlations were calculated for FPQ-9 and FPQ-III in comparison to PASS scores as a measure of convergent validity, as shown in Table 7. Moderate correlations across the board indicate good convergent validity and also suggest that the two measures tap similar, but distinct constructs.
Table 6 .
Correlations Among the Subscales of the FPQ-9, FPQ-III, and DFS
| Dental Fear Survey
|
||||||
|---|---|---|---|---|---|---|
| Avoidance/ Anticipatory Fear1 |
Fear of Specific Dental Stimuli1 |
Physiological Arousal1 |
Total Score1 |
DFS Item #202 |
||
| FPQ-9 | ||||||
| Severe | .22* | .32* | .22* | .28* | .19* | |
| Minor | .28* | .33* | .25* | .31* | .20* | |
| Medical | .45* | .57* | .43* | .53* | .41* | |
| Total | .38* | .49* | .36* | .45* | .33* | |
| FPQ-III | ||||||
| Severe | .21* | .30* | .21* | .26* | .10* | |
| Minor | .32* | .31* | .24* | .32* | .22* | |
| Medical | .45* | .57* | .37* | .52* | .35* | |
| Total | .39* | .47* | .33* | .44* | .26* | |
Note.FPQ-9 = Fear of Pain Questionnaire – 9; FPQ-III = Fear of Pain Questionnaire – III; DFS = Dental Fear Survey;
n = 177 undergraduates; data missing for 13 undergraduates.
n = 288 (100 chronic pain patients and 188 undergraduates; data missing for two participants);
p < .01.
Table 7.
Correlations Among the Subscales of the FPQ-9 and the PASS
| PASS
|
||||||
|---|---|---|---|---|---|---|
| Fear | Cognitive Anxiety |
Escape Avoidance |
Physiological Arousal |
Total | ||
| FPQ-9 | ||||||
| Severe | .35* | .38* | .34* | .30* | .40* | |
| Minor | .35* | .32* | .31* | .20* | .34* | |
| Medical | .42* | .45* | .34* | .36* | .46* | |
| Total | .46* | .48* | .41* | .36* | .50* | |
Note. FPQ-9 – Fear of Pain Questionnaire – 9; PASS – Pain Anxiety Symptoms Scale; n = 190 undergraduates;
p < .01.
Discussion and Conclusions
The aim of the current study was to create a shortened (i.e., fewer than 10 item) version of an instrument that measures fear of pain in clinical and basic research settings. The intent was to allow for time-efficient administration and scoring without sacrificing the accuracy or other psychometric properties of the longer instrument. These results provide psychometric evidence for the comparability of the FPQ in its full-length and current shortened FPQ-9 versions. The three subscales of the FPQ-III (i.e., Fear of Severe Pain, Fear of Minor Pain, and Fear of Medical/Dental Pain) were well represented and maintained in the FPQ-9 subscales. The similarity between the items that were selected as result of high item-total correlations and through factor analyses reinforces their representative strength as items in the FPQ-9 subscales. The factor loadings for the FPQ-9 were acceptable, especially given the adequate to good model fit produced by the analyses. The final factor structure tested in the CFA would be the recommended measurement model to initiate any subsequent analyses, regression or structural equation models (SEM) in further studies using the FPQ-9.
The FPQ-9 provides a more efficient measure of fear of pain than other measures of the construct, including the FPQ-9’s predecessor (the FPQ-III), which is an important strength. In fact, given that the number of items is reduced by more than two-thirds, there is a substantial savings in administration and scoring time; the FPQ-9 is the most economical instrument currently available. The full-length FPQ-III takes approximately four-to-five minutes to complete, and three-to-four minutes for the healthcare provider/researcher to score. Conversely, the FPQ-9 takes about two minutes or less to complete and less than one minute to score. Subscale scores are calculated by summing the three items in each subscale (e.g., Fear of Severe Pain subscale is calculated by summing values for items 1, 6, and 9). The total score then is determined by summing the three subscale scores. Additional scoring information is available in Appendix B.
As clinicians generally have stringent demands placed on their time, shortened assessment instruments that adequately and accurately measure constructs of interests are understood to be ideal for clinical application. Evidence from the current study suggests that the FPQ-9 is reliable and valid measure of fear and anxiety associated with pain and, at only 9 items, the instrument may be particularly well-suited for use in medical, dental, rehabilitation, and pain clinics, among other clinical contexts. The FPQ-9 can be administered and scored easily in a few minutes. Addressing fear of pain in certain clinical populations has the potential to improve treatment outcome, pain experience, and overall patient condition.
There are at least two apparent benefits to the utilization of this shorter measure in the research context. First, participants completing shorter instruments presumably are less likely to experience participant fatigue (Sitzia & Wood, 1997; Ben-Nun, 2008; Hoerger, M, 2010; Randall, McNeil, Crout, Weyant, & Marazita, 2013). Second, shorter assessment tools provide opportunity for the researcher to include additional measures in the spirit of more comprehensive evaluation. Of course, balance must be achieved between limiting participant fatigue and the thoroughness of assessment. The FPQ-9 exemplifies a significant step in the shortening of a commonly used measurement instrument, for the benefit of pain research. An additional strength of this shortened version of the FPQ-III is that each item maintains the wording used in the parent instrument, and so use of the FPQ-9 in languages other than English potentially could rely upon prior translations of the FPQ-III (e.g., Dutch; van Wijk & Hoogstraten, 2009).
In spite of the inclusion of both clinical and nonclinical samples, and careful methodological rigor, this study has some limitations. First, the FPQ-9, while including three dimensions like its parent instrument, still only assesses fear in the realm of self-report, so it, along with other questionnaire measures, is inherently limited. Second, the FPQ-9 likely measures both fear and anxiety, as do all currently extant instruments in this area. Although pain-related fear and anxiety are separate states (McNeil et al., 1993; McNeil et al., 2001; Craske, 2003; McNeil & Vowles, 2004; McNeil et al., 2012), the current state of the science is that fear and anxiety about pain are measured jointly, even though some scale titles (or subscale titles) would suggest otherwise. The FPQ-9 should be administered with the understanding that both fear and anxiety are being measured; future development of assessment tools that measure fear or anxiety, disentangling the two, may be warranted. A third limitation is that the length of time between the first and second administrations of the two versions of the FPQ differed between the pain outpatients and undergraduates, due to logistical constraints. Also, the fact that a pain clinic appointment intervened between the administrations for the outpatients introduces unknown variance. Finally, these development studies did not include measures of pain itself, either chronic or acute, and either current and/or past, which would have strengthened the methodology. Nevertheless, the results presented here demonstrate the strength of the FPQ-9, constructed within contemporary recommendations for short-form development (Adams, 2000; Reise, Waller, & Comrey, 2000), are most encouraging.
There still is a place for the full-length FPQ-III, and other, longer pain-related fear and anxiety assessments. When issues of fear and anxiety are suspected in pain patients, or in research that focuses on the relation between fear/anxiety and pain, the full length FPQ-III (or similar instruments, depending on the research or clinical question at hand), may be the most appropriate choice to allow the most comprehensive assessment.
This study of a truly shortened short form of the FPQ-III suggests that the FPQ-9 has overall good psychometric properties. Still, additional research is necessary to confirm the factor structure of the FPQ-9 in other and more diverse samples and settings. Test-retest reliability and construct validity of the FPQ-9 also should be the subject of future research. Additionally, future work should seek to establish FPQ-9 norms for the general population as well as specific clinical groups.
Emotions, particularly fear and anxiety, have an important role in the experience of both acute and chronic pain (Romano & Turner, 1985; Hursey & Jacks, 1992; McCracken et al., 1992; Geisser et al., 1994; Hirsh et al., 2008). Comprehensive assessment of problem emotional states likely will first depend on accurate screening, using an instrument that is sufficiently brief, accurate, and accessible to a variety of patient and nonclinical populations. The FPQ-9 has promise as such a short, respondent-completed instrument that will allow for more patient-centered care while still providing useful information to help guide further assessment and treatment.
Significance.
The FPQ-9 has considerable potential for dissemination and utility for routine, brief screening, given its length (completion time ~2 minutes; scoring time ~1 minute), reading level, and psychometric properties.
Acknowledgments
Sources of Funding - Preparation of this manuscript was supported in part by grants from the National Institute for Dental and Craniofacial Research, National Institutes of Health (R01 DE014899 and F31 DE023493), and from the National Institute of General Medical Sciences, National Institutes of Health (T32-GM081741).
The authors gratefully acknowledge the patients, including those from the West Virginia University Pain Clinic, and the students who participated in this project. Partial funding from the West Virginia University Undergraduate Enrichment Fund helped make this project possible. The contributions of research assistants and associates in the Anxiety, Psychophysiology, and Pain Research Laboratory at West Virginia University are noted with thanks.
Preparation of this manuscript was supported in part by grants from the National Institute for Dental and Craniofacial Research, National Institutes of Health (R01 DE014899 and F31 DE023493), and from the National Institute of General Medical Sciences, National Institutes of Health (T32-GM081741).
Appendix A
Appendix B
Scoring Instructions Fear of Pain Questionnaire-9
Score the Fear of Severe Pain subscale by summing values for the following items: 1, 6, 9
Score the Fear of Minor Pain subscale by summing values for the following items: 3, 5, 7
Score the Fear of Medical/Dental Pain subscale by summing values for the following items: 2, 4, 8
Calculate the Total Score by summing the three subscale values, or simply sum all 9 items. (You may wish to calculate the Total Score both ways, to check for possible errors.)
Note. Each subscale contains 3 items, so the possible range of scores for each subscale is 3 through 15. The Total score has a range of 9 through 45.
The 9 items of the Short Form-FPQ items correspond exactly to those in the 30 item Fear of Pain Questionnaire as follows:
| FPQ-9 Item # | FPQ-III Item # |
|---|---|
| 1 | 3 |
| 2 | 21 |
| 3 | 19 |
| 4 | 17 |
| 5 | 24 |
| 6 | 9 |
| 7 | 23 |
| 8 | 14 |
| 9 | 10 |
Footnotes
Conflicts of Interest - The authors have no conflicts of interest to disclose.
Author Contributions
DWM – Contributed to study conception and design, participated in and supervised data collection, participated in and supervised data analysis/interpretation, participated in manuscript preparation and critical revision, and gave final approval.
SGK – Contributed to study conception and design, collected data, participated in data input and data analysis/interpretation, participated in manuscript preparation and critical revision, and gave final approval.
CLR – Contributed to manuscript conception and design, participated in data analysis/interpretation, participated in manuscript preparation and critical revision, and gave final approval.
SHA – Contributed to manuscript conception and design, participated in data analysis/interpretation, participated in manuscript preparation and critical revision, and gave final approval.
CDW – Contributed to manuscript conception and design, participated in data analysis/interpretation, participated in manuscript preparation and critical revision, and gave final approval.
KGH – Contributed to study design, supervised data collection, provided clinical care to chronic pain patients, participated in manuscript critical revision, and gave final approval.
RV - Contributed to study design, supervised data collection, provided clinical care to chronic pain patients, participated in manuscript critical revision, and gave final approval.
References
- Adams KM. Practical and ethical issues pertaining to test revisions. Psychol Assess. 2000;12:281–286. doi: 10.1037/1040-3590.12.3.281. [DOI] [PubMed] [Google Scholar]
- Albaret MC, Sastre MTM, Cottencin A, Mullet E. The Fear of Pain questionnaire: Factor structure in samples of young, middle-aged and elderly European people. Eur J Pain. 2004;8:273–281. doi: 10.1016/j.ejpain.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Asmundson GJG, Bovell CV, Carleton RN, McWilliams LA. The Fear of Pain Questionnaire—Short Form (FPQ-SF): Factorial validity and psychometric properties. Pain. 2008;134:51–58. doi: 10.1016/j.pain.2007.03.033. [DOI] [PubMed] [Google Scholar]
- Ben-Nun P. Respondent fatigue. In: Lavakras P, editor. Encyclopedia of survey research methods. Thousand Oaks, CA: Sage Publications; 2008. p. 460. [Google Scholar]
- Bodenheimer TS, Smith MD. Primary care: Proposed solutions to the physician shortage without training more physicians. Health Aff. 2013;32:1881–1886. doi: 10.1377/hlthaff.2013.0234. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford; 2015. [Google Scholar]
- Buer N, Linton SJ. Fear-avoidance beliefs and catastrophizing: Occurrence and risk factor in back pain and ADL in the general population. Pain. 2002;99:485–491. doi: 10.1016/S0304-3959(02)00265-8. [DOI] [PubMed] [Google Scholar]
- Carter LE, McNeil DW, Vowles KE, Sorrell JT, Turk CL, Ries BJ, Hopko DR. Effects of emotion on pain reports, tolerance, and physiology. Pain Res Manag. 2002;7:21–30. doi: 10.1155/2002/426193. [DOI] [PubMed] [Google Scholar]
- Craske MG. Origins of phobias and anxiety disorders: Why more women than men? Oxford: Elsevier; 2003. [Google Scholar]
- Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–339. doi: 10.1016/S0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- DeVellis RF. Scale development: Theory and applications. Thousand Oaks: Sage; 2017. [Google Scholar]
- Geisser ME, Robinson ME, Keefe FJ, Weiner ML. Catastrophizing, depression and the sensory, affective and evaluative aspects of chronic pain. Pain. 1994;59:79–83. doi: 10.1016/0304-3959(94)90050-7. [DOI] [PubMed] [Google Scholar]
- George SZ, Dannecker EA, Robinson ME. Fear of pain, not pain catastrophizing, predicts acute pain intensity, but neither factor predicts tolerance or blood pressure reactivity: An experimental investigation in pain-free individuals. Eur J Pain. 2006;10:457–465. doi: 10.1016/j.ejpain.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Grimmer-Somers K, Vipond N, Kumar S, Hall G. A review and critique of assessment instruments for patients with persistent pain. J Pain Res. 2009;2:21–47. doi: 10.2147/jpr.s4949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaton LJ, Carlson CR, Smith TA, Baer RA, de Leeuw R. Predicting anxiety during dental treatment using patients' self-reports: Less is more. J Amer Dent Assoc. 2007;138:188–95. doi: 10.14219/jada.archive.2007.0135. [DOI] [PubMed] [Google Scholar]
- Hirsh AT, George SZ, Bialosky JE, Robinson ME. Fear of pain, pain catastrophizing, and acute pain perception: relative prediction and timing of assessment. J Pain. 2008;9:806–812. doi: 10.1016/j.jpain.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoerger M. Participant dropout as a function of survey length in internet-mediated studies: Implications for study design and voluntary participation in psychological research. Cyberpsychol Behav. 2010;13:697–700. doi: 10.1089/cyber.2009.0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hursey KG, Jacks SD. Fear of pain in recurrent headache sufferers. Headache. 1992;32:283–286. doi: 10.1111/j.1526-4610.1992.hed3206283.x. [DOI] [PubMed] [Google Scholar]
- Kleinknecht RA, Klepac RK, Alexander LD. Origins and characteristics of fear of dentistry. J Am Dent Assoc. 1973;86:842–848. doi: 10.14219/jada.archive.1973.0165. [DOI] [PubMed] [Google Scholar]
- Lee KC, Chiu TTW, Lam TH. The role of fear-avoidance beliefs in patients with neck pain: Relationships with current and future disability and work capacity. Clin Rehab. 2007;21:812–821. doi: 10.1177/0269215507077800. [DOI] [PubMed] [Google Scholar]
- LeMay K, Wilson KG, Buenger U, Jarvis V, Fitzgibbon E, Bhimji K, Dobkin P. Fear of pain in patients with advanced cancer or in patients with chronic noncancer pain. Clin J Pain. 2011;27:116–124. doi: 10.1097/AJP.0b013e3181f3f667. [DOI] [PubMed] [Google Scholar]
- Linzer M, Bitton A, Tu S, Plews-Ogan M, Horowitz KR, Schwartz MD. The end of the 15–20 minute primary care visit. JGIM. 2015;30:1584–1586. doi: 10.1007/s11606-015-3341-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken LM, Dhingra L. A short version of the Pain Anxiety Symptoms Scale (PASS-20): Preliminary development and validity. Pain Res Cl. 2002;7:45–50. doi: 10.1155/2002/517163. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Gross RT, Aikens J, Carnkike CLM., Jr The assessment of anxiety and fear in persons with chronic pain: A comparison of instruments. Behav Res Ther. 1996;34:927–933. doi: 10.1016/S0005-7967(96)00057-5. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Zayfert C, Gross RT. The Pain Anxiety Symptoms Scale: Development and validation of a scale to measure fear of pain. Pain. 1992;50:63–67. doi: 10.1016/0304-3959(92)90113-P. [DOI] [PubMed] [Google Scholar]
- McGlynn FD. Dental Fear Survey. In: Hersen M, Bellack A, editors. Dictionary of behavioral assessment techniques. New York: Pergamon; 1998. pp. 168–170. [Google Scholar]
- McGlynn FD, McNeil DW, Gallagher SL, Vrana S. Factor structure, stability, and internal consistency of the Dental Fear Survey. Beh Assess. 1987;9:57–66. [Google Scholar]
- McNeil DW, Au AR, Zvolensky MJ, McKee DR, Klineberg IJ, Ho CCK. Fear of pain in orofacial pain patients. Pain. 2001;89:245–52. doi: 10.1016/S0304-3959(00)00368-7. [DOI] [PubMed] [Google Scholar]
- McNeil D, Berryman L. Components of dental fear in adults? Behav ResTher. 1989;27:233–236. doi: 10.1016/0005-7967(89)90041-7. [DOI] [PubMed] [Google Scholar]
- McNeil DW, Rainwater AJ., III Development of the Fear of Pain Questionnaire-III. J Behav Med. 1998;21:169–190. doi: 10.1023/A:1018782831217. [DOI] [PubMed] [Google Scholar]
- McNeil DW, Randall CL. Dental fear and anxiety associated with oral health care: Conceptual and clinical issues. In: Mostofsky DI, Fortune F, editors. Behavioral dentistry. Ames: Wiley/Blackwell; 2014. pp. 165–192. [Google Scholar]
- McNeil DW, Vargovich AM, Turk CL, Ries BJ. Anxiety and fear. In: Ramachandran V, editor. Encyclopedia of human behavior. 2nd. Vol. 1. San Diego, CA: Academic Press; 2012. pp. 161–168. [Google Scholar]
- McNeil DW, Vowles KE. Assessment of fear and anxiety associated with pain: Conceptualization, methods, and measures. In: Asmundson G, Vlaeyen J, Crombez G, editors. Understanding and treating fear of pain. Oxford: Oxford University Press; 2004. pp. 189–211. [Google Scholar]
- McNeil DW, Vrana SR, Malamed BG, Cuthbert BN, Lang PJ. Emotional imagery in simple and social phobia: Fear versus anxiety. J Abnorm Psychol. 1993;102:212–225. doi: 10.1037/0021-843X.102.2.212. [DOI] [PubMed] [Google Scholar]
- Milgrom P, Weinstein P, Heaton LJ. Treating fearful dental patients: A patient management handbook. Seattle, WA: Dental Behavioral Resources; 2009. [Google Scholar]
- Nunnally JC. Psychometric theory. New York: McGraw-Hill; 1978. [Google Scholar]
- Okie S. The evolving primary care physician. N Eng Jour Med. 2012;363:1849–1853. doi: 10.1056/NEJMp1201526. [DOI] [PubMed] [Google Scholar]
- Osman A, Breitenstein JL, Barrios FX, Gutierrez PM, Kopper BA. The Fear of Pain Questionnaire-III: Further reliability and validity with nonclinical samples. J Behav Med. 2002;25:155–173. doi: 10.1023/A:1014884704974. [DOI] [PubMed] [Google Scholar]
- Parr JJ, Borsa PA, Fillingim RB, Tillman MD, Tillman MD, Gregory CM, George SZ. Pain-related fear and catastrophizing predict pain intensity and disability independently using an induced muscle injury model. J Pain. 2012;13:370–378. doi: 10.1016/j.jpain.2011.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall CL, McNeil DW, Crout RJ, Weyant RJ, Marazita ML. Collecting psychosocial self-report data in oral-health research: Impact of literacy level and computerized administration. Soc Sci Dent. 2013;2:80–87. [PMC free article] [PubMed] [Google Scholar]
- Randall CL, McNeil DW, Shaffer JR, Crout RJ, Weyant RJ, Marazita ML. Fear of pain mediates the association between MC1R genotype and dental fear. J Dent Res. 2016;95:1132–1137. doi: 10.1177/0022034516661151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise SP, Waller NG, Comrey AL. Factor analysis and scale revision. Psychol Assess. 2000;12:287–296. doi: 10.1037/1040-3590.12.3.287. [DOI] [PubMed] [Google Scholar]
- Roelofs J, Peters ML, Deutz J, Spijker C, Vlaeen JWS. The Fear of Pain Questionnaire (FPQ): Further psychometric examination in a non-clinical sample. Pain. 2005;116:339–346. doi: 10.1016/j.pain.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Romano JM, Turner JA. Chronic pain and depression: Does the evidence support a relationship? Psychol Bull. 1985;97:18–34. doi: 10.1037/0033-2909.97.1.18. [DOI] [PubMed] [Google Scholar]
- Shaw MK, Davis SA, Fleisher AB, Feldman SR. The duration of office visits in the United States, 1993 to 2010. Am J Mang Care. 2014;20:820–826. [PubMed] [Google Scholar]
- Sitzia J, Wood W. Patient satisfaction: A review of issues and concepts. Soc Sci Med. 1997;45:1829–1843. doi: 10.1016/S0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- Sperry-Clark JA, McNeil DW, Ciano-Federoff L. Assessing chronic pain patients: The Fear of Pain Questionnaire-III. In: VandeCreek L, Jackson T, editors. Innovations in clinical practice: A source book. Sarasota, FL: Professional Resource Press; 1999. pp. 293–305. [Google Scholar]
- Turk DC, Robinson JP, Burwinkle T. Prevalence of fear of pain and activity in patients with fibromyalgia syndrome. J Pain. 2004;5:483–490. doi: 10.1016/j.jpain.2004.08.002. [DOI] [PubMed] [Google Scholar]
- van Wijk AJ, Hoogstraten J. Dutch translation of the Fear of Pain Questionnaire: Factor structure, reliability, and validity. Eur J Pain. 2006;10:479–486. doi: 10.1016/j.ejpain.2005.06.008. [DOI] [PubMed] [Google Scholar]
- van Wijk AJ, Hoogstraten J. Anxiety and pain during dental injections. J Dent. 2009;37:700–704. doi: 10.1016/j.jdent.2009.05.023. [DOI] [PubMed] [Google Scholar]
- Vlaeyen JW, de Johng J, Geilen M, Heuts PHTG, van Breuklen G. Graded exposure in vivo in the treatment of pain-related fear: A replicated single-case experimental design in four patients with chronic low back pain. Behav Res Ther. 2001;39:151–66. doi: 10.1016/S0005-7967(99)00174-6. [DOI] [PubMed] [Google Scholar]
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: A shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117:1–2. doi: 10.1016/j.pain.2005.05.029. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Goodie JL, McNeil DW, Sperry JS, Sorrell JT. Anxiety sensitivity in the prediction of pain-related fear and anxiety in a heterogeneous chronic pain population. Behav Res Ther. 2001;39:683–696. doi: 10.1016/S0005-7967(00)00049-8. [DOI] [PubMed] [Google Scholar]


