Abstract
Atrial fibrillation (AF) is a common cardiac arrhythmia with significant clinical outcomes, and is associated with high medical and social costs. AF is complicated for patients because of its specialised terminology, long-term adherence, symptom monitoring, referral to specialty care, array of potential interventions and potential for adversity. Health literacy is a frequently under-recognised, yet fundamental, component towards successful care in AF. Health literacy is defined as the capacity to obtain, process and understand health information, and has had markedly limited study in AF. However, health literacy could contribute to how patients interpret symptoms, navigate care, and participate in treatment evaluation and decision-making. This review aims to summarise the clinical importance and essential relevance of health literacy in AF. We focus here on central aspects of AF care that are most related to self-care, including understanding the symptoms of AF, shared decision-making, adherence and anticoagulation for stroke prevention. We discuss opportunities to enhance AF care based on findings from the literature on health literacy, and identify important gaps. Our overall objective is to articulate the importance and relevance of integrating health literacy in the care of individuals with AF.
Keywords: Atrial fibrillation, health literacy, prevention, patients, risk factors, patient-centred care
Atrial fibrillation (AF) requires complex management to prevent adverse outcomes. To succeed with AF, patients need to learn specialised medical terminology and the self-care skills and activation to interpret and report symptoms. AF care involves long-term adherence to medications with deleterious side-effects, such as antiarrhythmics and anticoagulants. The patient experience of AF is further complicated by the range of debilitating symptoms, complications and navigation of specialty care. Health literacy is essential for patients to navigate AF management and self-care successfully. This review of health literacy and AF aims to: (a) identify the importance of health literacy for patients with AF; and (b) describe how healthcare providers’ attention to health literacy can improve the clinical management of AF.
Health literacy has had limited investigation in AF. Indeed, none of the large community-based studies or clinical trials in AF have included the measurement of health literacy. Multiple knowledge gaps remain in understanding the role of health literacy in AF; aspects of AF where health literacy is particularly relevant include: (a) assessment and monitoring of symptoms and quality of life (QOL); (b) patient engagement and activation for meaningful participation in shared decision-making; and (c) anticoagulation for prevention of ischaemic stroke. Within each of these domains, we identified pertinent studies to summarise present knowledge and identify critical gaps. We describe strategies at the patient, provider and system level for improving the experience of people with limited health literacy and AF.
The Clinical Significance of Health Literacy
Health literacy is the “capacity to obtain, process, and understand basic health information and services needed to make appropriate medical decisions”.1 Reading, writing and numeracy along with the ability to interact with health professionals, as well as seek and comprehend medical information, are fundamental to health literacy. Further dimensions include the ability to act on health-related information, evaluate treatment courses and the ability to navigate the healthcare system.2 National surveys have demonstrated that 36 % of US adults have limited health literacy.3
Limited health literacy is associated with limited knowledge of health conditions,4,5 poorer medication adherence,6 worse disease status, early hospital readmission and mortality.7 In multivariable analyses, including sociodemographic and health status, older adults with inadequate health literacy have a 1.5-fold increased risk of both cardiovascular and all-cause mortality, relative to those with adequate literacy.6 In patients with heart failure, limited health literacy has been associated with increased hospitalisation8 and a two-fold increase in mortality,9 relative to those with adequate literacy.
There are multiple gaps in our understanding of the clinical and epidemiological relations of health literacy and AF. Social determinants of health, such as health literacy, have been largely absent from investigations of AF epidemiology, risk factors and adverse outcomes. How health literacy and socioeconomic factors might influence AF merits examination to determine opportunities to improve patients’ QOL and outcomes. An important first step would be to incorporate validated measures of health literacy in AF clinical trials and registries. Table 1 summarises the future directions for examining the relations of health literacy and AF in such contexts.
Table 1.
Future Directions for Incorporating Health Literacy in Atrial Fibrillation (AF) Clinical Investigation and Epidemiology
| Domain | Specific direction |
|---|---|
| Clinical significance of health literacy |
|
| Management of AF | |
| Symptoms and quality of life |
|
| Knowledge and shared decision-making |
|
| Anticoagulation and thromboprophylaxis |
|
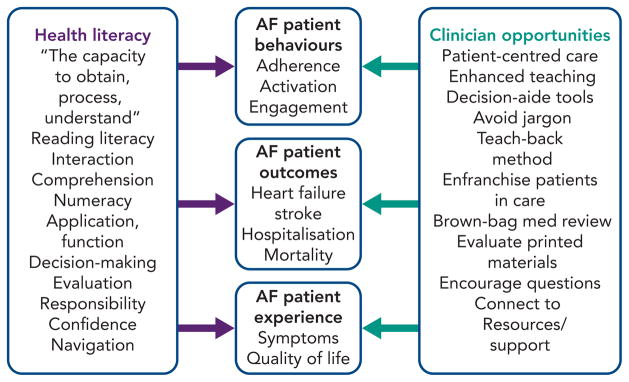
The Agency for Healthcare Research and Quality (AHRQ) has developed the Health Literacy Universal Precautions Toolkit.10 A fundamental premise is the professional and institutional mandate to make healthcare accessible for individuals across the spectrum of health literacy. The toolkit promotes a “universal precautions” approach – to confirm patient comprehension – as a mechanism to improve accessibility, communication and utilisation, regardless of a person’s level of health literacy. In Table 2, we adapted the 21 tools of the AHRQ Universal Precautions Toolkit to illustrate their application for individuals with AF. Figure 1 summarises the definition of health literacy, its potential impact in AF and multiple clinician opportunities, selected from the Toolkit. A common thread relates to opportunities that health systems and providers can take to simplify the experience of being a patient, and empower patients to succeed in their care.
Table 2.
AHRQ Health Literacy Universal Precautions Toolkit Components and Modification for Atrial Fibrillation (AF) Clinical Care and Practice10
| Tool | Title | Potential application in AF |
|---|---|---|
| 1 | Form a team | Develop a team of multidisciplinary stakeholders (e.g. anticoagulation, primary care, cardiology and electrophysiology representatives) to promote HL in AF |
| 2 | Create a health literacy improvement plan | Improve AF education, anticoagulation adherence or symptom assessment |
| 3 | Raise awareness | Educate staff about HL and challenges of HL relevant to AF |
| 4 | Communicate clearly | Use plain language, avoiding jargon, adopt the patient’s words, show pictures to teach about heart rhythm irregularity and stroke risk |
| 5 | Use the teach-back method | Use written materials, such as medication and INR logs, enhance teaching |
| 6 | Follow up with patients | Involve patient in monitoring (e.g. INR values, heart rates, symptom tracking) |
| 7 | Improve telephone access | Implement universal precautions to facilitate patient-centred communications |
| 8 | Conduct brown-bag medicine reviews | Review all medications as a standard for quality patient care, review anticoagulation logs and adherence routinely with patients. |
| 9 | Address language differences | Provide AF education and adherence counselling with a trained interpreter |
| 10 | Consider culture, customs and beliefs | Receive training in cultural competence; remember the patient’s expertise in the intersection of culture and beliefs with AF and other medical care |
| 11 | Assess, select and create easy-to-understand materials | Evaluate forms, informed consent, procedural brochures for readability |
| 12 | Use health-education material effectively | Create information order sets or collected materials on AF treatment options |
| 13 | Welcome patients: helpful attitude, signs and more | Use the environment to promote questions about AF and medication review |
| 14 | Encourage questions | Invite questions routinely on causes of AF; what patients experience, treatments |
| 15 | Make action plans | Have patients choose realisable goals on AF (e.g. adherence or addressing risk factors for AF, such as smoking, physical activity, blood pressure control) |
| 16 | Help patients remember how and when to take their medicine | Facilitate tools to support medication use; educate patients on systems for tracking medication; anticipate errors; provide tools, such as pill boxes |
| 17 | Get patient feedback | Utilise patient expertise on being a patient with AF through surveys and suggestions |
| 18 | Link patients to non-medical support | Appreciate the impact of social determinants on health, utilise community-based resources |
| 19 | Direct patients to medicine resources | Review insurance coverage and verify eligibility for anticoagulants, antiarrhythmics and other medications |
| 20 | Connect patients with literacy and math resources | Discern how literacy impacts patients’ lives and experience with a chronic condition, such as AF; identify community resources |
| 21 | Make referrals easy | Make sure the patient understands the rationale for a referral (e.g. explain electrophysiology and guide patient in utilising the visit) |
Full details regarding the tools are available at the indicated reference and not explicated here. AHRQ = Agency for Healthcare Research and Quality; INR = international normalised ratio; HL = health literacy.
Figure 1.
Addressing Atrial Fibrillation (AF) and Health Literacy
Health literacy has been associated with patient interaction with the healthcare system, increased risk for adverse outcomes and a poor experience of disease. Clinician opportunities for addressing health literacy are summarised and described in the AHRQ Universal Precautions Toolkit.10
Health Literacy in Symptoms and QOL in AF
Symptom severity and QOL guide AF treatment. Yet there are large differences in how patients experience and report AF symptoms.11 Socioeconomic status and education, both strongly related to health literacy, have been related to severity of AF symptoms.12 Health literacy affects how patients recognise and communicate their symptoms.5 In addition, health literacy is implicated in the burden and experience of symptoms. In a cross-sectional study of over 400 individuals with heart failure, for example, limited literacy was associated with worse QOL and a higher level of symptoms.13 A similar assessment in AF is lacking. Further, limited health literacy could influence symptom reporting in AF, particularly given the complexity of its associated symptoms.
Standardised instruments have been developed to quantify symptom burden in AF; we selected instruments commonly used for the assessment of symptoms and QOL in AF (see Table 3), and measured their reading level with validated measures. Specifically, we employed the Flesch–Kincaid Grade Level,14 Simple Measure of Gobbledygook score,15 Dale–Chall Readability16 and the Lexile Framework17 to quantify reading levels of the AF-specific instruments. While some are rated at a middle-school reading level, other tools are more complex and require college- or even graduate-level reading capacity. In contrast, the recommended reading level for health information is at a sixth-grade level.18
Table 3.
Readability and Grade Level of Selected Instruments for Patient-Reported Health Status
| Instrument | Flesch–Kincaid grade level14 | Simple Measure of Gobbledygook15 | Dale–Chall Readability16 | Estimated Lexile Measure |
|---|---|---|---|---|
| Generic | ||||
| SF-3643 | 6.1 | 6.8 | 6.1 | 1250 |
| SF-1244 | 6.1 | 6.7 | 5.9 | 1100 |
| EQ-5D-5L45 | 16.1 | 12.8 | 8.0 | 1920 |
| Selected Instruments, specific to AF | ||||
| AF Quality of Life Instrument46,47 | 4.3 | 5.4 | 7.2 | 1750 |
| AF Effect on Quality of Life48 | 12.9 | 11.6 | 8.0 | 1770 |
| AF Symptom and Burden49 | 10.5 | 9.6 | 7.4 | 1510 |
Items presented are not comprehensive. Flesch-Kincaid and Simple Measure of Gobbledygook provide grade-level estimates. Dale–Chall Readability is a scaled measure for evaluating the expected reading grade level for text comprehension; for example, a score of 7.0–7.9 indicates reading grade level 9–10, and 8.0–8.9 indicates grade level 11–12. Estimated Lexile Measure is an internationally-employed measure for gauging reading level, with higher scores corresponding to greater text complexity. AF = atrial fibrillation.
We identified no study testing the validity of any AF-related QOL measure for use with patients who have limited health literacy. Accordingly, the quality of the data gleaned from such instruments might be limited, especially for older adults, racial and ethnic minorities and individuals with lower income or educational attainment, populations with higher rates of limited health literacy.3 Assessments of symptoms and QOL are now routine in clinical studies, trials and registries of individuals with AF. The concurrent assessment of health literacy in such studies would enhance understanding of the real-world challenges experienced by individuals with AF. It is imperative that physicians treating individuals with AF incorporate strategies for identifying patient symptoms and optimising therapy, regardless of the level of health literacy. Adapting a patient’s treatment plan for AF in relation to their symptoms is paramount and complex, as this work needs to incorporate details of patients’ biopsychosocial circumstances, as well as their language skills, educational needs and health literacy.
Health Literacy, Patient Education, and Shared Decision-Making
There has been consistent recognition of adverse consequences associated with patients’ knowledge of AF. An international survey revealed that one in four patients was unable to explain AF.19 In a cohort of patients undergoing pulmonary vein isolation for AF, less than half were able to correctly answer questions regarding the condition. Knowledge deficits in AF were increased in individuals with less education.20 AF knowledge scales have been developed and validated for assessing and evaluating patient knowledge of AF.20,21 However, such measures have not been promulgated or used to trigger educational or empowerment interventions. To our knowledge, measurement of AF knowledge has not been implemented in settings with limited health literacy.
Single, one-time educational interventions have been shown to have marginal improvement of AF knowledge 2–8 weeks following the intervention.22,23 We identified patient education materials for AF from websites from medical professional societies, major academic medical centres and Internet-based medical references by conducting an Internet-based search, using widely-accessible search engines. Table 4 summarises a sample of the identified websites with information related to AF management. On average, these materials require a 10-grade reading level (range seventh grade to graduate level). Educational material written in simpler language or describing AF with images, cartoons, photo-novellas or descriptive narratives were not identified.
Table 4.
Selected online materials available for AF education, and their readability levels, as assessed by the FKGL and SMOG measures
Websites of selected medical professional societies, major academic medical centres and Internet-based medical references were identified through an Internet-based search using widely-accessible search engines. FKGL and SMOG provide grade-level estimates. Dale–Chall Readability is a scaled measure for evaluating the expected reading grade level for text comprehension; for example, a score of 7.0–7.9 indicates reading grade level 9–10, and 8.0–8.9 indicates grade level 11–12. Estimated Lexile Measure is an internationally-employed measure for gauging reading level, with higher scores corresponding to greater text complexity. FKGL = Flesch-Kincaid Grade Level; (for consistency) SMOG = Simple Measure of Gobbledygook score.
There has been increased attention on shared-decision making in AF.24 Shared decision-making requires a specific orientation of patients and their healthcare providers. Patients must have sufficient knowledge of the arrhythmia and the rationale for treatment strategies and options to participate. It also requires that patients have sufficient knowledge and initiative, i.e., activation, to participate in decision-making.25 Patient knowledge about the disease, available therapeutic options, and personal values and preferences are essential for successful participation in shared decision-making.26 Thus, by necessity, shared decision-making in AF requires that the patient have sufficient health literacy. Barriers to patient-centred, shared-decision making include lower educational level, inability to understand medical information and lack of sufficient information.26 For the clinician, successfully establishing shared decision-making requires an adaptive approach, one that accommodates patients’ health literacy in addition to other social determinants of health and patient characteristics. We did not identify studies examining the effects of health literacy on patient participation in shared decision-making in AF.
In a randomised, clinical trial, patients receiving nurse-directed care in AF clinics had decreased hospitalisation and better adherence to treatment guidelines compared to those receiving standard care. The intervention cohort received extended visits that included education and symptom recognition.27 This single-centre experience shows the promise of more extended visits, with a patient-centred focus. Other examples of educational intervention in chronic diseases could provide paradigms for improving AF care. Educational interventions in heart failure are associated with improved QOL28 and reduced hospitalisation and mortality rates.29 Interventions that have been studied include education on self-management, picture-based educational materials, scheduled telephone follow ups, telephone reinforcement of learning goals and self-management, and high-intensity, multidisciplinary education. In these trials, approximately 40 % of participants had limited health literacy.28 Interventions that have been studied in patients with diabetes include intensive educational sessions by pharmacists, frequent telephone or in person follow-up visits to ensure adherence and structured group educational programmes.30,31 In randomised trials, these interventions have been associated with improved diabetes knowledge, blood pressure and glycaemic control, weight loss, smoking cessation and patient satisfaction.
Educational interventions that improve AF knowledge and empowerment are essential. The European Heart Rhythm Association (EHRA) emphasised the central relevance of patient education as part of AF treatment and management in a consensus statement on patient values and preferences for addressing arrhythmias.32 Improvement of patients’ understanding of their symptoms and capacity to use their knowledge to advance their care is fundamental to guide and enhance meaningful shared decision-making. The EHRA consensus statement emphasises: (a) patients’ “expertise” in the experience of living with a chronic, highly-morbid condition; and (b) the essential role of developing educational interventions that are appropriately tailored for patients, based on their values, preferences, cognition and educational level.
Available studies evaluating educational interventions in AF have been limited by having short follow-up periods and lack of standardisation in the methods to quantify knowledge. Studies with longer follow-up periods, standardised instruments and appropriate across levels of health literacy are required. In this work, patients cannot be the only intervention target; improving clinicians’ communication skills, receptivity to shared decision-making and systems to support the collection of quality of life data to use in adapting treatment plans are all also part of the health literacy agenda. In addition, patients with AF are cared for in diverse settings, yet most data on educational interventions are derived from specialised arrhythmia or anticoagulation settings. Future studies are required to assess the utility and results of educational interventions across settings. Easy-to-use, plainly-written educational materials in all languages are essential. However, patient education materials are not likely to succeed in a vacuum. Implementation research is needed to determine how education and empowerment for patients, as well as clinicians and their staff, can become a routine element of the care for patients with AF. Whether educational materials written for a lower reading level improve communication, satisfaction, AF or anticoagulation knowledge and increase patient participation in shared decision-making, also merit investigation.
Health Literacy in AF and Anticoagulation
Oral anticoagulation is a mainstay for stroke prevention in AF. However, oral anticoagulation with warfarin is challenging, as warfarin is associated with increased risk for bleeding, and requires adherence with frequent monitoring. Studies have demonstrated that individuals receiving oral anticoagulation have significant knowledge deficits about the purpose of anticoagulation.33–35 In cross-sectional studies utilising anticoagulation-specific knowledge scales and questionnaires, patients answered correctly only 48–62 % of questions about anticoagulation.34,35 In a limited-sized (n=183), ethnically-diverse cohort, as few as 9 % of patients knew the indication for being prescribed warfarin, many reporting the indication as hypertension, high cholesterol or “thick blood”.33 Only 40–52 % of patients on anticoagulation therapy had even a basic understanding about the action of anticoagulants23 or the consequences of over- or under-dosing.36 In addition, patients with AF answered correctly <20 % of questions on drug, herbal and vitamin interactions with warfarin.35
Evidence regarding the associations between health literacy and anticoagulation knowledge remains limited. One study demonstrated a strong association between health literacy and anticoagulation knowledge.33 Other studies have used educational level, rather than assessments of health literacy. There is evidence, however, suggesting that improved knowledge is related to better metrics of anticoagulation. A higher knowledge level of both anticoagulation and AF has been associated with greater warfarin time in therapeutic range.37 Similarly, educational interventions have been shown to improve time in therapeutic range. Interventions that have been studied include one-on-one counselling sessions;38 a 20-minute, nurse-led class;39 a 2-hour, interactive, physician-led small-group session;40 educational videos36,37 and visual aids.41 Limitations include small-sized samples and short follow-up duration.
Overall, these interventions demonstrated modest improvement in patient knowledge over 12 months of follow up. Visual aids improved patients’ ability to describe their warfarin regimen.41 Informational videos focused on patient narrative were more effective than presentingstatisticalinformation.36 Asystematicreviewofeducational interventions for anticoagulation therapy in AF42 concluded that the effect on patient outcomes is inconclusive. The data remain limited by small sample sizes, inadequate follow up, absence of standardisation for educational or assessment methods and lack of health literacy assessments.
Multiple gaps remain in the investigation of health literacy and anticoagulation for stroke prevention in AF. The contribution of health literacy towards stroke risk and prevention has not been examined. Patient-centred AF care requires assessments of health literacy alongside adherence to anticoagulation, monitoring and dose adjustment. In addition, we identified no studies examining health literacy in the context of novel oral anticoagulants. In contrast, the EHRA consensus statement on patient values and preferences advocates for assessing health literacy as a starting point in evaluating patients with AF.32 Expectations of sustained adherence to anticoagulation is unrealistic without appropriate education, patient knowledge and expectations and commitment to treatment. Health literacy resides at the centre of such a model of patient-centred care.
Conclusion
Incorporation of health literacy has been identified by the Institute of Medicine as an essential priority to bolster healthcare quality and disease prevention. Health literacy has a fundamental contribution to patient safety, patient-centred care and AF treatment and has additionally emerged as a major barrier to the meaningful participation of patients in shared decision-making. Given the increasingly complicated therapeutic options and treatment decisions that characterise the management of AF, health literacy has a central role in patient experience and outcomes. We have highlighted multiple dimensions for future directions to assess the individual and public health benefits of integrating health literacy with AF management and care.
Footnotes
Disclosure: The authors have no conflict of interest to declare.
References
- 1.Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. National Academy Press; Washington DC: 2001. [PubMed] [Google Scholar]
- 2.Haun JN, Valerio MA, McCormack LA, et al. Health literacy measurement: an inventory and descriptive summary of 51 instruments. J Health Commun. 2014;19(Suppl 2):302–33. doi: 10.1080/10810730.2014.936571. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Education Statistics. The health literacy of America’s adults: results from the 2003. National Assessment of Adult Literacy; [accessed on 18 April 2017]. Available at: http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483. [Google Scholar]
- 4.McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNJ J. 2011;22(2):25–32. [PubMed] [Google Scholar]
- 5.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ and Couns. 2003;51(3):267–75. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 6.Baker DW, Wolf MS, Feinglass J, et al. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503–9. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 7.Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ. 2012;344:e1602. doi: 10.1136/bmj.e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu JR, Holmes GM, DeWalt DA, et al. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med. 2013;28(9):1174–80. doi: 10.1007/s11606-013-2394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305(16):1695–701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.AHRQ Health Literacy Universal Precautions Toolkit. Agency for Healthcare Research and Quality; Rockville, MD: [accessed on 18 April 2017]. http://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/index.html. [Google Scholar]
- 11.Sears SF, Serber ER, Alvarez LG, et al. Understanding atrial symptom reports: objective versus subjective predictors. Pacing Clin Electrophysiol. 2005;28(8):801–7. doi: 10.1111/j.1540-8159.2005.00171.x. [DOI] [PubMed] [Google Scholar]
- 12.Goli NM, Thompson T, Sears SF, et al. Educational attainment is associated with atrial fibrillation symptom severity. Pacing Clin Electrophysiol. 2012;35(9):1090–6. doi: 10.1111/j.1540-8159.2012.03482.x. [DOI] [PubMed] [Google Scholar]
- 13.Macabasco-O’Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26(9):979–86. doi: 10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kincaid JP, Fishburne RP, Rogers RL, Chissom BS. Research Branch Report. 1975. Derivation of new readability formulas (automated readability index, fog count, and Flesch reading ease formula) for navy enlisted personnel; pp. 8–75. Chief of Naval Technical Training: Naval Air Station Memphis. [Google Scholar]
- 15.McLaughlin GH. Smog grading: a new readability formula. Journal of Reading. 1969;12(8):639–46. [Google Scholar]
- 16. [accessed on 21 March 2017];New Dale–Chall readability formula. Available at: www.readabilityformulas.com/new-dale-chall-readability-formula.php.
- 17.MetaMetrics. [Accessed on 21 March 2017];The Lexile Framework for Reading. 2017 Available at: www.lexile.com/
- 18.Weiss BD, Coyne C. Communicating with patients who cannot read. N Engl J Med. 1997;337(4):272–4. doi: 10.1056/NEJM199707243370411. [DOI] [PubMed] [Google Scholar]
- 19.Aliot E, Breithardt G, Brugada J, et al. An international survey of physician and patient understanding, perception, and attitudes to atrial fibrillation and its contribution to cardiovascular disease morbidity and mortality. Europace. 2010;12(5):626–33. doi: 10.1093/europace/euq109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu W, Sun G, Lin Z, et al. Knowledge, attitude, and behavior in patients with atrial fibrillation undergoing radiofrequency catheter ablation. J Interv Card Electrophysiol. 2010;28(3):199–207. doi: 10.1007/s10840-010-9496-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hendriks JM, Crijns HJ, Tieleman RG, Vrijhoef HJ. The atrial fibrillation knowledge scale: development, validation and results. Int J Cardiol. 2013;168(2):1422–8. doi: 10.1016/j.ijcard.2012.12.047. [DOI] [PubMed] [Google Scholar]
- 22.McCabe PJ, Schad S, Hampton A, Holland DE. Knowledge and self-management behaviors of patients with recently detected atrial fibrillation. Heart Lung. 2008;37(2):79–90. doi: 10.1016/j.hrtlng.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Lane DA, Ponsford J, Shelley A, et al. Patient knowledge and perceptions of atrial fibrillation and anticoagulant therapy: effects of an educational intervention programme. The West Birmingham Atrial Fibrillation Project. Int J Cardiol. 2006;110(3):354–8. doi: 10.1016/j.ijcard.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 24.Seaburg L, Hess EP, Coylewright M, et al. Shared decision making in atrial fibrillation: where we are and where we should be going. Circulation. 2014;129(6):704–10. doi: 10.1161/CIRCULATIONAHA.113.004498. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell SE, Gardiner PM, Sadikova E, et al. Patient activation and 30-day post-discharge hospital utilization. J Gen Intern Med. 2014;29(2):349–55. doi: 10.1007/s11606-013-2647-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94(3):291–309. doi: 10.1016/j.pec.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 27.Hendriks JM, de Wit R, Crijns HJ, et al. Nurse-led care vs. usual care for patients with atrial fibrillation: results of a randomized trial of integrated chronic care vs. routine clinical care in ambulatory patients with atrial fibrillation. Eur Heart J. 2012;33(21):2692–9. doi: 10.1093/eurheartj/ehs071. [DOI] [PubMed] [Google Scholar]
- 28.Baker DW, Dewalt DA, Schillinger D, et al. The effect of progressive, reinforcing telephone education and counseling versus brief educational intervention on knowledge, self-care behaviors and heart failure symptoms. J Card Fail. 2011;17(10):789–96. doi: 10.1016/j.cardfail.2011.06.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeWalt DA, Malone RM, Bryant ME, et al. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial. BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothman RL, Malone R, Bryant B, et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med. 2005;118(3):276–84. doi: 10.1016/j.amjmed.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 31.Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ. 2008;336(7642):491–5. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lane DA, Aguinaga L, Blomstrom-Lundqvist C, et al. Cardiac tachyarrhythmias and patient values and preferences for their management: the European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulacion Cardiaca y Electrofisiologia (SOLEACE) Europace. 2015;17(12):1747–69. doi: 10.1093/europace/euv233. [DOI] [PubMed] [Google Scholar]
- 33.Fang MC, Panguluri P, Machtinger EL, Schillinger D. Language, literacy, and characterization of stroke among patients taking warfarin for stroke prevention: implications for health communication. Patient Educ and Couns. 2009;75(3):403–10. doi: 10.1016/j.pec.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rewiuk K, Bednarz S, Faryan P, Grodzicki T. Knowledge of antithrombotic prophylaxis among patients with atrial fibrillation. Cardiol J. 2007;14(1):44–9. [PubMed] [Google Scholar]
- 35.Smith MB, Christensen N, Wang S, et al. Warfarin knowledge in patients with atrial fibrillation: implications for safety, efficacy, and education strategies. Cardiology. 2010;116(1):61–9. doi: 10.1159/000314936. [DOI] [PubMed] [Google Scholar]
- 36.Mazor KM, Baril J, Dugan E, et al. Patient education about anticoagulant medication: is narrative evidence or statistical evidence more effective? Patient Educ and Couns. 2007;69(1–3):145–57. doi: 10.1016/j.pec.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Clarkesmith DE, Pattison HM, Lip GY, Lane DA. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One. 2013;8(9):e74037. doi: 10.1371/journal.pone.0074037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pernod G, Labarere J, Yver J, et al. EDUC’AVK: Reduction of oral anticoagulant-related adverse events after patient education: a prospective multicenter open randomized study. J Gen Intern Med. 2008;23(9):1441–6. doi: 10.1007/s11606-008-0690-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eickhoff JS, Wangen TM, Notch KB, et al. Creating an anticoagulant patient education class. J Vasc Nurs. 2010;28(4):132–5. doi: 10.1016/j.jvn.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Khan TI, Kamali F, Kesteven P, et al. The value of education and self-monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation. Br J Haematol. 2004;126(4):557–64. doi: 10.1111/j.1365-2141.2004.05074.x. [DOI] [PubMed] [Google Scholar]
- 41.Schillinger D, Machtinger EL, Wang F, et al. Language, literacy, and communication regarding medication in an anticoagulation clinic: are pictures better than words? In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology) Rockville, MD: Agency for Healthcare Research and Quality; 2005. [Accessed on 3 March 2017]. Available at: https://www.ncbi.nlm.nih.gov/books/NBK20494/?report=reader#_NBK20494_pubdet_. [PubMed] [Google Scholar]
- 42.Clarkesmith DE, Pattison HM, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database Syst Rev. 2013;6:CD008600. doi: 10.1002/14651858.CD008600.pub2. [DOI] [PubMed] [Google Scholar]
- 43.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 44.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20(10):1727–36. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Badia X, Arribas F, Ormaetxe JM, et al. Development of a questionnaire to measure health-related quality of life (HRQol) in patients with atrial fibrillation (AF-Qol) Health Qual Life Outcomes. 2007;5:37. doi: 10.1186/1477-7525-5-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arribas F, Ormaetxe JM, Peinado R, et al. Validation of the AF-Qol, a disease-specific quality of life questionnaire for patients with atrial fibrillation. Europace. 2010;12(3):364–70. doi: 10.1093/europace/eup421. [DOI] [PubMed] [Google Scholar]
- 48.Spertus J, Dorian P, Bubien R, et al. Development and validation of the atrial fibrillation effect on quality-of-life (AFEQT) questionnaire in patients with atrial fibrillation. Circ Arrhythm Electrophysiol. 2011;4(1):15–25. doi: 10.1161/CIRCEP.110.958033. [DOI] [PubMed] [Google Scholar]
- 49.Koci F, Forbes P, Mansour MC, et al. New classification scheme for atrial fibrillation symptom severity and burden. Am J Cardiol. 2014;114(2):260–5. doi: 10.1016/j.amjcard.2014.04.032. [DOI] [PubMed] [Google Scholar]